User login
The 12 Dangers of Christmas
The 12 Dangers of Christmas
The carol promises partridges and pears. The reality, every December, is a predictable spike in injuries, illness, and emergency care.
Framed around the familiar “12 Days of Christmas,” this seasonal guide sets out the most common festive hazards — many of them preventable — and the practical advice clinicians can share to help patients enjoy a safer holiday.
1. Fire
Candles, open fires, and busy kitchens make December the most dangerous month for house fires. Home fires rise 10% in December and peak on Christmas Day at 53% above average, according to the National Fire Chiefs Council.
Alcohol, distraction, and festive cooking all add to the risk.
- Check for fire hazards before Christmas.
- Never leave cookers or candle unattended.
- Check Christmas lights and avoid overloading sockets.
- Ensure a working smoke alarm on each floor and keep escape routes clear.
- Remember that emollient residues on fabrics are highly flammable.
2. Christmas Trees and Decorations
Trees and trimmings bring their own risk. Christmas trees injure about 1000 people each year, according to the Royal Society for the Prevention of Accidents (RoSPA).
A National Accident Helpline (NAH) survey found that 2.7% of respondents had experienced electric shock from faulty lights. Artificial trees, chosen by 76% of households, carry a sixfold higher injury risk. Real trees dry out and become highly flammable — “a giant bundle of kindling covered in electrical wires,” warned safety analysts TapRooT.
- Water live trees regularly — unplug lights first.
- Keep trees stable and at least 3 feet from heat sources.
- Switch off lights before bed or leaving the house.
- Do not hang stockings near open flames.
- Hang fragile decorations high up.
- Supervise children and pets.
3. Slips, Trips, and Falls
The third danger is underfoot. Falls, burns, and cuts send around 80,000 people to A&E each Christmas, according to RoSPA.
One in 50 people fall from their loft while retrieving decorations, the NAH warned.
- Use sturdy ladders and wear footwear with good grip.
- Keep floors clear of presents, wrapping, cables, and spills.
- Never melt ice with boiling water; refreezing can make surfaces more treacherous.
4. Food and Drug Interactions
Festive eating can interfere with medicines. The Medicines and Healthcare products Regulatory Agency (MHRA) warned that drug-food interactions are not always listed on packaging.
- Grapefruit interacts with multiple drugs.
- Cranberries can enhance warfarin's anticoagulant effect, while vitamin K-rich foods, including sprouts, may reduce it.
- Rich desserts can destabilize blood glucose.
- Tyramine-rich foods, including cheeses and dark chocolate, may trigger migraines or hypertensive crises with monoamine oxidase inhibitors.
5. Alcohol
Up to 70% of weekend A&E attendances are alcohol-related, with numbers rising over Christmas. The MHRA warned that mixing alcohol with medicines can cause drowsiness, impaired coordination, and accidents.
- Avoid drinking on an empty stomach.
- Be cautious of unfamiliar drinks.
- Alternate alcoholic and soft drinks.
- Avoid potentially aggressive intoxicated people.
6. Kitchen Calamities
The festive kitchen is a frequent source of injury. NAH data showed that 49% of people reported accidents while preparing Christmas food. Cuts accounted for 18%, and burns from hot fat 11%. In addition, the Food Standards Agency said that 46% of Christmas cooks do not check use-by dates.
- Keep children and trip hazards out of the kitchen.
- Use back hobs and turn saucepan handles inward.
- Never leave ovens or pans unattended.
- Discard out-of-date food.
- Refrigerate leftovers within 2 hours.
7. Children's Vulnerabilities
Christmas presents bring hidden dangers for children. Button batteries and magnets can inflict serious gastrointestinal damage if swallowed.
- Choose age-appropriate, well-made toys.
- Store batteries, magnets, medicines, and chemicals out of reach.
- Avoid sharp or breakable decorations.
- Place holly, mistletoe, and poinsettias well out of reach.
8. Eye Injuries
Eye injuries surge over Christmas. Champagne corks can travel at nearly 50 mph, risking globe rupture or retinal detachment.
Conifer needles, glitter, and artificial snow can all cause corneal injury.
- Point champagne bottles and party poppers away from people's faces.
- Take care when handling Christmas trees.
- Avoid hanging ornaments at children's eye level.
- Rinse glitter-contaminated eyes with sterile saline.
9. Existing Ailments
By the ninth day, routine has often collapsed. Festive excess, stress and disrupted schedules can destabilize chronic disease.
- Ensure adequate medicines and testing supplies.
- Let hosts know dietary needs in advance.
- Avoid excess salt and alcohol in cardiovascular disease, and excess potassium in kidney disease.
- Increase blood glucose monitoring in diabetes.
10. Presents
Not all gifts are benign. The Child Accident Prevention Trust warned that cheap or counterfeit products may bypass safety standards.
UK safety authorities report that counterfeit Labubu dolls have made up a large share of the roughly 259,000 counterfeit toys seized at UK borders this year, and many have failed safety tests.
- Be cautious when buying for toddlers.
- Look for recognized safety markings.
- Avoid toys with strong magnets or button batteries.
- Laser pointers can cause permanent damage to vision.
11. Stress
As Christmas approaches, pressure mounts. In an NAH survey, 12% of men and 20% of women said they felt rushed, 32% of women were stressed, and 18% overwhelmed.
- Prioritize sleep.
- Get outdoors for early morning light.
- Ask for help and delegate chores.
12. Other People
The final hazard is often the most familiar: Family tension is almost traditional. In one survey, 37% of people said Christmas "wouldn't be the same" without arguments, and 54% admitted enjoying them.
- Set boundaries and agree expectations early.
- Stick to a budget.
- Avoid known flashpoint topics, such as politics.
- Create a quiet space for time out.
- One in 9 people spend Christmas alone. Plan ahead to make it a special day.
The hazards may feel seasonal, but the outcomes are not. For clinicians, the 12 risks offer a reminder that small interventions before Christmas can prevent significant harm after it.
Dr Sheena Meredith is an established medical writer, editor, and consultant in healthcare communications, with extensive experience writing for medical professionals and the general public. She is qualified in medicine and in law and medical ethics.
A version of this article first appeared on Medscape.com.
The carol promises partridges and pears. The reality, every December, is a predictable spike in injuries, illness, and emergency care.
Framed around the familiar “12 Days of Christmas,” this seasonal guide sets out the most common festive hazards — many of them preventable — and the practical advice clinicians can share to help patients enjoy a safer holiday.
1. Fire
Candles, open fires, and busy kitchens make December the most dangerous month for house fires. Home fires rise 10% in December and peak on Christmas Day at 53% above average, according to the National Fire Chiefs Council.
Alcohol, distraction, and festive cooking all add to the risk.
- Check for fire hazards before Christmas.
- Never leave cookers or candle unattended.
- Check Christmas lights and avoid overloading sockets.
- Ensure a working smoke alarm on each floor and keep escape routes clear.
- Remember that emollient residues on fabrics are highly flammable.
2. Christmas Trees and Decorations
Trees and trimmings bring their own risk. Christmas trees injure about 1000 people each year, according to the Royal Society for the Prevention of Accidents (RoSPA).
A National Accident Helpline (NAH) survey found that 2.7% of respondents had experienced electric shock from faulty lights. Artificial trees, chosen by 76% of households, carry a sixfold higher injury risk. Real trees dry out and become highly flammable — “a giant bundle of kindling covered in electrical wires,” warned safety analysts TapRooT.
- Water live trees regularly — unplug lights first.
- Keep trees stable and at least 3 feet from heat sources.
- Switch off lights before bed or leaving the house.
- Do not hang stockings near open flames.
- Hang fragile decorations high up.
- Supervise children and pets.
3. Slips, Trips, and Falls
The third danger is underfoot. Falls, burns, and cuts send around 80,000 people to A&E each Christmas, according to RoSPA.
One in 50 people fall from their loft while retrieving decorations, the NAH warned.
- Use sturdy ladders and wear footwear with good grip.
- Keep floors clear of presents, wrapping, cables, and spills.
- Never melt ice with boiling water; refreezing can make surfaces more treacherous.
4. Food and Drug Interactions
Festive eating can interfere with medicines. The Medicines and Healthcare products Regulatory Agency (MHRA) warned that drug-food interactions are not always listed on packaging.
- Grapefruit interacts with multiple drugs.
- Cranberries can enhance warfarin's anticoagulant effect, while vitamin K-rich foods, including sprouts, may reduce it.
- Rich desserts can destabilize blood glucose.
- Tyramine-rich foods, including cheeses and dark chocolate, may trigger migraines or hypertensive crises with monoamine oxidase inhibitors.
5. Alcohol
Up to 70% of weekend A&E attendances are alcohol-related, with numbers rising over Christmas. The MHRA warned that mixing alcohol with medicines can cause drowsiness, impaired coordination, and accidents.
- Avoid drinking on an empty stomach.
- Be cautious of unfamiliar drinks.
- Alternate alcoholic and soft drinks.
- Avoid potentially aggressive intoxicated people.
6. Kitchen Calamities
The festive kitchen is a frequent source of injury. NAH data showed that 49% of people reported accidents while preparing Christmas food. Cuts accounted for 18%, and burns from hot fat 11%. In addition, the Food Standards Agency said that 46% of Christmas cooks do not check use-by dates.
- Keep children and trip hazards out of the kitchen.
- Use back hobs and turn saucepan handles inward.
- Never leave ovens or pans unattended.
- Discard out-of-date food.
- Refrigerate leftovers within 2 hours.
7. Children's Vulnerabilities
Christmas presents bring hidden dangers for children. Button batteries and magnets can inflict serious gastrointestinal damage if swallowed.
- Choose age-appropriate, well-made toys.
- Store batteries, magnets, medicines, and chemicals out of reach.
- Avoid sharp or breakable decorations.
- Place holly, mistletoe, and poinsettias well out of reach.
8. Eye Injuries
Eye injuries surge over Christmas. Champagne corks can travel at nearly 50 mph, risking globe rupture or retinal detachment.
Conifer needles, glitter, and artificial snow can all cause corneal injury.
- Point champagne bottles and party poppers away from people's faces.
- Take care when handling Christmas trees.
- Avoid hanging ornaments at children's eye level.
- Rinse glitter-contaminated eyes with sterile saline.
9. Existing Ailments
By the ninth day, routine has often collapsed. Festive excess, stress and disrupted schedules can destabilize chronic disease.
- Ensure adequate medicines and testing supplies.
- Let hosts know dietary needs in advance.
- Avoid excess salt and alcohol in cardiovascular disease, and excess potassium in kidney disease.
- Increase blood glucose monitoring in diabetes.
10. Presents
Not all gifts are benign. The Child Accident Prevention Trust warned that cheap or counterfeit products may bypass safety standards.
UK safety authorities report that counterfeit Labubu dolls have made up a large share of the roughly 259,000 counterfeit toys seized at UK borders this year, and many have failed safety tests.
- Be cautious when buying for toddlers.
- Look for recognized safety markings.
- Avoid toys with strong magnets or button batteries.
- Laser pointers can cause permanent damage to vision.
11. Stress
As Christmas approaches, pressure mounts. In an NAH survey, 12% of men and 20% of women said they felt rushed, 32% of women were stressed, and 18% overwhelmed.
- Prioritize sleep.
- Get outdoors for early morning light.
- Ask for help and delegate chores.
12. Other People
The final hazard is often the most familiar: Family tension is almost traditional. In one survey, 37% of people said Christmas "wouldn't be the same" without arguments, and 54% admitted enjoying them.
- Set boundaries and agree expectations early.
- Stick to a budget.
- Avoid known flashpoint topics, such as politics.
- Create a quiet space for time out.
- One in 9 people spend Christmas alone. Plan ahead to make it a special day.
The hazards may feel seasonal, but the outcomes are not. For clinicians, the 12 risks offer a reminder that small interventions before Christmas can prevent significant harm after it.
Dr Sheena Meredith is an established medical writer, editor, and consultant in healthcare communications, with extensive experience writing for medical professionals and the general public. She is qualified in medicine and in law and medical ethics.
A version of this article first appeared on Medscape.com.
The carol promises partridges and pears. The reality, every December, is a predictable spike in injuries, illness, and emergency care.
Framed around the familiar “12 Days of Christmas,” this seasonal guide sets out the most common festive hazards — many of them preventable — and the practical advice clinicians can share to help patients enjoy a safer holiday.
1. Fire
Candles, open fires, and busy kitchens make December the most dangerous month for house fires. Home fires rise 10% in December and peak on Christmas Day at 53% above average, according to the National Fire Chiefs Council.
Alcohol, distraction, and festive cooking all add to the risk.
- Check for fire hazards before Christmas.
- Never leave cookers or candle unattended.
- Check Christmas lights and avoid overloading sockets.
- Ensure a working smoke alarm on each floor and keep escape routes clear.
- Remember that emollient residues on fabrics are highly flammable.
2. Christmas Trees and Decorations
Trees and trimmings bring their own risk. Christmas trees injure about 1000 people each year, according to the Royal Society for the Prevention of Accidents (RoSPA).
A National Accident Helpline (NAH) survey found that 2.7% of respondents had experienced electric shock from faulty lights. Artificial trees, chosen by 76% of households, carry a sixfold higher injury risk. Real trees dry out and become highly flammable — “a giant bundle of kindling covered in electrical wires,” warned safety analysts TapRooT.
- Water live trees regularly — unplug lights first.
- Keep trees stable and at least 3 feet from heat sources.
- Switch off lights before bed or leaving the house.
- Do not hang stockings near open flames.
- Hang fragile decorations high up.
- Supervise children and pets.
3. Slips, Trips, and Falls
The third danger is underfoot. Falls, burns, and cuts send around 80,000 people to A&E each Christmas, according to RoSPA.
One in 50 people fall from their loft while retrieving decorations, the NAH warned.
- Use sturdy ladders and wear footwear with good grip.
- Keep floors clear of presents, wrapping, cables, and spills.
- Never melt ice with boiling water; refreezing can make surfaces more treacherous.
4. Food and Drug Interactions
Festive eating can interfere with medicines. The Medicines and Healthcare products Regulatory Agency (MHRA) warned that drug-food interactions are not always listed on packaging.
- Grapefruit interacts with multiple drugs.
- Cranberries can enhance warfarin's anticoagulant effect, while vitamin K-rich foods, including sprouts, may reduce it.
- Rich desserts can destabilize blood glucose.
- Tyramine-rich foods, including cheeses and dark chocolate, may trigger migraines or hypertensive crises with monoamine oxidase inhibitors.
5. Alcohol
Up to 70% of weekend A&E attendances are alcohol-related, with numbers rising over Christmas. The MHRA warned that mixing alcohol with medicines can cause drowsiness, impaired coordination, and accidents.
- Avoid drinking on an empty stomach.
- Be cautious of unfamiliar drinks.
- Alternate alcoholic and soft drinks.
- Avoid potentially aggressive intoxicated people.
6. Kitchen Calamities
The festive kitchen is a frequent source of injury. NAH data showed that 49% of people reported accidents while preparing Christmas food. Cuts accounted for 18%, and burns from hot fat 11%. In addition, the Food Standards Agency said that 46% of Christmas cooks do not check use-by dates.
- Keep children and trip hazards out of the kitchen.
- Use back hobs and turn saucepan handles inward.
- Never leave ovens or pans unattended.
- Discard out-of-date food.
- Refrigerate leftovers within 2 hours.
7. Children's Vulnerabilities
Christmas presents bring hidden dangers for children. Button batteries and magnets can inflict serious gastrointestinal damage if swallowed.
- Choose age-appropriate, well-made toys.
- Store batteries, magnets, medicines, and chemicals out of reach.
- Avoid sharp or breakable decorations.
- Place holly, mistletoe, and poinsettias well out of reach.
8. Eye Injuries
Eye injuries surge over Christmas. Champagne corks can travel at nearly 50 mph, risking globe rupture or retinal detachment.
Conifer needles, glitter, and artificial snow can all cause corneal injury.
- Point champagne bottles and party poppers away from people's faces.
- Take care when handling Christmas trees.
- Avoid hanging ornaments at children's eye level.
- Rinse glitter-contaminated eyes with sterile saline.
9. Existing Ailments
By the ninth day, routine has often collapsed. Festive excess, stress and disrupted schedules can destabilize chronic disease.
- Ensure adequate medicines and testing supplies.
- Let hosts know dietary needs in advance.
- Avoid excess salt and alcohol in cardiovascular disease, and excess potassium in kidney disease.
- Increase blood glucose monitoring in diabetes.
10. Presents
Not all gifts are benign. The Child Accident Prevention Trust warned that cheap or counterfeit products may bypass safety standards.
UK safety authorities report that counterfeit Labubu dolls have made up a large share of the roughly 259,000 counterfeit toys seized at UK borders this year, and many have failed safety tests.
- Be cautious when buying for toddlers.
- Look for recognized safety markings.
- Avoid toys with strong magnets or button batteries.
- Laser pointers can cause permanent damage to vision.
11. Stress
As Christmas approaches, pressure mounts. In an NAH survey, 12% of men and 20% of women said they felt rushed, 32% of women were stressed, and 18% overwhelmed.
- Prioritize sleep.
- Get outdoors for early morning light.
- Ask for help and delegate chores.
12. Other People
The final hazard is often the most familiar: Family tension is almost traditional. In one survey, 37% of people said Christmas "wouldn't be the same" without arguments, and 54% admitted enjoying them.
- Set boundaries and agree expectations early.
- Stick to a budget.
- Avoid known flashpoint topics, such as politics.
- Create a quiet space for time out.
- One in 9 people spend Christmas alone. Plan ahead to make it a special day.
The hazards may feel seasonal, but the outcomes are not. For clinicians, the 12 risks offer a reminder that small interventions before Christmas can prevent significant harm after it.
Dr Sheena Meredith is an established medical writer, editor, and consultant in healthcare communications, with extensive experience writing for medical professionals and the general public. She is qualified in medicine and in law and medical ethics.
A version of this article first appeared on Medscape.com.
The 12 Dangers of Christmas
The 12 Dangers of Christmas
Empowering Culture Change and Safety on the Journey to Zero Harm With Huddle Cards
Empowering Culture Change and Safety on the Journey to Zero Harm With Huddle Cards
Safety event reporting plays a vital role in fostering a culture of safety within a health care organization. The US Department of Veterans Affairs (VA) has shifted its focus from eradicating medical errors to minimizing or eliminating harm to patients.1 The National Center for Patient Safety’s objective is to prevent recurring errors by identifying and addressing systemic problems that may have been overlooked.2
Taking inspiration from industries known for high reliability, such as aviation and nuclear power, the Veterans Health Administration (VHA) patient safety program aims to identify and eliminate system vulnerabilities, such as medical errors. Learning from near misses, which occur more frequently than actual adverse events, is a crucial part of this process.3 By addressing these issues, the VHA can establish safer systems and encourage continuous identification of potential problems with proactive resolution.
All staff should participate actively in event reporting, which involves documenting and communicating details, outcomes, and relevant data about an event to understand what occurred, evaluate success, identify areas for improvement, and inform future decisions. This helps identify system weaknesses, create opportunities to standardize procedures and enhance patient care.
