User login
Clean Up Your Revenue Cycle Now: 6 Survival Tips for ICD-10–Induced Payment Slowdowns
Analysis of Intermediate Outcomes of Glenoid Bone Grafting in Revision Shoulder Arthroplasty
The Applications of Biologics in Orthopedic Surgery
As orthopedic surgeons, we have done a great job continually trying to improve the outcomes of our patients. During the first decade of the 21st century, many of these advances centered on strengthening the biomechanics of constructs used to repair patients’ pathologies. Trauma surgeons incorporated minimally invasive osteosynthesis with locked plates; shoulder surgeons began using double-row and transosseous-equivalent rotator cuff repairs. As a result of these shifts in treatment methods, healing rates and outcomes have improved. Unfortunately, to take rotator cuff repair as an example, healing rates have still not achieved 100%. To reach this goal in the future, biologic manipulation of the healing milieu will play a critical role.
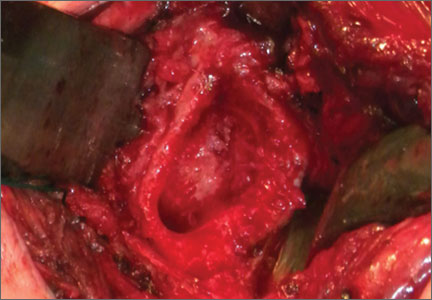
This issue of The American Journal of Orthopedics features an article on the “Analysis of Intermediate Outcomes of Glenoid Bone Grafting in Revision Shoulder Arthroplasty” by Dr. Schubkegel and colleagues. While not as cutting edge or in vogue as growth factors or stem cells, bone graft is one of the original biologics used by orthopedic surgeons. The authors review the midterm results of glenoid bone grafting secondary to failed total shoulder arthroplasty and find that bone grafting resulted in good functional outcomes. Studies such as this one highlight the important role that biologics play, particularly in challenging or revision cases.
Platelet-rich plasma (PRP) is another biologic that is presently available for use. Reviewing its use as it pertains to orthopedics highlights both the potential benefits
as well as the difficulties associated with incorporating biologics into everyday practice. In 2006, Mishra and colleagues1 published one of the first studies that looked at the potential benefits of using PRP to treat lateral epicondylitis. While, from a purist’s standpoint, it wasn’t the best-designed study, it did provide cause for optimism with regard to a novel treatment option for an age-old problem. Since that time, hundreds of studies have been done on PRP looking at its potential treatment uses in everything from tennis elbow to rotator cuff repairs.
Study designs have improved, and with that, so have our indications for using PRP. Interestingly though, the more we study PRP (and other exogenous growth factors), it almost seems as if more questions are raised than answered. For instance, preparing PRP from a given patient will result in different concentrations of the PRP depending on what time of the day the patient’s blood is drawn. What is the ideal time to prepare the PRP? Additionally, PRP prepared using different companies’ systems results in different concentrations of growth factors. So, not only is a given patient’s PRP different at different times of day, but these differences get magnified by using different preparation systems.
One of the main issues with tendon healing is that the tissue heals via reactive scar formation instead of truly regenerating new tendon. In this scenario, it is possible that adding PRP or other growth factors to the repair construct may only increase scar formation. Along these lines, newer work is focusing on cellular solutions to healing problems. Stem cells, which are undifferentiated, unspecialized cells, have shown potential to improve healing when added to injury/repair sites. Thus far, unfortunately, there is very little clinical data pertaining to their use in orthopedic surgery. Compounding this problem are the US Food and Drug Administration’s regulations on manipulating stem cells.
In the future, it is likely that growth factors, cytokines, PRP, and cellular approaches will be used to enhance healing. For now, a significant amount of preclinical work is being done to figure out the most advantageous ways to use such adjuvants. This is an extremely exciting field with ample opportunities to
answer well-designed research questions. Future issues of this journal will likely highlight such studies. ◾
Reference
1. Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered
platelet-rich plasma. Am J Sports Med. 2006;34(11):1774-1778.
As orthopedic surgeons, we have done a great job continually trying to improve the outcomes of our patients. During the first decade of the 21st century, many of these advances centered on strengthening the biomechanics of constructs used to repair patients’ pathologies. Trauma surgeons incorporated minimally invasive osteosynthesis with locked plates; shoulder surgeons began using double-row and transosseous-equivalent rotator cuff repairs. As a result of these shifts in treatment methods, healing rates and outcomes have improved. Unfortunately, to take rotator cuff repair as an example, healing rates have still not achieved 100%. To reach this goal in the future, biologic manipulation of the healing milieu will play a critical role.
This issue of The American Journal of Orthopedics features an article on the “Analysis of Intermediate Outcomes of Glenoid Bone Grafting in Revision Shoulder Arthroplasty” by Dr. Schubkegel and colleagues. While not as cutting edge or in vogue as growth factors or stem cells, bone graft is one of the original biologics used by orthopedic surgeons. The authors review the midterm results of glenoid bone grafting secondary to failed total shoulder arthroplasty and find that bone grafting resulted in good functional outcomes. Studies such as this one highlight the important role that biologics play, particularly in challenging or revision cases.
Platelet-rich plasma (PRP) is another biologic that is presently available for use. Reviewing its use as it pertains to orthopedics highlights both the potential benefits
as well as the difficulties associated with incorporating biologics into everyday practice. In 2006, Mishra and colleagues1 published one of the first studies that looked at the potential benefits of using PRP to treat lateral epicondylitis. While, from a purist’s standpoint, it wasn’t the best-designed study, it did provide cause for optimism with regard to a novel treatment option for an age-old problem. Since that time, hundreds of studies have been done on PRP looking at its potential treatment uses in everything from tennis elbow to rotator cuff repairs.
Study designs have improved, and with that, so have our indications for using PRP. Interestingly though, the more we study PRP (and other exogenous growth factors), it almost seems as if more questions are raised than answered. For instance, preparing PRP from a given patient will result in different concentrations of the PRP depending on what time of the day the patient’s blood is drawn. What is the ideal time to prepare the PRP? Additionally, PRP prepared using different companies’ systems results in different concentrations of growth factors. So, not only is a given patient’s PRP different at different times of day, but these differences get magnified by using different preparation systems.
One of the main issues with tendon healing is that the tissue heals via reactive scar formation instead of truly regenerating new tendon. In this scenario, it is possible that adding PRP or other growth factors to the repair construct may only increase scar formation. Along these lines, newer work is focusing on cellular solutions to healing problems. Stem cells, which are undifferentiated, unspecialized cells, have shown potential to improve healing when added to injury/repair sites. Thus far, unfortunately, there is very little clinical data pertaining to their use in orthopedic surgery. Compounding this problem are the US Food and Drug Administration’s regulations on manipulating stem cells.
