User login
Official Newspaper of the American College of Surgeons
U.S. surgeon supply projected to drop 18% by 2028
The supply of surgeons in the United States will decrease by nearly one-fifth by 2028, likely resulting in shortages in all but a handful of specialties, a study has shown.
Currently proposed changes to increase surgeon training will not be enough to offset the number of surgeons who will retire, predicted Erin P. Fraher, Ph.D., of the department of surgery at the University of North Carolina at Chapel Hill, and colleagues. If this trend continues, the overall supply of full-time-equivalent surgeons will have decreased 18% between 2009 and 2028, with declines in all specialties except colorectal, pediatric, neurologic, and vascular surgery.
Such a drop could result in a workforce insufficient to meet the needs of the U.S. population – particularly in light of the expanded access to and increased usage of health care services projected for the future. It could also exacerbate problems related to the geographic distribution of surgeons, the investigators cautioned, "leading to delayed or lost access to time-sensitive surgical procedures, particularly in rural areas" (Ann. Surg. 2012 [doi:10.1097/SLA.0b013e31826fccfa]).
These projections are lower than those forecast in a 2008 report by the U.S. Health Resources and Services Administration for general, cardiothoracic, orthopedic, urologic, plastic, ophthalmologic, and obstetrics/gynecologic surgeons. However, they are brighter than previously published projections for vascular and pediatric surgeons (J. Vasc. Surg. 2009;50:946-52; J. Pediatr. Surg. 2009;44:1677-82). Predictions of a decline in cardiothoracic surgeons are consistent with some earlier findings (Circulation 2009;120:488-94).
For the current research, the investigators used a stock-and-flow model, which calculates current numbers of physicians, projected numbers of physicians graduating from medical school, and physicians reentering the workforce, and subtracts from these anticipated deaths, retirements, and career breaks. They then adjusted the resulting head count to full-time-equivalent work participation rates of surgeons by age, sex, and specialty.
Data were drawn from databases maintained by the American Medical Association, the American Board of Medical Specialties, the National Resident Match Program, the San Francisco match for plastic surgery and ophthalmology, the American Urological Association, the Health Resources and Services Administration, and the North Carolina Health Professions Data System.
Unlike static projection models, this model allows for real-time updating to take into account changes in data and policy decisions, which enhances the accuracy of its workforce projections, according to the investigators.
Surgeons’ participation in patient care declines somewhat after age 60, they noted, making age a key factor in determining full-time equivalents for each specialty. Another factor considered in modeling was the "feminization" of various specialties. By 2019, Dr. Fraher and colleagues predicted, half of general surgery residents will be female, compared with 95% of obstetrics and gynecology residents and 28% of orthopedic surgery residents.
Furthermore, an estimated 25% of general surgery cases that have traditionally been performed by surgical specialists will, in the future, need to be made up by general surgeons, the investigators said.
The most important driver of future supply estimates, they said, "is whether anticipated declines in full-time equivalent rates will occur as expected and whether these full-time equivalent decreases will be offset, at least partially, by productivity gains."
Dr. Fraher and colleagues called their findings "a snapshot of trends that may or may not develop depending on whether there are changes in graduate medical education training pathways, in the length of training, and in attrition from residency programs."
Current proposals to either cut or increase graduate medical education funding under Medicare focus largely on increasing the supply of primary care physicians, but results from this model suggest that it is equally important to ensure an adequate supply of surgeons in the future, the authors said. They emphasized that current published recommendations to boost graduate medical education by the Council of Graduate Medical Education, Congress, and others, if implemented, would not avert declines in surgical workforce supply during the period forecasted.
Dr. Fraher and colleagues’ study was sponsored by the American College of Surgeons. None of its authors declared conflicts of interest.
The supply of surgeons in the United States will decrease by nearly one-fifth by 2028, likely resulting in shortages in all but a handful of specialties, a study has shown.
Currently proposed changes to increase surgeon training will not be enough to offset the number of surgeons who will retire, predicted Erin P. Fraher, Ph.D., of the department of surgery at the University of North Carolina at Chapel Hill, and colleagues. If this trend continues, the overall supply of full-time-equivalent surgeons will have decreased 18% between 2009 and 2028, with declines in all specialties except colorectal, pediatric, neurologic, and vascular surgery.
Such a drop could result in a workforce insufficient to meet the needs of the U.S. population – particularly in light of the expanded access to and increased usage of health care services projected for the future. It could also exacerbate problems related to the geographic distribution of surgeons, the investigators cautioned, "leading to delayed or lost access to time-sensitive surgical procedures, particularly in rural areas" (Ann. Surg. 2012 [doi:10.1097/SLA.0b013e31826fccfa]).
These projections are lower than those forecast in a 2008 report by the U.S. Health Resources and Services Administration for general, cardiothoracic, orthopedic, urologic, plastic, ophthalmologic, and obstetrics/gynecologic surgeons. However, they are brighter than previously published projections for vascular and pediatric surgeons (J. Vasc. Surg. 2009;50:946-52; J. Pediatr. Surg. 2009;44:1677-82). Predictions of a decline in cardiothoracic surgeons are consistent with some earlier findings (Circulation 2009;120:488-94).
For the current research, the investigators used a stock-and-flow model, which calculates current numbers of physicians, projected numbers of physicians graduating from medical school, and physicians reentering the workforce, and subtracts from these anticipated deaths, retirements, and career breaks. They then adjusted the resulting head count to full-time-equivalent work participation rates of surgeons by age, sex, and specialty.
Data were drawn from databases maintained by the American Medical Association, the American Board of Medical Specialties, the National Resident Match Program, the San Francisco match for plastic surgery and ophthalmology, the American Urological Association, the Health Resources and Services Administration, and the North Carolina Health Professions Data System.
Unlike static projection models, this model allows for real-time updating to take into account changes in data and policy decisions, which enhances the accuracy of its workforce projections, according to the investigators.
Surgeons’ participation in patient care declines somewhat after age 60, they noted, making age a key factor in determining full-time equivalents for each specialty. Another factor considered in modeling was the "feminization" of various specialties. By 2019, Dr. Fraher and colleagues predicted, half of general surgery residents will be female, compared with 95% of obstetrics and gynecology residents and 28% of orthopedic surgery residents.
Furthermore, an estimated 25% of general surgery cases that have traditionally been performed by surgical specialists will, in the future, need to be made up by general surgeons, the investigators said.
The most important driver of future supply estimates, they said, "is whether anticipated declines in full-time equivalent rates will occur as expected and whether these full-time equivalent decreases will be offset, at least partially, by productivity gains."
Dr. Fraher and colleagues called their findings "a snapshot of trends that may or may not develop depending on whether there are changes in graduate medical education training pathways, in the length of training, and in attrition from residency programs."
Current proposals to either cut or increase graduate medical education funding under Medicare focus largely on increasing the supply of primary care physicians, but results from this model suggest that it is equally important to ensure an adequate supply of surgeons in the future, the authors said. They emphasized that current published recommendations to boost graduate medical education by the Council of Graduate Medical Education, Congress, and others, if implemented, would not avert declines in surgical workforce supply during the period forecasted.
Dr. Fraher and colleagues’ study was sponsored by the American College of Surgeons. None of its authors declared conflicts of interest.
The supply of surgeons in the United States will decrease by nearly one-fifth by 2028, likely resulting in shortages in all but a handful of specialties, a study has shown.
Currently proposed changes to increase surgeon training will not be enough to offset the number of surgeons who will retire, predicted Erin P. Fraher, Ph.D., of the department of surgery at the University of North Carolina at Chapel Hill, and colleagues. If this trend continues, the overall supply of full-time-equivalent surgeons will have decreased 18% between 2009 and 2028, with declines in all specialties except colorectal, pediatric, neurologic, and vascular surgery.
Such a drop could result in a workforce insufficient to meet the needs of the U.S. population – particularly in light of the expanded access to and increased usage of health care services projected for the future. It could also exacerbate problems related to the geographic distribution of surgeons, the investigators cautioned, "leading to delayed or lost access to time-sensitive surgical procedures, particularly in rural areas" (Ann. Surg. 2012 [doi:10.1097/SLA.0b013e31826fccfa]).
These projections are lower than those forecast in a 2008 report by the U.S. Health Resources and Services Administration for general, cardiothoracic, orthopedic, urologic, plastic, ophthalmologic, and obstetrics/gynecologic surgeons. However, they are brighter than previously published projections for vascular and pediatric surgeons (J. Vasc. Surg. 2009;50:946-52; J. Pediatr. Surg. 2009;44:1677-82). Predictions of a decline in cardiothoracic surgeons are consistent with some earlier findings (Circulation 2009;120:488-94).
For the current research, the investigators used a stock-and-flow model, which calculates current numbers of physicians, projected numbers of physicians graduating from medical school, and physicians reentering the workforce, and subtracts from these anticipated deaths, retirements, and career breaks. They then adjusted the resulting head count to full-time-equivalent work participation rates of surgeons by age, sex, and specialty.
Data were drawn from databases maintained by the American Medical Association, the American Board of Medical Specialties, the National Resident Match Program, the San Francisco match for plastic surgery and ophthalmology, the American Urological Association, the Health Resources and Services Administration, and the North Carolina Health Professions Data System.
Unlike static projection models, this model allows for real-time updating to take into account changes in data and policy decisions, which enhances the accuracy of its workforce projections, according to the investigators.
Surgeons’ participation in patient care declines somewhat after age 60, they noted, making age a key factor in determining full-time equivalents for each specialty. Another factor considered in modeling was the "feminization" of various specialties. By 2019, Dr. Fraher and colleagues predicted, half of general surgery residents will be female, compared with 95% of obstetrics and gynecology residents and 28% of orthopedic surgery residents.
Furthermore, an estimated 25% of general surgery cases that have traditionally been performed by surgical specialists will, in the future, need to be made up by general surgeons, the investigators said.
The most important driver of future supply estimates, they said, "is whether anticipated declines in full-time equivalent rates will occur as expected and whether these full-time equivalent decreases will be offset, at least partially, by productivity gains."
Dr. Fraher and colleagues called their findings "a snapshot of trends that may or may not develop depending on whether there are changes in graduate medical education training pathways, in the length of training, and in attrition from residency programs."
Current proposals to either cut or increase graduate medical education funding under Medicare focus largely on increasing the supply of primary care physicians, but results from this model suggest that it is equally important to ensure an adequate supply of surgeons in the future, the authors said. They emphasized that current published recommendations to boost graduate medical education by the Council of Graduate Medical Education, Congress, and others, if implemented, would not avert declines in surgical workforce supply during the period forecasted.
Dr. Fraher and colleagues’ study was sponsored by the American College of Surgeons. None of its authors declared conflicts of interest.
FROM ANNALS OF SURGERY
Major Finding: The overall availability of surgeons in the United States will have decreased 18% by 2028 if current trends continue, with exceptions for some specialties.
Data Source: Databases maintained by the American Medical Association and several other organizations.
Disclosures: The study was sponsored by the American College of Surgeons. None of the authors declared conflicts of interest.
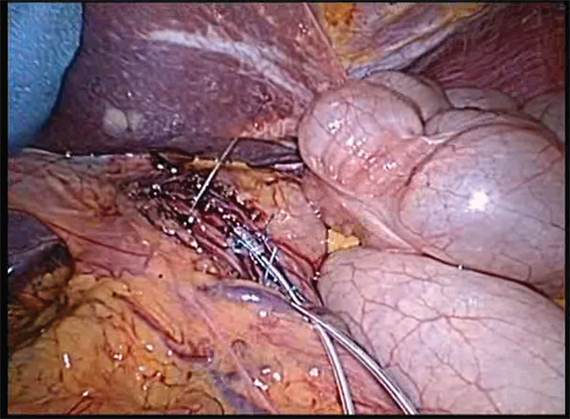
Lower esophageal electrical stimulation therapy targets GERD
Electrical stimulation of the lower esophageal sphincter using an implanted device shows promise for the treatment of gastroesophageal reflux, according to findings from three recent studies.
In one open-label pilot extension study, 77% of 23 patients treated with EndoStim’s Lower Esophageal Sphincter (LES) stimulation system reported normalization of (or at least a 50% reduction in) distal esophageal acid exposure at 12 months’ follow-up, Dr. Edy Soffer reported in October at the annual meeting of the American College of Gastroenterology.
The patients also experienced significant improvement in their median GERD-Health Related Quality of Life (GERD-HRQL) score while implanted with the LES stimulation system (LES-EST), compared with their score while on proton pump inhibitor (PPI) therapy (increase of 9 vs. 2 points) and while off PPI therapy (increase of 23.5 vs. 2), said Dr. Soffer, professor of clinical medicine and director of the GI motility program at the University of Southern California, Los Angeles.
All but one patient reported cessation of regular PPI use, and no implantation- or stimulation-related unanticipated adverse events or "untoward sensation" due to stimulation occurred during follow-up; nor was swallowing function as assessed by manometry affected.
Patients included in the study were GERD patients with a mean age of 53 years who were at least partially responsive to PPI therapy, and who had off-PPI GERD-HRQL scores of at least 20, as well as hiatal hernia.
