User login
More reassuring data on COVID-19 vaccines and pregnancy
Receiving a COVID-19 vaccine early in pregnancy is not associated with an increased risk for spontaneous abortion, new research suggests.
The study, published online in JAMA, evaluated the proportion of women who received the vaccine and had ongoing pregnancies in comparison with those who experienced a miscarriage or spontaneous abortion. The researchers analyzed data from 105,446 unique pregnancies over seven 4-week surveillance periods between December 2020 and June 2021. Ongoing pregnancies between 6 and 19 weeks’ gestation were identified on the last day of each 4-week surveillance period (index date). Spontaneous abortions were assigned to a 4-week surveillance period on the basis of their outcome date. There were 13,160 spontaneous abortions and 92,286 ongoing pregnancies.
Overall, a COVID-19 vaccine was received within 28 days prior to an index date among 8.0% of ongoing pregnancy surveillance periods versus 8.6% of spontaneous abortions.
“We’re hoping that this data can inform the ongoing conversations between providers and pregnant women [about the COVID-19 vaccines],” study author Elyse O. Kharbanda, MD, MPH, senior research investigator at HealthPartners Institute, told this news organization. “It should be considered in the context of all the data that’s coming out both on the risks of COVID infection and pregnancy and data on outcomes among women who are vaccinated and pregnant.”
Among the women whose pregnancies were followed, 7.8% received at least one dose of the Pfizer COVID-19 vaccine, 6% received at least one dose of the Moderna COVID-19 vaccine, and 0.5% received the Janssen vaccine.
In August, the American College of Obstetricians and Gynecologists (ACOG), the Centers for Disease Control and Prevention, and the Society for Maternal-Fetal Medicine strongly recommended that all pregnant women be vaccinated against COVID-19.
The new findings provide reassuring evidence about the safety of COVID vaccines, particularly mRNA vaccines, during pregnancy, said Denise J. Jamieson, MD, MPH, chair of the department of gynecology and obstetrics at Emory University, Atlanta, who was not involved in the study.
“The study design was a carefully conducted case-control study. Although ideally the best design for studying vaccine safety and efficacy is a randomized clinical trial, data are rapidly accumulating from a variety of sources that COVID vaccines are safe in pregnancy,” said Dr. Jamieson, who serves on several ACOG committees.
A version of this article first appeared on Medscape.com.
Receiving a COVID-19 vaccine early in pregnancy is not associated with an increased risk for spontaneous abortion, new research suggests.
The study, published online in JAMA, evaluated the proportion of women who received the vaccine and had ongoing pregnancies in comparison with those who experienced a miscarriage or spontaneous abortion. The researchers analyzed data from 105,446 unique pregnancies over seven 4-week surveillance periods between December 2020 and June 2021. Ongoing pregnancies between 6 and 19 weeks’ gestation were identified on the last day of each 4-week surveillance period (index date). Spontaneous abortions were assigned to a 4-week surveillance period on the basis of their outcome date. There were 13,160 spontaneous abortions and 92,286 ongoing pregnancies.
Overall, a COVID-19 vaccine was received within 28 days prior to an index date among 8.0% of ongoing pregnancy surveillance periods versus 8.6% of spontaneous abortions.
“We’re hoping that this data can inform the ongoing conversations between providers and pregnant women [about the COVID-19 vaccines],” study author Elyse O. Kharbanda, MD, MPH, senior research investigator at HealthPartners Institute, told this news organization. “It should be considered in the context of all the data that’s coming out both on the risks of COVID infection and pregnancy and data on outcomes among women who are vaccinated and pregnant.”
Among the women whose pregnancies were followed, 7.8% received at least one dose of the Pfizer COVID-19 vaccine, 6% received at least one dose of the Moderna COVID-19 vaccine, and 0.5% received the Janssen vaccine.
In August, the American College of Obstetricians and Gynecologists (ACOG), the Centers for Disease Control and Prevention, and the Society for Maternal-Fetal Medicine strongly recommended that all pregnant women be vaccinated against COVID-19.
The new findings provide reassuring evidence about the safety of COVID vaccines, particularly mRNA vaccines, during pregnancy, said Denise J. Jamieson, MD, MPH, chair of the department of gynecology and obstetrics at Emory University, Atlanta, who was not involved in the study.
“The study design was a carefully conducted case-control study. Although ideally the best design for studying vaccine safety and efficacy is a randomized clinical trial, data are rapidly accumulating from a variety of sources that COVID vaccines are safe in pregnancy,” said Dr. Jamieson, who serves on several ACOG committees.
A version of this article first appeared on Medscape.com.
Receiving a COVID-19 vaccine early in pregnancy is not associated with an increased risk for spontaneous abortion, new research suggests.
The study, published online in JAMA, evaluated the proportion of women who received the vaccine and had ongoing pregnancies in comparison with those who experienced a miscarriage or spontaneous abortion. The researchers analyzed data from 105,446 unique pregnancies over seven 4-week surveillance periods between December 2020 and June 2021. Ongoing pregnancies between 6 and 19 weeks’ gestation were identified on the last day of each 4-week surveillance period (index date). Spontaneous abortions were assigned to a 4-week surveillance period on the basis of their outcome date. There were 13,160 spontaneous abortions and 92,286 ongoing pregnancies.
Overall, a COVID-19 vaccine was received within 28 days prior to an index date among 8.0% of ongoing pregnancy surveillance periods versus 8.6% of spontaneous abortions.
“We’re hoping that this data can inform the ongoing conversations between providers and pregnant women [about the COVID-19 vaccines],” study author Elyse O. Kharbanda, MD, MPH, senior research investigator at HealthPartners Institute, told this news organization. “It should be considered in the context of all the data that’s coming out both on the risks of COVID infection and pregnancy and data on outcomes among women who are vaccinated and pregnant.”
Among the women whose pregnancies were followed, 7.8% received at least one dose of the Pfizer COVID-19 vaccine, 6% received at least one dose of the Moderna COVID-19 vaccine, and 0.5% received the Janssen vaccine.
In August, the American College of Obstetricians and Gynecologists (ACOG), the Centers for Disease Control and Prevention, and the Society for Maternal-Fetal Medicine strongly recommended that all pregnant women be vaccinated against COVID-19.
The new findings provide reassuring evidence about the safety of COVID vaccines, particularly mRNA vaccines, during pregnancy, said Denise J. Jamieson, MD, MPH, chair of the department of gynecology and obstetrics at Emory University, Atlanta, who was not involved in the study.
“The study design was a carefully conducted case-control study. Although ideally the best design for studying vaccine safety and efficacy is a randomized clinical trial, data are rapidly accumulating from a variety of sources that COVID vaccines are safe in pregnancy,” said Dr. Jamieson, who serves on several ACOG committees.
A version of this article first appeared on Medscape.com.
To scan or not to scan: Routine ultrasonography is not necessary after medication management of early pregnancy loss
CASE Patient finds that follow-up ultrasonography is burdensome
Ms. MB presents to the clinic for dating ultrasonography and is diagnosed with a missed abortion measuring 7 weeks. After reviewing her management options, she elects for medication management. She receives mifepristone 200 mg and misoprostol 800 µg, with a plan to follow-up in clinic for repeat ultrasonography in a week. The day of her follow-up appointment, there is a large snowstorm. She calls her care team to ask if she needs to have a follow-up visit, as she is certain she has passed tissue and her bleeding is now minimal. She is told, however, that a follow-up ultrasonography is required, per clinic policy, to ensure successful management. Despite Ms. MB’s grief and the difficult travel conditions, she makes the arduous journey back to the clinic to complete the ultrasound.
Do all patients need an ultrasound after medication management of early pregnancy loss? Or is there an alternative follow-up option?
Early pregnancy loss (EPL) is a common pregnancy complication, and its management is a routine part of reproductive health care. In the clinically stable patient, EPL may be managed expectantly, surgically, or medically, based on the patient’s preference. For patients who select medication management, clear evidence supports that a combination regimen of mifepristone and misoprostol is more effective than treatment with misoprostol alone.1,2 The data suggest that 91% of patients will experience expulsion of the gestational sac by 30 days with medication management.1 Because a minority of patients will have a retained gestational sac despite medication therapy, follow-up ensures complete expulsion of pregnancy tissue.
In the United States, most follow-up protocols include an ultrasound examination, which often entails transvaginal ultrasonography. Returning to clinic for an additional ultrasound may be costly and inconvenient—and during a global pandemic medically risky. Further, it may undermine a fundamental principle in management of EPL: autonomy. Many patients who select medication management do so out of a desire to minimize interventions or procedures. Follow-up protocols that align with patient preferences for fewer interventions are critically important to the provision of patient-centered care. Additionally, the COVID-19 pandemic highlights the value of offering an alternative follow-up strategy that minimizes the need for additional visits to a clinic or hospital.
Lessons from medication abortion management
In many ways, follow-up after medication management of EPL is analogous to follow-up after medication abortion. In both cases, the goal of follow-up is to ensure that complete expulsion has occurred without complication and to identify patients with incomplete expulsion of pregnancy tissue who may benefit from further treatment with additional medication or uterine aspiration. A key difference in the management of EPL is that there is no concern for ongoing pregnancy.
Historically, follow-up transvaginal ultrasonography was routinely performed after medication abortion to ensure complete expulsion of pregnancy.3 However, requiring patients to return to a health care facility for ultrasonography after abortion can be burdensome, both for patients and clinicians. To provide more accessible, patient-centered care, researchers have investigated alternative follow-up strategies for medication abortion that remove the necessity for ultrasonography. Guidelines from both the National Abortion Federation and the American College of Obstetricians and Gynecologists state that routine ultrasonography is not necessary after medication abortion.4,5
Quantitative serum human chorionic gonadotropin (hCG) testing before treatment and at a follow-up visit is one reasonable strategy to ensure successful treatment. In one study of medication abortion patients, an 80% decrease in serum hCG was predictive of complete expulsion in 98.5% of patients.6 While this strategy avoids ultrasonography, it still necessitates a visit to a health care facility for a blood draw. As an alternative, substantial evidence now demonstrates the safety and feasibility of using a combination of clinical symptoms and urine pregnancy testing to confirm completed medication abortion. The evidence for follow-up using a combination of clinical symptoms and urine pregnancy testing is discussed below.
Continue to: Symptoms...
Symptoms. An assessment of symptoms alone, by the patient or clinician, is an important indicator of treatment success and can be completed easily via telephone. In one study of medication abortion with mifepristone and misoprostol, patients correctly predicted passage of a gestational sac 85% of the time based on symptoms alone.7 In another study, the combined clinical assessment from the patient and the clinician had a sensitivity of 96% and a specificity of 67% for predicting complete pregnancy expulsion.8 Finally, in an analysis of 931 patients after medication abortion, when both the patient and clinician believed that the gestational sac had passed, ultrasonography demonstrated complete expulsion 99% of the time.9
Urine pregnancy testing. Several studies have demonstrated that the addition of urine pregnancy testing to a clinical assessment of symptoms is a safe and effective follow-up strategy in medication abortion. Contemporary over-the-counter pregnancy tests are high-sensitivity tests that have an hCG detection threshold of 25 to 50 mIU/mL. As these tests are widely and commercially available in the United States, they can be a useful tool in follow-up strategies.
In a study by Chen and colleagues, patients seeking medication abortion were offered a choice of follow-up with ultrasonography at 1 week versus a combination of a 1-week phone call and a 4-week high-sensitivity urine pregnancy test. In this study, approximately 40% of patients opted for phone follow-up. The rates of incomplete abortion and loss to follow-up were similar between the 2 groups, highlighting the significant number of individuals interested in alternative models of follow-up and the efficacy of phone and urine testing specifically.10
In another study that evaluated the feasibility of a telephone and urine testing follow-up strategy, 97% of patients completed follow-up and all continuing pregnancies were diagnosed prior to the 4-week urine pregnancy test.8
In a hospital in Edinburgh, where a telephone-based symptom assessment in combination with a 2-week low-sensitivity pregnancy test (hCG detection threshold of 2,000 mIU/mL; not commercially available in the United States) is the standard of care for medication abortion follow-up, Michie and Cameron reported a sensitivity of 100% and a specificity of 88% to detect ongoing pregnancies.11
Taken together, these data demonstrate that a combination of symptom assessment via telephone and home urine pregnancy testing (in addition to standard patient instructions and return precautions) is an appropriate strategy for medication abortion follow-up, and they suggest that similar strategies can be employed in the medication management of EPL.
To scan or not to scan?
Many published studies of EPL have used ultrasonography to confirm complete expulsion of pregnancy tissue; however, others have relied on either clinical evaluation or urine pregnancy testing to determine treatment success, using ultrasonography only as clinically indicated.12-14 In their evaluation of medication management versus surgical management of miscarriage, Niinimäki and colleagues performed urine hCG testing at a 5- to 6-week follow-up visit to determine treatment success; ultrasonography was obtained only if the urine hCG test was positive. They demonstrated a treatment success rate of 90% with mifepristone and misoprostol treatment,12 congruent with previously published results.
While a follow-up ultrasound scan may be helpful to accurately assess treatment efficacy in research protocols, it should not be considered necessary in clinical practice. Posttreatment imaging in an asymptomatic patient may place additional burden on the patient and health care system and may result in unnecessary intervention. Although treatment success is reliably defined by the absence of a gestational sac,15,16 the finding of a thickened endometrium or presence of vascularity may result in the patient receiving an unnecessary aspiration or other intervention.
The evidence from the medication abortion literature suggests that a combination of a 1-week telephone call to assess patient symptoms in addition to a 4-week high-sensitivity pregnancy test is a reasonable alternative follow-up strategy. A similar strategy is already used in the United Kingdom, where current National Institute for Health and Care Excellence guidelines for follow-up after medication management of EPL recommend home pregnancy testing in 3 weeks unless the patient experiences worsening pain or bleeding symptoms.17
Time to rethink follow-up care
Follow-up care for EPL should be provided in a way that is sensitive to the needs and preferences of the patient and, if desired, minimizes additional health care visits, testing, or procedures. While some patients may prefer ultrasonography follow-up, it is important for the clinician to recognize that there are safe and effective alternatives. Patient preference guides the choice of EPL management; this logic extends to follow-up strategies. As we strive to provide evidence-based, patient-centered EPL care, there is no need for universal follow-up ultrasonography. ●
- Schreiber CA, Creinin MD, Atrio J, et al. Mifepristone pretreatment for the medical management of early pregnancy loss. N Engl J Med. 2018;378:2161-2170.
- Chu JJ, Devall AJ, Beeson LF, et al. Mifepristone and misoprostol versus misoprostol alone for the management of missed miscarriage (MifeMiso): a randomised, double-blind, placebo-controlled trial. Lancet. 2020;396:770-778.
- Benson J, Clark KA, Gerhardt A, et al. Early abortion services in the United States: a provider survey. Contraception. 2003;67:287-294.
- Medication abortion up to 70 days of gestation: ACOG practice bulletin summary, No. 225. Obstet Gynecol. 2020;136:855-858.
- National Abortion Federation. 2020 Clinical Policy Guidelines for Abortion Care. Washington, DC; 2020. https://5aa1b2xfmfh2e2mk03kk8rsx-wpengine.netdna -ssl.com/wp-content/uploads/2020_CPGs.pdf. Accessed July 19, 2021.
- Fiala C, Safar P, Bygdeman M, et al. Verifying the effectiveness of medical abortion; ultrasound versus hCG testing. Eur J Obstet Gynecol Reprod Biol. 2003;109:190-195.
- Pymar HC, Creinin MD, Schwartz JL. Mifepristone followed on the same day by vaginal misoprostol for early abortion. Contraception. 2001;64:87-92.
- Perriera LK, Reeves MF, Chen BA, et al. Feasibility of telephone follow-up after medical abortion. Contraception. 2010;81:143-149.
- Rossi B, Creinin MD, Meyn LA. Ability of the clinician and patient to predict the outcome of mifepristone and misoprostol medical abortion. Contraception. 2004;70:313-317.
- Chen MJ, Rounds KM, Creinin MD, et al. Comparing office and telephone follow-up after medical abortion. Contraception. 2016;94:122-126.
- Michie L, Cameron ST. Simplified follow-up after early medical abortion: 12-month experience of a telephone call and self-performed low-sensitivity urine pregnancy test. Contraception. 2014;89:440-445.
- Niinimäki M, Jouppila P, Martikainen H, et al. A randomized study comparing efficacy and patient satisfaction in medical or surgical treatment of miscarriage. Fertil Steril. 2006;86:367- 372.
- Weeks A, Alia G, Blum J, et al. A randomized trial of misoprostol compared with manual vacuum aspiration for incomplete abortion. Obstet Gynecol. 2005;106:540-547.
- Wood SL, Brain PH. Medical management of missed abortion: a randomized clinical trial. Obstet Gynecol. 2002;99:563-566.
- Reeves MF, Lohr PA, Harwood B, et al. Ultrasonographic endometrial thickness after medical and surgical management of early pregnancy failure. Obstet Gynecol. 2008;111:106-112.
- Reeves MF, Fox MC, Lohr PA, et al. Endometrial thickness following medical abortion is not predictive of subsequent surgical intervention. Ultrasound Obstet Gynecol. 2009;34:104-109.
- National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. NICE guideline NG126. April 17, 2019. ttps:// www.nice.org.uk/guidance/ng126/chapter/Recommen dations#management-of-miscarriage. Accessed July 19, 2021.
CASE Patient finds that follow-up ultrasonography is burdensome
Ms. MB presents to the clinic for dating ultrasonography and is diagnosed with a missed abortion measuring 7 weeks. After reviewing her management options, she elects for medication management. She receives mifepristone 200 mg and misoprostol 800 µg, with a plan to follow-up in clinic for repeat ultrasonography in a week. The day of her follow-up appointment, there is a large snowstorm. She calls her care team to ask if she needs to have a follow-up visit, as she is certain she has passed tissue and her bleeding is now minimal. She is told, however, that a follow-up ultrasonography is required, per clinic policy, to ensure successful management. Despite Ms. MB’s grief and the difficult travel conditions, she makes the arduous journey back to the clinic to complete the ultrasound.
Do all patients need an ultrasound after medication management of early pregnancy loss? Or is there an alternative follow-up option?
Early pregnancy loss (EPL) is a common pregnancy complication, and its management is a routine part of reproductive health care. In the clinically stable patient, EPL may be managed expectantly, surgically, or medically, based on the patient’s preference. For patients who select medication management, clear evidence supports that a combination regimen of mifepristone and misoprostol is more effective than treatment with misoprostol alone.1,2 The data suggest that 91% of patients will experience expulsion of the gestational sac by 30 days with medication management.1 Because a minority of patients will have a retained gestational sac despite medication therapy, follow-up ensures complete expulsion of pregnancy tissue.
In the United States, most follow-up protocols include an ultrasound examination, which often entails transvaginal ultrasonography. Returning to clinic for an additional ultrasound may be costly and inconvenient—and during a global pandemic medically risky. Further, it may undermine a fundamental principle in management of EPL: autonomy. Many patients who select medication management do so out of a desire to minimize interventions or procedures. Follow-up protocols that align with patient preferences for fewer interventions are critically important to the provision of patient-centered care. Additionally, the COVID-19 pandemic highlights the value of offering an alternative follow-up strategy that minimizes the need for additional visits to a clinic or hospital.