In the future, it is likely that growth factors, cytokines, PRP, and cellular approaches will be used to enhance healing. For now, a significant amount of preclinical work is being done to figure out the most advantageous ways to use such adjuvants. This is an extremely exciting field with ample opportunities to
answer well-designed research questions. Future issues of this journal will likely highlight such studies. ◾
Reference
1. Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered
platelet-rich plasma. Am J Sports Med. 2006;34(11):1774-1778.
As orthopedic surgeons, we have done a great job continually trying to improve the outcomes of our patients. During the first decade of the 21st century, many of these advances centered on strengthening the biomechanics of constructs used to repair patients’ pathologies. Trauma surgeons incorporated minimally invasive osteosynthesis with locked plates; shoulder surgeons began using double-row and transosseous-equivalent rotator cuff repairs. As a result of these shifts in treatment methods, healing rates and outcomes have improved. Unfortunately, to take rotator cuff repair as an example, healing rates have still not achieved 100%. To reach this goal in the future, biologic manipulation of the healing milieu will play a critical role.
This issue of The American Journal of Orthopedics features an article on the “Analysis of Intermediate Outcomes of Glenoid Bone Grafting in Revision Shoulder Arthroplasty” by Dr. Schubkegel and colleagues. While not as cutting edge or in vogue as growth factors or stem cells, bone graft is one of the original biologics used by orthopedic surgeons. The authors review the midterm results of glenoid bone grafting secondary to failed total shoulder arthroplasty and find that bone grafting resulted in good functional outcomes. Studies such as this one highlight the important role that biologics play, particularly in challenging or revision cases.
Platelet-rich plasma (PRP) is another biologic that is presently available for use. Reviewing its use as it pertains to orthopedics highlights both the potential benefits
as well as the difficulties associated with incorporating biologics into everyday practice. In 2006, Mishra and colleagues1 published one of the first studies that looked at the potential benefits of using PRP to treat lateral epicondylitis. While, from a purist’s standpoint, it wasn’t the best-designed study, it did provide cause for optimism with regard to a novel treatment option for an age-old problem. Since that time, hundreds of studies have been done on PRP looking at its potential treatment uses in everything from tennis elbow to rotator cuff repairs.
Study designs have improved, and with that, so have our indications for using PRP. Interestingly though, the more we study PRP (and other exogenous growth factors), it almost seems as if more questions are raised than answered. For instance, preparing PRP from a given patient will result in different concentrations of the PRP depending on what time of the day the patient’s blood is drawn. What is the ideal time to prepare the PRP? Additionally, PRP prepared using different companies’ systems results in different concentrations of growth factors. So, not only is a given patient’s PRP different at different times of day, but these differences get magnified by using different preparation systems.
One of the main issues with tendon healing is that the tissue heals via reactive scar formation instead of truly regenerating new tendon. In this scenario, it is possible that adding PRP or other growth factors to the repair construct may only increase scar formation. Along these lines, newer work is focusing on cellular solutions to healing problems. Stem cells, which are undifferentiated, unspecialized cells, have shown potential to improve healing when added to injury/repair sites. Thus far, unfortunately, there is very little clinical data pertaining to their use in orthopedic surgery. Compounding this problem are the US Food and Drug Administration’s regulations on manipulating stem cells.
In the future, it is likely that growth factors, cytokines, PRP, and cellular approaches will be used to enhance healing. For now, a significant amount of preclinical work is being done to figure out the most advantageous ways to use such adjuvants. This is an extremely exciting field with ample opportunities to
answer well-designed research questions. Future issues of this journal will likely highlight such studies. ◾
Reference
1. Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered
platelet-rich plasma. Am J Sports Med. 2006;34(11):1774-1778.
Intraoperative wound anesthetic cut chronic pain after hip replacement
PARIS – Adding local anesthetic to the wound during total hip replacement surgery for osteoarthritis reduced chronic pain, according to a double-blind, randomized controlled trial.
At 12 months postoperative, the number of patients with severe pain was 8.6% with standard care, compared with 1.4% among those who also received 60 mL of 0.25% bupivacaine with lidocaine (Xylocaine) 1% with adrenaline 100 mcg/20 mL injected directly into the wound prior to closure.
The difference was statistically significant (P = .004; odds ratio, 10.19), but the confidence intervals were wide (95% C.I., 2.10-49.55) because of the small number of patients with severe pain, Vikki Wylde, Ph.D., said at the World Congress on Osteoarthritis.
She noted that 7%-23% of patients report moderate to severe chronic pain in the long term after total hip replacement, according to a recent systematic review (BMJ Open 2012:2:e000435), and that the severity of postoperative pain is a known risk factor for chronic postsurgical pain.
Local anesthetic wound infiltration has been shown to be effective at reducing the severity of acute postoperative pain after total hip replacement (J. Am Coll. Surg. 2006:203:914-32), but this is the first double-blind trial to assess its long-term effects.
Investigators at high-volume orthopedic centers in the United Kingdom randomly assigned 322 patients undergoing total hip replacement for osteoarthritis to standard care (spinal anesthesia with or without general anesthesia) alone or with local anesthetic infiltration. The primary outcome was WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) pain scale scores at 12 months postoperatively.
Use of in-patient analgesia or length of hospitalization did not differ between the groups, said Dr. Wylde, a research associate with the University of Bristol, England. Acute postoperative pain severity was also similar, except that patients in the intervention group reported less severe pain on postoperative night 2 (P = .008). This was unexpected, but the study was not powered to detect differences in these secondary measures, and no conclusions can be drawn from these data, she said at the meeting, sponsored by the Osteoarthritis Research Society International.
There were no differences in other secondary measures including the WOMAC function or stiffness scales or in ICOAP (Intermittent and Constant Osteoarthritis Pain) scores.
Local anesthetic infiltration, however, significantly reduced neuropathic pain at 12 months, as assessed using the PainDETECT questionnaire, Dr. Wylde said.
"Our study suggests that local anesthetic infiltration is unlikely to change long-term pain outcomes for the majority of patients, but potentially can improve pain relief for a small number of patients who may otherwise go on to develop severe long-term pain after surgery," she concluded.
In a separate interview, Dr. Jeffrey Katz, codirector, Brigham Spine Center, Brigham & Women’s Hospital and professor at Harvard Medical School, both in Boston, said the study was very interesting mechanistically and potentially interesting from a public health standpoint because there are about 400,000 hips done a year in the United States and thus 4,000 or so of these patients are having chronic pain. Moreover, the problem of chronic pain after surgery is even more common in the knee than in the hip.