At the high complexity Central Texas Veterans Health Care System (CTVHCS), the fiscal year (FY) 2023 All Employee Survey (AES) found that staff members require additional education and awareness regarding the reporting of patient safety concerns.4 The survey highlighted areas such as lack of education on reporting, doubts about the effectiveness of reporting, confusion about the process after a report is made, and insufficient feedback.
BACKGROUND
To improve the culture of safety and address deficiencies noted in the AES, the CTVHCS patient safety (PS) and high reliability organization (HRO) teams partnered to develop a quality improvement initiative to increase staff understanding of safety event reporting and strengthen the safety culture. The PS and HRO teams developed an innovative education model that integrates Joint Patient Safety Reporting System (JPSR) education into huddles.
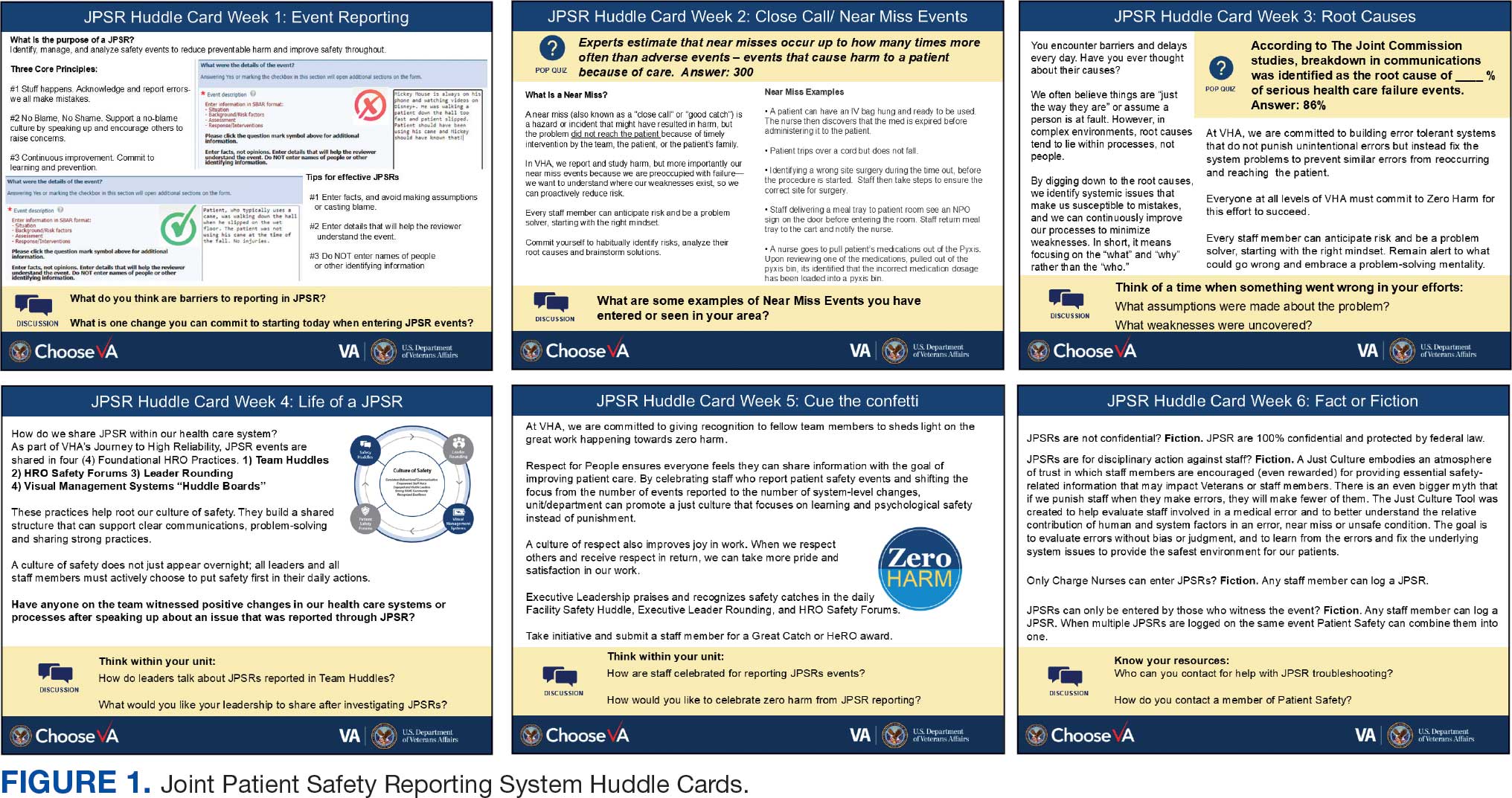
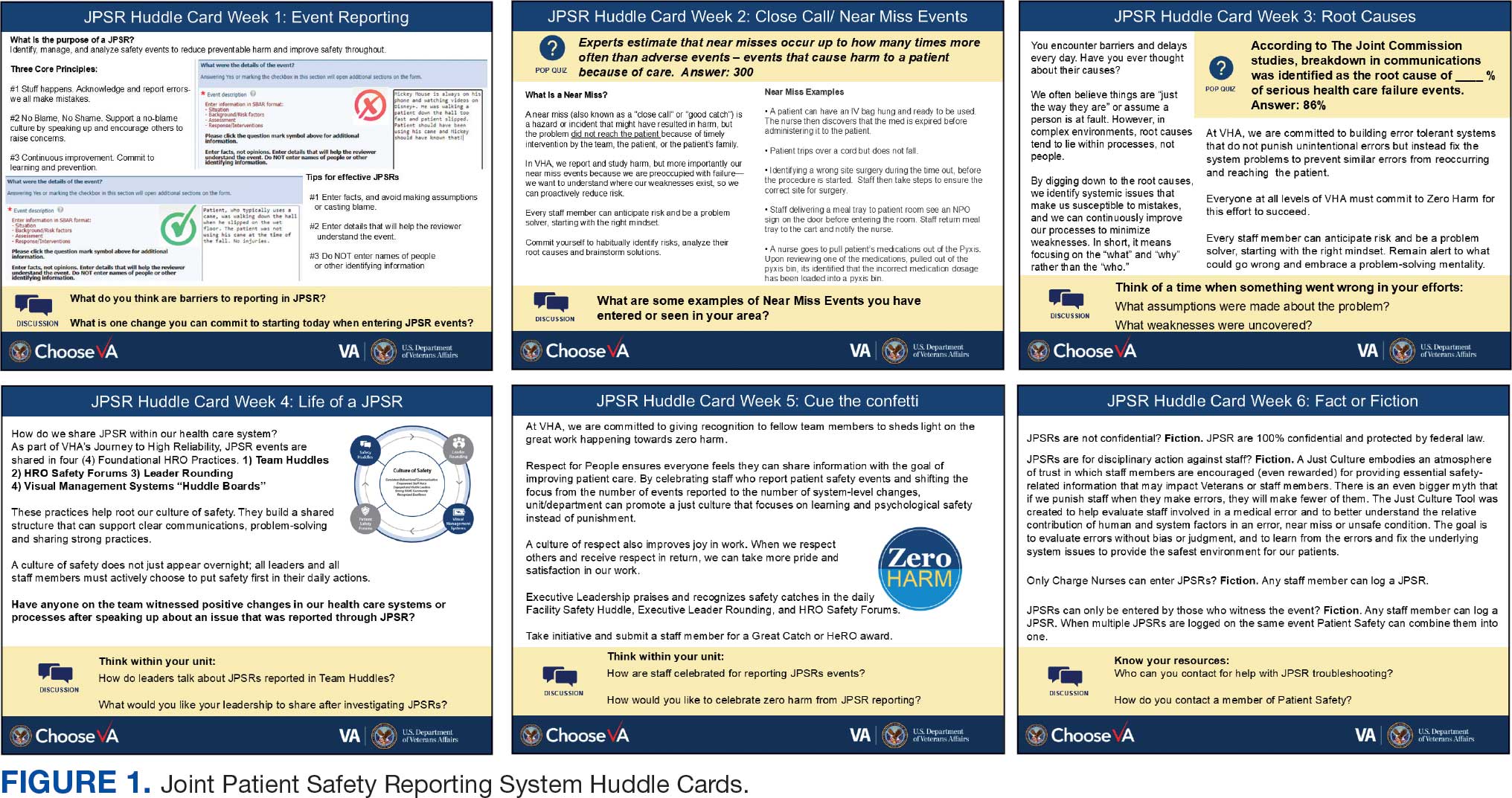
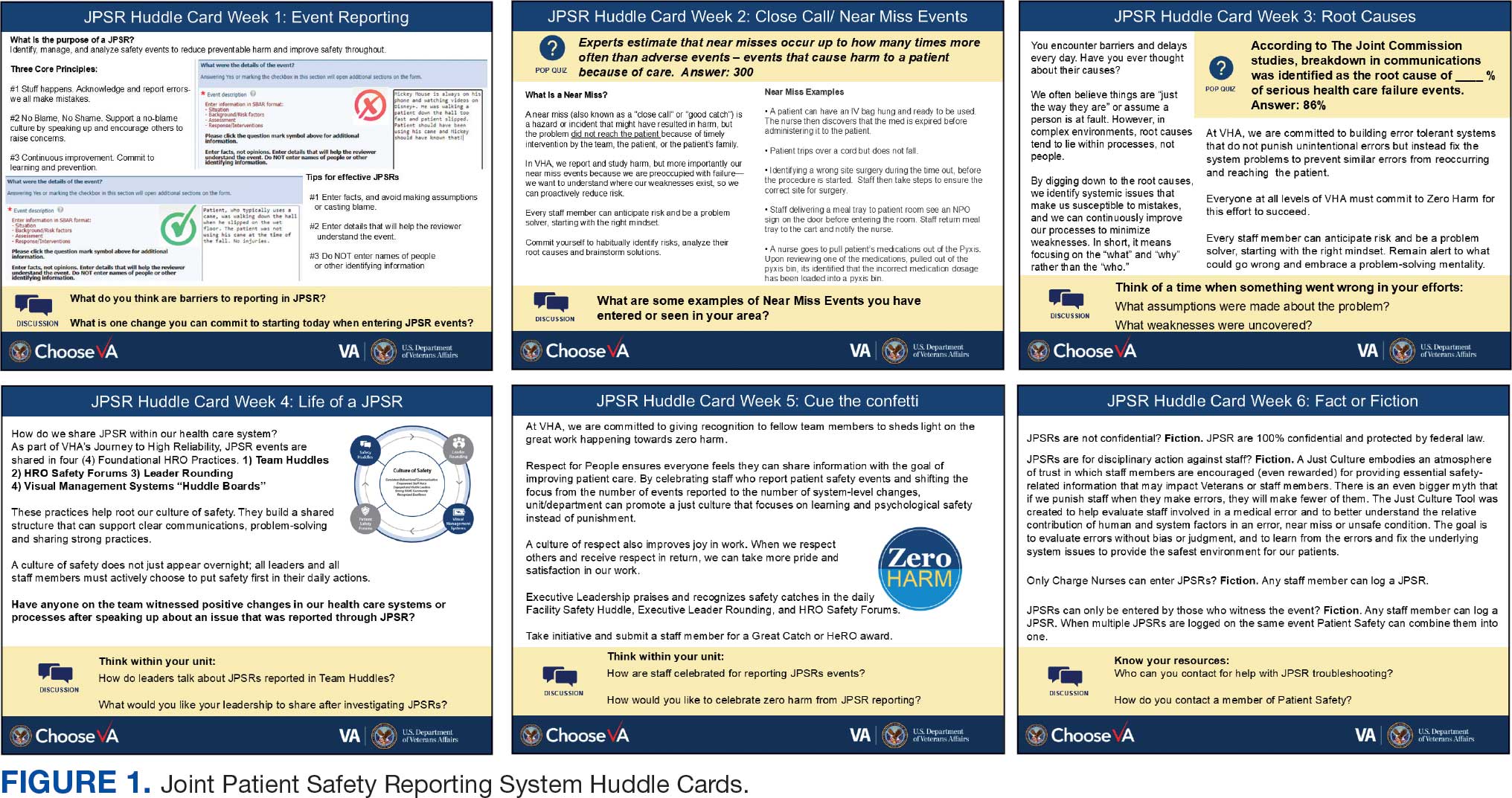
This initiative, called the JPSR Huddle Card Toolkit, sought to assess the impact of the toolkit on staff knowledge and behaviors related to patient safety event reporting. The toolkit consisted of educational materials encompassing 6 key areas: (1) reporting incidents; (2) close calls and near misses; (3) identification of root causes; (4) understanding the life cycle of a JPSR; (5) celebrating achievements; and (6) distinguishing between facts and fiction. Each JPSR huddle card included discussion points for the facilitator and was formatted on a 5 × 7-inch card (Figure 1). Topics were addressed during weekly safety huddles conducted in the pilot unit over a 6-week period. To evaluate its effectiveness, a pilot unit was selected and distributed an anonymous questionnaire paired with the JPSR huddle card toolkit to measure staff responses.
The pilot was conducted from November 2023 to January 2024. The participating pilot unit was a 10-bed critical care unit with 42 full-time employees. Nursing leadership, quality safety, and value personnel, and the Veterans Integrated Services Network (VISN) PS Team reviewed and approved the pilot.
Reporting of adverse events and near misses provides an opportunity to learn about latent systems errors.2 In 2018, the VHA began using the JPSR to standardize the capture and data management on medical errors and close calls across the Defense Health Administration (DHA) and VHA.1 The JPSR software is a joint application of the VHA and DHA. It improves the identification and documentation of patient safety-related events for VA medical centers, military hospitals and clinics, active-duty personnel, veterans and their families.
Event reporting is a key element in advancing high reliability and achieving zero preventable harm.1 Teams use these data to identify organizational patient safety trends and preempt common safety issues. All data are protected under 38 USC §5705 and 10 USC §1102.5 The JPSR single-source system standardizes the collection of core data points and increases collaboration between the DHA and VHA. This partnership increases insight into safety-related incidents, allowing for earlier detection and prevention of patient harm or injury incidents.
Numerous studies consistently commend huddles for their effectiveness in promoting teamwork and their positive impact on patient safety.6-8 Huddles facilitate connections between employees who may not typically interact, provide opportunities for discussions, and serve as a platform to encourage employees to voice their opinions. By fostering these interactions, huddles empower employees and create an environment for shared understanding, building trust, and promoting continuous learning.8
OBSERVATIONS
The JPSR huddle card initiative aimed to improve understanding of the JPSR process and promote knowledge and attitudes about patient safety and event reporting, while emphasizing shared responsibility. The goals focused on effective communication, respect for expertise, awareness of operational nuances, voicing concerns, and ensuring zero harm.
The facilitator initiated huddles by announcing their start to cultivate a constructive outcome.8 The JPSR huddle cards used a structured format designed to foster engagement and understanding of the topic. Each card begins with a factual statement or an open-ended question to gauge participants’ awareness or understanding. It then provides essential facts, principles, and relevant information to deepen knowledge. The card concludes with a discussion question, allowing facilitators to assess shared learning and encourage group reflection. This format promotes active participation and ensures that key concepts are both introduced and reinforced through dialogue.
The PS team standardized the format for all huddle cards, allowing 5 to 10 minutes for discussing training materials, receiving feedback, and concluding with a discussion question and call to action. Prior to each huddle, the facilitator would read a scripted remark that reviewed the objectives and ground rules for an effective huddle.
The PS and HRO teams promoted interactive discussions and welcomed ongoing feedback. Huddles provided a psychologically safe environment where individuals were encouraged to voice their thoughts and ideas.
Each weekly huddle card addressed a different patient safety topic. The Week 1 huddle card focuses on event reporting for safety improvement. The card outlines the purpose of JPSR as a tool to identify, manage, and analyze safety events to reduce preventable harm. The card emphasizes 3 core principles: (1) acknowledging mistakes, recognizing that errors happen; (2) no blame, no shame (encouraging a no-blame just culture to raise concerns); and (3) continuous improvement (committing to ongoing learning and prevention). It provides guidance on event details entry, advising staff to include facts in an SBAR (Situation, Background, Assessment, Response) format, avoid assumptions, and exclude personal identifiers. Tips include entering only relevant facts to help reviewers understand the incident. The card ends with discussion questions on reporting barriers and potential improvements in event reporting practices.
The Week 2 huddle card focuses on understanding and reporting near miss events, also known as close calls or good catches. A near miss is an incident where a potential hazard was identified and prevented before it reached the patient, avoiding harm due to timely intervention. The card emphasizes the importance of identifying these events to understand weaknesses and proactively reduce risks. Examples of near misses include discovering expired medication before use, catching a potential wrong-site surgery, and noticing incorrect medication dosages. Staff are encouraged to develop a mindset for anticipating and solving risks. The card ends with a discussion asking participants to share examples of near misses in their area.
The Week 3 huddle card covers root causes in preventing errors. The card highlights that errors in health care often stem from flawed processes rather than individual faults. By identifying root causes, systemic weaknesses can be addressed to reduce mistakes and build more error-tolerant and robust systems. All staff are advised to adopt a mindset of continuous improvement, error trapping behaviors and problem-solving. It concludes with discussion questions prompting reflection on assumptions and identifying weaknesses when something goes wrong.
The Week 4 huddle card covers the life of a JPSR, detailing that after entry JPSR events are viewed by the highest leadership levels at the morning report, and that lessons learned are distributed through frontline managers and chiefs in a monthly report to be shared with frontline staff. Additionally, JPSR trends are shared during monthly HRO safety forums. These practices promote a culture of safety through open communication and problem-solving. Staff and leaders are encouraged to prioritize safety daily. Discussion prompts ask team members if they had seen positive changes from JPSR reporting and what they would like leadership to communicate after investigations.
The Week 5 huddle card covers celebrating safety event reporting called Cue the Confetti. The VHA emphasizes recognizing staff who report safety events as part of their commitment to zero harm. By celebrating these contributions, the VHA fosters respect, joy, and satisfaction in the work. Staff are encouraged to nominate colleagues for recognition, reinforcing a supportive environment. Prompts invite teams to discuss how they celebrate JPSR reporting and how they’d like to enhance this culture of appreciation.
The Week 6 huddle card covers common misconceptions about JPSR. Key facts include that JPSRs are confidential, not for disciplinary action, and can be submitted by any staff member at any time. Only PS can view reporter identities for clarification purposes. The card concludes with prompts to ensure staff know how to access JPSR support and resources.
Measuring the impact on staff was essential to assess effectiveness and gather data for program improvement. To evaluate the impact of the huddle cards on the staff, the team provided a voluntary and anonymous 9 question survey (Figure 2). The survey was completed before the pilot began and again at the end of Week 6.
