User login
Infections, Pulmonary Complications Up Risk of Thrombotic Events
ORLANDO – Researchers have identified risk groups of common perioperative conditions that indicate an increased risk for venous thrombotic events during arterial reconstruction procedures in an analysis of a large administrative database.
The findings could lead to more aggressive venous thrombotic event (VTE) prophylaxis strategies for patients with those "risk families," Dr. Leila Mureebe said at the annual meeting of the American Venous Forum.
Infectious and pulmonary risk families were more commonly associated with VTE. Urinary and intestinal risk families were associated with a lower – although still important – risk of VTEs, said Dr. Mureebe, a vascular surgeon at Duke University in Durham, N.C.
Rates of deep vein thrombosis (DVT) and pulmonary embolism (PE) after common vascular procedures are poorly defined. However, determining the true incidence and/or prevalence would be impractical, she noted.
The researchers used administrative data from the National Inpatient Sample (NIS) to identify patients at increased risk of VTE by identifying associated pre- and postoperative factors. The NIS captures discharges by procedure, and is designed to approximate a 20% sample of U.S. community hospitals. All discharges from sampled hospitals are included in the NIS database, which contains clinical and resource-use information (typically included in a discharge abstract).
This study included all discharges during 2000-2008 with primary arterial operations (abdominal aortic aneurysm [open], aortobifemoral bypass, carotid endarterectomy, and infrainguinal bypass). Procedure codes were crossed by diagnosis code for DVT and PE diagnoses. Next the researchers subselected the population that was associated with VTE, including VTE discharges.
The incidence of VTE was 0.34% of 73,545 patients undergoing abdominal aortic aneurysm repair, 0.06% of 372,465 patients undergoing carotid endarterectomy, 0.27% of 50,415 patients undergoing aortobifemoral bypass, and 0.31% of 253,234 patients undergoing bypass graft.
"We then created risk families to capture the relatively common perioperative events," said Dr. Mureebe. The risk families included intestinal (ileus, small-bowel obstruction), pulmonary (aspiration, bronchitis, pneumonia, lobar pneumonia), urinary complications (urinary tract infection not otherwise specified, indwelling urinary catheter), infectious complications (postoperative infection, postoperative abscess, intra-abdominal infection, stitch abscess, subabscess, wound complications, septicemia, infection due to vascular device, and systemic inflammatory response syndrome), and cardiac (acute myocardial infarction, acute coronary occlusion without MI).
Potential confounders included age at admission, sex, a history of DVT/PE, and a history of a coagulopathy (clotting defect, thrombocytosis, heparin-induced thrombocytopenia, antithrombin deficiency, and mutations [factor V Leiden, prothrombin gene]). Logistic regression was used to assess the association between VTE and risk families. The model was adjusted for age and sex.
In all, 755,536 weighted procedures were identified. VTEs were found in 1,445 diagnoses, for an overall prevalence of 0.19%. "Interestingly, each family of complications was associated with a different risk of VTE," said Dr. Mureebe. The risk of intestinal family complications was 0.62%. Pulmonary, urinary, and infectious family risk rates were 1.2%, 0.66%, and 1.46%, respectively. "Cardiac fell out of all analyses and was not associated – at least in this dataset – with the development of VTEs."
Confounders were more strongly associated with VTEs, Dr. Mureebe noted. A history of VTE was associated with a 2.2% increased risk, and a history of coagulopathy was associated with a 1.68% increased risk.
"So, in addition to discrete risk families having increased risk, there’s also a different profile dependent upon the actual surgical procedure."
For example, in carotid endarterectomy – which is associated with an overall low risk of VTEs – "we really see a large contribution from these potential risk families," she said.
Dr. Mureebe did not report whether she had any relevant financial disclosures.
ORLANDO – Researchers have identified risk groups of common perioperative conditions that indicate an increased risk for venous thrombotic events during arterial reconstruction procedures in an analysis of a large administrative database.
The findings could lead to more aggressive venous thrombotic event (VTE) prophylaxis strategies for patients with those "risk families," Dr. Leila Mureebe said at the annual meeting of the American Venous Forum.
Infectious and pulmonary risk families were more commonly associated with VTE. Urinary and intestinal risk families were associated with a lower – although still important – risk of VTEs, said Dr. Mureebe, a vascular surgeon at Duke University in Durham, N.C.
Rates of deep vein thrombosis (DVT) and pulmonary embolism (PE) after common vascular procedures are poorly defined. However, determining the true incidence and/or prevalence would be impractical, she noted.
The researchers used administrative data from the National Inpatient Sample (NIS) to identify patients at increased risk of VTE by identifying associated pre- and postoperative factors. The NIS captures discharges by procedure, and is designed to approximate a 20% sample of U.S. community hospitals. All discharges from sampled hospitals are included in the NIS database, which contains clinical and resource-use information (typically included in a discharge abstract).
This study included all discharges during 2000-2008 with primary arterial operations (abdominal aortic aneurysm [open], aortobifemoral bypass, carotid endarterectomy, and infrainguinal bypass). Procedure codes were crossed by diagnosis code for DVT and PE diagnoses. Next the researchers subselected the population that was associated with VTE, including VTE discharges.
The incidence of VTE was 0.34% of 73,545 patients undergoing abdominal aortic aneurysm repair, 0.06% of 372,465 patients undergoing carotid endarterectomy, 0.27% of 50,415 patients undergoing aortobifemoral bypass, and 0.31% of 253,234 patients undergoing bypass graft.
"We then created risk families to capture the relatively common perioperative events," said Dr. Mureebe. The risk families included intestinal (ileus, small-bowel obstruction), pulmonary (aspiration, bronchitis, pneumonia, lobar pneumonia), urinary complications (urinary tract infection not otherwise specified, indwelling urinary catheter), infectious complications (postoperative infection, postoperative abscess, intra-abdominal infection, stitch abscess, subabscess, wound complications, septicemia, infection due to vascular device, and systemic inflammatory response syndrome), and cardiac (acute myocardial infarction, acute coronary occlusion without MI).
Potential confounders included age at admission, sex, a history of DVT/PE, and a history of a coagulopathy (clotting defect, thrombocytosis, heparin-induced thrombocytopenia, antithrombin deficiency, and mutations [factor V Leiden, prothrombin gene]). Logistic regression was used to assess the association between VTE and risk families. The model was adjusted for age and sex.
In all, 755,536 weighted procedures were identified. VTEs were found in 1,445 diagnoses, for an overall prevalence of 0.19%. "Interestingly, each family of complications was associated with a different risk of VTE," said Dr. Mureebe. The risk of intestinal family complications was 0.62%. Pulmonary, urinary, and infectious family risk rates were 1.2%, 0.66%, and 1.46%, respectively. "Cardiac fell out of all analyses and was not associated – at least in this dataset – with the development of VTEs."
Confounders were more strongly associated with VTEs, Dr. Mureebe noted. A history of VTE was associated with a 2.2% increased risk, and a history of coagulopathy was associated with a 1.68% increased risk.
"So, in addition to discrete risk families having increased risk, there’s also a different profile dependent upon the actual surgical procedure."
For example, in carotid endarterectomy – which is associated with an overall low risk of VTEs – "we really see a large contribution from these potential risk families," she said.
Dr. Mureebe did not report whether she had any relevant financial disclosures.
ORLANDO – Researchers have identified risk groups of common perioperative conditions that indicate an increased risk for venous thrombotic events during arterial reconstruction procedures in an analysis of a large administrative database.
The findings could lead to more aggressive venous thrombotic event (VTE) prophylaxis strategies for patients with those "risk families," Dr. Leila Mureebe said at the annual meeting of the American Venous Forum.
Infectious and pulmonary risk families were more commonly associated with VTE. Urinary and intestinal risk families were associated with a lower – although still important – risk of VTEs, said Dr. Mureebe, a vascular surgeon at Duke University in Durham, N.C.
Rates of deep vein thrombosis (DVT) and pulmonary embolism (PE) after common vascular procedures are poorly defined. However, determining the true incidence and/or prevalence would be impractical, she noted.
The researchers used administrative data from the National Inpatient Sample (NIS) to identify patients at increased risk of VTE by identifying associated pre- and postoperative factors. The NIS captures discharges by procedure, and is designed to approximate a 20% sample of U.S. community hospitals. All discharges from sampled hospitals are included in the NIS database, which contains clinical and resource-use information (typically included in a discharge abstract).
This study included all discharges during 2000-2008 with primary arterial operations (abdominal aortic aneurysm [open], aortobifemoral bypass, carotid endarterectomy, and infrainguinal bypass). Procedure codes were crossed by diagnosis code for DVT and PE diagnoses. Next the researchers subselected the population that was associated with VTE, including VTE discharges.
The incidence of VTE was 0.34% of 73,545 patients undergoing abdominal aortic aneurysm repair, 0.06% of 372,465 patients undergoing carotid endarterectomy, 0.27% of 50,415 patients undergoing aortobifemoral bypass, and 0.31% of 253,234 patients undergoing bypass graft.
"We then created risk families to capture the relatively common perioperative events," said Dr. Mureebe. The risk families included intestinal (ileus, small-bowel obstruction), pulmonary (aspiration, bronchitis, pneumonia, lobar pneumonia), urinary complications (urinary tract infection not otherwise specified, indwelling urinary catheter), infectious complications (postoperative infection, postoperative abscess, intra-abdominal infection, stitch abscess, subabscess, wound complications, septicemia, infection due to vascular device, and systemic inflammatory response syndrome), and cardiac (acute myocardial infarction, acute coronary occlusion without MI).
Potential confounders included age at admission, sex, a history of DVT/PE, and a history of a coagulopathy (clotting defect, thrombocytosis, heparin-induced thrombocytopenia, antithrombin deficiency, and mutations [factor V Leiden, prothrombin gene]). Logistic regression was used to assess the association between VTE and risk families. The model was adjusted for age and sex.
In all, 755,536 weighted procedures were identified. VTEs were found in 1,445 diagnoses, for an overall prevalence of 0.19%. "Interestingly, each family of complications was associated with a different risk of VTE," said Dr. Mureebe. The risk of intestinal family complications was 0.62%. Pulmonary, urinary, and infectious family risk rates were 1.2%, 0.66%, and 1.46%, respectively. "Cardiac fell out of all analyses and was not associated – at least in this dataset – with the development of VTEs."
Confounders were more strongly associated with VTEs, Dr. Mureebe noted. A history of VTE was associated with a 2.2% increased risk, and a history of coagulopathy was associated with a 1.68% increased risk.
"So, in addition to discrete risk families having increased risk, there’s also a different profile dependent upon the actual surgical procedure."
For example, in carotid endarterectomy – which is associated with an overall low risk of VTEs – "we really see a large contribution from these potential risk families," she said.
Dr. Mureebe did not report whether she had any relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN VENOUS FORUM
Establishing Acute Pain Service Deemed Worthwhile
PALM SPRINGS, CALIF. – The University of Louisville has had an acute pain service for nearly a decade, but for many hospitals in the United States this still is a new idea.
"What we’re seeing is the birth of a new modality in treatment" and possibly a new specialty, Dr. Laura Clark said.
An acute pain service (APS) primarily manages pain after traumatic injury or surgery. The basic aspects of an APS include standardization of analgesic techniques, increased pain monitoring and assessment, and the ability to respond to inadequate or excessive doses of analgesics.
Establishing an APS, however, takes a lot of persuasion and education, said Dr. Clark, professor of anesthesiology and director of acute pain and regional anesthesia at the University of Louisville (Ky.).
Hospital administrators must be convinced that an APS can benefit the hospital by increasing patient satisfaction (which is strongly associated with adequate pain relief) and by cutting costs through reducing nausea and vomiting, respiratory depression, the incidence of ileus (and thus the length of hospitalization), and the incidence of chronic pain.
Physicians and pharmacists need to be willing to accept an APS as part of the care team. Many anesthesiologists mistakenly think that a single nerve block that dissipates in 10 hours is sufficient acute pain management, she said. But more than anyone, surgeons need convincing, Dr. Clark said at the annual meeting of the American Academy of Pain Medicine.
Currently, a surgeon must request involvement of the APS and that request must be documented in order for the service to be covered by insurers. "That needs to change," she said.
To get surgeons on board, include them in developing protocols for all analgesic techniques, she suggested.
There are two groups that don’t need convincing about the benefits of an APS – patients and nurses, she said. Still, education of nurses and all staff about the APS is essential. Simply asking nurses to follow written orders is not sufficient, especially for the more advanced pain therapies. Good acute pain care requires a change in culture and attitudes; for example, nurses need to change empty bags of analgesics just as they change other bags of fluids.
Nurses can be certified in pain management, and "I recommend that you have your nurses do that," Dr. Clark said.
The need for better acute pain management has been established by major reports in the United States, England, Australia, Germany, Sweden, and elsewhere. At least eight published studies report that an APS improves pain relief, five studies report a lower incidence of side effects, and three studies suggest that an APS may reduce the incidence of persistent pain after surgery, she said.
One study reported reduced postoperative morbidity and mortality with an APS but noted that "the workload is considerable" (Anesthesia 2006;61:24-8).
A recent study concluded that an APS is "likely" to be cost effective, but the investigators "didn’t even study what we do," Dr. Clark said. Key treatment techniques such as peripheral nerve blocks and epidural patient-controlled analgesia were not included in the study (Anesth. Analg. 2010;111:1042-50). Had it included those, she believes the study would have shown that an APS is very cost effective, she said.
Better studies with hard data are needed, she added.
The service ideally is physician directed but multidisciplinary, including physicians, nurses, pharmacists, and physical therapists. The most common but least desirable model of an APS in the United States includes a private physician or regionalist who may not do rounds unless called by a surgeon to manage a problem, Dr. Clark said. A second model that may be the most flexible and cost effective for around-the-clock care involves a nurse-led physician consult, in which the nurse makes daily rounds, reports to the physician, and implements therapy based on standard orders and protocols developed by the pain physician and surgeon.
The most common model in academic centers, and Dr. Clark’s favorite, is a physician-led team with a pain management nurse. The team makes rounds and decides on care. The pain physician may or may not be the regionalist. Medical residents are on call for the pain service. The pain nurse is involved in cases before, during, and after surgery and implements advanced pain management techniques, provides consultations, and coordinates with trauma, surgery, and critical care services.
Once you’ve convinced your institution and colleagues to establish an APS, make sure that someone on the APS can be reached by telephone at any hour of every day. Establish "acute pain champions" on every floor and in every area of the hospital, and make sure that at least one champion is available on every shift.
Running an APS can be challenging, but it’s a therapeutic tool that’s worth the effort, she said: "With our twice-a-day rounds, we often hear from the patients that we talk to them more than any other physician. It can be quite rewarding."
Dr. Clark has been a speaker for Covidien and Cadence and an adviser and researcher for Covidien.
PALM SPRINGS, CALIF. – The University of Louisville has had an acute pain service for nearly a decade, but for many hospitals in the United States this still is a new idea.
"What we’re seeing is the birth of a new modality in treatment" and possibly a new specialty, Dr. Laura Clark said.
An acute pain service (APS) primarily manages pain after traumatic injury or surgery. The basic aspects of an APS include standardization of analgesic techniques, increased pain monitoring and assessment, and the ability to respond to inadequate or excessive doses of analgesics.
Establishing an APS, however, takes a lot of persuasion and education, said Dr. Clark, professor of anesthesiology and director of acute pain and regional anesthesia at the University of Louisville (Ky.).
Hospital administrators must be convinced that an APS can benefit the hospital by increasing patient satisfaction (which is strongly associated with adequate pain relief) and by cutting costs through reducing nausea and vomiting, respiratory depression, the incidence of ileus (and thus the length of hospitalization), and the incidence of chronic pain.
Physicians and pharmacists need to be willing to accept an APS as part of the care team. Many anesthesiologists mistakenly think that a single nerve block that dissipates in 10 hours is sufficient acute pain management, she said. But more than anyone, surgeons need convincing, Dr. Clark said at the annual meeting of the American Academy of Pain Medicine.
Currently, a surgeon must request involvement of the APS and that request must be documented in order for the service to be covered by insurers. "That needs to change," she said.
To get surgeons on board, include them in developing protocols for all analgesic techniques, she suggested.
There are two groups that don’t need convincing about the benefits of an APS – patients and nurses, she said. Still, education of nurses and all staff about the APS is essential. Simply asking nurses to follow written orders is not sufficient, especially for the more advanced pain therapies. Good acute pain care requires a change in culture and attitudes; for example, nurses need to change empty bags of analgesics just as they change other bags of fluids.
Nurses can be certified in pain management, and "I recommend that you have your nurses do that," Dr. Clark said.
