User login
The American Journal of Orthopedics is an Index Medicus publication that is valued by orthopedic surgeons for its peer-reviewed, practice-oriented clinical information. Most articles are written by specialists at leading teaching institutions and help incorporate the latest technology into everyday practice.
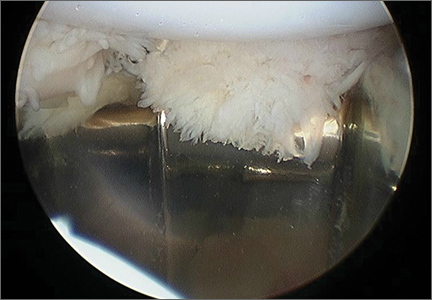
Patellofemoral Crepitation and Clunk Complicating Posterior-Stabilized Total Knee Arthroplasty
Biodegradable Surgical Pin Could Also Promote Bone Growth
Michele Manuel, PhD, Associate Professor of Materials Science and Engineering at the University of Florida in Gainesville, has developed a surgical pin made from magnesium and is working to control the rate at which the pin biodegrades in the body. In laboratory tests, the pin offered several advantages over traditional titanium, plastic, or stainless steel pins.
“The idea with this pin is that it would dissolve over time, and after it’s finished, your body is basically in the same state it was before you had an injury,” stated Dr. Manuel. “Surgical pins don’t have to become permanent fixtures in the body.”
In addition to being biodegradable, the pin also aids in the healing process. Magnesium builds bone, so it can function as a pin and as a nutrient. According to Dr. Manuel, the trick to using magnesium is controlling the rate at which it breaks down to give the body time to absorb the hydrogen that is release as a byproduct of breakdown. Along with controlling the rate at which the magnesium breaks down, Dr. Manuel is seeking to determine how much torque can be applied before the screw is stripped.
In laboratory tests, the magnesium pin has been inserted into the tibia of rats. X-rays show the rate at which the magnesium pins dissolve. At 6 weeks the new bone is indistinguishable from the bone before the break.
“People who have sensitivity to metal or inflammation from a foreign material in the body could benefit from this,” stated Dr. Manuel. “There are a lot of different applications that could be possible.”
Michele Manuel, PhD, Associate Professor of Materials Science and Engineering at the University of Florida in Gainesville, has developed a surgical pin made from magnesium and is working to control the rate at which the pin biodegrades in the body. In laboratory tests, the pin offered several advantages over traditional titanium, plastic, or stainless steel pins.
“The idea with this pin is that it would dissolve over time, and after it’s finished, your body is basically in the same state it was before you had an injury,” stated Dr. Manuel. “Surgical pins don’t have to become permanent fixtures in the body.”
In addition to being biodegradable, the pin also aids in the healing process. Magnesium builds bone, so it can function as a pin and as a nutrient. According to Dr. Manuel, the trick to using magnesium is controlling the rate at which it breaks down to give the body time to absorb the hydrogen that is release as a byproduct of breakdown. Along with controlling the rate at which the magnesium breaks down, Dr. Manuel is seeking to determine how much torque can be applied before the screw is stripped.
In laboratory tests, the magnesium pin has been inserted into the tibia of rats. X-rays show the rate at which the magnesium pins dissolve. At 6 weeks the new bone is indistinguishable from the bone before the break.
“People who have sensitivity to metal or inflammation from a foreign material in the body could benefit from this,” stated Dr. Manuel. “There are a lot of different applications that could be possible.”
Michele Manuel, PhD, Associate Professor of Materials Science and Engineering at the University of Florida in Gainesville, has developed a surgical pin made from magnesium and is working to control the rate at which the pin biodegrades in the body. In laboratory tests, the pin offered several advantages over traditional titanium, plastic, or stainless steel pins.
“The idea with this pin is that it would dissolve over time, and after it’s finished, your body is basically in the same state it was before you had an injury,” stated Dr. Manuel. “Surgical pins don’t have to become permanent fixtures in the body.”
In addition to being biodegradable, the pin also aids in the healing process. Magnesium builds bone, so it can function as a pin and as a nutrient. According to Dr. Manuel, the trick to using magnesium is controlling the rate at which it breaks down to give the body time to absorb the hydrogen that is release as a byproduct of breakdown. Along with controlling the rate at which the magnesium breaks down, Dr. Manuel is seeking to determine how much torque can be applied before the screw is stripped.
In laboratory tests, the magnesium pin has been inserted into the tibia of rats. X-rays show the rate at which the magnesium pins dissolve. At 6 weeks the new bone is indistinguishable from the bone before the break.
“People who have sensitivity to metal or inflammation from a foreign material in the body could benefit from this,” stated Dr. Manuel. “There are a lot of different applications that could be possible.”
Teen First North American to Undergo Incisionless Surgery for Bone Tumor
On July 17, Jack Campanile, age 16 years, a patient at the Hospital for Sick Children (SickKids) in Toronto, was the first teen to undergo a specialized procedure using magnetic resonance imaging (MRI) and ultrasound technology to destroy a tumor in his leg without piercing the skin. The lesion had caused the teen excruciating pain prior to electing to have this non-invasive procedure.