Lessons from medication abortion management
In many ways, follow-up after medication management of EPL is analogous to follow-up after medication abortion. In both cases, the goal of follow-up is to ensure that complete expulsion has occurred without complication and to identify patients with incomplete expulsion of pregnancy tissue who may benefit from further treatment with additional medication or uterine aspiration. A key difference in the management of EPL is that there is no concern for ongoing pregnancy.
Historically, follow-up transvaginal ultrasonography was routinely performed after medication abortion to ensure complete expulsion of pregnancy.3 However, requiring patients to return to a health care facility for ultrasonography after abortion can be burdensome, both for patients and clinicians. To provide more accessible, patient-centered care, researchers have investigated alternative follow-up strategies for medication abortion that remove the necessity for ultrasonography. Guidelines from both the National Abortion Federation and the American College of Obstetricians and Gynecologists state that routine ultrasonography is not necessary after medication abortion.4,5
Quantitative serum human chorionic gonadotropin (hCG) testing before treatment and at a follow-up visit is one reasonable strategy to ensure successful treatment. In one study of medication abortion patients, an 80% decrease in serum hCG was predictive of complete expulsion in 98.5% of patients.6 While this strategy avoids ultrasonography, it still necessitates a visit to a health care facility for a blood draw. As an alternative, substantial evidence now demonstrates the safety and feasibility of using a combination of clinical symptoms and urine pregnancy testing to confirm completed medication abortion. The evidence for follow-up using a combination of clinical symptoms and urine pregnancy testing is discussed below.
Continue to: Symptoms...
Symptoms. An assessment of symptoms alone, by the patient or clinician, is an important indicator of treatment success and can be completed easily via telephone. In one study of medication abortion with mifepristone and misoprostol, patients correctly predicted passage of a gestational sac 85% of the time based on symptoms alone.7 In another study, the combined clinical assessment from the patient and the clinician had a sensitivity of 96% and a specificity of 67% for predicting complete pregnancy expulsion.8 Finally, in an analysis of 931 patients after medication abortion, when both the patient and clinician believed that the gestational sac had passed, ultrasonography demonstrated complete expulsion 99% of the time.9
Urine pregnancy testing. Several studies have demonstrated that the addition of urine pregnancy testing to a clinical assessment of symptoms is a safe and effective follow-up strategy in medication abortion. Contemporary over-the-counter pregnancy tests are high-sensitivity tests that have an hCG detection threshold of 25 to 50 mIU/mL. As these tests are widely and commercially available in the United States, they can be a useful tool in follow-up strategies.
In a study by Chen and colleagues, patients seeking medication abortion were offered a choice of follow-up with ultrasonography at 1 week versus a combination of a 1-week phone call and a 4-week high-sensitivity urine pregnancy test. In this study, approximately 40% of patients opted for phone follow-up. The rates of incomplete abortion and loss to follow-up were similar between the 2 groups, highlighting the significant number of individuals interested in alternative models of follow-up and the efficacy of phone and urine testing specifically.10
In another study that evaluated the feasibility of a telephone and urine testing follow-up strategy, 97% of patients completed follow-up and all continuing pregnancies were diagnosed prior to the 4-week urine pregnancy test.8
In a hospital in Edinburgh, where a telephone-based symptom assessment in combination with a 2-week low-sensitivity pregnancy test (hCG detection threshold of 2,000 mIU/mL; not commercially available in the United States) is the standard of care for medication abortion follow-up, Michie and Cameron reported a sensitivity of 100% and a specificity of 88% to detect ongoing pregnancies.11
Taken together, these data demonstrate that a combination of symptom assessment via telephone and home urine pregnancy testing (in addition to standard patient instructions and return precautions) is an appropriate strategy for medication abortion follow-up, and they suggest that similar strategies can be employed in the medication management of EPL.
To scan or not to scan?
Many published studies of EPL have used ultrasonography to confirm complete expulsion of pregnancy tissue; however, others have relied on either clinical evaluation or urine pregnancy testing to determine treatment success, using ultrasonography only as clinically indicated.12-14 In their evaluation of medication management versus surgical management of miscarriage, Niinimäki and colleagues performed urine hCG testing at a 5- to 6-week follow-up visit to determine treatment success; ultrasonography was obtained only if the urine hCG test was positive. They demonstrated a treatment success rate of 90% with mifepristone and misoprostol treatment,12 congruent with previously published results.
While a follow-up ultrasound scan may be helpful to accurately assess treatment efficacy in research protocols, it should not be considered necessary in clinical practice. Posttreatment imaging in an asymptomatic patient may place additional burden on the patient and health care system and may result in unnecessary intervention. Although treatment success is reliably defined by the absence of a gestational sac,15,16 the finding of a thickened endometrium or presence of vascularity may result in the patient receiving an unnecessary aspiration or other intervention.
The evidence from the medication abortion literature suggests that a combination of a 1-week telephone call to assess patient symptoms in addition to a 4-week high-sensitivity pregnancy test is a reasonable alternative follow-up strategy. A similar strategy is already used in the United Kingdom, where current National Institute for Health and Care Excellence guidelines for follow-up after medication management of EPL recommend home pregnancy testing in 3 weeks unless the patient experiences worsening pain or bleeding symptoms.17
Time to rethink follow-up care
Follow-up care for EPL should be provided in a way that is sensitive to the needs and preferences of the patient and, if desired, minimizes additional health care visits, testing, or procedures. While some patients may prefer ultrasonography follow-up, it is important for the clinician to recognize that there are safe and effective alternatives. Patient preference guides the choice of EPL management; this logic extends to follow-up strategies. As we strive to provide evidence-based, patient-centered EPL care, there is no need for universal follow-up ultrasonography. ●
CASE Patient finds that follow-up ultrasonography is burdensome
Ms. MB presents to the clinic for dating ultrasonography and is diagnosed with a missed abortion measuring 7 weeks. After reviewing her management options, she elects for medication management. She receives mifepristone 200 mg and misoprostol 800 µg, with a plan to follow-up in clinic for repeat ultrasonography in a week. The day of her follow-up appointment, there is a large snowstorm. She calls her care team to ask if she needs to have a follow-up visit, as she is certain she has passed tissue and her bleeding is now minimal. She is told, however, that a follow-up ultrasonography is required, per clinic policy, to ensure successful management. Despite Ms. MB’s grief and the difficult travel conditions, she makes the arduous journey back to the clinic to complete the ultrasound.
Do all patients need an ultrasound after medication management of early pregnancy loss? Or is there an alternative follow-up option?
Early pregnancy loss (EPL) is a common pregnancy complication, and its management is a routine part of reproductive health care. In the clinically stable patient, EPL may be managed expectantly, surgically, or medically, based on the patient’s preference. For patients who select medication management, clear evidence supports that a combination regimen of mifepristone and misoprostol is more effective than treatment with misoprostol alone.1,2 The data suggest that 91% of patients will experience expulsion of the gestational sac by 30 days with medication management.1 Because a minority of patients will have a retained gestational sac despite medication therapy, follow-up ensures complete expulsion of pregnancy tissue.
In the United States, most follow-up protocols include an ultrasound examination, which often entails transvaginal ultrasonography. Returning to clinic for an additional ultrasound may be costly and inconvenient—and during a global pandemic medically risky. Further, it may undermine a fundamental principle in management of EPL: autonomy. Many patients who select medication management do so out of a desire to minimize interventions or procedures. Follow-up protocols that align with patient preferences for fewer interventions are critically important to the provision of patient-centered care. Additionally, the COVID-19 pandemic highlights the value of offering an alternative follow-up strategy that minimizes the need for additional visits to a clinic or hospital.
Lessons from medication abortion management
In many ways, follow-up after medication management of EPL is analogous to follow-up after medication abortion. In both cases, the goal of follow-up is to ensure that complete expulsion has occurred without complication and to identify patients with incomplete expulsion of pregnancy tissue who may benefit from further treatment with additional medication or uterine aspiration. A key difference in the management of EPL is that there is no concern for ongoing pregnancy.
Historically, follow-up transvaginal ultrasonography was routinely performed after medication abortion to ensure complete expulsion of pregnancy.3 However, requiring patients to return to a health care facility for ultrasonography after abortion can be burdensome, both for patients and clinicians. To provide more accessible, patient-centered care, researchers have investigated alternative follow-up strategies for medication abortion that remove the necessity for ultrasonography. Guidelines from both the National Abortion Federation and the American College of Obstetricians and Gynecologists state that routine ultrasonography is not necessary after medication abortion.4,5
Quantitative serum human chorionic gonadotropin (hCG) testing before treatment and at a follow-up visit is one reasonable strategy to ensure successful treatment. In one study of medication abortion patients, an 80% decrease in serum hCG was predictive of complete expulsion in 98.5% of patients.6 While this strategy avoids ultrasonography, it still necessitates a visit to a health care facility for a blood draw. As an alternative, substantial evidence now demonstrates the safety and feasibility of using a combination of clinical symptoms and urine pregnancy testing to confirm completed medication abortion. The evidence for follow-up using a combination of clinical symptoms and urine pregnancy testing is discussed below.
Continue to: Symptoms...
Symptoms. An assessment of symptoms alone, by the patient or clinician, is an important indicator of treatment success and can be completed easily via telephone. In one study of medication abortion with mifepristone and misoprostol, patients correctly predicted passage of a gestational sac 85% of the time based on symptoms alone.7 In another study, the combined clinical assessment from the patient and the clinician had a sensitivity of 96% and a specificity of 67% for predicting complete pregnancy expulsion.8 Finally, in an analysis of 931 patients after medication abortion, when both the patient and clinician believed that the gestational sac had passed, ultrasonography demonstrated complete expulsion 99% of the time.9
Urine pregnancy testing. Several studies have demonstrated that the addition of urine pregnancy testing to a clinical assessment of symptoms is a safe and effective follow-up strategy in medication abortion. Contemporary over-the-counter pregnancy tests are high-sensitivity tests that have an hCG detection threshold of 25 to 50 mIU/mL. As these tests are widely and commercially available in the United States, they can be a useful tool in follow-up strategies.
In a study by Chen and colleagues, patients seeking medication abortion were offered a choice of follow-up with ultrasonography at 1 week versus a combination of a 1-week phone call and a 4-week high-sensitivity urine pregnancy test. In this study, approximately 40% of patients opted for phone follow-up. The rates of incomplete abortion and loss to follow-up were similar between the 2 groups, highlighting the significant number of individuals interested in alternative models of follow-up and the efficacy of phone and urine testing specifically.10
In another study that evaluated the feasibility of a telephone and urine testing follow-up strategy, 97% of patients completed follow-up and all continuing pregnancies were diagnosed prior to the 4-week urine pregnancy test.8
In a hospital in Edinburgh, where a telephone-based symptom assessment in combination with a 2-week low-sensitivity pregnancy test (hCG detection threshold of 2,000 mIU/mL; not commercially available in the United States) is the standard of care for medication abortion follow-up, Michie and Cameron reported a sensitivity of 100% and a specificity of 88% to detect ongoing pregnancies.11
Taken together, these data demonstrate that a combination of symptom assessment via telephone and home urine pregnancy testing (in addition to standard patient instructions and return precautions) is an appropriate strategy for medication abortion follow-up, and they suggest that similar strategies can be employed in the medication management of EPL.
To scan or not to scan?
Many published studies of EPL have used ultrasonography to confirm complete expulsion of pregnancy tissue; however, others have relied on either clinical evaluation or urine pregnancy testing to determine treatment success, using ultrasonography only as clinically indicated.12-14 In their evaluation of medication management versus surgical management of miscarriage, Niinimäki and colleagues performed urine hCG testing at a 5- to 6-week follow-up visit to determine treatment success; ultrasonography was obtained only if the urine hCG test was positive. They demonstrated a treatment success rate of 90% with mifepristone and misoprostol treatment,12 congruent with previously published results.
While a follow-up ultrasound scan may be helpful to accurately assess treatment efficacy in research protocols, it should not be considered necessary in clinical practice. Posttreatment imaging in an asymptomatic patient may place additional burden on the patient and health care system and may result in unnecessary intervention. Although treatment success is reliably defined by the absence of a gestational sac,15,16 the finding of a thickened endometrium or presence of vascularity may result in the patient receiving an unnecessary aspiration or other intervention.
The evidence from the medication abortion literature suggests that a combination of a 1-week telephone call to assess patient symptoms in addition to a 4-week high-sensitivity pregnancy test is a reasonable alternative follow-up strategy. A similar strategy is already used in the United Kingdom, where current National Institute for Health and Care Excellence guidelines for follow-up after medication management of EPL recommend home pregnancy testing in 3 weeks unless the patient experiences worsening pain or bleeding symptoms.17
Time to rethink follow-up care
Follow-up care for EPL should be provided in a way that is sensitive to the needs and preferences of the patient and, if desired, minimizes additional health care visits, testing, or procedures. While some patients may prefer ultrasonography follow-up, it is important for the clinician to recognize that there are safe and effective alternatives. Patient preference guides the choice of EPL management; this logic extends to follow-up strategies. As we strive to provide evidence-based, patient-centered EPL care, there is no need for universal follow-up ultrasonography. ●
- Schreiber CA, Creinin MD, Atrio J, et al. Mifepristone pretreatment for the medical management of early pregnancy loss. N Engl J Med. 2018;378:2161-2170.
- Chu JJ, Devall AJ, Beeson LF, et al. Mifepristone and misoprostol versus misoprostol alone for the management of missed miscarriage (MifeMiso): a randomised, double-blind, placebo-controlled trial. Lancet. 2020;396:770-778.
- Benson J, Clark KA, Gerhardt A, et al. Early abortion services in the United States: a provider survey. Contraception. 2003;67:287-294.
- Medication abortion up to 70 days of gestation: ACOG practice bulletin summary, No. 225. Obstet Gynecol. 2020;136:855-858.
- National Abortion Federation. 2020 Clinical Policy Guidelines for Abortion Care. Washington, DC; 2020. https://5aa1b2xfmfh2e2mk03kk8rsx-wpengine.netdna -ssl.com/wp-content/uploads/2020_CPGs.pdf. Accessed July 19, 2021.
- Fiala C, Safar P, Bygdeman M, et al. Verifying the effectiveness of medical abortion; ultrasound versus hCG testing. Eur J Obstet Gynecol Reprod Biol. 2003;109:190-195.
- Pymar HC, Creinin MD, Schwartz JL. Mifepristone followed on the same day by vaginal misoprostol for early abortion. Contraception. 2001;64:87-92.
- Perriera LK, Reeves MF, Chen BA, et al. Feasibility of telephone follow-up after medical abortion. Contraception. 2010;81:143-149.
- Rossi B, Creinin MD, Meyn LA. Ability of the clinician and patient to predict the outcome of mifepristone and misoprostol medical abortion. Contraception. 2004;70:313-317.
- Chen MJ, Rounds KM, Creinin MD, et al. Comparing office and telephone follow-up after medical abortion. Contraception. 2016;94:122-126.
- Michie L, Cameron ST. Simplified follow-up after early medical abortion: 12-month experience of a telephone call and self-performed low-sensitivity urine pregnancy test. Contraception. 2014;89:440-445.
- Niinimäki M, Jouppila P, Martikainen H, et al. A randomized study comparing efficacy and patient satisfaction in medical or surgical treatment of miscarriage. Fertil Steril. 2006;86:367- 372.
- Weeks A, Alia G, Blum J, et al. A randomized trial of misoprostol compared with manual vacuum aspiration for incomplete abortion. Obstet Gynecol. 2005;106:540-547.
- Wood SL, Brain PH. Medical management of missed abortion: a randomized clinical trial. Obstet Gynecol. 2002;99:563-566.
- Reeves MF, Lohr PA, Harwood B, et al. Ultrasonographic endometrial thickness after medical and surgical management of early pregnancy failure. Obstet Gynecol. 2008;111:106-112.
- Reeves MF, Fox MC, Lohr PA, et al. Endometrial thickness following medical abortion is not predictive of subsequent surgical intervention. Ultrasound Obstet Gynecol. 2009;34:104-109.
- National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. NICE guideline NG126. April 17, 2019. ttps:// www.nice.org.uk/guidance/ng126/chapter/Recommen dations#management-of-miscarriage. Accessed July 19, 2021.
- Schreiber CA, Creinin MD, Atrio J, et al. Mifepristone pretreatment for the medical management of early pregnancy loss. N Engl J Med. 2018;378:2161-2170.
- Chu JJ, Devall AJ, Beeson LF, et al. Mifepristone and misoprostol versus misoprostol alone for the management of missed miscarriage (MifeMiso): a randomised, double-blind, placebo-controlled trial. Lancet. 2020;396:770-778.
- Benson J, Clark KA, Gerhardt A, et al. Early abortion services in the United States: a provider survey. Contraception. 2003;67:287-294.
- Medication abortion up to 70 days of gestation: ACOG practice bulletin summary, No. 225. Obstet Gynecol. 2020;136:855-858.
- National Abortion Federation. 2020 Clinical Policy Guidelines for Abortion Care. Washington, DC; 2020. https://5aa1b2xfmfh2e2mk03kk8rsx-wpengine.netdna -ssl.com/wp-content/uploads/2020_CPGs.pdf. Accessed July 19, 2021.
- Fiala C, Safar P, Bygdeman M, et al. Verifying the effectiveness of medical abortion; ultrasound versus hCG testing. Eur J Obstet Gynecol Reprod Biol. 2003;109:190-195.
- Pymar HC, Creinin MD, Schwartz JL. Mifepristone followed on the same day by vaginal misoprostol for early abortion. Contraception. 2001;64:87-92.
- Perriera LK, Reeves MF, Chen BA, et al. Feasibility of telephone follow-up after medical abortion. Contraception. 2010;81:143-149.
- Rossi B, Creinin MD, Meyn LA. Ability of the clinician and patient to predict the outcome of mifepristone and misoprostol medical abortion. Contraception. 2004;70:313-317.
- Chen MJ, Rounds KM, Creinin MD, et al. Comparing office and telephone follow-up after medical abortion. Contraception. 2016;94:122-126.
- Michie L, Cameron ST. Simplified follow-up after early medical abortion: 12-month experience of a telephone call and self-performed low-sensitivity urine pregnancy test. Contraception. 2014;89:440-445.
- Niinimäki M, Jouppila P, Martikainen H, et al. A randomized study comparing efficacy and patient satisfaction in medical or surgical treatment of miscarriage. Fertil Steril. 2006;86:367- 372.
- Weeks A, Alia G, Blum J, et al. A randomized trial of misoprostol compared with manual vacuum aspiration for incomplete abortion. Obstet Gynecol. 2005;106:540-547.
- Wood SL, Brain PH. Medical management of missed abortion: a randomized clinical trial. Obstet Gynecol. 2002;99:563-566.
- Reeves MF, Lohr PA, Harwood B, et al. Ultrasonographic endometrial thickness after medical and surgical management of early pregnancy failure. Obstet Gynecol. 2008;111:106-112.
- Reeves MF, Fox MC, Lohr PA, et al. Endometrial thickness following medical abortion is not predictive of subsequent surgical intervention. Ultrasound Obstet Gynecol. 2009;34:104-109.
- National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. NICE guideline NG126. April 17, 2019. ttps:// www.nice.org.uk/guidance/ng126/chapter/Recommen dations#management-of-miscarriage. Accessed July 19, 2021.
