User login
Lessons from Seattle: Prepping a critical care system for COVID-19
What can the nation’s critical care systems do to prepare for the worst of the COVID-19 pandemic?
Mark Tonelli, MD, is professor of medicine and section head of the University of Washington Medical Center’s division of pulmonary, critical care, and sleep medicine. In an audio interview, Dr. Tonelli outlines exactly how the University of Washington and the region’s other health systems are readying their critical care departments for the demands of the COVID-19 pandemic. And he offers advice from the front lines for health systems nationwide as they prep their own critical care systems.
To listen to the interview, click the play button below.
What can the nation’s critical care systems do to prepare for the worst of the COVID-19 pandemic?
Mark Tonelli, MD, is professor of medicine and section head of the University of Washington Medical Center’s division of pulmonary, critical care, and sleep medicine. In an audio interview, Dr. Tonelli outlines exactly how the University of Washington and the region’s other health systems are readying their critical care departments for the demands of the COVID-19 pandemic. And he offers advice from the front lines for health systems nationwide as they prep their own critical care systems.
To listen to the interview, click the play button below.
What can the nation’s critical care systems do to prepare for the worst of the COVID-19 pandemic?
Mark Tonelli, MD, is professor of medicine and section head of the University of Washington Medical Center’s division of pulmonary, critical care, and sleep medicine. In an audio interview, Dr. Tonelli outlines exactly how the University of Washington and the region’s other health systems are readying their critical care departments for the demands of the COVID-19 pandemic. And he offers advice from the front lines for health systems nationwide as they prep their own critical care systems.
To listen to the interview, click the play button below.
Hospitals muzzle doctors and nurses on PPE, COVID-19 cases
Over the past month, an orthopedic surgeon has watched as the crowd of sick patients at his hospital has grown, while the supply of personal protective equipment (PPE) for staff has diminished. As he prepares for another day of staffing testing tents and places his one and only mask across his face, he also receives a daily reminder from hospital management: Don’t talk about it.
The surgeon, who works in a COVID-19 hot spot in the Northeast, spoke on the condition of anonymity for fear of employer retribution.
“It’s very clear; no one is allowed to speak for the institution or of the institution,” he said in an interview. “We get a daily warning about being very prudent about posts on personal accounts. They’ve talked about this with respect to various issues: case numbers, case severity, testing availability, [and] PPEs.”
The warnings mean staff at the hospital suffer in silence, unable to share the troubling situation with the public or request assistance with supplies.
“I have one mask. We’re expected to reuse them, unless you were exposed or worked with a known COVID victim,” the surgeon said. “However, with the numbers in our region rapidly increasing, you can’t assume that people don’t have it or that you don’t have particles on your mask, even if you’re not in a known quarantine zone within the institution.”
As the COVID-19 health crisis rages on, online platforms have become a common place for health professionals to lament short supplies, share concerns, tell stories, and plead for help. But at the same time, other physicians, nurses, and health care workers are being muzzled by hospital administrators and threatened with discipline for speaking out about coronavirus caseloads and dwindling supplies. Some worry the gag orders are muddying the picture of how hospitals are faring in the pandemic, while placing the safety of frontline workers at risk.
The silencing of physicians by hospitals about PPE shortages and other COVID-19 issues has become widespread, said Nisha Mehta, MD, a physician advocate and community leader who writes about PPE on social media. Physicians are being warned not to speak or post publicly about their COVID-19 experiences, including PPE shortages, case specifics, and the percentage of full hospital beds, Dr. Mehta said in an interview. In some cases, physicians who have posted have been forced to take down the posts or have faced retribution for speaking out, she said.
“There’s definitely a big fear among physicians, particularly employed physicians, in terms of what the consequences may be for telling their stories,” Dr. Mehta said. “I find that counterproductive. I understand not inducing panic, but these are real stories that are important for people to understand so they do stay home and increase the systemic pressure to get sufficient PPE, so that we can preserve our health care workforce for a problem that is going to get worse before it gets better.”
Meanwhile, an Indiana hospitalist who took to social media to ask for masks for hospitals in his area says he was immediately reprimanded by his management after the posts came to light. The hospitalist posted on a social media platform to request donations of N95 masks after hearing members of the public had purchased such masks. He hoped his plea would aid preparation for the pandemic at local hospitals, explained the physician, who spoke on the condition of anonymity.
Shortly afterward, administrators from his hospital contacted the online forum’s moderator and the posts were removed, he said. During a subsequent conversation, administrators warned the doctor not to make such posts about PPE because it made the hospital appear incompetent.
“I was told, ‘we can handle this, we don’t need the public’s help,’” the physician said. “I was hurt and upset. I was trying to help protect my peers.”
After landing on the management’s radar, the hospitalist said he was reprimanded a second time about posts on a separate personal social media account. The second time, the private posts to friends and family were related to COVID-19 and PPE, but did not include any protected health information, he said. However, administrators did not like the content of the posts, and he was told management was monitoring his activity on social media, he said.
“The larger message is that patients are money,” the hospitalist said. “The corporate side of medicine rules out over the medicine side. Image and making sure there is a consistent cash flow trumps all else.”
Another frontline physician who works at a large New York hospital, said staff have been cautioned not to talk with the media and to be careful what they post on social media regarding COVID-19. The general rule is that only information approved by administrators can be shared, said the physician, who spoke on the condition of anonymity.
“[The health system] is very protective of their public image,” he said. “In the past, people that have posted things that they don’t like get spoken to quickly and/or fired depending on what was written. I could only imagine that would be the situation regarding COVID-19. They are very strict.”
The frontline physician, who has close contact with COVID-19 patients, said he has access to N95 masks at the moment, but when he requested higher-level protective gear, hospital management refused the request and denied that such supplies were needed.
“Safety of frontline workers appears to not be taken seriously,” he said of his hospital. “Everyone is stressed, but at the end of the day, the administration is sitting there, while the rest of us are putting ourselves at risk.”
We reached out to one hospital for comment, but messages were not returned. Other hospitals were not contacted because physicians feared they would face retribution. We also contacted the American Hospital Association but they did not immediately respond.
In Chicago, an email by a nurse to her coworkers about the safety of masks has resulted in a lawsuit after the nurse says she was fired for sharing her concerns with staff. The nurse, Lauri Mazurkiewicz, sent an email to staffers at Northwestern Memorial Hospital stating the surgical masks provided by the hospital were less effective against airborne particles than were N95 masks, according to a lawsuit filed March 23 in Cook County Circuit Court. Ms. Mazurkiewicz was terminated the next day in retaliation for her email, the lawsuit alleges.
Ms. Mazurkiewicz could not be reached for comment by press time.
Christopher King, a spokesman for Northwestern Medicine, said the hospital is reviewing the lawsuit.
“As Northwestern Medicine continues to respond to this unprecedented health care pandemic, the health and well-being of our patients, our staff and our employees is our highest priority,” he said in a statement. “We take these matters seriously and we are currently reviewing the complaint. At this time, we will not be commenting further.”
John Mandrola, MD, a Louisville, Ky.–based cardiologist who has written about the recent muzzling of frontline physicians with respect to the coronavirus, said he is not surprised that some hospitals are preventing physicians from sharing their experiences.
“Before C19, in many hospital systems, there was a culture of fear amongst employed clinicians,” he said. “Employed clinicians see other employed physicians being terminated for speaking frankly about problems. It takes scant few of these cases to create a culture of silence.”
Dr. Mandrola, who is a regular Medscape contributor, said that a number of doctors have reached out to him privately about PPE scarcity and shared that they were explicitly warned by administrators not to talk about the shortfalls. Leadership at Dr. Mandrola’s hospital has not issued the same warnings, he said.
“From the hat of total transparency, I think the public is not getting a full view of the impending potential problems that are going to come by doctors not speaking publicly,” he said. “On the other hand, hospital leadership is doing the best they can. It’s not the hospitals’ fault. Hospital administrators can’t manufacture masks.”
From a public health standpoint, Dr. Mehta said that not allowing health professionals to speak publicly about the situations at their hospitals is “irresponsible.” The public deserves to know what is happening, she said, and the health care workforce needs to prepare for what is to come.
“It’s so important that we hear from our colleagues,” she said. “It’s important to hear those accounts so we can prepare for what we’re about to face. Data is crucial. The more you learn from each other, the better shot we have at successfully treating cases and ultimately beating this.”
With the critical shortage of PPE at his hospital and the inability to speak out about the problem, the orthopedic surgeon foresees the dilemma continuing to worsen.
“It’s not only the lives of front-line health care workers that are at risk, but it’s those that they’re going to spread it to and those that are going to be coming to the hospital requiring our care,” he said. “If we don’t have a fully functioning health care force, our capacity is going to be diminished that much further.”
Over the past month, an orthopedic surgeon has watched as the crowd of sick patients at his hospital has grown, while the supply of personal protective equipment (PPE) for staff has diminished. As he prepares for another day of staffing testing tents and places his one and only mask across his face, he also receives a daily reminder from hospital management: Don’t talk about it.
The surgeon, who works in a COVID-19 hot spot in the Northeast, spoke on the condition of anonymity for fear of employer retribution.
“It’s very clear; no one is allowed to speak for the institution or of the institution,” he said in an interview. “We get a daily warning about being very prudent about posts on personal accounts. They’ve talked about this with respect to various issues: case numbers, case severity, testing availability, [and] PPEs.”
The warnings mean staff at the hospital suffer in silence, unable to share the troubling situation with the public or request assistance with supplies.
“I have one mask. We’re expected to reuse them, unless you were exposed or worked with a known COVID victim,” the surgeon said. “However, with the numbers in our region rapidly increasing, you can’t assume that people don’t have it or that you don’t have particles on your mask, even if you’re not in a known quarantine zone within the institution.”
As the COVID-19 health crisis rages on, online platforms have become a common place for health professionals to lament short supplies, share concerns, tell stories, and plead for help. But at the same time, other physicians, nurses, and health care workers are being muzzled by hospital administrators and threatened with discipline for speaking out about coronavirus caseloads and dwindling supplies. Some worry the gag orders are muddying the picture of how hospitals are faring in the pandemic, while placing the safety of frontline workers at risk.
The silencing of physicians by hospitals about PPE shortages and other COVID-19 issues has become widespread, said Nisha Mehta, MD, a physician advocate and community leader who writes about PPE on social media. Physicians are being warned not to speak or post publicly about their COVID-19 experiences, including PPE shortages, case specifics, and the percentage of full hospital beds, Dr. Mehta said in an interview. In some cases, physicians who have posted have been forced to take down the posts or have faced retribution for speaking out, she said.
“There’s definitely a big fear among physicians, particularly employed physicians, in terms of what the consequences may be for telling their stories,” Dr. Mehta said. “I find that counterproductive. I understand not inducing panic, but these are real stories that are important for people to understand so they do stay home and increase the systemic pressure to get sufficient PPE, so that we can preserve our health care workforce for a problem that is going to get worse before it gets better.”
Meanwhile, an Indiana hospitalist who took to social media to ask for masks for hospitals in his area says he was immediately reprimanded by his management after the posts came to light. The hospitalist posted on a social media platform to request donations of N95 masks after hearing members of the public had purchased such masks. He hoped his plea would aid preparation for the pandemic at local hospitals, explained the physician, who spoke on the condition of anonymity.
Shortly afterward, administrators from his hospital contacted the online forum’s moderator and the posts were removed, he said. During a subsequent conversation, administrators warned the doctor not to make such posts about PPE because it made the hospital appear incompetent.
