User login
Study suggests malaria is undertreated
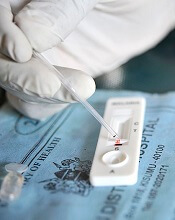
A large study suggests the use of rapid diagnostic tests (RDTs) for malaria can reduce overuse of artemisinin combination therapies (ACTs), but malaria may also go untreated.
Researchers analyzed data from more than 500,000 patient visits across malaria-endemic regions of Africa and Afghanistan.
They found that, in most settings, the introduction of RDTs improved antimalarial targeting.
However, a substantial number of patients who tested positive for malaria appeared to go untreated, and negative test results prompted a shift to antibiotic prescriptions.
Katia Bruxvoort, PhD, of London School of Hygiene & Tropical Medicine in the UK, and her colleagues reported these results in the American Journal of Tropical Medicine and Hygiene.
The researchers analyzed drug prescriptions written from 2007 to 2013 in 562,368 patient encounters documented in 10 related studies. Eight studies were conducted in sub-Saharan Africa (Cameroon, Ghana, Nigeria, Tanzania, and Uganda), and 2 were conducted in Afghanistan.
Overall, RDTs appeared to limit—though not eliminate—routine prescription of ACTs to patients presenting with fever but not malaria.
In most cases, fewer than 30% of patients who tested negative for malaria still received ACTs. However, in Cameroon and Ghana, 39% to 49% of patients who tested negative for malaria received ACTs.
“[I]n many places, a reduction in the use of ACTs was accompanied by an increase in the use of antibiotics, which may drive up the risk of antibiotic-resistant infections,” Dr Bruxvoort noted.
Overall, 75% of patients studied left the clinic with either an antibiotic or an ACT.
In most areas studied, antibiotics were given to 40% to 80% of patients who had tested negative for malaria.
The researchers believe the shift to antibiotic use after ruling out malaria may indicate that many patients and providers are not comfortable treating a fever using only supportive care (taking a fever-reducing drug and drinking plenty of fluids).
“A key challenge is that we don’t currently have a reliable way to determine which fevers are evidence of a bacterial infection that requires a specific antibiotic treatment and which fevers will resolve with supportive care only,” Dr Bruxvoort said.
In addition, Dr Bruxvoort and her colleagues were surprised to find that, in 5 of the 8 African studies, more than 20% of patients who tested positive for malaria were not prescribed ACTs.
“Drug supply issues did not seem to be a problem in most of the areas where these patients sought treatment,” Dr Bruxvoort said. “There might be other reasons either patients or providers are not using ACTs in these contexts, but the issue of undertreating malaria, even when there is clear evidence of the disease, is troubling and deserves further study.” ![]()
A large study suggests the use of rapid diagnostic tests (RDTs) for malaria can reduce overuse of artemisinin combination therapies (ACTs), but malaria may also go untreated.
Researchers analyzed data from more than 500,000 patient visits across malaria-endemic regions of Africa and Afghanistan.
They found that, in most settings, the introduction of RDTs improved antimalarial targeting.
However, a substantial number of patients who tested positive for malaria appeared to go untreated, and negative test results prompted a shift to antibiotic prescriptions.
Katia Bruxvoort, PhD, of London School of Hygiene & Tropical Medicine in the UK, and her colleagues reported these results in the American Journal of Tropical Medicine and Hygiene.
The researchers analyzed drug prescriptions written from 2007 to 2013 in 562,368 patient encounters documented in 10 related studies. Eight studies were conducted in sub-Saharan Africa (Cameroon, Ghana, Nigeria, Tanzania, and Uganda), and 2 were conducted in Afghanistan.
Overall, RDTs appeared to limit—though not eliminate—routine prescription of ACTs to patients presenting with fever but not malaria.
In most cases, fewer than 30% of patients who tested negative for malaria still received ACTs. However, in Cameroon and Ghana, 39% to 49% of patients who tested negative for malaria received ACTs.
“[I]n many places, a reduction in the use of ACTs was accompanied by an increase in the use of antibiotics, which may drive up the risk of antibiotic-resistant infections,” Dr Bruxvoort noted.
Overall, 75% of patients studied left the clinic with either an antibiotic or an ACT.
In most areas studied, antibiotics were given to 40% to 80% of patients who had tested negative for malaria.
The researchers believe the shift to antibiotic use after ruling out malaria may indicate that many patients and providers are not comfortable treating a fever using only supportive care (taking a fever-reducing drug and drinking plenty of fluids).
“A key challenge is that we don’t currently have a reliable way to determine which fevers are evidence of a bacterial infection that requires a specific antibiotic treatment and which fevers will resolve with supportive care only,” Dr Bruxvoort said.
In addition, Dr Bruxvoort and her colleagues were surprised to find that, in 5 of the 8 African studies, more than 20% of patients who tested positive for malaria were not prescribed ACTs.
“Drug supply issues did not seem to be a problem in most of the areas where these patients sought treatment,” Dr Bruxvoort said. “There might be other reasons either patients or providers are not using ACTs in these contexts, but the issue of undertreating malaria, even when there is clear evidence of the disease, is troubling and deserves further study.” ![]()
A large study suggests the use of rapid diagnostic tests (RDTs) for malaria can reduce overuse of artemisinin combination therapies (ACTs), but malaria may also go untreated.
Researchers analyzed data from more than 500,000 patient visits across malaria-endemic regions of Africa and Afghanistan.
They found that, in most settings, the introduction of RDTs improved antimalarial targeting.
However, a substantial number of patients who tested positive for malaria appeared to go untreated, and negative test results prompted a shift to antibiotic prescriptions.
Katia Bruxvoort, PhD, of London School of Hygiene & Tropical Medicine in the UK, and her colleagues reported these results in the American Journal of Tropical Medicine and Hygiene.
The researchers analyzed drug prescriptions written from 2007 to 2013 in 562,368 patient encounters documented in 10 related studies. Eight studies were conducted in sub-Saharan Africa (Cameroon, Ghana, Nigeria, Tanzania, and Uganda), and 2 were conducted in Afghanistan.
Overall, RDTs appeared to limit—though not eliminate—routine prescription of ACTs to patients presenting with fever but not malaria.
In most cases, fewer than 30% of patients who tested negative for malaria still received ACTs. However, in Cameroon and Ghana, 39% to 49% of patients who tested negative for malaria received ACTs.
“[I]n many places, a reduction in the use of ACTs was accompanied by an increase in the use of antibiotics, which may drive up the risk of antibiotic-resistant infections,” Dr Bruxvoort noted.
Overall, 75% of patients studied left the clinic with either an antibiotic or an ACT.
In most areas studied, antibiotics were given to 40% to 80% of patients who had tested negative for malaria.
The researchers believe the shift to antibiotic use after ruling out malaria may indicate that many patients and providers are not comfortable treating a fever using only supportive care (taking a fever-reducing drug and drinking plenty of fluids).
“A key challenge is that we don’t currently have a reliable way to determine which fevers are evidence of a bacterial infection that requires a specific antibiotic treatment and which fevers will resolve with supportive care only,” Dr Bruxvoort said.
In addition, Dr Bruxvoort and her colleagues were surprised to find that, in 5 of the 8 African studies, more than 20% of patients who tested positive for malaria were not prescribed ACTs.
“Drug supply issues did not seem to be a problem in most of the areas where these patients sought treatment,” Dr Bruxvoort said. “There might be other reasons either patients or providers are not using ACTs in these contexts, but the issue of undertreating malaria, even when there is clear evidence of the disease, is troubling and deserves further study.” ![]()
Advanced cancer patients have lower survival after cardiac arrest
A new study suggests patients with advanced cancer who suffer cardiac arrest in the hospital have a survival rate of less than 10%, which is about half the rate of patients without cancer who suffer cardiac arrest.
This finding helps to clear up some myths about cardiac arrest survival and can be used as a guidepost when hospitalized cancer patients and their families consider do-not-resuscitate (DNR) orders, said Jeffrey T. Bruckel, MD, of the University of Rochester Medical Center in New York.
“We’re hopeful that our study, in some way, will help doctors and cancer patients make more informed decisions about the end of life,” Dr Bruckel said. “It’s very important to have early, frank discussions around the goals of care.”
Dr Bruckel and his colleagues published their study in the Journal of Oncology Practice.
The researchers used a US-wide resuscitation registry to evaluate survival after cardiac arrest in patients treated at 369 hospitals.
The study excluded patients with implantable defibrillators and those who were admitted for surgery, emergency room treatment, rehabilitation, or treatment from cardiac catheterization labs or interventional radiology.
Of the 47,157 eligible patients who experienced cardiac arrest, 14% (n=6585) had advanced cancer, including hematologic malignancies.