"The difference in severe pain of 8% vs. 1% or 2% is a striking difference, but it’s a small incidence, and so it does bear replication," he added. "I thought it was a very exciting study and think it’s important information for folks to begin to work with and might change practice."
Dr. Wylde reported funding from the National Institute for Health Research, London.
PARIS – Adding local anesthetic to the wound during total hip replacement surgery for osteoarthritis reduced chronic pain, according to a double-blind, randomized controlled trial.
At 12 months postoperative, the number of patients with severe pain was 8.6% with standard care, compared with 1.4% among those who also received 60 mL of 0.25% bupivacaine with lidocaine (Xylocaine) 1% with adrenaline 100 mcg/20 mL injected directly into the wound prior to closure.
The difference was statistically significant (P = .004; odds ratio, 10.19), but the confidence intervals were wide (95% C.I., 2.10-49.55) because of the small number of patients with severe pain, Vikki Wylde, Ph.D., said at the World Congress on Osteoarthritis.
She noted that 7%-23% of patients report moderate to severe chronic pain in the long term after total hip replacement, according to a recent systematic review (BMJ Open 2012:2:e000435), and that the severity of postoperative pain is a known risk factor for chronic postsurgical pain.
Local anesthetic wound infiltration has been shown to be effective at reducing the severity of acute postoperative pain after total hip replacement (J. Am Coll. Surg. 2006:203:914-32), but this is the first double-blind trial to assess its long-term effects.
Investigators at high-volume orthopedic centers in the United Kingdom randomly assigned 322 patients undergoing total hip replacement for osteoarthritis to standard care (spinal anesthesia with or without general anesthesia) alone or with local anesthetic infiltration. The primary outcome was WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) pain scale scores at 12 months postoperatively.
Use of in-patient analgesia or length of hospitalization did not differ between the groups, said Dr. Wylde, a research associate with the University of Bristol, England. Acute postoperative pain severity was also similar, except that patients in the intervention group reported less severe pain on postoperative night 2 (P = .008). This was unexpected, but the study was not powered to detect differences in these secondary measures, and no conclusions can be drawn from these data, she said at the meeting, sponsored by the Osteoarthritis Research Society International.
There were no differences in other secondary measures including the WOMAC function or stiffness scales or in ICOAP (Intermittent and Constant Osteoarthritis Pain) scores.
Local anesthetic infiltration, however, significantly reduced neuropathic pain at 12 months, as assessed using the PainDETECT questionnaire, Dr. Wylde said.
"Our study suggests that local anesthetic infiltration is unlikely to change long-term pain outcomes for the majority of patients, but potentially can improve pain relief for a small number of patients who may otherwise go on to develop severe long-term pain after surgery," she concluded.
In a separate interview, Dr. Jeffrey Katz, codirector, Brigham Spine Center, Brigham & Women’s Hospital and professor at Harvard Medical School, both in Boston, said the study was very interesting mechanistically and potentially interesting from a public health standpoint because there are about 400,000 hips done a year in the United States and thus 4,000 or so of these patients are having chronic pain. Moreover, the problem of chronic pain after surgery is even more common in the knee than in the hip.
"The difference in severe pain of 8% vs. 1% or 2% is a striking difference, but it’s a small incidence, and so it does bear replication," he added. "I thought it was a very exciting study and think it’s important information for folks to begin to work with and might change practice."
Dr. Wylde reported funding from the National Institute for Health Research, London.
PARIS – Adding local anesthetic to the wound during total hip replacement surgery for osteoarthritis reduced chronic pain, according to a double-blind, randomized controlled trial.
At 12 months postoperative, the number of patients with severe pain was 8.6% with standard care, compared with 1.4% among those who also received 60 mL of 0.25% bupivacaine with lidocaine (Xylocaine) 1% with adrenaline 100 mcg/20 mL injected directly into the wound prior to closure.
The difference was statistically significant (P = .004; odds ratio, 10.19), but the confidence intervals were wide (95% C.I., 2.10-49.55) because of the small number of patients with severe pain, Vikki Wylde, Ph.D., said at the World Congress on Osteoarthritis.
She noted that 7%-23% of patients report moderate to severe chronic pain in the long term after total hip replacement, according to a recent systematic review (BMJ Open 2012:2:e000435), and that the severity of postoperative pain is a known risk factor for chronic postsurgical pain.
Local anesthetic wound infiltration has been shown to be effective at reducing the severity of acute postoperative pain after total hip replacement (J. Am Coll. Surg. 2006:203:914-32), but this is the first double-blind trial to assess its long-term effects.
Investigators at high-volume orthopedic centers in the United Kingdom randomly assigned 322 patients undergoing total hip replacement for osteoarthritis to standard care (spinal anesthesia with or without general anesthesia) alone or with local anesthetic infiltration. The primary outcome was WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) pain scale scores at 12 months postoperatively.
Use of in-patient analgesia or length of hospitalization did not differ between the groups, said Dr. Wylde, a research associate with the University of Bristol, England. Acute postoperative pain severity was also similar, except that patients in the intervention group reported less severe pain on postoperative night 2 (P = .008). This was unexpected, but the study was not powered to detect differences in these secondary measures, and no conclusions can be drawn from these data, she said at the meeting, sponsored by the Osteoarthritis Research Society International.
There were no differences in other secondary measures including the WOMAC function or stiffness scales or in ICOAP (Intermittent and Constant Osteoarthritis Pain) scores.
Local anesthetic infiltration, however, significantly reduced neuropathic pain at 12 months, as assessed using the PainDETECT questionnaire, Dr. Wylde said.
"Our study suggests that local anesthetic infiltration is unlikely to change long-term pain outcomes for the majority of patients, but potentially can improve pain relief for a small number of patients who may otherwise go on to develop severe long-term pain after surgery," she concluded.
In a separate interview, Dr. Jeffrey Katz, codirector, Brigham Spine Center, Brigham & Women’s Hospital and professor at Harvard Medical School, both in Boston, said the study was very interesting mechanistically and potentially interesting from a public health standpoint because there are about 400,000 hips done a year in the United States and thus 4,000 or so of these patients are having chronic pain. Moreover, the problem of chronic pain after surgery is even more common in the knee than in the hip.
"The difference in severe pain of 8% vs. 1% or 2% is a striking difference, but it’s a small incidence, and so it does bear replication," he added. "I thought it was a very exciting study and think it’s important information for folks to begin to work with and might change practice."
Dr. Wylde reported funding from the National Institute for Health Research, London.
AT OARSI 2014
Major finding: Severe pain at 12 months was reduced from 8.6% with standard care to 1.4% with the addition of local anesthetic wound infiltration (P = .004).
