User login
Standardized communication may prevent anticoagulant adverse drug events
Background: With increased use of anticoagulants, the amount of related ADEs has also increased. ADEs may be preventable through improved communication during transitions of care. The key communication elements are not standardized.
Study design: Delphi method.
Setting: Consensus panel in New York state.
Synopsis: The New York State Anticoagulation Coalition (NYSACC) tasked an expert multidisciplinary panel of physicians, pharmacists, nurse practitioners, and physician assistants to develop a list of minimum required data elements (RDEs) for transitions of care using the Delphi method.
The following items are the 15 RDEs that require documentation: (1) current anticoagulants; (2) indications; (3) new or previous user; (4) if new, start date, (5) short-term or long-term use; (6) if short term, intended duration; (7) last two doses given; (8) next dose due; (9) latest renal function; (10) provision of patient education materials; (11) assessment of patient/caregiver understanding; (12) future anticoagulation provider; and if warfarin, (13) the target range, (14) at least 2-3 consecutive international normalized ratio results, and (15) next INR level.
Bottom line: Standardized communication during transitions of care regarding anticoagulation may reduce anticoagulant ADEs. Objective evidence showing reduction of ADEs after implementation of the list is needed.
Citation: Triller D et al. Defining minimum necessary anticoagulation-related communication at discharge: Consensus of the Care Transitions Task Force of the New York State Anticoagulation Coalition. Jt Comm J Qual Patient Saf. 2018;44(11):630-40.
Dr. Vuong is an associate physician in the division of hospital medicine at the University of California, San Diego.
Background: With increased use of anticoagulants, the amount of related ADEs has also increased. ADEs may be preventable through improved communication during transitions of care. The key communication elements are not standardized.
Study design: Delphi method.
Setting: Consensus panel in New York state.
Synopsis: The New York State Anticoagulation Coalition (NYSACC) tasked an expert multidisciplinary panel of physicians, pharmacists, nurse practitioners, and physician assistants to develop a list of minimum required data elements (RDEs) for transitions of care using the Delphi method.
The following items are the 15 RDEs that require documentation: (1) current anticoagulants; (2) indications; (3) new or previous user; (4) if new, start date, (5) short-term or long-term use; (6) if short term, intended duration; (7) last two doses given; (8) next dose due; (9) latest renal function; (10) provision of patient education materials; (11) assessment of patient/caregiver understanding; (12) future anticoagulation provider; and if warfarin, (13) the target range, (14) at least 2-3 consecutive international normalized ratio results, and (15) next INR level.
Bottom line: Standardized communication during transitions of care regarding anticoagulation may reduce anticoagulant ADEs. Objective evidence showing reduction of ADEs after implementation of the list is needed.
Citation: Triller D et al. Defining minimum necessary anticoagulation-related communication at discharge: Consensus of the Care Transitions Task Force of the New York State Anticoagulation Coalition. Jt Comm J Qual Patient Saf. 2018;44(11):630-40.
Dr. Vuong is an associate physician in the division of hospital medicine at the University of California, San Diego.
Background: With increased use of anticoagulants, the amount of related ADEs has also increased. ADEs may be preventable through improved communication during transitions of care. The key communication elements are not standardized.
Study design: Delphi method.
Setting: Consensus panel in New York state.
Synopsis: The New York State Anticoagulation Coalition (NYSACC) tasked an expert multidisciplinary panel of physicians, pharmacists, nurse practitioners, and physician assistants to develop a list of minimum required data elements (RDEs) for transitions of care using the Delphi method.
The following items are the 15 RDEs that require documentation: (1) current anticoagulants; (2) indications; (3) new or previous user; (4) if new, start date, (5) short-term or long-term use; (6) if short term, intended duration; (7) last two doses given; (8) next dose due; (9) latest renal function; (10) provision of patient education materials; (11) assessment of patient/caregiver understanding; (12) future anticoagulation provider; and if warfarin, (13) the target range, (14) at least 2-3 consecutive international normalized ratio results, and (15) next INR level.
Bottom line: Standardized communication during transitions of care regarding anticoagulation may reduce anticoagulant ADEs. Objective evidence showing reduction of ADEs after implementation of the list is needed.
Citation: Triller D et al. Defining minimum necessary anticoagulation-related communication at discharge: Consensus of the Care Transitions Task Force of the New York State Anticoagulation Coalition. Jt Comm J Qual Patient Saf. 2018;44(11):630-40.
Dr. Vuong is an associate physician in the division of hospital medicine at the University of California, San Diego.
POP AGE shakes up DAPT in elderly
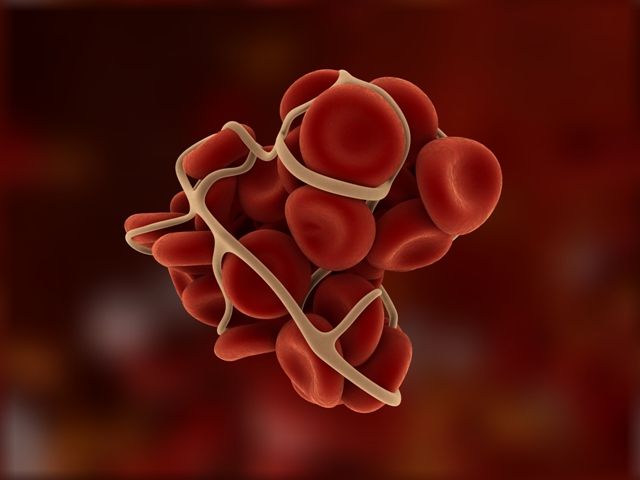
PARIS – Older patients with non-ST-elevation acute coronary syndrome who were assigned to 12 months of dual antiplatelet therapy with clopidogrel experienced significantly less major and minor bleeding than with ticagrelor or prasugrel and were similarly protected from thrombotic events in the prospective randomized POPular AGE trial, Marieke E. Gimbel, MD, reported at the annual congress of the European Society of Cardiology.
“Therefore, we consider clopidogrel the preferred treatment in patients age 70 or older with non-ST-elevation ACS,” said Dr. Gimbel, a cardiologist at St. Antonius Hospital in Nieuwegein, The Netherlands.
This stance is contrary to both the current ESC and U.S. guidelines on management of non-ST-elevation ACS, which preferentially recommend ticagrelor and prasugrel over clopidogrel, chiefly on the basis of the large PLATO (N Engl J Med 2009;361:1045-57) and TRITON TIMI 38 (N Engl J Med 2007;357:2001-15) randomized trials. Those studies from the previous decade reported significantly lower rates of the composite endpoint of cardiovascular death, acute MI, or stroke in patients on ticagrelor or prasugrel, respectively, than with clopidogrel. But this benefit came at a cost of significantly higher rates of TIMI major bleeding than with clopidogrel, and multiple studies have shown that major bleeding in ACS patients is associated with a sharply increased risk of death.
Bleeding is an issue of particular concern in the elderly. But older patients were greatly underrepresented in PLATO and TRITON, where they comprised just 13%-15% of participants, even though registry studies would suggest older individuals make up about 35% of all patients with non-ST-elevation ACS. Selective inclusion of elderly patients in the major trials means those study results can’t legitimately be extrapolated to the entire elderly patient population.
“The best course of action in the elderly has been unclear,” Dr. Gimbel argued.
The POPular AGE (POP AGE) trial was an open-label study featuring independent blinded adjudication of clinical events. The median age of participants was 77 years, and about one-quarter had a prior MI. It was basically an all-comers study in which 1,003 non-ST-elevation ACS patients age 70 or older at 11 Dutch medical centers were randomized within 3 days of hospital admission to 12 months of dual antiplatelet therapy with either ticagrelor or one of the two more potent antiplatelet agents. Although the choice of ticagrelor or prasugrel was left to the physician, it’s noteworthy that 94% of patients in the high-potency P2Y12 inhibitor study arm were discharged on ticagrelor. At 12 months, the adherence rate to the assigned regimen was 76% in the clopidogrel group and just 51% in what was essentially the ticagrelor arm. Bleeding was the number-one reason for the much higher discontinuation rate in the ticagrelor group, followed by initiation of oral anticoagulation and dyspnea.
The primary safety endpoint in POP AGE was the rate of major and minor bleeding as defined in the PLATO study. The rate was 17.6% with clopidogrel, compared with 23.1% in the ticagrelor group, for a highly significant 26% reduction in relative risk. Of note, the PLATO major bleeding rate was 4.4% with clopidogrel, versus 8% with ticagrelor/prasugrel.
The coprimary endpoint was net clinical benefit, defined as a composite of all-cause mortality, MI, stroke, and PLATO major and minor bleeding. The rate was 30.7% with ticagrelor and 27.3% in the clopidogrel group, for an absolute 3.4% risk difference favoring clopidogrel, which barely missed the prespecified cutoff for noninferiority. Indeed, even though the 12-month follow-up was 99.6% complete, Dr. Gimbel raised the possibility that when the results come in for the final 0.4% of the study population, the difference in net clinical benefit may reach significance.
In any case, she noted there was no between-group difference in the key secondary endpoint of death, MI, or stroke, with rates of 12.8% and 12.5% in the clopidogrel and ticagrelor groups, respectively.
“One might expect a higher ischemic event rate with clopidogrel compared to ticagrelor. However, in these elderly patients there was no difference between the two treatment strategies,” the cardiologist observed.
POP AGE is hailed as ‘a wake up call’
In an interview, Freek Verheugt, MD, PhD, professor emeritus of cardiology at Radboud University in Nijmegen, The Netherlands, called POP AGE “a very important study.”
“The problem with most studies in the elderly is that they are post hoc analyses from huge trials like PLATO and TRITON, and also the thrombolysis and primary PCI studies. The elderly do very well in those studies, because only the very fit elderly are included in the megatrials. It’s much more important to do a prospective randomized trial in the elderly only, and this is one of the very few done so far,” he observed.
Bleeding is a major problem in the elderly with ACS. It leads to more MIs, strokes, and increased mortality.
“Even minor bleeding is an issue,” Dr. Verheugt added. “Minor bleeding is a major problem, because patients who encounter minor bleeding – nose bleeds, gum bleeds, or even in their underwear – they do away with all drugs. They stop their antithrombotic, but they also stop their statin, their ACE inhibitor – their lifesavers – and that’s why they die.”
So is POP AGE a practice-changing study?
“No, of course not,” the cardiologist scoffed. “To be practice-changing you need several trials going in the same direction. But I think if there are more data prospectively accrued in the elderly alone, showing the same, then POP AGE would be practice-changing.”
“In my personal view, this study is a wake-up call. If you have an elderly, frail patient presenting with ACS, strongly consider good, old clopidogrel. Although people say that 30% of patients on clopidogrel don’t have appropriate platelet inhibition, that’s a laboratory finding. It’s not a clinical finding. POP AGE gave us a clinical finding showing that they do quite well,” he said.
Dr. Verheugt was on the independent data safety monitoring board for POP AGE, funded by ZonMw, a Dutch governmental research organization. Neither Dr. Verheugt nor Dr. Gimbel reported having any financial conflicts of interest.
SOURCE: Gimbel ME. ESC 2019, Abstract 84.
PARIS – Older patients with non-ST-elevation acute coronary syndrome who were assigned to 12 months of dual antiplatelet therapy with clopidogrel experienced significantly less major and minor bleeding than with ticagrelor or prasugrel and were similarly protected from thrombotic events in the prospective randomized POPular AGE trial, Marieke E. Gimbel, MD, reported at the annual congress of the European Society of Cardiology.
“Therefore, we consider clopidogrel the preferred treatment in patients age 70 or older with non-ST-elevation ACS,” said Dr. Gimbel, a cardiologist at St. Antonius Hospital in Nieuwegein, The Netherlands.
This stance is contrary to both the current ESC and U.S. guidelines on management of non-ST-elevation ACS, which preferentially recommend ticagrelor and prasugrel over clopidogrel, chiefly on the basis of the large PLATO (N Engl J Med 2009;361:1045-57) and TRITON TIMI 38 (N Engl J Med 2007;357:2001-15) randomized trials. Those studies from the previous decade reported significantly lower rates of the composite endpoint of cardiovascular death, acute MI, or stroke in patients on ticagrelor or prasugrel, respectively, than with clopidogrel. But this benefit came at a cost of significantly higher rates of TIMI major bleeding than with clopidogrel, and multiple studies have shown that major bleeding in ACS patients is associated with a sharply increased risk of death.
Bleeding is an issue of particular concern in the elderly. But older patients were greatly underrepresented in PLATO and TRITON, where they comprised just 13%-15% of participants, even though registry studies would suggest older individuals make up about 35% of all patients with non-ST-elevation ACS. Selective inclusion of elderly patients in the major trials means those study results can’t legitimately be extrapolated to the entire elderly patient population.
“The best course of action in the elderly has been unclear,” Dr. Gimbel argued.
The POPular AGE (POP AGE) trial was an open-label study featuring independent blinded adjudication of clinical events. The median age of participants was 77 years, and about one-quarter had a prior MI. It was basically an all-comers study in which 1,003 non-ST-elevation ACS patients age 70 or older at 11 Dutch medical centers were randomized within 3 days of hospital admission to 12 months of dual antiplatelet therapy with either ticagrelor or one of the two more potent antiplatelet agents. Although the choice of ticagrelor or prasugrel was left to the physician, it’s noteworthy that 94% of patients in the high-potency P2Y12 inhibitor study arm were discharged on ticagrelor. At 12 months, the adherence rate to the assigned regimen was 76% in the clopidogrel group and just 51% in what was essentially the ticagrelor arm. Bleeding was the number-one reason for the much higher discontinuation rate in the ticagrelor group, followed by initiation of oral anticoagulation and dyspnea.
The primary safety endpoint in POP AGE was the rate of major and minor bleeding as defined in the PLATO study. The rate was 17.6% with clopidogrel, compared with 23.1% in the ticagrelor group, for a highly significant 26% reduction in relative risk. Of note, the PLATO major bleeding rate was 4.4% with clopidogrel, versus 8% with ticagrelor/prasugrel.
The coprimary endpoint was net clinical benefit, defined as a composite of all-cause mortality, MI, stroke, and PLATO major and minor bleeding. The rate was 30.7% with ticagrelor and 27.3% in the clopidogrel group, for an absolute 3.4% risk difference favoring clopidogrel, which barely missed the prespecified cutoff for noninferiority. Indeed, even though the 12-month follow-up was 99.6% complete, Dr. Gimbel raised the possibility that when the results come in for the final 0.4% of the study population, the difference in net clinical benefit may reach significance.
In any case, she noted there was no between-group difference in the key secondary endpoint of death, MI, or stroke, with rates of 12.8% and 12.5% in the clopidogrel and ticagrelor groups, respectively.
“One might expect a higher ischemic event rate with clopidogrel compared to ticagrelor. However, in these elderly patients there was no difference between the two treatment strategies,” the cardiologist observed.
POP AGE is hailed as ‘a wake up call’
In an interview, Freek Verheugt, MD, PhD, professor emeritus of cardiology at Radboud University in Nijmegen, The Netherlands, called POP AGE “a very important study.”
“The problem with most studies in the elderly is that they are post hoc analyses from huge trials like PLATO and TRITON, and also the thrombolysis and primary PCI studies. The elderly do very well in those studies, because only the very fit elderly are included in the megatrials. It’s much more important to do a prospective randomized trial in the elderly only, and this is one of the very few done so far,” he observed.
Bleeding is a major problem in the elderly with ACS. It leads to more MIs, strokes, and increased mortality.
“Even minor bleeding is an issue,” Dr. Verheugt added. “Minor bleeding is a major problem, because patients who encounter minor bleeding – nose bleeds, gum bleeds, or even in their underwear – they do away with all drugs. They stop their antithrombotic, but they also stop their statin, their ACE inhibitor – their lifesavers – and that’s why they die.”
So is POP AGE a practice-changing study?
“No, of course not,” the cardiologist scoffed. “To be practice-changing you need several trials going in the same direction. But I think if there are more data prospectively accrued in the elderly alone, showing the same, then POP AGE would be practice-changing.”
“In my personal view, this study is a wake-up call. If you have an elderly, frail patient presenting with ACS, strongly consider good, old clopidogrel. Although people say that 30% of patients on clopidogrel don’t have appropriate platelet inhibition, that’s a laboratory finding. It’s not a clinical finding. POP AGE gave us a clinical finding showing that they do quite well,” he said.
Dr. Verheugt was on the independent data safety monitoring board for POP AGE, funded by ZonMw, a Dutch governmental research organization. Neither Dr. Verheugt nor Dr. Gimbel reported having any financial conflicts of interest.
SOURCE: Gimbel ME. ESC 2019, Abstract 84.
PARIS – Older patients with non-ST-elevation acute coronary syndrome who were assigned to 12 months of dual antiplatelet therapy with clopidogrel experienced significantly less major and minor bleeding than with ticagrelor or prasugrel and were similarly protected from thrombotic events in the prospective randomized POPular AGE trial, Marieke E. Gimbel, MD, reported at the annual congress of the European Society of Cardiology.
“Therefore, we consider clopidogrel the preferred treatment in patients age 70 or older with non-ST-elevation ACS,” said Dr. Gimbel, a cardiologist at St. Antonius Hospital in Nieuwegein, The Netherlands.
This stance is contrary to both the current ESC and U.S. guidelines on management of non-ST-elevation ACS, which preferentially recommend ticagrelor and prasugrel over clopidogrel, chiefly on the basis of the large PLATO (N Engl J Med 2009;361:1045-57) and TRITON TIMI 38 (N Engl J Med 2007;357:2001-15) randomized trials. Those studies from the previous decade reported significantly lower rates of the composite endpoint of cardiovascular death, acute MI, or stroke in patients on ticagrelor or prasugrel, respectively, than with clopidogrel. But this benefit came at a cost of significantly higher rates of TIMI major bleeding than with clopidogrel, and multiple studies have shown that major bleeding in ACS patients is associated with a sharply increased risk of death.
Bleeding is an issue of particular concern in the elderly. But older patients were greatly underrepresented in PLATO and TRITON, where they comprised just 13%-15% of participants, even though registry studies would suggest older individuals make up about 35% of all patients with non-ST-elevation ACS. Selective inclusion of elderly patients in the major trials means those study results can’t legitimately be extrapolated to the entire elderly patient population.
“The best course of action in the elderly has been unclear,” Dr. Gimbel argued.
The POPular AGE (POP AGE) trial was an open-label study featuring independent blinded adjudication of clinical events. The median age of participants was 77 years, and about one-quarter had a prior MI. It was basically an all-comers study in which 1,003 non-ST-elevation ACS patients age 70 or older at 11 Dutch medical centers were randomized within 3 days of hospital admission to 12 months of dual antiplatelet therapy with either ticagrelor or one of the two more potent antiplatelet agents. Although the choice of ticagrelor or prasugrel was left to the physician, it’s noteworthy that 94% of patients in the high-potency P2Y12 inhibitor study arm were discharged on ticagrelor. At 12 months, the adherence rate to the assigned regimen was 76% in the clopidogrel group and just 51% in what was essentially the ticagrelor arm. Bleeding was the number-one reason for the much higher discontinuation rate in the ticagrelor group, followed by initiation of oral anticoagulation and dyspnea.
The primary safety endpoint in POP AGE was the rate of major and minor bleeding as defined in the PLATO study. The rate was 17.6% with clopidogrel, compared with 23.1% in the ticagrelor group, for a highly significant 26% reduction in relative risk. Of note, the PLATO major bleeding rate was 4.4% with clopidogrel, versus 8% with ticagrelor/prasugrel.
