User login
Risk factors identified for the 1 in 500 likely to require postoperative CPR
PHOENIX – Pneumonia, dehydration, and septicemia topped the list of risk factors associated with the need for cardiopulmonary resuscitation during hospitalization for a major surgical procedure in 1 in 500 patients, a retrospective analysis found.
The large sample studied shows that having emergency rather than elective surgery, being older, being African American, and lacking health insurance were also associated with greater odds of needing CPR in this cohort, Dr. Ashima Das of Rainbow Children’s Hospital in Cleveland reported.
A review of 12,631,502 patient records found in the 2009 and 2010 National Inpatient Sample showed that 0.2% of all major surgery patients between 18 and 64 years went into cardiac arrest during their surgical hospitalization. Patients with postoperative pneumonia were at 3.05 (95% confidence interval = 2.75-3.39, P < .0001) times higher risk for needing CPR; meanwhile, major surgery patients with postoperative dehydration or other fluid and electrolyte disruptions faced an increased risk of 3.50 (95% CI = 3.18-3.85, P < .0001), Dr. Das reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Septicemia posed a 2.60 greater risk (95% CI = 2.34-2.86, P < .0001). The odds ratio of needing CPR for patients with coagulopathy was 2.54 (95% CI = 2.30-2.81, P < .0001).
Dr. Das and her colleagues found that 80% of the 23,858 surgical procedures performed in patients who also needed CPR were emergent rather than elective. Patients’ risk of cardiac arrest increased by 1.02 ( 95% CI = 1.01-1.03, P < .0001) with every year of age, while African Americans had a slightly higher risk of needing CPR, compared with whites (OR, 1.51; 95% CI = 1.35-1.68; P < .0001), as did the uninsured, compared with the insured (P < .0001).
The authors of this study said they had no relevant financial disclosures.
On Twitter @whitneymcknight
PHOENIX – Pneumonia, dehydration, and septicemia topped the list of risk factors associated with the need for cardiopulmonary resuscitation during hospitalization for a major surgical procedure in 1 in 500 patients, a retrospective analysis found.
The large sample studied shows that having emergency rather than elective surgery, being older, being African American, and lacking health insurance were also associated with greater odds of needing CPR in this cohort, Dr. Ashima Das of Rainbow Children’s Hospital in Cleveland reported.
A review of 12,631,502 patient records found in the 2009 and 2010 National Inpatient Sample showed that 0.2% of all major surgery patients between 18 and 64 years went into cardiac arrest during their surgical hospitalization. Patients with postoperative pneumonia were at 3.05 (95% confidence interval = 2.75-3.39, P < .0001) times higher risk for needing CPR; meanwhile, major surgery patients with postoperative dehydration or other fluid and electrolyte disruptions faced an increased risk of 3.50 (95% CI = 3.18-3.85, P < .0001), Dr. Das reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Septicemia posed a 2.60 greater risk (95% CI = 2.34-2.86, P < .0001). The odds ratio of needing CPR for patients with coagulopathy was 2.54 (95% CI = 2.30-2.81, P < .0001).
Dr. Das and her colleagues found that 80% of the 23,858 surgical procedures performed in patients who also needed CPR were emergent rather than elective. Patients’ risk of cardiac arrest increased by 1.02 ( 95% CI = 1.01-1.03, P < .0001) with every year of age, while African Americans had a slightly higher risk of needing CPR, compared with whites (OR, 1.51; 95% CI = 1.35-1.68; P < .0001), as did the uninsured, compared with the insured (P < .0001).
The authors of this study said they had no relevant financial disclosures.
On Twitter @whitneymcknight
PHOENIX – Pneumonia, dehydration, and septicemia topped the list of risk factors associated with the need for cardiopulmonary resuscitation during hospitalization for a major surgical procedure in 1 in 500 patients, a retrospective analysis found.
The large sample studied shows that having emergency rather than elective surgery, being older, being African American, and lacking health insurance were also associated with greater odds of needing CPR in this cohort, Dr. Ashima Das of Rainbow Children’s Hospital in Cleveland reported.
A review of 12,631,502 patient records found in the 2009 and 2010 National Inpatient Sample showed that 0.2% of all major surgery patients between 18 and 64 years went into cardiac arrest during their surgical hospitalization. Patients with postoperative pneumonia were at 3.05 (95% confidence interval = 2.75-3.39, P < .0001) times higher risk for needing CPR; meanwhile, major surgery patients with postoperative dehydration or other fluid and electrolyte disruptions faced an increased risk of 3.50 (95% CI = 3.18-3.85, P < .0001), Dr. Das reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Septicemia posed a 2.60 greater risk (95% CI = 2.34-2.86, P < .0001). The odds ratio of needing CPR for patients with coagulopathy was 2.54 (95% CI = 2.30-2.81, P < .0001).
Dr. Das and her colleagues found that 80% of the 23,858 surgical procedures performed in patients who also needed CPR were emergent rather than elective. Patients’ risk of cardiac arrest increased by 1.02 ( 95% CI = 1.01-1.03, P < .0001) with every year of age, while African Americans had a slightly higher risk of needing CPR, compared with whites (OR, 1.51; 95% CI = 1.35-1.68; P < .0001), as did the uninsured, compared with the insured (P < .0001).
The authors of this study said they had no relevant financial disclosures.
On Twitter @whitneymcknight
AT THE CRITICAL CARE CONGRESS
Key clinical point: Risk modification for certain patient populations undergoing major surgical procedures may help reduce the rates of associated CPR.
Major finding: One in 500 patients who had a major surgical procedure required cardiopulmonary resuscitation.
Data source: A retrospective analysis of 12,631,502 patient records from the 2009-2010 Nationwide Inpatient Sample, identifying several risk factors for cardiac arrest occurring during a surgical hospitalization.
Disclosures: The authors of this study said they had no relevant financial disclosures.
Pain control with ketorolac appears safe after pediatric heart surgery
PHOENIX – The NSAID ketorolac is safe to use in very young children after cardiac surgery, and dramatically decreases the length of intubation and ICU stay as well as the use of opioids, according to a retrospective cohort study from the Cohen Children’s Medical Center in New Hyde Park, N.Y.
Ketorolac is catching on in some places for postoperative pain control, but there are still significant concerns about nephrotoxicity and bleeding, especially in children, said Dr. Tracie Lin, a pediatrics resident at the medical center.
Those potential side effects didn’t turn out to be problems when her team compared outcomes in 26 children who received ketorolac – 0.5 mg/kg to a maximum of 30 mg/day – to 34 who did not receive it following congenital heart surgery.
“Think twice before holding back on ketorolac. There seems to be a lot of benefit, and less harm than someone might expect,” Dr. Lin said at the meeting sponsored by the Society for Critical Care Medicine.
Patients who received ketorolac, a mean of 35.5 months old, received less than 0.5 mg/kg per day of morphine IV equivalents in the first day after surgery, even less on day 2, and virtually none on day 3. They were, on average, intubated less than a day, in the ICU for 110 hours, and in the hospital for 5 days.
Patients in the no-ketorolac group, a mean of 2 months old, received almost 4 mg/kg per day of morphine IV equivalents in the first and second postop day, and about 2 mg/kg per day on day 3. They were intubated for an average of 3 days, in the ICU for 188 hours, and in the hospital for 17 days.
The age difference between the two groups probably reflects the hesitancy to use ketorolac in children under 6 months old. Only a couple children under 6 months old received ketorolac in the study; it didn’t cause them any kidney problems, Dr. Lin said.
Pain control was statistically equal in both groups, with pain-free assessments over 75% of the time during the first 3 postop days in both groups, and there were no statistically significant differences in the rates of breakthrough pain.
Meanwhile, “we found no additional nephrotoxicity” in the children taking ketorolac, Dr. Lin said.
At ICU arrival and after cardiac surgery, about 60% of those taking ketorolac had some degree of acute kidney injury, mostly stage 1 or 2; the finding was the same at 2 weeks post op. About 40% of children in the no-ketorolac group arrived at the ICU with some degree of acute kidney injury, again the majority stage 1 and 2; at 2 weeks assessment, that number had increased to almost 60%.
The investigators did not directly assess postoperative bleeding, but children taking ketorolac had their chest tubes pulled at about 3 days, while those in the no-ketorolac group retained their chest tubes for about 5 days. The finding suggests that ketorolac didn’t cause bleeding problems that prevented chest tube removal, Dr. Lin said.
There were other differences between the groups; ketorolac patients had RACH-1 [Risk Adjustment for Congenital Heart Surgery] scores of 3 or less, and almost all had sternotomies.
Children in the no-ketorolac group had RACH-1 scores ranging from 1 to 5, and although the majority had sternotomies, about a quarter had thoracotomies. The differences in incision types were most likely related to age-specific indications for surgery.
Dr. Lin and her team adjusted for all those differences on multivariate analysis, and found that the benefits of ketorolac remained; they “were not due to confounders,” she said.
The investigators have no relevant disclosures, and there was no external funding for the project.
PHOENIX – The NSAID ketorolac is safe to use in very young children after cardiac surgery, and dramatically decreases the length of intubation and ICU stay as well as the use of opioids, according to a retrospective cohort study from the Cohen Children’s Medical Center in New Hyde Park, N.Y.
Ketorolac is catching on in some places for postoperative pain control, but there are still significant concerns about nephrotoxicity and bleeding, especially in children, said Dr. Tracie Lin, a pediatrics resident at the medical center.
Those potential side effects didn’t turn out to be problems when her team compared outcomes in 26 children who received ketorolac – 0.5 mg/kg to a maximum of 30 mg/day – to 34 who did not receive it following congenital heart surgery.
“Think twice before holding back on ketorolac. There seems to be a lot of benefit, and less harm than someone might expect,” Dr. Lin said at the meeting sponsored by the Society for Critical Care Medicine.
Patients who received ketorolac, a mean of 35.5 months old, received less than 0.5 mg/kg per day of morphine IV equivalents in the first day after surgery, even less on day 2, and virtually none on day 3. They were, on average, intubated less than a day, in the ICU for 110 hours, and in the hospital for 5 days.
Patients in the no-ketorolac group, a mean of 2 months old, received almost 4 mg/kg per day of morphine IV equivalents in the first and second postop day, and about 2 mg/kg per day on day 3. They were intubated for an average of 3 days, in the ICU for 188 hours, and in the hospital for 17 days.
The age difference between the two groups probably reflects the hesitancy to use ketorolac in children under 6 months old. Only a couple children under 6 months old received ketorolac in the study; it didn’t cause them any kidney problems, Dr. Lin said.
Pain control was statistically equal in both groups, with pain-free assessments over 75% of the time during the first 3 postop days in both groups, and there were no statistically significant differences in the rates of breakthrough pain.
Meanwhile, “we found no additional nephrotoxicity” in the children taking ketorolac, Dr. Lin said.
At ICU arrival and after cardiac surgery, about 60% of those taking ketorolac had some degree of acute kidney injury, mostly stage 1 or 2; the finding was the same at 2 weeks post op. About 40% of children in the no-ketorolac group arrived at the ICU with some degree of acute kidney injury, again the majority stage 1 and 2; at 2 weeks assessment, that number had increased to almost 60%.
The investigators did not directly assess postoperative bleeding, but children taking ketorolac had their chest tubes pulled at about 3 days, while those in the no-ketorolac group retained their chest tubes for about 5 days. The finding suggests that ketorolac didn’t cause bleeding problems that prevented chest tube removal, Dr. Lin said.
There were other differences between the groups; ketorolac patients had RACH-1 [Risk Adjustment for Congenital Heart Surgery] scores of 3 or less, and almost all had sternotomies.
Children in the no-ketorolac group had RACH-1 scores ranging from 1 to 5, and although the majority had sternotomies, about a quarter had thoracotomies. The differences in incision types were most likely related to age-specific indications for surgery.
Dr. Lin and her team adjusted for all those differences on multivariate analysis, and found that the benefits of ketorolac remained; they “were not due to confounders,” she said.
The investigators have no relevant disclosures, and there was no external funding for the project.
PHOENIX – The NSAID ketorolac is safe to use in very young children after cardiac surgery, and dramatically decreases the length of intubation and ICU stay as well as the use of opioids, according to a retrospective cohort study from the Cohen Children’s Medical Center in New Hyde Park, N.Y.