The findings indicate that LES-EST, which uses low-energy electrical pulses to strengthen a weak or dysfunctional lower esophageal sphincter, is safe and effective for long-term use, he said.
In an interview, Dr. Soffer said that the findings have held up at 18 months of follow-up.
"The results are comparable to those observed at 12 months with regard to control of symptoms, and with near elimination of the use of PPIs," he said, noting that the safety profile remains excellent, with no new adverse event reported beyond those seen at 12 months’ follow-up.
Physiological studies such as esophageal pH will be conducted at 24 months, he said.
In a related study presented in a poster at the meeting, Michael Crowell, Ph.D., looked more closely at the effects of LES-EST on both distal and proximal esophageal acid exposure in a post hoc analysis.
In 19 patients with a median age of 54 years, LES-EST was associated with normalization of total and upright proximal esophageal acid exposure, which improved from 0.4% and 0.6%, respectively, at baseline to 0% at 12 months’ follow-up. Supine esophageal acid exposure was unchanged from 0% at baseline, said Dr. Crowell of the Mayo Clinic, Scottsdale, Ariz.
This was true even among seven patients with abnormal proximal esophageal pH, whose total, upright, and supine proximal esophageal acid exposure values at baseline were 1.7%, 2.9%, and 0.3%, respectively. Distal esophageal pH improved from 10.2% to 3.6% for the entire cohort, and from 9.3% to 3.4% in those seven patients.
Patients in this study had GERD that was at least partially responsive to PPIs, a hiatal hernia of less than 3 cm, and esophagitis of less than Los Angeles Classification grade D. Electrical stimulation was administered for 220 microseconds at 20 Hz and 5-8 mA in 6-12 30-minute sessions starting on day 1 after implantation.
No gastrointestinal side effects occurred in the patients, nor were there any device- or procedure-related adverse events.
LES-EST may be effective in treating proximal GERD, Dr. Crowell concluded.
In an interview, he added that the findings are important, particularly for the one-third of patients who remain symptomatic on PPIs.
"LES dysfunction is the root cause of GERD. Medications such as PPIs block stomach acid production, but do not address the pathophysiology of GERD. Hence, more than a third of patients continue to suffer from symptoms despite maximal medical therapy," he said.
Additionally, there are significant safety concerns with long-term acid suppression, he noted.
LES-EST, on the other hand, addresses the root cause of GERD by improving LES pressure and function, thereby restoring the LES physiology and its barrier function, preventing reflux of gastric acid into the esophagus.
"LES stimulation does not affect normal LES relaxation, allowing for the patient to swallow normally, and has no side effects," he said.
In a third, unrelated study also reported in a poster at the meeting, LES-EST was similarly effective.
Of 11 patients treated with EndoStim’s LES stimulation system as part of an international multicenter study, 10 were able to discontinue PPI therapy at 3-6 months of follow-up, according to Dr. Arjan J. Bredenoord of Academic Medical Center Utrecht, Rotterdam.
Those 10 patients experienced significant improvements in median GERD-HRQL scores from 32 (off PPIs) and 22 (on PPIs) to 9 (on LES-EST) at 3 months, and the scores remained stable at 9 points in 3 patients who were followed for 6 months.
Median esophageal acid exposure improved from 11.8% at baseline to 7.8% at 3 months and 7.3% at 6 months, Dr. Bredenoord said.
The remaining patient suffered a small bowl trocar perforation during implantation of the device and underwent successful repair. An additional 13 adverse events, including 1 serious adverse event, were reported in 4 patients. Nine of these were related to the device or procedure, including seven complaints of pain at the implant site and one case of postoperative nausea.
The treatment was safe, with no GI or cardiac side effects, Dr. Bredenoord concluded, noting that long-term safety and efficacy results in a larger group of patients are currently being analyzed.
In an interview, Dr. Bredenoord noted that the findings are among the first in patients outside South America, where the earliest trials of the EndoStim LES stimulation system were conducted.
"The data confirm the favorable outcome of the patients in Chile, and show that both symptoms and reflux are reduced in European patients as well," he said.
However, the experience remains limited, and additional study comparing the device with other treatments and/or with placebo is needed, as are longer-term outcomes data.
"I think that although these results suggest this is a promising treatment, it would be best to treat patients only in trials" at this point, he said. Because trial participants have been carefully selected, it remains unclear whether this treatment is suitable for the entire GERD population, he added.
Dr. Soffer agreed, and said that if the results are reproduced in additional studies with a larger number of patients, the intervention will provide an alternative therapy for GERD patients who are not satisfied with PPIs or who have concerns about side effects and the chronic use of treatment, and who also have concerns about the established surgical treatment for GERD.
"The importance of this intervention is in providing a bridge between the currently established drug therapy for GERD [PPIs] and the established surgical therapy [fundoplication]. While PPIs are effective in a substantial number of GERD patients, they do not correct the underlying pathophysiology of GERD, resulting in a substantial number of patients who remain symptomatic in spite of therapy," he said.
These patients can be offered fundoplication, which is effective in expert hands, but the surgery has side effects and is performed less and less often, he added.
"Consequently, there is a search for a bridge intervention, endoscopic or surgical, for the treatment of GERD," he said.
LES-EST appears to have the potential to be such a bridge intervention.
"The procedure is simple and nondisruptive, and addresses pathophysiology. The safety profile thus far is excellent, and the effect on esophageal acid exposure, symptoms, and PPI use is sustained over a period of 12-18 moths. Furthermore, the treatment can be optimized to individual needs by adjusting delivery of stimulation to coincide with periods when symptoms and acid reflux are detected," he said.
All three of these studies presented at the meeting were supported by EndoStim BV. Dr. Soffer disclosed that he has stockholder/ownership interest in the company. Dr. Crowell disclosed that he has served as a consultant to the company. Dr. Bredenoord reported receiving grant and/or research support from the company.
Gastroesophageal reflux disease is one of the most common chronic gastrointestinal disorders. The mainstay of medical therapy is to suppress gastric acid secretion with medications such as PPIs. An alternative approach to acid suppression is modulation of the antireflux barrier, composed of the lower esophageal sphincter (LES) and the crural diaphragm. Surgical fundoplication is a well-established method to augment the function of the antireflux barrier. Fundoplication has proven effective in high-quality trials, but it also has well-documented side effects such as dysphagia, bloating, and diarrhea in a subset of patients.
Additional means of enhancing the function of the antireflux barrier include pharmacological inhibition of transient LES relaxations (TLESR) with various agents and several endoscopic antireflux procedures. Unfortunately, the use of TLESR inhibitors and endoscopic procedures for GERD is very limited due to side effects and adverse events, along with insufficient efficacy.
Electrical stimulation of the LES has been previously shown to increase LES resting tone in an animal model (Am. J. Physiol. Gastrointest. Liver Physiol. 2008;295:G389-94). More recently, in a 6-month, open-label trial, electrical stimulation of the LES was found to reduce or eliminate PPI use and to improve symptoms and 24-hour esophageal pH parameters in GERD patients who were at least partially responsive to PPIs (Surg. Endosc. 2012 Oct. 17 [doi: 10.1007/s00464-012-2561-4]).
During the recent American College of Gastroenterology meeting, 1-year data for the open-label trial mentioned above was presented by Dr. Soffer, Dr. Crowell, and their collaborators, showing that improvement in symptoms, PPI use, and distal esophageal acid exposure persisted at 12 months with minimal side effects or adverse events.
Preliminary results of an international multicenter trial of LES electrical stimulation for refractory GERD were also presented at the meeting by Dr. Bredenoord and his colleagues. They found that LES electrical stimulation improved symptoms, PPI use, and esophageal acid exposure in this group of patients, but the preliminary number of patients was small and follow-up was mostly limited to 3 months. Importantly, they did report some adverse events.
These studies provide additional information to suggest that electrical stimulation of the LES may be an effective treatment for GERD. While the available data is compelling, more work will be required to evaluate the durability of the procedure, assess long-term safety and side effects, study the effects of stimulation on esophageal sensation, and define which GERD patients are best suited for this treatment. This will be ideally accomplished by randomized controlled trials that will compare electrical stimulation of the LES to the well-established pharmacological and surgical approaches currently used to treat GERD.
Marcelo F. Vela, M.D., is an associate professor of medicine and director of gastrointestinal motility at Baylor College of Medicine and the Michael E. DeBakey VA Medical Center, both in Houston. He is a member of an advisory panel for Given Imaging.
Gastroesophageal reflux disease is one of the most common chronic gastrointestinal disorders. The mainstay of medical therapy is to suppress gastric acid secretion with medications such as PPIs. An alternative approach to acid suppression is modulation of the antireflux barrier, composed of the lower esophageal sphincter (LES) and the crural diaphragm. Surgical fundoplication is a well-established method to augment the function of the antireflux barrier. Fundoplication has proven effective in high-quality trials, but it also has well-documented side effects such as dysphagia, bloating, and diarrhea in a subset of patients.
Additional means of enhancing the function of the antireflux barrier include pharmacological inhibition of transient LES relaxations (TLESR) with various agents and several endoscopic antireflux procedures. Unfortunately, the use of TLESR inhibitors and endoscopic procedures for GERD is very limited due to side effects and adverse events, along with insufficient efficacy.
Electrical stimulation of the LES has been previously shown to increase LES resting tone in an animal model (Am. J. Physiol. Gastrointest. Liver Physiol. 2008;295:G389-94). More recently, in a 6-month, open-label trial, electrical stimulation of the LES was found to reduce or eliminate PPI use and to improve symptoms and 24-hour esophageal pH parameters in GERD patients who were at least partially responsive to PPIs (Surg. Endosc. 2012 Oct. 17 [doi: 10.1007/s00464-012-2561-4]).
During the recent American College of Gastroenterology meeting, 1-year data for the open-label trial mentioned above was presented by Dr. Soffer, Dr. Crowell, and their collaborators, showing that improvement in symptoms, PPI use, and distal esophageal acid exposure persisted at 12 months with minimal side effects or adverse events.
Preliminary results of an international multicenter trial of LES electrical stimulation for refractory GERD were also presented at the meeting by Dr. Bredenoord and his colleagues. They found that LES electrical stimulation improved symptoms, PPI use, and esophageal acid exposure in this group of patients, but the preliminary number of patients was small and follow-up was mostly limited to 3 months. Importantly, they did report some adverse events.
These studies provide additional information to suggest that electrical stimulation of the LES may be an effective treatment for GERD. While the available data is compelling, more work will be required to evaluate the durability of the procedure, assess long-term safety and side effects, study the effects of stimulation on esophageal sensation, and define which GERD patients are best suited for this treatment. This will be ideally accomplished by randomized controlled trials that will compare electrical stimulation of the LES to the well-established pharmacological and surgical approaches currently used to treat GERD.
Marcelo F. Vela, M.D., is an associate professor of medicine and director of gastrointestinal motility at Baylor College of Medicine and the Michael E. DeBakey VA Medical Center, both in Houston. He is a member of an advisory panel for Given Imaging.
Gastroesophageal reflux disease is one of the most common chronic gastrointestinal disorders. The mainstay of medical therapy is to suppress gastric acid secretion with medications such as PPIs. An alternative approach to acid suppression is modulation of the antireflux barrier, composed of the lower esophageal sphincter (LES) and the crural diaphragm. Surgical fundoplication is a well-established method to augment the function of the antireflux barrier. Fundoplication has proven effective in high-quality trials, but it also has well-documented side effects such as dysphagia, bloating, and diarrhea in a subset of patients.
Additional means of enhancing the function of the antireflux barrier include pharmacological inhibition of transient LES relaxations (TLESR) with various agents and several endoscopic antireflux procedures. Unfortunately, the use of TLESR inhibitors and endoscopic procedures for GERD is very limited due to side effects and adverse events, along with insufficient efficacy.
Electrical stimulation of the LES has been previously shown to increase LES resting tone in an animal model (Am. J. Physiol. Gastrointest. Liver Physiol. 2008;295:G389-94). More recently, in a 6-month, open-label trial, electrical stimulation of the LES was found to reduce or eliminate PPI use and to improve symptoms and 24-hour esophageal pH parameters in GERD patients who were at least partially responsive to PPIs (Surg. Endosc. 2012 Oct. 17 [doi: 10.1007/s00464-012-2561-4]).
During the recent American College of Gastroenterology meeting, 1-year data for the open-label trial mentioned above was presented by Dr. Soffer, Dr. Crowell, and their collaborators, showing that improvement in symptoms, PPI use, and distal esophageal acid exposure persisted at 12 months with minimal side effects or adverse events.
Preliminary results of an international multicenter trial of LES electrical stimulation for refractory GERD were also presented at the meeting by Dr. Bredenoord and his colleagues. They found that LES electrical stimulation improved symptoms, PPI use, and esophageal acid exposure in this group of patients, but the preliminary number of patients was small and follow-up was mostly limited to 3 months. Importantly, they did report some adverse events.
These studies provide additional information to suggest that electrical stimulation of the LES may be an effective treatment for GERD. While the available data is compelling, more work will be required to evaluate the durability of the procedure, assess long-term safety and side effects, study the effects of stimulation on esophageal sensation, and define which GERD patients are best suited for this treatment. This will be ideally accomplished by randomized controlled trials that will compare electrical stimulation of the LES to the well-established pharmacological and surgical approaches currently used to treat GERD.