The coprimary endpoint was net clinical benefit, defined as a composite of all-cause mortality, MI, stroke, and PLATO major and minor bleeding. The rate was 30.7% with ticagrelor and 27.3% in the clopidogrel group, for an absolute 3.4% risk difference favoring clopidogrel, which barely missed the prespecified cutoff for noninferiority. Indeed, even though the 12-month follow-up was 99.6% complete, Dr. Gimbel raised the possibility that when the results come in for the final 0.4% of the study population, the difference in net clinical benefit may reach significance.
In any case, she noted there was no between-group difference in the key secondary endpoint of death, MI, or stroke, with rates of 12.8% and 12.5% in the clopidogrel and ticagrelor groups, respectively.
“One might expect a higher ischemic event rate with clopidogrel compared to ticagrelor. However, in these elderly patients there was no difference between the two treatment strategies,” the cardiologist observed.
POP AGE is hailed as ‘a wake up call’
In an interview, Freek Verheugt, MD, PhD, professor emeritus of cardiology at Radboud University in Nijmegen, The Netherlands, called POP AGE “a very important study.”
“The problem with most studies in the elderly is that they are post hoc analyses from huge trials like PLATO and TRITON, and also the thrombolysis and primary PCI studies. The elderly do very well in those studies, because only the very fit elderly are included in the megatrials. It’s much more important to do a prospective randomized trial in the elderly only, and this is one of the very few done so far,” he observed.
Bleeding is a major problem in the elderly with ACS. It leads to more MIs, strokes, and increased mortality.
“Even minor bleeding is an issue,” Dr. Verheugt added. “Minor bleeding is a major problem, because patients who encounter minor bleeding – nose bleeds, gum bleeds, or even in their underwear – they do away with all drugs. They stop their antithrombotic, but they also stop their statin, their ACE inhibitor – their lifesavers – and that’s why they die.”
So is POP AGE a practice-changing study?
“No, of course not,” the cardiologist scoffed. “To be practice-changing you need several trials going in the same direction. But I think if there are more data prospectively accrued in the elderly alone, showing the same, then POP AGE would be practice-changing.”
“In my personal view, this study is a wake-up call. If you have an elderly, frail patient presenting with ACS, strongly consider good, old clopidogrel. Although people say that 30% of patients on clopidogrel don’t have appropriate platelet inhibition, that’s a laboratory finding. It’s not a clinical finding. POP AGE gave us a clinical finding showing that they do quite well,” he said.
Dr. Verheugt was on the independent data safety monitoring board for POP AGE, funded by ZonMw, a Dutch governmental research organization. Neither Dr. Verheugt nor Dr. Gimbel reported having any financial conflicts of interest.
SOURCE: Gimbel ME. ESC 2019, Abstract 84.
AT THE ESC CONGRESS 2019
Key clinical point:
Major finding: The rate of major and minor bleeding was 17.6% with clopidogrel, compared with 23.1% in the ticagrelor group, for a highly significant 26% reduction in relative risk.
Study details: POPular AGE, an 11-center Dutch RCT, included 1,003 patients age 70 or older with non-ST-elevation ACS.
Disclosures: The presenter reported having no financial conflicts regarding the study, funded by the Dutch government.
Source: Gimbel ME. ESC 2019, Abstract 84.
Anticoagulant therapy for AFib in patients with end-stage renal disease
Warfarin or apixaban are sensible options
Case
A 78-year-old woman with end-stage renal disease (ESRD) is hospitalized with cellulitis and is incidentally found to be in atrial fibrillation. She does not have a history of mitral stenosis, nor does she have a prosthetic valve. She does have a history of hypertension, diabetes, and prior stroke without residual deficits.
After counseling her about the risk of stroke associated with atrial fibrillation (AFib) she makes it clear she is interested in pharmacologic therapy to minimize her risk of stroke and asks what medication you would recommend for anticoagulation.
Brief overview of the issue
Anticoagulation for AFib is indicated for stroke prophylaxis in patients with an elevated risk of stroke. The CHA2DS2-VASc score is useful in calculating an individual patient’s risk of stroke and as a decision tool to determine who would benefit from anticoagulation, and it is recommended in the American Heart Association guidelines.1
Low-risk patients (CHA2DS2-VASc score of 0 in men or 1 in women) should not be started on anticoagulation for stroke prophylaxis. For anyone with a risk factor, other than being female, anticoagulation is indicated and should be considered.
The guideline recommends anticoagulant therapy, not antiplatelet agents. For most of the recent past, this has meant a vitamin K antagonist (warfarin) or sometimes a low-molecular-weight heparin injected subcutaneously. Over the past decade, however, with the approval of multiple direct oral anticoagulants (DOACs), nonwarfarin oral anticoagulation has grown in popularity as the prophylactic medication of choice.2
While the data for patients with preserved renal function is robust, there is far less data to guide decision making for patients with end-stage renal disease.
Overview of the data
Until the introduction of DOACs, warfarin was the main agent used for stroke prophylaxis in patients with end-stage kidney disease and AFib. Professional guidelines favored warfarin for these patients who were mostly excluded from DOAC trials. Specialized conferences also looked at this issue.
The Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference, which reviewed chronic kidney disease and arrhythmias, noted that there were no randomized controlled trials that examined the efficacy and safety of anticoagulation in chronic kidney disease patients with estimated creatinine clearance less than 30 mL/min. They remarked that there was insufficient high-quality evidence to recommend warfarin for the prevention of stroke in patients with AFib and dialysis-dependent chronic kidney disease.
Since, according to other trials, DOACs had better safety profiles in other populations, the conference noted that lower-dose apixaban (2.5 mg orally twice daily) or rivaroxaban (15 mg daily) may be considered in this population until clinical safety data were available. Furthermore, the conference recommended that these patients be treated with a multidisciplinary approach in regards to anticoagulation and have an annual reevaluation of treatment goals, along with a risk-benefit assessment.3
Since the publication of the 2018 AHA guidelines and the guidance document that resulted from the KDIGO conference, additional research has been published comparing anticoagulation with a DOAC versus warfarin for AFib in patients with ESRD.
“Outcomes associated with apixaban use in patients with end-stage kidney disease and atrial fibrillation in the United States” was an observational, retrospective, cohort study that compared outcomes in dialysis patients who took warfarin for AFib with those who took apixaban.4 Patients’ data was taken from the U.S. Renal Data System database and were included in the final analysis if they had ESRD, a recent diagnosis of AFib or atrial flutter, and a new prescription for either warfarin or apixaban. Outcome measures were stroke or systemic embolism, major bleeding (critical site, transfusion, or death), gastrointestinal bleeding, intracranial bleeding, or death. Drug usage and compliance were assessed using Medicare Part D prescription information.
A total of 25,523 patients met the inclusion/exclusion criteria and had taken either warfarin (n = 23,172) or apixaban (n = 2,351). To account for selection bias in these cohorts, a subset of the warfarin patients was selected based on prognostic score matching. The prognostic score was calculated from the baseline characteristics (which included age, stroke history, diabetes, smoking, antiplatelet medication, liver disease, prior bleeding, and CHA2DS2-VASc score). Kaplan-Meier and Cox regression analysis were used to give hazard ratios and 95% confidence intervals for each outcome measure. Prespecified subgroup analyses were conducted to compare apixaban doses, where 44% were prescribed 5 mg b.i.d. and 56% were prescribed 2.5 mg b.i.d..
In the study, patients in the apixaban group had a significantly lower risk of major bleeding as compared with the warfarin group (HR, 0.72; 95% CI, 0.59-0.87; P less than .001) with overall high rates of major bleeding in both groups at 19.7 and 22.9 per 100 patient-years in the apixaban group and warfarin group, respectively. There was no difference in the rate of stroke/systemic embolism between patients receiving apixaban and warfarin (HR, 0.88; 95% CI, 0.69-1.12; P = .29). There was a nonsignificant trend toward decreased risk of GI bleeding in the apixaban group and no significant differences between the groups in the rates of intracranial bleeding. Apixaban was also associated with a nonsignificant trend toward lower risk of mortality (HR, 0.85; 95% CI, 0.71-1.01; P = .06).
Notably, censoring rates because of expired prescriptions or a 1-month gap between prescriptions were high in both groups and the majority of censoring occurred within the first 12 months. Additionally, in dose specific analyses, patients receiving the 5-mg, twice-daily dose were found to have statistically significant decreases in risk of stroke/systemic embolism (P = .035) and mortality (P = .005) as compared with the 2.5-mg, twice-daily dose without significant differences in GI or intracranial bleeding.
There are three ongoing, open-label, randomized, controlled trials examining anticoagulation for nonvalvular AFib in patients with ESRD on hemodialysis with two comparing apixaban to warfarin (or derivative) and the other warfarin versus no anticoagulation.5 All trials are in adult patients with documented AFib and CHA2DS2-VASc score of at least 2. AKADIA (Germany based) plans to enroll 222 patients and compares a vitamin K antagonist (INR goal, 2-3) with 2.5-mg b.i.d. apixaban patients with ESRD on hemodialysis for at least 3 months with primary outcome of major and clinically relevant nonmajor bleeding and secondary outcome of thromboembolic events, as well as apixaban levels pre- and post hemodialysis.
RENAL-AF (U.S. based) plans to enrolled 762 patients and compares 5-mg b.i.d. apixaban (with 2.5 mg for selected patients) with warfarin in people of chronic hemodialysis with primary outcome of days to first major or clinically relevant nonmajor bleeding event and secondary outcome of stroke, systemic embolism, mortality, adherence and plasma apixaban levels. AVKDIAL (France based) plans to enroll 855 patients and compares no anticoagulation with vitamin K antagonists in patients on hemodialysis for at least 1 month, with primary outcome of cumulative incidence of severe bleeding and thrombosis.
Application of the data to our original case
Our patient is Medicare age with ESRD and newly diagnosed nonvalvular AFib. Recent data suggests apixaban could be used for stroke prevention instead of the prior standard of care, warfarin. This approach is supported in the 2019 guidelines.1
Patients with ESRD have an increased risk of bleeding and apixaban was shown to have less bleeding complications than warfarin in this analysis. However, only standard-dose apixaban was associated with a statistically significant lower risk of stroke/systemic embolism, major bleeding, and death. Reduced-dose apixaban had a lower risk of major bleeding but no difference for stroke/systemic embolism or death. Reduced-dose apixaban is used for patients who have two out of the following three criteria: aged at least 80 years, weight of at least 60 kg, and creatinine of at least 1.5 mg/dL. Therefore, many Medicare-age patients with ESRD would not be indicated for the dose of apixaban that was shown to improve the most important outcomes of stroke/SE and death.
It may still be beneficial to use apixaban in this patient since it appears to work as well as warfarin for stroke/systemic embolism prevention with less bleeding complications.
Bottom line
For patients who have decided to pursue an anticoagulation strategy for stroke prevention in AFib and have end-stage renal disease, either warfarin or apixaban are sensible options.
Dr. Farber is a medical instructor at Duke University Health System in Durham, N.C. Dr. Stafford is a medical instructor at Duke University. Dr. Sata is assistant professor of medicine at Duke University. Dr. Abdo and Dr. Menon are hospitalists at Duke University. Dr. Brooks is assistant professor of medicine at Duke University. Dr. Wachter is associate medical director at Duke Regional Hospital and assistant professor of medicine at Duke University. Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and assistant professor of medicine at Duke University.
References
1. January CT et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;139. doi: 1161/CIR.0000000000000665.
2. Lippi G et al. Direct oral anticoagulants: Analysis of worldwide use and popularity using Google Trends. Ann Transl Med. 2017 Aug; 5(16):322. doi: 10.21037/atm.2017.06.65.
3. Turakhia MP et al. Chronic kidney disease and arrhythmias: Conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Eur Heart J. 2018 Jun 21;39(24):2314-25. doi: 10.1093/eurheartj/ehy060.
4. Siontis KC et al. Outcomes associated with apixaban use in patients with end-stage kidney disease and atrial fibrillation in the United States. Circulation. 2018 Oct 9;138(15):1519-29. doi: 10.1161/CIRCULATIONAHA.118.035418.
5. Nigwekar SU et al. Long-term anticoagulation for patient receiving dialysis: Tilting the benefit-to-risk ratio? Circulation. 2018 Oct 9;138(15):1530-3. doi: 10.1161/CIRCULATIONAHA.118.037091.
Key points
- According to 2019 American Heart Association guidelines, warfarin or apixaban are reasonable options for stroke prevention for patients who have end-stage renal disease and who plan for anticoagulation because of atrial fibrillation.
- Recent observational data suggests that apixaban may be safer than warfarin in this population.
- Several randomized, controlled trials are ongoing that may help determine the optimal agent to use in this setting.
- Until more definitive data is available, a reasonable approach is to discuss the risks and benefits of various treatment strategies with patients, and engage a multidisciplinary team (cardiologist, nephrologist, primary care provider, pharmacist) in the decision making process.
Additional reading
January CT et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;139. doi: 1161/CIR.0000000000000665.
Nigwekar SU et al. Long-term anticoagulation for patient receiving dialysis: Tilting the benefit to risk ratio? Circulation. 2018 Oct 9;138(15):1530-3. doi: 10.1161/CIRCULATIONAHA.118.037091.
Garlo KG et al. Demystifying the benefits and harms of anticoagulation for atrial fibrillation in chronic kidney disease. Clin J Am Soc Nephrol 2019;14:125-36. doi: 10.2215/CJN.06430518.
Quiz
Two days ago you admitted a 72-year-old woman with end-stage renal disease on dialysis who had developed new-onset atrial fibrillation causing a mild acute diastolic congestive heart failure exacerbation. Transthoracic ECG showed a preserved left ventricular ejection fraction and no significant valvular disease. After two sessions of dialysis in the hospital and initiation of a beta-blocker for control of her heart rate, she is stable and ready for discharge. Her discharge weight is 75 kg.
Which of the following recommendations should you make to this patient regarding anticoagulation for prevention of stroke and systemic embolism from atrial fibrillation?
A. Take warfarin with a international normalized ratio goal of 2.5.
B. Take apixaban 2.5 mg twice a day.
C. Take apixaban 5 mg twice a day.
D. Discuss the risks/benefits of various treatment approaches with the patient, and involve the hospital pharmacist as well as the patient’s nephrologist, cardiologist, and/or primary care provider in the decision making process to reach a consensus and to ensure a safe follow-up plan.
The best answer is D. While A, B, and C are all reasonable approaches based on the available data and current guidelines, the best approach is to involve the patient and the multidisciplinary team in the decision making process. When more clinical trial data becomes available in the future, the optimal approach to managing patients such as this one may become clearer, but until then it makes sense to take into account individual patient characteristics and patient preferences.
Warfarin or apixaban are sensible options
Warfarin or apixaban are sensible options
Case
A 78-year-old woman with end-stage renal disease (ESRD) is hospitalized with cellulitis and is incidentally found to be in atrial fibrillation. She does not have a history of mitral stenosis, nor does she have a prosthetic valve. She does have a history of hypertension, diabetes, and prior stroke without residual deficits.
After counseling her about the risk of stroke associated with atrial fibrillation (AFib) she makes it clear she is interested in pharmacologic therapy to minimize her risk of stroke and asks what medication you would recommend for anticoagulation.
Brief overview of the issue
Anticoagulation for AFib is indicated for stroke prophylaxis in patients with an elevated risk of stroke. The CHA2DS2-VASc score is useful in calculating an individual patient’s risk of stroke and as a decision tool to determine who would benefit from anticoagulation, and it is recommended in the American Heart Association guidelines.1
Low-risk patients (CHA2DS2-VASc score of 0 in men or 1 in women) should not be started on anticoagulation for stroke prophylaxis. For anyone with a risk factor, other than being female, anticoagulation is indicated and should be considered.
The guideline recommends anticoagulant therapy, not antiplatelet agents. For most of the recent past, this has meant a vitamin K antagonist (warfarin) or sometimes a low-molecular-weight heparin injected subcutaneously. Over the past decade, however, with the approval of multiple direct oral anticoagulants (DOACs), nonwarfarin oral anticoagulation has grown in popularity as the prophylactic medication of choice.2
While the data for patients with preserved renal function is robust, there is far less data to guide decision making for patients with end-stage renal disease.
Overview of the data
Until the introduction of DOACs, warfarin was the main agent used for stroke prophylaxis in patients with end-stage kidney disease and AFib. Professional guidelines favored warfarin for these patients who were mostly excluded from DOAC trials. Specialized conferences also looked at this issue.
The Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference, which reviewed chronic kidney disease and arrhythmias, noted that there were no randomized controlled trials that examined the efficacy and safety of anticoagulation in chronic kidney disease patients with estimated creatinine clearance less than 30 mL/min. They remarked that there was insufficient high-quality evidence to recommend warfarin for the prevention of stroke in patients with AFib and dialysis-dependent chronic kidney disease.
Since, according to other trials, DOACs had better safety profiles in other populations, the conference noted that lower-dose apixaban (2.5 mg orally twice daily) or rivaroxaban (15 mg daily) may be considered in this population until clinical safety data were available. Furthermore, the conference recommended that these patients be treated with a multidisciplinary approach in regards to anticoagulation and have an annual reevaluation of treatment goals, along with a risk-benefit assessment.3
Since the publication of the 2018 AHA guidelines and the guidance document that resulted from the KDIGO conference, additional research has been published comparing anticoagulation with a DOAC versus warfarin for AFib in patients with ESRD.
“Outcomes associated with apixaban use in patients with end-stage kidney disease and atrial fibrillation in the United States” was an observational, retrospective, cohort study that compared outcomes in dialysis patients who took warfarin for AFib with those who took apixaban.4 Patients’ data was taken from the U.S. Renal Data System database and were included in the final analysis if they had ESRD, a recent diagnosis of AFib or atrial flutter, and a new prescription for either warfarin or apixaban. Outcome measures were stroke or systemic embolism, major bleeding (critical site, transfusion, or death), gastrointestinal bleeding, intracranial bleeding, or death. Drug usage and compliance were assessed using Medicare Part D prescription information.
A total of 25,523 patients met the inclusion/exclusion criteria and had taken either warfarin (n = 23,172) or apixaban (n = 2,351). To account for selection bias in these cohorts, a subset of the warfarin patients was selected based on prognostic score matching. The prognostic score was calculated from the baseline characteristics (which included age, stroke history, diabetes, smoking, antiplatelet medication, liver disease, prior bleeding, and CHA2DS2-VASc score). Kaplan-Meier and Cox regression analysis were used to give hazard ratios and 95% confidence intervals for each outcome measure. Prespecified subgroup analyses were conducted to compare apixaban doses, where 44% were prescribed 5 mg b.i.d. and 56% were prescribed 2.5 mg b.i.d..
In the study, patients in the apixaban group had a significantly lower risk of major bleeding as compared with the warfarin group (HR, 0.72; 95% CI, 0.59-0.87; P less than .001) with overall high rates of major bleeding in both groups at 19.7 and 22.9 per 100 patient-years in the apixaban group and warfarin group, respectively. There was no difference in the rate of stroke/systemic embolism between patients receiving apixaban and warfarin (HR, 0.88; 95% CI, 0.69-1.12; P = .29). There was a nonsignificant trend toward decreased risk of GI bleeding in the apixaban group and no significant differences between the groups in the rates of intracranial bleeding. Apixaban was also associated with a nonsignificant trend toward lower risk of mortality (HR, 0.85; 95% CI, 0.71-1.01; P = .06).