Ketorolac is catching on in some places for postoperative pain control, but there are still significant concerns about nephrotoxicity and bleeding, especially in children, said Dr. Tracie Lin, a pediatrics resident at the medical center.
Those potential side effects didn’t turn out to be problems when her team compared outcomes in 26 children who received ketorolac – 0.5 mg/kg to a maximum of 30 mg/day – to 34 who did not receive it following congenital heart surgery.
“Think twice before holding back on ketorolac. There seems to be a lot of benefit, and less harm than someone might expect,” Dr. Lin said at the meeting sponsored by the Society for Critical Care Medicine.
Patients who received ketorolac, a mean of 35.5 months old, received less than 0.5 mg/kg per day of morphine IV equivalents in the first day after surgery, even less on day 2, and virtually none on day 3. They were, on average, intubated less than a day, in the ICU for 110 hours, and in the hospital for 5 days.
Patients in the no-ketorolac group, a mean of 2 months old, received almost 4 mg/kg per day of morphine IV equivalents in the first and second postop day, and about 2 mg/kg per day on day 3. They were intubated for an average of 3 days, in the ICU for 188 hours, and in the hospital for 17 days.
The age difference between the two groups probably reflects the hesitancy to use ketorolac in children under 6 months old. Only a couple children under 6 months old received ketorolac in the study; it didn’t cause them any kidney problems, Dr. Lin said.
Pain control was statistically equal in both groups, with pain-free assessments over 75% of the time during the first 3 postop days in both groups, and there were no statistically significant differences in the rates of breakthrough pain.
Meanwhile, “we found no additional nephrotoxicity” in the children taking ketorolac, Dr. Lin said.
At ICU arrival and after cardiac surgery, about 60% of those taking ketorolac had some degree of acute kidney injury, mostly stage 1 or 2; the finding was the same at 2 weeks post op. About 40% of children in the no-ketorolac group arrived at the ICU with some degree of acute kidney injury, again the majority stage 1 and 2; at 2 weeks assessment, that number had increased to almost 60%.
The investigators did not directly assess postoperative bleeding, but children taking ketorolac had their chest tubes pulled at about 3 days, while those in the no-ketorolac group retained their chest tubes for about 5 days. The finding suggests that ketorolac didn’t cause bleeding problems that prevented chest tube removal, Dr. Lin said.
There were other differences between the groups; ketorolac patients had RACH-1 [Risk Adjustment for Congenital Heart Surgery] scores of 3 or less, and almost all had sternotomies.
Children in the no-ketorolac group had RACH-1 scores ranging from 1 to 5, and although the majority had sternotomies, about a quarter had thoracotomies. The differences in incision types were most likely related to age-specific indications for surgery.
Dr. Lin and her team adjusted for all those differences on multivariate analysis, and found that the benefits of ketorolac remained; they “were not due to confounders,” she said.
The investigators have no relevant disclosures, and there was no external funding for the project.
AT THE CRITICAL CARE CONGRESS
Key clinical point: The benefits of postoperative ketorolac outweigh the risks, even in very young children.
Major finding: Following heart surgery, children with ketorolac as part of their pain control regimen were intubated for less than a day; children without ketorolac were intubated an average of 3 days.
Data source: Retrospective cohort study of 60 very young children following congenital heart surgery.
Disclosures:The investigators have no relevant disclosures, and there was no external funding for the project.
Postop NSAIDs may raise anastomotic complications
Postoperative NSAIDs appear to raise the risk for anastomotic complications among patients undergoing nonelective colorectal resection, according to a report in JAMA Surgery.
“Given that other analgesic regimens are effective and well tolerated, these data may be enough from some surgeons to alter practice patterns,” said Dr. Timo W. Hakkarainen of the department of surgery at the University of Washington, Seattle, and his associates.
The recent development of intravenous formulations of NSAIDs has expanded their use in postoperative patients, chiefly because the drugs don’t carry the adverse effects of opioid analgesia, which include impaired GI motility. However, several small and single-institution studies have suggested that NSAIDs used in this setting may impair anastomotic healing and may raise the rates of leakage.
Dr. Hakkarainen and his associates examined this issue using data from a statewide surveillance system for surgical quality. They analyzed 90-day complications among 13,082 adults (mean age, 58 years) who underwent surgery of the GI tract with anastomosis at 47 participating hospitals throughout Washington State during a 5-year period. The investigators tracked the use of ibuprofen, naproxen, ketorolac tromethamine, Caldolor, celecoxib, and diclofenac during the first 24 hours after surgery; they assumed that in most cases, this involved IV NSAIDs because such patients don’t take oral medications within that time period.
Postoperative NSAIDs were given to 24% of the study population. This use was associated with a significantly increased risk for anastomotic leakage during the next 90 days, with an OR of 1.24. Further analysis showed that this association was largely restricted to the subgroup of patients who had nonelective colorectal surgery, in whom the relationship was even stronger, with an OR of 1.70. Among patients who had nonelective colorectal surgery, those who received postoperative NSAIDs had a 12.3% rate of anastomotic leakage, compared with an 8.3% rate among those who did not receive NSAIDs, the investigators said (JAMA Surg. 2015 Jan. 21 [doi:10.1001/jamasurg.2014.2239]).
This study was limited in that the records didn’t specify the dose or duration of NSAID use, didn’t take into account preoperative NSAID use, and didn’t include the timing of anastomotic leakage (immediately following surgery vs. weeks or months later). “We believe that [these] results are sufficient to suggest caution in the use of NSAIDs in the postoperative treatment of patients undergoing nonelective colorectal surgery, and highlight the importance of further evaluation of this association,” the investigators added.
Postoperative NSAIDs appear to raise the risk for anastomotic complications among patients undergoing nonelective colorectal resection, according to a report in JAMA Surgery.
“Given that other analgesic regimens are effective and well tolerated, these data may be enough from some surgeons to alter practice patterns,” said Dr. Timo W. Hakkarainen of the department of surgery at the University of Washington, Seattle, and his associates.
The recent development of intravenous formulations of NSAIDs has expanded their use in postoperative patients, chiefly because the drugs don’t carry the adverse effects of opioid analgesia, which include impaired GI motility. However, several small and single-institution studies have suggested that NSAIDs used in this setting may impair anastomotic healing and may raise the rates of leakage.
Dr. Hakkarainen and his associates examined this issue using data from a statewide surveillance system for surgical quality. They analyzed 90-day complications among 13,082 adults (mean age, 58 years) who underwent surgery of the GI tract with anastomosis at 47 participating hospitals throughout Washington State during a 5-year period. The investigators tracked the use of ibuprofen, naproxen, ketorolac tromethamine, Caldolor, celecoxib, and diclofenac during the first 24 hours after surgery; they assumed that in most cases, this involved IV NSAIDs because such patients don’t take oral medications within that time period.
Postoperative NSAIDs were given to 24% of the study population. This use was associated with a significantly increased risk for anastomotic leakage during the next 90 days, with an OR of 1.24. Further analysis showed that this association was largely restricted to the subgroup of patients who had nonelective colorectal surgery, in whom the relationship was even stronger, with an OR of 1.70. Among patients who had nonelective colorectal surgery, those who received postoperative NSAIDs had a 12.3% rate of anastomotic leakage, compared with an 8.3% rate among those who did not receive NSAIDs, the investigators said (JAMA Surg. 2015 Jan. 21 [doi:10.1001/jamasurg.2014.2239]).
This study was limited in that the records didn’t specify the dose or duration of NSAID use, didn’t take into account preoperative NSAID use, and didn’t include the timing of anastomotic leakage (immediately following surgery vs. weeks or months later). “We believe that [these] results are sufficient to suggest caution in the use of NSAIDs in the postoperative treatment of patients undergoing nonelective colorectal surgery, and highlight the importance of further evaluation of this association,” the investigators added.
Postoperative NSAIDs appear to raise the risk for anastomotic complications among patients undergoing nonelective colorectal resection, according to a report in JAMA Surgery.
“Given that other analgesic regimens are effective and well tolerated, these data may be enough from some surgeons to alter practice patterns,” said Dr. Timo W. Hakkarainen of the department of surgery at the University of Washington, Seattle, and his associates.
The recent development of intravenous formulations of NSAIDs has expanded their use in postoperative patients, chiefly because the drugs don’t carry the adverse effects of opioid analgesia, which include impaired GI motility. However, several small and single-institution studies have suggested that NSAIDs used in this setting may impair anastomotic healing and may raise the rates of leakage.
Dr. Hakkarainen and his associates examined this issue using data from a statewide surveillance system for surgical quality. They analyzed 90-day complications among 13,082 adults (mean age, 58 years) who underwent surgery of the GI tract with anastomosis at 47 participating hospitals throughout Washington State during a 5-year period. The investigators tracked the use of ibuprofen, naproxen, ketorolac tromethamine, Caldolor, celecoxib, and diclofenac during the first 24 hours after surgery; they assumed that in most cases, this involved IV NSAIDs because such patients don’t take oral medications within that time period.
Postoperative NSAIDs were given to 24% of the study population. This use was associated with a significantly increased risk for anastomotic leakage during the next 90 days, with an OR of 1.24. Further analysis showed that this association was largely restricted to the subgroup of patients who had nonelective colorectal surgery, in whom the relationship was even stronger, with an OR of 1.70. Among patients who had nonelective colorectal surgery, those who received postoperative NSAIDs had a 12.3% rate of anastomotic leakage, compared with an 8.3% rate among those who did not receive NSAIDs, the investigators said (JAMA Surg. 2015 Jan. 21 [doi:10.1001/jamasurg.2014.2239]).
This study was limited in that the records didn’t specify the dose or duration of NSAID use, didn’t take into account preoperative NSAID use, and didn’t include the timing of anastomotic leakage (immediately following surgery vs. weeks or months later). “We believe that [these] results are sufficient to suggest caution in the use of NSAIDs in the postoperative treatment of patients undergoing nonelective colorectal surgery, and highlight the importance of further evaluation of this association,” the investigators added.
Key clinical point: Postoperative NSAIDs appear to raise the risk of anastomotic complications in patients undergoing nonelective colorectal resection.
Major finding: Among patients who had nonelective colorectal surgery, those who received postoperative NSAIDs had a 12.3% rate of anastomotic leakage, compared with an 8.3% rate among those who did not receive NSAIDs.
Data source: A secondary analysis of a cohort study involving 13,082 patients who had GI-tract surgery with anastomosis at 47 hospitals in Washington State during a 5-year period.
Disclosures: The Comparative Effective Research Translation Network of the Agency for Healthcare Research and Quality, the Washington State Life Science Discovery Fund, and the National Institutes of Health supported the study. Dr. Hakkarainen and his associates reported having no financial disclosures.
Postop pancreatectomy complications most deadly in elderly
Although rates of complications following pancreatectomy are relatively similar in patients both above and below the age of 80 years, significantly higher mortality rates occur in the older age group, according to the findings of a new study published online in the Annals of Surgery
“Previous studies have focused solely on mortality after pancreatectomy in older patients or failure to rescue for all patients undergoing pancreatectomy,” wrote lead author Dr. Nina P. Tamirisa of the University of Texas Medical Branch in Galveston, and her associates. “For older patients, it is not clear whether the observed increase in mortality rate is attributed to higher rates of postsurgical complications, higher failure to rescue from these postsurgical complications, or both” (Ann. Surg. 2015 [doi:10.1097/SLA.0000000000001093]).
In this study, “failure to rescue” was calculated as the number of patients who died from complications divided by total number of patients with complications and was understood to measure of a hospital’s ability to recognize and manage postoperative complications.
In a retrospective cohort study, Dr. Tamirisa and her coinvestigators looked at data on 2,805 patients in the American College of Surgeons’ National Surgical Quality Improvement Pancreatectomy Demonstration Project (ACS NSQIP) at 43 high-volume centers around the United States between November 2011 and December 2012. Institutions with fewer than 10 cases were excluded, leaving 2,694 subjects from 37 centers for the study.