Marcelo F. Vela, M.D., is an associate professor of medicine and director of gastrointestinal motility at Baylor College of Medicine and the Michael E. DeBakey VA Medical Center, both in Houston. He is a member of an advisory panel for Given Imaging.
Electrical stimulation of the lower esophageal sphincter using an implanted device shows promise for the treatment of gastroesophageal reflux, according to findings from three recent studies.
In one open-label pilot extension study, 77% of 23 patients treated with EndoStim’s Lower Esophageal Sphincter (LES) stimulation system reported normalization of (or at least a 50% reduction in) distal esophageal acid exposure at 12 months’ follow-up, Dr. Edy Soffer reported in October at the annual meeting of the American College of Gastroenterology.
The patients also experienced significant improvement in their median GERD-Health Related Quality of Life (GERD-HRQL) score while implanted with the LES stimulation system (LES-EST), compared with their score while on proton pump inhibitor (PPI) therapy (increase of 9 vs. 2 points) and while off PPI therapy (increase of 23.5 vs. 2), said Dr. Soffer, professor of clinical medicine and director of the GI motility program at the University of Southern California, Los Angeles.
All but one patient reported cessation of regular PPI use, and no implantation- or stimulation-related unanticipated adverse events or "untoward sensation" due to stimulation occurred during follow-up; nor was swallowing function as assessed by manometry affected.
Patients included in the study were GERD patients with a mean age of 53 years who were at least partially responsive to PPI therapy, and who had off-PPI GERD-HRQL scores of at least 20, as well as hiatal hernia.
The findings indicate that LES-EST, which uses low-energy electrical pulses to strengthen a weak or dysfunctional lower esophageal sphincter, is safe and effective for long-term use, he said.
In an interview, Dr. Soffer said that the findings have held up at 18 months of follow-up.
"The results are comparable to those observed at 12 months with regard to control of symptoms, and with near elimination of the use of PPIs," he said, noting that the safety profile remains excellent, with no new adverse event reported beyond those seen at 12 months’ follow-up.
Physiological studies such as esophageal pH will be conducted at 24 months, he said.
In a related study presented in a poster at the meeting, Michael Crowell, Ph.D., looked more closely at the effects of LES-EST on both distal and proximal esophageal acid exposure in a post hoc analysis.
In 19 patients with a median age of 54 years, LES-EST was associated with normalization of total and upright proximal esophageal acid exposure, which improved from 0.4% and 0.6%, respectively, at baseline to 0% at 12 months’ follow-up. Supine esophageal acid exposure was unchanged from 0% at baseline, said Dr. Crowell of the Mayo Clinic, Scottsdale, Ariz.
This was true even among seven patients with abnormal proximal esophageal pH, whose total, upright, and supine proximal esophageal acid exposure values at baseline were 1.7%, 2.9%, and 0.3%, respectively. Distal esophageal pH improved from 10.2% to 3.6% for the entire cohort, and from 9.3% to 3.4% in those seven patients.
Patients in this study had GERD that was at least partially responsive to PPIs, a hiatal hernia of less than 3 cm, and esophagitis of less than Los Angeles Classification grade D. Electrical stimulation was administered for 220 microseconds at 20 Hz and 5-8 mA in 6-12 30-minute sessions starting on day 1 after implantation.
No gastrointestinal side effects occurred in the patients, nor were there any device- or procedure-related adverse events.
LES-EST may be effective in treating proximal GERD, Dr. Crowell concluded.
In an interview, he added that the findings are important, particularly for the one-third of patients who remain symptomatic on PPIs.
"LES dysfunction is the root cause of GERD. Medications such as PPIs block stomach acid production, but do not address the pathophysiology of GERD. Hence, more than a third of patients continue to suffer from symptoms despite maximal medical therapy," he said.
Additionally, there are significant safety concerns with long-term acid suppression, he noted.
LES-EST, on the other hand, addresses the root cause of GERD by improving LES pressure and function, thereby restoring the LES physiology and its barrier function, preventing reflux of gastric acid into the esophagus.
"LES stimulation does not affect normal LES relaxation, allowing for the patient to swallow normally, and has no side effects," he said.
In a third, unrelated study also reported in a poster at the meeting, LES-EST was similarly effective.
Of 11 patients treated with EndoStim’s LES stimulation system as part of an international multicenter study, 10 were able to discontinue PPI therapy at 3-6 months of follow-up, according to Dr. Arjan J. Bredenoord of Academic Medical Center Utrecht, Rotterdam.
Those 10 patients experienced significant improvements in median GERD-HRQL scores from 32 (off PPIs) and 22 (on PPIs) to 9 (on LES-EST) at 3 months, and the scores remained stable at 9 points in 3 patients who were followed for 6 months.
Median esophageal acid exposure improved from 11.8% at baseline to 7.8% at 3 months and 7.3% at 6 months, Dr. Bredenoord said.
The remaining patient suffered a small bowl trocar perforation during implantation of the device and underwent successful repair. An additional 13 adverse events, including 1 serious adverse event, were reported in 4 patients. Nine of these were related to the device or procedure, including seven complaints of pain at the implant site and one case of postoperative nausea.
The treatment was safe, with no GI or cardiac side effects, Dr. Bredenoord concluded, noting that long-term safety and efficacy results in a larger group of patients are currently being analyzed.
In an interview, Dr. Bredenoord noted that the findings are among the first in patients outside South America, where the earliest trials of the EndoStim LES stimulation system were conducted.
"The data confirm the favorable outcome of the patients in Chile, and show that both symptoms and reflux are reduced in European patients as well," he said.
However, the experience remains limited, and additional study comparing the device with other treatments and/or with placebo is needed, as are longer-term outcomes data.
"I think that although these results suggest this is a promising treatment, it would be best to treat patients only in trials" at this point, he said. Because trial participants have been carefully selected, it remains unclear whether this treatment is suitable for the entire GERD population, he added.
Dr. Soffer agreed, and said that if the results are reproduced in additional studies with a larger number of patients, the intervention will provide an alternative therapy for GERD patients who are not satisfied with PPIs or who have concerns about side effects and the chronic use of treatment, and who also have concerns about the established surgical treatment for GERD.
"The importance of this intervention is in providing a bridge between the currently established drug therapy for GERD [PPIs] and the established surgical therapy [fundoplication]. While PPIs are effective in a substantial number of GERD patients, they do not correct the underlying pathophysiology of GERD, resulting in a substantial number of patients who remain symptomatic in spite of therapy," he said.
These patients can be offered fundoplication, which is effective in expert hands, but the surgery has side effects and is performed less and less often, he added.
"Consequently, there is a search for a bridge intervention, endoscopic or surgical, for the treatment of GERD," he said.
LES-EST appears to have the potential to be such a bridge intervention.
"The procedure is simple and nondisruptive, and addresses pathophysiology. The safety profile thus far is excellent, and the effect on esophageal acid exposure, symptoms, and PPI use is sustained over a period of 12-18 moths. Furthermore, the treatment can be optimized to individual needs by adjusting delivery of stimulation to coincide with periods when symptoms and acid reflux are detected," he said.
All three of these studies presented at the meeting were supported by EndoStim BV. Dr. Soffer disclosed that he has stockholder/ownership interest in the company. Dr. Crowell disclosed that he has served as a consultant to the company. Dr. Bredenoord reported receiving grant and/or research support from the company.
Electrical stimulation of the lower esophageal sphincter using an implanted device shows promise for the treatment of gastroesophageal reflux, according to findings from three recent studies.
In one open-label pilot extension study, 77% of 23 patients treated with EndoStim’s Lower Esophageal Sphincter (LES) stimulation system reported normalization of (or at least a 50% reduction in) distal esophageal acid exposure at 12 months’ follow-up, Dr. Edy Soffer reported in October at the annual meeting of the American College of Gastroenterology.
The patients also experienced significant improvement in their median GERD-Health Related Quality of Life (GERD-HRQL) score while implanted with the LES stimulation system (LES-EST), compared with their score while on proton pump inhibitor (PPI) therapy (increase of 9 vs. 2 points) and while off PPI therapy (increase of 23.5 vs. 2), said Dr. Soffer, professor of clinical medicine and director of the GI motility program at the University of Southern California, Los Angeles.
All but one patient reported cessation of regular PPI use, and no implantation- or stimulation-related unanticipated adverse events or "untoward sensation" due to stimulation occurred during follow-up; nor was swallowing function as assessed by manometry affected.
Patients included in the study were GERD patients with a mean age of 53 years who were at least partially responsive to PPI therapy, and who had off-PPI GERD-HRQL scores of at least 20, as well as hiatal hernia.
The findings indicate that LES-EST, which uses low-energy electrical pulses to strengthen a weak or dysfunctional lower esophageal sphincter, is safe and effective for long-term use, he said.
In an interview, Dr. Soffer said that the findings have held up at 18 months of follow-up.
"The results are comparable to those observed at 12 months with regard to control of symptoms, and with near elimination of the use of PPIs," he said, noting that the safety profile remains excellent, with no new adverse event reported beyond those seen at 12 months’ follow-up.
Physiological studies such as esophageal pH will be conducted at 24 months, he said.
In a related study presented in a poster at the meeting, Michael Crowell, Ph.D., looked more closely at the effects of LES-EST on both distal and proximal esophageal acid exposure in a post hoc analysis.
In 19 patients with a median age of 54 years, LES-EST was associated with normalization of total and upright proximal esophageal acid exposure, which improved from 0.4% and 0.6%, respectively, at baseline to 0% at 12 months’ follow-up. Supine esophageal acid exposure was unchanged from 0% at baseline, said Dr. Crowell of the Mayo Clinic, Scottsdale, Ariz.
This was true even among seven patients with abnormal proximal esophageal pH, whose total, upright, and supine proximal esophageal acid exposure values at baseline were 1.7%, 2.9%, and 0.3%, respectively. Distal esophageal pH improved from 10.2% to 3.6% for the entire cohort, and from 9.3% to 3.4% in those seven patients.
Patients in this study had GERD that was at least partially responsive to PPIs, a hiatal hernia of less than 3 cm, and esophagitis of less than Los Angeles Classification grade D. Electrical stimulation was administered for 220 microseconds at 20 Hz and 5-8 mA in 6-12 30-minute sessions starting on day 1 after implantation.
No gastrointestinal side effects occurred in the patients, nor were there any device- or procedure-related adverse events.
LES-EST may be effective in treating proximal GERD, Dr. Crowell concluded.
In an interview, he added that the findings are important, particularly for the one-third of patients who remain symptomatic on PPIs.
"LES dysfunction is the root cause of GERD. Medications such as PPIs block stomach acid production, but do not address the pathophysiology of GERD. Hence, more than a third of patients continue to suffer from symptoms despite maximal medical therapy," he said.
Additionally, there are significant safety concerns with long-term acid suppression, he noted.
LES-EST, on the other hand, addresses the root cause of GERD by improving LES pressure and function, thereby restoring the LES physiology and its barrier function, preventing reflux of gastric acid into the esophagus.
"LES stimulation does not affect normal LES relaxation, allowing for the patient to swallow normally, and has no side effects," he said.
In a third, unrelated study also reported in a poster at the meeting, LES-EST was similarly effective.
Of 11 patients treated with EndoStim’s LES stimulation system as part of an international multicenter study, 10 were able to discontinue PPI therapy at 3-6 months of follow-up, according to Dr. Arjan J. Bredenoord of Academic Medical Center Utrecht, Rotterdam.
Those 10 patients experienced significant improvements in median GERD-HRQL scores from 32 (off PPIs) and 22 (on PPIs) to 9 (on LES-EST) at 3 months, and the scores remained stable at 9 points in 3 patients who were followed for 6 months.
Median esophageal acid exposure improved from 11.8% at baseline to 7.8% at 3 months and 7.3% at 6 months, Dr. Bredenoord said.
The remaining patient suffered a small bowl trocar perforation during implantation of the device and underwent successful repair. An additional 13 adverse events, including 1 serious adverse event, were reported in 4 patients. Nine of these were related to the device or procedure, including seven complaints of pain at the implant site and one case of postoperative nausea.
The treatment was safe, with no GI or cardiac side effects, Dr. Bredenoord concluded, noting that long-term safety and efficacy results in a larger group of patients are currently being analyzed.
In an interview, Dr. Bredenoord noted that the findings are among the first in patients outside South America, where the earliest trials of the EndoStim LES stimulation system were conducted.
"The data confirm the favorable outcome of the patients in Chile, and show that both symptoms and reflux are reduced in European patients as well," he said.
However, the experience remains limited, and additional study comparing the device with other treatments and/or with placebo is needed, as are longer-term outcomes data.
"I think that although these results suggest this is a promising treatment, it would be best to treat patients only in trials" at this point, he said. Because trial participants have been carefully selected, it remains unclear whether this treatment is suitable for the entire GERD population, he added.
Dr. Soffer agreed, and said that if the results are reproduced in additional studies with a larger number of patients, the intervention will provide an alternative therapy for GERD patients who are not satisfied with PPIs or who have concerns about side effects and the chronic use of treatment, and who also have concerns about the established surgical treatment for GERD.