Notably, censoring rates because of expired prescriptions or a 1-month gap between prescriptions were high in both groups and the majority of censoring occurred within the first 12 months. Additionally, in dose specific analyses, patients receiving the 5-mg, twice-daily dose were found to have statistically significant decreases in risk of stroke/systemic embolism (P = .035) and mortality (P = .005) as compared with the 2.5-mg, twice-daily dose without significant differences in GI or intracranial bleeding.
There are three ongoing, open-label, randomized, controlled trials examining anticoagulation for nonvalvular AFib in patients with ESRD on hemodialysis with two comparing apixaban to warfarin (or derivative) and the other warfarin versus no anticoagulation.5 All trials are in adult patients with documented AFib and CHA2DS2-VASc score of at least 2. AKADIA (Germany based) plans to enroll 222 patients and compares a vitamin K antagonist (INR goal, 2-3) with 2.5-mg b.i.d. apixaban patients with ESRD on hemodialysis for at least 3 months with primary outcome of major and clinically relevant nonmajor bleeding and secondary outcome of thromboembolic events, as well as apixaban levels pre- and post hemodialysis.
RENAL-AF (U.S. based) plans to enrolled 762 patients and compares 5-mg b.i.d. apixaban (with 2.5 mg for selected patients) with warfarin in people of chronic hemodialysis with primary outcome of days to first major or clinically relevant nonmajor bleeding event and secondary outcome of stroke, systemic embolism, mortality, adherence and plasma apixaban levels. AVKDIAL (France based) plans to enroll 855 patients and compares no anticoagulation with vitamin K antagonists in patients on hemodialysis for at least 1 month, with primary outcome of cumulative incidence of severe bleeding and thrombosis.
Application of the data to our original case
Our patient is Medicare age with ESRD and newly diagnosed nonvalvular AFib. Recent data suggests apixaban could be used for stroke prevention instead of the prior standard of care, warfarin. This approach is supported in the 2019 guidelines.1
Patients with ESRD have an increased risk of bleeding and apixaban was shown to have less bleeding complications than warfarin in this analysis. However, only standard-dose apixaban was associated with a statistically significant lower risk of stroke/systemic embolism, major bleeding, and death. Reduced-dose apixaban had a lower risk of major bleeding but no difference for stroke/systemic embolism or death. Reduced-dose apixaban is used for patients who have two out of the following three criteria: aged at least 80 years, weight of at least 60 kg, and creatinine of at least 1.5 mg/dL. Therefore, many Medicare-age patients with ESRD would not be indicated for the dose of apixaban that was shown to improve the most important outcomes of stroke/SE and death.
It may still be beneficial to use apixaban in this patient since it appears to work as well as warfarin for stroke/systemic embolism prevention with less bleeding complications.
Bottom line
For patients who have decided to pursue an anticoagulation strategy for stroke prevention in AFib and have end-stage renal disease, either warfarin or apixaban are sensible options.
Dr. Farber is a medical instructor at Duke University Health System in Durham, N.C. Dr. Stafford is a medical instructor at Duke University. Dr. Sata is assistant professor of medicine at Duke University. Dr. Abdo and Dr. Menon are hospitalists at Duke University. Dr. Brooks is assistant professor of medicine at Duke University. Dr. Wachter is associate medical director at Duke Regional Hospital and assistant professor of medicine at Duke University. Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and assistant professor of medicine at Duke University.
References
1. January CT et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;139. doi: 1161/CIR.0000000000000665.
2. Lippi G et al. Direct oral anticoagulants: Analysis of worldwide use and popularity using Google Trends. Ann Transl Med. 2017 Aug; 5(16):322. doi: 10.21037/atm.2017.06.65.
3. Turakhia MP et al. Chronic kidney disease and arrhythmias: Conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Eur Heart J. 2018 Jun 21;39(24):2314-25. doi: 10.1093/eurheartj/ehy060.
4. Siontis KC et al. Outcomes associated with apixaban use in patients with end-stage kidney disease and atrial fibrillation in the United States. Circulation. 2018 Oct 9;138(15):1519-29. doi: 10.1161/CIRCULATIONAHA.118.035418.
5. Nigwekar SU et al. Long-term anticoagulation for patient receiving dialysis: Tilting the benefit-to-risk ratio? Circulation. 2018 Oct 9;138(15):1530-3. doi: 10.1161/CIRCULATIONAHA.118.037091.
Key points
- According to 2019 American Heart Association guidelines, warfarin or apixaban are reasonable options for stroke prevention for patients who have end-stage renal disease and who plan for anticoagulation because of atrial fibrillation.
- Recent observational data suggests that apixaban may be safer than warfarin in this population.
- Several randomized, controlled trials are ongoing that may help determine the optimal agent to use in this setting.
- Until more definitive data is available, a reasonable approach is to discuss the risks and benefits of various treatment strategies with patients, and engage a multidisciplinary team (cardiologist, nephrologist, primary care provider, pharmacist) in the decision making process.
Additional reading
January CT et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;139. doi: 1161/CIR.0000000000000665.
Nigwekar SU et al. Long-term anticoagulation for patient receiving dialysis: Tilting the benefit to risk ratio? Circulation. 2018 Oct 9;138(15):1530-3. doi: 10.1161/CIRCULATIONAHA.118.037091.
Garlo KG et al. Demystifying the benefits and harms of anticoagulation for atrial fibrillation in chronic kidney disease. Clin J Am Soc Nephrol 2019;14:125-36. doi: 10.2215/CJN.06430518.
Quiz
Two days ago you admitted a 72-year-old woman with end-stage renal disease on dialysis who had developed new-onset atrial fibrillation causing a mild acute diastolic congestive heart failure exacerbation. Transthoracic ECG showed a preserved left ventricular ejection fraction and no significant valvular disease. After two sessions of dialysis in the hospital and initiation of a beta-blocker for control of her heart rate, she is stable and ready for discharge. Her discharge weight is 75 kg.
Which of the following recommendations should you make to this patient regarding anticoagulation for prevention of stroke and systemic embolism from atrial fibrillation?
A. Take warfarin with a international normalized ratio goal of 2.5.
B. Take apixaban 2.5 mg twice a day.
C. Take apixaban 5 mg twice a day.
D. Discuss the risks/benefits of various treatment approaches with the patient, and involve the hospital pharmacist as well as the patient’s nephrologist, cardiologist, and/or primary care provider in the decision making process to reach a consensus and to ensure a safe follow-up plan.
The best answer is D. While A, B, and C are all reasonable approaches based on the available data and current guidelines, the best approach is to involve the patient and the multidisciplinary team in the decision making process. When more clinical trial data becomes available in the future, the optimal approach to managing patients such as this one may become clearer, but until then it makes sense to take into account individual patient characteristics and patient preferences.
Case
A 78-year-old woman with end-stage renal disease (ESRD) is hospitalized with cellulitis and is incidentally found to be in atrial fibrillation. She does not have a history of mitral stenosis, nor does she have a prosthetic valve. She does have a history of hypertension, diabetes, and prior stroke without residual deficits.
After counseling her about the risk of stroke associated with atrial fibrillation (AFib) she makes it clear she is interested in pharmacologic therapy to minimize her risk of stroke and asks what medication you would recommend for anticoagulation.
Brief overview of the issue
Anticoagulation for AFib is indicated for stroke prophylaxis in patients with an elevated risk of stroke. The CHA2DS2-VASc score is useful in calculating an individual patient’s risk of stroke and as a decision tool to determine who would benefit from anticoagulation, and it is recommended in the American Heart Association guidelines.1
Low-risk patients (CHA2DS2-VASc score of 0 in men or 1 in women) should not be started on anticoagulation for stroke prophylaxis. For anyone with a risk factor, other than being female, anticoagulation is indicated and should be considered.
The guideline recommends anticoagulant therapy, not antiplatelet agents. For most of the recent past, this has meant a vitamin K antagonist (warfarin) or sometimes a low-molecular-weight heparin injected subcutaneously. Over the past decade, however, with the approval of multiple direct oral anticoagulants (DOACs), nonwarfarin oral anticoagulation has grown in popularity as the prophylactic medication of choice.2
While the data for patients with preserved renal function is robust, there is far less data to guide decision making for patients with end-stage renal disease.
Overview of the data
Until the introduction of DOACs, warfarin was the main agent used for stroke prophylaxis in patients with end-stage kidney disease and AFib. Professional guidelines favored warfarin for these patients who were mostly excluded from DOAC trials. Specialized conferences also looked at this issue.
The Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference, which reviewed chronic kidney disease and arrhythmias, noted that there were no randomized controlled trials that examined the efficacy and safety of anticoagulation in chronic kidney disease patients with estimated creatinine clearance less than 30 mL/min. They remarked that there was insufficient high-quality evidence to recommend warfarin for the prevention of stroke in patients with AFib and dialysis-dependent chronic kidney disease.
Since, according to other trials, DOACs had better safety profiles in other populations, the conference noted that lower-dose apixaban (2.5 mg orally twice daily) or rivaroxaban (15 mg daily) may be considered in this population until clinical safety data were available. Furthermore, the conference recommended that these patients be treated with a multidisciplinary approach in regards to anticoagulation and have an annual reevaluation of treatment goals, along with a risk-benefit assessment.3
Since the publication of the 2018 AHA guidelines and the guidance document that resulted from the KDIGO conference, additional research has been published comparing anticoagulation with a DOAC versus warfarin for AFib in patients with ESRD.
“Outcomes associated with apixaban use in patients with end-stage kidney disease and atrial fibrillation in the United States” was an observational, retrospective, cohort study that compared outcomes in dialysis patients who took warfarin for AFib with those who took apixaban.4 Patients’ data was taken from the U.S. Renal Data System database and were included in the final analysis if they had ESRD, a recent diagnosis of AFib or atrial flutter, and a new prescription for either warfarin or apixaban. Outcome measures were stroke or systemic embolism, major bleeding (critical site, transfusion, or death), gastrointestinal bleeding, intracranial bleeding, or death. Drug usage and compliance were assessed using Medicare Part D prescription information.
A total of 25,523 patients met the inclusion/exclusion criteria and had taken either warfarin (n = 23,172) or apixaban (n = 2,351). To account for selection bias in these cohorts, a subset of the warfarin patients was selected based on prognostic score matching. The prognostic score was calculated from the baseline characteristics (which included age, stroke history, diabetes, smoking, antiplatelet medication, liver disease, prior bleeding, and CHA2DS2-VASc score). Kaplan-Meier and Cox regression analysis were used to give hazard ratios and 95% confidence intervals for each outcome measure. Prespecified subgroup analyses were conducted to compare apixaban doses, where 44% were prescribed 5 mg b.i.d. and 56% were prescribed 2.5 mg b.i.d..
In the study, patients in the apixaban group had a significantly lower risk of major bleeding as compared with the warfarin group (HR, 0.72; 95% CI, 0.59-0.87; P less than .001) with overall high rates of major bleeding in both groups at 19.7 and 22.9 per 100 patient-years in the apixaban group and warfarin group, respectively. There was no difference in the rate of stroke/systemic embolism between patients receiving apixaban and warfarin (HR, 0.88; 95% CI, 0.69-1.12; P = .29). There was a nonsignificant trend toward decreased risk of GI bleeding in the apixaban group and no significant differences between the groups in the rates of intracranial bleeding. Apixaban was also associated with a nonsignificant trend toward lower risk of mortality (HR, 0.85; 95% CI, 0.71-1.01; P = .06).
Notably, censoring rates because of expired prescriptions or a 1-month gap between prescriptions were high in both groups and the majority of censoring occurred within the first 12 months. Additionally, in dose specific analyses, patients receiving the 5-mg, twice-daily dose were found to have statistically significant decreases in risk of stroke/systemic embolism (P = .035) and mortality (P = .005) as compared with the 2.5-mg, twice-daily dose without significant differences in GI or intracranial bleeding.
There are three ongoing, open-label, randomized, controlled trials examining anticoagulation for nonvalvular AFib in patients with ESRD on hemodialysis with two comparing apixaban to warfarin (or derivative) and the other warfarin versus no anticoagulation.5 All trials are in adult patients with documented AFib and CHA2DS2-VASc score of at least 2. AKADIA (Germany based) plans to enroll 222 patients and compares a vitamin K antagonist (INR goal, 2-3) with 2.5-mg b.i.d. apixaban patients with ESRD on hemodialysis for at least 3 months with primary outcome of major and clinically relevant nonmajor bleeding and secondary outcome of thromboembolic events, as well as apixaban levels pre- and post hemodialysis.
RENAL-AF (U.S. based) plans to enrolled 762 patients and compares 5-mg b.i.d. apixaban (with 2.5 mg for selected patients) with warfarin in people of chronic hemodialysis with primary outcome of days to first major or clinically relevant nonmajor bleeding event and secondary outcome of stroke, systemic embolism, mortality, adherence and plasma apixaban levels. AVKDIAL (France based) plans to enroll 855 patients and compares no anticoagulation with vitamin K antagonists in patients on hemodialysis for at least 1 month, with primary outcome of cumulative incidence of severe bleeding and thrombosis.
Application of the data to our original case
Our patient is Medicare age with ESRD and newly diagnosed nonvalvular AFib. Recent data suggests apixaban could be used for stroke prevention instead of the prior standard of care, warfarin. This approach is supported in the 2019 guidelines.1
Patients with ESRD have an increased risk of bleeding and apixaban was shown to have less bleeding complications than warfarin in this analysis. However, only standard-dose apixaban was associated with a statistically significant lower risk of stroke/systemic embolism, major bleeding, and death. Reduced-dose apixaban had a lower risk of major bleeding but no difference for stroke/systemic embolism or death. Reduced-dose apixaban is used for patients who have two out of the following three criteria: aged at least 80 years, weight of at least 60 kg, and creatinine of at least 1.5 mg/dL. Therefore, many Medicare-age patients with ESRD would not be indicated for the dose of apixaban that was shown to improve the most important outcomes of stroke/SE and death.
It may still be beneficial to use apixaban in this patient since it appears to work as well as warfarin for stroke/systemic embolism prevention with less bleeding complications.
Bottom line
For patients who have decided to pursue an anticoagulation strategy for stroke prevention in AFib and have end-stage renal disease, either warfarin or apixaban are sensible options.
Dr. Farber is a medical instructor at Duke University Health System in Durham, N.C. Dr. Stafford is a medical instructor at Duke University. Dr. Sata is assistant professor of medicine at Duke University. Dr. Abdo and Dr. Menon are hospitalists at Duke University. Dr. Brooks is assistant professor of medicine at Duke University. Dr. Wachter is associate medical director at Duke Regional Hospital and assistant professor of medicine at Duke University. Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and assistant professor of medicine at Duke University.
References
1. January CT et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;139. doi: 1161/CIR.0000000000000665.
2. Lippi G et al. Direct oral anticoagulants: Analysis of worldwide use and popularity using Google Trends. Ann Transl Med. 2017 Aug; 5(16):322. doi: 10.21037/atm.2017.06.65.
3. Turakhia MP et al. Chronic kidney disease and arrhythmias: Conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Eur Heart J. 2018 Jun 21;39(24):2314-25. doi: 10.1093/eurheartj/ehy060.
4. Siontis KC et al. Outcomes associated with apixaban use in patients with end-stage kidney disease and atrial fibrillation in the United States. Circulation. 2018 Oct 9;138(15):1519-29. doi: 10.1161/CIRCULATIONAHA.118.035418.
5. Nigwekar SU et al. Long-term anticoagulation for patient receiving dialysis: Tilting the benefit-to-risk ratio? Circulation. 2018 Oct 9;138(15):1530-3. doi: 10.1161/CIRCULATIONAHA.118.037091.
Key points
- According to 2019 American Heart Association guidelines, warfarin or apixaban are reasonable options for stroke prevention for patients who have end-stage renal disease and who plan for anticoagulation because of atrial fibrillation.
- Recent observational data suggests that apixaban may be safer than warfarin in this population.
- Several randomized, controlled trials are ongoing that may help determine the optimal agent to use in this setting.
- Until more definitive data is available, a reasonable approach is to discuss the risks and benefits of various treatment strategies with patients, and engage a multidisciplinary team (cardiologist, nephrologist, primary care provider, pharmacist) in the decision making process.
Additional reading
January CT et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;139. doi: 1161/CIR.0000000000000665.
Nigwekar SU et al. Long-term anticoagulation for patient receiving dialysis: Tilting the benefit to risk ratio? Circulation. 2018 Oct 9;138(15):1530-3. doi: 10.1161/CIRCULATIONAHA.118.037091.
Garlo KG et al. Demystifying the benefits and harms of anticoagulation for atrial fibrillation in chronic kidney disease. Clin J Am Soc Nephrol 2019;14:125-36. doi: 10.2215/CJN.06430518.
Quiz
Two days ago you admitted a 72-year-old woman with end-stage renal disease on dialysis who had developed new-onset atrial fibrillation causing a mild acute diastolic congestive heart failure exacerbation. Transthoracic ECG showed a preserved left ventricular ejection fraction and no significant valvular disease. After two sessions of dialysis in the hospital and initiation of a beta-blocker for control of her heart rate, she is stable and ready for discharge. Her discharge weight is 75 kg.
Which of the following recommendations should you make to this patient regarding anticoagulation for prevention of stroke and systemic embolism from atrial fibrillation?
A. Take warfarin with a international normalized ratio goal of 2.5.
B. Take apixaban 2.5 mg twice a day.
C. Take apixaban 5 mg twice a day.
D. Discuss the risks/benefits of various treatment approaches with the patient, and involve the hospital pharmacist as well as the patient’s nephrologist, cardiologist, and/or primary care provider in the decision making process to reach a consensus and to ensure a safe follow-up plan.
The best answer is D. While A, B, and C are all reasonable approaches based on the available data and current guidelines, the best approach is to involve the patient and the multidisciplinary team in the decision making process. When more clinical trial data becomes available in the future, the optimal approach to managing patients such as this one may become clearer, but until then it makes sense to take into account individual patient characteristics and patient preferences.
Post-TAVR anticoagulation alone fails to cut stroke risk in AFib
In patients with atrial fibrillation (AFib) who have undergone transcatheter aortic valve replacement (TAVR) and had a CHA2DS2-VASc score of at least 2, oral anticoagulant (OAC) therapy alone was not linked to reduced stroke risk.
By contrast, antiplatelet therapy was linked to a reduced risk of stroke in those AFib-TAVR patients, regardless of whether an oral anticoagulant was on board, according to results of a substudy of the randomized PARTNER II (Placement of Aortic Transcatheter Valve II) trial and its associated registries.
“Anticoagulant therapy was associated with a reduced risk of stroke and the composite of death or stroke when used concomitantly with uninterrupted antiplatelet therapy following TAVR,” concluded authors of the analysis, led by Ioanna Kosmidou, MD, PhD, of Columbia University in New York.
Taken together, these findings suggest OAC alone is “not sufficient” to prevent cerebrovascular events after TAVR in patients with AFib, Dr. Kosmidou and colleagues reported in JACC: Cardiovascular Interventions.
The analysis of the PARTNER II substudy included a total of 1,621 patients with aortic stenosis treated with TAVR who had a history of AFib and an absolute indication for anticoagulation as evidenced by a CHA2DS2-VASc score of at least 2.
Despite the absolute indication for anticoagulation, more than 40% of these patients were not prescribed an OAC upon discharge, investigators wrote, though the rate of nonprescribing decreased over the 5-year enrollment period of 2011-2015.
