User login
Thyroid cancer increase observed in transgender female veterans
WASHINGTON – Experts urge a cautious interpretation of these recent study results.
“In our clinic of about 50 transgender women, we noticed that we had two diagnosed cases of thyroid cancer in a year,” first author John Christensen, MD, of UC Davis Health, division of endocrinology, diabetes & metabolism, Sacramento, said in an interivew. He presented their findings at the annual meeting of the American Thyroid Association.
Comparatively, the thyroid cancer prevalence among cisgender male veterans is estimated at about 0.19%; the rate among all those assigned male at birth in the general population is 0.13%, whereas the rate among those assigned female at birth, which has historically been higher for all thyroid cancer subtypes, is 0.44%, according to U.S. cancer statistics for 2020 from the National Cancer Institute.
“About one-third of our [veteran] patients had been receiving estrogen for an average of over 3 years before diagnosis, which could suggest estrogen gender‐affirming hormone therapy [GAHT] may be a potentially important risk factor,” Dr. Christensen said.
Sustained use of external estrogen, especially in cisgender women undergoing fertility treatments, has been linked to an increased risk for thyroid cancer. This is because it can lead to an increase in estrogen receptors in cancerous cells. But experts caution that many other factors also come into play.
“There is definitely an implication that if you give extra estrogen to someone assigned female at birth, you may have an increased risk of thyroid cancer,” Dr. Christensen said. “So, it would stand to reason that even in those who are not assigned female at birth, there may be a risk from exogenous estrogen that may lead to an increased risk of thyroid cancer down the line.”
To investigate the issue in a larger population, Dr. Christensen and colleagues evaluated data from the comprehensive, nationwide Veterans Affairs Informatics and Computing Infrastructure database, including approximately 9 million veterans who had outpatient visits between December 2017 and January 2022.
Of the veterans, 9,988 were determined to likely be transgender women, based on either having an ICD-10 diagnosis code for gender dysphoria or being assigned male at birth and having received an estrogen or estradiol prescription.
Of those patients, 76 had an ICD-10 code indicating thyroid cancer and 34 had verification of the thyroid cancer on chart review, representing a prevalence of 0.34% among transgender female veterans.
The average age at thyroid cancer diagnosis among the veterans was 53.8 years, and 29.4% (10 of 34) of those patients had extrathyroidal disease at the time of their thyroid cancer diagnosis. The median body mass index, available for 26 patients, was 32, which is indicative of obesity.
In terms of the patients’ thyroid cancer subtypes, 22 were papillary cancer, 5 were a follicular variant of papillary cancer, 5 were both papillary and follicular cancer, 4 were follicular cancer, 3 were a Hürthle cell variant of follicular cancer, and one was unknown.
Among 11 (32.3%) of the 34 veterans receiving estrogen GAHT at diagnosis, treatment began an average of 3.38 years prior to diagnosis at variable doses and using various routes of administration.
About half of the patients had a history of smoking; however, Dr. Christensen noted that the role of smoking as being a risk factor in estrogenic cancers has been debated. Though most patients were obese, obesity is both very common and not well established in terms of its quantitative impact on the risk for cancer development.
With the small size of the thyroid cancer cohort and omissions in the medical record among the study’s important limitations, Dr. Christensen urged a cautious interpretation of the findings.
“We are certainly suspicious that GAHT may be associated with an increased risk of thyroid cancer, but I would characterize the trends in our data as being potentially suggestive or hypothesis generating – not conclusive,” he added. “I would hate for any transgender women reading this to stop taking GAHT without talking to their doctors first.”
Commenting on the issue, Maurice Garcia, MD, a clinical associate professor of urology and director of the transgender surgery and health program at Cedars-Sinai Medical Center, Los Angeles, said that any definitive evidence of an increase in cancer risk among transgender people is lacking.
“With an estimated 1.5 [million] to 1.6 million people in the U.S. who are transgender, with many of them receiving GAHT, we haven’t observed a bump or high incidence of any kind of cancer among these people so far,” he said.
“There’s certainly a high potential that hormone therapy, whether it’s feminizing or masculinizing hormone therapy, can affect an individual’s cancer risk,” he added. “But we don’t know of any [definitive evidence] yet of an increase, and, there’s also even the question of whether there could be an opposite effect.”
Regarding the thyroid cancer data, Dr. Garcia agreed that the preliminary nature of the study is a key limitation. “It’s hard to tell if these were comparable groups, or whether those in the transgender group came in with higher risk factors for thyroid cancer.
“Until more statistical analysis is done, I think all that can be said is that it’s speculative.”
Dr. Garcia, who coauthored a review on cancer screening for transgender individuals, underscored that, despite a lack of data suggesting that transgender patients need cancer screening any more than their matched cisgender counterparts, “the point is that we cannot forget to screen them at all.”
Dr. Christensen and Dr. Garcia had no disclosures to report.
A version of this article first appeared on Medscape.com.
WASHINGTON – Experts urge a cautious interpretation of these recent study results.
“In our clinic of about 50 transgender women, we noticed that we had two diagnosed cases of thyroid cancer in a year,” first author John Christensen, MD, of UC Davis Health, division of endocrinology, diabetes & metabolism, Sacramento, said in an interivew. He presented their findings at the annual meeting of the American Thyroid Association.
Comparatively, the thyroid cancer prevalence among cisgender male veterans is estimated at about 0.19%; the rate among all those assigned male at birth in the general population is 0.13%, whereas the rate among those assigned female at birth, which has historically been higher for all thyroid cancer subtypes, is 0.44%, according to U.S. cancer statistics for 2020 from the National Cancer Institute.
“About one-third of our [veteran] patients had been receiving estrogen for an average of over 3 years before diagnosis, which could suggest estrogen gender‐affirming hormone therapy [GAHT] may be a potentially important risk factor,” Dr. Christensen said.
Sustained use of external estrogen, especially in cisgender women undergoing fertility treatments, has been linked to an increased risk for thyroid cancer. This is because it can lead to an increase in estrogen receptors in cancerous cells. But experts caution that many other factors also come into play.
“There is definitely an implication that if you give extra estrogen to someone assigned female at birth, you may have an increased risk of thyroid cancer,” Dr. Christensen said. “So, it would stand to reason that even in those who are not assigned female at birth, there may be a risk from exogenous estrogen that may lead to an increased risk of thyroid cancer down the line.”
To investigate the issue in a larger population, Dr. Christensen and colleagues evaluated data from the comprehensive, nationwide Veterans Affairs Informatics and Computing Infrastructure database, including approximately 9 million veterans who had outpatient visits between December 2017 and January 2022.
Of the veterans, 9,988 were determined to likely be transgender women, based on either having an ICD-10 diagnosis code for gender dysphoria or being assigned male at birth and having received an estrogen or estradiol prescription.
Of those patients, 76 had an ICD-10 code indicating thyroid cancer and 34 had verification of the thyroid cancer on chart review, representing a prevalence of 0.34% among transgender female veterans.
The average age at thyroid cancer diagnosis among the veterans was 53.8 years, and 29.4% (10 of 34) of those patients had extrathyroidal disease at the time of their thyroid cancer diagnosis. The median body mass index, available for 26 patients, was 32, which is indicative of obesity.
In terms of the patients’ thyroid cancer subtypes, 22 were papillary cancer, 5 were a follicular variant of papillary cancer, 5 were both papillary and follicular cancer, 4 were follicular cancer, 3 were a Hürthle cell variant of follicular cancer, and one was unknown.
Among 11 (32.3%) of the 34 veterans receiving estrogen GAHT at diagnosis, treatment began an average of 3.38 years prior to diagnosis at variable doses and using various routes of administration.
About half of the patients had a history of smoking; however, Dr. Christensen noted that the role of smoking as being a risk factor in estrogenic cancers has been debated. Though most patients were obese, obesity is both very common and not well established in terms of its quantitative impact on the risk for cancer development.
With the small size of the thyroid cancer cohort and omissions in the medical record among the study’s important limitations, Dr. Christensen urged a cautious interpretation of the findings.
“We are certainly suspicious that GAHT may be associated with an increased risk of thyroid cancer, but I would characterize the trends in our data as being potentially suggestive or hypothesis generating – not conclusive,” he added. “I would hate for any transgender women reading this to stop taking GAHT without talking to their doctors first.”
Commenting on the issue, Maurice Garcia, MD, a clinical associate professor of urology and director of the transgender surgery and health program at Cedars-Sinai Medical Center, Los Angeles, said that any definitive evidence of an increase in cancer risk among transgender people is lacking.
“With an estimated 1.5 [million] to 1.6 million people in the U.S. who are transgender, with many of them receiving GAHT, we haven’t observed a bump or high incidence of any kind of cancer among these people so far,” he said.
“There’s certainly a high potential that hormone therapy, whether it’s feminizing or masculinizing hormone therapy, can affect an individual’s cancer risk,” he added. “But we don’t know of any [definitive evidence] yet of an increase, and, there’s also even the question of whether there could be an opposite effect.”
Regarding the thyroid cancer data, Dr. Garcia agreed that the preliminary nature of the study is a key limitation. “It’s hard to tell if these were comparable groups, or whether those in the transgender group came in with higher risk factors for thyroid cancer.
“Until more statistical analysis is done, I think all that can be said is that it’s speculative.”
Dr. Garcia, who coauthored a review on cancer screening for transgender individuals, underscored that, despite a lack of data suggesting that transgender patients need cancer screening any more than their matched cisgender counterparts, “the point is that we cannot forget to screen them at all.”
Dr. Christensen and Dr. Garcia had no disclosures to report.
A version of this article first appeared on Medscape.com.
WASHINGTON – Experts urge a cautious interpretation of these recent study results.
“In our clinic of about 50 transgender women, we noticed that we had two diagnosed cases of thyroid cancer in a year,” first author John Christensen, MD, of UC Davis Health, division of endocrinology, diabetes & metabolism, Sacramento, said in an interivew. He presented their findings at the annual meeting of the American Thyroid Association.
Comparatively, the thyroid cancer prevalence among cisgender male veterans is estimated at about 0.19%; the rate among all those assigned male at birth in the general population is 0.13%, whereas the rate among those assigned female at birth, which has historically been higher for all thyroid cancer subtypes, is 0.44%, according to U.S. cancer statistics for 2020 from the National Cancer Institute.
“About one-third of our [veteran] patients had been receiving estrogen for an average of over 3 years before diagnosis, which could suggest estrogen gender‐affirming hormone therapy [GAHT] may be a potentially important risk factor,” Dr. Christensen said.
Sustained use of external estrogen, especially in cisgender women undergoing fertility treatments, has been linked to an increased risk for thyroid cancer. This is because it can lead to an increase in estrogen receptors in cancerous cells. But experts caution that many other factors also come into play.
“There is definitely an implication that if you give extra estrogen to someone assigned female at birth, you may have an increased risk of thyroid cancer,” Dr. Christensen said. “So, it would stand to reason that even in those who are not assigned female at birth, there may be a risk from exogenous estrogen that may lead to an increased risk of thyroid cancer down the line.”
To investigate the issue in a larger population, Dr. Christensen and colleagues evaluated data from the comprehensive, nationwide Veterans Affairs Informatics and Computing Infrastructure database, including approximately 9 million veterans who had outpatient visits between December 2017 and January 2022.
Of the veterans, 9,988 were determined to likely be transgender women, based on either having an ICD-10 diagnosis code for gender dysphoria or being assigned male at birth and having received an estrogen or estradiol prescription.
Of those patients, 76 had an ICD-10 code indicating thyroid cancer and 34 had verification of the thyroid cancer on chart review, representing a prevalence of 0.34% among transgender female veterans.
The average age at thyroid cancer diagnosis among the veterans was 53.8 years, and 29.4% (10 of 34) of those patients had extrathyroidal disease at the time of their thyroid cancer diagnosis. The median body mass index, available for 26 patients, was 32, which is indicative of obesity.
In terms of the patients’ thyroid cancer subtypes, 22 were papillary cancer, 5 were a follicular variant of papillary cancer, 5 were both papillary and follicular cancer, 4 were follicular cancer, 3 were a Hürthle cell variant of follicular cancer, and one was unknown.
Among 11 (32.3%) of the 34 veterans receiving estrogen GAHT at diagnosis, treatment began an average of 3.38 years prior to diagnosis at variable doses and using various routes of administration.
About half of the patients had a history of smoking; however, Dr. Christensen noted that the role of smoking as being a risk factor in estrogenic cancers has been debated. Though most patients were obese, obesity is both very common and not well established in terms of its quantitative impact on the risk for cancer development.
With the small size of the thyroid cancer cohort and omissions in the medical record among the study’s important limitations, Dr. Christensen urged a cautious interpretation of the findings.
“We are certainly suspicious that GAHT may be associated with an increased risk of thyroid cancer, but I would characterize the trends in our data as being potentially suggestive or hypothesis generating – not conclusive,” he added. “I would hate for any transgender women reading this to stop taking GAHT without talking to their doctors first.”
Commenting on the issue, Maurice Garcia, MD, a clinical associate professor of urology and director of the transgender surgery and health program at Cedars-Sinai Medical Center, Los Angeles, said that any definitive evidence of an increase in cancer risk among transgender people is lacking.
“With an estimated 1.5 [million] to 1.6 million people in the U.S. who are transgender, with many of them receiving GAHT, we haven’t observed a bump or high incidence of any kind of cancer among these people so far,” he said.
“There’s certainly a high potential that hormone therapy, whether it’s feminizing or masculinizing hormone therapy, can affect an individual’s cancer risk,” he added. “But we don’t know of any [definitive evidence] yet of an increase, and, there’s also even the question of whether there could be an opposite effect.”
Regarding the thyroid cancer data, Dr. Garcia agreed that the preliminary nature of the study is a key limitation. “It’s hard to tell if these were comparable groups, or whether those in the transgender group came in with higher risk factors for thyroid cancer.
“Until more statistical analysis is done, I think all that can be said is that it’s speculative.”
Dr. Garcia, who coauthored a review on cancer screening for transgender individuals, underscored that, despite a lack of data suggesting that transgender patients need cancer screening any more than their matched cisgender counterparts, “the point is that we cannot forget to screen them at all.”
Dr. Christensen and Dr. Garcia had no disclosures to report.
A version of this article first appeared on Medscape.com.
AT ATA 2023
Transgender patients report stigma, voyeurism in medical care
Transgender patients in the United States and Canada told researchers that they often face voyeuristic and stigmatizing treatment in medical clinics and they fear they’re getting substandard care.
“Transgender people feel that their care worsens when clinicians learn that they are transgender, and thus they often have to choose between stigma if clinicians learn that they are transgender and potentially ineffective clinical problem-solving if they do not,” said Yale Cancer Center instructor of medicine Ash B. Alpert, MD, MFA, lead author of the study, which was published in Annals of Family Medicine. For the qualitative study, researchers held seven online focus groups with 30 transgender adults (median age, 31; age range, 20-67; 40% people of color; and 47% with incomes of more than $40,000 a year). All but one were from the United States.
According to the study, the participants said clinicians often ask “irrelevant” questions, sometimes with intentions that appear voyeuristic. “I saw a pulmonologist earlier in the year and one of his first questions was, ‘When are you getting genital surgery?’ and I was like, ‘I’m here for my lungs,’ ” said a White, nonbinary participant. A White male participant said “As soon as I walk in, no matter what I’m there for, the first [order] of business is for them to determine my gender or sex assigned at birth ... and ... once they ... know they’re ... much more at ease.”
Participants also described how medical encounters went awry once clinicians realized they were transgender. “It wasn’t until after I told the doctor that I was on hormones for transition that I started being ‘he’d.’ ” Before that, it was “she,” said a Black transgender woman.
One participant, a Black person who declined to identify by gender, said “I don’t feel comfortable sharing medical records with physicians anyway because it’s a guarantee that I’m not gonna get services. So I lost [my medical records] and they’re good wherever they are now, far away from me.”
Ten participants were clinicians. “Many seemed concerned that transgender people are being put in distressing and difficult situations in medical settings and also seemed dubious that health care for transgender people would improve without a complete overhaul,” Dr. Alpert said.
In an interview, Boston University assistant professor of medicine C. Streed Jr., MD, MPH, who studies gender and health, praised the study. He said it plays an early role in revealing the problems faced by transgender people in the health system.
“We do not fully know the experience of transgender persons accessing care in various contexts, especially in specialty care such as oncology, pulmonology, nephrology, etc.” Dr. Streed said. “We do not know how they identify specialists who are welcoming, compassionate, and competent in care for transgender persons.”
The results aren’t surprising, Dr. Streed said, “given the lack of training in medical school, residency, and fellowship specific to the unique needs of transgender persons.”
How can clinicians improve interactions with transgender people?
What can clinicians do to help transgender patients feel comfortable? Dr. Alpert suggested they “ask [only] for medically relevant information and to explain to patients why it is medically relevant.”
“This is important because transgender people are often weighing the risks and benefits of disclosing information that could be used to stigmatize them,” Dr. Alpert said.
What if a clinician wants to create a personal connection with a patient by asking questions about their life? “If you as a clinician think it’s important to ask for nonmedical information to get to know a patient, explicitly clarify that your questions are optional and not medically relevant,” Dr. Alpert said. “That way patients have the ability to consent or not to questions that likely will not directly benefit their care.”
Dr. Streed offered a similar perspective. “Clinicians should only be asking questions of patients that will affect the care the patient is seeking and for which the clinician is trained to provide,” he said. “Having a transgender patient is not an opportunity for a clinician to satisfy their curiosity when it is not related to the care the patient is seeking or needs.”
More specifically, Dr. Streed offered an example: Clinicians should not be asking about a patient’s genitals if they are seeking care related to their asthma diagnosis.
Dr. Streed referred clinicians to resources from the American Medical Association and the Human Rights Campaign for guidelines on caring for transgender patients.
The study was funded by Conquer Cancer. The study authors and Dr. Streed have no relevant disclosures.
Transgender patients in the United States and Canada told researchers that they often face voyeuristic and stigmatizing treatment in medical clinics and they fear they’re getting substandard care.
“Transgender people feel that their care worsens when clinicians learn that they are transgender, and thus they often have to choose between stigma if clinicians learn that they are transgender and potentially ineffective clinical problem-solving if they do not,” said Yale Cancer Center instructor of medicine Ash B. Alpert, MD, MFA, lead author of the study, which was published in Annals of Family Medicine. For the qualitative study, researchers held seven online focus groups with 30 transgender adults (median age, 31; age range, 20-67; 40% people of color; and 47% with incomes of more than $40,000 a year). All but one were from the United States.
According to the study, the participants said clinicians often ask “irrelevant” questions, sometimes with intentions that appear voyeuristic. “I saw a pulmonologist earlier in the year and one of his first questions was, ‘When are you getting genital surgery?’ and I was like, ‘I’m here for my lungs,’ ” said a White, nonbinary participant. A White male participant said “As soon as I walk in, no matter what I’m there for, the first [order] of business is for them to determine my gender or sex assigned at birth ... and ... once they ... know they’re ... much more at ease.”
Participants also described how medical encounters went awry once clinicians realized they were transgender. “It wasn’t until after I told the doctor that I was on hormones for transition that I started being ‘he’d.’ ” Before that, it was “she,” said a Black transgender woman.
One participant, a Black person who declined to identify by gender, said “I don’t feel comfortable sharing medical records with physicians anyway because it’s a guarantee that I’m not gonna get services. So I lost [my medical records] and they’re good wherever they are now, far away from me.”
Ten participants were clinicians. “Many seemed concerned that transgender people are being put in distressing and difficult situations in medical settings and also seemed dubious that health care for transgender people would improve without a complete overhaul,” Dr. Alpert said.
In an interview, Boston University assistant professor of medicine C. Streed Jr., MD, MPH, who studies gender and health, praised the study. He said it plays an early role in revealing the problems faced by transgender people in the health system.
“We do not fully know the experience of transgender persons accessing care in various contexts, especially in specialty care such as oncology, pulmonology, nephrology, etc.” Dr. Streed said. “We do not know how they identify specialists who are welcoming, compassionate, and competent in care for transgender persons.”
The results aren’t surprising, Dr. Streed said, “given the lack of training in medical school, residency, and fellowship specific to the unique needs of transgender persons.”
How can clinicians improve interactions with transgender people?
What can clinicians do to help transgender patients feel comfortable? Dr. Alpert suggested they “ask [only] for medically relevant information and to explain to patients why it is medically relevant.”
“This is important because transgender people are often weighing the risks and benefits of disclosing information that could be used to stigmatize them,” Dr. Alpert said.
What if a clinician wants to create a personal connection with a patient by asking questions about their life? “If you as a clinician think it’s important to ask for nonmedical information to get to know a patient, explicitly clarify that your questions are optional and not medically relevant,” Dr. Alpert said. “That way patients have the ability to consent or not to questions that likely will not directly benefit their care.”