The need for better acute pain management has been established by major reports in the United States, England, Australia, Germany, Sweden, and elsewhere. At least eight published studies report that an APS improves pain relief, five studies report a lower incidence of side effects, and three studies suggest that an APS may reduce the incidence of persistent pain after surgery, she said.
One study reported reduced postoperative morbidity and mortality with an APS but noted that "the workload is considerable" (Anesthesia 2006;61:24-8).
A recent study concluded that an APS is "likely" to be cost effective, but the investigators "didn’t even study what we do," Dr. Clark said. Key treatment techniques such as peripheral nerve blocks and epidural patient-controlled analgesia were not included in the study (Anesth. Analg. 2010;111:1042-50). Had it included those, she believes the study would have shown that an APS is very cost effective, she said.
Better studies with hard data are needed, she added.
The service ideally is physician directed but multidisciplinary, including physicians, nurses, pharmacists, and physical therapists. The most common but least desirable model of an APS in the United States includes a private physician or regionalist who may not do rounds unless called by a surgeon to manage a problem, Dr. Clark said. A second model that may be the most flexible and cost effective for around-the-clock care involves a nurse-led physician consult, in which the nurse makes daily rounds, reports to the physician, and implements therapy based on standard orders and protocols developed by the pain physician and surgeon.
The most common model in academic centers, and Dr. Clark’s favorite, is a physician-led team with a pain management nurse. The team makes rounds and decides on care. The pain physician may or may not be the regionalist. Medical residents are on call for the pain service. The pain nurse is involved in cases before, during, and after surgery and implements advanced pain management techniques, provides consultations, and coordinates with trauma, surgery, and critical care services.
Once you’ve convinced your institution and colleagues to establish an APS, make sure that someone on the APS can be reached by telephone at any hour of every day. Establish "acute pain champions" on every floor and in every area of the hospital, and make sure that at least one champion is available on every shift.
Running an APS can be challenging, but it’s a therapeutic tool that’s worth the effort, she said: "With our twice-a-day rounds, we often hear from the patients that we talk to them more than any other physician. It can be quite rewarding."
Dr. Clark has been a speaker for Covidien and Cadence and an adviser and researcher for Covidien.
PALM SPRINGS, CALIF. – The University of Louisville has had an acute pain service for nearly a decade, but for many hospitals in the United States this still is a new idea.
"What we’re seeing is the birth of a new modality in treatment" and possibly a new specialty, Dr. Laura Clark said.
An acute pain service (APS) primarily manages pain after traumatic injury or surgery. The basic aspects of an APS include standardization of analgesic techniques, increased pain monitoring and assessment, and the ability to respond to inadequate or excessive doses of analgesics.
Establishing an APS, however, takes a lot of persuasion and education, said Dr. Clark, professor of anesthesiology and director of acute pain and regional anesthesia at the University of Louisville (Ky.).
Hospital administrators must be convinced that an APS can benefit the hospital by increasing patient satisfaction (which is strongly associated with adequate pain relief) and by cutting costs through reducing nausea and vomiting, respiratory depression, the incidence of ileus (and thus the length of hospitalization), and the incidence of chronic pain.
Physicians and pharmacists need to be willing to accept an APS as part of the care team. Many anesthesiologists mistakenly think that a single nerve block that dissipates in 10 hours is sufficient acute pain management, she said. But more than anyone, surgeons need convincing, Dr. Clark said at the annual meeting of the American Academy of Pain Medicine.
Currently, a surgeon must request involvement of the APS and that request must be documented in order for the service to be covered by insurers. "That needs to change," she said.
To get surgeons on board, include them in developing protocols for all analgesic techniques, she suggested.
There are two groups that don’t need convincing about the benefits of an APS – patients and nurses, she said. Still, education of nurses and all staff about the APS is essential. Simply asking nurses to follow written orders is not sufficient, especially for the more advanced pain therapies. Good acute pain care requires a change in culture and attitudes; for example, nurses need to change empty bags of analgesics just as they change other bags of fluids.
Nurses can be certified in pain management, and "I recommend that you have your nurses do that," Dr. Clark said.
The need for better acute pain management has been established by major reports in the United States, England, Australia, Germany, Sweden, and elsewhere. At least eight published studies report that an APS improves pain relief, five studies report a lower incidence of side effects, and three studies suggest that an APS may reduce the incidence of persistent pain after surgery, she said.
One study reported reduced postoperative morbidity and mortality with an APS but noted that "the workload is considerable" (Anesthesia 2006;61:24-8).
A recent study concluded that an APS is "likely" to be cost effective, but the investigators "didn’t even study what we do," Dr. Clark said. Key treatment techniques such as peripheral nerve blocks and epidural patient-controlled analgesia were not included in the study (Anesth. Analg. 2010;111:1042-50). Had it included those, she believes the study would have shown that an APS is very cost effective, she said.
Better studies with hard data are needed, she added.
The service ideally is physician directed but multidisciplinary, including physicians, nurses, pharmacists, and physical therapists. The most common but least desirable model of an APS in the United States includes a private physician or regionalist who may not do rounds unless called by a surgeon to manage a problem, Dr. Clark said. A second model that may be the most flexible and cost effective for around-the-clock care involves a nurse-led physician consult, in which the nurse makes daily rounds, reports to the physician, and implements therapy based on standard orders and protocols developed by the pain physician and surgeon.
The most common model in academic centers, and Dr. Clark’s favorite, is a physician-led team with a pain management nurse. The team makes rounds and decides on care. The pain physician may or may not be the regionalist. Medical residents are on call for the pain service. The pain nurse is involved in cases before, during, and after surgery and implements advanced pain management techniques, provides consultations, and coordinates with trauma, surgery, and critical care services.
Once you’ve convinced your institution and colleagues to establish an APS, make sure that someone on the APS can be reached by telephone at any hour of every day. Establish "acute pain champions" on every floor and in every area of the hospital, and make sure that at least one champion is available on every shift.
Running an APS can be challenging, but it’s a therapeutic tool that’s worth the effort, she said: "With our twice-a-day rounds, we often hear from the patients that we talk to them more than any other physician. It can be quite rewarding."
Dr. Clark has been a speaker for Covidien and Cadence and an adviser and researcher for Covidien.
FROM THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF PAIN MEDICINE
Repeat BAL Advised With Prolonged Therapy for Ventilator-Associated Pneumonia
HOUSTON – Repeat bronchoalveolar lavage should be considered for tailoring the duration of antibiotic therapy and for reassessing resistance profiles in patients with ventilator-associated pneumonia from infection with non–lactose fermenting gram-negative bacilli.
New clinical evidence endorses prolonged antibiotic therapy in these patients. Importantly, the findings also indicate that these patients have persistent primary infections, rather than recurrent infections, as has been previously suggested, Dr. Gina R. Shirah reported at Annual Congress of the Society for Critical Care Medicine.
The distinction between persistent and recurrent infection is important, she emphasized, as the former may signal drug resistance in some patients. For this reason, repeat bronchoalveolar lavage (BAL) should be considered during therapy, both to tailor duration of antibiotics and reassess for changes in resistance profiles.
The American Thoracic Society recommends an 8-day antimicrobial treatment protocol for ventilator-associated pneumonia (VAP) but advises a longer course of therapy in patients with non–lactose fermenting gram-negative rods (NLF-GNR), which include Pseudomonas aeruginosa, Acinetobacter baumannii, and Stenotrophomonas maltophilia (Am. J. Respir. Crit. Care Med. 2005;171:388-416). The recommendation is based on the findings of a pioneering randomized study by the PneumA Trial Group that showed 8-day treatment to be as effective as 15-day treatment except in a subgroup of patients with NLF-GNR, in whom they observed higher recurrence rates (JAMA 2003;290:2588-98).
Dr. Shirah and her fellow researchers at the Maricopa Integrated Health System in Phoenix, including lead investigator Dr. Tammy Kopelman, conducted a study that indicates 8-day antibiotic regimens were associated with persistent primary infections, not recurrent infections, in patients with gram-negative bacilli.
The researchers retrospectively studied patients at a level I trauma center admitted over a 4½-year time period. They examined data for all ventilator-associated pneumonia patients who were diagnosed via bronchoalveolar lavage – and who underwent subsequent BAL during the antimicrobial treatment course. Based upon initial BAL pathogen, the patients were classified into two groups: those with NLF-GNR and those with all other pathogens, including Enterobacteriaceae, methicillin-resistant Staphylococcus aureus, and community-acquired Haemophilus spp, methicillin-sensitive S. aureus, and Streptococcus spp. They were then further divided based on whether the repeat BAL was conducted within fewer than 8 days of appropriate antibiotic therapy or at day 8 or later, Dr. Shirah said. "Persistent primary infection was defined as a less than 2-log 10 decrease of the initial species on subsequent bronchoalveolar lavage," she explained.
Of the 77 surgical intensive care unit patients who met the study criteria, 99% received appropriate empiric therapy, said Dr. Shirah. The average subsequent BAL performance was on day 7 (range, 3-14 days), with 37 patients undergoing the procedure after 8 days of therapy; of those, 13 patients were in the NLF-GNR group. Within that group, persistent primary infection after more than 8 days of appropriate antimicrobial therapy was reported in nine of the patients (69%) – seven with P. aeruginosa and two with A. baumannii.
By comparison, only two patients in the second group (8%) – both with Enterobacteriaceae – had evidence of persistent primary infection, representing a statistically significant difference, she said. "Importantly, in the [NLF-GNB] group, 56% of the pathogens obtained on repeat BAL remained sensitive to the treatment antibiotics, so nearly half of the patients required alternative antibiotic treatment."
The investigators also sought to determine whether persistent infection could have been predicted. They separated patients into three groups based on treatment status: treated (microbiologic cure on subsequent BAL); persistently infected antimicrobial sensitive; and persistently infected antimicrobial resistant. A comparison of clinical parameters across the groups showed that although there was some variation in white blood cell count, temperature, and ventilator needs "none of the differences were statistically significant," and thus not predictive of short-course treatment success or persistent infection, Dr. Shirah said.
The data strongly support the conclusion that a shortened course of antibiotics in patients with VAP caused by NLF-GNR will frequently lead to a persistent primary infection, said Dr. Shirah, noting that, in the case of NLF-GNR, "changes in antibiotic profiles are common and without reliable clinical indicators." For this reason, she stressed, repeat BAL should be considered during therapy, both to tailor duration of antibiotics and to reassess for changes in resistance profiles.
"Eight days is simply not enough," Dr. Shirah said.
On behalf of her coinvestigators and herself, Dr. Shirah reported no conflicts of interest with respect to this study.
HOUSTON – Repeat bronchoalveolar lavage should be considered for tailoring the duration of antibiotic therapy and for reassessing resistance profiles in patients with ventilator-associated pneumonia from infection with non–lactose fermenting gram-negative bacilli.
New clinical evidence endorses prolonged antibiotic therapy in these patients. Importantly, the findings also indicate that these patients have persistent primary infections, rather than recurrent infections, as has been previously suggested, Dr. Gina R. Shirah reported at Annual Congress of the Society for Critical Care Medicine.
The distinction between persistent and recurrent infection is important, she emphasized, as the former may signal drug resistance in some patients. For this reason, repeat bronchoalveolar lavage (BAL) should be considered during therapy, both to tailor duration of antibiotics and reassess for changes in resistance profiles.
The American Thoracic Society recommends an 8-day antimicrobial treatment protocol for ventilator-associated pneumonia (VAP) but advises a longer course of therapy in patients with non–lactose fermenting gram-negative rods (NLF-GNR), which include Pseudomonas aeruginosa, Acinetobacter baumannii, and Stenotrophomonas maltophilia (Am. J. Respir. Crit. Care Med. 2005;171:388-416). The recommendation is based on the findings of a pioneering randomized study by the PneumA Trial Group that showed 8-day treatment to be as effective as 15-day treatment except in a subgroup of patients with NLF-GNR, in whom they observed higher recurrence rates (JAMA 2003;290:2588-98).
Dr. Shirah and her fellow researchers at the Maricopa Integrated Health System in Phoenix, including lead investigator Dr. Tammy Kopelman, conducted a study that indicates 8-day antibiotic regimens were associated with persistent primary infections, not recurrent infections, in patients with gram-negative bacilli.
The researchers retrospectively studied patients at a level I trauma center admitted over a 4½-year time period. They examined data for all ventilator-associated pneumonia patients who were diagnosed via bronchoalveolar lavage – and who underwent subsequent BAL during the antimicrobial treatment course. Based upon initial BAL pathogen, the patients were classified into two groups: those with NLF-GNR and those with all other pathogens, including Enterobacteriaceae, methicillin-resistant Staphylococcus aureus, and community-acquired Haemophilus spp, methicillin-sensitive S. aureus, and Streptococcus spp. They were then further divided based on whether the repeat BAL was conducted within fewer than 8 days of appropriate antibiotic therapy or at day 8 or later, Dr. Shirah said. "Persistent primary infection was defined as a less than 2-log 10 decrease of the initial species on subsequent bronchoalveolar lavage," she explained.
Of the 77 surgical intensive care unit patients who met the study criteria, 99% received appropriate empiric therapy, said Dr. Shirah. The average subsequent BAL performance was on day 7 (range, 3-14 days), with 37 patients undergoing the procedure after 8 days of therapy; of those, 13 patients were in the NLF-GNR group. Within that group, persistent primary infection after more than 8 days of appropriate antimicrobial therapy was reported in nine of the patients (69%) – seven with P. aeruginosa and two with A. baumannii.
By comparison, only two patients in the second group (8%) – both with Enterobacteriaceae – had evidence of persistent primary infection, representing a statistically significant difference, she said. "Importantly, in the [NLF-GNB] group, 56% of the pathogens obtained on repeat BAL remained sensitive to the treatment antibiotics, so nearly half of the patients required alternative antibiotic treatment."
The investigators also sought to determine whether persistent infection could have been predicted. They separated patients into three groups based on treatment status: treated (microbiologic cure on subsequent BAL); persistently infected antimicrobial sensitive; and persistently infected antimicrobial resistant. A comparison of clinical parameters across the groups showed that although there was some variation in white blood cell count, temperature, and ventilator needs "none of the differences were statistically significant," and thus not predictive of short-course treatment success or persistent infection, Dr. Shirah said.
The data strongly support the conclusion that a shortened course of antibiotics in patients with VAP caused by NLF-GNR will frequently lead to a persistent primary infection, said Dr. Shirah, noting that, in the case of NLF-GNR, "changes in antibiotic profiles are common and without reliable clinical indicators." For this reason, she stressed, repeat BAL should be considered during therapy, both to tailor duration of antibiotics and to reassess for changes in resistance profiles.
"Eight days is simply not enough," Dr. Shirah said.
On behalf of her coinvestigators and herself, Dr. Shirah reported no conflicts of interest with respect to this study.
HOUSTON – Repeat bronchoalveolar lavage should be considered for tailoring the duration of antibiotic therapy and for reassessing resistance profiles in patients with ventilator-associated pneumonia from infection with non–lactose fermenting gram-negative bacilli.
New clinical evidence endorses prolonged antibiotic therapy in these patients. Importantly, the findings also indicate that these patients have persistent primary infections, rather than recurrent infections, as has been previously suggested, Dr. Gina R. Shirah reported at Annual Congress of the Society for Critical Care Medicine.
The distinction between persistent and recurrent infection is important, she emphasized, as the former may signal drug resistance in some patients. For this reason, repeat bronchoalveolar lavage (BAL) should be considered during therapy, both to tailor duration of antibiotics and reassess for changes in resistance profiles.
The American Thoracic Society recommends an 8-day antimicrobial treatment protocol for ventilator-associated pneumonia (VAP) but advises a longer course of therapy in patients with non–lactose fermenting gram-negative rods (NLF-GNR), which include Pseudomonas aeruginosa, Acinetobacter baumannii, and Stenotrophomonas maltophilia (Am. J. Respir. Crit. Care Med. 2005;171:388-416). The recommendation is based on the findings of a pioneering randomized study by the PneumA Trial Group that showed 8-day treatment to be as effective as 15-day treatment except in a subgroup of patients with NLF-GNR, in whom they observed higher recurrence rates (JAMA 2003;290:2588-98).
Dr. Shirah and her fellow researchers at the Maricopa Integrated Health System in Phoenix, including lead investigator Dr. Tammy Kopelman, conducted a study that indicates 8-day antibiotic regimens were associated with persistent primary infections, not recurrent infections, in patients with gram-negative bacilli.
