User login
Short Takes
Pharmacist-led intervention reduced inappropriate medication prescriptions
An outpatient pharmacy-led intervention of notifying prescribing physicians to discontinue inappropriate Beers Criteria medications resulted in a greater discontinuation of inappropriate medications for older adults at 6 months, compared with the control group (43% vs. 12% discontinuation).
Citation: Martin P et al. Effect of a pharmacist-led educational intervention on inappropriate medication prescriptions in older adults: The D-PRESCRIBE randomized clinical trial. JAMA. 2018;320(18):1889-98.
Omadacycline noninferior for community-acquired pneumonia and acute bacterial soft tissue skin infections
Randomized, double-blind, double-dummy trials showed omadacycline is a noninferior alternative to moxifloxacin for the treatment of community-acquired pneumonia and to linezolid for acute bacterial soft-tissue skin infections.
Citation: Nuzyra (omadacycline) [package insert]. Boston, MA: Paratek Pharmaceuticals. 2018.
Lack of evidence to support low-salt diet in adult heart failure patients
Systematic review of multiple databases demonstrated there is limited high-quality evidence to support current guidelines that recommend a low-salt diet to heart failure patients.
Citation: Mahtani KR et al. Reduced salt intake for heart failure: A systematic review. JAMA Int Med. 2018;178(12):1693-700.
Magnesium for rate control in rapid atrial fibrillation
Randomized, controlled trial demonstrated that intravenous magnesium sulfate in combination with atrioventricular (AV) nodal blocking agents resulted in better rate control for atrial fibrillation with rapid ventricular response than did placebo given in combination with AV nodal blocking agents.
Citation: Bouida W et al. Low-dose magnesium sulfate versus high-dose in the early management of rapid atrial fibrillation: Randomized controlled double-blind study (LOMAGHI Study). Acad Emerg Med. 2019 Feb;26(2):183-91.
Low versus intermediate tidal volume strategy on ventilator-free days in ICU patients without ARDS
Randomized, clinical trial of low tidal volume versus intermediate tidal volume strategies in invasively ventilated patients without accute respiratory distress syndrome (ARDS) demonstrated no difference in number of ventilator-free days, ICU length of stay, hospital length of stay, incidence of ventilator-associated adverse events (ARDS, pneumonia, severe atelectasis, pneumothorax), or 28-day mortality.
Citation: Writing Group for the PReVENT Investigators, Simonis FD, Serpa Neto A. Effect of a low vs intermediate tidal volume strategy on ventilator-free days in intensive care unit patients without ARDS: A randomized clinical trial. JAMA. 2018;320(18):1872-80.
Pharmacist-led intervention reduced inappropriate medication prescriptions
An outpatient pharmacy-led intervention of notifying prescribing physicians to discontinue inappropriate Beers Criteria medications resulted in a greater discontinuation of inappropriate medications for older adults at 6 months, compared with the control group (43% vs. 12% discontinuation).
Citation: Martin P et al. Effect of a pharmacist-led educational intervention on inappropriate medication prescriptions in older adults: The D-PRESCRIBE randomized clinical trial. JAMA. 2018;320(18):1889-98.
Omadacycline noninferior for community-acquired pneumonia and acute bacterial soft tissue skin infections
Randomized, double-blind, double-dummy trials showed omadacycline is a noninferior alternative to moxifloxacin for the treatment of community-acquired pneumonia and to linezolid for acute bacterial soft-tissue skin infections.
Citation: Nuzyra (omadacycline) [package insert]. Boston, MA: Paratek Pharmaceuticals. 2018.
Lack of evidence to support low-salt diet in adult heart failure patients
Systematic review of multiple databases demonstrated there is limited high-quality evidence to support current guidelines that recommend a low-salt diet to heart failure patients.
Citation: Mahtani KR et al. Reduced salt intake for heart failure: A systematic review. JAMA Int Med. 2018;178(12):1693-700.
Magnesium for rate control in rapid atrial fibrillation
Randomized, controlled trial demonstrated that intravenous magnesium sulfate in combination with atrioventricular (AV) nodal blocking agents resulted in better rate control for atrial fibrillation with rapid ventricular response than did placebo given in combination with AV nodal blocking agents.
Citation: Bouida W et al. Low-dose magnesium sulfate versus high-dose in the early management of rapid atrial fibrillation: Randomized controlled double-blind study (LOMAGHI Study). Acad Emerg Med. 2019 Feb;26(2):183-91.
Low versus intermediate tidal volume strategy on ventilator-free days in ICU patients without ARDS
Randomized, clinical trial of low tidal volume versus intermediate tidal volume strategies in invasively ventilated patients without accute respiratory distress syndrome (ARDS) demonstrated no difference in number of ventilator-free days, ICU length of stay, hospital length of stay, incidence of ventilator-associated adverse events (ARDS, pneumonia, severe atelectasis, pneumothorax), or 28-day mortality.
Citation: Writing Group for the PReVENT Investigators, Simonis FD, Serpa Neto A. Effect of a low vs intermediate tidal volume strategy on ventilator-free days in intensive care unit patients without ARDS: A randomized clinical trial. JAMA. 2018;320(18):1872-80.
Pharmacist-led intervention reduced inappropriate medication prescriptions
An outpatient pharmacy-led intervention of notifying prescribing physicians to discontinue inappropriate Beers Criteria medications resulted in a greater discontinuation of inappropriate medications for older adults at 6 months, compared with the control group (43% vs. 12% discontinuation).
Citation: Martin P et al. Effect of a pharmacist-led educational intervention on inappropriate medication prescriptions in older adults: The D-PRESCRIBE randomized clinical trial. JAMA. 2018;320(18):1889-98.
Omadacycline noninferior for community-acquired pneumonia and acute bacterial soft tissue skin infections
Randomized, double-blind, double-dummy trials showed omadacycline is a noninferior alternative to moxifloxacin for the treatment of community-acquired pneumonia and to linezolid for acute bacterial soft-tissue skin infections.
Citation: Nuzyra (omadacycline) [package insert]. Boston, MA: Paratek Pharmaceuticals. 2018.
Lack of evidence to support low-salt diet in adult heart failure patients
Systematic review of multiple databases demonstrated there is limited high-quality evidence to support current guidelines that recommend a low-salt diet to heart failure patients.
Citation: Mahtani KR et al. Reduced salt intake for heart failure: A systematic review. JAMA Int Med. 2018;178(12):1693-700.
Magnesium for rate control in rapid atrial fibrillation
Randomized, controlled trial demonstrated that intravenous magnesium sulfate in combination with atrioventricular (AV) nodal blocking agents resulted in better rate control for atrial fibrillation with rapid ventricular response than did placebo given in combination with AV nodal blocking agents.
Citation: Bouida W et al. Low-dose magnesium sulfate versus high-dose in the early management of rapid atrial fibrillation: Randomized controlled double-blind study (LOMAGHI Study). Acad Emerg Med. 2019 Feb;26(2):183-91.
Low versus intermediate tidal volume strategy on ventilator-free days in ICU patients without ARDS
Randomized, clinical trial of low tidal volume versus intermediate tidal volume strategies in invasively ventilated patients without accute respiratory distress syndrome (ARDS) demonstrated no difference in number of ventilator-free days, ICU length of stay, hospital length of stay, incidence of ventilator-associated adverse events (ARDS, pneumonia, severe atelectasis, pneumothorax), or 28-day mortality.
Citation: Writing Group for the PReVENT Investigators, Simonis FD, Serpa Neto A. Effect of a low vs intermediate tidal volume strategy on ventilator-free days in intensive care unit patients without ARDS: A randomized clinical trial. JAMA. 2018;320(18):1872-80.
Educating teens, young adults about dangers of vaping
Physicians have been alarmed about the vaping craze for quite some time. This alarm has grown louder in the wake of news that electronic cigarettes have been associated with a mysterious lung disease.
Public health officials have reported that there have been 530 cases of vaping-related respiratory disease,1 and as of press time at least seven deaths had been attributed to vaping*. On Sept. 6, 2019, the Food and Drug Administration, Centers for Disease Control and Prevention, and other health officials issued an investigation notice on vaping and e-cigarettes,2 cautioning teenagers, young adults, and pregnant women to avoid e-cigarettes completely and cautioning all users to never buy e-cigarettes off the street or from social sources.
A few days later, on Sept. 9, the FDA’s Center for Tobacco Products issued a warning letter to JUUL Labs, makers of a popular e-cigarette, for illegal marketing of modified-risk tobacco products.3 Then on Sept. 10, health officials in Kansas reported that a sixth person has died of a lung illness related to vaping.4
Researchers have found that 80% of those diagnosed with the vaping illness used products that contained THC, the psychoactive ingredient in marijuana, 61% had used nicotine products, and 7% used cannabidiol (CBD) products. Vitamin E acetate is another substance identified in press reports as tied to the severe lung disease.
Most of the patients affected are adolescents and young adults, with the average age of 19 years.5 This comes as vaping among high school students rose 78% between 2017 and 2018.6 According the U.S. surgeon general, one in five teens vapes. Other data show that teen use of e-cigarettes comes with most users having never smoked a traditional cigarette.7 Teens and young adults frequently borrow buy* e-cigarette “pods” from gas stations but borrow and purchase from friends or peers. In addition, young people are known to alter the pods to insert other liquids, such as CBD and other marijuana products.
Teens and young adults are at higher risk for vaping complications. Their respiratory and immune systems are still developing. In addition to concerns about the recent surge of respiratory illnesses, nicotine is known to also suppress the immune system, which makes people who use it more susceptible to viral and bacterial infections – and also making it harder for them to recover.
In addition nicotine hyperactivates the reward centers of the brain, which can trigger addictive behaviors. Because the brains of young adults are not yet fully developed until at or after age 26, nicotine use before this can “prime the pump” of a still-developing brain, thereby increasing the likelihood for addiction to harder drugs. Nicotine has been shown to disrupt sleep patterns, which are critical for mental and physical health. Lastly, research shows that smoking increases the risks of various psychiatric disorders, such as depression and anxiety. My teen and young adult patients have endlessly debated with me the idea that smoking – either nicotine or marijuana – eases their anxiety or helps them get to sleep. I tell them that, in the long run, the data show that smoking makes those problems worse.8-11
Nationally, we are seeing an explosion of multistate legislation pushing marijuana as a health food. E-cigarettes have followed as the “healthy” alternative to traditional tobacco. As clinicians, we must counter those messages.
Finally, our world is now filled with smartphones, sexting, and social media overuse. An entire peer group exists that knows life only with constant electronic stimulation. It is not without irony that our national nicotine obsessions have morphed from paper cigarettes to electronic versions. This raises questions: Are teens and young adults using e-cigarettes because of boredom? Are we witnessing a generational ADHD borne from restlessness that stems from lives with fewer meaningful face-to-face human interactions?
In addition to educating our teens and young adults about the physical risks tied to vaping, we need to teach them to build meaning into their lives that exists outside of this digital age.
Dr. Jorandby is chief medical officer of Lakeview Health in Jacksonville, Fla. She trained in addiction psychiatry at Yale University, New Haven, Conn.
References
1. CDC. Outbreak of lung injury associated with e-cigarette use, or vaping. 2019 Sep 19.
2. CDC. Outbreak of lung illness associated with using e-cigarette products. Investigation notice. 2019 Sep 6.
3. FDA. Warning letter, JUUL Labs. 2019 Sep 9.
4. Sixth person dies of vaping-related illness. The Hill. 2019 Sep 10.
5. Layden JE. Pulmonary illness related to cigarette use in Illinois and Wisconsin – preliminary report. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMoa1911614.