"The importance of this intervention is in providing a bridge between the currently established drug therapy for GERD [PPIs] and the established surgical therapy [fundoplication]. While PPIs are effective in a substantial number of GERD patients, they do not correct the underlying pathophysiology of GERD, resulting in a substantial number of patients who remain symptomatic in spite of therapy," he said.
These patients can be offered fundoplication, which is effective in expert hands, but the surgery has side effects and is performed less and less often, he added.
"Consequently, there is a search for a bridge intervention, endoscopic or surgical, for the treatment of GERD," he said.
LES-EST appears to have the potential to be such a bridge intervention.
"The procedure is simple and nondisruptive, and addresses pathophysiology. The safety profile thus far is excellent, and the effect on esophageal acid exposure, symptoms, and PPI use is sustained over a period of 12-18 moths. Furthermore, the treatment can be optimized to individual needs by adjusting delivery of stimulation to coincide with periods when symptoms and acid reflux are detected," he said.
All three of these studies presented at the meeting were supported by EndoStim BV. Dr. Soffer disclosed that he has stockholder/ownership interest in the company. Dr. Crowell disclosed that he has served as a consultant to the company. Dr. Bredenoord reported receiving grant and/or research support from the company.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF GASTROENTEROLOGY
SLN surgery may suffice for node-positive breast cancer
SAN ANTONIO – Women undergoing neoadjuvant chemotherapy for node-positive breast cancer may be able to have sentinel lymph node surgery instead of an axillary lymph node dissection, but proper surgical technique is critical for staging accuracy, a phase II trial from the American College of Surgeons Oncology Group suggests.
Among the 637 women studied in ACOSOG Z1071, all received chemotherapy and then underwent both sentinel lymph node (SLN) surgery and axillary lymph node dissection (ALND). SLN surgery correctly identified nodal status in 91.2% of cases, lead investigator Dr. Judy C. Boughey reported at the San Antonio Breast Cancer Symposium.
The false-negative rate of SLN averaged 12.6% in women with clinical N1 disease who had at least two sentinel nodes examined – slightly higher than the 10% set as a predefined endpoint. But it was lower when both blue dye and radiolabeled colloid were used to identify sentinel nodes (10.8%) and when three or more sentinel nodes were examined (9.1%).
"SLN surgery is a useful tool for detecting residual nodal disease in those women who present with node-positive breast cancer receiving neoadjuvant chemotherapy," Dr. Boughey commented in a press briefing. "Using SLN surgery in this patient population will enable us to reduce the extent of axillary surgery and therefore decrease morbidities for women treated for breast cancer."
Women were eligible for the trial if they had node-positive (T0-4, N1-2) breast cancer. After neoadjuvant chemotherapy, they underwent definitive breast surgery (lumpectomy or mastectomy), along with SLN surgery followed by a completion ALND. Patients who had N3 disease, inflammatory breast cancer, or prior ipsilateral axillary surgery were excluded.
Nodes were defined as being positive if they contained a tumor deposit measuring greater than 0.2 mm on sections stained with hematoxylin and eosin.
Sentinel nodes were identified in 92.7% of patients overall. A total of 40% of patients had no detectable nodal disease after neoadjuvant chemotherapy and thus would be unlikely to benefit from undergoing ALND, according to Dr. Boughey, a surgeon at the Mayo Clinic in Rochester, Minn.
Among the 60% of patients with detectable nodal disease (subsequently used to assess the false-negative rate of SLN), 85% had only positive sentinel nodes.
When only a single SLN was examined, the false-negative rate of SLN surgery was 31.5%, so Dr. Boughey recommends resecting a minimum of two nodes.
The false-negative rate was also lower when sentinel nodes were pathologically examined and determined to contain histologic changes (10.8%) and when a clip placed in the node at initial diagnosis was subsequently found at definitive surgery (7.4%).
"It’s important to collaborate with our radiology colleagues regarding potential for clip placement in lymph nodes, as well as our pathologists for review of sentinel lymph nodes for the presence of treatment effect," she said.
In the session where the results were presented, Dr. J. Michael Dixon of the Western General Hospital in Edinburgh asked whether a minimum of three nodes should be taken, because "if you take three or more nodes, your false-negative rate is within the range that is acceptable. Yet your conclusions said two. So I wonder if you get a second chance, you can tell us that we can do this technique if we use dual isotope and if we take three or more sentinel nodes and follow your other rules."
"We framed the conclusion based on the way the protocol had been written up front with two or more, but I think your comments are spot on," replied Dr. Boughey.
Dr. Steven Vogl of the Montefiore Medical Center in the Bronx, New York, asked about pathologic complete response (pCR).
"We did not require any specific degree of response for the patients to be in the study, since all of the patients were getting a completion ALND," Dr. Boughey replied. "We are currently evaluating specifically that question about whether the breast response and/or the nodal response on ultrasound can help define the appropriate patient population for us to tailor this therapy to."
Dr. Vogl noted that for patients who are HER2-positive, ER-negative, and triple-negative, pCR is very important. "So if we can figure out very carefully who didn’t achieve a pCR, especially in the node, we can probably do something for those patients some day with the right agents," he said.
"Do you use clips in all patients? Do you use dual agents always? And do you always remove two sentinel nodes? What is the impact of this on what we should do next?" asked session moderator Dr. Anthony Lucci Jr., of the University of Texas M.D. Anderson Cancer Center in Houston.
Dr. Boughey replied, "The take-home message is ... I’ll be looking at clip placement, making sure that we use dual-agent tracer for these cases, and ensuring that we do a thorough evaluation of the axilla and resecting any node that is radioactive, blue, or palpable.
"One of the concerns always when you are doing the sentinel node and you know you are doing a planned dissection [thereafter] is that the completeness of the evaluation of the axilla may not be quite as thorough as if you are closing as soon as you finish that sentinel node biopsy. So I think that is where the onus rests on the surgeon, so that we thoroughly evaluate the axilla and ensure this technique is as thorough as possible," she added.
In an additional analysis of patients with clinical N2 disease, the false-negative rate of SLN was 0%.
"Further work is under way regarding the secondary endpoint of this study, which will look at correlating the axillary ultrasound after chemotherapy with the false-negative rate. ... Maybe this can help improve patient selection for the procedure and further lower the false-negative rate," Dr. Boughey said. "We are also continuing to work to evaluate lymphedema rates and quality of life in these patients."
Dr. Boughey disclosed no relevant conflicts of interest.
SAN ANTONIO – Women undergoing neoadjuvant chemotherapy for node-positive breast cancer may be able to have sentinel lymph node surgery instead of an axillary lymph node dissection, but proper surgical technique is critical for staging accuracy, a phase II trial from the American College of Surgeons Oncology Group suggests.
Among the 637 women studied in ACOSOG Z1071, all received chemotherapy and then underwent both sentinel lymph node (SLN) surgery and axillary lymph node dissection (ALND). SLN surgery correctly identified nodal status in 91.2% of cases, lead investigator Dr. Judy C. Boughey reported at the San Antonio Breast Cancer Symposium.
The false-negative rate of SLN averaged 12.6% in women with clinical N1 disease who had at least two sentinel nodes examined – slightly higher than the 10% set as a predefined endpoint. But it was lower when both blue dye and radiolabeled colloid were used to identify sentinel nodes (10.8%) and when three or more sentinel nodes were examined (9.1%).
"SLN surgery is a useful tool for detecting residual nodal disease in those women who present with node-positive breast cancer receiving neoadjuvant chemotherapy," Dr. Boughey commented in a press briefing. "Using SLN surgery in this patient population will enable us to reduce the extent of axillary surgery and therefore decrease morbidities for women treated for breast cancer."
Women were eligible for the trial if they had node-positive (T0-4, N1-2) breast cancer. After neoadjuvant chemotherapy, they underwent definitive breast surgery (lumpectomy or mastectomy), along with SLN surgery followed by a completion ALND. Patients who had N3 disease, inflammatory breast cancer, or prior ipsilateral axillary surgery were excluded.
Nodes were defined as being positive if they contained a tumor deposit measuring greater than 0.2 mm on sections stained with hematoxylin and eosin.
Sentinel nodes were identified in 92.7% of patients overall. A total of 40% of patients had no detectable nodal disease after neoadjuvant chemotherapy and thus would be unlikely to benefit from undergoing ALND, according to Dr. Boughey, a surgeon at the Mayo Clinic in Rochester, Minn.
Among the 60% of patients with detectable nodal disease (subsequently used to assess the false-negative rate of SLN), 85% had only positive sentinel nodes.
When only a single SLN was examined, the false-negative rate of SLN surgery was 31.5%, so Dr. Boughey recommends resecting a minimum of two nodes.
The false-negative rate was also lower when sentinel nodes were pathologically examined and determined to contain histologic changes (10.8%) and when a clip placed in the node at initial diagnosis was subsequently found at definitive surgery (7.4%).
"It’s important to collaborate with our radiology colleagues regarding potential for clip placement in lymph nodes, as well as our pathologists for review of sentinel lymph nodes for the presence of treatment effect," she said.
In the session where the results were presented, Dr. J. Michael Dixon of the Western General Hospital in Edinburgh asked whether a minimum of three nodes should be taken, because "if you take three or more nodes, your false-negative rate is within the range that is acceptable. Yet your conclusions said two. So I wonder if you get a second chance, you can tell us that we can do this technique if we use dual isotope and if we take three or more sentinel nodes and follow your other rules."
"We framed the conclusion based on the way the protocol had been written up front with two or more, but I think your comments are spot on," replied Dr. Boughey.
Dr. Steven Vogl of the Montefiore Medical Center in the Bronx, New York, asked about pathologic complete response (pCR).
"We did not require any specific degree of response for the patients to be in the study, since all of the patients were getting a completion ALND," Dr. Boughey replied. "We are currently evaluating specifically that question about whether the breast response and/or the nodal response on ultrasound can help define the appropriate patient population for us to tailor this therapy to."
Dr. Vogl noted that for patients who are HER2-positive, ER-negative, and triple-negative, pCR is very important. "So if we can figure out very carefully who didn’t achieve a pCR, especially in the node, we can probably do something for those patients some day with the right agents," he said.
"Do you use clips in all patients? Do you use dual agents always? And do you always remove two sentinel nodes? What is the impact of this on what we should do next?" asked session moderator Dr. Anthony Lucci Jr., of the University of Texas M.D. Anderson Cancer Center in Houston.
Dr. Boughey replied, "The take-home message is ... I’ll be looking at clip placement, making sure that we use dual-agent tracer for these cases, and ensuring that we do a thorough evaluation of the axilla and resecting any node that is radioactive, blue, or palpable.
"One of the concerns always when you are doing the sentinel node and you know you are doing a planned dissection [thereafter] is that the completeness of the evaluation of the axilla may not be quite as thorough as if you are closing as soon as you finish that sentinel node biopsy. So I think that is where the onus rests on the surgeon, so that we thoroughly evaluate the axilla and ensure this technique is as thorough as possible," she added.
In an additional analysis of patients with clinical N2 disease, the false-negative rate of SLN was 0%.
"Further work is under way regarding the secondary endpoint of this study, which will look at correlating the axillary ultrasound after chemotherapy with the false-negative rate. ... Maybe this can help improve patient selection for the procedure and further lower the false-negative rate," Dr. Boughey said. "We are also continuing to work to evaluate lymphedema rates and quality of life in these patients."
Dr. Boughey disclosed no relevant conflicts of interest.
SAN ANTONIO – Women undergoing neoadjuvant chemotherapy for node-positive breast cancer may be able to have sentinel lymph node surgery instead of an axillary lymph node dissection, but proper surgical technique is critical for staging accuracy, a phase II trial from the American College of Surgeons Oncology Group suggests.
Among the 637 women studied in ACOSOG Z1071, all received chemotherapy and then underwent both sentinel lymph node (SLN) surgery and axillary lymph node dissection (ALND). SLN surgery correctly identified nodal status in 91.2% of cases, lead investigator Dr. Judy C. Boughey reported at the San Antonio Breast Cancer Symposium.
The false-negative rate of SLN averaged 12.6% in women with clinical N1 disease who had at least two sentinel nodes examined – slightly higher than the 10% set as a predefined endpoint. But it was lower when both blue dye and radiolabeled colloid were used to identify sentinel nodes (10.8%) and when three or more sentinel nodes were examined (9.1%).
"SLN surgery is a useful tool for detecting residual nodal disease in those women who present with node-positive breast cancer receiving neoadjuvant chemotherapy," Dr. Boughey commented in a press briefing. "Using SLN surgery in this patient population will enable us to reduce the extent of axillary surgery and therefore decrease morbidities for women treated for breast cancer."
Women were eligible for the trial if they had node-positive (T0-4, N1-2) breast cancer. After neoadjuvant chemotherapy, they underwent definitive breast surgery (lumpectomy or mastectomy), along with SLN surgery followed by a completion ALND. Patients who had N3 disease, inflammatory breast cancer, or prior ipsilateral axillary surgery were excluded.