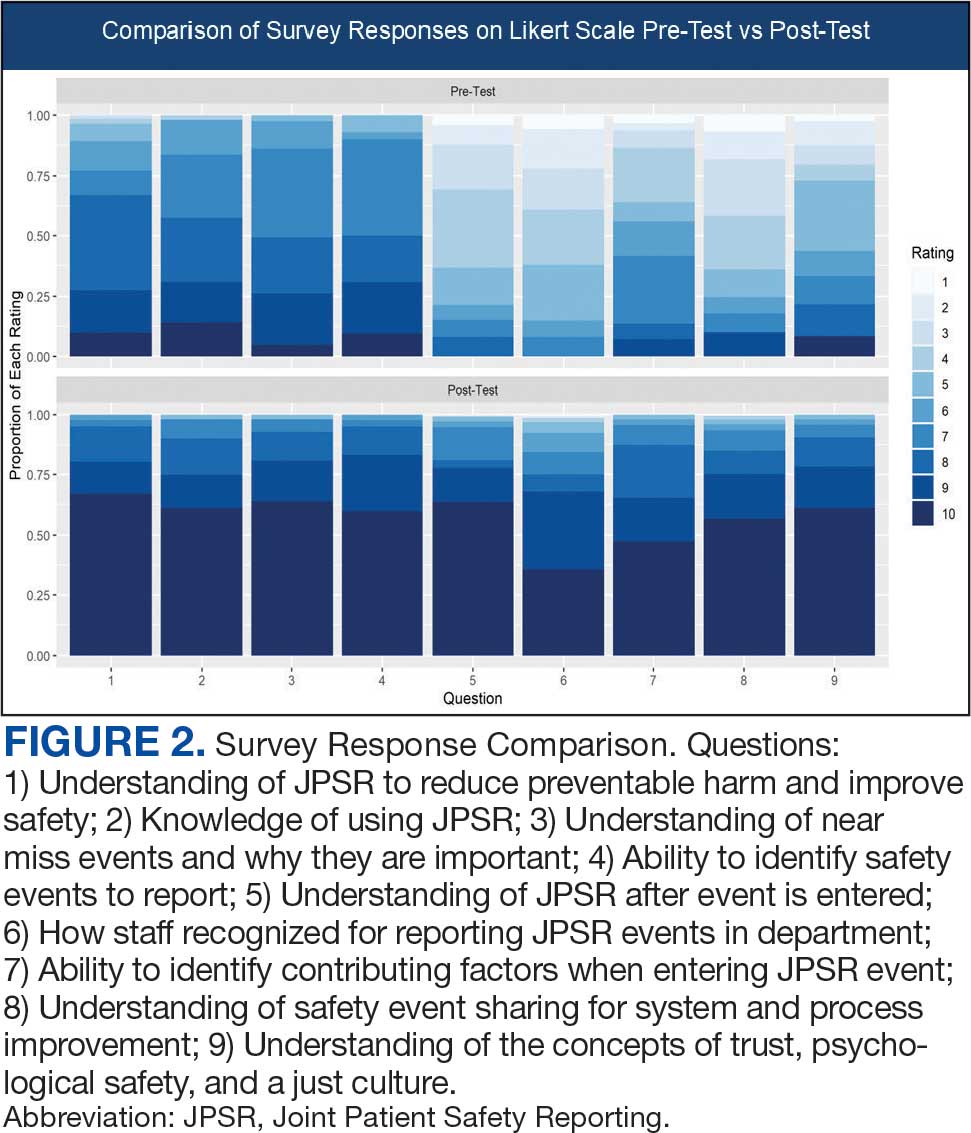
Questions 1 through 5 and 7 through 9 pertained to participants’ perceived knowledge and understanding of aspects of the JPSR. Perceived improvement among intensive care unit (ICU) participants ranged from 15% to 53%. There was a positive increase associated with every question with the top improvements: question 8, “How do you rate your understanding of how we share safety events for system and process improvement?” (53.4% increase); question 5, “How do you rate your understanding of what happens to a JPSR after it is entered?” (51.9% increase), and question 9, “How do you rate your understanding of the concepts of trust, psychological safety and a just culture?” (47.8% increase).
The survey analysis was not able to track individual changes. As a result, the findings reflect an overall change for the entire study group. Moreover, the questions assessed participants’ perceived knowledge rather than actual knowledge gained. It is important to note that there may be a significant gap between the actual knowledge gained and how participants perceive it. Additionally, improvement in knowledge and comprehension does not necessarily translate into behavior changes.
CONCLUSIONS
The use of JPSR huddle cards and direct engagement with staff during safety huddles yielded positive outcomes. On average, participants demonstrated higher scores in posttest questions compared to pretest questions. The posttest scores were consistently higher than the pretest scores, showing an average increase of around 2 standard deviations across all questions. This indicates an improvement in participants’ perceived knowledge and comprehension of the JPSR material.
During the pilot implementation of the huddle cards, there was a notable improvement in team member engagement. The structured format of the cards facilitated focused and meaningful discussions during safety huddles, encouraging open dialogue and fostering a culture of safety. Team members actively participated in identifying potential risks, sharing observations, and proposing actionable solutions, which reflected an enhanced sense of ownership regarding safety practices.
The support dialogue facilitated by the huddle cards highlighted the significance of mutual accountability and a collective commitment to achieving zero harm. This collaborative environment strengthened trust among team members and underscored the importance of shared vigilance in preventing adverse events. The pilot demonstrated the potential of huddle cards as an essential tool for enhancing team-based safety initiatives and promoting a culture of high reliability within the organization.
The total number of JPSR events in the ICU rose from 156 in FY 23 to 170 in FY 24. Adverse events increased from 19 to 31, while close calls saw a slight uptick from 137 to 139. Despite the overall rise in adverse events, a detailed analysis indicated that incidents of moderate harm decreased from 4 in FY 23 to 2 in FY 24. Furthermore, there was 1 reported case of death or severe harm in FY 23, which decreased to 0 in FY 24. This trend is consistent with the overarching objective of a high-reliability organization to achieve zero harm.
The next step is to expand this initiative across CTVHCS. This initiative aims to make this an annual education for all areas. The JPSR huddle card toolkit will be formatted by the media department for easy printing and retrieval. Leaders within units, clinics, and services will be empowered to facilitate the sessions in their safety huddles and reap the same outcomes as in the pilot. CTVHCS PS will monitor the effectiveness of this through ongoing CTVHCS patient safety rounding and future AES.
- Essen K, Villalobos C, Sculli GL, Steinbach L. Establishing a just culture: implications for the Veterans Health Administration journey to high reliability. Fed Pract. 2024;41:290-297. doi:10.12788/fp.0512
- Louis MY, Hussain LR, Dhanraj DN, et al. Improving patient safety event reporting among residents and teaching faculty. Ochsner J. 2016;16:73-80.
- Pimental CB, Snow AL, Carnes SL, et al. Huddles and their effectiveness at the frontlines of clinical care: a scoping review. J Gen Intern Med. 2021;36:2772-2783. doi:10.1007/s11606-021-06632-9
- National Academies of Sciences, Engineering, and Medicine. Appendix C: Nature of Veterans Health Administration Facilities Management (Engineering) Tasks and Staffing. Facilities Staffing Requirements for the Veterans Health Administration-Resource Planning and Methodology for the Future. National Academies Press. 2020:105-116. Accessed August 11, 2025. https://nap.nationalacademies.org/read/25454/chapter/11
- Woodier N, Burnett C, Moppett I. The value of learning from near misses to improve patient safety: a scoping review. J Patient Saf. 2023;19:42-47. doi:10.1097/pts.0000000000001078
- Ismail A, Khalid SNM. Patient safety culture and its determinants among healthcare professionals at a cluster hospital in Malaysia: a cross-sectional study. BMJ Open. 2022;12:e060546. doi:10.1136/bmjopen-2021-060546
- Ngo J, Lau D, Ploquin J, Receveur T, Stassen K, Del Castilho C. Improving incident reporting among physicians at south health campus hospital. BMJ Open Qual. 2022;11:e001945. doi:10.1136/bmjoq-2022-001945
- Oweidat I, Al-Mugheed K, Alsenany SA, et al. Awareness of reporting practices and barriers to incident reporting among nurses. BMC Nurs. 2023;22:231. doi:10.1186/s12912-023-01376-9
Safety event reporting plays a vital role in fostering a culture of safety within a health care organization. The US Department of Veterans Affairs (VA) has shifted its focus from eradicating medical errors to minimizing or eliminating harm to patients.1 The National Center for Patient Safety’s objective is to prevent recurring errors by identifying and addressing systemic problems that may have been overlooked.2
Taking inspiration from industries known for high reliability, such as aviation and nuclear power, the Veterans Health Administration (VHA) patient safety program aims to identify and eliminate system vulnerabilities, such as medical errors. Learning from near misses, which occur more frequently than actual adverse events, is a crucial part of this process.3 By addressing these issues, the VHA can establish safer systems and encourage continuous identification of potential problems with proactive resolution.
All staff should participate actively in event reporting, which involves documenting and communicating details, outcomes, and relevant data about an event to understand what occurred, evaluate success, identify areas for improvement, and inform future decisions. This helps identify system weaknesses, create opportunities to standardize procedures and enhance patient care.
At the high complexity Central Texas Veterans Health Care System (CTVHCS), the fiscal year (FY) 2023 All Employee Survey (AES) found that staff members require additional education and awareness regarding the reporting of patient safety concerns.4 The survey highlighted areas such as lack of education on reporting, doubts about the effectiveness of reporting, confusion about the process after a report is made, and insufficient feedback.
BACKGROUND
To improve the culture of safety and address deficiencies noted in the AES, the CTVHCS patient safety (PS) and high reliability organization (HRO) teams partnered to develop a quality improvement initiative to increase staff understanding of safety event reporting and strengthen the safety culture. The PS and HRO teams developed an innovative education model that integrates Joint Patient Safety Reporting System (JPSR) education into huddles.
This initiative, called the JPSR Huddle Card Toolkit, sought to assess the impact of the toolkit on staff knowledge and behaviors related to patient safety event reporting. The toolkit consisted of educational materials encompassing 6 key areas: (1) reporting incidents; (2) close calls and near misses; (3) identification of root causes; (4) understanding the life cycle of a JPSR; (5) celebrating achievements; and (6) distinguishing between facts and fiction. Each JPSR huddle card included discussion points for the facilitator and was formatted on a 5 × 7-inch card (Figure 1). Topics were addressed during weekly safety huddles conducted in the pilot unit over a 6-week period. To evaluate its effectiveness, a pilot unit was selected and distributed an anonymous questionnaire paired with the JPSR huddle card toolkit to measure staff responses.
The pilot was conducted from November 2023 to January 2024. The participating pilot unit was a 10-bed critical care unit with 42 full-time employees. Nursing leadership, quality safety, and value personnel, and the Veterans Integrated Services Network (VISN) PS Team reviewed and approved the pilot.
Reporting of adverse events and near misses provides an opportunity to learn about latent systems errors.2 In 2018, the VHA began using the JPSR to standardize the capture and data management on medical errors and close calls across the Defense Health Administration (DHA) and VHA.1 The JPSR software is a joint application of the VHA and DHA. It improves the identification and documentation of patient safety-related events for VA medical centers, military hospitals and clinics, active-duty personnel, veterans and their families.
Event reporting is a key element in advancing high reliability and achieving zero preventable harm.1 Teams use these data to identify organizational patient safety trends and preempt common safety issues. All data are protected under 38 USC §5705 and 10 USC §1102.5 The JPSR single-source system standardizes the collection of core data points and increases collaboration between the DHA and VHA. This partnership increases insight into safety-related incidents, allowing for earlier detection and prevention of patient harm or injury incidents.
Numerous studies consistently commend huddles for their effectiveness in promoting teamwork and their positive impact on patient safety.6-8 Huddles facilitate connections between employees who may not typically interact, provide opportunities for discussions, and serve as a platform to encourage employees to voice their opinions. By fostering these interactions, huddles empower employees and create an environment for shared understanding, building trust, and promoting continuous learning.8
OBSERVATIONS
The JPSR huddle card initiative aimed to improve understanding of the JPSR process and promote knowledge and attitudes about patient safety and event reporting, while emphasizing shared responsibility. The goals focused on effective communication, respect for expertise, awareness of operational nuances, voicing concerns, and ensuring zero harm.
The facilitator initiated huddles by announcing their start to cultivate a constructive outcome.8 The JPSR huddle cards used a structured format designed to foster engagement and understanding of the topic. Each card begins with a factual statement or an open-ended question to gauge participants’ awareness or understanding. It then provides essential facts, principles, and relevant information to deepen knowledge. The card concludes with a discussion question, allowing facilitators to assess shared learning and encourage group reflection. This format promotes active participation and ensures that key concepts are both introduced and reinforced through dialogue.
The PS team standardized the format for all huddle cards, allowing 5 to 10 minutes for discussing training materials, receiving feedback, and concluding with a discussion question and call to action. Prior to each huddle, the facilitator would read a scripted remark that reviewed the objectives and ground rules for an effective huddle.
The PS and HRO teams promoted interactive discussions and welcomed ongoing feedback. Huddles provided a psychologically safe environment where individuals were encouraged to voice their thoughts and ideas.
Each weekly huddle card addressed a different patient safety topic. The Week 1 huddle card focuses on event reporting for safety improvement. The card outlines the purpose of JPSR as a tool to identify, manage, and analyze safety events to reduce preventable harm. The card emphasizes 3 core principles: (1) acknowledging mistakes, recognizing that errors happen; (2) no blame, no shame (encouraging a no-blame just culture to raise concerns); and (3) continuous improvement (committing to ongoing learning and prevention). It provides guidance on event details entry, advising staff to include facts in an SBAR (Situation, Background, Assessment, Response) format, avoid assumptions, and exclude personal identifiers. Tips include entering only relevant facts to help reviewers understand the incident. The card ends with discussion questions on reporting barriers and potential improvements in event reporting practices.
The Week 2 huddle card focuses on understanding and reporting near miss events, also known as close calls or good catches. A near miss is an incident where a potential hazard was identified and prevented before it reached the patient, avoiding harm due to timely intervention. The card emphasizes the importance of identifying these events to understand weaknesses and proactively reduce risks. Examples of near misses include discovering expired medication before use, catching a potential wrong-site surgery, and noticing incorrect medication dosages. Staff are encouraged to develop a mindset for anticipating and solving risks. The card ends with a discussion asking participants to share examples of near misses in their area.
The Week 3 huddle card covers root causes in preventing errors. The card highlights that errors in health care often stem from flawed processes rather than individual faults. By identifying root causes, systemic weaknesses can be addressed to reduce mistakes and build more error-tolerant and robust systems. All staff are advised to adopt a mindset of continuous improvement, error trapping behaviors and problem-solving. It concludes with discussion questions prompting reflection on assumptions and identifying weaknesses when something goes wrong.
The Week 4 huddle card covers the life of a JPSR, detailing that after entry JPSR events are viewed by the highest leadership levels at the morning report, and that lessons learned are distributed through frontline managers and chiefs in a monthly report to be shared with frontline staff. Additionally, JPSR trends are shared during monthly HRO safety forums. These practices promote a culture of safety through open communication and problem-solving. Staff and leaders are encouraged to prioritize safety daily. Discussion prompts ask team members if they had seen positive changes from JPSR reporting and what they would like leadership to communicate after investigations.
The Week 5 huddle card covers celebrating safety event reporting called Cue the Confetti. The VHA emphasizes recognizing staff who report safety events as part of their commitment to zero harm. By celebrating these contributions, the VHA fosters respect, joy, and satisfaction in the work. Staff are encouraged to nominate colleagues for recognition, reinforcing a supportive environment. Prompts invite teams to discuss how they celebrate JPSR reporting and how they’d like to enhance this culture of appreciation.
The Week 6 huddle card covers common misconceptions about JPSR. Key facts include that JPSRs are confidential, not for disciplinary action, and can be submitted by any staff member at any time. Only PS can view reporter identities for clarification purposes. The card concludes with prompts to ensure staff know how to access JPSR support and resources.
Measuring the impact on staff was essential to assess effectiveness and gather data for program improvement. To evaluate the impact of the huddle cards on the staff, the team provided a voluntary and anonymous 9 question survey (Figure 2). The survey was completed before the pilot began and again at the end of Week 6.
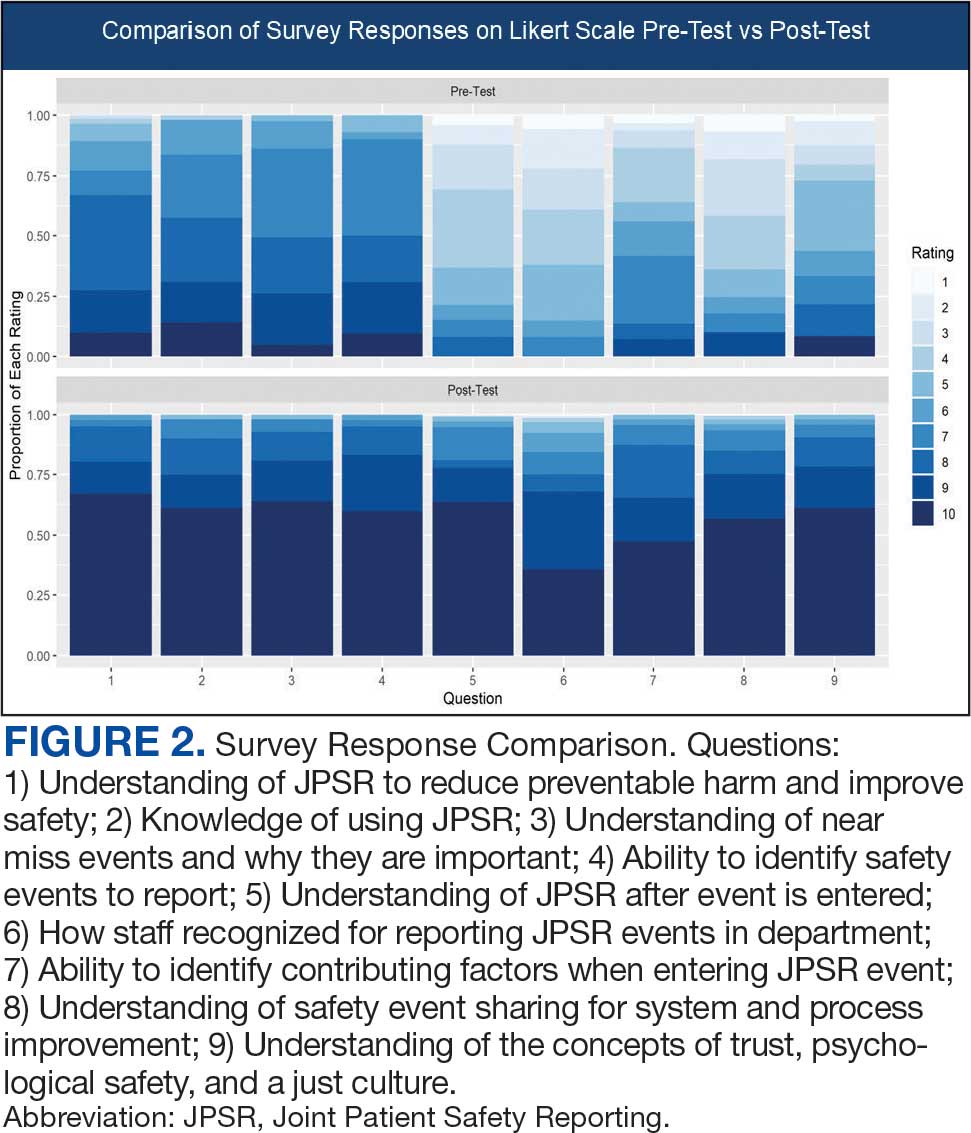
Questions 1 through 5 and 7 through 9 pertained to participants’ perceived knowledge and understanding of aspects of the JPSR. Perceived improvement among intensive care unit (ICU) participants ranged from 15% to 53%. There was a positive increase associated with every question with the top improvements: question 8, “How do you rate your understanding of how we share safety events for system and process improvement?” (53.4% increase); question 5, “How do you rate your understanding of what happens to a JPSR after it is entered?” (51.9% increase), and question 9, “How do you rate your understanding of the concepts of trust, psychological safety and a just culture?” (47.8% increase).