6. Cullen KA et al. CDC. MMWR. 2018 Nov 16;67(45):1276-7.
7. National Academies of Sciences, Engineering, and Medicine. Public health consequences of e-cigarettes. 2018.
8. Patton GC et al. Am J Public Health. 1996 Feb;86(2):225-30.
9. Leventhal AM et al. J Psychiatr Res. 2016 Feb;73:71-8.
10. Levine A et al. J Am Acad Child Adolesc Psychiatry. 2017 Mar;56(3):214-2.
11. Leadbeater BJ et al. Addiction. 2019 Feb;114(2):278-93.
* This column was updated 9/24/2019.
Physicians have been alarmed about the vaping craze for quite some time. This alarm has grown louder in the wake of news that electronic cigarettes have been associated with a mysterious lung disease.
Public health officials have reported that there have been 530 cases of vaping-related respiratory disease,1 and as of press time at least seven deaths had been attributed to vaping*. On Sept. 6, 2019, the Food and Drug Administration, Centers for Disease Control and Prevention, and other health officials issued an investigation notice on vaping and e-cigarettes,2 cautioning teenagers, young adults, and pregnant women to avoid e-cigarettes completely and cautioning all users to never buy e-cigarettes off the street or from social sources.
A few days later, on Sept. 9, the FDA’s Center for Tobacco Products issued a warning letter to JUUL Labs, makers of a popular e-cigarette, for illegal marketing of modified-risk tobacco products.3 Then on Sept. 10, health officials in Kansas reported that a sixth person has died of a lung illness related to vaping.4
Researchers have found that 80% of those diagnosed with the vaping illness used products that contained THC, the psychoactive ingredient in marijuana, 61% had used nicotine products, and 7% used cannabidiol (CBD) products. Vitamin E acetate is another substance identified in press reports as tied to the severe lung disease.
Most of the patients affected are adolescents and young adults, with the average age of 19 years.5 This comes as vaping among high school students rose 78% between 2017 and 2018.6 According the U.S. surgeon general, one in five teens vapes. Other data show that teen use of e-cigarettes comes with most users having never smoked a traditional cigarette.7 Teens and young adults frequently borrow buy* e-cigarette “pods” from gas stations but borrow and purchase from friends or peers. In addition, young people are known to alter the pods to insert other liquids, such as CBD and other marijuana products.
Teens and young adults are at higher risk for vaping complications. Their respiratory and immune systems are still developing. In addition to concerns about the recent surge of respiratory illnesses, nicotine is known to also suppress the immune system, which makes people who use it more susceptible to viral and bacterial infections – and also making it harder for them to recover.
In addition nicotine hyperactivates the reward centers of the brain, which can trigger addictive behaviors. Because the brains of young adults are not yet fully developed until at or after age 26, nicotine use before this can “prime the pump” of a still-developing brain, thereby increasing the likelihood for addiction to harder drugs. Nicotine has been shown to disrupt sleep patterns, which are critical for mental and physical health. Lastly, research shows that smoking increases the risks of various psychiatric disorders, such as depression and anxiety. My teen and young adult patients have endlessly debated with me the idea that smoking – either nicotine or marijuana – eases their anxiety or helps them get to sleep. I tell them that, in the long run, the data show that smoking makes those problems worse.8-11
Nationally, we are seeing an explosion of multistate legislation pushing marijuana as a health food. E-cigarettes have followed as the “healthy” alternative to traditional tobacco. As clinicians, we must counter those messages.
Finally, our world is now filled with smartphones, sexting, and social media overuse. An entire peer group exists that knows life only with constant electronic stimulation. It is not without irony that our national nicotine obsessions have morphed from paper cigarettes to electronic versions. This raises questions: Are teens and young adults using e-cigarettes because of boredom? Are we witnessing a generational ADHD borne from restlessness that stems from lives with fewer meaningful face-to-face human interactions?
In addition to educating our teens and young adults about the physical risks tied to vaping, we need to teach them to build meaning into their lives that exists outside of this digital age.
Dr. Jorandby is chief medical officer of Lakeview Health in Jacksonville, Fla. She trained in addiction psychiatry at Yale University, New Haven, Conn.
References
1. CDC. Outbreak of lung injury associated with e-cigarette use, or vaping. 2019 Sep 19.
2. CDC. Outbreak of lung illness associated with using e-cigarette products. Investigation notice. 2019 Sep 6.
3. FDA. Warning letter, JUUL Labs. 2019 Sep 9.
4. Sixth person dies of vaping-related illness. The Hill. 2019 Sep 10.
5. Layden JE. Pulmonary illness related to cigarette use in Illinois and Wisconsin – preliminary report. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMoa1911614.
6. Cullen KA et al. CDC. MMWR. 2018 Nov 16;67(45):1276-7.
7. National Academies of Sciences, Engineering, and Medicine. Public health consequences of e-cigarettes. 2018.
8. Patton GC et al. Am J Public Health. 1996 Feb;86(2):225-30.
9. Leventhal AM et al. J Psychiatr Res. 2016 Feb;73:71-8.
10. Levine A et al. J Am Acad Child Adolesc Psychiatry. 2017 Mar;56(3):214-2.
11. Leadbeater BJ et al. Addiction. 2019 Feb;114(2):278-93.
* This column was updated 9/24/2019.
Physicians have been alarmed about the vaping craze for quite some time. This alarm has grown louder in the wake of news that electronic cigarettes have been associated with a mysterious lung disease.
Public health officials have reported that there have been 530 cases of vaping-related respiratory disease,1 and as of press time at least seven deaths had been attributed to vaping*. On Sept. 6, 2019, the Food and Drug Administration, Centers for Disease Control and Prevention, and other health officials issued an investigation notice on vaping and e-cigarettes,2 cautioning teenagers, young adults, and pregnant women to avoid e-cigarettes completely and cautioning all users to never buy e-cigarettes off the street or from social sources.
A few days later, on Sept. 9, the FDA’s Center for Tobacco Products issued a warning letter to JUUL Labs, makers of a popular e-cigarette, for illegal marketing of modified-risk tobacco products.3 Then on Sept. 10, health officials in Kansas reported that a sixth person has died of a lung illness related to vaping.4
Researchers have found that 80% of those diagnosed with the vaping illness used products that contained THC, the psychoactive ingredient in marijuana, 61% had used nicotine products, and 7% used cannabidiol (CBD) products. Vitamin E acetate is another substance identified in press reports as tied to the severe lung disease.
Most of the patients affected are adolescents and young adults, with the average age of 19 years.5 This comes as vaping among high school students rose 78% between 2017 and 2018.6 According the U.S. surgeon general, one in five teens vapes. Other data show that teen use of e-cigarettes comes with most users having never smoked a traditional cigarette.7 Teens and young adults frequently borrow buy* e-cigarette “pods” from gas stations but borrow and purchase from friends or peers. In addition, young people are known to alter the pods to insert other liquids, such as CBD and other marijuana products.
Teens and young adults are at higher risk for vaping complications. Their respiratory and immune systems are still developing. In addition to concerns about the recent surge of respiratory illnesses, nicotine is known to also suppress the immune system, which makes people who use it more susceptible to viral and bacterial infections – and also making it harder for them to recover.
In addition nicotine hyperactivates the reward centers of the brain, which can trigger addictive behaviors. Because the brains of young adults are not yet fully developed until at or after age 26, nicotine use before this can “prime the pump” of a still-developing brain, thereby increasing the likelihood for addiction to harder drugs. Nicotine has been shown to disrupt sleep patterns, which are critical for mental and physical health. Lastly, research shows that smoking increases the risks of various psychiatric disorders, such as depression and anxiety. My teen and young adult patients have endlessly debated with me the idea that smoking – either nicotine or marijuana – eases their anxiety or helps them get to sleep. I tell them that, in the long run, the data show that smoking makes those problems worse.8-11
Nationally, we are seeing an explosion of multistate legislation pushing marijuana as a health food. E-cigarettes have followed as the “healthy” alternative to traditional tobacco. As clinicians, we must counter those messages.
Finally, our world is now filled with smartphones, sexting, and social media overuse. An entire peer group exists that knows life only with constant electronic stimulation. It is not without irony that our national nicotine obsessions have morphed from paper cigarettes to electronic versions. This raises questions: Are teens and young adults using e-cigarettes because of boredom? Are we witnessing a generational ADHD borne from restlessness that stems from lives with fewer meaningful face-to-face human interactions?
In addition to educating our teens and young adults about the physical risks tied to vaping, we need to teach them to build meaning into their lives that exists outside of this digital age.
Dr. Jorandby is chief medical officer of Lakeview Health in Jacksonville, Fla. She trained in addiction psychiatry at Yale University, New Haven, Conn.
References
1. CDC. Outbreak of lung injury associated with e-cigarette use, or vaping. 2019 Sep 19.
2. CDC. Outbreak of lung illness associated with using e-cigarette products. Investigation notice. 2019 Sep 6.
3. FDA. Warning letter, JUUL Labs. 2019 Sep 9.
4. Sixth person dies of vaping-related illness. The Hill. 2019 Sep 10.
5. Layden JE. Pulmonary illness related to cigarette use in Illinois and Wisconsin – preliminary report. N Engl J Med. 2019 Sep 6. doi: 10.1056/NEJMoa1911614.
6. Cullen KA et al. CDC. MMWR. 2018 Nov 16;67(45):1276-7.
7. National Academies of Sciences, Engineering, and Medicine. Public health consequences of e-cigarettes. 2018.
8. Patton GC et al. Am J Public Health. 1996 Feb;86(2):225-30.
9. Leventhal AM et al. J Psychiatr Res. 2016 Feb;73:71-8.
10. Levine A et al. J Am Acad Child Adolesc Psychiatry. 2017 Mar;56(3):214-2.
11. Leadbeater BJ et al. Addiction. 2019 Feb;114(2):278-93.
* This column was updated 9/24/2019.
Trump administration finalizing ban on flavored e-cigarettes
The Food and Drug Administration is finalizing a compliance policy that will target flavored e-cigarettes and aim to clear the market of unauthorized, non–tobacco-flavored e-cigarette products, U.S. Department of Health & Human Services Secretary Alex M. Azar II announced Sept. 11.
“The Trump administration is making it clear that we intend to clear the market of flavored e-cigarettes to reverse the deeply concerning epidemic of youth e-cigarette use that is impacting children, families, schools, and communities,” Mr. Azar said in a statement. “We will not stand idly by as these products become an on-ramp to combustible cigarettes or nicotine addiction for a generation of youth.”
The announcement comes as the Centers for Disease Control and Prevention and state health departments track hundreds of lung-related illnesses that are linked to the use of e-cigarettes. At least 450 cases have been reported in 33 states and one jurisdiction. Diagnoses include lipoid pneumonia, alveolar hemorrhage, and cryptogenic organizing pneumonia, according to a Sept. 6 press briefing by Ileana Arias, PhD, CDC acting deputy director for non-infectious diseases. Six deaths associated with the illnesses have been reported thus far.
Details of new regulatory action will be forthcoming and will outline enforcement policy for non–tobacco-flavored e-cigarette products that lack premarket authorization, HHS officials said. According to federal rules, all electronic nicotine delivery system (ENDS) products must file premarket tobacco product applications with the FDA within 2 years. Many ENDS products currently on the market are not being legally marketed and are subject to government action, according to the Trump administration.