Following this, patients were divided into cohorts of those younger than 80 years of age, and those aged 80 years or older, which contained 2,496 and 198 subjects, respectively. Overall and individual cohorts were split roughly evenly between males and females. Postoperative morbidity and in-hospital mortality rates were measured along with rate of “failure to rescue.”
Results indicated that there were no significant differences in the rates of complications between the cohorts: 41.4% in patients under 80 years and 39.4% in patients aged 80 years or older (P = .58). However, in-hospital mortality rates were significant higher in the 80 and older cohort (3.0%) than in the younger group (1.1%) (P = .01).
Overall, unadjusted complication rates in the 37 centers included in the study varied widely from 25.0% to as high as 72.2%, while failure to rescue rates at ranged from 0.0% to 25.0%.
Major complications were seen in 29.3% of patients aged 80 years or older and in 28.5% of patients under 80 years old (P = .79), with perioperative bleeding being the most prevalent. Among patients with postoperative complications, ascites, chronic obstructive pulmonary disease, and diabetes were the comorbidities most highly associated with failure to rescue, along with acute renal failure, septic shock, and postoperative pulmonary complications.
“It is always true that avoiding complications will decrease mortality for all patients undergoing pancreatectomy,” concluded the investigators, adding that it’s crucial for there to be more interventions to facilitate identification and aggressive treatment of complications to decrease mortality in vulnerable older patients.
“Several factors, such as individual surgeon volume, impact patient outcomes and failure to rescue rates are a significant but not the sole contributor to increased mortality rates in older patients undergoing pancreatectomy,” wrote Dr. Tamirisa and her coauthors.
This study was funded by grants from the Cancer Prevention Research Institute of Texas, UTMB Clinical and Translational Science Award, the National Institutes of Health, and the Agency for Healthcare Research & Quality. Coauthor Dr. Bruce L. Hall disclosed being a paid consulting director of the American College of Surgeons’ National Surgical Quality Improvement Program.
Although rates of complications following pancreatectomy are relatively similar in patients both above and below the age of 80 years, significantly higher mortality rates occur in the older age group, according to the findings of a new study published online in the Annals of Surgery
“Previous studies have focused solely on mortality after pancreatectomy in older patients or failure to rescue for all patients undergoing pancreatectomy,” wrote lead author Dr. Nina P. Tamirisa of the University of Texas Medical Branch in Galveston, and her associates. “For older patients, it is not clear whether the observed increase in mortality rate is attributed to higher rates of postsurgical complications, higher failure to rescue from these postsurgical complications, or both” (Ann. Surg. 2015 [doi:10.1097/SLA.0000000000001093]).
In this study, “failure to rescue” was calculated as the number of patients who died from complications divided by total number of patients with complications and was understood to measure of a hospital’s ability to recognize and manage postoperative complications.
In a retrospective cohort study, Dr. Tamirisa and her coinvestigators looked at data on 2,805 patients in the American College of Surgeons’ National Surgical Quality Improvement Pancreatectomy Demonstration Project (ACS NSQIP) at 43 high-volume centers around the United States between November 2011 and December 2012. Institutions with fewer than 10 cases were excluded, leaving 2,694 subjects from 37 centers for the study.
Following this, patients were divided into cohorts of those younger than 80 years of age, and those aged 80 years or older, which contained 2,496 and 198 subjects, respectively. Overall and individual cohorts were split roughly evenly between males and females. Postoperative morbidity and in-hospital mortality rates were measured along with rate of “failure to rescue.”
Results indicated that there were no significant differences in the rates of complications between the cohorts: 41.4% in patients under 80 years and 39.4% in patients aged 80 years or older (P = .58). However, in-hospital mortality rates were significant higher in the 80 and older cohort (3.0%) than in the younger group (1.1%) (P = .01).
Overall, unadjusted complication rates in the 37 centers included in the study varied widely from 25.0% to as high as 72.2%, while failure to rescue rates at ranged from 0.0% to 25.0%.
Major complications were seen in 29.3% of patients aged 80 years or older and in 28.5% of patients under 80 years old (P = .79), with perioperative bleeding being the most prevalent. Among patients with postoperative complications, ascites, chronic obstructive pulmonary disease, and diabetes were the comorbidities most highly associated with failure to rescue, along with acute renal failure, septic shock, and postoperative pulmonary complications.
“It is always true that avoiding complications will decrease mortality for all patients undergoing pancreatectomy,” concluded the investigators, adding that it’s crucial for there to be more interventions to facilitate identification and aggressive treatment of complications to decrease mortality in vulnerable older patients.
“Several factors, such as individual surgeon volume, impact patient outcomes and failure to rescue rates are a significant but not the sole contributor to increased mortality rates in older patients undergoing pancreatectomy,” wrote Dr. Tamirisa and her coauthors.
This study was funded by grants from the Cancer Prevention Research Institute of Texas, UTMB Clinical and Translational Science Award, the National Institutes of Health, and the Agency for Healthcare Research & Quality. Coauthor Dr. Bruce L. Hall disclosed being a paid consulting director of the American College of Surgeons’ National Surgical Quality Improvement Program.
Although rates of complications following pancreatectomy are relatively similar in patients both above and below the age of 80 years, significantly higher mortality rates occur in the older age group, according to the findings of a new study published online in the Annals of Surgery
“Previous studies have focused solely on mortality after pancreatectomy in older patients or failure to rescue for all patients undergoing pancreatectomy,” wrote lead author Dr. Nina P. Tamirisa of the University of Texas Medical Branch in Galveston, and her associates. “For older patients, it is not clear whether the observed increase in mortality rate is attributed to higher rates of postsurgical complications, higher failure to rescue from these postsurgical complications, or both” (Ann. Surg. 2015 [doi:10.1097/SLA.0000000000001093]).
In this study, “failure to rescue” was calculated as the number of patients who died from complications divided by total number of patients with complications and was understood to measure of a hospital’s ability to recognize and manage postoperative complications.
In a retrospective cohort study, Dr. Tamirisa and her coinvestigators looked at data on 2,805 patients in the American College of Surgeons’ National Surgical Quality Improvement Pancreatectomy Demonstration Project (ACS NSQIP) at 43 high-volume centers around the United States between November 2011 and December 2012. Institutions with fewer than 10 cases were excluded, leaving 2,694 subjects from 37 centers for the study.
Following this, patients were divided into cohorts of those younger than 80 years of age, and those aged 80 years or older, which contained 2,496 and 198 subjects, respectively. Overall and individual cohorts were split roughly evenly between males and females. Postoperative morbidity and in-hospital mortality rates were measured along with rate of “failure to rescue.”
Results indicated that there were no significant differences in the rates of complications between the cohorts: 41.4% in patients under 80 years and 39.4% in patients aged 80 years or older (P = .58). However, in-hospital mortality rates were significant higher in the 80 and older cohort (3.0%) than in the younger group (1.1%) (P = .01).
Overall, unadjusted complication rates in the 37 centers included in the study varied widely from 25.0% to as high as 72.2%, while failure to rescue rates at ranged from 0.0% to 25.0%.
Major complications were seen in 29.3% of patients aged 80 years or older and in 28.5% of patients under 80 years old (P = .79), with perioperative bleeding being the most prevalent. Among patients with postoperative complications, ascites, chronic obstructive pulmonary disease, and diabetes were the comorbidities most highly associated with failure to rescue, along with acute renal failure, septic shock, and postoperative pulmonary complications.
“It is always true that avoiding complications will decrease mortality for all patients undergoing pancreatectomy,” concluded the investigators, adding that it’s crucial for there to be more interventions to facilitate identification and aggressive treatment of complications to decrease mortality in vulnerable older patients.
“Several factors, such as individual surgeon volume, impact patient outcomes and failure to rescue rates are a significant but not the sole contributor to increased mortality rates in older patients undergoing pancreatectomy,” wrote Dr. Tamirisa and her coauthors.
This study was funded by grants from the Cancer Prevention Research Institute of Texas, UTMB Clinical and Translational Science Award, the National Institutes of Health, and the Agency for Healthcare Research & Quality. Coauthor Dr. Bruce L. Hall disclosed being a paid consulting director of the American College of Surgeons’ National Surgical Quality Improvement Program.
FROM THE ANNALS OF SURGERY
Key clinical point: Significantly higher rates of mortality are experienced in pancreatectomy patients aged 80 years or older, requiring urgent attention toward minimizing postoperative complications.
Major finding: In-hospital mortality rates were significant higher in the cohort aged 80 years and older (3.0%) than in the younger group (1.1%) (P = .01) even though rates of complications between the two groups were relatively similar.
Data source: Retrospective cohort study of 2,694 patients in the American College of Surgeons’ National Surgical Quality Improvement Pancreatectomy Demonstration Project at 37 high-volume U.S. centers.
Disclosures: Study was funded by grants from the Cancer Prevention Research Institute of Texas, UTMB Clinical and Translational Science Award, the National Institutes of Health, and the Agency for Healthcare Research & Quality. Coauthor Dr. Bruce L. Hall disclosed being a paid consulting director of the American College of Surgeons’ National Surgical Quality Improvement Program.
Transfusion linked to bad outcomes in percutaneous peripheral vascular interventions
CHICAGO – Periprocedural blood transfusion rates vary greatly among hospitals performing similar percutaneous interventions for peripheral arterial disease, but these rates can be markedly reduced via a focused quality improvement program.
That’s been the lesson learned in Michigan, where blood transfusion rates dropped by 52% statewide at the 44 hospitals participating in the Blue Cross Blue Shield of Michigan Cardiovascular Consortium Vascular Intervention Collaborative (BMC2 PCI-VIC), Dr. Peter K. Henke reported at the American Heart Association scientific sessions.
That’s good news because periprocedural blood transfusions in patients undergoing percutaneous interventions for peripheral arterial disease (PAD) are associated with startlingly high major morbidity and mortality rates. Indeed, among 18,127 patients undergoing nonhybrid percutaneous interventions for PAD in the BMC2 PCI-VIC registry, periprocedural blood transfusion was an independent predictor of a 25-fold increased risk of MI, a 12.7-fold increase in in-hospital mortality, a 6-fold increased risk of TIA/stroke, and a 49-fold increase in vascular access complications in a logistic regression analysis adjusted for patient demographics, comorbid disease states, and periprocedural medications, according to Dr. Henke, professor of vascular surgery at the University of Michigan, Ann Arbor.
That being said, he was quick to add that he believes these associations largely reflect correlation, not causality. Transfusion recipients were significantly older and sicker than nontransfused patients undergoing the same percutaneous peripheral vascular interventions. They were far more likely to have critical limb ischemia and undergo an urgent or emergent procedure. Of note, as statewide transfusion rates fell from about 6.6% to 3.2% in response to the quality improvement program, crude in-hospital mortality didn’t change significantly, again suggesting a noncausal relationship.
The quality improvement project was undertaken in response to the observation that periprocedural transfusion rates varied institutionally across the state from 0% to 14% for patients undergoing the same percutaneous interventions for PAD. That was a red flag indicating an opportunity for improved practice.
“The median nadir hemoglobin varied within a rather narrow range of 6.8-8.5 g/dL, yet the transfusion rates were quite wide ranging,” the surgeon observed.
Over a 2-year period, the BMC2 PCI-VIC quality improvement team made repeated site visits to the hospitals with the lowest transfusion rates. They performed detailed analysis of peripheral vascular procedure processes, protocols, and order sets in order to identify best practices. Those best practices were then shared at meetings with representatives of all the participating hospitals. Feedback was provided. And transfusion rates began dropping.
Analysis of the 18,000-plus patients enrolled in the registry led to identification of a specific set of risk factors for blood transfusions, most of which occurred after patients had left the catheterization lab. These risk factors included low creatinine clearance, preprocedural anemia, chronic obstructive pulmonary disease, use of warfarin, cerebrovascular disease, critical limb ischemia, and urgent or emergent procedures.
This was the largest-ever study focused on transfusion in patients undergoing endovascular procedures for PAD, according to Dr. Henke. He noted that the results are consistent with a recent report by other investigators regarding the implications of periprocedural blood transfusion in patients undergoing percutaneous coronary intervention. In more than 2.2 million patients who underwent PCI in 2009-2013, transfusion rates varied institutionally from 0% to 13%. Transfusion was associated with 4.6-fold in-hospital mortality, a 3.6-fold increase in acute MI, and a 7.7-fold increased risk of stroke (JAMA 2014;311:836-43).