The researchers retrospectively studied patients at a level I trauma center admitted over a 4½-year time period. They examined data for all ventilator-associated pneumonia patients who were diagnosed via bronchoalveolar lavage – and who underwent subsequent BAL during the antimicrobial treatment course. Based upon initial BAL pathogen, the patients were classified into two groups: those with NLF-GNR and those with all other pathogens, including Enterobacteriaceae, methicillin-resistant Staphylococcus aureus, and community-acquired Haemophilus spp, methicillin-sensitive S. aureus, and Streptococcus spp. They were then further divided based on whether the repeat BAL was conducted within fewer than 8 days of appropriate antibiotic therapy or at day 8 or later, Dr. Shirah said. "Persistent primary infection was defined as a less than 2-log 10 decrease of the initial species on subsequent bronchoalveolar lavage," she explained.
Of the 77 surgical intensive care unit patients who met the study criteria, 99% received appropriate empiric therapy, said Dr. Shirah. The average subsequent BAL performance was on day 7 (range, 3-14 days), with 37 patients undergoing the procedure after 8 days of therapy; of those, 13 patients were in the NLF-GNR group. Within that group, persistent primary infection after more than 8 days of appropriate antimicrobial therapy was reported in nine of the patients (69%) – seven with P. aeruginosa and two with A. baumannii.
By comparison, only two patients in the second group (8%) – both with Enterobacteriaceae – had evidence of persistent primary infection, representing a statistically significant difference, she said. "Importantly, in the [NLF-GNB] group, 56% of the pathogens obtained on repeat BAL remained sensitive to the treatment antibiotics, so nearly half of the patients required alternative antibiotic treatment."
The investigators also sought to determine whether persistent infection could have been predicted. They separated patients into three groups based on treatment status: treated (microbiologic cure on subsequent BAL); persistently infected antimicrobial sensitive; and persistently infected antimicrobial resistant. A comparison of clinical parameters across the groups showed that although there was some variation in white blood cell count, temperature, and ventilator needs "none of the differences were statistically significant," and thus not predictive of short-course treatment success or persistent infection, Dr. Shirah said.
The data strongly support the conclusion that a shortened course of antibiotics in patients with VAP caused by NLF-GNR will frequently lead to a persistent primary infection, said Dr. Shirah, noting that, in the case of NLF-GNR, "changes in antibiotic profiles are common and without reliable clinical indicators." For this reason, she stressed, repeat BAL should be considered during therapy, both to tailor duration of antibiotics and to reassess for changes in resistance profiles.
"Eight days is simply not enough," Dr. Shirah said.
On behalf of her coinvestigators and herself, Dr. Shirah reported no conflicts of interest with respect to this study.
FROM THE ANNUAL CONGRESS OF THE SOCIETY FOR CRITICAL CARE MEDICINE
Major Finding: Repeat bronchoalveolar lavage (BAL) of 37 patients after 8 days of appropriate antimicrobial therapy indicated that 69% patients with non–lactose fermenting gram-negative rods had persistent primary infection, compared with 8% patients with all other pathogens.
Data Source: Results came from a retrospective study of 77 patients with BAL-diagnosed ventilator-associated pneumonia who underwent repeat BAL while on antibiotic therapy at a level 1 trauma center.
Disclosures: The investigators reported having no relevant financial disclosures.
RAP Scores Guide Ultrasonography for VTE in Trauma Patients
HOUSTON – Nearly 30% of trauma patients who were identified upon admission as being high risk for venous thromboembolism using a validated risk assessment tool went on to develop the thrombotic condition during their ICU stay, a study has shown.
Importantly, the deep vein thromboses in most of these patients were asymptomatic and might have gone undetected with potentially life-threatening consequences but for periodic ultrasound screening, Dr. Chad Thorson reported at the annual congress of the Society of Critical Care Medicine.
"Routine venous thromboembolism screening in the trauma population has been widely debated, and there currently is no protocol for it," according to Dr. Thorson of the Ryder Trauma Center at the University of Miami. Although the principal diagnostic screening tool – venous duplex ultrasound (VDU) – is not considered cost effective for screening all trauma patients, the investigators sought to determine whether prescreening trauma patients using the risk assessment profile (RAP) would yield a cohort of high- risk patients in whom increased vigilance and VDU screening are warranted (J. Trauma 1997;42:100-3).
Toward this end, all patients admitted to the Ryder Center’s level 1 trauma intensive care unit from November 2009 through January 2012 were prospectively screened with RAP, which stratifies an individual’s venous thromboembolism (VTE) risk based on underlying conditions, iatrogenic factors, injury-related factors, and age, within 24 hours of admission.
"Patients with [RAP] scores of 10 or higher received bilateral lower-extremity venous duplex ultrasounds at the time of admission and then weekly throughout their ICU stay," Dr. Thorson said, noting that logistic regression was performed on risk factors to identify independent predictors of VTE development. Among the risk factors considered were RAP score, RAP score higher than 20, femoral central venous catheterization for more than 24 hours, operative intervention duration longer than 2 hours, lower-extremity fracture, pelvic fracture, and spinal cord injury with paraplegia.
Of 534 trauma ICU admissions during the study period, 106 patients (mean age, 47 years) were identified as high risk based on their RAP score. Blunt trauma was the primary mechanism of injury in 79% of the population, and the mean injury severity score of the predominantly male (74%) high-risk population was 30, said Dr. Thorson.
Routine VDU screening identified 30 VTEs, including 20 that were asymptomatic and 10 that were symptomatic, despite the patients having received thromboprophylaxis (heparin 5,000 U every 8 hours or dalteparin 5,000 U daily), Dr. Thorson reported. Four of the symptomatic events were pulmonary emboli, and of the asymptomatic VTEs, six were identified on admission, seven were identified within the first week of admission, and four were identified within 2 weeks of admission, he said.
A comparison of those who did and did not develop VTEs showed significant differences in the number of risk factors, overall RAP score, and RAP score greater than 20, Dr. Thorson reported. Specifically, those in the non-VTE group averaged five risk factors compared with seven in the VTE group, and the respective median RAP scores were 14 and 19, he said. In addition, 6 patients in the non-VTE and 11 in the VTE group had RAP scores higher than 20. In the stepwise logistic regression analysis, RAP score and a combination of pelvic fracture and prolonged operative intervention were independent predictors of VTE development, he said.
Prescreening trauma patients with RAP is useful for identifying patients at increased risk of VTE who may be candidates for increased surveillance, according to Dr. Thorson. "There is plenty of debate with regard to the utility and cost effectiveness of routine screening, as well as the benefit of identifying asymptomatic deep vein thromboses," Dr. Thorson said in an interview.
"Ideally, we hope to find a decrease in the rate of pulmonary embolism as a result of screening, as this consequence can be devastating."
An important implication of the screening protocol, however, is identifying that DVT/VTE should not be included on the Centers for Medicare and Medicaid Services’ list of preventable complications (defined as errors in medical care that are clearly identifiable and preventable, and thus may no longer be eligible for reimbursement).
"A decision to no longer pay for [VTE] treatment could have devastating effects on many urban trauma centers," Dr. Thorson stressed.
The prescreening study was supported by grants from the Office of Naval Research and the U.S. Army Medical Research and Materiel Command. Dr. Thorson reported that he had no relevant financial disclosures.
Trauma patients are at high risk for VTE, and in the absence of bleeding contraindications, all should be receiving pharmacologic prophylaxis with LDUH/LMWH. Therefore, a risk assessment program for VTE doesn't make much sense: Everyone "rules in" for VTE prophylaxis with medication unless a contraindication exists, according to Dr. Franklin A. Michota.
This observational study used a risk assessment program to identify patients for whom surveillance venous duplex ultrasound might be indicated on top of pharmacologic prophylaxis. Currently, VDU surveillance is not recommended in trauma patients, according to the recently published ninth American College of Chest Physicians' guidelines on antithrombotic therapy and the prevention of thrombosis (Chest 2012;141[suppl.]:e227S-77S). In fact, the ACCP specifically recommends that surveillance not be performed (grade 2C evidence). The rationale is well outlined in the guidelines. It is not clear that using VDU to detect and treat asymptomatic DVT reduces the risk of pulmonary embolism or fatal pulmonary embolism, and some studies have demonstrated that pulmonary embolism can occur even when VDU is negative.
As reported in the ACCP chapter on the prevention of VTE in surgery patients, a large retrospective study from a single center found that over a 6-year period ending in 2000, the frequency of surveillance VDU decreased from 32% to 3.4%, yet there was no increase in the incidence of pulmonary embolism. Also it is well known that surveillance VDU can lead to false-positive findings (asymptomatic distal clot that does not pose a risk for symptoms or embolization), and the risk of treating the false positives with full anticoagulation in the trauma surgery population may increase adverse outcomes.
This new study identified 30 VTEs in 106 high-risk trauma patients with surveillance VDU. However, the investigators reported that 10 of the events were symptomatic, so the VDU was not a screening tool; it was a diagnostic test for signs and symptoms, and therefore, those 10 symptomatic events need to be removed. That leaves you with 20 VTEs in 106 high-risk trauma patients (18.8%). So the real question is, Where were these clots located? If they were distal asymptomatic events, then they may all be false positives. If they were all proximal DVTs, then perhaps this study deserves more credit.
But we should also look at the intensity of VTE prophylaxis provided in this study cohort. The ACCP also recommends mechanical compression on top of pharmacologic prophylaxis in high-risk trauma patients. Was that done here? Perhaps the 20 VTEs were due to inadequate prophylaxis.
Dr. Michota is the director of academic affairs in the department of hospital medicine at the Cleveland Clinic. He reported having no relevant financial disclosures.
Trauma patients are at high risk for VTE, and in the absence of bleeding contraindications, all should be receiving pharmacologic prophylaxis with LDUH/LMWH. Therefore, a risk assessment program for VTE doesn't make much sense: Everyone "rules in" for VTE prophylaxis with medication unless a contraindication exists, according to Dr. Franklin A. Michota.
This observational study used a risk assessment program to identify patients for whom surveillance venous duplex ultrasound might be indicated on top of pharmacologic prophylaxis. Currently, VDU surveillance is not recommended in trauma patients, according to the recently published ninth American College of Chest Physicians' guidelines on antithrombotic therapy and the prevention of thrombosis (Chest 2012;141[suppl.]:e227S-77S). In fact, the ACCP specifically recommends that surveillance not be performed (grade 2C evidence). The rationale is well outlined in the guidelines. It is not clear that using VDU to detect and treat asymptomatic DVT reduces the risk of pulmonary embolism or fatal pulmonary embolism, and some studies have demonstrated that pulmonary embolism can occur even when VDU is negative.
As reported in the ACCP chapter on the prevention of VTE in surgery patients, a large retrospective study from a single center found that over a 6-year period ending in 2000, the frequency of surveillance VDU decreased from 32% to 3.4%, yet there was no increase in the incidence of pulmonary embolism. Also it is well known that surveillance VDU can lead to false-positive findings (asymptomatic distal clot that does not pose a risk for symptoms or embolization), and the risk of treating the false positives with full anticoagulation in the trauma surgery population may increase adverse outcomes.
This new study identified 30 VTEs in 106 high-risk trauma patients with surveillance VDU. However, the investigators reported that 10 of the events were symptomatic, so the VDU was not a screening tool; it was a diagnostic test for signs and symptoms, and therefore, those 10 symptomatic events need to be removed. That leaves you with 20 VTEs in 106 high-risk trauma patients (18.8%). So the real question is, Where were these clots located? If they were distal asymptomatic events, then they may all be false positives. If they were all proximal DVTs, then perhaps this study deserves more credit.
But we should also look at the intensity of VTE prophylaxis provided in this study cohort. The ACCP also recommends mechanical compression on top of pharmacologic prophylaxis in high-risk trauma patients. Was that done here? Perhaps the 20 VTEs were due to inadequate prophylaxis.
Dr. Michota is the director of academic affairs in the department of hospital medicine at the Cleveland Clinic. He reported having no relevant financial disclosures.
Trauma patients are at high risk for VTE, and in the absence of bleeding contraindications, all should be receiving pharmacologic prophylaxis with LDUH/LMWH. Therefore, a risk assessment program for VTE doesn't make much sense: Everyone "rules in" for VTE prophylaxis with medication unless a contraindication exists, according to Dr. Franklin A. Michota.
This observational study used a risk assessment program to identify patients for whom surveillance venous duplex ultrasound might be indicated on top of pharmacologic prophylaxis. Currently, VDU surveillance is not recommended in trauma patients, according to the recently published ninth American College of Chest Physicians' guidelines on antithrombotic therapy and the prevention of thrombosis (Chest 2012;141[suppl.]:e227S-77S). In fact, the ACCP specifically recommends that surveillance not be performed (grade 2C evidence). The rationale is well outlined in the guidelines. It is not clear that using VDU to detect and treat asymptomatic DVT reduces the risk of pulmonary embolism or fatal pulmonary embolism, and some studies have demonstrated that pulmonary embolism can occur even when VDU is negative.
As reported in the ACCP chapter on the prevention of VTE in surgery patients, a large retrospective study from a single center found that over a 6-year period ending in 2000, the frequency of surveillance VDU decreased from 32% to 3.4%, yet there was no increase in the incidence of pulmonary embolism. Also it is well known that surveillance VDU can lead to false-positive findings (asymptomatic distal clot that does not pose a risk for symptoms or embolization), and the risk of treating the false positives with full anticoagulation in the trauma surgery population may increase adverse outcomes.
This new study identified 30 VTEs in 106 high-risk trauma patients with surveillance VDU. However, the investigators reported that 10 of the events were symptomatic, so the VDU was not a screening tool; it was a diagnostic test for signs and symptoms, and therefore, those 10 symptomatic events need to be removed. That leaves you with 20 VTEs in 106 high-risk trauma patients (18.8%). So the real question is, Where were these clots located? If they were distal asymptomatic events, then they may all be false positives. If they were all proximal DVTs, then perhaps this study deserves more credit.
But we should also look at the intensity of VTE prophylaxis provided in this study cohort. The ACCP also recommends mechanical compression on top of pharmacologic prophylaxis in high-risk trauma patients. Was that done here? Perhaps the 20 VTEs were due to inadequate prophylaxis.
Dr. Michota is the director of academic affairs in the department of hospital medicine at the Cleveland Clinic. He reported having no relevant financial disclosures.
HOUSTON – Nearly 30% of trauma patients who were identified upon admission as being high risk for venous thromboembolism using a validated risk assessment tool went on to develop the thrombotic condition during their ICU stay, a study has shown.
Importantly, the deep vein thromboses in most of these patients were asymptomatic and might have gone undetected with potentially life-threatening consequences but for periodic ultrasound screening, Dr. Chad Thorson reported at the annual congress of the Society of Critical Care Medicine.
"Routine venous thromboembolism screening in the trauma population has been widely debated, and there currently is no protocol for it," according to Dr. Thorson of the Ryder Trauma Center at the University of Miami. Although the principal diagnostic screening tool – venous duplex ultrasound (VDU) – is not considered cost effective for screening all trauma patients, the investigators sought to determine whether prescreening trauma patients using the risk assessment profile (RAP) would yield a cohort of high- risk patients in whom increased vigilance and VDU screening are warranted (J. Trauma 1997;42:100-3).
Toward this end, all patients admitted to the Ryder Center’s level 1 trauma intensive care unit from November 2009 through January 2012 were prospectively screened with RAP, which stratifies an individual’s venous thromboembolism (VTE) risk based on underlying conditions, iatrogenic factors, injury-related factors, and age, within 24 hours of admission.
"Patients with [RAP] scores of 10 or higher received bilateral lower-extremity venous duplex ultrasounds at the time of admission and then weekly throughout their ICU stay," Dr. Thorson said, noting that logistic regression was performed on risk factors to identify independent predictors of VTE development. Among the risk factors considered were RAP score, RAP score higher than 20, femoral central venous catheterization for more than 24 hours, operative intervention duration longer than 2 hours, lower-extremity fracture, pelvic fracture, and spinal cord injury with paraplegia.
Of 534 trauma ICU admissions during the study period, 106 patients (mean age, 47 years) were identified as high risk based on their RAP score. Blunt trauma was the primary mechanism of injury in 79% of the population, and the mean injury severity score of the predominantly male (74%) high-risk population was 30, said Dr. Thorson.
Routine VDU screening identified 30 VTEs, including 20 that were asymptomatic and 10 that were symptomatic, despite the patients having received thromboprophylaxis (heparin 5,000 U every 8 hours or dalteparin 5,000 U daily), Dr. Thorson reported. Four of the symptomatic events were pulmonary emboli, and of the asymptomatic VTEs, six were identified on admission, seven were identified within the first week of admission, and four were identified within 2 weeks of admission, he said.