“I was told, ‘we can handle this, we don’t need the public’s help,’” the physician said. “I was hurt and upset. I was trying to help protect my peers.”
After landing on the management’s radar, the hospitalist said he was reprimanded a second time about posts on a separate personal social media account. The second time, the private posts to friends and family were related to COVID-19 and PPE, but did not include any protected health information, he said. However, administrators did not like the content of the posts, and he was told management was monitoring his activity on social media, he said.
“The larger message is that patients are money,” the hospitalist said. “The corporate side of medicine rules out over the medicine side. Image and making sure there is a consistent cash flow trumps all else.”
Another frontline physician who works at a large New York hospital, said staff have been cautioned not to talk with the media and to be careful what they post on social media regarding COVID-19. The general rule is that only information approved by administrators can be shared, said the physician, who spoke on the condition of anonymity.
“[The health system] is very protective of their public image,” he said. “In the past, people that have posted things that they don’t like get spoken to quickly and/or fired depending on what was written. I could only imagine that would be the situation regarding COVID-19. They are very strict.”
The frontline physician, who has close contact with COVID-19 patients, said he has access to N95 masks at the moment, but when he requested higher-level protective gear, hospital management refused the request and denied that such supplies were needed.
“Safety of frontline workers appears to not be taken seriously,” he said of his hospital. “Everyone is stressed, but at the end of the day, the administration is sitting there, while the rest of us are putting ourselves at risk.”
We reached out to one hospital for comment, but messages were not returned. Other hospitals were not contacted because physicians feared they would face retribution. We also contacted the American Hospital Association but they did not immediately respond.
In Chicago, an email by a nurse to her coworkers about the safety of masks has resulted in a lawsuit after the nurse says she was fired for sharing her concerns with staff. The nurse, Lauri Mazurkiewicz, sent an email to staffers at Northwestern Memorial Hospital stating the surgical masks provided by the hospital were less effective against airborne particles than were N95 masks, according to a lawsuit filed March 23 in Cook County Circuit Court. Ms. Mazurkiewicz was terminated the next day in retaliation for her email, the lawsuit alleges.
Ms. Mazurkiewicz could not be reached for comment by press time.
Christopher King, a spokesman for Northwestern Medicine, said the hospital is reviewing the lawsuit.
“As Northwestern Medicine continues to respond to this unprecedented health care pandemic, the health and well-being of our patients, our staff and our employees is our highest priority,” he said in a statement. “We take these matters seriously and we are currently reviewing the complaint. At this time, we will not be commenting further.”
John Mandrola, MD, a Louisville, Ky.–based cardiologist who has written about the recent muzzling of frontline physicians with respect to the coronavirus, said he is not surprised that some hospitals are preventing physicians from sharing their experiences.
“Before C19, in many hospital systems, there was a culture of fear amongst employed clinicians,” he said. “Employed clinicians see other employed physicians being terminated for speaking frankly about problems. It takes scant few of these cases to create a culture of silence.”
Dr. Mandrola, who is a regular Medscape contributor, said that a number of doctors have reached out to him privately about PPE scarcity and shared that they were explicitly warned by administrators not to talk about the shortfalls. Leadership at Dr. Mandrola’s hospital has not issued the same warnings, he said.
“From the hat of total transparency, I think the public is not getting a full view of the impending potential problems that are going to come by doctors not speaking publicly,” he said. “On the other hand, hospital leadership is doing the best they can. It’s not the hospitals’ fault. Hospital administrators can’t manufacture masks.”
From a public health standpoint, Dr. Mehta said that not allowing health professionals to speak publicly about the situations at their hospitals is “irresponsible.” The public deserves to know what is happening, she said, and the health care workforce needs to prepare for what is to come.
“It’s so important that we hear from our colleagues,” she said. “It’s important to hear those accounts so we can prepare for what we’re about to face. Data is crucial. The more you learn from each other, the better shot we have at successfully treating cases and ultimately beating this.”
With the critical shortage of PPE at his hospital and the inability to speak out about the problem, the orthopedic surgeon foresees the dilemma continuing to worsen.
“It’s not only the lives of front-line health care workers that are at risk, but it’s those that they’re going to spread it to and those that are going to be coming to the hospital requiring our care,” he said. “If we don’t have a fully functioning health care force, our capacity is going to be diminished that much further.”
Over the past month, an orthopedic surgeon has watched as the crowd of sick patients at his hospital has grown, while the supply of personal protective equipment (PPE) for staff has diminished. As he prepares for another day of staffing testing tents and places his one and only mask across his face, he also receives a daily reminder from hospital management: Don’t talk about it.
The surgeon, who works in a COVID-19 hot spot in the Northeast, spoke on the condition of anonymity for fear of employer retribution.
“It’s very clear; no one is allowed to speak for the institution or of the institution,” he said in an interview. “We get a daily warning about being very prudent about posts on personal accounts. They’ve talked about this with respect to various issues: case numbers, case severity, testing availability, [and] PPEs.”
The warnings mean staff at the hospital suffer in silence, unable to share the troubling situation with the public or request assistance with supplies.
“I have one mask. We’re expected to reuse them, unless you were exposed or worked with a known COVID victim,” the surgeon said. “However, with the numbers in our region rapidly increasing, you can’t assume that people don’t have it or that you don’t have particles on your mask, even if you’re not in a known quarantine zone within the institution.”
As the COVID-19 health crisis rages on, online platforms have become a common place for health professionals to lament short supplies, share concerns, tell stories, and plead for help. But at the same time, other physicians, nurses, and health care workers are being muzzled by hospital administrators and threatened with discipline for speaking out about coronavirus caseloads and dwindling supplies. Some worry the gag orders are muddying the picture of how hospitals are faring in the pandemic, while placing the safety of frontline workers at risk.
The silencing of physicians by hospitals about PPE shortages and other COVID-19 issues has become widespread, said Nisha Mehta, MD, a physician advocate and community leader who writes about PPE on social media. Physicians are being warned not to speak or post publicly about their COVID-19 experiences, including PPE shortages, case specifics, and the percentage of full hospital beds, Dr. Mehta said in an interview. In some cases, physicians who have posted have been forced to take down the posts or have faced retribution for speaking out, she said.
“There’s definitely a big fear among physicians, particularly employed physicians, in terms of what the consequences may be for telling their stories,” Dr. Mehta said. “I find that counterproductive. I understand not inducing panic, but these are real stories that are important for people to understand so they do stay home and increase the systemic pressure to get sufficient PPE, so that we can preserve our health care workforce for a problem that is going to get worse before it gets better.”
Meanwhile, an Indiana hospitalist who took to social media to ask for masks for hospitals in his area says he was immediately reprimanded by his management after the posts came to light. The hospitalist posted on a social media platform to request donations of N95 masks after hearing members of the public had purchased such masks. He hoped his plea would aid preparation for the pandemic at local hospitals, explained the physician, who spoke on the condition of anonymity.
Shortly afterward, administrators from his hospital contacted the online forum’s moderator and the posts were removed, he said. During a subsequent conversation, administrators warned the doctor not to make such posts about PPE because it made the hospital appear incompetent.
“I was told, ‘we can handle this, we don’t need the public’s help,’” the physician said. “I was hurt and upset. I was trying to help protect my peers.”
After landing on the management’s radar, the hospitalist said he was reprimanded a second time about posts on a separate personal social media account. The second time, the private posts to friends and family were related to COVID-19 and PPE, but did not include any protected health information, he said. However, administrators did not like the content of the posts, and he was told management was monitoring his activity on social media, he said.
“The larger message is that patients are money,” the hospitalist said. “The corporate side of medicine rules out over the medicine side. Image and making sure there is a consistent cash flow trumps all else.”
Another frontline physician who works at a large New York hospital, said staff have been cautioned not to talk with the media and to be careful what they post on social media regarding COVID-19. The general rule is that only information approved by administrators can be shared, said the physician, who spoke on the condition of anonymity.
“[The health system] is very protective of their public image,” he said. “In the past, people that have posted things that they don’t like get spoken to quickly and/or fired depending on what was written. I could only imagine that would be the situation regarding COVID-19. They are very strict.”
The frontline physician, who has close contact with COVID-19 patients, said he has access to N95 masks at the moment, but when he requested higher-level protective gear, hospital management refused the request and denied that such supplies were needed.
“Safety of frontline workers appears to not be taken seriously,” he said of his hospital. “Everyone is stressed, but at the end of the day, the administration is sitting there, while the rest of us are putting ourselves at risk.”
We reached out to one hospital for comment, but messages were not returned. Other hospitals were not contacted because physicians feared they would face retribution. We also contacted the American Hospital Association but they did not immediately respond.
In Chicago, an email by a nurse to her coworkers about the safety of masks has resulted in a lawsuit after the nurse says she was fired for sharing her concerns with staff. The nurse, Lauri Mazurkiewicz, sent an email to staffers at Northwestern Memorial Hospital stating the surgical masks provided by the hospital were less effective against airborne particles than were N95 masks, according to a lawsuit filed March 23 in Cook County Circuit Court. Ms. Mazurkiewicz was terminated the next day in retaliation for her email, the lawsuit alleges.
Ms. Mazurkiewicz could not be reached for comment by press time.
Christopher King, a spokesman for Northwestern Medicine, said the hospital is reviewing the lawsuit.
“As Northwestern Medicine continues to respond to this unprecedented health care pandemic, the health and well-being of our patients, our staff and our employees is our highest priority,” he said in a statement. “We take these matters seriously and we are currently reviewing the complaint. At this time, we will not be commenting further.”
John Mandrola, MD, a Louisville, Ky.–based cardiologist who has written about the recent muzzling of frontline physicians with respect to the coronavirus, said he is not surprised that some hospitals are preventing physicians from sharing their experiences.
“Before C19, in many hospital systems, there was a culture of fear amongst employed clinicians,” he said. “Employed clinicians see other employed physicians being terminated for speaking frankly about problems. It takes scant few of these cases to create a culture of silence.”
Dr. Mandrola, who is a regular Medscape contributor, said that a number of doctors have reached out to him privately about PPE scarcity and shared that they were explicitly warned by administrators not to talk about the shortfalls. Leadership at Dr. Mandrola’s hospital has not issued the same warnings, he said.
“From the hat of total transparency, I think the public is not getting a full view of the impending potential problems that are going to come by doctors not speaking publicly,” he said. “On the other hand, hospital leadership is doing the best they can. It’s not the hospitals’ fault. Hospital administrators can’t manufacture masks.”
From a public health standpoint, Dr. Mehta said that not allowing health professionals to speak publicly about the situations at their hospitals is “irresponsible.” The public deserves to know what is happening, she said, and the health care workforce needs to prepare for what is to come.
“It’s so important that we hear from our colleagues,” she said. “It’s important to hear those accounts so we can prepare for what we’re about to face. Data is crucial. The more you learn from each other, the better shot we have at successfully treating cases and ultimately beating this.”
With the critical shortage of PPE at his hospital and the inability to speak out about the problem, the orthopedic surgeon foresees the dilemma continuing to worsen.
“It’s not only the lives of front-line health care workers that are at risk, but it’s those that they’re going to spread it to and those that are going to be coming to the hospital requiring our care,” he said. “If we don’t have a fully functioning health care force, our capacity is going to be diminished that much further.”
FDA to allow alternative respiratory devices to treat COVID-19
“Whenever possible, health care facilities should use FDA-cleared conventional/standard full-featured ventilators when necessary to support patients with respiratory failure, or a device subject to an Emergency Use Authorization (EUA), if any,” FDA stated in a guidance document issued March 22.