Dr. Streed offered a similar perspective. “Clinicians should only be asking questions of patients that will affect the care the patient is seeking and for which the clinician is trained to provide,” he said. “Having a transgender patient is not an opportunity for a clinician to satisfy their curiosity when it is not related to the care the patient is seeking or needs.”
More specifically, Dr. Streed offered an example: Clinicians should not be asking about a patient’s genitals if they are seeking care related to their asthma diagnosis.
Dr. Streed referred clinicians to resources from the American Medical Association and the Human Rights Campaign for guidelines on caring for transgender patients.
The study was funded by Conquer Cancer. The study authors and Dr. Streed have no relevant disclosures.
Transgender patients in the United States and Canada told researchers that they often face voyeuristic and stigmatizing treatment in medical clinics and they fear they’re getting substandard care.
“Transgender people feel that their care worsens when clinicians learn that they are transgender, and thus they often have to choose between stigma if clinicians learn that they are transgender and potentially ineffective clinical problem-solving if they do not,” said Yale Cancer Center instructor of medicine Ash B. Alpert, MD, MFA, lead author of the study, which was published in Annals of Family Medicine. For the qualitative study, researchers held seven online focus groups with 30 transgender adults (median age, 31; age range, 20-67; 40% people of color; and 47% with incomes of more than $40,000 a year). All but one were from the United States.
According to the study, the participants said clinicians often ask “irrelevant” questions, sometimes with intentions that appear voyeuristic. “I saw a pulmonologist earlier in the year and one of his first questions was, ‘When are you getting genital surgery?’ and I was like, ‘I’m here for my lungs,’ ” said a White, nonbinary participant. A White male participant said “As soon as I walk in, no matter what I’m there for, the first [order] of business is for them to determine my gender or sex assigned at birth ... and ... once they ... know they’re ... much more at ease.”
Participants also described how medical encounters went awry once clinicians realized they were transgender. “It wasn’t until after I told the doctor that I was on hormones for transition that I started being ‘he’d.’ ” Before that, it was “she,” said a Black transgender woman.
One participant, a Black person who declined to identify by gender, said “I don’t feel comfortable sharing medical records with physicians anyway because it’s a guarantee that I’m not gonna get services. So I lost [my medical records] and they’re good wherever they are now, far away from me.”
Ten participants were clinicians. “Many seemed concerned that transgender people are being put in distressing and difficult situations in medical settings and also seemed dubious that health care for transgender people would improve without a complete overhaul,” Dr. Alpert said.
In an interview, Boston University assistant professor of medicine C. Streed Jr., MD, MPH, who studies gender and health, praised the study. He said it plays an early role in revealing the problems faced by transgender people in the health system.
“We do not fully know the experience of transgender persons accessing care in various contexts, especially in specialty care such as oncology, pulmonology, nephrology, etc.” Dr. Streed said. “We do not know how they identify specialists who are welcoming, compassionate, and competent in care for transgender persons.”
The results aren’t surprising, Dr. Streed said, “given the lack of training in medical school, residency, and fellowship specific to the unique needs of transgender persons.”
How can clinicians improve interactions with transgender people?
What can clinicians do to help transgender patients feel comfortable? Dr. Alpert suggested they “ask [only] for medically relevant information and to explain to patients why it is medically relevant.”
“This is important because transgender people are often weighing the risks and benefits of disclosing information that could be used to stigmatize them,” Dr. Alpert said.
What if a clinician wants to create a personal connection with a patient by asking questions about their life? “If you as a clinician think it’s important to ask for nonmedical information to get to know a patient, explicitly clarify that your questions are optional and not medically relevant,” Dr. Alpert said. “That way patients have the ability to consent or not to questions that likely will not directly benefit their care.”
Dr. Streed offered a similar perspective. “Clinicians should only be asking questions of patients that will affect the care the patient is seeking and for which the clinician is trained to provide,” he said. “Having a transgender patient is not an opportunity for a clinician to satisfy their curiosity when it is not related to the care the patient is seeking or needs.”
More specifically, Dr. Streed offered an example: Clinicians should not be asking about a patient’s genitals if they are seeking care related to their asthma diagnosis.
Dr. Streed referred clinicians to resources from the American Medical Association and the Human Rights Campaign for guidelines on caring for transgender patients.
The study was funded by Conquer Cancer. The study authors and Dr. Streed have no relevant disclosures.
FROM ANNALS OF FAMILY MEDICINE
Gender-affirming surgeries nearly tripled between 2016 and 2019: Study
a new study published in JAMA Network Open found.
Breast and chest surgeries were the most common procedures performed, and the number of surgical procedures carried out increased with age. The researchers said that, in addition to legal shifts, the established safety of the surgeries and resulting increase in quality of life may also help explain the increase.
“The point of this is to raise awareness and to really document the patterns of care in the United States,” said Jason Wright, MD, an associate professor at Columbia University, New York. “We hope that people understand that these procedures are being performed more commonly and they’re out there.”
A study published in 2022 in JAMA Pediatrics found that the number of chest reconstruction surgeries among U.S. adolescents rose fourfold between 2016 and 2019.
The new study included data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. More than 48,000 patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified. Age ranges were grouped as 12-18 (7.7%), 19-30 (52.3%), and 31-40 (21.8%).
The number of gender-affirming procedures rose from 4,552 in 2016 to a peak of 13,011 in 2019. (A slight decline to 12,818 procedures in 2020 was attributed to the COVID-19 pandemic.) The surgeries were grouped into three categories: breast and chest procedures, which occurred in 56.6% of patients; genital reconstructive surgeries (35.1%), and other facial cosmetic procedures (13.9%).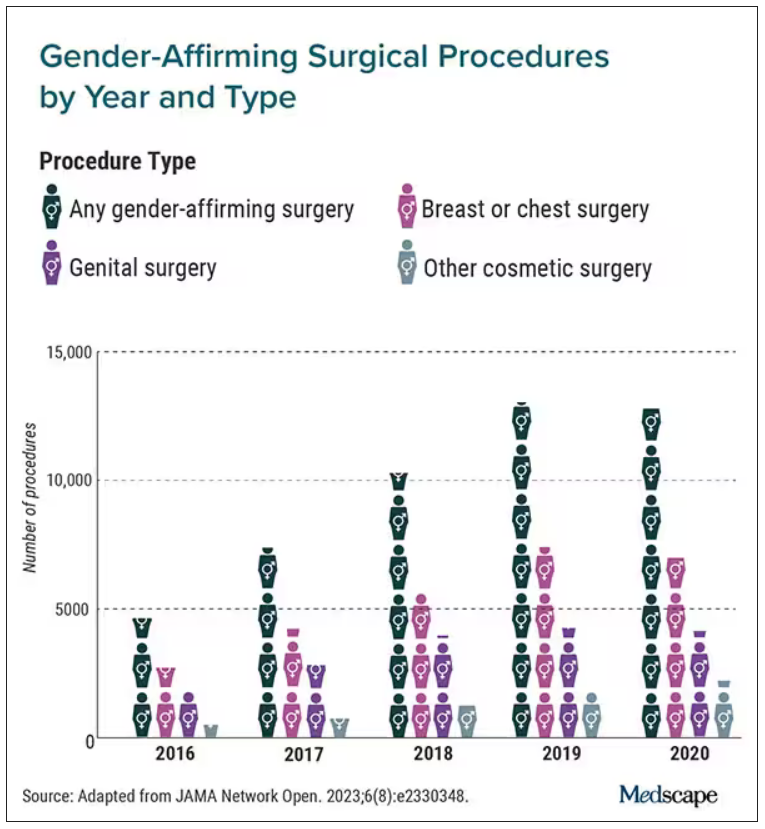
“We really wanted to try to make this as representative as we could,” Dr. Wright said. “I think this is really the best estimates that are available to date.”
Chest and breast procedures made up a higher percentage of surgeries in younger patients, while genital surgical procedures made up a higher percentage in older patients. For example, patients aged 19-30 made up 59.1% of breast or chest surgeries and 44.2% of genital surgeries. However, those aged 31-40 accounted for 26.2% of genital surgeries and 18.1% of breast or chest surgeries. For ages 41-50, the spread was more than double, accounting for 12.8% of genital surgeries and only 6.1% of breast or chest surgeries, according to the researchers.
Undocumented uptick
In addition to more inclusive health insurance, Dr. Wright said the increase in these procedures can also be attributed to studies showing their safety and the long-term association with high patient satisfaction.
Kevin Wang, MD, medical director of Providence–Swedish Health Services’ LGBTQIA+ program in Seattle, agreed that changes in health insurance coverage for gender-affirming surgery likely account in part for their increase. But he added that more clinicians are performing these procedures.
He said gender-affirming surgeries improve quality of life for the people who undergo them. The American Academy of Pediatrics has said it would be conducting a thorough review of the effects of transgender care on youth. A 2018 policy statement from the group said transgender youth should “have access to comprehensive, gender-affirming, and developmentally appropriate health care that is provided in a safe and inclusive clinical space.”
Dr. Wright cited several limitations to his group’s study that may result in the undercapture of transgender individuals and gender-affirming surgery; in particular, while the study captured inpatient and ambulatory surgical procedures in large, nationwide datasets, a small number of the procedures could have been performed in other settings.
Guiding a patient through gender-affirming care and surgical procedures can be an arduous process, including understanding their goals, using hormone therapy, and making referrals to specialists. Dr. Wang said he works to maximize his patients’ physical, mental, and emotional health, and helps them understand the risks.
He cited the double standard of a cisgender woman wanting breast augmentation without justification, but someone who identifies as transgender has many more boxes to check – for example, seeing a behavior health specialist to demonstrate they understand the risks and securing a letter of support from their primary care physician to undergo a similar procedure.
“It’s just interesting how the transgender community has to jump through so many more barriers and hoops for affirming, lifesaving procedures where you have other people who are doing it for aesthetic purposes and do not require any type of authorization,” Dr. Wang said.
Dr. Wright said he hopes the findings call attention to the need for more professionals working in the gender-affirming care field.
“I think for the medical community, it’s important to raise the idea that these procedures are becoming more common,” Dr. Wright said. “We are going to need specialists who have expertise in transgender care and surgeons who have the ability to perform these operations. Hopefully, this sheds light on the resources that are going to be required to care for these patients going forward.”
Dr. Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
a new study published in JAMA Network Open found.
Breast and chest surgeries were the most common procedures performed, and the number of surgical procedures carried out increased with age. The researchers said that, in addition to legal shifts, the established safety of the surgeries and resulting increase in quality of life may also help explain the increase.
“The point of this is to raise awareness and to really document the patterns of care in the United States,” said Jason Wright, MD, an associate professor at Columbia University, New York. “We hope that people understand that these procedures are being performed more commonly and they’re out there.”
A study published in 2022 in JAMA Pediatrics found that the number of chest reconstruction surgeries among U.S. adolescents rose fourfold between 2016 and 2019.
The new study included data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. More than 48,000 patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified. Age ranges were grouped as 12-18 (7.7%), 19-30 (52.3%), and 31-40 (21.8%).
The number of gender-affirming procedures rose from 4,552 in 2016 to a peak of 13,011 in 2019. (A slight decline to 12,818 procedures in 2020 was attributed to the COVID-19 pandemic.) The surgeries were grouped into three categories: breast and chest procedures, which occurred in 56.6% of patients; genital reconstructive surgeries (35.1%), and other facial cosmetic procedures (13.9%).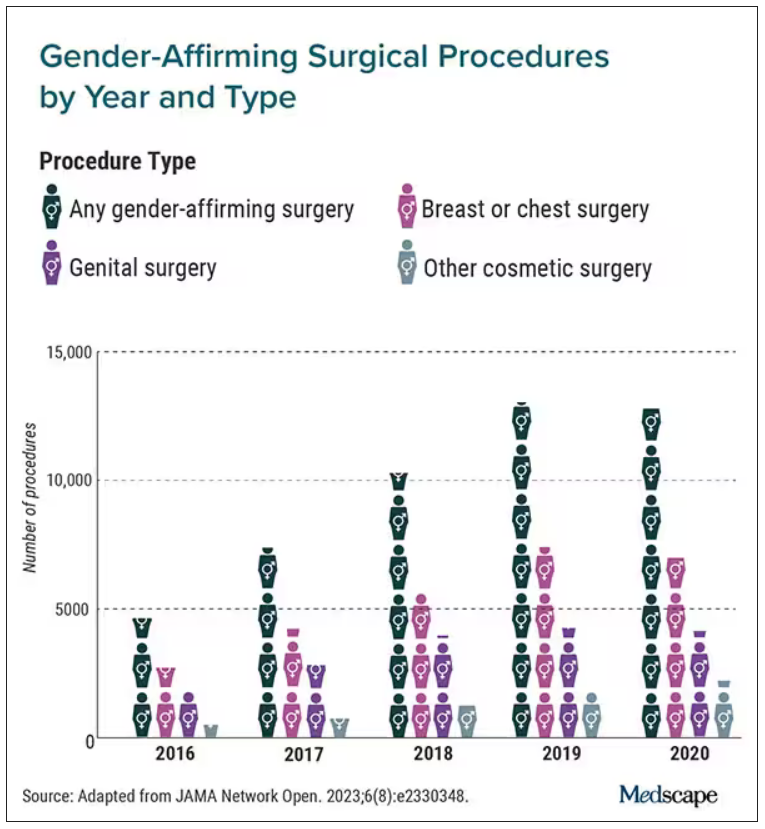
“We really wanted to try to make this as representative as we could,” Dr. Wright said. “I think this is really the best estimates that are available to date.”
Chest and breast procedures made up a higher percentage of surgeries in younger patients, while genital surgical procedures made up a higher percentage in older patients. For example, patients aged 19-30 made up 59.1% of breast or chest surgeries and 44.2% of genital surgeries. However, those aged 31-40 accounted for 26.2% of genital surgeries and 18.1% of breast or chest surgeries. For ages 41-50, the spread was more than double, accounting for 12.8% of genital surgeries and only 6.1% of breast or chest surgeries, according to the researchers.
Undocumented uptick
In addition to more inclusive health insurance, Dr. Wright said the increase in these procedures can also be attributed to studies showing their safety and the long-term association with high patient satisfaction.
Kevin Wang, MD, medical director of Providence–Swedish Health Services’ LGBTQIA+ program in Seattle, agreed that changes in health insurance coverage for gender-affirming surgery likely account in part for their increase. But he added that more clinicians are performing these procedures.
He said gender-affirming surgeries improve quality of life for the people who undergo them. The American Academy of Pediatrics has said it would be conducting a thorough review of the effects of transgender care on youth. A 2018 policy statement from the group said transgender youth should “have access to comprehensive, gender-affirming, and developmentally appropriate health care that is provided in a safe and inclusive clinical space.”
Dr. Wright cited several limitations to his group’s study that may result in the undercapture of transgender individuals and gender-affirming surgery; in particular, while the study captured inpatient and ambulatory surgical procedures in large, nationwide datasets, a small number of the procedures could have been performed in other settings.
Guiding a patient through gender-affirming care and surgical procedures can be an arduous process, including understanding their goals, using hormone therapy, and making referrals to specialists. Dr. Wang said he works to maximize his patients’ physical, mental, and emotional health, and helps them understand the risks.
He cited the double standard of a cisgender woman wanting breast augmentation without justification, but someone who identifies as transgender has many more boxes to check – for example, seeing a behavior health specialist to demonstrate they understand the risks and securing a letter of support from their primary care physician to undergo a similar procedure.
“It’s just interesting how the transgender community has to jump through so many more barriers and hoops for affirming, lifesaving procedures where you have other people who are doing it for aesthetic purposes and do not require any type of authorization,” Dr. Wang said.
Dr. Wright said he hopes the findings call attention to the need for more professionals working in the gender-affirming care field.
“I think for the medical community, it’s important to raise the idea that these procedures are becoming more common,” Dr. Wright said. “We are going to need specialists who have expertise in transgender care and surgeons who have the ability to perform these operations. Hopefully, this sheds light on the resources that are going to be required to care for these patients going forward.”
Dr. Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
a new study published in JAMA Network Open found.
Breast and chest surgeries were the most common procedures performed, and the number of surgical procedures carried out increased with age. The researchers said that, in addition to legal shifts, the established safety of the surgeries and resulting increase in quality of life may also help explain the increase.
“The point of this is to raise awareness and to really document the patterns of care in the United States,” said Jason Wright, MD, an associate professor at Columbia University, New York. “We hope that people understand that these procedures are being performed more commonly and they’re out there.”
A study published in 2022 in JAMA Pediatrics found that the number of chest reconstruction surgeries among U.S. adolescents rose fourfold between 2016 and 2019.
The new study included data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. More than 48,000 patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified. Age ranges were grouped as 12-18 (7.7%), 19-30 (52.3%), and 31-40 (21.8%).
The number of gender-affirming procedures rose from 4,552 in 2016 to a peak of 13,011 in 2019. (A slight decline to 12,818 procedures in 2020 was attributed to the COVID-19 pandemic.) The surgeries were grouped into three categories: breast and chest procedures, which occurred in 56.6% of patients; genital reconstructive surgeries (35.1%), and other facial cosmetic procedures (13.9%).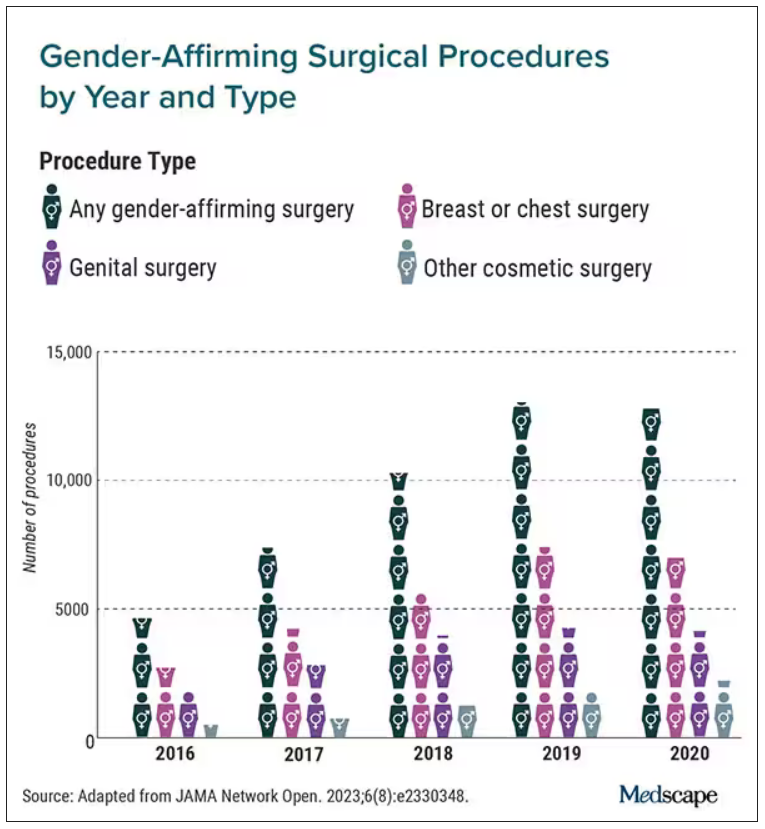
“We really wanted to try to make this as representative as we could,” Dr. Wright said. “I think this is really the best estimates that are available to date.”
Chest and breast procedures made up a higher percentage of surgeries in younger patients, while genital surgical procedures made up a higher percentage in older patients. For example, patients aged 19-30 made up 59.1% of breast or chest surgeries and 44.2% of genital surgeries. However, those aged 31-40 accounted for 26.2% of genital surgeries and 18.1% of breast or chest surgeries. For ages 41-50, the spread was more than double, accounting for 12.8% of genital surgeries and only 6.1% of breast or chest surgeries, according to the researchers.
Undocumented uptick
In addition to more inclusive health insurance, Dr. Wright said the increase in these procedures can also be attributed to studies showing their safety and the long-term association with high patient satisfaction.
Kevin Wang, MD, medical director of Providence–Swedish Health Services’ LGBTQIA+ program in Seattle, agreed that changes in health insurance coverage for gender-affirming surgery likely account in part for their increase. But he added that more clinicians are performing these procedures.
He said gender-affirming surgeries improve quality of life for the people who undergo them. The American Academy of Pediatrics has said it would be conducting a thorough review of the effects of transgender care on youth. A 2018 policy statement from the group said transgender youth should “have access to comprehensive, gender-affirming, and developmentally appropriate health care that is provided in a safe and inclusive clinical space.”