Supreme Court Case: Dobbs v Jackson Women’s Health Organization: What you need to know
This fall, the Supreme Court of the United States (SCOTUS) will announce when they will hear oral arguments for Dobbs v Jackson Women’s Health Organization. The court will examine a Mississippi law, known as the “Gestational Age Act,” originally passed in 2018, that sought to “limit abortions to fifteen weeks’ gestation except in a medical emergency or in cases of severe fetal abnormality.”1 This sets the stage for SCOTUS to make a major ruling on abortion, one which could affirm or upend landmark decisions and nearly 50 years of abortion legislative precedent. Additionally, SCOTUS’ recent decision to not intervene on Texas’ Senate Bill 8 (SB8), which essentially bans all abortions after 6 weeks’ gestational age, may foreshadow how this case will be decided. The current abortion restrictions in Texas and the implications of SB8 will be discussed in a forthcoming column.
SCOTUS and abortion rights
The decision to hear this case comes on the heels of another recent decision regarding a Louisiana law in June Medical Services v Russo. This case examined Louisiana Act 620, which would have required physicians to have hospital admitting privileges within 30 miles of where they provide abortion services.2 The law was deemed constitutionally invalid, with the majority noting the law would have drastically burdened a woman’s right to access abortion services. The Court ruled similarly in 2016 in Whole Women’s Health (WWH) v Hellerstedt, in which WWH challenged Texas House Bill 2, a nearly identical law requiring admitting privileges for abortion care providers. In both of these cases, SCOTUS pointed to precedent set by Southeastern Pennsylvania v Casey, which established that it is unconstitutional for a state to create an “undue burden” on a woman’s right to abortion prior to fetal viability.3 The precedent to this, Roe v Wade, and 5 decades of abortion legislation set may be upended by a SCOTUS decision this next term.
Dobbs v Jackson
On March 19, 2018, Mississippi enacted the “Gestational Age Act” into law. The newly enacted law would limit abortions to 15 weeks’ gestation except in a medical emergency or in cases of severe fetal anomalies. Jackson Women’s Health Organization, the only licensed abortion provider in the state, challenged the constitutionality of the law with legal support from Center for Reproductive Rights (CRR). The US District Court for the Southern District of Mississippi granted summary judgement in favor of the clinic and placed an injunction on the law’s enforcement. The state appealed to the Fifth Circuit Court of Appeals, which upheld the district court decision in a 3-0 decision in November 2019. Mississippi appealed to the Supreme Court, with their petition focusing on multiple questions from the appeals process. After repeatedly rescheduling the case, and multiple reviews in conference, SCOTUS agreed to hear the case. Most recently, the state has narrowed its argument, changing course, and attacking Roe v Wade directly. In a brief submitted in July 2021, the state argues the court should hold that all pre-viability prohibitions on elective abortions are constitutional.
Interestingly, during this time the Mississippi legislature also passed a law, House Bill 2116, also known as the “fetal heartbeat bill,” banning abortion with gestational ages after detection of a fetal heartbeat. This was also challenged, deemed unconstitutional, and affirmed on appeal by the Fifth US Circuit Court.
While recent challenges have focused on the “undue burden” state laws placed on those trying to access abortion care, this case will bring the issue of “viability” and gestational age limits to the forefront.4,5 In addition to Roe v Wade, the Court will have the opportunity to reexamine other relevant precedent, such as Southeastern Pennsylvania v Casey, in considering the most recent arguments of the state. In this most recent brief, the state argues that the Court should, “reject viability as a barrier to prohibiting elective abortions” and that a “viability rule has no constitutional basis.” The state goes on to argue the “Constitution does not protect a right to abortion or limit States’ authority to restrict it.”6 The language and tone in this brief are more direct and aggressive than the states’ petition submitted last June.
However, the composition of the Court is different than in the past. This case will be argued with Justice Amy Coney Barrett seated in place of Justice Ruth Bader Ginsburg, who was a strong advocate for women’s rights.7 She joins Justices Neil Gorsuch and Brett Kavanaugh, also appointed by President Donald Trump and widely viewed as conservative judges, tipping the scales to a more conservative Supreme Court. This case will also be argued in a polarized political environment.8,9 Given the conservative Supreme Court in the setting of an increasingly politically charged environment, reproductive right advocates are understandably worried that members of the anti-abortion movement view this as an opportunity to weaken or remove federal constitutional protections for abortion.
Continue to: Potential outcome of Dobbs v Jackson...
Potential outcome of Dobbs v Jackson
Should SCOTUS choose to rule in favor of Mississippi, it could severely weaken, or even overturn Roe v Wade. This would leave a legal path for states with pre-Roe abortion bans and currently unenforced post-Roe bans to take effect. These “trigger” laws are bans or severe restrictions on abortion providers and patients intended to take effect if Roe were to be overturned. Alternatively, the Court may overturn Southeastern Pennsylvania v Casey, but maintain Roe v Wade, essentially leaving the regulation of pre-viability abortion care to individual states. Currently 21 states have laws that would restrict the legal status of abortion.10 In addition, state legislatures are aggressively introducing abortion restrictions. As of June 2021, there have been 561 abortion restrictions, including 165 abortion bans, introduced across 47 states, putting 2021 on course to be the most devastating anti-abortion state legislative session in decades.11
The damage caused by such restriction on abortion care would be significant. It would block or push access out of reach for many. The negative effects of such legislative action would most heavily burden those already marginalized by systemic, structural inequalities including those of low socioeconomic status, people of color, young people, those in rural communities, and members of the LGBTQ community. The medical community has long recognized the harm caused by restricting access to abortion care. Restriction of access to safe abortion care paradoxically has been shown not to decrease the incidence of abortion, but rather increases the number of unsafe abortions.12 The American College of Obstetricians and Gynecologists (ACOG) acknowledge “individuals require access to safe, legal abortion” and that this represents “a necessary component for comprehensive health care.”13,14 They joined the American Medical Association and other professional groups in a 2019 amicus brief to SCOTUS opposing restrictions on abortion access.15 In addition, government laws restricting access to abortion care undermine the fundamental relationship between a person and their physician, limiting a physician’s obligation to honor patient autonomy and provide appropriate medical care.
By taking up the question whether all pre-viability bans on elective abortions violate the Constitution, SCOTUS is indicating a possible willingness to revisit the central holding of abortion jurisprudence. Their decision regarding this case will likely be the most significant ruling regarding the legal status of abortion care in decades, and will significantly affect the delivery of abortion care in the future.
Action items
- Reach out to your representatives to support the Women’s Health Protection Act, an initiative introduced to Congress to protect access to abortion care. If you reside in a state where your federal representatives support the Women’s Health Protection Act, reach out to friends and colleagues in states without supportive elected officials and ask them to call their representatives and ask them to support the bill.
- Get involved with local grassroots groups fighting to protect abortion access.
- Continue to speak out against laws and policies designed to limit access to safe abortion care.
- Connect with your local ACOG chapter for more ways to become involved.
- As always, make sure you are registered to vote, and exercise your right whenever you can.
- HB1510 (As Introduced) - 2018 Regular Session. http://billstatus.ls.state.ms.us/documents/2018/html/HB/1500-1599/HB1510IN.htm Accessed August 13, 2021.
- HB338. Louisiana State Legislature. 2014. http://www.legis.la.gov/legis/BillInfo.aspx?s=14RS&b=ACT620&sbi=y. Accessed August 13, 2021.
- Planned Parenthood of Southeastern Pennsylvania v. Casey. Cornell Law School Legal Information Institute. https://www.law.cornell.edu/supremecourt/text/505/833. Accessed August 13, 2021.
- 15-274 Whole Woman’s Health v. Hellerstedt (06/27/2016). Published online 2016:107.
- 18-1323 June Medical Services L. L. C. v. Russo (06/29/2020). Published online 2020:138.
- 19-1392 Dobbs v. Jackson Women’s Health Organization (07/22/2021). Published online 2021.
- What Ruth Bader Ginsburg said about abortion and Roe v. Wade. Time. August 2, 2018. https://time.com/5354490/ruth-bader-ginsburg-roe-v-wade/. Accessed August 13, 2021.
- Montanaro D. Poll: majority want to keep abortion legal, but they also want restrictions. NPR. June 7, 2019. https://www.npr.org/2019/06/07/730183531/poll-majority-want-to-keep-abortion-legal-but-they-also-want-restrictions. Accessed August 13, 2021.
- Abortion support remains steady despite growing partisan divide, survey finds. Washington Post. August 13, 2019. https://www.washingtonpost.com/health/2019/08/13/one-largest-ever-abortion-surveys-shows-growing-partisan-divide/. Accessed August 13, 2021.
- Abortion policy in the absence of Roe. Guttmacher Institute. September 1, 2021. https://www.guttmacher.org/state-policy/explore/abortion-policy-absence-roe#. Accessed September 8, 2021.
- 2021 is on track to become the most devastating antiabortion state legislative session in decades. Guttmacher Institute. Published April 30, 2021. Updated June 14, 2021. https://www.guttmacher.org/article/2021/04/2021-track-become-most-devastating-antiabortion-state-legislative-session-decades. Accessed August 13, 2021.
- Facts and consequences: legality, incidence and safety of abortion worldwide. Guttmacher Institute. November 20, 2009. https://www.guttmacher.org/gpr/2009/11/facts-and-consequences-legality-incidence-and-safety-abortion-worldwide. Accessed August 13, 2021.
- Increasing access to abortion. https://www.acog.org/en/clinical/clinical-guidance/committee-opinion/articles/2020/12/increasing-access-to-abortion. Accessed August 13, 2021.
- ACOG statement on Dobbs vs. Jackson Women’s Health. May 17, 2021. https://www.acog.org/en/news/news-releases/2021/05/acog-statement-dobbs-vs-jackson-womens-health. Accessed August 13, 2021.
- Perryman SL, Parker KA, Hickman SA. Brief of amici curiae American College of Obstetricians and Gynecologists, American Medical Associations, American Academy of Family Physicians, American Academy of Nursing, American Academy of Pediatrics, et al. In support of June Medical Services, LLC, et al. https://www.supremecourt.gov/
DocketPDF/18/18-1323/124091/ . Accessed August 13, 2021.20191202145531124_18-1323% 2018-1460%20tsac%20American% 20College%20of% 20Obstetricians%20and% 20Gynecologists%20et%20al.pdf
This fall, the Supreme Court of the United States (SCOTUS) will announce when they will hear oral arguments for Dobbs v Jackson Women’s Health Organization. The court will examine a Mississippi law, known as the “Gestational Age Act,” originally passed in 2018, that sought to “limit abortions to fifteen weeks’ gestation except in a medical emergency or in cases of severe fetal abnormality.”1 This sets the stage for SCOTUS to make a major ruling on abortion, one which could affirm or upend landmark decisions and nearly 50 years of abortion legislative precedent. Additionally, SCOTUS’ recent decision to not intervene on Texas’ Senate Bill 8 (SB8), which essentially bans all abortions after 6 weeks’ gestational age, may foreshadow how this case will be decided. The current abortion restrictions in Texas and the implications of SB8 will be discussed in a forthcoming column.
SCOTUS and abortion rights
The decision to hear this case comes on the heels of another recent decision regarding a Louisiana law in June Medical Services v Russo. This case examined Louisiana Act 620, which would have required physicians to have hospital admitting privileges within 30 miles of where they provide abortion services.2 The law was deemed constitutionally invalid, with the majority noting the law would have drastically burdened a woman’s right to access abortion services. The Court ruled similarly in 2016 in Whole Women’s Health (WWH) v Hellerstedt, in which WWH challenged Texas House Bill 2, a nearly identical law requiring admitting privileges for abortion care providers. In both of these cases, SCOTUS pointed to precedent set by Southeastern Pennsylvania v Casey, which established that it is unconstitutional for a state to create an “undue burden” on a woman’s right to abortion prior to fetal viability.3 The precedent to this, Roe v Wade, and 5 decades of abortion legislation set may be upended by a SCOTUS decision this next term.
Dobbs v Jackson
On March 19, 2018, Mississippi enacted the “Gestational Age Act” into law. The newly enacted law would limit abortions to 15 weeks’ gestation except in a medical emergency or in cases of severe fetal anomalies. Jackson Women’s Health Organization, the only licensed abortion provider in the state, challenged the constitutionality of the law with legal support from Center for Reproductive Rights (CRR). The US District Court for the Southern District of Mississippi granted summary judgement in favor of the clinic and placed an injunction on the law’s enforcement. The state appealed to the Fifth Circuit Court of Appeals, which upheld the district court decision in a 3-0 decision in November 2019. Mississippi appealed to the Supreme Court, with their petition focusing on multiple questions from the appeals process. After repeatedly rescheduling the case, and multiple reviews in conference, SCOTUS agreed to hear the case. Most recently, the state has narrowed its argument, changing course, and attacking Roe v Wade directly. In a brief submitted in July 2021, the state argues the court should hold that all pre-viability prohibitions on elective abortions are constitutional.
Interestingly, during this time the Mississippi legislature also passed a law, House Bill 2116, also known as the “fetal heartbeat bill,” banning abortion with gestational ages after detection of a fetal heartbeat. This was also challenged, deemed unconstitutional, and affirmed on appeal by the Fifth US Circuit Court.
While recent challenges have focused on the “undue burden” state laws placed on those trying to access abortion care, this case will bring the issue of “viability” and gestational age limits to the forefront.4,5 In addition to Roe v Wade, the Court will have the opportunity to reexamine other relevant precedent, such as Southeastern Pennsylvania v Casey, in considering the most recent arguments of the state. In this most recent brief, the state argues that the Court should, “reject viability as a barrier to prohibiting elective abortions” and that a “viability rule has no constitutional basis.” The state goes on to argue the “Constitution does not protect a right to abortion or limit States’ authority to restrict it.”6 The language and tone in this brief are more direct and aggressive than the states’ petition submitted last June.
However, the composition of the Court is different than in the past. This case will be argued with Justice Amy Coney Barrett seated in place of Justice Ruth Bader Ginsburg, who was a strong advocate for women’s rights.7 She joins Justices Neil Gorsuch and Brett Kavanaugh, also appointed by President Donald Trump and widely viewed as conservative judges, tipping the scales to a more conservative Supreme Court. This case will also be argued in a polarized political environment.8,9 Given the conservative Supreme Court in the setting of an increasingly politically charged environment, reproductive right advocates are understandably worried that members of the anti-abortion movement view this as an opportunity to weaken or remove federal constitutional protections for abortion.
Continue to: Potential outcome of Dobbs v Jackson...
Potential outcome of Dobbs v Jackson
Should SCOTUS choose to rule in favor of Mississippi, it could severely weaken, or even overturn Roe v Wade. This would leave a legal path for states with pre-Roe abortion bans and currently unenforced post-Roe bans to take effect. These “trigger” laws are bans or severe restrictions on abortion providers and patients intended to take effect if Roe were to be overturned. Alternatively, the Court may overturn Southeastern Pennsylvania v Casey, but maintain Roe v Wade, essentially leaving the regulation of pre-viability abortion care to individual states. Currently 21 states have laws that would restrict the legal status of abortion.10 In addition, state legislatures are aggressively introducing abortion restrictions. As of June 2021, there have been 561 abortion restrictions, including 165 abortion bans, introduced across 47 states, putting 2021 on course to be the most devastating anti-abortion state legislative session in decades.11
The damage caused by such restriction on abortion care would be significant. It would block or push access out of reach for many. The negative effects of such legislative action would most heavily burden those already marginalized by systemic, structural inequalities including those of low socioeconomic status, people of color, young people, those in rural communities, and members of the LGBTQ community. The medical community has long recognized the harm caused by restricting access to abortion care. Restriction of access to safe abortion care paradoxically has been shown not to decrease the incidence of abortion, but rather increases the number of unsafe abortions.12 The American College of Obstetricians and Gynecologists (ACOG) acknowledge “individuals require access to safe, legal abortion” and that this represents “a necessary component for comprehensive health care.”13,14 They joined the American Medical Association and other professional groups in a 2019 amicus brief to SCOTUS opposing restrictions on abortion access.15 In addition, government laws restricting access to abortion care undermine the fundamental relationship between a person and their physician, limiting a physician’s obligation to honor patient autonomy and provide appropriate medical care.
By taking up the question whether all pre-viability bans on elective abortions violate the Constitution, SCOTUS is indicating a possible willingness to revisit the central holding of abortion jurisprudence. Their decision regarding this case will likely be the most significant ruling regarding the legal status of abortion care in decades, and will significantly affect the delivery of abortion care in the future.
Action items
- Reach out to your representatives to support the Women’s Health Protection Act, an initiative introduced to Congress to protect access to abortion care. If you reside in a state where your federal representatives support the Women’s Health Protection Act, reach out to friends and colleagues in states without supportive elected officials and ask them to call their representatives and ask them to support the bill.
- Get involved with local grassroots groups fighting to protect abortion access.
- Continue to speak out against laws and policies designed to limit access to safe abortion care.
- Connect with your local ACOG chapter for more ways to become involved.
- As always, make sure you are registered to vote, and exercise your right whenever you can.
This fall, the Supreme Court of the United States (SCOTUS) will announce when they will hear oral arguments for Dobbs v Jackson Women’s Health Organization. The court will examine a Mississippi law, known as the “Gestational Age Act,” originally passed in 2018, that sought to “limit abortions to fifteen weeks’ gestation except in a medical emergency or in cases of severe fetal abnormality.”1 This sets the stage for SCOTUS to make a major ruling on abortion, one which could affirm or upend landmark decisions and nearly 50 years of abortion legislative precedent. Additionally, SCOTUS’ recent decision to not intervene on Texas’ Senate Bill 8 (SB8), which essentially bans all abortions after 6 weeks’ gestational age, may foreshadow how this case will be decided. The current abortion restrictions in Texas and the implications of SB8 will be discussed in a forthcoming column.
SCOTUS and abortion rights
The decision to hear this case comes on the heels of another recent decision regarding a Louisiana law in June Medical Services v Russo. This case examined Louisiana Act 620, which would have required physicians to have hospital admitting privileges within 30 miles of where they provide abortion services.2 The law was deemed constitutionally invalid, with the majority noting the law would have drastically burdened a woman’s right to access abortion services. The Court ruled similarly in 2016 in Whole Women’s Health (WWH) v Hellerstedt, in which WWH challenged Texas House Bill 2, a nearly identical law requiring admitting privileges for abortion care providers. In both of these cases, SCOTUS pointed to precedent set by Southeastern Pennsylvania v Casey, which established that it is unconstitutional for a state to create an “undue burden” on a woman’s right to abortion prior to fetal viability.3 The precedent to this, Roe v Wade, and 5 decades of abortion legislation set may be upended by a SCOTUS decision this next term.
Dobbs v Jackson
On March 19, 2018, Mississippi enacted the “Gestational Age Act” into law. The newly enacted law would limit abortions to 15 weeks’ gestation except in a medical emergency or in cases of severe fetal anomalies. Jackson Women’s Health Organization, the only licensed abortion provider in the state, challenged the constitutionality of the law with legal support from Center for Reproductive Rights (CRR). The US District Court for the Southern District of Mississippi granted summary judgement in favor of the clinic and placed an injunction on the law’s enforcement. The state appealed to the Fifth Circuit Court of Appeals, which upheld the district court decision in a 3-0 decision in November 2019. Mississippi appealed to the Supreme Court, with their petition focusing on multiple questions from the appeals process. After repeatedly rescheduling the case, and multiple reviews in conference, SCOTUS agreed to hear the case. Most recently, the state has narrowed its argument, changing course, and attacking Roe v Wade directly. In a brief submitted in July 2021, the state argues the court should hold that all pre-viability prohibitions on elective abortions are constitutional.
Interestingly, during this time the Mississippi legislature also passed a law, House Bill 2116, also known as the “fetal heartbeat bill,” banning abortion with gestational ages after detection of a fetal heartbeat. This was also challenged, deemed unconstitutional, and affirmed on appeal by the Fifth US Circuit Court.