OAC therapy alone was not linked to reduced stroke risk in this cohort, investigators said. After 2 years, the rate of stroke was 6.6% for AFib-TAVR patients on anticoagulant therapy, and 5.6% for those who were not on anticoagulant therapy, a nonsignificant difference at P = 0.53, according to the reported data.
By contrast, uninterrupted antiplatelet therapy reduced both risk of stroke and risk of the composite endpoint of stroke and death at 2 years “irrespective of concomitant anticoagulation,” Dr. Kosmidou and coinvestigators wrote in the report.
The stroke rates were 5.4% for antiplatelet therapy plus OAC, versus 11.1% for those receiving neither antithrombotic treatment (P = 0.03), while the rates of stroke or death were 29.7% and 40.1%, respectively (P = 0.01), according to investigators.
After adjustment, stroke risk was not significantly reduced for OAC when compared with no OAC or antiplatelet therapy (HR, 0.61; P = .16), whereas stroke risk was indeed reduced for antiplatelet therapy alone (HR, 0.32; P = .002) and antiplatelet therapy with oral anticoagulation (HR, 0.44; P = .018).
The PARTNER II study was funded by Edwards Lifesciences. Senior author Martin B. Leon, MD, and several other study coauthors reported disclosures related to Edwards Lifesciences, in addition to Abbott Vascular, Cordis, Medtronic, Boston Scientific, and other companies. Dr. Kosmidou reported no disclosures.
SOURCE: Kosmidou I et al. JACC Cardiovasc Interv. 2019;12:1580-9.
Results of this PARTNER II substudy investigation by Kosmidou and colleagues are timely and thought provoking because they imply that some current recommendations may be insufficient for preventing stroke in patients with atrial fibrillation (AFib) undergoing transcatheter aortic valve replacement (TAVR).
Specifically, the results showed no difference in risk of stroke or the composite of death and stroke at 2 years in oral anticoagulant (OAC) and non-OAC patient groups, whereas by contrast, antiplatelet therapy was linked with reduced stroke risk versus no antithrombotic therapy, whether or not the patients received OAC.
The substudy reinforces the understanding that TAVR itself is a determinant of stroke because of mechanisms that go beyond thrombus formation in the left atrial appendage and are essentially platelet mediated.
How to manage antithrombotic therapy in patients with AFib who undergo TAVR remains a residual field of ambiguity.
However, observational studies cannot be conclusive, they said, so results of relevant prospective, randomized trials are eagerly awaited.
For example, the effects of novel oral anticoagulants versus vitamin K antagonists will be evaluated in the ENVISAGE-TAVI study, as well as the ATLANTIS trial, which will additionally include non-OAC patients.
The relative benefits of OAC alone versus OAC plus antiplatelet therapy will be evaluated in the AVATAR study, which will include AFib-TAVR patients randomized to OAC versus OAC plus aspirin, while the POPular-TAVI and CLOE trials will also include cohorts that help provide a more eloquent answer regarding the benefit-risk ratio of combining antiplatelet therapy and OAC in these patients.
Davide Capodanno, MD, PhD, and Antonio Greco, MD, of the University of Catania (Italy) made these comments in an accompanying editorial (JACC: Cardiovasc Interv. 2019 Aug 19. doi: 10.1016/j.jcin.2019.07.004). Dr. Capodanno reported disclosures related to Abbott Vascular, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Daiichi-Sankyo, and Sanofi. Dr. Greco reported having no relevant disclosures.
Results of this PARTNER II substudy investigation by Kosmidou and colleagues are timely and thought provoking because they imply that some current recommendations may be insufficient for preventing stroke in patients with atrial fibrillation (AFib) undergoing transcatheter aortic valve replacement (TAVR).
Specifically, the results showed no difference in risk of stroke or the composite of death and stroke at 2 years in oral anticoagulant (OAC) and non-OAC patient groups, whereas by contrast, antiplatelet therapy was linked with reduced stroke risk versus no antithrombotic therapy, whether or not the patients received OAC.
The substudy reinforces the understanding that TAVR itself is a determinant of stroke because of mechanisms that go beyond thrombus formation in the left atrial appendage and are essentially platelet mediated.
How to manage antithrombotic therapy in patients with AFib who undergo TAVR remains a residual field of ambiguity.
However, observational studies cannot be conclusive, they said, so results of relevant prospective, randomized trials are eagerly awaited.
For example, the effects of novel oral anticoagulants versus vitamin K antagonists will be evaluated in the ENVISAGE-TAVI study, as well as the ATLANTIS trial, which will additionally include non-OAC patients.
The relative benefits of OAC alone versus OAC plus antiplatelet therapy will be evaluated in the AVATAR study, which will include AFib-TAVR patients randomized to OAC versus OAC plus aspirin, while the POPular-TAVI and CLOE trials will also include cohorts that help provide a more eloquent answer regarding the benefit-risk ratio of combining antiplatelet therapy and OAC in these patients.
Davide Capodanno, MD, PhD, and Antonio Greco, MD, of the University of Catania (Italy) made these comments in an accompanying editorial (JACC: Cardiovasc Interv. 2019 Aug 19. doi: 10.1016/j.jcin.2019.07.004). Dr. Capodanno reported disclosures related to Abbott Vascular, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Daiichi-Sankyo, and Sanofi. Dr. Greco reported having no relevant disclosures.
Results of this PARTNER II substudy investigation by Kosmidou and colleagues are timely and thought provoking because they imply that some current recommendations may be insufficient for preventing stroke in patients with atrial fibrillation (AFib) undergoing transcatheter aortic valve replacement (TAVR).
Specifically, the results showed no difference in risk of stroke or the composite of death and stroke at 2 years in oral anticoagulant (OAC) and non-OAC patient groups, whereas by contrast, antiplatelet therapy was linked with reduced stroke risk versus no antithrombotic therapy, whether or not the patients received OAC.
The substudy reinforces the understanding that TAVR itself is a determinant of stroke because of mechanisms that go beyond thrombus formation in the left atrial appendage and are essentially platelet mediated.
How to manage antithrombotic therapy in patients with AFib who undergo TAVR remains a residual field of ambiguity.
However, observational studies cannot be conclusive, they said, so results of relevant prospective, randomized trials are eagerly awaited.
For example, the effects of novel oral anticoagulants versus vitamin K antagonists will be evaluated in the ENVISAGE-TAVI study, as well as the ATLANTIS trial, which will additionally include non-OAC patients.
The relative benefits of OAC alone versus OAC plus antiplatelet therapy will be evaluated in the AVATAR study, which will include AFib-TAVR patients randomized to OAC versus OAC plus aspirin, while the POPular-TAVI and CLOE trials will also include cohorts that help provide a more eloquent answer regarding the benefit-risk ratio of combining antiplatelet therapy and OAC in these patients.
Davide Capodanno, MD, PhD, and Antonio Greco, MD, of the University of Catania (Italy) made these comments in an accompanying editorial (JACC: Cardiovasc Interv. 2019 Aug 19. doi: 10.1016/j.jcin.2019.07.004). Dr. Capodanno reported disclosures related to Abbott Vascular, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Daiichi-Sankyo, and Sanofi. Dr. Greco reported having no relevant disclosures.
In patients with atrial fibrillation (AFib) who have undergone transcatheter aortic valve replacement (TAVR) and had a CHA2DS2-VASc score of at least 2, oral anticoagulant (OAC) therapy alone was not linked to reduced stroke risk.
By contrast, antiplatelet therapy was linked to a reduced risk of stroke in those AFib-TAVR patients, regardless of whether an oral anticoagulant was on board, according to results of a substudy of the randomized PARTNER II (Placement of Aortic Transcatheter Valve II) trial and its associated registries.
“Anticoagulant therapy was associated with a reduced risk of stroke and the composite of death or stroke when used concomitantly with uninterrupted antiplatelet therapy following TAVR,” concluded authors of the analysis, led by Ioanna Kosmidou, MD, PhD, of Columbia University in New York.
Taken together, these findings suggest OAC alone is “not sufficient” to prevent cerebrovascular events after TAVR in patients with AFib, Dr. Kosmidou and colleagues reported in JACC: Cardiovascular Interventions.
The analysis of the PARTNER II substudy included a total of 1,621 patients with aortic stenosis treated with TAVR who had a history of AFib and an absolute indication for anticoagulation as evidenced by a CHA2DS2-VASc score of at least 2.
Despite the absolute indication for anticoagulation, more than 40% of these patients were not prescribed an OAC upon discharge, investigators wrote, though the rate of nonprescribing decreased over the 5-year enrollment period of 2011-2015.
OAC therapy alone was not linked to reduced stroke risk in this cohort, investigators said. After 2 years, the rate of stroke was 6.6% for AFib-TAVR patients on anticoagulant therapy, and 5.6% for those who were not on anticoagulant therapy, a nonsignificant difference at P = 0.53, according to the reported data.
By contrast, uninterrupted antiplatelet therapy reduced both risk of stroke and risk of the composite endpoint of stroke and death at 2 years “irrespective of concomitant anticoagulation,” Dr. Kosmidou and coinvestigators wrote in the report.
The stroke rates were 5.4% for antiplatelet therapy plus OAC, versus 11.1% for those receiving neither antithrombotic treatment (P = 0.03), while the rates of stroke or death were 29.7% and 40.1%, respectively (P = 0.01), according to investigators.
After adjustment, stroke risk was not significantly reduced for OAC when compared with no OAC or antiplatelet therapy (HR, 0.61; P = .16), whereas stroke risk was indeed reduced for antiplatelet therapy alone (HR, 0.32; P = .002) and antiplatelet therapy with oral anticoagulation (HR, 0.44; P = .018).
The PARTNER II study was funded by Edwards Lifesciences. Senior author Martin B. Leon, MD, and several other study coauthors reported disclosures related to Edwards Lifesciences, in addition to Abbott Vascular, Cordis, Medtronic, Boston Scientific, and other companies. Dr. Kosmidou reported no disclosures.
SOURCE: Kosmidou I et al. JACC Cardiovasc Interv. 2019;12:1580-9.
In patients with atrial fibrillation (AFib) who have undergone transcatheter aortic valve replacement (TAVR) and had a CHA2DS2-VASc score of at least 2, oral anticoagulant (OAC) therapy alone was not linked to reduced stroke risk.
By contrast, antiplatelet therapy was linked to a reduced risk of stroke in those AFib-TAVR patients, regardless of whether an oral anticoagulant was on board, according to results of a substudy of the randomized PARTNER II (Placement of Aortic Transcatheter Valve II) trial and its associated registries.
“Anticoagulant therapy was associated with a reduced risk of stroke and the composite of death or stroke when used concomitantly with uninterrupted antiplatelet therapy following TAVR,” concluded authors of the analysis, led by Ioanna Kosmidou, MD, PhD, of Columbia University in New York.
Taken together, these findings suggest OAC alone is “not sufficient” to prevent cerebrovascular events after TAVR in patients with AFib, Dr. Kosmidou and colleagues reported in JACC: Cardiovascular Interventions.
The analysis of the PARTNER II substudy included a total of 1,621 patients with aortic stenosis treated with TAVR who had a history of AFib and an absolute indication for anticoagulation as evidenced by a CHA2DS2-VASc score of at least 2.
Despite the absolute indication for anticoagulation, more than 40% of these patients were not prescribed an OAC upon discharge, investigators wrote, though the rate of nonprescribing decreased over the 5-year enrollment period of 2011-2015.
OAC therapy alone was not linked to reduced stroke risk in this cohort, investigators said. After 2 years, the rate of stroke was 6.6% for AFib-TAVR patients on anticoagulant therapy, and 5.6% for those who were not on anticoagulant therapy, a nonsignificant difference at P = 0.53, according to the reported data.
By contrast, uninterrupted antiplatelet therapy reduced both risk of stroke and risk of the composite endpoint of stroke and death at 2 years “irrespective of concomitant anticoagulation,” Dr. Kosmidou and coinvestigators wrote in the report.
The stroke rates were 5.4% for antiplatelet therapy plus OAC, versus 11.1% for those receiving neither antithrombotic treatment (P = 0.03), while the rates of stroke or death were 29.7% and 40.1%, respectively (P = 0.01), according to investigators.
After adjustment, stroke risk was not significantly reduced for OAC when compared with no OAC or antiplatelet therapy (HR, 0.61; P = .16), whereas stroke risk was indeed reduced for antiplatelet therapy alone (HR, 0.32; P = .002) and antiplatelet therapy with oral anticoagulation (HR, 0.44; P = .018).
The PARTNER II study was funded by Edwards Lifesciences. Senior author Martin B. Leon, MD, and several other study coauthors reported disclosures related to Edwards Lifesciences, in addition to Abbott Vascular, Cordis, Medtronic, Boston Scientific, and other companies. Dr. Kosmidou reported no disclosures.
SOURCE: Kosmidou I et al. JACC Cardiovasc Interv. 2019;12:1580-9.
FROM JACC: CARDIOVASCULAR INTERVENTIONS
ASCO VTE guideline update: DOACs now an option for prevention, treatment
The direct oral anticoagulants (DOACs) apixaban and rivaroxaban are now among the options for thromboprophylaxis in high-risk cancer outpatients with low risk for bleeding and drug interactions, according to a practice guideline update from the American Society of Clinical Oncology.
Rivaroxaban also has been added as an option for initial anticoagulation for venous thromboembolism (VTE), and both rivaroxaban and edoxaban are now options for long-term anticoagulation, Nigel S. Key, MB ChB, and colleagues wrote in the updated guideline on the prophylaxis and treatment of VTE – including deep vein thrombosis (DVT) and pulmonary embolism (PE) – in cancer patients (J Clin Oncol. 2019 Aug 5. doi: 10.1200/JCO.19.19.01461).
The addition of DOACs as options for VTE prophylaxis and treatment represents the most notable change to the guideline.
“Oral anticoagulants that target thrombin (direct thrombin inhibitor, dabigatran) or activated factor X (antifactor Xa inhibitors, rivaroxaban, apixaban, and edoxaban) are now approved for treatment of DVT or PE as well as for DVT prophylaxis following orthopedic surgery and for reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation,” the guideline panel wrote.
A systematic review of PubMed and the Cochrane Library for randomized controlled trials (RCTs) and meta-analyses of RCTs published from Aug. 1, 2014, through Dec. 4, 2018, identified 35 publications on VTE prophylaxis and treatment, including 2 RCTs of DOACs for prophylaxis and 2 others of DOAC treatment, as well as 8 publications on VTE risk assessment. A multidisciplinary expert panel appointed by ASCO and cochaired by Dr. Key of the University of North Carolina, Chapel Hill, used this evidence to develop the updated guideline.
The work was guided by “the ‘signals’ approach that is designed to identify only new, potentially practice-changing data – signals – that might translate into revised practice recommendations,” the authors explained.
DOAC-related updates
VTE prophylaxis. Based in part on findings from the recently published AVERT trial of apixaban in patients initiating a new course of chemotherapy and from the CASSINI trial of rivaroxaban in patients with solid tumors or lymphoma starting systemic antineoplastic therapy, the panel added both agents as thromboprophylactic options that can be offered to high-risk cancer outpatients with no significant risk factors for bleeding or drug interactions (N Engl J Med. 2019;380:711-19; N Engl J Med. 2019;380:720-8).
Low-molecular-weight heparin (LMWH) also remains an option in such patients; consideration of therapy should involve discussion with the patient about relative benefits and harms, drug costs, and “the uncertainty surrounding duration of prophylaxis in this setting,” they wrote.
Anticoagulation for VTE. Options for initial anticoagulation include LMWH, unfractionated heparin (UFH), fondaparinux, and now rivaroxaban, with the latter added based on findings from two RCTs – the SELECT-D trial and the Hokusai VTE-Cancer study – and multiple meta-analyses (J Clin Oncol. 2018;36:2017-23; N Engl J Med. 2018;378:615-24).
Long-term anticoagulation can involve treatment with LMWH, edoxaban, or rivaroxaban for at least 6 months, all of which have improved efficacy versus vitamin K agonists (VKAs), the panel noted. However, VKAs may be used if LMWH and DOACs are not accessible.
Importantly, the literature indicates an increased risk of major bleeding with DOACs, particularly in patients with gastrointestinal malignancies and potentially in those with genitourinary malignancies. “Caution with DOACs is also warranted in other settings with high risk for mucosal bleeding,” the panel wrote.
Additional updates
CNS metastases. The anticoagulation recommendations were also updated to include patients with metastatic central nervous system malignancies (those with primary CNS malignancies were included previously). Both those with primary and metastatic CNS malignancy should be offered anticoagulation for established VTE as described for patients with other types of cancer. However, the panel stressed that “uncertainties remain about choice of agents and selection of patients most likely to benefit.”
“Patients with intracranial tumors are at increased risk for thrombotic complications and intracranial hemorrhage (ICH), but the presence of a stable or active primary intracranial malignancy or brain metastases is not an absolute contraindication to anticoagulation,” they wrote.
Limited evidence suggests that therapeutic anticoagulation does not increase ICH risk in patients with brain metastases, but it may increase risk in those with primary brain tumors, the panel added.
Additionally, preliminary data from a retrospective cohort of patients with metastatic brain disease and venous thrombosis suggest that DOACs may be associated with a lower risk of ICH than is LMWH in this population.
Long-term postoperative LMWH. Extended prophylaxis with LMWH for up to 4 weeks is recommended after major open or laparoscopic abdominal or pelvic surgery in cancer patients with high-risk features, such as restricted mobility, obesity, history of VTE, or with additional risk factors. Lower-risk surgical settings require case-by-case decision making about appropriate thromboprophylaxis duration, according to the update.
A 2014 RCT looking at thromboprophylaxis duration in 225 patients undergoing laparoscopic surgery for colorectal cancer prompted the addition of laparoscopic surgery to this recommendation. In that study, VTE occurred by 4 weeks in nearly 10% of patients receiving 1 week of prophylaxis and in no patients in the 4-week arm. Major bleeding occurred in one versus zero patients in the thromboprophylaxis arms, respectively (Ann Surg. April 2014;259[4]:665-9).
Reaffirmed recommendations
Based on the latest available data, the panel reaffirmed that most hospitalized patients with cancer and an acute medical condition require thromboprophylaxis for the duration of their hospitalization and that thromboprophylaxis should not be routinely recommended for all outpatients with cancer.
The panel also reaffirmed the need for thromboprophylaxis starting preoperatively and continuing for at least 7-10 days in patients undergoing major cancer surgery, the need for periodic assessment of VTE risk in cancer patients, and the importance of patient education about the signs and symptoms of VTE.
Perspective and future directions
In an interview, David H. Henry, MD, said he was pleased to see ASCO incorporate the latest DOAC data into the VTE guideline.
The AVERT and CASSINI studies, in particular, highlight the value of using the Khorana Risk Score, which considers cancer type, blood counts, and body mass index to predict the risk of thrombosis in cancer patients and to guide decisions regarding prophylaxis, said Dr. Henry, vice chair of the department of medicine and clinical professor of medicine at Penn Medicine’s Abramson Cancer Center, Philadelphia.
The DOACs also represent “a nice new development in the treatment setting,” he said, adding that it’s been long known – since the 2003 CLOT trial – that cancer patients with VTE had much lower recurrence rates with LMWH versus warfarin (Coumadin).
“Now fast forward to the modern era ... and DOACs now appear to be a good idea,” he said.
Dr. Henry also addressed the recommendation for expanded postoperative LMWH use.
“That I found interesting; I’m not sure what took them so long,” he said, explaining that National Comprehensive Cancer Network and European Society of Medical Oncology recommendations have long stated that, for patients with abdominal cancers who undergo abdominopelvic surgery, DVT prophylaxis should continue for 4 weeks.