“However, to help ensure the availability of the greatest possible number of devices for this purpose, ... FDA does not intend to object to limited modifications to indications, claims, functionality, or to the hardware, software, or materials of FDA-cleared devices used to support patients with respiratory failure or respiratory insufficiency, without prior submission of a premarket notification” for the duration of the declared national emergency related to the COVID-19 pandemic.
FDA Commissioner Stephen Hahn, MD, said in a statement that the agency is doing everything it can to support patients, health care professionals, and others during this pandemic.
“One of the most impactful steps we can take is to help with access and availability to life-saving medical treatments,” he said. “Our policy issued today demonstrates our ability to react and adapt quickly during this pandemic and help very ill patients access the lifesaving ventilator support they need. To do that, we are providing maximum regulatory flexibility to facilitate an increase in ventilator inventory, while still providing crucial FDA oversight. We believe this action will immediately increase ventilator availability.”
The document identified examples of where modifications would not create undue risk, including the use of powered emergency ventilators and anesthesia gas machines for patients needing mechanical ventilation; the use of ventilators outside of their cleared environment; the use of devices used to treat patients with sleep apnea, such as CPAPs and BiPAPs, to treat respiratory insufficiency when appropriate design mitigations are in place to minimize aerosolization; and the use of oxygen concentrators for primary supply when medically necessary and clinically appropriate.
The agency also is allowing for changes to the hardware, software, and materials to FDA-cleared ventilators and anesthesia gas machines, such as modifications to motors, batteries, or other electrical components; material changes to components in the gas pathways or with other patient tissue contact; the introduction of filtration to minimize aerosolization; and other hardware and software modifications.
FDA is also allowing for products to be used past their indicated shelf life.
“Whenever possible, health care facilities should use FDA-cleared conventional/standard full-featured ventilators when necessary to support patients with respiratory failure, or a device subject to an Emergency Use Authorization (EUA), if any,” FDA stated in a guidance document issued March 22.
“However, to help ensure the availability of the greatest possible number of devices for this purpose, ... FDA does not intend to object to limited modifications to indications, claims, functionality, or to the hardware, software, or materials of FDA-cleared devices used to support patients with respiratory failure or respiratory insufficiency, without prior submission of a premarket notification” for the duration of the declared national emergency related to the COVID-19 pandemic.
FDA Commissioner Stephen Hahn, MD, said in a statement that the agency is doing everything it can to support patients, health care professionals, and others during this pandemic.
“One of the most impactful steps we can take is to help with access and availability to life-saving medical treatments,” he said. “Our policy issued today demonstrates our ability to react and adapt quickly during this pandemic and help very ill patients access the lifesaving ventilator support they need. To do that, we are providing maximum regulatory flexibility to facilitate an increase in ventilator inventory, while still providing crucial FDA oversight. We believe this action will immediately increase ventilator availability.”
The document identified examples of where modifications would not create undue risk, including the use of powered emergency ventilators and anesthesia gas machines for patients needing mechanical ventilation; the use of ventilators outside of their cleared environment; the use of devices used to treat patients with sleep apnea, such as CPAPs and BiPAPs, to treat respiratory insufficiency when appropriate design mitigations are in place to minimize aerosolization; and the use of oxygen concentrators for primary supply when medically necessary and clinically appropriate.
The agency also is allowing for changes to the hardware, software, and materials to FDA-cleared ventilators and anesthesia gas machines, such as modifications to motors, batteries, or other electrical components; material changes to components in the gas pathways or with other patient tissue contact; the introduction of filtration to minimize aerosolization; and other hardware and software modifications.
FDA is also allowing for products to be used past their indicated shelf life.
“Whenever possible, health care facilities should use FDA-cleared conventional/standard full-featured ventilators when necessary to support patients with respiratory failure, or a device subject to an Emergency Use Authorization (EUA), if any,” FDA stated in a guidance document issued March 22.
“However, to help ensure the availability of the greatest possible number of devices for this purpose, ... FDA does not intend to object to limited modifications to indications, claims, functionality, or to the hardware, software, or materials of FDA-cleared devices used to support patients with respiratory failure or respiratory insufficiency, without prior submission of a premarket notification” for the duration of the declared national emergency related to the COVID-19 pandemic.
FDA Commissioner Stephen Hahn, MD, said in a statement that the agency is doing everything it can to support patients, health care professionals, and others during this pandemic.
“One of the most impactful steps we can take is to help with access and availability to life-saving medical treatments,” he said. “Our policy issued today demonstrates our ability to react and adapt quickly during this pandemic and help very ill patients access the lifesaving ventilator support they need. To do that, we are providing maximum regulatory flexibility to facilitate an increase in ventilator inventory, while still providing crucial FDA oversight. We believe this action will immediately increase ventilator availability.”
The document identified examples of where modifications would not create undue risk, including the use of powered emergency ventilators and anesthesia gas machines for patients needing mechanical ventilation; the use of ventilators outside of their cleared environment; the use of devices used to treat patients with sleep apnea, such as CPAPs and BiPAPs, to treat respiratory insufficiency when appropriate design mitigations are in place to minimize aerosolization; and the use of oxygen concentrators for primary supply when medically necessary and clinically appropriate.
The agency also is allowing for changes to the hardware, software, and materials to FDA-cleared ventilators and anesthesia gas machines, such as modifications to motors, batteries, or other electrical components; material changes to components in the gas pathways or with other patient tissue contact; the introduction of filtration to minimize aerosolization; and other hardware and software modifications.
FDA is also allowing for products to be used past their indicated shelf life.
Stronger links forged between RA and asthma, COPD
Asthma and chronic obstructive pulmonary disease were both linked to an increased risk of rheumatoid arthritis in a recent large, prospective cohort study, researchers have reported, which adds to a growing body of evidence that airway inflammation is implicated in the development of this disease.
RA risk was increased by about 50% among asthma patients, even when excluding those who had ever smoked, according to the study’s results, which were based on more than 200,000 women in the Nurses’ Health Study I and II.
Risk of RA nearly doubled among those with chronic obstructive pulmonary disease (COPD), with an even stronger association seen in older ever-smokers, according to authors of the study.
The findings not only strengthen the case for the potential role of obstructive lung diseases in RA development, according to the study’s authors, but also suggest that health care providers need to lower the bar for evaluation of patients with lung diseases and inflammatory joint symptoms.
“If these patients develop arthralgias, then the clinicians taking care of them should have a low threshold to consider RA, and perhaps refer, or check these patients with a diagnostic test for RA,” said researcher Jeffrey A. Sparks, MD, of Brigham and Women’s Hospital and Harvard Medical School in Boston.
What’s perhaps not as clear now is whether screening obstructive lung disease patients in the absence of early RA signs would be warranted: “I don’t know if we’re quite at the point where we would need to screen these patients if they’re not symptomatic,” Dr. Sparks said in an interview.
The study by Dr. Sparks and colleagues is, by far, not the first study to implicate asthma or other lung conditions in RA development. However, most previous studies are retrospective, and interpretation of the findings has been subject to limitations such as inadequate power to detect an increased risk or lack of adjustment for important confounding factors, such as smoking.
As such, the study by Dr. Sparks and colleagues is believed to be the first-ever prospective study to evaluate asthma and COPD as risk factors for RA, study authors reported in Arthritis & Rheumatology.
Researchers were able to identify 1,060 incident RA cases that developed in 15,148 women with asthma and 3,573 with COPD in the study with more than 4 million person-years of follow-up.
The association between asthma and increased RA risk was seen not only for the asthma population as a whole (hazard ratio, 1.53; 95% confidence interval, 1.24-1.88), but also for the subset of women who had never smoked, to a similar degree (HR, 1.53; 95% CI, 1.14-2.05), the report shows.
COPD’s association with RA risk was apparent overall (HR, 1.89; 95% CI, 1.31-2.75) and even more so in the subgroup of ever-smokers 55 years of age and older (HR, 2.20; 95% CI, 1.38-3.51), the data further show.
Findings of studies looking at the inflammation of airways and other mucosal sites are “critically important to understand” when it comes to trying to prevent RA, said Kevin Deane, MD, of the University of Colorado at Denver at Aurora.
“If we indeed are trying to prevent rheumatoid arthritis in terms of the joint disease, we may need to look at these mucosal sites in individuals who don’t yet have joint disease as potential sites to target for prevention, or at least areas to study to understand how prevention may work,” said Dr. Deane, principal investigator on the National Institutes of Health–funded Strategy for the Prevention of RA (StopRA) trial.
With that in mind, it’s conceivable targeting a lung process might prevent joint disease in a patient with asthma or airway inflammation and blood markers that indicate a risk of RA, Dr. Deane said in an interview.
Blood markers of RA have been evaluated in some recent studies, with findings that provide further evidence of a link between lung diseases and RA, and vice versa.
In particular, anti–citrullinated protein antibodies (ACPA) are clearly central to RA pathogenesis. And while asthma is increasingly linked to RA risk, there have been relatively little data on any potential links between ACPA and asthma.
That research gap led to a case-control study of the Nurses’ Health Study I and II (on which Dr. Sparks was senior author) showing that asthma was strongly linked to elevated ACPA in blood drawn from patients prior to a diagnosis of RA.
Results, published last year in Arthritis Research & Therapy, showed a significant association between asthma and pre-RA ACPA elevation (odds ratio, 3.57; 95% CI, 1.58-8.04), after adjustment for smoking and other potentially confounding factors. Investigators said the findings provided evidence that chronic mucosal airway inflammation is a factor in the development of ACPA and in the pathogenesis of RA.
In a follow-up study published more recently in Arthritis Care & Research, investigators showed that, among women in the Nurses Health Study I and II, pre-RA ACPA elevation was linked to increased risk of COPD, compared with controls (HR, 3.04; 95% CI, 1.33-7.00), while the risk for development of asthma was similar in women with or without elevated pre-RA ACPA.
That study was in part an attempt to establish a “timeline” related to antibodies, lung diseases, and RA onset, Dr. Sparks said in the interview.
“We think that probably the asthma is more important in developing the antibody, but that once you have the antibody, if you didn’t have asthma by then, you’re unlikely to develop it,” he said. “So asthma seems to be something that could happen before the antibody production, whereas COPD seems to happen after – but ACPA seems to be the common link in both of these obstructive lung diseases.”
The study in Arthritis & Rheumatology linking asthma and COPD to risk of incident RA was supported by the National Institutes of Health. Dr. Sparks reported grant support from Amgen and Bristol Myers Squibb and consulting fees from Inova and Optum. Coauthors provided disclosures related to GlaxoSmithKline, AstraZeneca, Merck, Neutrolis, and Genentech.
SOURCE: Ford JA et al. Arthritis Rheumatol. 2020 Mar 4. doi: 10.1002/art.41194.
Asthma and chronic obstructive pulmonary disease were both linked to an increased risk of rheumatoid arthritis in a recent large, prospective cohort study, researchers have reported, which adds to a growing body of evidence that airway inflammation is implicated in the development of this disease.
RA risk was increased by about 50% among asthma patients, even when excluding those who had ever smoked, according to the study’s results, which were based on more than 200,000 women in the Nurses’ Health Study I and II.
Risk of RA nearly doubled among those with chronic obstructive pulmonary disease (COPD), with an even stronger association seen in older ever-smokers, according to authors of the study.
The findings not only strengthen the case for the potential role of obstructive lung diseases in RA development, according to the study’s authors, but also suggest that health care providers need to lower the bar for evaluation of patients with lung diseases and inflammatory joint symptoms.