Dr. Henke reported no financial conflicts of interest regarding the PAD transfusion study, which was funded by Blue Cross Blue Shield of Michigan and the Blue Care Network.
CHICAGO – Periprocedural blood transfusion rates vary greatly among hospitals performing similar percutaneous interventions for peripheral arterial disease, but these rates can be markedly reduced via a focused quality improvement program.
That’s been the lesson learned in Michigan, where blood transfusion rates dropped by 52% statewide at the 44 hospitals participating in the Blue Cross Blue Shield of Michigan Cardiovascular Consortium Vascular Intervention Collaborative (BMC2 PCI-VIC), Dr. Peter K. Henke reported at the American Heart Association scientific sessions.
That’s good news because periprocedural blood transfusions in patients undergoing percutaneous interventions for peripheral arterial disease (PAD) are associated with startlingly high major morbidity and mortality rates. Indeed, among 18,127 patients undergoing nonhybrid percutaneous interventions for PAD in the BMC2 PCI-VIC registry, periprocedural blood transfusion was an independent predictor of a 25-fold increased risk of MI, a 12.7-fold increase in in-hospital mortality, a 6-fold increased risk of TIA/stroke, and a 49-fold increase in vascular access complications in a logistic regression analysis adjusted for patient demographics, comorbid disease states, and periprocedural medications, according to Dr. Henke, professor of vascular surgery at the University of Michigan, Ann Arbor.
That being said, he was quick to add that he believes these associations largely reflect correlation, not causality. Transfusion recipients were significantly older and sicker than nontransfused patients undergoing the same percutaneous peripheral vascular interventions. They were far more likely to have critical limb ischemia and undergo an urgent or emergent procedure. Of note, as statewide transfusion rates fell from about 6.6% to 3.2% in response to the quality improvement program, crude in-hospital mortality didn’t change significantly, again suggesting a noncausal relationship.
The quality improvement project was undertaken in response to the observation that periprocedural transfusion rates varied institutionally across the state from 0% to 14% for patients undergoing the same percutaneous interventions for PAD. That was a red flag indicating an opportunity for improved practice.
“The median nadir hemoglobin varied within a rather narrow range of 6.8-8.5 g/dL, yet the transfusion rates were quite wide ranging,” the surgeon observed.
Over a 2-year period, the BMC2 PCI-VIC quality improvement team made repeated site visits to the hospitals with the lowest transfusion rates. They performed detailed analysis of peripheral vascular procedure processes, protocols, and order sets in order to identify best practices. Those best practices were then shared at meetings with representatives of all the participating hospitals. Feedback was provided. And transfusion rates began dropping.
Analysis of the 18,000-plus patients enrolled in the registry led to identification of a specific set of risk factors for blood transfusions, most of which occurred after patients had left the catheterization lab. These risk factors included low creatinine clearance, preprocedural anemia, chronic obstructive pulmonary disease, use of warfarin, cerebrovascular disease, critical limb ischemia, and urgent or emergent procedures.
This was the largest-ever study focused on transfusion in patients undergoing endovascular procedures for PAD, according to Dr. Henke. He noted that the results are consistent with a recent report by other investigators regarding the implications of periprocedural blood transfusion in patients undergoing percutaneous coronary intervention. In more than 2.2 million patients who underwent PCI in 2009-2013, transfusion rates varied institutionally from 0% to 13%. Transfusion was associated with 4.6-fold in-hospital mortality, a 3.6-fold increase in acute MI, and a 7.7-fold increased risk of stroke (JAMA 2014;311:836-43).
Dr. Henke reported no financial conflicts of interest regarding the PAD transfusion study, which was funded by Blue Cross Blue Shield of Michigan and the Blue Care Network.
CHICAGO – Periprocedural blood transfusion rates vary greatly among hospitals performing similar percutaneous interventions for peripheral arterial disease, but these rates can be markedly reduced via a focused quality improvement program.
That’s been the lesson learned in Michigan, where blood transfusion rates dropped by 52% statewide at the 44 hospitals participating in the Blue Cross Blue Shield of Michigan Cardiovascular Consortium Vascular Intervention Collaborative (BMC2 PCI-VIC), Dr. Peter K. Henke reported at the American Heart Association scientific sessions.
That’s good news because periprocedural blood transfusions in patients undergoing percutaneous interventions for peripheral arterial disease (PAD) are associated with startlingly high major morbidity and mortality rates. Indeed, among 18,127 patients undergoing nonhybrid percutaneous interventions for PAD in the BMC2 PCI-VIC registry, periprocedural blood transfusion was an independent predictor of a 25-fold increased risk of MI, a 12.7-fold increase in in-hospital mortality, a 6-fold increased risk of TIA/stroke, and a 49-fold increase in vascular access complications in a logistic regression analysis adjusted for patient demographics, comorbid disease states, and periprocedural medications, according to Dr. Henke, professor of vascular surgery at the University of Michigan, Ann Arbor.
That being said, he was quick to add that he believes these associations largely reflect correlation, not causality. Transfusion recipients were significantly older and sicker than nontransfused patients undergoing the same percutaneous peripheral vascular interventions. They were far more likely to have critical limb ischemia and undergo an urgent or emergent procedure. Of note, as statewide transfusion rates fell from about 6.6% to 3.2% in response to the quality improvement program, crude in-hospital mortality didn’t change significantly, again suggesting a noncausal relationship.
The quality improvement project was undertaken in response to the observation that periprocedural transfusion rates varied institutionally across the state from 0% to 14% for patients undergoing the same percutaneous interventions for PAD. That was a red flag indicating an opportunity for improved practice.
“The median nadir hemoglobin varied within a rather narrow range of 6.8-8.5 g/dL, yet the transfusion rates were quite wide ranging,” the surgeon observed.
Over a 2-year period, the BMC2 PCI-VIC quality improvement team made repeated site visits to the hospitals with the lowest transfusion rates. They performed detailed analysis of peripheral vascular procedure processes, protocols, and order sets in order to identify best practices. Those best practices were then shared at meetings with representatives of all the participating hospitals. Feedback was provided. And transfusion rates began dropping.
Analysis of the 18,000-plus patients enrolled in the registry led to identification of a specific set of risk factors for blood transfusions, most of which occurred after patients had left the catheterization lab. These risk factors included low creatinine clearance, preprocedural anemia, chronic obstructive pulmonary disease, use of warfarin, cerebrovascular disease, critical limb ischemia, and urgent or emergent procedures.
This was the largest-ever study focused on transfusion in patients undergoing endovascular procedures for PAD, according to Dr. Henke. He noted that the results are consistent with a recent report by other investigators regarding the implications of periprocedural blood transfusion in patients undergoing percutaneous coronary intervention. In more than 2.2 million patients who underwent PCI in 2009-2013, transfusion rates varied institutionally from 0% to 13%. Transfusion was associated with 4.6-fold in-hospital mortality, a 3.6-fold increase in acute MI, and a 7.7-fold increased risk of stroke (JAMA 2014;311:836-43).
Dr. Henke reported no financial conflicts of interest regarding the PAD transfusion study, which was funded by Blue Cross Blue Shield of Michigan and the Blue Care Network.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: High institutional blood transfusion rates in conjunction with percutaneous interventions for peripheral arterial disease can be sharply and safely lowered through a focused quality improvement program.
Major finding: The average periprocedural transfusion rate at 44 Michigan hospitals fell from 6.6% to 3.2% in response to the performance improvement program.
Data source: A retrospective analysis of prospectively gathered data on 18,127 Michigan patients who underwent nonhybrid percutaneous interventions for peripheral arterial disease.
Disclosures: The study was funded by Blue Cross Blue Shield of Michigan and the Blue Care Network. The presenter reported having no financial conflicts.
3D echocardography underpins percutaneous mitral valve repair
VIENNA – Three-dimensional transesophageal echocardiography “may be considered the gatekeeper for assessing the feasibility of and planning the strategy for percutaneous mitral valve repair,” Dr. Giovanni La Canna said at the annual meeting of the European Association of Association of Cardiovascular Imaging.
“Real-time, three-dimensional transesophageal echo is a new way of looking at the mitral valve,” and it supplies a highly accurate and reproducible anatomic view. It adds important additional information when selecting patients for percutaneous mitral valve repair by giving a comprehensive picture of annular dimensions and shape, intercommissural extension of target-leaflet lesions, and the extent of calcification on the annulus and leaflets, said Dr. La Canna, an echocardiographer at San Raffaele Hospital in Milan.
Three-dimensional echo aids both forms of percutaneous mitral valve repair: annuloplasty and clipping with the MitraClip system.
When performing mitral-leaflet clipping, use of 3D echo adds incremental information beyond 2D echo that aids in the selection of the site for transseptal puncture; facilitates device alignment; optimizes grasping of the leaflet with the clip; and helps in assessment of mitral-valve area and residual regurgitation, the need for additional clips, and any residual defect in the interatrial septum. For especially challenging cases, data from 2D echo can be integrated with the 3D data for the most complete imaging guidance, Dr. La Canna said.
Despite its value, 3D echo still has limitations. Resolution is currently low, parts of the imaging can “drop out” or contain artifacts, the catheter can produce an image shadow, and the image can decay during the course of the procedure, he said.
Dr. La Canna has been a consultant to Abbott Vascular, which markets the MitraClip.
On Twitter @mitchelzoler
VIENNA – Three-dimensional transesophageal echocardiography “may be considered the gatekeeper for assessing the feasibility of and planning the strategy for percutaneous mitral valve repair,” Dr. Giovanni La Canna said at the annual meeting of the European Association of Association of Cardiovascular Imaging.
“Real-time, three-dimensional transesophageal echo is a new way of looking at the mitral valve,” and it supplies a highly accurate and reproducible anatomic view. It adds important additional information when selecting patients for percutaneous mitral valve repair by giving a comprehensive picture of annular dimensions and shape, intercommissural extension of target-leaflet lesions, and the extent of calcification on the annulus and leaflets, said Dr. La Canna, an echocardiographer at San Raffaele Hospital in Milan.
Three-dimensional echo aids both forms of percutaneous mitral valve repair: annuloplasty and clipping with the MitraClip system.
When performing mitral-leaflet clipping, use of 3D echo adds incremental information beyond 2D echo that aids in the selection of the site for transseptal puncture; facilitates device alignment; optimizes grasping of the leaflet with the clip; and helps in assessment of mitral-valve area and residual regurgitation, the need for additional clips, and any residual defect in the interatrial septum. For especially challenging cases, data from 2D echo can be integrated with the 3D data for the most complete imaging guidance, Dr. La Canna said.
Despite its value, 3D echo still has limitations. Resolution is currently low, parts of the imaging can “drop out” or contain artifacts, the catheter can produce an image shadow, and the image can decay during the course of the procedure, he said.
Dr. La Canna has been a consultant to Abbott Vascular, which markets the MitraClip.
On Twitter @mitchelzoler
VIENNA – Three-dimensional transesophageal echocardiography “may be considered the gatekeeper for assessing the feasibility of and planning the strategy for percutaneous mitral valve repair,” Dr. Giovanni La Canna said at the annual meeting of the European Association of Association of Cardiovascular Imaging.
“Real-time, three-dimensional transesophageal echo is a new way of looking at the mitral valve,” and it supplies a highly accurate and reproducible anatomic view. It adds important additional information when selecting patients for percutaneous mitral valve repair by giving a comprehensive picture of annular dimensions and shape, intercommissural extension of target-leaflet lesions, and the extent of calcification on the annulus and leaflets, said Dr. La Canna, an echocardiographer at San Raffaele Hospital in Milan.
Three-dimensional echo aids both forms of percutaneous mitral valve repair: annuloplasty and clipping with the MitraClip system.
When performing mitral-leaflet clipping, use of 3D echo adds incremental information beyond 2D echo that aids in the selection of the site for transseptal puncture; facilitates device alignment; optimizes grasping of the leaflet with the clip; and helps in assessment of mitral-valve area and residual regurgitation, the need for additional clips, and any residual defect in the interatrial septum. For especially challenging cases, data from 2D echo can be integrated with the 3D data for the most complete imaging guidance, Dr. La Canna said.