The survey analysis was not able to track individual changes. As a result, the findings reflect an overall change for the entire study group. Moreover, the questions assessed participants’ perceived knowledge rather than actual knowledge gained. It is important to note that there may be a significant gap between the actual knowledge gained and how participants perceive it. Additionally, improvement in knowledge and comprehension does not necessarily translate into behavior changes.
CONCLUSIONS
The use of JPSR huddle cards and direct engagement with staff during safety huddles yielded positive outcomes. On average, participants demonstrated higher scores in posttest questions compared to pretest questions. The posttest scores were consistently higher than the pretest scores, showing an average increase of around 2 standard deviations across all questions. This indicates an improvement in participants’ perceived knowledge and comprehension of the JPSR material.
During the pilot implementation of the huddle cards, there was a notable improvement in team member engagement. The structured format of the cards facilitated focused and meaningful discussions during safety huddles, encouraging open dialogue and fostering a culture of safety. Team members actively participated in identifying potential risks, sharing observations, and proposing actionable solutions, which reflected an enhanced sense of ownership regarding safety practices.
The support dialogue facilitated by the huddle cards highlighted the significance of mutual accountability and a collective commitment to achieving zero harm. This collaborative environment strengthened trust among team members and underscored the importance of shared vigilance in preventing adverse events. The pilot demonstrated the potential of huddle cards as an essential tool for enhancing team-based safety initiatives and promoting a culture of high reliability within the organization.
The total number of JPSR events in the ICU rose from 156 in FY 23 to 170 in FY 24. Adverse events increased from 19 to 31, while close calls saw a slight uptick from 137 to 139. Despite the overall rise in adverse events, a detailed analysis indicated that incidents of moderate harm decreased from 4 in FY 23 to 2 in FY 24. Furthermore, there was 1 reported case of death or severe harm in FY 23, which decreased to 0 in FY 24. This trend is consistent with the overarching objective of a high-reliability organization to achieve zero harm.
The next step is to expand this initiative across CTVHCS. This initiative aims to make this an annual education for all areas. The JPSR huddle card toolkit will be formatted by the media department for easy printing and retrieval. Leaders within units, clinics, and services will be empowered to facilitate the sessions in their safety huddles and reap the same outcomes as in the pilot. CTVHCS PS will monitor the effectiveness of this through ongoing CTVHCS patient safety rounding and future AES.
Safety event reporting plays a vital role in fostering a culture of safety within a health care organization. The US Department of Veterans Affairs (VA) has shifted its focus from eradicating medical errors to minimizing or eliminating harm to patients.1 The National Center for Patient Safety’s objective is to prevent recurring errors by identifying and addressing systemic problems that may have been overlooked.2
Taking inspiration from industries known for high reliability, such as aviation and nuclear power, the Veterans Health Administration (VHA) patient safety program aims to identify and eliminate system vulnerabilities, such as medical errors. Learning from near misses, which occur more frequently than actual adverse events, is a crucial part of this process.3 By addressing these issues, the VHA can establish safer systems and encourage continuous identification of potential problems with proactive resolution.
All staff should participate actively in event reporting, which involves documenting and communicating details, outcomes, and relevant data about an event to understand what occurred, evaluate success, identify areas for improvement, and inform future decisions. This helps identify system weaknesses, create opportunities to standardize procedures and enhance patient care.
At the high complexity Central Texas Veterans Health Care System (CTVHCS), the fiscal year (FY) 2023 All Employee Survey (AES) found that staff members require additional education and awareness regarding the reporting of patient safety concerns.4 The survey highlighted areas such as lack of education on reporting, doubts about the effectiveness of reporting, confusion about the process after a report is made, and insufficient feedback.
BACKGROUND
To improve the culture of safety and address deficiencies noted in the AES, the CTVHCS patient safety (PS) and high reliability organization (HRO) teams partnered to develop a quality improvement initiative to increase staff understanding of safety event reporting and strengthen the safety culture. The PS and HRO teams developed an innovative education model that integrates Joint Patient Safety Reporting System (JPSR) education into huddles.
This initiative, called the JPSR Huddle Card Toolkit, sought to assess the impact of the toolkit on staff knowledge and behaviors related to patient safety event reporting. The toolkit consisted of educational materials encompassing 6 key areas: (1) reporting incidents; (2) close calls and near misses; (3) identification of root causes; (4) understanding the life cycle of a JPSR; (5) celebrating achievements; and (6) distinguishing between facts and fiction. Each JPSR huddle card included discussion points for the facilitator and was formatted on a 5 × 7-inch card (Figure 1). Topics were addressed during weekly safety huddles conducted in the pilot unit over a 6-week period. To evaluate its effectiveness, a pilot unit was selected and distributed an anonymous questionnaire paired with the JPSR huddle card toolkit to measure staff responses.
The pilot was conducted from November 2023 to January 2024. The participating pilot unit was a 10-bed critical care unit with 42 full-time employees. Nursing leadership, quality safety, and value personnel, and the Veterans Integrated Services Network (VISN) PS Team reviewed and approved the pilot.
Reporting of adverse events and near misses provides an opportunity to learn about latent systems errors.2 In 2018, the VHA began using the JPSR to standardize the capture and data management on medical errors and close calls across the Defense Health Administration (DHA) and VHA.1 The JPSR software is a joint application of the VHA and DHA. It improves the identification and documentation of patient safety-related events for VA medical centers, military hospitals and clinics, active-duty personnel, veterans and their families.
Event reporting is a key element in advancing high reliability and achieving zero preventable harm.1 Teams use these data to identify organizational patient safety trends and preempt common safety issues. All data are protected under 38 USC §5705 and 10 USC §1102.5 The JPSR single-source system standardizes the collection of core data points and increases collaboration between the DHA and VHA. This partnership increases insight into safety-related incidents, allowing for earlier detection and prevention of patient harm or injury incidents.
Numerous studies consistently commend huddles for their effectiveness in promoting teamwork and their positive impact on patient safety.6-8 Huddles facilitate connections between employees who may not typically interact, provide opportunities for discussions, and serve as a platform to encourage employees to voice their opinions. By fostering these interactions, huddles empower employees and create an environment for shared understanding, building trust, and promoting continuous learning.8
OBSERVATIONS
The JPSR huddle card initiative aimed to improve understanding of the JPSR process and promote knowledge and attitudes about patient safety and event reporting, while emphasizing shared responsibility. The goals focused on effective communication, respect for expertise, awareness of operational nuances, voicing concerns, and ensuring zero harm.
The facilitator initiated huddles by announcing their start to cultivate a constructive outcome.8 The JPSR huddle cards used a structured format designed to foster engagement and understanding of the topic. Each card begins with a factual statement or an open-ended question to gauge participants’ awareness or understanding. It then provides essential facts, principles, and relevant information to deepen knowledge. The card concludes with a discussion question, allowing facilitators to assess shared learning and encourage group reflection. This format promotes active participation and ensures that key concepts are both introduced and reinforced through dialogue.
The PS team standardized the format for all huddle cards, allowing 5 to 10 minutes for discussing training materials, receiving feedback, and concluding with a discussion question and call to action. Prior to each huddle, the facilitator would read a scripted remark that reviewed the objectives and ground rules for an effective huddle.
The PS and HRO teams promoted interactive discussions and welcomed ongoing feedback. Huddles provided a psychologically safe environment where individuals were encouraged to voice their thoughts and ideas.
Each weekly huddle card addressed a different patient safety topic. The Week 1 huddle card focuses on event reporting for safety improvement. The card outlines the purpose of JPSR as a tool to identify, manage, and analyze safety events to reduce preventable harm. The card emphasizes 3 core principles: (1) acknowledging mistakes, recognizing that errors happen; (2) no blame, no shame (encouraging a no-blame just culture to raise concerns); and (3) continuous improvement (committing to ongoing learning and prevention). It provides guidance on event details entry, advising staff to include facts in an SBAR (Situation, Background, Assessment, Response) format, avoid assumptions, and exclude personal identifiers. Tips include entering only relevant facts to help reviewers understand the incident. The card ends with discussion questions on reporting barriers and potential improvements in event reporting practices.
The Week 2 huddle card focuses on understanding and reporting near miss events, also known as close calls or good catches. A near miss is an incident where a potential hazard was identified and prevented before it reached the patient, avoiding harm due to timely intervention. The card emphasizes the importance of identifying these events to understand weaknesses and proactively reduce risks. Examples of near misses include discovering expired medication before use, catching a potential wrong-site surgery, and noticing incorrect medication dosages. Staff are encouraged to develop a mindset for anticipating and solving risks. The card ends with a discussion asking participants to share examples of near misses in their area.
The Week 3 huddle card covers root causes in preventing errors. The card highlights that errors in health care often stem from flawed processes rather than individual faults. By identifying root causes, systemic weaknesses can be addressed to reduce mistakes and build more error-tolerant and robust systems. All staff are advised to adopt a mindset of continuous improvement, error trapping behaviors and problem-solving. It concludes with discussion questions prompting reflection on assumptions and identifying weaknesses when something goes wrong.
The Week 4 huddle card covers the life of a JPSR, detailing that after entry JPSR events are viewed by the highest leadership levels at the morning report, and that lessons learned are distributed through frontline managers and chiefs in a monthly report to be shared with frontline staff. Additionally, JPSR trends are shared during monthly HRO safety forums. These practices promote a culture of safety through open communication and problem-solving. Staff and leaders are encouraged to prioritize safety daily. Discussion prompts ask team members if they had seen positive changes from JPSR reporting and what they would like leadership to communicate after investigations.
The Week 5 huddle card covers celebrating safety event reporting called Cue the Confetti. The VHA emphasizes recognizing staff who report safety events as part of their commitment to zero harm. By celebrating these contributions, the VHA fosters respect, joy, and satisfaction in the work. Staff are encouraged to nominate colleagues for recognition, reinforcing a supportive environment. Prompts invite teams to discuss how they celebrate JPSR reporting and how they’d like to enhance this culture of appreciation.
The Week 6 huddle card covers common misconceptions about JPSR. Key facts include that JPSRs are confidential, not for disciplinary action, and can be submitted by any staff member at any time. Only PS can view reporter identities for clarification purposes. The card concludes with prompts to ensure staff know how to access JPSR support and resources.
Measuring the impact on staff was essential to assess effectiveness and gather data for program improvement. To evaluate the impact of the huddle cards on the staff, the team provided a voluntary and anonymous 9 question survey (Figure 2). The survey was completed before the pilot began and again at the end of Week 6.
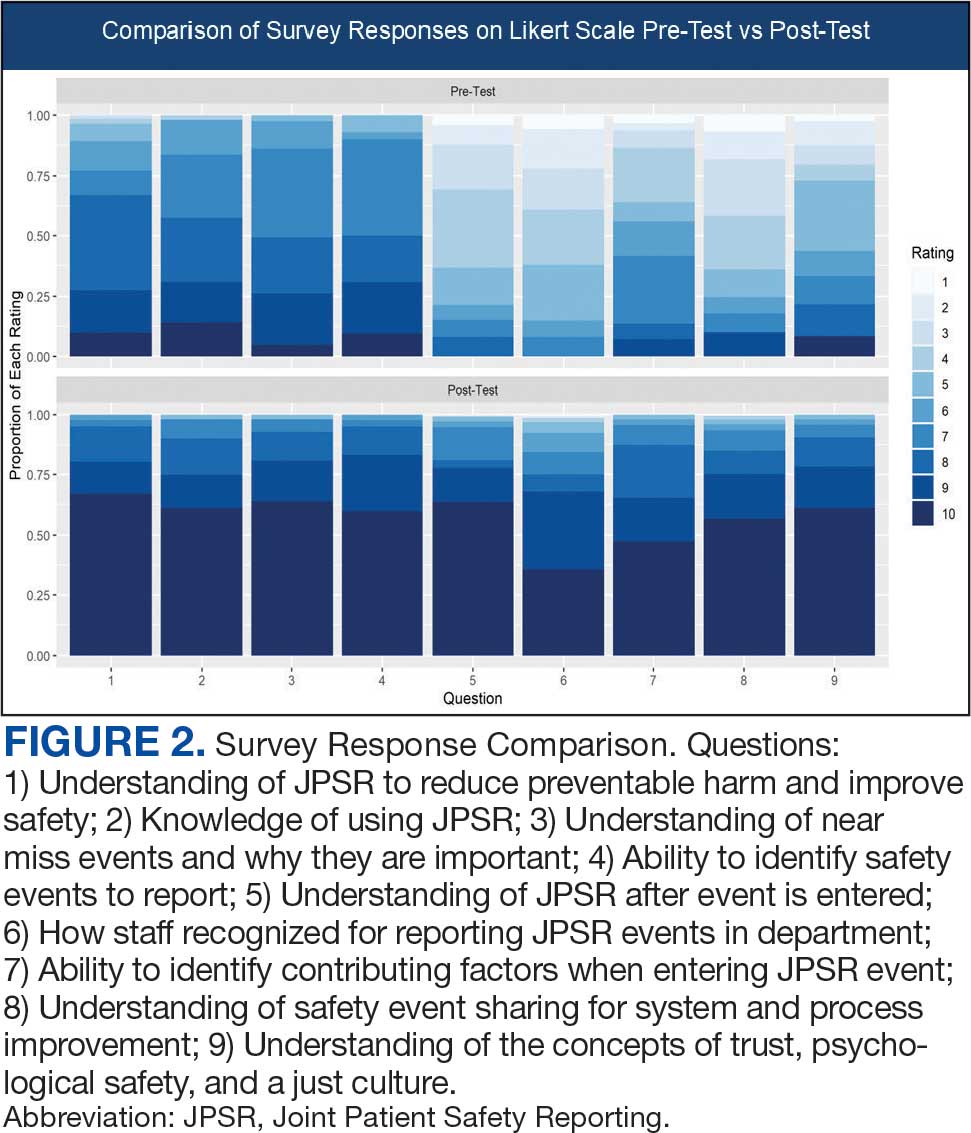
Questions 1 through 5 and 7 through 9 pertained to participants’ perceived knowledge and understanding of aspects of the JPSR. Perceived improvement among intensive care unit (ICU) participants ranged from 15% to 53%. There was a positive increase associated with every question with the top improvements: question 8, “How do you rate your understanding of how we share safety events for system and process improvement?” (53.4% increase); question 5, “How do you rate your understanding of what happens to a JPSR after it is entered?” (51.9% increase), and question 9, “How do you rate your understanding of the concepts of trust, psychological safety and a just culture?” (47.8% increase).
The survey analysis was not able to track individual changes. As a result, the findings reflect an overall change for the entire study group. Moreover, the questions assessed participants’ perceived knowledge rather than actual knowledge gained. It is important to note that there may be a significant gap between the actual knowledge gained and how participants perceive it. Additionally, improvement in knowledge and comprehension does not necessarily translate into behavior changes.
CONCLUSIONS
The use of JPSR huddle cards and direct engagement with staff during safety huddles yielded positive outcomes. On average, participants demonstrated higher scores in posttest questions compared to pretest questions. The posttest scores were consistently higher than the pretest scores, showing an average increase of around 2 standard deviations across all questions. This indicates an improvement in participants’ perceived knowledge and comprehension of the JPSR material.
During the pilot implementation of the huddle cards, there was a notable improvement in team member engagement. The structured format of the cards facilitated focused and meaningful discussions during safety huddles, encouraging open dialogue and fostering a culture of safety. Team members actively participated in identifying potential risks, sharing observations, and proposing actionable solutions, which reflected an enhanced sense of ownership regarding safety practices.
The support dialogue facilitated by the huddle cards highlighted the significance of mutual accountability and a collective commitment to achieving zero harm. This collaborative environment strengthened trust among team members and underscored the importance of shared vigilance in preventing adverse events. The pilot demonstrated the potential of huddle cards as an essential tool for enhancing team-based safety initiatives and promoting a culture of high reliability within the organization.
The total number of JPSR events in the ICU rose from 156 in FY 23 to 170 in FY 24. Adverse events increased from 19 to 31, while close calls saw a slight uptick from 137 to 139. Despite the overall rise in adverse events, a detailed analysis indicated that incidents of moderate harm decreased from 4 in FY 23 to 2 in FY 24. Furthermore, there was 1 reported case of death or severe harm in FY 23, which decreased to 0 in FY 24. This trend is consistent with the overarching objective of a high-reliability organization to achieve zero harm.
The next step is to expand this initiative across CTVHCS. This initiative aims to make this an annual education for all areas. The JPSR huddle card toolkit will be formatted by the media department for easy printing and retrieval. Leaders within units, clinics, and services will be empowered to facilitate the sessions in their safety huddles and reap the same outcomes as in the pilot. CTVHCS PS will monitor the effectiveness of this through ongoing CTVHCS patient safety rounding and future AES.
- Essen K, Villalobos C, Sculli GL, Steinbach L. Establishing a just culture: implications for the Veterans Health Administration journey to high reliability. Fed Pract. 2024;41:290-297. doi:10.12788/fp.0512
- Louis MY, Hussain LR, Dhanraj DN, et al. Improving patient safety event reporting among residents and teaching faculty. Ochsner J. 2016;16:73-80.
- Pimental CB, Snow AL, Carnes SL, et al. Huddles and their effectiveness at the frontlines of clinical care: a scoping review. J Gen Intern Med. 2021;36:2772-2783. doi:10.1007/s11606-021-06632-9
- National Academies of Sciences, Engineering, and Medicine. Appendix C: Nature of Veterans Health Administration Facilities Management (Engineering) Tasks and Staffing. Facilities Staffing Requirements for the Veterans Health Administration-Resource Planning and Methodology for the Future. National Academies Press. 2020:105-116. Accessed August 11, 2025. https://nap.nationalacademies.org/read/25454/chapter/11
- Woodier N, Burnett C, Moppett I. The value of learning from near misses to improve patient safety: a scoping review. J Patient Saf. 2023;19:42-47. doi:10.1097/pts.0000000000001078
- Ismail A, Khalid SNM. Patient safety culture and its determinants among healthcare professionals at a cluster hospital in Malaysia: a cross-sectional study. BMJ Open. 2022;12:e060546. doi:10.1136/bmjopen-2021-060546
- Ngo J, Lau D, Ploquin J, Receveur T, Stassen K, Del Castilho C. Improving incident reporting among physicians at south health campus hospital. BMJ Open Qual. 2022;11:e001945. doi:10.1136/bmjoq-2022-001945
- Oweidat I, Al-Mugheed K, Alsenany SA, et al. Awareness of reporting practices and barriers to incident reporting among nurses. BMC Nurs. 2023;22:231. doi:10.1186/s12912-023-01376-9
- Essen K, Villalobos C, Sculli GL, Steinbach L. Establishing a just culture: implications for the Veterans Health Administration journey to high reliability. Fed Pract. 2024;41:290-297. doi:10.12788/fp.0512
- Louis MY, Hussain LR, Dhanraj DN, et al. Improving patient safety event reporting among residents and teaching faculty. Ochsner J. 2016;16:73-80.
