User login
For some MST survivors, VA hospitals can trigger PTSD
Alternative treatment settings could be ‘easier access point’
SAN FRANCISCO – Veterans who are survivors of military sexual trauma during their service face unique challenges in their treatment and recovery. They are often reluctant to report their experiences – and understandably so.
“Military sexual assault represents a huge violation of that trust and safety. That’s what makes it so toxic and hard for participants to [come] forward, because they’re accused of breaking cohesion of their unit and breaking morale, and yet they have been mistreated,” Niranjan Karnik, MD, PhD, associate dean for community behavioral health at Rush Medical College, Chicago, said in an interview.
Dr. Karnik moderated a session on the prevalence and treatment of military sexual assault at the annual meeting of the American Psychiatric Association. Although the Department of Veterans Affairs treats many survivors of sexual assault, not all of them feel comfortable in that environment. “A VA hospital has a quasi-military feel to it, and that’s a reflection of what it is and the people who are there. That can be an inhibition – and can even be a trigger for [PTSD] symptoms,” Dr. Karnik said.
Survivors may also worry about being labeled, or about adverse entries going into their official record and how that could affect them in the future. The issue is a stark contrast to veterans who are suffering from combat-related trauma.
“When a combat trauma survivor goes to the VA, they feel protected because their colleagues are there. With military sexual trauma, because of that violation of trust from their peers, it can really exacerbate things,” Dr. Karnik said.
Fortunately, there are alternatives, such as the Road Home* Program at Rush Hospital, which has a few military accoutrements but more closely resembles a civilian center. “It can be an easier access point. The VA is taking care of a large majority of patients. We are a boutique program for the vets who can’t or feel unable to go through the VA program,” Dr. Karnik said.
Overall, 52.5% of women and 8.9% of men in the military report sexual harassment, and 23.6% of women and 1.9% of men report being sexually assaulted. That amounts to 14,900 service members, 8,600 women, and 6,300 men who were assaulted in 2016, according to Neeral K. Sheth, DO, assistant professor of psychiatry at Rush Medical College, who also presented at the session. The frequency of assault is higher among LGBTQ individuals, and African American men and women are more likely to experience sexual harassment.
There are options for treatment of military sexual trauma (MST). The 3-week Road Home intensive outpatient treatment program at Rush Hospital combines group and individual cognitive-processing therapy, which is a cognitive-behavioral therapy that has been shown to improve PTSD resulting from MST. The program places combat trauma and MST trauma patients into separate cohorts, each containing individual and group components. Individual sessions closely follow a manualized protocol, while group sessions offer an opportunity to practice cognitive-processing therapy skills.
The team adapted the program to MST treatment by incorporating dialectical-behavioral therapy skills modules in the first week of the program, and implemented one-on-one skills consultation by request throughout the program.
An analysis of 191 subjects participating in 19 cohorts (12 combat, 9 MST cohorts) showed a 92% completion rate, which was similar, regardless of gender or cohort type. Both cohorts had significant reductions in PTSD severity as measured by the PTSD Checklist for DSM-5, and depression symptoms as measured by the Patient Health Questionnaire–9.
Another program, Families OverComing Under Stress, can also be adapted to MST. It is designed to build resiliency and wellness within families dealing with trauma or loss. It incorporates family assessment, psychoeducation tailored to the needs of the entire family, family-level resilience skills, and a narrative component.
An important element is the identification and management of stress reminders – triggers that remind the individual of a trauma and may cause a sudden shift in mood or behavior. A family member’s knowledge that the survivor is experiencing a stress reminder can reduce misunderstandings or unhelpful interpretations of behavior.
In fact, family considerations are often what bring veterans in for help in the first place, according to Dr. Karnik. He or she may be concerned about behavioral problems in a child, which the VA cannot address because its federal funding dictates a sole focus on the veteran. “We will take care of the whole family,” Dr. Karnik said. “Often that’s the entry point, and that allows us to do some engagement with the veteran, and things start to get uncovered.”
Dr. Karnik has no relevant financial disclosures.
*CORRECTION, 5/21/2019
Alternative treatment settings could be ‘easier access point’
Alternative treatment settings could be ‘easier access point’
SAN FRANCISCO – Veterans who are survivors of military sexual trauma during their service face unique challenges in their treatment and recovery. They are often reluctant to report their experiences – and understandably so.
“Military sexual assault represents a huge violation of that trust and safety. That’s what makes it so toxic and hard for participants to [come] forward, because they’re accused of breaking cohesion of their unit and breaking morale, and yet they have been mistreated,” Niranjan Karnik, MD, PhD, associate dean for community behavioral health at Rush Medical College, Chicago, said in an interview.
Dr. Karnik moderated a session on the prevalence and treatment of military sexual assault at the annual meeting of the American Psychiatric Association. Although the Department of Veterans Affairs treats many survivors of sexual assault, not all of them feel comfortable in that environment. “A VA hospital has a quasi-military feel to it, and that’s a reflection of what it is and the people who are there. That can be an inhibition – and can even be a trigger for [PTSD] symptoms,” Dr. Karnik said.
Survivors may also worry about being labeled, or about adverse entries going into their official record and how that could affect them in the future. The issue is a stark contrast to veterans who are suffering from combat-related trauma.
“When a combat trauma survivor goes to the VA, they feel protected because their colleagues are there. With military sexual trauma, because of that violation of trust from their peers, it can really exacerbate things,” Dr. Karnik said.
Fortunately, there are alternatives, such as the Road Home* Program at Rush Hospital, which has a few military accoutrements but more closely resembles a civilian center. “It can be an easier access point. The VA is taking care of a large majority of patients. We are a boutique program for the vets who can’t or feel unable to go through the VA program,” Dr. Karnik said.
Overall, 52.5% of women and 8.9% of men in the military report sexual harassment, and 23.6% of women and 1.9% of men report being sexually assaulted. That amounts to 14,900 service members, 8,600 women, and 6,300 men who were assaulted in 2016, according to Neeral K. Sheth, DO, assistant professor of psychiatry at Rush Medical College, who also presented at the session. The frequency of assault is higher among LGBTQ individuals, and African American men and women are more likely to experience sexual harassment.
There are options for treatment of military sexual trauma (MST). The 3-week Road Home intensive outpatient treatment program at Rush Hospital combines group and individual cognitive-processing therapy, which is a cognitive-behavioral therapy that has been shown to improve PTSD resulting from MST. The program places combat trauma and MST trauma patients into separate cohorts, each containing individual and group components. Individual sessions closely follow a manualized protocol, while group sessions offer an opportunity to practice cognitive-processing therapy skills.
The team adapted the program to MST treatment by incorporating dialectical-behavioral therapy skills modules in the first week of the program, and implemented one-on-one skills consultation by request throughout the program.
An analysis of 191 subjects participating in 19 cohorts (12 combat, 9 MST cohorts) showed a 92% completion rate, which was similar, regardless of gender or cohort type. Both cohorts had significant reductions in PTSD severity as measured by the PTSD Checklist for DSM-5, and depression symptoms as measured by the Patient Health Questionnaire–9.
Another program, Families OverComing Under Stress, can also be adapted to MST. It is designed to build resiliency and wellness within families dealing with trauma or loss. It incorporates family assessment, psychoeducation tailored to the needs of the entire family, family-level resilience skills, and a narrative component.
An important element is the identification and management of stress reminders – triggers that remind the individual of a trauma and may cause a sudden shift in mood or behavior. A family member’s knowledge that the survivor is experiencing a stress reminder can reduce misunderstandings or unhelpful interpretations of behavior.
In fact, family considerations are often what bring veterans in for help in the first place, according to Dr. Karnik. He or she may be concerned about behavioral problems in a child, which the VA cannot address because its federal funding dictates a sole focus on the veteran. “We will take care of the whole family,” Dr. Karnik said. “Often that’s the entry point, and that allows us to do some engagement with the veteran, and things start to get uncovered.”
Dr. Karnik has no relevant financial disclosures.
*CORRECTION, 5/21/2019
SAN FRANCISCO – Veterans who are survivors of military sexual trauma during their service face unique challenges in their treatment and recovery. They are often reluctant to report their experiences – and understandably so.
“Military sexual assault represents a huge violation of that trust and safety. That’s what makes it so toxic and hard for participants to [come] forward, because they’re accused of breaking cohesion of their unit and breaking morale, and yet they have been mistreated,” Niranjan Karnik, MD, PhD, associate dean for community behavioral health at Rush Medical College, Chicago, said in an interview.
Dr. Karnik moderated a session on the prevalence and treatment of military sexual assault at the annual meeting of the American Psychiatric Association. Although the Department of Veterans Affairs treats many survivors of sexual assault, not all of them feel comfortable in that environment. “A VA hospital has a quasi-military feel to it, and that’s a reflection of what it is and the people who are there. That can be an inhibition – and can even be a trigger for [PTSD] symptoms,” Dr. Karnik said.
Survivors may also worry about being labeled, or about adverse entries going into their official record and how that could affect them in the future. The issue is a stark contrast to veterans who are suffering from combat-related trauma.
“When a combat trauma survivor goes to the VA, they feel protected because their colleagues are there. With military sexual trauma, because of that violation of trust from their peers, it can really exacerbate things,” Dr. Karnik said.
Fortunately, there are alternatives, such as the Road Home* Program at Rush Hospital, which has a few military accoutrements but more closely resembles a civilian center. “It can be an easier access point. The VA is taking care of a large majority of patients. We are a boutique program for the vets who can’t or feel unable to go through the VA program,” Dr. Karnik said.
Overall, 52.5% of women and 8.9% of men in the military report sexual harassment, and 23.6% of women and 1.9% of men report being sexually assaulted. That amounts to 14,900 service members, 8,600 women, and 6,300 men who were assaulted in 2016, according to Neeral K. Sheth, DO, assistant professor of psychiatry at Rush Medical College, who also presented at the session. The frequency of assault is higher among LGBTQ individuals, and African American men and women are more likely to experience sexual harassment.
There are options for treatment of military sexual trauma (MST). The 3-week Road Home intensive outpatient treatment program at Rush Hospital combines group and individual cognitive-processing therapy, which is a cognitive-behavioral therapy that has been shown to improve PTSD resulting from MST. The program places combat trauma and MST trauma patients into separate cohorts, each containing individual and group components. Individual sessions closely follow a manualized protocol, while group sessions offer an opportunity to practice cognitive-processing therapy skills.
The team adapted the program to MST treatment by incorporating dialectical-behavioral therapy skills modules in the first week of the program, and implemented one-on-one skills consultation by request throughout the program.
An analysis of 191 subjects participating in 19 cohorts (12 combat, 9 MST cohorts) showed a 92% completion rate, which was similar, regardless of gender or cohort type. Both cohorts had significant reductions in PTSD severity as measured by the PTSD Checklist for DSM-5, and depression symptoms as measured by the Patient Health Questionnaire–9.
Another program, Families OverComing Under Stress, can also be adapted to MST. It is designed to build resiliency and wellness within families dealing with trauma or loss. It incorporates family assessment, psychoeducation tailored to the needs of the entire family, family-level resilience skills, and a narrative component.
An important element is the identification and management of stress reminders – triggers that remind the individual of a trauma and may cause a sudden shift in mood or behavior. A family member’s knowledge that the survivor is experiencing a stress reminder can reduce misunderstandings or unhelpful interpretations of behavior.
In fact, family considerations are often what bring veterans in for help in the first place, according to Dr. Karnik. He or she may be concerned about behavioral problems in a child, which the VA cannot address because its federal funding dictates a sole focus on the veteran. “We will take care of the whole family,” Dr. Karnik said. “Often that’s the entry point, and that allows us to do some engagement with the veteran, and things start to get uncovered.”
Dr. Karnik has no relevant financial disclosures.
*CORRECTION, 5/21/2019
REPORTING FROM APA 2019
More empathy for women
At the risk of too much personal self-disclosure, I feel the need to write about my having developed more empathy for women. Having been described as a “manly man,” by a woman who feels she knows me, it has always been difficult for me to understand women. Fortunately, an experience I’ve had has given me more insight into women – shallow though it may still be.
About a year ago, I had learned I had prostate carcinoma, which is now in remission – thanks to a proctectomy, radiation, and hormone therapy. The antitestosterone hormones I need to take for 2 years are turning me into an old woman, thus my newfound empathy.
After the surgery, I found myself leaking – something that I probably only experienced as a child and of which I have little memory. I now have some more empathy for the problems women have with leaking each month or in general – it is a constant preoccupation. The leuprolide shots I am taking are giving me hot flashes, causing me to be more emotional about things I really don’t understand, and apparently I am at risk for getting osteoporosis – all things that happen to women that have been mildly on my radar for years but for which I lacked direct and personal experience.
Since having my testosterone turned off by the leuprolide, my joints are more prone to aches and pains from various injuries over the years. Because I understand that “motion is lotion,” I have some control of this problem. However, the hormone therapy has greatly reduced my endurance, so my exercise tolerance is far more limited – I understand fatigue now. When I was telling another woman who feels she knows me about my experience, she told me it was hormones that made it more difficult to lose weight. And, I am gaining weight.