“With high-intensity focused ultrasound, we are moving from minimally invasive to non-invasive therapy, significantly reducing risk to the patient and fast-tracking recovery,” said interventional radiologist Michael Temple, MD, Associate Professor of Medical Imaging at the University of Toronto, who led the team that performed the surgery.
During the 30-minute procedure, the team used the MRI to pinpoint the exact location of the osteoid osteoma and to help target the ultrasound waves to burn the whole tumor. Using an MRI also afforded the team the opportunity to monitor the temperature induced by the ultrasound to ensure that there was no unexpected increase in heat in surrounding tissue.
Hours after undergoing this procedure Jack was discharged. He initially experienced a few hours of pain, and then he was totally pain-free. Overall, he recovered quickly and smoothly; there also have been no reported complications. That night he had uninterrupted sleep for the first time in months. Most of his normal activities also were resumed 2 days after surgery.
“The osteoid osteoma tumor was chosen as our pilot study because the lesion is easily accessible and while the procedure is sophisticated, it is relatively straightforward. The success of this first case is great news for Jack, and exciting for our team as we look at developing more complex incisionless treatments in the future,” said Dr. Temple.
On July 17, Jack Campanile, age 16 years, a patient at the Hospital for Sick Children (SickKids) in Toronto, was the first teen to undergo a specialized procedure using magnetic resonance imaging (MRI) and ultrasound technology to destroy a tumor in his leg without piercing the skin. The lesion had caused the teen excruciating pain prior to electing to have this non-invasive procedure.
“With high-intensity focused ultrasound, we are moving from minimally invasive to non-invasive therapy, significantly reducing risk to the patient and fast-tracking recovery,” said interventional radiologist Michael Temple, MD, Associate Professor of Medical Imaging at the University of Toronto, who led the team that performed the surgery.
During the 30-minute procedure, the team used the MRI to pinpoint the exact location of the osteoid osteoma and to help target the ultrasound waves to burn the whole tumor. Using an MRI also afforded the team the opportunity to monitor the temperature induced by the ultrasound to ensure that there was no unexpected increase in heat in surrounding tissue.
Hours after undergoing this procedure Jack was discharged. He initially experienced a few hours of pain, and then he was totally pain-free. Overall, he recovered quickly and smoothly; there also have been no reported complications. That night he had uninterrupted sleep for the first time in months. Most of his normal activities also were resumed 2 days after surgery.
“The osteoid osteoma tumor was chosen as our pilot study because the lesion is easily accessible and while the procedure is sophisticated, it is relatively straightforward. The success of this first case is great news for Jack, and exciting for our team as we look at developing more complex incisionless treatments in the future,” said Dr. Temple.
On July 17, Jack Campanile, age 16 years, a patient at the Hospital for Sick Children (SickKids) in Toronto, was the first teen to undergo a specialized procedure using magnetic resonance imaging (MRI) and ultrasound technology to destroy a tumor in his leg without piercing the skin. The lesion had caused the teen excruciating pain prior to electing to have this non-invasive procedure.
“With high-intensity focused ultrasound, we are moving from minimally invasive to non-invasive therapy, significantly reducing risk to the patient and fast-tracking recovery,” said interventional radiologist Michael Temple, MD, Associate Professor of Medical Imaging at the University of Toronto, who led the team that performed the surgery.
During the 30-minute procedure, the team used the MRI to pinpoint the exact location of the osteoid osteoma and to help target the ultrasound waves to burn the whole tumor. Using an MRI also afforded the team the opportunity to monitor the temperature induced by the ultrasound to ensure that there was no unexpected increase in heat in surrounding tissue.
Hours after undergoing this procedure Jack was discharged. He initially experienced a few hours of pain, and then he was totally pain-free. Overall, he recovered quickly and smoothly; there also have been no reported complications. That night he had uninterrupted sleep for the first time in months. Most of his normal activities also were resumed 2 days after surgery.
“The osteoid osteoma tumor was chosen as our pilot study because the lesion is easily accessible and while the procedure is sophisticated, it is relatively straightforward. The success of this first case is great news for Jack, and exciting for our team as we look at developing more complex incisionless treatments in the future,” said Dr. Temple.
Pro Baseball Pitchers’ Missed Days Attributed to Weak Core
Professional baseball pitchers with poor core stability are more likely to miss 30 or more days in a single season because of injury compared with pitchers who have good control of muscles in their pelvis and lower back, according to a study published August 26 online ahead of print in the American Journal of Sports Medicine.
The study shows association, not causation, but does suggest that pitchers might benefit from training to improve their lumbopelvic control. “The nice thing about lumbopelvic control is that there’s not any downside we can think of to trying to improve it,” said Ajit Chaudhari, PhD, Associate Professor of Health and Rehabilitation Sciences and of Orthopedics at The Ohio State University and lead author of the study.
A total of 347 pitchers were assessed for lumbopelvic control during spring training, then followed for the ensuing season. Most participants were between the ages of 18 and 22 years and played on teams at the developmental, minor league, or major league level.