Dr. Wright cited several limitations to his group’s study that may result in the undercapture of transgender individuals and gender-affirming surgery; in particular, while the study captured inpatient and ambulatory surgical procedures in large, nationwide datasets, a small number of the procedures could have been performed in other settings.
Guiding a patient through gender-affirming care and surgical procedures can be an arduous process, including understanding their goals, using hormone therapy, and making referrals to specialists. Dr. Wang said he works to maximize his patients’ physical, mental, and emotional health, and helps them understand the risks.
He cited the double standard of a cisgender woman wanting breast augmentation without justification, but someone who identifies as transgender has many more boxes to check – for example, seeing a behavior health specialist to demonstrate they understand the risks and securing a letter of support from their primary care physician to undergo a similar procedure.
“It’s just interesting how the transgender community has to jump through so many more barriers and hoops for affirming, lifesaving procedures where you have other people who are doing it for aesthetic purposes and do not require any type of authorization,” Dr. Wang said.
Dr. Wright said he hopes the findings call attention to the need for more professionals working in the gender-affirming care field.
“I think for the medical community, it’s important to raise the idea that these procedures are becoming more common,” Dr. Wright said. “We are going to need specialists who have expertise in transgender care and surgeons who have the ability to perform these operations. Hopefully, this sheds light on the resources that are going to be required to care for these patients going forward.”
Dr. Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Gender-affirming care: The role of the pediatrician in a changing landscape
As the political targeting of transgender youth and families continues to play out on the national stage, it is more important than ever for pediatricians and other primary care providers to support this vulnerable population by defending the recommendations and guidelines of reputable medical organizations based in science and to show grace and humility in caring for their patients.
Guidelines and resources
All leading medical groups in the United States with statements or policies related to gender-affirming care (including the American Medical Association, the American Academy of Pediatrics, the Society for Adolescent Health and Medicine, the Pediatric Endocrine Society, the American Academy of Child and Adolescent Psychiatry, and many more) recognize that this care is medically necessary and that exclusions for gender-related services are harmful to patients and their families. As pediatricians, families and youth rely on our expertise and guidance related to childhood and adolescent development, including the development of gender identity and ways to create safe and supportive environments needed for youth to reach their full potential.1
While pediatricians are experts in youth development, some may have had limited access to training specific to LGBTQ+ identity development and interventions related to gender-affirming care. There are, however, readily accessible resources to help guide pediatricians in providing support and recommendations to families with concerns around gender or sexuality (See Resources). The American Academy of Pediatrics and Bright Futures recommend discussing the differences between assigned sex at birth and gender identity development with parents of those younger than 12 months of age as well as beginning to discuss and explore gender identity with all youth beginning at 4-5 years of age. Beginning at 8 years of age, pediatricians are also recommended to assess for a patient’s understanding and feelings toward emerging puberty to identify any potential concerns for gender dysphoria.2 If concerns or questions emerge from screening, the family can then be referred to a gender-affirming care specialist for more support.
Gender dysphoria and gender-affirming care
Gender dysphoria may present in different ways and at different times for each patient. Some patients may present early in childhood with gender-diverse behaviors or the assertion of a gender identity different than their assigned sex at birth. However, the most commonly seen presentation is just prior to or during puberty, when one’s physical body starts to change in ways that are not consistent with their gender identity. Many patients report distress around gender before this time, but the distress that comes with the physical changes of puberty often prompts patients to reach out to parents, friends, and/or medical providers for help. Other than youth specifically disclosing their gender identity, as with any life stressors, gender dysphoria may initially present with a decline in school or social functioning, increased mood irritability, depression, or anxiety.3
The goal of support prior to puberty is for youth to grow and thrive as any other child and to not have gender dysphoria get in the way of normal development and social functioning.4 Some families will pursue social transition, the process of making changes within different areas of social interaction (such as name, pronouns, clothing, hairstyle, etc.) to decrease distress around gender. The decision of whether to pursue social transition is unique to each patient and family. The goal of this process is to allow youth to explore these changes in an effort to decrease the distress they experience in social interactions. Youth should be centered in this process and be the leader of any potential changes with parents and schools providing safe and supportive environments.5 Social transition has been shown to decrease rates of depression in gender-diverse youth to the same level as that of their cisgender peers.6
It is important to note that there are no recommended medical interventions for gender-affirming care before the time of puberty and, once a patient reaches Sexual Maturity Rating II (early puberty), the first potential treatment option is the reversible suppression of puberty using gonadotropin-releasing hormone (GnRH) analogues. The goal of this type of medication is to allow youth more time to explore their gender and avoid the permanent physical changes that occur during their endogenous puberty that can have a significant negative impact on their gender dysphoria and psychosocial functioning. Youth and their families can then later decide to discontinue the medication and go through their endogenous puberty or to proceed with gender-affirming hormone treatment.7
With the growing number of states who have or are attempting to ban gender-affirming care for youth, more patients and families will be left with no options for accessing this potentially life-saving care and support within their home state. Some families have already been forced to relocate to more supportive environments or to travel significant distances to receive medically necessary care.8 This summer, the American Academy of Pediatrics reaffirmed their current policy stating, “The AAP opposes any laws or regulations that discriminate against transgender and gender-diverse individuals, or that interfere in the doctor-patient relationship,” and they “support giving transgender adolescents access to the health care they need.”9
Pediatricians should continue to utilize existing resources for recommended routine screening and subsequent referral for patients or families with concerns around gender identity. When possible, connect patients and families in need of more supportive services around gender-affirming care to appropriate specialty providers. If providers are uncertain about the current legal climate in their state, it is recommended to consult with legal counsel if needed. As pediatricians, we must strive to uphold the tenets of medicine, follow expert recommendations and guidelines based on the best available evidence to provide comprehensive care to all patients, and continue to advocate for our patients and families.
Dr. Warus is an adolescent medicine physician who specializes in care for transgender and gender-nonconforming youth, and LGBTQ health for youth at Children’s Hospital of Los Angeles. He is assistant professor of pediatrics at University of Southern California, Los Angeles.
Resources
Bright Futures – Promoting healthy development of sexuality and gender identity (Implementation tip sheet).
Rafferty J. AAP Committee on Psychosocial Aspects of Child and Family Health, AAP Committee on Adolescence, AAP Section on Lesbian, Gay, Bisexual, and Transgender Health and Wellness. Ensuring comprehensive care and support for transgender and gender-diverse children and adolescents.
References
1. Rafferty J. AAP Committee on Psychosocial Aspects of Child and Family Health, AAP Committee on Adolescence, AAP Section on Lesbian, Gay, Bisexual, and Transgender Health and Wellness. Ensuring comprehensive care and support for transgender and gender-diverse children and adolescents.
2. Bright Futures – Promoting healthy development of sexuality and gender identity (Implementation tip sheet).
3. Shumer DE et al. Advances in the care of transgender children and adolescents.
4. Vance SR et al. Psychological and medical care of gender nonconforming youth.
5. Ehrensaft D et al. Prepubertal social gender transitions: What we know; what we can learn – A view from a gender affirmative lens.
6. Olson KR et al. Mental health of transgender children who are supported in their identities.
7. Olson J et al. Management of the transgender adolescent.
8. Rodgers A and Goldberg M. New State laws force families with trans kids to seek gender-affirming care elsewhere.
9. Wyckoff AS, ed. AAP reaffirms gender-affirming care policy, authorizes systematic review of evidence to guide update.
As the political targeting of transgender youth and families continues to play out on the national stage, it is more important than ever for pediatricians and other primary care providers to support this vulnerable population by defending the recommendations and guidelines of reputable medical organizations based in science and to show grace and humility in caring for their patients.
Guidelines and resources
All leading medical groups in the United States with statements or policies related to gender-affirming care (including the American Medical Association, the American Academy of Pediatrics, the Society for Adolescent Health and Medicine, the Pediatric Endocrine Society, the American Academy of Child and Adolescent Psychiatry, and many more) recognize that this care is medically necessary and that exclusions for gender-related services are harmful to patients and their families. As pediatricians, families and youth rely on our expertise and guidance related to childhood and adolescent development, including the development of gender identity and ways to create safe and supportive environments needed for youth to reach their full potential.1
While pediatricians are experts in youth development, some may have had limited access to training specific to LGBTQ+ identity development and interventions related to gender-affirming care. There are, however, readily accessible resources to help guide pediatricians in providing support and recommendations to families with concerns around gender or sexuality (See Resources). The American Academy of Pediatrics and Bright Futures recommend discussing the differences between assigned sex at birth and gender identity development with parents of those younger than 12 months of age as well as beginning to discuss and explore gender identity with all youth beginning at 4-5 years of age. Beginning at 8 years of age, pediatricians are also recommended to assess for a patient’s understanding and feelings toward emerging puberty to identify any potential concerns for gender dysphoria.2 If concerns or questions emerge from screening, the family can then be referred to a gender-affirming care specialist for more support.
Gender dysphoria and gender-affirming care
Gender dysphoria may present in different ways and at different times for each patient. Some patients may present early in childhood with gender-diverse behaviors or the assertion of a gender identity different than their assigned sex at birth. However, the most commonly seen presentation is just prior to or during puberty, when one’s physical body starts to change in ways that are not consistent with their gender identity. Many patients report distress around gender before this time, but the distress that comes with the physical changes of puberty often prompts patients to reach out to parents, friends, and/or medical providers for help. Other than youth specifically disclosing their gender identity, as with any life stressors, gender dysphoria may initially present with a decline in school or social functioning, increased mood irritability, depression, or anxiety.3
The goal of support prior to puberty is for youth to grow and thrive as any other child and to not have gender dysphoria get in the way of normal development and social functioning.4 Some families will pursue social transition, the process of making changes within different areas of social interaction (such as name, pronouns, clothing, hairstyle, etc.) to decrease distress around gender. The decision of whether to pursue social transition is unique to each patient and family. The goal of this process is to allow youth to explore these changes in an effort to decrease the distress they experience in social interactions. Youth should be centered in this process and be the leader of any potential changes with parents and schools providing safe and supportive environments.5 Social transition has been shown to decrease rates of depression in gender-diverse youth to the same level as that of their cisgender peers.6
It is important to note that there are no recommended medical interventions for gender-affirming care before the time of puberty and, once a patient reaches Sexual Maturity Rating II (early puberty), the first potential treatment option is the reversible suppression of puberty using gonadotropin-releasing hormone (GnRH) analogues. The goal of this type of medication is to allow youth more time to explore their gender and avoid the permanent physical changes that occur during their endogenous puberty that can have a significant negative impact on their gender dysphoria and psychosocial functioning. Youth and their families can then later decide to discontinue the medication and go through their endogenous puberty or to proceed with gender-affirming hormone treatment.7
With the growing number of states who have or are attempting to ban gender-affirming care for youth, more patients and families will be left with no options for accessing this potentially life-saving care and support within their home state. Some families have already been forced to relocate to more supportive environments or to travel significant distances to receive medically necessary care.8 This summer, the American Academy of Pediatrics reaffirmed their current policy stating, “The AAP opposes any laws or regulations that discriminate against transgender and gender-diverse individuals, or that interfere in the doctor-patient relationship,” and they “support giving transgender adolescents access to the health care they need.”9
Pediatricians should continue to utilize existing resources for recommended routine screening and subsequent referral for patients or families with concerns around gender identity. When possible, connect patients and families in need of more supportive services around gender-affirming care to appropriate specialty providers. If providers are uncertain about the current legal climate in their state, it is recommended to consult with legal counsel if needed. As pediatricians, we must strive to uphold the tenets of medicine, follow expert recommendations and guidelines based on the best available evidence to provide comprehensive care to all patients, and continue to advocate for our patients and families.
Dr. Warus is an adolescent medicine physician who specializes in care for transgender and gender-nonconforming youth, and LGBTQ health for youth at Children’s Hospital of Los Angeles. He is assistant professor of pediatrics at University of Southern California, Los Angeles.
Resources
Bright Futures – Promoting healthy development of sexuality and gender identity (Implementation tip sheet).
Rafferty J. AAP Committee on Psychosocial Aspects of Child and Family Health, AAP Committee on Adolescence, AAP Section on Lesbian, Gay, Bisexual, and Transgender Health and Wellness. Ensuring comprehensive care and support for transgender and gender-diverse children and adolescents.
References
1. Rafferty J. AAP Committee on Psychosocial Aspects of Child and Family Health, AAP Committee on Adolescence, AAP Section on Lesbian, Gay, Bisexual, and Transgender Health and Wellness. Ensuring comprehensive care and support for transgender and gender-diverse children and adolescents.
2. Bright Futures – Promoting healthy development of sexuality and gender identity (Implementation tip sheet).
3. Shumer DE et al. Advances in the care of transgender children and adolescents.
4. Vance SR et al. Psychological and medical care of gender nonconforming youth.
5. Ehrensaft D et al. Prepubertal social gender transitions: What we know; what we can learn – A view from a gender affirmative lens.
6. Olson KR et al. Mental health of transgender children who are supported in their identities.
7. Olson J et al. Management of the transgender adolescent.
8. Rodgers A and Goldberg M. New State laws force families with trans kids to seek gender-affirming care elsewhere.
9. Wyckoff AS, ed. AAP reaffirms gender-affirming care policy, authorizes systematic review of evidence to guide update.
As the political targeting of transgender youth and families continues to play out on the national stage, it is more important than ever for pediatricians and other primary care providers to support this vulnerable population by defending the recommendations and guidelines of reputable medical organizations based in science and to show grace and humility in caring for their patients.
Guidelines and resources
All leading medical groups in the United States with statements or policies related to gender-affirming care (including the American Medical Association, the American Academy of Pediatrics, the Society for Adolescent Health and Medicine, the Pediatric Endocrine Society, the American Academy of Child and Adolescent Psychiatry, and many more) recognize that this care is medically necessary and that exclusions for gender-related services are harmful to patients and their families. As pediatricians, families and youth rely on our expertise and guidance related to childhood and adolescent development, including the development of gender identity and ways to create safe and supportive environments needed for youth to reach their full potential.1
While pediatricians are experts in youth development, some may have had limited access to training specific to LGBTQ+ identity development and interventions related to gender-affirming care. There are, however, readily accessible resources to help guide pediatricians in providing support and recommendations to families with concerns around gender or sexuality (See Resources). The American Academy of Pediatrics and Bright Futures recommend discussing the differences between assigned sex at birth and gender identity development with parents of those younger than 12 months of age as well as beginning to discuss and explore gender identity with all youth beginning at 4-5 years of age. Beginning at 8 years of age, pediatricians are also recommended to assess for a patient’s understanding and feelings toward emerging puberty to identify any potential concerns for gender dysphoria.2 If concerns or questions emerge from screening, the family can then be referred to a gender-affirming care specialist for more support.
Gender dysphoria and gender-affirming care
Gender dysphoria may present in different ways and at different times for each patient. Some patients may present early in childhood with gender-diverse behaviors or the assertion of a gender identity different than their assigned sex at birth. However, the most commonly seen presentation is just prior to or during puberty, when one’s physical body starts to change in ways that are not consistent with their gender identity. Many patients report distress around gender before this time, but the distress that comes with the physical changes of puberty often prompts patients to reach out to parents, friends, and/or medical providers for help. Other than youth specifically disclosing their gender identity, as with any life stressors, gender dysphoria may initially present with a decline in school or social functioning, increased mood irritability, depression, or anxiety.3
The goal of support prior to puberty is for youth to grow and thrive as any other child and to not have gender dysphoria get in the way of normal development and social functioning.4 Some families will pursue social transition, the process of making changes within different areas of social interaction (such as name, pronouns, clothing, hairstyle, etc.) to decrease distress around gender. The decision of whether to pursue social transition is unique to each patient and family. The goal of this process is to allow youth to explore these changes in an effort to decrease the distress they experience in social interactions. Youth should be centered in this process and be the leader of any potential changes with parents and schools providing safe and supportive environments.5 Social transition has been shown to decrease rates of depression in gender-diverse youth to the same level as that of their cisgender peers.6
It is important to note that there are no recommended medical interventions for gender-affirming care before the time of puberty and, once a patient reaches Sexual Maturity Rating II (early puberty), the first potential treatment option is the reversible suppression of puberty using gonadotropin-releasing hormone (GnRH) analogues. The goal of this type of medication is to allow youth more time to explore their gender and avoid the permanent physical changes that occur during their endogenous puberty that can have a significant negative impact on their gender dysphoria and psychosocial functioning. Youth and their families can then later decide to discontinue the medication and go through their endogenous puberty or to proceed with gender-affirming hormone treatment.7
With the growing number of states who have or are attempting to ban gender-affirming care for youth, more patients and families will be left with no options for accessing this potentially life-saving care and support within their home state. Some families have already been forced to relocate to more supportive environments or to travel significant distances to receive medically necessary care.8 This summer, the American Academy of Pediatrics reaffirmed their current policy stating, “The AAP opposes any laws or regulations that discriminate against transgender and gender-diverse individuals, or that interfere in the doctor-patient relationship,” and they “support giving transgender adolescents access to the health care they need.”9
Pediatricians should continue to utilize existing resources for recommended routine screening and subsequent referral for patients or families with concerns around gender identity. When possible, connect patients and families in need of more supportive services around gender-affirming care to appropriate specialty providers. If providers are uncertain about the current legal climate in their state, it is recommended to consult with legal counsel if needed. As pediatricians, we must strive to uphold the tenets of medicine, follow expert recommendations and guidelines based on the best available evidence to provide comprehensive care to all patients, and continue to advocate for our patients and families.
Dr. Warus is an adolescent medicine physician who specializes in care for transgender and gender-nonconforming youth, and LGBTQ health for youth at Children’s Hospital of Los Angeles. He is assistant professor of pediatrics at University of Southern California, Los Angeles.
Resources
Bright Futures – Promoting healthy development of sexuality and gender identity (Implementation tip sheet).
Rafferty J. AAP Committee on Psychosocial Aspects of Child and Family Health, AAP Committee on Adolescence, AAP Section on Lesbian, Gay, Bisexual, and Transgender Health and Wellness. Ensuring comprehensive care and support for transgender and gender-diverse children and adolescents.
References
1. Rafferty J. AAP Committee on Psychosocial Aspects of Child and Family Health, AAP Committee on Adolescence, AAP Section on Lesbian, Gay, Bisexual, and Transgender Health and Wellness. Ensuring comprehensive care and support for transgender and gender-diverse children and adolescents.
2. Bright Futures – Promoting healthy development of sexuality and gender identity (Implementation tip sheet).
3. Shumer DE et al. Advances in the care of transgender children and adolescents.
4. Vance SR et al. Psychological and medical care of gender nonconforming youth.
5. Ehrensaft D et al. Prepubertal social gender transitions: What we know; what we can learn – A view from a gender affirmative lens.
6. Olson KR et al. Mental health of transgender children who are supported in their identities.
7. Olson J et al. Management of the transgender adolescent.
8. Rodgers A and Goldberg M. New State laws force families with trans kids to seek gender-affirming care elsewhere.
9. Wyckoff AS, ed. AAP reaffirms gender-affirming care policy, authorizes systematic review of evidence to guide update.
Postpartum depression risk increased among sexual minority women
However, with sexual orientation highly underdocumented among women giving birth, understanding of the prevalence is lacking.
“To our knowledge, this cohort study was the first to examine perinatal depression screening and symptom endorsement among sexual minority women in a major medical center in the U.S.,” reported the authors of the study published in JAMA Psychiatry.
The results “highlight the need for investigations that include strategies for measuring sexual orientation because reliance on medical record review has substantial limitations with regard to the research questions and the validity of the data,” they noted.
Clinical guidelines recommend universal perinatal depression screening at obstetric and pediatric well-infant visits; however, there are significant gaps in data on the issue when it comes to sexual minority women.
To assess the prevalence of sexual minority people giving birth and compare perinatal depression screening rates and scores with those of heterosexual cisgender women, the authors conducted a review of medical records of 18,243 female patients who gave birth at a large, diverse, university-based medical center in Chicago between January and December of 2019.
Of the patients, 57.3% of whom were non-Hispanic White, 1.5% (280) had documentation of their sexual orientation, or sexual minority status.
The results show that those identified as being in sexual minorities, including lesbian, bisexual, queer, pansexual or asexual, were more likely than were heterosexual women to be more engaged in their care – they were more likely to have attended at least one prenatal visit (20.0% vs. 13.7%; P = .002) and at least one postpartum care visit (18.6% vs. 12.8%; P = .004), and more likely to be screened for depression during postpartum care (odds ratio, 1.77; P = .002).
Sexual minority women were also significantly more likely to screen positive for depression during the postpartum period than were heterosexual women (odds ratio, 2.38; P = .03); however, all other comparisons were not significantly different.
The finding regarding postpartum depression was consistent with recent literature, including a systematic review indicating that the stress of being in a sexual minority may be heightened during the postpartum period, the authors noted.