- Pimental CB, Snow AL, Carnes SL, et al. Huddles and their effectiveness at the frontlines of clinical care: a scoping review. J Gen Intern Med. 2021;36:2772-2783. doi:10.1007/s11606-021-06632-9
- National Academies of Sciences, Engineering, and Medicine. Appendix C: Nature of Veterans Health Administration Facilities Management (Engineering) Tasks and Staffing. Facilities Staffing Requirements for the Veterans Health Administration-Resource Planning and Methodology for the Future. National Academies Press. 2020:105-116. Accessed August 11, 2025. https://nap.nationalacademies.org/read/25454/chapter/11
- Woodier N, Burnett C, Moppett I. The value of learning from near misses to improve patient safety: a scoping review. J Patient Saf. 2023;19:42-47. doi:10.1097/pts.0000000000001078
- Ismail A, Khalid SNM. Patient safety culture and its determinants among healthcare professionals at a cluster hospital in Malaysia: a cross-sectional study. BMJ Open. 2022;12:e060546. doi:10.1136/bmjopen-2021-060546
- Ngo J, Lau D, Ploquin J, Receveur T, Stassen K, Del Castilho C. Improving incident reporting among physicians at south health campus hospital. BMJ Open Qual. 2022;11:e001945. doi:10.1136/bmjoq-2022-001945
- Oweidat I, Al-Mugheed K, Alsenany SA, et al. Awareness of reporting practices and barriers to incident reporting among nurses. BMC Nurs. 2023;22:231. doi:10.1186/s12912-023-01376-9
Empowering Culture Change and Safety on the Journey to Zero Harm With Huddle Cards
Empowering Culture Change and Safety on the Journey to Zero Harm With Huddle Cards
Improved Pharmacogenomic Testing Process for Veterans in Outpatient Settings by Clinical Pharmacist Practitioners
Peer-review, evidence-based, detailed gene/drug clinical practice guidelines suggest that genetic variations can impact how individuals metabolize medications, which is sometimes included in medication prescribing information.1-3 Pharmacogenomic testing identifies genetic markers so medication selection and dosing can be tailored to each individual by identifying whether a specific medication is likely to be safe and effective prior to prescribing.4
Pharmacogenomics can be a valuable tool for personalizing medicine but has had suboptimal implementation since its discovery. The US Department of Veterans Affairs (VA) health care system reviewed the implementation of the Pharmacogenomic Testing for Veterans (PHASER) program. This review identified clinician barriers pre- and post-PHASER program implementation; staffing issues, competing clinical priorities, and inadequate PHASER program resources were the most frequently reported barriers to implementation of pharmacogenomic testing.5
Another evaluation of the implementation of the PHASER program that surveyed VA patients found that patients could be separated into 3 groups. Acceptors of pharmacogenomic testing emphasized potential health benefits of testing. Patients that declined testing often cited concerns for genetic information affecting insurance coverage, being misused, or being susceptible to data breach. The third group—identified as contemplators—reported the need for clinician outreach to impact their decision on whether or not to receive pharmacogenomic testing.6 These studies suggest that removing barriers by providing ample pharmacogenomics resources to clinicians, in addition to detailed training on how to offer and follow up with patients regarding pharmacogenomic testing, is crucial to successful implementation of the PHASER program.
PHASER
In 2019, the VA began working with Sanford Health to establish the PHASER program and offer pharmacogenomic testing. PHASER has since expanded to 25 VA medical centers, including the VA Central Ohio Healthcare System (VACOHCS).7,8 Pharmacogenomic testing through PHASER is conducted using a standardized laboratory panel that includes 12 different medication classes.9 The drug classes include certain anti-infective, anticoagulant, antiplatelet, cardiovascular, cholesterol, gastrointestinal, mental health, neurological, oncology, pain, transplant, and other miscellaneous medications. Medications are correlated to each class and assessed for therapeutic impacts based on gene panel results.
Clinical recommendations for medication-gene interactions can range from monitoring for increased risk of adverse effects or therapeutic failure to recommending avoiding a medication. For example, patients who test positive for the HLA-B gene have significantly increased risk of hypersensitivity to abacavir, an HIV treatment.10
Similarly, patients who cannot adequately metabolize cytochrome P450 2C19 should consider avoiding clopidogrel as they are unlikely to convert clopidogrel to its active prodrug, which reduces its effectiveness.11 Pharmacists can play a critical role educating patients about pharmacogenomic testing, especially within hematology and oncology.12 Patients can benefit from this testing even if they are not currently taking medications with known concerns as they could be prescribed in the future. The SLCO1B1 gene-drug test, for example, can identify risk for statin-associated muscle symptoms.13
Clinical pharmacist practitioners (CPPs) can increase access to genetic testing because they interact with patients in a variety of settings and can order this laboratory test.12,14 Recent research has demonstrated that most VA patients carry ≥ 1 genetic variant that may influence medication decisions and that half of veterans are prescribed a medication with known gene-drug interactions.15 CPP ordering of pharmacogenomic tests at the VACOHCS outpatient clinic was evaluated through collection of baseline data from March 8, 2023, to September 8, 2023. A goal was identified to increase orders by 50% for a patient care quality improvement initiative and use CPPs to increase access to pharmacogenomic testing. The purpose of this quality improvement initiative was to expand access to pharmacogenomic testing through process implementation and improvement within CPP-led clinic settings.
Gap Analysis
Lean Six Sigma A3 methodology was used to identify ways to increase the use of pharmacogenomic testing for veterans at VACOHCS and develop an improved process for increased ordering of pharmacogenomic testing. Lean Six Sigma A3 methodology is a stepwise approach to process improvement that helps identify gaps in efficiency, sustainable changes, and eliminate waste.16 Baseline data were collected from March 8, 2023, to September 8, 2023, to determine the frequency of CPPs ordering pharmacogenomic laboratory panels during clinic appointments. The ordering of pharmacogenomic panels was monitored by the VACOHCS PHASER coordinator.
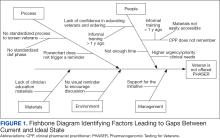
CPPs were surveyed to identify perceived barriers to PHASER implementation. A gap analysis was conducted using Lean Six Sigma A3 methodology. Gap analyses use lean tools such as a Fishbone Diagram to illustrate and identify the gap between current state and ideal state. (Figure 1).The following barriers were identified: lack of clinician education materials, lack of a standardized patient screening process, time constraints on patient education and ordering, higher priority clinical needs, forgetting to order, lack of comfort with pharmacogenomics ordering and education, lack of support for the initiative, and increased workload and burnout. Among these perceived barriers, higher priority clinical needs, forgetting to order, and time constraints ranked highest in importance among CPPs.
In line with Lean Six Sigma A3 methodology, several tests of change were used to improve pharmacogenomic testing ordering. These changes focused on increasing patient and clinician awareness, facilitating discussion, educating clinicians, and simplifying documentation to ease time constraints. Several strategies were employed postimplementation (Figure 2). Prefilled templates simplified documentation. These templates helped identify patients without pharmacogenomic testing, provided reminders, and saved documentation time during visits. CPPs also received training and materials on PHASER ordering and documentation within encounter notes. Additionally, patient-directed advertisements were displayed in CPP examination rooms to help inspire and facilitate discussion between veterans and CPPs.
Process Improvement Data
The quality improvement project goal was to increase PHASER orders by 50% after 3 months. PHASER orders increased from 87 at baseline (March 8, 2023, to September 8, 2023) to 196 during the intervention (November 16, 2023, to February 16, 2024), a 125% increase. Changes were consistent and sustained with 65 orders the first month, 67 orders the second month, and 64 orders the third month.
Discussion
Using Lean Six Sigma A3 methodology for a quality improvement process to increase PHASER orders by CPPs revealed barriers and guided potential solutions to overcome these barriers. Interventions included additional CPP training and ordering, tools for easier identification of potential patients, documentation best practices, patient-directed advertisements to facilitate conversations. These interventions required about 8 hours for preparation, distribution, development, and interpretation of surveys, education, and documentation materials. The financial impact of these interventions was already included in allotted office materials budgeted and provided. Additional funding was not needed to provide patient-directed advertisements or education materials. The VACOHCS pharmacogenomics CPP discusses PHASER test results with patients at a separate appointment.
Future directions include educating other CPPs to assist in discussing results with veterans. Overall, the changes implemented to improve the PHASER ordering process were low effort and exemplify the ease of streamlining future initiatives, allowing for sustained optimal implementation of pharmacogenomic testing.
Conclusions
A quality improvement initiative resulted in increased PHASER orders and a clearly defined process, allowing for a continued increase and sustained support. Perceived barriers were identified, and the changes implemented were often low effort but exhibited a sustained impact. The insights gleaned from this process will shape future process development initiatives and continue to sustain pharmacogenomic testing ordering by CPPs. This process will be extended to other VACOHCS clinical departments to further support increased access to pharmacogenomic testing, reduce medication trial and error, and reduce hospitalizations from adverse effects for veterans.
Cecchin E, Stocco G. Pharmacogenomics and personalized medicine. Genes (Basel). 2020;11(6):679. doi:10.3390/genes11060679
Guidelines. CPIC. Accessed April 16, 2025. https://cpicpgx.org/guidelines/
PharmGKB. PharmGKB. 2025. Accessed April 16, 2025. https://www.pharmgkb.org
Centers for Disease Control and Prevention. Pharmacogenomics. Updated November 13, 2024. Accessed April 16, 2024. https://www.cdc.gov/genomics-and-health/pharmacogenomics/
Dong OM, Roberts MC, Wu RR, et al. Evaluation of the Veterans Affairs Pharmacogenomic Testing for Veterans (PHASER) clinical program at initial test sites. Pharmacogenomics. 2021;22(17):1121-1133. doi:10.2217/pgs-2021-0089
Melendez K, Gutierrez-Meza D, Gavin KL, et al. Patient perspectives of barriers and facilitators for the uptake of pharmacogenomic testing in Veterans Affairs’ pharmacogenomic testing for the veterans (PHASER) program. J Pers Med. 2023;13(9):1367. doi:10.3390/jpm13091367
Sanford Health Imagenetics. FREQUENTLY ASKED QUESTIONS (FAQs) about the “Pharmacogenomic Teting for Vetans” (PHASER) Program. US Department of Veterans Affairs. December 20, 2019. Accessed April 16, 2025. https://www.va.gov/opa/publications/factsheets/PHASER-FLYER-VA-Patient-FAQ.pdf
Peterson H. PHASER program testing informs how you respond to medicines. VA News. September 6, 2022. Accessed April 16, 2025. https://news.va.gov/108091/phaser-program-testing-respond-medicines/
Pharmacogenomics (PGx). Sanford Health Imagenetics. 2025. Accessed April 16, 2025. https://imagenetics.sanfordhealth.org/pharmacogenomics/
Martin MA, Hoffman JM, Freimuth RR, et al. Clinical pharmacogenetics implementation consortium guidelines for HLA-B genotype and abacavir dosing: 2014 update. Clin Pharmacol Ther. 2014;95(5):499-500. doi:10.1038/clpt.2014.38
Lee CR, Luzum JA, Sangkuhl K, et al. Clinical pharmacogenetics implementation consortium guideline for CYP2C19 genotype and clopidogrel therapy: 2022 update. Clin Pharmacol Ther. 2022;112(5):959-967. doi:10.1002/cpt.2526
Dreischmeier E, Hecht H, Crocker E, et al. Integration of a clinical pharmacist practitioner-led pharmacogenomics service in a Veterans Affairs hematology/oncology clinic. Am J Health Syst Pharm. 2024;81(19):e634-e639. doi:10.1093/ajhp/zxae122
Tomcsanyi KM, Tran KA, Bates J, et al. Veterans Health Administration: implementation of pharmacogenomic clinical decision support with statin medications and the SLCO1B1 gene as an exemplar. Am J Health Syst Pharm. 2023;80(16):1082-1089. doi:10.1093/ajhp/zxad111
Gammal RS, Lee YM, Petry NJ, et al. Pharmacists leading the way to precision medicine: updates to the core pharmacist competencies in genomics. Am J Pharm Educ. 2022;86(4):8634. doi:10.5688/ajpe8634
Chanfreau-Coffinier C, Hull LE, Lynch JA, et al. Projected prevalence of actionable pharmacogenetic variants and level A drugs prescribed among US Veterans Health Administration pharmacy users. JAMA Netw Open. 2019;2(6):e195345. doi:10.1001/jamanetworkopen.2019.5345
Shaffie S, Shahbazi S. The McGraw-Hill 36-Hour Course: Lean Six Sigma. McGraw-Hill; 2012.
Peer-review, evidence-based, detailed gene/drug clinical practice guidelines suggest that genetic variations can impact how individuals metabolize medications, which is sometimes included in medication prescribing information.1-3 Pharmacogenomic testing identifies genetic markers so medication selection and dosing can be tailored to each individual by identifying whether a specific medication is likely to be safe and effective prior to prescribing.4
Pharmacogenomics can be a valuable tool for personalizing medicine but has had suboptimal implementation since its discovery. The US Department of Veterans Affairs (VA) health care system reviewed the implementation of the Pharmacogenomic Testing for Veterans (PHASER) program. This review identified clinician barriers pre- and post-PHASER program implementation; staffing issues, competing clinical priorities, and inadequate PHASER program resources were the most frequently reported barriers to implementation of pharmacogenomic testing.5
Another evaluation of the implementation of the PHASER program that surveyed VA patients found that patients could be separated into 3 groups. Acceptors of pharmacogenomic testing emphasized potential health benefits of testing. Patients that declined testing often cited concerns for genetic information affecting insurance coverage, being misused, or being susceptible to data breach. The third group—identified as contemplators—reported the need for clinician outreach to impact their decision on whether or not to receive pharmacogenomic testing.6 These studies suggest that removing barriers by providing ample pharmacogenomics resources to clinicians, in addition to detailed training on how to offer and follow up with patients regarding pharmacogenomic testing, is crucial to successful implementation of the PHASER program.
PHASER
In 2019, the VA began working with Sanford Health to establish the PHASER program and offer pharmacogenomic testing. PHASER has since expanded to 25 VA medical centers, including the VA Central Ohio Healthcare System (VACOHCS).7,8 Pharmacogenomic testing through PHASER is conducted using a standardized laboratory panel that includes 12 different medication classes.9 The drug classes include certain anti-infective, anticoagulant, antiplatelet, cardiovascular, cholesterol, gastrointestinal, mental health, neurological, oncology, pain, transplant, and other miscellaneous medications. Medications are correlated to each class and assessed for therapeutic impacts based on gene panel results.
Clinical recommendations for medication-gene interactions can range from monitoring for increased risk of adverse effects or therapeutic failure to recommending avoiding a medication. For example, patients who test positive for the HLA-B gene have significantly increased risk of hypersensitivity to abacavir, an HIV treatment.10
Similarly, patients who cannot adequately metabolize cytochrome P450 2C19 should consider avoiding clopidogrel as they are unlikely to convert clopidogrel to its active prodrug, which reduces its effectiveness.11 Pharmacists can play a critical role educating patients about pharmacogenomic testing, especially within hematology and oncology.12 Patients can benefit from this testing even if they are not currently taking medications with known concerns as they could be prescribed in the future. The SLCO1B1 gene-drug test, for example, can identify risk for statin-associated muscle symptoms.13
Clinical pharmacist practitioners (CPPs) can increase access to genetic testing because they interact with patients in a variety of settings and can order this laboratory test.12,14 Recent research has demonstrated that most VA patients carry ≥ 1 genetic variant that may influence medication decisions and that half of veterans are prescribed a medication with known gene-drug interactions.15 CPP ordering of pharmacogenomic tests at the VACOHCS outpatient clinic was evaluated through collection of baseline data from March 8, 2023, to September 8, 2023. A goal was identified to increase orders by 50% for a patient care quality improvement initiative and use CPPs to increase access to pharmacogenomic testing. The purpose of this quality improvement initiative was to expand access to pharmacogenomic testing through process implementation and improvement within CPP-led clinic settings.
Gap Analysis
Lean Six Sigma A3 methodology was used to identify ways to increase the use of pharmacogenomic testing for veterans at VACOHCS and develop an improved process for increased ordering of pharmacogenomic testing. Lean Six Sigma A3 methodology is a stepwise approach to process improvement that helps identify gaps in efficiency, sustainable changes, and eliminate waste.16 Baseline data were collected from March 8, 2023, to September 8, 2023, to determine the frequency of CPPs ordering pharmacogenomic laboratory panels during clinic appointments. The ordering of pharmacogenomic panels was monitored by the VACOHCS PHASER coordinator.
CPPs were surveyed to identify perceived barriers to PHASER implementation. A gap analysis was conducted using Lean Six Sigma A3 methodology. Gap analyses use lean tools such as a Fishbone Diagram to illustrate and identify the gap between current state and ideal state. (Figure 1).The following barriers were identified: lack of clinician education materials, lack of a standardized patient screening process, time constraints on patient education and ordering, higher priority clinical needs, forgetting to order, lack of comfort with pharmacogenomics ordering and education, lack of support for the initiative, and increased workload and burnout. Among these perceived barriers, higher priority clinical needs, forgetting to order, and time constraints ranked highest in importance among CPPs.
In line with Lean Six Sigma A3 methodology, several tests of change were used to improve pharmacogenomic testing ordering. These changes focused on increasing patient and clinician awareness, facilitating discussion, educating clinicians, and simplifying documentation to ease time constraints. Several strategies were employed postimplementation (Figure 2). Prefilled templates simplified documentation. These templates helped identify patients without pharmacogenomic testing, provided reminders, and saved documentation time during visits. CPPs also received training and materials on PHASER ordering and documentation within encounter notes. Additionally, patient-directed advertisements were displayed in CPP examination rooms to help inspire and facilitate discussion between veterans and CPPs.
Process Improvement Data
The quality improvement project goal was to increase PHASER orders by 50% after 3 months. PHASER orders increased from 87 at baseline (March 8, 2023, to September 8, 2023) to 196 during the intervention (November 16, 2023, to February 16, 2024), a 125% increase. Changes were consistent and sustained with 65 orders the first month, 67 orders the second month, and 64 orders the third month.
Discussion
Using Lean Six Sigma A3 methodology for a quality improvement process to increase PHASER orders by CPPs revealed barriers and guided potential solutions to overcome these barriers. Interventions included additional CPP training and ordering, tools for easier identification of potential patients, documentation best practices, patient-directed advertisements to facilitate conversations. These interventions required about 8 hours for preparation, distribution, development, and interpretation of surveys, education, and documentation materials. The financial impact of these interventions was already included in allotted office materials budgeted and provided. Additional funding was not needed to provide patient-directed advertisements or education materials. The VACOHCS pharmacogenomics CPP discusses PHASER test results with patients at a separate appointment.
Future directions include educating other CPPs to assist in discussing results with veterans. Overall, the changes implemented to improve the PHASER ordering process were low effort and exemplify the ease of streamlining future initiatives, allowing for sustained optimal implementation of pharmacogenomic testing.
Conclusions
A quality improvement initiative resulted in increased PHASER orders and a clearly defined process, allowing for a continued increase and sustained support. Perceived barriers were identified, and the changes implemented were often low effort but exhibited a sustained impact. The insights gleaned from this process will shape future process development initiatives and continue to sustain pharmacogenomic testing ordering by CPPs. This process will be extended to other VACOHCS clinical departments to further support increased access to pharmacogenomic testing, reduce medication trial and error, and reduce hospitalizations from adverse effects for veterans.