“Once finalized, this compliance policy will serve as a powerful tool that the FDA can use to combat the troubling trend of youth e-cigarette use,” Ned Sharpless, MD, acting FDA commissioner, said in the statement. “We must act swiftly against flavored e-cigarette products that are especially attractive to children. Moreover, if we see a migration to tobacco-flavored products by kids, we will take additional steps to address youth use of these products.”
Federal officials noted that preliminary numbers from the National Youth Tobacco Survey show a continued rise in youth e-cigarette use, with more than a quarter of high school students current e-cigarette users in 2019. The overwhelming majority of youth e-cigarette users cited the use of fruit, menthol, or mint flavors, according to the preliminary data, which have not yet been published.
According to 2018 survey data, e-cigarette use increased from 12% to 21% among high school students and from 3% to 5% among middle school students from 2017 to 2018. There were 1.5 million more youth e-cigarette users in 2018 than in 2017, and youth who were using e-cigarettes were using them more often, according to the survey.
The Food and Drug Administration is finalizing a compliance policy that will target flavored e-cigarettes and aim to clear the market of unauthorized, non–tobacco-flavored e-cigarette products, U.S. Department of Health & Human Services Secretary Alex M. Azar II announced Sept. 11.
“The Trump administration is making it clear that we intend to clear the market of flavored e-cigarettes to reverse the deeply concerning epidemic of youth e-cigarette use that is impacting children, families, schools, and communities,” Mr. Azar said in a statement. “We will not stand idly by as these products become an on-ramp to combustible cigarettes or nicotine addiction for a generation of youth.”
The announcement comes as the Centers for Disease Control and Prevention and state health departments track hundreds of lung-related illnesses that are linked to the use of e-cigarettes. At least 450 cases have been reported in 33 states and one jurisdiction. Diagnoses include lipoid pneumonia, alveolar hemorrhage, and cryptogenic organizing pneumonia, according to a Sept. 6 press briefing by Ileana Arias, PhD, CDC acting deputy director for non-infectious diseases. Six deaths associated with the illnesses have been reported thus far.
Details of new regulatory action will be forthcoming and will outline enforcement policy for non–tobacco-flavored e-cigarette products that lack premarket authorization, HHS officials said. According to federal rules, all electronic nicotine delivery system (ENDS) products must file premarket tobacco product applications with the FDA within 2 years. Many ENDS products currently on the market are not being legally marketed and are subject to government action, according to the Trump administration.
“Once finalized, this compliance policy will serve as a powerful tool that the FDA can use to combat the troubling trend of youth e-cigarette use,” Ned Sharpless, MD, acting FDA commissioner, said in the statement. “We must act swiftly against flavored e-cigarette products that are especially attractive to children. Moreover, if we see a migration to tobacco-flavored products by kids, we will take additional steps to address youth use of these products.”
Federal officials noted that preliminary numbers from the National Youth Tobacco Survey show a continued rise in youth e-cigarette use, with more than a quarter of high school students current e-cigarette users in 2019. The overwhelming majority of youth e-cigarette users cited the use of fruit, menthol, or mint flavors, according to the preliminary data, which have not yet been published.
According to 2018 survey data, e-cigarette use increased from 12% to 21% among high school students and from 3% to 5% among middle school students from 2017 to 2018. There were 1.5 million more youth e-cigarette users in 2018 than in 2017, and youth who were using e-cigarettes were using them more often, according to the survey.
The Food and Drug Administration is finalizing a compliance policy that will target flavored e-cigarettes and aim to clear the market of unauthorized, non–tobacco-flavored e-cigarette products, U.S. Department of Health & Human Services Secretary Alex M. Azar II announced Sept. 11.
“The Trump administration is making it clear that we intend to clear the market of flavored e-cigarettes to reverse the deeply concerning epidemic of youth e-cigarette use that is impacting children, families, schools, and communities,” Mr. Azar said in a statement. “We will not stand idly by as these products become an on-ramp to combustible cigarettes or nicotine addiction for a generation of youth.”
The announcement comes as the Centers for Disease Control and Prevention and state health departments track hundreds of lung-related illnesses that are linked to the use of e-cigarettes. At least 450 cases have been reported in 33 states and one jurisdiction. Diagnoses include lipoid pneumonia, alveolar hemorrhage, and cryptogenic organizing pneumonia, according to a Sept. 6 press briefing by Ileana Arias, PhD, CDC acting deputy director for non-infectious diseases. Six deaths associated with the illnesses have been reported thus far.
Details of new regulatory action will be forthcoming and will outline enforcement policy for non–tobacco-flavored e-cigarette products that lack premarket authorization, HHS officials said. According to federal rules, all electronic nicotine delivery system (ENDS) products must file premarket tobacco product applications with the FDA within 2 years. Many ENDS products currently on the market are not being legally marketed and are subject to government action, according to the Trump administration.
“Once finalized, this compliance policy will serve as a powerful tool that the FDA can use to combat the troubling trend of youth e-cigarette use,” Ned Sharpless, MD, acting FDA commissioner, said in the statement. “We must act swiftly against flavored e-cigarette products that are especially attractive to children. Moreover, if we see a migration to tobacco-flavored products by kids, we will take additional steps to address youth use of these products.”
Federal officials noted that preliminary numbers from the National Youth Tobacco Survey show a continued rise in youth e-cigarette use, with more than a quarter of high school students current e-cigarette users in 2019. The overwhelming majority of youth e-cigarette users cited the use of fruit, menthol, or mint flavors, according to the preliminary data, which have not yet been published.
According to 2018 survey data, e-cigarette use increased from 12% to 21% among high school students and from 3% to 5% among middle school students from 2017 to 2018. There were 1.5 million more youth e-cigarette users in 2018 than in 2017, and youth who were using e-cigarettes were using them more often, according to the survey.
Consider triple therapy for the management of COPD
Background: The Global Initiative for Obstructive Lung Disease (GOLD) recommends triple therapy with inhaled corticosteroids, long-acting beta2-adrenoceptor agonists (LABA), and long-acting muscarinic receptor antagonists (LAMA) for patients with severe COPD who have frequent exacerbations despite treatment with a LABA and LAMA. Triple therapy has been shown to improve forced expiratory volume in 1 second (FEV1), but its effect on preventing exacerbations has not been well documented in previous meta-analyses.
Study design: Meta-analysis.
Setting: Studies published on PubMed, Embase, Cochrane Library website, Cochrane Central Register of Controlled Trials (CENTRAL), and ClinicalTrials.gov databases.
Synopsis: 21 randomized, controlled trials of triple therapy in stable cases of moderate to very severe COPD were included in this meta-analysis. Triple therapy was associated with a significantly greater reduction in the rate of COPD exacerbations, compared with dual therapy of LAMA and LABA (rate ratio, 0.78; 95% confidence interval, 0.70-0.88), inhaled corticosteroid and LABA (rate ratio, 0.77; 95% CI, 0.66-0.91), or LAMA monotherapy (rate ratio, 0.71; 95% CI, 0.60-0.85). Triple therapy was also associated with greater improvement in FEV1.
There was a significantly higher incidence of pneumonia in patients using triple therapy, compared with those using dual therapy (LAMA and LABA), and there also was a trend toward increased pneumonia incidence with triple therapy, compared with LAMA monotherapy. Triple therapy was not shown to improve survival; however, most trials lasted less than 6 months, which limits their analysis of survival outcomes.
Bottom line: In patients with advanced COPD, triple therapy is associated with lower rates of COPD exacerbations and improved lung function, compared with dual therapy or monotherapy.
Citation: Zheng Y et al. Triple therapy in the management of chronic obstructive pulmonary disease: Systemic review and meta-analysis. BMJ. 2018;363:k4388.
Dr. Chace is an associate physician in the division of hospital medicine at the University of California, San Diego.
Background: The Global Initiative for Obstructive Lung Disease (GOLD) recommends triple therapy with inhaled corticosteroids, long-acting beta2-adrenoceptor agonists (LABA), and long-acting muscarinic receptor antagonists (LAMA) for patients with severe COPD who have frequent exacerbations despite treatment with a LABA and LAMA. Triple therapy has been shown to improve forced expiratory volume in 1 second (FEV1), but its effect on preventing exacerbations has not been well documented in previous meta-analyses.
Study design: Meta-analysis.
Setting: Studies published on PubMed, Embase, Cochrane Library website, Cochrane Central Register of Controlled Trials (CENTRAL), and ClinicalTrials.gov databases.
Synopsis: 21 randomized, controlled trials of triple therapy in stable cases of moderate to very severe COPD were included in this meta-analysis. Triple therapy was associated with a significantly greater reduction in the rate of COPD exacerbations, compared with dual therapy of LAMA and LABA (rate ratio, 0.78; 95% confidence interval, 0.70-0.88), inhaled corticosteroid and LABA (rate ratio, 0.77; 95% CI, 0.66-0.91), or LAMA monotherapy (rate ratio, 0.71; 95% CI, 0.60-0.85). Triple therapy was also associated with greater improvement in FEV1.
There was a significantly higher incidence of pneumonia in patients using triple therapy, compared with those using dual therapy (LAMA and LABA), and there also was a trend toward increased pneumonia incidence with triple therapy, compared with LAMA monotherapy. Triple therapy was not shown to improve survival; however, most trials lasted less than 6 months, which limits their analysis of survival outcomes.
Bottom line: In patients with advanced COPD, triple therapy is associated with lower rates of COPD exacerbations and improved lung function, compared with dual therapy or monotherapy.
Citation: Zheng Y et al. Triple therapy in the management of chronic obstructive pulmonary disease: Systemic review and meta-analysis. BMJ. 2018;363:k4388.
Dr. Chace is an associate physician in the division of hospital medicine at the University of California, San Diego.
Background: The Global Initiative for Obstructive Lung Disease (GOLD) recommends triple therapy with inhaled corticosteroids, long-acting beta2-adrenoceptor agonists (LABA), and long-acting muscarinic receptor antagonists (LAMA) for patients with severe COPD who have frequent exacerbations despite treatment with a LABA and LAMA. Triple therapy has been shown to improve forced expiratory volume in 1 second (FEV1), but its effect on preventing exacerbations has not been well documented in previous meta-analyses.
Study design: Meta-analysis.
Setting: Studies published on PubMed, Embase, Cochrane Library website, Cochrane Central Register of Controlled Trials (CENTRAL), and ClinicalTrials.gov databases.
Synopsis: 21 randomized, controlled trials of triple therapy in stable cases of moderate to very severe COPD were included in this meta-analysis. Triple therapy was associated with a significantly greater reduction in the rate of COPD exacerbations, compared with dual therapy of LAMA and LABA (rate ratio, 0.78; 95% confidence interval, 0.70-0.88), inhaled corticosteroid and LABA (rate ratio, 0.77; 95% CI, 0.66-0.91), or LAMA monotherapy (rate ratio, 0.71; 95% CI, 0.60-0.85). Triple therapy was also associated with greater improvement in FEV1.
There was a significantly higher incidence of pneumonia in patients using triple therapy, compared with those using dual therapy (LAMA and LABA), and there also was a trend toward increased pneumonia incidence with triple therapy, compared with LAMA monotherapy. Triple therapy was not shown to improve survival; however, most trials lasted less than 6 months, which limits their analysis of survival outcomes.
Bottom line: In patients with advanced COPD, triple therapy is associated with lower rates of COPD exacerbations and improved lung function, compared with dual therapy or monotherapy.
Citation: Zheng Y et al. Triple therapy in the management of chronic obstructive pulmonary disease: Systemic review and meta-analysis. BMJ. 2018;363:k4388.
