User login
For MD-IQ only
Genomic Medicine and Genetic Counseling in the Department of Veterans Affairs and Department of Defense (FULL)
Vickie Venne, MS. What is the Genomic Medicine Service (GMS) at the US Department of Veterans Affairs (VA)?
Renee Rider, JD, MS, LCGC. GMS is a telehealth service. We are part of central office and field stationed at the George E. Wahlen VA Medical Center (VAMC) in Salt Lake City, Utah. We provide care to about 90 VAMCs and their associated clinics. Veterans are referred to us by entering an interfacility consult in the VA Computerized Patient Record System (CPRS). We review the consult to determine whether the patient needs to be seen, whether we can answer with an e-consult, or whether we need more information. For the patients who need an appointment, the telehealth department at the veteran’s VA facility will contact the patient to arrange a visit with us. At the time of the appointment, the facility has a staff member available to seat the patient and connect them to us using video equipment.
We provide genetic care for all specialties, including cancer, women’s health, cardiology and neurology. In today’s discussion, we are focusing on cancer care.
Vickie Venne. What do patients do at facilities that don’t get care through GMS?
Renee Rider. There are a handful of facilities that provide their own genetic care in-house. For example, VA Boston Healthcare System in Massachusetts and the Michael E. DeBakey VAMC in Houston, Texas each have their own programs. For veterans who are not at a VA facility that has an agreement with GMS and do not have a different genetics program, their providers need to make referrals to community care.
Vickie Venne. How do patients get referred and what happens at their facility when the patients return to the specialty and primary care providers (PCP)? Ishta, who do you refer to GMS and how do you define them initially?
Ishta Thakar, MD, FACP. Referrals can come at a couple of points during a veteran’s journey at the VA. The VA covers obstetrics care for women veterans. Whenever a PCP or a women’s health provider is doing the initial history and physical on a new patient, if the female veteran has an extensive family history of breast, ovarian, colon, or endometrial cancer, then we take more history and we send a consult to GMS. The second instance would be if she tells us that she has had a personal history of breast, ovarian, or endometrial cancer and she has never had genetic testing. The third instance would be whenever we have a female veteran who is diagnosed with breast, ovarian, endometrial, or colon cancer. We would definitely talk to her about genetic counseling and send a referral to GMS. We would ask for a GMS consult for a patient with advanced maternal age, with exposure to some kind of teratogens, with an abnormal ultrasound, a family history of chromosomal disorders, or if she’s seeing an obstetrician who wants her to be tested. And finally, if a patient has a constellation of multiple cancers in the family and we don’t know what’s going on, we would also refer the patient to GMS.
Vickie Venne. That would be why GMS fields over 150 referrals every week. It is a large list. We also see veterans with personal or family histories of neurologic or cardiologic concerns as well.
Renee, as somebody who fields many of these referrals from unaffected individuals, what is the family history process?
Renee Rider. We don’t expect the referring provider to be a genetic expert. When a provider is seeing a constellation of several different cancers and he or she doesn’t know if there’s anything going on genetically or even if it’s possible, absolutely they should put in a referral to GMS. We have a triage counselor who reviews every consult that comes into our service within 24 hours.
Many cancers are due to exposures that are not concerning for a genetic etiology. We can let you know that it is not concerning, and the PCP can counsel the patient that it is very unlikely to be genetic in nature. We still give feedback even if it’s not someone who is appropriate for genetic counseling and testing. It is important to reach out to GMS even if you don’t know whether a cancer is genetic in nature.
It also is important to take your time when gathering family histories. We get a lot of patients who say, “There’s a lot of cancer in my family. I have no idea who had cancer, but I know a lot of people had cancer.” That’s not the day to put in a referral to GMS. At that point, providers should tell the patient to get as much information as they can about the family history and then reassess. It’s important for us to have accurate information. We’ve had several times where we receive a referral because the veteran says that their sister had ovarian cancer. And then when our staff calls, they later find out it was cervical cancer. That’s not a good use of the veteran’s time, and it’s not a good use of VA resources.
The other important thing about family histories is keeping the questions open-ended. Often a PCP or specialist will ask about a certain type of cancer: “Does anyone in your family have breast cancer, ovarian cancer?” Or if the veteran
is getting a colonoscopy, they ask, “Does anybody have colon cancer?” Where really, we need to be a little bit more open-ended. We prefer questions like, “Has anyone in your family
had cancer?” because that’s the question that prompts a response of, “Yes, 3 people in my family have had thyroid cancer.” That’s very important for us to know, too.
If you do get a positive response, probe a little bit more: what kind of cancer did someone have, how old were they when they had their cancer? And how are they related? Is this an aunt on your mom’s side or on your dad’s side? Those are the types of information that we need to figure out if that person needs a referral.
Vickie Venne. It’s a different story when people already have a cancer diagnosis. Which hematology or oncology patients are good referrals and why?
Lisa Arfons, MD. When patients come in with newly diagnosed cancer, breast for example, it is an emotional diagnosis and psychologicallydistressing. Oftentimes, they want to know why this happened to them. The issues surrounding
genetic testing also becomes very emotional. They want to know whether their children are at risk as well.
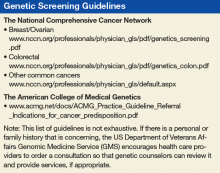
Genetic discussions take a long time. I rarely do that on the first visit. I always record for myself in my clinic note if something strikes me regarding the patient’s diagnosis. I quickly run through the National Comprehensive Cancer Network (NCCN) guidelines to remind myself of what I need to go over with the patient at our next meeting. Most patients don’t need to be referred to GMS, and most patients don’t need to be tested once they’re seen.
I often save the referral discussion for after I have established a rapport with a patient, we have a treatment plan, or they already have had their first surgery. Therefore, we are not making decisions about their first surgery based on the genetic medicine results.
If I’m considering a referral, I do a deeper dive with the patient. Is the patient older or younger than 45 years? I pull up NCCN guidelines and we go through the entire checklist.
We have male breast cancer patients at the VA—probably more than the community—so we refer those patients. At the Louis Stokes Cleveland VAMC in Ohio, we have had some in-depth discussions about referring male breast cancer patients for genetic testing and whether it was beneficial to older patients with male breast cancer. Ultimately, we decided that it was important for our male veterans to be tested because it empowered them to have better understanding of their medical conditions that may not just have effect on them but on their offspring, and that that can be a source of psychological and emotional support.
I don’t refer most people to GMS once I go through the checklist. I appreciate the action for an e-consult within the CPRS telemedicine consult itself, as Renee noted. If it is not necessary, GMS makes it an e-consult. I try to communicate that I don’t know whether it is necessary or not so that GMS understands where I’m coming from.
Vickie Venne. In the US Department of Defense (DoD) the process is quite different. Mauricio, can you explain the clinical referral process, who is referred, and how that works from a laboratory perspective?
Maj De Castro, MD, FACMG, USAF. The VA has led the way in demonstrating how to best provide for the medical genetic needs of a large, decentralized population distributed all over the country. Over the last 5 to 10 years, the DoD has made strides in recognizing the role genetics plays in the practice of everyday medicine and redoubling efforts to meet the needs of servicemembers.
The way that it traditionally has worked in the DoD is that military treatment facilities (MTFs) that have dedicated geneticists and genetic counselors: Kessler Medical Center in Mississippi, Walter Reed National Military Medical
Center in Maryland, Tripler Army Medical Center in Hawaii, Madigan Army Medical Center in Washington, Brooke Army Medical Center in Texas, Naval Medical Center San Diego in California, and Naval Medical Center Portsmouth in Virginia. A patient seeking genetic evaluation, counseling, or testing in those larger facilities would be referred to the genetics service by their primary care manager. Wait times vary, but it would usually be weeks, maybe months. However, the great majority of MTFs do not have dedicated genetics support. Most of the time, those patients would have to be referred to the local civilian community—there was no process for them to be seen in in the military healthcare system—with wait times that exceed 6 to 8 months in some cases. This is due to just not a military but a national shortage of genetics professionals (counselors and physicians).
Last year we started the telegenetics initiative, which is small compared to the VA—it is comprised of 2 geneticists and 1 genetic counselor—but with the full intent of growing it over time. Its purpose is to extend the resources we
had to other MTFs. Genetics professionals stationed state-side can provide care to remote facilities with limited access to local genetics support such as Cannon Air Force Base (AFB) or overseas facilities such as Spangdahlem AFB in Germany.
We recognize there are military-specific needs for the DoD regarding the genetic counseling process that have to take into account readiness, genetic discrimination, continued ability to serve and fitness for duty. For this important reason, we are seeking to expand our telegenetics initiative. The goal is to be able to provide 100% of all genetic counseling in-house, so to speak.
Currently, providers at the 4 pilot sites (Cannon AFB, Fort Bragg, Spangdahlem AFB, and Guantanamo Bay) send us referrals. We triage them and assign the patient to see a geneticist or a counselor depending on the indication.
On the laboratory side, it has been a very interesting experience. Because we provide comprehensive germline cancer testing at very little cost to the provider at any MTF, we have had high numbers of test requests over the years.
In addition to saving the DoD millions of dollars in testing, we have learned some interesting lessons in the process. For instance, we have worked closely with several different groups to better understand how to educate providers on the genetic counseling and testing process. This has allowed us to craft a thorough and inclusive consent form that addresses the needs of the DoD. We have also learned valuable lessons about population-based screening vs evidence-based testing, and lessons surrounding narrow-based testing (BRCA1 and BRCA2 only testing) vs ordering a more comprehensive panel that includes other genes supported by strong evidence (such as PALB2, CHEK2, or TP53).
For example, we have found that in a significant proportion of individuals with and without family history, there are clinically relevant variants in genes other than BRCA1 or BRCA2. And so, we have made part of our consent process,
a statement on secondary findings. If the patient consents, we will report pathogenic variants in other genes known to be associated with cancer (with strong evidence) even if the provider ordered a narrow panel such as BRCA1 and BRCA2 testing only. In about 1% to 4% of patients that would otherwise not meet NCCN guidelines, we’ve reported variants that were clinically actionable and changed the medical management of that patient.
We feel strongly that this is a conversation that we need to have in our field, and we realize it’s a complex issue, maybe we need to expand who gets testing. Guideline based testing is missing some patients out there that could benefit from it.
Vickie Venne. There certainly are many sides to the conversation of population-based vs evidence-based genetic testing. Genetic testing policies are changing rapidly. There are teams exploring comprehensive gene sequencing for
newborns and how that potential 1-time test can provide information will be reinterpreted as a person goes from cradle to grave. However, unlike the current DoD process, in the VA there are patients who we don’t see.
Renee Rider. I want to talk about money. When we order a genetic test, that test is paid for by the pathology department at the patient’s VAMC. Most of the pathology departments we work with are clear that they only can provide
genetic testing that is considered medically necessary. Thus, we review each test to make sure it meets established guidelines for testing. We don’t do population genetic screening as there isn’t evidence or guidelines to support offering it. We are strict about who does and does not get genetic testing, partly because we have a responsibility to pathology departments and to the taxpayers.
GMS focuses on conditions that are inherited, that is to say, we deal with germline genetics. Therefore, we discontinue referrals for somatic requests, such as when an OncotypeDX test is requested. It is my understanding that pharmacogenetic referrals may be sent to the new PHASeR initiative, which is a joint collaboration between the VA and Sanford Health and is headed by Deepak Voora, MD.
We generally don’t see patients who still are having diagnostic procedures done. For example, if a veteran has a suspicious breast mass, we recommend that the provider workup the mass before referring to GMS. Regardless of a genetic test result, a suspicious mass needs to be worked up. And, knowing if the mass is cancerous could change how we would proceed with the genetic workup. For example, if the mass were not cancerous, we may recommend that an affected relative have the first genetic evaluation. Furthermore, knowing if the patient has cancer changes how we interpret negative test results.
Another group of patients we don’t see are those who already had genetic testing done by the referring provider. It’s a VA directive that if you order a test, you’re the person who is responsible for giving the results. We agree with
this directive. If you don’t feel comfortable giving back test results, don’t order the test. Often, when a provider sends a patient to us after the test was done, we discover that the patient didn’t have appropriate pretest counseling. A test result, such as a variant of uncertain significance (VUS), should never be a surprise to either the provider or the patient.
Ishta Thakar. For newly diagnosed cancers, the first call is to the patient to inform them that they have cancer. We usually bring up genetic counseling or testing, if applicable, when they are ready to accept the diagnosis and have a conversation about it. All our consults are via telehealth, so none of our patients physically come to GMS in Salt Lake City. All the consults are done virtually.
For newly diagnosed patients, we would send a consult in within a couple of weeks. For patients who had a family history, the referral would not be urgent: They can be seen within about 3 months. The turnaround times for GMS are so much better than what we have available in the community where it’s often at least 6 months, as previously noted.
Vickie Venne. Thank you. We continue to work on that. One of the interesting things that we’ve done, which is the brainchild of Renee, is shared medical appointments.
Renee Rider. We have now created 4 group appointments for people who have concerns surrounding cancer. One group is for people who don’t have cancer but have family members who have cancer who may be the best testing candidate. For example, that might be a 30-year old who tells you that her mother had breast cancer at age 45 years. Her mother is still living, but she’s never had genetic testing. We would put her in a group where we discuss the importance of talking to the family members and encouraging them to go get that first genetic evaluation in the family.