“If these patients develop arthralgias, then the clinicians taking care of them should have a low threshold to consider RA, and perhaps refer, or check these patients with a diagnostic test for RA,” said researcher Jeffrey A. Sparks, MD, of Brigham and Women’s Hospital and Harvard Medical School in Boston.
What’s perhaps not as clear now is whether screening obstructive lung disease patients in the absence of early RA signs would be warranted: “I don’t know if we’re quite at the point where we would need to screen these patients if they’re not symptomatic,” Dr. Sparks said in an interview.
The study by Dr. Sparks and colleagues is, by far, not the first study to implicate asthma or other lung conditions in RA development. However, most previous studies are retrospective, and interpretation of the findings has been subject to limitations such as inadequate power to detect an increased risk or lack of adjustment for important confounding factors, such as smoking.
As such, the study by Dr. Sparks and colleagues is believed to be the first-ever prospective study to evaluate asthma and COPD as risk factors for RA, study authors reported in Arthritis & Rheumatology.
Researchers were able to identify 1,060 incident RA cases that developed in 15,148 women with asthma and 3,573 with COPD in the study with more than 4 million person-years of follow-up.
The association between asthma and increased RA risk was seen not only for the asthma population as a whole (hazard ratio, 1.53; 95% confidence interval, 1.24-1.88), but also for the subset of women who had never smoked, to a similar degree (HR, 1.53; 95% CI, 1.14-2.05), the report shows.
COPD’s association with RA risk was apparent overall (HR, 1.89; 95% CI, 1.31-2.75) and even more so in the subgroup of ever-smokers 55 years of age and older (HR, 2.20; 95% CI, 1.38-3.51), the data further show.
Findings of studies looking at the inflammation of airways and other mucosal sites are “critically important to understand” when it comes to trying to prevent RA, said Kevin Deane, MD, of the University of Colorado at Denver at Aurora.
“If we indeed are trying to prevent rheumatoid arthritis in terms of the joint disease, we may need to look at these mucosal sites in individuals who don’t yet have joint disease as potential sites to target for prevention, or at least areas to study to understand how prevention may work,” said Dr. Deane, principal investigator on the National Institutes of Health–funded Strategy for the Prevention of RA (StopRA) trial.
With that in mind, it’s conceivable targeting a lung process might prevent joint disease in a patient with asthma or airway inflammation and blood markers that indicate a risk of RA, Dr. Deane said in an interview.
Blood markers of RA have been evaluated in some recent studies, with findings that provide further evidence of a link between lung diseases and RA, and vice versa.
In particular, anti–citrullinated protein antibodies (ACPA) are clearly central to RA pathogenesis. And while asthma is increasingly linked to RA risk, there have been relatively little data on any potential links between ACPA and asthma.
That research gap led to a case-control study of the Nurses’ Health Study I and II (on which Dr. Sparks was senior author) showing that asthma was strongly linked to elevated ACPA in blood drawn from patients prior to a diagnosis of RA.
Results, published last year in Arthritis Research & Therapy, showed a significant association between asthma and pre-RA ACPA elevation (odds ratio, 3.57; 95% CI, 1.58-8.04), after adjustment for smoking and other potentially confounding factors. Investigators said the findings provided evidence that chronic mucosal airway inflammation is a factor in the development of ACPA and in the pathogenesis of RA.
In a follow-up study published more recently in Arthritis Care & Research, investigators showed that, among women in the Nurses Health Study I and II, pre-RA ACPA elevation was linked to increased risk of COPD, compared with controls (HR, 3.04; 95% CI, 1.33-7.00), while the risk for development of asthma was similar in women with or without elevated pre-RA ACPA.
That study was in part an attempt to establish a “timeline” related to antibodies, lung diseases, and RA onset, Dr. Sparks said in the interview.
“We think that probably the asthma is more important in developing the antibody, but that once you have the antibody, if you didn’t have asthma by then, you’re unlikely to develop it,” he said. “So asthma seems to be something that could happen before the antibody production, whereas COPD seems to happen after – but ACPA seems to be the common link in both of these obstructive lung diseases.”
The study in Arthritis & Rheumatology linking asthma and COPD to risk of incident RA was supported by the National Institutes of Health. Dr. Sparks reported grant support from Amgen and Bristol Myers Squibb and consulting fees from Inova and Optum. Coauthors provided disclosures related to GlaxoSmithKline, AstraZeneca, Merck, Neutrolis, and Genentech.
SOURCE: Ford JA et al. Arthritis Rheumatol. 2020 Mar 4. doi: 10.1002/art.41194.
Asthma and chronic obstructive pulmonary disease were both linked to an increased risk of rheumatoid arthritis in a recent large, prospective cohort study, researchers have reported, which adds to a growing body of evidence that airway inflammation is implicated in the development of this disease.
RA risk was increased by about 50% among asthma patients, even when excluding those who had ever smoked, according to the study’s results, which were based on more than 200,000 women in the Nurses’ Health Study I and II.
Risk of RA nearly doubled among those with chronic obstructive pulmonary disease (COPD), with an even stronger association seen in older ever-smokers, according to authors of the study.
The findings not only strengthen the case for the potential role of obstructive lung diseases in RA development, according to the study’s authors, but also suggest that health care providers need to lower the bar for evaluation of patients with lung diseases and inflammatory joint symptoms.
“If these patients develop arthralgias, then the clinicians taking care of them should have a low threshold to consider RA, and perhaps refer, or check these patients with a diagnostic test for RA,” said researcher Jeffrey A. Sparks, MD, of Brigham and Women’s Hospital and Harvard Medical School in Boston.
What’s perhaps not as clear now is whether screening obstructive lung disease patients in the absence of early RA signs would be warranted: “I don’t know if we’re quite at the point where we would need to screen these patients if they’re not symptomatic,” Dr. Sparks said in an interview.
The study by Dr. Sparks and colleagues is, by far, not the first study to implicate asthma or other lung conditions in RA development. However, most previous studies are retrospective, and interpretation of the findings has been subject to limitations such as inadequate power to detect an increased risk or lack of adjustment for important confounding factors, such as smoking.
As such, the study by Dr. Sparks and colleagues is believed to be the first-ever prospective study to evaluate asthma and COPD as risk factors for RA, study authors reported in Arthritis & Rheumatology.
Researchers were able to identify 1,060 incident RA cases that developed in 15,148 women with asthma and 3,573 with COPD in the study with more than 4 million person-years of follow-up.
The association between asthma and increased RA risk was seen not only for the asthma population as a whole (hazard ratio, 1.53; 95% confidence interval, 1.24-1.88), but also for the subset of women who had never smoked, to a similar degree (HR, 1.53; 95% CI, 1.14-2.05), the report shows.
COPD’s association with RA risk was apparent overall (HR, 1.89; 95% CI, 1.31-2.75) and even more so in the subgroup of ever-smokers 55 years of age and older (HR, 2.20; 95% CI, 1.38-3.51), the data further show.
Findings of studies looking at the inflammation of airways and other mucosal sites are “critically important to understand” when it comes to trying to prevent RA, said Kevin Deane, MD, of the University of Colorado at Denver at Aurora.
“If we indeed are trying to prevent rheumatoid arthritis in terms of the joint disease, we may need to look at these mucosal sites in individuals who don’t yet have joint disease as potential sites to target for prevention, or at least areas to study to understand how prevention may work,” said Dr. Deane, principal investigator on the National Institutes of Health–funded Strategy for the Prevention of RA (StopRA) trial.
With that in mind, it’s conceivable targeting a lung process might prevent joint disease in a patient with asthma or airway inflammation and blood markers that indicate a risk of RA, Dr. Deane said in an interview.
Blood markers of RA have been evaluated in some recent studies, with findings that provide further evidence of a link between lung diseases and RA, and vice versa.
In particular, anti–citrullinated protein antibodies (ACPA) are clearly central to RA pathogenesis. And while asthma is increasingly linked to RA risk, there have been relatively little data on any potential links between ACPA and asthma.
That research gap led to a case-control study of the Nurses’ Health Study I and II (on which Dr. Sparks was senior author) showing that asthma was strongly linked to elevated ACPA in blood drawn from patients prior to a diagnosis of RA.
Results, published last year in Arthritis Research & Therapy, showed a significant association between asthma and pre-RA ACPA elevation (odds ratio, 3.57; 95% CI, 1.58-8.04), after adjustment for smoking and other potentially confounding factors. Investigators said the findings provided evidence that chronic mucosal airway inflammation is a factor in the development of ACPA and in the pathogenesis of RA.
In a follow-up study published more recently in Arthritis Care & Research, investigators showed that, among women in the Nurses Health Study I and II, pre-RA ACPA elevation was linked to increased risk of COPD, compared with controls (HR, 3.04; 95% CI, 1.33-7.00), while the risk for development of asthma was similar in women with or without elevated pre-RA ACPA.
That study was in part an attempt to establish a “timeline” related to antibodies, lung diseases, and RA onset, Dr. Sparks said in the interview.
“We think that probably the asthma is more important in developing the antibody, but that once you have the antibody, if you didn’t have asthma by then, you’re unlikely to develop it,” he said. “So asthma seems to be something that could happen before the antibody production, whereas COPD seems to happen after – but ACPA seems to be the common link in both of these obstructive lung diseases.”
The study in Arthritis & Rheumatology linking asthma and COPD to risk of incident RA was supported by the National Institutes of Health. Dr. Sparks reported grant support from Amgen and Bristol Myers Squibb and consulting fees from Inova and Optum. Coauthors provided disclosures related to GlaxoSmithKline, AstraZeneca, Merck, Neutrolis, and Genentech.
SOURCE: Ford JA et al. Arthritis Rheumatol. 2020 Mar 4. doi: 10.1002/art.41194.
FROM ARTHRITIS & RHEUMATOLOGY
Study: Delays filling biologic prescriptions have consequences
Insurance and specialty pharmacy delays in authorizing new biologic prescriptions for severe allergies leave waiting patients at risk of asthma attacks, hospitalizations, emergency department visits and prednisone shots and their known side effects, according to a single-center study that was to have been presented at the annual meeting of the American Academy of Allergy, Asthma and Immunology.
The AAAAI canceled their annual meeting and provided abstracts and access to presenters for press coverage.
The study of 80 patients in State College, Pa., found that they waited an average of 44 days from when their doctor submitted the preauthorization request to the insurance company until the practice received the shipment for dispensing to the patient, investigator Faoud Ishmael, MD, PhD, of Mount Nittany Medical Group said in an interview. “The implication here is that these are really the most severe patients who, you would argue, need their medications the quickest, and it’s taking longer to get them than it would an inhaler,” Dr. Ishmael said.
The study focused on patients with severe asthma (n = 60) or urticarial (n = 20) who received a new prescription of monoclonal antibody therapy from March 2014 to August 2019. For asthma treatments, the average time was 45.8 days; for urticaria, 40.6 days (P = .573), Dr. Ishmael said. The researchers divided the total amount of time into two components: insurance plan review and approval (P = .654, and specialty pharmacy review and dispensing of the medicine, each of which averaged 22.8 days (P = .384), he said.
He also noted wide disparity in the range of approval times. “The shortest approval time was 1 day, and the longest 97 days,” Dr. Ishmael said. “It’s interesting that we had this really broad spread.”
What’s more, the study found no trend for the delays among insurers and specialty pharmacies, Dr. Ishmael added. “When these prescriptions get submitted, it’s like a black box,” he said. “It really seems arbitrary why some of them take so long and some of them don’t.” The findings were independent of type of coverage, whether commercial or government, or even specific insurance plans. “It’s more the process that is flawed rather than one insurance company being the bad guy,” he said.