All in all, I believe my experience has given me more empathy for women, but I realize I still have a very long way to go. Nonetheless, I will continue in my quest to understand the opposite sex, as I am told “women hold up half the sky,” and I have always believed that to be true.
Fortunately, women are ascending in psychiatry and, with some serious dedication, the dearth of scientific understanding of women’s issues will be a thing of the past. and fill that void of knowledge that we men psychiatrists have in our testosterone-bathed brains.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital’s Medical/Surgical-Psychiatry Inpatient Unit in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
At the risk of too much personal self-disclosure, I feel the need to write about my having developed more empathy for women. Having been described as a “manly man,” by a woman who feels she knows me, it has always been difficult for me to understand women. Fortunately, an experience I’ve had has given me more insight into women – shallow though it may still be.
About a year ago, I had learned I had prostate carcinoma, which is now in remission – thanks to a proctectomy, radiation, and hormone therapy. The antitestosterone hormones I need to take for 2 years are turning me into an old woman, thus my newfound empathy.
After the surgery, I found myself leaking – something that I probably only experienced as a child and of which I have little memory. I now have some more empathy for the problems women have with leaking each month or in general – it is a constant preoccupation. The leuprolide shots I am taking are giving me hot flashes, causing me to be more emotional about things I really don’t understand, and apparently I am at risk for getting osteoporosis – all things that happen to women that have been mildly on my radar for years but for which I lacked direct and personal experience.
Since having my testosterone turned off by the leuprolide, my joints are more prone to aches and pains from various injuries over the years. Because I understand that “motion is lotion,” I have some control of this problem. However, the hormone therapy has greatly reduced my endurance, so my exercise tolerance is far more limited – I understand fatigue now. When I was telling another woman who feels she knows me about my experience, she told me it was hormones that made it more difficult to lose weight. And, I am gaining weight.
All in all, I believe my experience has given me more empathy for women, but I realize I still have a very long way to go. Nonetheless, I will continue in my quest to understand the opposite sex, as I am told “women hold up half the sky,” and I have always believed that to be true.
Fortunately, women are ascending in psychiatry and, with some serious dedication, the dearth of scientific understanding of women’s issues will be a thing of the past. and fill that void of knowledge that we men psychiatrists have in our testosterone-bathed brains.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital’s Medical/Surgical-Psychiatry Inpatient Unit in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
At the risk of too much personal self-disclosure, I feel the need to write about my having developed more empathy for women. Having been described as a “manly man,” by a woman who feels she knows me, it has always been difficult for me to understand women. Fortunately, an experience I’ve had has given me more insight into women – shallow though it may still be.
About a year ago, I had learned I had prostate carcinoma, which is now in remission – thanks to a proctectomy, radiation, and hormone therapy. The antitestosterone hormones I need to take for 2 years are turning me into an old woman, thus my newfound empathy.
After the surgery, I found myself leaking – something that I probably only experienced as a child and of which I have little memory. I now have some more empathy for the problems women have with leaking each month or in general – it is a constant preoccupation. The leuprolide shots I am taking are giving me hot flashes, causing me to be more emotional about things I really don’t understand, and apparently I am at risk for getting osteoporosis – all things that happen to women that have been mildly on my radar for years but for which I lacked direct and personal experience.
Since having my testosterone turned off by the leuprolide, my joints are more prone to aches and pains from various injuries over the years. Because I understand that “motion is lotion,” I have some control of this problem. However, the hormone therapy has greatly reduced my endurance, so my exercise tolerance is far more limited – I understand fatigue now. When I was telling another woman who feels she knows me about my experience, she told me it was hormones that made it more difficult to lose weight. And, I am gaining weight.
All in all, I believe my experience has given me more empathy for women, but I realize I still have a very long way to go. Nonetheless, I will continue in my quest to understand the opposite sex, as I am told “women hold up half the sky,” and I have always believed that to be true.
Fortunately, women are ascending in psychiatry and, with some serious dedication, the dearth of scientific understanding of women’s issues will be a thing of the past. and fill that void of knowledge that we men psychiatrists have in our testosterone-bathed brains.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital’s Medical/Surgical-Psychiatry Inpatient Unit in Chicago, clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago, former president/CEO of Community Mental Health Council, and former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
Thrice yearly cytologic testing may best annual cervical screenings
Less-frequent cytologic testing, followed by hrHPV tests
George F. Sawaya, MD, from the University of California, San Francisco, and colleagues enrolled 451 English-speaking or Spanish-speaking women aged 21-65 years from women’s health clinics between September 2014 and June 2016. The women were mean 38 years old, and 57% were nonwhite women. The researchers examined utilities for 23 different health states associated with cervical cancer, and created a Markov decision model of type-specific high-risk human papillomavirus (hrHPV)–induced cervical carcinogenesis.
The researchers evaluated 12 screening strategies, which included the following scenarios:
- For women aged 21-65 years, cytologic testing every 3 years; if atypical squamous cells of undetermined significance (ASCUS) are found, repeat cytologic testing in 1 year or switch to immediate hrHPV triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with cytologic testing plus hrHPV testing (cotesting) for women 30-65 years old; if a normal cytologic test result and positive hrHPV test results, move to cotesting in 1 year or immediate genotyping triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with hrHPV testing alone every 3-5 years for women 30-65 years; if there are positive hrHPV results, move to immediate cytologic testing triage or immediate genotyping triage. Women with positive hrHPV and negative genotyping results receive additional cytologic testing triage.
In the strategies that switched the women from cytologic testing to hrHPV tests, the study also tested doing the switch at age 25 years rather than 30 years, the investigators reported.
Overall, with regard to cost, screening resulted in more cost savings ($1,267-$2,577) than not screening ($2,891 per woman). Women received the most benefit as measured by lifetime quality-adjusted life-years (QALY) if they received cytologic test every 3 years and received repeat testing for ASCUS. The strategy with the lowest cost was cytologic testing every 3 years and hrHPV triage for ASCUS ($1,267), and the strategy of 3-year cytology testing with repeat testing for ASCUS had more QALY but at a higher cost ($2,166). Other higher-cost strategies relative to QALYs included cotesting and primary hrHPV and also annual cytologic testing ($2,577).
“Both the American College of Obstetricians and Gynecologists and the American Cancer Society consider cotesting the preferred cervical cancer screening strategy, and the U.S. Preventive Services Task Force considers it an alternative strategy,” Dr. Sawaya and colleagues noted. “Our findings challenge these endorsements.”
“Our analyses suggest that it is not cost effective to begin primary hrHPV testing prior to age 30 years, to perform hrHPV testing every 3 years, or to perform cytologic testing annually. Comparative modeling is needed to confirm these findings,” they concluded.
Dual stain vs. cytologic testing alone
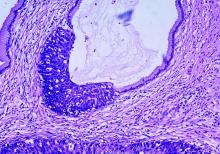
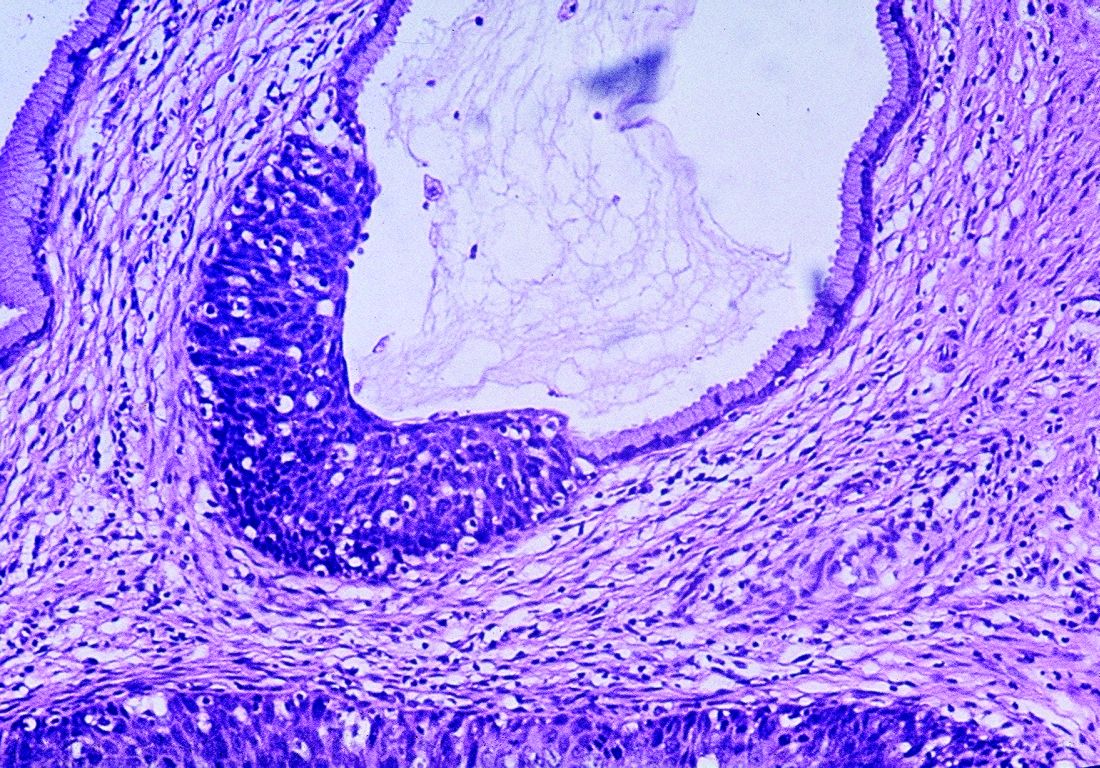
In a second study, Nicolas Wentzensen, MD, PhD, from the National Cancer Institute and colleagues performed a prospective observational study of 3,225 women who tested positive for human papillomavirus (HPV) who underwent p16/Ki-67 dual stain (DS) and HPV16/18 genotyping.
p16/Ki-67 DS was more effective at risk stratification for cervical intraepithelial neoplasia grade 3 or more severe neoplasia (CIN3+) than cytologic testing alone, and women with positive DS results had a higher risk of developing CIN3+ (12%) than did women with cytologic testing alone (10%; P = .005). Women who were HPV16/18 negative were the most likely to not have CIN3+ if they had negative DS results, and DS strategies resulted in fewer overall colposcopies relative to CIN3+ detections, compared with cytologic testing alone.
“We found that, for primary HPV screening, DS has both higher sensitivity and specificity compared with cytologic testing for triage of HPV-positive women Because of the greater reassurance of negative DS results, screening intervals can be extended compared with the screening intervals after negative cytologic results. Dual stain reduces unnecessary colposcopy referral and unnecessary cervical biopsies, and may reduce unnecessary treatment compared with Papanicolaou cytologic testing,” Dr. Wentzensen and colleagues concluded. “Our estimates of sensitivity, absolute risk, and colposcopy referral for various triage strategies can guide implementation of primary HPV screening.”
Five authors of Sawaya et al. reported receiving grants from the National Cancer Institute, and Dr. Megan J. Huchko reported receiving a grant from the University of California, San Francisco, during that study. That study was funded by a grant from the NCI. Six authors from Wentzensen et al. reported receiving grants from the NCI or being employed by the NCI or NIH. Dr. Philip E. Castle reported receiving low-cost or free cervical screening tests from Roche, Becton Dickinson, Cepheid, and Arbor Vita Corp. The other authors from both studies reported no relevant conflicts of interest.
SOURCES: Sawaya GF et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0299; Wentzensen N et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0306.
Cervical cancer screening can be simplified and managed by reducing annual screening to every 3 years for women with normal cytological test results, Sarah Feldman, MD, MPH, wrote in a related editorial. There is evidence from large studies that this is possible for women with average risk of cervical cancer.
Primary human papillomavirus (HPV) screening also is an option for patients, and although there are no current guidelines, 2015 expert guidance states HPV16/18 genotyping and reflex cytologic testing should be used in cases of abnormal results. Transitioning from cytologic testing to primary HPV testing may require a period of using both tests in clinical practice, but this may raise issues with creating false positive results.
“The biggest challenge for cervical cancer screening, however, is likely not which test to use, but determining which women are at low enough risk of cervical cancer to undergo screening at less-frequent intervals,” wrote Dr. Feldman. In these cases, a better infrastructure where clinicians can access women’s prior screening results and make recommendations with decision support systems is needed.
But challenges remain. “These challenges include clinician and patient education and acceptance; access to primary HPV tests; the development of simple, easily implementable, and evidence-based management advice; and systems-based approaches to help clinicians implement optimal care.”
While women 30 years or older are likely to receive primary HPV testing as a standard of care, the risk of cervical cancer also should decrease as more children receive the HPV vaccine, concluded Dr. Feldman.
“Ultimately, once all children have received the HPV vaccination, the incidence of both cervical cancer and precancerous abnormalities should markedly diminish,” Dr. Feldman said. “Ultimately, we may hope to prevent all cervical cancer.”
Dr. Feldman is from the division of gynecologic oncology at Brigham and Women’s Hospital in Boston. Her editorial accompanied the reports by Sawaya et al. and Wentzensen et al. (JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0298). She reported no relevant conflicts of interest.