Our second group is for people who don’t have cancer themselves, but have a family history of cancer and those affected relatives have passed away. The family needs a genetic evaluation, and the veteran is the best living testing candidate.
That group is geared towards education about the test and informed consent.
The third group is for people with cancer who qualify for genetic testing. We provide all of the information that they need to make an informed decision on having (or not having) genetic testing.
The final group is for people who have family histories of known genetic mutations in cancer genes. Again, we provide them with all of the information that they need to make an informed decision regarding genetic testing.
With the shared medical appointments, we have been able to greatly increase the number of patients that we can see. Our first 3 groups all meet once a week and can have 10 or 12 veterans. Our last group meets every other week and has a maximum of 6 veterans. Wait times for our groups are generally ≤ 2 weeks. All veterans can choose to have an individual appointment if they prefer. We regularly get unsolicited feedback from veterans that they learn a lot during our groups and appreciate it.
Our group appointments have lowered the wait time for the people in the groups. And, they’ve lowered the wait time for the people who are seen individually. They’ve allowed us to address the backlog of patients waiting to see us in a more timely manner. Our wait time for individual appointment had been approaching 6 months, and it is now about 1.5 months.
We also think that being in a group normalizes the experience. Most people don’t know anyone who has had genetic testing. Now, they are in a group with others going through the same experience. In one of my groups, a male veteran talked about his breast cancer being really rare. Another male in the group volunteer that he had breast cancer, too. They both seemed to appreciate not feeling alone.
Vickie Venne. I want to move to our final piece. What do the referring providers tell the patients about a genetics referral and what should they expect?
Lisa Arfons. First and foremost, I tell the patient that it is a discussion with a genetic counselor. I make it clear that they understand that it is a discussion. They then can agree or not agree to accept genetic testing if it’s recommended.
I talk in general terms about why I think it can be important for them to have the discussion, but that we don’t have great data for decisionmaking. We understand that there are more options for preventive measures but then it ultimately will be a discussion between the PCP, the patient, and their family members about how they proceed about the preventive measures. I want them to start thinking about how the genetic test results, regardless of if they are positive, negative, or a variant that is not yet understood, can impact their offspring.
Probably I am biased, as my mom had breast cancer and she underwent genetic testing. So, I have a bit of an offspring focus as well. I already mentioned that you must discuss about whether or not it’s worth screening or doing any preventive measures on contralateral breast, or screening for things like prostate cancer at age 75 years. And so I focus more on the family members.
I try to stay in my lane. I am extremely uncomfortable when I hear about someone in our facility sending off a blood test and then asking someone else to interpret the results and discuss it with the patient. Just because it’s a blood test and it’s easy to order doesn’t mean that it is easy to know what to do with it, and it needs to be respected as such.
Ishta Thakar. Our PCPs let the patients know that GMS will contact the patient to schedule a video appointment and that if they want to bring any family members along with them, they’re welcome to. We also explain that certain cancers are genetically based and that if they have a genetic mutation, it can be passed on to their offspring. I also explain that if they have certain mutations, then we would be more vigilant in screening them for other kinds of cancers. That’s the reason that we refer that they get counseled. After counseling if they’re ready for the testing, then the counselor orders the test and does the posttest discussion with the patient.
Vickie Venne. In the VA, people are invited to attend a genetic counseling session but can certainly decline. Does the the DoD have a different approach?
Maj De Castro. I would say that the great majority of active duty patients have limited knowledge of what to expect out of a genetics appointment. One of the main things we do is educate them on their rights and protections and the potential risks associated with performing genetic testing, in particular when it comes to their continued ability to serve. Genetic testing for clinical purposes is not mandatory in the DoD, patients can certainly decline testing. Because genetic testing has the potential to alter someone’s career, it is critical we have a very thorough and comprehensive pre- and posttest counseling sessions that includes everything from career implications to the Genetic Information Nondiscrimination Act (GINA) and genetic discrimination in the military, in addition to the standard of care medical information.
Scenarios in which a servicemember is negatively impacted by pursuing a genetic diagnosis are very rare. More than 90% of the time, genetic counseling and/or testing has no adverse career effect. When they do, it is out of concern for the safety and wellbeing of a servicemember. For instance, if we diagnosis a patient with a genetic form of some arrhythmogenic disorder, part of the treatment plan can be to limit that person’s level of exertion, because it could potentially lead to death. We don’t want to put someone in a situation that may trigger that.
Vickie Venne. We also have a certain number of veterans who ask us about their service disability pay and the impact of genetic testing on it. One example is veterans with prostate cancer who were exposed to Agent Orange, which has been associated with increased risk for developing prostate cancer. I have had men who have been referred for genetic evaluation ask, “Well, if I have an identifiable mutation, how will that impact my service disability?” So we discuss the carcinogenic process that may include an inherited component as well as the environmental risk factors. I think that’s a unique issue for a population we’re honored to be able to serve.
Renee Rider. When we are talking about how the population of veterans is unique, I think it is also important to acknowledge mental health. I’ve had several patients tell me that they have posttraumatic stress disorder or anxiety and the idea of getting an indeterminant test result, such as VUS, would really weigh on them.
In the community, a lot of providers order the biggest panel they can, but for these patients who are worried about getting those indeterminant test results, I’ve been able to work with them to limit the size of the panel. I order a small panel that only has genes that have implications for that veteran’s clinical management. For example, in a patient with ductal breast cancer, I remove the genes that cause lobular breast cancer. This takes a bit of knowledge and critical thinking that our VA genetic counselors have because they have experience with veterans and their needs.
As our time draws to a close, I have one final thought. This has been a heartwarming conversation today. It is really nice to hear that GMS services are appreciated. We in GMS want to partner with our referring providers. Help us help you! When you enter a referral, please let us know how we can help you. The more we understand why you are sending your veteran to GMS, the more we can help meet your needs. If there are any questions or problems, feel free to send us an email or pick up the phone and call us.
Vickie Venne, MS. What is the Genomic Medicine Service (GMS) at the US Department of Veterans Affairs (VA)?
Renee Rider, JD, MS, LCGC. GMS is a telehealth service. We are part of central office and field stationed at the George E. Wahlen VA Medical Center (VAMC) in Salt Lake City, Utah. We provide care to about 90 VAMCs and their associated clinics. Veterans are referred to us by entering an interfacility consult in the VA Computerized Patient Record System (CPRS). We review the consult to determine whether the patient needs to be seen, whether we can answer with an e-consult, or whether we need more information. For the patients who need an appointment, the telehealth department at the veteran’s VA facility will contact the patient to arrange a visit with us. At the time of the appointment, the facility has a staff member available to seat the patient and connect them to us using video equipment.
We provide genetic care for all specialties, including cancer, women’s health, cardiology and neurology. In today’s discussion, we are focusing on cancer care.
Vickie Venne. What do patients do at facilities that don’t get care through GMS?
Renee Rider. There are a handful of facilities that provide their own genetic care in-house. For example, VA Boston Healthcare System in Massachusetts and the Michael E. DeBakey VAMC in Houston, Texas each have their own programs. For veterans who are not at a VA facility that has an agreement with GMS and do not have a different genetics program, their providers need to make referrals to community care.
Vickie Venne. How do patients get referred and what happens at their facility when the patients return to the specialty and primary care providers (PCP)? Ishta, who do you refer to GMS and how do you define them initially?
Ishta Thakar, MD, FACP. Referrals can come at a couple of points during a veteran’s journey at the VA. The VA covers obstetrics care for women veterans. Whenever a PCP or a women’s health provider is doing the initial history and physical on a new patient, if the female veteran has an extensive family history of breast, ovarian, colon, or endometrial cancer, then we take more history and we send a consult to GMS. The second instance would be if she tells us that she has had a personal history of breast, ovarian, or endometrial cancer and she has never had genetic testing. The third instance would be whenever we have a female veteran who is diagnosed with breast, ovarian, endometrial, or colon cancer. We would definitely talk to her about genetic counseling and send a referral to GMS. We would ask for a GMS consult for a patient with advanced maternal age, with exposure to some kind of teratogens, with an abnormal ultrasound, a family history of chromosomal disorders, or if she’s seeing an obstetrician who wants her to be tested. And finally, if a patient has a constellation of multiple cancers in the family and we don’t know what’s going on, we would also refer the patient to GMS.
Vickie Venne. That would be why GMS fields over 150 referrals every week. It is a large list. We also see veterans with personal or family histories of neurologic or cardiologic concerns as well.
Renee, as somebody who fields many of these referrals from unaffected individuals, what is the family history process?
Renee Rider. We don’t expect the referring provider to be a genetic expert. When a provider is seeing a constellation of several different cancers and he or she doesn’t know if there’s anything going on genetically or even if it’s possible, absolutely they should put in a referral to GMS. We have a triage counselor who reviews every consult that comes into our service within 24 hours.
Many cancers are due to exposures that are not concerning for a genetic etiology. We can let you know that it is not concerning, and the PCP can counsel the patient that it is very unlikely to be genetic in nature. We still give feedback even if it’s not someone who is appropriate for genetic counseling and testing. It is important to reach out to GMS even if you don’t know whether a cancer is genetic in nature.
It also is important to take your time when gathering family histories. We get a lot of patients who say, “There’s a lot of cancer in my family. I have no idea who had cancer, but I know a lot of people had cancer.” That’s not the day to put in a referral to GMS. At that point, providers should tell the patient to get as much information as they can about the family history and then reassess. It’s important for us to have accurate information. We’ve had several times where we receive a referral because the veteran says that their sister had ovarian cancer. And then when our staff calls, they later find out it was cervical cancer. That’s not a good use of the veteran’s time, and it’s not a good use of VA resources.
The other important thing about family histories is keeping the questions open-ended. Often a PCP or specialist will ask about a certain type of cancer: “Does anyone in your family have breast cancer, ovarian cancer?” Or if the veteran
is getting a colonoscopy, they ask, “Does anybody have colon cancer?” Where really, we need to be a little bit more open-ended. We prefer questions like, “Has anyone in your family
had cancer?” because that’s the question that prompts a response of, “Yes, 3 people in my family have had thyroid cancer.” That’s very important for us to know, too.
If you do get a positive response, probe a little bit more: what kind of cancer did someone have, how old were they when they had their cancer? And how are they related? Is this an aunt on your mom’s side or on your dad’s side? Those are the types of information that we need to figure out if that person needs a referral.
Vickie Venne. It’s a different story when people already have a cancer diagnosis. Which hematology or oncology patients are good referrals and why?
Lisa Arfons, MD. When patients come in with newly diagnosed cancer, breast for example, it is an emotional diagnosis and psychologicallydistressing. Oftentimes, they want to know why this happened to them. The issues surrounding
genetic testing also becomes very emotional. They want to know whether their children are at risk as well.
Genetic discussions take a long time. I rarely do that on the first visit. I always record for myself in my clinic note if something strikes me regarding the patient’s diagnosis. I quickly run through the National Comprehensive Cancer Network (NCCN) guidelines to remind myself of what I need to go over with the patient at our next meeting. Most patients don’t need to be referred to GMS, and most patients don’t need to be tested once they’re seen.
I often save the referral discussion for after I have established a rapport with a patient, we have a treatment plan, or they already have had their first surgery. Therefore, we are not making decisions about their first surgery based on the genetic medicine results.
If I’m considering a referral, I do a deeper dive with the patient. Is the patient older or younger than 45 years? I pull up NCCN guidelines and we go through the entire checklist.
We have male breast cancer patients at the VA—probably more than the community—so we refer those patients. At the Louis Stokes Cleveland VAMC in Ohio, we have had some in-depth discussions about referring male breast cancer patients for genetic testing and whether it was beneficial to older patients with male breast cancer. Ultimately, we decided that it was important for our male veterans to be tested because it empowered them to have better understanding of their medical conditions that may not just have effect on them but on their offspring, and that that can be a source of psychological and emotional support.
I don’t refer most people to GMS once I go through the checklist. I appreciate the action for an e-consult within the CPRS telemedicine consult itself, as Renee noted. If it is not necessary, GMS makes it an e-consult. I try to communicate that I don’t know whether it is necessary or not so that GMS understands where I’m coming from.
Vickie Venne. In the US Department of Defense (DoD) the process is quite different. Mauricio, can you explain the clinical referral process, who is referred, and how that works from a laboratory perspective?
Maj De Castro, MD, FACMG, USAF. The VA has led the way in demonstrating how to best provide for the medical genetic needs of a large, decentralized population distributed all over the country. Over the last 5 to 10 years, the DoD has made strides in recognizing the role genetics plays in the practice of everyday medicine and redoubling efforts to meet the needs of servicemembers.
The way that it traditionally has worked in the DoD is that military treatment facilities (MTFs) that have dedicated geneticists and genetic counselors: Kessler Medical Center in Mississippi, Walter Reed National Military Medical
Center in Maryland, Tripler Army Medical Center in Hawaii, Madigan Army Medical Center in Washington, Brooke Army Medical Center in Texas, Naval Medical Center San Diego in California, and Naval Medical Center Portsmouth in Virginia. A patient seeking genetic evaluation, counseling, or testing in those larger facilities would be referred to the genetics service by their primary care manager. Wait times vary, but it would usually be weeks, maybe months. However, the great majority of MTFs do not have dedicated genetics support. Most of the time, those patients would have to be referred to the local civilian community—there was no process for them to be seen in in the military healthcare system—with wait times that exceed 6 to 8 months in some cases. This is due to just not a military but a national shortage of genetics professionals (counselors and physicians).