A comparison of those who did and did not develop VTEs showed significant differences in the number of risk factors, overall RAP score, and RAP score greater than 20, Dr. Thorson reported. Specifically, those in the non-VTE group averaged five risk factors compared with seven in the VTE group, and the respective median RAP scores were 14 and 19, he said. In addition, 6 patients in the non-VTE and 11 in the VTE group had RAP scores higher than 20. In the stepwise logistic regression analysis, RAP score and a combination of pelvic fracture and prolonged operative intervention were independent predictors of VTE development, he said.
Prescreening trauma patients with RAP is useful for identifying patients at increased risk of VTE who may be candidates for increased surveillance, according to Dr. Thorson. "There is plenty of debate with regard to the utility and cost effectiveness of routine screening, as well as the benefit of identifying asymptomatic deep vein thromboses," Dr. Thorson said in an interview.
"Ideally, we hope to find a decrease in the rate of pulmonary embolism as a result of screening, as this consequence can be devastating."
An important implication of the screening protocol, however, is identifying that DVT/VTE should not be included on the Centers for Medicare and Medicaid Services’ list of preventable complications (defined as errors in medical care that are clearly identifiable and preventable, and thus may no longer be eligible for reimbursement).
"A decision to no longer pay for [VTE] treatment could have devastating effects on many urban trauma centers," Dr. Thorson stressed.
The prescreening study was supported by grants from the Office of Naval Research and the U.S. Army Medical Research and Materiel Command. Dr. Thorson reported that he had no relevant financial disclosures.
HOUSTON – Nearly 30% of trauma patients who were identified upon admission as being high risk for venous thromboembolism using a validated risk assessment tool went on to develop the thrombotic condition during their ICU stay, a study has shown.
Importantly, the deep vein thromboses in most of these patients were asymptomatic and might have gone undetected with potentially life-threatening consequences but for periodic ultrasound screening, Dr. Chad Thorson reported at the annual congress of the Society of Critical Care Medicine.
"Routine venous thromboembolism screening in the trauma population has been widely debated, and there currently is no protocol for it," according to Dr. Thorson of the Ryder Trauma Center at the University of Miami. Although the principal diagnostic screening tool – venous duplex ultrasound (VDU) – is not considered cost effective for screening all trauma patients, the investigators sought to determine whether prescreening trauma patients using the risk assessment profile (RAP) would yield a cohort of high- risk patients in whom increased vigilance and VDU screening are warranted (J. Trauma 1997;42:100-3).
Toward this end, all patients admitted to the Ryder Center’s level 1 trauma intensive care unit from November 2009 through January 2012 were prospectively screened with RAP, which stratifies an individual’s venous thromboembolism (VTE) risk based on underlying conditions, iatrogenic factors, injury-related factors, and age, within 24 hours of admission.
"Patients with [RAP] scores of 10 or higher received bilateral lower-extremity venous duplex ultrasounds at the time of admission and then weekly throughout their ICU stay," Dr. Thorson said, noting that logistic regression was performed on risk factors to identify independent predictors of VTE development. Among the risk factors considered were RAP score, RAP score higher than 20, femoral central venous catheterization for more than 24 hours, operative intervention duration longer than 2 hours, lower-extremity fracture, pelvic fracture, and spinal cord injury with paraplegia.
Of 534 trauma ICU admissions during the study period, 106 patients (mean age, 47 years) were identified as high risk based on their RAP score. Blunt trauma was the primary mechanism of injury in 79% of the population, and the mean injury severity score of the predominantly male (74%) high-risk population was 30, said Dr. Thorson.
Routine VDU screening identified 30 VTEs, including 20 that were asymptomatic and 10 that were symptomatic, despite the patients having received thromboprophylaxis (heparin 5,000 U every 8 hours or dalteparin 5,000 U daily), Dr. Thorson reported. Four of the symptomatic events were pulmonary emboli, and of the asymptomatic VTEs, six were identified on admission, seven were identified within the first week of admission, and four were identified within 2 weeks of admission, he said.
A comparison of those who did and did not develop VTEs showed significant differences in the number of risk factors, overall RAP score, and RAP score greater than 20, Dr. Thorson reported. Specifically, those in the non-VTE group averaged five risk factors compared with seven in the VTE group, and the respective median RAP scores were 14 and 19, he said. In addition, 6 patients in the non-VTE and 11 in the VTE group had RAP scores higher than 20. In the stepwise logistic regression analysis, RAP score and a combination of pelvic fracture and prolonged operative intervention were independent predictors of VTE development, he said.
Prescreening trauma patients with RAP is useful for identifying patients at increased risk of VTE who may be candidates for increased surveillance, according to Dr. Thorson. "There is plenty of debate with regard to the utility and cost effectiveness of routine screening, as well as the benefit of identifying asymptomatic deep vein thromboses," Dr. Thorson said in an interview.
"Ideally, we hope to find a decrease in the rate of pulmonary embolism as a result of screening, as this consequence can be devastating."
An important implication of the screening protocol, however, is identifying that DVT/VTE should not be included on the Centers for Medicare and Medicaid Services’ list of preventable complications (defined as errors in medical care that are clearly identifiable and preventable, and thus may no longer be eligible for reimbursement).
"A decision to no longer pay for [VTE] treatment could have devastating effects on many urban trauma centers," Dr. Thorson stressed.
The prescreening study was supported by grants from the Office of Naval Research and the U.S. Army Medical Research and Materiel Command. Dr. Thorson reported that he had no relevant financial disclosures.
FROM THE ANNUAL CONGRESS OF THE SOCIETY OF CRITICAL CARE MEDICINE
Major Finding: Of 106 trauma patients identified through a prescreening protocol as being high risk for venous thromboembolism, 30 developed the condition during their ICU stay despite their receiving standard thromboprophylaxis.
Data Source: A prospective study in which 106 patients deemed to be at high risk of venous thromboembolism underwent venous duplex ultrasound at the time of admission and then weekly throughout their ICU stay.
Disclosures: The prescreening study was supported by grants from the Office of Naval Research and the U.S. Army Medical Research and Materiel Command. Dr. Thorson reported that he had no relevant financial disclosures.
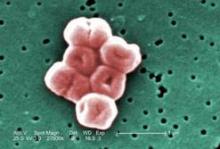
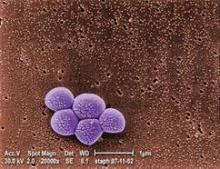
Screen Open-Airway Surgery Patients for MRSA
Children who are to have open airway surgery should first be screened for methicillin-resistant Staphylococcus aureus colonization because the prevalence is particularly high in this patient group and treatment drastically reduces postoperative infections, graft loss, and wound dehiscence, researchers reported.
In a retrospective cohort study at a single tertiary pediatric medical center, the prevalence of MRSA colonization was 32.5% during a 2-year period among 175 children who underwent 197 open airway operations, a rate considerably higher than has been reported in patients undergoing other types of surgery, said Dr. Melissa McCarty Statham of the department of otolaryngology–head and neck surgery, Emory University, Atlanta, and her associates. The findings were reported in the February issue of the Archives of Otolaryngology and Head & Neck Surgery.
Because these MRSA-colonized patients were identified and treated appropriately, they did not develop any postoperative MRSA infections, graft losses, or cases of surgical site dehiscence, the investigators noted.
Dr. McCarty Statham and her colleagues studied this issue because, "in our experience, MRSA infection in open airway procedures can be a devastating complication." Such procedures include laryngotracheal reconstruction and grafting, correction of laryngotracheoesophageal clefts, repair of tracheoesophageal fistulas, and laryngotracheal separations.
These patients are at high risk for MRSA colonization because most are preterm; have been tracheotomized; and have serious comorbidities such as pulmonary, gastrointestinal, and cardiac disease. "We consider these factors to be proxies for frequent hospitalization and exposure to antibiotics," the researchers said.
They assessed the 175 patients who underwent such surgery (at a median age of 4 years) at the Cincinnati Children’s Hospital Medical Center in the 2 years after a program of MRSA screening and treatment had been instituted there. Their purpose was to document the prevalence of MRSA colonization in this vulnerable patient population and to assess the effect of the program. Preoperatively, all patients were cultured for MRSA at the nares, perianal area, axila, gastrostomy tube (if present), and tracheotomy tube aspirate (if present).
Colonized patients were given double-strength trimethoprim-sulfamethoxazole empirically for 72 hours before surgery, with clindamycin serving as an alternative in patients who were allergic to sulfa drugs or were carrying organisms resistant to TMP-SMX. Patients with positive nasal cultures also received intranasal mupirocin twice daily.
Perioperatively, colonized patients received either intravenous vancomycin or clindamycin. Postoperatively, they received the same antibiotic regimen for 14 days as they had been given before surgery.
No MRSA-associated infections developed in patients treated according to this protocol, Dr. McCarty Statham and her associates said (Arch. Otolaryngol. Head Neck Surg. 2012;138:153-7).
Postoperative rates of any infection were comparable between the patients colonized with MRSA and those not colonized. There were 10 infections in the MRSA-positive patients (a rate of 15.9%) and 23 infections in the noncolonized patients (a rate of 17.4%).
All 10 infections in the MRSA-colonized patients were caused by nosocomial non-MRSA organisms, as were 19 of the 23 infections in the noncolonized patients.
Three patients who had been MRSA-negative at screening nevertheless developed postoperative MRSA infections after surgery, suggesting that their MRSA was acquired during this hospitalization, the investigators said.
Overall, there were two failures of laryngotracheal reconstruction cartilage grafts and one case of surgical site dehiscence, but none of them occurred in MRSA-positive patients. One graft failure was attributed to impaired wound healing as a result of corticosteroid use; the other to beta-hemolytic Streptococcus infection. The dehiscence was caused by Haemophilus influenzae infection at the surgical site.
This finding suggests that "there is an inherent risk of graft loss and dehiscence in all patients who undergo airway surgery. Infections other than MRSA may be causative factors," Dr. McCarty Statham and her associates noted.
"In view of our results, we advise instituting MRSA screening and treatment protocols in patients undergoing airway surgery," they added.
One of Dr. McCarty Statham’s associates reported being an adviser or consultant to Acclarent, Gyrus/Olympus, Boston Medical Products, Hood Laboratories, Bryan Medical, and Karl Storz.
Children who are to have open airway surgery should first be screened for methicillin-resistant Staphylococcus aureus colonization because the prevalence is particularly high in this patient group and treatment drastically reduces postoperative infections, graft loss, and wound dehiscence, researchers reported.
In a retrospective cohort study at a single tertiary pediatric medical center, the prevalence of MRSA colonization was 32.5% during a 2-year period among 175 children who underwent 197 open airway operations, a rate considerably higher than has been reported in patients undergoing other types of surgery, said Dr. Melissa McCarty Statham of the department of otolaryngology–head and neck surgery, Emory University, Atlanta, and her associates. The findings were reported in the February issue of the Archives of Otolaryngology and Head & Neck Surgery.
Because these MRSA-colonized patients were identified and treated appropriately, they did not develop any postoperative MRSA infections, graft losses, or cases of surgical site dehiscence, the investigators noted.
Dr. McCarty Statham and her colleagues studied this issue because, "in our experience, MRSA infection in open airway procedures can be a devastating complication." Such procedures include laryngotracheal reconstruction and grafting, correction of laryngotracheoesophageal clefts, repair of tracheoesophageal fistulas, and laryngotracheal separations.
These patients are at high risk for MRSA colonization because most are preterm; have been tracheotomized; and have serious comorbidities such as pulmonary, gastrointestinal, and cardiac disease. "We consider these factors to be proxies for frequent hospitalization and exposure to antibiotics," the researchers said.
They assessed the 175 patients who underwent such surgery (at a median age of 4 years) at the Cincinnati Children’s Hospital Medical Center in the 2 years after a program of MRSA screening and treatment had been instituted there. Their purpose was to document the prevalence of MRSA colonization in this vulnerable patient population and to assess the effect of the program. Preoperatively, all patients were cultured for MRSA at the nares, perianal area, axila, gastrostomy tube (if present), and tracheotomy tube aspirate (if present).
Colonized patients were given double-strength trimethoprim-sulfamethoxazole empirically for 72 hours before surgery, with clindamycin serving as an alternative in patients who were allergic to sulfa drugs or were carrying organisms resistant to TMP-SMX. Patients with positive nasal cultures also received intranasal mupirocin twice daily.
Perioperatively, colonized patients received either intravenous vancomycin or clindamycin. Postoperatively, they received the same antibiotic regimen for 14 days as they had been given before surgery.
No MRSA-associated infections developed in patients treated according to this protocol, Dr. McCarty Statham and her associates said (Arch. Otolaryngol. Head Neck Surg. 2012;138:153-7).
Postoperative rates of any infection were comparable between the patients colonized with MRSA and those not colonized. There were 10 infections in the MRSA-positive patients (a rate of 15.9%) and 23 infections in the noncolonized patients (a rate of 17.4%).
All 10 infections in the MRSA-colonized patients were caused by nosocomial non-MRSA organisms, as were 19 of the 23 infections in the noncolonized patients.
Three patients who had been MRSA-negative at screening nevertheless developed postoperative MRSA infections after surgery, suggesting that their MRSA was acquired during this hospitalization, the investigators said.
Overall, there were two failures of laryngotracheal reconstruction cartilage grafts and one case of surgical site dehiscence, but none of them occurred in MRSA-positive patients. One graft failure was attributed to impaired wound healing as a result of corticosteroid use; the other to beta-hemolytic Streptococcus infection. The dehiscence was caused by Haemophilus influenzae infection at the surgical site.
This finding suggests that "there is an inherent risk of graft loss and dehiscence in all patients who undergo airway surgery. Infections other than MRSA may be causative factors," Dr. McCarty Statham and her associates noted.
"In view of our results, we advise instituting MRSA screening and treatment protocols in patients undergoing airway surgery," they added.
One of Dr. McCarty Statham’s associates reported being an adviser or consultant to Acclarent, Gyrus/Olympus, Boston Medical Products, Hood Laboratories, Bryan Medical, and Karl Storz.
Children who are to have open airway surgery should first be screened for methicillin-resistant Staphylococcus aureus colonization because the prevalence is particularly high in this patient group and treatment drastically reduces postoperative infections, graft loss, and wound dehiscence, researchers reported.
In a retrospective cohort study at a single tertiary pediatric medical center, the prevalence of MRSA colonization was 32.5% during a 2-year period among 175 children who underwent 197 open airway operations, a rate considerably higher than has been reported in patients undergoing other types of surgery, said Dr. Melissa McCarty Statham of the department of otolaryngology–head and neck surgery, Emory University, Atlanta, and her associates. The findings were reported in the February issue of the Archives of Otolaryngology and Head & Neck Surgery.
Because these MRSA-colonized patients were identified and treated appropriately, they did not develop any postoperative MRSA infections, graft losses, or cases of surgical site dehiscence, the investigators noted.
Dr. McCarty Statham and her colleagues studied this issue because, "in our experience, MRSA infection in open airway procedures can be a devastating complication." Such procedures include laryngotracheal reconstruction and grafting, correction of laryngotracheoesophageal clefts, repair of tracheoesophageal fistulas, and laryngotracheal separations.
These patients are at high risk for MRSA colonization because most are preterm; have been tracheotomized; and have serious comorbidities such as pulmonary, gastrointestinal, and cardiac disease. "We consider these factors to be proxies for frequent hospitalization and exposure to antibiotics," the researchers said.
They assessed the 175 patients who underwent such surgery (at a median age of 4 years) at the Cincinnati Children’s Hospital Medical Center in the 2 years after a program of MRSA screening and treatment had been instituted there. Their purpose was to document the prevalence of MRSA colonization in this vulnerable patient population and to assess the effect of the program. Preoperatively, all patients were cultured for MRSA at the nares, perianal area, axila, gastrostomy tube (if present), and tracheotomy tube aspirate (if present).
Colonized patients were given double-strength trimethoprim-sulfamethoxazole empirically for 72 hours before surgery, with clindamycin serving as an alternative in patients who were allergic to sulfa drugs or were carrying organisms resistant to TMP-SMX. Patients with positive nasal cultures also received intranasal mupirocin twice daily.
Perioperatively, colonized patients received either intravenous vancomycin or clindamycin. Postoperatively, they received the same antibiotic regimen for 14 days as they had been given before surgery.
No MRSA-associated infections developed in patients treated according to this protocol, Dr. McCarty Statham and her associates said (Arch. Otolaryngol. Head Neck Surg. 2012;138:153-7).
Postoperative rates of any infection were comparable between the patients colonized with MRSA and those not colonized. There were 10 infections in the MRSA-positive patients (a rate of 15.9%) and 23 infections in the noncolonized patients (a rate of 17.4%).