The study also looked at what happened to patients while they were waiting for their prescriptions to be delivered. “What we found is that over half of asthmatics had an exacerbation – 51% had at least one asthma attack where they needed prednisone,” Dr. Ishmael said (P = .0015), “and we had three patients admitted to the hospital over that time frame when they were waiting for the drugs.” One of those patients had been admitted twice, making four total hospitalizations. Preliminary data analysis showed that about 40% of the patients who had attacks went to the emergency department.
For asthmatics who needed prednisone, the average dose was 480 mg (P = .284) – “a pretty substantial number,” in Dr. Ishmael’s words. He noted that a large portion of the study patients were obese, with a mean body mass index of 33 kg/m2. Other comorbidities prevalent in the study population were hypertension and type 2 diabetes. “Prednisone is something that could worsen all of those conditions, so it’s not a trivial issue,” he said.
The study, however, didn’t evaluate costs of the interventions during the delay period vs. the costs of the medications themselves. Of the 80 prescriptions Dr. Ishmael and coauthors submitted, only one was rejected, that person being a smoker, he said. “I understand these are expensive medicines, but it’s counterproductive to delay them because in the long run the insurance company ends up paying for the hospitalization and the drug rather than just the drug,” he said.
Timothy Craig, DO, of Penn State Health Allergy, Asthma, and Immunology and professor of medicine and pediatrics at Penn State College of Medicine, both in Hershey, said he was surprised at the brevity of the delays reported in Dr. Ishmael’s study. “They do much better than we do with preauthorization,” he said, noting that, in his experience, these approvals take much longer. He added that his own research has found faulty insurance plan algorithms are at the heart of these delays. “We need more studies to clarify how much this is interfering with patient care and how much risk they’re putting patients in,” he said.
The COVID-19 pandemic poses a double-edged sword for physicians managing patients with severe asthma, Dr. Craig noted. “Their asthma care is important, especially if they do test for COVID-19,” he said. On the other hand, doctors and nurses attending to COVID-19 patients will have less time to haggle with payers to expedite coverage for biologics for their severe asthma patients, he said. “I hope the flexibility is there, especially at this time to allow people to get on the biologics and stay on them,” he said.
Dr. Ishmael said these findings have serious implications because biologics are getting prescribed ever more frequently for asthma and hives. Steps his practice has taken to streamline the process include following the payer’s approval guidelines as closely as possible. This sometimes can mean making sure a patient with severe asthma has been maximized on controller medications before submitting the biologic prescription, he said. Another step is to use drug company programs to remove barriers to coverage.
Nonetheless, the approval process can be daunting even when taking those steps, he said. “Those guidelines that constitute approval may vary a lot from one insurer to another; and sometimes those guidelines are different from the criteria that studies may have used when these drugs were being evaluated in clinical trials,” he said. It would be helpful, he said, if payers used the National Heart, Lung and Blood institute and the Global Initiative for Asthma guidelines for biologics.
One of the goals of the researchers is to present their findings to payers, “to let them know, here are some of the hang-ups and the real risks associated with delaying these medications,” Dr. Ishmael said.
“When specialists especially prescribe these therapies, there’s usually a valid reason,” he said. “We really need to do something about the current process – if there are ways to make it more transparent, faster.”
Dr. Ishmael has no relevant financial relationships to disclose.
SOURCE: Ishmael F et al. AAAAI 2020. Session 3609, Presentation 558.
Insurance and specialty pharmacy delays in authorizing new biologic prescriptions for severe allergies leave waiting patients at risk of asthma attacks, hospitalizations, emergency department visits and prednisone shots and their known side effects, according to a single-center study that was to have been presented at the annual meeting of the American Academy of Allergy, Asthma and Immunology.
The AAAAI canceled their annual meeting and provided abstracts and access to presenters for press coverage.
The study of 80 patients in State College, Pa., found that they waited an average of 44 days from when their doctor submitted the preauthorization request to the insurance company until the practice received the shipment for dispensing to the patient, investigator Faoud Ishmael, MD, PhD, of Mount Nittany Medical Group said in an interview. “The implication here is that these are really the most severe patients who, you would argue, need their medications the quickest, and it’s taking longer to get them than it would an inhaler,” Dr. Ishmael said.
The study focused on patients with severe asthma (n = 60) or urticarial (n = 20) who received a new prescription of monoclonal antibody therapy from March 2014 to August 2019. For asthma treatments, the average time was 45.8 days; for urticaria, 40.6 days (P = .573), Dr. Ishmael said. The researchers divided the total amount of time into two components: insurance plan review and approval (P = .654, and specialty pharmacy review and dispensing of the medicine, each of which averaged 22.8 days (P = .384), he said.
He also noted wide disparity in the range of approval times. “The shortest approval time was 1 day, and the longest 97 days,” Dr. Ishmael said. “It’s interesting that we had this really broad spread.”
What’s more, the study found no trend for the delays among insurers and specialty pharmacies, Dr. Ishmael added. “When these prescriptions get submitted, it’s like a black box,” he said. “It really seems arbitrary why some of them take so long and some of them don’t.” The findings were independent of type of coverage, whether commercial or government, or even specific insurance plans. “It’s more the process that is flawed rather than one insurance company being the bad guy,” he said.
The study also looked at what happened to patients while they were waiting for their prescriptions to be delivered. “What we found is that over half of asthmatics had an exacerbation – 51% had at least one asthma attack where they needed prednisone,” Dr. Ishmael said (P = .0015), “and we had three patients admitted to the hospital over that time frame when they were waiting for the drugs.” One of those patients had been admitted twice, making four total hospitalizations. Preliminary data analysis showed that about 40% of the patients who had attacks went to the emergency department.
For asthmatics who needed prednisone, the average dose was 480 mg (P = .284) – “a pretty substantial number,” in Dr. Ishmael’s words. He noted that a large portion of the study patients were obese, with a mean body mass index of 33 kg/m2. Other comorbidities prevalent in the study population were hypertension and type 2 diabetes. “Prednisone is something that could worsen all of those conditions, so it’s not a trivial issue,” he said.
The study, however, didn’t evaluate costs of the interventions during the delay period vs. the costs of the medications themselves. Of the 80 prescriptions Dr. Ishmael and coauthors submitted, only one was rejected, that person being a smoker, he said. “I understand these are expensive medicines, but it’s counterproductive to delay them because in the long run the insurance company ends up paying for the hospitalization and the drug rather than just the drug,” he said.
Timothy Craig, DO, of Penn State Health Allergy, Asthma, and Immunology and professor of medicine and pediatrics at Penn State College of Medicine, both in Hershey, said he was surprised at the brevity of the delays reported in Dr. Ishmael’s study. “They do much better than we do with preauthorization,” he said, noting that, in his experience, these approvals take much longer. He added that his own research has found faulty insurance plan algorithms are at the heart of these delays. “We need more studies to clarify how much this is interfering with patient care and how much risk they’re putting patients in,” he said.
The COVID-19 pandemic poses a double-edged sword for physicians managing patients with severe asthma, Dr. Craig noted. “Their asthma care is important, especially if they do test for COVID-19,” he said. On the other hand, doctors and nurses attending to COVID-19 patients will have less time to haggle with payers to expedite coverage for biologics for their severe asthma patients, he said. “I hope the flexibility is there, especially at this time to allow people to get on the biologics and stay on them,” he said.
Dr. Ishmael said these findings have serious implications because biologics are getting prescribed ever more frequently for asthma and hives. Steps his practice has taken to streamline the process include following the payer’s approval guidelines as closely as possible. This sometimes can mean making sure a patient with severe asthma has been maximized on controller medications before submitting the biologic prescription, he said. Another step is to use drug company programs to remove barriers to coverage.
Nonetheless, the approval process can be daunting even when taking those steps, he said. “Those guidelines that constitute approval may vary a lot from one insurer to another; and sometimes those guidelines are different from the criteria that studies may have used when these drugs were being evaluated in clinical trials,” he said. It would be helpful, he said, if payers used the National Heart, Lung and Blood institute and the Global Initiative for Asthma guidelines for biologics.
One of the goals of the researchers is to present their findings to payers, “to let them know, here are some of the hang-ups and the real risks associated with delaying these medications,” Dr. Ishmael said.
“When specialists especially prescribe these therapies, there’s usually a valid reason,” he said. “We really need to do something about the current process – if there are ways to make it more transparent, faster.”
Dr. Ishmael has no relevant financial relationships to disclose.
SOURCE: Ishmael F et al. AAAAI 2020. Session 3609, Presentation 558.
Insurance and specialty pharmacy delays in authorizing new biologic prescriptions for severe allergies leave waiting patients at risk of asthma attacks, hospitalizations, emergency department visits and prednisone shots and their known side effects, according to a single-center study that was to have been presented at the annual meeting of the American Academy of Allergy, Asthma and Immunology.
The AAAAI canceled their annual meeting and provided abstracts and access to presenters for press coverage.
The study of 80 patients in State College, Pa., found that they waited an average of 44 days from when their doctor submitted the preauthorization request to the insurance company until the practice received the shipment for dispensing to the patient, investigator Faoud Ishmael, MD, PhD, of Mount Nittany Medical Group said in an interview. “The implication here is that these are really the most severe patients who, you would argue, need their medications the quickest, and it’s taking longer to get them than it would an inhaler,” Dr. Ishmael said.
The study focused on patients with severe asthma (n = 60) or urticarial (n = 20) who received a new prescription of monoclonal antibody therapy from March 2014 to August 2019. For asthma treatments, the average time was 45.8 days; for urticaria, 40.6 days (P = .573), Dr. Ishmael said. The researchers divided the total amount of time into two components: insurance plan review and approval (P = .654, and specialty pharmacy review and dispensing of the medicine, each of which averaged 22.8 days (P = .384), he said.
He also noted wide disparity in the range of approval times. “The shortest approval time was 1 day, and the longest 97 days,” Dr. Ishmael said. “It’s interesting that we had this really broad spread.”
What’s more, the study found no trend for the delays among insurers and specialty pharmacies, Dr. Ishmael added. “When these prescriptions get submitted, it’s like a black box,” he said. “It really seems arbitrary why some of them take so long and some of them don’t.” The findings were independent of type of coverage, whether commercial or government, or even specific insurance plans. “It’s more the process that is flawed rather than one insurance company being the bad guy,” he said.
The study also looked at what happened to patients while they were waiting for their prescriptions to be delivered. “What we found is that over half of asthmatics had an exacerbation – 51% had at least one asthma attack where they needed prednisone,” Dr. Ishmael said (P = .0015), “and we had three patients admitted to the hospital over that time frame when they were waiting for the drugs.” One of those patients had been admitted twice, making four total hospitalizations. Preliminary data analysis showed that about 40% of the patients who had attacks went to the emergency department.
For asthmatics who needed prednisone, the average dose was 480 mg (P = .284) – “a pretty substantial number,” in Dr. Ishmael’s words. He noted that a large portion of the study patients were obese, with a mean body mass index of 33 kg/m2. Other comorbidities prevalent in the study population were hypertension and type 2 diabetes. “Prednisone is something that could worsen all of those conditions, so it’s not a trivial issue,” he said.
The study, however, didn’t evaluate costs of the interventions during the delay period vs. the costs of the medications themselves. Of the 80 prescriptions Dr. Ishmael and coauthors submitted, only one was rejected, that person being a smoker, he said. “I understand these are expensive medicines, but it’s counterproductive to delay them because in the long run the insurance company ends up paying for the hospitalization and the drug rather than just the drug,” he said.