While recent challenges have focused on the “undue burden” state laws placed on those trying to access abortion care, this case will bring the issue of “viability” and gestational age limits to the forefront.4,5 In addition to Roe v Wade, the Court will have the opportunity to reexamine other relevant precedent, such as Southeastern Pennsylvania v Casey, in considering the most recent arguments of the state. In this most recent brief, the state argues that the Court should, “reject viability as a barrier to prohibiting elective abortions” and that a “viability rule has no constitutional basis.” The state goes on to argue the “Constitution does not protect a right to abortion or limit States’ authority to restrict it.”6 The language and tone in this brief are more direct and aggressive than the states’ petition submitted last June.
However, the composition of the Court is different than in the past. This case will be argued with Justice Amy Coney Barrett seated in place of Justice Ruth Bader Ginsburg, who was a strong advocate for women’s rights.7 She joins Justices Neil Gorsuch and Brett Kavanaugh, also appointed by President Donald Trump and widely viewed as conservative judges, tipping the scales to a more conservative Supreme Court. This case will also be argued in a polarized political environment.8,9 Given the conservative Supreme Court in the setting of an increasingly politically charged environment, reproductive right advocates are understandably worried that members of the anti-abortion movement view this as an opportunity to weaken or remove federal constitutional protections for abortion.
Continue to: Potential outcome of Dobbs v Jackson...
Potential outcome of Dobbs v Jackson
Should SCOTUS choose to rule in favor of Mississippi, it could severely weaken, or even overturn Roe v Wade. This would leave a legal path for states with pre-Roe abortion bans and currently unenforced post-Roe bans to take effect. These “trigger” laws are bans or severe restrictions on abortion providers and patients intended to take effect if Roe were to be overturned. Alternatively, the Court may overturn Southeastern Pennsylvania v Casey, but maintain Roe v Wade, essentially leaving the regulation of pre-viability abortion care to individual states. Currently 21 states have laws that would restrict the legal status of abortion.10 In addition, state legislatures are aggressively introducing abortion restrictions. As of June 2021, there have been 561 abortion restrictions, including 165 abortion bans, introduced across 47 states, putting 2021 on course to be the most devastating anti-abortion state legislative session in decades.11
The damage caused by such restriction on abortion care would be significant. It would block or push access out of reach for many. The negative effects of such legislative action would most heavily burden those already marginalized by systemic, structural inequalities including those of low socioeconomic status, people of color, young people, those in rural communities, and members of the LGBTQ community. The medical community has long recognized the harm caused by restricting access to abortion care. Restriction of access to safe abortion care paradoxically has been shown not to decrease the incidence of abortion, but rather increases the number of unsafe abortions.12 The American College of Obstetricians and Gynecologists (ACOG) acknowledge “individuals require access to safe, legal abortion” and that this represents “a necessary component for comprehensive health care.”13,14 They joined the American Medical Association and other professional groups in a 2019 amicus brief to SCOTUS opposing restrictions on abortion access.15 In addition, government laws restricting access to abortion care undermine the fundamental relationship between a person and their physician, limiting a physician’s obligation to honor patient autonomy and provide appropriate medical care.
By taking up the question whether all pre-viability bans on elective abortions violate the Constitution, SCOTUS is indicating a possible willingness to revisit the central holding of abortion jurisprudence. Their decision regarding this case will likely be the most significant ruling regarding the legal status of abortion care in decades, and will significantly affect the delivery of abortion care in the future.
Action items
- Reach out to your representatives to support the Women’s Health Protection Act, an initiative introduced to Congress to protect access to abortion care. If you reside in a state where your federal representatives support the Women’s Health Protection Act, reach out to friends and colleagues in states without supportive elected officials and ask them to call their representatives and ask them to support the bill.
- Get involved with local grassroots groups fighting to protect abortion access.
- Continue to speak out against laws and policies designed to limit access to safe abortion care.
- Connect with your local ACOG chapter for more ways to become involved.
- As always, make sure you are registered to vote, and exercise your right whenever you can.
- HB1510 (As Introduced) - 2018 Regular Session. http://billstatus.ls.state.ms.us/documents/2018/html/HB/1500-1599/HB1510IN.htm Accessed August 13, 2021.
- HB338. Louisiana State Legislature. 2014. http://www.legis.la.gov/legis/BillInfo.aspx?s=14RS&b=ACT620&sbi=y. Accessed August 13, 2021.
- Planned Parenthood of Southeastern Pennsylvania v. Casey. Cornell Law School Legal Information Institute. https://www.law.cornell.edu/supremecourt/text/505/833. Accessed August 13, 2021.
- 15-274 Whole Woman’s Health v. Hellerstedt (06/27/2016). Published online 2016:107.
- 18-1323 June Medical Services L. L. C. v. Russo (06/29/2020). Published online 2020:138.
- 19-1392 Dobbs v. Jackson Women’s Health Organization (07/22/2021). Published online 2021.
- What Ruth Bader Ginsburg said about abortion and Roe v. Wade. Time. August 2, 2018. https://time.com/5354490/ruth-bader-ginsburg-roe-v-wade/. Accessed August 13, 2021.
- Montanaro D. Poll: majority want to keep abortion legal, but they also want restrictions. NPR. June 7, 2019. https://www.npr.org/2019/06/07/730183531/poll-majority-want-to-keep-abortion-legal-but-they-also-want-restrictions. Accessed August 13, 2021.
- Abortion support remains steady despite growing partisan divide, survey finds. Washington Post. August 13, 2019. https://www.washingtonpost.com/health/2019/08/13/one-largest-ever-abortion-surveys-shows-growing-partisan-divide/. Accessed August 13, 2021.
- Abortion policy in the absence of Roe. Guttmacher Institute. September 1, 2021. https://www.guttmacher.org/state-policy/explore/abortion-policy-absence-roe#. Accessed September 8, 2021.
- 2021 is on track to become the most devastating antiabortion state legislative session in decades. Guttmacher Institute. Published April 30, 2021. Updated June 14, 2021. https://www.guttmacher.org/article/2021/04/2021-track-become-most-devastating-antiabortion-state-legislative-session-decades. Accessed August 13, 2021.
- Facts and consequences: legality, incidence and safety of abortion worldwide. Guttmacher Institute. November 20, 2009. https://www.guttmacher.org/gpr/2009/11/facts-and-consequences-legality-incidence-and-safety-abortion-worldwide. Accessed August 13, 2021.
- Increasing access to abortion. https://www.acog.org/en/clinical/clinical-guidance/committee-opinion/articles/2020/12/increasing-access-to-abortion. Accessed August 13, 2021.
- ACOG statement on Dobbs vs. Jackson Women’s Health. May 17, 2021. https://www.acog.org/en/news/news-releases/2021/05/acog-statement-dobbs-vs-jackson-womens-health. Accessed August 13, 2021.
- Perryman SL, Parker KA, Hickman SA. Brief of amici curiae American College of Obstetricians and Gynecologists, American Medical Associations, American Academy of Family Physicians, American Academy of Nursing, American Academy of Pediatrics, et al. In support of June Medical Services, LLC, et al. https://www.supremecourt.gov/
DocketPDF/18/18-1323/124091/ . Accessed August 13, 2021.20191202145531124_18-1323% 2018-1460%20tsac%20American% 20College%20of% 20Obstetricians%20and% 20Gynecologists%20et%20al.pdf
- HB1510 (As Introduced) - 2018 Regular Session. http://billstatus.ls.state.ms.us/documents/2018/html/HB/1500-1599/HB1510IN.htm Accessed August 13, 2021.
- HB338. Louisiana State Legislature. 2014. http://www.legis.la.gov/legis/BillInfo.aspx?s=14RS&b=ACT620&sbi=y. Accessed August 13, 2021.
- Planned Parenthood of Southeastern Pennsylvania v. Casey. Cornell Law School Legal Information Institute. https://www.law.cornell.edu/supremecourt/text/505/833. Accessed August 13, 2021.
- 15-274 Whole Woman’s Health v. Hellerstedt (06/27/2016). Published online 2016:107.
- 18-1323 June Medical Services L. L. C. v. Russo (06/29/2020). Published online 2020:138.
- 19-1392 Dobbs v. Jackson Women’s Health Organization (07/22/2021). Published online 2021.
- What Ruth Bader Ginsburg said about abortion and Roe v. Wade. Time. August 2, 2018. https://time.com/5354490/ruth-bader-ginsburg-roe-v-wade/. Accessed August 13, 2021.
- Montanaro D. Poll: majority want to keep abortion legal, but they also want restrictions. NPR. June 7, 2019. https://www.npr.org/2019/06/07/730183531/poll-majority-want-to-keep-abortion-legal-but-they-also-want-restrictions. Accessed August 13, 2021.
- Abortion support remains steady despite growing partisan divide, survey finds. Washington Post. August 13, 2019. https://www.washingtonpost.com/health/2019/08/13/one-largest-ever-abortion-surveys-shows-growing-partisan-divide/. Accessed August 13, 2021.
- Abortion policy in the absence of Roe. Guttmacher Institute. September 1, 2021. https://www.guttmacher.org/state-policy/explore/abortion-policy-absence-roe#. Accessed September 8, 2021.
- 2021 is on track to become the most devastating antiabortion state legislative session in decades. Guttmacher Institute. Published April 30, 2021. Updated June 14, 2021. https://www.guttmacher.org/article/2021/04/2021-track-become-most-devastating-antiabortion-state-legislative-session-decades. Accessed August 13, 2021.
- Facts and consequences: legality, incidence and safety of abortion worldwide. Guttmacher Institute. November 20, 2009. https://www.guttmacher.org/gpr/2009/11/facts-and-consequences-legality-incidence-and-safety-abortion-worldwide. Accessed August 13, 2021.
- Increasing access to abortion. https://www.acog.org/en/clinical/clinical-guidance/committee-opinion/articles/2020/12/increasing-access-to-abortion. Accessed August 13, 2021.
- ACOG statement on Dobbs vs. Jackson Women’s Health. May 17, 2021. https://www.acog.org/en/news/news-releases/2021/05/acog-statement-dobbs-vs-jackson-womens-health. Accessed August 13, 2021.
- Perryman SL, Parker KA, Hickman SA. Brief of amici curiae American College of Obstetricians and Gynecologists, American Medical Associations, American Academy of Family Physicians, American Academy of Nursing, American Academy of Pediatrics, et al. In support of June Medical Services, LLC, et al. https://www.supremecourt.gov/
DocketPDF/18/18-1323/124091/ . Accessed August 13, 2021.20191202145531124_18-1323% 2018-1460%20tsac%20American% 20College%20of% 20Obstetricians%20and% 20Gynecologists%20et%20al.pdf
Iron deficiency in pregnancy is common, yet many aren’t being screened for it
Many pregnant patients are not being screened for iron deficiency despite it being a common cause of anemia in pregnancy that could increase the risk of maternal and infant death.
Researchers analyzed data from 44,552 pregnant patients in Ontario, Canada, collected between 2013 and 2018 to determine the prevalence of ferritin testing, the standard test for iron deficiency, over the course of 5 years.
Their study, published in Blood Advances, revealed that only 59.4% of pregnant persons received a ferritin test, the standard test for iron deficiency. Of those pregnant persons, 25.2% were iron insufficient and 52.8% were iron deficient at least once during pregnancy.
They also found that 71% of these iron tests were ordered during the first trimester, when the risk of iron deficiency is lowest.
“We are not only missing a very large proportion of women who are iron deficient going into pregnancy, but we’re missing those that become iron deficient later on in their pregnancies,” study author Dr. Jennifer Teichman, hematology resident at the University of Toronto, said in an interview. Researchers said iron deficiency during pregnancy is associated with maternal fatigue, cognitive dysfunction, depression, low birth weight, and poor brain development of the child.
Dr. Teichman explained that if iron deficiency during pregnancy is identified early enough, doctors would have enough time to treat the condition with iron supplements before the patient goes into delivery. She also explained prenatal vitamins, which contain some iron, do not contain enough of the mineral to fix iron deficiency.
“One really important point is that the amount of iron contained in a prenatal vitamin is really low,” Dr. Teichman explained. “It’s enough to make up the difference of the additional iron that she needs to sustain her pregnancy, but it’s not enough to treat a woman who’s already got low iron going into pregnancy. So there’s a difference between a prenatal vitamin and true iron supplementation.”
Researchers also found that those who came from a household with a low annual income were even less likely to receive a ferritin test, which was a troubling finding since women of lower socioeconomic status are more likely to be iron deficient in pregnancy.
“[This] says something about how we as health care providers are contributing to this gap in care,” Dr. Teichman said. “Women of lower socioeconomic status sort of have a triple whammy: They’re more likely to be iron deficient, they’re less likely to have it diagnosed, and they’re less likely to have it corrected.”
Dr. Teichman and her colleagues took a unique approach by looking at isolated ferritin levels as opposed to complete blood counts, which is the typical screening for anemia in pregnancy, said Lissette Tanner, MD, MPH, FACOG, who was not involved with the study.
“Those who meet the criteria for anemia should be evaluated for the cause with initial suspicion for iron deficiency anemia, as that is the most common etiology,” said Dr. Tanner, assistant professor of gynecology and obstetrics at Emory University, Atlanta.
The Centers for Disease Control and Prevention recommends screening for iron deficiency anemia in pregnant persons, in addition to universal iron supplementation to meet the iron requirements of pregnancy.
Additionally, the American College of Obstetricians and Gynecologists recommends that all pregnant persons be screened for anemia with a complete blood count in the first trimester and again between 24 and 28 weeks of pregnancy.
However, iron deficiency is completely missed by ACOG’s recommendations, said Michael Auerbach, MD, of the department of medicine, Georgetown University, Washington.
“They recommend a [complete blood count] on all presenting pregnant women, but they do not recommend iron parameters, including a ferritin test, unless the mother is anemic,” said Dr. Auerbach, who was not involved in the study. “I think those guidelines are in need of revision.”
Dr. Teichman hopes her team’s findings will motivate change in obstetric and hematologic guidelines that recommend routine prenatal testing.
“I think ferritin should be a part of routine prenatal testing,” Dr. Teichman said. “And I also think that patients need to be empowered to ask what their iron levels are in pregnancy and providers need to know what a normal iron level is.”
None of the experts interviewed for this story had financial conflicts of interest.
Many pregnant patients are not being screened for iron deficiency despite it being a common cause of anemia in pregnancy that could increase the risk of maternal and infant death.
Researchers analyzed data from 44,552 pregnant patients in Ontario, Canada, collected between 2013 and 2018 to determine the prevalence of ferritin testing, the standard test for iron deficiency, over the course of 5 years.
Their study, published in Blood Advances, revealed that only 59.4% of pregnant persons received a ferritin test, the standard test for iron deficiency. Of those pregnant persons, 25.2% were iron insufficient and 52.8% were iron deficient at least once during pregnancy.
They also found that 71% of these iron tests were ordered during the first trimester, when the risk of iron deficiency is lowest.
“We are not only missing a very large proportion of women who are iron deficient going into pregnancy, but we’re missing those that become iron deficient later on in their pregnancies,” study author Dr. Jennifer Teichman, hematology resident at the University of Toronto, said in an interview. Researchers said iron deficiency during pregnancy is associated with maternal fatigue, cognitive dysfunction, depression, low birth weight, and poor brain development of the child.
Dr. Teichman explained that if iron deficiency during pregnancy is identified early enough, doctors would have enough time to treat the condition with iron supplements before the patient goes into delivery. She also explained prenatal vitamins, which contain some iron, do not contain enough of the mineral to fix iron deficiency.
“One really important point is that the amount of iron contained in a prenatal vitamin is really low,” Dr. Teichman explained. “It’s enough to make up the difference of the additional iron that she needs to sustain her pregnancy, but it’s not enough to treat a woman who’s already got low iron going into pregnancy. So there’s a difference between a prenatal vitamin and true iron supplementation.”
Researchers also found that those who came from a household with a low annual income were even less likely to receive a ferritin test, which was a troubling finding since women of lower socioeconomic status are more likely to be iron deficient in pregnancy.
“[This] says something about how we as health care providers are contributing to this gap in care,” Dr. Teichman said. “Women of lower socioeconomic status sort of have a triple whammy: They’re more likely to be iron deficient, they’re less likely to have it diagnosed, and they’re less likely to have it corrected.”
Dr. Teichman and her colleagues took a unique approach by looking at isolated ferritin levels as opposed to complete blood counts, which is the typical screening for anemia in pregnancy, said Lissette Tanner, MD, MPH, FACOG, who was not involved with the study.
“Those who meet the criteria for anemia should be evaluated for the cause with initial suspicion for iron deficiency anemia, as that is the most common etiology,” said Dr. Tanner, assistant professor of gynecology and obstetrics at Emory University, Atlanta.
The Centers for Disease Control and Prevention recommends screening for iron deficiency anemia in pregnant persons, in addition to universal iron supplementation to meet the iron requirements of pregnancy.
Additionally, the American College of Obstetricians and Gynecologists recommends that all pregnant persons be screened for anemia with a complete blood count in the first trimester and again between 24 and 28 weeks of pregnancy.
However, iron deficiency is completely missed by ACOG’s recommendations, said Michael Auerbach, MD, of the department of medicine, Georgetown University, Washington.
“They recommend a [complete blood count] on all presenting pregnant women, but they do not recommend iron parameters, including a ferritin test, unless the mother is anemic,” said Dr. Auerbach, who was not involved in the study. “I think those guidelines are in need of revision.”
Dr. Teichman hopes her team’s findings will motivate change in obstetric and hematologic guidelines that recommend routine prenatal testing.
“I think ferritin should be a part of routine prenatal testing,” Dr. Teichman said. “And I also think that patients need to be empowered to ask what their iron levels are in pregnancy and providers need to know what a normal iron level is.”
None of the experts interviewed for this story had financial conflicts of interest.
Many pregnant patients are not being screened for iron deficiency despite it being a common cause of anemia in pregnancy that could increase the risk of maternal and infant death.
Researchers analyzed data from 44,552 pregnant patients in Ontario, Canada, collected between 2013 and 2018 to determine the prevalence of ferritin testing, the standard test for iron deficiency, over the course of 5 years.
Their study, published in Blood Advances, revealed that only 59.4% of pregnant persons received a ferritin test, the standard test for iron deficiency. Of those pregnant persons, 25.2% were iron insufficient and 52.8% were iron deficient at least once during pregnancy.
They also found that 71% of these iron tests were ordered during the first trimester, when the risk of iron deficiency is lowest.
“We are not only missing a very large proportion of women who are iron deficient going into pregnancy, but we’re missing those that become iron deficient later on in their pregnancies,” study author Dr. Jennifer Teichman, hematology resident at the University of Toronto, said in an interview. Researchers said iron deficiency during pregnancy is associated with maternal fatigue, cognitive dysfunction, depression, low birth weight, and poor brain development of the child.
Dr. Teichman explained that if iron deficiency during pregnancy is identified early enough, doctors would have enough time to treat the condition with iron supplements before the patient goes into delivery. She also explained prenatal vitamins, which contain some iron, do not contain enough of the mineral to fix iron deficiency.
“One really important point is that the amount of iron contained in a prenatal vitamin is really low,” Dr. Teichman explained. “It’s enough to make up the difference of the additional iron that she needs to sustain her pregnancy, but it’s not enough to treat a woman who’s already got low iron going into pregnancy. So there’s a difference between a prenatal vitamin and true iron supplementation.”