Cervical cancer screening can be simplified and managed by reducing annual screening to every 3 years for women with normal cytological test results, Sarah Feldman, MD, MPH, wrote in a related editorial. There is evidence from large studies that this is possible for women with average risk of cervical cancer.
Primary human papillomavirus (HPV) screening also is an option for patients, and although there are no current guidelines, 2015 expert guidance states HPV16/18 genotyping and reflex cytologic testing should be used in cases of abnormal results. Transitioning from cytologic testing to primary HPV testing may require a period of using both tests in clinical practice, but this may raise issues with creating false positive results.
“The biggest challenge for cervical cancer screening, however, is likely not which test to use, but determining which women are at low enough risk of cervical cancer to undergo screening at less-frequent intervals,” wrote Dr. Feldman. In these cases, a better infrastructure where clinicians can access women’s prior screening results and make recommendations with decision support systems is needed.
But challenges remain. “These challenges include clinician and patient education and acceptance; access to primary HPV tests; the development of simple, easily implementable, and evidence-based management advice; and systems-based approaches to help clinicians implement optimal care.”
While women 30 years or older are likely to receive primary HPV testing as a standard of care, the risk of cervical cancer also should decrease as more children receive the HPV vaccine, concluded Dr. Feldman.
“Ultimately, once all children have received the HPV vaccination, the incidence of both cervical cancer and precancerous abnormalities should markedly diminish,” Dr. Feldman said. “Ultimately, we may hope to prevent all cervical cancer.”
Dr. Feldman is from the division of gynecologic oncology at Brigham and Women’s Hospital in Boston. Her editorial accompanied the reports by Sawaya et al. and Wentzensen et al. (JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0298). She reported no relevant conflicts of interest.
Cervical cancer screening can be simplified and managed by reducing annual screening to every 3 years for women with normal cytological test results, Sarah Feldman, MD, MPH, wrote in a related editorial. There is evidence from large studies that this is possible for women with average risk of cervical cancer.
Primary human papillomavirus (HPV) screening also is an option for patients, and although there are no current guidelines, 2015 expert guidance states HPV16/18 genotyping and reflex cytologic testing should be used in cases of abnormal results. Transitioning from cytologic testing to primary HPV testing may require a period of using both tests in clinical practice, but this may raise issues with creating false positive results.
“The biggest challenge for cervical cancer screening, however, is likely not which test to use, but determining which women are at low enough risk of cervical cancer to undergo screening at less-frequent intervals,” wrote Dr. Feldman. In these cases, a better infrastructure where clinicians can access women’s prior screening results and make recommendations with decision support systems is needed.
But challenges remain. “These challenges include clinician and patient education and acceptance; access to primary HPV tests; the development of simple, easily implementable, and evidence-based management advice; and systems-based approaches to help clinicians implement optimal care.”
While women 30 years or older are likely to receive primary HPV testing as a standard of care, the risk of cervical cancer also should decrease as more children receive the HPV vaccine, concluded Dr. Feldman.
“Ultimately, once all children have received the HPV vaccination, the incidence of both cervical cancer and precancerous abnormalities should markedly diminish,” Dr. Feldman said. “Ultimately, we may hope to prevent all cervical cancer.”
Dr. Feldman is from the division of gynecologic oncology at Brigham and Women’s Hospital in Boston. Her editorial accompanied the reports by Sawaya et al. and Wentzensen et al. (JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0298). She reported no relevant conflicts of interest.
Less-frequent cytologic testing, followed by hrHPV tests
George F. Sawaya, MD, from the University of California, San Francisco, and colleagues enrolled 451 English-speaking or Spanish-speaking women aged 21-65 years from women’s health clinics between September 2014 and June 2016. The women were mean 38 years old, and 57% were nonwhite women. The researchers examined utilities for 23 different health states associated with cervical cancer, and created a Markov decision model of type-specific high-risk human papillomavirus (hrHPV)–induced cervical carcinogenesis.
The researchers evaluated 12 screening strategies, which included the following scenarios:
- For women aged 21-65 years, cytologic testing every 3 years; if atypical squamous cells of undetermined significance (ASCUS) are found, repeat cytologic testing in 1 year or switch to immediate hrHPV triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with cytologic testing plus hrHPV testing (cotesting) for women 30-65 years old; if a normal cytologic test result and positive hrHPV test results, move to cotesting in 1 year or immediate genotyping triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with hrHPV testing alone every 3-5 years for women 30-65 years; if there are positive hrHPV results, move to immediate cytologic testing triage or immediate genotyping triage. Women with positive hrHPV and negative genotyping results receive additional cytologic testing triage.
In the strategies that switched the women from cytologic testing to hrHPV tests, the study also tested doing the switch at age 25 years rather than 30 years, the investigators reported.
Overall, with regard to cost, screening resulted in more cost savings ($1,267-$2,577) than not screening ($2,891 per woman). Women received the most benefit as measured by lifetime quality-adjusted life-years (QALY) if they received cytologic test every 3 years and received repeat testing for ASCUS. The strategy with the lowest cost was cytologic testing every 3 years and hrHPV triage for ASCUS ($1,267), and the strategy of 3-year cytology testing with repeat testing for ASCUS had more QALY but at a higher cost ($2,166). Other higher-cost strategies relative to QALYs included cotesting and primary hrHPV and also annual cytologic testing ($2,577).
“Both the American College of Obstetricians and Gynecologists and the American Cancer Society consider cotesting the preferred cervical cancer screening strategy, and the U.S. Preventive Services Task Force considers it an alternative strategy,” Dr. Sawaya and colleagues noted. “Our findings challenge these endorsements.”
“Our analyses suggest that it is not cost effective to begin primary hrHPV testing prior to age 30 years, to perform hrHPV testing every 3 years, or to perform cytologic testing annually. Comparative modeling is needed to confirm these findings,” they concluded.
Dual stain vs. cytologic testing alone
In a second study, Nicolas Wentzensen, MD, PhD, from the National Cancer Institute and colleagues performed a prospective observational study of 3,225 women who tested positive for human papillomavirus (HPV) who underwent p16/Ki-67 dual stain (DS) and HPV16/18 genotyping.
p16/Ki-67 DS was more effective at risk stratification for cervical intraepithelial neoplasia grade 3 or more severe neoplasia (CIN3+) than cytologic testing alone, and women with positive DS results had a higher risk of developing CIN3+ (12%) than did women with cytologic testing alone (10%; P = .005). Women who were HPV16/18 negative were the most likely to not have CIN3+ if they had negative DS results, and DS strategies resulted in fewer overall colposcopies relative to CIN3+ detections, compared with cytologic testing alone.
“We found that, for primary HPV screening, DS has both higher sensitivity and specificity compared with cytologic testing for triage of HPV-positive women Because of the greater reassurance of negative DS results, screening intervals can be extended compared with the screening intervals after negative cytologic results. Dual stain reduces unnecessary colposcopy referral and unnecessary cervical biopsies, and may reduce unnecessary treatment compared with Papanicolaou cytologic testing,” Dr. Wentzensen and colleagues concluded. “Our estimates of sensitivity, absolute risk, and colposcopy referral for various triage strategies can guide implementation of primary HPV screening.”
Five authors of Sawaya et al. reported receiving grants from the National Cancer Institute, and Dr. Megan J. Huchko reported receiving a grant from the University of California, San Francisco, during that study. That study was funded by a grant from the NCI. Six authors from Wentzensen et al. reported receiving grants from the NCI or being employed by the NCI or NIH. Dr. Philip E. Castle reported receiving low-cost or free cervical screening tests from Roche, Becton Dickinson, Cepheid, and Arbor Vita Corp. The other authors from both studies reported no relevant conflicts of interest.
SOURCES: Sawaya GF et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0299; Wentzensen N et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0306.
Less-frequent cytologic testing, followed by hrHPV tests
George F. Sawaya, MD, from the University of California, San Francisco, and colleagues enrolled 451 English-speaking or Spanish-speaking women aged 21-65 years from women’s health clinics between September 2014 and June 2016. The women were mean 38 years old, and 57% were nonwhite women. The researchers examined utilities for 23 different health states associated with cervical cancer, and created a Markov decision model of type-specific high-risk human papillomavirus (hrHPV)–induced cervical carcinogenesis.
The researchers evaluated 12 screening strategies, which included the following scenarios:
- For women aged 21-65 years, cytologic testing every 3 years; if atypical squamous cells of undetermined significance (ASCUS) are found, repeat cytologic testing in 1 year or switch to immediate hrHPV triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with cytologic testing plus hrHPV testing (cotesting) for women 30-65 years old; if a normal cytologic test result and positive hrHPV test results, move to cotesting in 1 year or immediate genotyping triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with hrHPV testing alone every 3-5 years for women 30-65 years; if there are positive hrHPV results, move to immediate cytologic testing triage or immediate genotyping triage. Women with positive hrHPV and negative genotyping results receive additional cytologic testing triage.
In the strategies that switched the women from cytologic testing to hrHPV tests, the study also tested doing the switch at age 25 years rather than 30 years, the investigators reported.
Overall, with regard to cost, screening resulted in more cost savings ($1,267-$2,577) than not screening ($2,891 per woman). Women received the most benefit as measured by lifetime quality-adjusted life-years (QALY) if they received cytologic test every 3 years and received repeat testing for ASCUS. The strategy with the lowest cost was cytologic testing every 3 years and hrHPV triage for ASCUS ($1,267), and the strategy of 3-year cytology testing with repeat testing for ASCUS had more QALY but at a higher cost ($2,166). Other higher-cost strategies relative to QALYs included cotesting and primary hrHPV and also annual cytologic testing ($2,577).
“Both the American College of Obstetricians and Gynecologists and the American Cancer Society consider cotesting the preferred cervical cancer screening strategy, and the U.S. Preventive Services Task Force considers it an alternative strategy,” Dr. Sawaya and colleagues noted. “Our findings challenge these endorsements.”
“Our analyses suggest that it is not cost effective to begin primary hrHPV testing prior to age 30 years, to perform hrHPV testing every 3 years, or to perform cytologic testing annually. Comparative modeling is needed to confirm these findings,” they concluded.
Dual stain vs. cytologic testing alone
In a second study, Nicolas Wentzensen, MD, PhD, from the National Cancer Institute and colleagues performed a prospective observational study of 3,225 women who tested positive for human papillomavirus (HPV) who underwent p16/Ki-67 dual stain (DS) and HPV16/18 genotyping.
p16/Ki-67 DS was more effective at risk stratification for cervical intraepithelial neoplasia grade 3 or more severe neoplasia (CIN3+) than cytologic testing alone, and women with positive DS results had a higher risk of developing CIN3+ (12%) than did women with cytologic testing alone (10%; P = .005). Women who were HPV16/18 negative were the most likely to not have CIN3+ if they had negative DS results, and DS strategies resulted in fewer overall colposcopies relative to CIN3+ detections, compared with cytologic testing alone.
“We found that, for primary HPV screening, DS has both higher sensitivity and specificity compared with cytologic testing for triage of HPV-positive women Because of the greater reassurance of negative DS results, screening intervals can be extended compared with the screening intervals after negative cytologic results. Dual stain reduces unnecessary colposcopy referral and unnecessary cervical biopsies, and may reduce unnecessary treatment compared with Papanicolaou cytologic testing,” Dr. Wentzensen and colleagues concluded. “Our estimates of sensitivity, absolute risk, and colposcopy referral for various triage strategies can guide implementation of primary HPV screening.”
Five authors of Sawaya et al. reported receiving grants from the National Cancer Institute, and Dr. Megan J. Huchko reported receiving a grant from the University of California, San Francisco, during that study. That study was funded by a grant from the NCI. Six authors from Wentzensen et al. reported receiving grants from the NCI or being employed by the NCI or NIH. Dr. Philip E. Castle reported receiving low-cost or free cervical screening tests from Roche, Becton Dickinson, Cepheid, and Arbor Vita Corp. The other authors from both studies reported no relevant conflicts of interest.
SOURCES: Sawaya GF et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0299; Wentzensen N et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0306.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Current ways of testing women for cervical testing may be replaced in the near future.
Major finding: Two studies challenge existing recommendations on when women should be screened for cervical cancer and explore how to manage abnormal results.
Study details: It is not cost effective to begin primary hrHPV testing prior to age 30 years, to perform hrHPV testing every 3 years, or to perform cytologic testing annually. Dual stain reduces unnecessary colposcopy referral and unnecessary cervical biopsies, and may reduce unnecessary treatment, compared with Papanicolaou cytologic testing.
Disclosures: Five authors from Sawaya et al. reported receiving grants from the National Cancer Institute and Dr. Megan J. Huchko reported receiving a grant from the University of California, San Francisco, during that study. That study was funded by a grant from the NCI. Six authors from Wentzensen et al. reported receiving grants from the NCI or being employed by the NCI or National Institutes of Health. Dr. Philip E. Castle reported receiving low-cost or free cervical screening tests from Roche, Becton Dickinson, Cepheid, and Arbor Vita Corp. The other authors from both studies reported no relevant conflicts of interest.