Last year we started the telegenetics initiative, which is small compared to the VA—it is comprised of 2 geneticists and 1 genetic counselor—but with the full intent of growing it over time. Its purpose is to extend the resources we
had to other MTFs. Genetics professionals stationed state-side can provide care to remote facilities with limited access to local genetics support such as Cannon Air Force Base (AFB) or overseas facilities such as Spangdahlem AFB in Germany.
We recognize there are military-specific needs for the DoD regarding the genetic counseling process that have to take into account readiness, genetic discrimination, continued ability to serve and fitness for duty. For this important reason, we are seeking to expand our telegenetics initiative. The goal is to be able to provide 100% of all genetic counseling in-house, so to speak.
Currently, providers at the 4 pilot sites (Cannon AFB, Fort Bragg, Spangdahlem AFB, and Guantanamo Bay) send us referrals. We triage them and assign the patient to see a geneticist or a counselor depending on the indication.
On the laboratory side, it has been a very interesting experience. Because we provide comprehensive germline cancer testing at very little cost to the provider at any MTF, we have had high numbers of test requests over the years.
In addition to saving the DoD millions of dollars in testing, we have learned some interesting lessons in the process. For instance, we have worked closely with several different groups to better understand how to educate providers on the genetic counseling and testing process. This has allowed us to craft a thorough and inclusive consent form that addresses the needs of the DoD. We have also learned valuable lessons about population-based screening vs evidence-based testing, and lessons surrounding narrow-based testing (BRCA1 and BRCA2 only testing) vs ordering a more comprehensive panel that includes other genes supported by strong evidence (such as PALB2, CHEK2, or TP53).
For example, we have found that in a significant proportion of individuals with and without family history, there are clinically relevant variants in genes other than BRCA1 or BRCA2. And so, we have made part of our consent process,
a statement on secondary findings. If the patient consents, we will report pathogenic variants in other genes known to be associated with cancer (with strong evidence) even if the provider ordered a narrow panel such as BRCA1 and BRCA2 testing only. In about 1% to 4% of patients that would otherwise not meet NCCN guidelines, we’ve reported variants that were clinically actionable and changed the medical management of that patient.
We feel strongly that this is a conversation that we need to have in our field, and we realize it’s a complex issue, maybe we need to expand who gets testing. Guideline based testing is missing some patients out there that could benefit from it.
Vickie Venne. There certainly are many sides to the conversation of population-based vs evidence-based genetic testing. Genetic testing policies are changing rapidly. There are teams exploring comprehensive gene sequencing for
newborns and how that potential 1-time test can provide information will be reinterpreted as a person goes from cradle to grave. However, unlike the current DoD process, in the VA there are patients who we don’t see.
Renee Rider. I want to talk about money. When we order a genetic test, that test is paid for by the pathology department at the patient’s VAMC. Most of the pathology departments we work with are clear that they only can provide
genetic testing that is considered medically necessary. Thus, we review each test to make sure it meets established guidelines for testing. We don’t do population genetic screening as there isn’t evidence or guidelines to support offering it. We are strict about who does and does not get genetic testing, partly because we have a responsibility to pathology departments and to the taxpayers.
GMS focuses on conditions that are inherited, that is to say, we deal with germline genetics. Therefore, we discontinue referrals for somatic requests, such as when an OncotypeDX test is requested. It is my understanding that pharmacogenetic referrals may be sent to the new PHASeR initiative, which is a joint collaboration between the VA and Sanford Health and is headed by Deepak Voora, MD.
We generally don’t see patients who still are having diagnostic procedures done. For example, if a veteran has a suspicious breast mass, we recommend that the provider workup the mass before referring to GMS. Regardless of a genetic test result, a suspicious mass needs to be worked up. And, knowing if the mass is cancerous could change how we would proceed with the genetic workup. For example, if the mass were not cancerous, we may recommend that an affected relative have the first genetic evaluation. Furthermore, knowing if the patient has cancer changes how we interpret negative test results.
Another group of patients we don’t see are those who already had genetic testing done by the referring provider. It’s a VA directive that if you order a test, you’re the person who is responsible for giving the results. We agree with
this directive. If you don’t feel comfortable giving back test results, don’t order the test. Often, when a provider sends a patient to us after the test was done, we discover that the patient didn’t have appropriate pretest counseling. A test result, such as a variant of uncertain significance (VUS), should never be a surprise to either the provider or the patient.
Ishta Thakar. For newly diagnosed cancers, the first call is to the patient to inform them that they have cancer. We usually bring up genetic counseling or testing, if applicable, when they are ready to accept the diagnosis and have a conversation about it. All our consults are via telehealth, so none of our patients physically come to GMS in Salt Lake City. All the consults are done virtually.
For newly diagnosed patients, we would send a consult in within a couple of weeks. For patients who had a family history, the referral would not be urgent: They can be seen within about 3 months. The turnaround times for GMS are so much better than what we have available in the community where it’s often at least 6 months, as previously noted.
Vickie Venne. Thank you. We continue to work on that. One of the interesting things that we’ve done, which is the brainchild of Renee, is shared medical appointments.
Renee Rider. We have now created 4 group appointments for people who have concerns surrounding cancer. One group is for people who don’t have cancer but have family members who have cancer who may be the best testing candidate. For example, that might be a 30-year old who tells you that her mother had breast cancer at age 45 years. Her mother is still living, but she’s never had genetic testing. We would put her in a group where we discuss the importance of talking to the family members and encouraging them to go get that first genetic evaluation in the family.
Our second group is for people who don’t have cancer themselves, but have a family history of cancer and those affected relatives have passed away. The family needs a genetic evaluation, and the veteran is the best living testing candidate.
That group is geared towards education about the test and informed consent.
The third group is for people with cancer who qualify for genetic testing. We provide all of the information that they need to make an informed decision on having (or not having) genetic testing.
The final group is for people who have family histories of known genetic mutations in cancer genes. Again, we provide them with all of the information that they need to make an informed decision regarding genetic testing.
With the shared medical appointments, we have been able to greatly increase the number of patients that we can see. Our first 3 groups all meet once a week and can have 10 or 12 veterans. Our last group meets every other week and has a maximum of 6 veterans. Wait times for our groups are generally ≤ 2 weeks. All veterans can choose to have an individual appointment if they prefer. We regularly get unsolicited feedback from veterans that they learn a lot during our groups and appreciate it.
Our group appointments have lowered the wait time for the people in the groups. And, they’ve lowered the wait time for the people who are seen individually. They’ve allowed us to address the backlog of patients waiting to see us in a more timely manner. Our wait time for individual appointment had been approaching 6 months, and it is now about 1.5 months.
We also think that being in a group normalizes the experience. Most people don’t know anyone who has had genetic testing. Now, they are in a group with others going through the same experience. In one of my groups, a male veteran talked about his breast cancer being really rare. Another male in the group volunteer that he had breast cancer, too. They both seemed to appreciate not feeling alone.
Vickie Venne. I want to move to our final piece. What do the referring providers tell the patients about a genetics referral and what should they expect?
Lisa Arfons. First and foremost, I tell the patient that it is a discussion with a genetic counselor. I make it clear that they understand that it is a discussion. They then can agree or not agree to accept genetic testing if it’s recommended.
I talk in general terms about why I think it can be important for them to have the discussion, but that we don’t have great data for decisionmaking. We understand that there are more options for preventive measures but then it ultimately will be a discussion between the PCP, the patient, and their family members about how they proceed about the preventive measures. I want them to start thinking about how the genetic test results, regardless of if they are positive, negative, or a variant that is not yet understood, can impact their offspring.
Probably I am biased, as my mom had breast cancer and she underwent genetic testing. So, I have a bit of an offspring focus as well. I already mentioned that you must discuss about whether or not it’s worth screening or doing any preventive measures on contralateral breast, or screening for things like prostate cancer at age 75 years. And so I focus more on the family members.
I try to stay in my lane. I am extremely uncomfortable when I hear about someone in our facility sending off a blood test and then asking someone else to interpret the results and discuss it with the patient. Just because it’s a blood test and it’s easy to order doesn’t mean that it is easy to know what to do with it, and it needs to be respected as such.
Ishta Thakar. Our PCPs let the patients know that GMS will contact the patient to schedule a video appointment and that if they want to bring any family members along with them, they’re welcome to. We also explain that certain cancers are genetically based and that if they have a genetic mutation, it can be passed on to their offspring. I also explain that if they have certain mutations, then we would be more vigilant in screening them for other kinds of cancers. That’s the reason that we refer that they get counseled. After counseling if they’re ready for the testing, then the counselor orders the test and does the posttest discussion with the patient.
Vickie Venne. In the VA, people are invited to attend a genetic counseling session but can certainly decline. Does the the DoD have a different approach?
Maj De Castro. I would say that the great majority of active duty patients have limited knowledge of what to expect out of a genetics appointment. One of the main things we do is educate them on their rights and protections and the potential risks associated with performing genetic testing, in particular when it comes to their continued ability to serve. Genetic testing for clinical purposes is not mandatory in the DoD, patients can certainly decline testing. Because genetic testing has the potential to alter someone’s career, it is critical we have a very thorough and comprehensive pre- and posttest counseling sessions that includes everything from career implications to the Genetic Information Nondiscrimination Act (GINA) and genetic discrimination in the military, in addition to the standard of care medical information.
Scenarios in which a servicemember is negatively impacted by pursuing a genetic diagnosis are very rare. More than 90% of the time, genetic counseling and/or testing has no adverse career effect. When they do, it is out of concern for the safety and wellbeing of a servicemember. For instance, if we diagnosis a patient with a genetic form of some arrhythmogenic disorder, part of the treatment plan can be to limit that person’s level of exertion, because it could potentially lead to death. We don’t want to put someone in a situation that may trigger that.
Vickie Venne. We also have a certain number of veterans who ask us about their service disability pay and the impact of genetic testing on it. One example is veterans with prostate cancer who were exposed to Agent Orange, which has been associated with increased risk for developing prostate cancer. I have had men who have been referred for genetic evaluation ask, “Well, if I have an identifiable mutation, how will that impact my service disability?” So we discuss the carcinogenic process that may include an inherited component as well as the environmental risk factors. I think that’s a unique issue for a population we’re honored to be able to serve.
Renee Rider. When we are talking about how the population of veterans is unique, I think it is also important to acknowledge mental health. I’ve had several patients tell me that they have posttraumatic stress disorder or anxiety and the idea of getting an indeterminant test result, such as VUS, would really weigh on them.
In the community, a lot of providers order the biggest panel they can, but for these patients who are worried about getting those indeterminant test results, I’ve been able to work with them to limit the size of the panel. I order a small panel that only has genes that have implications for that veteran’s clinical management. For example, in a patient with ductal breast cancer, I remove the genes that cause lobular breast cancer. This takes a bit of knowledge and critical thinking that our VA genetic counselors have because they have experience with veterans and their needs.
As our time draws to a close, I have one final thought. This has been a heartwarming conversation today. It is really nice to hear that GMS services are appreciated. We in GMS want to partner with our referring providers. Help us help you! When you enter a referral, please let us know how we can help you. The more we understand why you are sending your veteran to GMS, the more we can help meet your needs. If there are any questions or problems, feel free to send us an email or pick up the phone and call us.
Vickie Venne, MS. What is the Genomic Medicine Service (GMS) at the US Department of Veterans Affairs (VA)?
Renee Rider, JD, MS, LCGC. GMS is a telehealth service. We are part of central office and field stationed at the George E. Wahlen VA Medical Center (VAMC) in Salt Lake City, Utah. We provide care to about 90 VAMCs and their associated clinics. Veterans are referred to us by entering an interfacility consult in the VA Computerized Patient Record System (CPRS). We review the consult to determine whether the patient needs to be seen, whether we can answer with an e-consult, or whether we need more information. For the patients who need an appointment, the telehealth department at the veteran’s VA facility will contact the patient to arrange a visit with us. At the time of the appointment, the facility has a staff member available to seat the patient and connect them to us using video equipment.
We provide genetic care for all specialties, including cancer, women’s health, cardiology and neurology. In today’s discussion, we are focusing on cancer care.
Vickie Venne. What do patients do at facilities that don’t get care through GMS?
Renee Rider. There are a handful of facilities that provide their own genetic care in-house. For example, VA Boston Healthcare System in Massachusetts and the Michael E. DeBakey VAMC in Houston, Texas each have their own programs. For veterans who are not at a VA facility that has an agreement with GMS and do not have a different genetics program, their providers need to make referrals to community care.
Vickie Venne. How do patients get referred and what happens at their facility when the patients return to the specialty and primary care providers (PCP)? Ishta, who do you refer to GMS and how do you define them initially?
Ishta Thakar, MD, FACP. Referrals can come at a couple of points during a veteran’s journey at the VA. The VA covers obstetrics care for women veterans. Whenever a PCP or a women’s health provider is doing the initial history and physical on a new patient, if the female veteran has an extensive family history of breast, ovarian, colon, or endometrial cancer, then we take more history and we send a consult to GMS. The second instance would be if she tells us that she has had a personal history of breast, ovarian, or endometrial cancer and she has never had genetic testing. The third instance would be whenever we have a female veteran who is diagnosed with breast, ovarian, endometrial, or colon cancer. We would definitely talk to her about genetic counseling and send a referral to GMS. We would ask for a GMS consult for a patient with advanced maternal age, with exposure to some kind of teratogens, with an abnormal ultrasound, a family history of chromosomal disorders, or if she’s seeing an obstetrician who wants her to be tested. And finally, if a patient has a constellation of multiple cancers in the family and we don’t know what’s going on, we would also refer the patient to GMS.