Data source: Double-blind, randomized controlled trial in 322 patients undergoing total hip replacement for osteoarthritis.
Disclosures: Dr. Wylde reported funding from the National Institute for Health Research, London.
PCPs waffle in referrals for total joint replacement
PARIS – Primary care physicians are only moderately confident about which patients to refer for total hip or knee replacement, according to cross-sectional survey of 218 physicians.
One-quarter (27.4%) were unsure about the risks of total joint arthroplasty (TJA), and 44.3% reported they were discouraged from referring patients for TJA because of a lack of clarity about surgical indications.
When asked how confident they were in deciding which patients should be referred to orthopedic surgery for consideration of hip or knee replacement, the average response was 6.9 on a 10-point scale from "not at all" to "highly confident," indicating a moderate level of confidence, Esther* Waugh, Ph.D., reported at the World Congress on Osteoarthritis.
"The results suggest the need for increased guidance for primary care physicians regarding which patient, and when, total joint arthroplasty should be considered," she concluded. "While lack of confidence does not necessarily equate with decreased competence, additional clarity may result in enhanced physician confidence, improved decision making, and ultimately better surgical outcomes through better patient selection of appropriate candidates."
A total of 376 primary care physicians (PCPs) were recruited from among those providing care to participants of an established community cohort with symptomatic hip or knee osteoarthritis (OA) in Ontario, Canada, with 218 (58%) completing the standardized questionnaire by mail or online.
One-third reported seeing more than 10 moderate to severe hip/knee OA patients in the previous 2 weeks.
Most had been in practice for more than 15 years (77%), were in group practice (63%), and were older than age 50 years (65%). One-third practiced in a rural location, and 31% had more than 10 TJA referrals per year.
Interestingly, total hip and total knee arthroplasty was perceived as "very effective" by 53% and 40% of physicians, respectively, according to Dr. Waugh of the physical therapy department at the University of Toronto.
Still, TJA was viewed as carrying high risks of death by 11.3%, of complications by 35%, and need for revision surgery by 12.3%.
Lower confidence in referring patients for TJA was independently associated with lack of clarity about surgical indications (P less than .0001; parameter estimate, –1.02) and female sex (P = .02; parameter estimate, –0.54), in multiple linear regression analysis.
Both factors were associated with fewer years of practice, she noted. Female physicians were significantly more likely to report fewer years of practice (P less than .0001), fewer OA patients (P = .0004), practicing in a group practice (P = .003), urban practice location (P = .003), and being unsure about risks (P = .02).
Confidence was not associated with uncertainty of TJA risks, volume of OA patients in the prior 2 weeks, group practice, years of practice, or rural practice setting, Dr. Waugh reported at the meeting, sponsored by the Osteoarthritis Research Society International.
Prior research by the University of Toronto team demonstrated underuse of total joint arthroplasty, but concerns have recently been raised regarding possible overuse, particularly in younger patients. In Canada, PCPs are responsible for referrals to orthopedic surgery for TJA. Thus, "inappropriate under- or overuse of TJA may be a consequence of uncertainty among PCPs about indications for TJA," the authors noted in the poster presentation
Conflict of interest disclosures were not available at press time.
*Correction, 5/8/2014: An earlier version of this story misspelled Dr. Esther Waugh's name.
PARIS – Primary care physicians are only moderately confident about which patients to refer for total hip or knee replacement, according to cross-sectional survey of 218 physicians.
One-quarter (27.4%) were unsure about the risks of total joint arthroplasty (TJA), and 44.3% reported they were discouraged from referring patients for TJA because of a lack of clarity about surgical indications.
When asked how confident they were in deciding which patients should be referred to orthopedic surgery for consideration of hip or knee replacement, the average response was 6.9 on a 10-point scale from "not at all" to "highly confident," indicating a moderate level of confidence, Esther* Waugh, Ph.D., reported at the World Congress on Osteoarthritis.
"The results suggest the need for increased guidance for primary care physicians regarding which patient, and when, total joint arthroplasty should be considered," she concluded. "While lack of confidence does not necessarily equate with decreased competence, additional clarity may result in enhanced physician confidence, improved decision making, and ultimately better surgical outcomes through better patient selection of appropriate candidates."
A total of 376 primary care physicians (PCPs) were recruited from among those providing care to participants of an established community cohort with symptomatic hip or knee osteoarthritis (OA) in Ontario, Canada, with 218 (58%) completing the standardized questionnaire by mail or online.
One-third reported seeing more than 10 moderate to severe hip/knee OA patients in the previous 2 weeks.
Most had been in practice for more than 15 years (77%), were in group practice (63%), and were older than age 50 years (65%). One-third practiced in a rural location, and 31% had more than 10 TJA referrals per year.
Interestingly, total hip and total knee arthroplasty was perceived as "very effective" by 53% and 40% of physicians, respectively, according to Dr. Waugh of the physical therapy department at the University of Toronto.
Still, TJA was viewed as carrying high risks of death by 11.3%, of complications by 35%, and need for revision surgery by 12.3%.
Lower confidence in referring patients for TJA was independently associated with lack of clarity about surgical indications (P less than .0001; parameter estimate, –1.02) and female sex (P = .02; parameter estimate, –0.54), in multiple linear regression analysis.
Both factors were associated with fewer years of practice, she noted. Female physicians were significantly more likely to report fewer years of practice (P less than .0001), fewer OA patients (P = .0004), practicing in a group practice (P = .003), urban practice location (P = .003), and being unsure about risks (P = .02).
Confidence was not associated with uncertainty of TJA risks, volume of OA patients in the prior 2 weeks, group practice, years of practice, or rural practice setting, Dr. Waugh reported at the meeting, sponsored by the Osteoarthritis Research Society International.
Prior research by the University of Toronto team demonstrated underuse of total joint arthroplasty, but concerns have recently been raised regarding possible overuse, particularly in younger patients. In Canada, PCPs are responsible for referrals to orthopedic surgery for TJA. Thus, "inappropriate under- or overuse of TJA may be a consequence of uncertainty among PCPs about indications for TJA," the authors noted in the poster presentation
Conflict of interest disclosures were not available at press time.
*Correction, 5/8/2014: An earlier version of this story misspelled Dr. Esther Waugh's name.
PARIS – Primary care physicians are only moderately confident about which patients to refer for total hip or knee replacement, according to cross-sectional survey of 218 physicians.
One-quarter (27.4%) were unsure about the risks of total joint arthroplasty (TJA), and 44.3% reported they were discouraged from referring patients for TJA because of a lack of clarity about surgical indications.