Despite its value, 3D echo still has limitations. Resolution is currently low, parts of the imaging can “drop out” or contain artifacts, the catheter can produce an image shadow, and the image can decay during the course of the procedure, he said.
Dr. La Canna has been a consultant to Abbott Vascular, which markets the MitraClip.
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM EUROECHO-IMAGING 2014
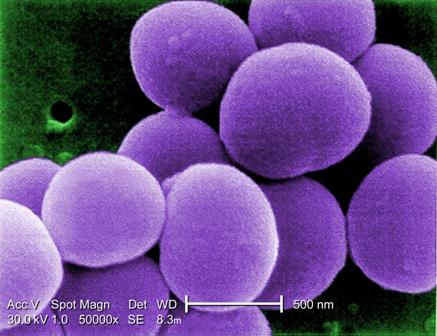
Bundled intervention tackles S. aureus SSIs
PHILADELPHIA – A bundled intervention including Staphylococcus aureus screening, decolonization, and targeted perioperative prophylaxis significantly decreased the rate of complex S. aureus surgical site infections in a multicenter quasi-experimental effectiveness study of patients undergoing cardiac operations or total joint arthroplasty.
The pooled rate of complex S. aureus surgical site infections (SSIs) decreased from 0.36% following 28,218 procedures performed during the preintervention period to 0.20% after 14,316 procedures performed during the intervention period (rate ratio, 0.58), Dr. Loreen A. Herwaldt of the University of Iowa, Iowa City, reported at an annual scientific meeting on infectious diseases.
Further, the number of months with no complex S. aureus SSIs increased from 2 of 39 months (5.1%) to 8 of 22 months (36.4%) Dr. Herwaldt said, noting that the median rate and range of complex SSIs became zero by intervention month 4.
The decrease in SSIs was greatest for joint arthroplasties, she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Subgroup analyses also demonstrated significantly lower rates of complex SSIs for scheduled vs. nonscheduled or emergent operations (rate ratio, 0.55), fully adherent vs. partially or nonadherent operations (rate ratio, 0.26), and for operations in which the surgeon (in accordance with hospital participation) implemented at least some bundle elements vs. no bundle elements (rate ratio, 0.54), she said, explaining that surgeons could opt out of the study even if a hospital was participating.
The rate of complex SSIs caused by any pathogen also was reduced (rate ratio, 0.67).
“We were very pleased to note that gram negative SSIs did not increase. The rate ratio was 0.86, and the confidence interval did cross 1 and the P value was 0.67,” she said.
The study, known as STOP SSI, was conducted at 20 Hospital Corporation of America (HCA) hospitals in nine states from March 1, 2009, to March 31, 2014. Patients who tested positive for methicillin-resistant or methicillin-susceptible S. aureus on a preoperative nares screen within 30 days before surgery were asked to apply mupirocin intranasally twice daily for 5 days and to bathe with chlorhexidine gluconate once daily for 5 days prior to their operation, including on the night before and the morning of surgery. Those who tested negative for MRSA and MSSA bathed with chlorhexidine gluconate only on the night before surgery and the morning of surgery.
Those with MRSA were treated with vancomycin and cefazolin perioperatively, and those without MRSA received only cefazolin.
If the patient’s status was unknown at the time of the operation, the goal was to have the patient bathe in chlorhexidine and to give as many intranasal doses of mupirocin as possible before surgery. The patient was treated perioperatively with vancomycin and cefazolin, and if it was later determined that the patient was positive for MRSA, the mupirocin was continued after surgery until the patient had been treated for 5 days.
After a 3-month phase-in period, 48% of the hospitals were fully compliant with this protocol, and 20% were partially compliant.
The use of a bundled intervention similar to the one used in this study was shown in a recent meta-analysis (BMJ 2013;346:f2743) to be likely to reduce the rate of S. aureus SSIs, but the approach had not been studied in a multicenter trial, Dr. Herwaldt said.
“Implementation of this SSI bundle was associated with significantly lower rates of complex S. aureus SSIs in the total cohort and in the hip and knee arthroplasty group. It was not associated with an increase in gram-negative SSIs, and thus we feel that if people actually did implement this bundle, it could substantially reduce patient morbidity and the cost of care,” she concluded, noting that the effect was seen only with implementation of the full bundle.
The Agency for Healthcare Research and Quality funded the study. Dr. Herwaldt reported having no disclosures.
PHILADELPHIA – A bundled intervention including Staphylococcus aureus screening, decolonization, and targeted perioperative prophylaxis significantly decreased the rate of complex S. aureus surgical site infections in a multicenter quasi-experimental effectiveness study of patients undergoing cardiac operations or total joint arthroplasty.
The pooled rate of complex S. aureus surgical site infections (SSIs) decreased from 0.36% following 28,218 procedures performed during the preintervention period to 0.20% after 14,316 procedures performed during the intervention period (rate ratio, 0.58), Dr. Loreen A. Herwaldt of the University of Iowa, Iowa City, reported at an annual scientific meeting on infectious diseases.
Further, the number of months with no complex S. aureus SSIs increased from 2 of 39 months (5.1%) to 8 of 22 months (36.4%) Dr. Herwaldt said, noting that the median rate and range of complex SSIs became zero by intervention month 4.
The decrease in SSIs was greatest for joint arthroplasties, she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Subgroup analyses also demonstrated significantly lower rates of complex SSIs for scheduled vs. nonscheduled or emergent operations (rate ratio, 0.55), fully adherent vs. partially or nonadherent operations (rate ratio, 0.26), and for operations in which the surgeon (in accordance with hospital participation) implemented at least some bundle elements vs. no bundle elements (rate ratio, 0.54), she said, explaining that surgeons could opt out of the study even if a hospital was participating.
The rate of complex SSIs caused by any pathogen also was reduced (rate ratio, 0.67).
“We were very pleased to note that gram negative SSIs did not increase. The rate ratio was 0.86, and the confidence interval did cross 1 and the P value was 0.67,” she said.
The study, known as STOP SSI, was conducted at 20 Hospital Corporation of America (HCA) hospitals in nine states from March 1, 2009, to March 31, 2014. Patients who tested positive for methicillin-resistant or methicillin-susceptible S. aureus on a preoperative nares screen within 30 days before surgery were asked to apply mupirocin intranasally twice daily for 5 days and to bathe with chlorhexidine gluconate once daily for 5 days prior to their operation, including on the night before and the morning of surgery. Those who tested negative for MRSA and MSSA bathed with chlorhexidine gluconate only on the night before surgery and the morning of surgery.
Those with MRSA were treated with vancomycin and cefazolin perioperatively, and those without MRSA received only cefazolin.
If the patient’s status was unknown at the time of the operation, the goal was to have the patient bathe in chlorhexidine and to give as many intranasal doses of mupirocin as possible before surgery. The patient was treated perioperatively with vancomycin and cefazolin, and if it was later determined that the patient was positive for MRSA, the mupirocin was continued after surgery until the patient had been treated for 5 days.
After a 3-month phase-in period, 48% of the hospitals were fully compliant with this protocol, and 20% were partially compliant.
The use of a bundled intervention similar to the one used in this study was shown in a recent meta-analysis (BMJ 2013;346:f2743) to be likely to reduce the rate of S. aureus SSIs, but the approach had not been studied in a multicenter trial, Dr. Herwaldt said.
“Implementation of this SSI bundle was associated with significantly lower rates of complex S. aureus SSIs in the total cohort and in the hip and knee arthroplasty group. It was not associated with an increase in gram-negative SSIs, and thus we feel that if people actually did implement this bundle, it could substantially reduce patient morbidity and the cost of care,” she concluded, noting that the effect was seen only with implementation of the full bundle.
The Agency for Healthcare Research and Quality funded the study. Dr. Herwaldt reported having no disclosures.
PHILADELPHIA – A bundled intervention including Staphylococcus aureus screening, decolonization, and targeted perioperative prophylaxis significantly decreased the rate of complex S. aureus surgical site infections in a multicenter quasi-experimental effectiveness study of patients undergoing cardiac operations or total joint arthroplasty.
The pooled rate of complex S. aureus surgical site infections (SSIs) decreased from 0.36% following 28,218 procedures performed during the preintervention period to 0.20% after 14,316 procedures performed during the intervention period (rate ratio, 0.58), Dr. Loreen A. Herwaldt of the University of Iowa, Iowa City, reported at an annual scientific meeting on infectious diseases.
Further, the number of months with no complex S. aureus SSIs increased from 2 of 39 months (5.1%) to 8 of 22 months (36.4%) Dr. Herwaldt said, noting that the median rate and range of complex SSIs became zero by intervention month 4.
The decrease in SSIs was greatest for joint arthroplasties, she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Subgroup analyses also demonstrated significantly lower rates of complex SSIs for scheduled vs. nonscheduled or emergent operations (rate ratio, 0.55), fully adherent vs. partially or nonadherent operations (rate ratio, 0.26), and for operations in which the surgeon (in accordance with hospital participation) implemented at least some bundle elements vs. no bundle elements (rate ratio, 0.54), she said, explaining that surgeons could opt out of the study even if a hospital was participating.
The rate of complex SSIs caused by any pathogen also was reduced (rate ratio, 0.67).
“We were very pleased to note that gram negative SSIs did not increase. The rate ratio was 0.86, and the confidence interval did cross 1 and the P value was 0.67,” she said.
The study, known as STOP SSI, was conducted at 20 Hospital Corporation of America (HCA) hospitals in nine states from March 1, 2009, to March 31, 2014. Patients who tested positive for methicillin-resistant or methicillin-susceptible S. aureus on a preoperative nares screen within 30 days before surgery were asked to apply mupirocin intranasally twice daily for 5 days and to bathe with chlorhexidine gluconate once daily for 5 days prior to their operation, including on the night before and the morning of surgery. Those who tested negative for MRSA and MSSA bathed with chlorhexidine gluconate only on the night before surgery and the morning of surgery.
Those with MRSA were treated with vancomycin and cefazolin perioperatively, and those without MRSA received only cefazolin.
If the patient’s status was unknown at the time of the operation, the goal was to have the patient bathe in chlorhexidine and to give as many intranasal doses of mupirocin as possible before surgery. The patient was treated perioperatively with vancomycin and cefazolin, and if it was later determined that the patient was positive for MRSA, the mupirocin was continued after surgery until the patient had been treated for 5 days.
After a 3-month phase-in period, 48% of the hospitals were fully compliant with this protocol, and 20% were partially compliant.
The use of a bundled intervention similar to the one used in this study was shown in a recent meta-analysis (BMJ 2013;346:f2743) to be likely to reduce the rate of S. aureus SSIs, but the approach had not been studied in a multicenter trial, Dr. Herwaldt said.
“Implementation of this SSI bundle was associated with significantly lower rates of complex S. aureus SSIs in the total cohort and in the hip and knee arthroplasty group. It was not associated with an increase in gram-negative SSIs, and thus we feel that if people actually did implement this bundle, it could substantially reduce patient morbidity and the cost of care,” she concluded, noting that the effect was seen only with implementation of the full bundle.
The Agency for Healthcare Research and Quality funded the study. Dr. Herwaldt reported having no disclosures.
AT IDWEEK 2014
Key clinical point: Implementing a bundled intervention reduced S. aureus SSIs and could reduce patient morbidity and costs.
Major finding: The pooled S. aureus SSI rate decreased from 0.36% to 0.20% (rate ratio, 0.58).
Data source: A multicenter quasi-experimental effectiveness study of 42,534 procedures.
Disclosures: The Agency for Healthcare Research and Quality funded the study. Dr. Herwaldt reported having no disclosures.
VTE risk models target a formidable surgery foe
CHICAGO – Implementation of preoperative venous thromboembolism prophylaxis requires a highly individualized approach and a little boost from information technology, one expert suggested.
“What may not be appreciated by some vascular surgeons is that for certain procedures we do, our patients actually have a high VTE [venous thromboembolism] risk. I know people think, ‘We use heparin, so our patients aren’t at high risk,’ but they actually are,” Dr. Melina Kibbe said at a symposium on vascular surgery sponsored by Northwestern University.