Sources: Sawaya GF et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0299; Wentzensen N et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0306.
Better screening needed to reduce pregnancy-related overdose, death
reported Marcela C. Smid, MD, of the University of Utah, Salt Lake City, and her associates.
The stressful demands of newborn care, postpartum depression and anxiety, sleep deprivation, and other factors “may result in the ‘perfect storm’ leading to drug use, relapse, overdose, and death,” they cautioned.
Dr. Smid and associates conducted a retrospective cohort study of all pregnancy-associated deaths occurring in Utah between January 2005 and December 2014 using data from the Utah Perinatal Mortality Review Committee database. The authors defined pregnancy-associated deaths as those occurring during or within 1 year of the end of pregnancy, but not pregnancy related. A total of 136 pregnancy-associated deaths, including 69 pregnancy-related deaths, were identified.
During the 10-year span of the study, the three most common causes of pregnancy-associated deaths were drugs (n = 35, 26%), thromboembolic disease (n = 18, 13%), and automobile accidents (n = 17, 12%). The remainder of deaths in this group (n = 66, 49%) were caused by cardiac conditions, hypertension, infection, homicide or suicide, hemorrhage, malignancy, or other unspecified causes.
Over the study period, the authors observed a 76% increase in the pregnancy-associated mortality ratio; overall drug-induced pregnancy-associated mortality increased by 200% – from 4 in 2005 to 12 in 2014. About 77% of the drug-induced deaths were caused by opioids. Of the 35 women with drug-induced deaths, 54% were accidental overdoses, 26% were intentional, and the remaining 20% could not be determined.
Of key interest, a detailed review of the records showed that women were not systematically screened for drug use with validated screening tools. In fact, most women received no mental health or drug treatment, nor were they prescribed pharmacotherapy for the treatment of opioid use disorder. Those who died primarily in the late postpartum period and were known to have a drug-induced, pregnancy-associated death already had discontinued obstetrical health care. These findings are consistent with other published studies in Maryland and Georgia.
A 2018 study by Schiff et al. in Massachusetts reported a corresponding decrease in the rate of overdose deaths among those who were receiving pharmacotherapy, especially during the late postpartum period (Obstet Gynecol. 2018 Aug;132[2]:466-74). Dr. Smid and colleagues characterized their findings, in which those with drug-induced deaths were not receiving any kind of treatment, as “a missed opportunity for potentially lifesaving interventions.”
The authors considered their assessment of awareness of drug misuse prior to drug-induced death among obstetric health care providers to be their “unique contribution.” While the majority of women included in the study had known drug misuse or substance abuse disorder, for the 46% of who experienced drug-induced death, this use was not noted at any time during their obstetric care.
The primary limitations of the study were the inability to systematically capture insurance status or coverage lapses. The investigators also could not identify those who carried insurance at the time of their death or to what extent, if any, insurance status proved a barrier to access of mental health or addiction specialty care.
Although the Utah Perinatal Mortality Review Committee characterized 85% of drug-induced pregnancy-associated deaths as unpreventable between 2005 and 2014, new onset or exacerbations of conditions such as depression, anxiety, chronic pain, and substance use disorders generally have been acknowledged to occur both during pregnancy and post partum. Beginning in 2015, the committee began classifying drug-induced deaths as pregnancy related.
Dr. Smid and colleagues speculated that, with ongoing discussion of this topic at national mortality meetings, this kind of important change in classification may be implemented in other states in the future. Such a move would aid in determining the preventability of deaths, thereby leading to a growing awareness of and screening for drug use, both during and after pregnancy. Improved access to mental health and addiction services, as well as increased support for new mothers beyond the traditional 6-week postpartum visit, especially, would be highly beneficial.
Recommendations also have been recently published by the American College of Obstetricians and Gynecologists and the Council on Patient Safety in Women’s Health safety bundle committee on the care of pregnant and postpartum women with opioid use disorders. Separately, ACOG published a committee opinion that reconceptualizes “postpartum care as the extended ‘fourth trimester.’ ” It has further urged that “continued engagement and coordinated care for women with preexisting conditions, including substance use disorder and mental health conditions, is imperative” for reducing severe maternal morbidity and mortality.
“Our results support the mounting evidence that pregnant, and particularly postpartum, women with history of drug use and overdose, psychiatric comorbidities, prior suicide attempt, and polysubstance use need enhanced and ongoing care,” Dr. Smid and associates wrote.
They suggested that additional studies also are needed to better comprehend in what context pregnant and postpartum women are experiencing drug use, relapse, and overdose. “These studies are urgently needed to develop effective strategies to reduce the catastrophic event of maternal death.”
Dr. Smid is supported by Women’s Reproductive Health Research Career Development Program. The authors reported no other financial relationships or potential conflicts of interest.
SOURCE: Smid M et al. Obstet Gynecol. 2019;133:1131-40.
reported Marcela C. Smid, MD, of the University of Utah, Salt Lake City, and her associates.
The stressful demands of newborn care, postpartum depression and anxiety, sleep deprivation, and other factors “may result in the ‘perfect storm’ leading to drug use, relapse, overdose, and death,” they cautioned.
Dr. Smid and associates conducted a retrospective cohort study of all pregnancy-associated deaths occurring in Utah between January 2005 and December 2014 using data from the Utah Perinatal Mortality Review Committee database. The authors defined pregnancy-associated deaths as those occurring during or within 1 year of the end of pregnancy, but not pregnancy related. A total of 136 pregnancy-associated deaths, including 69 pregnancy-related deaths, were identified.
During the 10-year span of the study, the three most common causes of pregnancy-associated deaths were drugs (n = 35, 26%), thromboembolic disease (n = 18, 13%), and automobile accidents (n = 17, 12%). The remainder of deaths in this group (n = 66, 49%) were caused by cardiac conditions, hypertension, infection, homicide or suicide, hemorrhage, malignancy, or other unspecified causes.
Over the study period, the authors observed a 76% increase in the pregnancy-associated mortality ratio; overall drug-induced pregnancy-associated mortality increased by 200% – from 4 in 2005 to 12 in 2014. About 77% of the drug-induced deaths were caused by opioids. Of the 35 women with drug-induced deaths, 54% were accidental overdoses, 26% were intentional, and the remaining 20% could not be determined.
Of key interest, a detailed review of the records showed that women were not systematically screened for drug use with validated screening tools. In fact, most women received no mental health or drug treatment, nor were they prescribed pharmacotherapy for the treatment of opioid use disorder. Those who died primarily in the late postpartum period and were known to have a drug-induced, pregnancy-associated death already had discontinued obstetrical health care. These findings are consistent with other published studies in Maryland and Georgia.
A 2018 study by Schiff et al. in Massachusetts reported a corresponding decrease in the rate of overdose deaths among those who were receiving pharmacotherapy, especially during the late postpartum period (Obstet Gynecol. 2018 Aug;132[2]:466-74). Dr. Smid and colleagues characterized their findings, in which those with drug-induced deaths were not receiving any kind of treatment, as “a missed opportunity for potentially lifesaving interventions.”
The authors considered their assessment of awareness of drug misuse prior to drug-induced death among obstetric health care providers to be their “unique contribution.” While the majority of women included in the study had known drug misuse or substance abuse disorder, for the 46% of who experienced drug-induced death, this use was not noted at any time during their obstetric care.
The primary limitations of the study were the inability to systematically capture insurance status or coverage lapses. The investigators also could not identify those who carried insurance at the time of their death or to what extent, if any, insurance status proved a barrier to access of mental health or addiction specialty care.
Although the Utah Perinatal Mortality Review Committee characterized 85% of drug-induced pregnancy-associated deaths as unpreventable between 2005 and 2014, new onset or exacerbations of conditions such as depression, anxiety, chronic pain, and substance use disorders generally have been acknowledged to occur both during pregnancy and post partum. Beginning in 2015, the committee began classifying drug-induced deaths as pregnancy related.
Dr. Smid and colleagues speculated that, with ongoing discussion of this topic at national mortality meetings, this kind of important change in classification may be implemented in other states in the future. Such a move would aid in determining the preventability of deaths, thereby leading to a growing awareness of and screening for drug use, both during and after pregnancy. Improved access to mental health and addiction services, as well as increased support for new mothers beyond the traditional 6-week postpartum visit, especially, would be highly beneficial.
Recommendations also have been recently published by the American College of Obstetricians and Gynecologists and the Council on Patient Safety in Women’s Health safety bundle committee on the care of pregnant and postpartum women with opioid use disorders. Separately, ACOG published a committee opinion that reconceptualizes “postpartum care as the extended ‘fourth trimester.’ ” It has further urged that “continued engagement and coordinated care for women with preexisting conditions, including substance use disorder and mental health conditions, is imperative” for reducing severe maternal morbidity and mortality.
“Our results support the mounting evidence that pregnant, and particularly postpartum, women with history of drug use and overdose, psychiatric comorbidities, prior suicide attempt, and polysubstance use need enhanced and ongoing care,” Dr. Smid and associates wrote.
They suggested that additional studies also are needed to better comprehend in what context pregnant and postpartum women are experiencing drug use, relapse, and overdose. “These studies are urgently needed to develop effective strategies to reduce the catastrophic event of maternal death.”
Dr. Smid is supported by Women’s Reproductive Health Research Career Development Program. The authors reported no other financial relationships or potential conflicts of interest.
SOURCE: Smid M et al. Obstet Gynecol. 2019;133:1131-40.
reported Marcela C. Smid, MD, of the University of Utah, Salt Lake City, and her associates.
The stressful demands of newborn care, postpartum depression and anxiety, sleep deprivation, and other factors “may result in the ‘perfect storm’ leading to drug use, relapse, overdose, and death,” they cautioned.
Dr. Smid and associates conducted a retrospective cohort study of all pregnancy-associated deaths occurring in Utah between January 2005 and December 2014 using data from the Utah Perinatal Mortality Review Committee database. The authors defined pregnancy-associated deaths as those occurring during or within 1 year of the end of pregnancy, but not pregnancy related. A total of 136 pregnancy-associated deaths, including 69 pregnancy-related deaths, were identified.
During the 10-year span of the study, the three most common causes of pregnancy-associated deaths were drugs (n = 35, 26%), thromboembolic disease (n = 18, 13%), and automobile accidents (n = 17, 12%). The remainder of deaths in this group (n = 66, 49%) were caused by cardiac conditions, hypertension, infection, homicide or suicide, hemorrhage, malignancy, or other unspecified causes.
Over the study period, the authors observed a 76% increase in the pregnancy-associated mortality ratio; overall drug-induced pregnancy-associated mortality increased by 200% – from 4 in 2005 to 12 in 2014. About 77% of the drug-induced deaths were caused by opioids. Of the 35 women with drug-induced deaths, 54% were accidental overdoses, 26% were intentional, and the remaining 20% could not be determined.
Of key interest, a detailed review of the records showed that women were not systematically screened for drug use with validated screening tools. In fact, most women received no mental health or drug treatment, nor were they prescribed pharmacotherapy for the treatment of opioid use disorder. Those who died primarily in the late postpartum period and were known to have a drug-induced, pregnancy-associated death already had discontinued obstetrical health care. These findings are consistent with other published studies in Maryland and Georgia.
A 2018 study by Schiff et al. in Massachusetts reported a corresponding decrease in the rate of overdose deaths among those who were receiving pharmacotherapy, especially during the late postpartum period (Obstet Gynecol. 2018 Aug;132[2]:466-74). Dr. Smid and colleagues characterized their findings, in which those with drug-induced deaths were not receiving any kind of treatment, as “a missed opportunity for potentially lifesaving interventions.”
The authors considered their assessment of awareness of drug misuse prior to drug-induced death among obstetric health care providers to be their “unique contribution.” While the majority of women included in the study had known drug misuse or substance abuse disorder, for the 46% of who experienced drug-induced death, this use was not noted at any time during their obstetric care.
The primary limitations of the study were the inability to systematically capture insurance status or coverage lapses. The investigators also could not identify those who carried insurance at the time of their death or to what extent, if any, insurance status proved a barrier to access of mental health or addiction specialty care.
Although the Utah Perinatal Mortality Review Committee characterized 85% of drug-induced pregnancy-associated deaths as unpreventable between 2005 and 2014, new onset or exacerbations of conditions such as depression, anxiety, chronic pain, and substance use disorders generally have been acknowledged to occur both during pregnancy and post partum. Beginning in 2015, the committee began classifying drug-induced deaths as pregnancy related.
Dr. Smid and colleagues speculated that, with ongoing discussion of this topic at national mortality meetings, this kind of important change in classification may be implemented in other states in the future. Such a move would aid in determining the preventability of deaths, thereby leading to a growing awareness of and screening for drug use, both during and after pregnancy. Improved access to mental health and addiction services, as well as increased support for new mothers beyond the traditional 6-week postpartum visit, especially, would be highly beneficial.