Reasons for the heightened stress may include “being perceived as inadequate parents, heteronormativity in perinatal care, such as intake forms asking for information about the child’s father, and lack of familial social support due to nonacceptance of the parents’ sexual orientation,” the researchers explained.
The rate of only 1.5% of people giving birth who identified as a sexual minority was significantly lower than expected, and much lower that the 17% reported in a recent nationally representative sample of women, first author Leiszle Lapping-Carr, PhD, director of the sexual and relationship health program, department of psychiatry and behavioral sciences, Northwestern University, Chicago, said in an interview.
“I did not expect a rate as low at 1.5%,” she said. “I anticipated it would not be as high as the 17%, but this was quite low. I think one primary reason is that women are not interested in disclosing their sexual orientation to their ob.gyns. if they don’t have to.”
Furthermore, Dr. Lapping-Carr said, “most medical systems do not have an easy way to document sexual orientation or gender identity, and even if it exists many physicians are unaware of the process.”
On a broader level, the lower rates may be indicative of a lack of acknowledgment of sexual minorities in the ob.gyn. setting, Dr. Lapping-Carr added.
“There is a heteronormative bias implicit in most obstetrics clinics, in which pregnant people are automatically gendered as women and assumed to be heterosexual, especially if they present with a male partner,” she said.
Because of those factors, even if a pregnant person discloses sexual identity, that person may request that it not be documented in the chart, she noted.
The higher rates of postpartum depression are consistent with higher rates of mental illness that are reported in general among sexual minority women, pregnant or not, including depression, anxiety, higher rates of substance abuse, stressful life events, and intimate partner violence, compared with heterosexual women, the authors noted.
Develop more supportive systems
To address postpartum depression among sexual minority women, Dr. Lapping-Carr suggested that clinicians generally start by avoiding language and behaviors that could suggest the potential bias that sexual minority patients can face.
“The main change [in treatment] that would likely be helpful for postpartum depression treatment is removing heteronormative language, e.g., not referring to partners as ‘fathers,’ ” she said.
Also, patients may benefit from “discussion of issues of relevance to people with sexual minority identities, such as the process of adoption for female non-birthing partners,” Dr. Lapping-Carr added.
“Starting to create spaces that are inclusive and welcoming for people of all identities will go a long way in increasing your patient’s trust in you,” she said.
While there is a lack of published data regarding increases in rates of sexual minority patients who are giving birth, societal trends suggest the rates may likely be on the rise, Dr. Lapping-Carr said.
“We do know that among adolescents, endorsement of sexual and gender minority identities is much higher than in previous generations, so it would follow that the proportion of birthing people with sexual and gender minority identities would also increase,” she said.
Commenting on the study, K. Ashley Brandt, DO, obstetrics section chief and medical director of Gender Affirming Surgery at Reading Hospital, in West Reading, Pa., noted that limitations include a lack of information about the bigger picture of patients’ risk factors.
“There is no documentation of other risks factors, including rates of depression in the antenatal period, which is higher in LGBTQ individuals and also a risk factor for postpartum depression,” Dr. Brandt told this news organization.
She agreed, however, that patients may be reluctant to report their sexual minority status on the record – but such issues are often addressed.
“I believe that obstetricians do ask this question far more than other providers, but it may not be easily captured in medical records, and patients may also hesitate to disclose sexual practices and sexual orientation due to fear of medical discrimination, which is still extremely prevalent,” Dr. Brandt said.
The study underscores, however, that “same-sex parents are a reality that providers will face,” she said. “They have unique social determinants for health that often go undocumented and unaddressed, which could contribute to higher rates of depression in the postpartum period.”
Factors that may be ignored or undocumented, such as sexual minorities’ religious beliefs or social and familial support, can play significant roles in health care outcomes, Dr. Brandt added.
“Providers need to find ways to better educate themselves about LGBTQ individuals and develop more supportive systems to ensure patients feel safe in disclosing their identities.”
The authors and Dr. Brandt had no disclosures to report.
However, with sexual orientation highly underdocumented among women giving birth, understanding of the prevalence is lacking.
“To our knowledge, this cohort study was the first to examine perinatal depression screening and symptom endorsement among sexual minority women in a major medical center in the U.S.,” reported the authors of the study published in JAMA Psychiatry.
The results “highlight the need for investigations that include strategies for measuring sexual orientation because reliance on medical record review has substantial limitations with regard to the research questions and the validity of the data,” they noted.
Clinical guidelines recommend universal perinatal depression screening at obstetric and pediatric well-infant visits; however, there are significant gaps in data on the issue when it comes to sexual minority women.
To assess the prevalence of sexual minority people giving birth and compare perinatal depression screening rates and scores with those of heterosexual cisgender women, the authors conducted a review of medical records of 18,243 female patients who gave birth at a large, diverse, university-based medical center in Chicago between January and December of 2019.
Of the patients, 57.3% of whom were non-Hispanic White, 1.5% (280) had documentation of their sexual orientation, or sexual minority status.
The results show that those identified as being in sexual minorities, including lesbian, bisexual, queer, pansexual or asexual, were more likely than were heterosexual women to be more engaged in their care – they were more likely to have attended at least one prenatal visit (20.0% vs. 13.7%; P = .002) and at least one postpartum care visit (18.6% vs. 12.8%; P = .004), and more likely to be screened for depression during postpartum care (odds ratio, 1.77; P = .002).
Sexual minority women were also significantly more likely to screen positive for depression during the postpartum period than were heterosexual women (odds ratio, 2.38; P = .03); however, all other comparisons were not significantly different.
The finding regarding postpartum depression was consistent with recent literature, including a systematic review indicating that the stress of being in a sexual minority may be heightened during the postpartum period, the authors noted.
Reasons for the heightened stress may include “being perceived as inadequate parents, heteronormativity in perinatal care, such as intake forms asking for information about the child’s father, and lack of familial social support due to nonacceptance of the parents’ sexual orientation,” the researchers explained.
The rate of only 1.5% of people giving birth who identified as a sexual minority was significantly lower than expected, and much lower that the 17% reported in a recent nationally representative sample of women, first author Leiszle Lapping-Carr, PhD, director of the sexual and relationship health program, department of psychiatry and behavioral sciences, Northwestern University, Chicago, said in an interview.
“I did not expect a rate as low at 1.5%,” she said. “I anticipated it would not be as high as the 17%, but this was quite low. I think one primary reason is that women are not interested in disclosing their sexual orientation to their ob.gyns. if they don’t have to.”
Furthermore, Dr. Lapping-Carr said, “most medical systems do not have an easy way to document sexual orientation or gender identity, and even if it exists many physicians are unaware of the process.”
On a broader level, the lower rates may be indicative of a lack of acknowledgment of sexual minorities in the ob.gyn. setting, Dr. Lapping-Carr added.
“There is a heteronormative bias implicit in most obstetrics clinics, in which pregnant people are automatically gendered as women and assumed to be heterosexual, especially if they present with a male partner,” she said.
Because of those factors, even if a pregnant person discloses sexual identity, that person may request that it not be documented in the chart, she noted.
The higher rates of postpartum depression are consistent with higher rates of mental illness that are reported in general among sexual minority women, pregnant or not, including depression, anxiety, higher rates of substance abuse, stressful life events, and intimate partner violence, compared with heterosexual women, the authors noted.
Develop more supportive systems
To address postpartum depression among sexual minority women, Dr. Lapping-Carr suggested that clinicians generally start by avoiding language and behaviors that could suggest the potential bias that sexual minority patients can face.
“The main change [in treatment] that would likely be helpful for postpartum depression treatment is removing heteronormative language, e.g., not referring to partners as ‘fathers,’ ” she said.
Also, patients may benefit from “discussion of issues of relevance to people with sexual minority identities, such as the process of adoption for female non-birthing partners,” Dr. Lapping-Carr added.
“Starting to create spaces that are inclusive and welcoming for people of all identities will go a long way in increasing your patient’s trust in you,” she said.
While there is a lack of published data regarding increases in rates of sexual minority patients who are giving birth, societal trends suggest the rates may likely be on the rise, Dr. Lapping-Carr said.
“We do know that among adolescents, endorsement of sexual and gender minority identities is much higher than in previous generations, so it would follow that the proportion of birthing people with sexual and gender minority identities would also increase,” she said.
Commenting on the study, K. Ashley Brandt, DO, obstetrics section chief and medical director of Gender Affirming Surgery at Reading Hospital, in West Reading, Pa., noted that limitations include a lack of information about the bigger picture of patients’ risk factors.
“There is no documentation of other risks factors, including rates of depression in the antenatal period, which is higher in LGBTQ individuals and also a risk factor for postpartum depression,” Dr. Brandt told this news organization.
She agreed, however, that patients may be reluctant to report their sexual minority status on the record – but such issues are often addressed.
“I believe that obstetricians do ask this question far more than other providers, but it may not be easily captured in medical records, and patients may also hesitate to disclose sexual practices and sexual orientation due to fear of medical discrimination, which is still extremely prevalent,” Dr. Brandt said.
The study underscores, however, that “same-sex parents are a reality that providers will face,” she said. “They have unique social determinants for health that often go undocumented and unaddressed, which could contribute to higher rates of depression in the postpartum period.”
Factors that may be ignored or undocumented, such as sexual minorities’ religious beliefs or social and familial support, can play significant roles in health care outcomes, Dr. Brandt added.
“Providers need to find ways to better educate themselves about LGBTQ individuals and develop more supportive systems to ensure patients feel safe in disclosing their identities.”
The authors and Dr. Brandt had no disclosures to report.
However, with sexual orientation highly underdocumented among women giving birth, understanding of the prevalence is lacking.
“To our knowledge, this cohort study was the first to examine perinatal depression screening and symptom endorsement among sexual minority women in a major medical center in the U.S.,” reported the authors of the study published in JAMA Psychiatry.
The results “highlight the need for investigations that include strategies for measuring sexual orientation because reliance on medical record review has substantial limitations with regard to the research questions and the validity of the data,” they noted.
Clinical guidelines recommend universal perinatal depression screening at obstetric and pediatric well-infant visits; however, there are significant gaps in data on the issue when it comes to sexual minority women.
To assess the prevalence of sexual minority people giving birth and compare perinatal depression screening rates and scores with those of heterosexual cisgender women, the authors conducted a review of medical records of 18,243 female patients who gave birth at a large, diverse, university-based medical center in Chicago between January and December of 2019.
Of the patients, 57.3% of whom were non-Hispanic White, 1.5% (280) had documentation of their sexual orientation, or sexual minority status.
The results show that those identified as being in sexual minorities, including lesbian, bisexual, queer, pansexual or asexual, were more likely than were heterosexual women to be more engaged in their care – they were more likely to have attended at least one prenatal visit (20.0% vs. 13.7%; P = .002) and at least one postpartum care visit (18.6% vs. 12.8%; P = .004), and more likely to be screened for depression during postpartum care (odds ratio, 1.77; P = .002).
Sexual minority women were also significantly more likely to screen positive for depression during the postpartum period than were heterosexual women (odds ratio, 2.38; P = .03); however, all other comparisons were not significantly different.
The finding regarding postpartum depression was consistent with recent literature, including a systematic review indicating that the stress of being in a sexual minority may be heightened during the postpartum period, the authors noted.
Reasons for the heightened stress may include “being perceived as inadequate parents, heteronormativity in perinatal care, such as intake forms asking for information about the child’s father, and lack of familial social support due to nonacceptance of the parents’ sexual orientation,” the researchers explained.
The rate of only 1.5% of people giving birth who identified as a sexual minority was significantly lower than expected, and much lower that the 17% reported in a recent nationally representative sample of women, first author Leiszle Lapping-Carr, PhD, director of the sexual and relationship health program, department of psychiatry and behavioral sciences, Northwestern University, Chicago, said in an interview.
“I did not expect a rate as low at 1.5%,” she said. “I anticipated it would not be as high as the 17%, but this was quite low. I think one primary reason is that women are not interested in disclosing their sexual orientation to their ob.gyns. if they don’t have to.”
Furthermore, Dr. Lapping-Carr said, “most medical systems do not have an easy way to document sexual orientation or gender identity, and even if it exists many physicians are unaware of the process.”
On a broader level, the lower rates may be indicative of a lack of acknowledgment of sexual minorities in the ob.gyn. setting, Dr. Lapping-Carr added.
“There is a heteronormative bias implicit in most obstetrics clinics, in which pregnant people are automatically gendered as women and assumed to be heterosexual, especially if they present with a male partner,” she said.
Because of those factors, even if a pregnant person discloses sexual identity, that person may request that it not be documented in the chart, she noted.
The higher rates of postpartum depression are consistent with higher rates of mental illness that are reported in general among sexual minority women, pregnant or not, including depression, anxiety, higher rates of substance abuse, stressful life events, and intimate partner violence, compared with heterosexual women, the authors noted.
Develop more supportive systems
To address postpartum depression among sexual minority women, Dr. Lapping-Carr suggested that clinicians generally start by avoiding language and behaviors that could suggest the potential bias that sexual minority patients can face.
“The main change [in treatment] that would likely be helpful for postpartum depression treatment is removing heteronormative language, e.g., not referring to partners as ‘fathers,’ ” she said.
Also, patients may benefit from “discussion of issues of relevance to people with sexual minority identities, such as the process of adoption for female non-birthing partners,” Dr. Lapping-Carr added.
“Starting to create spaces that are inclusive and welcoming for people of all identities will go a long way in increasing your patient’s trust in you,” she said.
While there is a lack of published data regarding increases in rates of sexual minority patients who are giving birth, societal trends suggest the rates may likely be on the rise, Dr. Lapping-Carr said.
“We do know that among adolescents, endorsement of sexual and gender minority identities is much higher than in previous generations, so it would follow that the proportion of birthing people with sexual and gender minority identities would also increase,” she said.
Commenting on the study, K. Ashley Brandt, DO, obstetrics section chief and medical director of Gender Affirming Surgery at Reading Hospital, in West Reading, Pa., noted that limitations include a lack of information about the bigger picture of patients’ risk factors.
“There is no documentation of other risks factors, including rates of depression in the antenatal period, which is higher in LGBTQ individuals and also a risk factor for postpartum depression,” Dr. Brandt told this news organization.
She agreed, however, that patients may be reluctant to report their sexual minority status on the record – but such issues are often addressed.
“I believe that obstetricians do ask this question far more than other providers, but it may not be easily captured in medical records, and patients may also hesitate to disclose sexual practices and sexual orientation due to fear of medical discrimination, which is still extremely prevalent,” Dr. Brandt said.
The study underscores, however, that “same-sex parents are a reality that providers will face,” she said. “They have unique social determinants for health that often go undocumented and unaddressed, which could contribute to higher rates of depression in the postpartum period.”
Factors that may be ignored or undocumented, such as sexual minorities’ religious beliefs or social and familial support, can play significant roles in health care outcomes, Dr. Brandt added.
“Providers need to find ways to better educate themselves about LGBTQ individuals and develop more supportive systems to ensure patients feel safe in disclosing their identities.”
The authors and Dr. Brandt had no disclosures to report.
FROM JAMA PSYCHIATRY
A primer on gender-affirming care for transgender youth
Over the past few years, there has been rampant misinformation regarding gender-affirming care for transgender youth. In particular, there has been confusion regarding how care is administered, and what types of care are considered at various stages of development. This primer will help you understand the developmental approach to supporting transgender youth.
While people generally think of medical and surgical aspects of gender-affirming care, other domains can be just as important. For example, a 2020 publication in The Lancet Public Health found that access to gender-congruent government identification documents was associated with lower odds of severe psychological distress and suicidality.1
Considerations for prepubertal children
The youngest developmental stage at which a young person may seek care regarding gender diversity is the prepubertal childhood stage. Guidelines set forth by The Endocrine Society and The World Professional Association for Transgender Health make it clear that no medical or surgical interventions are considered at this developmental stage.2,3 However, some young people may choose to pursue a “social transition.” Though this may sound like one thing, social transition can mean very different things for different people. It may include any combination of adopting a new name, pronouns, hairstyle, clothing, etc. Young people may also choose to pursue these various aspects of social transition in all settings, or sometimes only in some settings (for example, only at home if they don’t yet feel comfortable doing so at school). Research so far shows that prepubertal children who are allowed to socially transition have levels of anxiety and depression nearly indistinguishable from their cisgender peers.4 While some in the past have raised the question of whether a social transition increases a child’s degree of gender incongruence and thus their likelihood to “persist” in a transgender identity, research has suggested this is not the case, and that gender identity does not meaningfully differ before and after a social transition.5 It’s worth noting, that “desistance” of a young person’s transgender identity is generally not considered an ethical goal and that gender identity conversion efforts (that is, attempts to force transgender people to be cisgender) have been labeled unethical by the American Academy of Child & Adolescent Psychiatry.
Sadly, transgender children are victims of bullying at high rates in their schools and communities. Creating safe and affirming school and community environments can be some of the highest yield ways in which providers can support the mental health of gender-diverse youth at this stage. Gender Spectrum is an excellent nonprofit that provides resources to help families and communities with some of these nonmedical supports.
Early adolescence and pubertal suppression
The earliest gender-affirming medical intervention that may be considered is pubertal suppression. Pubertal suppression is achieved with gonadotropin-releasing hormone agonists. This class of medications is Food and Drug Administration approved in pediatrics for precocious puberty – a condition in which young people enter puberty much earlier than expected (sometimes as early as age 3). For that condition, the rationale is to delay puberty until the patient reaches a more developmentally normative age for puberty to begin. The rationale for pubertal suppression for adolescent gender dysphoria is somewhat similar – these medications allow for the temporary pausing of puberty, which can be particularly helpful for adolescents who are having severe negative psychological reactions to the ways in which their bodies are developing. The major advantage here is that pubertal suppression can be reversed (if the medication is stopped, endogenous puberty will proceed), whereas puberty itself cannot be easily reversed (resulting in adult transgender people needing surgery and other interventions later in life, if these changes can be fully undone at all). As with all medications, puberty blockers do carry known side effects, including falling behind on bone density (sex hormones are needed to mineralize bones). Because of this, it is generally recommended that adolescents have their bone density monitored during treatment, pursue avenues to improve bone health (for example, exercise), and either stop the puberty blocker to undergo endogenous puberty or start gender-affirming hormones (estrogen or testosterone) by around age 16.
It is also important to note that, under current guidelines, an adolescent must first undergo a comprehensive biopsychosocial mental health evaluation prior to starting pubertal suppression to ensure the clinical team has a comprehensive understanding of the adolescent’s mental health, that all potential gender supports that are needed are put into place, and that the adolescent and their guardians have a strong understanding of the medical intervention, its risks, side effects, and potential benefits. In addition, consent must be provided by parents or legal guardians, whereas adolescents themselves provide assent. Several studies have linked access to pubertal suppression, when indicated for gender dysphoria, to improved mental health outcomes (for example, van der Miesen and colleagues, Turban and colleagues, de Vries and colleagues, and Costa and colleagues).6-9
Later adolescence and gender-affirming hormones
Later in adolescence, transgender youth may be candidates for gender-affirming hormone treatment (for example, estrogen or testosterone) to induce pubertal changes that align with their gender identities. Once again, under current guidelines, a comprehensive mental health biopsychosocial evaluation must be conducted prior to initiation of these treatments. Part of this evaluation includes fertility counseling and consideration of fertility preservation (for example, oocyte or semen cryopreservation), given the potential for these medications to impact fertility. It also involves discussion of several of the physiologic changes from these medications that can be irreversible (for example, voice changes from testosterone are particularly difficult to reverse in the future). Tables of the physical changes from these medications, when they begin after starting, and when they generally reach their maximum are available in the Endocrine Society guidelines.2 The past endocrine society guidelines recommended not initiating gender-affirming hormones until age 16. The most recent guidelines note that there may be instances in which providers may consider starting them as early as age 13 (for example, to reduce risk of falling behind on bone density, or if a patient is having psychological distress related to their peers going through puberty while they are still in a prepubertal state). The latest World Professional Association for Transgender Health Standards of Care removed specific age cutoffs, highlighting the importance of a multidisciplinary team of mental health and hormone prescribing providers working together to understand the best course of action for a particular patient. As with pubertal suppression, several studies have linked access to gender-affirming hormones to improve mental health for adolescents with gender dysphoria (for example, Turban and colleagues, Chen and colleagues, de Vries and colleagues, Allen and colleagues, and Tordoff and colleagues).10-14
Gender-affirming surgeries
The vast majority of gender-affirming surgeries are not considered until adulthood. The most notable exception to this is masculinizing top surgery for trans masculine and nonbinary adolescents. As with all surgeries, this is a major decision, and requires agreement from a mental health provider, a medical provider, and the surgeon. Early research suggests such surgeries result in improved chest dysphoria and that regret rates appear to be low.15,16 While the latest World Professional Association for Transgender Health similarly removed strict age cutoffs for gender-affirming surgery, again noting the importance of individualized care, I suspect most will read this change in the context of the Endocrine Society guidelines and past WPATH guidelines that noted gender-affirming genital surgeries are not offered until adulthood (a rare exception perhaps being someone pursuing a gender-affirming vaginoplasty at say age 17 in the summer prior to college to avoid needing to take off from school for surgical recovery). Gender-affirming genital surgeries are generally much more involved surgeries with prolonged recovery times.