The VTE risk is 4.2% for open thoracoabdominal aortic aneurysm repair and 2.2% for thoracic endovascular aortic repair in the American College of Surgeons National Surgical Quality Improvement Program database. That may be an underestimation, however, because the NSQIP database captures only symptomatic events documented by imaging and those events occurring in the first 30 days after surgery.
Smaller studies looking at the problem prospectively suggest the VTE risk is closer to 2%-12% after open aortic surgery and 5.3% after endovascular aortic repair, she said.
Add to that the U.S. Surgeon General’s 2008 call to action to prevent VTE and the Institute of Medicine’s stance that failure to provide VTE prophylaxis qualifies as a medical error, and it would be tempting for vascular surgeons to prescribe pharmacologic prophylaxis for all of their patients, or at least do so based on the type of procedure.
“But VTE formation is really secondary to patient-specific and procedure-related factors,” said Dr. Kibbe, a professor of vascular surgery at Northwestern University in Chicago.
She highlighted five current VTE risk assessment models (RAMs) and the potential returns when RAMs are incorporated into clinical decision support systems.
• Kucher model. One of the earlier and most straightforward RAMs is the Kucher model. It assessed eight weighted risk factors (advanced age, obesity, bed rest, hormone replacement therapy/oral contraceptives, major surgery, cancer, prior VTE, and hypercoagulability) and provided surgeons with electronic alerts regarding prophylaxis.
VTE rates dropped from 8.2% to 4.9% in the high-risk category (score ≥ 4) with the use of the simple physician reminders (N. Engl. J. Med. 2005;352:969-77). Prospective validation showed that VTE increased proportionally with higher scores, Dr. Kibbe said. On the other hand, the model lacked sensitivity at low VTE risk, because 20% of patients with a score of 4 or less actually had VTEs.
“So, while it was simple, it only works well for the high-risk category,” she said.
• Rogers model. One of the most vigorously studied and developed RAMs is the Rogers model (J. Am. Coll. Surg. 2007;204:1211-21). It identified 15 variables (including lab values, patient characteristics, disease states, work relative-value unit, and type of operation) that were independently associated with VTE formation among 183,609 patients undergoing general, vascular, or thoracic procedures at 142 Veterans Health Administration and private hospitals. Each variable is assigned a value from 0 to 9 and added together to create a Rogers score.
Validation showed that VTE risk correlates with the Rogers score, rising from 0.11% for patients with a low score (< 7) to 1.32% for those with a high score (> 10), Dr. Kibbe said. Criticisms of the model are that it is complex, VTE incidence in the entire cohort was low at just 0.63%, the type of VTE prophylaxis used was unclear, and the model lacks prospective validation in a vascular surgery cohort.
• Caprini model. The most commonly used RAM is the 2005 Caprini model (Dis. Mon. 2005;51:70-8), which assigns a weighted score based on more than 30 VTE risk factors compiled by the authors. It has been prospectively validated in numerous studies and shown to accurately stratify 30-day VTE risk at 0.5% for patients at very low risk, 1.5% for low risk, 3% for moderate risk, and 6% for high risk.
The Caprini model, however, was not developed with the same rigor as the Rogers RAM, some of the risk factors have been shown not to be a risk for VTE, and it is complex, Dr. Kibbe observed.
• Pannucci model. The Pannucci model was created specifically to counteract the complexity of the Rogers and Caprini RAMs and incorporates only seven risk factors (personal history of VTE, current cancer, age ≥ 60 years, body mass index ≥ 40 kg/m2, male sex, sepsis/septic shock/systemic inflammatory response syndrome, and family history of VTE) into a weighted index for 90-day VTE risk (Chest 2014;145:567-73). The model was developed using a statewide database and a derivation cohort made up of 20% vascular surgery patients.
Both the derivation and validation cohorts identified an 18-fold variation in VTE risk from the lowest- to highest-risk surgical population, showing that the model stratifies patients correctly. Further prospective validation is needed, Dr. Kibbe said.
• Scarborough model. Finally, in an attempt to develop a RAM specific to vascular surgery patients, Dr. John Scarborough and colleagues examined 6,035 patients undergoing open AAA repair in the NSQIP database. The 30-day VTE rate was 2.4% for the entire cohort. Eight independent perioperative risk factors were identified and used to create a nonweighted scoring system (J. Am. Coll. Surg. 2012;214:620-6).
Overall, 65% of patients had 0-1 risk factor and a VTE incidence of 1.5%, while 15% had 3 or more risk factors and a VTE incidence of 6.1%. The Scarborough model has good risk stratification, Dr. Kibbe said, but it is limited by the aforementioned criticisms regarding the NSQIP database, and it also needs prospective validation.
“We all know that proper VTE prophylaxis is very important for our patients; but we need mechanisms by which the attention given to this need for prophylaxis, which is a lot, is turned into proper implementation,” she said.
For Dr. Kibbe and her colleagues, proper implementation meant developing a RAM that was incorporated into the electronic medical record system for all surgical patients at the Jesse Brown VA Medical Center in Chicago. Clinicians were prompted to complete the RAM upon placing orders for preanesthesia testing clearance, and the clinical decision support system would provide a recommended prophylaxis regimen and easily selected electronic orders that could be signed.
A pre- and postimplementation analysis involving 400 consecutive patients revealed an 82% increase in patients with preoperative VTE prophylaxis ordered (22% vs. 40%), a 75% decrease in inappropriate cancellation of orders more than 12 hours before surgery (37% vs. 9%), and a nearly sevenfold increase in the number of patients receiving pharmacologic and mechanical prophylaxis (5% vs. 32%), she said. There was an 80% and 36% decline in DVT rates at 30 and 90 days postoperative, but event rates were too low to detect a significant difference (J. Vasc. Surg. 2010;51:648-54).
Dr. Kibbe reported having no financial disclosures.
CHICAGO – Implementation of preoperative venous thromboembolism prophylaxis requires a highly individualized approach and a little boost from information technology, one expert suggested.
“What may not be appreciated by some vascular surgeons is that for certain procedures we do, our patients actually have a high VTE [venous thromboembolism] risk. I know people think, ‘We use heparin, so our patients aren’t at high risk,’ but they actually are,” Dr. Melina Kibbe said at a symposium on vascular surgery sponsored by Northwestern University.
The VTE risk is 4.2% for open thoracoabdominal aortic aneurysm repair and 2.2% for thoracic endovascular aortic repair in the American College of Surgeons National Surgical Quality Improvement Program database. That may be an underestimation, however, because the NSQIP database captures only symptomatic events documented by imaging and those events occurring in the first 30 days after surgery.
Smaller studies looking at the problem prospectively suggest the VTE risk is closer to 2%-12% after open aortic surgery and 5.3% after endovascular aortic repair, she said.
Add to that the U.S. Surgeon General’s 2008 call to action to prevent VTE and the Institute of Medicine’s stance that failure to provide VTE prophylaxis qualifies as a medical error, and it would be tempting for vascular surgeons to prescribe pharmacologic prophylaxis for all of their patients, or at least do so based on the type of procedure.
“But VTE formation is really secondary to patient-specific and procedure-related factors,” said Dr. Kibbe, a professor of vascular surgery at Northwestern University in Chicago.
She highlighted five current VTE risk assessment models (RAMs) and the potential returns when RAMs are incorporated into clinical decision support systems.
• Kucher model. One of the earlier and most straightforward RAMs is the Kucher model. It assessed eight weighted risk factors (advanced age, obesity, bed rest, hormone replacement therapy/oral contraceptives, major surgery, cancer, prior VTE, and hypercoagulability) and provided surgeons with electronic alerts regarding prophylaxis.
VTE rates dropped from 8.2% to 4.9% in the high-risk category (score ≥ 4) with the use of the simple physician reminders (N. Engl. J. Med. 2005;352:969-77). Prospective validation showed that VTE increased proportionally with higher scores, Dr. Kibbe said. On the other hand, the model lacked sensitivity at low VTE risk, because 20% of patients with a score of 4 or less actually had VTEs.
“So, while it was simple, it only works well for the high-risk category,” she said.
• Rogers model. One of the most vigorously studied and developed RAMs is the Rogers model (J. Am. Coll. Surg. 2007;204:1211-21). It identified 15 variables (including lab values, patient characteristics, disease states, work relative-value unit, and type of operation) that were independently associated with VTE formation among 183,609 patients undergoing general, vascular, or thoracic procedures at 142 Veterans Health Administration and private hospitals. Each variable is assigned a value from 0 to 9 and added together to create a Rogers score.
Validation showed that VTE risk correlates with the Rogers score, rising from 0.11% for patients with a low score (< 7) to 1.32% for those with a high score (> 10), Dr. Kibbe said. Criticisms of the model are that it is complex, VTE incidence in the entire cohort was low at just 0.63%, the type of VTE prophylaxis used was unclear, and the model lacks prospective validation in a vascular surgery cohort.
• Caprini model. The most commonly used RAM is the 2005 Caprini model (Dis. Mon. 2005;51:70-8), which assigns a weighted score based on more than 30 VTE risk factors compiled by the authors. It has been prospectively validated in numerous studies and shown to accurately stratify 30-day VTE risk at 0.5% for patients at very low risk, 1.5% for low risk, 3% for moderate risk, and 6% for high risk.
The Caprini model, however, was not developed with the same rigor as the Rogers RAM, some of the risk factors have been shown not to be a risk for VTE, and it is complex, Dr. Kibbe observed.
• Pannucci model. The Pannucci model was created specifically to counteract the complexity of the Rogers and Caprini RAMs and incorporates only seven risk factors (personal history of VTE, current cancer, age ≥ 60 years, body mass index ≥ 40 kg/m2, male sex, sepsis/septic shock/systemic inflammatory response syndrome, and family history of VTE) into a weighted index for 90-day VTE risk (Chest 2014;145:567-73). The model was developed using a statewide database and a derivation cohort made up of 20% vascular surgery patients.
Both the derivation and validation cohorts identified an 18-fold variation in VTE risk from the lowest- to highest-risk surgical population, showing that the model stratifies patients correctly. Further prospective validation is needed, Dr. Kibbe said.
• Scarborough model. Finally, in an attempt to develop a RAM specific to vascular surgery patients, Dr. John Scarborough and colleagues examined 6,035 patients undergoing open AAA repair in the NSQIP database. The 30-day VTE rate was 2.4% for the entire cohort. Eight independent perioperative risk factors were identified and used to create a nonweighted scoring system (J. Am. Coll. Surg. 2012;214:620-6).
Overall, 65% of patients had 0-1 risk factor and a VTE incidence of 1.5%, while 15% had 3 or more risk factors and a VTE incidence of 6.1%. The Scarborough model has good risk stratification, Dr. Kibbe said, but it is limited by the aforementioned criticisms regarding the NSQIP database, and it also needs prospective validation.
“We all know that proper VTE prophylaxis is very important for our patients; but we need mechanisms by which the attention given to this need for prophylaxis, which is a lot, is turned into proper implementation,” she said.
For Dr. Kibbe and her colleagues, proper implementation meant developing a RAM that was incorporated into the electronic medical record system for all surgical patients at the Jesse Brown VA Medical Center in Chicago. Clinicians were prompted to complete the RAM upon placing orders for preanesthesia testing clearance, and the clinical decision support system would provide a recommended prophylaxis regimen and easily selected electronic orders that could be signed.
A pre- and postimplementation analysis involving 400 consecutive patients revealed an 82% increase in patients with preoperative VTE prophylaxis ordered (22% vs. 40%), a 75% decrease in inappropriate cancellation of orders more than 12 hours before surgery (37% vs. 9%), and a nearly sevenfold increase in the number of patients receiving pharmacologic and mechanical prophylaxis (5% vs. 32%), she said. There was an 80% and 36% decline in DVT rates at 30 and 90 days postoperative, but event rates were too low to detect a significant difference (J. Vasc. Surg. 2010;51:648-54).
Dr. Kibbe reported having no financial disclosures.
CHICAGO – Implementation of preoperative venous thromboembolism prophylaxis requires a highly individualized approach and a little boost from information technology, one expert suggested.