Investigators tested their lumbopelvic control by assessing how much the pelvis tilted forward or backward as pitchers lifted a single foot about 10 cm in a movement similar to stepping up onto a curb or beginning a pitch. Study authors then placed an iPod-based tilt sensor on each participant’s sacrum and a score was assigned to each player based on the magnitude of the tilt.
Medical staff from each baseball organization recorded how many missed days players had throughout the season that followed spring training (a missed day was defined as any day a study participant could not complete his scheduled work because of an injury suffered during baseball-related activity). The majority of injuries recorded were elbow strains, shoulder strains, tears, and fractures. The subjects also were placed into 1 of 3 categories—those whose pelvises tilted less than 4 degrees, between 4 and 7.9 degrees, and more than 8 degrees from the starting position.
Players were categorized by the total numbers of days missed during the season (fewer than 30 days or 30 or more days). The analysis showed that the chances of missing 30 or more days in the season were 3 times higher for the high-tilt group than for pitchers in the lowest-tilt group. It was also 2.2 times higher than for players in the moderate-tilt group.
Further analysis suggested that of the 108 (31.1%) participants who missed at least 1 day because of injury, the average number of days missed was significantly different among the 3 groups. On average, those with poor lumbopelvic control missed 99 days, those with moderate control missed 46 days, and the well-controlled group missed 44 days.
“The core could help prevent injury by spreading out the energy load, allowing pitchers to use their legs more and their throwing arm less,” Dr. Chaudhari said.
Suggested Reading
Chaudhari AM, McKenzie CS, Pan X, Oñate JA. Lumbopelvic control and days missed because of injury in professional baseball pitchers. Am J Sports Med. 2014 Aug 26. pii: 0363546514545861. [Epub ahead of print]
Professional baseball pitchers with poor core stability are more likely to miss 30 or more days in a single season because of injury compared with pitchers who have good control of muscles in their pelvis and lower back, according to a study published August 26 online ahead of print in the American Journal of Sports Medicine.
The study shows association, not causation, but does suggest that pitchers might benefit from training to improve their lumbopelvic control. “The nice thing about lumbopelvic control is that there’s not any downside we can think of to trying to improve it,” said Ajit Chaudhari, PhD, Associate Professor of Health and Rehabilitation Sciences and of Orthopedics at The Ohio State University and lead author of the study.
A total of 347 pitchers were assessed for lumbopelvic control during spring training, then followed for the ensuing season. Most participants were between the ages of 18 and 22 years and played on teams at the developmental, minor league, or major league level.
Investigators tested their lumbopelvic control by assessing how much the pelvis tilted forward or backward as pitchers lifted a single foot about 10 cm in a movement similar to stepping up onto a curb or beginning a pitch. Study authors then placed an iPod-based tilt sensor on each participant’s sacrum and a score was assigned to each player based on the magnitude of the tilt.
Medical staff from each baseball organization recorded how many missed days players had throughout the season that followed spring training (a missed day was defined as any day a study participant could not complete his scheduled work because of an injury suffered during baseball-related activity). The majority of injuries recorded were elbow strains, shoulder strains, tears, and fractures. The subjects also were placed into 1 of 3 categories—those whose pelvises tilted less than 4 degrees, between 4 and 7.9 degrees, and more than 8 degrees from the starting position.
Players were categorized by the total numbers of days missed during the season (fewer than 30 days or 30 or more days). The analysis showed that the chances of missing 30 or more days in the season were 3 times higher for the high-tilt group than for pitchers in the lowest-tilt group. It was also 2.2 times higher than for players in the moderate-tilt group.
Further analysis suggested that of the 108 (31.1%) participants who missed at least 1 day because of injury, the average number of days missed was significantly different among the 3 groups. On average, those with poor lumbopelvic control missed 99 days, those with moderate control missed 46 days, and the well-controlled group missed 44 days.
“The core could help prevent injury by spreading out the energy load, allowing pitchers to use their legs more and their throwing arm less,” Dr. Chaudhari said.
Professional baseball pitchers with poor core stability are more likely to miss 30 or more days in a single season because of injury compared with pitchers who have good control of muscles in their pelvis and lower back, according to a study published August 26 online ahead of print in the American Journal of Sports Medicine.
The study shows association, not causation, but does suggest that pitchers might benefit from training to improve their lumbopelvic control. “The nice thing about lumbopelvic control is that there’s not any downside we can think of to trying to improve it,” said Ajit Chaudhari, PhD, Associate Professor of Health and Rehabilitation Sciences and of Orthopedics at The Ohio State University and lead author of the study.
A total of 347 pitchers were assessed for lumbopelvic control during spring training, then followed for the ensuing season. Most participants were between the ages of 18 and 22 years and played on teams at the developmental, minor league, or major league level.
Investigators tested their lumbopelvic control by assessing how much the pelvis tilted forward or backward as pitchers lifted a single foot about 10 cm in a movement similar to stepping up onto a curb or beginning a pitch. Study authors then placed an iPod-based tilt sensor on each participant’s sacrum and a score was assigned to each player based on the magnitude of the tilt.