Vickie Venne. That would be why GMS fields over 150 referrals every week. It is a large list. We also see veterans with personal or family histories of neurologic or cardiologic concerns as well.
Renee, as somebody who fields many of these referrals from unaffected individuals, what is the family history process?
Renee Rider. We don’t expect the referring provider to be a genetic expert. When a provider is seeing a constellation of several different cancers and he or she doesn’t know if there’s anything going on genetically or even if it’s possible, absolutely they should put in a referral to GMS. We have a triage counselor who reviews every consult that comes into our service within 24 hours.
Many cancers are due to exposures that are not concerning for a genetic etiology. We can let you know that it is not concerning, and the PCP can counsel the patient that it is very unlikely to be genetic in nature. We still give feedback even if it’s not someone who is appropriate for genetic counseling and testing. It is important to reach out to GMS even if you don’t know whether a cancer is genetic in nature.
It also is important to take your time when gathering family histories. We get a lot of patients who say, “There’s a lot of cancer in my family. I have no idea who had cancer, but I know a lot of people had cancer.” That’s not the day to put in a referral to GMS. At that point, providers should tell the patient to get as much information as they can about the family history and then reassess. It’s important for us to have accurate information. We’ve had several times where we receive a referral because the veteran says that their sister had ovarian cancer. And then when our staff calls, they later find out it was cervical cancer. That’s not a good use of the veteran’s time, and it’s not a good use of VA resources.
The other important thing about family histories is keeping the questions open-ended. Often a PCP or specialist will ask about a certain type of cancer: “Does anyone in your family have breast cancer, ovarian cancer?” Or if the veteran
is getting a colonoscopy, they ask, “Does anybody have colon cancer?” Where really, we need to be a little bit more open-ended. We prefer questions like, “Has anyone in your family
had cancer?” because that’s the question that prompts a response of, “Yes, 3 people in my family have had thyroid cancer.” That’s very important for us to know, too.
If you do get a positive response, probe a little bit more: what kind of cancer did someone have, how old were they when they had their cancer? And how are they related? Is this an aunt on your mom’s side or on your dad’s side? Those are the types of information that we need to figure out if that person needs a referral.
Vickie Venne. It’s a different story when people already have a cancer diagnosis. Which hematology or oncology patients are good referrals and why?
Lisa Arfons, MD. When patients come in with newly diagnosed cancer, breast for example, it is an emotional diagnosis and psychologicallydistressing. Oftentimes, they want to know why this happened to them. The issues surrounding
genetic testing also becomes very emotional. They want to know whether their children are at risk as well.
Genetic discussions take a long time. I rarely do that on the first visit. I always record for myself in my clinic note if something strikes me regarding the patient’s diagnosis. I quickly run through the National Comprehensive Cancer Network (NCCN) guidelines to remind myself of what I need to go over with the patient at our next meeting. Most patients don’t need to be referred to GMS, and most patients don’t need to be tested once they’re seen.
I often save the referral discussion for after I have established a rapport with a patient, we have a treatment plan, or they already have had their first surgery. Therefore, we are not making decisions about their first surgery based on the genetic medicine results.
If I’m considering a referral, I do a deeper dive with the patient. Is the patient older or younger than 45 years? I pull up NCCN guidelines and we go through the entire checklist.
We have male breast cancer patients at the VA—probably more than the community—so we refer those patients. At the Louis Stokes Cleveland VAMC in Ohio, we have had some in-depth discussions about referring male breast cancer patients for genetic testing and whether it was beneficial to older patients with male breast cancer. Ultimately, we decided that it was important for our male veterans to be tested because it empowered them to have better understanding of their medical conditions that may not just have effect on them but on their offspring, and that that can be a source of psychological and emotional support.
I don’t refer most people to GMS once I go through the checklist. I appreciate the action for an e-consult within the CPRS telemedicine consult itself, as Renee noted. If it is not necessary, GMS makes it an e-consult. I try to communicate that I don’t know whether it is necessary or not so that GMS understands where I’m coming from.
Vickie Venne. In the US Department of Defense (DoD) the process is quite different. Mauricio, can you explain the clinical referral process, who is referred, and how that works from a laboratory perspective?
Maj De Castro, MD, FACMG, USAF. The VA has led the way in demonstrating how to best provide for the medical genetic needs of a large, decentralized population distributed all over the country. Over the last 5 to 10 years, the DoD has made strides in recognizing the role genetics plays in the practice of everyday medicine and redoubling efforts to meet the needs of servicemembers.
The way that it traditionally has worked in the DoD is that military treatment facilities (MTFs) that have dedicated geneticists and genetic counselors: Kessler Medical Center in Mississippi, Walter Reed National Military Medical
Center in Maryland, Tripler Army Medical Center in Hawaii, Madigan Army Medical Center in Washington, Brooke Army Medical Center in Texas, Naval Medical Center San Diego in California, and Naval Medical Center Portsmouth in Virginia. A patient seeking genetic evaluation, counseling, or testing in those larger facilities would be referred to the genetics service by their primary care manager. Wait times vary, but it would usually be weeks, maybe months. However, the great majority of MTFs do not have dedicated genetics support. Most of the time, those patients would have to be referred to the local civilian community—there was no process for them to be seen in in the military healthcare system—with wait times that exceed 6 to 8 months in some cases. This is due to just not a military but a national shortage of genetics professionals (counselors and physicians).
Last year we started the telegenetics initiative, which is small compared to the VA—it is comprised of 2 geneticists and 1 genetic counselor—but with the full intent of growing it over time. Its purpose is to extend the resources we
had to other MTFs. Genetics professionals stationed state-side can provide care to remote facilities with limited access to local genetics support such as Cannon Air Force Base (AFB) or overseas facilities such as Spangdahlem AFB in Germany.
We recognize there are military-specific needs for the DoD regarding the genetic counseling process that have to take into account readiness, genetic discrimination, continued ability to serve and fitness for duty. For this important reason, we are seeking to expand our telegenetics initiative. The goal is to be able to provide 100% of all genetic counseling in-house, so to speak.
Currently, providers at the 4 pilot sites (Cannon AFB, Fort Bragg, Spangdahlem AFB, and Guantanamo Bay) send us referrals. We triage them and assign the patient to see a geneticist or a counselor depending on the indication.
On the laboratory side, it has been a very interesting experience. Because we provide comprehensive germline cancer testing at very little cost to the provider at any MTF, we have had high numbers of test requests over the years.
In addition to saving the DoD millions of dollars in testing, we have learned some interesting lessons in the process. For instance, we have worked closely with several different groups to better understand how to educate providers on the genetic counseling and testing process. This has allowed us to craft a thorough and inclusive consent form that addresses the needs of the DoD. We have also learned valuable lessons about population-based screening vs evidence-based testing, and lessons surrounding narrow-based testing (BRCA1 and BRCA2 only testing) vs ordering a more comprehensive panel that includes other genes supported by strong evidence (such as PALB2, CHEK2, or TP53).
For example, we have found that in a significant proportion of individuals with and without family history, there are clinically relevant variants in genes other than BRCA1 or BRCA2. And so, we have made part of our consent process,
a statement on secondary findings. If the patient consents, we will report pathogenic variants in other genes known to be associated with cancer (with strong evidence) even if the provider ordered a narrow panel such as BRCA1 and BRCA2 testing only. In about 1% to 4% of patients that would otherwise not meet NCCN guidelines, we’ve reported variants that were clinically actionable and changed the medical management of that patient.
We feel strongly that this is a conversation that we need to have in our field, and we realize it’s a complex issue, maybe we need to expand who gets testing. Guideline based testing is missing some patients out there that could benefit from it.
Vickie Venne. There certainly are many sides to the conversation of population-based vs evidence-based genetic testing. Genetic testing policies are changing rapidly. There are teams exploring comprehensive gene sequencing for
newborns and how that potential 1-time test can provide information will be reinterpreted as a person goes from cradle to grave. However, unlike the current DoD process, in the VA there are patients who we don’t see.
Renee Rider. I want to talk about money. When we order a genetic test, that test is paid for by the pathology department at the patient’s VAMC. Most of the pathology departments we work with are clear that they only can provide
genetic testing that is considered medically necessary. Thus, we review each test to make sure it meets established guidelines for testing. We don’t do population genetic screening as there isn’t evidence or guidelines to support offering it. We are strict about who does and does not get genetic testing, partly because we have a responsibility to pathology departments and to the taxpayers.
GMS focuses on conditions that are inherited, that is to say, we deal with germline genetics. Therefore, we discontinue referrals for somatic requests, such as when an OncotypeDX test is requested. It is my understanding that pharmacogenetic referrals may be sent to the new PHASeR initiative, which is a joint collaboration between the VA and Sanford Health and is headed by Deepak Voora, MD.
We generally don’t see patients who still are having diagnostic procedures done. For example, if a veteran has a suspicious breast mass, we recommend that the provider workup the mass before referring to GMS. Regardless of a genetic test result, a suspicious mass needs to be worked up. And, knowing if the mass is cancerous could change how we would proceed with the genetic workup. For example, if the mass were not cancerous, we may recommend that an affected relative have the first genetic evaluation. Furthermore, knowing if the patient has cancer changes how we interpret negative test results.
Another group of patients we don’t see are those who already had genetic testing done by the referring provider. It’s a VA directive that if you order a test, you’re the person who is responsible for giving the results. We agree with
this directive. If you don’t feel comfortable giving back test results, don’t order the test. Often, when a provider sends a patient to us after the test was done, we discover that the patient didn’t have appropriate pretest counseling. A test result, such as a variant of uncertain significance (VUS), should never be a surprise to either the provider or the patient.
Ishta Thakar. For newly diagnosed cancers, the first call is to the patient to inform them that they have cancer. We usually bring up genetic counseling or testing, if applicable, when they are ready to accept the diagnosis and have a conversation about it. All our consults are via telehealth, so none of our patients physically come to GMS in Salt Lake City. All the consults are done virtually.
For newly diagnosed patients, we would send a consult in within a couple of weeks. For patients who had a family history, the referral would not be urgent: They can be seen within about 3 months. The turnaround times for GMS are so much better than what we have available in the community where it’s often at least 6 months, as previously noted.
Vickie Venne. Thank you. We continue to work on that. One of the interesting things that we’ve done, which is the brainchild of Renee, is shared medical appointments.
Renee Rider. We have now created 4 group appointments for people who have concerns surrounding cancer. One group is for people who don’t have cancer but have family members who have cancer who may be the best testing candidate. For example, that might be a 30-year old who tells you that her mother had breast cancer at age 45 years. Her mother is still living, but she’s never had genetic testing. We would put her in a group where we discuss the importance of talking to the family members and encouraging them to go get that first genetic evaluation in the family.
Our second group is for people who don’t have cancer themselves, but have a family history of cancer and those affected relatives have passed away. The family needs a genetic evaluation, and the veteran is the best living testing candidate.
That group is geared towards education about the test and informed consent.
The third group is for people with cancer who qualify for genetic testing. We provide all of the information that they need to make an informed decision on having (or not having) genetic testing.
The final group is for people who have family histories of known genetic mutations in cancer genes. Again, we provide them with all of the information that they need to make an informed decision regarding genetic testing.
With the shared medical appointments, we have been able to greatly increase the number of patients that we can see. Our first 3 groups all meet once a week and can have 10 or 12 veterans. Our last group meets every other week and has a maximum of 6 veterans. Wait times for our groups are generally ≤ 2 weeks. All veterans can choose to have an individual appointment if they prefer. We regularly get unsolicited feedback from veterans that they learn a lot during our groups and appreciate it.
Our group appointments have lowered the wait time for the people in the groups. And, they’ve lowered the wait time for the people who are seen individually. They’ve allowed us to address the backlog of patients waiting to see us in a more timely manner. Our wait time for individual appointment had been approaching 6 months, and it is now about 1.5 months.
We also think that being in a group normalizes the experience. Most people don’t know anyone who has had genetic testing. Now, they are in a group with others going through the same experience. In one of my groups, a male veteran talked about his breast cancer being really rare. Another male in the group volunteer that he had breast cancer, too. They both seemed to appreciate not feeling alone.
Vickie Venne. I want to move to our final piece. What do the referring providers tell the patients about a genetics referral and what should they expect?
Lisa Arfons. First and foremost, I tell the patient that it is a discussion with a genetic counselor. I make it clear that they understand that it is a discussion. They then can agree or not agree to accept genetic testing if it’s recommended.
I talk in general terms about why I think it can be important for them to have the discussion, but that we don’t have great data for decisionmaking. We understand that there are more options for preventive measures but then it ultimately will be a discussion between the PCP, the patient, and their family members about how they proceed about the preventive measures. I want them to start thinking about how the genetic test results, regardless of if they are positive, negative, or a variant that is not yet understood, can impact their offspring.
Probably I am biased, as my mom had breast cancer and she underwent genetic testing. So, I have a bit of an offspring focus as well. I already mentioned that you must discuss about whether or not it’s worth screening or doing any preventive measures on contralateral breast, or screening for things like prostate cancer at age 75 years. And so I focus more on the family members.