Timothy Craig, DO, of Penn State Health Allergy, Asthma, and Immunology and professor of medicine and pediatrics at Penn State College of Medicine, both in Hershey, said he was surprised at the brevity of the delays reported in Dr. Ishmael’s study. “They do much better than we do with preauthorization,” he said, noting that, in his experience, these approvals take much longer. He added that his own research has found faulty insurance plan algorithms are at the heart of these delays. “We need more studies to clarify how much this is interfering with patient care and how much risk they’re putting patients in,” he said.
The COVID-19 pandemic poses a double-edged sword for physicians managing patients with severe asthma, Dr. Craig noted. “Their asthma care is important, especially if they do test for COVID-19,” he said. On the other hand, doctors and nurses attending to COVID-19 patients will have less time to haggle with payers to expedite coverage for biologics for their severe asthma patients, he said. “I hope the flexibility is there, especially at this time to allow people to get on the biologics and stay on them,” he said.
Dr. Ishmael said these findings have serious implications because biologics are getting prescribed ever more frequently for asthma and hives. Steps his practice has taken to streamline the process include following the payer’s approval guidelines as closely as possible. This sometimes can mean making sure a patient with severe asthma has been maximized on controller medications before submitting the biologic prescription, he said. Another step is to use drug company programs to remove barriers to coverage.
Nonetheless, the approval process can be daunting even when taking those steps, he said. “Those guidelines that constitute approval may vary a lot from one insurer to another; and sometimes those guidelines are different from the criteria that studies may have used when these drugs were being evaluated in clinical trials,” he said. It would be helpful, he said, if payers used the National Heart, Lung and Blood institute and the Global Initiative for Asthma guidelines for biologics.
One of the goals of the researchers is to present their findings to payers, “to let them know, here are some of the hang-ups and the real risks associated with delaying these medications,” Dr. Ishmael said.
“When specialists especially prescribe these therapies, there’s usually a valid reason,” he said. “We really need to do something about the current process – if there are ways to make it more transparent, faster.”
Dr. Ishmael has no relevant financial relationships to disclose.
SOURCE: Ishmael F et al. AAAAI 2020. Session 3609, Presentation 558.
REPORTING FROM AAAAI
How texting unites Seattle’s critical care departments
One of a smartphone’s simplest features has become a powerful communication and coordination tool for metro Seattle’s critical care departments.
Anne B. Lipke, MD, is the medical director of Swedish Medical Center’s Issaquah, Wash., campus in suburban Seattle. In an audio interview, Dr. Lipke explains how texting has become a fast, effective component of Seattle’s critical care response to COVID-19. And she offers lessons for physicians across the country who may soon be seeing situations similar to Seattle’s.
One of a smartphone’s simplest features has become a powerful communication and coordination tool for metro Seattle’s critical care departments.
Anne B. Lipke, MD, is the medical director of Swedish Medical Center’s Issaquah, Wash., campus in suburban Seattle. In an audio interview, Dr. Lipke explains how texting has become a fast, effective component of Seattle’s critical care response to COVID-19. And she offers lessons for physicians across the country who may soon be seeing situations similar to Seattle’s.
One of a smartphone’s simplest features has become a powerful communication and coordination tool for metro Seattle’s critical care departments.
Anne B. Lipke, MD, is the medical director of Swedish Medical Center’s Issaquah, Wash., campus in suburban Seattle. In an audio interview, Dr. Lipke explains how texting has become a fast, effective component of Seattle’s critical care response to COVID-19. And she offers lessons for physicians across the country who may soon be seeing situations similar to Seattle’s.
Managing the COVID-19 isolation floor at UCSF Medical Center
Robert Wachter, MD, MHM, chair of the department of medicine at UCSF, interviewed Armond Esmaili, MD, a hospitalist and assistant professor of medicine at UCSF, who is the leader of the Respiratory Isolation Unit at UCSF Medical Center, where the institution's COVID-19 and rule-out COVID-19 patients are being cohorted.
Robert Wachter, MD, MHM, chair of the department of medicine at UCSF, interviewed Armond Esmaili, MD, a hospitalist and assistant professor of medicine at UCSF, who is the leader of the Respiratory Isolation Unit at UCSF Medical Center, where the institution's COVID-19 and rule-out COVID-19 patients are being cohorted.
Robert Wachter, MD, MHM, chair of the department of medicine at UCSF, interviewed Armond Esmaili, MD, a hospitalist and assistant professor of medicine at UCSF, who is the leader of the Respiratory Isolation Unit at UCSF Medical Center, where the institution's COVID-19 and rule-out COVID-19 patients are being cohorted.
Flu now riding on COVID-19’s coattails
The viral tsunami that is COVID-19 has hit the United States, and influenza appears to be riding the crest of the wave.
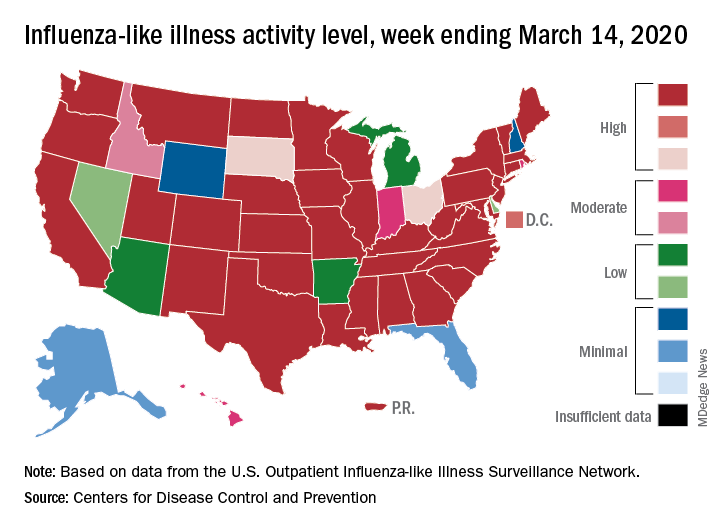
according to the Centers for Disease Control. Flu-related visits went from 5.2% of all outpatient visits the week before to 5.8% during the week ending March 14.
“The COVID-19 outbreak unfolding in the United States may affect healthcare seeking behavior which in turn would impact data from” the U.S. Outpatient Influenza-like Illness Surveillance Network, the CDC explained.
Data from clinical laboratories show that, despite the increased activity, fewer respiratory specimens tested positive for influenza: 15.3% for the week of March 8-14, compared with 21.1% the week before, the CDC’s influenza division said in its latest FluView report.
Influenza activity also increased slightly among the states, with 35 states and Puerto Rico at the highest level on the CDC’s 1-10 scale, versus 34 states and Puerto Rico the previous week. The count was down to 33 for the last week of February, CDC data show.
Severity measures remain mixed as overall hospitalization continues to be moderate but rates for children aged 0-4 years and adults aged 18-49 years are the highest on record and rates for children aged 5-17 years are the highest since the 2009 pandemic, the influenza division said.
Mortality data present a similar picture: The overall death rate is low, but the 149 flu-related deaths reported among children is the most for this point of the season since 2009, the CDC said.
The viral tsunami that is COVID-19 has hit the United States, and influenza appears to be riding the crest of the wave.
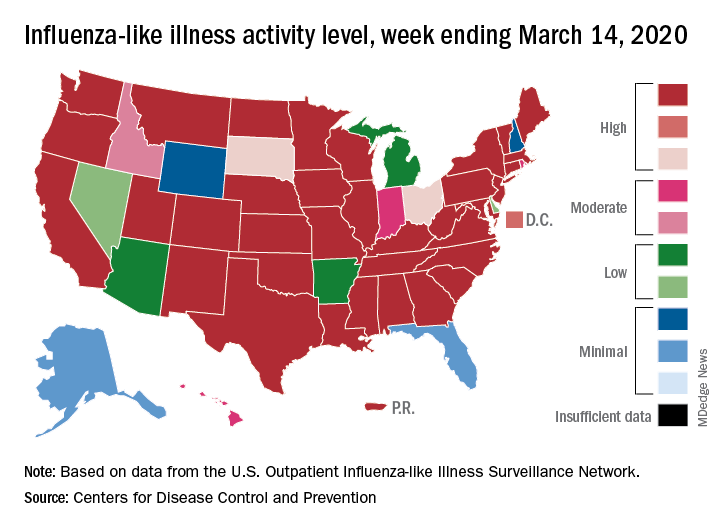
according to the Centers for Disease Control. Flu-related visits went from 5.2% of all outpatient visits the week before to 5.8% during the week ending March 14.
“The COVID-19 outbreak unfolding in the United States may affect healthcare seeking behavior which in turn would impact data from” the U.S. Outpatient Influenza-like Illness Surveillance Network, the CDC explained.
Data from clinical laboratories show that, despite the increased activity, fewer respiratory specimens tested positive for influenza: 15.3% for the week of March 8-14, compared with 21.1% the week before, the CDC’s influenza division said in its latest FluView report.
Influenza activity also increased slightly among the states, with 35 states and Puerto Rico at the highest level on the CDC’s 1-10 scale, versus 34 states and Puerto Rico the previous week. The count was down to 33 for the last week of February, CDC data show.
Severity measures remain mixed as overall hospitalization continues to be moderate but rates for children aged 0-4 years and adults aged 18-49 years are the highest on record and rates for children aged 5-17 years are the highest since the 2009 pandemic, the influenza division said.
Mortality data present a similar picture: The overall death rate is low, but the 149 flu-related deaths reported among children is the most for this point of the season since 2009, the CDC said.
The viral tsunami that is COVID-19 has hit the United States, and influenza appears to be riding the crest of the wave.
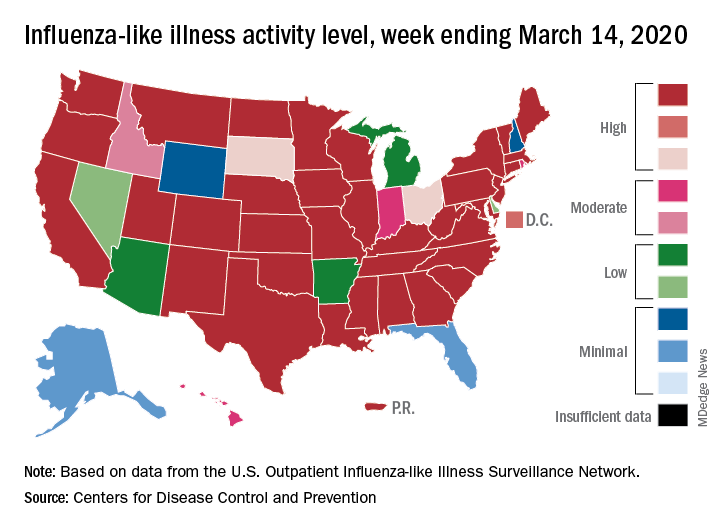
according to the Centers for Disease Control. Flu-related visits went from 5.2% of all outpatient visits the week before to 5.8% during the week ending March 14.
“The COVID-19 outbreak unfolding in the United States may affect healthcare seeking behavior which in turn would impact data from” the U.S. Outpatient Influenza-like Illness Surveillance Network, the CDC explained.
Data from clinical laboratories show that, despite the increased activity, fewer respiratory specimens tested positive for influenza: 15.3% for the week of March 8-14, compared with 21.1% the week before, the CDC’s influenza division said in its latest FluView report.
Influenza activity also increased slightly among the states, with 35 states and Puerto Rico at the highest level on the CDC’s 1-10 scale, versus 34 states and Puerto Rico the previous week. The count was down to 33 for the last week of February, CDC data show.