Peer-review, evidence-based, detailed gene/drug clinical practice guidelines suggest that genetic variations can impact how individuals metabolize medications, which is sometimes included in medication prescribing information.1-3 Pharmacogenomic testing identifies genetic markers so medication selection and dosing can be tailored to each individual by identifying whether a specific medication is likely to be safe and effective prior to prescribing.4
Pharmacogenomics can be a valuable tool for personalizing medicine but has had suboptimal implementation since its discovery. The US Department of Veterans Affairs (VA) health care system reviewed the implementation of the Pharmacogenomic Testing for Veterans (PHASER) program. This review identified clinician barriers pre- and post-PHASER program implementation; staffing issues, competing clinical priorities, and inadequate PHASER program resources were the most frequently reported barriers to implementation of pharmacogenomic testing.5
Another evaluation of the implementation of the PHASER program that surveyed VA patients found that patients could be separated into 3 groups. Acceptors of pharmacogenomic testing emphasized potential health benefits of testing. Patients that declined testing often cited concerns for genetic information affecting insurance coverage, being misused, or being susceptible to data breach. The third group—identified as contemplators—reported the need for clinician outreach to impact their decision on whether or not to receive pharmacogenomic testing.6 These studies suggest that removing barriers by providing ample pharmacogenomics resources to clinicians, in addition to detailed training on how to offer and follow up with patients regarding pharmacogenomic testing, is crucial to successful implementation of the PHASER program.
PHASER
In 2019, the VA began working with Sanford Health to establish the PHASER program and offer pharmacogenomic testing. PHASER has since expanded to 25 VA medical centers, including the VA Central Ohio Healthcare System (VACOHCS).7,8 Pharmacogenomic testing through PHASER is conducted using a standardized laboratory panel that includes 12 different medication classes.9 The drug classes include certain anti-infective, anticoagulant, antiplatelet, cardiovascular, cholesterol, gastrointestinal, mental health, neurological, oncology, pain, transplant, and other miscellaneous medications. Medications are correlated to each class and assessed for therapeutic impacts based on gene panel results.
Clinical recommendations for medication-gene interactions can range from monitoring for increased risk of adverse effects or therapeutic failure to recommending avoiding a medication. For example, patients who test positive for the HLA-B gene have significantly increased risk of hypersensitivity to abacavir, an HIV treatment.10
Similarly, patients who cannot adequately metabolize cytochrome P450 2C19 should consider avoiding clopidogrel as they are unlikely to convert clopidogrel to its active prodrug, which reduces its effectiveness.11 Pharmacists can play a critical role educating patients about pharmacogenomic testing, especially within hematology and oncology.12 Patients can benefit from this testing even if they are not currently taking medications with known concerns as they could be prescribed in the future. The SLCO1B1 gene-drug test, for example, can identify risk for statin-associated muscle symptoms.13
Clinical pharmacist practitioners (CPPs) can increase access to genetic testing because they interact with patients in a variety of settings and can order this laboratory test.12,14 Recent research has demonstrated that most VA patients carry ≥ 1 genetic variant that may influence medication decisions and that half of veterans are prescribed a medication with known gene-drug interactions.15 CPP ordering of pharmacogenomic tests at the VACOHCS outpatient clinic was evaluated through collection of baseline data from March 8, 2023, to September 8, 2023. A goal was identified to increase orders by 50% for a patient care quality improvement initiative and use CPPs to increase access to pharmacogenomic testing. The purpose of this quality improvement initiative was to expand access to pharmacogenomic testing through process implementation and improvement within CPP-led clinic settings.
Gap Analysis
Lean Six Sigma A3 methodology was used to identify ways to increase the use of pharmacogenomic testing for veterans at VACOHCS and develop an improved process for increased ordering of pharmacogenomic testing. Lean Six Sigma A3 methodology is a stepwise approach to process improvement that helps identify gaps in efficiency, sustainable changes, and eliminate waste.16 Baseline data were collected from March 8, 2023, to September 8, 2023, to determine the frequency of CPPs ordering pharmacogenomic laboratory panels during clinic appointments. The ordering of pharmacogenomic panels was monitored by the VACOHCS PHASER coordinator.
CPPs were surveyed to identify perceived barriers to PHASER implementation. A gap analysis was conducted using Lean Six Sigma A3 methodology. Gap analyses use lean tools such as a Fishbone Diagram to illustrate and identify the gap between current state and ideal state. (Figure 1).The following barriers were identified: lack of clinician education materials, lack of a standardized patient screening process, time constraints on patient education and ordering, higher priority clinical needs, forgetting to order, lack of comfort with pharmacogenomics ordering and education, lack of support for the initiative, and increased workload and burnout. Among these perceived barriers, higher priority clinical needs, forgetting to order, and time constraints ranked highest in importance among CPPs.
In line with Lean Six Sigma A3 methodology, several tests of change were used to improve pharmacogenomic testing ordering. These changes focused on increasing patient and clinician awareness, facilitating discussion, educating clinicians, and simplifying documentation to ease time constraints. Several strategies were employed postimplementation (Figure 2). Prefilled templates simplified documentation. These templates helped identify patients without pharmacogenomic testing, provided reminders, and saved documentation time during visits. CPPs also received training and materials on PHASER ordering and documentation within encounter notes. Additionally, patient-directed advertisements were displayed in CPP examination rooms to help inspire and facilitate discussion between veterans and CPPs.
Process Improvement Data
The quality improvement project goal was to increase PHASER orders by 50% after 3 months. PHASER orders increased from 87 at baseline (March 8, 2023, to September 8, 2023) to 196 during the intervention (November 16, 2023, to February 16, 2024), a 125% increase. Changes were consistent and sustained with 65 orders the first month, 67 orders the second month, and 64 orders the third month.
Discussion
Using Lean Six Sigma A3 methodology for a quality improvement process to increase PHASER orders by CPPs revealed barriers and guided potential solutions to overcome these barriers. Interventions included additional CPP training and ordering, tools for easier identification of potential patients, documentation best practices, patient-directed advertisements to facilitate conversations. These interventions required about 8 hours for preparation, distribution, development, and interpretation of surveys, education, and documentation materials. The financial impact of these interventions was already included in allotted office materials budgeted and provided. Additional funding was not needed to provide patient-directed advertisements or education materials. The VACOHCS pharmacogenomics CPP discusses PHASER test results with patients at a separate appointment.
Future directions include educating other CPPs to assist in discussing results with veterans. Overall, the changes implemented to improve the PHASER ordering process were low effort and exemplify the ease of streamlining future initiatives, allowing for sustained optimal implementation of pharmacogenomic testing.
Conclusions
A quality improvement initiative resulted in increased PHASER orders and a clearly defined process, allowing for a continued increase and sustained support. Perceived barriers were identified, and the changes implemented were often low effort but exhibited a sustained impact. The insights gleaned from this process will shape future process development initiatives and continue to sustain pharmacogenomic testing ordering by CPPs. This process will be extended to other VACOHCS clinical departments to further support increased access to pharmacogenomic testing, reduce medication trial and error, and reduce hospitalizations from adverse effects for veterans.
Cecchin E, Stocco G. Pharmacogenomics and personalized medicine. Genes (Basel). 2020;11(6):679. doi:10.3390/genes11060679
Guidelines. CPIC. Accessed April 16, 2025. https://cpicpgx.org/guidelines/
PharmGKB. PharmGKB. 2025. Accessed April 16, 2025. https://www.pharmgkb.org
Centers for Disease Control and Prevention. Pharmacogenomics. Updated November 13, 2024. Accessed April 16, 2024. https://www.cdc.gov/genomics-and-health/pharmacogenomics/
Dong OM, Roberts MC, Wu RR, et al. Evaluation of the Veterans Affairs Pharmacogenomic Testing for Veterans (PHASER) clinical program at initial test sites. Pharmacogenomics. 2021;22(17):1121-1133. doi:10.2217/pgs-2021-0089
Melendez K, Gutierrez-Meza D, Gavin KL, et al. Patient perspectives of barriers and facilitators for the uptake of pharmacogenomic testing in Veterans Affairs’ pharmacogenomic testing for the veterans (PHASER) program. J Pers Med. 2023;13(9):1367. doi:10.3390/jpm13091367
Sanford Health Imagenetics. FREQUENTLY ASKED QUESTIONS (FAQs) about the “Pharmacogenomic Teting for Vetans” (PHASER) Program. US Department of Veterans Affairs. December 20, 2019. Accessed April 16, 2025. https://www.va.gov/opa/publications/factsheets/PHASER-FLYER-VA-Patient-FAQ.pdf
Peterson H. PHASER program testing informs how you respond to medicines. VA News. September 6, 2022. Accessed April 16, 2025. https://news.va.gov/108091/phaser-program-testing-respond-medicines/
Pharmacogenomics (PGx). Sanford Health Imagenetics. 2025. Accessed April 16, 2025. https://imagenetics.sanfordhealth.org/pharmacogenomics/
Martin MA, Hoffman JM, Freimuth RR, et al. Clinical pharmacogenetics implementation consortium guidelines for HLA-B genotype and abacavir dosing: 2014 update. Clin Pharmacol Ther. 2014;95(5):499-500. doi:10.1038/clpt.2014.38
Lee CR, Luzum JA, Sangkuhl K, et al. Clinical pharmacogenetics implementation consortium guideline for CYP2C19 genotype and clopidogrel therapy: 2022 update. Clin Pharmacol Ther. 2022;112(5):959-967. doi:10.1002/cpt.2526
Dreischmeier E, Hecht H, Crocker E, et al. Integration of a clinical pharmacist practitioner-led pharmacogenomics service in a Veterans Affairs hematology/oncology clinic. Am J Health Syst Pharm. 2024;81(19):e634-e639. doi:10.1093/ajhp/zxae122
Tomcsanyi KM, Tran KA, Bates J, et al. Veterans Health Administration: implementation of pharmacogenomic clinical decision support with statin medications and the SLCO1B1 gene as an exemplar. Am J Health Syst Pharm. 2023;80(16):1082-1089. doi:10.1093/ajhp/zxad111
Gammal RS, Lee YM, Petry NJ, et al. Pharmacists leading the way to precision medicine: updates to the core pharmacist competencies in genomics. Am J Pharm Educ. 2022;86(4):8634. doi:10.5688/ajpe8634
Chanfreau-Coffinier C, Hull LE, Lynch JA, et al. Projected prevalence of actionable pharmacogenetic variants and level A drugs prescribed among US Veterans Health Administration pharmacy users. JAMA Netw Open. 2019;2(6):e195345. doi:10.1001/jamanetworkopen.2019.5345
Shaffie S, Shahbazi S. The McGraw-Hill 36-Hour Course: Lean Six Sigma. McGraw-Hill; 2012.
Cecchin E, Stocco G. Pharmacogenomics and personalized medicine. Genes (Basel). 2020;11(6):679. doi:10.3390/genes11060679
Guidelines. CPIC. Accessed April 16, 2025. https://cpicpgx.org/guidelines/
PharmGKB. PharmGKB. 2025. Accessed April 16, 2025. https://www.pharmgkb.org
Centers for Disease Control and Prevention. Pharmacogenomics. Updated November 13, 2024. Accessed April 16, 2024. https://www.cdc.gov/genomics-and-health/pharmacogenomics/
Dong OM, Roberts MC, Wu RR, et al. Evaluation of the Veterans Affairs Pharmacogenomic Testing for Veterans (PHASER) clinical program at initial test sites. Pharmacogenomics. 2021;22(17):1121-1133. doi:10.2217/pgs-2021-0089
Melendez K, Gutierrez-Meza D, Gavin KL, et al. Patient perspectives of barriers and facilitators for the uptake of pharmacogenomic testing in Veterans Affairs’ pharmacogenomic testing for the veterans (PHASER) program. J Pers Med. 2023;13(9):1367. doi:10.3390/jpm13091367
Sanford Health Imagenetics. FREQUENTLY ASKED QUESTIONS (FAQs) about the “Pharmacogenomic Teting for Vetans” (PHASER) Program. US Department of Veterans Affairs. December 20, 2019. Accessed April 16, 2025. https://www.va.gov/opa/publications/factsheets/PHASER-FLYER-VA-Patient-FAQ.pdf
Peterson H. PHASER program testing informs how you respond to medicines. VA News. September 6, 2022. Accessed April 16, 2025. https://news.va.gov/108091/phaser-program-testing-respond-medicines/
Pharmacogenomics (PGx). Sanford Health Imagenetics. 2025. Accessed April 16, 2025. https://imagenetics.sanfordhealth.org/pharmacogenomics/
Martin MA, Hoffman JM, Freimuth RR, et al. Clinical pharmacogenetics implementation consortium guidelines for HLA-B genotype and abacavir dosing: 2014 update. Clin Pharmacol Ther. 2014;95(5):499-500. doi:10.1038/clpt.2014.38
Lee CR, Luzum JA, Sangkuhl K, et al. Clinical pharmacogenetics implementation consortium guideline for CYP2C19 genotype and clopidogrel therapy: 2022 update. Clin Pharmacol Ther. 2022;112(5):959-967. doi:10.1002/cpt.2526
Dreischmeier E, Hecht H, Crocker E, et al. Integration of a clinical pharmacist practitioner-led pharmacogenomics service in a Veterans Affairs hematology/oncology clinic. Am J Health Syst Pharm. 2024;81(19):e634-e639. doi:10.1093/ajhp/zxae122
Tomcsanyi KM, Tran KA, Bates J, et al. Veterans Health Administration: implementation of pharmacogenomic clinical decision support with statin medications and the SLCO1B1 gene as an exemplar. Am J Health Syst Pharm. 2023;80(16):1082-1089. doi:10.1093/ajhp/zxad111
Gammal RS, Lee YM, Petry NJ, et al. Pharmacists leading the way to precision medicine: updates to the core pharmacist competencies in genomics. Am J Pharm Educ. 2022;86(4):8634. doi:10.5688/ajpe8634
Chanfreau-Coffinier C, Hull LE, Lynch JA, et al. Projected prevalence of actionable pharmacogenetic variants and level A drugs prescribed among US Veterans Health Administration pharmacy users. JAMA Netw Open. 2019;2(6):e195345. doi:10.1001/jamanetworkopen.2019.5345
Shaffie S, Shahbazi S. The McGraw-Hill 36-Hour Course: Lean Six Sigma. McGraw-Hill; 2012.
The Physician Associate Advantage: A Vital Solution for Better Patient Care
Late last year, the Health Resources and Services Administration projected a shortage of nearly 190,000 physicians across specialties by 2037. They noted, however, that we could mitigate the lack of doctors in some specialties by increasing the use of physician associates (PAs), especially with new and pending legislation expanding PAs’ scope of practice. A new survey conducted by Morning Consult, a business intelligence company, and the American Academy of Physician Associates (AAPA) found that doctors mostly agree with this assessment.
Lisa Gables, CPA, chief executive officer of the AAPA, said, “anecdotally,” physicians have long heralded the value of PAs. But, with organizations like the American Medical Association (AMA) campaigning to end PA “scope creep,” the AAPA thought it was important to do a direct study. Most (90%) of physicians see PAs as important to enhancing care delivery.
“For change to happen — and to make sure we can continue to provide the best possible care for patients — all healthcare providers must work together to find solutions,” Gables told this news organization. “The doctors who work with PAs appreciate the work they do and recognize the barriers they face. But anecdotes aren’t data. We thought it was important to do a formal survey so physicians across the nation could share how they work with PAs and where we can find common ground to address the challenges healthcare is facing.”
The survey included a national sample of 999 physicians. It found that 86% of respondents, even those who do not work directly with PAs, believe that PAs can help expand access to care. Moreover, 68% of respondents said that they support modernizing PA laws and regulations to ease provider shortages and reduce wait times for patients.
Physicians Trust PAs
Currently, most laws dictate that physicians must supervise PAs as they work — yet, what constitutes supervision varies. The physicians surveyed said their PAs often see patients on their own in primary and specialty care settings. And 63% of the respondents reported never or rarely being physically present in the room while a PA delivers care. Gables said that while she is well aware of PAs’ strong skills and capabilities, she was surprised to see that this percentage was so high.
“The supervising agreement and supervision language that you see in so many state laws suggests that constant physician oversight is necessary. But in day-to-day practice, that’s not what is happening,” she said. “Physicians report they are rarely in the room with PAs during patient interactions and spend little time monitoring the care they provide. Physicians really trust their PAs — and it would be good to see laws that reflect that.”
PAs Improve Care Delivery
One of the AMA’s arguments about the dangers of scope creep is that patients may come to harm if a physician is not directly involved with patient care. They say PAs may not have the training or experience to identify some issues or to understand when a referral is required. Yet, a significant number of physicians surveyed in the AAPA study stated that they believed PAs are trained to perform comprehensive history and physical exams (61%), make referrals (59%), diagnose conditions and other disease states (50%), and develop and implement treatment plans (48%).
This is important, said Gables, because those same physicians reported there aren’t enough healthcare providers available, and they are struggling with current patient loads. The survey highlights the need to find ways to improve not just access to care but care delivery itself — and, given their skill sets, PAs are in a prime position to help.
“Most healthcare providers today will tell you that they are overworked. There are shortages everywhere,” said Gables. “Physicians see that patients are having a hard time accessing healthcare. There are long waits for appointments. And they also see that PAs have the skills necessary to help alleviate those shortages. More than three quarters of the doctors who work with PAs say they provide safe, effective care to patients — and they know when they need to consult with a physician or make a referral,” she said.
Autonomy Leads to Access
The AAPA has long called for policy changes to lessen the barriers that make it harder for PAs to serve the needs of patients. Gables said that what they are advocating for is not what the AMA calls scope creep but rather to lessen different barriers that interfere with PAs helping to deliver care. And it appears that physicians also see the value in loosening PA-related practice policies. About 68% of respondents said they support removing mandatory physician agreements to help ease provider shortages and improve care delivery for patients. Gables hopes that the AMA will see these results and think about ways providers can come together to make healthcare more accessible and equitable across the country.
“Looking at these results, I see that there’s the AMA, and then there’s the physicians who work with PAs. Those physicians know what PAs can do. And they know that we should all work together to solve the problems we share,” she said. “A previous survey shows that patients understand who PAs are and the value they bring to healthcare teams. Now we see that physicians understand that, too…So when we are thinking about how to make healthcare better, we all have a role to play in helping patients get the care they need and deserve.” Gables thinks we will be closer to achieving that when PAs practice at the highest levels of their training.
A version of this article first appeared on Medscape.com.
Late last year, the Health Resources and Services Administration projected a shortage of nearly 190,000 physicians across specialties by 2037. They noted, however, that we could mitigate the lack of doctors in some specialties by increasing the use of physician associates (PAs), especially with new and pending legislation expanding PAs’ scope of practice. A new survey conducted by Morning Consult, a business intelligence company, and the American Academy of Physician Associates (AAPA) found that doctors mostly agree with this assessment.
Lisa Gables, CPA, chief executive officer of the AAPA, said, “anecdotally,” physicians have long heralded the value of PAs. But, with organizations like the American Medical Association (AMA) campaigning to end PA “scope creep,” the AAPA thought it was important to do a direct study. Most (90%) of physicians see PAs as important to enhancing care delivery.