After cardiac arrest, 57.5% of the advanced cancer patients were resuscitated successfully, as were 63% of non-cancer patients (P<0.001).
After resuscitation, 9.6% of the cancer patients survived to be discharged, compared to 19.2% of non-cancer patients (P<0.001).
When the researchers adjusted their analysis for potential confounders, results were similar. The rate of successful resuscitation was 52.3% in advanced cancer patients and 56.6% in non-cancer patients (P<0.001). The rate of survival to discharge was 7.4% and 13.4%, respectively (P<0.001).
Dr Bruckel said there was no evidence to suggest that patients with advanced cancer received less aggressive resuscitation care.
However, there was a significant difference in the mean duration of resuscitation time among non-survivors with cancer—22.5 minutes—and non-survivors without cancer—24.2 minutes (P<0.001). After adjustment, the mean duration of resuscitation was 22.5 minutes and 24.1 minutes, respectively (P<0.001).
Cancer patients were more likely than those without cancer to sign DNR orders after resuscitation—55.6% and 43%, respectively (P<0.001). Results were similar after adjustment—50.4% and 41.6%, respectively (P<0.001).
Dr Bruckel and his colleagues said there were several limitations to this study, including a lack of detailed data on the types of advanced cancer and cancer treatments being given at the time of cardiac arrest.
Therefore, the next step in advancing this work is to gather data on the types of cancer diagnosis and treatment plans of patients who undergo in-hospital cardiac arrest.
Dr Bruckel also believes it is important to know how patients feel about this data and how both patients and physicians are using this data in decision-making.
“A large component of end-of-life care involves patient and family care decision-making, and a lot of that is driven by the routine discussions that we have,” Dr Bruckel said. “Not every patient is going to want detailed information, but for those that do, it’s important to have it. It’s important to tell them what we know.” ![]()
A new study suggests patients with advanced cancer who suffer cardiac arrest in the hospital have a survival rate of less than 10%, which is about half the rate of patients without cancer who suffer cardiac arrest.
This finding helps to clear up some myths about cardiac arrest survival and can be used as a guidepost when hospitalized cancer patients and their families consider do-not-resuscitate (DNR) orders, said Jeffrey T. Bruckel, MD, of the University of Rochester Medical Center in New York.
“We’re hopeful that our study, in some way, will help doctors and cancer patients make more informed decisions about the end of life,” Dr Bruckel said. “It’s very important to have early, frank discussions around the goals of care.”
Dr Bruckel and his colleagues published their study in the Journal of Oncology Practice.
The researchers used a US-wide resuscitation registry to evaluate survival after cardiac arrest in patients treated at 369 hospitals.
The study excluded patients with implantable defibrillators and those who were admitted for surgery, emergency room treatment, rehabilitation, or treatment from cardiac catheterization labs or interventional radiology.
Of the 47,157 eligible patients who experienced cardiac arrest, 14% (n=6585) had advanced cancer, including hematologic malignancies.
After cardiac arrest, 57.5% of the advanced cancer patients were resuscitated successfully, as were 63% of non-cancer patients (P<0.001).
After resuscitation, 9.6% of the cancer patients survived to be discharged, compared to 19.2% of non-cancer patients (P<0.001).
When the researchers adjusted their analysis for potential confounders, results were similar. The rate of successful resuscitation was 52.3% in advanced cancer patients and 56.6% in non-cancer patients (P<0.001). The rate of survival to discharge was 7.4% and 13.4%, respectively (P<0.001).
Dr Bruckel said there was no evidence to suggest that patients with advanced cancer received less aggressive resuscitation care.
However, there was a significant difference in the mean duration of resuscitation time among non-survivors with cancer—22.5 minutes—and non-survivors without cancer—24.2 minutes (P<0.001). After adjustment, the mean duration of resuscitation was 22.5 minutes and 24.1 minutes, respectively (P<0.001).
Cancer patients were more likely than those without cancer to sign DNR orders after resuscitation—55.6% and 43%, respectively (P<0.001). Results were similar after adjustment—50.4% and 41.6%, respectively (P<0.001).
Dr Bruckel and his colleagues said there were several limitations to this study, including a lack of detailed data on the types of advanced cancer and cancer treatments being given at the time of cardiac arrest.
Therefore, the next step in advancing this work is to gather data on the types of cancer diagnosis and treatment plans of patients who undergo in-hospital cardiac arrest.
Dr Bruckel also believes it is important to know how patients feel about this data and how both patients and physicians are using this data in decision-making.
“A large component of end-of-life care involves patient and family care decision-making, and a lot of that is driven by the routine discussions that we have,” Dr Bruckel said. “Not every patient is going to want detailed information, but for those that do, it’s important to have it. It’s important to tell them what we know.” ![]()
A new study suggests patients with advanced cancer who suffer cardiac arrest in the hospital have a survival rate of less than 10%, which is about half the rate of patients without cancer who suffer cardiac arrest.
This finding helps to clear up some myths about cardiac arrest survival and can be used as a guidepost when hospitalized cancer patients and their families consider do-not-resuscitate (DNR) orders, said Jeffrey T. Bruckel, MD, of the University of Rochester Medical Center in New York.
“We’re hopeful that our study, in some way, will help doctors and cancer patients make more informed decisions about the end of life,” Dr Bruckel said. “It’s very important to have early, frank discussions around the goals of care.”
Dr Bruckel and his colleagues published their study in the Journal of Oncology Practice.
The researchers used a US-wide resuscitation registry to evaluate survival after cardiac arrest in patients treated at 369 hospitals.
The study excluded patients with implantable defibrillators and those who were admitted for surgery, emergency room treatment, rehabilitation, or treatment from cardiac catheterization labs or interventional radiology.
Of the 47,157 eligible patients who experienced cardiac arrest, 14% (n=6585) had advanced cancer, including hematologic malignancies.
After cardiac arrest, 57.5% of the advanced cancer patients were resuscitated successfully, as were 63% of non-cancer patients (P<0.001).
After resuscitation, 9.6% of the cancer patients survived to be discharged, compared to 19.2% of non-cancer patients (P<0.001).
When the researchers adjusted their analysis for potential confounders, results were similar. The rate of successful resuscitation was 52.3% in advanced cancer patients and 56.6% in non-cancer patients (P<0.001). The rate of survival to discharge was 7.4% and 13.4%, respectively (P<0.001).
Dr Bruckel said there was no evidence to suggest that patients with advanced cancer received less aggressive resuscitation care.
However, there was a significant difference in the mean duration of resuscitation time among non-survivors with cancer—22.5 minutes—and non-survivors without cancer—24.2 minutes (P<0.001). After adjustment, the mean duration of resuscitation was 22.5 minutes and 24.1 minutes, respectively (P<0.001).
Cancer patients were more likely than those without cancer to sign DNR orders after resuscitation—55.6% and 43%, respectively (P<0.001). Results were similar after adjustment—50.4% and 41.6%, respectively (P<0.001).
Dr Bruckel and his colleagues said there were several limitations to this study, including a lack of detailed data on the types of advanced cancer and cancer treatments being given at the time of cardiac arrest.
Therefore, the next step in advancing this work is to gather data on the types of cancer diagnosis and treatment plans of patients who undergo in-hospital cardiac arrest.
Dr Bruckel also believes it is important to know how patients feel about this data and how both patients and physicians are using this data in decision-making.
“A large component of end-of-life care involves patient and family care decision-making, and a lot of that is driven by the routine discussions that we have,” Dr Bruckel said. “Not every patient is going to want detailed information, but for those that do, it’s important to have it. It’s important to tell them what we know.” ![]()
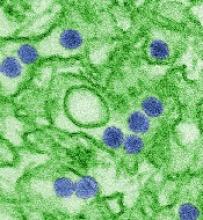
FDA issues EUA for Zika virus test
The US Food and Drug Administration (FDA) has issued an emergency use authorization (EUA) for Thermo Fisher Scientific’s TaqPath Zika Virus Kit.
This means the TaqPath Zika Virus Kit is authorized for the qualitative detection of RNA from Zika virus and diagnosis of Zika virus infection in human serum and urine (collected alongside a patient-matched serum specimen) from individuals meeting the US Centers for Disease Control and Prevention’s criteria for testing.
The EUA does not mean the TaqPath Zika Virus Kit is FDA cleared or approved.
An EUA allows for the use of unapproved medical products or unapproved uses of approved medical products in an emergency. The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
The EUA for the TaqPath Zika Virus Kit means the test is only authorized as long as circumstances exist to justify the emergency use of in vitro diagnostics for the detection of Zika virus, unless the authorization is terminated or revoked sooner.