Recommendations also have been recently published by the American College of Obstetricians and Gynecologists and the Council on Patient Safety in Women’s Health safety bundle committee on the care of pregnant and postpartum women with opioid use disorders. Separately, ACOG published a committee opinion that reconceptualizes “postpartum care as the extended ‘fourth trimester.’ ” It has further urged that “continued engagement and coordinated care for women with preexisting conditions, including substance use disorder and mental health conditions, is imperative” for reducing severe maternal morbidity and mortality.
“Our results support the mounting evidence that pregnant, and particularly postpartum, women with history of drug use and overdose, psychiatric comorbidities, prior suicide attempt, and polysubstance use need enhanced and ongoing care,” Dr. Smid and associates wrote.
They suggested that additional studies also are needed to better comprehend in what context pregnant and postpartum women are experiencing drug use, relapse, and overdose. “These studies are urgently needed to develop effective strategies to reduce the catastrophic event of maternal death.”
Dr. Smid is supported by Women’s Reproductive Health Research Career Development Program. The authors reported no other financial relationships or potential conflicts of interest.
SOURCE: Smid M et al. Obstet Gynecol. 2019;133:1131-40.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: Drug-induced death is the leading cause of pregnancy-associated death in Utah, primarily occurring in the late postpartum period.
Major finding: Despite known history, pregnant women were not systematically screened for drug use or treated for mental health disorders or drug misuse.
Study details: A retrospective cohort study of 136 pregnancy-associated deaths, of which 26% were drug induced.
Disclosures: Dr. Smid is supported by the Women’s Reproductive Health Research Career Development Program. The authors reported no other financial relationships or potential conflicts of interest.
Source: Smid M et al. Obstet Gynecol. 2019;133:1131-40.
Benzodiazepines nearly double the odds of spontaneous abortion
Early-pregnancy spontaneous abortion was almost twice as common among women who used benzodiazepines, according to 17 years’ worth of data from the Quebec Pregnancy Cohort, which prospectively collects data on all pregnancies of women covered by the Quebec Public Prescription Drug Insurance Plan.
The findings suggest the need for caution before prescribing benzodiazepines to treat insomnia and mood or anxiety disorders in early pregnancy. “Alternative nonpharmacologic treatments exist and are recommended, but if benzodiazepines are needed, they should be prescribed for short durations,” wrote Odile Sheehy, MSc, of the Research Center at Centre Hospitalier Universitaire Sainte-Justine, Montreal, and colleagues, in a study published in JAMA Psychiatry.
The researchers evaluated data from 27,149 study-eligible women who had a spontaneous abortion after 6 weeks’ gestation and before 20 weeks’ gestation between Jan. 1, 1998, and Dec. 31, 2015. Among filled prescriptions, at least one benzodiazepine was used by 375 (1.4%) of the women. These women were matched with five randomly selected control pregnancies per case. The data were adjusted for diagnoses of mood and anxiety disorders and insomnia as well as for several documented proxies of these diseases, such as concomitant exposure to antidepressants or antipsychotics, visits to a psychiatrist, comorbidities, and hospitalizations.
The investigators found an adjusted odds ratio (aOR) of 1.85 (95% confidence interval, 1.61-2.12) for benzodiazepine use. The odds of spontaneous abortion was increased with use of all types of benzodiazepines evaluated in the study, with aORs as low as 1.13 and as high as 3.43, as well as similar aORs between long-acting and short-acting benzodiazepines (1.81 vs. 1.73, respectively).
While the information is accurate regarding filled prescriptions, the findings might not apply to women with private drug insurance as the study included only women in a prescription drug program, the researchers said. They noted, however, that pregnant women receiving medication insurance from Quebec’s public system have characteristics and comorbidities similar to those of women who are covered by private medication insurance.
One author reported being a consultant for plaintiffs in litigations involving antidepressants and birth defects. No other disclosures were reported.
SOURCE: Sheehy O et al. JAMA Psychiatry. 2019 May 15. doi: 10.1001/jamapsychiatry.2019.0963.
Early-pregnancy spontaneous abortion was almost twice as common among women who used benzodiazepines, according to 17 years’ worth of data from the Quebec Pregnancy Cohort, which prospectively collects data on all pregnancies of women covered by the Quebec Public Prescription Drug Insurance Plan.
The findings suggest the need for caution before prescribing benzodiazepines to treat insomnia and mood or anxiety disorders in early pregnancy. “Alternative nonpharmacologic treatments exist and are recommended, but if benzodiazepines are needed, they should be prescribed for short durations,” wrote Odile Sheehy, MSc, of the Research Center at Centre Hospitalier Universitaire Sainte-Justine, Montreal, and colleagues, in a study published in JAMA Psychiatry.
The researchers evaluated data from 27,149 study-eligible women who had a spontaneous abortion after 6 weeks’ gestation and before 20 weeks’ gestation between Jan. 1, 1998, and Dec. 31, 2015. Among filled prescriptions, at least one benzodiazepine was used by 375 (1.4%) of the women. These women were matched with five randomly selected control pregnancies per case. The data were adjusted for diagnoses of mood and anxiety disorders and insomnia as well as for several documented proxies of these diseases, such as concomitant exposure to antidepressants or antipsychotics, visits to a psychiatrist, comorbidities, and hospitalizations.
The investigators found an adjusted odds ratio (aOR) of 1.85 (95% confidence interval, 1.61-2.12) for benzodiazepine use. The odds of spontaneous abortion was increased with use of all types of benzodiazepines evaluated in the study, with aORs as low as 1.13 and as high as 3.43, as well as similar aORs between long-acting and short-acting benzodiazepines (1.81 vs. 1.73, respectively).
While the information is accurate regarding filled prescriptions, the findings might not apply to women with private drug insurance as the study included only women in a prescription drug program, the researchers said. They noted, however, that pregnant women receiving medication insurance from Quebec’s public system have characteristics and comorbidities similar to those of women who are covered by private medication insurance.
One author reported being a consultant for plaintiffs in litigations involving antidepressants and birth defects. No other disclosures were reported.
SOURCE: Sheehy O et al. JAMA Psychiatry. 2019 May 15. doi: 10.1001/jamapsychiatry.2019.0963.
Early-pregnancy spontaneous abortion was almost twice as common among women who used benzodiazepines, according to 17 years’ worth of data from the Quebec Pregnancy Cohort, which prospectively collects data on all pregnancies of women covered by the Quebec Public Prescription Drug Insurance Plan.
The findings suggest the need for caution before prescribing benzodiazepines to treat insomnia and mood or anxiety disorders in early pregnancy. “Alternative nonpharmacologic treatments exist and are recommended, but if benzodiazepines are needed, they should be prescribed for short durations,” wrote Odile Sheehy, MSc, of the Research Center at Centre Hospitalier Universitaire Sainte-Justine, Montreal, and colleagues, in a study published in JAMA Psychiatry.
The researchers evaluated data from 27,149 study-eligible women who had a spontaneous abortion after 6 weeks’ gestation and before 20 weeks’ gestation between Jan. 1, 1998, and Dec. 31, 2015. Among filled prescriptions, at least one benzodiazepine was used by 375 (1.4%) of the women. These women were matched with five randomly selected control pregnancies per case. The data were adjusted for diagnoses of mood and anxiety disorders and insomnia as well as for several documented proxies of these diseases, such as concomitant exposure to antidepressants or antipsychotics, visits to a psychiatrist, comorbidities, and hospitalizations.
The investigators found an adjusted odds ratio (aOR) of 1.85 (95% confidence interval, 1.61-2.12) for benzodiazepine use. The odds of spontaneous abortion was increased with use of all types of benzodiazepines evaluated in the study, with aORs as low as 1.13 and as high as 3.43, as well as similar aORs between long-acting and short-acting benzodiazepines (1.81 vs. 1.73, respectively).
While the information is accurate regarding filled prescriptions, the findings might not apply to women with private drug insurance as the study included only women in a prescription drug program, the researchers said. They noted, however, that pregnant women receiving medication insurance from Quebec’s public system have characteristics and comorbidities similar to those of women who are covered by private medication insurance.
One author reported being a consultant for plaintiffs in litigations involving antidepressants and birth defects. No other disclosures were reported.
SOURCE: Sheehy O et al. JAMA Psychiatry. 2019 May 15. doi: 10.1001/jamapsychiatry.2019.0963.
FROM JAMA PSYCHIATRY
Treatment Guidelines for Pregnant Native Women With Opioid Use Disorder
To provide better “culturally responsive” care, the IHS and American College of Obstetricians and Gynecologists (ACOG) have announced new clinical recommendations for health care providers (HCPs) who treat Native American pregnant woman and women of childbearing age with opioid use disorder (OUD).
There are no current comprehensive guidelines to manage the care of pregnant women with opioid dependence who live in rural or remote communities, ACOG acknowledges. That absence, in addition to a lack of resources, lack of training in treating substance use disorder in pregnancy, and providers’ discomfort with opioid agonist therapy in pregnancy, has contributed to “wide variation in the quality of care these women receive.”
Disparities are particularly extreme for American Indian and Alaska Native women (AI/AN), ACOG notes. They have the highest risk of dying of prescription opioid overdose, and they face specific barriers to accessing treatment. For instance, there are few opioid treatment programs offering methadone treatment on tribal lands.
The new recommendations were developed in partnership with tribes and ACOG’s Committee on American Indian and Alaska Native Women’s Health, based on critical feedback from listening sessions and tribal consultations in the past year. The specific guidelines are tailored for Native women.
The committee recognizes, it says, the “necessary wide-ranging scope of treatment for OUD, especially among AI/AN childbearing women.” Key recommendations include strategies to avoid or minimize the use of opioids for pain management and encourage alternative pain therapies, such as physical therapy, acupuncture, and mindfulness-based therapy. In pregnancy, ACOG recommends that obstetric providers perform universal screening and brief intervention using a validated tool as early in prenatal care as possible.
Treatment may require management of co-occurring polysubstance use disorders; concomitant alcohol and methamphetamine use predominate in many tribal areas. HCPs also may need to offer personalized care that “acknowledges the contributions of intergenerational and personal trauma,” the guidelines say. Trauma-informed interdisciplinary approaches to posttraumatic stress disorder that engage tribal resources, social structures, and assets are “crucial to impactful care of opioid use disorder.”
The postpartum period is associated with a high rate of relapse, ACOG says. Histories of trauma, for instance, can exacerbate mood disorders. Moreover, substance use and overdose are increasingly being recognized as key contributors to pregnancy-associated death in the US; a disproportionate share of deaths are postpartum. Infants of untreated, depressed mothers demonstrate poor outcomes, including impaired motor adaptation and self-regulation, developmental delay, and higher arousal scores. The guidelines advise treating mothers and infants as dyads to improve the course of neonatal opioid withdrawal syndrome (NOWS). The proportion of infants with NOWS who need pharmacologic treatment has risen dramatically, the committee notes.
“[I]t is clear from our site visits and clinical experience,” the committee members note, “that adaptation of systems for integration and reach in rural settings is necessary, with potentially different needs and assets in Native and rural populations.” Native culture and traditions, they add, offer opportunities for community engagement and support that can be integrated into medical care for the women and their infants.
To provide better “culturally responsive” care, the IHS and American College of Obstetricians and Gynecologists (ACOG) have announced new clinical recommendations for health care providers (HCPs) who treat Native American pregnant woman and women of childbearing age with opioid use disorder (OUD).
There are no current comprehensive guidelines to manage the care of pregnant women with opioid dependence who live in rural or remote communities, ACOG acknowledges. That absence, in addition to a lack of resources, lack of training in treating substance use disorder in pregnancy, and providers’ discomfort with opioid agonist therapy in pregnancy, has contributed to “wide variation in the quality of care these women receive.”
Disparities are particularly extreme for American Indian and Alaska Native women (AI/AN), ACOG notes. They have the highest risk of dying of prescription opioid overdose, and they face specific barriers to accessing treatment. For instance, there are few opioid treatment programs offering methadone treatment on tribal lands.
The new recommendations were developed in partnership with tribes and ACOG’s Committee on American Indian and Alaska Native Women’s Health, based on critical feedback from listening sessions and tribal consultations in the past year. The specific guidelines are tailored for Native women.
The committee recognizes, it says, the “necessary wide-ranging scope of treatment for OUD, especially among AI/AN childbearing women.” Key recommendations include strategies to avoid or minimize the use of opioids for pain management and encourage alternative pain therapies, such as physical therapy, acupuncture, and mindfulness-based therapy. In pregnancy, ACOG recommends that obstetric providers perform universal screening and brief intervention using a validated tool as early in prenatal care as possible.
Treatment may require management of co-occurring polysubstance use disorders; concomitant alcohol and methamphetamine use predominate in many tribal areas. HCPs also may need to offer personalized care that “acknowledges the contributions of intergenerational and personal trauma,” the guidelines say. Trauma-informed interdisciplinary approaches to posttraumatic stress disorder that engage tribal resources, social structures, and assets are “crucial to impactful care of opioid use disorder.”
The postpartum period is associated with a high rate of relapse, ACOG says. Histories of trauma, for instance, can exacerbate mood disorders. Moreover, substance use and overdose are increasingly being recognized as key contributors to pregnancy-associated death in the US; a disproportionate share of deaths are postpartum. Infants of untreated, depressed mothers demonstrate poor outcomes, including impaired motor adaptation and self-regulation, developmental delay, and higher arousal scores. The guidelines advise treating mothers and infants as dyads to improve the course of neonatal opioid withdrawal syndrome (NOWS). The proportion of infants with NOWS who need pharmacologic treatment has risen dramatically, the committee notes.