Given the substantial proportion of young people who openly identify as transgender,17 and the proliferation of misinformation, political rhetoric, and legislation that can impact gender-affirming care for adolescents with gender dysphoria,18 it is essential that providers have accurate, up-to-date information on what this care entails and how it is provided.
Dr. Turban is director of the gender psychiatry program at the University of California, San Francisco, where he is an assistant professor of child & adolescent psychiatry and affiliate faculty at the Philip R. Lee Institute for Health Policy Studies. He is on Twitter @jack_turban.
References
1. Malta M et al. Lancet Public Health. 2020 Apr;5(4):e178-9.
2. Hembree WC et al. J Clin Endocrinol Metab. 2017 Nov 1;102(11):3869-903.
3. Coleman E et al. Int J Transgend Health. 2022 Sep 6;23(Suppl 1):S1-259.
4. Durwood L et al. J Am Acad Child Adolesc Psychiatry. 2017 Feb;56(2):116-23.e2.
5. Rae JR et al. Psychol Sci. 2019 May;30(5):669-81.
6. van der Miesen AIR et al. J Adolesc Health. 2020 Jun;66(6):699-704.
7. Turban JL et al. Pediatrics. 2020 Feb;145(2):e20191725.
8. de Vries ALC et al. J Sex Med. 2011 Aug;8(8):2276-83.
9. Costa R et al. J Sex Med. 2015 Nov;12(11):2206-14.
10. Turban JL et al. PLoS One. 2022 Jan 12;17(1):e0261039.
11. Chen D et al. N Engl J Med. 2023;388:240-50.
12. de Vries ALC et al. Pediatrics. 2014 Oct;134(4):696-70.
13. Allen LR et al. Clin Pract Pediatr Psychol. 2019. doi: 10.1037/cpp0000288.
14. Tordoff DM et al. JAMA Netw Open. 2022 Feb 1;5(2):e220978.
15. Olson-Kennedy J et al. JAMA Pediatr. 2018;172(5):431-6.
16. Tang A et al. Ann Plast Surg. 2022 May;88(4 Suppl):S325-31
17. Johns MM et al. Morb Mortal Wkly Rep. 2019 Jan 25;68(3):67-71.
18. Turban JL et al. JAMA. 2021;325(22):2251-2.
Over the past few years, there has been rampant misinformation regarding gender-affirming care for transgender youth. In particular, there has been confusion regarding how care is administered, and what types of care are considered at various stages of development. This primer will help you understand the developmental approach to supporting transgender youth.
While people generally think of medical and surgical aspects of gender-affirming care, other domains can be just as important. For example, a 2020 publication in The Lancet Public Health found that access to gender-congruent government identification documents was associated with lower odds of severe psychological distress and suicidality.1
Considerations for prepubertal children
The youngest developmental stage at which a young person may seek care regarding gender diversity is the prepubertal childhood stage. Guidelines set forth by The Endocrine Society and The World Professional Association for Transgender Health make it clear that no medical or surgical interventions are considered at this developmental stage.2,3 However, some young people may choose to pursue a “social transition.” Though this may sound like one thing, social transition can mean very different things for different people. It may include any combination of adopting a new name, pronouns, hairstyle, clothing, etc. Young people may also choose to pursue these various aspects of social transition in all settings, or sometimes only in some settings (for example, only at home if they don’t yet feel comfortable doing so at school). Research so far shows that prepubertal children who are allowed to socially transition have levels of anxiety and depression nearly indistinguishable from their cisgender peers.4 While some in the past have raised the question of whether a social transition increases a child’s degree of gender incongruence and thus their likelihood to “persist” in a transgender identity, research has suggested this is not the case, and that gender identity does not meaningfully differ before and after a social transition.5 It’s worth noting, that “desistance” of a young person’s transgender identity is generally not considered an ethical goal and that gender identity conversion efforts (that is, attempts to force transgender people to be cisgender) have been labeled unethical by the American Academy of Child & Adolescent Psychiatry.
Sadly, transgender children are victims of bullying at high rates in their schools and communities. Creating safe and affirming school and community environments can be some of the highest yield ways in which providers can support the mental health of gender-diverse youth at this stage. Gender Spectrum is an excellent nonprofit that provides resources to help families and communities with some of these nonmedical supports.
Early adolescence and pubertal suppression
The earliest gender-affirming medical intervention that may be considered is pubertal suppression. Pubertal suppression is achieved with gonadotropin-releasing hormone agonists. This class of medications is Food and Drug Administration approved in pediatrics for precocious puberty – a condition in which young people enter puberty much earlier than expected (sometimes as early as age 3). For that condition, the rationale is to delay puberty until the patient reaches a more developmentally normative age for puberty to begin. The rationale for pubertal suppression for adolescent gender dysphoria is somewhat similar – these medications allow for the temporary pausing of puberty, which can be particularly helpful for adolescents who are having severe negative psychological reactions to the ways in which their bodies are developing. The major advantage here is that pubertal suppression can be reversed (if the medication is stopped, endogenous puberty will proceed), whereas puberty itself cannot be easily reversed (resulting in adult transgender people needing surgery and other interventions later in life, if these changes can be fully undone at all). As with all medications, puberty blockers do carry known side effects, including falling behind on bone density (sex hormones are needed to mineralize bones). Because of this, it is generally recommended that adolescents have their bone density monitored during treatment, pursue avenues to improve bone health (for example, exercise), and either stop the puberty blocker to undergo endogenous puberty or start gender-affirming hormones (estrogen or testosterone) by around age 16.
It is also important to note that, under current guidelines, an adolescent must first undergo a comprehensive biopsychosocial mental health evaluation prior to starting pubertal suppression to ensure the clinical team has a comprehensive understanding of the adolescent’s mental health, that all potential gender supports that are needed are put into place, and that the adolescent and their guardians have a strong understanding of the medical intervention, its risks, side effects, and potential benefits. In addition, consent must be provided by parents or legal guardians, whereas adolescents themselves provide assent. Several studies have linked access to pubertal suppression, when indicated for gender dysphoria, to improved mental health outcomes (for example, van der Miesen and colleagues, Turban and colleagues, de Vries and colleagues, and Costa and colleagues).6-9
Later adolescence and gender-affirming hormones
Later in adolescence, transgender youth may be candidates for gender-affirming hormone treatment (for example, estrogen or testosterone) to induce pubertal changes that align with their gender identities. Once again, under current guidelines, a comprehensive mental health biopsychosocial evaluation must be conducted prior to initiation of these treatments. Part of this evaluation includes fertility counseling and consideration of fertility preservation (for example, oocyte or semen cryopreservation), given the potential for these medications to impact fertility. It also involves discussion of several of the physiologic changes from these medications that can be irreversible (for example, voice changes from testosterone are particularly difficult to reverse in the future). Tables of the physical changes from these medications, when they begin after starting, and when they generally reach their maximum are available in the Endocrine Society guidelines.2 The past endocrine society guidelines recommended not initiating gender-affirming hormones until age 16. The most recent guidelines note that there may be instances in which providers may consider starting them as early as age 13 (for example, to reduce risk of falling behind on bone density, or if a patient is having psychological distress related to their peers going through puberty while they are still in a prepubertal state). The latest World Professional Association for Transgender Health Standards of Care removed specific age cutoffs, highlighting the importance of a multidisciplinary team of mental health and hormone prescribing providers working together to understand the best course of action for a particular patient. As with pubertal suppression, several studies have linked access to gender-affirming hormones to improve mental health for adolescents with gender dysphoria (for example, Turban and colleagues, Chen and colleagues, de Vries and colleagues, Allen and colleagues, and Tordoff and colleagues).10-14
Gender-affirming surgeries
The vast majority of gender-affirming surgeries are not considered until adulthood. The most notable exception to this is masculinizing top surgery for trans masculine and nonbinary adolescents. As with all surgeries, this is a major decision, and requires agreement from a mental health provider, a medical provider, and the surgeon. Early research suggests such surgeries result in improved chest dysphoria and that regret rates appear to be low.15,16 While the latest World Professional Association for Transgender Health similarly removed strict age cutoffs for gender-affirming surgery, again noting the importance of individualized care, I suspect most will read this change in the context of the Endocrine Society guidelines and past WPATH guidelines that noted gender-affirming genital surgeries are not offered until adulthood (a rare exception perhaps being someone pursuing a gender-affirming vaginoplasty at say age 17 in the summer prior to college to avoid needing to take off from school for surgical recovery). Gender-affirming genital surgeries are generally much more involved surgeries with prolonged recovery times.
Given the substantial proportion of young people who openly identify as transgender,17 and the proliferation of misinformation, political rhetoric, and legislation that can impact gender-affirming care for adolescents with gender dysphoria,18 it is essential that providers have accurate, up-to-date information on what this care entails and how it is provided.
Dr. Turban is director of the gender psychiatry program at the University of California, San Francisco, where he is an assistant professor of child & adolescent psychiatry and affiliate faculty at the Philip R. Lee Institute for Health Policy Studies. He is on Twitter @jack_turban.
References
1. Malta M et al. Lancet Public Health. 2020 Apr;5(4):e178-9.
2. Hembree WC et al. J Clin Endocrinol Metab. 2017 Nov 1;102(11):3869-903.
3. Coleman E et al. Int J Transgend Health. 2022 Sep 6;23(Suppl 1):S1-259.
4. Durwood L et al. J Am Acad Child Adolesc Psychiatry. 2017 Feb;56(2):116-23.e2.
5. Rae JR et al. Psychol Sci. 2019 May;30(5):669-81.
6. van der Miesen AIR et al. J Adolesc Health. 2020 Jun;66(6):699-704.
7. Turban JL et al. Pediatrics. 2020 Feb;145(2):e20191725.
8. de Vries ALC et al. J Sex Med. 2011 Aug;8(8):2276-83.
9. Costa R et al. J Sex Med. 2015 Nov;12(11):2206-14.
10. Turban JL et al. PLoS One. 2022 Jan 12;17(1):e0261039.
11. Chen D et al. N Engl J Med. 2023;388:240-50.
12. de Vries ALC et al. Pediatrics. 2014 Oct;134(4):696-70.
13. Allen LR et al. Clin Pract Pediatr Psychol. 2019. doi: 10.1037/cpp0000288.
14. Tordoff DM et al. JAMA Netw Open. 2022 Feb 1;5(2):e220978.
15. Olson-Kennedy J et al. JAMA Pediatr. 2018;172(5):431-6.
16. Tang A et al. Ann Plast Surg. 2022 May;88(4 Suppl):S325-31
17. Johns MM et al. Morb Mortal Wkly Rep. 2019 Jan 25;68(3):67-71.
18. Turban JL et al. JAMA. 2021;325(22):2251-2.
Over the past few years, there has been rampant misinformation regarding gender-affirming care for transgender youth. In particular, there has been confusion regarding how care is administered, and what types of care are considered at various stages of development. This primer will help you understand the developmental approach to supporting transgender youth.
While people generally think of medical and surgical aspects of gender-affirming care, other domains can be just as important. For example, a 2020 publication in The Lancet Public Health found that access to gender-congruent government identification documents was associated with lower odds of severe psychological distress and suicidality.1
Considerations for prepubertal children
The youngest developmental stage at which a young person may seek care regarding gender diversity is the prepubertal childhood stage. Guidelines set forth by The Endocrine Society and The World Professional Association for Transgender Health make it clear that no medical or surgical interventions are considered at this developmental stage.2,3 However, some young people may choose to pursue a “social transition.” Though this may sound like one thing, social transition can mean very different things for different people. It may include any combination of adopting a new name, pronouns, hairstyle, clothing, etc. Young people may also choose to pursue these various aspects of social transition in all settings, or sometimes only in some settings (for example, only at home if they don’t yet feel comfortable doing so at school). Research so far shows that prepubertal children who are allowed to socially transition have levels of anxiety and depression nearly indistinguishable from their cisgender peers.4 While some in the past have raised the question of whether a social transition increases a child’s degree of gender incongruence and thus their likelihood to “persist” in a transgender identity, research has suggested this is not the case, and that gender identity does not meaningfully differ before and after a social transition.5 It’s worth noting, that “desistance” of a young person’s transgender identity is generally not considered an ethical goal and that gender identity conversion efforts (that is, attempts to force transgender people to be cisgender) have been labeled unethical by the American Academy of Child & Adolescent Psychiatry.
Sadly, transgender children are victims of bullying at high rates in their schools and communities. Creating safe and affirming school and community environments can be some of the highest yield ways in which providers can support the mental health of gender-diverse youth at this stage. Gender Spectrum is an excellent nonprofit that provides resources to help families and communities with some of these nonmedical supports.
Early adolescence and pubertal suppression
The earliest gender-affirming medical intervention that may be considered is pubertal suppression. Pubertal suppression is achieved with gonadotropin-releasing hormone agonists. This class of medications is Food and Drug Administration approved in pediatrics for precocious puberty – a condition in which young people enter puberty much earlier than expected (sometimes as early as age 3). For that condition, the rationale is to delay puberty until the patient reaches a more developmentally normative age for puberty to begin. The rationale for pubertal suppression for adolescent gender dysphoria is somewhat similar – these medications allow for the temporary pausing of puberty, which can be particularly helpful for adolescents who are having severe negative psychological reactions to the ways in which their bodies are developing. The major advantage here is that pubertal suppression can be reversed (if the medication is stopped, endogenous puberty will proceed), whereas puberty itself cannot be easily reversed (resulting in adult transgender people needing surgery and other interventions later in life, if these changes can be fully undone at all). As with all medications, puberty blockers do carry known side effects, including falling behind on bone density (sex hormones are needed to mineralize bones). Because of this, it is generally recommended that adolescents have their bone density monitored during treatment, pursue avenues to improve bone health (for example, exercise), and either stop the puberty blocker to undergo endogenous puberty or start gender-affirming hormones (estrogen or testosterone) by around age 16.
It is also important to note that, under current guidelines, an adolescent must first undergo a comprehensive biopsychosocial mental health evaluation prior to starting pubertal suppression to ensure the clinical team has a comprehensive understanding of the adolescent’s mental health, that all potential gender supports that are needed are put into place, and that the adolescent and their guardians have a strong understanding of the medical intervention, its risks, side effects, and potential benefits. In addition, consent must be provided by parents or legal guardians, whereas adolescents themselves provide assent. Several studies have linked access to pubertal suppression, when indicated for gender dysphoria, to improved mental health outcomes (for example, van der Miesen and colleagues, Turban and colleagues, de Vries and colleagues, and Costa and colleagues).6-9
Later adolescence and gender-affirming hormones
Later in adolescence, transgender youth may be candidates for gender-affirming hormone treatment (for example, estrogen or testosterone) to induce pubertal changes that align with their gender identities. Once again, under current guidelines, a comprehensive mental health biopsychosocial evaluation must be conducted prior to initiation of these treatments. Part of this evaluation includes fertility counseling and consideration of fertility preservation (for example, oocyte or semen cryopreservation), given the potential for these medications to impact fertility. It also involves discussion of several of the physiologic changes from these medications that can be irreversible (for example, voice changes from testosterone are particularly difficult to reverse in the future). Tables of the physical changes from these medications, when they begin after starting, and when they generally reach their maximum are available in the Endocrine Society guidelines.2 The past endocrine society guidelines recommended not initiating gender-affirming hormones until age 16. The most recent guidelines note that there may be instances in which providers may consider starting them as early as age 13 (for example, to reduce risk of falling behind on bone density, or if a patient is having psychological distress related to their peers going through puberty while they are still in a prepubertal state). The latest World Professional Association for Transgender Health Standards of Care removed specific age cutoffs, highlighting the importance of a multidisciplinary team of mental health and hormone prescribing providers working together to understand the best course of action for a particular patient. As with pubertal suppression, several studies have linked access to gender-affirming hormones to improve mental health for adolescents with gender dysphoria (for example, Turban and colleagues, Chen and colleagues, de Vries and colleagues, Allen and colleagues, and Tordoff and colleagues).10-14
Gender-affirming surgeries
The vast majority of gender-affirming surgeries are not considered until adulthood. The most notable exception to this is masculinizing top surgery for trans masculine and nonbinary adolescents. As with all surgeries, this is a major decision, and requires agreement from a mental health provider, a medical provider, and the surgeon. Early research suggests such surgeries result in improved chest dysphoria and that regret rates appear to be low.15,16 While the latest World Professional Association for Transgender Health similarly removed strict age cutoffs for gender-affirming surgery, again noting the importance of individualized care, I suspect most will read this change in the context of the Endocrine Society guidelines and past WPATH guidelines that noted gender-affirming genital surgeries are not offered until adulthood (a rare exception perhaps being someone pursuing a gender-affirming vaginoplasty at say age 17 in the summer prior to college to avoid needing to take off from school for surgical recovery). Gender-affirming genital surgeries are generally much more involved surgeries with prolonged recovery times.
Given the substantial proportion of young people who openly identify as transgender,17 and the proliferation of misinformation, political rhetoric, and legislation that can impact gender-affirming care for adolescents with gender dysphoria,18 it is essential that providers have accurate, up-to-date information on what this care entails and how it is provided.
Dr. Turban is director of the gender psychiatry program at the University of California, San Francisco, where he is an assistant professor of child & adolescent psychiatry and affiliate faculty at the Philip R. Lee Institute for Health Policy Studies. He is on Twitter @jack_turban.
References
1. Malta M et al. Lancet Public Health. 2020 Apr;5(4):e178-9.
2. Hembree WC et al. J Clin Endocrinol Metab. 2017 Nov 1;102(11):3869-903.
3. Coleman E et al. Int J Transgend Health. 2022 Sep 6;23(Suppl 1):S1-259.
4. Durwood L et al. J Am Acad Child Adolesc Psychiatry. 2017 Feb;56(2):116-23.e2.
5. Rae JR et al. Psychol Sci. 2019 May;30(5):669-81.
6. van der Miesen AIR et al. J Adolesc Health. 2020 Jun;66(6):699-704.
7. Turban JL et al. Pediatrics. 2020 Feb;145(2):e20191725.
8. de Vries ALC et al. J Sex Med. 2011 Aug;8(8):2276-83.
9. Costa R et al. J Sex Med. 2015 Nov;12(11):2206-14.
10. Turban JL et al. PLoS One. 2022 Jan 12;17(1):e0261039.
11. Chen D et al. N Engl J Med. 2023;388:240-50.
12. de Vries ALC et al. Pediatrics. 2014 Oct;134(4):696-70.
13. Allen LR et al. Clin Pract Pediatr Psychol. 2019. doi: 10.1037/cpp0000288.
14. Tordoff DM et al. JAMA Netw Open. 2022 Feb 1;5(2):e220978.
15. Olson-Kennedy J et al. JAMA Pediatr. 2018;172(5):431-6.
16. Tang A et al. Ann Plast Surg. 2022 May;88(4 Suppl):S325-31
17. Johns MM et al. Morb Mortal Wkly Rep. 2019 Jan 25;68(3):67-71.
18. Turban JL et al. JAMA. 2021;325(22):2251-2.
Updates on pregnancy outcomes in transgender men
Despite increased societal gains, transgender individuals are still a medically and socially underserved group. The historic rise of antitransgender legislation and the overturning of Roe v. Wade, further compound existing health care disparities, particularly in the realm of contraception and pregnancy. Obstetrician-gynecologists and midwives are typically first-line providers when discussing family planning and fertility options for all patients assigned female at birth. Unfortunately,
Only individuals who are assigned female at birth and have a uterus are capable of pregnancy. This can include both cisgender women and nonbinary/transgender men. However, societal and medical institutions are struggling with this shift in perspective from a traditionally gendered role to a more inclusive one. Obstetrician-gynecologists and midwives can serve to bridge this gap between these patients and societal misconceptions surrounding transgender men who desire and experience pregnancy.
Providers need to remember that many transmasculine individuals will still retain their uterus and are therefore capable of getting pregnant. While testosterone causes amenorrhea, if patients are engaging in penile-vaginal intercourse, conception is still possible. If a patient does not desire pregnancy, all contraceptive options available for cisgender women, which also include combined oral contraceptives, should be offered.