Dr. Chace is an associate physician in the division of hospital medicine at the University of California, San Diego.
FDA issues warning to JUUL on illegal marketing of e-cigarettes
, citing violation of the Federal Food, Drug, and Cosmetic Act.
According to the letter, JUUL has marketed its e-cigarettes and e-liquids as modified-risk tobacco products without receiving FDA authorization to do so. JUUL’s labeling, advertising, and other consumer-oriented activities to this effect could reasonably lead consumers to believe that JUUL products represent a lower risk of tobacco-related disease, compared with other tobacco products; that they contain a reduced level of a substance; and that they are free of a particular substance or substances.
As evidence, the letter cited testimony given at a July 2019 hearing held by the Subcommittee on Economic and Consumer Policy of the Committee on Oversight and Reform of the House of Representatives, in which a representative from JUUL, speaking to students at a school presentation, said that JUUL products were “much safer than cigarettes” and that the “FDA would approve it any day,” that JUUL products were “totally safe,” that a student “should mention JUUL to his [nicotine-addicted] friend ... because that’s a safer alternative than smoking cigarettes, and it would be better for the kid to use,” and that the FDA “was about to come out and say it [JUUL] was 99% safer than cigarettes ... and that ... would happen very soon.”
In addition, a “Letter from the CEO” that appeared on the JUUL website and was emailed to a parent in response to her complaint that the company sold JUUL products to her child stated that “[JUUL’s] simple and convenient system incorporates temperature regulation to heat nicotine liquid and deliver smokers the satisfaction that they want without the combustion and the harm associated with it.”
In a related press release, acting FDA Commissioner Ned Sharpless, MD, said that “regardless of where products like e-cigarettes fall on the continuum of tobacco product risk, the law is clear that, before marketing tobacco products for reduced risk, companies must demonstrate with scientific evidence that their specific product does in fact pose less risk or is less harmful. JUUL has ignored the law, and very concerningly, has made some of these statements in school to our nation’s youth.”
The FDA has requested a response from JUUL within 15 working days of the letter’s issue. Failure to comply with the Federal Food, Drug, and Cosmetic Act could result in the FDA’s initiating further actions such as civil money penalties, seizure, and/or injunction.
, citing violation of the Federal Food, Drug, and Cosmetic Act.
According to the letter, JUUL has marketed its e-cigarettes and e-liquids as modified-risk tobacco products without receiving FDA authorization to do so. JUUL’s labeling, advertising, and other consumer-oriented activities to this effect could reasonably lead consumers to believe that JUUL products represent a lower risk of tobacco-related disease, compared with other tobacco products; that they contain a reduced level of a substance; and that they are free of a particular substance or substances.
As evidence, the letter cited testimony given at a July 2019 hearing held by the Subcommittee on Economic and Consumer Policy of the Committee on Oversight and Reform of the House of Representatives, in which a representative from JUUL, speaking to students at a school presentation, said that JUUL products were “much safer than cigarettes” and that the “FDA would approve it any day,” that JUUL products were “totally safe,” that a student “should mention JUUL to his [nicotine-addicted] friend ... because that’s a safer alternative than smoking cigarettes, and it would be better for the kid to use,” and that the FDA “was about to come out and say it [JUUL] was 99% safer than cigarettes ... and that ... would happen very soon.”
In addition, a “Letter from the CEO” that appeared on the JUUL website and was emailed to a parent in response to her complaint that the company sold JUUL products to her child stated that “[JUUL’s] simple and convenient system incorporates temperature regulation to heat nicotine liquid and deliver smokers the satisfaction that they want without the combustion and the harm associated with it.”
In a related press release, acting FDA Commissioner Ned Sharpless, MD, said that “regardless of where products like e-cigarettes fall on the continuum of tobacco product risk, the law is clear that, before marketing tobacco products for reduced risk, companies must demonstrate with scientific evidence that their specific product does in fact pose less risk or is less harmful. JUUL has ignored the law, and very concerningly, has made some of these statements in school to our nation’s youth.”
The FDA has requested a response from JUUL within 15 working days of the letter’s issue. Failure to comply with the Federal Food, Drug, and Cosmetic Act could result in the FDA’s initiating further actions such as civil money penalties, seizure, and/or injunction.
, citing violation of the Federal Food, Drug, and Cosmetic Act.
According to the letter, JUUL has marketed its e-cigarettes and e-liquids as modified-risk tobacco products without receiving FDA authorization to do so. JUUL’s labeling, advertising, and other consumer-oriented activities to this effect could reasonably lead consumers to believe that JUUL products represent a lower risk of tobacco-related disease, compared with other tobacco products; that they contain a reduced level of a substance; and that they are free of a particular substance or substances.
As evidence, the letter cited testimony given at a July 2019 hearing held by the Subcommittee on Economic and Consumer Policy of the Committee on Oversight and Reform of the House of Representatives, in which a representative from JUUL, speaking to students at a school presentation, said that JUUL products were “much safer than cigarettes” and that the “FDA would approve it any day,” that JUUL products were “totally safe,” that a student “should mention JUUL to his [nicotine-addicted] friend ... because that’s a safer alternative than smoking cigarettes, and it would be better for the kid to use,” and that the FDA “was about to come out and say it [JUUL] was 99% safer than cigarettes ... and that ... would happen very soon.”
In addition, a “Letter from the CEO” that appeared on the JUUL website and was emailed to a parent in response to her complaint that the company sold JUUL products to her child stated that “[JUUL’s] simple and convenient system incorporates temperature regulation to heat nicotine liquid and deliver smokers the satisfaction that they want without the combustion and the harm associated with it.”
In a related press release, acting FDA Commissioner Ned Sharpless, MD, said that “regardless of where products like e-cigarettes fall on the continuum of tobacco product risk, the law is clear that, before marketing tobacco products for reduced risk, companies must demonstrate with scientific evidence that their specific product does in fact pose less risk or is less harmful. JUUL has ignored the law, and very concerningly, has made some of these statements in school to our nation’s youth.”
The FDA has requested a response from JUUL within 15 working days of the letter’s issue. Failure to comply with the Federal Food, Drug, and Cosmetic Act could result in the FDA’s initiating further actions such as civil money penalties, seizure, and/or injunction.
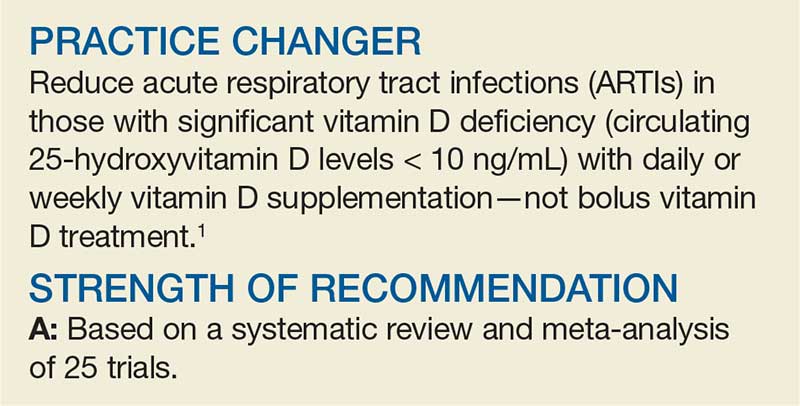
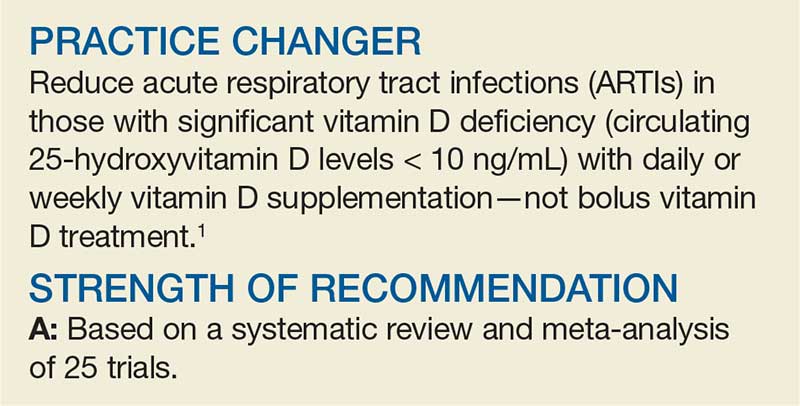
Can Vitamin D Prevent Acute Respiratory Infections?
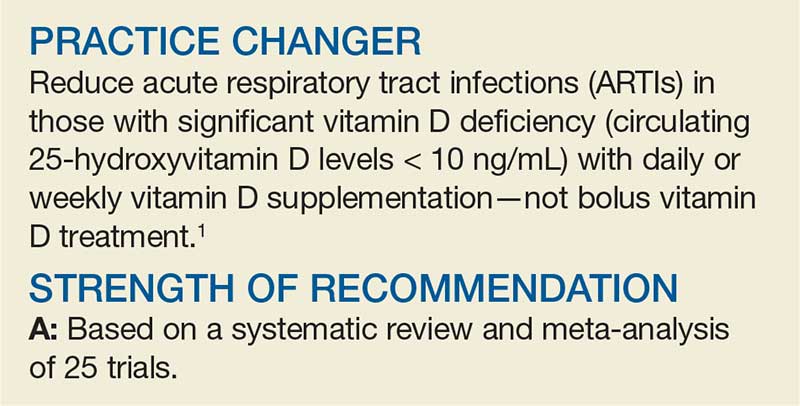
Ms. M, a generally healthy 55-year-old woman, was diagnosed recently with severe vitamin D deficiency (serum 25-hydroxyvitamin D [25(OH)D] level of 8 ng/mL). She presents with her second episode of acute viral bronchitis in the past 6 months. She has no history of significant smoking or exposure or history of asthma and does not take respiratory medications. Standard treatment for her level of vitamin D deficiency is 50,000 IU/wk in bolus dosing—but is that your best option for the patient?
ARTIs include nonspecific upper respiratory illnesses, otitis media, sinusitis (~70% viral), pharyngitis, acute bronchitis (also ~70% viral), influenza, respiratory syncytial virus, and pneumonia.1,2 In the United States, ARTIs strain the health care system and are the most common reason for ambulatory care visits, accounting for almost 120 million (about 10% of all) visits per year.3 In addition, ARTIs account for almost 50% of antibiotic prescriptions for adults and almost 75% of antibiotic prescriptions for children—many of which are unnecessary.2,4
While patient and parent education, antibiotic stewardship programs, and demand management may reduce inappropriate antibiotic use and the overall burden of ARTIs on the health care system, prevention of infections is a powerful tool within the overall approach to managing ARTIs.
STUDY SUMMARY
Vitamin D is protective in smaller doses
This 2017 systematic review and meta-analysis of 25 trials (N = 10,933) evaluated vitamin D supplementation for the prevention of ARTIs in the primary care setting. Individual participant data were reevaluated to reduce risk for bias. The Cochrane risk-for-bias tool was used to address threats to validity.
The study included institutional review board–approved, randomized, double-blind, placebo-controlled trials of vitamin D3 or D2 supplementation of any duration and in any language. The incidence of ARTI was a prespecified efficacy outcome. Duration of the included randomized controlled trials (RCTs) ranged from 7 weeks to 1.5 years.
Outcomes. The primary outcome was an incidence of at least 1 ARTI. Secondary outcomes included incidence of upper and lower ARTIs; incidence of adverse reactions to vitamin D; incidence of emergency department visits or hospital admission or both for ARTI; use of antimicrobials for ARTI; absence from work or school due to ARTI; and mortality (ARTI-related and all-cause).