Researchers also found that those who came from a household with a low annual income were even less likely to receive a ferritin test, which was a troubling finding since women of lower socioeconomic status are more likely to be iron deficient in pregnancy.
“[This] says something about how we as health care providers are contributing to this gap in care,” Dr. Teichman said. “Women of lower socioeconomic status sort of have a triple whammy: They’re more likely to be iron deficient, they’re less likely to have it diagnosed, and they’re less likely to have it corrected.”
Dr. Teichman and her colleagues took a unique approach by looking at isolated ferritin levels as opposed to complete blood counts, which is the typical screening for anemia in pregnancy, said Lissette Tanner, MD, MPH, FACOG, who was not involved with the study.
“Those who meet the criteria for anemia should be evaluated for the cause with initial suspicion for iron deficiency anemia, as that is the most common etiology,” said Dr. Tanner, assistant professor of gynecology and obstetrics at Emory University, Atlanta.
The Centers for Disease Control and Prevention recommends screening for iron deficiency anemia in pregnant persons, in addition to universal iron supplementation to meet the iron requirements of pregnancy.
Additionally, the American College of Obstetricians and Gynecologists recommends that all pregnant persons be screened for anemia with a complete blood count in the first trimester and again between 24 and 28 weeks of pregnancy.
However, iron deficiency is completely missed by ACOG’s recommendations, said Michael Auerbach, MD, of the department of medicine, Georgetown University, Washington.
“They recommend a [complete blood count] on all presenting pregnant women, but they do not recommend iron parameters, including a ferritin test, unless the mother is anemic,” said Dr. Auerbach, who was not involved in the study. “I think those guidelines are in need of revision.”
Dr. Teichman hopes her team’s findings will motivate change in obstetric and hematologic guidelines that recommend routine prenatal testing.
“I think ferritin should be a part of routine prenatal testing,” Dr. Teichman said. “And I also think that patients need to be empowered to ask what their iron levels are in pregnancy and providers need to know what a normal iron level is.”
None of the experts interviewed for this story had financial conflicts of interest.
FROM BLOOD ADVANCES
COVID-19 linked to baby bust in high-income countries
In an assessment of the pandemic’s early effects, Arnstein Aassve, PhD, and colleagues found a significant COVID-19–related decline in crude birth rates (CBRs) in 7 of 22 high-income countries, particularly in Southwestern Europe.
Dr. Aassve, an economist at the Carlo F. Dondena Center for Research on Social Dynamics and Public Policy at the Università Commerciale Luigi Bocconi, Milan, and colleagues report the results in an article published online August 30 in the Proceedings of the National Academy of Sciences.
Defining the start of the COVID-19 pandemic as February 2020, the study identifies strong declines in Italy (-9.1%), Hungary (-8.5%), Spain (-8.4%), and Portugal (-6.6%) beyond those predicted by past trends. In the United States, CBRs fell by 7.1% relative to 2019 for births occurring in Nov. and Dec. 2020 following conceptions in February and March of that year.
Significant declines in CBR also occurred in Belgium, Austria, and Singapore.
A year-to-year comparison of the mean for monthly CBRs per 1,000 population before and during the pandemic suggests a negative difference for all countries studied except for Denmark, Finland, Germany, and the Netherlands, Dr. Aassve and colleagues write. These findings may have policy implications for childcare, housing, and the labor market.
The Milan researchers compared monthly vital statistics data on live births from the international Human Fertility Database for the period of Jan. 2016 to March 2021. These figures reflect conceptions carried to term between April 2015 and June 2020. The 22 countries in the analysis represent 37% of the total reported COVID-19 cases and 34% of deaths worldwide.
The study findings align with surveys on “fertility intentions” collected early in the first COVID-19 wave in Germany, France, Spain, and the United Kingdom. These surveys indicated that 73% of people who were planning pregnancies in 2020 either decided to delay the pregnancy or they abandoned their plans.
“The popular media speculated that the lockdown would lead to a baby boom, as couples spent more time together,” Dr. Aassve told this news organization. “There’s very little evidence of this when you look to previous disasters and shocks, and the first data suggest more of an immediate collapse than a boom. But as you also see from the paper, the collapse is not seen everywhere.” Other current studies suggest the fertility drop is immediate but temporary, says Dr. Aassve, who is also a professor of demography.
Interestingly, Dr. Aassve and colleagues found that CBRs were relatively stable in Northern Europe. The authors point to supportive social and family policies in that region that might have reduced the effect of the pandemic on births. “These factors are likely to affect CBRs in the subsequent pandemic waves,” they write. They call for future studies to assess the full population implications of the pandemic, the moderating impact of policy interventions, and the nexus between short- and long-run effects in relation to the various waves of the COVID-19 pandemic.
Rebounds
Some regions have already reported a rebound from the COVID-19 fertility trough. Molly J. Stout, MD, director of maternal fetal medicine at the University of Michigan, Ann Arbor, and colleagues used electronic medical records to predict a surge in births after the initial decline.
“The surge we’ve seen at the end of this summer is exceeding the usual annual birth rate, as predicted,” she said in an interview. “But I think there’ll be a return to normal after this transient escalation. I don’t think birth rates will stay elevated above the normal because the birth surge is a temporary response to an event, although there will likely be regional differences.”
Looking ahead, Dr. Stout, who was not involved in Dr. Aassve’s analysis, is not certain how a fourth pandemic wave might ultimately modify a couple’s overall family size. But the toll the health crisis has taken on working women who have been forced to withdraw from the economy because of a lack of childcare points to a societal need that should be addressed.
According to Philip N. Cohen, PhD, a professor of sociology at the University of Maryland, College Park, who’s been tracking fertility trends since the onset of the COVID-19 emergency, the pandemic has combined a health crisis with an economic crisis, along with “the additional factor of social distancing and isolation, which all contributed to the decline in birth rates. Some people changed their plans to hold off on having children, while others didn’t get pregnant because they weren’t socializing and meeting people as much.”
Dr. Cohen, who was not involved in the study by Dr. Aassve and associates, said his provisional data show that although in many places, birth rates have rebounded more or less to prepandemic levels after a nadir around Jan. 2021, some areas of the United States still show substantially lower rates, including California, Hawaii, and Oregon.
As to the duration of the pandemic effect, Dr. Aassve cautions that his group’s estimates refer to the first wave only. “We then have the second, third, and currently the fourth wave. We can’t be sure about the impact of these waves on fertility since the data are not there yet, but I’d be surprised if they didn’t continue to have an impact on fertility rates,” he said.
Dr. Cohen agreed: “Some people who delayed childbearing will make up the delay. However, whenever there’s a delay, there’s inevitably some portion of the decline that’s not recouped.”
As for the wider effect across the world, Dr. Aassve said his team’s figures derive from high-income countries where data are readily available. For middle- and low-income countries, fewer data exist, and the quality of those data is not as good.
The lessons from this and other upheavals teach us that unforeseen shocks almost always have a negative impact on fertility, says Dr. Aassve. “[B]ut these effects may be separate from existing declining trends. The issue here is that those overall declining trends may be driven by other factors. In contrast, the shock of the pandemic is short-lived, and we may return to normal rather quickly. But if the pandemic also impacts other societal structures, such as the occupational and industrial sectors, then the pandemic might exacerbate the negative trend.”
The study was supported by funding from the European Research Council for funding under the European Union’s Horizon 2020 Research and Innovation Programme. The study authors, Dr. Stout, and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In an assessment of the pandemic’s early effects, Arnstein Aassve, PhD, and colleagues found a significant COVID-19–related decline in crude birth rates (CBRs) in 7 of 22 high-income countries, particularly in Southwestern Europe.
Dr. Aassve, an economist at the Carlo F. Dondena Center for Research on Social Dynamics and Public Policy at the Università Commerciale Luigi Bocconi, Milan, and colleagues report the results in an article published online August 30 in the Proceedings of the National Academy of Sciences.
Defining the start of the COVID-19 pandemic as February 2020, the study identifies strong declines in Italy (-9.1%), Hungary (-8.5%), Spain (-8.4%), and Portugal (-6.6%) beyond those predicted by past trends. In the United States, CBRs fell by 7.1% relative to 2019 for births occurring in Nov. and Dec. 2020 following conceptions in February and March of that year.
Significant declines in CBR also occurred in Belgium, Austria, and Singapore.
A year-to-year comparison of the mean for monthly CBRs per 1,000 population before and during the pandemic suggests a negative difference for all countries studied except for Denmark, Finland, Germany, and the Netherlands, Dr. Aassve and colleagues write. These findings may have policy implications for childcare, housing, and the labor market.
The Milan researchers compared monthly vital statistics data on live births from the international Human Fertility Database for the period of Jan. 2016 to March 2021. These figures reflect conceptions carried to term between April 2015 and June 2020. The 22 countries in the analysis represent 37% of the total reported COVID-19 cases and 34% of deaths worldwide.
The study findings align with surveys on “fertility intentions” collected early in the first COVID-19 wave in Germany, France, Spain, and the United Kingdom. These surveys indicated that 73% of people who were planning pregnancies in 2020 either decided to delay the pregnancy or they abandoned their plans.
“The popular media speculated that the lockdown would lead to a baby boom, as couples spent more time together,” Dr. Aassve told this news organization. “There’s very little evidence of this when you look to previous disasters and shocks, and the first data suggest more of an immediate collapse than a boom. But as you also see from the paper, the collapse is not seen everywhere.” Other current studies suggest the fertility drop is immediate but temporary, says Dr. Aassve, who is also a professor of demography.
Interestingly, Dr. Aassve and colleagues found that CBRs were relatively stable in Northern Europe. The authors point to supportive social and family policies in that region that might have reduced the effect of the pandemic on births. “These factors are likely to affect CBRs in the subsequent pandemic waves,” they write. They call for future studies to assess the full population implications of the pandemic, the moderating impact of policy interventions, and the nexus between short- and long-run effects in relation to the various waves of the COVID-19 pandemic.
Rebounds
Some regions have already reported a rebound from the COVID-19 fertility trough. Molly J. Stout, MD, director of maternal fetal medicine at the University of Michigan, Ann Arbor, and colleagues used electronic medical records to predict a surge in births after the initial decline.
“The surge we’ve seen at the end of this summer is exceeding the usual annual birth rate, as predicted,” she said in an interview. “But I think there’ll be a return to normal after this transient escalation. I don’t think birth rates will stay elevated above the normal because the birth surge is a temporary response to an event, although there will likely be regional differences.”
Looking ahead, Dr. Stout, who was not involved in Dr. Aassve’s analysis, is not certain how a fourth pandemic wave might ultimately modify a couple’s overall family size. But the toll the health crisis has taken on working women who have been forced to withdraw from the economy because of a lack of childcare points to a societal need that should be addressed.
According to Philip N. Cohen, PhD, a professor of sociology at the University of Maryland, College Park, who’s been tracking fertility trends since the onset of the COVID-19 emergency, the pandemic has combined a health crisis with an economic crisis, along with “the additional factor of social distancing and isolation, which all contributed to the decline in birth rates. Some people changed their plans to hold off on having children, while others didn’t get pregnant because they weren’t socializing and meeting people as much.”
Dr. Cohen, who was not involved in the study by Dr. Aassve and associates, said his provisional data show that although in many places, birth rates have rebounded more or less to prepandemic levels after a nadir around Jan. 2021, some areas of the United States still show substantially lower rates, including California, Hawaii, and Oregon.
As to the duration of the pandemic effect, Dr. Aassve cautions that his group’s estimates refer to the first wave only. “We then have the second, third, and currently the fourth wave. We can’t be sure about the impact of these waves on fertility since the data are not there yet, but I’d be surprised if they didn’t continue to have an impact on fertility rates,” he said.
Dr. Cohen agreed: “Some people who delayed childbearing will make up the delay. However, whenever there’s a delay, there’s inevitably some portion of the decline that’s not recouped.”
As for the wider effect across the world, Dr. Aassve said his team’s figures derive from high-income countries where data are readily available. For middle- and low-income countries, fewer data exist, and the quality of those data is not as good.
The lessons from this and other upheavals teach us that unforeseen shocks almost always have a negative impact on fertility, says Dr. Aassve. “[B]ut these effects may be separate from existing declining trends. The issue here is that those overall declining trends may be driven by other factors. In contrast, the shock of the pandemic is short-lived, and we may return to normal rather quickly. But if the pandemic also impacts other societal structures, such as the occupational and industrial sectors, then the pandemic might exacerbate the negative trend.”
The study was supported by funding from the European Research Council for funding under the European Union’s Horizon 2020 Research and Innovation Programme. The study authors, Dr. Stout, and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In an assessment of the pandemic’s early effects, Arnstein Aassve, PhD, and colleagues found a significant COVID-19–related decline in crude birth rates (CBRs) in 7 of 22 high-income countries, particularly in Southwestern Europe.
Dr. Aassve, an economist at the Carlo F. Dondena Center for Research on Social Dynamics and Public Policy at the Università Commerciale Luigi Bocconi, Milan, and colleagues report the results in an article published online August 30 in the Proceedings of the National Academy of Sciences.
Defining the start of the COVID-19 pandemic as February 2020, the study identifies strong declines in Italy (-9.1%), Hungary (-8.5%), Spain (-8.4%), and Portugal (-6.6%) beyond those predicted by past trends. In the United States, CBRs fell by 7.1% relative to 2019 for births occurring in Nov. and Dec. 2020 following conceptions in February and March of that year.
Significant declines in CBR also occurred in Belgium, Austria, and Singapore.
A year-to-year comparison of the mean for monthly CBRs per 1,000 population before and during the pandemic suggests a negative difference for all countries studied except for Denmark, Finland, Germany, and the Netherlands, Dr. Aassve and colleagues write. These findings may have policy implications for childcare, housing, and the labor market.
The Milan researchers compared monthly vital statistics data on live births from the international Human Fertility Database for the period of Jan. 2016 to March 2021. These figures reflect conceptions carried to term between April 2015 and June 2020. The 22 countries in the analysis represent 37% of the total reported COVID-19 cases and 34% of deaths worldwide.
The study findings align with surveys on “fertility intentions” collected early in the first COVID-19 wave in Germany, France, Spain, and the United Kingdom. These surveys indicated that 73% of people who were planning pregnancies in 2020 either decided to delay the pregnancy or they abandoned their plans.
“The popular media speculated that the lockdown would lead to a baby boom, as couples spent more time together,” Dr. Aassve told this news organization. “There’s very little evidence of this when you look to previous disasters and shocks, and the first data suggest more of an immediate collapse than a boom. But as you also see from the paper, the collapse is not seen everywhere.” Other current studies suggest the fertility drop is immediate but temporary, says Dr. Aassve, who is also a professor of demography.
Interestingly, Dr. Aassve and colleagues found that CBRs were relatively stable in Northern Europe. The authors point to supportive social and family policies in that region that might have reduced the effect of the pandemic on births. “These factors are likely to affect CBRs in the subsequent pandemic waves,” they write. They call for future studies to assess the full population implications of the pandemic, the moderating impact of policy interventions, and the nexus between short- and long-run effects in relation to the various waves of the COVID-19 pandemic.
Rebounds
Some regions have already reported a rebound from the COVID-19 fertility trough. Molly J. Stout, MD, director of maternal fetal medicine at the University of Michigan, Ann Arbor, and colleagues used electronic medical records to predict a surge in births after the initial decline.
“The surge we’ve seen at the end of this summer is exceeding the usual annual birth rate, as predicted,” she said in an interview. “But I think there’ll be a return to normal after this transient escalation. I don’t think birth rates will stay elevated above the normal because the birth surge is a temporary response to an event, although there will likely be regional differences.”
Looking ahead, Dr. Stout, who was not involved in Dr. Aassve’s analysis, is not certain how a fourth pandemic wave might ultimately modify a couple’s overall family size. But the toll the health crisis has taken on working women who have been forced to withdraw from the economy because of a lack of childcare points to a societal need that should be addressed.
According to Philip N. Cohen, PhD, a professor of sociology at the University of Maryland, College Park, who’s been tracking fertility trends since the onset of the COVID-19 emergency, the pandemic has combined a health crisis with an economic crisis, along with “the additional factor of social distancing and isolation, which all contributed to the decline in birth rates. Some people changed their plans to hold off on having children, while others didn’t get pregnant because they weren’t socializing and meeting people as much.”
Dr. Cohen, who was not involved in the study by Dr. Aassve and associates, said his provisional data show that although in many places, birth rates have rebounded more or less to prepandemic levels after a nadir around Jan. 2021, some areas of the United States still show substantially lower rates, including California, Hawaii, and Oregon.
As to the duration of the pandemic effect, Dr. Aassve cautions that his group’s estimates refer to the first wave only. “We then have the second, third, and currently the fourth wave. We can’t be sure about the impact of these waves on fertility since the data are not there yet, but I’d be surprised if they didn’t continue to have an impact on fertility rates,” he said.
Dr. Cohen agreed: “Some people who delayed childbearing will make up the delay. However, whenever there’s a delay, there’s inevitably some portion of the decline that’s not recouped.”
As for the wider effect across the world, Dr. Aassve said his team’s figures derive from high-income countries where data are readily available. For middle- and low-income countries, fewer data exist, and the quality of those data is not as good.
The lessons from this and other upheavals teach us that unforeseen shocks almost always have a negative impact on fertility, says Dr. Aassve. “[B]ut these effects may be separate from existing declining trends. The issue here is that those overall declining trends may be driven by other factors. In contrast, the shock of the pandemic is short-lived, and we may return to normal rather quickly. But if the pandemic also impacts other societal structures, such as the occupational and industrial sectors, then the pandemic might exacerbate the negative trend.”
The study was supported by funding from the European Research Council for funding under the European Union’s Horizon 2020 Research and Innovation Programme. The study authors, Dr. Stout, and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
‘Countdown to zero’: Endocrine disruptors and worldwide sperm counts
In medical school, I remember thinking that telling a patient “you have cancer” would be the most professionally challenging phrase I would ever utter. And don’t get me wrong – it certainly isn’t easy; but, compared with telling someone “you are infertile,” it’s a cakewalk.
Maybe it’s because people “have” cancer and cancer is something you “fight.” Or maybe because, unlike infertility, cancer has become a part of public life (think lapel pins and support groups) and is now easier to accept. On the other hand, someone “is” infertile. The condition is a source of embarrassment for the couple and is often hidden from society.
Here’s another concerning point of contrast: While the overall rate of cancer death has declined since the early 1990s, infertility is increasing. Reports now show that one in six couples have problems conceiving and the use of assisted reproductive technologies is increasing by 5%-10% per year. Many theories exist to explain these trends, chief among them the rise in average maternal age and the increasing incidence of obesity, as well as various other male- and female-specific factors.
But interestingly, recent data suggest that the most male of all male-specific factors – total sperm count – may be specifically to blame.
According to a recent meta-analysis, the average total sperm count in men declined by 59.3% between 1973 and 2011. While these data certainly have limitations – including the exclusion of non-English publications, the reliance on total sperm count and not sperm motility, and the potential bias of those patients willing to give a semen sample – the overall trend nevertheless seems to be clearly downward. What’s more concerning, if you believe the data presented, is that there does not appear to be a leveling off of the downward curve in total sperm count.
Think about that last statement. At the current rate of decline, the average sperm count will be zero in 2045. One of the lead authors on the meta-analysis, Hagai Levine, MD, MPH, goes so far as to state, “We should hope for the best and prepare for the worst.”