“For change to happen — and to make sure we can continue to provide the best possible care for patients — all healthcare providers must work together to find solutions,” Gables told this news organization. “The doctors who work with PAs appreciate the work they do and recognize the barriers they face. But anecdotes aren’t data. We thought it was important to do a formal survey so physicians across the nation could share how they work with PAs and where we can find common ground to address the challenges healthcare is facing.”
The survey included a national sample of 999 physicians. It found that 86% of respondents, even those who do not work directly with PAs, believe that PAs can help expand access to care. Moreover, 68% of respondents said that they support modernizing PA laws and regulations to ease provider shortages and reduce wait times for patients.
Physicians Trust PAs
Currently, most laws dictate that physicians must supervise PAs as they work — yet, what constitutes supervision varies. The physicians surveyed said their PAs often see patients on their own in primary and specialty care settings. And 63% of the respondents reported never or rarely being physically present in the room while a PA delivers care. Gables said that while she is well aware of PAs’ strong skills and capabilities, she was surprised to see that this percentage was so high.
“The supervising agreement and supervision language that you see in so many state laws suggests that constant physician oversight is necessary. But in day-to-day practice, that’s not what is happening,” she said. “Physicians report they are rarely in the room with PAs during patient interactions and spend little time monitoring the care they provide. Physicians really trust their PAs — and it would be good to see laws that reflect that.”
PAs Improve Care Delivery
One of the AMA’s arguments about the dangers of scope creep is that patients may come to harm if a physician is not directly involved with patient care. They say PAs may not have the training or experience to identify some issues or to understand when a referral is required. Yet, a significant number of physicians surveyed in the AAPA study stated that they believed PAs are trained to perform comprehensive history and physical exams (61%), make referrals (59%), diagnose conditions and other disease states (50%), and develop and implement treatment plans (48%).
This is important, said Gables, because those same physicians reported there aren’t enough healthcare providers available, and they are struggling with current patient loads. The survey highlights the need to find ways to improve not just access to care but care delivery itself — and, given their skill sets, PAs are in a prime position to help.
“Most healthcare providers today will tell you that they are overworked. There are shortages everywhere,” said Gables. “Physicians see that patients are having a hard time accessing healthcare. There are long waits for appointments. And they also see that PAs have the skills necessary to help alleviate those shortages. More than three quarters of the doctors who work with PAs say they provide safe, effective care to patients — and they know when they need to consult with a physician or make a referral,” she said.
Autonomy Leads to Access
The AAPA has long called for policy changes to lessen the barriers that make it harder for PAs to serve the needs of patients. Gables said that what they are advocating for is not what the AMA calls scope creep but rather to lessen different barriers that interfere with PAs helping to deliver care. And it appears that physicians also see the value in loosening PA-related practice policies. About 68% of respondents said they support removing mandatory physician agreements to help ease provider shortages and improve care delivery for patients. Gables hopes that the AMA will see these results and think about ways providers can come together to make healthcare more accessible and equitable across the country.
“Looking at these results, I see that there’s the AMA, and then there’s the physicians who work with PAs. Those physicians know what PAs can do. And they know that we should all work together to solve the problems we share,” she said. “A previous survey shows that patients understand who PAs are and the value they bring to healthcare teams. Now we see that physicians understand that, too…So when we are thinking about how to make healthcare better, we all have a role to play in helping patients get the care they need and deserve.” Gables thinks we will be closer to achieving that when PAs practice at the highest levels of their training.
A version of this article first appeared on Medscape.com.
Late last year, the Health Resources and Services Administration projected a shortage of nearly 190,000 physicians across specialties by 2037. They noted, however, that we could mitigate the lack of doctors in some specialties by increasing the use of physician associates (PAs), especially with new and pending legislation expanding PAs’ scope of practice. A new survey conducted by Morning Consult, a business intelligence company, and the American Academy of Physician Associates (AAPA) found that doctors mostly agree with this assessment.
Lisa Gables, CPA, chief executive officer of the AAPA, said, “anecdotally,” physicians have long heralded the value of PAs. But, with organizations like the American Medical Association (AMA) campaigning to end PA “scope creep,” the AAPA thought it was important to do a direct study. Most (90%) of physicians see PAs as important to enhancing care delivery.
“For change to happen — and to make sure we can continue to provide the best possible care for patients — all healthcare providers must work together to find solutions,” Gables told this news organization. “The doctors who work with PAs appreciate the work they do and recognize the barriers they face. But anecdotes aren’t data. We thought it was important to do a formal survey so physicians across the nation could share how they work with PAs and where we can find common ground to address the challenges healthcare is facing.”
The survey included a national sample of 999 physicians. It found that 86% of respondents, even those who do not work directly with PAs, believe that PAs can help expand access to care. Moreover, 68% of respondents said that they support modernizing PA laws and regulations to ease provider shortages and reduce wait times for patients.
Physicians Trust PAs
Currently, most laws dictate that physicians must supervise PAs as they work — yet, what constitutes supervision varies. The physicians surveyed said their PAs often see patients on their own in primary and specialty care settings. And 63% of the respondents reported never or rarely being physically present in the room while a PA delivers care. Gables said that while she is well aware of PAs’ strong skills and capabilities, she was surprised to see that this percentage was so high.
“The supervising agreement and supervision language that you see in so many state laws suggests that constant physician oversight is necessary. But in day-to-day practice, that’s not what is happening,” she said. “Physicians report they are rarely in the room with PAs during patient interactions and spend little time monitoring the care they provide. Physicians really trust their PAs — and it would be good to see laws that reflect that.”
PAs Improve Care Delivery
One of the AMA’s arguments about the dangers of scope creep is that patients may come to harm if a physician is not directly involved with patient care. They say PAs may not have the training or experience to identify some issues or to understand when a referral is required. Yet, a significant number of physicians surveyed in the AAPA study stated that they believed PAs are trained to perform comprehensive history and physical exams (61%), make referrals (59%), diagnose conditions and other disease states (50%), and develop and implement treatment plans (48%).
This is important, said Gables, because those same physicians reported there aren’t enough healthcare providers available, and they are struggling with current patient loads. The survey highlights the need to find ways to improve not just access to care but care delivery itself — and, given their skill sets, PAs are in a prime position to help.
“Most healthcare providers today will tell you that they are overworked. There are shortages everywhere,” said Gables. “Physicians see that patients are having a hard time accessing healthcare. There are long waits for appointments. And they also see that PAs have the skills necessary to help alleviate those shortages. More than three quarters of the doctors who work with PAs say they provide safe, effective care to patients — and they know when they need to consult with a physician or make a referral,” she said.
Autonomy Leads to Access
The AAPA has long called for policy changes to lessen the barriers that make it harder for PAs to serve the needs of patients. Gables said that what they are advocating for is not what the AMA calls scope creep but rather to lessen different barriers that interfere with PAs helping to deliver care. And it appears that physicians also see the value in loosening PA-related practice policies. About 68% of respondents said they support removing mandatory physician agreements to help ease provider shortages and improve care delivery for patients. Gables hopes that the AMA will see these results and think about ways providers can come together to make healthcare more accessible and equitable across the country.
“Looking at these results, I see that there’s the AMA, and then there’s the physicians who work with PAs. Those physicians know what PAs can do. And they know that we should all work together to solve the problems we share,” she said. “A previous survey shows that patients understand who PAs are and the value they bring to healthcare teams. Now we see that physicians understand that, too…So when we are thinking about how to make healthcare better, we all have a role to play in helping patients get the care they need and deserve.” Gables thinks we will be closer to achieving that when PAs practice at the highest levels of their training.
A version of this article first appeared on Medscape.com.
Emergency department visits from adverse drug events
Clinical question: The purpose of this study was to describe emergency department (ED) visits for adverse drug events in year 2013-2014 compared to year 2005-2006 to learn changing patterns of ADEs and to help advance medication safety initiatives in outpatient settings.
Background: Adverse drug events (ADEs) are the most common cause of iatrogenic harm to patients and there have been significant national-level initiatives to prevent them as a part of patient safety. In the outpatient setting, where 90% of prescription drug expenditures occur, preventing ADEs remains a patient safety challenge because patients can have complex medication regimens, at times prescribed by multiple clinicians, with far less monitoring compared with hospitalized patients.
Setting and study design: Active, public health surveillance in 58 EDs in the United States that participate in the National Electronic Injury Surveillance System–Cooperative Adverse Drug Event Surveillance Project (NEISS-CADES). Trained data abstractors at each hospital reviewed each ED visit to identify any clinician-diagnosed ADEs that were the reason for the ED visit. Reports were coded by CDC and analyzed.
Synopsis: Based on 42,585 cases, 4.0 (95% CI, 3.1-5) ED visits for ADEs per 1,000 individuals occurred annually in the United States in 2013-2014 and 27.3% (22.2%-32.4%) of ED visits for ADEs resulted in hospitalization.
An estimated 34.5 % (95% CI, 30.3-38.8) of ED visits for ADEs occurred among adults aged 65 or older in 2013 compared with an estimated 25.6% (95% CI, 21-30) in 2005-2006. The population rate for adults older than 65 years was 9.7 visits per 1,000 individuals, compared with 3.1 visits per 1,000 individuals for those younger than 65 years. Older adults experienced higher hospitalization rates 43.6% (95% CI, 36.6-50.5). When adjusted for the U.S. population, the hospitalization rate for ADEs among older individuals was seven times higher compared with younger patients.
A single medication was implicated in most ED visits for ADEs (83.8%; 95% CI, 81.5-86.1). Supratherapeutic effects of ingestion of excess dose was the most common type of ADE (37.2%; 95% CI, 34.7-39.6). Medication errors were documented in 1 of 10 ED visits for ADEs (10.5%; 95% CI, 8.9-12.2).
The most commonly implicated drug classes were anticoagulants (17.6%), systemic antibiotics (16.1%), diabetes agents (13.3%), opioid analgesics (6.8%), antiplatelets (6.6%), renin-angiotensin system inhibitors (3.5%), antineoplastic agents (3%) and sedative/hypnotics (3%). Since 2005-2006, the proportions of ED visits for ADEs involving anticoagulants, antiplatelets, and diabetic agents have increased, whereas proportions involving antibiotics have decreased.
In children aged 5 years or younger, antibiotics were the most common drug class (56.4; 95% CI, 51.8-61). Among children and adolescents aged 6-19 years, antibiotics also were the most common class (31.8%; 95% CI, 28.7-34.9), followed by antipsychotics (4.5%; 95% CI, 3.3-5.6).
Among older adults, three drug classes recently targeted by federal patient safety initiatives (anticoagulants, diabetes agents, and opioid analgesics) were implicated in an estimated 59.9% (95% CI, 56.8-62.9) of ED visits. Four anticoagulants (warfarin, rivaroxaban, dabigatran, and enoxaparin) and five diabetes agents (insulin and four oral agents) were among the 15 most common drugs implicated. Medications to always avoid in older adults according to Beers criteria were implicated in 1.8% (95% CI, 1.5-2.1) of ED visits for adverse drug events.
Summary: The most common drug classes implicated in ED visits for ADEs in the United States are the same ones identified a decade ago – anticoagulants, antibiotics, diabetes agents, and opioid analgesics. The proportion of ED visits for ADEs involving anticoagulants has increased during the last decade with increased anticoagulant use. The prevalence of potentially inappropriate medication use in older patients also remains high.
Citation: JAMA. 2016;316(20):2115-25. doi: 10.1001/jama.2016.16201.
Dr. Patel is a hospitalist in the division of hospital medicine and assistant professor of medicine at Cooper Medical School of Rowan University, Camden, N.J. He is CMSRU’s associate residency program director and serves as codirector of the Foundation of Medical Practice curriculum.
Clinical question: The purpose of this study was to describe emergency department (ED) visits for adverse drug events in year 2013-2014 compared to year 2005-2006 to learn changing patterns of ADEs and to help advance medication safety initiatives in outpatient settings.
Background: Adverse drug events (ADEs) are the most common cause of iatrogenic harm to patients and there have been significant national-level initiatives to prevent them as a part of patient safety. In the outpatient setting, where 90% of prescription drug expenditures occur, preventing ADEs remains a patient safety challenge because patients can have complex medication regimens, at times prescribed by multiple clinicians, with far less monitoring compared with hospitalized patients.
Setting and study design: Active, public health surveillance in 58 EDs in the United States that participate in the National Electronic Injury Surveillance System–Cooperative Adverse Drug Event Surveillance Project (NEISS-CADES). Trained data abstractors at each hospital reviewed each ED visit to identify any clinician-diagnosed ADEs that were the reason for the ED visit. Reports were coded by CDC and analyzed.
Synopsis: Based on 42,585 cases, 4.0 (95% CI, 3.1-5) ED visits for ADEs per 1,000 individuals occurred annually in the United States in 2013-2014 and 27.3% (22.2%-32.4%) of ED visits for ADEs resulted in hospitalization.
An estimated 34.5 % (95% CI, 30.3-38.8) of ED visits for ADEs occurred among adults aged 65 or older in 2013 compared with an estimated 25.6% (95% CI, 21-30) in 2005-2006. The population rate for adults older than 65 years was 9.7 visits per 1,000 individuals, compared with 3.1 visits per 1,000 individuals for those younger than 65 years. Older adults experienced higher hospitalization rates 43.6% (95% CI, 36.6-50.5). When adjusted for the U.S. population, the hospitalization rate for ADEs among older individuals was seven times higher compared with younger patients.
A single medication was implicated in most ED visits for ADEs (83.8%; 95% CI, 81.5-86.1). Supratherapeutic effects of ingestion of excess dose was the most common type of ADE (37.2%; 95% CI, 34.7-39.6). Medication errors were documented in 1 of 10 ED visits for ADEs (10.5%; 95% CI, 8.9-12.2).
The most commonly implicated drug classes were anticoagulants (17.6%), systemic antibiotics (16.1%), diabetes agents (13.3%), opioid analgesics (6.8%), antiplatelets (6.6%), renin-angiotensin system inhibitors (3.5%), antineoplastic agents (3%) and sedative/hypnotics (3%). Since 2005-2006, the proportions of ED visits for ADEs involving anticoagulants, antiplatelets, and diabetic agents have increased, whereas proportions involving antibiotics have decreased.
In children aged 5 years or younger, antibiotics were the most common drug class (56.4; 95% CI, 51.8-61). Among children and adolescents aged 6-19 years, antibiotics also were the most common class (31.8%; 95% CI, 28.7-34.9), followed by antipsychotics (4.5%; 95% CI, 3.3-5.6).
Among older adults, three drug classes recently targeted by federal patient safety initiatives (anticoagulants, diabetes agents, and opioid analgesics) were implicated in an estimated 59.9% (95% CI, 56.8-62.9) of ED visits. Four anticoagulants (warfarin, rivaroxaban, dabigatran, and enoxaparin) and five diabetes agents (insulin and four oral agents) were among the 15 most common drugs implicated. Medications to always avoid in older adults according to Beers criteria were implicated in 1.8% (95% CI, 1.5-2.1) of ED visits for adverse drug events.
Summary: The most common drug classes implicated in ED visits for ADEs in the United States are the same ones identified a decade ago – anticoagulants, antibiotics, diabetes agents, and opioid analgesics. The proportion of ED visits for ADEs involving anticoagulants has increased during the last decade with increased anticoagulant use. The prevalence of potentially inappropriate medication use in older patients also remains high.
Citation: JAMA. 2016;316(20):2115-25. doi: 10.1001/jama.2016.16201.
Dr. Patel is a hospitalist in the division of hospital medicine and assistant professor of medicine at Cooper Medical School of Rowan University, Camden, N.J. He is CMSRU’s associate residency program director and serves as codirector of the Foundation of Medical Practice curriculum.
Clinical question: The purpose of this study was to describe emergency department (ED) visits for adverse drug events in year 2013-2014 compared to year 2005-2006 to learn changing patterns of ADEs and to help advance medication safety initiatives in outpatient settings.
Background: Adverse drug events (ADEs) are the most common cause of iatrogenic harm to patients and there have been significant national-level initiatives to prevent them as a part of patient safety. In the outpatient setting, where 90% of prescription drug expenditures occur, preventing ADEs remains a patient safety challenge because patients can have complex medication regimens, at times prescribed by multiple clinicians, with far less monitoring compared with hospitalized patients.
Setting and study design: Active, public health surveillance in 58 EDs in the United States that participate in the National Electronic Injury Surveillance System–Cooperative Adverse Drug Event Surveillance Project (NEISS-CADES). Trained data abstractors at each hospital reviewed each ED visit to identify any clinician-diagnosed ADEs that were the reason for the ED visit. Reports were coded by CDC and analyzed.
Synopsis: Based on 42,585 cases, 4.0 (95% CI, 3.1-5) ED visits for ADEs per 1,000 individuals occurred annually in the United States in 2013-2014 and 27.3% (22.2%-32.4%) of ED visits for ADEs resulted in hospitalization.
An estimated 34.5 % (95% CI, 30.3-38.8) of ED visits for ADEs occurred among adults aged 65 or older in 2013 compared with an estimated 25.6% (95% CI, 21-30) in 2005-2006. The population rate for adults older than 65 years was 9.7 visits per 1,000 individuals, compared with 3.1 visits per 1,000 individuals for those younger than 65 years. Older adults experienced higher hospitalization rates 43.6% (95% CI, 36.6-50.5). When adjusted for the U.S. population, the hospitalization rate for ADEs among older individuals was seven times higher compared with younger patients.
A single medication was implicated in most ED visits for ADEs (83.8%; 95% CI, 81.5-86.1). Supratherapeutic effects of ingestion of excess dose was the most common type of ADE (37.2%; 95% CI, 34.7-39.6). Medication errors were documented in 1 of 10 ED visits for ADEs (10.5%; 95% CI, 8.9-12.2).
The most commonly implicated drug classes were anticoagulants (17.6%), systemic antibiotics (16.1%), diabetes agents (13.3%), opioid analgesics (6.8%), antiplatelets (6.6%), renin-angiotensin system inhibitors (3.5%), antineoplastic agents (3%) and sedative/hypnotics (3%). Since 2005-2006, the proportions of ED visits for ADEs involving anticoagulants, antiplatelets, and diabetic agents have increased, whereas proportions involving antibiotics have decreased.
In children aged 5 years or younger, antibiotics were the most common drug class (56.4; 95% CI, 51.8-61). Among children and adolescents aged 6-19 years, antibiotics also were the most common class (31.8%; 95% CI, 28.7-34.9), followed by antipsychotics (4.5%; 95% CI, 3.3-5.6).
Among older adults, three drug classes recently targeted by federal patient safety initiatives (anticoagulants, diabetes agents, and opioid analgesics) were implicated in an estimated 59.9% (95% CI, 56.8-62.9) of ED visits. Four anticoagulants (warfarin, rivaroxaban, dabigatran, and enoxaparin) and five diabetes agents (insulin and four oral agents) were among the 15 most common drugs implicated. Medications to always avoid in older adults according to Beers criteria were implicated in 1.8% (95% CI, 1.5-2.1) of ED visits for adverse drug events.
Summary: The most common drug classes implicated in ED visits for ADEs in the United States are the same ones identified a decade ago – anticoagulants, antibiotics, diabetes agents, and opioid analgesics. The proportion of ED visits for ADEs involving anticoagulants has increased during the last decade with increased anticoagulant use. The prevalence of potentially inappropriate medication use in older patients also remains high.