Medical staff from each baseball organization recorded how many missed days players had throughout the season that followed spring training (a missed day was defined as any day a study participant could not complete his scheduled work because of an injury suffered during baseball-related activity). The majority of injuries recorded were elbow strains, shoulder strains, tears, and fractures. The subjects also were placed into 1 of 3 categories—those whose pelvises tilted less than 4 degrees, between 4 and 7.9 degrees, and more than 8 degrees from the starting position.
Players were categorized by the total numbers of days missed during the season (fewer than 30 days or 30 or more days). The analysis showed that the chances of missing 30 or more days in the season were 3 times higher for the high-tilt group than for pitchers in the lowest-tilt group. It was also 2.2 times higher than for players in the moderate-tilt group.
Further analysis suggested that of the 108 (31.1%) participants who missed at least 1 day because of injury, the average number of days missed was significantly different among the 3 groups. On average, those with poor lumbopelvic control missed 99 days, those with moderate control missed 46 days, and the well-controlled group missed 44 days.
“The core could help prevent injury by spreading out the energy load, allowing pitchers to use their legs more and their throwing arm less,” Dr. Chaudhari said.
Suggested Reading
Chaudhari AM, McKenzie CS, Pan X, Oñate JA. Lumbopelvic control and days missed because of injury in professional baseball pitchers. Am J Sports Med. 2014 Aug 26. pii: 0363546514545861. [Epub ahead of print]
Suggested Reading
Chaudhari AM, McKenzie CS, Pan X, Oñate JA. Lumbopelvic control and days missed because of injury in professional baseball pitchers. Am J Sports Med. 2014 Aug 26. pii: 0363546514545861. [Epub ahead of print]
Advanced Technology Reveals Tiny Strains in Body Tissue Pre-Injury
Researchers have developed algorithms to pinpoint weak spots in the tendons, bones, and muscles that are prone to breaking or tearing, according to a study published online August 27 in the Journal of the Royal Society Interface.
“Tendons are constantly stretching as muscles pull on them, and bones also bend or compress as we carry out everyday activities,” said senior investigator Stavros Thomopoulos, PhD, Professor of Orthopaedic Surgery at Washington University in St. Louis. “Small cracks or tears can result from these loads and lead to major injuries. Understanding how these tears and cracks develop over time therefore is important for diagnosing and tracking injuries.”
The investigators developed a way to visualize and predict spots where tissues are weakened. This was accomplished by stretching tissues and tracking the results as their shapes changed. Algorithms were then developed that can identify areas of weakening prior to breakage. The algorithm was tested in various materials and in animal models. “The new algorithm allowed us to find the places where the tears were beginning to form and to track them as they extended. Older algorithms are not as good at finding and tracking localized strains,” the researchers reported.
One of the two algorithms is 1,000 times more accurate than older methods at quantifying very large stretches near tiny cracks and tears. A second algorithm has the ability to predict where cracks and failures are likely to form.
Overall, the researchers aim to use these algorithms to prevent additional injuries following surgery to repair shoulders, knees, and other tissue. “It’s vital to understand the ways that physical forces cause structures and tissues to deform so that we can identify the onset of failures and eventually predict them.”
Suggested Reading
Boyle JJ, Kume M, Wyczalkowski MA, et al. Simple and accurate methods for quantifying deformation, disruption, and development in biological tissues. J R Soc Interface. 2014 Nov 6;11(100). pii: 20140685. doi: 10.1098/rsif.2014.0685.
Researchers have developed algorithms to pinpoint weak spots in the tendons, bones, and muscles that are prone to breaking or tearing, according to a study published online August 27 in the Journal of the Royal Society Interface.
“Tendons are constantly stretching as muscles pull on them, and bones also bend or compress as we carry out everyday activities,” said senior investigator Stavros Thomopoulos, PhD, Professor of Orthopaedic Surgery at Washington University in St. Louis. “Small cracks or tears can result from these loads and lead to major injuries. Understanding how these tears and cracks develop over time therefore is important for diagnosing and tracking injuries.”
The investigators developed a way to visualize and predict spots where tissues are weakened. This was accomplished by stretching tissues and tracking the results as their shapes changed. Algorithms were then developed that can identify areas of weakening prior to breakage. The algorithm was tested in various materials and in animal models. “The new algorithm allowed us to find the places where the tears were beginning to form and to track them as they extended. Older algorithms are not as good at finding and tracking localized strains,” the researchers reported.
One of the two algorithms is 1,000 times more accurate than older methods at quantifying very large stretches near tiny cracks and tears. A second algorithm has the ability to predict where cracks and failures are likely to form.
Overall, the researchers aim to use these algorithms to prevent additional injuries following surgery to repair shoulders, knees, and other tissue. “It’s vital to understand the ways that physical forces cause structures and tissues to deform so that we can identify the onset of failures and eventually predict them.”
Researchers have developed algorithms to pinpoint weak spots in the tendons, bones, and muscles that are prone to breaking or tearing, according to a study published online August 27 in the Journal of the Royal Society Interface.