When asked how confident they were in deciding which patients should be referred to orthopedic surgery for consideration of hip or knee replacement, the average response was 6.9 on a 10-point scale from "not at all" to "highly confident," indicating a moderate level of confidence, Esther* Waugh, Ph.D., reported at the World Congress on Osteoarthritis.
"The results suggest the need for increased guidance for primary care physicians regarding which patient, and when, total joint arthroplasty should be considered," she concluded. "While lack of confidence does not necessarily equate with decreased competence, additional clarity may result in enhanced physician confidence, improved decision making, and ultimately better surgical outcomes through better patient selection of appropriate candidates."
A total of 376 primary care physicians (PCPs) were recruited from among those providing care to participants of an established community cohort with symptomatic hip or knee osteoarthritis (OA) in Ontario, Canada, with 218 (58%) completing the standardized questionnaire by mail or online.
One-third reported seeing more than 10 moderate to severe hip/knee OA patients in the previous 2 weeks.
Most had been in practice for more than 15 years (77%), were in group practice (63%), and were older than age 50 years (65%). One-third practiced in a rural location, and 31% had more than 10 TJA referrals per year.
Interestingly, total hip and total knee arthroplasty was perceived as "very effective" by 53% and 40% of physicians, respectively, according to Dr. Waugh of the physical therapy department at the University of Toronto.
Still, TJA was viewed as carrying high risks of death by 11.3%, of complications by 35%, and need for revision surgery by 12.3%.
Lower confidence in referring patients for TJA was independently associated with lack of clarity about surgical indications (P less than .0001; parameter estimate, –1.02) and female sex (P = .02; parameter estimate, –0.54), in multiple linear regression analysis.
Both factors were associated with fewer years of practice, she noted. Female physicians were significantly more likely to report fewer years of practice (P less than .0001), fewer OA patients (P = .0004), practicing in a group practice (P = .003), urban practice location (P = .003), and being unsure about risks (P = .02).
Confidence was not associated with uncertainty of TJA risks, volume of OA patients in the prior 2 weeks, group practice, years of practice, or rural practice setting, Dr. Waugh reported at the meeting, sponsored by the Osteoarthritis Research Society International.
Prior research by the University of Toronto team demonstrated underuse of total joint arthroplasty, but concerns have recently been raised regarding possible overuse, particularly in younger patients. In Canada, PCPs are responsible for referrals to orthopedic surgery for TJA. Thus, "inappropriate under- or overuse of TJA may be a consequence of uncertainty among PCPs about indications for TJA," the authors noted in the poster presentation
Conflict of interest disclosures were not available at press time.
*Correction, 5/8/2014: An earlier version of this story misspelled Dr. Esther Waugh's name.
AT OARSI 2014
Major finding: Lack of clarity about indications thwarted 44.3% of primary care physicians from referring patients for arthroplasty.
Data source: A cross-sectional survey of 218 primary care physicians.
Disclosures: Conflict of interest disclosures were not available at press time.
Men have more major complications after hip, knee replacement
PARIS – After total hip or knee replacement, men are at higher risk than women for heart attack, infection, and revision surgery, according to a large database analysis.
The elevated risk was particularly apparent following total knee arthroplasty (TKA), Dr. Gillian Hawker said at the World Congress on Osteoarthritis.
Prior research suggests that younger patients and males who have joint replacement are at higher risk of certain complications such as early revision, and that joint replacement is underutilized in women.
Based on the current study, underuse of total joint arthroplasty among women versus men does not appear to be explained by higher surgical risk, she said.
The investigators used administrative databases to analyze 97,445 patients who underwent primary, elective total joint arthroplasty in Ontario, Canada, between 2002 and 2009. In all, 59,564 patients (39% male) underwent TKA and 37,881 patients (46% male) had total hip arthroplasty.
Knee arthroplasty
Men had more acute myocardial infarctions within 90 days of undergoing TKA than did women (1.1% vs. 0.8%), more infection within 2 years of surgery (1.1% vs. 0.7%), and more revision TKA within 2 years (1.5% vs. 1%), said Dr. Hawker, professor of medicine at the University of Toronto and physician-in-chief of medicine, Women’s College Hospital, Toronto.
At baseline, the men were similar in age to women, but less likely to be frail (4% vs. 6.7%) and more likely to have a Charlson Comorbidity Index score of 2 or more (5.7% vs. 3.4%).
In Cox regression analysis, the risk for acute MI was significantly increased (hazard ratio, 1.79; P less than .0001) after adjustment for age, sex, income quartile, rurality, frailty, Charlson score, and hospital volume, she said.
Men were also at significantly increased risk for infection (HR, 1.67; P less than .0001) and revision TKA within 2 years (HR, 1.49; P less than .0001), after further adjustment for surgeon volume.
The investigators, led by colleague and orthopedic surgery resident Bheeshma Ravi, Ph.D., postulate that the increased risk of infection and revision among men is due to the high-impact activities that men may engage in after their prosthesis.
No sex differences were found for venous thromboembolism within 90 days or periprosthetic fracture within 2 years.
Hip arthroplasty
Men undergoing total hip replacement had higher rates of early acute MI than women (0.9% vs. 0.7%), but lower rates of periprosthetic fracture within 2 years (0.3% vs. 0.5%), Dr. Hawker said.
At baseline, male patients were younger than their female counterparts (65 years vs. 70 years) and less likely to be frail (3.5% vs. 6.6%), but more likely to have a Charlson score of 2 or more (5.3% vs. 3.7%).
After full adjustment, men were at significantly increased risk for acute MI (HR, 1.64; P less than .0001) and reduced risk for periprosthetic fracture (HR, 0.52; P = .0005), Dr. Hawker said at the meeting, which was sponsored by the Osteoarthritis Research Society International.
"We think the potential explanations for acute MI after both hip and knee replacement may be additional cardiovascular risk factors," she said. "We did not control for preexisting cardiovascular risk; that is something we are doing now."
The study excluded patients who had a pre–joint replacement fragility fracture, but because of the quality of the data postoperatively and the availability of drug benefit data, "we don’t feel we have adequate control for the presence of osteoporosis," Dr. Hawker observed.
No differences were found between sexes in the hip replacement cohort for infection, death, venous thromboembolism, dislocation, or revision.
Session comoderator Dr. Martin Englund, of Lund (Sweden) University, commented that the study was well conducted and the findings very interesting, but he cautioned against generalizing the results too broadly.
"We have seen before, that results from Sweden are not necessarily the same as in North America," he said in an interview. "I’m sure these results are probably very generalizable in Canada and in that type of health care setting, but may not be the same elsewhere. ... These are also things that might change over time. So we just need to keep monitoring outcomes and repeating these studies and adjust our treatment to what we find."