I try to stay in my lane. I am extremely uncomfortable when I hear about someone in our facility sending off a blood test and then asking someone else to interpret the results and discuss it with the patient. Just because it’s a blood test and it’s easy to order doesn’t mean that it is easy to know what to do with it, and it needs to be respected as such.
Ishta Thakar. Our PCPs let the patients know that GMS will contact the patient to schedule a video appointment and that if they want to bring any family members along with them, they’re welcome to. We also explain that certain cancers are genetically based and that if they have a genetic mutation, it can be passed on to their offspring. I also explain that if they have certain mutations, then we would be more vigilant in screening them for other kinds of cancers. That’s the reason that we refer that they get counseled. After counseling if they’re ready for the testing, then the counselor orders the test and does the posttest discussion with the patient.
Vickie Venne. In the VA, people are invited to attend a genetic counseling session but can certainly decline. Does the the DoD have a different approach?
Maj De Castro. I would say that the great majority of active duty patients have limited knowledge of what to expect out of a genetics appointment. One of the main things we do is educate them on their rights and protections and the potential risks associated with performing genetic testing, in particular when it comes to their continued ability to serve. Genetic testing for clinical purposes is not mandatory in the DoD, patients can certainly decline testing. Because genetic testing has the potential to alter someone’s career, it is critical we have a very thorough and comprehensive pre- and posttest counseling sessions that includes everything from career implications to the Genetic Information Nondiscrimination Act (GINA) and genetic discrimination in the military, in addition to the standard of care medical information.
Scenarios in which a servicemember is negatively impacted by pursuing a genetic diagnosis are very rare. More than 90% of the time, genetic counseling and/or testing has no adverse career effect. When they do, it is out of concern for the safety and wellbeing of a servicemember. For instance, if we diagnosis a patient with a genetic form of some arrhythmogenic disorder, part of the treatment plan can be to limit that person’s level of exertion, because it could potentially lead to death. We don’t want to put someone in a situation that may trigger that.
Vickie Venne. We also have a certain number of veterans who ask us about their service disability pay and the impact of genetic testing on it. One example is veterans with prostate cancer who were exposed to Agent Orange, which has been associated with increased risk for developing prostate cancer. I have had men who have been referred for genetic evaluation ask, “Well, if I have an identifiable mutation, how will that impact my service disability?” So we discuss the carcinogenic process that may include an inherited component as well as the environmental risk factors. I think that’s a unique issue for a population we’re honored to be able to serve.
Renee Rider. When we are talking about how the population of veterans is unique, I think it is also important to acknowledge mental health. I’ve had several patients tell me that they have posttraumatic stress disorder or anxiety and the idea of getting an indeterminant test result, such as VUS, would really weigh on them.
In the community, a lot of providers order the biggest panel they can, but for these patients who are worried about getting those indeterminant test results, I’ve been able to work with them to limit the size of the panel. I order a small panel that only has genes that have implications for that veteran’s clinical management. For example, in a patient with ductal breast cancer, I remove the genes that cause lobular breast cancer. This takes a bit of knowledge and critical thinking that our VA genetic counselors have because they have experience with veterans and their needs.
As our time draws to a close, I have one final thought. This has been a heartwarming conversation today. It is really nice to hear that GMS services are appreciated. We in GMS want to partner with our referring providers. Help us help you! When you enter a referral, please let us know how we can help you. The more we understand why you are sending your veteran to GMS, the more we can help meet your needs. If there are any questions or problems, feel free to send us an email or pick up the phone and call us.
A Safe Treatment Switch for Patients With Prostate Cancer
Degarelix was developed as a novel gonadotropin-releasing hormone (GnRH) antagonist, with the aim of counteracting the testosterone surge often experienced with GnRH agonists. Degarelix blocks the GnRH receptors in the pituitary gland, rapidly reducing testosterone production, but the effects last only for a month. It is common practice to switch from degarelix to a GnRH agonist once the testosterone levels are down and stable. Degarelix is safe and effective for the short term, but what about the long term?
Researchers from Osaka City University and Bell Land General Hospital in Japan evaluated 5-year survival and time to castration-resistant prostate cancer (CRPC) in 108 patients with prostate cancer treated with degarelix. In the study, 57 patients were switched from degarelix to a GnRH agonist; 51 continued on degarelix.
Overall 5-year survival was high (89%) but statistically superior in the changed group (97% vs 74%). The 5-year cancer-specific survival also was longer in the changed group (100% vs 85%). Average time to CRCP was comparable in both groups (43 months in the changed group, 35 months in the continued group). The CRPC conversion did not reach the median at the time of data analysis. The median percentage decrease in prostate-specific antigen level for all patients treated with degarelix was 99.7%. The lowered levels were maintained even after switching to GnRH agonists.
The researchers say theirs is the first report of long-term data on degarelix and the first study to report that changing the treatment from a GnRH antagonist to a GnRH agonist did not affect the oncologic outcomes in patients with hormone-sensitive prostate cancer.
Source:
Asakawa J, Iguchi T, Tamada S, et al. Basic Clin Androl. 2018;28:9.
doi: 10.1186/s12610-018-0074-2.
Degarelix was developed as a novel gonadotropin-releasing hormone (GnRH) antagonist, with the aim of counteracting the testosterone surge often experienced with GnRH agonists. Degarelix blocks the GnRH receptors in the pituitary gland, rapidly reducing testosterone production, but the effects last only for a month. It is common practice to switch from degarelix to a GnRH agonist once the testosterone levels are down and stable. Degarelix is safe and effective for the short term, but what about the long term?
Researchers from Osaka City University and Bell Land General Hospital in Japan evaluated 5-year survival and time to castration-resistant prostate cancer (CRPC) in 108 patients with prostate cancer treated with degarelix. In the study, 57 patients were switched from degarelix to a GnRH agonist; 51 continued on degarelix.
Overall 5-year survival was high (89%) but statistically superior in the changed group (97% vs 74%). The 5-year cancer-specific survival also was longer in the changed group (100% vs 85%). Average time to CRCP was comparable in both groups (43 months in the changed group, 35 months in the continued group). The CRPC conversion did not reach the median at the time of data analysis. The median percentage decrease in prostate-specific antigen level for all patients treated with degarelix was 99.7%. The lowered levels were maintained even after switching to GnRH agonists.
The researchers say theirs is the first report of long-term data on degarelix and the first study to report that changing the treatment from a GnRH antagonist to a GnRH agonist did not affect the oncologic outcomes in patients with hormone-sensitive prostate cancer.
Source:
Asakawa J, Iguchi T, Tamada S, et al. Basic Clin Androl. 2018;28:9.
doi: 10.1186/s12610-018-0074-2.
Degarelix was developed as a novel gonadotropin-releasing hormone (GnRH) antagonist, with the aim of counteracting the testosterone surge often experienced with GnRH agonists. Degarelix blocks the GnRH receptors in the pituitary gland, rapidly reducing testosterone production, but the effects last only for a month. It is common practice to switch from degarelix to a GnRH agonist once the testosterone levels are down and stable. Degarelix is safe and effective for the short term, but what about the long term?
Researchers from Osaka City University and Bell Land General Hospital in Japan evaluated 5-year survival and time to castration-resistant prostate cancer (CRPC) in 108 patients with prostate cancer treated with degarelix. In the study, 57 patients were switched from degarelix to a GnRH agonist; 51 continued on degarelix.
Overall 5-year survival was high (89%) but statistically superior in the changed group (97% vs 74%). The 5-year cancer-specific survival also was longer in the changed group (100% vs 85%). Average time to CRCP was comparable in both groups (43 months in the changed group, 35 months in the continued group). The CRPC conversion did not reach the median at the time of data analysis. The median percentage decrease in prostate-specific antigen level for all patients treated with degarelix was 99.7%. The lowered levels were maintained even after switching to GnRH agonists.
The researchers say theirs is the first report of long-term data on degarelix and the first study to report that changing the treatment from a GnRH antagonist to a GnRH agonist did not affect the oncologic outcomes in patients with hormone-sensitive prostate cancer.
Source:
Asakawa J, Iguchi T, Tamada S, et al. Basic Clin Androl. 2018;28:9.
doi: 10.1186/s12610-018-0074-2.
Multilevel Predictors of Surveillance PSA Guideline Concordance After Radical Prostatectomy: A National Veterans Affairs Study
Purpose/Rationale: To examine national trends and predictors of annual surveillance prostate specific antigen (PSA attainment after radical prostatectomy among veterans with prostate cancer.
Background: Guidelines recommend men treated for prostate cancer undergo PSA surveillance at least annually, as salvage treatments exist when recurrence is detected early. Predictors of adherence are poorly understood. We therefore examined national trends in PSA surveillance after prostatectomy.
Methods: We used the Veterans Affairs Central Cancer Registry to identify 9,648 patients treated with radical prostatectomy from 2005-2008 with follow up through 2012. We defined guideline-concordant PSA surveillance as receipt of at least one PSA annually. We used multivariable logistic regression to examine associations between guideline concordance and demographic and clinical factors, including PSA values in the preceding year. We assessed facility predictors and variation using multilevel regression.
Results: We found decreasing annual concordance over time ( > 90% years 1-2, 80% year 7) and 69.7% five-year concordance. On multivariable analysis, guideline concordance was lower among those who were black, non-married, non-Hispanic, had PSA at diagnosis > 10 and 20, and had negative or unknown surgical margins (P < .05). Guideline concordance significantly increased once the PSA increased beyond 4 ng/ml. Controlling for facility level variation and covariates eliminated the disparity for black men. Facility-level guideline concordance ranged from 17-100% and was inversely related to urologist workforce (aOR 0.97 [FTE/patient], P = .009).
Conclusions: The majority of patients receive guideline concordant PSA surveillance after prostate cancer surgery, but wide facility level variation exists. Concordance sharply increases when PSA values increase past 4, suggesting that a lab threshold that is not relevant in the post-prostatectomy setting is providing false reassurance to providers and possibly contributing to missed opportunities to salvage men with curable disease. Racial disparities exist, which are related to facility-level variation. Better understanding risk stratification for surveillance and the impact of broad interventions (eg, survivorship care plans, electronic reminders, provider education) on guideline concordance appears warranted.
Purpose/Rationale: To examine national trends and predictors of annual surveillance prostate specific antigen (PSA attainment after radical prostatectomy among veterans with prostate cancer.
Background: Guidelines recommend men treated for prostate cancer undergo PSA surveillance at least annually, as salvage treatments exist when recurrence is detected early. Predictors of adherence are poorly understood. We therefore examined national trends in PSA surveillance after prostatectomy.
Methods: We used the Veterans Affairs Central Cancer Registry to identify 9,648 patients treated with radical prostatectomy from 2005-2008 with follow up through 2012. We defined guideline-concordant PSA surveillance as receipt of at least one PSA annually. We used multivariable logistic regression to examine associations between guideline concordance and demographic and clinical factors, including PSA values in the preceding year. We assessed facility predictors and variation using multilevel regression.
Results: We found decreasing annual concordance over time ( > 90% years 1-2, 80% year 7) and 69.7% five-year concordance. On multivariable analysis, guideline concordance was lower among those who were black, non-married, non-Hispanic, had PSA at diagnosis > 10 and 20, and had negative or unknown surgical margins (P < .05). Guideline concordance significantly increased once the PSA increased beyond 4 ng/ml. Controlling for facility level variation and covariates eliminated the disparity for black men. Facility-level guideline concordance ranged from 17-100% and was inversely related to urologist workforce (aOR 0.97 [FTE/patient], P = .009).
Conclusions: The majority of patients receive guideline concordant PSA surveillance after prostate cancer surgery, but wide facility level variation exists. Concordance sharply increases when PSA values increase past 4, suggesting that a lab threshold that is not relevant in the post-prostatectomy setting is providing false reassurance to providers and possibly contributing to missed opportunities to salvage men with curable disease. Racial disparities exist, which are related to facility-level variation. Better understanding risk stratification for surveillance and the impact of broad interventions (eg, survivorship care plans, electronic reminders, provider education) on guideline concordance appears warranted.
Purpose/Rationale: To examine national trends and predictors of annual surveillance prostate specific antigen (PSA attainment after radical prostatectomy among veterans with prostate cancer.
Background: Guidelines recommend men treated for prostate cancer undergo PSA surveillance at least annually, as salvage treatments exist when recurrence is detected early. Predictors of adherence are poorly understood. We therefore examined national trends in PSA surveillance after prostatectomy.
Methods: We used the Veterans Affairs Central Cancer Registry to identify 9,648 patients treated with radical prostatectomy from 2005-2008 with follow up through 2012. We defined guideline-concordant PSA surveillance as receipt of at least one PSA annually. We used multivariable logistic regression to examine associations between guideline concordance and demographic and clinical factors, including PSA values in the preceding year. We assessed facility predictors and variation using multilevel regression.
Results: We found decreasing annual concordance over time ( > 90% years 1-2, 80% year 7) and 69.7% five-year concordance. On multivariable analysis, guideline concordance was lower among those who were black, non-married, non-Hispanic, had PSA at diagnosis > 10 and 20, and had negative or unknown surgical margins (P < .05). Guideline concordance significantly increased once the PSA increased beyond 4 ng/ml. Controlling for facility level variation and covariates eliminated the disparity for black men. Facility-level guideline concordance ranged from 17-100% and was inversely related to urologist workforce (aOR 0.97 [FTE/patient], P = .009).