Testing using the TaqPath Zika Virus Kit is authorized to be conducted by laboratories in the US that are certified under the Clinical Laboratory Improvement Amendments of 1988, 42 U.S.C. § 263a, to perform high complexity tests, or by similarly qualified non-US laboratories.
More information on the TaqPath Zika Virus Kit and other Zika tests granted EUAs can be found on the FDA’s EUA page. ![]()
The US Food and Drug Administration (FDA) has issued an emergency use authorization (EUA) for Thermo Fisher Scientific’s TaqPath Zika Virus Kit.
This means the TaqPath Zika Virus Kit is authorized for the qualitative detection of RNA from Zika virus and diagnosis of Zika virus infection in human serum and urine (collected alongside a patient-matched serum specimen) from individuals meeting the US Centers for Disease Control and Prevention’s criteria for testing.
The EUA does not mean the TaqPath Zika Virus Kit is FDA cleared or approved.
An EUA allows for the use of unapproved medical products or unapproved uses of approved medical products in an emergency. The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
The EUA for the TaqPath Zika Virus Kit means the test is only authorized as long as circumstances exist to justify the emergency use of in vitro diagnostics for the detection of Zika virus, unless the authorization is terminated or revoked sooner.
Testing using the TaqPath Zika Virus Kit is authorized to be conducted by laboratories in the US that are certified under the Clinical Laboratory Improvement Amendments of 1988, 42 U.S.C. § 263a, to perform high complexity tests, or by similarly qualified non-US laboratories.
More information on the TaqPath Zika Virus Kit and other Zika tests granted EUAs can be found on the FDA’s EUA page. ![]()
The US Food and Drug Administration (FDA) has issued an emergency use authorization (EUA) for Thermo Fisher Scientific’s TaqPath Zika Virus Kit.
This means the TaqPath Zika Virus Kit is authorized for the qualitative detection of RNA from Zika virus and diagnosis of Zika virus infection in human serum and urine (collected alongside a patient-matched serum specimen) from individuals meeting the US Centers for Disease Control and Prevention’s criteria for testing.
The EUA does not mean the TaqPath Zika Virus Kit is FDA cleared or approved.
An EUA allows for the use of unapproved medical products or unapproved uses of approved medical products in an emergency. The products must be used to diagnose, treat, or prevent serious or life-threatening conditions caused by chemical, biological, radiological, or nuclear threat agents, when there are no adequate alternatives.
The EUA for the TaqPath Zika Virus Kit means the test is only authorized as long as circumstances exist to justify the emergency use of in vitro diagnostics for the detection of Zika virus, unless the authorization is terminated or revoked sooner.
Testing using the TaqPath Zika Virus Kit is authorized to be conducted by laboratories in the US that are certified under the Clinical Laboratory Improvement Amendments of 1988, 42 U.S.C. § 263a, to perform high complexity tests, or by similarly qualified non-US laboratories.
More information on the TaqPath Zika Virus Kit and other Zika tests granted EUAs can be found on the FDA’s EUA page. ![]()
Delirium linked to early death in advanced cancer patients
A diagnosis of delirium during a visit to the emergency department (ED) is a poor prognostic factor for patients with advanced cancer, according to research published in The Oncologist.
The study showed that patients with advanced cancer who were diagnosed with delirium during an ED visit were more likely to be admitted to the hospital or intensive care unit (ICU) and more likely to die earlier than patients without delirium.
This shows the importance of accurately diagnosing delirium in advanced cancer patients, said Ahmed Elsayem, MD, of the University of Texas MD Anderson Cancer Center in Houston.
Previous studies have shown that delirium is associated with poor survival in advanced cancer patients being treated in ICUs or receiving palliative care in hospices, but no one had investigated whether the same was true for patients visiting EDs.
“To the best our knowledge, this is the first study to show the poor survival of advanced cancer patients in the emergency department setting,” Dr Elsayem said.
He and his colleagues previously conducted a study in which they assessed the frequency of delirium in advanced cancer patients visiting the ED at MD Anderson. The researchers tested for delirium using 2 questionnaires—the Confusion Assessment Method (CAM) and Memorial Delirium Assessment Scale (MDAS).
Questioning 243 patients in total, the team found that 44 patients, or 18%, were suffering with delirium according to at least 1 of the questionnaires.
In the current study, Dr Elsayem and his colleagues determined how many of these cancer patients, with and without delirium, were subsequently admitted to hospital and ICUs, as well as how long the patients lived after their visit to the ED.
Results
The rate of hospitalization was 82% among patients with delirium according to CAM and/or MDAS, 77% among patients with delirium according to MDAS only, and 49% among patients without delirium (P=0.0013). Rates of ICU admission were 18%, 14%, and 2%, respectively (P=0.0004).
The median overall survival was 1.23 months for patients with delirium according to CAM and/or MDAS, 4.70 months for patients with delirium according to MDAS only, and 10.45 months for patients without delirium. The difference between the patients with and without delirium was significant (P<0.0001).
Given the influence delirium appears to have on survival, Dr Elsayem said prompt diagnosis and management in hospital EDs is essential.
He noted that, in many cases, delirium in advanced cancer patients can be resolved by simply stopping or modifying their medication and treating any associated infections.
“Treating the triggers if known—such as stopping medications—is the main treatment for an episode of delirium,” Dr Elsayem said.
He also suggested that further research needs to be done on this topic, including conducting similar studies on delirium in advanced cancer patients in other EDs and with larger groups of patients. ![]()
A diagnosis of delirium during a visit to the emergency department (ED) is a poor prognostic factor for patients with advanced cancer, according to research published in The Oncologist.
The study showed that patients with advanced cancer who were diagnosed with delirium during an ED visit were more likely to be admitted to the hospital or intensive care unit (ICU) and more likely to die earlier than patients without delirium.
This shows the importance of accurately diagnosing delirium in advanced cancer patients, said Ahmed Elsayem, MD, of the University of Texas MD Anderson Cancer Center in Houston.
Previous studies have shown that delirium is associated with poor survival in advanced cancer patients being treated in ICUs or receiving palliative care in hospices, but no one had investigated whether the same was true for patients visiting EDs.
“To the best our knowledge, this is the first study to show the poor survival of advanced cancer patients in the emergency department setting,” Dr Elsayem said.
He and his colleagues previously conducted a study in which they assessed the frequency of delirium in advanced cancer patients visiting the ED at MD Anderson. The researchers tested for delirium using 2 questionnaires—the Confusion Assessment Method (CAM) and Memorial Delirium Assessment Scale (MDAS).
Questioning 243 patients in total, the team found that 44 patients, or 18%, were suffering with delirium according to at least 1 of the questionnaires.
In the current study, Dr Elsayem and his colleagues determined how many of these cancer patients, with and without delirium, were subsequently admitted to hospital and ICUs, as well as how long the patients lived after their visit to the ED.
Results
The rate of hospitalization was 82% among patients with delirium according to CAM and/or MDAS, 77% among patients with delirium according to MDAS only, and 49% among patients without delirium (P=0.0013). Rates of ICU admission were 18%, 14%, and 2%, respectively (P=0.0004).
The median overall survival was 1.23 months for patients with delirium according to CAM and/or MDAS, 4.70 months for patients with delirium according to MDAS only, and 10.45 months for patients without delirium. The difference between the patients with and without delirium was significant (P<0.0001).
Given the influence delirium appears to have on survival, Dr Elsayem said prompt diagnosis and management in hospital EDs is essential.
He noted that, in many cases, delirium in advanced cancer patients can be resolved by simply stopping or modifying their medication and treating any associated infections.
“Treating the triggers if known—such as stopping medications—is the main treatment for an episode of delirium,” Dr Elsayem said.
He also suggested that further research needs to be done on this topic, including conducting similar studies on delirium in advanced cancer patients in other EDs and with larger groups of patients. ![]()
A diagnosis of delirium during a visit to the emergency department (ED) is a poor prognostic factor for patients with advanced cancer, according to research published in The Oncologist.
The study showed that patients with advanced cancer who were diagnosed with delirium during an ED visit were more likely to be admitted to the hospital or intensive care unit (ICU) and more likely to die earlier than patients without delirium.
This shows the importance of accurately diagnosing delirium in advanced cancer patients, said Ahmed Elsayem, MD, of the University of Texas MD Anderson Cancer Center in Houston.
Previous studies have shown that delirium is associated with poor survival in advanced cancer patients being treated in ICUs or receiving palliative care in hospices, but no one had investigated whether the same was true for patients visiting EDs.
“To the best our knowledge, this is the first study to show the poor survival of advanced cancer patients in the emergency department setting,” Dr Elsayem said.
He and his colleagues previously conducted a study in which they assessed the frequency of delirium in advanced cancer patients visiting the ED at MD Anderson. The researchers tested for delirium using 2 questionnaires—the Confusion Assessment Method (CAM) and Memorial Delirium Assessment Scale (MDAS).