Nodes were defined as being positive if they contained a tumor deposit measuring greater than 0.2 mm on sections stained with hematoxylin and eosin.
Sentinel nodes were identified in 92.7% of patients overall. A total of 40% of patients had no detectable nodal disease after neoadjuvant chemotherapy and thus would be unlikely to benefit from undergoing ALND, according to Dr. Boughey, a surgeon at the Mayo Clinic in Rochester, Minn.
Among the 60% of patients with detectable nodal disease (subsequently used to assess the false-negative rate of SLN), 85% had only positive sentinel nodes.
When only a single SLN was examined, the false-negative rate of SLN surgery was 31.5%, so Dr. Boughey recommends resecting a minimum of two nodes.
The false-negative rate was also lower when sentinel nodes were pathologically examined and determined to contain histologic changes (10.8%) and when a clip placed in the node at initial diagnosis was subsequently found at definitive surgery (7.4%).
"It’s important to collaborate with our radiology colleagues regarding potential for clip placement in lymph nodes, as well as our pathologists for review of sentinel lymph nodes for the presence of treatment effect," she said.
In the session where the results were presented, Dr. J. Michael Dixon of the Western General Hospital in Edinburgh asked whether a minimum of three nodes should be taken, because "if you take three or more nodes, your false-negative rate is within the range that is acceptable. Yet your conclusions said two. So I wonder if you get a second chance, you can tell us that we can do this technique if we use dual isotope and if we take three or more sentinel nodes and follow your other rules."
"We framed the conclusion based on the way the protocol had been written up front with two or more, but I think your comments are spot on," replied Dr. Boughey.
Dr. Steven Vogl of the Montefiore Medical Center in the Bronx, New York, asked about pathologic complete response (pCR).
"We did not require any specific degree of response for the patients to be in the study, since all of the patients were getting a completion ALND," Dr. Boughey replied. "We are currently evaluating specifically that question about whether the breast response and/or the nodal response on ultrasound can help define the appropriate patient population for us to tailor this therapy to."
Dr. Vogl noted that for patients who are HER2-positive, ER-negative, and triple-negative, pCR is very important. "So if we can figure out very carefully who didn’t achieve a pCR, especially in the node, we can probably do something for those patients some day with the right agents," he said.
"Do you use clips in all patients? Do you use dual agents always? And do you always remove two sentinel nodes? What is the impact of this on what we should do next?" asked session moderator Dr. Anthony Lucci Jr., of the University of Texas M.D. Anderson Cancer Center in Houston.
Dr. Boughey replied, "The take-home message is ... I’ll be looking at clip placement, making sure that we use dual-agent tracer for these cases, and ensuring that we do a thorough evaluation of the axilla and resecting any node that is radioactive, blue, or palpable.
"One of the concerns always when you are doing the sentinel node and you know you are doing a planned dissection [thereafter] is that the completeness of the evaluation of the axilla may not be quite as thorough as if you are closing as soon as you finish that sentinel node biopsy. So I think that is where the onus rests on the surgeon, so that we thoroughly evaluate the axilla and ensure this technique is as thorough as possible," she added.
In an additional analysis of patients with clinical N2 disease, the false-negative rate of SLN was 0%.
"Further work is under way regarding the secondary endpoint of this study, which will look at correlating the axillary ultrasound after chemotherapy with the false-negative rate. ... Maybe this can help improve patient selection for the procedure and further lower the false-negative rate," Dr. Boughey said. "We are also continuing to work to evaluate lymphedema rates and quality of life in these patients."
Dr. Boughey disclosed no relevant conflicts of interest.
AT THE SAN ANTONIO BREAST CANCER SYMPOSIUM
Major Finding: SLN surgery correctly identified axillary nodal status in 91.2% of patients. The false-negative rate was 12.6% among women with clinical N1 disease who had at least two sentinel nodes examined.
Data Source: A multicenter phase II trial involving 637 patients with node-positive breast cancer who received neoadjuvant chemotherapy (the ACOSOG Z1071 trial).
Disclosures: Dr. Boughey disclosed no relevant conflicts of interest.
Dr. Raul Ruiz goes to Washington
Dr. Raul Ruiz has traded in his white coat for an office on Capitol Hill. An emergency physician from California’s Coachella Valley, Dr. Ruiz is the newest physician, and one of three democrat physicians, serving in Congress. When the 113th Congress begins on Jan. 3, Dr. Ruiz said he will focus on physician payment reform as well as addressing disparities in income, healthcare, and education.
Unlike many congressional physicians – the majority of whom are Republicans – Dr. Ruiz said he wants to keep some Affordable Care Act provisions in place, while ensuring the health care workforce can support them. To find out more about Dr. Ruiz, check out our video.
Dr. Raul Ruiz has traded in his white coat for an office on Capitol Hill. An emergency physician from California’s Coachella Valley, Dr. Ruiz is the newest physician, and one of three democrat physicians, serving in Congress. When the 113th Congress begins on Jan. 3, Dr. Ruiz said he will focus on physician payment reform as well as addressing disparities in income, healthcare, and education.
Unlike many congressional physicians – the majority of whom are Republicans – Dr. Ruiz said he wants to keep some Affordable Care Act provisions in place, while ensuring the health care workforce can support them. To find out more about Dr. Ruiz, check out our video.
Dr. Raul Ruiz has traded in his white coat for an office on Capitol Hill. An emergency physician from California’s Coachella Valley, Dr. Ruiz is the newest physician, and one of three democrat physicians, serving in Congress. When the 113th Congress begins on Jan. 3, Dr. Ruiz said he will focus on physician payment reform as well as addressing disparities in income, healthcare, and education.
Unlike many congressional physicians – the majority of whom are Republicans – Dr. Ruiz said he wants to keep some Affordable Care Act provisions in place, while ensuring the health care workforce can support them. To find out more about Dr. Ruiz, check out our video.
Docs to Congress: SGR fix can't wait
The American Medical Association, the American College of Family Physicians, the American College of Physicians, the American College of Surgeons, and the American Osteopathic Association together met with more than a dozen lawmakers.
The American Medical Association, the American College of Family Physicians, the American College of Physicians, the American College of Surgeons, and the American Osteopathic Association together met with more than a dozen lawmakers.
The American Medical Association, the American College of Family Physicians, the American College of Physicians, the American College of Surgeons, and the American Osteopathic Association together met with more than a dozen lawmakers.
Contact precautions linked to fewer and shorter patient visits
Health care workers spent less time with patients who were on contact precautions, based on results from a prospective study in the January 2013 issue of Infection Control and Hospital Epidemiology.
Patients on contact precautions for drug-resistant infections had almost 40% fewer visits from health care workers. Further, when they did visit, health care workers spent significantly less time in the rooms of patients on precautions, reported Dr. Daniel Morgan and his associates.
On a positive note, handwashing hygiene improved when health care workers saw patient on contact precautions (Infect. Control Hosp. Epidemiol. 2013;34:69-73).
"Contact precautions modify health care workers’ behavior. This has positive and negative consequences," Dr. Morgan, the lead author, said in an interview.
"Health care workers should be aware of the tendency to visit patients less often and question their own behavior when caring for these patients," said Dr. Morgan of the University of Maryland and the Veterans Affairs (VA) Maryland Health Care System, Baltimore. "Do they visit them less often? Are they at risk of missing anything because a patient is on precautions? Are they creating workarounds for the inconvenience that may impact the patient?"
Research is underway looking at outcomes of patients on isolation and ways to improve these outcomes, "but for a start, it is important that health care workers consider how their behavior may be shaped by contact precautions," he added.
In the prospective cohort study, the activity of health care workers at four acute hospitals was observed for 1-hour periods over 19 months. The trained observers – so-called "secret shoppers" – observed a total of 7,743 visits over 1,989 hours in seven intensive care units and six medical surgical wards at three VA Hospitals and at one medical center, the University of Maryland Medical Center in Baltimore.
Patients on contact precautions had 2.78 visits per hour from health care workers, compared with 4.37 visits per hour among those not on precautions, a statistically significant difference.
Health care workers also spent significantly less time – nearly 18% less – with patients on contact precautions. Time spent per hour was 14 minutes for patients on precautions and 17 minutes for other patients. The time spent with patients in ICUs, however, was similar irrespective of contact precautions.
Health care workers were almost 16% more likely to comply with proper hand hygiene techniques when exiting the rooms of patients on contact precautions. Proper hand washing was observed 63% of the time when leaving the room of a patient on precautions and 47% of the time when exiting the room of a patient not on precautions. This statistically significant difference was "more pronounced" in the ICU setting, the authors wrote.
Contact precautions did not appear to affect compliance with hand hygiene when entering a patient’s room. Overall, the compliance rate with gowns and gloves was 66% for patients on contact precautions.
The compliance rates for hand hygiene and use of gown and gloves recorded in the study were lower than the rates hospitals often report to hospital regulators, but they are in the range of what is routinely reported in more rigorous research, Dr. Morgan said in an interview.
The reduced contact between patients on contact precautions and health care workers was "likely" caused by the "inconvenience of donning gowns and gloves," the authors wrote. The lack of a difference in contact in the ICU could be the "higher acuity of care" or the higher nurse-to-patient ratio, whereby gloves and gowns do not need to be changed as frequently.
The "unintended consequences" of contact precautions are a particular concern now that contact precautions have become more common with programs like the Department of Veterans Affairs MRSA Prevention Initiative, Dr. Morgan and his associates said. The decrease in contact with health care workers "may lead to increased adverse events and a lower quality of patient care due to less consistent patient monitoring and poorer adherence to standard adverse event prevention methods" such as protocols to prevent pressure ulcers, they suggested.
The only non-ICU units observed in the study were in VA hospitals, which was one of the limitations of the study cited by the authors. The strengths of the study included the nearly 2,000 hours of observations at hospitals in different parts of the country.
"We don’t know whether less frequent visits to the patient room necessarily means more adverse events," Dr. Anthony Harris, professor of epidemiology and public health at the University of Maryland, said in an interview. Previous research indicating that contact precautions led to adverse events had some serious methodological flaws.
Dr. Harris, acting medical director of infection control at the University of Maryland Medical Center, is involved in a randomized study evaluating whether universal glove and gown precautions lead to improved or worse outcomes. The study, funded by the Agency for Healthcare Research and Quality (AHRQ), also is examining the frequency of health care worker visits and adverse events and should "provide more definitive answers to the important question of whether contact precautions lead to more adverse events," he said.
Financial support for Dr. Morgan’s study was provided by the VA Health Affairs Services Research and Development Investigator Initiated Research, Association of American Medical Colleges/Centers for Disease Control and Prevention, and AHRQ. Dr. Morgan disclosed having received an unrestricted research grant from Merck; the other authors had no relevant conflicts of interest to disclose. Dr. Harris is on the board of the Society for Healthcare Epidemiology of America, which publishes Infection Control and Hospital Epidemiology.
Health care workers spent less time with patients who were on contact precautions, based on results from a prospective study in the January 2013 issue of Infection Control and Hospital Epidemiology.
Patients on contact precautions for drug-resistant infections had almost 40% fewer visits from health care workers. Further, when they did visit, health care workers spent significantly less time in the rooms of patients on precautions, reported Dr. Daniel Morgan and his associates.
On a positive note, handwashing hygiene improved when health care workers saw patient on contact precautions (Infect. Control Hosp. Epidemiol. 2013;34:69-73).
"Contact precautions modify health care workers’ behavior. This has positive and negative consequences," Dr. Morgan, the lead author, said in an interview.
"Health care workers should be aware of the tendency to visit patients less often and question their own behavior when caring for these patients," said Dr. Morgan of the University of Maryland and the Veterans Affairs (VA) Maryland Health Care System, Baltimore. "Do they visit them less often? Are they at risk of missing anything because a patient is on precautions? Are they creating workarounds for the inconvenience that may impact the patient?"
Research is underway looking at outcomes of patients on isolation and ways to improve these outcomes, "but for a start, it is important that health care workers consider how their behavior may be shaped by contact precautions," he added.
In the prospective cohort study, the activity of health care workers at four acute hospitals was observed for 1-hour periods over 19 months. The trained observers – so-called "secret shoppers" – observed a total of 7,743 visits over 1,989 hours in seven intensive care units and six medical surgical wards at three VA Hospitals and at one medical center, the University of Maryland Medical Center in Baltimore.
Patients on contact precautions had 2.78 visits per hour from health care workers, compared with 4.37 visits per hour among those not on precautions, a statistically significant difference.
Health care workers also spent significantly less time – nearly 18% less – with patients on contact precautions. Time spent per hour was 14 minutes for patients on precautions and 17 minutes for other patients. The time spent with patients in ICUs, however, was similar irrespective of contact precautions.
Health care workers were almost 16% more likely to comply with proper hand hygiene techniques when exiting the rooms of patients on contact precautions. Proper hand washing was observed 63% of the time when leaving the room of a patient on precautions and 47% of the time when exiting the room of a patient not on precautions. This statistically significant difference was "more pronounced" in the ICU setting, the authors wrote.
Contact precautions did not appear to affect compliance with hand hygiene when entering a patient’s room. Overall, the compliance rate with gowns and gloves was 66% for patients on contact precautions.