Conclusions: The majority of patients receive guideline concordant PSA surveillance after prostate cancer surgery, but wide facility level variation exists. Concordance sharply increases when PSA values increase past 4, suggesting that a lab threshold that is not relevant in the post-prostatectomy setting is providing false reassurance to providers and possibly contributing to missed opportunities to salvage men with curable disease. Racial disparities exist, which are related to facility-level variation. Better understanding risk stratification for surveillance and the impact of broad interventions (eg, survivorship care plans, electronic reminders, provider education) on guideline concordance appears warranted.
Bladder Toxicity After Volumetric Arc Radiation Therapy (VMAT) Treatment for Prostate Cancer Following Prostatectomy
Methods: We did a retrospective review of 55 patients with prostate cancer treated using external beam radiation therapy VMAT between 2013 through 2017.
Results: Sixteen were adjuvant/salvage therapy to the prostate fossa (PF) after a prostatectomy while 39 had primary radiation therapy for intact prostate cancer. The dose volume histogram (DVH) institutional bladder constraints were v65 200 cc, 55% when > 150 cc and there were no incidences of hematuria when the PTV was < 150 cc.
Conclusions: (1) Overall incidence of hematuria with VMAT treatment to the prostate was 10/55(18%); (2) Higher bladder DVH v65 volumes correlated with higher incidence of hematuria; (3) Higher PTV in PF group correlated with higher incidence of hematuria with the greatest risk occurring when the PTV was greater than 200 cc. This is due to more bladder in the treatment field; (4) Careful patient selection should be made for surgery to avoid post-surgery radiation therapy; (5) When treating PF keep the PTV volume under 150 cc; and (6) This finding should be studied with larger number of patients.
Methods: We did a retrospective review of 55 patients with prostate cancer treated using external beam radiation therapy VMAT between 2013 through 2017.
Results: Sixteen were adjuvant/salvage therapy to the prostate fossa (PF) after a prostatectomy while 39 had primary radiation therapy for intact prostate cancer. The dose volume histogram (DVH) institutional bladder constraints were v65 200 cc, 55% when > 150 cc and there were no incidences of hematuria when the PTV was < 150 cc.
Conclusions: (1) Overall incidence of hematuria with VMAT treatment to the prostate was 10/55(18%); (2) Higher bladder DVH v65 volumes correlated with higher incidence of hematuria; (3) Higher PTV in PF group correlated with higher incidence of hematuria with the greatest risk occurring when the PTV was greater than 200 cc. This is due to more bladder in the treatment field; (4) Careful patient selection should be made for surgery to avoid post-surgery radiation therapy; (5) When treating PF keep the PTV volume under 150 cc; and (6) This finding should be studied with larger number of patients.
Methods: We did a retrospective review of 55 patients with prostate cancer treated using external beam radiation therapy VMAT between 2013 through 2017.
Results: Sixteen were adjuvant/salvage therapy to the prostate fossa (PF) after a prostatectomy while 39 had primary radiation therapy for intact prostate cancer. The dose volume histogram (DVH) institutional bladder constraints were v65 200 cc, 55% when > 150 cc and there were no incidences of hematuria when the PTV was < 150 cc.
Conclusions: (1) Overall incidence of hematuria with VMAT treatment to the prostate was 10/55(18%); (2) Higher bladder DVH v65 volumes correlated with higher incidence of hematuria; (3) Higher PTV in PF group correlated with higher incidence of hematuria with the greatest risk occurring when the PTV was greater than 200 cc. This is due to more bladder in the treatment field; (4) Careful patient selection should be made for surgery to avoid post-surgery radiation therapy; (5) When treating PF keep the PTV volume under 150 cc; and (6) This finding should be studied with larger number of patients.
Presentation of A Rare Malignancy: Leiomyosarcoma of the Prostate
Background: Prostatic leiomyosarcoma is a rare tumor that accounts for less than 0.1% of all primary prostatic malignancies. This neoplasm is composed of highly aggressive prostatic smooth muscle cells that presents with nonspecific signs and symptoms mimicking other forms of prostatic pathology.
Case Report: A 72-year-old male presented with 6 months of progressive severe lower urinary tract symptoms (LUTS) secondary to bladder outlet obstruction. The patient was refractory to medical management and required multiple emergent bladder catheterizations. Workup with urinalysis, blood biochemistry, and PSA levels were persistently normal. He denied hematuria, weight loss, or perineal pain. On rectal exam, a mass like induration was noted along the right upper lobe of the prostate.
The patient was referred for transurethral resection of the prostate (TURP) for suspected severe BPH. Histopathological examination demonstrated atypical cytology consistent with high-grade leiomyosarcoma. A PET scan revealed a 1.9 cm tumor with uptake of 12.6 SUV in the right posterior prostate.
Discussion: Fewer than 200 cases of prostatic leiomyosarcoma have been reported. Patients typically present between 41-78 years of age (mean age of 61 years) with signs and symptoms related to LUTS (89.4%) and perineal or rectal pain (25.6%). Constitutional symptoms, burning on ejaculation, and hematuria are uncommon. PSA levels remain normal, due to its non-epithelial etiology, which may contribute to delays in diagnosis.
Diagnosis is usually achieved after a TURP procedure or transrectal needle biopsy. Pathology demonstrates neoplastic spindle cells with nuclear atypia, multifocal necrosis, and cystic degeneration. Immunohistochemistry is characteristically positive for desmin, smooth muscle actin, and vimentin. Tumors have been reported to range between 2-31 cm in size, frequently presenting with invasion of local structures. The lungs are the most common site of distant metastasis.
Treatment may include a multimodal approach of surgery, radiation, and chemotherapy. Long-term prognosis is poor due to the tumors aggressive nature, and recurrence is common. Median survival is estimated at 17 months and 50-75% of patients die within 2-5 years of diagnosis. Due to the substantially high risk of death, prostatic leiomyosarcoma may be one of the most aggressive and poorly prognostic malignancies involving the prostate.
Background: Prostatic leiomyosarcoma is a rare tumor that accounts for less than 0.1% of all primary prostatic malignancies. This neoplasm is composed of highly aggressive prostatic smooth muscle cells that presents with nonspecific signs and symptoms mimicking other forms of prostatic pathology.
Case Report: A 72-year-old male presented with 6 months of progressive severe lower urinary tract symptoms (LUTS) secondary to bladder outlet obstruction. The patient was refractory to medical management and required multiple emergent bladder catheterizations. Workup with urinalysis, blood biochemistry, and PSA levels were persistently normal. He denied hematuria, weight loss, or perineal pain. On rectal exam, a mass like induration was noted along the right upper lobe of the prostate.
The patient was referred for transurethral resection of the prostate (TURP) for suspected severe BPH. Histopathological examination demonstrated atypical cytology consistent with high-grade leiomyosarcoma. A PET scan revealed a 1.9 cm tumor with uptake of 12.6 SUV in the right posterior prostate.
Discussion: Fewer than 200 cases of prostatic leiomyosarcoma have been reported. Patients typically present between 41-78 years of age (mean age of 61 years) with signs and symptoms related to LUTS (89.4%) and perineal or rectal pain (25.6%). Constitutional symptoms, burning on ejaculation, and hematuria are uncommon. PSA levels remain normal, due to its non-epithelial etiology, which may contribute to delays in diagnosis.
Diagnosis is usually achieved after a TURP procedure or transrectal needle biopsy. Pathology demonstrates neoplastic spindle cells with nuclear atypia, multifocal necrosis, and cystic degeneration. Immunohistochemistry is characteristically positive for desmin, smooth muscle actin, and vimentin. Tumors have been reported to range between 2-31 cm in size, frequently presenting with invasion of local structures. The lungs are the most common site of distant metastasis.
Treatment may include a multimodal approach of surgery, radiation, and chemotherapy. Long-term prognosis is poor due to the tumors aggressive nature, and recurrence is common. Median survival is estimated at 17 months and 50-75% of patients die within 2-5 years of diagnosis. Due to the substantially high risk of death, prostatic leiomyosarcoma may be one of the most aggressive and poorly prognostic malignancies involving the prostate.
Background: Prostatic leiomyosarcoma is a rare tumor that accounts for less than 0.1% of all primary prostatic malignancies. This neoplasm is composed of highly aggressive prostatic smooth muscle cells that presents with nonspecific signs and symptoms mimicking other forms of prostatic pathology.
Case Report: A 72-year-old male presented with 6 months of progressive severe lower urinary tract symptoms (LUTS) secondary to bladder outlet obstruction. The patient was refractory to medical management and required multiple emergent bladder catheterizations. Workup with urinalysis, blood biochemistry, and PSA levels were persistently normal. He denied hematuria, weight loss, or perineal pain. On rectal exam, a mass like induration was noted along the right upper lobe of the prostate.
The patient was referred for transurethral resection of the prostate (TURP) for suspected severe BPH. Histopathological examination demonstrated atypical cytology consistent with high-grade leiomyosarcoma. A PET scan revealed a 1.9 cm tumor with uptake of 12.6 SUV in the right posterior prostate.
Discussion: Fewer than 200 cases of prostatic leiomyosarcoma have been reported. Patients typically present between 41-78 years of age (mean age of 61 years) with signs and symptoms related to LUTS (89.4%) and perineal or rectal pain (25.6%). Constitutional symptoms, burning on ejaculation, and hematuria are uncommon. PSA levels remain normal, due to its non-epithelial etiology, which may contribute to delays in diagnosis.
Diagnosis is usually achieved after a TURP procedure or transrectal needle biopsy. Pathology demonstrates neoplastic spindle cells with nuclear atypia, multifocal necrosis, and cystic degeneration. Immunohistochemistry is characteristically positive for desmin, smooth muscle actin, and vimentin. Tumors have been reported to range between 2-31 cm in size, frequently presenting with invasion of local structures. The lungs are the most common site of distant metastasis.
Treatment may include a multimodal approach of surgery, radiation, and chemotherapy. Long-term prognosis is poor due to the tumors aggressive nature, and recurrence is common. Median survival is estimated at 17 months and 50-75% of patients die within 2-5 years of diagnosis. Due to the substantially high risk of death, prostatic leiomyosarcoma may be one of the most aggressive and poorly prognostic malignancies involving the prostate.
Survival Rates of Black and White Veterans With Metastatic Castration-Resistant Prostate Cancer
Rationale: Understand the survival outcomes of black and white Veterans with metastatic castration-resistant prostate cancer (mCRPC).
Background: Black men have a higher incidence of prostate cancer and are more likely to be diagnosed at an earlier age, have a more aggressive disease at presentation and experience worse clinical outcome than white men. Evidence has shown that at diagnosis race is associated with disease progression, however, few studies have examined whether race is associated with survival in men once they reach an advanced stage of the disease. This study examines the survival outcomes among black and white men with mCRPC treated in the Veterans Health Administration (VHA).
Methods: Patient information from the Veterans Affairs (VA) Central Cancer Registry and the VA Corporate Data Warehouse was used to identify patients who were diagnosed with prostate cancer and later developed mCRPC, defined as: (1) Radiologic evidence of metastasis obtained from radiology reports using a natural language processing algorithm; (2) Evidence of rising prostate-specific antigen (PSA); and (3) Evidence of ongoing androgen deprivation consisting of a serum testosterone level of 50 ng/dL. Patient demographics, disease characteristics and treatment practices, and survival outcomes were extracted.
Results: From 2006 to 2015, 120,374 patients were diagnosed and treated with prostate cancer in the VHA; with 3,637 developing mCRPC. At diagnosis 2,429 (67%) were white, 1,066 (29%) were black, and 142 (4%) were reported as other. Compared to white men, black men were younger (66 vs 69 years) and had a higher PSA (92 vs 41 ng/mL), although there were no differences in disease characteristics
(Gleason score and stage) and early treatments (radiation prostatectomy, surgical orchiectomy, castration by agonists, castration by agonists/androgen deprivation). There were no significant differences between black and white men with mCRPC and their overall survival on both univariable (HR, .95; P = .203) or multivariable (HR, 1.0; P = .971) analyses.
Conclusions: Consistent with prior reports, black men are more likely to develop mCRPC than white men, although once black men progress to advanced disease, a multivariable analysis suggests that race is not associated with overall survival.
Rationale: Understand the survival outcomes of black and white Veterans with metastatic castration-resistant prostate cancer (mCRPC).
Background: Black men have a higher incidence of prostate cancer and are more likely to be diagnosed at an earlier age, have a more aggressive disease at presentation and experience worse clinical outcome than white men. Evidence has shown that at diagnosis race is associated with disease progression, however, few studies have examined whether race is associated with survival in men once they reach an advanced stage of the disease. This study examines the survival outcomes among black and white men with mCRPC treated in the Veterans Health Administration (VHA).
Methods: Patient information from the Veterans Affairs (VA) Central Cancer Registry and the VA Corporate Data Warehouse was used to identify patients who were diagnosed with prostate cancer and later developed mCRPC, defined as: (1) Radiologic evidence of metastasis obtained from radiology reports using a natural language processing algorithm; (2) Evidence of rising prostate-specific antigen (PSA); and (3) Evidence of ongoing androgen deprivation consisting of a serum testosterone level of 50 ng/dL. Patient demographics, disease characteristics and treatment practices, and survival outcomes were extracted.