Questioning 243 patients in total, the team found that 44 patients, or 18%, were suffering with delirium according to at least 1 of the questionnaires.
In the current study, Dr Elsayem and his colleagues determined how many of these cancer patients, with and without delirium, were subsequently admitted to hospital and ICUs, as well as how long the patients lived after their visit to the ED.
Results
The rate of hospitalization was 82% among patients with delirium according to CAM and/or MDAS, 77% among patients with delirium according to MDAS only, and 49% among patients without delirium (P=0.0013). Rates of ICU admission were 18%, 14%, and 2%, respectively (P=0.0004).
The median overall survival was 1.23 months for patients with delirium according to CAM and/or MDAS, 4.70 months for patients with delirium according to MDAS only, and 10.45 months for patients without delirium. The difference between the patients with and without delirium was significant (P<0.0001).
Given the influence delirium appears to have on survival, Dr Elsayem said prompt diagnosis and management in hospital EDs is essential.
He noted that, in many cases, delirium in advanced cancer patients can be resolved by simply stopping or modifying their medication and treating any associated infections.
“Treating the triggers if known—such as stopping medications—is the main treatment for an episode of delirium,” Dr Elsayem said.
He also suggested that further research needs to be done on this topic, including conducting similar studies on delirium in advanced cancer patients in other EDs and with larger groups of patients. ![]()
Thalassemia case provides insight into history of malaria
The earliest documented case of β-thalassemia in Sardinia suggests malaria was widespread on the island long before the Middle Ages, according to researchers.
The team noted that Sardinia has one of the highest incidence rates of β-thalassemia in Europe due to its long history of endemic malaria.
However, it has been assumed that malaria was only endemic on the island since the Middle Ages (500-1500 CE).
New research, published in the American Journal of Physical Anthropology, suggests malaria was probably already endemic on Sardinia during the Roman period.
Since ancient DNA of malaria is difficult to extract, the researchers studied thalassemia and other genetic adaptations in its place.
The team studied a thalassemia allele called cod39 β-thalassemia, which is dominant on Sardinia. They were able to confirm the presence of the cod39 allele in the 2000-year-old (approximately 300 BCE to 100 CE) remains of a Roman man.
“This is the very first documented case of the genetic adaptation to malaria on Sardinia,” said study author Claudia Vigano, of the Institute for Evolutionary Medicine of the University of Zurich in Switzerland.
“We also discovered that the person was genetically a Sardinian in all probability and not an immigrant from another area.”
“Our study shows the importance of a multidisciplinary approach to history,” said Abigail Bouwman, also of the Institute for Evolutionary Medicine of the University of Zurich.
“We are researching the evolution of today’s diseases, such as malaria, to explain why the human body becomes sick at all and how adaptations occur.” ![]()
The earliest documented case of β-thalassemia in Sardinia suggests malaria was widespread on the island long before the Middle Ages, according to researchers.
The team noted that Sardinia has one of the highest incidence rates of β-thalassemia in Europe due to its long history of endemic malaria.
However, it has been assumed that malaria was only endemic on the island since the Middle Ages (500-1500 CE).
New research, published in the American Journal of Physical Anthropology, suggests malaria was probably already endemic on Sardinia during the Roman period.
Since ancient DNA of malaria is difficult to extract, the researchers studied thalassemia and other genetic adaptations in its place.
The team studied a thalassemia allele called cod39 β-thalassemia, which is dominant on Sardinia. They were able to confirm the presence of the cod39 allele in the 2000-year-old (approximately 300 BCE to 100 CE) remains of a Roman man.
“This is the very first documented case of the genetic adaptation to malaria on Sardinia,” said study author Claudia Vigano, of the Institute for Evolutionary Medicine of the University of Zurich in Switzerland.
“We also discovered that the person was genetically a Sardinian in all probability and not an immigrant from another area.”
“Our study shows the importance of a multidisciplinary approach to history,” said Abigail Bouwman, also of the Institute for Evolutionary Medicine of the University of Zurich.
“We are researching the evolution of today’s diseases, such as malaria, to explain why the human body becomes sick at all and how adaptations occur.” ![]()
The earliest documented case of β-thalassemia in Sardinia suggests malaria was widespread on the island long before the Middle Ages, according to researchers.
The team noted that Sardinia has one of the highest incidence rates of β-thalassemia in Europe due to its long history of endemic malaria.
However, it has been assumed that malaria was only endemic on the island since the Middle Ages (500-1500 CE).
New research, published in the American Journal of Physical Anthropology, suggests malaria was probably already endemic on Sardinia during the Roman period.
Since ancient DNA of malaria is difficult to extract, the researchers studied thalassemia and other genetic adaptations in its place.
The team studied a thalassemia allele called cod39 β-thalassemia, which is dominant on Sardinia. They were able to confirm the presence of the cod39 allele in the 2000-year-old (approximately 300 BCE to 100 CE) remains of a Roman man.
“This is the very first documented case of the genetic adaptation to malaria on Sardinia,” said study author Claudia Vigano, of the Institute for Evolutionary Medicine of the University of Zurich in Switzerland.
“We also discovered that the person was genetically a Sardinian in all probability and not an immigrant from another area.”
“Our study shows the importance of a multidisciplinary approach to history,” said Abigail Bouwman, also of the Institute for Evolutionary Medicine of the University of Zurich.
“We are researching the evolution of today’s diseases, such as malaria, to explain why the human body becomes sick at all and how adaptations occur.” ![]()
ASCO updates guidelines on antiemetic use in cancer patients
The American Society of Clinical Oncology (ASCO) has updated its clinical practice guidelines on the use of antiemetics in cancer patients.
The update, published in the Journal of Clinical Oncology, provides new evidence-based information on the appropriate use of olanzapine, NK1 receptor antagonists, and dexamethasone.
“The adverse impact of inadequately controlled nausea and vomiting on patients’ quality of life is well documented,” said Paul J. Hesketh, MD, co-chair of the ASCO expert panel that updated the guidelines.
“By following the ASCO antiemetics guideline, clinicians have the opportunity to improve patients’ quality of life by minimizing treatment-induced emesis.”
To update ASCO’s guidelines on antiemetics, the expert panel conducted a systematic review of the medical literature published between November 2009 and June 2016. The panel included members with expertise in medical oncology, radiation oncology, nursing, pharmacy, and health services research, as well as a patient representative.
“Tremendous progress has been realized over the last 25 years in the prevention of chemotherapy-induced nausea and vomiting with the introduction of new classes of antiemetic agents,” said Mark G. Kris, MD, co-chair of the expert panel that updated the guidelines.
“The full benefit of these treatment advances will only be realized, however, if evidence-based guidelines are fully implemented.”
Key recommendations in the updated guidelines include:
For adults receiving chemotherapy with a high risk for nausea and vomiting (eg, cisplatin or the combination of cyclophosphamide and an anthracycline), olanzapine should be added to standard antiemetic regimens (the combination of a 5-HT3 receptor antagonist, an NK1 receptor antagonist, and dexamethasone). Olanzapine also helps individuals who experience symptoms despite receiving medicines to prevent vomiting before chemotherapy is given.
For adults receiving carboplatin-based chemotherapy or high-dose chemotherapy and children receiving chemotherapy with a high risk for nausea and vomiting, an NK1 receptor antagonist should be added to the standard antiemetic regimen (the combination of 5-HT3 receptor antagonist and dexamethasone).
Dexamethasone treatment can be limited to the day of chemotherapy administration in patients receiving an anthracycline and cyclophosphamide.
Dronabinol and nabilone, cannabinoids approved by the US Food and Drug Administration, can be used to treat nausea and vomiting that is resistant to standard antiemetic therapies. Evidence remains insufficient to recommend medical marijuana for either prevention or treatment of nausea and vomiting in patients with cancer receiving chemotherapy or radiation therapy. ![]()
The American Society of Clinical Oncology (ASCO) has updated its clinical practice guidelines on the use of antiemetics in cancer patients.
The update, published in the Journal of Clinical Oncology, provides new evidence-based information on the appropriate use of olanzapine, NK1 receptor antagonists, and dexamethasone.
“The adverse impact of inadequately controlled nausea and vomiting on patients’ quality of life is well documented,” said Paul J. Hesketh, MD, co-chair of the ASCO expert panel that updated the guidelines.
“By following the ASCO antiemetics guideline, clinicians have the opportunity to improve patients’ quality of life by minimizing treatment-induced emesis.”
To update ASCO’s guidelines on antiemetics, the expert panel conducted a systematic review of the medical literature published between November 2009 and June 2016. The panel included members with expertise in medical oncology, radiation oncology, nursing, pharmacy, and health services research, as well as a patient representative.