As a matter of personal philosophy, I’m not a huge fan of end-of-the-world predictions because they tend not to come true (think Montanism back in the 2nd century; the 2012 Mayan calendar scare; or my personal favorite, the Prophet Hen of Leeds). On the other hand, the overall trend of decreased total sperm count in the English-speaking world seems to be true and it raises the interesting question of why.
According to the Mayo Clinic, causes of decreased sperm count include everything from anatomical factors (like varicoceles and ejaculatory issues) and lifestyle issues (such as recreational drugs, weight gain, and emotional stress) to environmental exposures (heavy metal or radiation). The senior author of the aforementioned meta-analysis, Shanna Swan, PhD, has championed another theory: the widespread exposure to endocrine-disrupting chemicals in everyday plastics.
It turns out that at least two chemicals used in the plastics industry, bisphenol A and phthalates, can mimic the effect of estrogen when ingested into the body. Even low levels of these chemicals in our bodies can lead to health problems.
Consider for a moment the presence of plastics in your life: the plastic wrappings on your food, plastic containers for shampoos and beauty products, and even the coatings of our oral supplements. A study by the Centers for Disease Control and Prevention looked at the urine of people participating in the National Health and Nutrition Examination Survey and found detectable concentrations of both of these chemicals in nearly all participants.
In 2045, I intend to be retired. But in the meantime, I think we all need to be aware of the potential impact that various endocrine-disrupting chemicals could be having on humanity. We need more research. If indeed the connection between endocrine disruptors and decreased sperm count is borne out, changes in our environmental exposure to these chemicals need to be made.
Henry Rosevear, MD, is a private-practice urologist based in Colorado Springs. He comes from a long line of doctors, but before entering medicine he served in the U.S. Navy as an officer aboard the USS Pittsburgh, a fast-attack submarine based out of New London, Conn. During his time in the Navy, he served in two deployments to the Persian Gulf, including combat experience as part of Operation Iraqi Freedom. Dr. Rosevear disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
In medical school, I remember thinking that telling a patient “you have cancer” would be the most professionally challenging phrase I would ever utter. And don’t get me wrong – it certainly isn’t easy; but, compared with telling someone “you are infertile,” it’s a cakewalk.
Maybe it’s because people “have” cancer and cancer is something you “fight.” Or maybe because, unlike infertility, cancer has become a part of public life (think lapel pins and support groups) and is now easier to accept. On the other hand, someone “is” infertile. The condition is a source of embarrassment for the couple and is often hidden from society.
Here’s another concerning point of contrast: While the overall rate of cancer death has declined since the early 1990s, infertility is increasing. Reports now show that one in six couples have problems conceiving and the use of assisted reproductive technologies is increasing by 5%-10% per year. Many theories exist to explain these trends, chief among them the rise in average maternal age and the increasing incidence of obesity, as well as various other male- and female-specific factors.
But interestingly, recent data suggest that the most male of all male-specific factors – total sperm count – may be specifically to blame.
According to a recent meta-analysis, the average total sperm count in men declined by 59.3% between 1973 and 2011. While these data certainly have limitations – including the exclusion of non-English publications, the reliance on total sperm count and not sperm motility, and the potential bias of those patients willing to give a semen sample – the overall trend nevertheless seems to be clearly downward. What’s more concerning, if you believe the data presented, is that there does not appear to be a leveling off of the downward curve in total sperm count.
Think about that last statement. At the current rate of decline, the average sperm count will be zero in 2045. One of the lead authors on the meta-analysis, Hagai Levine, MD, MPH, goes so far as to state, “We should hope for the best and prepare for the worst.”
As a matter of personal philosophy, I’m not a huge fan of end-of-the-world predictions because they tend not to come true (think Montanism back in the 2nd century; the 2012 Mayan calendar scare; or my personal favorite, the Prophet Hen of Leeds). On the other hand, the overall trend of decreased total sperm count in the English-speaking world seems to be true and it raises the interesting question of why.
According to the Mayo Clinic, causes of decreased sperm count include everything from anatomical factors (like varicoceles and ejaculatory issues) and lifestyle issues (such as recreational drugs, weight gain, and emotional stress) to environmental exposures (heavy metal or radiation). The senior author of the aforementioned meta-analysis, Shanna Swan, PhD, has championed another theory: the widespread exposure to endocrine-disrupting chemicals in everyday plastics.
It turns out that at least two chemicals used in the plastics industry, bisphenol A and phthalates, can mimic the effect of estrogen when ingested into the body. Even low levels of these chemicals in our bodies can lead to health problems.
Consider for a moment the presence of plastics in your life: the plastic wrappings on your food, plastic containers for shampoos and beauty products, and even the coatings of our oral supplements. A study by the Centers for Disease Control and Prevention looked at the urine of people participating in the National Health and Nutrition Examination Survey and found detectable concentrations of both of these chemicals in nearly all participants.
In 2045, I intend to be retired. But in the meantime, I think we all need to be aware of the potential impact that various endocrine-disrupting chemicals could be having on humanity. We need more research. If indeed the connection between endocrine disruptors and decreased sperm count is borne out, changes in our environmental exposure to these chemicals need to be made.
Henry Rosevear, MD, is a private-practice urologist based in Colorado Springs. He comes from a long line of doctors, but before entering medicine he served in the U.S. Navy as an officer aboard the USS Pittsburgh, a fast-attack submarine based out of New London, Conn. During his time in the Navy, he served in two deployments to the Persian Gulf, including combat experience as part of Operation Iraqi Freedom. Dr. Rosevear disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
In medical school, I remember thinking that telling a patient “you have cancer” would be the most professionally challenging phrase I would ever utter. And don’t get me wrong – it certainly isn’t easy; but, compared with telling someone “you are infertile,” it’s a cakewalk.
Maybe it’s because people “have” cancer and cancer is something you “fight.” Or maybe because, unlike infertility, cancer has become a part of public life (think lapel pins and support groups) and is now easier to accept. On the other hand, someone “is” infertile. The condition is a source of embarrassment for the couple and is often hidden from society.
Here’s another concerning point of contrast: While the overall rate of cancer death has declined since the early 1990s, infertility is increasing. Reports now show that one in six couples have problems conceiving and the use of assisted reproductive technologies is increasing by 5%-10% per year. Many theories exist to explain these trends, chief among them the rise in average maternal age and the increasing incidence of obesity, as well as various other male- and female-specific factors.
But interestingly, recent data suggest that the most male of all male-specific factors – total sperm count – may be specifically to blame.
According to a recent meta-analysis, the average total sperm count in men declined by 59.3% between 1973 and 2011. While these data certainly have limitations – including the exclusion of non-English publications, the reliance on total sperm count and not sperm motility, and the potential bias of those patients willing to give a semen sample – the overall trend nevertheless seems to be clearly downward. What’s more concerning, if you believe the data presented, is that there does not appear to be a leveling off of the downward curve in total sperm count.
Think about that last statement. At the current rate of decline, the average sperm count will be zero in 2045. One of the lead authors on the meta-analysis, Hagai Levine, MD, MPH, goes so far as to state, “We should hope for the best and prepare for the worst.”
As a matter of personal philosophy, I’m not a huge fan of end-of-the-world predictions because they tend not to come true (think Montanism back in the 2nd century; the 2012 Mayan calendar scare; or my personal favorite, the Prophet Hen of Leeds). On the other hand, the overall trend of decreased total sperm count in the English-speaking world seems to be true and it raises the interesting question of why.
According to the Mayo Clinic, causes of decreased sperm count include everything from anatomical factors (like varicoceles and ejaculatory issues) and lifestyle issues (such as recreational drugs, weight gain, and emotional stress) to environmental exposures (heavy metal or radiation). The senior author of the aforementioned meta-analysis, Shanna Swan, PhD, has championed another theory: the widespread exposure to endocrine-disrupting chemicals in everyday plastics.
It turns out that at least two chemicals used in the plastics industry, bisphenol A and phthalates, can mimic the effect of estrogen when ingested into the body. Even low levels of these chemicals in our bodies can lead to health problems.
Consider for a moment the presence of plastics in your life: the plastic wrappings on your food, plastic containers for shampoos and beauty products, and even the coatings of our oral supplements. A study by the Centers for Disease Control and Prevention looked at the urine of people participating in the National Health and Nutrition Examination Survey and found detectable concentrations of both of these chemicals in nearly all participants.
In 2045, I intend to be retired. But in the meantime, I think we all need to be aware of the potential impact that various endocrine-disrupting chemicals could be having on humanity. We need more research. If indeed the connection between endocrine disruptors and decreased sperm count is borne out, changes in our environmental exposure to these chemicals need to be made.
Henry Rosevear, MD, is a private-practice urologist based in Colorado Springs. He comes from a long line of doctors, but before entering medicine he served in the U.S. Navy as an officer aboard the USS Pittsburgh, a fast-attack submarine based out of New London, Conn. During his time in the Navy, he served in two deployments to the Persian Gulf, including combat experience as part of Operation Iraqi Freedom. Dr. Rosevear disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
Headache seen affecting some pregnancy outcomes
, according to results from an observational study.
Migraine during pregnancy has been associated in previous studies with hypertensive pregnancy complications including preeclampsia; however, little is known about other headache types and their effects on pregnancy and birth outcomes.
For their research, published online July 20 in Cephalalgia, Isabella Neri, MD, PhD, and colleagues at Hospital Policlinico of Modena, Italy, looked at headache status for 515 consecutive pregnant women evaluated during their first trimester and followed through childbirth.
Altogether 224 women, or 43.5% of the cohort, were diagnosed with migraine without aura (n = 72), migraine with aura (n = 27), or tension-type headache (n = 125). The authors did not report on the severity or frequency of headaches.
Women with migraine with aura and tension-type headache saw higher rates of small-for-gestational-age infants (25.9% and 10.4% of births, respectively) compared with 5.5% for women without headache. Women presenting with tension-type headache saw elevated risk for small-for-gestational-age infants (odds ratio [OR] 4.19, P = .004) as did women with migraine with aura (OR 5.37, P = .02).
Admission to neonatal intensive care was significantly higher in all the headache groups. However, the authors found no statistically significant associations between headaches and any other perinatal outcome investigated in the study, including gestational diabetes, placental abruption, gestational hypertension, and preterm delivery.
A previous study conducted by the same research group had reported a relationship between migraine and gestational hypertension. The authors cited the small sample size of the migraine groups in the current study, “the diverse features of the population,” and the popularity of low-dose aspirin administration as potentially affecting that outcome.
Interpret findings with caution
Asked by this news organization to comment on the research, two headache neurologists praised Dr. Neri and colleagues’ research for focusing on an understudied topic – but also said that the results would not change their practice unless replicated in larger studies.
Elizabeth W. Loder, MD, MPH, chief emeritus of the division of headache at Brigham and Women’s Faulkner Hospital in Boston, urged caution in interpreting the findings, particularly with regard to tension-type headache. “This study adds to information suggesting that pregnancy complications probably are higher in women who have migraine with aura, and there’s biological plausibility for that,” Dr. Loder said. “Having aura means you may have some vascular abnormalities and things that logically might be associated with an increased risk of small-for-gestational age infants.” But the small size of the migraine-with-aura group in this study – 27 women – and the fact that other perinatal outcomes measured in the study did not reach significance, allows for the possibility that the small-for-gestational-age findings were due to chance, Dr. Loder noted.
With tension-type headache, a biological rationale for small-for-gestational-age risk is more elusive, Dr. Loder said. “I would want to see that association replicated in another study before I thought that I needed to warn women with tension-type headache about this potential outcome. There’s lot of uncertainty here about the magnitude of the risk.”
While Dr. Neri and colleagues described the instruments used in their study to diagnose migraine and migraine with aura, they did not explain how tension-type headache was diagnosed.
Tension-type headache, while common, is still not well characterized, Dr. Loder noted, and may represent a heterogeneous condition or the milder end of a biological continuum that includes migraine with aura. Also, the group in the study had a higher prevalence of smoking, and though the authors made statistical adjustments for smoking status, “smokers are systematically different than people who aren’t in other ways that could be associated with these outcomes,” Dr. Loder said.
While the authors of the study suggested that interventions might be indicated for women with tension-type headache in pregnancy, “showing an association doesn’t necessarily mean that intervening would make a difference” on pregnancy outcomes, Dr. Loder said.
Amaal J. Starling, MD, of the Mayo Clinic in Phoenix, Ariz., said in an interview that she, too, appreciated that this study looked at pregnancy outcomes in the setting of headache disorders. “Unfortunately even though headache disorders and especially migraine affect women so much, we still know very little about migraine in pregnancy,” she said.
Dr. Starling noted that many women with migraine are discouraged by their health care providers from becoming pregnant, because of the false belief that migraine cannot be managed in pregnancy. In her own practice, she said, she treats many patients with severe headache who become pregnant and who require pharmacological intervention during pregnancy.
This does not mean she regards headache in pregnancy as innocent. “I want patients to be on high alert for changes in headache symptoms in pregnancy. If someone has worsening of headache or migraine or aura in the setting of pregnancy, we consider that a red flag,” potentially indicating complications such as high blood pressure, gestational hypertension, or a blood clot.
Like Dr. Loder, Dr. Starling said she was not surprised by Dr. Neri and colleagues’ finding that migraine with aura might impact pregnancy outcomes. “We know that migraine with aura has a lot of vascular abnormalities that underlie the pathogenesis,” she said.
Dr. Starling found the findings related to tension-type headache less convincing, not least because the diagnostic criteria for tension-type headache was not made clear in the study. “I view this as an exploratory study that says maybe there’s a signal here. A larger epidemiological study would need to be done to confirm or refute this data,” Dr. Starling said. Until the findings can be replicated, “this study would not affect my clinical practice in any way.”
Dr. Neri and colleagues described no outside funding for their research or financial conflicts of interest. Dr. Starling has received consulting fees from pharmaceutical manufacturers but reported no disclosures relevant to the study discussed. Dr. Loder reported no financial conflicts of interest.
, according to results from an observational study.
Migraine during pregnancy has been associated in previous studies with hypertensive pregnancy complications including preeclampsia; however, little is known about other headache types and their effects on pregnancy and birth outcomes.
For their research, published online July 20 in Cephalalgia, Isabella Neri, MD, PhD, and colleagues at Hospital Policlinico of Modena, Italy, looked at headache status for 515 consecutive pregnant women evaluated during their first trimester and followed through childbirth.
Altogether 224 women, or 43.5% of the cohort, were diagnosed with migraine without aura (n = 72), migraine with aura (n = 27), or tension-type headache (n = 125). The authors did not report on the severity or frequency of headaches.
Women with migraine with aura and tension-type headache saw higher rates of small-for-gestational-age infants (25.9% and 10.4% of births, respectively) compared with 5.5% for women without headache. Women presenting with tension-type headache saw elevated risk for small-for-gestational-age infants (odds ratio [OR] 4.19, P = .004) as did women with migraine with aura (OR 5.37, P = .02).
Admission to neonatal intensive care was significantly higher in all the headache groups. However, the authors found no statistically significant associations between headaches and any other perinatal outcome investigated in the study, including gestational diabetes, placental abruption, gestational hypertension, and preterm delivery.
A previous study conducted by the same research group had reported a relationship between migraine and gestational hypertension. The authors cited the small sample size of the migraine groups in the current study, “the diverse features of the population,” and the popularity of low-dose aspirin administration as potentially affecting that outcome.
Interpret findings with caution
Asked by this news organization to comment on the research, two headache neurologists praised Dr. Neri and colleagues’ research for focusing on an understudied topic – but also said that the results would not change their practice unless replicated in larger studies.
Elizabeth W. Loder, MD, MPH, chief emeritus of the division of headache at Brigham and Women’s Faulkner Hospital in Boston, urged caution in interpreting the findings, particularly with regard to tension-type headache. “This study adds to information suggesting that pregnancy complications probably are higher in women who have migraine with aura, and there’s biological plausibility for that,” Dr. Loder said. “Having aura means you may have some vascular abnormalities and things that logically might be associated with an increased risk of small-for-gestational age infants.” But the small size of the migraine-with-aura group in this study – 27 women – and the fact that other perinatal outcomes measured in the study did not reach significance, allows for the possibility that the small-for-gestational-age findings were due to chance, Dr. Loder noted.
With tension-type headache, a biological rationale for small-for-gestational-age risk is more elusive, Dr. Loder said. “I would want to see that association replicated in another study before I thought that I needed to warn women with tension-type headache about this potential outcome. There’s lot of uncertainty here about the magnitude of the risk.”
While Dr. Neri and colleagues described the instruments used in their study to diagnose migraine and migraine with aura, they did not explain how tension-type headache was diagnosed.
Tension-type headache, while common, is still not well characterized, Dr. Loder noted, and may represent a heterogeneous condition or the milder end of a biological continuum that includes migraine with aura. Also, the group in the study had a higher prevalence of smoking, and though the authors made statistical adjustments for smoking status, “smokers are systematically different than people who aren’t in other ways that could be associated with these outcomes,” Dr. Loder said.
While the authors of the study suggested that interventions might be indicated for women with tension-type headache in pregnancy, “showing an association doesn’t necessarily mean that intervening would make a difference” on pregnancy outcomes, Dr. Loder said.
Amaal J. Starling, MD, of the Mayo Clinic in Phoenix, Ariz., said in an interview that she, too, appreciated that this study looked at pregnancy outcomes in the setting of headache disorders. “Unfortunately even though headache disorders and especially migraine affect women so much, we still know very little about migraine in pregnancy,” she said.
Dr. Starling noted that many women with migraine are discouraged by their health care providers from becoming pregnant, because of the false belief that migraine cannot be managed in pregnancy. In her own practice, she said, she treats many patients with severe headache who become pregnant and who require pharmacological intervention during pregnancy.
This does not mean she regards headache in pregnancy as innocent. “I want patients to be on high alert for changes in headache symptoms in pregnancy. If someone has worsening of headache or migraine or aura in the setting of pregnancy, we consider that a red flag,” potentially indicating complications such as high blood pressure, gestational hypertension, or a blood clot.
Like Dr. Loder, Dr. Starling said she was not surprised by Dr. Neri and colleagues’ finding that migraine with aura might impact pregnancy outcomes. “We know that migraine with aura has a lot of vascular abnormalities that underlie the pathogenesis,” she said.
Dr. Starling found the findings related to tension-type headache less convincing, not least because the diagnostic criteria for tension-type headache was not made clear in the study. “I view this as an exploratory study that says maybe there’s a signal here. A larger epidemiological study would need to be done to confirm or refute this data,” Dr. Starling said. Until the findings can be replicated, “this study would not affect my clinical practice in any way.”
Dr. Neri and colleagues described no outside funding for their research or financial conflicts of interest. Dr. Starling has received consulting fees from pharmaceutical manufacturers but reported no disclosures relevant to the study discussed. Dr. Loder reported no financial conflicts of interest.
, according to results from an observational study.
Migraine during pregnancy has been associated in previous studies with hypertensive pregnancy complications including preeclampsia; however, little is known about other headache types and their effects on pregnancy and birth outcomes.
For their research, published online July 20 in Cephalalgia, Isabella Neri, MD, PhD, and colleagues at Hospital Policlinico of Modena, Italy, looked at headache status for 515 consecutive pregnant women evaluated during their first trimester and followed through childbirth.
Altogether 224 women, or 43.5% of the cohort, were diagnosed with migraine without aura (n = 72), migraine with aura (n = 27), or tension-type headache (n = 125). The authors did not report on the severity or frequency of headaches.