Dr. Ravi reported fellowship support from the University of Toronto, Canadian Institutes of Health Research, and Women’s College Research Institute.
PARIS – After total hip or knee replacement, men are at higher risk than women for heart attack, infection, and revision surgery, according to a large database analysis.
The elevated risk was particularly apparent following total knee arthroplasty (TKA), Dr. Gillian Hawker said at the World Congress on Osteoarthritis.
Prior research suggests that younger patients and males who have joint replacement are at higher risk of certain complications such as early revision, and that joint replacement is underutilized in women.
Based on the current study, underuse of total joint arthroplasty among women versus men does not appear to be explained by higher surgical risk, she said.
The investigators used administrative databases to analyze 97,445 patients who underwent primary, elective total joint arthroplasty in Ontario, Canada, between 2002 and 2009. In all, 59,564 patients (39% male) underwent TKA and 37,881 patients (46% male) had total hip arthroplasty.
Knee arthroplasty
Men had more acute myocardial infarctions within 90 days of undergoing TKA than did women (1.1% vs. 0.8%), more infection within 2 years of surgery (1.1% vs. 0.7%), and more revision TKA within 2 years (1.5% vs. 1%), said Dr. Hawker, professor of medicine at the University of Toronto and physician-in-chief of medicine, Women’s College Hospital, Toronto.
At baseline, the men were similar in age to women, but less likely to be frail (4% vs. 6.7%) and more likely to have a Charlson Comorbidity Index score of 2 or more (5.7% vs. 3.4%).
In Cox regression analysis, the risk for acute MI was significantly increased (hazard ratio, 1.79; P less than .0001) after adjustment for age, sex, income quartile, rurality, frailty, Charlson score, and hospital volume, she said.
Men were also at significantly increased risk for infection (HR, 1.67; P less than .0001) and revision TKA within 2 years (HR, 1.49; P less than .0001), after further adjustment for surgeon volume.
The investigators, led by colleague and orthopedic surgery resident Bheeshma Ravi, Ph.D., postulate that the increased risk of infection and revision among men is due to the high-impact activities that men may engage in after their prosthesis.
No sex differences were found for venous thromboembolism within 90 days or periprosthetic fracture within 2 years.
Hip arthroplasty
Men undergoing total hip replacement had higher rates of early acute MI than women (0.9% vs. 0.7%), but lower rates of periprosthetic fracture within 2 years (0.3% vs. 0.5%), Dr. Hawker said.
At baseline, male patients were younger than their female counterparts (65 years vs. 70 years) and less likely to be frail (3.5% vs. 6.6%), but more likely to have a Charlson score of 2 or more (5.3% vs. 3.7%).
After full adjustment, men were at significantly increased risk for acute MI (HR, 1.64; P less than .0001) and reduced risk for periprosthetic fracture (HR, 0.52; P = .0005), Dr. Hawker said at the meeting, which was sponsored by the Osteoarthritis Research Society International.
"We think the potential explanations for acute MI after both hip and knee replacement may be additional cardiovascular risk factors," she said. "We did not control for preexisting cardiovascular risk; that is something we are doing now."
The study excluded patients who had a pre–joint replacement fragility fracture, but because of the quality of the data postoperatively and the availability of drug benefit data, "we don’t feel we have adequate control for the presence of osteoporosis," Dr. Hawker observed.
No differences were found between sexes in the hip replacement cohort for infection, death, venous thromboembolism, dislocation, or revision.
Session comoderator Dr. Martin Englund, of Lund (Sweden) University, commented that the study was well conducted and the findings very interesting, but he cautioned against generalizing the results too broadly.
"We have seen before, that results from Sweden are not necessarily the same as in North America," he said in an interview. "I’m sure these results are probably very generalizable in Canada and in that type of health care setting, but may not be the same elsewhere. ... These are also things that might change over time. So we just need to keep monitoring outcomes and repeating these studies and adjust our treatment to what we find."
Dr. Ravi reported fellowship support from the University of Toronto, Canadian Institutes of Health Research, and Women’s College Research Institute.
PARIS – After total hip or knee replacement, men are at higher risk than women for heart attack, infection, and revision surgery, according to a large database analysis.
The elevated risk was particularly apparent following total knee arthroplasty (TKA), Dr. Gillian Hawker said at the World Congress on Osteoarthritis.
Prior research suggests that younger patients and males who have joint replacement are at higher risk of certain complications such as early revision, and that joint replacement is underutilized in women.
Based on the current study, underuse of total joint arthroplasty among women versus men does not appear to be explained by higher surgical risk, she said.
The investigators used administrative databases to analyze 97,445 patients who underwent primary, elective total joint arthroplasty in Ontario, Canada, between 2002 and 2009. In all, 59,564 patients (39% male) underwent TKA and 37,881 patients (46% male) had total hip arthroplasty.
Knee arthroplasty
Men had more acute myocardial infarctions within 90 days of undergoing TKA than did women (1.1% vs. 0.8%), more infection within 2 years of surgery (1.1% vs. 0.7%), and more revision TKA within 2 years (1.5% vs. 1%), said Dr. Hawker, professor of medicine at the University of Toronto and physician-in-chief of medicine, Women’s College Hospital, Toronto.
At baseline, the men were similar in age to women, but less likely to be frail (4% vs. 6.7%) and more likely to have a Charlson Comorbidity Index score of 2 or more (5.7% vs. 3.4%).
In Cox regression analysis, the risk for acute MI was significantly increased (hazard ratio, 1.79; P less than .0001) after adjustment for age, sex, income quartile, rurality, frailty, Charlson score, and hospital volume, she said.
Men were also at significantly increased risk for infection (HR, 1.67; P less than .0001) and revision TKA within 2 years (HR, 1.49; P less than .0001), after further adjustment for surgeon volume.
The investigators, led by colleague and orthopedic surgery resident Bheeshma Ravi, Ph.D., postulate that the increased risk of infection and revision among men is due to the high-impact activities that men may engage in after their prosthesis.
No sex differences were found for venous thromboembolism within 90 days or periprosthetic fracture within 2 years.
Hip arthroplasty
Men undergoing total hip replacement had higher rates of early acute MI than women (0.9% vs. 0.7%), but lower rates of periprosthetic fracture within 2 years (0.3% vs. 0.5%), Dr. Hawker said.
At baseline, male patients were younger than their female counterparts (65 years vs. 70 years) and less likely to be frail (3.5% vs. 6.6%), but more likely to have a Charlson score of 2 or more (5.3% vs. 3.7%).
After full adjustment, men were at significantly increased risk for acute MI (HR, 1.64; P less than .0001) and reduced risk for periprosthetic fracture (HR, 0.52; P = .0005), Dr. Hawker said at the meeting, which was sponsored by the Osteoarthritis Research Society International.