“Tendons are constantly stretching as muscles pull on them, and bones also bend or compress as we carry out everyday activities,” said senior investigator Stavros Thomopoulos, PhD, Professor of Orthopaedic Surgery at Washington University in St. Louis. “Small cracks or tears can result from these loads and lead to major injuries. Understanding how these tears and cracks develop over time therefore is important for diagnosing and tracking injuries.”
The investigators developed a way to visualize and predict spots where tissues are weakened. This was accomplished by stretching tissues and tracking the results as their shapes changed. Algorithms were then developed that can identify areas of weakening prior to breakage. The algorithm was tested in various materials and in animal models. “The new algorithm allowed us to find the places where the tears were beginning to form and to track them as they extended. Older algorithms are not as good at finding and tracking localized strains,” the researchers reported.
One of the two algorithms is 1,000 times more accurate than older methods at quantifying very large stretches near tiny cracks and tears. A second algorithm has the ability to predict where cracks and failures are likely to form.
Overall, the researchers aim to use these algorithms to prevent additional injuries following surgery to repair shoulders, knees, and other tissue. “It’s vital to understand the ways that physical forces cause structures and tissues to deform so that we can identify the onset of failures and eventually predict them.”
Suggested Reading
Boyle JJ, Kume M, Wyczalkowski MA, et al. Simple and accurate methods for quantifying deformation, disruption, and development in biological tissues. J R Soc Interface. 2014 Nov 6;11(100). pii: 20140685. doi: 10.1098/rsif.2014.0685.
Suggested Reading
Boyle JJ, Kume M, Wyczalkowski MA, et al. Simple and accurate methods for quantifying deformation, disruption, and development in biological tissues. J R Soc Interface. 2014 Nov 6;11(100). pii: 20140685. doi: 10.1098/rsif.2014.0685.
Zorvolex® Approved by FDA for Treatment of Osteoarthritis Pain
Iroko Pharmaceuticals (Philadelphia, Pennsylvania) announced that the FDA has approved Zorvolex (diclofenac) capsules, a nonsteroidal anti-inflammatory drug (NSAID) for the management of mild to moderate acute pain and osteoarthritis pain. This marks the second indication for the drug, which was approved by the FDA in October 2013 for treatment of mild to moderate acute pain in adults.
Zorvolex was created to align with recommendations from the FDA and several medical organizations that NSAIDs be used at the lowest effective dose and for the shortest possible duration. This low-dose NSAID was developed using SoluMatrix Fine Particle Technology. Zorvolex contains diclofenac as submicron particles that are approximately 20 times smaller than their original size. The reduction in particle size provides an increased surface area, which leads to faster dissolution.
“NSAIDs continue to be an integral part of the management for osteoarthritis and their use is likely to increase as the US population continues to age and the incidence of osteoarthritis rises,” said Roy Altman, MD, Professor of Medicine in Rheumatology at UCLA.
The approval of Zorvolex is supported by data from a 12-week multicenter, randomized, double-blind, parallel-group, placebo-controlled study. The study included 305 patients aged 41 to 90 years with osteoarthrisis of the knee or hip. Half of the patients were between the ages of 61 and 90 years. They were randomized to 35 mg of Zorvolex three times a day, 35 mg twice daily, or placebo. The Supplemental New Drug Application also included data from a 12-month open-label safety study of 602 patients.
Zorvolex is available in 18 mg or 35 mg capsules. “The approval of Zorvolex is a welcome and meaningful advance and is the first SoluMatrix NSAID option approved by the FDA for osteoarthritis pain,” Dr. Altman stated.
Iroko Pharmaceuticals (Philadelphia, Pennsylvania) announced that the FDA has approved Zorvolex (diclofenac) capsules, a nonsteroidal anti-inflammatory drug (NSAID) for the management of mild to moderate acute pain and osteoarthritis pain. This marks the second indication for the drug, which was approved by the FDA in October 2013 for treatment of mild to moderate acute pain in adults.
Zorvolex was created to align with recommendations from the FDA and several medical organizations that NSAIDs be used at the lowest effective dose and for the shortest possible duration. This low-dose NSAID was developed using SoluMatrix Fine Particle Technology. Zorvolex contains diclofenac as submicron particles that are approximately 20 times smaller than their original size. The reduction in particle size provides an increased surface area, which leads to faster dissolution.
“NSAIDs continue to be an integral part of the management for osteoarthritis and their use is likely to increase as the US population continues to age and the incidence of osteoarthritis rises,” said Roy Altman, MD, Professor of Medicine in Rheumatology at UCLA.
The approval of Zorvolex is supported by data from a 12-week multicenter, randomized, double-blind, parallel-group, placebo-controlled study. The study included 305 patients aged 41 to 90 years with osteoarthrisis of the knee or hip. Half of the patients were between the ages of 61 and 90 years. They were randomized to 35 mg of Zorvolex three times a day, 35 mg twice daily, or placebo. The Supplemental New Drug Application also included data from a 12-month open-label safety study of 602 patients.
Zorvolex is available in 18 mg or 35 mg capsules. “The approval of Zorvolex is a welcome and meaningful advance and is the first SoluMatrix NSAID option approved by the FDA for osteoarthritis pain,” Dr. Altman stated.