Dr. Henry said that a survey at his center showed that those recommendations were “very poorly followed,” with surgeons giving 4 weeks of prophylaxis in just 5% of cases.
“The good news from our survey was that not many people had a VTE, despite not many people following the recommendations, but I must say I think our surgeons are catching on,” he said.
Overall, the updated guideline highlights the importance of considering the “cancer variable” when it comes to VTE prevention and treatment.
“We’ve known forever that when we diagnose a DVT or PE in the outpatient setting – and this is independent of cancer – that you should treat it. Add the cancer variable and we now know that we should worry and try to prevent the VTE in certain high-risk patients, and there are some drugs to do it with,” he said, adding that “you should worry about the person you’ve just provoked [with surgery] as well.”
An important question not addressed in the guideline update is the indefinite use of DOACs in cancer patients with ongoing risk, he said.
“When we see DVT or PE, we usually treat for 3 months – that’s the industry standard – and at the end of 3 months ... you do a time out and you say to yourself, ‘Was this person provoked?’ ” he said.
For example, if they took a long flight or if pregnancy was a factor, treatment can usually be safely stopped. However, in a cancer patient who still has cancer, the provocation continues, and the patient may require indefinite treatment.
Questions that remain involve defining “indefinite” and include whether (and which of) these drugs can be used indefinitely in such patients, Dr. Henry said.
Dr. Key reported receiving honoraria from Novo Nordisk, research funding to his institution from Baxter Biosciences, Grifols, and Pfizer, and serving as a consultant or advisor for Genentech, Roche, Uniqure, Seattle Genetics, and Shire Human Genetic Therapies. Numerous disclosures were also reported by other expert panel members.
The direct oral anticoagulants (DOACs) apixaban and rivaroxaban are now among the options for thromboprophylaxis in high-risk cancer outpatients with low risk for bleeding and drug interactions, according to a practice guideline update from the American Society of Clinical Oncology.
Rivaroxaban also has been added as an option for initial anticoagulation for venous thromboembolism (VTE), and both rivaroxaban and edoxaban are now options for long-term anticoagulation, Nigel S. Key, MB ChB, and colleagues wrote in the updated guideline on the prophylaxis and treatment of VTE – including deep vein thrombosis (DVT) and pulmonary embolism (PE) – in cancer patients (J Clin Oncol. 2019 Aug 5. doi: 10.1200/JCO.19.19.01461).
The addition of DOACs as options for VTE prophylaxis and treatment represents the most notable change to the guideline.
“Oral anticoagulants that target thrombin (direct thrombin inhibitor, dabigatran) or activated factor X (antifactor Xa inhibitors, rivaroxaban, apixaban, and edoxaban) are now approved for treatment of DVT or PE as well as for DVT prophylaxis following orthopedic surgery and for reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation,” the guideline panel wrote.
A systematic review of PubMed and the Cochrane Library for randomized controlled trials (RCTs) and meta-analyses of RCTs published from Aug. 1, 2014, through Dec. 4, 2018, identified 35 publications on VTE prophylaxis and treatment, including 2 RCTs of DOACs for prophylaxis and 2 others of DOAC treatment, as well as 8 publications on VTE risk assessment. A multidisciplinary expert panel appointed by ASCO and cochaired by Dr. Key of the University of North Carolina, Chapel Hill, used this evidence to develop the updated guideline.
The work was guided by “the ‘signals’ approach that is designed to identify only new, potentially practice-changing data – signals – that might translate into revised practice recommendations,” the authors explained.
DOAC-related updates
VTE prophylaxis. Based in part on findings from the recently published AVERT trial of apixaban in patients initiating a new course of chemotherapy and from the CASSINI trial of rivaroxaban in patients with solid tumors or lymphoma starting systemic antineoplastic therapy, the panel added both agents as thromboprophylactic options that can be offered to high-risk cancer outpatients with no significant risk factors for bleeding or drug interactions (N Engl J Med. 2019;380:711-19; N Engl J Med. 2019;380:720-8).
Low-molecular-weight heparin (LMWH) also remains an option in such patients; consideration of therapy should involve discussion with the patient about relative benefits and harms, drug costs, and “the uncertainty surrounding duration of prophylaxis in this setting,” they wrote.
Anticoagulation for VTE. Options for initial anticoagulation include LMWH, unfractionated heparin (UFH), fondaparinux, and now rivaroxaban, with the latter added based on findings from two RCTs – the SELECT-D trial and the Hokusai VTE-Cancer study – and multiple meta-analyses (J Clin Oncol. 2018;36:2017-23; N Engl J Med. 2018;378:615-24).
Long-term anticoagulation can involve treatment with LMWH, edoxaban, or rivaroxaban for at least 6 months, all of which have improved efficacy versus vitamin K agonists (VKAs), the panel noted. However, VKAs may be used if LMWH and DOACs are not accessible.
Importantly, the literature indicates an increased risk of major bleeding with DOACs, particularly in patients with gastrointestinal malignancies and potentially in those with genitourinary malignancies. “Caution with DOACs is also warranted in other settings with high risk for mucosal bleeding,” the panel wrote.
Additional updates
CNS metastases. The anticoagulation recommendations were also updated to include patients with metastatic central nervous system malignancies (those with primary CNS malignancies were included previously). Both those with primary and metastatic CNS malignancy should be offered anticoagulation for established VTE as described for patients with other types of cancer. However, the panel stressed that “uncertainties remain about choice of agents and selection of patients most likely to benefit.”
“Patients with intracranial tumors are at increased risk for thrombotic complications and intracranial hemorrhage (ICH), but the presence of a stable or active primary intracranial malignancy or brain metastases is not an absolute contraindication to anticoagulation,” they wrote.
Limited evidence suggests that therapeutic anticoagulation does not increase ICH risk in patients with brain metastases, but it may increase risk in those with primary brain tumors, the panel added.
Additionally, preliminary data from a retrospective cohort of patients with metastatic brain disease and venous thrombosis suggest that DOACs may be associated with a lower risk of ICH than is LMWH in this population.
Long-term postoperative LMWH. Extended prophylaxis with LMWH for up to 4 weeks is recommended after major open or laparoscopic abdominal or pelvic surgery in cancer patients with high-risk features, such as restricted mobility, obesity, history of VTE, or with additional risk factors. Lower-risk surgical settings require case-by-case decision making about appropriate thromboprophylaxis duration, according to the update.
A 2014 RCT looking at thromboprophylaxis duration in 225 patients undergoing laparoscopic surgery for colorectal cancer prompted the addition of laparoscopic surgery to this recommendation. In that study, VTE occurred by 4 weeks in nearly 10% of patients receiving 1 week of prophylaxis and in no patients in the 4-week arm. Major bleeding occurred in one versus zero patients in the thromboprophylaxis arms, respectively (Ann Surg. April 2014;259[4]:665-9).
Reaffirmed recommendations
Based on the latest available data, the panel reaffirmed that most hospitalized patients with cancer and an acute medical condition require thromboprophylaxis for the duration of their hospitalization and that thromboprophylaxis should not be routinely recommended for all outpatients with cancer.
The panel also reaffirmed the need for thromboprophylaxis starting preoperatively and continuing for at least 7-10 days in patients undergoing major cancer surgery, the need for periodic assessment of VTE risk in cancer patients, and the importance of patient education about the signs and symptoms of VTE.
Perspective and future directions
In an interview, David H. Henry, MD, said he was pleased to see ASCO incorporate the latest DOAC data into the VTE guideline.
The AVERT and CASSINI studies, in particular, highlight the value of using the Khorana Risk Score, which considers cancer type, blood counts, and body mass index to predict the risk of thrombosis in cancer patients and to guide decisions regarding prophylaxis, said Dr. Henry, vice chair of the department of medicine and clinical professor of medicine at Penn Medicine’s Abramson Cancer Center, Philadelphia.
The DOACs also represent “a nice new development in the treatment setting,” he said, adding that it’s been long known – since the 2003 CLOT trial – that cancer patients with VTE had much lower recurrence rates with LMWH versus warfarin (Coumadin).
“Now fast forward to the modern era ... and DOACs now appear to be a good idea,” he said.
Dr. Henry also addressed the recommendation for expanded postoperative LMWH use.
“That I found interesting; I’m not sure what took them so long,” he said, explaining that National Comprehensive Cancer Network and European Society of Medical Oncology recommendations have long stated that, for patients with abdominal cancers who undergo abdominopelvic surgery, DVT prophylaxis should continue for 4 weeks.
Dr. Henry said that a survey at his center showed that those recommendations were “very poorly followed,” with surgeons giving 4 weeks of prophylaxis in just 5% of cases.
“The good news from our survey was that not many people had a VTE, despite not many people following the recommendations, but I must say I think our surgeons are catching on,” he said.
Overall, the updated guideline highlights the importance of considering the “cancer variable” when it comes to VTE prevention and treatment.
“We’ve known forever that when we diagnose a DVT or PE in the outpatient setting – and this is independent of cancer – that you should treat it. Add the cancer variable and we now know that we should worry and try to prevent the VTE in certain high-risk patients, and there are some drugs to do it with,” he said, adding that “you should worry about the person you’ve just provoked [with surgery] as well.”
An important question not addressed in the guideline update is the indefinite use of DOACs in cancer patients with ongoing risk, he said.
“When we see DVT or PE, we usually treat for 3 months – that’s the industry standard – and at the end of 3 months ... you do a time out and you say to yourself, ‘Was this person provoked?’ ” he said.
For example, if they took a long flight or if pregnancy was a factor, treatment can usually be safely stopped. However, in a cancer patient who still has cancer, the provocation continues, and the patient may require indefinite treatment.
Questions that remain involve defining “indefinite” and include whether (and which of) these drugs can be used indefinitely in such patients, Dr. Henry said.
Dr. Key reported receiving honoraria from Novo Nordisk, research funding to his institution from Baxter Biosciences, Grifols, and Pfizer, and serving as a consultant or advisor for Genentech, Roche, Uniqure, Seattle Genetics, and Shire Human Genetic Therapies. Numerous disclosures were also reported by other expert panel members.
The direct oral anticoagulants (DOACs) apixaban and rivaroxaban are now among the options for thromboprophylaxis in high-risk cancer outpatients with low risk for bleeding and drug interactions, according to a practice guideline update from the American Society of Clinical Oncology.
Rivaroxaban also has been added as an option for initial anticoagulation for venous thromboembolism (VTE), and both rivaroxaban and edoxaban are now options for long-term anticoagulation, Nigel S. Key, MB ChB, and colleagues wrote in the updated guideline on the prophylaxis and treatment of VTE – including deep vein thrombosis (DVT) and pulmonary embolism (PE) – in cancer patients (J Clin Oncol. 2019 Aug 5. doi: 10.1200/JCO.19.19.01461).
The addition of DOACs as options for VTE prophylaxis and treatment represents the most notable change to the guideline.
“Oral anticoagulants that target thrombin (direct thrombin inhibitor, dabigatran) or activated factor X (antifactor Xa inhibitors, rivaroxaban, apixaban, and edoxaban) are now approved for treatment of DVT or PE as well as for DVT prophylaxis following orthopedic surgery and for reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation,” the guideline panel wrote.
A systematic review of PubMed and the Cochrane Library for randomized controlled trials (RCTs) and meta-analyses of RCTs published from Aug. 1, 2014, through Dec. 4, 2018, identified 35 publications on VTE prophylaxis and treatment, including 2 RCTs of DOACs for prophylaxis and 2 others of DOAC treatment, as well as 8 publications on VTE risk assessment. A multidisciplinary expert panel appointed by ASCO and cochaired by Dr. Key of the University of North Carolina, Chapel Hill, used this evidence to develop the updated guideline.
The work was guided by “the ‘signals’ approach that is designed to identify only new, potentially practice-changing data – signals – that might translate into revised practice recommendations,” the authors explained.
DOAC-related updates
VTE prophylaxis. Based in part on findings from the recently published AVERT trial of apixaban in patients initiating a new course of chemotherapy and from the CASSINI trial of rivaroxaban in patients with solid tumors or lymphoma starting systemic antineoplastic therapy, the panel added both agents as thromboprophylactic options that can be offered to high-risk cancer outpatients with no significant risk factors for bleeding or drug interactions (N Engl J Med. 2019;380:711-19; N Engl J Med. 2019;380:720-8).
Low-molecular-weight heparin (LMWH) also remains an option in such patients; consideration of therapy should involve discussion with the patient about relative benefits and harms, drug costs, and “the uncertainty surrounding duration of prophylaxis in this setting,” they wrote.
Anticoagulation for VTE. Options for initial anticoagulation include LMWH, unfractionated heparin (UFH), fondaparinux, and now rivaroxaban, with the latter added based on findings from two RCTs – the SELECT-D trial and the Hokusai VTE-Cancer study – and multiple meta-analyses (J Clin Oncol. 2018;36:2017-23; N Engl J Med. 2018;378:615-24).
Long-term anticoagulation can involve treatment with LMWH, edoxaban, or rivaroxaban for at least 6 months, all of which have improved efficacy versus vitamin K agonists (VKAs), the panel noted. However, VKAs may be used if LMWH and DOACs are not accessible.
Importantly, the literature indicates an increased risk of major bleeding with DOACs, particularly in patients with gastrointestinal malignancies and potentially in those with genitourinary malignancies. “Caution with DOACs is also warranted in other settings with high risk for mucosal bleeding,” the panel wrote.
Additional updates
CNS metastases. The anticoagulation recommendations were also updated to include patients with metastatic central nervous system malignancies (those with primary CNS malignancies were included previously). Both those with primary and metastatic CNS malignancy should be offered anticoagulation for established VTE as described for patients with other types of cancer. However, the panel stressed that “uncertainties remain about choice of agents and selection of patients most likely to benefit.”
“Patients with intracranial tumors are at increased risk for thrombotic complications and intracranial hemorrhage (ICH), but the presence of a stable or active primary intracranial malignancy or brain metastases is not an absolute contraindication to anticoagulation,” they wrote.
Limited evidence suggests that therapeutic anticoagulation does not increase ICH risk in patients with brain metastases, but it may increase risk in those with primary brain tumors, the panel added.
Additionally, preliminary data from a retrospective cohort of patients with metastatic brain disease and venous thrombosis suggest that DOACs may be associated with a lower risk of ICH than is LMWH in this population.
Long-term postoperative LMWH. Extended prophylaxis with LMWH for up to 4 weeks is recommended after major open or laparoscopic abdominal or pelvic surgery in cancer patients with high-risk features, such as restricted mobility, obesity, history of VTE, or with additional risk factors. Lower-risk surgical settings require case-by-case decision making about appropriate thromboprophylaxis duration, according to the update.
A 2014 RCT looking at thromboprophylaxis duration in 225 patients undergoing laparoscopic surgery for colorectal cancer prompted the addition of laparoscopic surgery to this recommendation. In that study, VTE occurred by 4 weeks in nearly 10% of patients receiving 1 week of prophylaxis and in no patients in the 4-week arm. Major bleeding occurred in one versus zero patients in the thromboprophylaxis arms, respectively (Ann Surg. April 2014;259[4]:665-9).
Reaffirmed recommendations
Based on the latest available data, the panel reaffirmed that most hospitalized patients with cancer and an acute medical condition require thromboprophylaxis for the duration of their hospitalization and that thromboprophylaxis should not be routinely recommended for all outpatients with cancer.
The panel also reaffirmed the need for thromboprophylaxis starting preoperatively and continuing for at least 7-10 days in patients undergoing major cancer surgery, the need for periodic assessment of VTE risk in cancer patients, and the importance of patient education about the signs and symptoms of VTE.
Perspective and future directions
In an interview, David H. Henry, MD, said he was pleased to see ASCO incorporate the latest DOAC data into the VTE guideline.
The AVERT and CASSINI studies, in particular, highlight the value of using the Khorana Risk Score, which considers cancer type, blood counts, and body mass index to predict the risk of thrombosis in cancer patients and to guide decisions regarding prophylaxis, said Dr. Henry, vice chair of the department of medicine and clinical professor of medicine at Penn Medicine’s Abramson Cancer Center, Philadelphia.
The DOACs also represent “a nice new development in the treatment setting,” he said, adding that it’s been long known – since the 2003 CLOT trial – that cancer patients with VTE had much lower recurrence rates with LMWH versus warfarin (Coumadin).
“Now fast forward to the modern era ... and DOACs now appear to be a good idea,” he said.
Dr. Henry also addressed the recommendation for expanded postoperative LMWH use.
“That I found interesting; I’m not sure what took them so long,” he said, explaining that National Comprehensive Cancer Network and European Society of Medical Oncology recommendations have long stated that, for patients with abdominal cancers who undergo abdominopelvic surgery, DVT prophylaxis should continue for 4 weeks.
Dr. Henry said that a survey at his center showed that those recommendations were “very poorly followed,” with surgeons giving 4 weeks of prophylaxis in just 5% of cases.
“The good news from our survey was that not many people had a VTE, despite not many people following the recommendations, but I must say I think our surgeons are catching on,” he said.
Overall, the updated guideline highlights the importance of considering the “cancer variable” when it comes to VTE prevention and treatment.
“We’ve known forever that when we diagnose a DVT or PE in the outpatient setting – and this is independent of cancer – that you should treat it. Add the cancer variable and we now know that we should worry and try to prevent the VTE in certain high-risk patients, and there are some drugs to do it with,” he said, adding that “you should worry about the person you’ve just provoked [with surgery] as well.”
An important question not addressed in the guideline update is the indefinite use of DOACs in cancer patients with ongoing risk, he said.
“When we see DVT or PE, we usually treat for 3 months – that’s the industry standard – and at the end of 3 months ... you do a time out and you say to yourself, ‘Was this person provoked?’ ” he said.
For example, if they took a long flight or if pregnancy was a factor, treatment can usually be safely stopped. However, in a cancer patient who still has cancer, the provocation continues, and the patient may require indefinite treatment.
Questions that remain involve defining “indefinite” and include whether (and which of) these drugs can be used indefinitely in such patients, Dr. Henry said.
Dr. Key reported receiving honoraria from Novo Nordisk, research funding to his institution from Baxter Biosciences, Grifols, and Pfizer, and serving as a consultant or advisor for Genentech, Roche, Uniqure, Seattle Genetics, and Shire Human Genetic Therapies. Numerous disclosures were also reported by other expert panel members.
Researchers combine genetic and clinical factors in new VTE risk score
MELBOURNE – A venous thromboembolism risk score that combines clinical risk factors, such as lymphoma type and stage, along with genetic variables, could offer a better way to predict venous thromboembolism in patients with lymphoma, according to new findings presented at the International Society on Thrombosis and Haemostasis congress.
Cristina Pascual, MD, of the Hospital Universitario Gregorio Marañon in Madrid presented data from a development and validation study of a clinical-genetic risk model for thrombosis in lymphoma in 208 patients with lymphoma, 31 of whom experienced a venous thromboembolic event.
While the relationship between cancer and increased thrombosis risk is well recognized, lymphoma patients are at particularly high risk, with an estimated thrombosis incidence of 5%-10%, Dr. Pascual said.
Currently, the Khorana score is the most validated risk score for thrombosis in patients with solid tumors, using factors such as tumor site, platelet and leukocyte count, hemoglobin levels, and body mass index. However, Dr. Pascual pointed out that just 10% of the validation cohort for the Khorana score were lymphoma patients, and it had previously been found to be not as useful for that population.
More recently, researchers had developed the ThroLy score for predicting thromboembolic events specifically in patients with lymphoma, incorporating clinical variables such as mediastinal involvement and extranodal localization.