Findings. Daily or weekly vitamin D supplementation (in doses ranging from < 20 to ≥ 50 µg/d) reduced the risk for ARTI (adjusted odds ratio [AOR], 0.88; number needed to treat [NNT], 33). In subgroup analysis, daily or weekly vitamin D was protective (AOR, 0.81), but bolus dosing (≥ 30,000 IU) was not (AOR, 0.97).
In 2-step analysis, patients benefited if they had baseline circulating 25(OH)D concentrations < 10 ng/mL (AOR, 0.30; NNT, 4); had baseline circulating 25(OH)D levels of 10 to 28 ng/mL (AOR, 0.75; NNT, 15); were ages 1.1 to 15.9 (AOR, 0.59); were ages 16 to 65 (AOR, 0.79); or had a BMI < 25 (AOR, 0.82).
Higher D levels are a different story. Vitamin D supplementation in people with circulating levels of 25(OH)D ≥ 30 ng/mL did not appear to provide benefit (AOR, 0.96). Supplementation in this population did not influence any of the secondary outcomes, including risk for all-cause serious adverse events (AOR, 0.98).
WHAT’S NEW
A more accurate snapshot
Previous studies of vitamin D and respiratory tract infections were mostly observational in nature. Those that were RCTs used variable doses of vitamin D, had variable baseline 25(OH)D levels, and employed various methods to monitor ARTI symptoms/incidence.5-8 This is the first systematic review and meta-analysis of randomized, double-blind, placebo-controlled trials with supplementation using vitamin D3 or D2 that used individual participant-level data, which gives a more accurate estimate of outcomes when compared with traditional meta-analyses.
CAVEATS
Only the most deficient benefit?
Vitamin D supplementation was safe and protected against ARTIs overall, but the greatest effect was noted in those who were most severely vitamin D deficient (those with circulating 25(OH)D levels < 10 ng/mL [NNT, 4] and those with circulating 25(OH)D levels 10-28 ng/mL [NNT, 15]). There was no demonstrable effect once circulating 25(OH)D levels reached 30 ng/mL.
CHALLENGES TO IMPLEMENTATION
Breaking tradition
The study found that both daily and weekly doses of vitamin D were effective in reducing the incidence of ARTIs. However, the doses studied were much lower than those commonly used (10,000 to 50,000 IU bolus), which were ineffective in reducing ARTIs in this meta-analysis. Changing from bolus dosing may prove challenging, a
In addition, the authors of the study suggest that one way to provide this level of vitamin D is through food fortification. But this method is often complicated by emotional and/or political issues that could thwart implementation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2019. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2019;68[4]:230-231).
1. Martineau AR, Jolliffe DA, Hooper RL, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583.
2. Renati S, Linder JA. Necessity of office visits for acute respiratory infections in primary care. Fam Pract. 2016,33:312-317.
3. CDC National Center for Health Statistics. National Health Care Surveys. www.cdc.gov/nchs/dhcs.htm. Accessed September 5, 2019.
4. Grijalva CG, Nuorti JP, Griffin MR. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. JAMA. 2009;302:758-766.
5. Rees JR, Hendricks K, Barry EL, et al. Vitamin D3 supplementation and upper respiratory tract infections in a randomized, controlled trial. Clin Infect Dis. 2013;57:1384-1392.
6. Murdoch DR, Slow S, Chambers ST, et al. Effect of vitamin D3 supplementation on upper respiratory tract infections in healthy adults: the VIDARIS randomized controlled trial. JAMA. 2012;308:1333-1339.
7. Laaksi I, Ruohola J-P, Mattila V, et al. Vitamin D supplementation for the prevention of acute respiratory tract infection: a randomized, double-blinded trial among young Finnish men. Infect Dis. 2010;202:809-814.
8. Bergman P, Norlin A-C, Hansen S, et al. Vitamin D3 supplementation in patients with frequent respiratory tract infections: a randomised and double-blind intervention study. BMJ Open. 2012;2:e001663.
Ms. M, a generally healthy 55-year-old woman, was diagnosed recently with severe vitamin D deficiency (serum 25-hydroxyvitamin D [25(OH)D] level of 8 ng/mL). She presents with her second episode of acute viral bronchitis in the past 6 months. She has no history of significant smoking or exposure or history of asthma and does not take respiratory medications. Standard treatment for her level of vitamin D deficiency is 50,000 IU/wk in bolus dosing—but is that your best option for the patient?
ARTIs include nonspecific upper respiratory illnesses, otitis media, sinusitis (~70% viral), pharyngitis, acute bronchitis (also ~70% viral), influenza, respiratory syncytial virus, and pneumonia.1,2 In the United States, ARTIs strain the health care system and are the most common reason for ambulatory care visits, accounting for almost 120 million (about 10% of all) visits per year.3 In addition, ARTIs account for almost 50% of antibiotic prescriptions for adults and almost 75% of antibiotic prescriptions for children—many of which are unnecessary.2,4
While patient and parent education, antibiotic stewardship programs, and demand management may reduce inappropriate antibiotic use and the overall burden of ARTIs on the health care system, prevention of infections is a powerful tool within the overall approach to managing ARTIs.
STUDY SUMMARY
Vitamin D is protective in smaller doses
This 2017 systematic review and meta-analysis of 25 trials (N = 10,933) evaluated vitamin D supplementation for the prevention of ARTIs in the primary care setting. Individual participant data were reevaluated to reduce risk for bias. The Cochrane risk-for-bias tool was used to address threats to validity.
The study included institutional review board–approved, randomized, double-blind, placebo-controlled trials of vitamin D3 or D2 supplementation of any duration and in any language. The incidence of ARTI was a prespecified efficacy outcome. Duration of the included randomized controlled trials (RCTs) ranged from 7 weeks to 1.5 years.
Outcomes. The primary outcome was an incidence of at least 1 ARTI. Secondary outcomes included incidence of upper and lower ARTIs; incidence of adverse reactions to vitamin D; incidence of emergency department visits or hospital admission or both for ARTI; use of antimicrobials for ARTI; absence from work or school due to ARTI; and mortality (ARTI-related and all-cause).
Findings. Daily or weekly vitamin D supplementation (in doses ranging from < 20 to ≥ 50 µg/d) reduced the risk for ARTI (adjusted odds ratio [AOR], 0.88; number needed to treat [NNT], 33). In subgroup analysis, daily or weekly vitamin D was protective (AOR, 0.81), but bolus dosing (≥ 30,000 IU) was not (AOR, 0.97).
In 2-step analysis, patients benefited if they had baseline circulating 25(OH)D concentrations < 10 ng/mL (AOR, 0.30; NNT, 4); had baseline circulating 25(OH)D levels of 10 to 28 ng/mL (AOR, 0.75; NNT, 15); were ages 1.1 to 15.9 (AOR, 0.59); were ages 16 to 65 (AOR, 0.79); or had a BMI < 25 (AOR, 0.82).
Higher D levels are a different story. Vitamin D supplementation in people with circulating levels of 25(OH)D ≥ 30 ng/mL did not appear to provide benefit (AOR, 0.96). Supplementation in this population did not influence any of the secondary outcomes, including risk for all-cause serious adverse events (AOR, 0.98).
WHAT’S NEW
A more accurate snapshot
Previous studies of vitamin D and respiratory tract infections were mostly observational in nature. Those that were RCTs used variable doses of vitamin D, had variable baseline 25(OH)D levels, and employed various methods to monitor ARTI symptoms/incidence.5-8 This is the first systematic review and meta-analysis of randomized, double-blind, placebo-controlled trials with supplementation using vitamin D3 or D2 that used individual participant-level data, which gives a more accurate estimate of outcomes when compared with traditional meta-analyses.
CAVEATS
Only the most deficient benefit?
Vitamin D supplementation was safe and protected against ARTIs overall, but the greatest effect was noted in those who were most severely vitamin D deficient (those with circulating 25(OH)D levels < 10 ng/mL [NNT, 4] and those with circulating 25(OH)D levels 10-28 ng/mL [NNT, 15]). There was no demonstrable effect once circulating 25(OH)D levels reached 30 ng/mL.
CHALLENGES TO IMPLEMENTATION
Breaking tradition
The study found that both daily and weekly doses of vitamin D were effective in reducing the incidence of ARTIs. However, the doses studied were much lower than those commonly used (10,000 to 50,000 IU bolus), which were ineffective in reducing ARTIs in this meta-analysis. Changing from bolus dosing may prove challenging, a
In addition, the authors of the study suggest that one way to provide this level of vitamin D is through food fortification. But this method is often complicated by emotional and/or political issues that could thwart implementation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2019. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2019;68[4]:230-231).
Ms. M, a generally healthy 55-year-old woman, was diagnosed recently with severe vitamin D deficiency (serum 25-hydroxyvitamin D [25(OH)D] level of 8 ng/mL). She presents with her second episode of acute viral bronchitis in the past 6 months. She has no history of significant smoking or exposure or history of asthma and does not take respiratory medications. Standard treatment for her level of vitamin D deficiency is 50,000 IU/wk in bolus dosing—but is that your best option for the patient?
ARTIs include nonspecific upper respiratory illnesses, otitis media, sinusitis (~70% viral), pharyngitis, acute bronchitis (also ~70% viral), influenza, respiratory syncytial virus, and pneumonia.1,2 In the United States, ARTIs strain the health care system and are the most common reason for ambulatory care visits, accounting for almost 120 million (about 10% of all) visits per year.3 In addition, ARTIs account for almost 50% of antibiotic prescriptions for adults and almost 75% of antibiotic prescriptions for children—many of which are unnecessary.2,4
While patient and parent education, antibiotic stewardship programs, and demand management may reduce inappropriate antibiotic use and the overall burden of ARTIs on the health care system, prevention of infections is a powerful tool within the overall approach to managing ARTIs.
STUDY SUMMARY
Vitamin D is protective in smaller doses
This 2017 systematic review and meta-analysis of 25 trials (N = 10,933) evaluated vitamin D supplementation for the prevention of ARTIs in the primary care setting. Individual participant data were reevaluated to reduce risk for bias. The Cochrane risk-for-bias tool was used to address threats to validity.
The study included institutional review board–approved, randomized, double-blind, placebo-controlled trials of vitamin D3 or D2 supplementation of any duration and in any language. The incidence of ARTI was a prespecified efficacy outcome. Duration of the included randomized controlled trials (RCTs) ranged from 7 weeks to 1.5 years.
Outcomes. The primary outcome was an incidence of at least 1 ARTI. Secondary outcomes included incidence of upper and lower ARTIs; incidence of adverse reactions to vitamin D; incidence of emergency department visits or hospital admission or both for ARTI; use of antimicrobials for ARTI; absence from work or school due to ARTI; and mortality (ARTI-related and all-cause).
Findings. Daily or weekly vitamin D supplementation (in doses ranging from < 20 to ≥ 50 µg/d) reduced the risk for ARTI (adjusted odds ratio [AOR], 0.88; number needed to treat [NNT], 33). In subgroup analysis, daily or weekly vitamin D was protective (AOR, 0.81), but bolus dosing (≥ 30,000 IU) was not (AOR, 0.97).
In 2-step analysis, patients benefited if they had baseline circulating 25(OH)D concentrations < 10 ng/mL (AOR, 0.30; NNT, 4); had baseline circulating 25(OH)D levels of 10 to 28 ng/mL (AOR, 0.75; NNT, 15); were ages 1.1 to 15.9 (AOR, 0.59); were ages 16 to 65 (AOR, 0.79); or had a BMI < 25 (AOR, 0.82).