All 10 infections in the MRSA-colonized patients were caused by nosocomial non-MRSA organisms, as were 19 of the 23 infections in the noncolonized patients.
Three patients who had been MRSA-negative at screening nevertheless developed postoperative MRSA infections after surgery, suggesting that their MRSA was acquired during this hospitalization, the investigators said.
Overall, there were two failures of laryngotracheal reconstruction cartilage grafts and one case of surgical site dehiscence, but none of them occurred in MRSA-positive patients. One graft failure was attributed to impaired wound healing as a result of corticosteroid use; the other to beta-hemolytic Streptococcus infection. The dehiscence was caused by Haemophilus influenzae infection at the surgical site.
This finding suggests that "there is an inherent risk of graft loss and dehiscence in all patients who undergo airway surgery. Infections other than MRSA may be causative factors," Dr. McCarty Statham and her associates noted.
"In view of our results, we advise instituting MRSA screening and treatment protocols in patients undergoing airway surgery," they added.
One of Dr. McCarty Statham’s associates reported being an adviser or consultant to Acclarent, Gyrus/Olympus, Boston Medical Products, Hood Laboratories, Bryan Medical, and Karl Storz.
FROM ARCHIVES OF OTOLARYNGOLOGY AND HEAD & NECK SURGERY
Major Finding: The overall rate of MRSA colonization was 33%, but no MRSA infections developed in the screened and treated carriers; rates of any postoperative infection were comparable between colonized (15.9%) and noncolonized (17.4%) patients.
Data Source: This was a retrospective cohort study of 175 children who underwent 197 open airway surgeries at a single pediatric medical center in a 2-year period.
Disclosures: One of Dr. McCarty Statham’s associates reported ties to Acclarent, Gyrus/Olympus, Boston Medical Products, Hood Laboratories, Bryan Medical, and Karl Storz.
Many Updates for Hospitalists Promised at Perioperative Medicine Summit
MIAMI – The Perioperative Medicine Summit in Miami Beach promises to deliver several clinical updates for hospitalists presented in innovative and interactive formats, according to summit director Dr. Amir K. Jaffer.
"The meeting in general is about patients having surgery. It’s been documented time and again in surveys that a large number of hospitalists across the country spend part of their time managing the medical aspect of surgical patients," Dr. Jaffer said in an interview.
Therefore, attendees will learn strategies and tools to better manage patients in the perioperative period, a core competency of the Society of Hospital Medicine. Dr. Jaffer is division chief of hospital medicine within the department of medicine at the University of Miami.
The meeting will run from March 15-17. During a plenary session scheduled to kick off the meeting, Dr. Thanjavur S. Ravikumar will outline his models to improve hospitalwide patient outcomes. He will explain how his strategies also decrease health care utilization and costs. Dr. Ravikumar is the chief quality officer, surgery and interventional procedures, and director of the center for surgical innovation at Geisinger Health System in Wilkes Barre, Pa.
A point-counterpoint session on optimization of deep vein thrombosis prophylaxis in major joint replacement surgery is expected to be another highlight. The back and forth between thromboembolism specialist James D. Douketis and orthopedic surgeon Cliff W. Colwell is sure to include relevant clinical guidelines just released in February by the American College of Chest Physicians, Dr. Jaffer said.
Dr. Jaffer, who is on the board of advisers for Hospitalist News, will also present at the meeting. "I’m going to be talking about the perioperative management of new and old antithrombotic therapies."
The second day of the summit is set to start with relevant and practical talk on the role of hospitalist medicine in the era of value-based care. Dr. Joseph Ming Wah Li will share his unique perspective as current president of the Society for Hospital Medicine.
Rapid-fire, 1-minute perioperative consults are a new feature of the summit this year. These will include advice on identification of noncardiopulmonary triggers for transfusion in postoperative anemia, with a discussion of blood transfusion alternatives. Other topics include when noninvasive coronary assessment is indicated for asymptomatic patients undergoing surgery for cancer and whether discontinuation of immunomodulatory medications in the perioperative period is warranted. The idea for these rapid-fire consults came from similar and well-attended sessions at the American College of Physicians meeting in which experts answer specific clinical questions.
The summit has a global reach, Dr. Jaffer said. "We do have people coming from all over the world ... including attendees signed up from New Zealand, Australia, and Singapore." In addition to hospitalists, attendees will include internists, anesthesiologists, physician assistants, and nurse practitioners.
The scope of the summit also goes beyond a single-institution or regional meeting, he added. This is in large part due to the summit codirectors and cosponsors. For example, Dr. Franklin A. Michota Jr. who is on the medicine faculty at the Cleveland Clinic Lerner College of Medicine at Case Western Reserve University brings his expertise as director of academic affairs for the department of hospital medicine at the Cleveland Clinic. The Cleveland Clinic is cosponsoring the meeting along with the University of Miami Miller School of Medicine. Dr. Michota is the medical editor for Hospitalist News. Another codirector, Dr. Darin J. Correll, is director of the acute postoperative pain management service at Brigham and Women’s Hospital in Boston and a member of the governing board of the Society for Perioperative Assessment and Quality Improvement, a third cosponsor of the meeting.
Visit periopmedicine.org for additional information and updates on the seventh Perioperative Medicine Summit.
MIAMI – The Perioperative Medicine Summit in Miami Beach promises to deliver several clinical updates for hospitalists presented in innovative and interactive formats, according to summit director Dr. Amir K. Jaffer.
"The meeting in general is about patients having surgery. It’s been documented time and again in surveys that a large number of hospitalists across the country spend part of their time managing the medical aspect of surgical patients," Dr. Jaffer said in an interview.
Therefore, attendees will learn strategies and tools to better manage patients in the perioperative period, a core competency of the Society of Hospital Medicine. Dr. Jaffer is division chief of hospital medicine within the department of medicine at the University of Miami.
The meeting will run from March 15-17. During a plenary session scheduled to kick off the meeting, Dr. Thanjavur S. Ravikumar will outline his models to improve hospitalwide patient outcomes. He will explain how his strategies also decrease health care utilization and costs. Dr. Ravikumar is the chief quality officer, surgery and interventional procedures, and director of the center for surgical innovation at Geisinger Health System in Wilkes Barre, Pa.
A point-counterpoint session on optimization of deep vein thrombosis prophylaxis in major joint replacement surgery is expected to be another highlight. The back and forth between thromboembolism specialist James D. Douketis and orthopedic surgeon Cliff W. Colwell is sure to include relevant clinical guidelines just released in February by the American College of Chest Physicians, Dr. Jaffer said.
Dr. Jaffer, who is on the board of advisers for Hospitalist News, will also present at the meeting. "I’m going to be talking about the perioperative management of new and old antithrombotic therapies."
The second day of the summit is set to start with relevant and practical talk on the role of hospitalist medicine in the era of value-based care. Dr. Joseph Ming Wah Li will share his unique perspective as current president of the Society for Hospital Medicine.
Rapid-fire, 1-minute perioperative consults are a new feature of the summit this year. These will include advice on identification of noncardiopulmonary triggers for transfusion in postoperative anemia, with a discussion of blood transfusion alternatives. Other topics include when noninvasive coronary assessment is indicated for asymptomatic patients undergoing surgery for cancer and whether discontinuation of immunomodulatory medications in the perioperative period is warranted. The idea for these rapid-fire consults came from similar and well-attended sessions at the American College of Physicians meeting in which experts answer specific clinical questions.
The summit has a global reach, Dr. Jaffer said. "We do have people coming from all over the world ... including attendees signed up from New Zealand, Australia, and Singapore." In addition to hospitalists, attendees will include internists, anesthesiologists, physician assistants, and nurse practitioners.
The scope of the summit also goes beyond a single-institution or regional meeting, he added. This is in large part due to the summit codirectors and cosponsors. For example, Dr. Franklin A. Michota Jr. who is on the medicine faculty at the Cleveland Clinic Lerner College of Medicine at Case Western Reserve University brings his expertise as director of academic affairs for the department of hospital medicine at the Cleveland Clinic. The Cleveland Clinic is cosponsoring the meeting along with the University of Miami Miller School of Medicine. Dr. Michota is the medical editor for Hospitalist News. Another codirector, Dr. Darin J. Correll, is director of the acute postoperative pain management service at Brigham and Women’s Hospital in Boston and a member of the governing board of the Society for Perioperative Assessment and Quality Improvement, a third cosponsor of the meeting.
Visit periopmedicine.org for additional information and updates on the seventh Perioperative Medicine Summit.
MIAMI – The Perioperative Medicine Summit in Miami Beach promises to deliver several clinical updates for hospitalists presented in innovative and interactive formats, according to summit director Dr. Amir K. Jaffer.
"The meeting in general is about patients having surgery. It’s been documented time and again in surveys that a large number of hospitalists across the country spend part of their time managing the medical aspect of surgical patients," Dr. Jaffer said in an interview.
Therefore, attendees will learn strategies and tools to better manage patients in the perioperative period, a core competency of the Society of Hospital Medicine. Dr. Jaffer is division chief of hospital medicine within the department of medicine at the University of Miami.
The meeting will run from March 15-17. During a plenary session scheduled to kick off the meeting, Dr. Thanjavur S. Ravikumar will outline his models to improve hospitalwide patient outcomes. He will explain how his strategies also decrease health care utilization and costs. Dr. Ravikumar is the chief quality officer, surgery and interventional procedures, and director of the center for surgical innovation at Geisinger Health System in Wilkes Barre, Pa.
A point-counterpoint session on optimization of deep vein thrombosis prophylaxis in major joint replacement surgery is expected to be another highlight. The back and forth between thromboembolism specialist James D. Douketis and orthopedic surgeon Cliff W. Colwell is sure to include relevant clinical guidelines just released in February by the American College of Chest Physicians, Dr. Jaffer said.
Dr. Jaffer, who is on the board of advisers for Hospitalist News, will also present at the meeting. "I’m going to be talking about the perioperative management of new and old antithrombotic therapies."
The second day of the summit is set to start with relevant and practical talk on the role of hospitalist medicine in the era of value-based care. Dr. Joseph Ming Wah Li will share his unique perspective as current president of the Society for Hospital Medicine.
Rapid-fire, 1-minute perioperative consults are a new feature of the summit this year. These will include advice on identification of noncardiopulmonary triggers for transfusion in postoperative anemia, with a discussion of blood transfusion alternatives. Other topics include when noninvasive coronary assessment is indicated for asymptomatic patients undergoing surgery for cancer and whether discontinuation of immunomodulatory medications in the perioperative period is warranted. The idea for these rapid-fire consults came from similar and well-attended sessions at the American College of Physicians meeting in which experts answer specific clinical questions.
The summit has a global reach, Dr. Jaffer said. "We do have people coming from all over the world ... including attendees signed up from New Zealand, Australia, and Singapore." In addition to hospitalists, attendees will include internists, anesthesiologists, physician assistants, and nurse practitioners.
The scope of the summit also goes beyond a single-institution or regional meeting, he added. This is in large part due to the summit codirectors and cosponsors. For example, Dr. Franklin A. Michota Jr. who is on the medicine faculty at the Cleveland Clinic Lerner College of Medicine at Case Western Reserve University brings his expertise as director of academic affairs for the department of hospital medicine at the Cleveland Clinic. The Cleveland Clinic is cosponsoring the meeting along with the University of Miami Miller School of Medicine. Dr. Michota is the medical editor for Hospitalist News. Another codirector, Dr. Darin J. Correll, is director of the acute postoperative pain management service at Brigham and Women’s Hospital in Boston and a member of the governing board of the Society for Perioperative Assessment and Quality Improvement, a third cosponsor of the meeting.
Visit periopmedicine.org for additional information and updates on the seventh Perioperative Medicine Summit.
Alcohol Withdrawal Syndrome Worsens Cancer Surgery Outcomes
MIAMI BEACH – Patients with head and neck cancers who develop alcohol withdrawal syndrome perioperatively experience significantly more complications after undergoing surgery, a large database analysis indicates.
The presence of withdrawal symptoms was associated with a 25% incidence of postoperative complications, compared with 14% among patients who abused alcohol and 7% among those without alcohol abuse, Dr. Dane J. Genther said at the Triological Society’s Combined Sections Meeting. The risk for wound complications was nearly double in this population (odds ratio, 1.9).
Dr. Genther, a resident in otolaryngologyhead and neck surgery at Johns Hopkins Hospital in Baltimore, and his associates used ICD-9 codes in the Nationwide Inpatient Sample discharge database to identify more than 92,000 patients who underwent an ablative procedure for head and neck cancer in 2003-2008. The retrospective, cross-sectional study included patients with malignant oral cavity, laryngeal, hypopharyngeal, and oropharyngeal neoplasms.
In a multivariate analysis, alcohol withdrawal syndrome was significantly more likely for patients undergoing a major procedure (OR, 2.0) and was significantly associated with Medicare payer status and a need for additional health care following discharge, Dr. Genther said.
The researchers found no significant association between alcohol withdrawal syndrome and increased risk for postoperative infections or in-hospital mortality, but there was a significant increase in hospital stay and related costs associated with the syndrome.
Having a major procedure and experiencing alcohol withdrawal contributed approximately $15,000 per admission in 2011 U.S. dollars, Dr. Genther said.
The findings point to a need for alternatives to current alcohol withdrawal prevention therapies, Dr. Genther said. "Despite prophylaxis, which is our current treatment to attempt to stem the onset of alcohol withdrawal syndrome, complications do occur and they are no less severe or frequent than in the absence of prophylaxis."
Abstinence from alcohol for at least 4 weeks is another strategy proposed to minimize risk of alcohol withdrawal syndrome for any at-risk surgical patient, said Dr. Genther. However, he added, "for many cancer patients, especially those with more advanced disease, waiting a prolonged period of time to possibly gain that benefit from abstinence is not necessarily a viable option."
Another aim of the study was to assess factors contributing to alcohol abuse. Patients aged 40-64 years had the highest proportion of alcohol abuse, and this age range was a significant factor (OR, 2.37). Those who abused alcohol were more often male and more often underwent major procedures, Dr. Genther said at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. In addition, alcohol abuse was significantly associated with pneumonia and need for additional postdischarge health care.
Dr. Genther received a G. Slaughter Fitz-Hugh Resident Research Award for this study from the Triological Society. He reported having no financial disclosures.
MIAMI BEACH – Patients with head and neck cancers who develop alcohol withdrawal syndrome perioperatively experience significantly more complications after undergoing surgery, a large database analysis indicates.
The presence of withdrawal symptoms was associated with a 25% incidence of postoperative complications, compared with 14% among patients who abused alcohol and 7% among those without alcohol abuse, Dr. Dane J. Genther said at the Triological Society’s Combined Sections Meeting. The risk for wound complications was nearly double in this population (odds ratio, 1.9).
Dr. Genther, a resident in otolaryngologyhead and neck surgery at Johns Hopkins Hospital in Baltimore, and his associates used ICD-9 codes in the Nationwide Inpatient Sample discharge database to identify more than 92,000 patients who underwent an ablative procedure for head and neck cancer in 2003-2008. The retrospective, cross-sectional study included patients with malignant oral cavity, laryngeal, hypopharyngeal, and oropharyngeal neoplasms.
In a multivariate analysis, alcohol withdrawal syndrome was significantly more likely for patients undergoing a major procedure (OR, 2.0) and was significantly associated with Medicare payer status and a need for additional health care following discharge, Dr. Genther said.
The researchers found no significant association between alcohol withdrawal syndrome and increased risk for postoperative infections or in-hospital mortality, but there was a significant increase in hospital stay and related costs associated with the syndrome.
Having a major procedure and experiencing alcohol withdrawal contributed approximately $15,000 per admission in 2011 U.S. dollars, Dr. Genther said.
The findings point to a need for alternatives to current alcohol withdrawal prevention therapies, Dr. Genther said. "Despite prophylaxis, which is our current treatment to attempt to stem the onset of alcohol withdrawal syndrome, complications do occur and they are no less severe or frequent than in the absence of prophylaxis."
Abstinence from alcohol for at least 4 weeks is another strategy proposed to minimize risk of alcohol withdrawal syndrome for any at-risk surgical patient, said Dr. Genther. However, he added, "for many cancer patients, especially those with more advanced disease, waiting a prolonged period of time to possibly gain that benefit from abstinence is not necessarily a viable option."
Another aim of the study was to assess factors contributing to alcohol abuse. Patients aged 40-64 years had the highest proportion of alcohol abuse, and this age range was a significant factor (OR, 2.37). Those who abused alcohol were more often male and more often underwent major procedures, Dr. Genther said at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. In addition, alcohol abuse was significantly associated with pneumonia and need for additional postdischarge health care.
Dr. Genther received a G. Slaughter Fitz-Hugh Resident Research Award for this study from the Triological Society. He reported having no financial disclosures.