Another group took a different approach by incorporating genetic risk factors for thrombosis to create Thrombo inCode-Oncology (TiC-Onco) for solid tumors. This assessment included four genetic variants known to increase the risk of thromboembolic events in cancer patients, as well as the clinical risk factors of body mass index, family history of thrombosis, primary tumor site, and tumor stage.
Dr. Pascual and colleagues developed a unique risk factor model that combined both the ThroLy and TiC-Onco elements.
In 208 patients with lymphoma who were not receiving anticoagulant treatment, researchers identified five clinical factors that were most predictive of venous thrombosis: a history of thrombosis, immobilization for more than 3 days, lymphoma type, Ann Arbor score for lymphoma stage, and mediastinal extension.
They combined these clinical risk factors with the genetic risk factors from the TiC-Onco score to develop the TiC-Onco–associated lymphoma score (TiC-Lympho).
When validated in the same group of patients, the TiC-Lympho score had a sensitivity of 93.55%, a specificity of 54.49%, positive predictive value of 26.36%, and negative predictive value of 97.94%.
The researchers also compared TiC-Lympho’s performance with that of the ThroLy and TiC-Onco models, and found it performed better on sensitivity and negative predictive value. The area under the curve for TiC-Lympho (0.783) was significantly higher than that seen with the other two risk models.
Session chair Kate Burbury, MBBS, of the Peter MacCallum Cancer Centre in Melbourne, raised the question of how the score – and particularly the genetic risk factor assessment – might be applied in the real-world clinical setting.
In an interview, Dr. Pascual said the findings represented preliminary data only, so the model was not ready to be applied to clinical practice yet. She also stressed that this was based on retrospective data, and needed to be further validated in other cohorts of lymphoma patients.
No conflicts of interest were reported.
SOURCE: Pascual C et al. 2019 ISTH Congress, Abstract OC 41.3.
MELBOURNE – A venous thromboembolism risk score that combines clinical risk factors, such as lymphoma type and stage, along with genetic variables, could offer a better way to predict venous thromboembolism in patients with lymphoma, according to new findings presented at the International Society on Thrombosis and Haemostasis congress.
Cristina Pascual, MD, of the Hospital Universitario Gregorio Marañon in Madrid presented data from a development and validation study of a clinical-genetic risk model for thrombosis in lymphoma in 208 patients with lymphoma, 31 of whom experienced a venous thromboembolic event.
While the relationship between cancer and increased thrombosis risk is well recognized, lymphoma patients are at particularly high risk, with an estimated thrombosis incidence of 5%-10%, Dr. Pascual said.
Currently, the Khorana score is the most validated risk score for thrombosis in patients with solid tumors, using factors such as tumor site, platelet and leukocyte count, hemoglobin levels, and body mass index. However, Dr. Pascual pointed out that just 10% of the validation cohort for the Khorana score were lymphoma patients, and it had previously been found to be not as useful for that population.
More recently, researchers had developed the ThroLy score for predicting thromboembolic events specifically in patients with lymphoma, incorporating clinical variables such as mediastinal involvement and extranodal localization.
Another group took a different approach by incorporating genetic risk factors for thrombosis to create Thrombo inCode-Oncology (TiC-Onco) for solid tumors. This assessment included four genetic variants known to increase the risk of thromboembolic events in cancer patients, as well as the clinical risk factors of body mass index, family history of thrombosis, primary tumor site, and tumor stage.
Dr. Pascual and colleagues developed a unique risk factor model that combined both the ThroLy and TiC-Onco elements.
In 208 patients with lymphoma who were not receiving anticoagulant treatment, researchers identified five clinical factors that were most predictive of venous thrombosis: a history of thrombosis, immobilization for more than 3 days, lymphoma type, Ann Arbor score for lymphoma stage, and mediastinal extension.
They combined these clinical risk factors with the genetic risk factors from the TiC-Onco score to develop the TiC-Onco–associated lymphoma score (TiC-Lympho).
When validated in the same group of patients, the TiC-Lympho score had a sensitivity of 93.55%, a specificity of 54.49%, positive predictive value of 26.36%, and negative predictive value of 97.94%.
The researchers also compared TiC-Lympho’s performance with that of the ThroLy and TiC-Onco models, and found it performed better on sensitivity and negative predictive value. The area under the curve for TiC-Lympho (0.783) was significantly higher than that seen with the other two risk models.
Session chair Kate Burbury, MBBS, of the Peter MacCallum Cancer Centre in Melbourne, raised the question of how the score – and particularly the genetic risk factor assessment – might be applied in the real-world clinical setting.
In an interview, Dr. Pascual said the findings represented preliminary data only, so the model was not ready to be applied to clinical practice yet. She also stressed that this was based on retrospective data, and needed to be further validated in other cohorts of lymphoma patients.
No conflicts of interest were reported.
SOURCE: Pascual C et al. 2019 ISTH Congress, Abstract OC 41.3.
MELBOURNE – A venous thromboembolism risk score that combines clinical risk factors, such as lymphoma type and stage, along with genetic variables, could offer a better way to predict venous thromboembolism in patients with lymphoma, according to new findings presented at the International Society on Thrombosis and Haemostasis congress.
Cristina Pascual, MD, of the Hospital Universitario Gregorio Marañon in Madrid presented data from a development and validation study of a clinical-genetic risk model for thrombosis in lymphoma in 208 patients with lymphoma, 31 of whom experienced a venous thromboembolic event.
While the relationship between cancer and increased thrombosis risk is well recognized, lymphoma patients are at particularly high risk, with an estimated thrombosis incidence of 5%-10%, Dr. Pascual said.
Currently, the Khorana score is the most validated risk score for thrombosis in patients with solid tumors, using factors such as tumor site, platelet and leukocyte count, hemoglobin levels, and body mass index. However, Dr. Pascual pointed out that just 10% of the validation cohort for the Khorana score were lymphoma patients, and it had previously been found to be not as useful for that population.
More recently, researchers had developed the ThroLy score for predicting thromboembolic events specifically in patients with lymphoma, incorporating clinical variables such as mediastinal involvement and extranodal localization.
Another group took a different approach by incorporating genetic risk factors for thrombosis to create Thrombo inCode-Oncology (TiC-Onco) for solid tumors. This assessment included four genetic variants known to increase the risk of thromboembolic events in cancer patients, as well as the clinical risk factors of body mass index, family history of thrombosis, primary tumor site, and tumor stage.
Dr. Pascual and colleagues developed a unique risk factor model that combined both the ThroLy and TiC-Onco elements.
In 208 patients with lymphoma who were not receiving anticoagulant treatment, researchers identified five clinical factors that were most predictive of venous thrombosis: a history of thrombosis, immobilization for more than 3 days, lymphoma type, Ann Arbor score for lymphoma stage, and mediastinal extension.
They combined these clinical risk factors with the genetic risk factors from the TiC-Onco score to develop the TiC-Onco–associated lymphoma score (TiC-Lympho).
When validated in the same group of patients, the TiC-Lympho score had a sensitivity of 93.55%, a specificity of 54.49%, positive predictive value of 26.36%, and negative predictive value of 97.94%.
The researchers also compared TiC-Lympho’s performance with that of the ThroLy and TiC-Onco models, and found it performed better on sensitivity and negative predictive value. The area under the curve for TiC-Lympho (0.783) was significantly higher than that seen with the other two risk models.
Session chair Kate Burbury, MBBS, of the Peter MacCallum Cancer Centre in Melbourne, raised the question of how the score – and particularly the genetic risk factor assessment – might be applied in the real-world clinical setting.
In an interview, Dr. Pascual said the findings represented preliminary data only, so the model was not ready to be applied to clinical practice yet. She also stressed that this was based on retrospective data, and needed to be further validated in other cohorts of lymphoma patients.
No conflicts of interest were reported.
SOURCE: Pascual C et al. 2019 ISTH Congress, Abstract OC 41.3.
REPORTING FROM 2019 ISTH CONGRESS
Does endovascular thrombectomy benefit stroke patients with large infarcts?
Endovascular thrombectomy may benefit patients with stroke with large infarcts, an analysis suggests. The intervention may be more likely to benefit patients who “are treated early and have a core volume less than 100 cm3,” researchers reported in JAMA Neurology.
Clinical trials evaluating thrombectomy have largely excluded patients with large ischemic cores. To examine whether thrombectomy produces reasonable functional and safety outcomes in patients with stroke with large infarcts, compared with medical management alone, the investigators conducted a prespecified secondary analysis of data from the Optimizing Patient Selection for Endovascular Treatment in Acute Ischemic Stroke (SELECT) study.
A nonrandomized study
Amrou Sarraj, MD, of the University of Texas, Houston, and his coauthors analyzed data from 105 patients in the prospective, multicenter cohort study, which enrolled patients between January 2016 and February 2018. Their analysis included data from patients who had large ischemic cores on CT (Alberta Stroke Program Early CT Score, 0-5) or on CT perfusion images (an ischemic core volume of at least 50 cm3). The SELECT study included patients with moderate to severe stroke and anterior circulation large-vessel occlusion who presented up to 24 hours from the time they last were known to be well. In the SELECT study, local investigators decided whether patients received endovascular thrombectomy or medical management alone in a nonrandomized fashion.
The 105 patients had a median age of 66 years, and 43% were female. Of the patients with large infarcts, 62 (59%) received endovascular thrombectomy plus medical management, and the rest received medical management alone.
At 90 days, 31% of the patients who received endovascular thrombectomy achieved functional independence (modified Rankin Scale score of 0-2), compared with 14% of patients who received medical management alone (odds ratio, 3.27). In addition, endovascular thrombectomy was associated with better functional outcome, less infarct growth (44 vs. 98 mL), and smaller final infarct volume (97 vs. 190 mL).
The rates of neurologic worsening and symptomatic intracerebral hemorrhage were similar in both treatment groups, while mortality was lower among patients who received thrombectomy (29% vs. 42%). The likelihood of functional independence with endovascular thrombectomy decreased by 40% with each 1-hour delay in treatment and by 42% with each 10-cm3 increase in stroke volume.
Of 10 patients with core volumes greater than 100 cm3 who received endovascular thrombectomy, none had a favorable outcome.
“Although the odds of good outcomes for patients with large cores who received [endovascular thrombectomy] markedly decline with increasing core size and time to treatment, these data suggest potential benefits,” Dr. Sarraj and colleagues concluded. “Randomized clinical trials are needed.”
The authors noted that the results “did not reach significance after adjusting for baseline imbalances” and that “the small sample size limits the power of this analysis.”
The study was funded by an unrestricted grant from Stryker Neurovascular to the University of Texas. Dr. Sarraj is a consultant, speaker bureau member, and advisory board member for Stryker and is the principal investigator for a planned randomized, controlled trial (SELECT 2) funded by an unrestricted grant from Stryker to his institution. In addition, he is a site principal investigator for the TREVO Registry and DEFUSE 3 trials. Coauthors reported financial ties with Stryker and various device and pharmaceutical companies.
SOURCE: Sarraj A et al. JAMA Neurol. 2019 Jul 29. doi: 10.1001/jamaneurol.2019.2109.
Patients who had thrombectomies had improved outcomes in an unadjusted statistical analysis, but these differences did not remain significant after adjustment for baseline age, clinical severity, and other key prognostic variables. However, the analysis was underpowered.
A key finding was that favorable outcomes in patients with large core volumes was strongly time dependent, which was consistent with previous data from the Highly Effective Reperfusion Using Multiple Endovascular Devices (HERMES) collaboration.
Faster treatment is the key to maximizing benefit for patients with poor collateral blood flow and a large ischemic core at baseline. As treatment work flow improves and more patients are transported directly to a thrombectomy-capable center, the number who benefit from reperfusion, despite a large ischemic core, is likely to further increase.
Ongoing randomized clinical trials are assessing the practical question of who to treat with thrombectomy when the estimated ischemic core volume is large.
Bruce C. V. Campbell, MBBS, PhD , of the University of Melbourne made these comments in an accompanying editorial. He reported research support from the several Australian research foundations. He also reported unrestricted grant funding for the Extending the Time for Thrombolysis in Emergency Neurological Deficits–Intra-Arterial (EXTEND-IA) trial to the Florey Institute of Neuroscience and Mental Health in Parkville, Australia, from Covidien (Medtronic).
Patients who had thrombectomies had improved outcomes in an unadjusted statistical analysis, but these differences did not remain significant after adjustment for baseline age, clinical severity, and other key prognostic variables. However, the analysis was underpowered.
A key finding was that favorable outcomes in patients with large core volumes was strongly time dependent, which was consistent with previous data from the Highly Effective Reperfusion Using Multiple Endovascular Devices (HERMES) collaboration.
Faster treatment is the key to maximizing benefit for patients with poor collateral blood flow and a large ischemic core at baseline. As treatment work flow improves and more patients are transported directly to a thrombectomy-capable center, the number who benefit from reperfusion, despite a large ischemic core, is likely to further increase.
Ongoing randomized clinical trials are assessing the practical question of who to treat with thrombectomy when the estimated ischemic core volume is large.
Bruce C. V. Campbell, MBBS, PhD , of the University of Melbourne made these comments in an accompanying editorial. He reported research support from the several Australian research foundations. He also reported unrestricted grant funding for the Extending the Time for Thrombolysis in Emergency Neurological Deficits–Intra-Arterial (EXTEND-IA) trial to the Florey Institute of Neuroscience and Mental Health in Parkville, Australia, from Covidien (Medtronic).
Patients who had thrombectomies had improved outcomes in an unadjusted statistical analysis, but these differences did not remain significant after adjustment for baseline age, clinical severity, and other key prognostic variables. However, the analysis was underpowered.
A key finding was that favorable outcomes in patients with large core volumes was strongly time dependent, which was consistent with previous data from the Highly Effective Reperfusion Using Multiple Endovascular Devices (HERMES) collaboration.
Faster treatment is the key to maximizing benefit for patients with poor collateral blood flow and a large ischemic core at baseline. As treatment work flow improves and more patients are transported directly to a thrombectomy-capable center, the number who benefit from reperfusion, despite a large ischemic core, is likely to further increase.
Ongoing randomized clinical trials are assessing the practical question of who to treat with thrombectomy when the estimated ischemic core volume is large.
Bruce C. V. Campbell, MBBS, PhD , of the University of Melbourne made these comments in an accompanying editorial. He reported research support from the several Australian research foundations. He also reported unrestricted grant funding for the Extending the Time for Thrombolysis in Emergency Neurological Deficits–Intra-Arterial (EXTEND-IA) trial to the Florey Institute of Neuroscience and Mental Health in Parkville, Australia, from Covidien (Medtronic).
Endovascular thrombectomy may benefit patients with stroke with large infarcts, an analysis suggests. The intervention may be more likely to benefit patients who “are treated early and have a core volume less than 100 cm3,” researchers reported in JAMA Neurology.
Clinical trials evaluating thrombectomy have largely excluded patients with large ischemic cores. To examine whether thrombectomy produces reasonable functional and safety outcomes in patients with stroke with large infarcts, compared with medical management alone, the investigators conducted a prespecified secondary analysis of data from the Optimizing Patient Selection for Endovascular Treatment in Acute Ischemic Stroke (SELECT) study.
A nonrandomized study
Amrou Sarraj, MD, of the University of Texas, Houston, and his coauthors analyzed data from 105 patients in the prospective, multicenter cohort study, which enrolled patients between January 2016 and February 2018. Their analysis included data from patients who had large ischemic cores on CT (Alberta Stroke Program Early CT Score, 0-5) or on CT perfusion images (an ischemic core volume of at least 50 cm3). The SELECT study included patients with moderate to severe stroke and anterior circulation large-vessel occlusion who presented up to 24 hours from the time they last were known to be well. In the SELECT study, local investigators decided whether patients received endovascular thrombectomy or medical management alone in a nonrandomized fashion.
The 105 patients had a median age of 66 years, and 43% were female. Of the patients with large infarcts, 62 (59%) received endovascular thrombectomy plus medical management, and the rest received medical management alone.
At 90 days, 31% of the patients who received endovascular thrombectomy achieved functional independence (modified Rankin Scale score of 0-2), compared with 14% of patients who received medical management alone (odds ratio, 3.27). In addition, endovascular thrombectomy was associated with better functional outcome, less infarct growth (44 vs. 98 mL), and smaller final infarct volume (97 vs. 190 mL).
The rates of neurologic worsening and symptomatic intracerebral hemorrhage were similar in both treatment groups, while mortality was lower among patients who received thrombectomy (29% vs. 42%). The likelihood of functional independence with endovascular thrombectomy decreased by 40% with each 1-hour delay in treatment and by 42% with each 10-cm3 increase in stroke volume.
Of 10 patients with core volumes greater than 100 cm3 who received endovascular thrombectomy, none had a favorable outcome.
“Although the odds of good outcomes for patients with large cores who received [endovascular thrombectomy] markedly decline with increasing core size and time to treatment, these data suggest potential benefits,” Dr. Sarraj and colleagues concluded. “Randomized clinical trials are needed.”
The authors noted that the results “did not reach significance after adjusting for baseline imbalances” and that “the small sample size limits the power of this analysis.”
The study was funded by an unrestricted grant from Stryker Neurovascular to the University of Texas. Dr. Sarraj is a consultant, speaker bureau member, and advisory board member for Stryker and is the principal investigator for a planned randomized, controlled trial (SELECT 2) funded by an unrestricted grant from Stryker to his institution. In addition, he is a site principal investigator for the TREVO Registry and DEFUSE 3 trials. Coauthors reported financial ties with Stryker and various device and pharmaceutical companies.
SOURCE: Sarraj A et al. JAMA Neurol. 2019 Jul 29. doi: 10.1001/jamaneurol.2019.2109.
Endovascular thrombectomy may benefit patients with stroke with large infarcts, an analysis suggests. The intervention may be more likely to benefit patients who “are treated early and have a core volume less than 100 cm3,” researchers reported in JAMA Neurology.
Clinical trials evaluating thrombectomy have largely excluded patients with large ischemic cores. To examine whether thrombectomy produces reasonable functional and safety outcomes in patients with stroke with large infarcts, compared with medical management alone, the investigators conducted a prespecified secondary analysis of data from the Optimizing Patient Selection for Endovascular Treatment in Acute Ischemic Stroke (SELECT) study.
A nonrandomized study
Amrou Sarraj, MD, of the University of Texas, Houston, and his coauthors analyzed data from 105 patients in the prospective, multicenter cohort study, which enrolled patients between January 2016 and February 2018. Their analysis included data from patients who had large ischemic cores on CT (Alberta Stroke Program Early CT Score, 0-5) or on CT perfusion images (an ischemic core volume of at least 50 cm3). The SELECT study included patients with moderate to severe stroke and anterior circulation large-vessel occlusion who presented up to 24 hours from the time they last were known to be well. In the SELECT study, local investigators decided whether patients received endovascular thrombectomy or medical management alone in a nonrandomized fashion.
The 105 patients had a median age of 66 years, and 43% were female. Of the patients with large infarcts, 62 (59%) received endovascular thrombectomy plus medical management, and the rest received medical management alone.
At 90 days, 31% of the patients who received endovascular thrombectomy achieved functional independence (modified Rankin Scale score of 0-2), compared with 14% of patients who received medical management alone (odds ratio, 3.27). In addition, endovascular thrombectomy was associated with better functional outcome, less infarct growth (44 vs. 98 mL), and smaller final infarct volume (97 vs. 190 mL).