“Tremendous progress has been realized over the last 25 years in the prevention of chemotherapy-induced nausea and vomiting with the introduction of new classes of antiemetic agents,” said Mark G. Kris, MD, co-chair of the expert panel that updated the guidelines.
“The full benefit of these treatment advances will only be realized, however, if evidence-based guidelines are fully implemented.”
Key recommendations in the updated guidelines include:
For adults receiving chemotherapy with a high risk for nausea and vomiting (eg, cisplatin or the combination of cyclophosphamide and an anthracycline), olanzapine should be added to standard antiemetic regimens (the combination of a 5-HT3 receptor antagonist, an NK1 receptor antagonist, and dexamethasone). Olanzapine also helps individuals who experience symptoms despite receiving medicines to prevent vomiting before chemotherapy is given.
For adults receiving carboplatin-based chemotherapy or high-dose chemotherapy and children receiving chemotherapy with a high risk for nausea and vomiting, an NK1 receptor antagonist should be added to the standard antiemetic regimen (the combination of 5-HT3 receptor antagonist and dexamethasone).
Dexamethasone treatment can be limited to the day of chemotherapy administration in patients receiving an anthracycline and cyclophosphamide.
Dronabinol and nabilone, cannabinoids approved by the US Food and Drug Administration, can be used to treat nausea and vomiting that is resistant to standard antiemetic therapies. Evidence remains insufficient to recommend medical marijuana for either prevention or treatment of nausea and vomiting in patients with cancer receiving chemotherapy or radiation therapy. ![]()
The American Society of Clinical Oncology (ASCO) has updated its clinical practice guidelines on the use of antiemetics in cancer patients.
The update, published in the Journal of Clinical Oncology, provides new evidence-based information on the appropriate use of olanzapine, NK1 receptor antagonists, and dexamethasone.
“The adverse impact of inadequately controlled nausea and vomiting on patients’ quality of life is well documented,” said Paul J. Hesketh, MD, co-chair of the ASCO expert panel that updated the guidelines.
“By following the ASCO antiemetics guideline, clinicians have the opportunity to improve patients’ quality of life by minimizing treatment-induced emesis.”
To update ASCO’s guidelines on antiemetics, the expert panel conducted a systematic review of the medical literature published between November 2009 and June 2016. The panel included members with expertise in medical oncology, radiation oncology, nursing, pharmacy, and health services research, as well as a patient representative.
“Tremendous progress has been realized over the last 25 years in the prevention of chemotherapy-induced nausea and vomiting with the introduction of new classes of antiemetic agents,” said Mark G. Kris, MD, co-chair of the expert panel that updated the guidelines.
“The full benefit of these treatment advances will only be realized, however, if evidence-based guidelines are fully implemented.”
Key recommendations in the updated guidelines include:
For adults receiving chemotherapy with a high risk for nausea and vomiting (eg, cisplatin or the combination of cyclophosphamide and an anthracycline), olanzapine should be added to standard antiemetic regimens (the combination of a 5-HT3 receptor antagonist, an NK1 receptor antagonist, and dexamethasone). Olanzapine also helps individuals who experience symptoms despite receiving medicines to prevent vomiting before chemotherapy is given.
For adults receiving carboplatin-based chemotherapy or high-dose chemotherapy and children receiving chemotherapy with a high risk for nausea and vomiting, an NK1 receptor antagonist should be added to the standard antiemetic regimen (the combination of 5-HT3 receptor antagonist and dexamethasone).
Dexamethasone treatment can be limited to the day of chemotherapy administration in patients receiving an anthracycline and cyclophosphamide.
Dronabinol and nabilone, cannabinoids approved by the US Food and Drug Administration, can be used to treat nausea and vomiting that is resistant to standard antiemetic therapies. Evidence remains insufficient to recommend medical marijuana for either prevention or treatment of nausea and vomiting in patients with cancer receiving chemotherapy or radiation therapy. ![]()
Survey reveals change in public perception of clinical trials
More Americans are viewing clinical trials in a positive light, according to a survey commissioned by Research!America and the Association of Clinical Research Organizations (ACRO).
The results of the survey, which included 1000 participants and was conducted this month, reveal a shift in public attitudes about clinical trials since a similar survey was commissioned in 2013.
Thirty-seven percent of respondents involved in the current survey said they would “very likely” enroll in a clinical trial if their doctor recommended it. This represents an 11% increase from 2013.
Eighty-four percent of current survey respondents said they are willing to share personal health information, assuming that appropriate privacy protections are in place, so researchers can better understand diseases and develop new ways to prevent, treat, and cure them. This is a 10% increase from 2013.
When asked how much they admire people who volunteer for clinical trials, 46% of current respondents said “a great deal,” which is a 9% increase from 2013.
“More and more Americans appear to recognize the value of clinical trials—a very positive sign—but stubborn barriers to participation remain in place,” said Mary Woolley, president and CEO of Research!America.
“Development of incentives to drive more discussions between patients and healthcare professionals about the importance of participating in trials could encourage both ill and healthy individuals to view this as a routine health behavior.”
“We are pleased to have joined with Research!America in commissioning this important survey and gratified that the public’s knowledge of and attitudes toward clinical trials have moved in positive directions since 2013,” said Doug Peddicord, executive director of ACRO.
“The option to participate in a clinical trial, when appropriate, should be a routine part of the healthcare encounter, and ACRO will continue to work with Research!America and others to spread that message to doctors and patients alike.”
Survey results
The survey of 1000 US adults was conducted by Zogby Analytics for Research!America and ACRO in July 2017. The margin of error is +/- 3.1 percentage points.
Ninety percent of survey respondents said clinical trials are important to advancing science, and 87% said trials are important to improving the nation’s health. Seventy-five percent said taking part in clinical trials is as valuable to the US healthcare system as giving blood.
Eighty-six percent of respondents said healthcare professionals should discuss clinical trials with patients diagnosed with a disease as part of their standard care.
And 44% of respondents said clinical trial participation should be a routine health behavior, whether a person is healthy or ill, similar to getting an annual checkup with a healthcare provider.
Men (48%) were significantly more likely than women (39%) to say trial participation should be routine. A larger percentage of 18- to 29-year-olds (53%) and 30- to 49-year olds (48%) were in favor of routine trial participation, compared to people ages 50 to 64 (38%) and those 65 and older (34%).
Eighty percent of respondents said they had heard of a clinical trial, and 18% said they or someone in their family had participated in one.
Seventy-four percent of respondents said they would participate in a clinical trial if asked by someone they trust.
However, respondents were split on whether it’s important for everyone to take part in a clinical trial if asked. Forty-four percent said it is important, 45% disagreed, and 12% were not sure.
More than half of respondents (55%) said people don’t participate in clinical trials because of lack of awareness and information, 43% said it’s because trials are viewed as “too risky,” 41% said it’s due to a lack of information about the process, 38% said it’s due to a lack of trust, and 34% said it’s due to the risk of adverse health effects.
Nearly two-thirds of respondents (64%) said a doctor or healthcare provider is a reliable source for clinical trial information.
Respondents said doctors and other healthcare providers (44%), followed by the government (23%), have the greatest responsibility in educating the public about clinical trials. However, 74% said no healthcare professional has ever talked to them about medical research.
Seventy-two percent of respondents said they would be likely to use technology such as apps and monitoring devices to share their personal health data for clinical research.
Eighty-eight percent said clinical trial participants should have access to trial results. And 47% said they would like having clinical trial information/data/results delivered through their phone. ![]()
More Americans are viewing clinical trials in a positive light, according to a survey commissioned by Research!America and the Association of Clinical Research Organizations (ACRO).
The results of the survey, which included 1000 participants and was conducted this month, reveal a shift in public attitudes about clinical trials since a similar survey was commissioned in 2013.
Thirty-seven percent of respondents involved in the current survey said they would “very likely” enroll in a clinical trial if their doctor recommended it. This represents an 11% increase from 2013.
Eighty-four percent of current survey respondents said they are willing to share personal health information, assuming that appropriate privacy protections are in place, so researchers can better understand diseases and develop new ways to prevent, treat, and cure them. This is a 10% increase from 2013.
When asked how much they admire people who volunteer for clinical trials, 46% of current respondents said “a great deal,” which is a 9% increase from 2013.
“More and more Americans appear to recognize the value of clinical trials—a very positive sign—but stubborn barriers to participation remain in place,” said Mary Woolley, president and CEO of Research!America.
“Development of incentives to drive more discussions between patients and healthcare professionals about the importance of participating in trials could encourage both ill and healthy individuals to view this as a routine health behavior.”
“We are pleased to have joined with Research!America in commissioning this important survey and gratified that the public’s knowledge of and attitudes toward clinical trials have moved in positive directions since 2013,” said Doug Peddicord, executive director of ACRO.