MIAMI BEACH – Patients with head and neck cancers who develop alcohol withdrawal syndrome perioperatively experience significantly more complications after undergoing surgery, a large database analysis indicates.
The presence of withdrawal symptoms was associated with a 25% incidence of postoperative complications, compared with 14% among patients who abused alcohol and 7% among those without alcohol abuse, Dr. Dane J. Genther said at the Triological Society’s Combined Sections Meeting. The risk for wound complications was nearly double in this population (odds ratio, 1.9).
Dr. Genther, a resident in otolaryngologyhead and neck surgery at Johns Hopkins Hospital in Baltimore, and his associates used ICD-9 codes in the Nationwide Inpatient Sample discharge database to identify more than 92,000 patients who underwent an ablative procedure for head and neck cancer in 2003-2008. The retrospective, cross-sectional study included patients with malignant oral cavity, laryngeal, hypopharyngeal, and oropharyngeal neoplasms.
In a multivariate analysis, alcohol withdrawal syndrome was significantly more likely for patients undergoing a major procedure (OR, 2.0) and was significantly associated with Medicare payer status and a need for additional health care following discharge, Dr. Genther said.
The researchers found no significant association between alcohol withdrawal syndrome and increased risk for postoperative infections or in-hospital mortality, but there was a significant increase in hospital stay and related costs associated with the syndrome.
Having a major procedure and experiencing alcohol withdrawal contributed approximately $15,000 per admission in 2011 U.S. dollars, Dr. Genther said.
The findings point to a need for alternatives to current alcohol withdrawal prevention therapies, Dr. Genther said. "Despite prophylaxis, which is our current treatment to attempt to stem the onset of alcohol withdrawal syndrome, complications do occur and they are no less severe or frequent than in the absence of prophylaxis."
Abstinence from alcohol for at least 4 weeks is another strategy proposed to minimize risk of alcohol withdrawal syndrome for any at-risk surgical patient, said Dr. Genther. However, he added, "for many cancer patients, especially those with more advanced disease, waiting a prolonged period of time to possibly gain that benefit from abstinence is not necessarily a viable option."
Another aim of the study was to assess factors contributing to alcohol abuse. Patients aged 40-64 years had the highest proportion of alcohol abuse, and this age range was a significant factor (OR, 2.37). Those who abused alcohol were more often male and more often underwent major procedures, Dr. Genther said at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. In addition, alcohol abuse was significantly associated with pneumonia and need for additional postdischarge health care.
Dr. Genther received a G. Slaughter Fitz-Hugh Resident Research Award for this study from the Triological Society. He reported having no financial disclosures.
FROM THE TRIOLOGICAL SOCIETY'S COMBINED SECTIONS MEETING
Major Finding: The presence of alcohol withdrawal symptoms was associated with a significantly higher incidence of postoperative complications, 25%, compared with 14% among patients who abused alcohol and 7% for those without alcohol abuse.
Data Source: Data were taken from a retrospective, cross-sectional study of 92,312 ablative procedures for head and neck cancer from the NIS database in 2003-2008.
Disclosures: Dr. Genther reported having no financial disclosures.
EDEN Trial Questions Restricting Nutrition to ALI Patients
HOUSTON – Restricting the amount of initial enteral intake in mechanically ventilated patients who have acute lung injury neither reduces the duration of mechanical ventilation nor improves mortality relative to full enteral feeding, but the nutritional strategy may be slightly easier on the stomach, according to a study reported Feb. 5 at the annual meeting of the Society of Critical Care Medicine Critical Care Congress.
The importance of nutrition support in critically ill patients with acute lung injury (ALI) is well accepted as a means of maintaining gut integrity, modulating both stress and the systemic immune response, and attenuating disease severity, but conflicting data regarding the timing, formulation, and amount of enteral nutrition have contributed to uncertainty about the optimal feeding protocol, according to Dr. Todd W. Rice of Vanderbilt University Medical Center in Nashville, Tenn.
"How much nutrition we need to promote the protective benefits, we don’t know. Providing a little bit of nutrition (called trophic feeding) has been shown to decrease intestinal intolerances, compared with full-calorie feeds, but it may do so at the risk of malnutrition, worse immune function, and loss of muscle strength," he said. Full-calorie feeding, on the other hand, may lead to more intolerances, may cause hyperglycemia and other imbalances, may increase septic complications, and may fuel the inflammatory fire, he added.
In the current study, which was published simultaneously in JAMA, Dr. Rice and colleagues in the EDEN (Early Vs. Delayed Enteral Nutrition in ALI) trial, sought to examine the relative advantages of restricting the amount of initial enteral intake in mechanically ventilated ALI patients. Specifically, the prospective, randomized, open-label trial compared the effect on clinical outcomes and survival of initial trophic enteral feeding – approximately 25% of the full target feeding – with initial full-calorie feeding for the first 6 days of mechanical ventilation in ALI patients. "We hypothesized that reduced trophic feeding during the first [6 days] would increase ventilator-free days and reduce instances of gastrointestinal intolerances compared with the conventional full enteral nutrition strategy," he said.
"How much nutrition we need to promote the protective benefits, we don’t know."
The study’s primary end point was ventilator-free days through day 28; secondary end points were daily percentage of goal enteral feeding, frequency of gastrointestinal intolerances, 60-day mortality before hospital discharge with unassisted breathing, ICU- and organ failure–free days, and new infections (JAMA 2012 Feb. 5 [doi:10.1001/jama2012.137]).
The multicenter study population comprised 1,000 patients, from January 2008 through mid-April 2011, who were initiated on mechanical ventilation within 48 hours of developing ALI. Within 6 hours of randomization, enteric nutrition was initiated in 508 patients assigned to trophic nutrition and 492 assigned to full feeding, and was continued until death, extubation, or day 6, Dr. Rice explained. Per standard protocol, enteral nutrition in the full-feeding group began at 25 mL/hr and advanced to goal weights (25-30 kcal/day of nonprotein calories and 1.2-1.6 g/kg per day of protein) as quickly as possible; gastric residual volumes were checked every 6 hours while enteral feeding was increased. In the trophic group, enteral feeding was initiated at 10-20 kcal/hr and gastric residual volumes were checked every 12 hours. After 6 days, patients in the trophic group who still required mechanical ventilation were advanced to the full-energy feeding rates, he said.
Baseline characteristics of the two groups were similar, Dr. Rice noted. "The primary etiologies of lung injury in both groups of patients were pneumonia and sepsis, and the average APACHE III [Acute Physiology and Chronic Health Evaluation III] score was approximately 92. These were sick patients," he said. For the first 6 days, the full- and trophic feeding groups received 1,300 kcal/day and 400 kcal/day, respectively.
With respect to the primary end point (28 days), the average number of ventilator-free days in both groups was similar, at 14.9 in the trophic group and 15.0 in the full-feeding group. "There were also no differences in 60-day mortality, organ failure–free days, ICU-free days, or the incidence of infection between groups," he said. Similarly, with respect to body mass index category or lung injury severity, "there were no between-group differences in ventilator free days or survival."
The full-feeding group did have a higher number of gastrointestinal intolerances on any one day, and statistically significant increase on days 2 and 3, but the overall percentages of intolerances were low, Dr. Rice said. There were no differences in albumin and protein levels between the groups over the first 7 days, he said.
Regarding the immediate clinical relevance of the findings, Dr. Rice stressed that the study wasn’t designed as an equivalence trial, "so I can’t tell you both feeding strategies are similar, but you can look at the results." In fact, he said, although the study did not show a benefit other than improved gastrointestinal tolerance, his group has moved toward trophic feeds because of the ease of administration. "Our nurses love the trophic feeds. Starting at 10-20 cc/hr and running it for 6 days is a lot less hassle than worrying about trying to ramp it up and get to goals," he said.
"Looking ahead, there are a number of places to go" with this research, Dr. Rice said. "Some of the questions we’ve thought about are what role does this play in the [total parenteral nutrition] question, and whether we need to be feeding patients at all. Initially, we thought the idea of not feeding patients would be a hard study to sell, but with these data, it may not be an unreasonable thing to look at."
Dr. Rice disclosed no financial conflicts of interest.
HOUSTON – Restricting the amount of initial enteral intake in mechanically ventilated patients who have acute lung injury neither reduces the duration of mechanical ventilation nor improves mortality relative to full enteral feeding, but the nutritional strategy may be slightly easier on the stomach, according to a study reported Feb. 5 at the annual meeting of the Society of Critical Care Medicine Critical Care Congress.
The importance of nutrition support in critically ill patients with acute lung injury (ALI) is well accepted as a means of maintaining gut integrity, modulating both stress and the systemic immune response, and attenuating disease severity, but conflicting data regarding the timing, formulation, and amount of enteral nutrition have contributed to uncertainty about the optimal feeding protocol, according to Dr. Todd W. Rice of Vanderbilt University Medical Center in Nashville, Tenn.
"How much nutrition we need to promote the protective benefits, we don’t know. Providing a little bit of nutrition (called trophic feeding) has been shown to decrease intestinal intolerances, compared with full-calorie feeds, but it may do so at the risk of malnutrition, worse immune function, and loss of muscle strength," he said. Full-calorie feeding, on the other hand, may lead to more intolerances, may cause hyperglycemia and other imbalances, may increase septic complications, and may fuel the inflammatory fire, he added.
In the current study, which was published simultaneously in JAMA, Dr. Rice and colleagues in the EDEN (Early Vs. Delayed Enteral Nutrition in ALI) trial, sought to examine the relative advantages of restricting the amount of initial enteral intake in mechanically ventilated ALI patients. Specifically, the prospective, randomized, open-label trial compared the effect on clinical outcomes and survival of initial trophic enteral feeding – approximately 25% of the full target feeding – with initial full-calorie feeding for the first 6 days of mechanical ventilation in ALI patients. "We hypothesized that reduced trophic feeding during the first [6 days] would increase ventilator-free days and reduce instances of gastrointestinal intolerances compared with the conventional full enteral nutrition strategy," he said.
"How much nutrition we need to promote the protective benefits, we don’t know."
The study’s primary end point was ventilator-free days through day 28; secondary end points were daily percentage of goal enteral feeding, frequency of gastrointestinal intolerances, 60-day mortality before hospital discharge with unassisted breathing, ICU- and organ failure–free days, and new infections (JAMA 2012 Feb. 5 [doi:10.1001/jama2012.137]).
The multicenter study population comprised 1,000 patients, from January 2008 through mid-April 2011, who were initiated on mechanical ventilation within 48 hours of developing ALI. Within 6 hours of randomization, enteric nutrition was initiated in 508 patients assigned to trophic nutrition and 492 assigned to full feeding, and was continued until death, extubation, or day 6, Dr. Rice explained. Per standard protocol, enteral nutrition in the full-feeding group began at 25 mL/hr and advanced to goal weights (25-30 kcal/day of nonprotein calories and 1.2-1.6 g/kg per day of protein) as quickly as possible; gastric residual volumes were checked every 6 hours while enteral feeding was increased. In the trophic group, enteral feeding was initiated at 10-20 kcal/hr and gastric residual volumes were checked every 12 hours. After 6 days, patients in the trophic group who still required mechanical ventilation were advanced to the full-energy feeding rates, he said.
Baseline characteristics of the two groups were similar, Dr. Rice noted. "The primary etiologies of lung injury in both groups of patients were pneumonia and sepsis, and the average APACHE III [Acute Physiology and Chronic Health Evaluation III] score was approximately 92. These were sick patients," he said. For the first 6 days, the full- and trophic feeding groups received 1,300 kcal/day and 400 kcal/day, respectively.
With respect to the primary end point (28 days), the average number of ventilator-free days in both groups was similar, at 14.9 in the trophic group and 15.0 in the full-feeding group. "There were also no differences in 60-day mortality, organ failure–free days, ICU-free days, or the incidence of infection between groups," he said. Similarly, with respect to body mass index category or lung injury severity, "there were no between-group differences in ventilator free days or survival."
The full-feeding group did have a higher number of gastrointestinal intolerances on any one day, and statistically significant increase on days 2 and 3, but the overall percentages of intolerances were low, Dr. Rice said. There were no differences in albumin and protein levels between the groups over the first 7 days, he said.
Regarding the immediate clinical relevance of the findings, Dr. Rice stressed that the study wasn’t designed as an equivalence trial, "so I can’t tell you both feeding strategies are similar, but you can look at the results." In fact, he said, although the study did not show a benefit other than improved gastrointestinal tolerance, his group has moved toward trophic feeds because of the ease of administration. "Our nurses love the trophic feeds. Starting at 10-20 cc/hr and running it for 6 days is a lot less hassle than worrying about trying to ramp it up and get to goals," he said.
"Looking ahead, there are a number of places to go" with this research, Dr. Rice said. "Some of the questions we’ve thought about are what role does this play in the [total parenteral nutrition] question, and whether we need to be feeding patients at all. Initially, we thought the idea of not feeding patients would be a hard study to sell, but with these data, it may not be an unreasonable thing to look at."
Dr. Rice disclosed no financial conflicts of interest.
HOUSTON – Restricting the amount of initial enteral intake in mechanically ventilated patients who have acute lung injury neither reduces the duration of mechanical ventilation nor improves mortality relative to full enteral feeding, but the nutritional strategy may be slightly easier on the stomach, according to a study reported Feb. 5 at the annual meeting of the Society of Critical Care Medicine Critical Care Congress.
The importance of nutrition support in critically ill patients with acute lung injury (ALI) is well accepted as a means of maintaining gut integrity, modulating both stress and the systemic immune response, and attenuating disease severity, but conflicting data regarding the timing, formulation, and amount of enteral nutrition have contributed to uncertainty about the optimal feeding protocol, according to Dr. Todd W. Rice of Vanderbilt University Medical Center in Nashville, Tenn.
"How much nutrition we need to promote the protective benefits, we don’t know. Providing a little bit of nutrition (called trophic feeding) has been shown to decrease intestinal intolerances, compared with full-calorie feeds, but it may do so at the risk of malnutrition, worse immune function, and loss of muscle strength," he said. Full-calorie feeding, on the other hand, may lead to more intolerances, may cause hyperglycemia and other imbalances, may increase septic complications, and may fuel the inflammatory fire, he added.
In the current study, which was published simultaneously in JAMA, Dr. Rice and colleagues in the EDEN (Early Vs. Delayed Enteral Nutrition in ALI) trial, sought to examine the relative advantages of restricting the amount of initial enteral intake in mechanically ventilated ALI patients. Specifically, the prospective, randomized, open-label trial compared the effect on clinical outcomes and survival of initial trophic enteral feeding – approximately 25% of the full target feeding – with initial full-calorie feeding for the first 6 days of mechanical ventilation in ALI patients. "We hypothesized that reduced trophic feeding during the first [6 days] would increase ventilator-free days and reduce instances of gastrointestinal intolerances compared with the conventional full enteral nutrition strategy," he said.
"How much nutrition we need to promote the protective benefits, we don’t know."
The study’s primary end point was ventilator-free days through day 28; secondary end points were daily percentage of goal enteral feeding, frequency of gastrointestinal intolerances, 60-day mortality before hospital discharge with unassisted breathing, ICU- and organ failure–free days, and new infections (JAMA 2012 Feb. 5 [doi:10.1001/jama2012.137]).
The multicenter study population comprised 1,000 patients, from January 2008 through mid-April 2011, who were initiated on mechanical ventilation within 48 hours of developing ALI. Within 6 hours of randomization, enteric nutrition was initiated in 508 patients assigned to trophic nutrition and 492 assigned to full feeding, and was continued until death, extubation, or day 6, Dr. Rice explained. Per standard protocol, enteral nutrition in the full-feeding group began at 25 mL/hr and advanced to goal weights (25-30 kcal/day of nonprotein calories and 1.2-1.6 g/kg per day of protein) as quickly as possible; gastric residual volumes were checked every 6 hours while enteral feeding was increased. In the trophic group, enteral feeding was initiated at 10-20 kcal/hr and gastric residual volumes were checked every 12 hours. After 6 days, patients in the trophic group who still required mechanical ventilation were advanced to the full-energy feeding rates, he said.
Baseline characteristics of the two groups were similar, Dr. Rice noted. "The primary etiologies of lung injury in both groups of patients were pneumonia and sepsis, and the average APACHE III [Acute Physiology and Chronic Health Evaluation III] score was approximately 92. These were sick patients," he said. For the first 6 days, the full- and trophic feeding groups received 1,300 kcal/day and 400 kcal/day, respectively.