“What may not be appreciated by some vascular surgeons is that for certain procedures we do, our patients actually have a high VTE [venous thromboembolism] risk. I know people think, ‘We use heparin, so our patients aren’t at high risk,’ but they actually are,” Dr. Melina Kibbe said at a symposium on vascular surgery sponsored by Northwestern University.
The VTE risk is 4.2% for open thoracoabdominal aortic aneurysm repair and 2.2% for thoracic endovascular aortic repair in the American College of Surgeons National Surgical Quality Improvement Program database. That may be an underestimation, however, because the NSQIP database captures only symptomatic events documented by imaging and those events occurring in the first 30 days after surgery.
Smaller studies looking at the problem prospectively suggest the VTE risk is closer to 2%-12% after open aortic surgery and 5.3% after endovascular aortic repair, she said.
Add to that the U.S. Surgeon General’s 2008 call to action to prevent VTE and the Institute of Medicine’s stance that failure to provide VTE prophylaxis qualifies as a medical error, and it would be tempting for vascular surgeons to prescribe pharmacologic prophylaxis for all of their patients, or at least do so based on the type of procedure.
“But VTE formation is really secondary to patient-specific and procedure-related factors,” said Dr. Kibbe, a professor of vascular surgery at Northwestern University in Chicago.
She highlighted five current VTE risk assessment models (RAMs) and the potential returns when RAMs are incorporated into clinical decision support systems.
• Kucher model. One of the earlier and most straightforward RAMs is the Kucher model. It assessed eight weighted risk factors (advanced age, obesity, bed rest, hormone replacement therapy/oral contraceptives, major surgery, cancer, prior VTE, and hypercoagulability) and provided surgeons with electronic alerts regarding prophylaxis.
VTE rates dropped from 8.2% to 4.9% in the high-risk category (score ≥ 4) with the use of the simple physician reminders (N. Engl. J. Med. 2005;352:969-77). Prospective validation showed that VTE increased proportionally with higher scores, Dr. Kibbe said. On the other hand, the model lacked sensitivity at low VTE risk, because 20% of patients with a score of 4 or less actually had VTEs.
“So, while it was simple, it only works well for the high-risk category,” she said.
• Rogers model. One of the most vigorously studied and developed RAMs is the Rogers model (J. Am. Coll. Surg. 2007;204:1211-21). It identified 15 variables (including lab values, patient characteristics, disease states, work relative-value unit, and type of operation) that were independently associated with VTE formation among 183,609 patients undergoing general, vascular, or thoracic procedures at 142 Veterans Health Administration and private hospitals. Each variable is assigned a value from 0 to 9 and added together to create a Rogers score.
Validation showed that VTE risk correlates with the Rogers score, rising from 0.11% for patients with a low score (< 7) to 1.32% for those with a high score (> 10), Dr. Kibbe said. Criticisms of the model are that it is complex, VTE incidence in the entire cohort was low at just 0.63%, the type of VTE prophylaxis used was unclear, and the model lacks prospective validation in a vascular surgery cohort.
• Caprini model. The most commonly used RAM is the 2005 Caprini model (Dis. Mon. 2005;51:70-8), which assigns a weighted score based on more than 30 VTE risk factors compiled by the authors. It has been prospectively validated in numerous studies and shown to accurately stratify 30-day VTE risk at 0.5% for patients at very low risk, 1.5% for low risk, 3% for moderate risk, and 6% for high risk.
The Caprini model, however, was not developed with the same rigor as the Rogers RAM, some of the risk factors have been shown not to be a risk for VTE, and it is complex, Dr. Kibbe observed.
• Pannucci model. The Pannucci model was created specifically to counteract the complexity of the Rogers and Caprini RAMs and incorporates only seven risk factors (personal history of VTE, current cancer, age ≥ 60 years, body mass index ≥ 40 kg/m2, male sex, sepsis/septic shock/systemic inflammatory response syndrome, and family history of VTE) into a weighted index for 90-day VTE risk (Chest 2014;145:567-73). The model was developed using a statewide database and a derivation cohort made up of 20% vascular surgery patients.
Both the derivation and validation cohorts identified an 18-fold variation in VTE risk from the lowest- to highest-risk surgical population, showing that the model stratifies patients correctly. Further prospective validation is needed, Dr. Kibbe said.
• Scarborough model. Finally, in an attempt to develop a RAM specific to vascular surgery patients, Dr. John Scarborough and colleagues examined 6,035 patients undergoing open AAA repair in the NSQIP database. The 30-day VTE rate was 2.4% for the entire cohort. Eight independent perioperative risk factors were identified and used to create a nonweighted scoring system (J. Am. Coll. Surg. 2012;214:620-6).
Overall, 65% of patients had 0-1 risk factor and a VTE incidence of 1.5%, while 15% had 3 or more risk factors and a VTE incidence of 6.1%. The Scarborough model has good risk stratification, Dr. Kibbe said, but it is limited by the aforementioned criticisms regarding the NSQIP database, and it also needs prospective validation.
“We all know that proper VTE prophylaxis is very important for our patients; but we need mechanisms by which the attention given to this need for prophylaxis, which is a lot, is turned into proper implementation,” she said.
For Dr. Kibbe and her colleagues, proper implementation meant developing a RAM that was incorporated into the electronic medical record system for all surgical patients at the Jesse Brown VA Medical Center in Chicago. Clinicians were prompted to complete the RAM upon placing orders for preanesthesia testing clearance, and the clinical decision support system would provide a recommended prophylaxis regimen and easily selected electronic orders that could be signed.
A pre- and postimplementation analysis involving 400 consecutive patients revealed an 82% increase in patients with preoperative VTE prophylaxis ordered (22% vs. 40%), a 75% decrease in inappropriate cancellation of orders more than 12 hours before surgery (37% vs. 9%), and a nearly sevenfold increase in the number of patients receiving pharmacologic and mechanical prophylaxis (5% vs. 32%), she said. There was an 80% and 36% decline in DVT rates at 30 and 90 days postoperative, but event rates were too low to detect a significant difference (J. Vasc. Surg. 2010;51:648-54).
Dr. Kibbe reported having no financial disclosures.
AT THE NORTHWESTERN VASCULAR SYMPOSIUM
Sofosbuvir and ribavirin critical to preventing posttransplantation HCV recurrence
Sofosbuvir and ribavirin treatments should be administered to patients with hepatitis C virus who undergo liver transplantations in order to significantly decrease the risks of posttransplant HCV recurrence, according to two new studies published in the January issue of Gastroenterology (10.1053/j.gastro.2014.09.023 and 10.1053/j.gastro.2014.10.001).
“In clinical trials, administration of sofosbuvir with ribavirin was associated with rapid decreases of HCV RNA to undetectable levels in patients with HCV genotype 1, 2, 3, 4, and 6 infections,” wrote lead author Dr. Michael P. Curry of the Beth Israel Deaconess Medical Center in Boston, and his coauthors on the first of these two studies. “In more than 3,000 patients treated to date, sofosbuvir has been shown to be safe, viral breakthrough during treatment has been rare (and associated with nonadherence), and few drug interactions have been observed.”
In a phase II, open-label study, Dr. Curry and his coinvestigators enrolled 61 patients with HCV of any genotype, and cirrhosis with a Child-Turcotte-Pugh score no greater than 7, who were all wait-listed to receive liver transplantations. Subjects received up to 48 weeks of treatment with 400 mg of sofosbuvir, and a separate dose of ribavirin prior to liver transplantation, while 43 patients received transplantations alone. The primary outcome sought by investigators was HCV-RNA levels less than 25 IU/mL at 12 weeks after transplantation among patients that had this level prior to the operation.
The investigators found that 43 subjects had the desired HCV-RNA levels; of that population, 49% had a posttransplantation virologic response, with the most frequent side effects reported by subjects being fatigue (38%), headache (23%), and anemia (21%). Of the 43 applicable subjects, 30 (70% of the population) had a posttransplantation virologic response at 12 weeks, 10 (23%) had recurrent infection, and 3 (7%) died.
“This study provides proof of concept that virologic suppression without interferon significantly can reduce the rate of recurrent HCV after liver transplantation,” the study says, adding that the results “compare favorably with those observed in other trials of pretransplantation antiviral therapy.”
In the second study, the authors ascertained that combination therapy consisting of sofosbuvir and ribavirin for 24 weeks is effective at preventing hepatitis C virus recurrence in patients who undergo liver transplantations.
“Recurrent HCV infection is the most common cause of mortality and graft loss following transplantation, and up to 30% of patients with recurrent infection develop cirrhosis within 5 years,” wrote the study’s authors, led by Dr. Michael Charlton of the Mayo Clinic in Rochester, Minn.
Using a prospective, multicenter, open-label pilot study, investigators enrolled and treated 40 patients with a 24-week regimen of 400 mg sofosbuvir and ribavirin starting at 400 mg, which was subsequently adjusted per patient based on individual creatinine clearance and hemoglobin levels. Subjects were 78% male and 85% white, with 83% having HCV genotype 1, 40% having cirrhosis, and 88% having been previously treated with interferon. The primary outcome investigators looked for was “sustained virologic response 12 weeks after treatment (SVR12).”
Data showed that SVR12 was achieved by 28 of the 40 subjects that received treatment, or 70%. The most commonly reported adverse effects were fatigue (30%), diarrhea (28%), headache (25%), and anemia (20%). No patients exhibited detectable viral resistance during or after treatment, and although two patients terminated their treatment because of adverse events, investigators reported no deaths, graft losses, or episodes of rejection.
“In contrast,” Dr. Charlton and his coauthors noted, “interferon-based treatments have been associated with posttreatment immunological dysfunction (particularly plasma cell hepatitis) and even hepatic decompensation in LT [liver transplant] recipients.”
The authors of the first study disclosed that Dr. Curry has received grants from and been affiliated with Gilead, which was a sponsor of the study. The authors of the second study reported no relevant financial disclosures.
Sofosbuvir and ribavirin treatments should be administered to patients with hepatitis C virus who undergo liver transplantations in order to significantly decrease the risks of posttransplant HCV recurrence, according to two new studies published in the January issue of Gastroenterology (10.1053/j.gastro.2014.09.023 and 10.1053/j.gastro.2014.10.001).
“In clinical trials, administration of sofosbuvir with ribavirin was associated with rapid decreases of HCV RNA to undetectable levels in patients with HCV genotype 1, 2, 3, 4, and 6 infections,” wrote lead author Dr. Michael P. Curry of the Beth Israel Deaconess Medical Center in Boston, and his coauthors on the first of these two studies. “In more than 3,000 patients treated to date, sofosbuvir has been shown to be safe, viral breakthrough during treatment has been rare (and associated with nonadherence), and few drug interactions have been observed.”
In a phase II, open-label study, Dr. Curry and his coinvestigators enrolled 61 patients with HCV of any genotype, and cirrhosis with a Child-Turcotte-Pugh score no greater than 7, who were all wait-listed to receive liver transplantations. Subjects received up to 48 weeks of treatment with 400 mg of sofosbuvir, and a separate dose of ribavirin prior to liver transplantation, while 43 patients received transplantations alone. The primary outcome sought by investigators was HCV-RNA levels less than 25 IU/mL at 12 weeks after transplantation among patients that had this level prior to the operation.
The investigators found that 43 subjects had the desired HCV-RNA levels; of that population, 49% had a posttransplantation virologic response, with the most frequent side effects reported by subjects being fatigue (38%), headache (23%), and anemia (21%). Of the 43 applicable subjects, 30 (70% of the population) had a posttransplantation virologic response at 12 weeks, 10 (23%) had recurrent infection, and 3 (7%) died.
“This study provides proof of concept that virologic suppression without interferon significantly can reduce the rate of recurrent HCV after liver transplantation,” the study says, adding that the results “compare favorably with those observed in other trials of pretransplantation antiviral therapy.”
In the second study, the authors ascertained that combination therapy consisting of sofosbuvir and ribavirin for 24 weeks is effective at preventing hepatitis C virus recurrence in patients who undergo liver transplantations.
“Recurrent HCV infection is the most common cause of mortality and graft loss following transplantation, and up to 30% of patients with recurrent infection develop cirrhosis within 5 years,” wrote the study’s authors, led by Dr. Michael Charlton of the Mayo Clinic in Rochester, Minn.