"We think the potential explanations for acute MI after both hip and knee replacement may be additional cardiovascular risk factors," she said. "We did not control for preexisting cardiovascular risk; that is something we are doing now."
The study excluded patients who had a pre–joint replacement fragility fracture, but because of the quality of the data postoperatively and the availability of drug benefit data, "we don’t feel we have adequate control for the presence of osteoporosis," Dr. Hawker observed.
No differences were found between sexes in the hip replacement cohort for infection, death, venous thromboembolism, dislocation, or revision.
Session comoderator Dr. Martin Englund, of Lund (Sweden) University, commented that the study was well conducted and the findings very interesting, but he cautioned against generalizing the results too broadly.
"We have seen before, that results from Sweden are not necessarily the same as in North America," he said in an interview. "I’m sure these results are probably very generalizable in Canada and in that type of health care setting, but may not be the same elsewhere. ... These are also things that might change over time. So we just need to keep monitoring outcomes and repeating these studies and adjust our treatment to what we find."
Dr. Ravi reported fellowship support from the University of Toronto, Canadian Institutes of Health Research, and Women’s College Research Institute.
AT OARSI 2014
Major finding: Men had more acute MIs within 90 days after total knee arthroplasty than did women (1.1% vs. 0.8%), more infection within 2 years of surgery (1.1% vs. 0.7%), and more revision surgery within 2 years (1.5% vs. 1%). After total hip replacement, men had a higher rate of early acute MI (0.9% vs. 0.7%), but less periprosthetic fracture within 2 years (0.3% vs. 0.5%).
Data source: Database analysis of 97,445 patients who received primary, elective hip or knee arthroplasty.
Disclosures: Dr. Ravi reported fellowship support from the University of Toronto, Canadian Institutes of Health Research, and Women’s College Research Institute.
How Long Do Uncemented Hip Replacements Last?
Uncemented hip replacements have gained popularity and are increasingly being used in the U.S. However, that popularity may be undeserved and in opposition to the data, say researchers from Turku University Hospital, Helsinki University, and The Coxa Hospital for Joint Replacement in Tampere, all in Finland; Haukeland University Hospital and the University of Bergen, both in Bergen, Norway; Odense University Hospital and Aarhus University Hospital, both in Denmark; the University of Gothenburg in Mölndal and Skåne University Hospital in Lund, both in Sweden; and Massachusetts General Hospital in Boston.
All types of fixation techniques have excellent track records of survivorship, including traditional cemented implants. Nevertheless, the increased use of uncemented implants has been influenced by reports from experts in single centers with good outcomes, the researchers say. They also add that intense marketing of the more expensive uncemented implants may be a factor in their growing popularity.
In their study, the researchers analyzed data from patients in the multinational Nordic Arthroplasty Register Association database, including 347,899 total hip replacements. Of those, 232,603 used cemented implants, 71,454 patients used uncemented, 28,215 hips were hybrid (uncemented cup with cemented stem), and 15,627 used reverse hybrid (cemented cup and uncemented stem). The mean follow-up time was 7 years (range, 0-17) for cemented, 4.9 years (range, 0-17) for uncemented, 7.5 years for hybrid, and 3.4 years for reverse hybrid.
The researchers found that the 10-year survival of cemented implants in patients aged 65 to 74 years and aged ≥ 75 years was higher than that of uncemented, hybrid, and reverse hybrid implants. For example, 95.9% of cemented implants survived at 10 years in patients aged ≥75 years compared with 93% of uncemented, 93.9% of hybrid, and 93.2% of reverse hybrid. The survival of cemented replacements in patients aged 55 to 64 years was similar.
Moreover, during the first 6 months, the risk of revision was lower with cemented implants than with that of all other types of fixation in all age groups.
Source
Mäkelä KT, Matilainen M, Pulkkinen P, et al. BMJ. 2014;348:f7592.
doi: 10.1136/bmj.f7592.
Uncemented hip replacements have gained popularity and are increasingly being used in the U.S. However, that popularity may be undeserved and in opposition to the data, say researchers from Turku University Hospital, Helsinki University, and The Coxa Hospital for Joint Replacement in Tampere, all in Finland; Haukeland University Hospital and the University of Bergen, both in Bergen, Norway; Odense University Hospital and Aarhus University Hospital, both in Denmark; the University of Gothenburg in Mölndal and Skåne University Hospital in Lund, both in Sweden; and Massachusetts General Hospital in Boston.
All types of fixation techniques have excellent track records of survivorship, including traditional cemented implants. Nevertheless, the increased use of uncemented implants has been influenced by reports from experts in single centers with good outcomes, the researchers say. They also add that intense marketing of the more expensive uncemented implants may be a factor in their growing popularity.
In their study, the researchers analyzed data from patients in the multinational Nordic Arthroplasty Register Association database, including 347,899 total hip replacements. Of those, 232,603 used cemented implants, 71,454 patients used uncemented, 28,215 hips were hybrid (uncemented cup with cemented stem), and 15,627 used reverse hybrid (cemented cup and uncemented stem). The mean follow-up time was 7 years (range, 0-17) for cemented, 4.9 years (range, 0-17) for uncemented, 7.5 years for hybrid, and 3.4 years for reverse hybrid.
The researchers found that the 10-year survival of cemented implants in patients aged 65 to 74 years and aged ≥ 75 years was higher than that of uncemented, hybrid, and reverse hybrid implants. For example, 95.9% of cemented implants survived at 10 years in patients aged ≥75 years compared with 93% of uncemented, 93.9% of hybrid, and 93.2% of reverse hybrid. The survival of cemented replacements in patients aged 55 to 64 years was similar.
Moreover, during the first 6 months, the risk of revision was lower with cemented implants than with that of all other types of fixation in all age groups.
Source
Mäkelä KT, Matilainen M, Pulkkinen P, et al. BMJ. 2014;348:f7592.
doi: 10.1136/bmj.f7592.
Uncemented hip replacements have gained popularity and are increasingly being used in the U.S. However, that popularity may be undeserved and in opposition to the data, say researchers from Turku University Hospital, Helsinki University, and The Coxa Hospital for Joint Replacement in Tampere, all in Finland; Haukeland University Hospital and the University of Bergen, both in Bergen, Norway; Odense University Hospital and Aarhus University Hospital, both in Denmark; the University of Gothenburg in Mölndal and Skåne University Hospital in Lund, both in Sweden; and Massachusetts General Hospital in Boston.
All types of fixation techniques have excellent track records of survivorship, including traditional cemented implants. Nevertheless, the increased use of uncemented implants has been influenced by reports from experts in single centers with good outcomes, the researchers say. They also add that intense marketing of the more expensive uncemented implants may be a factor in their growing popularity.