The compliance rates for hand hygiene and use of gown and gloves recorded in the study were lower than the rates hospitals often report to hospital regulators, but they are in the range of what is routinely reported in more rigorous research, Dr. Morgan said in an interview.
The reduced contact between patients on contact precautions and health care workers was "likely" caused by the "inconvenience of donning gowns and gloves," the authors wrote. The lack of a difference in contact in the ICU could be the "higher acuity of care" or the higher nurse-to-patient ratio, whereby gloves and gowns do not need to be changed as frequently.
The "unintended consequences" of contact precautions are a particular concern now that contact precautions have become more common with programs like the Department of Veterans Affairs MRSA Prevention Initiative, Dr. Morgan and his associates said. The decrease in contact with health care workers "may lead to increased adverse events and a lower quality of patient care due to less consistent patient monitoring and poorer adherence to standard adverse event prevention methods" such as protocols to prevent pressure ulcers, they suggested.
The only non-ICU units observed in the study were in VA hospitals, which was one of the limitations of the study cited by the authors. The strengths of the study included the nearly 2,000 hours of observations at hospitals in different parts of the country.
"We don’t know whether less frequent visits to the patient room necessarily means more adverse events," Dr. Anthony Harris, professor of epidemiology and public health at the University of Maryland, said in an interview. Previous research indicating that contact precautions led to adverse events had some serious methodological flaws.
Dr. Harris, acting medical director of infection control at the University of Maryland Medical Center, is involved in a randomized study evaluating whether universal glove and gown precautions lead to improved or worse outcomes. The study, funded by the Agency for Healthcare Research and Quality (AHRQ), also is examining the frequency of health care worker visits and adverse events and should "provide more definitive answers to the important question of whether contact precautions lead to more adverse events," he said.
Financial support for Dr. Morgan’s study was provided by the VA Health Affairs Services Research and Development Investigator Initiated Research, Association of American Medical Colleges/Centers for Disease Control and Prevention, and AHRQ. Dr. Morgan disclosed having received an unrestricted research grant from Merck; the other authors had no relevant conflicts of interest to disclose. Dr. Harris is on the board of the Society for Healthcare Epidemiology of America, which publishes Infection Control and Hospital Epidemiology.
Health care workers spent less time with patients who were on contact precautions, based on results from a prospective study in the January 2013 issue of Infection Control and Hospital Epidemiology.
Patients on contact precautions for drug-resistant infections had almost 40% fewer visits from health care workers. Further, when they did visit, health care workers spent significantly less time in the rooms of patients on precautions, reported Dr. Daniel Morgan and his associates.
On a positive note, handwashing hygiene improved when health care workers saw patient on contact precautions (Infect. Control Hosp. Epidemiol. 2013;34:69-73).
"Contact precautions modify health care workers’ behavior. This has positive and negative consequences," Dr. Morgan, the lead author, said in an interview.
"Health care workers should be aware of the tendency to visit patients less often and question their own behavior when caring for these patients," said Dr. Morgan of the University of Maryland and the Veterans Affairs (VA) Maryland Health Care System, Baltimore. "Do they visit them less often? Are they at risk of missing anything because a patient is on precautions? Are they creating workarounds for the inconvenience that may impact the patient?"
Research is underway looking at outcomes of patients on isolation and ways to improve these outcomes, "but for a start, it is important that health care workers consider how their behavior may be shaped by contact precautions," he added.
In the prospective cohort study, the activity of health care workers at four acute hospitals was observed for 1-hour periods over 19 months. The trained observers – so-called "secret shoppers" – observed a total of 7,743 visits over 1,989 hours in seven intensive care units and six medical surgical wards at three VA Hospitals and at one medical center, the University of Maryland Medical Center in Baltimore.
Patients on contact precautions had 2.78 visits per hour from health care workers, compared with 4.37 visits per hour among those not on precautions, a statistically significant difference.
Health care workers also spent significantly less time – nearly 18% less – with patients on contact precautions. Time spent per hour was 14 minutes for patients on precautions and 17 minutes for other patients. The time spent with patients in ICUs, however, was similar irrespective of contact precautions.
Health care workers were almost 16% more likely to comply with proper hand hygiene techniques when exiting the rooms of patients on contact precautions. Proper hand washing was observed 63% of the time when leaving the room of a patient on precautions and 47% of the time when exiting the room of a patient not on precautions. This statistically significant difference was "more pronounced" in the ICU setting, the authors wrote.
Contact precautions did not appear to affect compliance with hand hygiene when entering a patient’s room. Overall, the compliance rate with gowns and gloves was 66% for patients on contact precautions.
The compliance rates for hand hygiene and use of gown and gloves recorded in the study were lower than the rates hospitals often report to hospital regulators, but they are in the range of what is routinely reported in more rigorous research, Dr. Morgan said in an interview.
The reduced contact between patients on contact precautions and health care workers was "likely" caused by the "inconvenience of donning gowns and gloves," the authors wrote. The lack of a difference in contact in the ICU could be the "higher acuity of care" or the higher nurse-to-patient ratio, whereby gloves and gowns do not need to be changed as frequently.
The "unintended consequences" of contact precautions are a particular concern now that contact precautions have become more common with programs like the Department of Veterans Affairs MRSA Prevention Initiative, Dr. Morgan and his associates said. The decrease in contact with health care workers "may lead to increased adverse events and a lower quality of patient care due to less consistent patient monitoring and poorer adherence to standard adverse event prevention methods" such as protocols to prevent pressure ulcers, they suggested.
The only non-ICU units observed in the study were in VA hospitals, which was one of the limitations of the study cited by the authors. The strengths of the study included the nearly 2,000 hours of observations at hospitals in different parts of the country.
"We don’t know whether less frequent visits to the patient room necessarily means more adverse events," Dr. Anthony Harris, professor of epidemiology and public health at the University of Maryland, said in an interview. Previous research indicating that contact precautions led to adverse events had some serious methodological flaws.
Dr. Harris, acting medical director of infection control at the University of Maryland Medical Center, is involved in a randomized study evaluating whether universal glove and gown precautions lead to improved or worse outcomes. The study, funded by the Agency for Healthcare Research and Quality (AHRQ), also is examining the frequency of health care worker visits and adverse events and should "provide more definitive answers to the important question of whether contact precautions lead to more adverse events," he said.
Financial support for Dr. Morgan’s study was provided by the VA Health Affairs Services Research and Development Investigator Initiated Research, Association of American Medical Colleges/Centers for Disease Control and Prevention, and AHRQ. Dr. Morgan disclosed having received an unrestricted research grant from Merck; the other authors had no relevant conflicts of interest to disclose. Dr. Harris is on the board of the Society for Healthcare Epidemiology of America, which publishes Infection Control and Hospital Epidemiology.
FROM INFECTION CONTROL AND HOSPITAL EPIDEMIOLOGY
Major Finding: Patients on contact precautions had 2.78 visits per hour from health care workers, compared with 4.37 visits per hour among those not on precautions.
Data Source: In the prospective cohort study, trained observers secretly monitored the activity of health care workers at four acute care hospitals for a total of 7,743 visits.
Disclosures: Financial support for the study was provided by the VA Health Affairs Services Research and Development Investigator Initiated Research, Association of American Medical Colleges/Centers for Disease Control and Prevention, and the Agency for Healthcare Research and Quality. Dr. Morgan disclosed having received an unrestricted research grant from Merck; the other authors had no relevant conflicts.
Rate of pediatric caustic ingestion injuries quite low
The prevalence of caustic ingestion injuries among children and adolescents in the United States is quite low, estimated to be only 1.08 per 100,000 population, according to a report in the December issue of Archives of Otolaryngology and Head & Neck Surgery.
This represents a substantial decrease from figures widely stated in the literature, which are based on data from the 1970s and 1980s, when public health measures were first taken to reduce children’s exposure to lye and other caustics, said Dr. Christopher M. Johnson and Dr. Matthew T. Brigger of the department of otolaryngology, Naval Medical Center, San Diego.
"The burden of caustic ingestion injuries in children appears to have decreased over time, and past public health interventions appear to have been successful," Dr. Johnson and Dr. Brigger wrote.
They examined this issue in part because of the paucity of epidemiologic data regarding caustic ingestions. To assess the current public health burden of these pediatric injuries, they analyzed information in the Kids’ Inpatient Database (KID), a national resource maintained by the Agency for Healthcare Research and Quality, which collects nationally representative samples of all pediatric hospital discharges each year.
The researchers assessed KID data for 2009, when 3,407,146 pediatric hospitalizations were sampled.
Extrapolating the data to the entire U.S. population, the investigators estimated that there were 807 hospitalizations nationwide for caustic ingestion injuries among patients aged 0-18 years in 2009, for a prevalence of 1.08 per 100,000.
Previously published estimates ranged from 5,000 to 15,000 cases each year but were based on outdated data, the investigators noted (Arch. Otolaryngol. Head Neck Surg. 2012;138:1111-5).
Even though the actual prevalence of these injuries has dropped so precipitously, children with caustic ingestion injuries still accounted for more than $22 million in hospital charges and more than 3,300 inpatient days in 2009, they reported.
Approximately 60% of these ingestions occurred in children aged 4 years and younger. A second peak in prevalence occurred in the adolescent age group, presumably because of intentional ingestions in suicide attempts.
Only about half of all pediatric patients hospitalized for caustic ingestion underwent esophagoscopy in 2009. Since this procedure is recommended for all children with a "strongly suggestive" history as well as for those who are symptomatic, "a logical conclusion is that a large proportion of children are admitted to the hospital for observation, even if suspicion of significant injury is low," Dr. Johnson and Dr. Brigger said.
"We found a higher burden of injury in urban hospitals and in patients who lived in zip codes in the bottom quartile of median annual income in the United States. This finding is consistent with available pediatric poisoning data that indicate that low-income urban households are more likely to store dangerous household products improperly," they added.
No financial conflicts of interest were reported.
The prevalence of caustic ingestion injuries among children and adolescents in the United States is quite low, estimated to be only 1.08 per 100,000 population, according to a report in the December issue of Archives of Otolaryngology and Head & Neck Surgery.
This represents a substantial decrease from figures widely stated in the literature, which are based on data from the 1970s and 1980s, when public health measures were first taken to reduce children’s exposure to lye and other caustics, said Dr. Christopher M. Johnson and Dr. Matthew T. Brigger of the department of otolaryngology, Naval Medical Center, San Diego.
"The burden of caustic ingestion injuries in children appears to have decreased over time, and past public health interventions appear to have been successful," Dr. Johnson and Dr. Brigger wrote.
They examined this issue in part because of the paucity of epidemiologic data regarding caustic ingestions. To assess the current public health burden of these pediatric injuries, they analyzed information in the Kids’ Inpatient Database (KID), a national resource maintained by the Agency for Healthcare Research and Quality, which collects nationally representative samples of all pediatric hospital discharges each year.
The researchers assessed KID data for 2009, when 3,407,146 pediatric hospitalizations were sampled.
Extrapolating the data to the entire U.S. population, the investigators estimated that there were 807 hospitalizations nationwide for caustic ingestion injuries among patients aged 0-18 years in 2009, for a prevalence of 1.08 per 100,000.
Previously published estimates ranged from 5,000 to 15,000 cases each year but were based on outdated data, the investigators noted (Arch. Otolaryngol. Head Neck Surg. 2012;138:1111-5).
Even though the actual prevalence of these injuries has dropped so precipitously, children with caustic ingestion injuries still accounted for more than $22 million in hospital charges and more than 3,300 inpatient days in 2009, they reported.
Approximately 60% of these ingestions occurred in children aged 4 years and younger. A second peak in prevalence occurred in the adolescent age group, presumably because of intentional ingestions in suicide attempts.
Only about half of all pediatric patients hospitalized for caustic ingestion underwent esophagoscopy in 2009. Since this procedure is recommended for all children with a "strongly suggestive" history as well as for those who are symptomatic, "a logical conclusion is that a large proportion of children are admitted to the hospital for observation, even if suspicion of significant injury is low," Dr. Johnson and Dr. Brigger said.
"We found a higher burden of injury in urban hospitals and in patients who lived in zip codes in the bottom quartile of median annual income in the United States. This finding is consistent with available pediatric poisoning data that indicate that low-income urban households are more likely to store dangerous household products improperly," they added.
No financial conflicts of interest were reported.
The prevalence of caustic ingestion injuries among children and adolescents in the United States is quite low, estimated to be only 1.08 per 100,000 population, according to a report in the December issue of Archives of Otolaryngology and Head & Neck Surgery.
This represents a substantial decrease from figures widely stated in the literature, which are based on data from the 1970s and 1980s, when public health measures were first taken to reduce children’s exposure to lye and other caustics, said Dr. Christopher M. Johnson and Dr. Matthew T. Brigger of the department of otolaryngology, Naval Medical Center, San Diego.
"The burden of caustic ingestion injuries in children appears to have decreased over time, and past public health interventions appear to have been successful," Dr. Johnson and Dr. Brigger wrote.