Women with migraine with aura and tension-type headache saw higher rates of small-for-gestational-age infants (25.9% and 10.4% of births, respectively) compared with 5.5% for women without headache. Women presenting with tension-type headache saw elevated risk for small-for-gestational-age infants (odds ratio [OR] 4.19, P = .004) as did women with migraine with aura (OR 5.37, P = .02).
Admission to neonatal intensive care was significantly higher in all the headache groups. However, the authors found no statistically significant associations between headaches and any other perinatal outcome investigated in the study, including gestational diabetes, placental abruption, gestational hypertension, and preterm delivery.
A previous study conducted by the same research group had reported a relationship between migraine and gestational hypertension. The authors cited the small sample size of the migraine groups in the current study, “the diverse features of the population,” and the popularity of low-dose aspirin administration as potentially affecting that outcome.
Interpret findings with caution
Asked by this news organization to comment on the research, two headache neurologists praised Dr. Neri and colleagues’ research for focusing on an understudied topic – but also said that the results would not change their practice unless replicated in larger studies.
Elizabeth W. Loder, MD, MPH, chief emeritus of the division of headache at Brigham and Women’s Faulkner Hospital in Boston, urged caution in interpreting the findings, particularly with regard to tension-type headache. “This study adds to information suggesting that pregnancy complications probably are higher in women who have migraine with aura, and there’s biological plausibility for that,” Dr. Loder said. “Having aura means you may have some vascular abnormalities and things that logically might be associated with an increased risk of small-for-gestational age infants.” But the small size of the migraine-with-aura group in this study – 27 women – and the fact that other perinatal outcomes measured in the study did not reach significance, allows for the possibility that the small-for-gestational-age findings were due to chance, Dr. Loder noted.
With tension-type headache, a biological rationale for small-for-gestational-age risk is more elusive, Dr. Loder said. “I would want to see that association replicated in another study before I thought that I needed to warn women with tension-type headache about this potential outcome. There’s lot of uncertainty here about the magnitude of the risk.”
While Dr. Neri and colleagues described the instruments used in their study to diagnose migraine and migraine with aura, they did not explain how tension-type headache was diagnosed.
Tension-type headache, while common, is still not well characterized, Dr. Loder noted, and may represent a heterogeneous condition or the milder end of a biological continuum that includes migraine with aura. Also, the group in the study had a higher prevalence of smoking, and though the authors made statistical adjustments for smoking status, “smokers are systematically different than people who aren’t in other ways that could be associated with these outcomes,” Dr. Loder said.
While the authors of the study suggested that interventions might be indicated for women with tension-type headache in pregnancy, “showing an association doesn’t necessarily mean that intervening would make a difference” on pregnancy outcomes, Dr. Loder said.
Amaal J. Starling, MD, of the Mayo Clinic in Phoenix, Ariz., said in an interview that she, too, appreciated that this study looked at pregnancy outcomes in the setting of headache disorders. “Unfortunately even though headache disorders and especially migraine affect women so much, we still know very little about migraine in pregnancy,” she said.
Dr. Starling noted that many women with migraine are discouraged by their health care providers from becoming pregnant, because of the false belief that migraine cannot be managed in pregnancy. In her own practice, she said, she treats many patients with severe headache who become pregnant and who require pharmacological intervention during pregnancy.
This does not mean she regards headache in pregnancy as innocent. “I want patients to be on high alert for changes in headache symptoms in pregnancy. If someone has worsening of headache or migraine or aura in the setting of pregnancy, we consider that a red flag,” potentially indicating complications such as high blood pressure, gestational hypertension, or a blood clot.
Like Dr. Loder, Dr. Starling said she was not surprised by Dr. Neri and colleagues’ finding that migraine with aura might impact pregnancy outcomes. “We know that migraine with aura has a lot of vascular abnormalities that underlie the pathogenesis,” she said.
Dr. Starling found the findings related to tension-type headache less convincing, not least because the diagnostic criteria for tension-type headache was not made clear in the study. “I view this as an exploratory study that says maybe there’s a signal here. A larger epidemiological study would need to be done to confirm or refute this data,” Dr. Starling said. Until the findings can be replicated, “this study would not affect my clinical practice in any way.”
Dr. Neri and colleagues described no outside funding for their research or financial conflicts of interest. Dr. Starling has received consulting fees from pharmaceutical manufacturers but reported no disclosures relevant to the study discussed. Dr. Loder reported no financial conflicts of interest.
FROM CEPHALALGIA
Toward a clearer risk model for postpartum psychosis
Postpartum depression, in many respects, has become a household term. Over the last decade, there has been increasing awareness of the importance of screening for postpartum depression, with increased systematic screening across clinical settings where care is delivered to women during pregnancy and the postpartum period. There have also been greater efforts to identify women who are suffering postpartum depression and to support them with appropriate clinical interventions, whether through psychotherapy and/or pharmacologic therapy. Clinical interventions are supplemented by the increasing awareness of the value of community-based support groups for women who are suffering from postpartum mood and anxiety disorders.
Despite the growing, appropriate focus on recognition and acute treatment of postpartum depression as well as assessing clinical outcomes for those who suffer from postpartum mood and anxiety disorders, less attention has been given to postpartum psychosis, the most severe form of postpartum depression. It is indeed, the least common postpartum psychiatric syndrome (1 in 1,000 births) and comes to public attention when there has been a tragedy during the acute postpartum period such as maternal suicide or infanticide. In this sense, postpartum psychosis is ironically an underappreciated clinical entity across America given its severity, the effect it has on longer-term psychiatric morbidity, and its effect on children and families.
Our group at the Center for Women’s Mental Health has been interested in postpartum psychosis for years and started the Postpartum Psychosis Project in an effort to better understand the phenomenology, course, treatment, outcome, and genomic underpinnings of postpartum psychosis. Risk factors that are well established for postpartum psychosis have been described and overwhelmingly include patients with bipolar disorder. The risk for recurrent postpartum psychosis in women who have had a previous episode is as great as 75%-90% in the absence of prophylactic intervention. With that said, we are extremely interested in understanding the etiology of postpartum psychosis. Various studies over the last 5 years have looked at a whole host of psychosocial as well as neurobiologic variables that may contribute to risk for postpartum psychosis, including dysregulation of the stress axis, heightened inflammation as well as a history of child adversity and heightened experience of stress during the perinatal period.
There have also been anecdotal reports during Virtual Rounds at the Center for Women’s Mental Health of higher recent rates of postpartum psychosis manifesting during the postpartum period. This is a clinical observation and has not been systematically studied. However, one can wonder whether the experience of the pandemic has constituted a stressor for at-risk women, tipping the scales toward women becoming ill, or whether clinicians are seeing this finding more because of our ability to observe it more within the context of the pandemic.
Precise quantification of risk for postpartum psychosis is complicated; as noted, women with bipolar disorder have a predictably high risk for getting ill during the postpartum period and many go on to have clinical courses consistent with recurrent bipolar disorder. However, there are other women who have circumscribed episodes of psychotic illness in the postpartum period who recover and are totally well without any evidence of psychiatric disorder until they have another child, at which time the risk for recurrence of postpartum psychosis is very high. Interest in developing a model of risk that could reliably predict an illness as serious as postpartum psychosis is on the minds of researchers around the world.
One recent study that highlights the multiple factors involved in risk of postpartum psychosis involved a prospective longitudinal study of a group of women who were followed across the peripartum period from the third trimester until 4 weeks postpartum. In this group, 51 women were at increased risk for postpartum psychosis based on their diagnosis of bipolar disorder, schizoaffective disorder, or a previous episode of postpartum psychosis. These women were matched with a control group with no past or current diagnosis of psychiatric disorder or family history of postpartum psychosis. The findings suggested that women at risk for postpartum psychosis who experienced a psychiatric relapse during the first 4 weeks postpartum relative to women at risk who remained well had histories of severe childhood adversity as well as biomarkers consistent with a dysregulated stress axis (a statistically higher daily cortisol level). This is consistent with other data that have implicated the complex role between psychosocial variables as well as neurobiologic variables, such as a dysregulation in the hypothalamic pituitary adrenal axis and other studies that suggest that dysregulated inflammatory status may also drive risk for postpartum psychosis (Hazelgrove K et al. Psychoneuroendocrinology. 2021 Jun. doi: 10.1016/j.psyneuen.2021.105218).
At the end of the day, postpartum psychosis is a psychiatric and obstetrical emergency. In our center, it is rare for women not to be hospitalized with this condition to ensure the safety of the mother as well as her newborn, and to also get her recompensated and functioning as quickly and as significantly as possible. However, an interesting extrapolation of the findings noted by Hazelgrove and colleagues is that it raises the question of what effective treatments might be used to mitigate risk for those at greatest risk for postpartum psychosis. For example, are there other treatments over and above the few effective ones that have been studied as prophylactic pharmacologic interventions that might mitigate risk for recurrence of an illness as serious as postpartum psychosis?
The data suggesting dysregulation of the stress axis as a predictor variable for risk in women vulnerable to postpartum psychosis opens an array of opportunities that are nonpharmacologic, such as mindfulness-based cognitive therapy or other interventions that help to modulate the stress axis. This is a terrific opportunity to have pharmacologic intervention meet nonpharmacologic intervention to potentially mitigate risk for postpartum psychosis with its attendant serious sequelae.
In our own work, where we are evaluating genomic data in an extremely well-characterized group of women with known histories of postpartum psychosis, we are interested to see if we can enhance understanding of the model of risk for postpartum psychosis by factoring in genomic underpinning, history of diagnosis, and psychosocial variables to optimally craft interventions for this population of at-risk women. This brings us one step closer to the future in women’s mental health, to the practice of “precision reproductive psychiatry,” matching interventions to specific presentations across perinatal populations.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
Postpartum depression, in many respects, has become a household term. Over the last decade, there has been increasing awareness of the importance of screening for postpartum depression, with increased systematic screening across clinical settings where care is delivered to women during pregnancy and the postpartum period. There have also been greater efforts to identify women who are suffering postpartum depression and to support them with appropriate clinical interventions, whether through psychotherapy and/or pharmacologic therapy. Clinical interventions are supplemented by the increasing awareness of the value of community-based support groups for women who are suffering from postpartum mood and anxiety disorders.
Despite the growing, appropriate focus on recognition and acute treatment of postpartum depression as well as assessing clinical outcomes for those who suffer from postpartum mood and anxiety disorders, less attention has been given to postpartum psychosis, the most severe form of postpartum depression. It is indeed, the least common postpartum psychiatric syndrome (1 in 1,000 births) and comes to public attention when there has been a tragedy during the acute postpartum period such as maternal suicide or infanticide. In this sense, postpartum psychosis is ironically an underappreciated clinical entity across America given its severity, the effect it has on longer-term psychiatric morbidity, and its effect on children and families.
Our group at the Center for Women’s Mental Health has been interested in postpartum psychosis for years and started the Postpartum Psychosis Project in an effort to better understand the phenomenology, course, treatment, outcome, and genomic underpinnings of postpartum psychosis. Risk factors that are well established for postpartum psychosis have been described and overwhelmingly include patients with bipolar disorder. The risk for recurrent postpartum psychosis in women who have had a previous episode is as great as 75%-90% in the absence of prophylactic intervention. With that said, we are extremely interested in understanding the etiology of postpartum psychosis. Various studies over the last 5 years have looked at a whole host of psychosocial as well as neurobiologic variables that may contribute to risk for postpartum psychosis, including dysregulation of the stress axis, heightened inflammation as well as a history of child adversity and heightened experience of stress during the perinatal period.
There have also been anecdotal reports during Virtual Rounds at the Center for Women’s Mental Health of higher recent rates of postpartum psychosis manifesting during the postpartum period. This is a clinical observation and has not been systematically studied. However, one can wonder whether the experience of the pandemic has constituted a stressor for at-risk women, tipping the scales toward women becoming ill, or whether clinicians are seeing this finding more because of our ability to observe it more within the context of the pandemic.
Precise quantification of risk for postpartum psychosis is complicated; as noted, women with bipolar disorder have a predictably high risk for getting ill during the postpartum period and many go on to have clinical courses consistent with recurrent bipolar disorder. However, there are other women who have circumscribed episodes of psychotic illness in the postpartum period who recover and are totally well without any evidence of psychiatric disorder until they have another child, at which time the risk for recurrence of postpartum psychosis is very high. Interest in developing a model of risk that could reliably predict an illness as serious as postpartum psychosis is on the minds of researchers around the world.
One recent study that highlights the multiple factors involved in risk of postpartum psychosis involved a prospective longitudinal study of a group of women who were followed across the peripartum period from the third trimester until 4 weeks postpartum. In this group, 51 women were at increased risk for postpartum psychosis based on their diagnosis of bipolar disorder, schizoaffective disorder, or a previous episode of postpartum psychosis. These women were matched with a control group with no past or current diagnosis of psychiatric disorder or family history of postpartum psychosis. The findings suggested that women at risk for postpartum psychosis who experienced a psychiatric relapse during the first 4 weeks postpartum relative to women at risk who remained well had histories of severe childhood adversity as well as biomarkers consistent with a dysregulated stress axis (a statistically higher daily cortisol level). This is consistent with other data that have implicated the complex role between psychosocial variables as well as neurobiologic variables, such as a dysregulation in the hypothalamic pituitary adrenal axis and other studies that suggest that dysregulated inflammatory status may also drive risk for postpartum psychosis (Hazelgrove K et al. Psychoneuroendocrinology. 2021 Jun. doi: 10.1016/j.psyneuen.2021.105218).
At the end of the day, postpartum psychosis is a psychiatric and obstetrical emergency. In our center, it is rare for women not to be hospitalized with this condition to ensure the safety of the mother as well as her newborn, and to also get her recompensated and functioning as quickly and as significantly as possible. However, an interesting extrapolation of the findings noted by Hazelgrove and colleagues is that it raises the question of what effective treatments might be used to mitigate risk for those at greatest risk for postpartum psychosis. For example, are there other treatments over and above the few effective ones that have been studied as prophylactic pharmacologic interventions that might mitigate risk for recurrence of an illness as serious as postpartum psychosis?
The data suggesting dysregulation of the stress axis as a predictor variable for risk in women vulnerable to postpartum psychosis opens an array of opportunities that are nonpharmacologic, such as mindfulness-based cognitive therapy or other interventions that help to modulate the stress axis. This is a terrific opportunity to have pharmacologic intervention meet nonpharmacologic intervention to potentially mitigate risk for postpartum psychosis with its attendant serious sequelae.
In our own work, where we are evaluating genomic data in an extremely well-characterized group of women with known histories of postpartum psychosis, we are interested to see if we can enhance understanding of the model of risk for postpartum psychosis by factoring in genomic underpinning, history of diagnosis, and psychosocial variables to optimally craft interventions for this population of at-risk women. This brings us one step closer to the future in women’s mental health, to the practice of “precision reproductive psychiatry,” matching interventions to specific presentations across perinatal populations.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
Postpartum depression, in many respects, has become a household term. Over the last decade, there has been increasing awareness of the importance of screening for postpartum depression, with increased systematic screening across clinical settings where care is delivered to women during pregnancy and the postpartum period. There have also been greater efforts to identify women who are suffering postpartum depression and to support them with appropriate clinical interventions, whether through psychotherapy and/or pharmacologic therapy. Clinical interventions are supplemented by the increasing awareness of the value of community-based support groups for women who are suffering from postpartum mood and anxiety disorders.
Despite the growing, appropriate focus on recognition and acute treatment of postpartum depression as well as assessing clinical outcomes for those who suffer from postpartum mood and anxiety disorders, less attention has been given to postpartum psychosis, the most severe form of postpartum depression. It is indeed, the least common postpartum psychiatric syndrome (1 in 1,000 births) and comes to public attention when there has been a tragedy during the acute postpartum period such as maternal suicide or infanticide. In this sense, postpartum psychosis is ironically an underappreciated clinical entity across America given its severity, the effect it has on longer-term psychiatric morbidity, and its effect on children and families.
Our group at the Center for Women’s Mental Health has been interested in postpartum psychosis for years and started the Postpartum Psychosis Project in an effort to better understand the phenomenology, course, treatment, outcome, and genomic underpinnings of postpartum psychosis. Risk factors that are well established for postpartum psychosis have been described and overwhelmingly include patients with bipolar disorder. The risk for recurrent postpartum psychosis in women who have had a previous episode is as great as 75%-90% in the absence of prophylactic intervention. With that said, we are extremely interested in understanding the etiology of postpartum psychosis. Various studies over the last 5 years have looked at a whole host of psychosocial as well as neurobiologic variables that may contribute to risk for postpartum psychosis, including dysregulation of the stress axis, heightened inflammation as well as a history of child adversity and heightened experience of stress during the perinatal period.
There have also been anecdotal reports during Virtual Rounds at the Center for Women’s Mental Health of higher recent rates of postpartum psychosis manifesting during the postpartum period. This is a clinical observation and has not been systematically studied. However, one can wonder whether the experience of the pandemic has constituted a stressor for at-risk women, tipping the scales toward women becoming ill, or whether clinicians are seeing this finding more because of our ability to observe it more within the context of the pandemic.
Precise quantification of risk for postpartum psychosis is complicated; as noted, women with bipolar disorder have a predictably high risk for getting ill during the postpartum period and many go on to have clinical courses consistent with recurrent bipolar disorder. However, there are other women who have circumscribed episodes of psychotic illness in the postpartum period who recover and are totally well without any evidence of psychiatric disorder until they have another child, at which time the risk for recurrence of postpartum psychosis is very high. Interest in developing a model of risk that could reliably predict an illness as serious as postpartum psychosis is on the minds of researchers around the world.
One recent study that highlights the multiple factors involved in risk of postpartum psychosis involved a prospective longitudinal study of a group of women who were followed across the peripartum period from the third trimester until 4 weeks postpartum. In this group, 51 women were at increased risk for postpartum psychosis based on their diagnosis of bipolar disorder, schizoaffective disorder, or a previous episode of postpartum psychosis. These women were matched with a control group with no past or current diagnosis of psychiatric disorder or family history of postpartum psychosis. The findings suggested that women at risk for postpartum psychosis who experienced a psychiatric relapse during the first 4 weeks postpartum relative to women at risk who remained well had histories of severe childhood adversity as well as biomarkers consistent with a dysregulated stress axis (a statistically higher daily cortisol level). This is consistent with other data that have implicated the complex role between psychosocial variables as well as neurobiologic variables, such as a dysregulation in the hypothalamic pituitary adrenal axis and other studies that suggest that dysregulated inflammatory status may also drive risk for postpartum psychosis (Hazelgrove K et al. Psychoneuroendocrinology. 2021 Jun. doi: 10.1016/j.psyneuen.2021.105218).
At the end of the day, postpartum psychosis is a psychiatric and obstetrical emergency. In our center, it is rare for women not to be hospitalized with this condition to ensure the safety of the mother as well as her newborn, and to also get her recompensated and functioning as quickly and as significantly as possible. However, an interesting extrapolation of the findings noted by Hazelgrove and colleagues is that it raises the question of what effective treatments might be used to mitigate risk for those at greatest risk for postpartum psychosis. For example, are there other treatments over and above the few effective ones that have been studied as prophylactic pharmacologic interventions that might mitigate risk for recurrence of an illness as serious as postpartum psychosis?
The data suggesting dysregulation of the stress axis as a predictor variable for risk in women vulnerable to postpartum psychosis opens an array of opportunities that are nonpharmacologic, such as mindfulness-based cognitive therapy or other interventions that help to modulate the stress axis. This is a terrific opportunity to have pharmacologic intervention meet nonpharmacologic intervention to potentially mitigate risk for postpartum psychosis with its attendant serious sequelae.
