User login
Research coalition issues plan for curing hepatitis B virus
VIENNA – They hope either to have a cure or to have made substantial progress toward this goal over the next 10 years.
Treatments already are on the market that effectively inhibit hepatitis B replication in infected patients (and an effective preventive vaccine also exists). Still, these treatments are not curative, and for the vast majority of patients treatment must continue indefinitely, while their risk for liver cancer and their virally induced immune system abnormalities remain, Peter A. Revill, PhD, said during a press briefing that introduced a strategy for hepatitis B virus (HBV) cure development from the International Coalition to Eliminate HBV. Concurrently with the briefing session, the strategy appeared in an article published online (Lancet Gastroenterol Hepatol. 2019 Apr 10. doi: 10.1016/s2468-1253(19)30119-0).
The way forward will likely be a “two-pronged approach or restoring immune responses and targeting the virus,” Dr. Revill, head of molecular virology at the Doherty Institute in Melbourne, said in a video interview.
The new strategy recognizes the huge challenge of devising a treatment that produces a total cure that includes elimination of all traces of viral DNA from patients and for the immediate future focuses on the goal of functional cure. The term functional cure means a sustained period without detectable HBV surface antigen or HBV DNA in a patient’s serum, as well as suppressed virus release. Another feature of a functional cure would be a halt to progression of liver disease, replaced by liver regeneration, said Anna S. Lok, MD, professor of medicine and director of clinical hepatology at the University of Michigan, Ann Arbor, and a member of the strategy-writing group. She and her colleagues who wrote the strategy foresee the need for drug combinations with agents that can hit multiple viral targets as well as agents that restore normal immune function.
Several novel drug classes aimed at new viral targets, such as capsid inhibitors, are in various stages of clinical development, said Fabien Zoulim, MD, head of the gastroenterology and hepatology service at the Red Cross Hospital in Lyon, France, and another member of the writing panel. “We have many drug candidates” that use novel approaches to further restrict viral growth, roughly 50 agents in phase 1 and 2 studies, he said during the press briefing, held during the meeting sponsored by the European Association for the Study of the Liver. The other, immunologic aspect of the two-part cure strategy – restoring the “exhausted” HBV-specific T-cell population and stimulating production of neutralizing antibody to HBV – remains hypothetical right now, however. “It’s a concept that needs development,” Dr. Zoulim said.
A reason members of the coalition are optimistic about eventual prospects for a cure is that currently about 1% of patients on HBV antiviral treatments have a functional cure after relatively brief treatment, and the percentage of cured patients plateaus at about 10% among those who remain on current HBV antiviral drugs for several years. In addition, a substantial fraction of patients spontaneously resolve their HBV infection without any treatment. Experts estimate that more than 1 billion people worldwide have been infected by HBV and then later had their infection clear “naturally,” said Dr. Revill. But the mechanism by which this happens is currently a mystery. “We don’t know how or why” so many infected people are “cured” naturally, Dr. Revill admitted, but it gives him and his colleagues hope that the numbers can expand once more and better treatments for HBV infection are available.
VIENNA – They hope either to have a cure or to have made substantial progress toward this goal over the next 10 years.
Treatments already are on the market that effectively inhibit hepatitis B replication in infected patients (and an effective preventive vaccine also exists). Still, these treatments are not curative, and for the vast majority of patients treatment must continue indefinitely, while their risk for liver cancer and their virally induced immune system abnormalities remain, Peter A. Revill, PhD, said during a press briefing that introduced a strategy for hepatitis B virus (HBV) cure development from the International Coalition to Eliminate HBV. Concurrently with the briefing session, the strategy appeared in an article published online (Lancet Gastroenterol Hepatol. 2019 Apr 10. doi: 10.1016/s2468-1253(19)30119-0).
The way forward will likely be a “two-pronged approach or restoring immune responses and targeting the virus,” Dr. Revill, head of molecular virology at the Doherty Institute in Melbourne, said in a video interview.
The new strategy recognizes the huge challenge of devising a treatment that produces a total cure that includes elimination of all traces of viral DNA from patients and for the immediate future focuses on the goal of functional cure. The term functional cure means a sustained period without detectable HBV surface antigen or HBV DNA in a patient’s serum, as well as suppressed virus release. Another feature of a functional cure would be a halt to progression of liver disease, replaced by liver regeneration, said Anna S. Lok, MD, professor of medicine and director of clinical hepatology at the University of Michigan, Ann Arbor, and a member of the strategy-writing group. She and her colleagues who wrote the strategy foresee the need for drug combinations with agents that can hit multiple viral targets as well as agents that restore normal immune function.
Several novel drug classes aimed at new viral targets, such as capsid inhibitors, are in various stages of clinical development, said Fabien Zoulim, MD, head of the gastroenterology and hepatology service at the Red Cross Hospital in Lyon, France, and another member of the writing panel. “We have many drug candidates” that use novel approaches to further restrict viral growth, roughly 50 agents in phase 1 and 2 studies, he said during the press briefing, held during the meeting sponsored by the European Association for the Study of the Liver. The other, immunologic aspect of the two-part cure strategy – restoring the “exhausted” HBV-specific T-cell population and stimulating production of neutralizing antibody to HBV – remains hypothetical right now, however. “It’s a concept that needs development,” Dr. Zoulim said.
A reason members of the coalition are optimistic about eventual prospects for a cure is that currently about 1% of patients on HBV antiviral treatments have a functional cure after relatively brief treatment, and the percentage of cured patients plateaus at about 10% among those who remain on current HBV antiviral drugs for several years. In addition, a substantial fraction of patients spontaneously resolve their HBV infection without any treatment. Experts estimate that more than 1 billion people worldwide have been infected by HBV and then later had their infection clear “naturally,” said Dr. Revill. But the mechanism by which this happens is currently a mystery. “We don’t know how or why” so many infected people are “cured” naturally, Dr. Revill admitted, but it gives him and his colleagues hope that the numbers can expand once more and better treatments for HBV infection are available.