The rates of neurologic worsening and symptomatic intracerebral hemorrhage were similar in both treatment groups, while mortality was lower among patients who received thrombectomy (29% vs. 42%). The likelihood of functional independence with endovascular thrombectomy decreased by 40% with each 1-hour delay in treatment and by 42% with each 10-cm3 increase in stroke volume.
Of 10 patients with core volumes greater than 100 cm3 who received endovascular thrombectomy, none had a favorable outcome.
“Although the odds of good outcomes for patients with large cores who received [endovascular thrombectomy] markedly decline with increasing core size and time to treatment, these data suggest potential benefits,” Dr. Sarraj and colleagues concluded. “Randomized clinical trials are needed.”
The authors noted that the results “did not reach significance after adjusting for baseline imbalances” and that “the small sample size limits the power of this analysis.”
The study was funded by an unrestricted grant from Stryker Neurovascular to the University of Texas. Dr. Sarraj is a consultant, speaker bureau member, and advisory board member for Stryker and is the principal investigator for a planned randomized, controlled trial (SELECT 2) funded by an unrestricted grant from Stryker to his institution. In addition, he is a site principal investigator for the TREVO Registry and DEFUSE 3 trials. Coauthors reported financial ties with Stryker and various device and pharmaceutical companies.
SOURCE: Sarraj A et al. JAMA Neurol. 2019 Jul 29. doi: 10.1001/jamaneurol.2019.2109.
FROM JAMA NEUROLOGY
Key clinical point: and who have a core volume less than 100 mL.
Major finding: At 90 days, 31% of the patients who received endovascular thrombectomy achieved functional independence (modified Rankin Scale score of 0-2), compared with 14% of patients who received medical management alone (odds ratio, 3.27).
Study details: A prespecified secondary analysis of nonrandomized data from 105 patients in the Optimizing Patient Selection for Endovascular Treatment in Acute Ischemic Stroke (SELECT) study.
Disclosures: The study was funded by an unrestricted grant from Stryker Neurovascular. Dr. Sarraj is a consultant, speaker bureau member, and advisory board member for Stryker and is the principal investigator for a planned randomized, controlled trial (SELECT 2) funded by an unrestricted grant from Stryker to his institution. Coauthors reported financial ties with Stryker and various device and pharmaceutical companies.
Source: Sarraj A et al. JAMA Neurol. 2019 Jul 29. doi: 10.1001/jamaneurol.2019.2109.
Shorter vs. longer DAPT following coronary stent placement
Clinical question: Is 6 months of dual antiplatelet therapy (DAPT) therapy noninferior to 12 months, following ST-elevation myocardial infarction (STEMI) with placement of second-generation drug-eluting stents?
Background: DAPT has been the standard of care to prevent abrupt thrombotic closure of vessels following percutaneous coronary intervention (PCI) and placement of stents. The recommended duration of DAPT was lengthened from at least 30 days in bare metal stents to at least 12 months in earlier-generation drug-eluting stents after observation of high rates of in-stent thrombosis of drug-eluting stents.
Trials have shown that there is no difference in outcomes comparing 6 month vs. 12 months in DAPT for PCI in the cases of non-ST-elevation MI and unstable angina. However, there are no randomized controlled studies comparing 6 vs. 12 months of DAPT with newer drug-eluting stents following STEMI. Newer drug-eluting stents are made of biocompatible polymers with thinner struts and are thought to be fully absorbed by 3 months. International guidelines still recommend 12 months of DAPT following drug-eluting stent placement following STEMI.
Study design: Prospective, unblinded, randomized, multicenter noninferiority trial.
Setting: The study was performed at 17 sites in the Netherlands, Norway, Poland, and Switzerland.
Synopsis: This study enrolled 1100 patients with STEMI started on DAPT during December 2011-June 2015. Overall, 870 patients were randomized to continue DAPT or to change to single antiplatelet therapy (SAPT) at 6 months. Exclusions included embolic events, cardiogenic shock, revascularization, bleeding, or being on anticoagulation. Patients were followed for 24 months.
The primary endpoint was a composite of all-cause mortality, any MI, any revascularization, stroke, or thrombolysis. Incidence of the composite endpoint was 4.8% of SAPT cases, and 6.6% of DAPT cases. Noninferiority was met (P = .004) because the upper 95% confidence interval of 1.27 was smaller than the prespecified noninferiority margin of 1.66. The secondary endpoint of safety and bleeding at 18 months was 3.2% for SAPT, and 4.3% for DAPT with HR of 0.75.
Medtronic’s new stent was used in 92% of the cases of this industry-sponsored study. Despite usage of a composite endpoint, there was no difference in the individual elements of the composite in subgroup analyses. There was a low event rate in both arms likely because of the exclusions that led to a lower-risk population. The individual operators were able to choose the P2Y12 inhibitor.
Bottom line: This industry-sponsored randomized, control trial showed noninferiority of 6 months of DAPT to 12 months of therapy following STEMI to prevent in-stent thrombosis with newer second- generation drug-eluting stents. However, the study’s results may be limited to lower-risk patients, without need for revascularization, oral anticoagulation, or with stroke or cardiogenic shock.
Citation: Kedhi E et al. Six months versus 12 months of dual antiplatelet therapy after drug-eluting stent implantation in ST-elevation myocardial infarction (DAPT-STEMI): Randomised, multicenter, noninferiority trial. BMJ. 2018;363:k3793.
Dr. Lennon is an instructor of medicine at Northwestern University Feinberg School of Medicine and a hospitalist at Northwestern Memorial Hospital, both in Chicago.
Clinical question: Is 6 months of dual antiplatelet therapy (DAPT) therapy noninferior to 12 months, following ST-elevation myocardial infarction (STEMI) with placement of second-generation drug-eluting stents?
Background: DAPT has been the standard of care to prevent abrupt thrombotic closure of vessels following percutaneous coronary intervention (PCI) and placement of stents. The recommended duration of DAPT was lengthened from at least 30 days in bare metal stents to at least 12 months in earlier-generation drug-eluting stents after observation of high rates of in-stent thrombosis of drug-eluting stents.
Trials have shown that there is no difference in outcomes comparing 6 month vs. 12 months in DAPT for PCI in the cases of non-ST-elevation MI and unstable angina. However, there are no randomized controlled studies comparing 6 vs. 12 months of DAPT with newer drug-eluting stents following STEMI. Newer drug-eluting stents are made of biocompatible polymers with thinner struts and are thought to be fully absorbed by 3 months. International guidelines still recommend 12 months of DAPT following drug-eluting stent placement following STEMI.
Study design: Prospective, unblinded, randomized, multicenter noninferiority trial.
Setting: The study was performed at 17 sites in the Netherlands, Norway, Poland, and Switzerland.
Synopsis: This study enrolled 1100 patients with STEMI started on DAPT during December 2011-June 2015. Overall, 870 patients were randomized to continue DAPT or to change to single antiplatelet therapy (SAPT) at 6 months. Exclusions included embolic events, cardiogenic shock, revascularization, bleeding, or being on anticoagulation. Patients were followed for 24 months.
The primary endpoint was a composite of all-cause mortality, any MI, any revascularization, stroke, or thrombolysis. Incidence of the composite endpoint was 4.8% of SAPT cases, and 6.6% of DAPT cases. Noninferiority was met (P = .004) because the upper 95% confidence interval of 1.27 was smaller than the prespecified noninferiority margin of 1.66. The secondary endpoint of safety and bleeding at 18 months was 3.2% for SAPT, and 4.3% for DAPT with HR of 0.75.
Medtronic’s new stent was used in 92% of the cases of this industry-sponsored study. Despite usage of a composite endpoint, there was no difference in the individual elements of the composite in subgroup analyses. There was a low event rate in both arms likely because of the exclusions that led to a lower-risk population. The individual operators were able to choose the P2Y12 inhibitor.
Bottom line: This industry-sponsored randomized, control trial showed noninferiority of 6 months of DAPT to 12 months of therapy following STEMI to prevent in-stent thrombosis with newer second- generation drug-eluting stents. However, the study’s results may be limited to lower-risk patients, without need for revascularization, oral anticoagulation, or with stroke or cardiogenic shock.
Citation: Kedhi E et al. Six months versus 12 months of dual antiplatelet therapy after drug-eluting stent implantation in ST-elevation myocardial infarction (DAPT-STEMI): Randomised, multicenter, noninferiority trial. BMJ. 2018;363:k3793.
Dr. Lennon is an instructor of medicine at Northwestern University Feinberg School of Medicine and a hospitalist at Northwestern Memorial Hospital, both in Chicago.
Clinical question: Is 6 months of dual antiplatelet therapy (DAPT) therapy noninferior to 12 months, following ST-elevation myocardial infarction (STEMI) with placement of second-generation drug-eluting stents?
Background: DAPT has been the standard of care to prevent abrupt thrombotic closure of vessels following percutaneous coronary intervention (PCI) and placement of stents. The recommended duration of DAPT was lengthened from at least 30 days in bare metal stents to at least 12 months in earlier-generation drug-eluting stents after observation of high rates of in-stent thrombosis of drug-eluting stents.
Trials have shown that there is no difference in outcomes comparing 6 month vs. 12 months in DAPT for PCI in the cases of non-ST-elevation MI and unstable angina. However, there are no randomized controlled studies comparing 6 vs. 12 months of DAPT with newer drug-eluting stents following STEMI. Newer drug-eluting stents are made of biocompatible polymers with thinner struts and are thought to be fully absorbed by 3 months. International guidelines still recommend 12 months of DAPT following drug-eluting stent placement following STEMI.
Study design: Prospective, unblinded, randomized, multicenter noninferiority trial.
Setting: The study was performed at 17 sites in the Netherlands, Norway, Poland, and Switzerland.
Synopsis: This study enrolled 1100 patients with STEMI started on DAPT during December 2011-June 2015. Overall, 870 patients were randomized to continue DAPT or to change to single antiplatelet therapy (SAPT) at 6 months. Exclusions included embolic events, cardiogenic shock, revascularization, bleeding, or being on anticoagulation. Patients were followed for 24 months.
The primary endpoint was a composite of all-cause mortality, any MI, any revascularization, stroke, or thrombolysis. Incidence of the composite endpoint was 4.8% of SAPT cases, and 6.6% of DAPT cases. Noninferiority was met (P = .004) because the upper 95% confidence interval of 1.27 was smaller than the prespecified noninferiority margin of 1.66. The secondary endpoint of safety and bleeding at 18 months was 3.2% for SAPT, and 4.3% for DAPT with HR of 0.75.
Medtronic’s new stent was used in 92% of the cases of this industry-sponsored study. Despite usage of a composite endpoint, there was no difference in the individual elements of the composite in subgroup analyses. There was a low event rate in both arms likely because of the exclusions that led to a lower-risk population. The individual operators were able to choose the P2Y12 inhibitor.
Bottom line: This industry-sponsored randomized, control trial showed noninferiority of 6 months of DAPT to 12 months of therapy following STEMI to prevent in-stent thrombosis with newer second- generation drug-eluting stents. However, the study’s results may be limited to lower-risk patients, without need for revascularization, oral anticoagulation, or with stroke or cardiogenic shock.
Citation: Kedhi E et al. Six months versus 12 months of dual antiplatelet therapy after drug-eluting stent implantation in ST-elevation myocardial infarction (DAPT-STEMI): Randomised, multicenter, noninferiority trial. BMJ. 2018;363:k3793.
Dr. Lennon is an instructor of medicine at Northwestern University Feinberg School of Medicine and a hospitalist at Northwestern Memorial Hospital, both in Chicago.
First adult APS recommendations released by European society
MADRID – Low-dose aspirin is recommended for the primary prevention of antiphospholipid syndrome (APS) in patients at high risk for developing the condition, according to new recommendations developed by the European League Against Rheumatism (EULAR).
Indeed, the NSAID should be given at a dose of between 75 mg and 100 mg per day, in patients with a “high risk” antiphospholipid (aPL) antibody profile, including asymptomatic aPL antibody carriers, patients with systemic lupus erythematosus (SLE) without APS, and in women who are not pregnant but who have a history of obstetric APS.
The recommendations aim to help guide practice and ultimately to improve the quality of care for patients and their outcomes following treatment, Maria G. Tektonidou, MD, PhD, said at the European Congress of Rheumatology.
The guidance is necessary as “clinical practice in APS remains highly variable,” said Dr. Tektonidou of the National and Kapodistrian University of Athens. This is perhaps because APS is a “rare disease and also because it’s a newly recognized disease – it’s only 35 years old – and knowledge about the clinical spectrum, classification, and management is continuously advancing.”
Dr. Tektonidou, who was the convener of the EULAR Task Force that wrote the recommendations, noted that they were now published in Annals of the Rheumatic Diseases and considered three main groups of patients: those with thrombotic APS, those with obstetric APS, and those with catastrophic APS (CAPS). There are three overarching principles, 12 recommendations, and 29 graded statements, she said.
The three overarching principles concerned risk stratification, general measures for managing patients who test positive for aPL antibodies, and patient education and counseling on various topics, such as treatment adherence, therapeutic drug monitoring, contraceptive use, and lifestyle interventions.
Dr. Tektonidou highlighted how risk stratification was important and that a high-risk aPL profile was defined as the presence of lupus anticoagulant (LA) on at least two occasions, measured 12 weeks apart according to International Society on Thrombosis and Haemostasis guidelines, or the presence of two or even three aPL antibodies, or persistently high aPL antibody titers. By contrast, a low-risk aPL profile was defined as the isolated presence of anticardiolipin (aCL) or anti–beta-2 glycoprotein I antibodies at low-medium titers, particularly if transiently positive.
“Risk stratification should include the determination of the high-risk aPL profile; a prior history of thrombotic or obstetric [APS]; the coexistence of other systemic autoimmune diseases, and the presence of traditional cardiovascular risk factors,” Dr. Tektonidou said.
Four of the recommendations focus on the secondary prevention of APS, giving guidance on anticoagulant treatment with definite APS, first provoked or unprovoked venous thrombosis, and how to manage recurrent venous thrombosis. There also is a recommendation for the management of patients with definite APS and a first arterial thrombosis, outlining the type and intensity of anticoagulant therapy that should be given. Another four of the recommendations focus on the management of obstetric APS, with a focus on how to manage the various types of complications seen in pregnant women. Then the final recommendation concerns CAPS, it’s prevention and first-line treatment, and how to manage refractory patients.
With regards to CAPS, Ricard Cervera, MD, PhD, of the Hospital Clinic of Barcelona, this is “terrible” but “thankfully rare” form of APS that was first described in the early 1990s.
Although fewer than 1% of the APS adult population have CAPS (Arthritis Rheum. 2002;46[4]:1019-27), it’s a condition in which several thrombotic events occur simultaneously, affecting multiple systems or organs and which can be life threatening if not treated quickly.
New treatment guidelines for catastrophic APS
During a separate clinical science session at the conference, Dr. Cervera discussed the development of treatment guidelines for CAPS, noting that this had been one of the focus points of the McMaster RARE-Bestpractices project group in 2016. The group selected CAPS for a pilot exercise in guideline development for a rare disease and published their recommendations in 2018 (J Thromb Haemost. 2018;16:1656-64). Ten recommendations were developed, most of which were conditional, Dr. Cervera said, due to the lack of, or very low certainty, of the evidence.
The new EULAR 2019 adult APS recommendations now include CAPS and recommendation number 12 is split into two parts. The first, part A, states that prompt treatment of infections is needed in all patients positive for aPL antibodies and that anticoagulation should have minimal interruption or be used at level to help prevent the development of CAPS.
The second, part B, states that the first-line treatment of CAPS should be a triple combination therapy of glucocorticoids, heparin, and plasma exchange, or intravenous immunoglobulins, rather than single-agent treatment. Plus, it says that any triggering factor should be treated accordingly.
“Finally,” Dr. Cervera said, “in patients with refractory CAPS, B-cell depletion with rituximab or complement inhibitors, for example eculizumab, may be considered.”
The adult APS recommendations project was funded by EULAR. Dr. Tektonidou and Dr. Cervera reported having no relevant conflicts of interest.
SOURCES: Tektonidou M. Ann Rheum Dis. Jun 2019;78(Suppl 2):59-60. Abstract SP0191, doi: 0.1136/annrheumdis-2019-eular.8601; and Cervera R et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):62. Abstract SP0201. doi: 10.1136/annrheumdis-2019-eular.8444.
MADRID – Low-dose aspirin is recommended for the primary prevention of antiphospholipid syndrome (APS) in patients at high risk for developing the condition, according to new recommendations developed by the European League Against Rheumatism (EULAR).
Indeed, the NSAID should be given at a dose of between 75 mg and 100 mg per day, in patients with a “high risk” antiphospholipid (aPL) antibody profile, including asymptomatic aPL antibody carriers, patients with systemic lupus erythematosus (SLE) without APS, and in women who are not pregnant but who have a history of obstetric APS.
The recommendations aim to help guide practice and ultimately to improve the quality of care for patients and their outcomes following treatment, Maria G. Tektonidou, MD, PhD, said at the European Congress of Rheumatology.
The guidance is necessary as “clinical practice in APS remains highly variable,” said Dr. Tektonidou of the National and Kapodistrian University of Athens. This is perhaps because APS is a “rare disease and also because it’s a newly recognized disease – it’s only 35 years old – and knowledge about the clinical spectrum, classification, and management is continuously advancing.”
Dr. Tektonidou, who was the convener of the EULAR Task Force that wrote the recommendations, noted that they were now published in Annals of the Rheumatic Diseases and considered three main groups of patients: those with thrombotic APS, those with obstetric APS, and those with catastrophic APS (CAPS). There are three overarching principles, 12 recommendations, and 29 graded statements, she said.
The three overarching principles concerned risk stratification, general measures for managing patients who test positive for aPL antibodies, and patient education and counseling on various topics, such as treatment adherence, therapeutic drug monitoring, contraceptive use, and lifestyle interventions.
Dr. Tektonidou highlighted how risk stratification was important and that a high-risk aPL profile was defined as the presence of lupus anticoagulant (LA) on at least two occasions, measured 12 weeks apart according to International Society on Thrombosis and Haemostasis guidelines, or the presence of two or even three aPL antibodies, or persistently high aPL antibody titers. By contrast, a low-risk aPL profile was defined as the isolated presence of anticardiolipin (aCL) or anti–beta-2 glycoprotein I antibodies at low-medium titers, particularly if transiently positive.
“Risk stratification should include the determination of the high-risk aPL profile; a prior history of thrombotic or obstetric [APS]; the coexistence of other systemic autoimmune diseases, and the presence of traditional cardiovascular risk factors,” Dr. Tektonidou said.
Four of the recommendations focus on the secondary prevention of APS, giving guidance on anticoagulant treatment with definite APS, first provoked or unprovoked venous thrombosis, and how to manage recurrent venous thrombosis. There also is a recommendation for the management of patients with definite APS and a first arterial thrombosis, outlining the type and intensity of anticoagulant therapy that should be given. Another four of the recommendations focus on the management of obstetric APS, with a focus on how to manage the various types of complications seen in pregnant women. Then the final recommendation concerns CAPS, it’s prevention and first-line treatment, and how to manage refractory patients.
With regards to CAPS, Ricard Cervera, MD, PhD, of the Hospital Clinic of Barcelona, this is “terrible” but “thankfully rare” form of APS that was first described in the early 1990s.
Although fewer than 1% of the APS adult population have CAPS (Arthritis Rheum. 2002;46[4]:1019-27), it’s a condition in which several thrombotic events occur simultaneously, affecting multiple systems or organs and which can be life threatening if not treated quickly.