Severity measures remain mixed as overall hospitalization continues to be moderate but rates for children aged 0-4 years and adults aged 18-49 years are the highest on record and rates for children aged 5-17 years are the highest since the 2009 pandemic, the influenza division said.
Mortality data present a similar picture: The overall death rate is low, but the 149 flu-related deaths reported among children is the most for this point of the season since 2009, the CDC said.
Expansion of the donor pool in lung transplantation
Lung transplants are increasing, with 2,562 performed in the United States in 2018 – a 31% increase over the preceding 5 years. With this increased demand for donor lungs, waitlist mortality in the United States is 9.4 deaths per 100 waitlist-years for obstructive lung diseases and as high as 29.7 deaths per 100 waitlist-years for restrictive lung diseases (Valapour M, et al. Lung. Am J Transplant. 2020;20[suppl s1]:427). Conversely, lungs are utilized from eligible multiorgan donors only 15% to 20% of the time, usually due to concerns over donor history or organ quality (Young KA, et al. Chest. 2019;155[3]:465). In light of this imbalance of supply and demand, lung transplant specialists are making significant efforts to expand the donor pool of available organs. Three of these strategies include: (1) applications of ex-vivo lung perfusion (EVLP) technology; (2) use of lungs from hepatitis C-positive donors for hep-C negative recipients; and (3) increasing utilization of donation after cardiac death.
Normothermic ex-vivo lung perfusion is a technology which allows donor lungs to be perfused and ventilated after removal from the donor but before transplant into the recipient. This is in contrast to the traditional method of cold static preservation. The proposed advantage of using this technology is to allow time for a more thorough assessment of graft quality and to improve function of grafts not meeting established criteria for transplant, all-the-while decreasing organ ischemia despite an increased cross-clamp time. There are currently four commercial systems available capable of EVLP. Broadly speaking, three EVLP management protocols exist (Toronto, Lund, and OCS), which differ in perfusate composition, target flow, pulmonary arterial pressure, left atrial pressure, and ventilatory settings. Notably, the Toronto protocol uses a closed left atrium, whereas the Lund and OCS protocol use an open left atrium. There are excellent published reviews of the different systems (Possoz J, et al. J Thorac Dis. 2019;11[4]:1635). EVLP has now been studied for two different goals: (1) to allow an extended evaluation of lungs of questionable quality before transplant; or (2) for routine use in all lung transplantations in place of cold static preservation.
In most studies concerning the use of EVLP for reconditioning of donor lungs, “high risk” or “extended criteria” refers to one or more of the following: P/F ratios < 300 on arterial blood gas, macroscopic abnormalities (eg, pulmonary edema, poor lung compliance), donation after circulatory death, or high-risk history (eg, aspiration). The largest cohort with the longest follow-up addressing the role of EVLP for donation of lungs with extended criteria was published from the Toronto Lung Transplant Group. Their results have demonstrated equivalent graft survival and rates of chronic lung allograft dysfunction (CLAD) up to 9 years posttransplant compared with standard criteria donor lungs, despite utilizing lower quality lungs and having a longer median preservation (Divithotawela C, et al. JAMA Surg. 2019;154[12]:1143). The group’s subsequent lung transplant rates have increased over the past decade.
A separate study addressed the same question but differed in that it was a single-arm, multicenter, international trial that tracked the outcomes of 93 extended criteria lungs placed on EVLP (including a large proportion acquired via donation after circulatory death) (Loor G, et al. Lancet Respir Med. 2019;7[11]:975). Among these, 87% of eligible lungs were transplanted, and outcomes were excellent, albeit shorter in follow-up compared with the Toronto cohort (eg, primary graft dysfunction grade 3 (PGD3) within 72 hours was 44% and 1-year survival was 91%). Based on these trials and many other retrospective reports, it has been concluded by many experts in the field that EVLP-treated extended criteria donor lungs perform equally well to standard criteria donor lungs.
Two RCTs have been conducted to evaluate whether EVLP is noninferior to static cold storage with donor lungs meeting “standard criteria” for transplant. The first was a single center study at the Medical University of Vienna, that looked at 80 recipient/donor pairs. Lungs in the EVLP arm underwent 4 hours of perfusion with frequent reassessment of quality before transplant, whereas the lungs in the control arm went directly to transplant. This study met noninferiority criteria looking at primary outcomes of PGD grade >1 and 30-day survival (Slama A, et al. J Heart Lung Transplant. 2017;36[7]:744). The second study was a phase 3, multicenter, international trial that included 320 recipient/donor pairs randomized to either EVLP (without a prespecified time on the EVLP system) or static cold storage. This trial met noninferiority for safety endpoints (lung graft-related adverse events within 30 days) and a composite primary outcome of PGD grade 3 incidence within 72 hours and 30-day survival (Warnecke G, et al. Lancet Respir Med. 2018;6[5]:357). The authors also tested and found superiority of EVLP in lower PGD grade 3 frequency compared with control. While these RCTs may suggest a role for EVLP in the procurement process of standard criteria organs in addition to extended criteria organs in the future, major criticisms for these trials include the lack of a demonstrable clinical benefit over cold storage beyond the lower PGD3 rates.
In the era of direct-acting antiviral agents available to treat HCV infection, there has been efforts to study the early use of anti-HCV medications to prevent infection as a result of heart or lung transplant from HCV viremic donors to HCV-negative recipients. In one major trial on efficacy, it was found that 4 weeks of sofosbuvir and velpatasvir, when started within a few hours of transplant, was sufficient to achieve a sustained (undetectable) virologic response at 12 weeks after completion of the antiviral regimen (Woolley AE, et al. N Engl J Med. 2019;380[17]:1606). Therefore, many transplant centers have adopted protocols to increase the donor pool (by CDC estimates about 4% of solid organ donors are HCV-positive) by accepting HCV nucleic acid amplification test (NAT)-positive donors for HCV-negative recipients, after appropriate informed consent.
Donation after cardiac death (DCD), which is alternatively known as donation after circulatory determination of death (DCDD), generally refers to organ procurement taking place after cessation of circulation, often after inpatient withdrawal of support. This is in contrast to the much more common practice of donation after brain death (DBD). Addressing concerns over the quality of lungs donated in the context of DCD compared with DBD, analyses of ISHLT registry data have demonstrated no differences in hospital length of stay or survival at 1 or 5 years (Van Raemdonck D, et al. J Heart Lung Transplant. 2019;38[12]:1235). Outcomes comparing specific mechanisms of donor death in DCD remain relatively unknown, such as outcomes from donors withdrawn from life support vs donors who had an uncontrolled cardiac death.
These methods for expanding the donor pool are not mutually exclusive, and, in fact, application of EVLP for lungs obtained in the context of DCD seems to be increasingly common. Optimization of protocols with collaboration between lung transplant centers will be paramount as we move forward in advancing this field. As we do so, efforts to successfully increase the donor pool will serve to provide a life-saving therapy to an ever-growing number of patients with end-stage lung disease.
Dr. Sala and Dr. Tomic are with the Division of Pulmonary and Critical Care Medicine, Northwestern University, Chicago, Illinois.
Lung transplants are increasing, with 2,562 performed in the United States in 2018 – a 31% increase over the preceding 5 years. With this increased demand for donor lungs, waitlist mortality in the United States is 9.4 deaths per 100 waitlist-years for obstructive lung diseases and as high as 29.7 deaths per 100 waitlist-years for restrictive lung diseases (Valapour M, et al. Lung. Am J Transplant. 2020;20[suppl s1]:427). Conversely, lungs are utilized from eligible multiorgan donors only 15% to 20% of the time, usually due to concerns over donor history or organ quality (Young KA, et al. Chest. 2019;155[3]:465). In light of this imbalance of supply and demand, lung transplant specialists are making significant efforts to expand the donor pool of available organs. Three of these strategies include: (1) applications of ex-vivo lung perfusion (EVLP) technology; (2) use of lungs from hepatitis C-positive donors for hep-C negative recipients; and (3) increasing utilization of donation after cardiac death.
Normothermic ex-vivo lung perfusion is a technology which allows donor lungs to be perfused and ventilated after removal from the donor but before transplant into the recipient. This is in contrast to the traditional method of cold static preservation. The proposed advantage of using this technology is to allow time for a more thorough assessment of graft quality and to improve function of grafts not meeting established criteria for transplant, all-the-while decreasing organ ischemia despite an increased cross-clamp time. There are currently four commercial systems available capable of EVLP. Broadly speaking, three EVLP management protocols exist (Toronto, Lund, and OCS), which differ in perfusate composition, target flow, pulmonary arterial pressure, left atrial pressure, and ventilatory settings. Notably, the Toronto protocol uses a closed left atrium, whereas the Lund and OCS protocol use an open left atrium. There are excellent published reviews of the different systems (Possoz J, et al. J Thorac Dis. 2019;11[4]:1635). EVLP has now been studied for two different goals: (1) to allow an extended evaluation of lungs of questionable quality before transplant; or (2) for routine use in all lung transplantations in place of cold static preservation.
In most studies concerning the use of EVLP for reconditioning of donor lungs, “high risk” or “extended criteria” refers to one or more of the following: P/F ratios < 300 on arterial blood gas, macroscopic abnormalities (eg, pulmonary edema, poor lung compliance), donation after circulatory death, or high-risk history (eg, aspiration). The largest cohort with the longest follow-up addressing the role of EVLP for donation of lungs with extended criteria was published from the Toronto Lung Transplant Group. Their results have demonstrated equivalent graft survival and rates of chronic lung allograft dysfunction (CLAD) up to 9 years posttransplant compared with standard criteria donor lungs, despite utilizing lower quality lungs and having a longer median preservation (Divithotawela C, et al. JAMA Surg. 2019;154[12]:1143). The group’s subsequent lung transplant rates have increased over the past decade.
A separate study addressed the same question but differed in that it was a single-arm, multicenter, international trial that tracked the outcomes of 93 extended criteria lungs placed on EVLP (including a large proportion acquired via donation after circulatory death) (Loor G, et al. Lancet Respir Med. 2019;7[11]:975). Among these, 87% of eligible lungs were transplanted, and outcomes were excellent, albeit shorter in follow-up compared with the Toronto cohort (eg, primary graft dysfunction grade 3 (PGD3) within 72 hours was 44% and 1-year survival was 91%). Based on these trials and many other retrospective reports, it has been concluded by many experts in the field that EVLP-treated extended criteria donor lungs perform equally well to standard criteria donor lungs.
Two RCTs have been conducted to evaluate whether EVLP is noninferior to static cold storage with donor lungs meeting “standard criteria” for transplant. The first was a single center study at the Medical University of Vienna, that looked at 80 recipient/donor pairs. Lungs in the EVLP arm underwent 4 hours of perfusion with frequent reassessment of quality before transplant, whereas the lungs in the control arm went directly to transplant. This study met noninferiority criteria looking at primary outcomes of PGD grade >1 and 30-day survival (Slama A, et al. J Heart Lung Transplant. 2017;36[7]:744). The second study was a phase 3, multicenter, international trial that included 320 recipient/donor pairs randomized to either EVLP (without a prespecified time on the EVLP system) or static cold storage. This trial met noninferiority for safety endpoints (lung graft-related adverse events within 30 days) and a composite primary outcome of PGD grade 3 incidence within 72 hours and 30-day survival (Warnecke G, et al. Lancet Respir Med. 2018;6[5]:357). The authors also tested and found superiority of EVLP in lower PGD grade 3 frequency compared with control. While these RCTs may suggest a role for EVLP in the procurement process of standard criteria organs in addition to extended criteria organs in the future, major criticisms for these trials include the lack of a demonstrable clinical benefit over cold storage beyond the lower PGD3 rates.