They examined this issue in part because of the paucity of epidemiologic data regarding caustic ingestions. To assess the current public health burden of these pediatric injuries, they analyzed information in the Kids’ Inpatient Database (KID), a national resource maintained by the Agency for Healthcare Research and Quality, which collects nationally representative samples of all pediatric hospital discharges each year.
The researchers assessed KID data for 2009, when 3,407,146 pediatric hospitalizations were sampled.
Extrapolating the data to the entire U.S. population, the investigators estimated that there were 807 hospitalizations nationwide for caustic ingestion injuries among patients aged 0-18 years in 2009, for a prevalence of 1.08 per 100,000.
Previously published estimates ranged from 5,000 to 15,000 cases each year but were based on outdated data, the investigators noted (Arch. Otolaryngol. Head Neck Surg. 2012;138:1111-5).
Even though the actual prevalence of these injuries has dropped so precipitously, children with caustic ingestion injuries still accounted for more than $22 million in hospital charges and more than 3,300 inpatient days in 2009, they reported.
Approximately 60% of these ingestions occurred in children aged 4 years and younger. A second peak in prevalence occurred in the adolescent age group, presumably because of intentional ingestions in suicide attempts.
Only about half of all pediatric patients hospitalized for caustic ingestion underwent esophagoscopy in 2009. Since this procedure is recommended for all children with a "strongly suggestive" history as well as for those who are symptomatic, "a logical conclusion is that a large proportion of children are admitted to the hospital for observation, even if suspicion of significant injury is low," Dr. Johnson and Dr. Brigger said.
"We found a higher burden of injury in urban hospitals and in patients who lived in zip codes in the bottom quartile of median annual income in the United States. This finding is consistent with available pediatric poisoning data that indicate that low-income urban households are more likely to store dangerous household products improperly," they added.
No financial conflicts of interest were reported.
FROM ARCHIVES OF OTOLARYNGOLOGY AND HEAD & NECK SURGERY
Major Finding: There were an estimated 807 children and adolescents hospitalized nationwide for caustic ingestion injuries in 2009, for a prevalence of 1.08 per 100,000.
Data Source: An analysis of pediatric hospitalizations for caustic ingestion injuries using data from the Agency for Healthcare Research and Quality's Kids’ Inpatient Database.
Disclosures: No financial conflicts of interest were reported.
Late stop to antirheumatics may risk postsurgical infection
WASHINGTON – The risk of infection following orthopedic surgery is increased in patients with inflammatory rheumatic disease, compared with those with degenerative disease or traumatic injury, according to findings from a review of more than 50,000 surgical procedures.
The risk is greatest in those inflammatory rheumatic disease patients treated with conventional disease-modifying anti-rheumatic drugs (cDMARDs) or tumor necrosis factor (TNF) inhibitors, especially those receiving more than one cDMARD or TNF inhibitor with a long administration interval, and when surgery takes place without discontinuation of treatment, Catrina B. Scherrer reported at the annual meeting of the American College of Rheumatology.
Of 50,359 surgical procedures performed in 37,137 patients from a hospital surgery registry, 422 resulted in surgery-related infections. Of these infections, 49 occurred in 2,472 patients with an inflammatory rheumatic disease (IRD; 2%), and 373 occurred in 47,887 patients with degenerative disease/posttraumatic injury (0.8%). The difference was statistically significant, even after adjustment for other risk factors, including age, gender, diabetes, being overweight, cardiovascular disease, smoking, and type of surgery, said Ms. Scherrer of the Schulthess Clinic, Zürich.
The lowest rates of infection occurred with hand and shoulder surgery; the highest rates occurred with elbow surgery, she noted.
In 1,329 patients in the IRD group for whom complete information about medication was available, 171 (13%) had documented use of TNF inhibitors, and 49 of these (29%) discontinued treatment more than three administration intervals before surgery. Of the remaining 122 TNF inhibitor users, the time lag was three or fewer administration intervals.
An increased infection rate was seen in those who used more than one cDMARD (odds ratio, 2.425) and more than one TNF inhibitor (OR, 2.627) prior to surgery, and the risk of infection was increased tenfold when surgery was performed within one administration interval (OR, 10.047).
Patients who had their last treatment within one administration interval before surgery included 81% of infliximab users, compared with only 33% of adalimumab users and 24% of etanercept users, Ms. Scherrer noted.
Surgery patients in this study were followed over 8 years as part of a single-center surgery registry. The findings, which are limited by the study’s retrospective design and thus require confirmation in prospective studies, are nonetheless important because patients with aggressive disease such as IRDs frequently require orthopedic surgery.
The study findings suggest that IRD patients are, in general, at high risk of postoperative infection, that special attention should be paid to patients using more than one cDMARD or TNF inhibitor with long administration intervals, and that the last intake of TNF inhibitors – particularly infliximab – should be at least more than one administration interval before planned surgery, as the risk of postoperative infection is significantly increased if surgery occurs within this period, she concluded.
Ms. Scherrer reported having no disclosures.
WASHINGTON – The risk of infection following orthopedic surgery is increased in patients with inflammatory rheumatic disease, compared with those with degenerative disease or traumatic injury, according to findings from a review of more than 50,000 surgical procedures.
The risk is greatest in those inflammatory rheumatic disease patients treated with conventional disease-modifying anti-rheumatic drugs (cDMARDs) or tumor necrosis factor (TNF) inhibitors, especially those receiving more than one cDMARD or TNF inhibitor with a long administration interval, and when surgery takes place without discontinuation of treatment, Catrina B. Scherrer reported at the annual meeting of the American College of Rheumatology.
Of 50,359 surgical procedures performed in 37,137 patients from a hospital surgery registry, 422 resulted in surgery-related infections. Of these infections, 49 occurred in 2,472 patients with an inflammatory rheumatic disease (IRD; 2%), and 373 occurred in 47,887 patients with degenerative disease/posttraumatic injury (0.8%). The difference was statistically significant, even after adjustment for other risk factors, including age, gender, diabetes, being overweight, cardiovascular disease, smoking, and type of surgery, said Ms. Scherrer of the Schulthess Clinic, Zürich.
The lowest rates of infection occurred with hand and shoulder surgery; the highest rates occurred with elbow surgery, she noted.
In 1,329 patients in the IRD group for whom complete information about medication was available, 171 (13%) had documented use of TNF inhibitors, and 49 of these (29%) discontinued treatment more than three administration intervals before surgery. Of the remaining 122 TNF inhibitor users, the time lag was three or fewer administration intervals.
An increased infection rate was seen in those who used more than one cDMARD (odds ratio, 2.425) and more than one TNF inhibitor (OR, 2.627) prior to surgery, and the risk of infection was increased tenfold when surgery was performed within one administration interval (OR, 10.047).
Patients who had their last treatment within one administration interval before surgery included 81% of infliximab users, compared with only 33% of adalimumab users and 24% of etanercept users, Ms. Scherrer noted.
Surgery patients in this study were followed over 8 years as part of a single-center surgery registry. The findings, which are limited by the study’s retrospective design and thus require confirmation in prospective studies, are nonetheless important because patients with aggressive disease such as IRDs frequently require orthopedic surgery.
The study findings suggest that IRD patients are, in general, at high risk of postoperative infection, that special attention should be paid to patients using more than one cDMARD or TNF inhibitor with long administration intervals, and that the last intake of TNF inhibitors – particularly infliximab – should be at least more than one administration interval before planned surgery, as the risk of postoperative infection is significantly increased if surgery occurs within this period, she concluded.
Ms. Scherrer reported having no disclosures.
WASHINGTON – The risk of infection following orthopedic surgery is increased in patients with inflammatory rheumatic disease, compared with those with degenerative disease or traumatic injury, according to findings from a review of more than 50,000 surgical procedures.
The risk is greatest in those inflammatory rheumatic disease patients treated with conventional disease-modifying anti-rheumatic drugs (cDMARDs) or tumor necrosis factor (TNF) inhibitors, especially those receiving more than one cDMARD or TNF inhibitor with a long administration interval, and when surgery takes place without discontinuation of treatment, Catrina B. Scherrer reported at the annual meeting of the American College of Rheumatology.
Of 50,359 surgical procedures performed in 37,137 patients from a hospital surgery registry, 422 resulted in surgery-related infections. Of these infections, 49 occurred in 2,472 patients with an inflammatory rheumatic disease (IRD; 2%), and 373 occurred in 47,887 patients with degenerative disease/posttraumatic injury (0.8%). The difference was statistically significant, even after adjustment for other risk factors, including age, gender, diabetes, being overweight, cardiovascular disease, smoking, and type of surgery, said Ms. Scherrer of the Schulthess Clinic, Zürich.
The lowest rates of infection occurred with hand and shoulder surgery; the highest rates occurred with elbow surgery, she noted.
In 1,329 patients in the IRD group for whom complete information about medication was available, 171 (13%) had documented use of TNF inhibitors, and 49 of these (29%) discontinued treatment more than three administration intervals before surgery. Of the remaining 122 TNF inhibitor users, the time lag was three or fewer administration intervals.
An increased infection rate was seen in those who used more than one cDMARD (odds ratio, 2.425) and more than one TNF inhibitor (OR, 2.627) prior to surgery, and the risk of infection was increased tenfold when surgery was performed within one administration interval (OR, 10.047).
Patients who had their last treatment within one administration interval before surgery included 81% of infliximab users, compared with only 33% of adalimumab users and 24% of etanercept users, Ms. Scherrer noted.
Surgery patients in this study were followed over 8 years as part of a single-center surgery registry. The findings, which are limited by the study’s retrospective design and thus require confirmation in prospective studies, are nonetheless important because patients with aggressive disease such as IRDs frequently require orthopedic surgery.
The study findings suggest that IRD patients are, in general, at high risk of postoperative infection, that special attention should be paid to patients using more than one cDMARD or TNF inhibitor with long administration intervals, and that the last intake of TNF inhibitors – particularly infliximab – should be at least more than one administration interval before planned surgery, as the risk of postoperative infection is significantly increased if surgery occurs within this period, she concluded.
Ms. Scherrer reported having no disclosures.
AT THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF RHEUMATOLOGY
Major Finding: An increased infection rate was seen in patients who used more than one cDMARD (odds ratio, 2.425) and more than one TNF inhibitor (OR, 2.627) prior to surgery, and the risk of infection was increased 10-fold when surgery was performed within one treatment administration interval (OR, 10.047).
Data Source: A retrospective study of surgery cases.
Disclosures: Ms. Scherrer reported having no disclosures.
Ten-year data back shorter radiotherapy for breast cancer
SAN ANTONIO – A lower-dose, briefer radiotherapy regimen than is standard for early-stage breast cancer in the U.S. demonstrated comparable efficacy with fewer side effects at 10 years of follow-up in a pair of landmark U.K. studies.
"Long-term follow-up confirms that a lower total dose of radiation in fewer, slightly larger fractions delivered over a shorter treatment time is at least as safe and effective as standard 5-week schedules of curative radiotherapy in women with early breast cancer," Dr. John R. Yarnold declared in presenting the latest data from the U.K. START (Standardization of Breast Radiotherapy) trials at the annual San Antonio Breast Cancer Symposium.
The historical standard of care for radiotherapy in patients with surgically excised early breast cancer is 50 Gy delivered in 25 fractions of 2.0 Gy each over the course of 5 weeks. That’s still standard practice in the United States.
In the United Kingdom, however, the standard nationwide is 40 Gy in 15 fractions of 2.67 Gy over 3 weeks. Radiologists term this "hypofractionation": delivering a lower total dose of radiation using fewer but larger fractions. Hypofractionation has standard practice in the United Kingdom since the National Institute for Health and Clinical Excellence–issued guidelines to that effect in 2009. Those guidelines were based in large part on the earlier, highly favorable 5-year outcomes of START A (Lancet Oncology 2008;9:331-41) and START B (Lancet 2008;371:1098-107).
The START investigators deemed it essential to conduct the new 10-year analysis because adverse effects of radiotherapy given for breast cancer can arise after the 5-year mark. Also, it was important to learn whether the early antitumor effects of hypofractionated radiotherapy persisted, explained Dr. Yarnold, professor of clinical oncology at the Institute of Cancer Research, London.
The two key findings at the 10-year mark of START are, first, that both breast cancer and the dose-limiting normal tissues respond similarly to fraction size, so there’s no advantage in continuing the 2 Gy fractions that have historically been the international standard; and, second, that a 15-fraction/3-week schedule is gentler on normal tissues and comparable in antitumor efficacy to a 25-fraction/5-week regimen.
The clinical implications are clear, Dr. Yarnold emphasized: "Patients can safely be treated to a lower total dose with fewer fractions than the historical standard of 50 Gy and 25 fractions. There are no detrimental effects of hypofractionation noted in any of the subgroups studied."
The 10-year rate of moderate to marked adverse treatment effects on normal tissues in START A survivors who received 39 Gy in 13 fractions over 5 weeks was 43.9% compared with 50.4% in those randomized to 50 Gy in 25 fractions over 5 weeks. The resultant 20% relative risk reduction with a lower total radiation dose delivered in fewer fractions was statistically significant. In contrast, the 10-year locoregional tumor relapse rates in the two groups were similarly low.