“The option to participate in a clinical trial, when appropriate, should be a routine part of the healthcare encounter, and ACRO will continue to work with Research!America and others to spread that message to doctors and patients alike.”
Survey results
The survey of 1000 US adults was conducted by Zogby Analytics for Research!America and ACRO in July 2017. The margin of error is +/- 3.1 percentage points.
Ninety percent of survey respondents said clinical trials are important to advancing science, and 87% said trials are important to improving the nation’s health. Seventy-five percent said taking part in clinical trials is as valuable to the US healthcare system as giving blood.
Eighty-six percent of respondents said healthcare professionals should discuss clinical trials with patients diagnosed with a disease as part of their standard care.
And 44% of respondents said clinical trial participation should be a routine health behavior, whether a person is healthy or ill, similar to getting an annual checkup with a healthcare provider.
Men (48%) were significantly more likely than women (39%) to say trial participation should be routine. A larger percentage of 18- to 29-year-olds (53%) and 30- to 49-year olds (48%) were in favor of routine trial participation, compared to people ages 50 to 64 (38%) and those 65 and older (34%).
Eighty percent of respondents said they had heard of a clinical trial, and 18% said they or someone in their family had participated in one.
Seventy-four percent of respondents said they would participate in a clinical trial if asked by someone they trust.
However, respondents were split on whether it’s important for everyone to take part in a clinical trial if asked. Forty-four percent said it is important, 45% disagreed, and 12% were not sure.
More than half of respondents (55%) said people don’t participate in clinical trials because of lack of awareness and information, 43% said it’s because trials are viewed as “too risky,” 41% said it’s due to a lack of information about the process, 38% said it’s due to a lack of trust, and 34% said it’s due to the risk of adverse health effects.
Nearly two-thirds of respondents (64%) said a doctor or healthcare provider is a reliable source for clinical trial information.
Respondents said doctors and other healthcare providers (44%), followed by the government (23%), have the greatest responsibility in educating the public about clinical trials. However, 74% said no healthcare professional has ever talked to them about medical research.
Seventy-two percent of respondents said they would be likely to use technology such as apps and monitoring devices to share their personal health data for clinical research.
Eighty-eight percent said clinical trial participants should have access to trial results. And 47% said they would like having clinical trial information/data/results delivered through their phone. ![]()
More Americans are viewing clinical trials in a positive light, according to a survey commissioned by Research!America and the Association of Clinical Research Organizations (ACRO).
The results of the survey, which included 1000 participants and was conducted this month, reveal a shift in public attitudes about clinical trials since a similar survey was commissioned in 2013.
Thirty-seven percent of respondents involved in the current survey said they would “very likely” enroll in a clinical trial if their doctor recommended it. This represents an 11% increase from 2013.
Eighty-four percent of current survey respondents said they are willing to share personal health information, assuming that appropriate privacy protections are in place, so researchers can better understand diseases and develop new ways to prevent, treat, and cure them. This is a 10% increase from 2013.
When asked how much they admire people who volunteer for clinical trials, 46% of current respondents said “a great deal,” which is a 9% increase from 2013.
“More and more Americans appear to recognize the value of clinical trials—a very positive sign—but stubborn barriers to participation remain in place,” said Mary Woolley, president and CEO of Research!America.
“Development of incentives to drive more discussions between patients and healthcare professionals about the importance of participating in trials could encourage both ill and healthy individuals to view this as a routine health behavior.”
“We are pleased to have joined with Research!America in commissioning this important survey and gratified that the public’s knowledge of and attitudes toward clinical trials have moved in positive directions since 2013,” said Doug Peddicord, executive director of ACRO.
“The option to participate in a clinical trial, when appropriate, should be a routine part of the healthcare encounter, and ACRO will continue to work with Research!America and others to spread that message to doctors and patients alike.”
Survey results
The survey of 1000 US adults was conducted by Zogby Analytics for Research!America and ACRO in July 2017. The margin of error is +/- 3.1 percentage points.
Ninety percent of survey respondents said clinical trials are important to advancing science, and 87% said trials are important to improving the nation’s health. Seventy-five percent said taking part in clinical trials is as valuable to the US healthcare system as giving blood.
Eighty-six percent of respondents said healthcare professionals should discuss clinical trials with patients diagnosed with a disease as part of their standard care.
And 44% of respondents said clinical trial participation should be a routine health behavior, whether a person is healthy or ill, similar to getting an annual checkup with a healthcare provider.
Men (48%) were significantly more likely than women (39%) to say trial participation should be routine. A larger percentage of 18- to 29-year-olds (53%) and 30- to 49-year olds (48%) were in favor of routine trial participation, compared to people ages 50 to 64 (38%) and those 65 and older (34%).
Eighty percent of respondents said they had heard of a clinical trial, and 18% said they or someone in their family had participated in one.
Seventy-four percent of respondents said they would participate in a clinical trial if asked by someone they trust.
However, respondents were split on whether it’s important for everyone to take part in a clinical trial if asked. Forty-four percent said it is important, 45% disagreed, and 12% were not sure.
More than half of respondents (55%) said people don’t participate in clinical trials because of lack of awareness and information, 43% said it’s because trials are viewed as “too risky,” 41% said it’s due to a lack of information about the process, 38% said it’s due to a lack of trust, and 34% said it’s due to the risk of adverse health effects.
Nearly two-thirds of respondents (64%) said a doctor or healthcare provider is a reliable source for clinical trial information.
Respondents said doctors and other healthcare providers (44%), followed by the government (23%), have the greatest responsibility in educating the public about clinical trials. However, 74% said no healthcare professional has ever talked to them about medical research.
Seventy-two percent of respondents said they would be likely to use technology such as apps and monitoring devices to share their personal health data for clinical research.
Eighty-eight percent said clinical trial participants should have access to trial results. And 47% said they would like having clinical trial information/data/results delivered through their phone.
AYA cancer survivors struggle with social functioning
New research suggests young cancer survivors struggle to get their social lives “back to normal” within the first 2 years of their diagnosis.
The study showed that adolescents and young adults (AYAs) with cancer had significantly worse social functioning than the general population around the time of cancer diagnosis as well as 1 year and 2 years later.
These findings were published in Cancer.
“The research is important to help these young survivors better reintegrate into society,” said study author Brad Zebrack, PhD, of the University of Michigan in Ann Arbor.
He and his colleagues collected data from 141 AYA cancer patients (ages 14 to 39) who visited 1 of 5 US medical facilities between March 2008 and April 2010.
The patients completed a self-report measure of social functioning within the first 4 months of diagnosis, then again at 12 months and 24 months.
Compared to the general population, the AYA cancer patients had significantly worse social functioning scores at all time points:
- Around the time of diagnosis—52.0 vs 85.1 (P<0.001)
- At 12 months—73.1 vs 85.1 (P<0.001)
- At 24 months—69.2 vs 85.1 (P<0.001).
Overall, the patients did experience improvements in social functioning from baseline to the 12-month time point, but their scores remained stable after that.
The researchers noted that 9% of patients had consistently high/normal social functioning, 47% had improvements in social functioning over time, 13% had worsening social functioning over time, and 32% had consistently low social functioning.
“This finding highlights the need to screen, identify, and respond to the needs of high-risk young adult-adolescent patients at the time of diagnosis and then monitor them over time,” Dr Zebrack said.
“They are likely the ones most in need of help in managing work, school, and potentially problematic relationships with family members and friends.”
New research suggests young cancer survivors struggle to get their social lives “back to normal” within the first 2 years of their diagnosis.
The study showed that adolescents and young adults (AYAs) with cancer had significantly worse social functioning than the general population around the time of cancer diagnosis as well as 1 year and 2 years later.
These findings were published in Cancer.
“The research is important to help these young survivors better reintegrate into society,” said study author Brad Zebrack, PhD, of the University of Michigan in Ann Arbor.
He and his colleagues collected data from 141 AYA cancer patients (ages 14 to 39) who visited 1 of 5 US medical facilities between March 2008 and April 2010.
The patients completed a self-report measure of social functioning within the first 4 months of diagnosis, then again at 12 months and 24 months.
Compared to the general population, the AYA cancer patients had significantly worse social functioning scores at all time points:
- Around the time of diagnosis—52.0 vs 85.1 (P<0.001)
- At 12 months—73.1 vs 85.1 (P<0.001)
- At 24 months—69.2 vs 85.1 (P<0.001).
Overall, the patients did experience improvements in social functioning from baseline to the 12-month time point, but their scores remained stable after that.
The researchers noted that 9% of patients had consistently high/normal social functioning, 47% had improvements in social functioning over time, 13% had worsening social functioning over time, and 32% had consistently low social functioning.