In their study, the researchers analyzed data from patients in the multinational Nordic Arthroplasty Register Association database, including 347,899 total hip replacements. Of those, 232,603 used cemented implants, 71,454 patients used uncemented, 28,215 hips were hybrid (uncemented cup with cemented stem), and 15,627 used reverse hybrid (cemented cup and uncemented stem). The mean follow-up time was 7 years (range, 0-17) for cemented, 4.9 years (range, 0-17) for uncemented, 7.5 years for hybrid, and 3.4 years for reverse hybrid.
The researchers found that the 10-year survival of cemented implants in patients aged 65 to 74 years and aged ≥ 75 years was higher than that of uncemented, hybrid, and reverse hybrid implants. For example, 95.9% of cemented implants survived at 10 years in patients aged ≥75 years compared with 93% of uncemented, 93.9% of hybrid, and 93.2% of reverse hybrid. The survival of cemented replacements in patients aged 55 to 64 years was similar.
Moreover, during the first 6 months, the risk of revision was lower with cemented implants than with that of all other types of fixation in all age groups.
Source
Mäkelä KT, Matilainen M, Pulkkinen P, et al. BMJ. 2014;348:f7592.
doi: 10.1136/bmj.f7592.
Perioperative Pain Management in Hip and Knee Replacement Surgery
Authors’ Response
I thank Dr. Strauss for his comments regarding our article—“Chronic Exertional Compartment Syndrome in a Collegiate Soccer Player: A Case Report and Literature Review” (Am J Orthop. 2008;37(7):374-377).
The history in most cases alone is not sufficient to justify compartment pressure measurements as the first diagnostic test. Many athletes with leg pain have the more common diagnosis of tibial periostitis or stress fracture, and certainly radiographs and an MRI scan may not only be diagnostic but also noninvasive. However, as Dr. Strauss suggests, in some patients, the history alone, if more classic for chronic exertional compartment syndrome, may make it reasonable to
proceed with compartment pressure measurements initially. I also agree that if the diagnosis of chronic exertional compartment syndrome can be made from the resting compartment pressure measurements alone, additional needlesticks post-exercise may not be necessary. I still believe that the standard diagnostic protocol, as described by Pedowitz and colleagues,1 should be used to set the diagnostic criteria for chronic exertional compartment syndrome. Even in the runner who required 45 minutes before the chronic exertional compartment symptoms manifested themselves, it is possible that, with the standard protocol, elevation of compartment pressures may have existed prior to, immediately after,
or 5 minutes after exercise as well.
Once again, I greatly appreciate Dr. Strauss’s insight. I do agree that further research in the diagnosis of chronic exertional compartment syndrome is needed. I hope that our article demonstrating a representative case of this entity with
an encompassing literature review was a help to readers.
Harlan Selesnick, MD
Coral Gables, FL
Reference
1. Pedowitz RA, Hargens AR, Mubarak SJ, Gershuni DH. Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med. 1990;18(1):35-40.
I thank Dr. Strauss for his comments regarding our article—“Chronic Exertional Compartment Syndrome in a Collegiate Soccer Player: A Case Report and Literature Review” (Am J Orthop. 2008;37(7):374-377).
The history in most cases alone is not sufficient to justify compartment pressure measurements as the first diagnostic test. Many athletes with leg pain have the more common diagnosis of tibial periostitis or stress fracture, and certainly radiographs and an MRI scan may not only be diagnostic but also noninvasive. However, as Dr. Strauss suggests, in some patients, the history alone, if more classic for chronic exertional compartment syndrome, may make it reasonable to
proceed with compartment pressure measurements initially. I also agree that if the diagnosis of chronic exertional compartment syndrome can be made from the resting compartment pressure measurements alone, additional needlesticks post-exercise may not be necessary. I still believe that the standard diagnostic protocol, as described by Pedowitz and colleagues,1 should be used to set the diagnostic criteria for chronic exertional compartment syndrome. Even in the runner who required 45 minutes before the chronic exertional compartment symptoms manifested themselves, it is possible that, with the standard protocol, elevation of compartment pressures may have existed prior to, immediately after,
or 5 minutes after exercise as well.
Once again, I greatly appreciate Dr. Strauss’s insight. I do agree that further research in the diagnosis of chronic exertional compartment syndrome is needed. I hope that our article demonstrating a representative case of this entity with
an encompassing literature review was a help to readers.
Harlan Selesnick, MD
Coral Gables, FL
Reference
1. Pedowitz RA, Hargens AR, Mubarak SJ, Gershuni DH. Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med. 1990;18(1):35-40.
I thank Dr. Strauss for his comments regarding our article—“Chronic Exertional Compartment Syndrome in a Collegiate Soccer Player: A Case Report and Literature Review” (Am J Orthop. 2008;37(7):374-377).
The history in most cases alone is not sufficient to justify compartment pressure measurements as the first diagnostic test. Many athletes with leg pain have the more common diagnosis of tibial periostitis or stress fracture, and certainly radiographs and an MRI scan may not only be diagnostic but also noninvasive. However, as Dr. Strauss suggests, in some patients, the history alone, if more classic for chronic exertional compartment syndrome, may make it reasonable to
proceed with compartment pressure measurements initially. I also agree that if the diagnosis of chronic exertional compartment syndrome can be made from the resting compartment pressure measurements alone, additional needlesticks post-exercise may not be necessary. I still believe that the standard diagnostic protocol, as described by Pedowitz and colleagues,1 should be used to set the diagnostic criteria for chronic exertional compartment syndrome. Even in the runner who required 45 minutes before the chronic exertional compartment symptoms manifested themselves, it is possible that, with the standard protocol, elevation of compartment pressures may have existed prior to, immediately after,
or 5 minutes after exercise as well.
Once again, I greatly appreciate Dr. Strauss’s insight. I do agree that further research in the diagnosis of chronic exertional compartment syndrome is needed. I hope that our article demonstrating a representative case of this entity with
an encompassing literature review was a help to readers.
Harlan Selesnick, MD
Coral Gables, FL
Reference
1. Pedowitz RA, Hargens AR, Mubarak SJ, Gershuni DH. Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med. 1990;18(1):35-40.
Failed First Metatarsophalangeal Arthroplasty Salvaged by Hamstring Interposition Arthroplasty: Metallic Debris From Grommets
joint, arthroplasty, implant, metallic debris, grommets, titanium, synovitis, foot
joint, arthroplasty, implant, metallic debris, grommets, titanium, synovitis, foot
joint, arthroplasty, implant, metallic debris, grommets, titanium, synovitis, foot