Higher D levels are a different story. Vitamin D supplementation in people with circulating levels of 25(OH)D ≥ 30 ng/mL did not appear to provide benefit (AOR, 0.96). Supplementation in this population did not influence any of the secondary outcomes, including risk for all-cause serious adverse events (AOR, 0.98).
WHAT’S NEW
A more accurate snapshot
Previous studies of vitamin D and respiratory tract infections were mostly observational in nature. Those that were RCTs used variable doses of vitamin D, had variable baseline 25(OH)D levels, and employed various methods to monitor ARTI symptoms/incidence.5-8 This is the first systematic review and meta-analysis of randomized, double-blind, placebo-controlled trials with supplementation using vitamin D3 or D2 that used individual participant-level data, which gives a more accurate estimate of outcomes when compared with traditional meta-analyses.
CAVEATS
Only the most deficient benefit?
Vitamin D supplementation was safe and protected against ARTIs overall, but the greatest effect was noted in those who were most severely vitamin D deficient (those with circulating 25(OH)D levels < 10 ng/mL [NNT, 4] and those with circulating 25(OH)D levels 10-28 ng/mL [NNT, 15]). There was no demonstrable effect once circulating 25(OH)D levels reached 30 ng/mL.
CHALLENGES TO IMPLEMENTATION
Breaking tradition
The study found that both daily and weekly doses of vitamin D were effective in reducing the incidence of ARTIs. However, the doses studied were much lower than those commonly used (10,000 to 50,000 IU bolus), which were ineffective in reducing ARTIs in this meta-analysis. Changing from bolus dosing may prove challenging, a
In addition, the authors of the study suggest that one way to provide this level of vitamin D is through food fortification. But this method is often complicated by emotional and/or political issues that could thwart implementation.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2019. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2019;68[4]:230-231).
1. Martineau AR, Jolliffe DA, Hooper RL, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583.
2. Renati S, Linder JA. Necessity of office visits for acute respiratory infections in primary care. Fam Pract. 2016,33:312-317.
3. CDC National Center for Health Statistics. National Health Care Surveys. www.cdc.gov/nchs/dhcs.htm. Accessed September 5, 2019.
4. Grijalva CG, Nuorti JP, Griffin MR. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. JAMA. 2009;302:758-766.
5. Rees JR, Hendricks K, Barry EL, et al. Vitamin D3 supplementation and upper respiratory tract infections in a randomized, controlled trial. Clin Infect Dis. 2013;57:1384-1392.
6. Murdoch DR, Slow S, Chambers ST, et al. Effect of vitamin D3 supplementation on upper respiratory tract infections in healthy adults: the VIDARIS randomized controlled trial. JAMA. 2012;308:1333-1339.
7. Laaksi I, Ruohola J-P, Mattila V, et al. Vitamin D supplementation for the prevention of acute respiratory tract infection: a randomized, double-blinded trial among young Finnish men. Infect Dis. 2010;202:809-814.
8. Bergman P, Norlin A-C, Hansen S, et al. Vitamin D3 supplementation in patients with frequent respiratory tract infections: a randomised and double-blind intervention study. BMJ Open. 2012;2:e001663.
1. Martineau AR, Jolliffe DA, Hooper RL, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583.
2. Renati S, Linder JA. Necessity of office visits for acute respiratory infections in primary care. Fam Pract. 2016,33:312-317.
3. CDC National Center for Health Statistics. National Health Care Surveys. www.cdc.gov/nchs/dhcs.htm. Accessed September 5, 2019.
4. Grijalva CG, Nuorti JP, Griffin MR. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. JAMA. 2009;302:758-766.
5. Rees JR, Hendricks K, Barry EL, et al. Vitamin D3 supplementation and upper respiratory tract infections in a randomized, controlled trial. Clin Infect Dis. 2013;57:1384-1392.
6. Murdoch DR, Slow S, Chambers ST, et al. Effect of vitamin D3 supplementation on upper respiratory tract infections in healthy adults: the VIDARIS randomized controlled trial. JAMA. 2012;308:1333-1339.
7. Laaksi I, Ruohola J-P, Mattila V, et al. Vitamin D supplementation for the prevention of acute respiratory tract infection: a randomized, double-blinded trial among young Finnish men. Infect Dis. 2010;202:809-814.
8. Bergman P, Norlin A-C, Hansen S, et al. Vitamin D3 supplementation in patients with frequent respiratory tract infections: a randomised and double-blind intervention study. BMJ Open. 2012;2:e001663.
FDA approves nintedanib for scleroderma interstitial lung disease
The Food and Drug Administration has approved nintedanib (Ofev) for the rare but sometimes deadly form of interstitial lung disease that’s caused by systemic sclerosis, or scleroderma.
Although scleroderma itself is rare, half of those patients present with scleroderma-related interstitial lung disease (SSc-ILD), and it remains the leading cause of death in scleroderma patients because it can lead to loss of pulmonary function. Nintedanib appears to slow the progress of SSc-ILD and is the first treatment approved for it, according to a news release from the FDA.
The approval is based on a randomized, double-blind, placebo-controlled trial of 576 patients aged 20-79 years with SSc-ILD. The primary efficacy endpoint was forced vital capacity, and patients on nintedanib showed less decline than did those on placebo.
The most frequent serious adverse event reported in this trial was pneumonia (2.8% with nintedanib vs. 0.3% with placebo). Adverse reactions that led to permanent dose reductions occurred in 34% of nintedanib patients and 4% of placebo-treated patients; the most common of these was diarrhea.
The full prescribing information, which is available on the FDA website, includes warnings for patients with moderate to severe hepatic impairment, elevated liver enzymes, and drug-induced liver injury, as well as those with gastrointestinal disorders. Nintedanib may cause embryo-fetal toxicity, so women of childbearing age should be counseled to avoid pregnancy while taking this drug.
Nintedanib received both Priority Review and Orphan Drug designation. The former meant the FDA intends to take action on the application within 6 months because the agency has determined that, if approved, it would have important effects on treatment of a serious condition. The latter provides incentives to assist and encourage development of drugs for rare diseases. The drug was approved in 2014 for adult patients with idiopathic pulmonary fibrosis, another interstitial lung disease.
The full release is available on the FDA website.
The Food and Drug Administration has approved nintedanib (Ofev) for the rare but sometimes deadly form of interstitial lung disease that’s caused by systemic sclerosis, or scleroderma.
Although scleroderma itself is rare, half of those patients present with scleroderma-related interstitial lung disease (SSc-ILD), and it remains the leading cause of death in scleroderma patients because it can lead to loss of pulmonary function. Nintedanib appears to slow the progress of SSc-ILD and is the first treatment approved for it, according to a news release from the FDA.
The approval is based on a randomized, double-blind, placebo-controlled trial of 576 patients aged 20-79 years with SSc-ILD. The primary efficacy endpoint was forced vital capacity, and patients on nintedanib showed less decline than did those on placebo.
The most frequent serious adverse event reported in this trial was pneumonia (2.8% with nintedanib vs. 0.3% with placebo). Adverse reactions that led to permanent dose reductions occurred in 34% of nintedanib patients and 4% of placebo-treated patients; the most common of these was diarrhea.
The full prescribing information, which is available on the FDA website, includes warnings for patients with moderate to severe hepatic impairment, elevated liver enzymes, and drug-induced liver injury, as well as those with gastrointestinal disorders. Nintedanib may cause embryo-fetal toxicity, so women of childbearing age should be counseled to avoid pregnancy while taking this drug.
Nintedanib received both Priority Review and Orphan Drug designation. The former meant the FDA intends to take action on the application within 6 months because the agency has determined that, if approved, it would have important effects on treatment of a serious condition. The latter provides incentives to assist and encourage development of drugs for rare diseases. The drug was approved in 2014 for adult patients with idiopathic pulmonary fibrosis, another interstitial lung disease.
The full release is available on the FDA website.
The Food and Drug Administration has approved nintedanib (Ofev) for the rare but sometimes deadly form of interstitial lung disease that’s caused by systemic sclerosis, or scleroderma.
Although scleroderma itself is rare, half of those patients present with scleroderma-related interstitial lung disease (SSc-ILD), and it remains the leading cause of death in scleroderma patients because it can lead to loss of pulmonary function. Nintedanib appears to slow the progress of SSc-ILD and is the first treatment approved for it, according to a news release from the FDA.
The approval is based on a randomized, double-blind, placebo-controlled trial of 576 patients aged 20-79 years with SSc-ILD. The primary efficacy endpoint was forced vital capacity, and patients on nintedanib showed less decline than did those on placebo.
The most frequent serious adverse event reported in this trial was pneumonia (2.8% with nintedanib vs. 0.3% with placebo). Adverse reactions that led to permanent dose reductions occurred in 34% of nintedanib patients and 4% of placebo-treated patients; the most common of these was diarrhea.
The full prescribing information, which is available on the FDA website, includes warnings for patients with moderate to severe hepatic impairment, elevated liver enzymes, and drug-induced liver injury, as well as those with gastrointestinal disorders. Nintedanib may cause embryo-fetal toxicity, so women of childbearing age should be counseled to avoid pregnancy while taking this drug.
Nintedanib received both Priority Review and Orphan Drug designation. The former meant the FDA intends to take action on the application within 6 months because the agency has determined that, if approved, it would have important effects on treatment of a serious condition. The latter provides incentives to assist and encourage development of drugs for rare diseases. The drug was approved in 2014 for adult patients with idiopathic pulmonary fibrosis, another interstitial lung disease.
The full release is available on the FDA website.
Less CPAP time linked to exacerbation in COPD/OSA overlap syndrome
and all‐cause mortality, according to a retrospective cohort study.
“These factors should be taken into account when considering the management and prognosis of these patients,” the researchers said in the Clinical Respiratory Journal.
Prior studies have found that patients with COPD and OSA – that is, with overlap syndrome – “have a substantially greater risk of morbidity and mortality, compared to those with either COPD or OSA alone,” said Philippe E. Jaoude, MD, and Ali A. El Solh, MD, both of the Veterans Affairs Western New York Healthcare System in Buffalo and the University at Buffalo.
To identify factors associated with COPD exacerbation and all‐cause mortality in patients with overlap syndrome, Dr. Jaoude and Dr. El Solh reviewed the electronic health records of patients with simultaneous COPD and OSA. They compared patients with overlap syndrome who had an acute exacerbation of COPD during a 42-month period with a control group of patients with overlap syndrome who did not have exacerbations during that time. Patients with exacerbations and controls were matched 1:1 by age and body mass index.
Eligible patients were aged 42-90 years, had objectively confirmed COPD, and had documented OSA by in-laboratory polysomnography (that is, at least five obstructive apneas and hypopneas per hour). The investigators defined a COPD exacerbation as a sustained worsening of a patient’s respiratory condition that warranted additional treatment.
Of 225 eligible patients, 92 had at least one COPD exacerbation between March 2014 and September 2017. Patients with COPD exacerbation and controls had a mean age of about 68 years. The group of patients with exacerbation had a higher percentage of active smokers (21% vs. 9%) and had poorer lung function (mean forced expiratory volume in 1 second percent predicted: 55.2% vs. 64.5%).
“Although the rate of CPAP adherence between the two groups was not significantly different, the average time of CPAP use was significantly higher in patients with no recorded exacerbation,” the researchers reported – 285.4 min/night versus 238.2 min/night.