“This finding highlights the need to screen, identify, and respond to the needs of high-risk young adult-adolescent patients at the time of diagnosis and then monitor them over time,” Dr Zebrack said.
“They are likely the ones most in need of help in managing work, school, and potentially problematic relationships with family members and friends.”
New research suggests young cancer survivors struggle to get their social lives “back to normal” within the first 2 years of their diagnosis.
The study showed that adolescents and young adults (AYAs) with cancer had significantly worse social functioning than the general population around the time of cancer diagnosis as well as 1 year and 2 years later.
These findings were published in Cancer.
“The research is important to help these young survivors better reintegrate into society,” said study author Brad Zebrack, PhD, of the University of Michigan in Ann Arbor.
He and his colleagues collected data from 141 AYA cancer patients (ages 14 to 39) who visited 1 of 5 US medical facilities between March 2008 and April 2010.
The patients completed a self-report measure of social functioning within the first 4 months of diagnosis, then again at 12 months and 24 months.
Compared to the general population, the AYA cancer patients had significantly worse social functioning scores at all time points:
- Around the time of diagnosis—52.0 vs 85.1 (P<0.001)
- At 12 months—73.1 vs 85.1 (P<0.001)
- At 24 months—69.2 vs 85.1 (P<0.001).
Overall, the patients did experience improvements in social functioning from baseline to the 12-month time point, but their scores remained stable after that.
The researchers noted that 9% of patients had consistently high/normal social functioning, 47% had improvements in social functioning over time, 13% had worsening social functioning over time, and 32% had consistently low social functioning.
“This finding highlights the need to screen, identify, and respond to the needs of high-risk young adult-adolescent patients at the time of diagnosis and then monitor them over time,” Dr Zebrack said.
“They are likely the ones most in need of help in managing work, school, and potentially problematic relationships with family members and friends.”
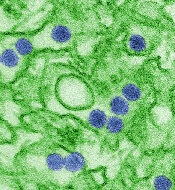
Vaccines protect unborn mice from Zika infection
Researchers have reported that 2 different vaccines can protect mice from Zika virus-induced congenital disease.
Female mice that were vaccinated before pregnancy and infected with Zika virus while pregnant bore pups that showed no trace of the virus.
These results, published in Cell, offer the first evidence that a vaccine administered prior to pregnancy can protect fetuses from Zika infection and resulting injury.
“There are several vaccines in human trials right now, but, to date, none of them has been shown to protect during pregnancy,” said Michael S. Diamond, MD, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We tested 2 different vaccines, and they both provided substantial protection.”
Last year, Dr Diamond and his colleagues developed a mouse model of Zika infection that mimics the effects of the infection in pregnant women.
Using this model, the researchers evaluated the ability of 2 vaccines to protect fetuses whose mothers were infected during pregnancy.
One of the vaccines is a messenger RNA (mRNA) vaccine, developed by Moderna Therapeutics, that is currently in safety testing in men and women who are not pregnant.
The other is a live-attenuated vaccine, developed by the University of Texas Medical Branch, that is being tested in animals.
For this study, groups of 18 to 20 female mice were vaccinated with one of the vaccines or a placebo, and some animals received a second dose of the same vaccine or placebo a month later.
Three weeks later, the researchers measured antibody levels in the mice’s blood as a measure of the strength of their immune response.
Both vaccines elicited very high levels of neutralizing antibodies against Zika, while the placebos did not.
After the mice became pregnant, they were infected with Zika on the sixth day of pregnancy, to mimic the experience of a woman bitten by a Zika-carrying mosquito early in pregnancy.
One week after infection, the researchers measured the amount of virus in the mothers and fetuses.
With both vaccines, fetuses and placentas from vaccinated mice contained very low levels of Zika’s genetic material.
For the mRNA vaccine, more than half of the placentas and fetuses had no detectable viral genetic material at all.
The live-attenuated vaccine was even more effective. In 78% of the placentas and 83% of the fetuses, no viral genetic material was found.
“The amount of viral genetic material in the placentas and fetuses from the vaccinated females was just above the limit of detection,” Dr Diamond said. “It’s not totally clear whether it was infectious virus or just remnants of viruses that had already been killed.”
In contrast, the amount of detectable viral material in the placentas and fetuses of unvaccinated mice was hundreds to thousands of times higher.
The researchers repeated the experiment with different mice so they could evaluate the pups at birth.
None of the mothers in the placebo group made it to term. The mothers became seriously ill, many of the fetuses showed high levels of infection and died in utero, and the placentas showed severe damage.
In contrast, the vaccinated mothers remained healthy, all of their pups were born without obvious signs of injury, and the newborn pups had no measurable Zika virus in their heads.
“In general, most doctors don’t want to vaccinate during pregnancy on the outside chance that the immune response itself could harm the fetus,” Dr Diamond said. “But if you’re in an area where Zika is circulating, you might vaccinate during pregnancy because the risk of Zika infection is worse than some theoretical risk of immune-mediated damage.”
The researchers did not assess whether the vaccines are safe and effective for use during pregnancy.
Such studies couldn’t really be done in mice, Dr Diamond explained, because mouse pregnancies only last 19 days. That doesn’t allow enough time for a protective immune response to develop before the pups are born.
Additionally, this study did not address the question of whether the vaccines work when pregnant women are infected with Zika through sexual contact. It is possible that Zika virus in semen can travel to the uterus and then to the fetus without passing through the bloodstream.
“The question is, ‘Would the immunity still hold up if the virus does not pass through the bloodstream?’“ Dr Diamond said. “We think it will hold up, but that has to be tested.”
Researchers have reported that 2 different vaccines can protect mice from Zika virus-induced congenital disease.
Female mice that were vaccinated before pregnancy and infected with Zika virus while pregnant bore pups that showed no trace of the virus.
These results, published in Cell, offer the first evidence that a vaccine administered prior to pregnancy can protect fetuses from Zika infection and resulting injury.
“There are several vaccines in human trials right now, but, to date, none of them has been shown to protect during pregnancy,” said Michael S. Diamond, MD, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We tested 2 different vaccines, and they both provided substantial protection.”
Last year, Dr Diamond and his colleagues developed a mouse model of Zika infection that mimics the effects of the infection in pregnant women.
Using this model, the researchers evaluated the ability of 2 vaccines to protect fetuses whose mothers were infected during pregnancy.
One of the vaccines is a messenger RNA (mRNA) vaccine, developed by Moderna Therapeutics, that is currently in safety testing in men and women who are not pregnant.
The other is a live-attenuated vaccine, developed by the University of Texas Medical Branch, that is being tested in animals.
For this study, groups of 18 to 20 female mice were vaccinated with one of the vaccines or a placebo, and some animals received a second dose of the same vaccine or placebo a month later.
Three weeks later, the researchers measured antibody levels in the mice’s blood as a measure of the strength of their immune response.
Both vaccines elicited very high levels of neutralizing antibodies against Zika, while the placebos did not.
After the mice became pregnant, they were infected with Zika on the sixth day of pregnancy, to mimic the experience of a woman bitten by a Zika-carrying mosquito early in pregnancy.
One week after infection, the researchers measured the amount of virus in the mothers and fetuses.
With both vaccines, fetuses and placentas from vaccinated mice contained very low levels of Zika’s genetic material.
For the mRNA vaccine, more than half of the placentas and fetuses had no detectable viral genetic material at all.
The live-attenuated vaccine was even more effective. In 78% of the placentas and 83% of the fetuses, no viral genetic material was found.
“The amount of viral genetic material in the placentas and fetuses from the vaccinated females was just above the limit of detection,” Dr Diamond said. “It’s not totally clear whether it was infectious virus or just remnants of viruses that had already been killed.”
In contrast, the amount of detectable viral material in the placentas and fetuses of unvaccinated mice was hundreds to thousands of times higher.
The researchers repeated the experiment with different mice so they could evaluate the pups at birth.
None of the mothers in the placebo group made it to term. The mothers became seriously ill, many of the fetuses showed high levels of infection and died in utero, and the placentas showed severe damage.
In contrast, the vaccinated mothers remained healthy, all of their pups were born without obvious signs of injury, and the newborn pups had no measurable Zika virus in their heads.
“In general, most doctors don’t want to vaccinate during pregnancy on the outside chance that the immune response itself could harm the fetus,” Dr Diamond said. “But if you’re in an area where Zika is circulating, you might vaccinate during pregnancy because the risk of Zika infection is worse than some theoretical risk of immune-mediated damage.”
The researchers did not assess whether the vaccines are safe and effective for use during pregnancy.
Such studies couldn’t really be done in mice, Dr Diamond explained, because mouse pregnancies only last 19 days. That doesn’t allow enough time for a protective immune response to develop before the pups are born.