Results: From 2006 to 2015, 120,374 patients were diagnosed and treated with prostate cancer in the VHA; with 3,637 developing mCRPC. At diagnosis 2,429 (67%) were white, 1,066 (29%) were black, and 142 (4%) were reported as other. Compared to white men, black men were younger (66 vs 69 years) and had a higher PSA (92 vs 41 ng/mL), although there were no differences in disease characteristics
(Gleason score and stage) and early treatments (radiation prostatectomy, surgical orchiectomy, castration by agonists, castration by agonists/androgen deprivation). There were no significant differences between black and white men with mCRPC and their overall survival on both univariable (HR, .95; P = .203) or multivariable (HR, 1.0; P = .971) analyses.
Conclusions: Consistent with prior reports, black men are more likely to develop mCRPC than white men, although once black men progress to advanced disease, a multivariable analysis suggests that race is not associated with overall survival.
Rationale: Understand the survival outcomes of black and white Veterans with metastatic castration-resistant prostate cancer (mCRPC).
Background: Black men have a higher incidence of prostate cancer and are more likely to be diagnosed at an earlier age, have a more aggressive disease at presentation and experience worse clinical outcome than white men. Evidence has shown that at diagnosis race is associated with disease progression, however, few studies have examined whether race is associated with survival in men once they reach an advanced stage of the disease. This study examines the survival outcomes among black and white men with mCRPC treated in the Veterans Health Administration (VHA).
Methods: Patient information from the Veterans Affairs (VA) Central Cancer Registry and the VA Corporate Data Warehouse was used to identify patients who were diagnosed with prostate cancer and later developed mCRPC, defined as: (1) Radiologic evidence of metastasis obtained from radiology reports using a natural language processing algorithm; (2) Evidence of rising prostate-specific antigen (PSA); and (3) Evidence of ongoing androgen deprivation consisting of a serum testosterone level of 50 ng/dL. Patient demographics, disease characteristics and treatment practices, and survival outcomes were extracted.
Results: From 2006 to 2015, 120,374 patients were diagnosed and treated with prostate cancer in the VHA; with 3,637 developing mCRPC. At diagnosis 2,429 (67%) were white, 1,066 (29%) were black, and 142 (4%) were reported as other. Compared to white men, black men were younger (66 vs 69 years) and had a higher PSA (92 vs 41 ng/mL), although there were no differences in disease characteristics
(Gleason score and stage) and early treatments (radiation prostatectomy, surgical orchiectomy, castration by agonists, castration by agonists/androgen deprivation). There were no significant differences between black and white men with mCRPC and their overall survival on both univariable (HR, .95; P = .203) or multivariable (HR, 1.0; P = .971) analyses.
Conclusions: Consistent with prior reports, black men are more likely to develop mCRPC than white men, although once black men progress to advanced disease, a multivariable analysis suggests that race is not associated with overall survival.
Association of Prostate-Specific Antigen (PSA) Trajectories With Mortality in Veterans With Non-Metastatic Castration-Resistant Prostate Cancer (nmCRPC)
Background: There are nearly 40,000 patients with nmCRPC in the US. This study aims to describe the characteristics of Veterans with nmCRPC and assess the impact of PSA trajectory, baseline PSA and development of metastases on OS.
Methods: Veterans Health Administration electronic health record data (01/2007-08/2017) were used to conduct a retrospective longitudinal study in Veterans with nmCRPC. Patients with castrate testosterone levels ( < 50 ng/dL) or continuous androgen deprivation therapy, a 25% rise in PSA from nadir and absolute increase of 2 ng/mL (index), and a PC diagnosis 12 months before index were selected. Patients were excluded if they had < 12 months of enrollment before or < 6 months after the index date, evidence of metastatic disease 12 months before index (defined based on diagnoses for metastatic disease, use of chemotherapy, immunotherapy, radiopharmaceuticals, or oral mCRPC therapy), or evidence of participation in a clinical trial (defined based on diagnosis codes or prescription for experimental therapies). PSA was measured in the 12 months before index, at index, and 6 months after index. Patients with similar PSA trajectories (PSA patterns over time) were grouped using group-based trajectory analysis (GBTA). OS was assessed with a Cox proportional hazards model adjusted for baseline characteristics, PSA trajectory group, and a timevarying indicator for metastases.
Results: 13,552 Veterans formed the study population. Mean (SD) age was 76.4 (9.4) years and most were white (66%). During follow up (mean [SD]=36 [26] months) there were 6,552 (48%) deaths; median OS was 47 months. GBTA resulted in 4 PSA trajectory groups. The Cox model showed that PSA trajectory group was a strong predictor of OS; compared to Group 1 (n = 213), patients in the other groups were more likely to die (Group 2 [n = 6,558]: HR=1.602, P < .001; Group 3 [n = 5,323]: HR = 1.716, P < .001; Group 4 [n = 1,458]: HR = 2.005, P < .001). Higher log PSA at baseline increased risk of death (HR = 1.092, P < .001). Moreover, compared to patients without metastases, patients who eventually developed metastases were more likely to die (HR: 3.661, P < .001).
Conclusions: In this study of Veterans with nmCRPC, higher baseline PSA, PSA trajectory group, and development of metastases were associated with increased risk of death.
Background: There are nearly 40,000 patients with nmCRPC in the US. This study aims to describe the characteristics of Veterans with nmCRPC and assess the impact of PSA trajectory, baseline PSA and development of metastases on OS.
Methods: Veterans Health Administration electronic health record data (01/2007-08/2017) were used to conduct a retrospective longitudinal study in Veterans with nmCRPC. Patients with castrate testosterone levels ( < 50 ng/dL) or continuous androgen deprivation therapy, a 25% rise in PSA from nadir and absolute increase of 2 ng/mL (index), and a PC diagnosis 12 months before index were selected. Patients were excluded if they had < 12 months of enrollment before or < 6 months after the index date, evidence of metastatic disease 12 months before index (defined based on diagnoses for metastatic disease, use of chemotherapy, immunotherapy, radiopharmaceuticals, or oral mCRPC therapy), or evidence of participation in a clinical trial (defined based on diagnosis codes or prescription for experimental therapies). PSA was measured in the 12 months before index, at index, and 6 months after index. Patients with similar PSA trajectories (PSA patterns over time) were grouped using group-based trajectory analysis (GBTA). OS was assessed with a Cox proportional hazards model adjusted for baseline characteristics, PSA trajectory group, and a timevarying indicator for metastases.
Results: 13,552 Veterans formed the study population. Mean (SD) age was 76.4 (9.4) years and most were white (66%). During follow up (mean [SD]=36 [26] months) there were 6,552 (48%) deaths; median OS was 47 months. GBTA resulted in 4 PSA trajectory groups. The Cox model showed that PSA trajectory group was a strong predictor of OS; compared to Group 1 (n = 213), patients in the other groups were more likely to die (Group 2 [n = 6,558]: HR=1.602, P < .001; Group 3 [n = 5,323]: HR = 1.716, P < .001; Group 4 [n = 1,458]: HR = 2.005, P < .001). Higher log PSA at baseline increased risk of death (HR = 1.092, P < .001). Moreover, compared to patients without metastases, patients who eventually developed metastases were more likely to die (HR: 3.661, P < .001).
Conclusions: In this study of Veterans with nmCRPC, higher baseline PSA, PSA trajectory group, and development of metastases were associated with increased risk of death.
Background: There are nearly 40,000 patients with nmCRPC in the US. This study aims to describe the characteristics of Veterans with nmCRPC and assess the impact of PSA trajectory, baseline PSA and development of metastases on OS.
Methods: Veterans Health Administration electronic health record data (01/2007-08/2017) were used to conduct a retrospective longitudinal study in Veterans with nmCRPC. Patients with castrate testosterone levels ( < 50 ng/dL) or continuous androgen deprivation therapy, a 25% rise in PSA from nadir and absolute increase of 2 ng/mL (index), and a PC diagnosis 12 months before index were selected. Patients were excluded if they had < 12 months of enrollment before or < 6 months after the index date, evidence of metastatic disease 12 months before index (defined based on diagnoses for metastatic disease, use of chemotherapy, immunotherapy, radiopharmaceuticals, or oral mCRPC therapy), or evidence of participation in a clinical trial (defined based on diagnosis codes or prescription for experimental therapies). PSA was measured in the 12 months before index, at index, and 6 months after index. Patients with similar PSA trajectories (PSA patterns over time) were grouped using group-based trajectory analysis (GBTA). OS was assessed with a Cox proportional hazards model adjusted for baseline characteristics, PSA trajectory group, and a timevarying indicator for metastases.
Results: 13,552 Veterans formed the study population. Mean (SD) age was 76.4 (9.4) years and most were white (66%). During follow up (mean [SD]=36 [26] months) there were 6,552 (48%) deaths; median OS was 47 months. GBTA resulted in 4 PSA trajectory groups. The Cox model showed that PSA trajectory group was a strong predictor of OS; compared to Group 1 (n = 213), patients in the other groups were more likely to die (Group 2 [n = 6,558]: HR=1.602, P < .001; Group 3 [n = 5,323]: HR = 1.716, P < .001; Group 4 [n = 1,458]: HR = 2.005, P < .001). Higher log PSA at baseline increased risk of death (HR = 1.092, P < .001). Moreover, compared to patients without metastases, patients who eventually developed metastases were more likely to die (HR: 3.661, P < .001).
Conclusions: In this study of Veterans with nmCRPC, higher baseline PSA, PSA trajectory group, and development of metastases were associated with increased risk of death.
Efficacy of Enzalutamide and Abiraterone Sequences in Metastatic Castration-Resistant Prostate Cancer
Purpose: To determine which sequence of abiraterone (ABI) and enzalutamide (ENZA) shows better survival outcomes in Veterans diagnosed with metastatic castration-resistant prostate cancer (mCRPC) at VA San Diego.
Background: Prostate cancer is the leading cancer diagnosis among American men who eventually develop mCRPC. Therapies for mCRPC include androgen receptor pathway inhibitors like ABI and ENZA. Both improve survival independently; however, the optimal treatment sequence has not been determined. Retrospective studies have shown that the ABI-ENZA sequence significantly improves progression-free survival (PFS) and combined prostate-specific antigen PFS (cPSA-PFS), but not overall survival (OS).
Methods: A retrospective chart review was conducted in subjects with mCRPC who had received ABI and ENZA sequentially in either order. Subjects must have received at least one month of each drug; those who had an interruption of treatment sequence were excluded. The primary outcomes were to compare cPSA-PFS and OS between the two sequences; cPSA-PFS represented time from start of drug 1 to > 25% PSA increase from baseline/nadir on drug 2, while OS represented time from start of drug 1 to death from any cause. OS and cPSA-PFS were reported via Kaplan-
Meier curves and hazard ratios (HR). Ninety-eight subjects per group were needed to reach 80% power for an effect size of 0.404 in cPSA-PFS.
Results: Forty subjects were identified and 8 were excluded; of the remaining, 9 received ENZA-ABI and 23 received ABIENZA. Baseline characteristics were similar. There were no differences in cPSA-PFS between ENZA-ABI and ABI-ENZA: median 406 days versus 534 days (HR 1.39, 95% CI 0.59-1.53, P = .59), respectively. OS did not differ between ENZAABI and ABI-ENZA: median 711 days versus 803 days (HR 0.88, 95% CI 0.35-1.59, P = .21), respectively.
Conclusions: There were no significant differences in outcomes between sequences although ABI-ENZA showed longer cPSA-PFS and OS. This is consistent with previous studies where ABI-ENZA had significantly longer PFS and cPSA-PFS; ABI-ENZA OS was longer but not significantly different in those studies. Limitations included a small sample size and uneven groups. Ultimately, ABI-ENZA should be considered as the sequence-of-choice for treatment of mCRPC until prospective studies confirm the optimal sequence.
Purpose: To determine which sequence of abiraterone (ABI) and enzalutamide (ENZA) shows better survival outcomes in Veterans diagnosed with metastatic castration-resistant prostate cancer (mCRPC) at VA San Diego.
Background: Prostate cancer is the leading cancer diagnosis among American men who eventually develop mCRPC. Therapies for mCRPC include androgen receptor pathway inhibitors like ABI and ENZA. Both improve survival independently; however, the optimal treatment sequence has not been determined. Retrospective studies have shown that the ABI-ENZA sequence significantly improves progression-free survival (PFS) and combined prostate-specific antigen PFS (cPSA-PFS), but not overall survival (OS).
Methods: A retrospective chart review was conducted in subjects with mCRPC who had received ABI and ENZA sequentially in either order. Subjects must have received at least one month of each drug; those who had an interruption of treatment sequence were excluded. The primary outcomes were to compare cPSA-PFS and OS between the two sequences; cPSA-PFS represented time from start of drug 1 to > 25% PSA increase from baseline/nadir on drug 2, while OS represented time from start of drug 1 to death from any cause. OS and cPSA-PFS were reported via Kaplan-
Meier curves and hazard ratios (HR). Ninety-eight subjects per group were needed to reach 80% power for an effect size of 0.404 in cPSA-PFS.
Results: Forty subjects were identified and 8 were excluded; of the remaining, 9 received ENZA-ABI and 23 received ABIENZA. Baseline characteristics were similar. There were no differences in cPSA-PFS between ENZA-ABI and ABI-ENZA: median 406 days versus 534 days (HR 1.39, 95% CI 0.59-1.53, P = .59), respectively. OS did not differ between ENZAABI and ABI-ENZA: median 711 days versus 803 days (HR 0.88, 95% CI 0.35-1.59, P = .21), respectively.