In the era of direct-acting antiviral agents available to treat HCV infection, there has been efforts to study the early use of anti-HCV medications to prevent infection as a result of heart or lung transplant from HCV viremic donors to HCV-negative recipients. In one major trial on efficacy, it was found that 4 weeks of sofosbuvir and velpatasvir, when started within a few hours of transplant, was sufficient to achieve a sustained (undetectable) virologic response at 12 weeks after completion of the antiviral regimen (Woolley AE, et al. N Engl J Med. 2019;380[17]:1606). Therefore, many transplant centers have adopted protocols to increase the donor pool (by CDC estimates about 4% of solid organ donors are HCV-positive) by accepting HCV nucleic acid amplification test (NAT)-positive donors for HCV-negative recipients, after appropriate informed consent.
Donation after cardiac death (DCD), which is alternatively known as donation after circulatory determination of death (DCDD), generally refers to organ procurement taking place after cessation of circulation, often after inpatient withdrawal of support. This is in contrast to the much more common practice of donation after brain death (DBD). Addressing concerns over the quality of lungs donated in the context of DCD compared with DBD, analyses of ISHLT registry data have demonstrated no differences in hospital length of stay or survival at 1 or 5 years (Van Raemdonck D, et al. J Heart Lung Transplant. 2019;38[12]:1235). Outcomes comparing specific mechanisms of donor death in DCD remain relatively unknown, such as outcomes from donors withdrawn from life support vs donors who had an uncontrolled cardiac death.
These methods for expanding the donor pool are not mutually exclusive, and, in fact, application of EVLP for lungs obtained in the context of DCD seems to be increasingly common. Optimization of protocols with collaboration between lung transplant centers will be paramount as we move forward in advancing this field. As we do so, efforts to successfully increase the donor pool will serve to provide a life-saving therapy to an ever-growing number of patients with end-stage lung disease.
Dr. Sala and Dr. Tomic are with the Division of Pulmonary and Critical Care Medicine, Northwestern University, Chicago, Illinois.
Lung transplants are increasing, with 2,562 performed in the United States in 2018 – a 31% increase over the preceding 5 years. With this increased demand for donor lungs, waitlist mortality in the United States is 9.4 deaths per 100 waitlist-years for obstructive lung diseases and as high as 29.7 deaths per 100 waitlist-years for restrictive lung diseases (Valapour M, et al. Lung. Am J Transplant. 2020;20[suppl s1]:427). Conversely, lungs are utilized from eligible multiorgan donors only 15% to 20% of the time, usually due to concerns over donor history or organ quality (Young KA, et al. Chest. 2019;155[3]:465). In light of this imbalance of supply and demand, lung transplant specialists are making significant efforts to expand the donor pool of available organs. Three of these strategies include: (1) applications of ex-vivo lung perfusion (EVLP) technology; (2) use of lungs from hepatitis C-positive donors for hep-C negative recipients; and (3) increasing utilization of donation after cardiac death.
Normothermic ex-vivo lung perfusion is a technology which allows donor lungs to be perfused and ventilated after removal from the donor but before transplant into the recipient. This is in contrast to the traditional method of cold static preservation. The proposed advantage of using this technology is to allow time for a more thorough assessment of graft quality and to improve function of grafts not meeting established criteria for transplant, all-the-while decreasing organ ischemia despite an increased cross-clamp time. There are currently four commercial systems available capable of EVLP. Broadly speaking, three EVLP management protocols exist (Toronto, Lund, and OCS), which differ in perfusate composition, target flow, pulmonary arterial pressure, left atrial pressure, and ventilatory settings. Notably, the Toronto protocol uses a closed left atrium, whereas the Lund and OCS protocol use an open left atrium. There are excellent published reviews of the different systems (Possoz J, et al. J Thorac Dis. 2019;11[4]:1635). EVLP has now been studied for two different goals: (1) to allow an extended evaluation of lungs of questionable quality before transplant; or (2) for routine use in all lung transplantations in place of cold static preservation.
In most studies concerning the use of EVLP for reconditioning of donor lungs, “high risk” or “extended criteria” refers to one or more of the following: P/F ratios < 300 on arterial blood gas, macroscopic abnormalities (eg, pulmonary edema, poor lung compliance), donation after circulatory death, or high-risk history (eg, aspiration). The largest cohort with the longest follow-up addressing the role of EVLP for donation of lungs with extended criteria was published from the Toronto Lung Transplant Group. Their results have demonstrated equivalent graft survival and rates of chronic lung allograft dysfunction (CLAD) up to 9 years posttransplant compared with standard criteria donor lungs, despite utilizing lower quality lungs and having a longer median preservation (Divithotawela C, et al. JAMA Surg. 2019;154[12]:1143). The group’s subsequent lung transplant rates have increased over the past decade.
A separate study addressed the same question but differed in that it was a single-arm, multicenter, international trial that tracked the outcomes of 93 extended criteria lungs placed on EVLP (including a large proportion acquired via donation after circulatory death) (Loor G, et al. Lancet Respir Med. 2019;7[11]:975). Among these, 87% of eligible lungs were transplanted, and outcomes were excellent, albeit shorter in follow-up compared with the Toronto cohort (eg, primary graft dysfunction grade 3 (PGD3) within 72 hours was 44% and 1-year survival was 91%). Based on these trials and many other retrospective reports, it has been concluded by many experts in the field that EVLP-treated extended criteria donor lungs perform equally well to standard criteria donor lungs.
Two RCTs have been conducted to evaluate whether EVLP is noninferior to static cold storage with donor lungs meeting “standard criteria” for transplant. The first was a single center study at the Medical University of Vienna, that looked at 80 recipient/donor pairs. Lungs in the EVLP arm underwent 4 hours of perfusion with frequent reassessment of quality before transplant, whereas the lungs in the control arm went directly to transplant. This study met noninferiority criteria looking at primary outcomes of PGD grade >1 and 30-day survival (Slama A, et al. J Heart Lung Transplant. 2017;36[7]:744). The second study was a phase 3, multicenter, international trial that included 320 recipient/donor pairs randomized to either EVLP (without a prespecified time on the EVLP system) or static cold storage. This trial met noninferiority for safety endpoints (lung graft-related adverse events within 30 days) and a composite primary outcome of PGD grade 3 incidence within 72 hours and 30-day survival (Warnecke G, et al. Lancet Respir Med. 2018;6[5]:357). The authors also tested and found superiority of EVLP in lower PGD grade 3 frequency compared with control. While these RCTs may suggest a role for EVLP in the procurement process of standard criteria organs in addition to extended criteria organs in the future, major criticisms for these trials include the lack of a demonstrable clinical benefit over cold storage beyond the lower PGD3 rates.
In the era of direct-acting antiviral agents available to treat HCV infection, there has been efforts to study the early use of anti-HCV medications to prevent infection as a result of heart or lung transplant from HCV viremic donors to HCV-negative recipients. In one major trial on efficacy, it was found that 4 weeks of sofosbuvir and velpatasvir, when started within a few hours of transplant, was sufficient to achieve a sustained (undetectable) virologic response at 12 weeks after completion of the antiviral regimen (Woolley AE, et al. N Engl J Med. 2019;380[17]:1606). Therefore, many transplant centers have adopted protocols to increase the donor pool (by CDC estimates about 4% of solid organ donors are HCV-positive) by accepting HCV nucleic acid amplification test (NAT)-positive donors for HCV-negative recipients, after appropriate informed consent.
Donation after cardiac death (DCD), which is alternatively known as donation after circulatory determination of death (DCDD), generally refers to organ procurement taking place after cessation of circulation, often after inpatient withdrawal of support. This is in contrast to the much more common practice of donation after brain death (DBD). Addressing concerns over the quality of lungs donated in the context of DCD compared with DBD, analyses of ISHLT registry data have demonstrated no differences in hospital length of stay or survival at 1 or 5 years (Van Raemdonck D, et al. J Heart Lung Transplant. 2019;38[12]:1235). Outcomes comparing specific mechanisms of donor death in DCD remain relatively unknown, such as outcomes from donors withdrawn from life support vs donors who had an uncontrolled cardiac death.
These methods for expanding the donor pool are not mutually exclusive, and, in fact, application of EVLP for lungs obtained in the context of DCD seems to be increasingly common. Optimization of protocols with collaboration between lung transplant centers will be paramount as we move forward in advancing this field. As we do so, efforts to successfully increase the donor pool will serve to provide a life-saving therapy to an ever-growing number of patients with end-stage lung disease.
Dr. Sala and Dr. Tomic are with the Division of Pulmonary and Critical Care Medicine, Northwestern University, Chicago, Illinois.
What to know about CFTR modulator therapy for cystic fibrosis
Cystic fibrosis transmembrane conductance regulator modulators are bringing new hope to many patients with CF. But what do physicians and patients need to know about the latest CFTR modulator therapies?
Susan M. Millard, MD, is a pediatric pulmonologist at Helen DeVos Children's Hospital in Grand Rapids, Mich. In an audio interview, Dr. Millard discusses the new Food and Drug Administration-approved combination therapy of elexacaftor, tezacaftor, and ivacaftor (Trikafta). It's a trio that could make a significant difference for the roughly 90% of patients with at least one F508del mutation.
Dr. Millard outlines which patients are candidates for the combination therapy, what physicians and patients can expect with Trikafta use, and how the drug affects patients' use of other CF therapies. She also explains the steps physicians should take before starting patients on the therapy, and what side effects to watch for during treatment.
Dr. Millard is the local principal investigator for CF research at Helen DeVos Children’s Hospital, including Mylan, Therapeutic Development Network, and Vertex clinical studies.
Cystic fibrosis transmembrane conductance regulator modulators are bringing new hope to many patients with CF. But what do physicians and patients need to know about the latest CFTR modulator therapies?
Susan M. Millard, MD, is a pediatric pulmonologist at Helen DeVos Children's Hospital in Grand Rapids, Mich. In an audio interview, Dr. Millard discusses the new Food and Drug Administration-approved combination therapy of elexacaftor, tezacaftor, and ivacaftor (Trikafta). It's a trio that could make a significant difference for the roughly 90% of patients with at least one F508del mutation.
Dr. Millard outlines which patients are candidates for the combination therapy, what physicians and patients can expect with Trikafta use, and how the drug affects patients' use of other CF therapies. She also explains the steps physicians should take before starting patients on the therapy, and what side effects to watch for during treatment.
Dr. Millard is the local principal investigator for CF research at Helen DeVos Children’s Hospital, including Mylan, Therapeutic Development Network, and Vertex clinical studies.
Cystic fibrosis transmembrane conductance regulator modulators are bringing new hope to many patients with CF. But what do physicians and patients need to know about the latest CFTR modulator therapies?
Susan M. Millard, MD, is a pediatric pulmonologist at Helen DeVos Children's Hospital in Grand Rapids, Mich. In an audio interview, Dr. Millard discusses the new Food and Drug Administration-approved combination therapy of elexacaftor, tezacaftor, and ivacaftor (Trikafta). It's a trio that could make a significant difference for the roughly 90% of patients with at least one F508del mutation.
Dr. Millard outlines which patients are candidates for the combination therapy, what physicians and patients can expect with Trikafta use, and how the drug affects patients' use of other CF therapies. She also explains the steps physicians should take before starting patients on the therapy, and what side effects to watch for during treatment.
Dr. Millard is the local principal investigator for CF research at Helen DeVos Children’s Hospital, including Mylan, Therapeutic Development Network, and Vertex clinical studies.