“[I]t is clear from our site visits and clinical experience,” the committee members note, “that adaptation of systems for integration and reach in rural settings is necessary, with potentially different needs and assets in Native and rural populations.” Native culture and traditions, they add, offer opportunities for community engagement and support that can be integrated into medical care for the women and their infants.
To provide better “culturally responsive” care, the IHS and American College of Obstetricians and Gynecologists (ACOG) have announced new clinical recommendations for health care providers (HCPs) who treat Native American pregnant woman and women of childbearing age with opioid use disorder (OUD).
There are no current comprehensive guidelines to manage the care of pregnant women with opioid dependence who live in rural or remote communities, ACOG acknowledges. That absence, in addition to a lack of resources, lack of training in treating substance use disorder in pregnancy, and providers’ discomfort with opioid agonist therapy in pregnancy, has contributed to “wide variation in the quality of care these women receive.”
Disparities are particularly extreme for American Indian and Alaska Native women (AI/AN), ACOG notes. They have the highest risk of dying of prescription opioid overdose, and they face specific barriers to accessing treatment. For instance, there are few opioid treatment programs offering methadone treatment on tribal lands.
The new recommendations were developed in partnership with tribes and ACOG’s Committee on American Indian and Alaska Native Women’s Health, based on critical feedback from listening sessions and tribal consultations in the past year. The specific guidelines are tailored for Native women.
The committee recognizes, it says, the “necessary wide-ranging scope of treatment for OUD, especially among AI/AN childbearing women.” Key recommendations include strategies to avoid or minimize the use of opioids for pain management and encourage alternative pain therapies, such as physical therapy, acupuncture, and mindfulness-based therapy. In pregnancy, ACOG recommends that obstetric providers perform universal screening and brief intervention using a validated tool as early in prenatal care as possible.
Treatment may require management of co-occurring polysubstance use disorders; concomitant alcohol and methamphetamine use predominate in many tribal areas. HCPs also may need to offer personalized care that “acknowledges the contributions of intergenerational and personal trauma,” the guidelines say. Trauma-informed interdisciplinary approaches to posttraumatic stress disorder that engage tribal resources, social structures, and assets are “crucial to impactful care of opioid use disorder.”
The postpartum period is associated with a high rate of relapse, ACOG says. Histories of trauma, for instance, can exacerbate mood disorders. Moreover, substance use and overdose are increasingly being recognized as key contributors to pregnancy-associated death in the US; a disproportionate share of deaths are postpartum. Infants of untreated, depressed mothers demonstrate poor outcomes, including impaired motor adaptation and self-regulation, developmental delay, and higher arousal scores. The guidelines advise treating mothers and infants as dyads to improve the course of neonatal opioid withdrawal syndrome (NOWS). The proportion of infants with NOWS who need pharmacologic treatment has risen dramatically, the committee notes.
“[I]t is clear from our site visits and clinical experience,” the committee members note, “that adaptation of systems for integration and reach in rural settings is necessary, with potentially different needs and assets in Native and rural populations.” Native culture and traditions, they add, offer opportunities for community engagement and support that can be integrated into medical care for the women and their infants.
Immediate postpartum LARC: ‘Agony and ecstasy’
NASHVILLE, TENN. – according to Eve Espey, MD.
“I think [the rate] is going to settle out at around 15%-20%, but good cost-effectiveness studies show that, even if it were that high, it is still highly cost effective,” she said during an update on contraceptives at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Immediate postpartum long-acting reversible contraception (LARC), including an IUD or implant, may reduce rapid-repeat pregnancy, she added, noting, however, that while Medicaid is covering it in many states, “it turns out that payment models are very cumbersome; they actually don’t work very well.”
At the University of New Mexico (UNM) in Albuquerque, where Dr .Espey is a professor and chair of the department of obstetrics and gynecology and director of the family planning fellowship, immediate postpartum LARC is offered to women with Medicaid coverage, and payment is received in about 97% of cases.
It took about 4 years of persistent effort to make that happen, she said, adding that the UNM Hospital still is the only one in the state offering the service, although efforts are underway to help other hospitals “troubleshoot the issues.”
Another challenge is the lack of private insurance coverage for immediate postpartum LARC, she said.
“I was super enthusiastic about this a few years ago, and I remain super enthusiastic about it, but I think it’s going to take another 5 years or so [for better coverage], and honestly I think what we really need is an inpatient LARC CPT code to make this happen.”
In this video interview, Dr. Espey discusses the “agony and ecstasy” of immediate postpartum LARC, summarizing the main points regarding its benefits and challenges as presented during an “EdTalk” she gave at the meeting.
Dr. Espey reported having no relevant financial disclosures.
NASHVILLE, TENN. – according to Eve Espey, MD.
“I think [the rate] is going to settle out at around 15%-20%, but good cost-effectiveness studies show that, even if it were that high, it is still highly cost effective,” she said during an update on contraceptives at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Immediate postpartum long-acting reversible contraception (LARC), including an IUD or implant, may reduce rapid-repeat pregnancy, she added, noting, however, that while Medicaid is covering it in many states, “it turns out that payment models are very cumbersome; they actually don’t work very well.”
At the University of New Mexico (UNM) in Albuquerque, where Dr .Espey is a professor and chair of the department of obstetrics and gynecology and director of the family planning fellowship, immediate postpartum LARC is offered to women with Medicaid coverage, and payment is received in about 97% of cases.
It took about 4 years of persistent effort to make that happen, she said, adding that the UNM Hospital still is the only one in the state offering the service, although efforts are underway to help other hospitals “troubleshoot the issues.”
Another challenge is the lack of private insurance coverage for immediate postpartum LARC, she said.
“I was super enthusiastic about this a few years ago, and I remain super enthusiastic about it, but I think it’s going to take another 5 years or so [for better coverage], and honestly I think what we really need is an inpatient LARC CPT code to make this happen.”
In this video interview, Dr. Espey discusses the “agony and ecstasy” of immediate postpartum LARC, summarizing the main points regarding its benefits and challenges as presented during an “EdTalk” she gave at the meeting.
Dr. Espey reported having no relevant financial disclosures.
NASHVILLE, TENN. – according to Eve Espey, MD.
“I think [the rate] is going to settle out at around 15%-20%, but good cost-effectiveness studies show that, even if it were that high, it is still highly cost effective,” she said during an update on contraceptives at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Immediate postpartum long-acting reversible contraception (LARC), including an IUD or implant, may reduce rapid-repeat pregnancy, she added, noting, however, that while Medicaid is covering it in many states, “it turns out that payment models are very cumbersome; they actually don’t work very well.”
At the University of New Mexico (UNM) in Albuquerque, where Dr .Espey is a professor and chair of the department of obstetrics and gynecology and director of the family planning fellowship, immediate postpartum LARC is offered to women with Medicaid coverage, and payment is received in about 97% of cases.
It took about 4 years of persistent effort to make that happen, she said, adding that the UNM Hospital still is the only one in the state offering the service, although efforts are underway to help other hospitals “troubleshoot the issues.”
Another challenge is the lack of private insurance coverage for immediate postpartum LARC, she said.
“I was super enthusiastic about this a few years ago, and I remain super enthusiastic about it, but I think it’s going to take another 5 years or so [for better coverage], and honestly I think what we really need is an inpatient LARC CPT code to make this happen.”
In this video interview, Dr. Espey discusses the “agony and ecstasy” of immediate postpartum LARC, summarizing the main points regarding its benefits and challenges as presented during an “EdTalk” she gave at the meeting.
Dr. Espey reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM ACOG 2019
Antiabortion measures may lead to Supreme Court showdown
The debate over abortion rights could be headed to the U.S. Supreme Court after two recent state measures that aim to restrict access to abortion.
On May 7, 2019, Georgia Gov. Brian Kemp (R) signed into law a statute that bars physicians from performing an abortion after a heartbeat is detected – usually at about 6 weeks of pregnancy. The law allows exceptions if the pregnancy poses death or serious harm to the woman, and in cases of rape or incest.
A week later, the Alabama Senate on May 14 approved a measure that would ban abortion at every pregnancy stage and penalize physicians with a Class A felony for performing an abortion and charge them with a Class C felony for attempting to perform an abortion. The Alabama bill includes an exception if a woman’s life is at risk, but not for cases of rape or incest. Alabama Gov. Kay Ivey (R) signed the bill into law on May 15.
Both measures will likely be challenged in court; the Alabama law, in particular, could land in front of the U.S. Supreme Court as a direct challenge to Roe v. Wade.
Abortion critics have been encouraged by the Supreme Court appointment of right-leaning Associate Justice Brett M. Kavanaugh and hope the Alabama measure will drive the Supreme Court to reconsider its central holding in Roe, according to Fatima Goss Graves, president of the National Women’s Law Center, a liberal-leaning legal firm that advocates gender equality.
“After decades of chipping away at Roe, antiabortion legislators and advocates are feeling emboldened with the addition of Justice Kavanaugh on the Supreme Court and they are exposing their true goal – to ban abortion altogether,” Ms. Graves said in a statement. “And make no mistake, [passage of the Alabama bill] is extreme overreach: The vast majority of people in this country do not support criminalizing women or doctors and want abortion to be safe and legal.”
National antiabortion group Susan B. Anthony List called Alabama’s measure a landmark victory and indicated that the bill passage may ultimately change the outcome of Roe v. Wade.
“Across the nation there is growing momentum, informed by science and compassion, and spurred on in reaction to abortion extremism in New York and Virginia, to recognize the humanity of the unborn child in the law,” Susan B. Anthony List President Marjorie Dannenfelser said in a statement. “It is clearer than ever that Roe is far from being settled law in the eyes and hearts of the American people, and this is increasingly reflected in state legislatures. ... The time is coming for the Supreme Court to let that debate go forward.”
Other states have recently passed laws similar to Georgia’s measure, dubbed the “fetal heartbeat bills,” including Kentucky, Mississippi, and Ohio.
On May 15, the American Civil Liberties Union and Planned Parenthood of Greater Ohio issued a joint legal challenge against Ohio’s law, calling it blatantly unconstitutional. Meanwhile, the Center for Reproductive Rights has pledged to sue Georgia over its law.
Ted Anderson, MD, president of the American College of Obstetricians and Gynecologists, said the many recent restrictions to abortion access across the country are harmful to women’s health and detrimental to the physician-patient relationship.
“Lawmakers must support health policies based on sound science and evidence. Politicians must seek to improve access to care, not restrict it,” Dr. Anderson said in a statement. “Legislative restrictions fundamentally interfere with the patient-provider relationship and decrease access to necessary care for all women, and particularly for low-income women and those living long distances from health care providers. Health care decisions should be made jointly only by patients and their trusted health care professionals, not by politicians.”
The debate over abortion rights could be headed to the U.S. Supreme Court after two recent state measures that aim to restrict access to abortion.
On May 7, 2019, Georgia Gov. Brian Kemp (R) signed into law a statute that bars physicians from performing an abortion after a heartbeat is detected – usually at about 6 weeks of pregnancy. The law allows exceptions if the pregnancy poses death or serious harm to the woman, and in cases of rape or incest.
A week later, the Alabama Senate on May 14 approved a measure that would ban abortion at every pregnancy stage and penalize physicians with a Class A felony for performing an abortion and charge them with a Class C felony for attempting to perform an abortion. The Alabama bill includes an exception if a woman’s life is at risk, but not for cases of rape or incest. Alabama Gov. Kay Ivey (R) signed the bill into law on May 15.
Both measures will likely be challenged in court; the Alabama law, in particular, could land in front of the U.S. Supreme Court as a direct challenge to Roe v. Wade.
Abortion critics have been encouraged by the Supreme Court appointment of right-leaning Associate Justice Brett M. Kavanaugh and hope the Alabama measure will drive the Supreme Court to reconsider its central holding in Roe, according to Fatima Goss Graves, president of the National Women’s Law Center, a liberal-leaning legal firm that advocates gender equality.
“After decades of chipping away at Roe, antiabortion legislators and advocates are feeling emboldened with the addition of Justice Kavanaugh on the Supreme Court and they are exposing their true goal – to ban abortion altogether,” Ms. Graves said in a statement. “And make no mistake, [passage of the Alabama bill] is extreme overreach: The vast majority of people in this country do not support criminalizing women or doctors and want abortion to be safe and legal.”
National antiabortion group Susan B. Anthony List called Alabama’s measure a landmark victory and indicated that the bill passage may ultimately change the outcome of Roe v. Wade.
“Across the nation there is growing momentum, informed by science and compassion, and spurred on in reaction to abortion extremism in New York and Virginia, to recognize the humanity of the unborn child in the law,” Susan B. Anthony List President Marjorie Dannenfelser said in a statement. “It is clearer than ever that Roe is far from being settled law in the eyes and hearts of the American people, and this is increasingly reflected in state legislatures. ... The time is coming for the Supreme Court to let that debate go forward.”