Using a prospective, multicenter, open-label pilot study, investigators enrolled and treated 40 patients with a 24-week regimen of 400 mg sofosbuvir and ribavirin starting at 400 mg, which was subsequently adjusted per patient based on individual creatinine clearance and hemoglobin levels. Subjects were 78% male and 85% white, with 83% having HCV genotype 1, 40% having cirrhosis, and 88% having been previously treated with interferon. The primary outcome investigators looked for was “sustained virologic response 12 weeks after treatment (SVR12).”
Data showed that SVR12 was achieved by 28 of the 40 subjects that received treatment, or 70%. The most commonly reported adverse effects were fatigue (30%), diarrhea (28%), headache (25%), and anemia (20%). No patients exhibited detectable viral resistance during or after treatment, and although two patients terminated their treatment because of adverse events, investigators reported no deaths, graft losses, or episodes of rejection.
“In contrast,” Dr. Charlton and his coauthors noted, “interferon-based treatments have been associated with posttreatment immunological dysfunction (particularly plasma cell hepatitis) and even hepatic decompensation in LT [liver transplant] recipients.”
The authors of the first study disclosed that Dr. Curry has received grants from and been affiliated with Gilead, which was a sponsor of the study. The authors of the second study reported no relevant financial disclosures.
Sofosbuvir and ribavirin treatments should be administered to patients with hepatitis C virus who undergo liver transplantations in order to significantly decrease the risks of posttransplant HCV recurrence, according to two new studies published in the January issue of Gastroenterology (10.1053/j.gastro.2014.09.023 and 10.1053/j.gastro.2014.10.001).
“In clinical trials, administration of sofosbuvir with ribavirin was associated with rapid decreases of HCV RNA to undetectable levels in patients with HCV genotype 1, 2, 3, 4, and 6 infections,” wrote lead author Dr. Michael P. Curry of the Beth Israel Deaconess Medical Center in Boston, and his coauthors on the first of these two studies. “In more than 3,000 patients treated to date, sofosbuvir has been shown to be safe, viral breakthrough during treatment has been rare (and associated with nonadherence), and few drug interactions have been observed.”
In a phase II, open-label study, Dr. Curry and his coinvestigators enrolled 61 patients with HCV of any genotype, and cirrhosis with a Child-Turcotte-Pugh score no greater than 7, who were all wait-listed to receive liver transplantations. Subjects received up to 48 weeks of treatment with 400 mg of sofosbuvir, and a separate dose of ribavirin prior to liver transplantation, while 43 patients received transplantations alone. The primary outcome sought by investigators was HCV-RNA levels less than 25 IU/mL at 12 weeks after transplantation among patients that had this level prior to the operation.
The investigators found that 43 subjects had the desired HCV-RNA levels; of that population, 49% had a posttransplantation virologic response, with the most frequent side effects reported by subjects being fatigue (38%), headache (23%), and anemia (21%). Of the 43 applicable subjects, 30 (70% of the population) had a posttransplantation virologic response at 12 weeks, 10 (23%) had recurrent infection, and 3 (7%) died.
“This study provides proof of concept that virologic suppression without interferon significantly can reduce the rate of recurrent HCV after liver transplantation,” the study says, adding that the results “compare favorably with those observed in other trials of pretransplantation antiviral therapy.”
In the second study, the authors ascertained that combination therapy consisting of sofosbuvir and ribavirin for 24 weeks is effective at preventing hepatitis C virus recurrence in patients who undergo liver transplantations.
“Recurrent HCV infection is the most common cause of mortality and graft loss following transplantation, and up to 30% of patients with recurrent infection develop cirrhosis within 5 years,” wrote the study’s authors, led by Dr. Michael Charlton of the Mayo Clinic in Rochester, Minn.
Using a prospective, multicenter, open-label pilot study, investigators enrolled and treated 40 patients with a 24-week regimen of 400 mg sofosbuvir and ribavirin starting at 400 mg, which was subsequently adjusted per patient based on individual creatinine clearance and hemoglobin levels. Subjects were 78% male and 85% white, with 83% having HCV genotype 1, 40% having cirrhosis, and 88% having been previously treated with interferon. The primary outcome investigators looked for was “sustained virologic response 12 weeks after treatment (SVR12).”
Data showed that SVR12 was achieved by 28 of the 40 subjects that received treatment, or 70%. The most commonly reported adverse effects were fatigue (30%), diarrhea (28%), headache (25%), and anemia (20%). No patients exhibited detectable viral resistance during or after treatment, and although two patients terminated their treatment because of adverse events, investigators reported no deaths, graft losses, or episodes of rejection.
“In contrast,” Dr. Charlton and his coauthors noted, “interferon-based treatments have been associated with posttreatment immunological dysfunction (particularly plasma cell hepatitis) and even hepatic decompensation in LT [liver transplant] recipients.”
The authors of the first study disclosed that Dr. Curry has received grants from and been affiliated with Gilead, which was a sponsor of the study. The authors of the second study reported no relevant financial disclosures.
FROM GASTROENTEROLOGY
Care bundle cut emergency laparotomy death rate by 39%
An evidence-based care bundle implemented in four U.K. hospitals almost doubled the proportion of lives saved with emergency laparotomy, researchers reported in the British Journal of Surgery.
In addition, 30-day mortality dropped 39%, from 15.6% to 9.6% (risk ratio, 0.61; 95% confidence interval, 0.45 to 0.83; P = .002) at the four hospitals that undertook the quality improvement measures, said Dr. Sam Huddart of Royal Surrey County Hospital NHS Foundation Trust in Guildford, England.
Although a common procedure, emergency laparotomy recently has been linked to death rates of 14% to 19.5% in the United Kingdom, the United States, and Denmark, the researchers said. In the United Kingdom, contributing factors include lack of consultation with surgical and anesthesia specialists, underuse of fluid therapy during surgery, and insufficient use of postoperative ICUs, they added (Br. J. Surg. 2014 Nov. 10 [doi:10.1002/bjs.9658]).
To address these problems, the researchers bundled key recommendations from the Royal College of Surgeons of England and the Department of Health.
The emergency laparotomy pathway quality improvement care (ELPQuiC) bundle included only implemented practices with a strong evidence base, including using an early warning score for all emergency admissions, with graded escalation policies for referring patients to senior clinicians or to the ICU; giving broad-spectrum antibiotics to all patients with sepsis or suspected peritoneal contamination; performing laparotomies within 6 hours of deciding to do so, or as soon as the next available space opened in the emergency operating suite; using goal-directed resuscitation techniques as soon as possible or within 6 hours of admission; and admitting all patients to the ICU after emergency laparotomy, they said.
Eight months later, the number of lives saved per 100 patients treated had risen from 6.47 (or 299 patients) to 12.44 (P < .001), Dr. Huddart and associates reported. “These results were achieved within existing resources, without adversely affecting the length of hospital stay, while the case-mix profile remained relatively stable,” they wrote.
In the regression analysis, only one hospital significantly cut its risk of 30-day mortality, possibly because the study was underpowered. They did not look at emergency laparotomy mortality rates at other hospitals during the study period, they noted.
The research was supported by the Health Foundation, the South West Strategic Health Authority, and LiDCO Group. One coauthor reported receiving lecture fees from LiDCO. The other investigators declared no financial conflicts.
An evidence-based care bundle implemented in four U.K. hospitals almost doubled the proportion of lives saved with emergency laparotomy, researchers reported in the British Journal of Surgery.
In addition, 30-day mortality dropped 39%, from 15.6% to 9.6% (risk ratio, 0.61; 95% confidence interval, 0.45 to 0.83; P = .002) at the four hospitals that undertook the quality improvement measures, said Dr. Sam Huddart of Royal Surrey County Hospital NHS Foundation Trust in Guildford, England.
Although a common procedure, emergency laparotomy recently has been linked to death rates of 14% to 19.5% in the United Kingdom, the United States, and Denmark, the researchers said. In the United Kingdom, contributing factors include lack of consultation with surgical and anesthesia specialists, underuse of fluid therapy during surgery, and insufficient use of postoperative ICUs, they added (Br. J. Surg. 2014 Nov. 10 [doi:10.1002/bjs.9658]).
To address these problems, the researchers bundled key recommendations from the Royal College of Surgeons of England and the Department of Health.
The emergency laparotomy pathway quality improvement care (ELPQuiC) bundle included only implemented practices with a strong evidence base, including using an early warning score for all emergency admissions, with graded escalation policies for referring patients to senior clinicians or to the ICU; giving broad-spectrum antibiotics to all patients with sepsis or suspected peritoneal contamination; performing laparotomies within 6 hours of deciding to do so, or as soon as the next available space opened in the emergency operating suite; using goal-directed resuscitation techniques as soon as possible or within 6 hours of admission; and admitting all patients to the ICU after emergency laparotomy, they said.
Eight months later, the number of lives saved per 100 patients treated had risen from 6.47 (or 299 patients) to 12.44 (P < .001), Dr. Huddart and associates reported. “These results were achieved within existing resources, without adversely affecting the length of hospital stay, while the case-mix profile remained relatively stable,” they wrote.
In the regression analysis, only one hospital significantly cut its risk of 30-day mortality, possibly because the study was underpowered. They did not look at emergency laparotomy mortality rates at other hospitals during the study period, they noted.
The research was supported by the Health Foundation, the South West Strategic Health Authority, and LiDCO Group. One coauthor reported receiving lecture fees from LiDCO. The other investigators declared no financial conflicts.
An evidence-based care bundle implemented in four U.K. hospitals almost doubled the proportion of lives saved with emergency laparotomy, researchers reported in the British Journal of Surgery.
In addition, 30-day mortality dropped 39%, from 15.6% to 9.6% (risk ratio, 0.61; 95% confidence interval, 0.45 to 0.83; P = .002) at the four hospitals that undertook the quality improvement measures, said Dr. Sam Huddart of Royal Surrey County Hospital NHS Foundation Trust in Guildford, England.
Although a common procedure, emergency laparotomy recently has been linked to death rates of 14% to 19.5% in the United Kingdom, the United States, and Denmark, the researchers said. In the United Kingdom, contributing factors include lack of consultation with surgical and anesthesia specialists, underuse of fluid therapy during surgery, and insufficient use of postoperative ICUs, they added (Br. J. Surg. 2014 Nov. 10 [doi:10.1002/bjs.9658]).
To address these problems, the researchers bundled key recommendations from the Royal College of Surgeons of England and the Department of Health.
The emergency laparotomy pathway quality improvement care (ELPQuiC) bundle included only implemented practices with a strong evidence base, including using an early warning score for all emergency admissions, with graded escalation policies for referring patients to senior clinicians or to the ICU; giving broad-spectrum antibiotics to all patients with sepsis or suspected peritoneal contamination; performing laparotomies within 6 hours of deciding to do so, or as soon as the next available space opened in the emergency operating suite; using goal-directed resuscitation techniques as soon as possible or within 6 hours of admission; and admitting all patients to the ICU after emergency laparotomy, they said.
Eight months later, the number of lives saved per 100 patients treated had risen from 6.47 (or 299 patients) to 12.44 (P < .001), Dr. Huddart and associates reported. “These results were achieved within existing resources, without adversely affecting the length of hospital stay, while the case-mix profile remained relatively stable,” they wrote.
In the regression analysis, only one hospital significantly cut its risk of 30-day mortality, possibly because the study was underpowered. They did not look at emergency laparotomy mortality rates at other hospitals during the study period, they noted.
The research was supported by the Health Foundation, the South West Strategic Health Authority, and LiDCO Group. One coauthor reported receiving lecture fees from LiDCO. The other investigators declared no financial conflicts.
Key clinical point: A set of quality improvement measures cut 30-day emergency laparotomy mortality by about 39%.
Major finding: Thirty-day mortality dropped from 15.6% to 9.6% (risk ratio, 0.61; 95% confidence interval, 0.45 to 0.83; P = .002).
Data source: Prospective, 8-month study of emergency laparotomy outcomes at four hospitals in England.
Disclosures: The research was supported by the Health Foundation, the South West Strategic Health Authority, and LiDCO Group. One coauthor reported receiving lecture fees from LiDCO. The other investigators declared no financial conflicts.