Conclusions: There were no significant differences in outcomes between sequences although ABI-ENZA showed longer cPSA-PFS and OS. This is consistent with previous studies where ABI-ENZA had significantly longer PFS and cPSA-PFS; ABI-ENZA OS was longer but not significantly different in those studies. Limitations included a small sample size and uneven groups. Ultimately, ABI-ENZA should be considered as the sequence-of-choice for treatment of mCRPC until prospective studies confirm the optimal sequence.
Purpose: To determine which sequence of abiraterone (ABI) and enzalutamide (ENZA) shows better survival outcomes in Veterans diagnosed with metastatic castration-resistant prostate cancer (mCRPC) at VA San Diego.
Background: Prostate cancer is the leading cancer diagnosis among American men who eventually develop mCRPC. Therapies for mCRPC include androgen receptor pathway inhibitors like ABI and ENZA. Both improve survival independently; however, the optimal treatment sequence has not been determined. Retrospective studies have shown that the ABI-ENZA sequence significantly improves progression-free survival (PFS) and combined prostate-specific antigen PFS (cPSA-PFS), but not overall survival (OS).
Methods: A retrospective chart review was conducted in subjects with mCRPC who had received ABI and ENZA sequentially in either order. Subjects must have received at least one month of each drug; those who had an interruption of treatment sequence were excluded. The primary outcomes were to compare cPSA-PFS and OS between the two sequences; cPSA-PFS represented time from start of drug 1 to > 25% PSA increase from baseline/nadir on drug 2, while OS represented time from start of drug 1 to death from any cause. OS and cPSA-PFS were reported via Kaplan-
Meier curves and hazard ratios (HR). Ninety-eight subjects per group were needed to reach 80% power for an effect size of 0.404 in cPSA-PFS.
Results: Forty subjects were identified and 8 were excluded; of the remaining, 9 received ENZA-ABI and 23 received ABIENZA. Baseline characteristics were similar. There were no differences in cPSA-PFS between ENZA-ABI and ABI-ENZA: median 406 days versus 534 days (HR 1.39, 95% CI 0.59-1.53, P = .59), respectively. OS did not differ between ENZAABI and ABI-ENZA: median 711 days versus 803 days (HR 0.88, 95% CI 0.35-1.59, P = .21), respectively.
Conclusions: There were no significant differences in outcomes between sequences although ABI-ENZA showed longer cPSA-PFS and OS. This is consistent with previous studies where ABI-ENZA had significantly longer PFS and cPSA-PFS; ABI-ENZA OS was longer but not significantly different in those studies. Limitations included a small sample size and uneven groups. Ultimately, ABI-ENZA should be considered as the sequence-of-choice for treatment of mCRPC until prospective studies confirm the optimal sequence.
Implementation of Dietary Education Within a Multidisciplinary Team Approach to Improve Treatment Accuracy and Efficiency in Prostate Cancer External Beam Radiation Therapy
Background: Prostate cancer is the most common cancer in the Veterans Health Administration. Radiation is an important treatment option for prostate cancer patients. Imaging is done before each daily radiation treatment to ensure the radiation beam is aimed accurately. Imaging can be inaccurate due to excess gas or stool in the rectum, which alters the treatment field and leads to delays in the daily treatment schedule, increased radiation exposure due to re-imaging, repetitive staff treatment delivery interventions, and an unsatisfactory veteran experience.
Methods: A quality improvement project utilizing A3.9 box process improvement methodology (problem solving template) was undertaken to address identified gastrointestinal concerns hindering daily treatment. A dietitian integrated services into the radiation oncology clinic by providing dietary education and counseling to avoid gasproducing foods and manage bowel regularity for prostate cancer patients. Daily images were reviewed for accuracy. For 3 months prior to intervention, we examined daily treatment images and documented any interruption in treatment delivery from gas or stool in the rectum as a nutrition-related defect. Initial data analysis revealed that 62 of 195 (31.79%) daily treatment deliveries experienced nutrition-related defects.
Results: As a result of changing the radiation therapy process to include dietary education to patients, we experienced a 53% reduction rate in nutrition-related defects (from 31.79% to 14.87%). Calculated cost avoidance showed an annual savings of approximately $19,300 with
implementation of a multidisciplinary approach. A total of 120 daily treatment visits and 90 patient treatment hours can be saved annually with this approach.
Conclusions: This project improved overall clinic function by implementing a multidisciplinary approach to prostate cancer radiation oncology care, increased patient’s satisfaction, reduced excess radiation exposure, and improved department efficiency.
Background: Prostate cancer is the most common cancer in the Veterans Health Administration. Radiation is an important treatment option for prostate cancer patients. Imaging is done before each daily radiation treatment to ensure the radiation beam is aimed accurately. Imaging can be inaccurate due to excess gas or stool in the rectum, which alters the treatment field and leads to delays in the daily treatment schedule, increased radiation exposure due to re-imaging, repetitive staff treatment delivery interventions, and an unsatisfactory veteran experience.
Methods: A quality improvement project utilizing A3.9 box process improvement methodology (problem solving template) was undertaken to address identified gastrointestinal concerns hindering daily treatment. A dietitian integrated services into the radiation oncology clinic by providing dietary education and counseling to avoid gasproducing foods and manage bowel regularity for prostate cancer patients. Daily images were reviewed for accuracy. For 3 months prior to intervention, we examined daily treatment images and documented any interruption in treatment delivery from gas or stool in the rectum as a nutrition-related defect. Initial data analysis revealed that 62 of 195 (31.79%) daily treatment deliveries experienced nutrition-related defects.
Results: As a result of changing the radiation therapy process to include dietary education to patients, we experienced a 53% reduction rate in nutrition-related defects (from 31.79% to 14.87%). Calculated cost avoidance showed an annual savings of approximately $19,300 with
implementation of a multidisciplinary approach. A total of 120 daily treatment visits and 90 patient treatment hours can be saved annually with this approach.
Conclusions: This project improved overall clinic function by implementing a multidisciplinary approach to prostate cancer radiation oncology care, increased patient’s satisfaction, reduced excess radiation exposure, and improved department efficiency.
Background: Prostate cancer is the most common cancer in the Veterans Health Administration. Radiation is an important treatment option for prostate cancer patients. Imaging is done before each daily radiation treatment to ensure the radiation beam is aimed accurately. Imaging can be inaccurate due to excess gas or stool in the rectum, which alters the treatment field and leads to delays in the daily treatment schedule, increased radiation exposure due to re-imaging, repetitive staff treatment delivery interventions, and an unsatisfactory veteran experience.
Methods: A quality improvement project utilizing A3.9 box process improvement methodology (problem solving template) was undertaken to address identified gastrointestinal concerns hindering daily treatment. A dietitian integrated services into the radiation oncology clinic by providing dietary education and counseling to avoid gasproducing foods and manage bowel regularity for prostate cancer patients. Daily images were reviewed for accuracy. For 3 months prior to intervention, we examined daily treatment images and documented any interruption in treatment delivery from gas or stool in the rectum as a nutrition-related defect. Initial data analysis revealed that 62 of 195 (31.79%) daily treatment deliveries experienced nutrition-related defects.
Results: As a result of changing the radiation therapy process to include dietary education to patients, we experienced a 53% reduction rate in nutrition-related defects (from 31.79% to 14.87%). Calculated cost avoidance showed an annual savings of approximately $19,300 with
implementation of a multidisciplinary approach. A total of 120 daily treatment visits and 90 patient treatment hours can be saved annually with this approach.
Conclusions: This project improved overall clinic function by implementing a multidisciplinary approach to prostate cancer radiation oncology care, increased patient’s satisfaction, reduced excess radiation exposure, and improved department efficiency.
Improving Prostate Cancer Education Among Veterans at the Palo Alto VA
Purpose: This project was created to improve prostate cancer education at VA Palo Alto Health Care System (VAPAHCS) and to explore Veterans’ knowledge about their diagnosis and its treatment. Prostate cancer is the most commonly diagnosed form of cancer in the VA and makes up one-third of all cancer cases in Veterans. Clinical experiences in our outpatient Urology-Oncology clinic suggested that Veterans may benefit from additional information about tumor stages, risk factors, and treatment options. Thus, a quality improvement project was conducted in order to measure baseline knowledge.
Methods: Veterans diagnosed with prostate cancer completed a survey to determine baseline knowledge. Surveys were conducted by a psychology trainee or social worker during regularly scheduled Urology-Oncology appointments. After completing the survey, Veterans were provided with written educational materials and had the option of watching a brief educational video on a tablet in their exam room.
Data Analysis: Descriptive statistics were used to analyze demographic information and to determine Veteran’s baseline levels of knowledge.
Results: 26 Veterans completed the survey between March and June 2018. 25 participants identified as male; one as a transgender female. Average age was 74 years, with a range from 63-88 years. 65% identified as white, 12% as black or African American, 12% Hispanic, and 11% unknown. Average time since diagnosis was 7.3 years, with a range from 0-21 years. 92% of Veterans knew what type of cancer they were diagnosed with, 62% were familiar with the different stages of prostate cancer, 54% were familiar with the risk factors for developing prostate cancer, 77% knew what their treatment options were, and 88% felt comfortable asking their doctor questions about their cancer and its treatment.
Implications: These results indicate that Veterans are well informed about the type of cancer they have been diagnosed with and are comfortable communicating with their doctor, but are less familiar with tumor stages, risk factors, and treatment options. This suggests that additional resources for prostate cancer education are warranted in our clinics. Future directions include the
development of additional educational programs within the VAPAHCS and incorporating assessment of Veteran knowledge during clinic visits.
Purpose: This project was created to improve prostate cancer education at VA Palo Alto Health Care System (VAPAHCS) and to explore Veterans’ knowledge about their diagnosis and its treatment. Prostate cancer is the most commonly diagnosed form of cancer in the VA and makes up one-third of all cancer cases in Veterans. Clinical experiences in our outpatient Urology-Oncology clinic suggested that Veterans may benefit from additional information about tumor stages, risk factors, and treatment options. Thus, a quality improvement project was conducted in order to measure baseline knowledge.
Methods: Veterans diagnosed with prostate cancer completed a survey to determine baseline knowledge. Surveys were conducted by a psychology trainee or social worker during regularly scheduled Urology-Oncology appointments. After completing the survey, Veterans were provided with written educational materials and had the option of watching a brief educational video on a tablet in their exam room.
Data Analysis: Descriptive statistics were used to analyze demographic information and to determine Veteran’s baseline levels of knowledge.
Results: 26 Veterans completed the survey between March and June 2018. 25 participants identified as male; one as a transgender female. Average age was 74 years, with a range from 63-88 years. 65% identified as white, 12% as black or African American, 12% Hispanic, and 11% unknown. Average time since diagnosis was 7.3 years, with a range from 0-21 years. 92% of Veterans knew what type of cancer they were diagnosed with, 62% were familiar with the different stages of prostate cancer, 54% were familiar with the risk factors for developing prostate cancer, 77% knew what their treatment options were, and 88% felt comfortable asking their doctor questions about their cancer and its treatment.
Implications: These results indicate that Veterans are well informed about the type of cancer they have been diagnosed with and are comfortable communicating with their doctor, but are less familiar with tumor stages, risk factors, and treatment options. This suggests that additional resources for prostate cancer education are warranted in our clinics. Future directions include the
development of additional educational programs within the VAPAHCS and incorporating assessment of Veteran knowledge during clinic visits.
Purpose: This project was created to improve prostate cancer education at VA Palo Alto Health Care System (VAPAHCS) and to explore Veterans’ knowledge about their diagnosis and its treatment. Prostate cancer is the most commonly diagnosed form of cancer in the VA and makes up one-third of all cancer cases in Veterans. Clinical experiences in our outpatient Urology-Oncology clinic suggested that Veterans may benefit from additional information about tumor stages, risk factors, and treatment options. Thus, a quality improvement project was conducted in order to measure baseline knowledge.
Methods: Veterans diagnosed with prostate cancer completed a survey to determine baseline knowledge. Surveys were conducted by a psychology trainee or social worker during regularly scheduled Urology-Oncology appointments. After completing the survey, Veterans were provided with written educational materials and had the option of watching a brief educational video on a tablet in their exam room.
Data Analysis: Descriptive statistics were used to analyze demographic information and to determine Veteran’s baseline levels of knowledge.
Results: 26 Veterans completed the survey between March and June 2018. 25 participants identified as male; one as a transgender female. Average age was 74 years, with a range from 63-88 years. 65% identified as white, 12% as black or African American, 12% Hispanic, and 11% unknown. Average time since diagnosis was 7.3 years, with a range from 0-21 years. 92% of Veterans knew what type of cancer they were diagnosed with, 62% were familiar with the different stages of prostate cancer, 54% were familiar with the risk factors for developing prostate cancer, 77% knew what their treatment options were, and 88% felt comfortable asking their doctor questions about their cancer and its treatment.
Implications: These results indicate that Veterans are well informed about the type of cancer they have been diagnosed with and are comfortable communicating with their doctor, but are less familiar with tumor stages, risk factors, and treatment options. This suggests that additional resources for prostate cancer education are warranted in our clinics. Future directions include the
development of additional educational programs within the VAPAHCS and incorporating assessment of Veteran knowledge during clinic visits.