In all, 146 patients (79.4%) survived, and 38 patients (20.6%) died during the study period. The crude mortality rate was significantly higher in the group with COPD exacerbations (14% vs. 7%).
“Multivariate logistic regression analysis identified the independent risk factors associated with COPD exacerbations as active smoking, worse airflow limitation, and lower CPAP utilization,” they said. “As for all-cause mortality, a higher burden of comorbidities, worse airflow limitation, and lower time of CPAP use were independently associated with poor outcome.”
The researchers noted that they cannot rule out the possibility that patients who were adherent to CPAP were systematically different from those who were not.
The authors had no conflicts of interest.
SOURCE: Jaoude P et al. Clin Respir J. 2019 Aug 22. doi: 10.1111/crj.13079.
and all‐cause mortality, according to a retrospective cohort study.
“These factors should be taken into account when considering the management and prognosis of these patients,” the researchers said in the Clinical Respiratory Journal.
Prior studies have found that patients with COPD and OSA – that is, with overlap syndrome – “have a substantially greater risk of morbidity and mortality, compared to those with either COPD or OSA alone,” said Philippe E. Jaoude, MD, and Ali A. El Solh, MD, both of the Veterans Affairs Western New York Healthcare System in Buffalo and the University at Buffalo.
To identify factors associated with COPD exacerbation and all‐cause mortality in patients with overlap syndrome, Dr. Jaoude and Dr. El Solh reviewed the electronic health records of patients with simultaneous COPD and OSA. They compared patients with overlap syndrome who had an acute exacerbation of COPD during a 42-month period with a control group of patients with overlap syndrome who did not have exacerbations during that time. Patients with exacerbations and controls were matched 1:1 by age and body mass index.
Eligible patients were aged 42-90 years, had objectively confirmed COPD, and had documented OSA by in-laboratory polysomnography (that is, at least five obstructive apneas and hypopneas per hour). The investigators defined a COPD exacerbation as a sustained worsening of a patient’s respiratory condition that warranted additional treatment.
Of 225 eligible patients, 92 had at least one COPD exacerbation between March 2014 and September 2017. Patients with COPD exacerbation and controls had a mean age of about 68 years. The group of patients with exacerbation had a higher percentage of active smokers (21% vs. 9%) and had poorer lung function (mean forced expiratory volume in 1 second percent predicted: 55.2% vs. 64.5%).
“Although the rate of CPAP adherence between the two groups was not significantly different, the average time of CPAP use was significantly higher in patients with no recorded exacerbation,” the researchers reported – 285.4 min/night versus 238.2 min/night.
In all, 146 patients (79.4%) survived, and 38 patients (20.6%) died during the study period. The crude mortality rate was significantly higher in the group with COPD exacerbations (14% vs. 7%).
“Multivariate logistic regression analysis identified the independent risk factors associated with COPD exacerbations as active smoking, worse airflow limitation, and lower CPAP utilization,” they said. “As for all-cause mortality, a higher burden of comorbidities, worse airflow limitation, and lower time of CPAP use were independently associated with poor outcome.”
The researchers noted that they cannot rule out the possibility that patients who were adherent to CPAP were systematically different from those who were not.
The authors had no conflicts of interest.
SOURCE: Jaoude P et al. Clin Respir J. 2019 Aug 22. doi: 10.1111/crj.13079.
and all‐cause mortality, according to a retrospective cohort study.
“These factors should be taken into account when considering the management and prognosis of these patients,” the researchers said in the Clinical Respiratory Journal.
Prior studies have found that patients with COPD and OSA – that is, with overlap syndrome – “have a substantially greater risk of morbidity and mortality, compared to those with either COPD or OSA alone,” said Philippe E. Jaoude, MD, and Ali A. El Solh, MD, both of the Veterans Affairs Western New York Healthcare System in Buffalo and the University at Buffalo.
To identify factors associated with COPD exacerbation and all‐cause mortality in patients with overlap syndrome, Dr. Jaoude and Dr. El Solh reviewed the electronic health records of patients with simultaneous COPD and OSA. They compared patients with overlap syndrome who had an acute exacerbation of COPD during a 42-month period with a control group of patients with overlap syndrome who did not have exacerbations during that time. Patients with exacerbations and controls were matched 1:1 by age and body mass index.
Eligible patients were aged 42-90 years, had objectively confirmed COPD, and had documented OSA by in-laboratory polysomnography (that is, at least five obstructive apneas and hypopneas per hour). The investigators defined a COPD exacerbation as a sustained worsening of a patient’s respiratory condition that warranted additional treatment.
Of 225 eligible patients, 92 had at least one COPD exacerbation between March 2014 and September 2017. Patients with COPD exacerbation and controls had a mean age of about 68 years. The group of patients with exacerbation had a higher percentage of active smokers (21% vs. 9%) and had poorer lung function (mean forced expiratory volume in 1 second percent predicted: 55.2% vs. 64.5%).
“Although the rate of CPAP adherence between the two groups was not significantly different, the average time of CPAP use was significantly higher in patients with no recorded exacerbation,” the researchers reported – 285.4 min/night versus 238.2 min/night.
In all, 146 patients (79.4%) survived, and 38 patients (20.6%) died during the study period. The crude mortality rate was significantly higher in the group with COPD exacerbations (14% vs. 7%).
“Multivariate logistic regression analysis identified the independent risk factors associated with COPD exacerbations as active smoking, worse airflow limitation, and lower CPAP utilization,” they said. “As for all-cause mortality, a higher burden of comorbidities, worse airflow limitation, and lower time of CPAP use were independently associated with poor outcome.”
The researchers noted that they cannot rule out the possibility that patients who were adherent to CPAP were systematically different from those who were not.
The authors had no conflicts of interest.
SOURCE: Jaoude P et al. Clin Respir J. 2019 Aug 22. doi: 10.1111/crj.13079.
FROM CLINICAL RESPIRATORY JOURNAL
Guideline: Blood CO2 can be used to screen for OHS
A blood test for elevated carbon dioxide may be used in screening adults for obesity hypoventilation syndrome, according to new guidelines.
Obese adults with sleep-disordered breathing and increased blood carbon dioxide levels during the day are likely to have obesity hypoventilation syndrome (OHS), a result of shallow or slow breathing that can lead to respiratory failure, heart failure, pulmonary hypertension, and death. Pulmonologists and sleep specialists may be the first to see and diagnose patients with OHS in the outpatient setting, while other cases are diagnosed in the hospital when patients present with hypercapnic respiratory failure.
Screening for OHS usually involves measuring arterial blood gases, which is not standard practice in outpatient clinics. Patients often remain undiagnosed and untreated until late in the course of the disease, according to the American Thoracic Society, which in August published a new diagnosis and management guideline aiming to boost early diagnosis and reduce variability in treatment (Am J Respir Crit Care Med. 2019;200:3,e6–e24).
The guideline authors, led by Babak Mokhlesi, MD, of the University of Chicago, recommend a simpler screening method – measuring serum bicarbonate only – to rule out OHS in obese patients with nighttime breathing problems.
Serum bicarbonate should be measured in obese patients with sleep-disordered breathing and a low likelihood of OHS, Dr. Mokhlesi and colleagues recommend in the guideline. If serum bicarbonate is below 27 mmol/L, it is not necessary to conduct further testing as the patient is unlikely to have OHS.
In patients whose serum bicarbonate is higher than 27 mmol/L, or who are strongly suspected of having OHS at presentation because of severe obesity or other symptoms, arterial blood gases should be measured and a sleep study conducted. The guideline authors said that there is insufficient evidence to recommend that pulse oximetry be used in the diagnostic pathway for OHS.
First-line treatment for stable, ambulatory patients with OHS should be positive airway pressure during sleep, rather than noninvasive ventilation, Dr. Mokhlesi and colleagues concluded. For patients with comorbid obstructive sleep apnea – as many as 70% of OHS patients also have OSA – the first-line treatment should be continuous positive airway pressure (CPAP) at night, the guideline states.
Patients hospitalized with respiratory failure and suspected of having OHS should be discharged with noninvasive ventilation until diagnostic procedures can be performed, along with PAP titration in a sleep lab.
In patients initially treated with CPAP who remain symptomatic or whose blood carbon dioxide does not improve, noninvasive ventilation can be tried, the guidelines say. Finally, patients diagnosed with OHS should be guided to weight loss interventions with the aim of reducing body weight by 25%-30%. This can include referral for bariatric surgery in patients without contraindications.
Dr. Mokhlesi and colleagues acknowledged that all of the recommendations contained in the guideline are classed as “conditional,” based on the quality of evidence assessed.
The American Thoracic Society funded the study. Dr. Mokhlesi and 7 coauthors disclosed financial conflicts of interest, while an additional 13 coauthors had none. Disclosures can be found on the AJRCCM website.
SOURCE: Mokhlesi B et al. Am J Respir Crit Care Med. 2019;200:3,e6-e24
A blood test for elevated carbon dioxide may be used in screening adults for obesity hypoventilation syndrome, according to new guidelines.
Obese adults with sleep-disordered breathing and increased blood carbon dioxide levels during the day are likely to have obesity hypoventilation syndrome (OHS), a result of shallow or slow breathing that can lead to respiratory failure, heart failure, pulmonary hypertension, and death. Pulmonologists and sleep specialists may be the first to see and diagnose patients with OHS in the outpatient setting, while other cases are diagnosed in the hospital when patients present with hypercapnic respiratory failure.
Screening for OHS usually involves measuring arterial blood gases, which is not standard practice in outpatient clinics. Patients often remain undiagnosed and untreated until late in the course of the disease, according to the American Thoracic Society, which in August published a new diagnosis and management guideline aiming to boost early diagnosis and reduce variability in treatment (Am J Respir Crit Care Med. 2019;200:3,e6–e24).
The guideline authors, led by Babak Mokhlesi, MD, of the University of Chicago, recommend a simpler screening method – measuring serum bicarbonate only – to rule out OHS in obese patients with nighttime breathing problems.
Serum bicarbonate should be measured in obese patients with sleep-disordered breathing and a low likelihood of OHS, Dr. Mokhlesi and colleagues recommend in the guideline. If serum bicarbonate is below 27 mmol/L, it is not necessary to conduct further testing as the patient is unlikely to have OHS.
In patients whose serum bicarbonate is higher than 27 mmol/L, or who are strongly suspected of having OHS at presentation because of severe obesity or other symptoms, arterial blood gases should be measured and a sleep study conducted. The guideline authors said that there is insufficient evidence to recommend that pulse oximetry be used in the diagnostic pathway for OHS.
First-line treatment for stable, ambulatory patients with OHS should be positive airway pressure during sleep, rather than noninvasive ventilation, Dr. Mokhlesi and colleagues concluded. For patients with comorbid obstructive sleep apnea – as many as 70% of OHS patients also have OSA – the first-line treatment should be continuous positive airway pressure (CPAP) at night, the guideline states.
Patients hospitalized with respiratory failure and suspected of having OHS should be discharged with noninvasive ventilation until diagnostic procedures can be performed, along with PAP titration in a sleep lab.
In patients initially treated with CPAP who remain symptomatic or whose blood carbon dioxide does not improve, noninvasive ventilation can be tried, the guidelines say. Finally, patients diagnosed with OHS should be guided to weight loss interventions with the aim of reducing body weight by 25%-30%. This can include referral for bariatric surgery in patients without contraindications.
Dr. Mokhlesi and colleagues acknowledged that all of the recommendations contained in the guideline are classed as “conditional,” based on the quality of evidence assessed.