New treatment guidelines for catastrophic APS
During a separate clinical science session at the conference, Dr. Cervera discussed the development of treatment guidelines for CAPS, noting that this had been one of the focus points of the McMaster RARE-Bestpractices project group in 2016. The group selected CAPS for a pilot exercise in guideline development for a rare disease and published their recommendations in 2018 (J Thromb Haemost. 2018;16:1656-64). Ten recommendations were developed, most of which were conditional, Dr. Cervera said, due to the lack of, or very low certainty, of the evidence.
The new EULAR 2019 adult APS recommendations now include CAPS and recommendation number 12 is split into two parts. The first, part A, states that prompt treatment of infections is needed in all patients positive for aPL antibodies and that anticoagulation should have minimal interruption or be used at level to help prevent the development of CAPS.
The second, part B, states that the first-line treatment of CAPS should be a triple combination therapy of glucocorticoids, heparin, and plasma exchange, or intravenous immunoglobulins, rather than single-agent treatment. Plus, it says that any triggering factor should be treated accordingly.
“Finally,” Dr. Cervera said, “in patients with refractory CAPS, B-cell depletion with rituximab or complement inhibitors, for example eculizumab, may be considered.”
The adult APS recommendations project was funded by EULAR. Dr. Tektonidou and Dr. Cervera reported having no relevant conflicts of interest.
SOURCES: Tektonidou M. Ann Rheum Dis. Jun 2019;78(Suppl 2):59-60. Abstract SP0191, doi: 0.1136/annrheumdis-2019-eular.8601; and Cervera R et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):62. Abstract SP0201. doi: 10.1136/annrheumdis-2019-eular.8444.
MADRID – Low-dose aspirin is recommended for the primary prevention of antiphospholipid syndrome (APS) in patients at high risk for developing the condition, according to new recommendations developed by the European League Against Rheumatism (EULAR).
Indeed, the NSAID should be given at a dose of between 75 mg and 100 mg per day, in patients with a “high risk” antiphospholipid (aPL) antibody profile, including asymptomatic aPL antibody carriers, patients with systemic lupus erythematosus (SLE) without APS, and in women who are not pregnant but who have a history of obstetric APS.
The recommendations aim to help guide practice and ultimately to improve the quality of care for patients and their outcomes following treatment, Maria G. Tektonidou, MD, PhD, said at the European Congress of Rheumatology.
The guidance is necessary as “clinical practice in APS remains highly variable,” said Dr. Tektonidou of the National and Kapodistrian University of Athens. This is perhaps because APS is a “rare disease and also because it’s a newly recognized disease – it’s only 35 years old – and knowledge about the clinical spectrum, classification, and management is continuously advancing.”
Dr. Tektonidou, who was the convener of the EULAR Task Force that wrote the recommendations, noted that they were now published in Annals of the Rheumatic Diseases and considered three main groups of patients: those with thrombotic APS, those with obstetric APS, and those with catastrophic APS (CAPS). There are three overarching principles, 12 recommendations, and 29 graded statements, she said.
The three overarching principles concerned risk stratification, general measures for managing patients who test positive for aPL antibodies, and patient education and counseling on various topics, such as treatment adherence, therapeutic drug monitoring, contraceptive use, and lifestyle interventions.
Dr. Tektonidou highlighted how risk stratification was important and that a high-risk aPL profile was defined as the presence of lupus anticoagulant (LA) on at least two occasions, measured 12 weeks apart according to International Society on Thrombosis and Haemostasis guidelines, or the presence of two or even three aPL antibodies, or persistently high aPL antibody titers. By contrast, a low-risk aPL profile was defined as the isolated presence of anticardiolipin (aCL) or anti–beta-2 glycoprotein I antibodies at low-medium titers, particularly if transiently positive.
“Risk stratification should include the determination of the high-risk aPL profile; a prior history of thrombotic or obstetric [APS]; the coexistence of other systemic autoimmune diseases, and the presence of traditional cardiovascular risk factors,” Dr. Tektonidou said.
Four of the recommendations focus on the secondary prevention of APS, giving guidance on anticoagulant treatment with definite APS, first provoked or unprovoked venous thrombosis, and how to manage recurrent venous thrombosis. There also is a recommendation for the management of patients with definite APS and a first arterial thrombosis, outlining the type and intensity of anticoagulant therapy that should be given. Another four of the recommendations focus on the management of obstetric APS, with a focus on how to manage the various types of complications seen in pregnant women. Then the final recommendation concerns CAPS, it’s prevention and first-line treatment, and how to manage refractory patients.
With regards to CAPS, Ricard Cervera, MD, PhD, of the Hospital Clinic of Barcelona, this is “terrible” but “thankfully rare” form of APS that was first described in the early 1990s.
Although fewer than 1% of the APS adult population have CAPS (Arthritis Rheum. 2002;46[4]:1019-27), it’s a condition in which several thrombotic events occur simultaneously, affecting multiple systems or organs and which can be life threatening if not treated quickly.
New treatment guidelines for catastrophic APS
During a separate clinical science session at the conference, Dr. Cervera discussed the development of treatment guidelines for CAPS, noting that this had been one of the focus points of the McMaster RARE-Bestpractices project group in 2016. The group selected CAPS for a pilot exercise in guideline development for a rare disease and published their recommendations in 2018 (J Thromb Haemost. 2018;16:1656-64). Ten recommendations were developed, most of which were conditional, Dr. Cervera said, due to the lack of, or very low certainty, of the evidence.
The new EULAR 2019 adult APS recommendations now include CAPS and recommendation number 12 is split into two parts. The first, part A, states that prompt treatment of infections is needed in all patients positive for aPL antibodies and that anticoagulation should have minimal interruption or be used at level to help prevent the development of CAPS.
The second, part B, states that the first-line treatment of CAPS should be a triple combination therapy of glucocorticoids, heparin, and plasma exchange, or intravenous immunoglobulins, rather than single-agent treatment. Plus, it says that any triggering factor should be treated accordingly.
“Finally,” Dr. Cervera said, “in patients with refractory CAPS, B-cell depletion with rituximab or complement inhibitors, for example eculizumab, may be considered.”
The adult APS recommendations project was funded by EULAR. Dr. Tektonidou and Dr. Cervera reported having no relevant conflicts of interest.
SOURCES: Tektonidou M. Ann Rheum Dis. Jun 2019;78(Suppl 2):59-60. Abstract SP0191, doi: 0.1136/annrheumdis-2019-eular.8601; and Cervera R et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):62. Abstract SP0201. doi: 10.1136/annrheumdis-2019-eular.8444.
REPORTING FROM THE EULAR 2019 Congress
NOACs benefit early stage chronic kidney disease patients
Non–vitamin K oral anticoagulants (NOACs) significantly reduced the risk of stroke or systemic embolism compared to vitamin K antagonists (VKAs) for patients in the early stages of chronic kidney disease and comorbid atrial fibrillation, based on data from a meta-analysis of roughly 34,000 patients.
Chronic kidney disease increases the risk of complications including stroke, congestive heart failure, and death in patients who also have atrial fibrillation, but most trials of anticoagulant therapy to reduce the risk of such events have excluded these patients, wrote Jeffrey T. Ha, MBBS, of the George Institute for Global Health, Newtown, Australia, and colleagues.
To assess the benefits and harms of oral anticoagulants for multiple indications in chronic kidney disease patients, the researchers conducted a meta-analysis of 45 studies including 34,082 individuals. The findings were published in the Annals of Internal Medicine. The analysis included 8 trials of end stage kidney disease patients on dialysis; the remaining trials excluded patients with creatinine clearance less than 20 mL/min or an estimated glomerular filtration rate less than 15 mL/min per 1.73 m2. The interventional agents were rivaroxaban, dabigatran, apixaban, edoxaban, betrixaban, warfarin, and acenocoumarol.
A notable finding was the significant reduction in relative risk of stroke or systemic embolism (21%), hemorrhagic stroke (52%), and intracranial hemorrhage (51%) for early-stage chronic kidney disease patients with atrial fibrillation given NOACs, compared with those given VKAs.
The evidence for the superiority of NOACs over VKAs for reducing risk of venous thromboembolism (VTE) or VTE-related death was uncertain, as was the evidence to draw any conclusions about benefits and harms of either NOACs or VKAs for patients with advanced or end-stage kidney disease.
Across all trials, NOACs appeared to reduce the relative risk of major bleeding, compared with VKAs by roughly 25%, but the difference was not statistically significant, the researchers noted.
The findings were limited by the lack of evidence for oral anticoagulant use in patients with advanced chronic or end-stage kidney disease, as well as inability to assess differences among NOACs, the researchers noted. However, the results suggest that NOACs may be recommended over VKAs for the subgroup of early-stage chronic kidney disease patients with atrial fibrillation, they said.
Several additional trials are in progress, and future trials “should include not only participants with dialysis-dependent ESKD [end-stage kidney disease] but also those with CrCl [creatinine clearance of] less than 25 mL/min,” and compare NOACs with placebo as well, they noted.
Lead author Dr. Ha is supported by a University Postgraduate Award from University of New South Wales, Sydney, but had no financial conflicts to disclose; coauthors disclosed support from various organizations as well as pharmaceutical companies including Baxter, Amgen, Eli Lilly, Boehringer Ingelheim, Vifor Pharma, Janssen, Pfizer, Bristol-Myers Squibb, and GlaxoSmithKline.
SOURCE: Ha JT et al. Ann Intern Med. 2019 July 15. doi: 10.7326/M19-0087
The significant reduction in risk of hemorrhagic stroke, recurrent venous thromboembolism, and VTE-related deaths in patients with early-stage chronic kidney disease given a NOAC [non–vitamin K oral anticoagulants] in a meta-analysis supports clinical application, but is there a level of renal dysfunction for which clinicians should apply greater caution in extrapolating these findings? As the evidence supporting the safety and effectiveness of NOACs in the general population increases, there is a renewed interest in defining the role of anticoagulant therapy to prevent stroke and VTE in patients with chronic kidney disease and end-stage kidney disease. This interest is driven in part by uncertainty as to the benefits vs. harms of warfarin for patients with chronic kidney disease. The data in the meta-analysis by Ha and colleagues do not support any benefits for patients with end-stage disease, but the results of two ongoing clinical trials of patients with atrial fibrillation and end-stage kidney disease may offer insights.
Until the results of these trials become available, the decision to use anticoagulant therapy in patients with end-stage kidney disease will continue to require an individualized approach that balances potential benefits and harms.
Ainslie Hildebrand, MD, of University of Alberta, Edmonton; Christine Ribic, MD, of McMaster University, Hamilton, Ont.; and Deborah Zimmerman, MD, of the University of Ottawa, made these comments in an accompanying editorial (Ann Intern Med. 2019 July 15. doi:10.7326/M19-1504). Dr. Ribic disclosed grants from Pfizer, Leo Pharma, and Astellas Pharma. Dr. Hildebrand and Dr. Zimmerman had no financial conflicts to disclose.
The significant reduction in risk of hemorrhagic stroke, recurrent venous thromboembolism, and VTE-related deaths in patients with early-stage chronic kidney disease given a NOAC [non–vitamin K oral anticoagulants] in a meta-analysis supports clinical application, but is there a level of renal dysfunction for which clinicians should apply greater caution in extrapolating these findings? As the evidence supporting the safety and effectiveness of NOACs in the general population increases, there is a renewed interest in defining the role of anticoagulant therapy to prevent stroke and VTE in patients with chronic kidney disease and end-stage kidney disease. This interest is driven in part by uncertainty as to the benefits vs. harms of warfarin for patients with chronic kidney disease. The data in the meta-analysis by Ha and colleagues do not support any benefits for patients with end-stage disease, but the results of two ongoing clinical trials of patients with atrial fibrillation and end-stage kidney disease may offer insights.
Until the results of these trials become available, the decision to use anticoagulant therapy in patients with end-stage kidney disease will continue to require an individualized approach that balances potential benefits and harms.
Ainslie Hildebrand, MD, of University of Alberta, Edmonton; Christine Ribic, MD, of McMaster University, Hamilton, Ont.; and Deborah Zimmerman, MD, of the University of Ottawa, made these comments in an accompanying editorial (Ann Intern Med. 2019 July 15. doi:10.7326/M19-1504). Dr. Ribic disclosed grants from Pfizer, Leo Pharma, and Astellas Pharma. Dr. Hildebrand and Dr. Zimmerman had no financial conflicts to disclose.
The significant reduction in risk of hemorrhagic stroke, recurrent venous thromboembolism, and VTE-related deaths in patients with early-stage chronic kidney disease given a NOAC [non–vitamin K oral anticoagulants] in a meta-analysis supports clinical application, but is there a level of renal dysfunction for which clinicians should apply greater caution in extrapolating these findings? As the evidence supporting the safety and effectiveness of NOACs in the general population increases, there is a renewed interest in defining the role of anticoagulant therapy to prevent stroke and VTE in patients with chronic kidney disease and end-stage kidney disease. This interest is driven in part by uncertainty as to the benefits vs. harms of warfarin for patients with chronic kidney disease. The data in the meta-analysis by Ha and colleagues do not support any benefits for patients with end-stage disease, but the results of two ongoing clinical trials of patients with atrial fibrillation and end-stage kidney disease may offer insights.
Until the results of these trials become available, the decision to use anticoagulant therapy in patients with end-stage kidney disease will continue to require an individualized approach that balances potential benefits and harms.
Ainslie Hildebrand, MD, of University of Alberta, Edmonton; Christine Ribic, MD, of McMaster University, Hamilton, Ont.; and Deborah Zimmerman, MD, of the University of Ottawa, made these comments in an accompanying editorial (Ann Intern Med. 2019 July 15. doi:10.7326/M19-1504). Dr. Ribic disclosed grants from Pfizer, Leo Pharma, and Astellas Pharma. Dr. Hildebrand and Dr. Zimmerman had no financial conflicts to disclose.
Non–vitamin K oral anticoagulants (NOACs) significantly reduced the risk of stroke or systemic embolism compared to vitamin K antagonists (VKAs) for patients in the early stages of chronic kidney disease and comorbid atrial fibrillation, based on data from a meta-analysis of roughly 34,000 patients.
Chronic kidney disease increases the risk of complications including stroke, congestive heart failure, and death in patients who also have atrial fibrillation, but most trials of anticoagulant therapy to reduce the risk of such events have excluded these patients, wrote Jeffrey T. Ha, MBBS, of the George Institute for Global Health, Newtown, Australia, and colleagues.
To assess the benefits and harms of oral anticoagulants for multiple indications in chronic kidney disease patients, the researchers conducted a meta-analysis of 45 studies including 34,082 individuals. The findings were published in the Annals of Internal Medicine. The analysis included 8 trials of end stage kidney disease patients on dialysis; the remaining trials excluded patients with creatinine clearance less than 20 mL/min or an estimated glomerular filtration rate less than 15 mL/min per 1.73 m2. The interventional agents were rivaroxaban, dabigatran, apixaban, edoxaban, betrixaban, warfarin, and acenocoumarol.
A notable finding was the significant reduction in relative risk of stroke or systemic embolism (21%), hemorrhagic stroke (52%), and intracranial hemorrhage (51%) for early-stage chronic kidney disease patients with atrial fibrillation given NOACs, compared with those given VKAs.
The evidence for the superiority of NOACs over VKAs for reducing risk of venous thromboembolism (VTE) or VTE-related death was uncertain, as was the evidence to draw any conclusions about benefits and harms of either NOACs or VKAs for patients with advanced or end-stage kidney disease.
Across all trials, NOACs appeared to reduce the relative risk of major bleeding, compared with VKAs by roughly 25%, but the difference was not statistically significant, the researchers noted.
The findings were limited by the lack of evidence for oral anticoagulant use in patients with advanced chronic or end-stage kidney disease, as well as inability to assess differences among NOACs, the researchers noted. However, the results suggest that NOACs may be recommended over VKAs for the subgroup of early-stage chronic kidney disease patients with atrial fibrillation, they said.
Several additional trials are in progress, and future trials “should include not only participants with dialysis-dependent ESKD [end-stage kidney disease] but also those with CrCl [creatinine clearance of] less than 25 mL/min,” and compare NOACs with placebo as well, they noted.
Lead author Dr. Ha is supported by a University Postgraduate Award from University of New South Wales, Sydney, but had no financial conflicts to disclose; coauthors disclosed support from various organizations as well as pharmaceutical companies including Baxter, Amgen, Eli Lilly, Boehringer Ingelheim, Vifor Pharma, Janssen, Pfizer, Bristol-Myers Squibb, and GlaxoSmithKline.
SOURCE: Ha JT et al. Ann Intern Med. 2019 July 15. doi: 10.7326/M19-0087
Non–vitamin K oral anticoagulants (NOACs) significantly reduced the risk of stroke or systemic embolism compared to vitamin K antagonists (VKAs) for patients in the early stages of chronic kidney disease and comorbid atrial fibrillation, based on data from a meta-analysis of roughly 34,000 patients.
Chronic kidney disease increases the risk of complications including stroke, congestive heart failure, and death in patients who also have atrial fibrillation, but most trials of anticoagulant therapy to reduce the risk of such events have excluded these patients, wrote Jeffrey T. Ha, MBBS, of the George Institute for Global Health, Newtown, Australia, and colleagues.
To assess the benefits and harms of oral anticoagulants for multiple indications in chronic kidney disease patients, the researchers conducted a meta-analysis of 45 studies including 34,082 individuals. The findings were published in the Annals of Internal Medicine. The analysis included 8 trials of end stage kidney disease patients on dialysis; the remaining trials excluded patients with creatinine clearance less than 20 mL/min or an estimated glomerular filtration rate less than 15 mL/min per 1.73 m2. The interventional agents were rivaroxaban, dabigatran, apixaban, edoxaban, betrixaban, warfarin, and acenocoumarol.
A notable finding was the significant reduction in relative risk of stroke or systemic embolism (21%), hemorrhagic stroke (52%), and intracranial hemorrhage (51%) for early-stage chronic kidney disease patients with atrial fibrillation given NOACs, compared with those given VKAs.
The evidence for the superiority of NOACs over VKAs for reducing risk of venous thromboembolism (VTE) or VTE-related death was uncertain, as was the evidence to draw any conclusions about benefits and harms of either NOACs or VKAs for patients with advanced or end-stage kidney disease.
Across all trials, NOACs appeared to reduce the relative risk of major bleeding, compared with VKAs by roughly 25%, but the difference was not statistically significant, the researchers noted.
The findings were limited by the lack of evidence for oral anticoagulant use in patients with advanced chronic or end-stage kidney disease, as well as inability to assess differences among NOACs, the researchers noted. However, the results suggest that NOACs may be recommended over VKAs for the subgroup of early-stage chronic kidney disease patients with atrial fibrillation, they said.
Several additional trials are in progress, and future trials “should include not only participants with dialysis-dependent ESKD [end-stage kidney disease] but also those with CrCl [creatinine clearance of] less than 25 mL/min,” and compare NOACs with placebo as well, they noted.
Lead author Dr. Ha is supported by a University Postgraduate Award from University of New South Wales, Sydney, but had no financial conflicts to disclose; coauthors disclosed support from various organizations as well as pharmaceutical companies including Baxter, Amgen, Eli Lilly, Boehringer Ingelheim, Vifor Pharma, Janssen, Pfizer, Bristol-Myers Squibb, and GlaxoSmithKline.
SOURCE: Ha JT et al. Ann Intern Med. 2019 July 15. doi: 10.7326/M19-0087
FROM THE ANNALS OF INTERNAL MEDICINE