Iroko Pharmaceuticals (Philadelphia, Pennsylvania) announced that the FDA has approved Zorvolex (diclofenac) capsules, a nonsteroidal anti-inflammatory drug (NSAID) for the management of mild to moderate acute pain and osteoarthritis pain. This marks the second indication for the drug, which was approved by the FDA in October 2013 for treatment of mild to moderate acute pain in adults.
Zorvolex was created to align with recommendations from the FDA and several medical organizations that NSAIDs be used at the lowest effective dose and for the shortest possible duration. This low-dose NSAID was developed using SoluMatrix Fine Particle Technology. Zorvolex contains diclofenac as submicron particles that are approximately 20 times smaller than their original size. The reduction in particle size provides an increased surface area, which leads to faster dissolution.
“NSAIDs continue to be an integral part of the management for osteoarthritis and their use is likely to increase as the US population continues to age and the incidence of osteoarthritis rises,” said Roy Altman, MD, Professor of Medicine in Rheumatology at UCLA.
The approval of Zorvolex is supported by data from a 12-week multicenter, randomized, double-blind, parallel-group, placebo-controlled study. The study included 305 patients aged 41 to 90 years with osteoarthrisis of the knee or hip. Half of the patients were between the ages of 61 and 90 years. They were randomized to 35 mg of Zorvolex three times a day, 35 mg twice daily, or placebo. The Supplemental New Drug Application also included data from a 12-month open-label safety study of 602 patients.
Zorvolex is available in 18 mg or 35 mg capsules. “The approval of Zorvolex is a welcome and meaningful advance and is the first SoluMatrix NSAID option approved by the FDA for osteoarthritis pain,” Dr. Altman stated.
Knee Surgery Not Necessary for Middle-Aged Patients with Mild Osteoarthritis
New meta-analysis evidence suggests that there is no benefit to having arthroscopic meniscal debridement for degenerative meniscal tears in comparison with nonoperative treatments or sham treatments in middle-aged patients with mild or no concomitant osteoarthritis. The findings were published August 25 online ahead of print in the Canadian Medical Association Journal.
“Doctors need to carefully weigh the costs and benefits when deciding who should undergo such surgery,” said Moin Khan, MD, lead author of the study and research fellow in orthopedic surgery in the Michael G. DeGroote School of Medicine at McMaster University in Hamilton, Ontario.
Dr. Khan and colleagues conducted a meta-analysis of 7 randomized controlled trials published between 1946 and January 20, 2014, on arthroscopic partial meniscectomy in patients with mild to no osteoarthritis compared with nonoperative treatments. Two reviewers independently screened all abstracts and titles for eligibility. In total, there were 811 knees in 805 patients with a mean age of 56 years. The pooled treatment effect of arthroscopic surgery did not show a significant or minimally important difference between treatment arms for long-term functional outcomes. Short-term functional outcomes between groups were significant but did not exceed the threshold for minimally important difference. Arthroscopic surgery did not result in a significant improvement in either short- or long-term pain scores.
“This study shows that surgery should not be the initial option for middle-age or older patients, as there is limited evidence supporting partial meniscectomy surgery for meniscus tears,” Dr. Khan said. “Other treatments should be used first.”
“Arthroscopic debridement or washout of knee osteoarthritis has come under lots of scrutiny based upon trials that suggest patients get no benefit from the procedure. We’re concerned that many surgeons worldwide may still be doing this procedure,” stated the researchers.
Suggested Reading
Khan M, Evaniew N, Bedi A, et al. Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. CMAJ. 2014 Aug 25. pii: cmaj.140433. [Epub ahead of print]
New meta-analysis evidence suggests that there is no benefit to having arthroscopic meniscal debridement for degenerative meniscal tears in comparison with nonoperative treatments or sham treatments in middle-aged patients with mild or no concomitant osteoarthritis. The findings were published August 25 online ahead of print in the Canadian Medical Association Journal.
“Doctors need to carefully weigh the costs and benefits when deciding who should undergo such surgery,” said Moin Khan, MD, lead author of the study and research fellow in orthopedic surgery in the Michael G. DeGroote School of Medicine at McMaster University in Hamilton, Ontario.
Dr. Khan and colleagues conducted a meta-analysis of 7 randomized controlled trials published between 1946 and January 20, 2014, on arthroscopic partial meniscectomy in patients with mild to no osteoarthritis compared with nonoperative treatments. Two reviewers independently screened all abstracts and titles for eligibility. In total, there were 811 knees in 805 patients with a mean age of 56 years. The pooled treatment effect of arthroscopic surgery did not show a significant or minimally important difference between treatment arms for long-term functional outcomes. Short-term functional outcomes between groups were significant but did not exceed the threshold for minimally important difference. Arthroscopic surgery did not result in a significant improvement in either short- or long-term pain scores.
“This study shows that surgery should not be the initial option for middle-age or older patients, as there is limited evidence supporting partial meniscectomy surgery for meniscus tears,” Dr. Khan said. “Other treatments should be used first.”