For patients seeking to become pregnant, testosterone must be discontinued. Testosterone is teratogenic; it can cause abnormal urogenital development in the female fetus and should be avoided even prior to conception.1,2 The timing of testosterone discontinuation is debatable. There are no well-established guidelines dictating how early pregnancy can be attempted after cessation of testosterone, but typically if menses has resumed, the teratogenic effects of testosterone are less likely.
For amenorrheic patients on testosterone, menses will occur, on average, 3-6 months after testosterone is stopped. Of note, the longer that testosterone has been suspended, the greater the likelihood of achieving pregnancy.3 In a study by Light et al., 72% of patients conceived within 6 months of attempting pregnancy, 80% resumed menses within 6 months of stopping testosterone, and 20% of individuals conceived while they were amenorrheic from testosterone.4
Psychosocial support is an essential part of pregnancy care in transgender men. For some patients, pregnancy can worsen gender dysphoria, whereas others are empowered by the experience. Insurance companies may also deny obstetric care services to transgender males who have already changed their gender marker from female to male on insurance policies.
Whether transmasculine individuals are at higher risk for pregnancy complications is largely unknown, although emerging research in this field has yielded interesting results. While testosterone can cause vaginal atrophy, it does not seem to increase a patient’s risk of vaginal lacerations or their ability to have a successful vaginal delivery. For transgender men with significant discomfort around their genitalia, an elective cesarean section may be appropriate.5
More recently, Stroumsa et al. conducted an analysis of all deliveries at a Michigan institution from 2014 to 2018. Patients with male gender at the time of delivery or with the diagnostic code of gender dysphoria were identified as transgender.6 The primary outcome of this study was severe parental morbidity (such as amniotic fluid embolism, acute myocardial infarction, eclampsia, etc.), with secondary outcomes investigating rates of cesarean delivery and preterm birth.
During this time period, the researchers identified 256 transgender patients and 1.3 million cisgender patients in their Medicaid database and 1,651 transgender patients and 1.5 million cisgender patients in the commercial database who had experienced a delivery.6 Compared with cisgender patients, transgender patients in the Medicaid database were younger, less likely to be white, and more likely to have a chronic condition.6 Compared with cisgender patients in the commercial database, transgender patients experienced higher rates of anxiety and depression.6 Both transgender and cisgender patients had similar rates of severe parental morbidity. Ironically, rates of cesarean delivery were lower, compared with cisgender patients, in both the Medicaid and commercial databases, with no differences observed between rates of preterm birth.6
While more research is needed on pregnancy in transgender men, this analysis is not only one of the largest to date, but it also challenges many misconceptions providers have regarding pregnancy outcomes. Even though transmasculine patients may require additional medical interventions to achieve pregnancy, such as assisted reproductive technology, or increased psychosocial support during the process, these initial studies are reassuring. Based on current evidence, these patients are not at greater risk for perinatal complications than their cisgender counterparts.
Despite these encouraging findings, there are still several challenges faced by transgender men when it comes to getting pregnant. For instance, they may have difficulty accessing fertility services because of financial constraints or experience a lack of awareness or prejudice from providers; they might also be subject to discrimination or stigma within health care settings. As front-line providers for obstetrical care, we must lead the way towards improving the care for pregnant transmasculine individuals.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Light A et al. Family planning and contraception use in transgender men. Contraception. 2018 Oct. doi: 10.1016/j.contraception.2018.06.006.
2. Krempasky C et al. Contraception across the transmasculine spectrum. Am J Obstet Gynecol. 2020 Feb. doi: 10.1016/j.ajog.2019.07.043.
3. Obedin-Maliver J, De Haan G. “Gynecologic care for transgender patients” in Ferrando C, ed., Comprehensive Care of the Transgender Patient. Philadelphia: Elsevier, 2019. 131-51.
4. Light AD et al. Transgender men who experienced pregnancy after female-to-male gender transitioning. Obstet Gynecol. 2014 Dec. doi: 10.1097/AOG.0000000000000540.
5. Brandt JS et al. Transgender men, pregnancy, and the “new” advanced paternal age: A review of the literature. Maturitas. 2019 Oct. doi: 10.1016/j.maturitas.2019.07.004.
6. Stroumsa D et al. Pregnancy outcomes in a U.S. cohort of transgender people. JAMA. 2023 Jun 6. doi: 10.1001/jama.2023.7688.
Despite increased societal gains, transgender individuals are still a medically and socially underserved group. The historic rise of antitransgender legislation and the overturning of Roe v. Wade, further compound existing health care disparities, particularly in the realm of contraception and pregnancy. Obstetrician-gynecologists and midwives are typically first-line providers when discussing family planning and fertility options for all patients assigned female at birth. Unfortunately,
Only individuals who are assigned female at birth and have a uterus are capable of pregnancy. This can include both cisgender women and nonbinary/transgender men. However, societal and medical institutions are struggling with this shift in perspective from a traditionally gendered role to a more inclusive one. Obstetrician-gynecologists and midwives can serve to bridge this gap between these patients and societal misconceptions surrounding transgender men who desire and experience pregnancy.
Providers need to remember that many transmasculine individuals will still retain their uterus and are therefore capable of getting pregnant. While testosterone causes amenorrhea, if patients are engaging in penile-vaginal intercourse, conception is still possible. If a patient does not desire pregnancy, all contraceptive options available for cisgender women, which also include combined oral contraceptives, should be offered.
For patients seeking to become pregnant, testosterone must be discontinued. Testosterone is teratogenic; it can cause abnormal urogenital development in the female fetus and should be avoided even prior to conception.1,2 The timing of testosterone discontinuation is debatable. There are no well-established guidelines dictating how early pregnancy can be attempted after cessation of testosterone, but typically if menses has resumed, the teratogenic effects of testosterone are less likely.
For amenorrheic patients on testosterone, menses will occur, on average, 3-6 months after testosterone is stopped. Of note, the longer that testosterone has been suspended, the greater the likelihood of achieving pregnancy.3 In a study by Light et al., 72% of patients conceived within 6 months of attempting pregnancy, 80% resumed menses within 6 months of stopping testosterone, and 20% of individuals conceived while they were amenorrheic from testosterone.4
Psychosocial support is an essential part of pregnancy care in transgender men. For some patients, pregnancy can worsen gender dysphoria, whereas others are empowered by the experience. Insurance companies may also deny obstetric care services to transgender males who have already changed their gender marker from female to male on insurance policies.
Whether transmasculine individuals are at higher risk for pregnancy complications is largely unknown, although emerging research in this field has yielded interesting results. While testosterone can cause vaginal atrophy, it does not seem to increase a patient’s risk of vaginal lacerations or their ability to have a successful vaginal delivery. For transgender men with significant discomfort around their genitalia, an elective cesarean section may be appropriate.5
More recently, Stroumsa et al. conducted an analysis of all deliveries at a Michigan institution from 2014 to 2018. Patients with male gender at the time of delivery or with the diagnostic code of gender dysphoria were identified as transgender.6 The primary outcome of this study was severe parental morbidity (such as amniotic fluid embolism, acute myocardial infarction, eclampsia, etc.), with secondary outcomes investigating rates of cesarean delivery and preterm birth.
During this time period, the researchers identified 256 transgender patients and 1.3 million cisgender patients in their Medicaid database and 1,651 transgender patients and 1.5 million cisgender patients in the commercial database who had experienced a delivery.6 Compared with cisgender patients, transgender patients in the Medicaid database were younger, less likely to be white, and more likely to have a chronic condition.6 Compared with cisgender patients in the commercial database, transgender patients experienced higher rates of anxiety and depression.6 Both transgender and cisgender patients had similar rates of severe parental morbidity. Ironically, rates of cesarean delivery were lower, compared with cisgender patients, in both the Medicaid and commercial databases, with no differences observed between rates of preterm birth.6
While more research is needed on pregnancy in transgender men, this analysis is not only one of the largest to date, but it also challenges many misconceptions providers have regarding pregnancy outcomes. Even though transmasculine patients may require additional medical interventions to achieve pregnancy, such as assisted reproductive technology, or increased psychosocial support during the process, these initial studies are reassuring. Based on current evidence, these patients are not at greater risk for perinatal complications than their cisgender counterparts.
Despite these encouraging findings, there are still several challenges faced by transgender men when it comes to getting pregnant. For instance, they may have difficulty accessing fertility services because of financial constraints or experience a lack of awareness or prejudice from providers; they might also be subject to discrimination or stigma within health care settings. As front-line providers for obstetrical care, we must lead the way towards improving the care for pregnant transmasculine individuals.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Light A et al. Family planning and contraception use in transgender men. Contraception. 2018 Oct. doi: 10.1016/j.contraception.2018.06.006.
2. Krempasky C et al. Contraception across the transmasculine spectrum. Am J Obstet Gynecol. 2020 Feb. doi: 10.1016/j.ajog.2019.07.043.
3. Obedin-Maliver J, De Haan G. “Gynecologic care for transgender patients” in Ferrando C, ed., Comprehensive Care of the Transgender Patient. Philadelphia: Elsevier, 2019. 131-51.
4. Light AD et al. Transgender men who experienced pregnancy after female-to-male gender transitioning. Obstet Gynecol. 2014 Dec. doi: 10.1097/AOG.0000000000000540.
5. Brandt JS et al. Transgender men, pregnancy, and the “new” advanced paternal age: A review of the literature. Maturitas. 2019 Oct. doi: 10.1016/j.maturitas.2019.07.004.
6. Stroumsa D et al. Pregnancy outcomes in a U.S. cohort of transgender people. JAMA. 2023 Jun 6. doi: 10.1001/jama.2023.7688.
Despite increased societal gains, transgender individuals are still a medically and socially underserved group. The historic rise of antitransgender legislation and the overturning of Roe v. Wade, further compound existing health care disparities, particularly in the realm of contraception and pregnancy. Obstetrician-gynecologists and midwives are typically first-line providers when discussing family planning and fertility options for all patients assigned female at birth. Unfortunately,
Only individuals who are assigned female at birth and have a uterus are capable of pregnancy. This can include both cisgender women and nonbinary/transgender men. However, societal and medical institutions are struggling with this shift in perspective from a traditionally gendered role to a more inclusive one. Obstetrician-gynecologists and midwives can serve to bridge this gap between these patients and societal misconceptions surrounding transgender men who desire and experience pregnancy.
Providers need to remember that many transmasculine individuals will still retain their uterus and are therefore capable of getting pregnant. While testosterone causes amenorrhea, if patients are engaging in penile-vaginal intercourse, conception is still possible. If a patient does not desire pregnancy, all contraceptive options available for cisgender women, which also include combined oral contraceptives, should be offered.
For patients seeking to become pregnant, testosterone must be discontinued. Testosterone is teratogenic; it can cause abnormal urogenital development in the female fetus and should be avoided even prior to conception.1,2 The timing of testosterone discontinuation is debatable. There are no well-established guidelines dictating how early pregnancy can be attempted after cessation of testosterone, but typically if menses has resumed, the teratogenic effects of testosterone are less likely.
For amenorrheic patients on testosterone, menses will occur, on average, 3-6 months after testosterone is stopped. Of note, the longer that testosterone has been suspended, the greater the likelihood of achieving pregnancy.3 In a study by Light et al., 72% of patients conceived within 6 months of attempting pregnancy, 80% resumed menses within 6 months of stopping testosterone, and 20% of individuals conceived while they were amenorrheic from testosterone.4
Psychosocial support is an essential part of pregnancy care in transgender men. For some patients, pregnancy can worsen gender dysphoria, whereas others are empowered by the experience. Insurance companies may also deny obstetric care services to transgender males who have already changed their gender marker from female to male on insurance policies.
Whether transmasculine individuals are at higher risk for pregnancy complications is largely unknown, although emerging research in this field has yielded interesting results. While testosterone can cause vaginal atrophy, it does not seem to increase a patient’s risk of vaginal lacerations or their ability to have a successful vaginal delivery. For transgender men with significant discomfort around their genitalia, an elective cesarean section may be appropriate.5
More recently, Stroumsa et al. conducted an analysis of all deliveries at a Michigan institution from 2014 to 2018. Patients with male gender at the time of delivery or with the diagnostic code of gender dysphoria were identified as transgender.6 The primary outcome of this study was severe parental morbidity (such as amniotic fluid embolism, acute myocardial infarction, eclampsia, etc.), with secondary outcomes investigating rates of cesarean delivery and preterm birth.
During this time period, the researchers identified 256 transgender patients and 1.3 million cisgender patients in their Medicaid database and 1,651 transgender patients and 1.5 million cisgender patients in the commercial database who had experienced a delivery.6 Compared with cisgender patients, transgender patients in the Medicaid database were younger, less likely to be white, and more likely to have a chronic condition.6 Compared with cisgender patients in the commercial database, transgender patients experienced higher rates of anxiety and depression.6 Both transgender and cisgender patients had similar rates of severe parental morbidity. Ironically, rates of cesarean delivery were lower, compared with cisgender patients, in both the Medicaid and commercial databases, with no differences observed between rates of preterm birth.6
While more research is needed on pregnancy in transgender men, this analysis is not only one of the largest to date, but it also challenges many misconceptions providers have regarding pregnancy outcomes. Even though transmasculine patients may require additional medical interventions to achieve pregnancy, such as assisted reproductive technology, or increased psychosocial support during the process, these initial studies are reassuring. Based on current evidence, these patients are not at greater risk for perinatal complications than their cisgender counterparts.
Despite these encouraging findings, there are still several challenges faced by transgender men when it comes to getting pregnant. For instance, they may have difficulty accessing fertility services because of financial constraints or experience a lack of awareness or prejudice from providers; they might also be subject to discrimination or stigma within health care settings. As front-line providers for obstetrical care, we must lead the way towards improving the care for pregnant transmasculine individuals.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Light A et al. Family planning and contraception use in transgender men. Contraception. 2018 Oct. doi: 10.1016/j.contraception.2018.06.006.
2. Krempasky C et al. Contraception across the transmasculine spectrum. Am J Obstet Gynecol. 2020 Feb. doi: 10.1016/j.ajog.2019.07.043.
3. Obedin-Maliver J, De Haan G. “Gynecologic care for transgender patients” in Ferrando C, ed., Comprehensive Care of the Transgender Patient. Philadelphia: Elsevier, 2019. 131-51.
4. Light AD et al. Transgender men who experienced pregnancy after female-to-male gender transitioning. Obstet Gynecol. 2014 Dec. doi: 10.1097/AOG.0000000000000540.
5. Brandt JS et al. Transgender men, pregnancy, and the “new” advanced paternal age: A review of the literature. Maturitas. 2019 Oct. doi: 10.1016/j.maturitas.2019.07.004.
6. Stroumsa D et al. Pregnancy outcomes in a U.S. cohort of transgender people. JAMA. 2023 Jun 6. doi: 10.1001/jama.2023.7688.
Gender-diverse teens face barriers to physical activity
WASHINGTON – in a poster presented at the Pediatric Academic Societies annual meeting. Other barriers included body dissatisfaction and discomfort or pain from binding or tucking, based on data from 160 individuals.
Previous studies suggest that gender-diverse teens have lower levels of physical activity than cisgender teens, but data on the specific barriers to physical activity reported by gender-diverse adolescents are lacking, according to Karishma Desai, BA, a medical student at Northwestern University, Chicago, and colleagues.
The researchers reviewed data from adolescents aged 13-18 years who identified as transgender or nonbinary and lived in the United States. Participants were recruited through flyers, wallet cards, email, and social media. They completed an online survey that included questions on preferred types of physical activity and potential barriers to physical activity. Major barriers were defined as items that “almost always” or “always” got in the way of physical activity.
Overall, 51% of the participants identified as female/transfeminine, 31% as male/transmasculine, 9% as genderqueer or agender, 8% as nonbinary, and 1% as unsure. A total of 86 participants were assigned male at birth, 73 were assigned female, and 1 was assigned intersex or other. Nearly all of the participants (96%) had begun social transition; approximately half (48%) reported using a chest binder, and 75% had been or were currently taking gender-affirming hormones.
Potential negative judgment from others was the top barrier to physical activity (cited by 39% of participants), followed by body dissatisfaction from gender dysphoria (38%) and discomfort with the available options for locker rooms or changing rooms (38%). Approximately one-third (36%) of respondents reported physical discomfort or pain from binding or tucking as a barrier to physical activity, and 34% cited discomfort with requirements for a physical activity uniform or athletic clothing at school. Other gender-diverse specific barriers to physical activity included bullying related to being transgender (31%) and the inability to participate in a group of choice because of gender identity (24%).
In addition, participants cited general barriers to physical activity including bullying related to weight (33%), dissatisfaction with weight or size (31%), and bullying in general or for reasons other than gender status (29%).
However, more than 50% of respondents said they were comfortable or very comfortable (4 or 5 on a 5-point Likert Scale) with physical activity in the settings of coed or all-gender teams (61%) or engaging in individual activities (71%). By contrast, 36% were comfortable or very comfortable with a team, group, or class that aligned with sex assignment at birth.
The majority of participants (81%) were comfortable or very comfortable with their homes or a private location as a setting for physical activity, 54% with a public space such as a park, and 43% with a school setting.
Increasing gender congruence was the biggest facilitator of physical activity, reported by 53% of participants, the researchers noted. Other facilitators of physical activity included increasing body satisfaction (43%), staying healthy to avoid long-term health problems in the future (43%), and staying healthy to prepare for gender-related surgery in the future (18%).
The study findings were limited by the use of self-reports and the use of a convenience sample, as well as the lack of data on race, the researchers noted. However, the results suggest that access to all-gender teams, standardizing physical activity clothing, and increasing inclusive facilities may promote greater physical activity participation by gender-diverse adolescents, and offering private or individual options may increase comfort with physical activity, they concluded.
Study provides teens’ perspectives
The current study is especially timely given the recent passage by the U.S. House of Representatives of the anti-trans sports bill preventing transgender women and girls from playing on sports teams “consistent with their gender identity,” said Margaret Thew, DNP, medical director of adolescent medicine at Children’s Wisconsin in Milwaukee, in an interview. Ms. Thew was not involved in the current study.
“The House bill seeks to amend federal law to require that sex shall be recognized based solely on a person’s reproductive biology and genetics at birth, for the purpose of determining compliance with Title IX in athletics,” Ms. Thew said.
“Despite political responses to sports participation for transgender adolescents, we have not heard the perspective of the teens themselves,” she emphasized. “It is imperative for parents, coaches, and clinicians to hear the adolescents’ concerns so they can advocate for the students and provide the needed support.” In addition, Ms. Thew noted, “these concerns may also provide overdue changes to the required uniforms described for specific sports.”
Ms. Thew said she was surprised by the finding of transgender teens’ comfort with coed teams and individual activities, both of which may be opportunities to promote physical activity for transgender adolescents.
However, she added that she was not surprised by some of the results. “Many transgender adolescents experience the discomfort and further body dysmorphia of being put into gender-conforming attire such as swimwear, spandex shorts for female volleyball players, or field hockey skirts, for example.”
Although many schools are establishing safe, comfortable places for all adolescents to change clothing prior to physical education and sports participation, “resources are limited, and students and parents need to advocate within the school system,” Ms. Thew noted.
“We as a society, including athletic clothing makers, need to hear the testimony of transgender adolescents on the discomfort from body modifications to better support and innovate attire to meet their needs,” she added.
“The take-home message for clinicians is twofold,” said Ms. Thew. “Clinicians need to advocate for transgender patients to have the same opportunities as all teens when it comes to sports participation and physical activity. Also, clinicians need to ask all adolescents about their comfort in participating in physical activity both on club/school teams and independently,” she said. “If barriers are identified, clinicians need to work to support the adolescent with alternative activities/attire that will promote healthy physical activities for overall health.”
The current study also suggests that transgender adolescents who may have interest in, but discomfort with, physical activity should be redirected to coed or individual sports available in their communities, Ms. Thew added.
More research is needed on innovative sports attire that would improve comfort for transgender adolescents and thereby encourage physical activity, Ms. Thew told this news organization. More data also are needed on which sports transgender adolescents participate in and why, and how these activities might be promoted, she said.
Finally, more research will be needed to examine the impact of the recent House bills on physical activity for transgender youth, Ms. Thew said.
The study was supported by the Potocsnak Family Division of Adolescent and Young Adult Medicine at Ann and Robert H. Lurie’s Children’s Hospital of Chicago. The researchers had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose, but she serves on the Editorial Advisory Board of Pediatric News.
WASHINGTON – in a poster presented at the Pediatric Academic Societies annual meeting. Other barriers included body dissatisfaction and discomfort or pain from binding or tucking, based on data from 160 individuals.
Previous studies suggest that gender-diverse teens have lower levels of physical activity than cisgender teens, but data on the specific barriers to physical activity reported by gender-diverse adolescents are lacking, according to Karishma Desai, BA, a medical student at Northwestern University, Chicago, and colleagues.