With respect to the primary end point (28 days), the average number of ventilator-free days in both groups was similar, at 14.9 in the trophic group and 15.0 in the full-feeding group. "There were also no differences in 60-day mortality, organ failure–free days, ICU-free days, or the incidence of infection between groups," he said. Similarly, with respect to body mass index category or lung injury severity, "there were no between-group differences in ventilator free days or survival."
The full-feeding group did have a higher number of gastrointestinal intolerances on any one day, and statistically significant increase on days 2 and 3, but the overall percentages of intolerances were low, Dr. Rice said. There were no differences in albumin and protein levels between the groups over the first 7 days, he said.
Regarding the immediate clinical relevance of the findings, Dr. Rice stressed that the study wasn’t designed as an equivalence trial, "so I can’t tell you both feeding strategies are similar, but you can look at the results." In fact, he said, although the study did not show a benefit other than improved gastrointestinal tolerance, his group has moved toward trophic feeds because of the ease of administration. "Our nurses love the trophic feeds. Starting at 10-20 cc/hr and running it for 6 days is a lot less hassle than worrying about trying to ramp it up and get to goals," he said.
"Looking ahead, there are a number of places to go" with this research, Dr. Rice said. "Some of the questions we’ve thought about are what role does this play in the [total parenteral nutrition] question, and whether we need to be feeding patients at all. Initially, we thought the idea of not feeding patients would be a hard study to sell, but with these data, it may not be an unreasonable thing to look at."
Dr. Rice disclosed no financial conflicts of interest.
FROM THE ANNUAL CONGRESS OF THE SOCIETY OF CRITICAL CARE MEDICINE
Skipping Antibiotic Guidelines Ups Trauma Surgical Infections
LAKE BUENA VISTA, FLA. – Just 49.3% of patients undergoing emergency trauma laparotomy received antibiotics in accordance with the Surgical Care Improvement Project guidelines in a multicenter, retrospective analysis of 306 patients.
"Many of the non-SCIP patients received the wrong antibiotic or antibiotics for too long after their index operation," lead author Brian P. Smith said at the annual meeting of the Eastern Association for the Surgery of Trauma.
Moreover, compliance with the guidelines slashed surgical site infection rates from 32.9% among patients with noncompliant antibiotic management to 16.6% (P less than .001).
The Surgical Care Improvement Project (SCIP) established surgical antibiotic prophylaxis guidelines as part of a collaborative effort by the Centers for Medicare and Medicaid Services and the Centers for Disease Control and Prevention to reduce surgical complications. While these antibiotic prophylaxis guidelines have become well established in patients undergoing elective operative procedures, they have never been studied in trauma patients undergoing emergency surgery, said Dr. Smith, a surgical resident at Temple University Hospital in Philadelphia.*
He reported on an analysis involving 306 trauma patients who survived for more than 4 days after undergoing emergency laparotomy within 2 hours of admission at two level 1 trauma centers during 2007 and 2008. Patients were compared on the basis of adherence to the following SCIP guidelines: prophylactic antibiotic given, antibiotic received within 1 hour prior to incision, correct antibiotic selection, and discontinuation of antibiotic within 24 hours after surgery.
Their mean age was 32 years, 70% had penetrating wounds, 44% had enteric injuries, and 20% had preoperative hypotension.
In all, 155 patients received noncompliant perioperative antibiotic management. Of these, 55% received no prophylaxis or incorrect antibiotics, 46% received antibiotics outside of the recommended 60-minute window, and 54% received them beyond the 24-hour limit, Dr. Smith said.
"It’s important to note these because they represent simple practice maneuvers that can be changed to help improve antibiotic stewardship in our trauma patients," he said.
The SCIP group spent significantly fewer days than the non-SCIP group in the ICU (mean 4 days vs. 7 days; P = .02) and in the hospital (mean 14 days vs. 19 days; P = .01), although no significant difference in mortality was detected (3% vs. 6%; P = .41).
Notably, Injury Severity Score was higher at admission in the non-SCIP group at 16 vs. 13 in the SCIP group (P = .03). Prehospital transfer time, which could influence the prolongation of antibiotics before surgery, was not available.
In a multivariate regression analysis that adjusted for such confounding factors as age, Injury Severity Score, shock, presence of enteric injury, transfusion requirements, damage control surgery, surgery duration, and hospital, complete adherence to the four SCIP guidelines independently decreased the risk of a surgical site infection (odds ratio, 0.448).
The non-SCIP group had significantly more enteric injuries than the SCIP group (52% vs. 35%; P = .027), and the rate of prolonged antibiotics was higher in patients with enteric injuries, compared with those without enteric injuries (38.6% vs. 19.4%; P = .001), Dr. Smith pointed out.
"This suggests the possibility that the extent of antibiotics rather than the enteric injuries themselves explained the wound infection rates in these two groups," he said.
Discussant Dr. John Santaniello, a critical care surgeon from Loyola University Chicago, Maywood, Ill., said the authors need to further elucidate antibiotic usage in patients with enteric injuries to distinguish true SCIP prophylaxis violations from empiric treatment for contamination.
He also questioned why the authors included only four of the six SCIP measures, omitting preoperative skin preparation and intraoperative normothermia maintenance, which have been shown to reduce surgical wound infections.
Dr. Smith said missing data and difficulty in abstracting data from handwritten records kept them from analyzing these two measures.
Attendee Dr. Patrick Reilly, chief of traumatology, surgical critical care, and emergency surgery at the University of Pennsylvania in Philadelphia, questioned how SCIP compliance was defined in a damage-control patient, and asked whether the investigators have a routine way of closing the skin when the fascia can be closed in these patients.
"For a number of years, we have had a practice – we don’t really call it a practice management guideline because we don’t really have any evidence for it – where we leave the skin open if we close the fascia, at least initially, because we’ve realized a high incidence of wound infections regardless of what antibiotic regimen we use," Dr. Reilly said.
Dr. Smith responded that they used the time from the index operation as the cut-point for SCIP compliance in the damage-control setting, but acknowledged that in many practices, patients receive another dose of antibiotics when they return to the operating room for a second look or washout.
Preliminary data on skin management in damage-control patients is being analyzed, but "we suspect, as you do at your institution, that it is probably the management of the skin in the setting of the fascial closure that may contribute to surgical site infections and are looking at a future study," he said.
Finally, when asked how the results have changed practice at Temple University, Dr. Smith said they’d like to believe they are using only 24 hours’ worth of antibiotics in the setting of prophylaxis but lack the evidence to confirm this. He pointed out that although more than a decade has passed since the Eastern Association for the Surgery of Trauma published its own antibiotic guidelines, more than 50% of surgeons in the study were not in compliance.
"Certainly, there is always room for improvement in how we treat our patients," he added.
Dr. Smith and Dr. Santaniello reported no conflicts of interest. Conflict of interest information for Dr. Reilly was not available.
*Correction, 2/22/2012: An earlier version of this article misidentified the lead author of the study.
LAKE BUENA VISTA, FLA. – Just 49.3% of patients undergoing emergency trauma laparotomy received antibiotics in accordance with the Surgical Care Improvement Project guidelines in a multicenter, retrospective analysis of 306 patients.
"Many of the non-SCIP patients received the wrong antibiotic or antibiotics for too long after their index operation," lead author Brian P. Smith said at the annual meeting of the Eastern Association for the Surgery of Trauma.
Moreover, compliance with the guidelines slashed surgical site infection rates from 32.9% among patients with noncompliant antibiotic management to 16.6% (P less than .001).
The Surgical Care Improvement Project (SCIP) established surgical antibiotic prophylaxis guidelines as part of a collaborative effort by the Centers for Medicare and Medicaid Services and the Centers for Disease Control and Prevention to reduce surgical complications. While these antibiotic prophylaxis guidelines have become well established in patients undergoing elective operative procedures, they have never been studied in trauma patients undergoing emergency surgery, said Dr. Smith, a surgical resident at Temple University Hospital in Philadelphia.*
He reported on an analysis involving 306 trauma patients who survived for more than 4 days after undergoing emergency laparotomy within 2 hours of admission at two level 1 trauma centers during 2007 and 2008. Patients were compared on the basis of adherence to the following SCIP guidelines: prophylactic antibiotic given, antibiotic received within 1 hour prior to incision, correct antibiotic selection, and discontinuation of antibiotic within 24 hours after surgery.
Their mean age was 32 years, 70% had penetrating wounds, 44% had enteric injuries, and 20% had preoperative hypotension.
In all, 155 patients received noncompliant perioperative antibiotic management. Of these, 55% received no prophylaxis or incorrect antibiotics, 46% received antibiotics outside of the recommended 60-minute window, and 54% received them beyond the 24-hour limit, Dr. Smith said.
"It’s important to note these because they represent simple practice maneuvers that can be changed to help improve antibiotic stewardship in our trauma patients," he said.
The SCIP group spent significantly fewer days than the non-SCIP group in the ICU (mean 4 days vs. 7 days; P = .02) and in the hospital (mean 14 days vs. 19 days; P = .01), although no significant difference in mortality was detected (3% vs. 6%; P = .41).
Notably, Injury Severity Score was higher at admission in the non-SCIP group at 16 vs. 13 in the SCIP group (P = .03). Prehospital transfer time, which could influence the prolongation of antibiotics before surgery, was not available.
In a multivariate regression analysis that adjusted for such confounding factors as age, Injury Severity Score, shock, presence of enteric injury, transfusion requirements, damage control surgery, surgery duration, and hospital, complete adherence to the four SCIP guidelines independently decreased the risk of a surgical site infection (odds ratio, 0.448).
The non-SCIP group had significantly more enteric injuries than the SCIP group (52% vs. 35%; P = .027), and the rate of prolonged antibiotics was higher in patients with enteric injuries, compared with those without enteric injuries (38.6% vs. 19.4%; P = .001), Dr. Smith pointed out.
"This suggests the possibility that the extent of antibiotics rather than the enteric injuries themselves explained the wound infection rates in these two groups," he said.
Discussant Dr. John Santaniello, a critical care surgeon from Loyola University Chicago, Maywood, Ill., said the authors need to further elucidate antibiotic usage in patients with enteric injuries to distinguish true SCIP prophylaxis violations from empiric treatment for contamination.
He also questioned why the authors included only four of the six SCIP measures, omitting preoperative skin preparation and intraoperative normothermia maintenance, which have been shown to reduce surgical wound infections.
Dr. Smith said missing data and difficulty in abstracting data from handwritten records kept them from analyzing these two measures.
Attendee Dr. Patrick Reilly, chief of traumatology, surgical critical care, and emergency surgery at the University of Pennsylvania in Philadelphia, questioned how SCIP compliance was defined in a damage-control patient, and asked whether the investigators have a routine way of closing the skin when the fascia can be closed in these patients.
"For a number of years, we have had a practice – we don’t really call it a practice management guideline because we don’t really have any evidence for it – where we leave the skin open if we close the fascia, at least initially, because we’ve realized a high incidence of wound infections regardless of what antibiotic regimen we use," Dr. Reilly said.
Dr. Smith responded that they used the time from the index operation as the cut-point for SCIP compliance in the damage-control setting, but acknowledged that in many practices, patients receive another dose of antibiotics when they return to the operating room for a second look or washout.
Preliminary data on skin management in damage-control patients is being analyzed, but "we suspect, as you do at your institution, that it is probably the management of the skin in the setting of the fascial closure that may contribute to surgical site infections and are looking at a future study," he said.
Finally, when asked how the results have changed practice at Temple University, Dr. Smith said they’d like to believe they are using only 24 hours’ worth of antibiotics in the setting of prophylaxis but lack the evidence to confirm this. He pointed out that although more than a decade has passed since the Eastern Association for the Surgery of Trauma published its own antibiotic guidelines, more than 50% of surgeons in the study were not in compliance.
"Certainly, there is always room for improvement in how we treat our patients," he added.
Dr. Smith and Dr. Santaniello reported no conflicts of interest. Conflict of interest information for Dr. Reilly was not available.
*Correction, 2/22/2012: An earlier version of this article misidentified the lead author of the study.
LAKE BUENA VISTA, FLA. – Just 49.3% of patients undergoing emergency trauma laparotomy received antibiotics in accordance with the Surgical Care Improvement Project guidelines in a multicenter, retrospective analysis of 306 patients.
"Many of the non-SCIP patients received the wrong antibiotic or antibiotics for too long after their index operation," lead author Brian P. Smith said at the annual meeting of the Eastern Association for the Surgery of Trauma.
Moreover, compliance with the guidelines slashed surgical site infection rates from 32.9% among patients with noncompliant antibiotic management to 16.6% (P less than .001).
The Surgical Care Improvement Project (SCIP) established surgical antibiotic prophylaxis guidelines as part of a collaborative effort by the Centers for Medicare and Medicaid Services and the Centers for Disease Control and Prevention to reduce surgical complications. While these antibiotic prophylaxis guidelines have become well established in patients undergoing elective operative procedures, they have never been studied in trauma patients undergoing emergency surgery, said Dr. Smith, a surgical resident at Temple University Hospital in Philadelphia.*
He reported on an analysis involving 306 trauma patients who survived for more than 4 days after undergoing emergency laparotomy within 2 hours of admission at two level 1 trauma centers during 2007 and 2008. Patients were compared on the basis of adherence to the following SCIP guidelines: prophylactic antibiotic given, antibiotic received within 1 hour prior to incision, correct antibiotic selection, and discontinuation of antibiotic within 24 hours after surgery.
Their mean age was 32 years, 70% had penetrating wounds, 44% had enteric injuries, and 20% had preoperative hypotension.
In all, 155 patients received noncompliant perioperative antibiotic management. Of these, 55% received no prophylaxis or incorrect antibiotics, 46% received antibiotics outside of the recommended 60-minute window, and 54% received them beyond the 24-hour limit, Dr. Smith said.
"It’s important to note these because they represent simple practice maneuvers that can be changed to help improve antibiotic stewardship in our trauma patients," he said.
The SCIP group spent significantly fewer days than the non-SCIP group in the ICU (mean 4 days vs. 7 days; P = .02) and in the hospital (mean 14 days vs. 19 days; P = .01), although no significant difference in mortality was detected (3% vs. 6%; P = .41).
Notably, Injury Severity Score was higher at admission in the non-SCIP group at 16 vs. 13 in the SCIP group (P = .03). Prehospital transfer time, which could influence the prolongation of antibiotics before surgery, was not available.
In a multivariate regression analysis that adjusted for such confounding factors as age, Injury Severity Score, shock, presence of enteric injury, transfusion requirements, damage control surgery, surgery duration, and hospital, complete adherence to the four SCIP guidelines independently decreased the risk of a surgical site infection (odds ratio, 0.448).
The non-SCIP group had significantly more enteric injuries than the SCIP group (52% vs. 35%; P = .027), and the rate of prolonged antibiotics was higher in patients with enteric injuries, compared with those without enteric injuries (38.6% vs. 19.4%; P = .001), Dr. Smith pointed out.
"This suggests the possibility that the extent of antibiotics rather than the enteric injuries themselves explained the wound infection rates in these two groups," he said.
Discussant Dr. John Santaniello, a critical care surgeon from Loyola University Chicago, Maywood, Ill., said the authors need to further elucidate antibiotic usage in patients with enteric injuries to distinguish true SCIP prophylaxis violations from empiric treatment for contamination.
He also questioned why the authors included only four of the six SCIP measures, omitting preoperative skin preparation and intraoperative normothermia maintenance, which have been shown to reduce surgical wound infections.
Dr. Smith said missing data and difficulty in abstracting data from handwritten records kept them from analyzing these two measures.
Attendee Dr. Patrick Reilly, chief of traumatology, surgical critical care, and emergency surgery at the University of Pennsylvania in Philadelphia, questioned how SCIP compliance was defined in a damage-control patient, and asked whether the investigators have a routine way of closing the skin when the fascia can be closed in these patients.
"For a number of years, we have had a practice – we don’t really call it a practice management guideline because we don’t really have any evidence for it – where we leave the skin open if we close the fascia, at least initially, because we’ve realized a high incidence of wound infections regardless of what antibiotic regimen we use," Dr. Reilly said.
Dr. Smith responded that they used the time from the index operation as the cut-point for SCIP compliance in the damage-control setting, but acknowledged that in many practices, patients receive another dose of antibiotics when they return to the operating room for a second look or washout.
Preliminary data on skin management in damage-control patients is being analyzed, but "we suspect, as you do at your institution, that it is probably the management of the skin in the setting of the fascial closure that may contribute to surgical site infections and are looking at a future study," he said.
Finally, when asked how the results have changed practice at Temple University, Dr. Smith said they’d like to believe they are using only 24 hours’ worth of antibiotics in the setting of prophylaxis but lack the evidence to confirm this. He pointed out that although more than a decade has passed since the Eastern Association for the Surgery of Trauma published its own antibiotic guidelines, more than 50% of surgeons in the study were not in compliance.