“Arthroscopic debridement or washout of knee osteoarthritis has come under lots of scrutiny based upon trials that suggest patients get no benefit from the procedure. We’re concerned that many surgeons worldwide may still be doing this procedure,” stated the researchers.
New meta-analysis evidence suggests that there is no benefit to having arthroscopic meniscal debridement for degenerative meniscal tears in comparison with nonoperative treatments or sham treatments in middle-aged patients with mild or no concomitant osteoarthritis. The findings were published August 25 online ahead of print in the Canadian Medical Association Journal.
“Doctors need to carefully weigh the costs and benefits when deciding who should undergo such surgery,” said Moin Khan, MD, lead author of the study and research fellow in orthopedic surgery in the Michael G. DeGroote School of Medicine at McMaster University in Hamilton, Ontario.
Dr. Khan and colleagues conducted a meta-analysis of 7 randomized controlled trials published between 1946 and January 20, 2014, on arthroscopic partial meniscectomy in patients with mild to no osteoarthritis compared with nonoperative treatments. Two reviewers independently screened all abstracts and titles for eligibility. In total, there were 811 knees in 805 patients with a mean age of 56 years. The pooled treatment effect of arthroscopic surgery did not show a significant or minimally important difference between treatment arms for long-term functional outcomes. Short-term functional outcomes between groups were significant but did not exceed the threshold for minimally important difference. Arthroscopic surgery did not result in a significant improvement in either short- or long-term pain scores.
“This study shows that surgery should not be the initial option for middle-age or older patients, as there is limited evidence supporting partial meniscectomy surgery for meniscus tears,” Dr. Khan said. “Other treatments should be used first.”
“Arthroscopic debridement or washout of knee osteoarthritis has come under lots of scrutiny based upon trials that suggest patients get no benefit from the procedure. We’re concerned that many surgeons worldwide may still be doing this procedure,” stated the researchers.
Suggested Reading
Khan M, Evaniew N, Bedi A, et al. Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. CMAJ. 2014 Aug 25. pii: cmaj.140433. [Epub ahead of print]
Suggested Reading
Khan M, Evaniew N, Bedi A, et al. Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. CMAJ. 2014 Aug 25. pii: cmaj.140433. [Epub ahead of print]
Osteoporosis Drugs’ Ability to Protect Women from Breast Cancer Challenged
Recent observational studies have suggested that bisphosphonates may protect women from breast cancer, but this theory has not been tested in randomized trials—until now. Researchers assessed the effects of the 2 most widely used osteoporosis drugs—alendronate (Fosamax) and zoledronic acid (Reclast)—and determined that neither drug protected women with osteoporosis from developing breast cancer. Study findings were published August 11 online ahead of print in JAMA Internal Medicine.
“They may have seen a lower risk of breast cancer in women using bisphosphonates in the earlier observational studies because those women had a lower risk of breast cancer to begin with,” said lead author Trisha Hue, PhD, an epidemiologist with the San Francisco Coordinating Center, Department of Epidemiology and Biostatistics, at the University of California, San Francisco. Dr. Hue and her coinvestigators believe that the link found in the previous observational studies between taking the drugs and having a lower incidence of breast cancer may be due to low estrogen levels in the women studied.
Data analyzed in this study came from 2 large randomized, double-blind, placebo-controlled clinical trials—The Fracture Intervention Trial (FIT) and the Health Outcomes and Reduced Incidence With Zoledronic Acid Once Yearly Pivotal Fracture Trial (HORIZON-PFT). In both trials, women who received bisphosphonates had a slightly higher but statistically nonsignificant incidence of breast cancer.
FIT randomly assigned 6,459 women aged 55 to 81 years from the United States to alendronate or placebo for an average follow-up of 3.8 years. No significant difference in the rate of breast cancers was seen: Fifty-seven women (1.8%) who received the drug developed breast cancer, while 46 (1.5%) of those given placebo developed the disease.
HORIZON-PFT randomly assigned 7,765 women aged 65 to 89 years from the United States, Canada, Asia, Europe, and South America to annual intravenous zoledronic acid or placebo for an average follow up of 2.8 years. Results showed that 33 women (0.9%) who received the drug developed breast cancer and 29 (0.8%) women given placebo developed the disease.
Women in either study who reported a history of breast cancer or who had recurrent breast cancer were excluded from the analyses.
“These two randomized clinical trials do not support the findings from observational research,” Dr. Hue and colleagues reported. “Contrary to the results from observational studies, we found that 3 to 4 years of bisphosphonate treatment did not decrease the risk of invasive postmenopausal breast cancer.”
Suggested Reading
Hue TF, Cummings SR, Cauley JA, et al. Effect of bisphosphonate use on risk of postmenopausal breast cancer: Results from the randomized clinical trials of alendronate and zoledronic acid. JAMA Intern Med. 2014 Aug 11. doi: 10.1001/jamainternmed.2014.3634. [Epub ahead of print]
Recent observational studies have suggested that bisphosphonates may protect women from breast cancer, but this theory has not been tested in randomized trials—until now. Researchers assessed the effects of the 2 most widely used osteoporosis drugs—alendronate (Fosamax) and zoledronic acid (Reclast)—and determined that neither drug protected women with osteoporosis from developing breast cancer. Study findings were published August 11 online ahead of print in JAMA Internal Medicine.