The researchers reviewed data from adolescents aged 13-18 years who identified as transgender or nonbinary and lived in the United States. Participants were recruited through flyers, wallet cards, email, and social media. They completed an online survey that included questions on preferred types of physical activity and potential barriers to physical activity. Major barriers were defined as items that “almost always” or “always” got in the way of physical activity.
Overall, 51% of the participants identified as female/transfeminine, 31% as male/transmasculine, 9% as genderqueer or agender, 8% as nonbinary, and 1% as unsure. A total of 86 participants were assigned male at birth, 73 were assigned female, and 1 was assigned intersex or other. Nearly all of the participants (96%) had begun social transition; approximately half (48%) reported using a chest binder, and 75% had been or were currently taking gender-affirming hormones.
Potential negative judgment from others was the top barrier to physical activity (cited by 39% of participants), followed by body dissatisfaction from gender dysphoria (38%) and discomfort with the available options for locker rooms or changing rooms (38%). Approximately one-third (36%) of respondents reported physical discomfort or pain from binding or tucking as a barrier to physical activity, and 34% cited discomfort with requirements for a physical activity uniform or athletic clothing at school. Other gender-diverse specific barriers to physical activity included bullying related to being transgender (31%) and the inability to participate in a group of choice because of gender identity (24%).
In addition, participants cited general barriers to physical activity including bullying related to weight (33%), dissatisfaction with weight or size (31%), and bullying in general or for reasons other than gender status (29%).
However, more than 50% of respondents said they were comfortable or very comfortable (4 or 5 on a 5-point Likert Scale) with physical activity in the settings of coed or all-gender teams (61%) or engaging in individual activities (71%). By contrast, 36% were comfortable or very comfortable with a team, group, or class that aligned with sex assignment at birth.
The majority of participants (81%) were comfortable or very comfortable with their homes or a private location as a setting for physical activity, 54% with a public space such as a park, and 43% with a school setting.
Increasing gender congruence was the biggest facilitator of physical activity, reported by 53% of participants, the researchers noted. Other facilitators of physical activity included increasing body satisfaction (43%), staying healthy to avoid long-term health problems in the future (43%), and staying healthy to prepare for gender-related surgery in the future (18%).
The study findings were limited by the use of self-reports and the use of a convenience sample, as well as the lack of data on race, the researchers noted. However, the results suggest that access to all-gender teams, standardizing physical activity clothing, and increasing inclusive facilities may promote greater physical activity participation by gender-diverse adolescents, and offering private or individual options may increase comfort with physical activity, they concluded.
Study provides teens’ perspectives
The current study is especially timely given the recent passage by the U.S. House of Representatives of the anti-trans sports bill preventing transgender women and girls from playing on sports teams “consistent with their gender identity,” said Margaret Thew, DNP, medical director of adolescent medicine at Children’s Wisconsin in Milwaukee, in an interview. Ms. Thew was not involved in the current study.
“The House bill seeks to amend federal law to require that sex shall be recognized based solely on a person’s reproductive biology and genetics at birth, for the purpose of determining compliance with Title IX in athletics,” Ms. Thew said.
“Despite political responses to sports participation for transgender adolescents, we have not heard the perspective of the teens themselves,” she emphasized. “It is imperative for parents, coaches, and clinicians to hear the adolescents’ concerns so they can advocate for the students and provide the needed support.” In addition, Ms. Thew noted, “these concerns may also provide overdue changes to the required uniforms described for specific sports.”
Ms. Thew said she was surprised by the finding of transgender teens’ comfort with coed teams and individual activities, both of which may be opportunities to promote physical activity for transgender adolescents.
However, she added that she was not surprised by some of the results. “Many transgender adolescents experience the discomfort and further body dysmorphia of being put into gender-conforming attire such as swimwear, spandex shorts for female volleyball players, or field hockey skirts, for example.”
Although many schools are establishing safe, comfortable places for all adolescents to change clothing prior to physical education and sports participation, “resources are limited, and students and parents need to advocate within the school system,” Ms. Thew noted.
“We as a society, including athletic clothing makers, need to hear the testimony of transgender adolescents on the discomfort from body modifications to better support and innovate attire to meet their needs,” she added.
“The take-home message for clinicians is twofold,” said Ms. Thew. “Clinicians need to advocate for transgender patients to have the same opportunities as all teens when it comes to sports participation and physical activity. Also, clinicians need to ask all adolescents about their comfort in participating in physical activity both on club/school teams and independently,” she said. “If barriers are identified, clinicians need to work to support the adolescent with alternative activities/attire that will promote healthy physical activities for overall health.”
The current study also suggests that transgender adolescents who may have interest in, but discomfort with, physical activity should be redirected to coed or individual sports available in their communities, Ms. Thew added.
More research is needed on innovative sports attire that would improve comfort for transgender adolescents and thereby encourage physical activity, Ms. Thew told this news organization. More data also are needed on which sports transgender adolescents participate in and why, and how these activities might be promoted, she said.
Finally, more research will be needed to examine the impact of the recent House bills on physical activity for transgender youth, Ms. Thew said.
The study was supported by the Potocsnak Family Division of Adolescent and Young Adult Medicine at Ann and Robert H. Lurie’s Children’s Hospital of Chicago. The researchers had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose, but she serves on the Editorial Advisory Board of Pediatric News.
WASHINGTON – in a poster presented at the Pediatric Academic Societies annual meeting. Other barriers included body dissatisfaction and discomfort or pain from binding or tucking, based on data from 160 individuals.
Previous studies suggest that gender-diverse teens have lower levels of physical activity than cisgender teens, but data on the specific barriers to physical activity reported by gender-diverse adolescents are lacking, according to Karishma Desai, BA, a medical student at Northwestern University, Chicago, and colleagues.
The researchers reviewed data from adolescents aged 13-18 years who identified as transgender or nonbinary and lived in the United States. Participants were recruited through flyers, wallet cards, email, and social media. They completed an online survey that included questions on preferred types of physical activity and potential barriers to physical activity. Major barriers were defined as items that “almost always” or “always” got in the way of physical activity.
Overall, 51% of the participants identified as female/transfeminine, 31% as male/transmasculine, 9% as genderqueer or agender, 8% as nonbinary, and 1% as unsure. A total of 86 participants were assigned male at birth, 73 were assigned female, and 1 was assigned intersex or other. Nearly all of the participants (96%) had begun social transition; approximately half (48%) reported using a chest binder, and 75% had been or were currently taking gender-affirming hormones.
Potential negative judgment from others was the top barrier to physical activity (cited by 39% of participants), followed by body dissatisfaction from gender dysphoria (38%) and discomfort with the available options for locker rooms or changing rooms (38%). Approximately one-third (36%) of respondents reported physical discomfort or pain from binding or tucking as a barrier to physical activity, and 34% cited discomfort with requirements for a physical activity uniform or athletic clothing at school. Other gender-diverse specific barriers to physical activity included bullying related to being transgender (31%) and the inability to participate in a group of choice because of gender identity (24%).
In addition, participants cited general barriers to physical activity including bullying related to weight (33%), dissatisfaction with weight or size (31%), and bullying in general or for reasons other than gender status (29%).
However, more than 50% of respondents said they were comfortable or very comfortable (4 or 5 on a 5-point Likert Scale) with physical activity in the settings of coed or all-gender teams (61%) or engaging in individual activities (71%). By contrast, 36% were comfortable or very comfortable with a team, group, or class that aligned with sex assignment at birth.
The majority of participants (81%) were comfortable or very comfortable with their homes or a private location as a setting for physical activity, 54% with a public space such as a park, and 43% with a school setting.
Increasing gender congruence was the biggest facilitator of physical activity, reported by 53% of participants, the researchers noted. Other facilitators of physical activity included increasing body satisfaction (43%), staying healthy to avoid long-term health problems in the future (43%), and staying healthy to prepare for gender-related surgery in the future (18%).
The study findings were limited by the use of self-reports and the use of a convenience sample, as well as the lack of data on race, the researchers noted. However, the results suggest that access to all-gender teams, standardizing physical activity clothing, and increasing inclusive facilities may promote greater physical activity participation by gender-diverse adolescents, and offering private or individual options may increase comfort with physical activity, they concluded.
Study provides teens’ perspectives
The current study is especially timely given the recent passage by the U.S. House of Representatives of the anti-trans sports bill preventing transgender women and girls from playing on sports teams “consistent with their gender identity,” said Margaret Thew, DNP, medical director of adolescent medicine at Children’s Wisconsin in Milwaukee, in an interview. Ms. Thew was not involved in the current study.
“The House bill seeks to amend federal law to require that sex shall be recognized based solely on a person’s reproductive biology and genetics at birth, for the purpose of determining compliance with Title IX in athletics,” Ms. Thew said.
“Despite political responses to sports participation for transgender adolescents, we have not heard the perspective of the teens themselves,” she emphasized. “It is imperative for parents, coaches, and clinicians to hear the adolescents’ concerns so they can advocate for the students and provide the needed support.” In addition, Ms. Thew noted, “these concerns may also provide overdue changes to the required uniforms described for specific sports.”
Ms. Thew said she was surprised by the finding of transgender teens’ comfort with coed teams and individual activities, both of which may be opportunities to promote physical activity for transgender adolescents.
However, she added that she was not surprised by some of the results. “Many transgender adolescents experience the discomfort and further body dysmorphia of being put into gender-conforming attire such as swimwear, spandex shorts for female volleyball players, or field hockey skirts, for example.”
Although many schools are establishing safe, comfortable places for all adolescents to change clothing prior to physical education and sports participation, “resources are limited, and students and parents need to advocate within the school system,” Ms. Thew noted.
“We as a society, including athletic clothing makers, need to hear the testimony of transgender adolescents on the discomfort from body modifications to better support and innovate attire to meet their needs,” she added.
“The take-home message for clinicians is twofold,” said Ms. Thew. “Clinicians need to advocate for transgender patients to have the same opportunities as all teens when it comes to sports participation and physical activity. Also, clinicians need to ask all adolescents about their comfort in participating in physical activity both on club/school teams and independently,” she said. “If barriers are identified, clinicians need to work to support the adolescent with alternative activities/attire that will promote healthy physical activities for overall health.”
The current study also suggests that transgender adolescents who may have interest in, but discomfort with, physical activity should be redirected to coed or individual sports available in their communities, Ms. Thew added.
More research is needed on innovative sports attire that would improve comfort for transgender adolescents and thereby encourage physical activity, Ms. Thew told this news organization. More data also are needed on which sports transgender adolescents participate in and why, and how these activities might be promoted, she said.
Finally, more research will be needed to examine the impact of the recent House bills on physical activity for transgender youth, Ms. Thew said.
The study was supported by the Potocsnak Family Division of Adolescent and Young Adult Medicine at Ann and Robert H. Lurie’s Children’s Hospital of Chicago. The researchers had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose, but she serves on the Editorial Advisory Board of Pediatric News.
AT PAS 2023
LGBTQ+ Youth Consult Questions remain over use of sex hormone therapy
“They Paused Puberty but Is There a Cost?”
“Bone Health: Puberty Blockers Not Fully Reversible.”
Headlines such as these from major national news outlets have begun to cast doubt on one of the medications used in treating gender-diverse adolescents and young adults. GnRH agonists, such as leuprorelin and triptorelin, were first approved by the Food and Drug Administration in the 1980s and have been used since then for a variety of medical indications. In the decades since, these medications have been successfully used with a generally favorable side effect profile.
GnRH agonists and puberty
In the treatment of precocious puberty, GnRH agonists are often started prior to the age of 7, depending on the age at which the affected patient begins showing signs of central puberty. These include breast development, scrotal enlargement, and so on. GnRH agonists typically are continued until age 10-12, depending on the patient and an informed discussion with the patient’s parents about optimal outcomes.1 Therefore, it is not uncommon to see these medications used for anywhere from 1 to 4 years, depending on the age at which precocious puberty started.
GnRH agonists are used in two populations of transgender individuals. The first group is those youths who have just started their natal, or biological, puberty. The medication is not started until the patient has biochemical or physical exam evidence that puberty has started. The medication is then continued until hormones are started. This is usually 2-3 years on average, depending on the age at which the medication was started. This is essentially comparable with cisgender youths who have taken these medications for precocious puberty. The second population of individuals who use GnRH agonists is transgender women who are also on estrogen therapy. In these women, the GnRH agonist is used for androgen (testosterone) suppression.
Concerns over bone health
One of the main concerns recently expressed about long-term use of GnRH agonists is their effect on bone density. Adolescence is a critical time for bone mineral density (BMD) accrual and this is driven by sex hormones. When GnRH agonists are used to delay puberty in transgender adolescents, this then delays the maturation of the adult skeleton until the GnRH agonist is stopped (and natal puberty resumes) or cross-sex hormones are started. In a recent multicenter study2 looking at baseline BMD of transgender youth at the time of GnRH agonist initiation, 30% of those assigned male at birth and 13% of those assigned female at birth had low bone mineral density for age (defined as a BMD z score of <–2). For those with low BMD, their physical activity scores were significantly lower than those with normal BMD. Thus, these adolescents require close follow-up, just like their cisgender peers.
There are currently no long-term data on the risk of developing fractures or osteoporosis in those individuals who were treated with GnRH agonists and then went on to start cross-sex hormone therapy. Some studies suggest that there is a risk that BMD does not recover after being on cross-sex hormones,3 while another study suggested that transgender men recover their BMD after being on testosterone.4 It is still unclear in that study why transgender women did not recover their BMD or why they were low at baseline. Interestingly, a 2012 study5 from Brazil showed that there was no difference in BMD for cisgender girls who had been off their GnRH agonist therapy for at least 3 years, as compared with their age-matched controls who had never been on GnRH agonist therapy. These conflicting data highlight the importance of long-term follow-up, as well as the need to include age-matched, cisgender control subjects, to better understand if there is truly a difference in transgender individuals or if today’s adolescents, in general, have low BMD.
Lingering questions
In summary, the use of GnRH agonists in transgender adolescents remains controversial because of the potential long-term effects on bone mineral density. However, this risk must be balanced against the risks of allowing natal puberty to progress in certain transgender individuals with the development of undesired secondary sex characteristics. More longitudinal studies are needed to better understand the long-term risks of osteoporosis and fractures in those who have undergone GnRH agonist therapy as part of their gender-affirming medical care, as well as any clinical interventions that might help mitigate this risk.
Dr. Cooper is assistant professor of pediatrics at UT Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Harrington J et al. Treatment of precocious puberty. UpToDate. www.uptodate.com/contents/treatment-of-precocious-puberty.
2. Lee JY et al. J Endocr Soc. 2020;4(9):bvaa065. doi: 10.1210/jendso/bvaa065.
3. Klink D et al. J Clin Endocrinol Metab. 2015;100(2):E270-5. doi: 10.1210/jc.2014-2439.
4. Schagen SEE et al. J Clin Endocrinol Metab. 2020;105(12):e4252-e4263. doi: 10.1210/clinem/dgaa604.
5. Alessandri SB et al. Clinics (Sao Paulo). 2012;67(6):591-6. doi: 10.6061/clinics/2012(06)08.
“They Paused Puberty but Is There a Cost?”
“Bone Health: Puberty Blockers Not Fully Reversible.”
Headlines such as these from major national news outlets have begun to cast doubt on one of the medications used in treating gender-diverse adolescents and young adults. GnRH agonists, such as leuprorelin and triptorelin, were first approved by the Food and Drug Administration in the 1980s and have been used since then for a variety of medical indications. In the decades since, these medications have been successfully used with a generally favorable side effect profile.
GnRH agonists and puberty
In the treatment of precocious puberty, GnRH agonists are often started prior to the age of 7, depending on the age at which the affected patient begins showing signs of central puberty. These include breast development, scrotal enlargement, and so on. GnRH agonists typically are continued until age 10-12, depending on the patient and an informed discussion with the patient’s parents about optimal outcomes.1 Therefore, it is not uncommon to see these medications used for anywhere from 1 to 4 years, depending on the age at which precocious puberty started.
GnRH agonists are used in two populations of transgender individuals. The first group is those youths who have just started their natal, or biological, puberty. The medication is not started until the patient has biochemical or physical exam evidence that puberty has started. The medication is then continued until hormones are started. This is usually 2-3 years on average, depending on the age at which the medication was started. This is essentially comparable with cisgender youths who have taken these medications for precocious puberty. The second population of individuals who use GnRH agonists is transgender women who are also on estrogen therapy. In these women, the GnRH agonist is used for androgen (testosterone) suppression.
Concerns over bone health
One of the main concerns recently expressed about long-term use of GnRH agonists is their effect on bone density. Adolescence is a critical time for bone mineral density (BMD) accrual and this is driven by sex hormones. When GnRH agonists are used to delay puberty in transgender adolescents, this then delays the maturation of the adult skeleton until the GnRH agonist is stopped (and natal puberty resumes) or cross-sex hormones are started. In a recent multicenter study2 looking at baseline BMD of transgender youth at the time of GnRH agonist initiation, 30% of those assigned male at birth and 13% of those assigned female at birth had low bone mineral density for age (defined as a BMD z score of <–2). For those with low BMD, their physical activity scores were significantly lower than those with normal BMD. Thus, these adolescents require close follow-up, just like their cisgender peers.
There are currently no long-term data on the risk of developing fractures or osteoporosis in those individuals who were treated with GnRH agonists and then went on to start cross-sex hormone therapy. Some studies suggest that there is a risk that BMD does not recover after being on cross-sex hormones,3 while another study suggested that transgender men recover their BMD after being on testosterone.4 It is still unclear in that study why transgender women did not recover their BMD or why they were low at baseline. Interestingly, a 2012 study5 from Brazil showed that there was no difference in BMD for cisgender girls who had been off their GnRH agonist therapy for at least 3 years, as compared with their age-matched controls who had never been on GnRH agonist therapy. These conflicting data highlight the importance of long-term follow-up, as well as the need to include age-matched, cisgender control subjects, to better understand if there is truly a difference in transgender individuals or if today’s adolescents, in general, have low BMD.
Lingering questions
In summary, the use of GnRH agonists in transgender adolescents remains controversial because of the potential long-term effects on bone mineral density. However, this risk must be balanced against the risks of allowing natal puberty to progress in certain transgender individuals with the development of undesired secondary sex characteristics. More longitudinal studies are needed to better understand the long-term risks of osteoporosis and fractures in those who have undergone GnRH agonist therapy as part of their gender-affirming medical care, as well as any clinical interventions that might help mitigate this risk.
Dr. Cooper is assistant professor of pediatrics at UT Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Harrington J et al. Treatment of precocious puberty. UpToDate. www.uptodate.com/contents/treatment-of-precocious-puberty.
2. Lee JY et al. J Endocr Soc. 2020;4(9):bvaa065. doi: 10.1210/jendso/bvaa065.
3. Klink D et al. J Clin Endocrinol Metab. 2015;100(2):E270-5. doi: 10.1210/jc.2014-2439.
4. Schagen SEE et al. J Clin Endocrinol Metab. 2020;105(12):e4252-e4263. doi: 10.1210/clinem/dgaa604.
5. Alessandri SB et al. Clinics (Sao Paulo). 2012;67(6):591-6. doi: 10.6061/clinics/2012(06)08.
“They Paused Puberty but Is There a Cost?”
“Bone Health: Puberty Blockers Not Fully Reversible.”
Headlines such as these from major national news outlets have begun to cast doubt on one of the medications used in treating gender-diverse adolescents and young adults. GnRH agonists, such as leuprorelin and triptorelin, were first approved by the Food and Drug Administration in the 1980s and have been used since then for a variety of medical indications. In the decades since, these medications have been successfully used with a generally favorable side effect profile.
GnRH agonists and puberty
In the treatment of precocious puberty, GnRH agonists are often started prior to the age of 7, depending on the age at which the affected patient begins showing signs of central puberty. These include breast development, scrotal enlargement, and so on. GnRH agonists typically are continued until age 10-12, depending on the patient and an informed discussion with the patient’s parents about optimal outcomes.1 Therefore, it is not uncommon to see these medications used for anywhere from 1 to 4 years, depending on the age at which precocious puberty started.
GnRH agonists are used in two populations of transgender individuals. The first group is those youths who have just started their natal, or biological, puberty. The medication is not started until the patient has biochemical or physical exam evidence that puberty has started. The medication is then continued until hormones are started. This is usually 2-3 years on average, depending on the age at which the medication was started. This is essentially comparable with cisgender youths who have taken these medications for precocious puberty. The second population of individuals who use GnRH agonists is transgender women who are also on estrogen therapy. In these women, the GnRH agonist is used for androgen (testosterone) suppression.