Other states have recently passed laws similar to Georgia’s measure, dubbed the “fetal heartbeat bills,” including Kentucky, Mississippi, and Ohio.
On May 15, the American Civil Liberties Union and Planned Parenthood of Greater Ohio issued a joint legal challenge against Ohio’s law, calling it blatantly unconstitutional. Meanwhile, the Center for Reproductive Rights has pledged to sue Georgia over its law.
Ted Anderson, MD, president of the American College of Obstetricians and Gynecologists, said the many recent restrictions to abortion access across the country are harmful to women’s health and detrimental to the physician-patient relationship.
“Lawmakers must support health policies based on sound science and evidence. Politicians must seek to improve access to care, not restrict it,” Dr. Anderson said in a statement. “Legislative restrictions fundamentally interfere with the patient-provider relationship and decrease access to necessary care for all women, and particularly for low-income women and those living long distances from health care providers. Health care decisions should be made jointly only by patients and their trusted health care professionals, not by politicians.”
The debate over abortion rights could be headed to the U.S. Supreme Court after two recent state measures that aim to restrict access to abortion.
On May 7, 2019, Georgia Gov. Brian Kemp (R) signed into law a statute that bars physicians from performing an abortion after a heartbeat is detected – usually at about 6 weeks of pregnancy. The law allows exceptions if the pregnancy poses death or serious harm to the woman, and in cases of rape or incest.
A week later, the Alabama Senate on May 14 approved a measure that would ban abortion at every pregnancy stage and penalize physicians with a Class A felony for performing an abortion and charge them with a Class C felony for attempting to perform an abortion. The Alabama bill includes an exception if a woman’s life is at risk, but not for cases of rape or incest. Alabama Gov. Kay Ivey (R) signed the bill into law on May 15.
Both measures will likely be challenged in court; the Alabama law, in particular, could land in front of the U.S. Supreme Court as a direct challenge to Roe v. Wade.
Abortion critics have been encouraged by the Supreme Court appointment of right-leaning Associate Justice Brett M. Kavanaugh and hope the Alabama measure will drive the Supreme Court to reconsider its central holding in Roe, according to Fatima Goss Graves, president of the National Women’s Law Center, a liberal-leaning legal firm that advocates gender equality.
“After decades of chipping away at Roe, antiabortion legislators and advocates are feeling emboldened with the addition of Justice Kavanaugh on the Supreme Court and they are exposing their true goal – to ban abortion altogether,” Ms. Graves said in a statement. “And make no mistake, [passage of the Alabama bill] is extreme overreach: The vast majority of people in this country do not support criminalizing women or doctors and want abortion to be safe and legal.”
National antiabortion group Susan B. Anthony List called Alabama’s measure a landmark victory and indicated that the bill passage may ultimately change the outcome of Roe v. Wade.
“Across the nation there is growing momentum, informed by science and compassion, and spurred on in reaction to abortion extremism in New York and Virginia, to recognize the humanity of the unborn child in the law,” Susan B. Anthony List President Marjorie Dannenfelser said in a statement. “It is clearer than ever that Roe is far from being settled law in the eyes and hearts of the American people, and this is increasingly reflected in state legislatures. ... The time is coming for the Supreme Court to let that debate go forward.”
Other states have recently passed laws similar to Georgia’s measure, dubbed the “fetal heartbeat bills,” including Kentucky, Mississippi, and Ohio.
On May 15, the American Civil Liberties Union and Planned Parenthood of Greater Ohio issued a joint legal challenge against Ohio’s law, calling it blatantly unconstitutional. Meanwhile, the Center for Reproductive Rights has pledged to sue Georgia over its law.
Ted Anderson, MD, president of the American College of Obstetricians and Gynecologists, said the many recent restrictions to abortion access across the country are harmful to women’s health and detrimental to the physician-patient relationship.
“Lawmakers must support health policies based on sound science and evidence. Politicians must seek to improve access to care, not restrict it,” Dr. Anderson said in a statement. “Legislative restrictions fundamentally interfere with the patient-provider relationship and decrease access to necessary care for all women, and particularly for low-income women and those living long distances from health care providers. Health care decisions should be made jointly only by patients and their trusted health care professionals, not by politicians.”
Study finds link between intrahepatic cholestasis of pregnancy and risk of NAFLD
Patients with intrahepatic cholestasis of pregnancy (ICP) were nearly six times more likely to have a diagnosis of nonalcoholic fatty liver disease (NAFLD) than were controls, results from a retrospective, single-center study demonstrated.
“If this connection is confirmed with future studies, intrahepatic cholestasis of pregnancy may prove a novel model through which to investigate bile acid metabolism in patients with fatty liver disease,” one of the study authors, Tatyana Kushner, MD, MSCE, said during a media briefing in advance of the annual Digestive Disease Week. “This could have implications for future management of fatty liver disease. Additionally, these findings suggest that ICP patients should be seen by a liver specialist because they may go on to develop chronic liver disease or may already have already existing underlying liver disease.”
ICP is characterized by a build-up of bile acids during pregnancy and is associated with an increased risk of negative fetal outcomes and fetal death if left untreated, said Dr. Kushner, of the division of liver diseases at the Icahn School of Medicine at Mount Sinai, New York. The most notable symptom during pregnancy is severe pruritus. In what is believed to be the first study of its kind, Dr. Kushner and colleagues set out to evaluate the association between ICP and NAFLD and associated metabolic risk factors, including obesity, dyslipidemia, hypertension, and diabetes. Between January and December of 2017, they drew from the electronic medical records of a New York City health system to identify 149 pregnancies complicated by ICP and compared them to a control group of 200 pregnancies without an ICP diagnosis. The researchers used Pearson’s chi-square or Fisher’s exact test and Wilcoxon rank-sum tests to evaluate association of ICP with categorical variables and continuous variables, respectively, and unadjusted odds ratios to compare the ICP and control groups for clinically significant outcomes.
The median age of the study population was 30 years, their mean body mass index was 27.5 kg/m2, and there was a higher proportion of Hispanic women in the ICP group, compared with the control group (75% vs. 62%, respectively). Dr. Kushner and colleagues found that Hispanic women were nearly twice as likely to be diagnosed with ICP than non-Hispanic women (OR, 1.90; 95% confidence interval, 1.87-3.03). However, patients in both the ICP and control groups were similar for median age (OR, 1.02; 95% CI, 0.99-1.06), nulliparity (OR, 0.79; 95% CI, 0.48-1.30), and prevalence of hepatitis C (OR, 1.35; 95% CI, 0.08-21.67). The two groups were also similar for certain metabolic risk factors, including prevalence of obesity (OR, 1.01; 95% CI, 0.62-1.61), hypertension (OR, 0.69; 95% CI, 0.31-1.52), hemoglobin A1c greater than 5.5% (OR, 0.80; 95% CI, 0.34-1.9), and total cholesterol above 200 mg/dL (OR, 4.15; 95% CI, 0.83-20.84). Median bile acid levels were 30.6 micromoles (interquartile range, 11.6, 32.7) in the ICP group.
Compared with patients in the control group, those in the ICP group had higher median levels of alanine aminotransferase (ALT) (32 vs. 16 U/L; P less than .0001), alkaline phosphatase (181 vs. 128 U/L; P less than .0001), and total bilirubin (0.5 vs. 0.35 mg/dL; P less than .0001). ICP patients were also more likely than their counterparts to have ALT levels above 50 U/L (two times the upper limit of normal; OR, 3.22; 95% CI, 1.48-7.03), a history of biliary disease (OR, 3.29; 95% CI, 1.39-7.80), and to have evidence of steatosis on liver imaging (OR, 4.69; 95% CI, 1.68-13.12). When the researchers evaluated a diagnosis of NAFLD based on ICD-10 codes or evidence of steatosis on liver imaging, ICP patients were significantly more likely to have a diagnosis of NAFLD than controls (OR, 5.7; 95% CI, 2.08-15.65).
“We recommend additional research to look at differences in NAFLD progression in women who had NAFLD and were later diagnosed with ICP, compared to women with NAFLD who did not go on to develop ICP, because that may be a reflection of the role that bile acid metabolism plays in these particular patients,” Dr. Kushner said.
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
The study’s primary author was Erica Monrose, MD. The researchers reported having no financial disclosures.
SOURCE: Monrose E et al. DDW 2019, Abstract Sa1562.
Patients with intrahepatic cholestasis of pregnancy (ICP) were nearly six times more likely to have a diagnosis of nonalcoholic fatty liver disease (NAFLD) than were controls, results from a retrospective, single-center study demonstrated.
“If this connection is confirmed with future studies, intrahepatic cholestasis of pregnancy may prove a novel model through which to investigate bile acid metabolism in patients with fatty liver disease,” one of the study authors, Tatyana Kushner, MD, MSCE, said during a media briefing in advance of the annual Digestive Disease Week. “This could have implications for future management of fatty liver disease. Additionally, these findings suggest that ICP patients should be seen by a liver specialist because they may go on to develop chronic liver disease or may already have already existing underlying liver disease.”
ICP is characterized by a build-up of bile acids during pregnancy and is associated with an increased risk of negative fetal outcomes and fetal death if left untreated, said Dr. Kushner, of the division of liver diseases at the Icahn School of Medicine at Mount Sinai, New York. The most notable symptom during pregnancy is severe pruritus. In what is believed to be the first study of its kind, Dr. Kushner and colleagues set out to evaluate the association between ICP and NAFLD and associated metabolic risk factors, including obesity, dyslipidemia, hypertension, and diabetes. Between January and December of 2017, they drew from the electronic medical records of a New York City health system to identify 149 pregnancies complicated by ICP and compared them to a control group of 200 pregnancies without an ICP diagnosis. The researchers used Pearson’s chi-square or Fisher’s exact test and Wilcoxon rank-sum tests to evaluate association of ICP with categorical variables and continuous variables, respectively, and unadjusted odds ratios to compare the ICP and control groups for clinically significant outcomes.
The median age of the study population was 30 years, their mean body mass index was 27.5 kg/m2, and there was a higher proportion of Hispanic women in the ICP group, compared with the control group (75% vs. 62%, respectively). Dr. Kushner and colleagues found that Hispanic women were nearly twice as likely to be diagnosed with ICP than non-Hispanic women (OR, 1.90; 95% confidence interval, 1.87-3.03). However, patients in both the ICP and control groups were similar for median age (OR, 1.02; 95% CI, 0.99-1.06), nulliparity (OR, 0.79; 95% CI, 0.48-1.30), and prevalence of hepatitis C (OR, 1.35; 95% CI, 0.08-21.67). The two groups were also similar for certain metabolic risk factors, including prevalence of obesity (OR, 1.01; 95% CI, 0.62-1.61), hypertension (OR, 0.69; 95% CI, 0.31-1.52), hemoglobin A1c greater than 5.5% (OR, 0.80; 95% CI, 0.34-1.9), and total cholesterol above 200 mg/dL (OR, 4.15; 95% CI, 0.83-20.84). Median bile acid levels were 30.6 micromoles (interquartile range, 11.6, 32.7) in the ICP group.
Compared with patients in the control group, those in the ICP group had higher median levels of alanine aminotransferase (ALT) (32 vs. 16 U/L; P less than .0001), alkaline phosphatase (181 vs. 128 U/L; P less than .0001), and total bilirubin (0.5 vs. 0.35 mg/dL; P less than .0001). ICP patients were also more likely than their counterparts to have ALT levels above 50 U/L (two times the upper limit of normal; OR, 3.22; 95% CI, 1.48-7.03), a history of biliary disease (OR, 3.29; 95% CI, 1.39-7.80), and to have evidence of steatosis on liver imaging (OR, 4.69; 95% CI, 1.68-13.12). When the researchers evaluated a diagnosis of NAFLD based on ICD-10 codes or evidence of steatosis on liver imaging, ICP patients were significantly more likely to have a diagnosis of NAFLD than controls (OR, 5.7; 95% CI, 2.08-15.65).
“We recommend additional research to look at differences in NAFLD progression in women who had NAFLD and were later diagnosed with ICP, compared to women with NAFLD who did not go on to develop ICP, because that may be a reflection of the role that bile acid metabolism plays in these particular patients,” Dr. Kushner said.
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
The study’s primary author was Erica Monrose, MD. The researchers reported having no financial disclosures.
SOURCE: Monrose E et al. DDW 2019, Abstract Sa1562.
Patients with intrahepatic cholestasis of pregnancy (ICP) were nearly six times more likely to have a diagnosis of nonalcoholic fatty liver disease (NAFLD) than were controls, results from a retrospective, single-center study demonstrated.
“If this connection is confirmed with future studies, intrahepatic cholestasis of pregnancy may prove a novel model through which to investigate bile acid metabolism in patients with fatty liver disease,” one of the study authors, Tatyana Kushner, MD, MSCE, said during a media briefing in advance of the annual Digestive Disease Week. “This could have implications for future management of fatty liver disease. Additionally, these findings suggest that ICP patients should be seen by a liver specialist because they may go on to develop chronic liver disease or may already have already existing underlying liver disease.”