At 10 years in START B, patients who received 40 Gy in 15 fractions over 3 weeks had a 37.9% rate of moderate-to-marked adverse effects on normal tissues, compared with a 45.3% rate in those who got 50 Gy in 25 fractions over 5 weeks, for a highly significant 23% risk reduction. The relapse rate was 4.3% after 40 Gy and 5.5% after 50 Gy, a nonsignificant difference.
In both trials, all types of side effects involving normal tissues were significantly less common in the lower-total-dose, fewer-fraction groups. That includes brachial plexus injury, which has been a concern expressed by supporters of the historical standard regimen, Dr. Yarnold added.
Radiologists and surgeons in the audience called the 10-year START results "very, very important" and likely to be practice changing.
Canada has already switched from the historical standard to 42.5 Gy delivered in 16 fractions over the course of 22 days. Asked if he thinks U.S. radiologists, too, should change their practice in light of the START findings, Dr. Yarnold was diplomatic. "I foresee no scientific reasons why they should not consider that very carefully," he replied.
Follow-up will continue in the START trials, which are funded by the Institute for Cancer Research, Cancer Research UK, the Medical Research Council, and the National Cancer Research Institute. Dr. Yarnold reported having no financial conflicts.
Institute of Cancer Research, London,
SAN ANTONIO – A lower-dose, briefer radiotherapy regimen than is standard for early-stage breast cancer in the U.S. demonstrated comparable efficacy with fewer side effects at 10 years of follow-up in a pair of landmark U.K. studies.
"Long-term follow-up confirms that a lower total dose of radiation in fewer, slightly larger fractions delivered over a shorter treatment time is at least as safe and effective as standard 5-week schedules of curative radiotherapy in women with early breast cancer," Dr. John R. Yarnold declared in presenting the latest data from the U.K. START (Standardization of Breast Radiotherapy) trials at the annual San Antonio Breast Cancer Symposium.
The historical standard of care for radiotherapy in patients with surgically excised early breast cancer is 50 Gy delivered in 25 fractions of 2.0 Gy each over the course of 5 weeks. That’s still standard practice in the United States.
In the United Kingdom, however, the standard nationwide is 40 Gy in 15 fractions of 2.67 Gy over 3 weeks. Radiologists term this "hypofractionation": delivering a lower total dose of radiation using fewer but larger fractions. Hypofractionation has standard practice in the United Kingdom since the National Institute for Health and Clinical Excellence–issued guidelines to that effect in 2009. Those guidelines were based in large part on the earlier, highly favorable 5-year outcomes of START A (Lancet Oncology 2008;9:331-41) and START B (Lancet 2008;371:1098-107).
The START investigators deemed it essential to conduct the new 10-year analysis because adverse effects of radiotherapy given for breast cancer can arise after the 5-year mark. Also, it was important to learn whether the early antitumor effects of hypofractionated radiotherapy persisted, explained Dr. Yarnold, professor of clinical oncology at the Institute of Cancer Research, London.
The two key findings at the 10-year mark of START are, first, that both breast cancer and the dose-limiting normal tissues respond similarly to fraction size, so there’s no advantage in continuing the 2 Gy fractions that have historically been the international standard; and, second, that a 15-fraction/3-week schedule is gentler on normal tissues and comparable in antitumor efficacy to a 25-fraction/5-week regimen.
The clinical implications are clear, Dr. Yarnold emphasized: "Patients can safely be treated to a lower total dose with fewer fractions than the historical standard of 50 Gy and 25 fractions. There are no detrimental effects of hypofractionation noted in any of the subgroups studied."
The 10-year rate of moderate to marked adverse treatment effects on normal tissues in START A survivors who received 39 Gy in 13 fractions over 5 weeks was 43.9% compared with 50.4% in those randomized to 50 Gy in 25 fractions over 5 weeks. The resultant 20% relative risk reduction with a lower total radiation dose delivered in fewer fractions was statistically significant. In contrast, the 10-year locoregional tumor relapse rates in the two groups were similarly low.
At 10 years in START B, patients who received 40 Gy in 15 fractions over 3 weeks had a 37.9% rate of moderate-to-marked adverse effects on normal tissues, compared with a 45.3% rate in those who got 50 Gy in 25 fractions over 5 weeks, for a highly significant 23% risk reduction. The relapse rate was 4.3% after 40 Gy and 5.5% after 50 Gy, a nonsignificant difference.
In both trials, all types of side effects involving normal tissues were significantly less common in the lower-total-dose, fewer-fraction groups. That includes brachial plexus injury, which has been a concern expressed by supporters of the historical standard regimen, Dr. Yarnold added.
Radiologists and surgeons in the audience called the 10-year START results "very, very important" and likely to be practice changing.
Canada has already switched from the historical standard to 42.5 Gy delivered in 16 fractions over the course of 22 days. Asked if he thinks U.S. radiologists, too, should change their practice in light of the START findings, Dr. Yarnold was diplomatic. "I foresee no scientific reasons why they should not consider that very carefully," he replied.
Follow-up will continue in the START trials, which are funded by the Institute for Cancer Research, Cancer Research UK, the Medical Research Council, and the National Cancer Research Institute. Dr. Yarnold reported having no financial conflicts.
SAN ANTONIO – A lower-dose, briefer radiotherapy regimen than is standard for early-stage breast cancer in the U.S. demonstrated comparable efficacy with fewer side effects at 10 years of follow-up in a pair of landmark U.K. studies.
"Long-term follow-up confirms that a lower total dose of radiation in fewer, slightly larger fractions delivered over a shorter treatment time is at least as safe and effective as standard 5-week schedules of curative radiotherapy in women with early breast cancer," Dr. John R. Yarnold declared in presenting the latest data from the U.K. START (Standardization of Breast Radiotherapy) trials at the annual San Antonio Breast Cancer Symposium.
The historical standard of care for radiotherapy in patients with surgically excised early breast cancer is 50 Gy delivered in 25 fractions of 2.0 Gy each over the course of 5 weeks. That’s still standard practice in the United States.
In the United Kingdom, however, the standard nationwide is 40 Gy in 15 fractions of 2.67 Gy over 3 weeks. Radiologists term this "hypofractionation": delivering a lower total dose of radiation using fewer but larger fractions. Hypofractionation has standard practice in the United Kingdom since the National Institute for Health and Clinical Excellence–issued guidelines to that effect in 2009. Those guidelines were based in large part on the earlier, highly favorable 5-year outcomes of START A (Lancet Oncology 2008;9:331-41) and START B (Lancet 2008;371:1098-107).
The START investigators deemed it essential to conduct the new 10-year analysis because adverse effects of radiotherapy given for breast cancer can arise after the 5-year mark. Also, it was important to learn whether the early antitumor effects of hypofractionated radiotherapy persisted, explained Dr. Yarnold, professor of clinical oncology at the Institute of Cancer Research, London.
The two key findings at the 10-year mark of START are, first, that both breast cancer and the dose-limiting normal tissues respond similarly to fraction size, so there’s no advantage in continuing the 2 Gy fractions that have historically been the international standard; and, second, that a 15-fraction/3-week schedule is gentler on normal tissues and comparable in antitumor efficacy to a 25-fraction/5-week regimen.
The clinical implications are clear, Dr. Yarnold emphasized: "Patients can safely be treated to a lower total dose with fewer fractions than the historical standard of 50 Gy and 25 fractions. There are no detrimental effects of hypofractionation noted in any of the subgroups studied."
The 10-year rate of moderate to marked adverse treatment effects on normal tissues in START A survivors who received 39 Gy in 13 fractions over 5 weeks was 43.9% compared with 50.4% in those randomized to 50 Gy in 25 fractions over 5 weeks. The resultant 20% relative risk reduction with a lower total radiation dose delivered in fewer fractions was statistically significant. In contrast, the 10-year locoregional tumor relapse rates in the two groups were similarly low.
At 10 years in START B, patients who received 40 Gy in 15 fractions over 3 weeks had a 37.9% rate of moderate-to-marked adverse effects on normal tissues, compared with a 45.3% rate in those who got 50 Gy in 25 fractions over 5 weeks, for a highly significant 23% risk reduction. The relapse rate was 4.3% after 40 Gy and 5.5% after 50 Gy, a nonsignificant difference.
In both trials, all types of side effects involving normal tissues were significantly less common in the lower-total-dose, fewer-fraction groups. That includes brachial plexus injury, which has been a concern expressed by supporters of the historical standard regimen, Dr. Yarnold added.
Radiologists and surgeons in the audience called the 10-year START results "very, very important" and likely to be practice changing.
Canada has already switched from the historical standard to 42.5 Gy delivered in 16 fractions over the course of 22 days. Asked if he thinks U.S. radiologists, too, should change their practice in light of the START findings, Dr. Yarnold was diplomatic. "I foresee no scientific reasons why they should not consider that very carefully," he replied.
Follow-up will continue in the START trials, which are funded by the Institute for Cancer Research, Cancer Research UK, the Medical Research Council, and the National Cancer Research Institute. Dr. Yarnold reported having no financial conflicts.
Institute of Cancer Research, London,
Institute of Cancer Research, London,
AT THE ANNUAL SAN ANTONIO BREAST CANCER SYMPOSIUM
Major Finding: The relapse rate at 10 years was 4.3% after the shorter 40 Gy regimen and 5.5% after the longer 50 Gy regimen, a nonsignificant difference in the START B trial.
Data Source: The U.K. START A and B trials are randomized, multicenter studies involving 4,451.
Disclosures: The START trials are funded by the Institute for Cancer Research, Cancer Research UK, the Medical Research Council, and the National Cancer Research Institute. The presenter reported having no financial conflicts.
ACA rollout gets bumpy: The Policy & Practice Podcast
As the end of the year grows closer, Congress—and doctors—are scrambling to prevent a series of actions that will hit pocketbooks hard. Without congressional action, physicians face a 27% pay cut mandated by the Sustainable Growth Rate formula, and an additional 2% reduction from sequestration--automatic budget cuts aimed at curbing the deficit.
Thus, large numbers of physicians went door-to-door in Congress last week, seeking to get their message out: The cuts must be stopped.
Meanwhile, another Affordable Care Act deadline has passed—states had until December 14 to say whether they would run an exchange on their own. Several states publicly said last week they would not go it alone—Tennessee, New Jersey and Pennsylvania--while Idaho’s governor said that his state would operate its exchange. As of Friday’s deadline, 18 states and the District of Columbia said they’d run their own exchange, and seven states said they’d partner with the feds. The remaining 25 are leaving it to the feds to operate the exchange in their state. States have until February to elect for a federal partnership.
Some state officials testified at a House subcommittee hearing that the federal government had not given them enough information on exchanges to make a good decision—and that’s why they were opting to let HHS run the exchanges for them.
For more on this and the Administration’s latest pronouncement on Medicaid expansion under the ACA, please take a listen.
---Alicia Ault (@aliciaault)
As the end of the year grows closer, Congress—and doctors—are scrambling to prevent a series of actions that will hit pocketbooks hard. Without congressional action, physicians face a 27% pay cut mandated by the Sustainable Growth Rate formula, and an additional 2% reduction from sequestration--automatic budget cuts aimed at curbing the deficit.
Thus, large numbers of physicians went door-to-door in Congress last week, seeking to get their message out: The cuts must be stopped.
Meanwhile, another Affordable Care Act deadline has passed—states had until December 14 to say whether they would run an exchange on their own. Several states publicly said last week they would not go it alone—Tennessee, New Jersey and Pennsylvania--while Idaho’s governor said that his state would operate its exchange. As of Friday’s deadline, 18 states and the District of Columbia said they’d run their own exchange, and seven states said they’d partner with the feds. The remaining 25 are leaving it to the feds to operate the exchange in their state. States have until February to elect for a federal partnership.
Some state officials testified at a House subcommittee hearing that the federal government had not given them enough information on exchanges to make a good decision—and that’s why they were opting to let HHS run the exchanges for them.
For more on this and the Administration’s latest pronouncement on Medicaid expansion under the ACA, please take a listen.
---Alicia Ault (@aliciaault)
As the end of the year grows closer, Congress—and doctors—are scrambling to prevent a series of actions that will hit pocketbooks hard. Without congressional action, physicians face a 27% pay cut mandated by the Sustainable Growth Rate formula, and an additional 2% reduction from sequestration--automatic budget cuts aimed at curbing the deficit.
Thus, large numbers of physicians went door-to-door in Congress last week, seeking to get their message out: The cuts must be stopped.
Meanwhile, another Affordable Care Act deadline has passed—states had until December 14 to say whether they would run an exchange on their own. Several states publicly said last week they would not go it alone—Tennessee, New Jersey and Pennsylvania--while Idaho’s governor said that his state would operate its exchange. As of Friday’s deadline, 18 states and the District of Columbia said they’d run their own exchange, and seven states said they’d partner with the feds. The remaining 25 are leaving it to the feds to operate the exchange in their state. States have until February to elect for a federal partnership.
Some state officials testified at a House subcommittee hearing that the federal government had not given them enough information on exchanges to make a good decision—and that’s why they were opting to let HHS run the exchanges for them.
For more on this and the Administration’s latest pronouncement on Medicaid expansion under the ACA, please take a listen.
---Alicia Ault (@aliciaault)