Citation: JAMA. 2016;316(20):2115-25. doi: 10.1001/jama.2016.16201.
Dr. Patel is a hospitalist in the division of hospital medicine and assistant professor of medicine at Cooper Medical School of Rowan University, Camden, N.J. He is CMSRU’s associate residency program director and serves as codirector of the Foundation of Medical Practice curriculum.
Trending at SHM
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Female physicians, lower mortality, lower readmissions: A case study
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.

My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at [email protected].
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.

My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at [email protected].
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.

My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at [email protected].
Hospital factors play key role in readmission risk after surgery
CORONADO, CALIF. – Variation in readmission risk across hospitals following certain surgical procedures is more attributable to hospital factors than to patient characteristics, results from a large analysis demonstrated.
Such is the impact of the care delivery macro environment (CDM), which Sarah A. Brownlee and coauthors defined as a series of complex interactions between patient characteristics and imposed hospital attributes than can impact patient outcomes postoperatively.
The purpose of the current study was to determine the relative contribution of various aspects of the CDM to 1-year readmission risk after surgery. Working with colleagues Anai Kothari, MD, and Paul Kuo MD, in the One:MAP Section of Clinical informatics and Analytics in the department of surgery at Loyola University Medical Center, Ms. Brownlee analyzed the Healthcare Cost and Utilization Project State Inpatient Databases from Florida, New York, and Washington between 2009 and 2013, which were linked to the American Hospital Association Annual Survey from that same time period.
The researchers used smoothed hazard estimates to determine all-cause readmission in the year after surgery, and multilevel survival models with shared frailty to determine the relative impact of hospital versus patient characteristics on the heterogeneity of readmission risk between hospitals. They limited the analysis to patients aged 18 years and older who underwent one the following procedures: abdominal aortic aneurysm repair, pancreatectomy, colectomy, coronary artery bypass graft, and total hip arthroplasty.
Ms. Brownlee reported results from 502,157 patients who underwent surgical procedures at 347 hospitals. The 1-year readmission rate was 23.5%, and ranged from 12% to 36% across procedures. After controlling for procedure, the researchers observed a 7.9% variation in readmission risk between hospitals. Staffing accounted for 9.8% of variance, followed by hospital structural characteristics such as teaching status and clinical programs (7.5%), patient ZIP code (3.8%), hospital perioperative resources such as inpatient rehab (2.9%), hospital volume (2.8%), and patient clinical characteristics (2.1%). The following hospital characteristics were significantly associated with a lower risk of 1-year readmission: high physician/bed ratio (hazard ratio 0.85; P = .00017); transplant status (HR 0.87; P = .022); high-income ZIP code (HR 0.89; P less than .001); high nurse bed/bed ratio (HR 0.90; P = .047), and cancer center designation (HR 0.93; P = .021).
“Compared to patient clinical characteristics, hospital factors such as staffing ratios, perioperative resources, and structural elements account for more variation in postoperative outcomes,” Ms. Brownlee concluded. “However, it’s important to note that in the present study, over 70% of variation in readmission rates is not explained by the covariates that we analyzed. It’s possible that there are other factors we need to consider. That’s where the direction of this research is going. Much of the variation in readmission risk across hospitals cannot be characterized with currently utilized administrative data.”
The National Institutes of Health provided funding for the study. Ms. Brownlee reported having no financial disclosures.
CORONADO, CALIF. – Variation in readmission risk across hospitals following certain surgical procedures is more attributable to hospital factors than to patient characteristics, results from a large analysis demonstrated.
Such is the impact of the care delivery macro environment (CDM), which Sarah A. Brownlee and coauthors defined as a series of complex interactions between patient characteristics and imposed hospital attributes than can impact patient outcomes postoperatively.
The purpose of the current study was to determine the relative contribution of various aspects of the CDM to 1-year readmission risk after surgery. Working with colleagues Anai Kothari, MD, and Paul Kuo MD, in the One:MAP Section of Clinical informatics and Analytics in the department of surgery at Loyola University Medical Center, Ms. Brownlee analyzed the Healthcare Cost and Utilization Project State Inpatient Databases from Florida, New York, and Washington between 2009 and 2013, which were linked to the American Hospital Association Annual Survey from that same time period.
The researchers used smoothed hazard estimates to determine all-cause readmission in the year after surgery, and multilevel survival models with shared frailty to determine the relative impact of hospital versus patient characteristics on the heterogeneity of readmission risk between hospitals. They limited the analysis to patients aged 18 years and older who underwent one the following procedures: abdominal aortic aneurysm repair, pancreatectomy, colectomy, coronary artery bypass graft, and total hip arthroplasty.
Ms. Brownlee reported results from 502,157 patients who underwent surgical procedures at 347 hospitals. The 1-year readmission rate was 23.5%, and ranged from 12% to 36% across procedures. After controlling for procedure, the researchers observed a 7.9% variation in readmission risk between hospitals. Staffing accounted for 9.8% of variance, followed by hospital structural characteristics such as teaching status and clinical programs (7.5%), patient ZIP code (3.8%), hospital perioperative resources such as inpatient rehab (2.9%), hospital volume (2.8%), and patient clinical characteristics (2.1%). The following hospital characteristics were significantly associated with a lower risk of 1-year readmission: high physician/bed ratio (hazard ratio 0.85; P = .00017); transplant status (HR 0.87; P = .022); high-income ZIP code (HR 0.89; P less than .001); high nurse bed/bed ratio (HR 0.90; P = .047), and cancer center designation (HR 0.93; P = .021).
“Compared to patient clinical characteristics, hospital factors such as staffing ratios, perioperative resources, and structural elements account for more variation in postoperative outcomes,” Ms. Brownlee concluded. “However, it’s important to note that in the present study, over 70% of variation in readmission rates is not explained by the covariates that we analyzed. It’s possible that there are other factors we need to consider. That’s where the direction of this research is going. Much of the variation in readmission risk across hospitals cannot be characterized with currently utilized administrative data.”
The National Institutes of Health provided funding for the study. Ms. Brownlee reported having no financial disclosures.
CORONADO, CALIF. – Variation in readmission risk across hospitals following certain surgical procedures is more attributable to hospital factors than to patient characteristics, results from a large analysis demonstrated.
Such is the impact of the care delivery macro environment (CDM), which Sarah A. Brownlee and coauthors defined as a series of complex interactions between patient characteristics and imposed hospital attributes than can impact patient outcomes postoperatively.
The purpose of the current study was to determine the relative contribution of various aspects of the CDM to 1-year readmission risk after surgery. Working with colleagues Anai Kothari, MD, and Paul Kuo MD, in the One:MAP Section of Clinical informatics and Analytics in the department of surgery at Loyola University Medical Center, Ms. Brownlee analyzed the Healthcare Cost and Utilization Project State Inpatient Databases from Florida, New York, and Washington between 2009 and 2013, which were linked to the American Hospital Association Annual Survey from that same time period.
The researchers used smoothed hazard estimates to determine all-cause readmission in the year after surgery, and multilevel survival models with shared frailty to determine the relative impact of hospital versus patient characteristics on the heterogeneity of readmission risk between hospitals. They limited the analysis to patients aged 18 years and older who underwent one the following procedures: abdominal aortic aneurysm repair, pancreatectomy, colectomy, coronary artery bypass graft, and total hip arthroplasty.
Ms. Brownlee reported results from 502,157 patients who underwent surgical procedures at 347 hospitals. The 1-year readmission rate was 23.5%, and ranged from 12% to 36% across procedures. After controlling for procedure, the researchers observed a 7.9% variation in readmission risk between hospitals. Staffing accounted for 9.8% of variance, followed by hospital structural characteristics such as teaching status and clinical programs (7.5%), patient ZIP code (3.8%), hospital perioperative resources such as inpatient rehab (2.9%), hospital volume (2.8%), and patient clinical characteristics (2.1%). The following hospital characteristics were significantly associated with a lower risk of 1-year readmission: high physician/bed ratio (hazard ratio 0.85; P = .00017); transplant status (HR 0.87; P = .022); high-income ZIP code (HR 0.89; P less than .001); high nurse bed/bed ratio (HR 0.90; P = .047), and cancer center designation (HR 0.93; P = .021).
“Compared to patient clinical characteristics, hospital factors such as staffing ratios, perioperative resources, and structural elements account for more variation in postoperative outcomes,” Ms. Brownlee concluded. “However, it’s important to note that in the present study, over 70% of variation in readmission rates is not explained by the covariates that we analyzed. It’s possible that there are other factors we need to consider. That’s where the direction of this research is going. Much of the variation in readmission risk across hospitals cannot be characterized with currently utilized administrative data.”
The National Institutes of Health provided funding for the study. Ms. Brownlee reported having no financial disclosures.
AT WSA 2016
Key clinical point:
Major finding: Staffing accounted for 9.8% of variance in readmission risk between hospitals, followed by hospital structural characteristics such as teaching status and clinical programs (7.5%).
Data source: Results from 502,157 patients who underwent surgical procedures at 347 hospitals in three states.
Disclosures: The National Institutes of Health provided funding for the study. Ms. Brownlee reported having no financial disclosures.
Tips for Improving Early Discharge Rates
Discharging patients before noon has many advantages: It creates open beds to accommodate the surge in admissions in the afternoon and helps minimize the bottleneck in system-wide patient flow, says Ragu P. Sanjeev, MD, unit-based medical director at Christiana Hospital in Newark, Del.
“Doing so can reduce ER wait times, reduce the percentage of patients leaving the ED without being seen—a safety issue for those patients—and also help to place the right patient in the right bed in a timely manner,” he says. “It’s a not just a patient flow issue; it’s a patient safety issue, as well.”
At his hospital, hospitalists developed a “Discharge by Appointment” process to address the issue systematically and completed a pilot project to test it. Their “‘Discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon,” was an abstract presented at HM16.1
“Giving patients that have a high predictability of being discharged next day, an appointment, and set off a series of steps to be completed the day before discharge including, notifying the transport team/family members of the appointment, helped improve the number of discharges before noon significantly,” according to the abstract.
Their successful pilot project has led to lasting changes, Dr. Sanjeev says. For about 16 months, the number of discharges before noon has been steadily increasing, helping the acute medicine service line perform better than its “Discharge by Noon” goal by 44.4% this fiscal year.
“As hospitalists, we have a great potential to positively impact the hospital-wide issues like patient flow and patient safety,” Dr. Sanjeev says. “By actively participating in important hospital committees, you can understand better and get inspired by the ongoing improvement efforts. By partnering with your care team, including bedside nurses, case managers, and social workers, we can make a big difference in early discharges. This success can be expanded to discharges throughout the day with appointments, thereby keeping the flow faucet open at all times.”
Reference
- Sanjeev R, McMillen J, Fedyk A. ‘discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon [abstract]. J Hosp Med. http://www.shmabstracts.com/abstract/discharge-by-appointment-improves-patient-flow-by-increasing-number-of-discharges-before-noon/. Accessed April 27, 2016.
Discharging patients before noon has many advantages: It creates open beds to accommodate the surge in admissions in the afternoon and helps minimize the bottleneck in system-wide patient flow, says Ragu P. Sanjeev, MD, unit-based medical director at Christiana Hospital in Newark, Del.
“Doing so can reduce ER wait times, reduce the percentage of patients leaving the ED without being seen—a safety issue for those patients—and also help to place the right patient in the right bed in a timely manner,” he says. “It’s a not just a patient flow issue; it’s a patient safety issue, as well.”
At his hospital, hospitalists developed a “Discharge by Appointment” process to address the issue systematically and completed a pilot project to test it. Their “‘Discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon,” was an abstract presented at HM16.1
“Giving patients that have a high predictability of being discharged next day, an appointment, and set off a series of steps to be completed the day before discharge including, notifying the transport team/family members of the appointment, helped improve the number of discharges before noon significantly,” according to the abstract.
Their successful pilot project has led to lasting changes, Dr. Sanjeev says. For about 16 months, the number of discharges before noon has been steadily increasing, helping the acute medicine service line perform better than its “Discharge by Noon” goal by 44.4% this fiscal year.
“As hospitalists, we have a great potential to positively impact the hospital-wide issues like patient flow and patient safety,” Dr. Sanjeev says. “By actively participating in important hospital committees, you can understand better and get inspired by the ongoing improvement efforts. By partnering with your care team, including bedside nurses, case managers, and social workers, we can make a big difference in early discharges. This success can be expanded to discharges throughout the day with appointments, thereby keeping the flow faucet open at all times.”
Reference
- Sanjeev R, McMillen J, Fedyk A. ‘discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon [abstract]. J Hosp Med. http://www.shmabstracts.com/abstract/discharge-by-appointment-improves-patient-flow-by-increasing-number-of-discharges-before-noon/. Accessed April 27, 2016.
Discharging patients before noon has many advantages: It creates open beds to accommodate the surge in admissions in the afternoon and helps minimize the bottleneck in system-wide patient flow, says Ragu P. Sanjeev, MD, unit-based medical director at Christiana Hospital in Newark, Del.
“Doing so can reduce ER wait times, reduce the percentage of patients leaving the ED without being seen—a safety issue for those patients—and also help to place the right patient in the right bed in a timely manner,” he says. “It’s a not just a patient flow issue; it’s a patient safety issue, as well.”
At his hospital, hospitalists developed a “Discharge by Appointment” process to address the issue systematically and completed a pilot project to test it. Their “‘Discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon,” was an abstract presented at HM16.1
“Giving patients that have a high predictability of being discharged next day, an appointment, and set off a series of steps to be completed the day before discharge including, notifying the transport team/family members of the appointment, helped improve the number of discharges before noon significantly,” according to the abstract.
Their successful pilot project has led to lasting changes, Dr. Sanjeev says. For about 16 months, the number of discharges before noon has been steadily increasing, helping the acute medicine service line perform better than its “Discharge by Noon” goal by 44.4% this fiscal year.
“As hospitalists, we have a great potential to positively impact the hospital-wide issues like patient flow and patient safety,” Dr. Sanjeev says. “By actively participating in important hospital committees, you can understand better and get inspired by the ongoing improvement efforts. By partnering with your care team, including bedside nurses, case managers, and social workers, we can make a big difference in early discharges. This success can be expanded to discharges throughout the day with appointments, thereby keeping the flow faucet open at all times.”
Reference
- Sanjeev R, McMillen J, Fedyk A. ‘discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon [abstract]. J Hosp Med. http://www.shmabstracts.com/abstract/discharge-by-appointment-improves-patient-flow-by-increasing-number-of-discharges-before-noon/. Accessed April 27, 2016.
Barriers to Achieving High Reliability
The conceptual models being used in healthcare’s efforts to achieve high reliability may have weaknesses, according to Marc T. Edwards, MD, MBA, author of “An Organizational Learning Framework for Patient Safety,” published in the American Journal of Medical Quality. Those weaknesses could explain why controversy over basic issues around the subject remain.
His paper analyzes those barriers to achieving high reliability in healthcare and points to a way forward—specifically, a different framework for identifying leverage points for improvement based on organizational learning theory.
“Organizations learn from others, from defects, from measurement, and from mindfulness,” he writes. “These learning modes correspond with contemporary themes of collaboration, no blame for human error, accountability for performance, and managing the unexpected. The collaborative model has dominated improvement efforts. Greater attention to the underdeveloped modes of organizational learning may foster more rapid progress in patient safety by increasing organizational capabilities, strengthening a culture of safety, and fixing more of the process problems that contribute to patient harm.”
To help bring this about, hospitalists can contribute by “embracing accountability for clinical performance, developing appropriate measures, and engaging in safety improvement activities — the most salient and important of which is reporting adverse events, near misses, and hazardous conditions affecting their own patients,” Dr. Edwards says. “This means taking responsibility for ending the culture of blame in healthcare, which currently blocks physicians from such self-reporting.”
He adds that hospitalists can do this by changing the model by which they conduct clinical peer review: Instead of focusing on whether individual physicians practiced according to standards, they could look broadly at learning opportunities for improvement in the system of care.
Reference
- Edwards MT. An organizational learning framework for patient safety [published online ahead of print February 25, 2016]. Am J Med Qual. pii:1062860616632295.
The conceptual models being used in healthcare’s efforts to achieve high reliability may have weaknesses, according to Marc T. Edwards, MD, MBA, author of “An Organizational Learning Framework for Patient Safety,” published in the American Journal of Medical Quality. Those weaknesses could explain why controversy over basic issues around the subject remain.
His paper analyzes those barriers to achieving high reliability in healthcare and points to a way forward—specifically, a different framework for identifying leverage points for improvement based on organizational learning theory.
“Organizations learn from others, from defects, from measurement, and from mindfulness,” he writes. “These learning modes correspond with contemporary themes of collaboration, no blame for human error, accountability for performance, and managing the unexpected. The collaborative model has dominated improvement efforts. Greater attention to the underdeveloped modes of organizational learning may foster more rapid progress in patient safety by increasing organizational capabilities, strengthening a culture of safety, and fixing more of the process problems that contribute to patient harm.”
To help bring this about, hospitalists can contribute by “embracing accountability for clinical performance, developing appropriate measures, and engaging in safety improvement activities — the most salient and important of which is reporting adverse events, near misses, and hazardous conditions affecting their own patients,” Dr. Edwards says. “This means taking responsibility for ending the culture of blame in healthcare, which currently blocks physicians from such self-reporting.”
He adds that hospitalists can do this by changing the model by which they conduct clinical peer review: Instead of focusing on whether individual physicians practiced according to standards, they could look broadly at learning opportunities for improvement in the system of care.
Reference
- Edwards MT. An organizational learning framework for patient safety [published online ahead of print February 25, 2016]. Am J Med Qual. pii:1062860616632295.
The conceptual models being used in healthcare’s efforts to achieve high reliability may have weaknesses, according to Marc T. Edwards, MD, MBA, author of “An Organizational Learning Framework for Patient Safety,” published in the American Journal of Medical Quality. Those weaknesses could explain why controversy over basic issues around the subject remain.
His paper analyzes those barriers to achieving high reliability in healthcare and points to a way forward—specifically, a different framework for identifying leverage points for improvement based on organizational learning theory.
“Organizations learn from others, from defects, from measurement, and from mindfulness,” he writes. “These learning modes correspond with contemporary themes of collaboration, no blame for human error, accountability for performance, and managing the unexpected. The collaborative model has dominated improvement efforts. Greater attention to the underdeveloped modes of organizational learning may foster more rapid progress in patient safety by increasing organizational capabilities, strengthening a culture of safety, and fixing more of the process problems that contribute to patient harm.”
To help bring this about, hospitalists can contribute by “embracing accountability for clinical performance, developing appropriate measures, and engaging in safety improvement activities — the most salient and important of which is reporting adverse events, near misses, and hazardous conditions affecting their own patients,” Dr. Edwards says. “This means taking responsibility for ending the culture of blame in healthcare, which currently blocks physicians from such self-reporting.”
He adds that hospitalists can do this by changing the model by which they conduct clinical peer review: Instead of focusing on whether individual physicians practiced according to standards, they could look broadly at learning opportunities for improvement in the system of care.
Reference
- Edwards MT. An organizational learning framework for patient safety [published online ahead of print February 25, 2016]. Am J Med Qual. pii:1062860616632295.