“They may have seen a lower risk of breast cancer in women using bisphosphonates in the earlier observational studies because those women had a lower risk of breast cancer to begin with,” said lead author Trisha Hue, PhD, an epidemiologist with the San Francisco Coordinating Center, Department of Epidemiology and Biostatistics, at the University of California, San Francisco. Dr. Hue and her coinvestigators believe that the link found in the previous observational studies between taking the drugs and having a lower incidence of breast cancer may be due to low estrogen levels in the women studied.
Data analyzed in this study came from 2 large randomized, double-blind, placebo-controlled clinical trials—The Fracture Intervention Trial (FIT) and the Health Outcomes and Reduced Incidence With Zoledronic Acid Once Yearly Pivotal Fracture Trial (HORIZON-PFT). In both trials, women who received bisphosphonates had a slightly higher but statistically nonsignificant incidence of breast cancer.
FIT randomly assigned 6,459 women aged 55 to 81 years from the United States to alendronate or placebo for an average follow-up of 3.8 years. No significant difference in the rate of breast cancers was seen: Fifty-seven women (1.8%) who received the drug developed breast cancer, while 46 (1.5%) of those given placebo developed the disease.
HORIZON-PFT randomly assigned 7,765 women aged 65 to 89 years from the United States, Canada, Asia, Europe, and South America to annual intravenous zoledronic acid or placebo for an average follow up of 2.8 years. Results showed that 33 women (0.9%) who received the drug developed breast cancer and 29 (0.8%) women given placebo developed the disease.
Women in either study who reported a history of breast cancer or who had recurrent breast cancer were excluded from the analyses.
“These two randomized clinical trials do not support the findings from observational research,” Dr. Hue and colleagues reported. “Contrary to the results from observational studies, we found that 3 to 4 years of bisphosphonate treatment did not decrease the risk of invasive postmenopausal breast cancer.”
Recent observational studies have suggested that bisphosphonates may protect women from breast cancer, but this theory has not been tested in randomized trials—until now. Researchers assessed the effects of the 2 most widely used osteoporosis drugs—alendronate (Fosamax) and zoledronic acid (Reclast)—and determined that neither drug protected women with osteoporosis from developing breast cancer. Study findings were published August 11 online ahead of print in JAMA Internal Medicine.
“They may have seen a lower risk of breast cancer in women using bisphosphonates in the earlier observational studies because those women had a lower risk of breast cancer to begin with,” said lead author Trisha Hue, PhD, an epidemiologist with the San Francisco Coordinating Center, Department of Epidemiology and Biostatistics, at the University of California, San Francisco. Dr. Hue and her coinvestigators believe that the link found in the previous observational studies between taking the drugs and having a lower incidence of breast cancer may be due to low estrogen levels in the women studied.
Data analyzed in this study came from 2 large randomized, double-blind, placebo-controlled clinical trials—The Fracture Intervention Trial (FIT) and the Health Outcomes and Reduced Incidence With Zoledronic Acid Once Yearly Pivotal Fracture Trial (HORIZON-PFT). In both trials, women who received bisphosphonates had a slightly higher but statistically nonsignificant incidence of breast cancer.
FIT randomly assigned 6,459 women aged 55 to 81 years from the United States to alendronate or placebo for an average follow-up of 3.8 years. No significant difference in the rate of breast cancers was seen: Fifty-seven women (1.8%) who received the drug developed breast cancer, while 46 (1.5%) of those given placebo developed the disease.
HORIZON-PFT randomly assigned 7,765 women aged 65 to 89 years from the United States, Canada, Asia, Europe, and South America to annual intravenous zoledronic acid or placebo for an average follow up of 2.8 years. Results showed that 33 women (0.9%) who received the drug developed breast cancer and 29 (0.8%) women given placebo developed the disease.
Women in either study who reported a history of breast cancer or who had recurrent breast cancer were excluded from the analyses.
“These two randomized clinical trials do not support the findings from observational research,” Dr. Hue and colleagues reported. “Contrary to the results from observational studies, we found that 3 to 4 years of bisphosphonate treatment did not decrease the risk of invasive postmenopausal breast cancer.”
Suggested Reading
Hue TF, Cummings SR, Cauley JA, et al. Effect of bisphosphonate use on risk of postmenopausal breast cancer: Results from the randomized clinical trials of alendronate and zoledronic acid. JAMA Intern Med. 2014 Aug 11. doi: 10.1001/jamainternmed.2014.3634. [Epub ahead of print]
Suggested Reading
Hue TF, Cummings SR, Cauley JA, et al. Effect of bisphosphonate use on risk of postmenopausal breast cancer: Results from the randomized clinical trials of alendronate and zoledronic acid. JAMA Intern Med. 2014 Aug 11. doi: 10.1001/jamainternmed.2014.3634. [Epub ahead of print]