"Certainly, there is always room for improvement in how we treat our patients," he added.
Dr. Smith and Dr. Santaniello reported no conflicts of interest. Conflict of interest information for Dr. Reilly was not available.
*Correction, 2/22/2012: An earlier version of this article misidentified the lead author of the study.
FROM THE ANNUAL MEETING OF THE EASTERN ASSOCIATION FOR THE SURGERY OF TRAUMA
Major Finding: Surgical site infection rates were 32.9% in the SCIP noncompliant group vs. 16.6% in the SCIP-compliant group (P less than .001).
Data Source: Researchers conducted a multicenter, retrospective analysis of 306 patients who underwent emergency trauma laparotomy.
Disclosures: Dr. Smith and Dr. Santaniello reported no conflicts of interest. Conflict of interest information for Dr. Reilly was not available.
Team-Based Geriatric Protocol Cuts Trauma Mortality
LAKE BUENA VISTA, FLA. – Mortality was sharply reduced in elderly patients undergoing trauma care with an aggressive protocol marked by multidisciplinary teamwork and prompt identification of occult shock.
The survival benefit was significant even among patients older than 75 years, a group with notoriously high mortality rates, Dr. Eric Bradburn said at the annual meeting of the Eastern Association for the Surgery of Trauma.
Injured geriatric patients pose unique challenges to the trauma team because of their abnormal responses to shock and injury and frequent polypharmacy. They are also increasing in numbers with today’s active geriatric population, comprising 36% of all admissions at his own level II trauma center, said Dr. Bradburn, an acute care surgeon at Lancaster General Hospital in Hershey, Pa.
With the protocol, patients older than 65 years were screened on admission for high-risk injuries, comorbidities, and/or physiologic parameters associated with increased geriatric mortality in the literature. If one or more high-risk indicator was present, a high-risk protocol was initiated that included:
• ICU admission.
• STAT arterial blood gas (ABG).
• An ABG every 4 hours, if base deficit is –6 mmol/L or more, until base deficit is –2 mmol/L.
• STAT echocardiogram (EKG).
• Basic metabolic profile; magnesium and phosphorus tests in morning.
• Prothrombin time, partial thromboplastin time, and international normalized ratio in morning.
• Neurologic checks every hour for 24 hours.
• For unexplained hemodynamic instability, obtain a STAT EKG.
• Geriatric medicine consult.
The protocol was initiated in January 2006, with all 4,534 geriatric trauma patients admitted from 2000 to 2010 included in the analysis. Of these, 309 patients died for an overall mortality rate of 6.8%, Dr. Bradburn said.
Mortality rates increased sharply at age 75 years – consistent with the literature – from less than 4% to more than 6% and rose steadily to more than 11% by age 95 years.
In multivariate adjusted analysis of 3,902 patients with full data available, mortality significantly improved for geriatric patients on the protocol (odds ratio, 0.63), he said. The receiver operating curve was 0.86. Variables includes in the analysis were Injury Severity Score (ISS), trauma level, Revised Trauma Score (RTS), and age.
Patients on the protocol had significantly lower mortality rates regardless of whether they were 75-84 years (OR, 2.72), older than 85 years (OR, 4.62), had an Injury Severity Score of 17-25 (OR, 6.45) or ISS greater than 25 (OR, 15.93).
Furthermore, mortality was significantly lower among patients who received the full protocol even at the highest ISS categories, compared with those who did not receive the protocol or received either the protocol or the geriatric consult, "demonstrating the synergy and impact our full protocol has on this population," Dr. Bradburn said.
"We believe the implications of this study demonstrate that an aggressive approach to the geriatric trauma patient can result in a positive outcome in this population," he concluded.
Invited discussant Dr. Carl Schulman, a trauma and burn surgeon at the University of Miami’s Ryder Trauma Center, pointed out that geriatric consultations alone have been shown to improve mortality.
"Can you really show that your protocol added anything to this?" he asked. "Maybe all the results you have shown are from the geriatric consult alone, and this geriatric protocol is unnecessary. This would save a lot of unnecessary testing and improve the cost/benefit ratio, by simply having the geriatric consult."
The audience also questioned what services the geriatricians provided.
Dr. Bradburn said the geriatricians assisted most with social, rehabilitative, and end-of-life issues and medication issues, but also managed some comorbidities. He said the combined approach goes beyond these issues by alerting the trauma team early on to abnormal values "rather than waiting until the reserves are tapped." He noted that elderly trauma patients often present with occult hypotension leading to bias and that the literature is replete with data showing that not enough attention is paid to this population until it is too late.
Later, in a interview following the meeting, Dr. Bradburn explained that his trauma team managed the patients "from the bay to discharge."
Additional input from the geriatric team included recommendations continuing/discontinuing certain medications; assisting with management of delirium; and addressing DNR status, preinjury functional assessments, as well as social and rehab needs, he said.
"They were key in addressing the polypharmacy issue removing many of those medications that might lead to falls or increased risk for delirium."
Geriatricians’ direction on appropriate rehabilitation can boost measures such as 30-day mortality or 6-month mortality, he said. For example, in the case of an elderly fall resulting in a traumatic brain injury and extremity fractures, aggressive focused rehab to address the preexisting physical deficits that led to the fall, as well as the deficits acquired by the fall, would certainly improve the quality of life for that individual and potentially prevent additional falls.
At the meeting, Dr. Schulman also asked whether the high DNR rate of 20% could have contributed to the results. Dr. Bradburn responded that if a DNR is put into the regression model, it actually makes the results better, changing the odds ratio from 0.63 to 0.36.
Dr. Bradburn said his team had hoped to investigate functional outcomes, but that these data were not complete.
He noted that the current study is limited by its retrospective design and acknowledged that "from our data you cannot fully attribute its success solely to one part of our protocol." Still, he said, the benefits are "clear."
"This study lays the groundwork for a prospective multi-institutional study – in which we can potentially tease if one part of our protocol is more effective than any other."
The protocol should be replicable beyond Lancaster General Hospital, he said. "We think the approach is unique, but believe with further study we can show this can be applied at other institutions with equivalent successes."
Dr. Bradburn and Dr. Schulman reported no relevant conflicts of interest.
LAKE BUENA VISTA, FLA. – Mortality was sharply reduced in elderly patients undergoing trauma care with an aggressive protocol marked by multidisciplinary teamwork and prompt identification of occult shock.
The survival benefit was significant even among patients older than 75 years, a group with notoriously high mortality rates, Dr. Eric Bradburn said at the annual meeting of the Eastern Association for the Surgery of Trauma.
Injured geriatric patients pose unique challenges to the trauma team because of their abnormal responses to shock and injury and frequent polypharmacy. They are also increasing in numbers with today’s active geriatric population, comprising 36% of all admissions at his own level II trauma center, said Dr. Bradburn, an acute care surgeon at Lancaster General Hospital in Hershey, Pa.
With the protocol, patients older than 65 years were screened on admission for high-risk injuries, comorbidities, and/or physiologic parameters associated with increased geriatric mortality in the literature. If one or more high-risk indicator was present, a high-risk protocol was initiated that included:
• ICU admission.
• STAT arterial blood gas (ABG).
• An ABG every 4 hours, if base deficit is –6 mmol/L or more, until base deficit is –2 mmol/L.
• STAT echocardiogram (EKG).
• Basic metabolic profile; magnesium and phosphorus tests in morning.
• Prothrombin time, partial thromboplastin time, and international normalized ratio in morning.
• Neurologic checks every hour for 24 hours.
• For unexplained hemodynamic instability, obtain a STAT EKG.
• Geriatric medicine consult.
The protocol was initiated in January 2006, with all 4,534 geriatric trauma patients admitted from 2000 to 2010 included in the analysis. Of these, 309 patients died for an overall mortality rate of 6.8%, Dr. Bradburn said.
Mortality rates increased sharply at age 75 years – consistent with the literature – from less than 4% to more than 6% and rose steadily to more than 11% by age 95 years.
In multivariate adjusted analysis of 3,902 patients with full data available, mortality significantly improved for geriatric patients on the protocol (odds ratio, 0.63), he said. The receiver operating curve was 0.86. Variables includes in the analysis were Injury Severity Score (ISS), trauma level, Revised Trauma Score (RTS), and age.
Patients on the protocol had significantly lower mortality rates regardless of whether they were 75-84 years (OR, 2.72), older than 85 years (OR, 4.62), had an Injury Severity Score of 17-25 (OR, 6.45) or ISS greater than 25 (OR, 15.93).
Furthermore, mortality was significantly lower among patients who received the full protocol even at the highest ISS categories, compared with those who did not receive the protocol or received either the protocol or the geriatric consult, "demonstrating the synergy and impact our full protocol has on this population," Dr. Bradburn said.
"We believe the implications of this study demonstrate that an aggressive approach to the geriatric trauma patient can result in a positive outcome in this population," he concluded.
Invited discussant Dr. Carl Schulman, a trauma and burn surgeon at the University of Miami’s Ryder Trauma Center, pointed out that geriatric consultations alone have been shown to improve mortality.
"Can you really show that your protocol added anything to this?" he asked. "Maybe all the results you have shown are from the geriatric consult alone, and this geriatric protocol is unnecessary. This would save a lot of unnecessary testing and improve the cost/benefit ratio, by simply having the geriatric consult."
The audience also questioned what services the geriatricians provided.
Dr. Bradburn said the geriatricians assisted most with social, rehabilitative, and end-of-life issues and medication issues, but also managed some comorbidities. He said the combined approach goes beyond these issues by alerting the trauma team early on to abnormal values "rather than waiting until the reserves are tapped." He noted that elderly trauma patients often present with occult hypotension leading to bias and that the literature is replete with data showing that not enough attention is paid to this population until it is too late.
Later, in a interview following the meeting, Dr. Bradburn explained that his trauma team managed the patients "from the bay to discharge."
Additional input from the geriatric team included recommendations continuing/discontinuing certain medications; assisting with management of delirium; and addressing DNR status, preinjury functional assessments, as well as social and rehab needs, he said.
"They were key in addressing the polypharmacy issue removing many of those medications that might lead to falls or increased risk for delirium."
Geriatricians’ direction on appropriate rehabilitation can boost measures such as 30-day mortality or 6-month mortality, he said. For example, in the case of an elderly fall resulting in a traumatic brain injury and extremity fractures, aggressive focused rehab to address the preexisting physical deficits that led to the fall, as well as the deficits acquired by the fall, would certainly improve the quality of life for that individual and potentially prevent additional falls.
At the meeting, Dr. Schulman also asked whether the high DNR rate of 20% could have contributed to the results. Dr. Bradburn responded that if a DNR is put into the regression model, it actually makes the results better, changing the odds ratio from 0.63 to 0.36.
Dr. Bradburn said his team had hoped to investigate functional outcomes, but that these data were not complete.
He noted that the current study is limited by its retrospective design and acknowledged that "from our data you cannot fully attribute its success solely to one part of our protocol." Still, he said, the benefits are "clear."
"This study lays the groundwork for a prospective multi-institutional study – in which we can potentially tease if one part of our protocol is more effective than any other."
The protocol should be replicable beyond Lancaster General Hospital, he said. "We think the approach is unique, but believe with further study we can show this can be applied at other institutions with equivalent successes."
Dr. Bradburn and Dr. Schulman reported no relevant conflicts of interest.
LAKE BUENA VISTA, FLA. – Mortality was sharply reduced in elderly patients undergoing trauma care with an aggressive protocol marked by multidisciplinary teamwork and prompt identification of occult shock.
The survival benefit was significant even among patients older than 75 years, a group with notoriously high mortality rates, Dr. Eric Bradburn said at the annual meeting of the Eastern Association for the Surgery of Trauma.
Injured geriatric patients pose unique challenges to the trauma team because of their abnormal responses to shock and injury and frequent polypharmacy. They are also increasing in numbers with today’s active geriatric population, comprising 36% of all admissions at his own level II trauma center, said Dr. Bradburn, an acute care surgeon at Lancaster General Hospital in Hershey, Pa.
With the protocol, patients older than 65 years were screened on admission for high-risk injuries, comorbidities, and/or physiologic parameters associated with increased geriatric mortality in the literature. If one or more high-risk indicator was present, a high-risk protocol was initiated that included:
• ICU admission.
• STAT arterial blood gas (ABG).
• An ABG every 4 hours, if base deficit is –6 mmol/L or more, until base deficit is –2 mmol/L.
• STAT echocardiogram (EKG).
• Basic metabolic profile; magnesium and phosphorus tests in morning.
• Prothrombin time, partial thromboplastin time, and international normalized ratio in morning.
• Neurologic checks every hour for 24 hours.
• For unexplained hemodynamic instability, obtain a STAT EKG.
• Geriatric medicine consult.
The protocol was initiated in January 2006, with all 4,534 geriatric trauma patients admitted from 2000 to 2010 included in the analysis. Of these, 309 patients died for an overall mortality rate of 6.8%, Dr. Bradburn said.
Mortality rates increased sharply at age 75 years – consistent with the literature – from less than 4% to more than 6% and rose steadily to more than 11% by age 95 years.
In multivariate adjusted analysis of 3,902 patients with full data available, mortality significantly improved for geriatric patients on the protocol (odds ratio, 0.63), he said. The receiver operating curve was 0.86. Variables includes in the analysis were Injury Severity Score (ISS), trauma level, Revised Trauma Score (RTS), and age.
Patients on the protocol had significantly lower mortality rates regardless of whether they were 75-84 years (OR, 2.72), older than 85 years (OR, 4.62), had an Injury Severity Score of 17-25 (OR, 6.45) or ISS greater than 25 (OR, 15.93).
Furthermore, mortality was significantly lower among patients who received the full protocol even at the highest ISS categories, compared with those who did not receive the protocol or received either the protocol or the geriatric consult, "demonstrating the synergy and impact our full protocol has on this population," Dr. Bradburn said.
"We believe the implications of this study demonstrate that an aggressive approach to the geriatric trauma patient can result in a positive outcome in this population," he concluded.
Invited discussant Dr. Carl Schulman, a trauma and burn surgeon at the University of Miami’s Ryder Trauma Center, pointed out that geriatric consultations alone have been shown to improve mortality.
"Can you really show that your protocol added anything to this?" he asked. "Maybe all the results you have shown are from the geriatric consult alone, and this geriatric protocol is unnecessary. This would save a lot of unnecessary testing and improve the cost/benefit ratio, by simply having the geriatric consult."
The audience also questioned what services the geriatricians provided.
Dr. Bradburn said the geriatricians assisted most with social, rehabilitative, and end-of-life issues and medication issues, but also managed some comorbidities. He said the combined approach goes beyond these issues by alerting the trauma team early on to abnormal values "rather than waiting until the reserves are tapped." He noted that elderly trauma patients often present with occult hypotension leading to bias and that the literature is replete with data showing that not enough attention is paid to this population until it is too late.
Later, in a interview following the meeting, Dr. Bradburn explained that his trauma team managed the patients "from the bay to discharge."
Additional input from the geriatric team included recommendations continuing/discontinuing certain medications; assisting with management of delirium; and addressing DNR status, preinjury functional assessments, as well as social and rehab needs, he said.
"They were key in addressing the polypharmacy issue removing many of those medications that might lead to falls or increased risk for delirium."
Geriatricians’ direction on appropriate rehabilitation can boost measures such as 30-day mortality or 6-month mortality, he said. For example, in the case of an elderly fall resulting in a traumatic brain injury and extremity fractures, aggressive focused rehab to address the preexisting physical deficits that led to the fall, as well as the deficits acquired by the fall, would certainly improve the quality of life for that individual and potentially prevent additional falls.
At the meeting, Dr. Schulman also asked whether the high DNR rate of 20% could have contributed to the results. Dr. Bradburn responded that if a DNR is put into the regression model, it actually makes the results better, changing the odds ratio from 0.63 to 0.36.
Dr. Bradburn said his team had hoped to investigate functional outcomes, but that these data were not complete.
He noted that the current study is limited by its retrospective design and acknowledged that "from our data you cannot fully attribute its success solely to one part of our protocol." Still, he said, the benefits are "clear."
"This study lays the groundwork for a prospective multi-institutional study – in which we can potentially tease if one part of our protocol is more effective than any other."
The protocol should be replicable beyond Lancaster General Hospital, he said. "We think the approach is unique, but believe with further study we can show this can be applied at other institutions with equivalent successes."
Dr. Bradburn and Dr. Schulman reported no relevant conflicts of interest.
FROM THE ANNUAL MEETING OF THE EASTERN ASSOCIATION FOR THE SURGERY OF TRAUMA