ICP is characterized by a build-up of bile acids during pregnancy and is associated with an increased risk of negative fetal outcomes and fetal death if left untreated, said Dr. Kushner, of the division of liver diseases at the Icahn School of Medicine at Mount Sinai, New York. The most notable symptom during pregnancy is severe pruritus. In what is believed to be the first study of its kind, Dr. Kushner and colleagues set out to evaluate the association between ICP and NAFLD and associated metabolic risk factors, including obesity, dyslipidemia, hypertension, and diabetes. Between January and December of 2017, they drew from the electronic medical records of a New York City health system to identify 149 pregnancies complicated by ICP and compared them to a control group of 200 pregnancies without an ICP diagnosis. The researchers used Pearson’s chi-square or Fisher’s exact test and Wilcoxon rank-sum tests to evaluate association of ICP with categorical variables and continuous variables, respectively, and unadjusted odds ratios to compare the ICP and control groups for clinically significant outcomes.
The median age of the study population was 30 years, their mean body mass index was 27.5 kg/m2, and there was a higher proportion of Hispanic women in the ICP group, compared with the control group (75% vs. 62%, respectively). Dr. Kushner and colleagues found that Hispanic women were nearly twice as likely to be diagnosed with ICP than non-Hispanic women (OR, 1.90; 95% confidence interval, 1.87-3.03). However, patients in both the ICP and control groups were similar for median age (OR, 1.02; 95% CI, 0.99-1.06), nulliparity (OR, 0.79; 95% CI, 0.48-1.30), and prevalence of hepatitis C (OR, 1.35; 95% CI, 0.08-21.67). The two groups were also similar for certain metabolic risk factors, including prevalence of obesity (OR, 1.01; 95% CI, 0.62-1.61), hypertension (OR, 0.69; 95% CI, 0.31-1.52), hemoglobin A1c greater than 5.5% (OR, 0.80; 95% CI, 0.34-1.9), and total cholesterol above 200 mg/dL (OR, 4.15; 95% CI, 0.83-20.84). Median bile acid levels were 30.6 micromoles (interquartile range, 11.6, 32.7) in the ICP group.
Compared with patients in the control group, those in the ICP group had higher median levels of alanine aminotransferase (ALT) (32 vs. 16 U/L; P less than .0001), alkaline phosphatase (181 vs. 128 U/L; P less than .0001), and total bilirubin (0.5 vs. 0.35 mg/dL; P less than .0001). ICP patients were also more likely than their counterparts to have ALT levels above 50 U/L (two times the upper limit of normal; OR, 3.22; 95% CI, 1.48-7.03), a history of biliary disease (OR, 3.29; 95% CI, 1.39-7.80), and to have evidence of steatosis on liver imaging (OR, 4.69; 95% CI, 1.68-13.12). When the researchers evaluated a diagnosis of NAFLD based on ICD-10 codes or evidence of steatosis on liver imaging, ICP patients were significantly more likely to have a diagnosis of NAFLD than controls (OR, 5.7; 95% CI, 2.08-15.65).
“We recommend additional research to look at differences in NAFLD progression in women who had NAFLD and were later diagnosed with ICP, compared to women with NAFLD who did not go on to develop ICP, because that may be a reflection of the role that bile acid metabolism plays in these particular patients,” Dr. Kushner said.
Digestive Disease Week is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
The study’s primary author was Erica Monrose, MD. The researchers reported having no financial disclosures.
SOURCE: Monrose E et al. DDW 2019, Abstract Sa1562.
REPORTING FROM DDW 2019
C-sections play role in 300% higher severe maternal morbidity in twin pregnancies
according to findings from the prospective EPIMOMS study.
The population-based incidence of severe acute maternal morbidity occurring between 22 weeks’ of gestation and 42 days post partum in the 2012-2013 French multicenter study was 6.2% among 3,202 twin pregnancies and 1.3% among 179,107 singleton pregnancies, Hugo Madar, MD, MPH, of Bordeaux University Hospital, France, and colleagues reported on behalf of the EPIMOMS (Epidémiologie de la Morbidité Maternelle Sévère) study group.
For the current analysis – a population-based, cohort-nested, case-control analysis of study data – the investigators compared 2,500 case patients (8% had twin pregnancies) and 3,650 controls (2% had twin pregnancies) who did not experience severe acute maternal morbidity during that time period (odds ratio, 4.7). After accounting for confounding factors, the increased risk among women with twin versus singleton pregnancies persisted (OR, 4.2) during both the antepartum (OR, 4.1) and intrapartum/postpartum (OR, 4.2) periods.
The majority of events (77%) occurred during the latter periods, and the two most common underlying causal conditions were severe obstetric hemorrhage (66%) and severe hypertensive complications (20%); however, the increased risk in twin pregnancies was apparent, regardless of the underlying cause.
The cesarean delivery rates for twin versus singleton pregnancies were 72% and 34%, respectively, in the case group, and 58% and 18%, respectively, in the control group. A path analysis taking potential indication bias into account showed that 21% of the total risk of intrapartum or postpartum severe acute maternal morbidity risk associated with twin pregnancy was mediated by cesarean delivery, Dr. Madar and associates noted, explaining that, “in other words, if twin pregnancies had the same probability of cesarean delivery as singleton pregnancies, the association found between twin pregnancy and intrapartum or postpartum severe acute maternal morbidity would be reduced by one-fifth.”
This provides further support for limiting the use of cesarean for twin deliveries to cases with clear medical indications, as increasing the rate of vaginal deliveries may decrease the rate of severe acute maternal morbidity, they concluded.
EPIMOMS was supported by the National Research Agency and the Ile de France Regional Health Agency. Dr. Madar received a training grant from the Aquitaine Regional Health Agency. The authors reported having no other relevant financial disclosures.
SOURCE: Madar H et al. Obstet Gynecol. 2019;133:1141-50.
Twin pregnancies are known to be associated with increased risk of maternal morbidity, so the findings of this “very well-designed” study by Madar et al. are “not strikingly different than what we know,” according to Ozhan M. Turan, MD, PhD.
These data alone will do little to change practice, but paired with an increased focus on training with respect to vaginal twin delivery – including in cases of breech presentation of the second baby – they could lead to improved maternal outcomes, he explained, adding that “breech extraction can be very fast and safe in skilled hands.”
Except for the lack of information in the study about whether the twins were monozygotic or dizygotic, the study is sound, and the data may prove useful for counseling patients about the risks and benefits of vaginal versus cesarean delivery and for promoting improved training of residents, maternal-fetal medicine fellows, and junior obstetricians in vaginal twin delivery techniques, he said.
Dr. Turan is director of the division of maternal and fetal medicine and of fetal therapy & complex obstetric surgery at the University of Maryland, Baltimore County. He reported having no relevant financial disclosures.
Twin pregnancies are known to be associated with increased risk of maternal morbidity, so the findings of this “very well-designed” study by Madar et al. are “not strikingly different than what we know,” according to Ozhan M. Turan, MD, PhD.
These data alone will do little to change practice, but paired with an increased focus on training with respect to vaginal twin delivery – including in cases of breech presentation of the second baby – they could lead to improved maternal outcomes, he explained, adding that “breech extraction can be very fast and safe in skilled hands.”
Except for the lack of information in the study about whether the twins were monozygotic or dizygotic, the study is sound, and the data may prove useful for counseling patients about the risks and benefits of vaginal versus cesarean delivery and for promoting improved training of residents, maternal-fetal medicine fellows, and junior obstetricians in vaginal twin delivery techniques, he said.
Dr. Turan is director of the division of maternal and fetal medicine and of fetal therapy & complex obstetric surgery at the University of Maryland, Baltimore County. He reported having no relevant financial disclosures.
Twin pregnancies are known to be associated with increased risk of maternal morbidity, so the findings of this “very well-designed” study by Madar et al. are “not strikingly different than what we know,” according to Ozhan M. Turan, MD, PhD.
These data alone will do little to change practice, but paired with an increased focus on training with respect to vaginal twin delivery – including in cases of breech presentation of the second baby – they could lead to improved maternal outcomes, he explained, adding that “breech extraction can be very fast and safe in skilled hands.”
Except for the lack of information in the study about whether the twins were monozygotic or dizygotic, the study is sound, and the data may prove useful for counseling patients about the risks and benefits of vaginal versus cesarean delivery and for promoting improved training of residents, maternal-fetal medicine fellows, and junior obstetricians in vaginal twin delivery techniques, he said.
Dr. Turan is director of the division of maternal and fetal medicine and of fetal therapy & complex obstetric surgery at the University of Maryland, Baltimore County. He reported having no relevant financial disclosures.
according to findings from the prospective EPIMOMS study.
The population-based incidence of severe acute maternal morbidity occurring between 22 weeks’ of gestation and 42 days post partum in the 2012-2013 French multicenter study was 6.2% among 3,202 twin pregnancies and 1.3% among 179,107 singleton pregnancies, Hugo Madar, MD, MPH, of Bordeaux University Hospital, France, and colleagues reported on behalf of the EPIMOMS (Epidémiologie de la Morbidité Maternelle Sévère) study group.
For the current analysis – a population-based, cohort-nested, case-control analysis of study data – the investigators compared 2,500 case patients (8% had twin pregnancies) and 3,650 controls (2% had twin pregnancies) who did not experience severe acute maternal morbidity during that time period (odds ratio, 4.7). After accounting for confounding factors, the increased risk among women with twin versus singleton pregnancies persisted (OR, 4.2) during both the antepartum (OR, 4.1) and intrapartum/postpartum (OR, 4.2) periods.
The majority of events (77%) occurred during the latter periods, and the two most common underlying causal conditions were severe obstetric hemorrhage (66%) and severe hypertensive complications (20%); however, the increased risk in twin pregnancies was apparent, regardless of the underlying cause.
The cesarean delivery rates for twin versus singleton pregnancies were 72% and 34%, respectively, in the case group, and 58% and 18%, respectively, in the control group. A path analysis taking potential indication bias into account showed that 21% of the total risk of intrapartum or postpartum severe acute maternal morbidity risk associated with twin pregnancy was mediated by cesarean delivery, Dr. Madar and associates noted, explaining that, “in other words, if twin pregnancies had the same probability of cesarean delivery as singleton pregnancies, the association found between twin pregnancy and intrapartum or postpartum severe acute maternal morbidity would be reduced by one-fifth.”
This provides further support for limiting the use of cesarean for twin deliveries to cases with clear medical indications, as increasing the rate of vaginal deliveries may decrease the rate of severe acute maternal morbidity, they concluded.
EPIMOMS was supported by the National Research Agency and the Ile de France Regional Health Agency. Dr. Madar received a training grant from the Aquitaine Regional Health Agency. The authors reported having no other relevant financial disclosures.
SOURCE: Madar H et al. Obstet Gynecol. 2019;133:1141-50.
according to findings from the prospective EPIMOMS study.
The population-based incidence of severe acute maternal morbidity occurring between 22 weeks’ of gestation and 42 days post partum in the 2012-2013 French multicenter study was 6.2% among 3,202 twin pregnancies and 1.3% among 179,107 singleton pregnancies, Hugo Madar, MD, MPH, of Bordeaux University Hospital, France, and colleagues reported on behalf of the EPIMOMS (Epidémiologie de la Morbidité Maternelle Sévère) study group.
For the current analysis – a population-based, cohort-nested, case-control analysis of study data – the investigators compared 2,500 case patients (8% had twin pregnancies) and 3,650 controls (2% had twin pregnancies) who did not experience severe acute maternal morbidity during that time period (odds ratio, 4.7). After accounting for confounding factors, the increased risk among women with twin versus singleton pregnancies persisted (OR, 4.2) during both the antepartum (OR, 4.1) and intrapartum/postpartum (OR, 4.2) periods.
The majority of events (77%) occurred during the latter periods, and the two most common underlying causal conditions were severe obstetric hemorrhage (66%) and severe hypertensive complications (20%); however, the increased risk in twin pregnancies was apparent, regardless of the underlying cause.
The cesarean delivery rates for twin versus singleton pregnancies were 72% and 34%, respectively, in the case group, and 58% and 18%, respectively, in the control group. A path analysis taking potential indication bias into account showed that 21% of the total risk of intrapartum or postpartum severe acute maternal morbidity risk associated with twin pregnancy was mediated by cesarean delivery, Dr. Madar and associates noted, explaining that, “in other words, if twin pregnancies had the same probability of cesarean delivery as singleton pregnancies, the association found between twin pregnancy and intrapartum or postpartum severe acute maternal morbidity would be reduced by one-fifth.”
This provides further support for limiting the use of cesarean for twin deliveries to cases with clear medical indications, as increasing the rate of vaginal deliveries may decrease the rate of severe acute maternal morbidity, they concluded.
EPIMOMS was supported by the National Research Agency and the Ile de France Regional Health Agency. Dr. Madar received a training grant from the Aquitaine Regional Health Agency. The authors reported having no other relevant financial disclosures.
SOURCE: Madar H et al. Obstet Gynecol. 2019;133:1141-50.
FROM OBSTETRICS & GYNECOLOGY