Additionally, this study did not address the question of whether the vaccines work when pregnant women are infected with Zika through sexual contact. It is possible that Zika virus in semen can travel to the uterus and then to the fetus without passing through the bloodstream.
“The question is, ‘Would the immunity still hold up if the virus does not pass through the bloodstream?’“ Dr Diamond said. “We think it will hold up, but that has to be tested.”
Researchers have reported that 2 different vaccines can protect mice from Zika virus-induced congenital disease.
Female mice that were vaccinated before pregnancy and infected with Zika virus while pregnant bore pups that showed no trace of the virus.
These results, published in Cell, offer the first evidence that a vaccine administered prior to pregnancy can protect fetuses from Zika infection and resulting injury.
“There are several vaccines in human trials right now, but, to date, none of them has been shown to protect during pregnancy,” said Michael S. Diamond, MD, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We tested 2 different vaccines, and they both provided substantial protection.”
Last year, Dr Diamond and his colleagues developed a mouse model of Zika infection that mimics the effects of the infection in pregnant women.
Using this model, the researchers evaluated the ability of 2 vaccines to protect fetuses whose mothers were infected during pregnancy.
One of the vaccines is a messenger RNA (mRNA) vaccine, developed by Moderna Therapeutics, that is currently in safety testing in men and women who are not pregnant.
The other is a live-attenuated vaccine, developed by the University of Texas Medical Branch, that is being tested in animals.
For this study, groups of 18 to 20 female mice were vaccinated with one of the vaccines or a placebo, and some animals received a second dose of the same vaccine or placebo a month later.
Three weeks later, the researchers measured antibody levels in the mice’s blood as a measure of the strength of their immune response.
Both vaccines elicited very high levels of neutralizing antibodies against Zika, while the placebos did not.
After the mice became pregnant, they were infected with Zika on the sixth day of pregnancy, to mimic the experience of a woman bitten by a Zika-carrying mosquito early in pregnancy.
One week after infection, the researchers measured the amount of virus in the mothers and fetuses.
With both vaccines, fetuses and placentas from vaccinated mice contained very low levels of Zika’s genetic material.
For the mRNA vaccine, more than half of the placentas and fetuses had no detectable viral genetic material at all.
The live-attenuated vaccine was even more effective. In 78% of the placentas and 83% of the fetuses, no viral genetic material was found.
“The amount of viral genetic material in the placentas and fetuses from the vaccinated females was just above the limit of detection,” Dr Diamond said. “It’s not totally clear whether it was infectious virus or just remnants of viruses that had already been killed.”
In contrast, the amount of detectable viral material in the placentas and fetuses of unvaccinated mice was hundreds to thousands of times higher.
The researchers repeated the experiment with different mice so they could evaluate the pups at birth.
None of the mothers in the placebo group made it to term. The mothers became seriously ill, many of the fetuses showed high levels of infection and died in utero, and the placentas showed severe damage.
In contrast, the vaccinated mothers remained healthy, all of their pups were born without obvious signs of injury, and the newborn pups had no measurable Zika virus in their heads.
“In general, most doctors don’t want to vaccinate during pregnancy on the outside chance that the immune response itself could harm the fetus,” Dr Diamond said. “But if you’re in an area where Zika is circulating, you might vaccinate during pregnancy because the risk of Zika infection is worse than some theoretical risk of immune-mediated damage.”
The researchers did not assess whether the vaccines are safe and effective for use during pregnancy.
Such studies couldn’t really be done in mice, Dr Diamond explained, because mouse pregnancies only last 19 days. That doesn’t allow enough time for a protective immune response to develop before the pups are born.
Additionally, this study did not address the question of whether the vaccines work when pregnant women are infected with Zika through sexual contact. It is possible that Zika virus in semen can travel to the uterus and then to the fetus without passing through the bloodstream.
“The question is, ‘Would the immunity still hold up if the virus does not pass through the bloodstream?’“ Dr Diamond said. “We think it will hold up, but that has to be tested.”
Company launches automated hematology analyzers in US
Sysmex America, Inc. has launched its XN-L™ automated hematology analyzers in the US.
The company says this new, smaller XN-L line delivers the same clinical and operational value as its XN-Series™ to lower-volume hematology laboratories.
“The XN-Series has been our flagship hematology analyzer line, and, today, we expand our offering by introducing the XN-L Series to meet the demands of lower-volume facilities,” said Andy Hay, chief operating officer of Sysmex America.
“With an XN-L analyzer, clinicians can rely upon the same expanded complete blood count (CBC) featured in our XN-Series analyzers to assess and monitor patients. This expanded CBC goes well beyond the 3-part differential that is currently available to most of the low-volume segment today and can aid in the assessment of sepsis and other hematological disorders.”
The XN-L automated hematology analyzers offer a 6-part differential, including immature granulocyte analysis on each sample.
In addition, the XN-L Series offers optional software licenses for (1) a reticulocyte channel to aid in anemia management and (2) body fluid cell counts.
The XN-L analyzers will also be the first to feature BeyondCare Quality Monitor, a new approach to quality assurance.
“BeyondCare Quality Monitor, a Sysmex proprietary innovation, is a leading-edge, evidence-based QC and calibration verification management program that partners Sysmex with the laboratory to proactively monitor quality assurance metrics,” Hay said. “It will be standard on all XN-L hematology analyzers.
Additional information on XN-L analyzers is available on the Sysmex website at www.sysmex.com/XNL.
The XN-L analyzers will be available both directly through the company and through its distribution partners. Interested parties should contact their Sysmex representative or Sysmex distributor for complete details.
Sysmex America, Inc. has launched its XN-L™ automated hematology analyzers in the US.
The company says this new, smaller XN-L line delivers the same clinical and operational value as its XN-Series™ to lower-volume hematology laboratories.
“The XN-Series has been our flagship hematology analyzer line, and, today, we expand our offering by introducing the XN-L Series to meet the demands of lower-volume facilities,” said Andy Hay, chief operating officer of Sysmex America.
“With an XN-L analyzer, clinicians can rely upon the same expanded complete blood count (CBC) featured in our XN-Series analyzers to assess and monitor patients. This expanded CBC goes well beyond the 3-part differential that is currently available to most of the low-volume segment today and can aid in the assessment of sepsis and other hematological disorders.”
The XN-L automated hematology analyzers offer a 6-part differential, including immature granulocyte analysis on each sample.
In addition, the XN-L Series offers optional software licenses for (1) a reticulocyte channel to aid in anemia management and (2) body fluid cell counts.
The XN-L analyzers will also be the first to feature BeyondCare Quality Monitor, a new approach to quality assurance.
“BeyondCare Quality Monitor, a Sysmex proprietary innovation, is a leading-edge, evidence-based QC and calibration verification management program that partners Sysmex with the laboratory to proactively monitor quality assurance metrics,” Hay said. “It will be standard on all XN-L hematology analyzers.
Additional information on XN-L analyzers is available on the Sysmex website at www.sysmex.com/XNL.
The XN-L analyzers will be available both directly through the company and through its distribution partners. Interested parties should contact their Sysmex representative or Sysmex distributor for complete details.
Sysmex America, Inc. has launched its XN-L™ automated hematology analyzers in the US.
The company says this new, smaller XN-L line delivers the same clinical and operational value as its XN-Series™ to lower-volume hematology laboratories.
“The XN-Series has been our flagship hematology analyzer line, and, today, we expand our offering by introducing the XN-L Series to meet the demands of lower-volume facilities,” said Andy Hay, chief operating officer of Sysmex America.
“With an XN-L analyzer, clinicians can rely upon the same expanded complete blood count (CBC) featured in our XN-Series analyzers to assess and monitor patients. This expanded CBC goes well beyond the 3-part differential that is currently available to most of the low-volume segment today and can aid in the assessment of sepsis and other hematological disorders.”
The XN-L automated hematology analyzers offer a 6-part differential, including immature granulocyte analysis on each sample.
In addition, the XN-L Series offers optional software licenses for (1) a reticulocyte channel to aid in anemia management and (2) body fluid cell counts.
The XN-L analyzers will also be the first to feature BeyondCare Quality Monitor, a new approach to quality assurance.
“BeyondCare Quality Monitor, a Sysmex proprietary innovation, is a leading-edge, evidence-based QC and calibration verification management program that partners Sysmex with the laboratory to proactively monitor quality assurance metrics,” Hay said. “It will be standard on all XN-L hematology analyzers.
Additional information on XN-L analyzers is available on the Sysmex website at www.sysmex.com/XNL.
The XN-L analyzers will be available both directly through the company and through its distribution partners. Interested parties should contact their Sysmex representative or Sysmex distributor for complete details.