In our own work, where we are evaluating genomic data in an extremely well-characterized group of women with known histories of postpartum psychosis, we are interested to see if we can enhance understanding of the model of risk for postpartum psychosis by factoring in genomic underpinning, history of diagnosis, and psychosocial variables to optimally craft interventions for this population of at-risk women. This brings us one step closer to the future in women’s mental health, to the practice of “precision reproductive psychiatry,” matching interventions to specific presentations across perinatal populations.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
Preterm and early term birth linked to an increased risk of autism
Preterm and early birth is associated with an increased risk of autism independent of genetic or environmental factors, according to new research published in Pediatrics.
Although previous studies have linked preterm births to an increased risk of autism – one 2017 study published in Cerebral Cortex found that 27.4% of the children born extremely preterm were diagnosed with autism – Casey Crump, MD, PhD, said potential causality, sex-specific differences, and association with early-term births were still unclear.
“Preterm birth had previously been linked with higher risk of autism; however, several important questions remained unanswered,” said Dr. Crump, professor and vice chair for research at the department of family medicine and community health and professor of epidemiology in the department of population health science and policy at Icahn School of Medicine at Mount Sinai New York. “To our knowledge, [our study] is the largest to date of gestational age at birth in relation to autism, and one of the first to investigate sex-specific differences, early term birth, or the influence of shared familial factors.”
Dr. Crump and colleagues examined data from more than 4 million infants born in Sweden between 1973 and 2013 who were followed-up for autism spectrum disorder identified from nationwide outpatient and inpatient diagnoses through December 2015. Children born between 22 and 27 weeks were considered extremely preterm, those born between 28 and 33 week were characterized as very to moderate preterm, and those born between 34 and 36 weeks were considered late preterm. Early-term births are characterized as infants born between 37 and 38 weeks and children born between 39 and 41 weeks were considered term births.
They found that 6.1% of those born extremely preterm were diagnosed with autism. Meanwhile, autism spectrum disorder prevalences were 2.6% for very to moderate preterm, 1.9% for late preterm, 2.1% for all preterm, and 1.6% for early term, compared with 1.4% for term birth.
The researchers’ analysis showed that preterm and early birth were associated with a significantly increased risk of autism in males and females. Children who were born extremely preterm had an approximately fourfold increased risk of autism. Researchers also found that each additional week of gestation was associated with a 5% lower prevalence of autism spectrum disorder (ASD) on average.
“The elevated risk even in [late preterm] infants is not completely surprising because a number of investigators have shown higher incidences of early cognitive, language motor and impairment, and school problems ... and psychiatric disorders, some of which may extend to adulthood,” Elisabeth McGowan, MD, who was not involved in the study, said in a solicited editorial commentary about the study.
Dr. Crump believes the association between preterm birth and autism may be because of increased inflammatory marker levels. A 2009 study published in Reproductive Sciences found that increased proinflammatory cytokine levels have been associated with the timing and initiation of preterm birth, and also have been detected in the brain and cerebrospinal fluid of individuals with autism “and may play a key role in its pathogenesis,” Dr. Crump said.
“Inflammatory-driven alteration of neuronal connections during critical periods of brain development may be central to the development of autism,” Dr. Crump explained.
However, Dr. Crump said that, although the relative risks of autism were higher in those born preterm, the absolute risk of the condition is low.
“The report by Crump is in many ways a definitive accounting of the elevated rates of ASD in preterm infants,” said Dr. McGowan, associate professor of pediatrics at the Women and Infants Hospital, Providence, R.I. “And although the impact of prematurity on brain development may be part of the causal chain resulting in ASD (or other neurodevelopmental outcomes), these factors are operating in a complex biological landscape, with pathways to ASD outcomes that can be expected to be heterogeneous.”
ASD is a developmental condition that affects about 1 in 54 children, according to the Centers for Disease Control and Prevention. Many children are not diagnosed with ASD until later in childhood, which in some cases delays treatment and early intervention. ASD may be detected as early as 18 months, but the average age of diagnosis for ASD is 4.3 years, according to the CDC.
“Children born prematurely need early evaluation and long-term follow-up to facilitate timely detection and treatment of autism, especially those born at the earliest gestational ages,” Dr. Crump said in an interview. “In patients of all ages, gestational age at birth should be routinely included in history-taking and medical records to help identify in clinical practice those born preterm or early term. Such information can provide additional valuable context for understanding patients’ health and may facilitate earlier evaluation for autism and other neurodevelopmental conditions in those born prematurely.”
Dr. Crump and colleagues said more research is needed to understand the biologic mechanisms linking preterm birth with higher risks of autism, which “may reveal new targets for intervention at critical windows of neurodevelopment to improve the disease trajectory.”
Experts interviewed did not disclose any relevant financial relationships.
Preterm and early birth is associated with an increased risk of autism independent of genetic or environmental factors, according to new research published in Pediatrics.
Although previous studies have linked preterm births to an increased risk of autism – one 2017 study published in Cerebral Cortex found that 27.4% of the children born extremely preterm were diagnosed with autism – Casey Crump, MD, PhD, said potential causality, sex-specific differences, and association with early-term births were still unclear.
“Preterm birth had previously been linked with higher risk of autism; however, several important questions remained unanswered,” said Dr. Crump, professor and vice chair for research at the department of family medicine and community health and professor of epidemiology in the department of population health science and policy at Icahn School of Medicine at Mount Sinai New York. “To our knowledge, [our study] is the largest to date of gestational age at birth in relation to autism, and one of the first to investigate sex-specific differences, early term birth, or the influence of shared familial factors.”
Dr. Crump and colleagues examined data from more than 4 million infants born in Sweden between 1973 and 2013 who were followed-up for autism spectrum disorder identified from nationwide outpatient and inpatient diagnoses through December 2015. Children born between 22 and 27 weeks were considered extremely preterm, those born between 28 and 33 week were characterized as very to moderate preterm, and those born between 34 and 36 weeks were considered late preterm. Early-term births are characterized as infants born between 37 and 38 weeks and children born between 39 and 41 weeks were considered term births.
They found that 6.1% of those born extremely preterm were diagnosed with autism. Meanwhile, autism spectrum disorder prevalences were 2.6% for very to moderate preterm, 1.9% for late preterm, 2.1% for all preterm, and 1.6% for early term, compared with 1.4% for term birth.
The researchers’ analysis showed that preterm and early birth were associated with a significantly increased risk of autism in males and females. Children who were born extremely preterm had an approximately fourfold increased risk of autism. Researchers also found that each additional week of gestation was associated with a 5% lower prevalence of autism spectrum disorder (ASD) on average.
“The elevated risk even in [late preterm] infants is not completely surprising because a number of investigators have shown higher incidences of early cognitive, language motor and impairment, and school problems ... and psychiatric disorders, some of which may extend to adulthood,” Elisabeth McGowan, MD, who was not involved in the study, said in a solicited editorial commentary about the study.
Dr. Crump believes the association between preterm birth and autism may be because of increased inflammatory marker levels. A 2009 study published in Reproductive Sciences found that increased proinflammatory cytokine levels have been associated with the timing and initiation of preterm birth, and also have been detected in the brain and cerebrospinal fluid of individuals with autism “and may play a key role in its pathogenesis,” Dr. Crump said.
“Inflammatory-driven alteration of neuronal connections during critical periods of brain development may be central to the development of autism,” Dr. Crump explained.
However, Dr. Crump said that, although the relative risks of autism were higher in those born preterm, the absolute risk of the condition is low.
“The report by Crump is in many ways a definitive accounting of the elevated rates of ASD in preterm infants,” said Dr. McGowan, associate professor of pediatrics at the Women and Infants Hospital, Providence, R.I. “And although the impact of prematurity on brain development may be part of the causal chain resulting in ASD (or other neurodevelopmental outcomes), these factors are operating in a complex biological landscape, with pathways to ASD outcomes that can be expected to be heterogeneous.”
ASD is a developmental condition that affects about 1 in 54 children, according to the Centers for Disease Control and Prevention. Many children are not diagnosed with ASD until later in childhood, which in some cases delays treatment and early intervention. ASD may be detected as early as 18 months, but the average age of diagnosis for ASD is 4.3 years, according to the CDC.
“Children born prematurely need early evaluation and long-term follow-up to facilitate timely detection and treatment of autism, especially those born at the earliest gestational ages,” Dr. Crump said in an interview. “In patients of all ages, gestational age at birth should be routinely included in history-taking and medical records to help identify in clinical practice those born preterm or early term. Such information can provide additional valuable context for understanding patients’ health and may facilitate earlier evaluation for autism and other neurodevelopmental conditions in those born prematurely.”
Dr. Crump and colleagues said more research is needed to understand the biologic mechanisms linking preterm birth with higher risks of autism, which “may reveal new targets for intervention at critical windows of neurodevelopment to improve the disease trajectory.”
Experts interviewed did not disclose any relevant financial relationships.
Preterm and early birth is associated with an increased risk of autism independent of genetic or environmental factors, according to new research published in Pediatrics.
Although previous studies have linked preterm births to an increased risk of autism – one 2017 study published in Cerebral Cortex found that 27.4% of the children born extremely preterm were diagnosed with autism – Casey Crump, MD, PhD, said potential causality, sex-specific differences, and association with early-term births were still unclear.
“Preterm birth had previously been linked with higher risk of autism; however, several important questions remained unanswered,” said Dr. Crump, professor and vice chair for research at the department of family medicine and community health and professor of epidemiology in the department of population health science and policy at Icahn School of Medicine at Mount Sinai New York. “To our knowledge, [our study] is the largest to date of gestational age at birth in relation to autism, and one of the first to investigate sex-specific differences, early term birth, or the influence of shared familial factors.”
Dr. Crump and colleagues examined data from more than 4 million infants born in Sweden between 1973 and 2013 who were followed-up for autism spectrum disorder identified from nationwide outpatient and inpatient diagnoses through December 2015. Children born between 22 and 27 weeks were considered extremely preterm, those born between 28 and 33 week were characterized as very to moderate preterm, and those born between 34 and 36 weeks were considered late preterm. Early-term births are characterized as infants born between 37 and 38 weeks and children born between 39 and 41 weeks were considered term births.
They found that 6.1% of those born extremely preterm were diagnosed with autism. Meanwhile, autism spectrum disorder prevalences were 2.6% for very to moderate preterm, 1.9% for late preterm, 2.1% for all preterm, and 1.6% for early term, compared with 1.4% for term birth.
The researchers’ analysis showed that preterm and early birth were associated with a significantly increased risk of autism in males and females. Children who were born extremely preterm had an approximately fourfold increased risk of autism. Researchers also found that each additional week of gestation was associated with a 5% lower prevalence of autism spectrum disorder (ASD) on average.
“The elevated risk even in [late preterm] infants is not completely surprising because a number of investigators have shown higher incidences of early cognitive, language motor and impairment, and school problems ... and psychiatric disorders, some of which may extend to adulthood,” Elisabeth McGowan, MD, who was not involved in the study, said in a solicited editorial commentary about the study.
Dr. Crump believes the association between preterm birth and autism may be because of increased inflammatory marker levels. A 2009 study published in Reproductive Sciences found that increased proinflammatory cytokine levels have been associated with the timing and initiation of preterm birth, and also have been detected in the brain and cerebrospinal fluid of individuals with autism “and may play a key role in its pathogenesis,” Dr. Crump said.
“Inflammatory-driven alteration of neuronal connections during critical periods of brain development may be central to the development of autism,” Dr. Crump explained.
However, Dr. Crump said that, although the relative risks of autism were higher in those born preterm, the absolute risk of the condition is low.
“The report by Crump is in many ways a definitive accounting of the elevated rates of ASD in preterm infants,” said Dr. McGowan, associate professor of pediatrics at the Women and Infants Hospital, Providence, R.I. “And although the impact of prematurity on brain development may be part of the causal chain resulting in ASD (or other neurodevelopmental outcomes), these factors are operating in a complex biological landscape, with pathways to ASD outcomes that can be expected to be heterogeneous.”
ASD is a developmental condition that affects about 1 in 54 children, according to the Centers for Disease Control and Prevention. Many children are not diagnosed with ASD until later in childhood, which in some cases delays treatment and early intervention. ASD may be detected as early as 18 months, but the average age of diagnosis for ASD is 4.3 years, according to the CDC.
“Children born prematurely need early evaluation and long-term follow-up to facilitate timely detection and treatment of autism, especially those born at the earliest gestational ages,” Dr. Crump said in an interview. “In patients of all ages, gestational age at birth should be routinely included in history-taking and medical records to help identify in clinical practice those born preterm or early term. Such information can provide additional valuable context for understanding patients’ health and may facilitate earlier evaluation for autism and other neurodevelopmental conditions in those born prematurely.”
Dr. Crump and colleagues said more research is needed to understand the biologic mechanisms linking preterm birth with higher risks of autism, which “may reveal new targets for intervention at critical windows of neurodevelopment to improve the disease trajectory.”
Experts interviewed did not disclose any relevant financial relationships.
FROM PEDIATRICS
‘Reassuring’ findings for second-generation antipsychotics during pregnancy
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.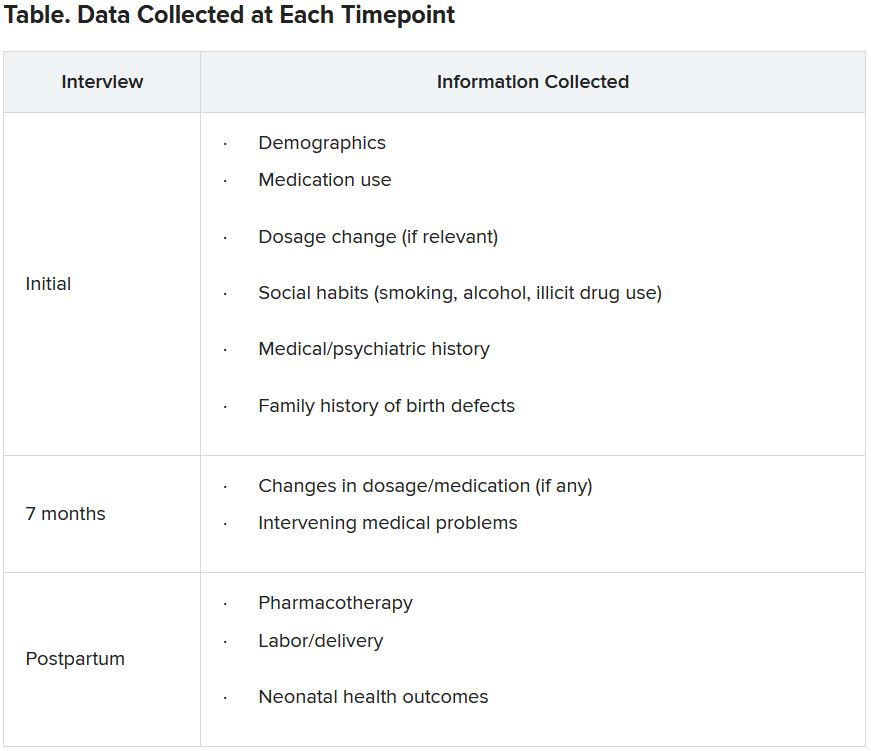
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.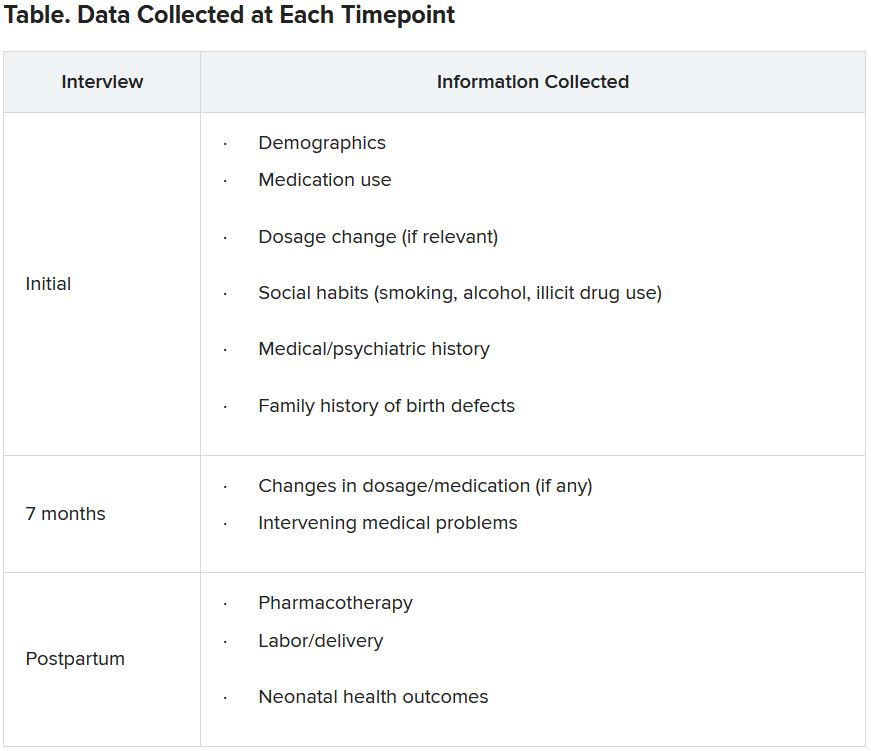
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.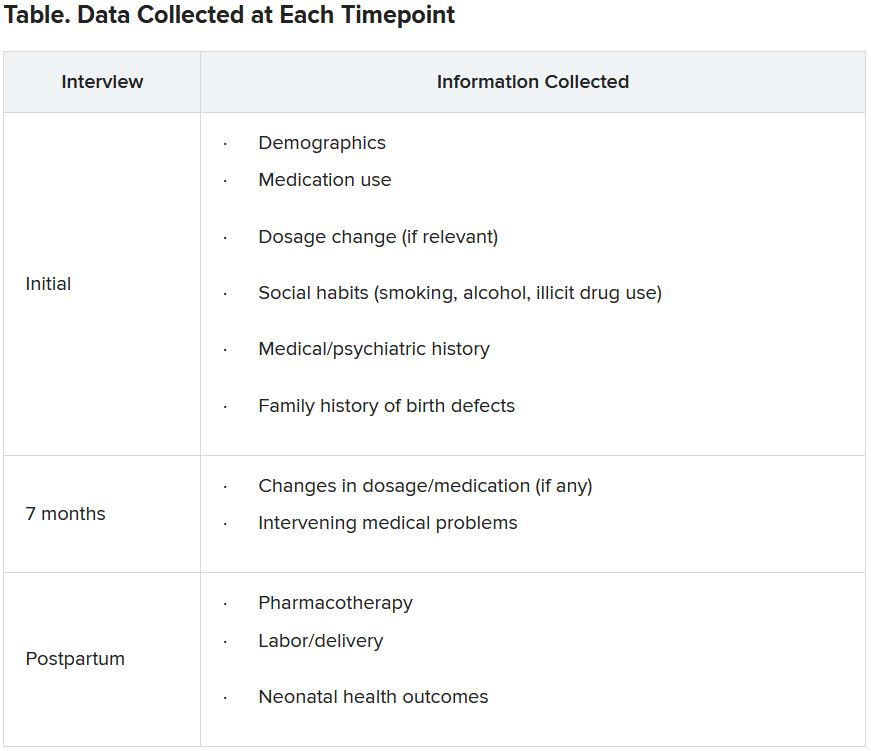
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.