Concerns over bone health
One of the main concerns recently expressed about long-term use of GnRH agonists is their effect on bone density. Adolescence is a critical time for bone mineral density (BMD) accrual and this is driven by sex hormones. When GnRH agonists are used to delay puberty in transgender adolescents, this then delays the maturation of the adult skeleton until the GnRH agonist is stopped (and natal puberty resumes) or cross-sex hormones are started. In a recent multicenter study2 looking at baseline BMD of transgender youth at the time of GnRH agonist initiation, 30% of those assigned male at birth and 13% of those assigned female at birth had low bone mineral density for age (defined as a BMD z score of <–2). For those with low BMD, their physical activity scores were significantly lower than those with normal BMD. Thus, these adolescents require close follow-up, just like their cisgender peers.
There are currently no long-term data on the risk of developing fractures or osteoporosis in those individuals who were treated with GnRH agonists and then went on to start cross-sex hormone therapy. Some studies suggest that there is a risk that BMD does not recover after being on cross-sex hormones,3 while another study suggested that transgender men recover their BMD after being on testosterone.4 It is still unclear in that study why transgender women did not recover their BMD or why they were low at baseline. Interestingly, a 2012 study5 from Brazil showed that there was no difference in BMD for cisgender girls who had been off their GnRH agonist therapy for at least 3 years, as compared with their age-matched controls who had never been on GnRH agonist therapy. These conflicting data highlight the importance of long-term follow-up, as well as the need to include age-matched, cisgender control subjects, to better understand if there is truly a difference in transgender individuals or if today’s adolescents, in general, have low BMD.
Lingering questions
In summary, the use of GnRH agonists in transgender adolescents remains controversial because of the potential long-term effects on bone mineral density. However, this risk must be balanced against the risks of allowing natal puberty to progress in certain transgender individuals with the development of undesired secondary sex characteristics. More longitudinal studies are needed to better understand the long-term risks of osteoporosis and fractures in those who have undergone GnRH agonist therapy as part of their gender-affirming medical care, as well as any clinical interventions that might help mitigate this risk.
Dr. Cooper is assistant professor of pediatrics at UT Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Harrington J et al. Treatment of precocious puberty. UpToDate. www.uptodate.com/contents/treatment-of-precocious-puberty.
2. Lee JY et al. J Endocr Soc. 2020;4(9):bvaa065. doi: 10.1210/jendso/bvaa065.
3. Klink D et al. J Clin Endocrinol Metab. 2015;100(2):E270-5. doi: 10.1210/jc.2014-2439.
4. Schagen SEE et al. J Clin Endocrinol Metab. 2020;105(12):e4252-e4263. doi: 10.1210/clinem/dgaa604.
5. Alessandri SB et al. Clinics (Sao Paulo). 2012;67(6):591-6. doi: 10.6061/clinics/2012(06)08.
LGBTQ+ teens in homophobic high schools
I am a psychiatrist now but had another life teaching English in public high school for 17 years. My teaching life, in which I was an openly gay teacher, spanned 2001-2018 and was divided between two urban California schools – in Berkeley and San Leandro. I came out by responding honestly to student questions about whether I had a girlfriend, and what I did over the weekend. At Berkeley High my openness wasn’t an issue at all. The school had a vibrant Gay Straight Alliance/GSA for years, there were many openly gay staff and many openly gay students. No students felt the need to come out to me in search of a gay mentor.
Two years later, I began teaching in San Leandro, 20 miles away, and it was a lesson in how even the San Francisco Bay Area, an LGBTQ+ bastion, could harbor homophobia. When I was hired in 2003, San Leandro High had one openly gay teacher, Q. I quickly realized how much braver his coming out was compared with mine in Berkeley.
In San Leandro, gay slurs were heard nonstop in the hallways, no students were out, and by the end of my first year Q had quit, confiding in me that he couldn’t handle the homophobic harassment from students anymore. There was no GSA. A few years ago, two lesbians had held hands during lunch and inspired the wrath of a group of parents who advocated for their expulsion. In response, a teacher tried to introduce gay sensitivity training into his class and the same group of parents tried to get him fired. He was reprimanded by the principal, he countersued in a case that went all the way to the California Supreme Court, and won. Comparing these two local high schools reinforced to me how visibility really matters in creating a childhood experience that is nurturing versus traumatizing.1
Two Chinese girls in love
N and T were two Chinese girls who grew up in San Leandro. They went to the same elementary school and had crushes on each other since then. In their junior year, they joined our first student GSA, becoming president and vice-president. They were out. And, of course, they must’ve known that their families, who would not have been supportive, would become aware. I remember sitting at an outdoor concert when I got a text from N warning me her father had found out and blamed me for having corrupted her. He planned on coming to school to demand I be fired. And such was the unrelenting pressure that N and T faced every time they went home from school and sat at their dinner tables. Eventually, they broke up. They didn’t do so tearfully, but more wearily.
This story illustrates how difficult it is for love between two LGBTQ+ teens to be nurtured. Love in youth can already be volatile because of the lack of emotional regulation and experience. The questioning of identity and the threat of family disintegration at a time when these teens do not have the economic means to protect themselves makes love dangerous. It is no wonder that gay teens are at increased risk for homelessness.2
The family incident that led to the girls’ breakup reveals how culture affects homophobic pressure. N resisted her parents’ disapproval for months, but she capitulated when her father had a heart attack and blamed it on her. “And it’s true,” N confided. “After my parents found out, they were continually stressed. I could see it affect their health. And it breaks my heart to see my dad in the hospital.”
For N, she had not capitulated from fear, but perhaps because of filial piety, or one’s obligation to protect one’s parent. It was a choice between two heartbreaks. Double minorities, like N and T, face a double threat and often can find no safe place. One of my patients who is gay and Black put it best: “It’s like being beaten up at school only to come home to another beating.” This double threat is evidenced by the higher suicide risk of ethnicities who are LGBTQ+ relative to their white counterparts.3
The confusion of a gay athlete
R was a star point guard, a senior who had secured an athletic scholarship, and was recognized as the best athlete in our county. A popular boy, he flaunted his physique and flirted with all the girls. And then when he was enrolled in my class, he began flirting with all the boys, too. There was gossip that R was bisexual. Then one day, not unexpectedly, he came out to me as gay. He admitted he only flirted with girls for his reputation.
By this time many students had come out to me but he flirted with me with his revelation. I corrected him and warned him unequivocally that it was inappropriate but I was worried because I knew he had placed his trust in me. I also knew he came from a homophobic family that was violent – his father had attacked him physically at a school game and our coaches had to pull him off.
Instinctively, I felt I had to have a witness so I confided in another teacher and documented the situation meticulously. Then, one day, just as I feared, he went too far. He stayed after class and said he wanted to show me something on his phone. And that something turned out to be a picture of himself naked. I immediately confiscated the phone and reported it to the administration. This was not how I wanted him to come out: His family notified by the police that he had sexually harassed his teacher, expulsion pending, and scholarship inevitably revoked. Fortunately, we did find a resolution that restored R’s future.
Let’s examine the circumstances that could’ve informed his transgressive behavior. If we consider sexual harassment a form of bullying, R’s history of having a father who publicly bullied him – and may have bullied others in front of him – is a known risk factor.4 It is also common knowledge that organized team sports were and still are a bastion of homophobia and that gay athletes had to accept a culture of explicit homophobia.5
So, it is not hard to understand the constant public pressures that R faced in addition to those from his family. Let’s also consider that appropriate sexual behaviors are not something we are born with, but something that is learned. Of course, inappropriate sexual behavior also happens in the heterosexual world. But heterosexual sexual behavior often has more accepted paths of trial and error. Children experiment with these behaviors and are corrected by adults and older peers as they mature.
However, for homosexual behaviors, there is not usually the fine-tuning about what is appropriate.
Summary
An educational environment where LGBTQ+ persons are highly visible and accepted is a more nurturing environment for LGBTQ teens than one that is not. Specific subcultures within the LGBTQ population involving race, culture, gender, and athletics modulate the experience of coming out and the nature of homophobic oppression.
Dr. Nguyen is a first-year psychiatry resident at the University of San Francisco School of Medicine at Fresno.
References
1. Kosciw JG et al. The effect of negative school climate on academic outcomes for LGBT youth and the role of in-school supports. J Sch Violence. 2013;12(1):45-63.
2. Center for American Progress. Gay and Transgender Youth Homelessness by the Numbers. June 21, 2010).
3. O’Donnell S et al. Increased risk of suicide attempts among Black and Latino lesbians, gay men, and bisexuals. Am J Public Health. 2011;101(6):1055-9.
4. Farrington D and Baldry A. Individual risk factors for school bullying. J Aggress Confl Peace Res. 2010 Jan;2(1):4-16.
5. Anderson E. Openly gay athletes: Contesting hegemonic masculinity in a homophobic environment Gend Soc. 2002 Dec:16(6):860-77.
I am a psychiatrist now but had another life teaching English in public high school for 17 years. My teaching life, in which I was an openly gay teacher, spanned 2001-2018 and was divided between two urban California schools – in Berkeley and San Leandro. I came out by responding honestly to student questions about whether I had a girlfriend, and what I did over the weekend. At Berkeley High my openness wasn’t an issue at all. The school had a vibrant Gay Straight Alliance/GSA for years, there were many openly gay staff and many openly gay students. No students felt the need to come out to me in search of a gay mentor.
Two years later, I began teaching in San Leandro, 20 miles away, and it was a lesson in how even the San Francisco Bay Area, an LGBTQ+ bastion, could harbor homophobia. When I was hired in 2003, San Leandro High had one openly gay teacher, Q. I quickly realized how much braver his coming out was compared with mine in Berkeley.
In San Leandro, gay slurs were heard nonstop in the hallways, no students were out, and by the end of my first year Q had quit, confiding in me that he couldn’t handle the homophobic harassment from students anymore. There was no GSA. A few years ago, two lesbians had held hands during lunch and inspired the wrath of a group of parents who advocated for their expulsion. In response, a teacher tried to introduce gay sensitivity training into his class and the same group of parents tried to get him fired. He was reprimanded by the principal, he countersued in a case that went all the way to the California Supreme Court, and won. Comparing these two local high schools reinforced to me how visibility really matters in creating a childhood experience that is nurturing versus traumatizing.1
Two Chinese girls in love
N and T were two Chinese girls who grew up in San Leandro. They went to the same elementary school and had crushes on each other since then. In their junior year, they joined our first student GSA, becoming president and vice-president. They were out. And, of course, they must’ve known that their families, who would not have been supportive, would become aware. I remember sitting at an outdoor concert when I got a text from N warning me her father had found out and blamed me for having corrupted her. He planned on coming to school to demand I be fired. And such was the unrelenting pressure that N and T faced every time they went home from school and sat at their dinner tables. Eventually, they broke up. They didn’t do so tearfully, but more wearily.
This story illustrates how difficult it is for love between two LGBTQ+ teens to be nurtured. Love in youth can already be volatile because of the lack of emotional regulation and experience. The questioning of identity and the threat of family disintegration at a time when these teens do not have the economic means to protect themselves makes love dangerous. It is no wonder that gay teens are at increased risk for homelessness.2
The family incident that led to the girls’ breakup reveals how culture affects homophobic pressure. N resisted her parents’ disapproval for months, but she capitulated when her father had a heart attack and blamed it on her. “And it’s true,” N confided. “After my parents found out, they were continually stressed. I could see it affect their health. And it breaks my heart to see my dad in the hospital.”
For N, she had not capitulated from fear, but perhaps because of filial piety, or one’s obligation to protect one’s parent. It was a choice between two heartbreaks. Double minorities, like N and T, face a double threat and often can find no safe place. One of my patients who is gay and Black put it best: “It’s like being beaten up at school only to come home to another beating.” This double threat is evidenced by the higher suicide risk of ethnicities who are LGBTQ+ relative to their white counterparts.3
The confusion of a gay athlete
R was a star point guard, a senior who had secured an athletic scholarship, and was recognized as the best athlete in our county. A popular boy, he flaunted his physique and flirted with all the girls. And then when he was enrolled in my class, he began flirting with all the boys, too. There was gossip that R was bisexual. Then one day, not unexpectedly, he came out to me as gay. He admitted he only flirted with girls for his reputation.
By this time many students had come out to me but he flirted with me with his revelation. I corrected him and warned him unequivocally that it was inappropriate but I was worried because I knew he had placed his trust in me. I also knew he came from a homophobic family that was violent – his father had attacked him physically at a school game and our coaches had to pull him off.
Instinctively, I felt I had to have a witness so I confided in another teacher and documented the situation meticulously. Then, one day, just as I feared, he went too far. He stayed after class and said he wanted to show me something on his phone. And that something turned out to be a picture of himself naked. I immediately confiscated the phone and reported it to the administration. This was not how I wanted him to come out: His family notified by the police that he had sexually harassed his teacher, expulsion pending, and scholarship inevitably revoked. Fortunately, we did find a resolution that restored R’s future.
Let’s examine the circumstances that could’ve informed his transgressive behavior. If we consider sexual harassment a form of bullying, R’s history of having a father who publicly bullied him – and may have bullied others in front of him – is a known risk factor.4 It is also common knowledge that organized team sports were and still are a bastion of homophobia and that gay athletes had to accept a culture of explicit homophobia.5
So, it is not hard to understand the constant public pressures that R faced in addition to those from his family. Let’s also consider that appropriate sexual behaviors are not something we are born with, but something that is learned. Of course, inappropriate sexual behavior also happens in the heterosexual world. But heterosexual sexual behavior often has more accepted paths of trial and error. Children experiment with these behaviors and are corrected by adults and older peers as they mature.
However, for homosexual behaviors, there is not usually the fine-tuning about what is appropriate.
Summary
An educational environment where LGBTQ+ persons are highly visible and accepted is a more nurturing environment for LGBTQ teens than one that is not. Specific subcultures within the LGBTQ population involving race, culture, gender, and athletics modulate the experience of coming out and the nature of homophobic oppression.
Dr. Nguyen is a first-year psychiatry resident at the University of San Francisco School of Medicine at Fresno.
References
1. Kosciw JG et al. The effect of negative school climate on academic outcomes for LGBT youth and the role of in-school supports. J Sch Violence. 2013;12(1):45-63.
2. Center for American Progress. Gay and Transgender Youth Homelessness by the Numbers. June 21, 2010).
3. O’Donnell S et al. Increased risk of suicide attempts among Black and Latino lesbians, gay men, and bisexuals. Am J Public Health. 2011;101(6):1055-9.
4. Farrington D and Baldry A. Individual risk factors for school bullying. J Aggress Confl Peace Res. 2010 Jan;2(1):4-16.
5. Anderson E. Openly gay athletes: Contesting hegemonic masculinity in a homophobic environment Gend Soc. 2002 Dec:16(6):860-77.
I am a psychiatrist now but had another life teaching English in public high school for 17 years. My teaching life, in which I was an openly gay teacher, spanned 2001-2018 and was divided between two urban California schools – in Berkeley and San Leandro. I came out by responding honestly to student questions about whether I had a girlfriend, and what I did over the weekend. At Berkeley High my openness wasn’t an issue at all. The school had a vibrant Gay Straight Alliance/GSA for years, there were many openly gay staff and many openly gay students. No students felt the need to come out to me in search of a gay mentor.
Two years later, I began teaching in San Leandro, 20 miles away, and it was a lesson in how even the San Francisco Bay Area, an LGBTQ+ bastion, could harbor homophobia. When I was hired in 2003, San Leandro High had one openly gay teacher, Q. I quickly realized how much braver his coming out was compared with mine in Berkeley.
In San Leandro, gay slurs were heard nonstop in the hallways, no students were out, and by the end of my first year Q had quit, confiding in me that he couldn’t handle the homophobic harassment from students anymore. There was no GSA. A few years ago, two lesbians had held hands during lunch and inspired the wrath of a group of parents who advocated for their expulsion. In response, a teacher tried to introduce gay sensitivity training into his class and the same group of parents tried to get him fired. He was reprimanded by the principal, he countersued in a case that went all the way to the California Supreme Court, and won. Comparing these two local high schools reinforced to me how visibility really matters in creating a childhood experience that is nurturing versus traumatizing.1
Two Chinese girls in love
N and T were two Chinese girls who grew up in San Leandro. They went to the same elementary school and had crushes on each other since then. In their junior year, they joined our first student GSA, becoming president and vice-president. They were out. And, of course, they must’ve known that their families, who would not have been supportive, would become aware. I remember sitting at an outdoor concert when I got a text from N warning me her father had found out and blamed me for having corrupted her. He planned on coming to school to demand I be fired. And such was the unrelenting pressure that N and T faced every time they went home from school and sat at their dinner tables. Eventually, they broke up. They didn’t do so tearfully, but more wearily.
This story illustrates how difficult it is for love between two LGBTQ+ teens to be nurtured. Love in youth can already be volatile because of the lack of emotional regulation and experience. The questioning of identity and the threat of family disintegration at a time when these teens do not have the economic means to protect themselves makes love dangerous. It is no wonder that gay teens are at increased risk for homelessness.2
The family incident that led to the girls’ breakup reveals how culture affects homophobic pressure. N resisted her parents’ disapproval for months, but she capitulated when her father had a heart attack and blamed it on her. “And it’s true,” N confided. “After my parents found out, they were continually stressed. I could see it affect their health. And it breaks my heart to see my dad in the hospital.”
For N, she had not capitulated from fear, but perhaps because of filial piety, or one’s obligation to protect one’s parent. It was a choice between two heartbreaks. Double minorities, like N and T, face a double threat and often can find no safe place. One of my patients who is gay and Black put it best: “It’s like being beaten up at school only to come home to another beating.” This double threat is evidenced by the higher suicide risk of ethnicities who are LGBTQ+ relative to their white counterparts.3
The confusion of a gay athlete
R was a star point guard, a senior who had secured an athletic scholarship, and was recognized as the best athlete in our county. A popular boy, he flaunted his physique and flirted with all the girls. And then when he was enrolled in my class, he began flirting with all the boys, too. There was gossip that R was bisexual. Then one day, not unexpectedly, he came out to me as gay. He admitted he only flirted with girls for his reputation.
By this time many students had come out to me but he flirted with me with his revelation. I corrected him and warned him unequivocally that it was inappropriate but I was worried because I knew he had placed his trust in me. I also knew he came from a homophobic family that was violent – his father had attacked him physically at a school game and our coaches had to pull him off.
Instinctively, I felt I had to have a witness so I confided in another teacher and documented the situation meticulously. Then, one day, just as I feared, he went too far. He stayed after class and said he wanted to show me something on his phone. And that something turned out to be a picture of himself naked. I immediately confiscated the phone and reported it to the administration. This was not how I wanted him to come out: His family notified by the police that he had sexually harassed his teacher, expulsion pending, and scholarship inevitably revoked. Fortunately, we did find a resolution that restored R’s future.
Let’s examine the circumstances that could’ve informed his transgressive behavior. If we consider sexual harassment a form of bullying, R’s history of having a father who publicly bullied him – and may have bullied others in front of him – is a known risk factor.4 It is also common knowledge that organized team sports were and still are a bastion of homophobia and that gay athletes had to accept a culture of explicit homophobia.5
So, it is not hard to understand the constant public pressures that R faced in addition to those from his family. Let’s also consider that appropriate sexual behaviors are not something we are born with, but something that is learned. Of course, inappropriate sexual behavior also happens in the heterosexual world. But heterosexual sexual behavior often has more accepted paths of trial and error. Children experiment with these behaviors and are corrected by adults and older peers as they mature.
However, for homosexual behaviors, there is not usually the fine-tuning about what is appropriate.
Summary
An educational environment where LGBTQ+ persons are highly visible and accepted is a more nurturing environment for LGBTQ teens than one that is not. Specific subcultures within the LGBTQ population involving race, culture, gender, and athletics modulate the experience of coming out and the nature of homophobic oppression.
Dr. Nguyen is a first-year psychiatry resident at the University of San Francisco School of Medicine at Fresno.
References
1. Kosciw JG et al. The effect of negative school climate on academic outcomes for LGBT youth and the role of in-school supports. J Sch Violence. 2013;12(1):45-63.
2. Center for American Progress. Gay and Transgender Youth Homelessness by the Numbers. June 21, 2010).
3. O’Donnell S et al. Increased risk of suicide attempts among Black and Latino lesbians, gay men, and bisexuals. Am J Public Health. 2011;101(6):1055-9.
4. Farrington D and Baldry A. Individual risk factors for school bullying. J Aggress Confl Peace Res. 2010 Jan;2(1):4-16.
5. Anderson E. Openly gay athletes: Contesting hegemonic masculinity in a homophobic environment Gend Soc. 2002 Dec:16(6):860-77.