The American Thoracic Society funded the study. Dr. Mokhlesi and 7 coauthors disclosed financial conflicts of interest, while an additional 13 coauthors had none. Disclosures can be found on the AJRCCM website.
SOURCE: Mokhlesi B et al. Am J Respir Crit Care Med. 2019;200:3,e6-e24
A blood test for elevated carbon dioxide may be used in screening adults for obesity hypoventilation syndrome, according to new guidelines.
Obese adults with sleep-disordered breathing and increased blood carbon dioxide levels during the day are likely to have obesity hypoventilation syndrome (OHS), a result of shallow or slow breathing that can lead to respiratory failure, heart failure, pulmonary hypertension, and death. Pulmonologists and sleep specialists may be the first to see and diagnose patients with OHS in the outpatient setting, while other cases are diagnosed in the hospital when patients present with hypercapnic respiratory failure.
Screening for OHS usually involves measuring arterial blood gases, which is not standard practice in outpatient clinics. Patients often remain undiagnosed and untreated until late in the course of the disease, according to the American Thoracic Society, which in August published a new diagnosis and management guideline aiming to boost early diagnosis and reduce variability in treatment (Am J Respir Crit Care Med. 2019;200:3,e6–e24).
The guideline authors, led by Babak Mokhlesi, MD, of the University of Chicago, recommend a simpler screening method – measuring serum bicarbonate only – to rule out OHS in obese patients with nighttime breathing problems.
Serum bicarbonate should be measured in obese patients with sleep-disordered breathing and a low likelihood of OHS, Dr. Mokhlesi and colleagues recommend in the guideline. If serum bicarbonate is below 27 mmol/L, it is not necessary to conduct further testing as the patient is unlikely to have OHS.
In patients whose serum bicarbonate is higher than 27 mmol/L, or who are strongly suspected of having OHS at presentation because of severe obesity or other symptoms, arterial blood gases should be measured and a sleep study conducted. The guideline authors said that there is insufficient evidence to recommend that pulse oximetry be used in the diagnostic pathway for OHS.
First-line treatment for stable, ambulatory patients with OHS should be positive airway pressure during sleep, rather than noninvasive ventilation, Dr. Mokhlesi and colleagues concluded. For patients with comorbid obstructive sleep apnea – as many as 70% of OHS patients also have OSA – the first-line treatment should be continuous positive airway pressure (CPAP) at night, the guideline states.
Patients hospitalized with respiratory failure and suspected of having OHS should be discharged with noninvasive ventilation until diagnostic procedures can be performed, along with PAP titration in a sleep lab.
In patients initially treated with CPAP who remain symptomatic or whose blood carbon dioxide does not improve, noninvasive ventilation can be tried, the guidelines say. Finally, patients diagnosed with OHS should be guided to weight loss interventions with the aim of reducing body weight by 25%-30%. This can include referral for bariatric surgery in patients without contraindications.
Dr. Mokhlesi and colleagues acknowledged that all of the recommendations contained in the guideline are classed as “conditional,” based on the quality of evidence assessed.
The American Thoracic Society funded the study. Dr. Mokhlesi and 7 coauthors disclosed financial conflicts of interest, while an additional 13 coauthors had none. Disclosures can be found on the AJRCCM website.
SOURCE: Mokhlesi B et al. Am J Respir Crit Care Med. 2019;200:3,e6-e24
FROM THE AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
Vape lung disease cases exceed 400, 3 dead
Vitamin E acetate is one possible culprit in the mysterious vaping-associated lung disease that has killed three patients, sickened 450, and baffled clinicians and investigators all summer.
Another death may be linked to the disorder, officials said during a joint press briefing held by the Centers for Disease Control and Prevention and the Food and Drug Administration. In all, 450 potential cases have been reported and e-cigarette use confirmed in 215. Cases have occurred in 33 states and one territory. A total of 84% of the patients reported having used tetrahydrocannabinol (THC) products in e-cigarette devices.
A preliminary report on the situation by Jennifer Layden, MD, of the department of public health in Illinois and colleagues – including a preliminary case definition – was simultaneously released in the New England Journal of Medicine (2019 Sep 6. doi: 10.1056/NEJMoa1911614).
No single device or substance was common to all the cases, leading officials to issue a blanket warning against e-cigarettes, especially those containing THC.
“We believe a chemical exposure is likely related, but more information is needed to determine what substances. Some labs have identified vitamin E acetate in some samples,” said Dana Meaney-Delman, MD, MPH, incident manager, CDC 2019 Lung Injury Response. “Continued investigation is needed to identify the risk associated with a specific product or substance.”
Besides vitamin E acetate, federal labs are looking at other cannabinoids, cutting agents, diluting agents, pesticides, opioids, and toxins.
Officials also issued a general warning about the products. Youths, young people, and pregnant women should never use e-cigarettes, they cautioned, and no one should buy them from a noncertified source, a street vendor, or a social contact. Even cartridges originally obtained from a certified source should never have been altered in any way.
Dr. Layden and colleagues reported that bilateral lung infiltrates was characterized in 98% of the 53 patients hospitalized with the recently reported e-cigarette–induced lung injury. Nonspecific constitutional symptoms, including fever, chills, weight loss, and fatigue, were present in all of the patients.
Patients may show some symptoms days or even weeks before acute respiratory failure develops, and many had sought medical help before that. All presented with bilateral lung infiltrates, part of an evolving case definition. Many complained of nonspecific constitutional symptoms, including fever, chills, gastrointestinal symptoms, and weight loss. Of the patients who underwent bronchoscopy, many were diagnosed as having lipoid pneumonia, a rare condition characterized by lipid-laden macrophages.
“We don’t know the significance of the lipid-containing macrophages, and we don’t know if the lipids are endogenous or exogenous,” Dr. Meaney-Delman said.
The incidence of such cases appears to be rising rapidly, Dr. Layden noted. An epidemiologic review of cases in Illinois found that the mean monthly rate of visits related to severe respiratory illness in June-August was twice that observed during the same months last year.
SOURCE: Layden JE et al. N Engl J Med. 2019 Sep 6. doi: 1 0.1056/NEJMoa1911614.
Vitamin E acetate is one possible culprit in the mysterious vaping-associated lung disease that has killed three patients, sickened 450, and baffled clinicians and investigators all summer.
Another death may be linked to the disorder, officials said during a joint press briefing held by the Centers for Disease Control and Prevention and the Food and Drug Administration. In all, 450 potential cases have been reported and e-cigarette use confirmed in 215. Cases have occurred in 33 states and one territory. A total of 84% of the patients reported having used tetrahydrocannabinol (THC) products in e-cigarette devices.
A preliminary report on the situation by Jennifer Layden, MD, of the department of public health in Illinois and colleagues – including a preliminary case definition – was simultaneously released in the New England Journal of Medicine (2019 Sep 6. doi: 10.1056/NEJMoa1911614).
No single device or substance was common to all the cases, leading officials to issue a blanket warning against e-cigarettes, especially those containing THC.
“We believe a chemical exposure is likely related, but more information is needed to determine what substances. Some labs have identified vitamin E acetate in some samples,” said Dana Meaney-Delman, MD, MPH, incident manager, CDC 2019 Lung Injury Response. “Continued investigation is needed to identify the risk associated with a specific product or substance.”
Besides vitamin E acetate, federal labs are looking at other cannabinoids, cutting agents, diluting agents, pesticides, opioids, and toxins.
Officials also issued a general warning about the products. Youths, young people, and pregnant women should never use e-cigarettes, they cautioned, and no one should buy them from a noncertified source, a street vendor, or a social contact. Even cartridges originally obtained from a certified source should never have been altered in any way.
Dr. Layden and colleagues reported that bilateral lung infiltrates was characterized in 98% of the 53 patients hospitalized with the recently reported e-cigarette–induced lung injury. Nonspecific constitutional symptoms, including fever, chills, weight loss, and fatigue, were present in all of the patients.
Patients may show some symptoms days or even weeks before acute respiratory failure develops, and many had sought medical help before that. All presented with bilateral lung infiltrates, part of an evolving case definition. Many complained of nonspecific constitutional symptoms, including fever, chills, gastrointestinal symptoms, and weight loss. Of the patients who underwent bronchoscopy, many were diagnosed as having lipoid pneumonia, a rare condition characterized by lipid-laden macrophages.
“We don’t know the significance of the lipid-containing macrophages, and we don’t know if the lipids are endogenous or exogenous,” Dr. Meaney-Delman said.
The incidence of such cases appears to be rising rapidly, Dr. Layden noted. An epidemiologic review of cases in Illinois found that the mean monthly rate of visits related to severe respiratory illness in June-August was twice that observed during the same months last year.
SOURCE: Layden JE et al. N Engl J Med. 2019 Sep 6. doi: 1 0.1056/NEJMoa1911614.
Vitamin E acetate is one possible culprit in the mysterious vaping-associated lung disease that has killed three patients, sickened 450, and baffled clinicians and investigators all summer.
Another death may be linked to the disorder, officials said during a joint press briefing held by the Centers for Disease Control and Prevention and the Food and Drug Administration. In all, 450 potential cases have been reported and e-cigarette use confirmed in 215. Cases have occurred in 33 states and one territory. A total of 84% of the patients reported having used tetrahydrocannabinol (THC) products in e-cigarette devices.
A preliminary report on the situation by Jennifer Layden, MD, of the department of public health in Illinois and colleagues – including a preliminary case definition – was simultaneously released in the New England Journal of Medicine (2019 Sep 6. doi: 10.1056/NEJMoa1911614).
No single device or substance was common to all the cases, leading officials to issue a blanket warning against e-cigarettes, especially those containing THC.
“We believe a chemical exposure is likely related, but more information is needed to determine what substances. Some labs have identified vitamin E acetate in some samples,” said Dana Meaney-Delman, MD, MPH, incident manager, CDC 2019 Lung Injury Response. “Continued investigation is needed to identify the risk associated with a specific product or substance.”
Besides vitamin E acetate, federal labs are looking at other cannabinoids, cutting agents, diluting agents, pesticides, opioids, and toxins.
Officials also issued a general warning about the products. Youths, young people, and pregnant women should never use e-cigarettes, they cautioned, and no one should buy them from a noncertified source, a street vendor, or a social contact. Even cartridges originally obtained from a certified source should never have been altered in any way.
Dr. Layden and colleagues reported that bilateral lung infiltrates was characterized in 98% of the 53 patients hospitalized with the recently reported e-cigarette–induced lung injury. Nonspecific constitutional symptoms, including fever, chills, weight loss, and fatigue, were present in all of the patients.
Patients may show some symptoms days or even weeks before acute respiratory failure develops, and many had sought medical help before that. All presented with bilateral lung infiltrates, part of an evolving case definition. Many complained of nonspecific constitutional symptoms, including fever, chills, gastrointestinal symptoms, and weight loss. Of the patients who underwent bronchoscopy, many were diagnosed as having lipoid pneumonia, a rare condition characterized by lipid-laden macrophages.
“We don’t know the significance of the lipid-containing macrophages, and we don’t know if the lipids are endogenous or exogenous,” Dr. Meaney-Delman said.
The incidence of such cases appears to be rising rapidly, Dr. Layden noted. An epidemiologic review of cases in Illinois found that the mean monthly rate of visits related to severe respiratory illness in June-August was twice that observed during the same months last year.
SOURCE: Layden JE et al. N Engl J Med. 2019 Sep 6. doi: 1 0.1056/NEJMoa1911614.
FROM A CDC TELECONFERENCE AND NEJM