VIENNA – They hope either to have a cure or to have made substantial progress toward this goal over the next 10 years.
Treatments already are on the market that effectively inhibit hepatitis B replication in infected patients (and an effective preventive vaccine also exists). Still, these treatments are not curative, and for the vast majority of patients treatment must continue indefinitely, while their risk for liver cancer and their virally induced immune system abnormalities remain, Peter A. Revill, PhD, said during a press briefing that introduced a strategy for hepatitis B virus (HBV) cure development from the International Coalition to Eliminate HBV. Concurrently with the briefing session, the strategy appeared in an article published online (Lancet Gastroenterol Hepatol. 2019 Apr 10. doi: 10.1016/s2468-1253(19)30119-0).
The way forward will likely be a “two-pronged approach or restoring immune responses and targeting the virus,” Dr. Revill, head of molecular virology at the Doherty Institute in Melbourne, said in a video interview.
The new strategy recognizes the huge challenge of devising a treatment that produces a total cure that includes elimination of all traces of viral DNA from patients and for the immediate future focuses on the goal of functional cure. The term functional cure means a sustained period without detectable HBV surface antigen or HBV DNA in a patient’s serum, as well as suppressed virus release. Another feature of a functional cure would be a halt to progression of liver disease, replaced by liver regeneration, said Anna S. Lok, MD, professor of medicine and director of clinical hepatology at the University of Michigan, Ann Arbor, and a member of the strategy-writing group. She and her colleagues who wrote the strategy foresee the need for drug combinations with agents that can hit multiple viral targets as well as agents that restore normal immune function.
Several novel drug classes aimed at new viral targets, such as capsid inhibitors, are in various stages of clinical development, said Fabien Zoulim, MD, head of the gastroenterology and hepatology service at the Red Cross Hospital in Lyon, France, and another member of the writing panel. “We have many drug candidates” that use novel approaches to further restrict viral growth, roughly 50 agents in phase 1 and 2 studies, he said during the press briefing, held during the meeting sponsored by the European Association for the Study of the Liver. The other, immunologic aspect of the two-part cure strategy – restoring the “exhausted” HBV-specific T-cell population and stimulating production of neutralizing antibody to HBV – remains hypothetical right now, however. “It’s a concept that needs development,” Dr. Zoulim said.
A reason members of the coalition are optimistic about eventual prospects for a cure is that currently about 1% of patients on HBV antiviral treatments have a functional cure after relatively brief treatment, and the percentage of cured patients plateaus at about 10% among those who remain on current HBV antiviral drugs for several years. In addition, a substantial fraction of patients spontaneously resolve their HBV infection without any treatment. Experts estimate that more than 1 billion people worldwide have been infected by HBV and then later had their infection clear “naturally,” said Dr. Revill. But the mechanism by which this happens is currently a mystery. “We don’t know how or why” so many infected people are “cured” naturally, Dr. Revill admitted, but it gives him and his colleagues hope that the numbers can expand once more and better treatments for HBV infection are available.
REPORTING FROM ILC 2019
Geroscience brings bench science to the real-world problems of aging
NEW ORLEANS – Patients ask their doctors whether dietary manipulation can extend lifespan and promote healthy aging. Right now, basic scientists and clinicians from many disciplines are teaming up under the broad umbrella of the field of geroscience to try to answer these and other concerns relevant to an aging population.
“The idea here is that, instead of going after each disease one at a time, as we do ... [we] instead go after disease vulnerability – and this is something that is shared, as a function of age,” Rozalyn Anderson, PhD, said of this new discipline. The work touches on disparate diseases such as cancer, dementia, and diabetes, she pointed out during a video interview at the annual meeting of the Endocrine Society.
“I separate these things out into ‘front-end’ and ‘back-end,’ work,” said Dr. Anderson of the University of Wisconsin-Madison’s aging and caloric restriction program. She explained that the caloric restriction she researches is back-end work to support the rapidly evolving field of nutritional modulation of aging.
When the basic science builds the framework, physicians and scientists can turn to front-end research, looking at humans to see which dietary manipulations are effective – and which are achievable.
“Take a paradigm that works, and then try to understand how it works,” said Dr. Anderson. “So [for example], we have this paradigm, and it’s tremendously effective in rodents. It’s effective in flies, in worms, in yeast, in spiders, in dogs – and in nonhuman primates.” Then, she and her team try to pull out clues “about the biology of aging itself, and what creates disease vulnerability as a function of age,” she said.
“The most important thing of all is that we can modify aging. This is not a foregone conclusion – no one would have believed it. But even in a primate species, we can change how they age. And the way in which we change is through nutrition.”
Dr Anderson added that “the paradigm of caloric restriction is tremendously effective, but [in reality], people are not going to do it.” It’s simply not practical to ask individuals to restrict calories by 30% or more over a lifespan, so “.”
Dr. Anderson reported no relevant conflicts of interest or disclosures.
NEW ORLEANS – Patients ask their doctors whether dietary manipulation can extend lifespan and promote healthy aging. Right now, basic scientists and clinicians from many disciplines are teaming up under the broad umbrella of the field of geroscience to try to answer these and other concerns relevant to an aging population.
“The idea here is that, instead of going after each disease one at a time, as we do ... [we] instead go after disease vulnerability – and this is something that is shared, as a function of age,” Rozalyn Anderson, PhD, said of this new discipline. The work touches on disparate diseases such as cancer, dementia, and diabetes, she pointed out during a video interview at the annual meeting of the Endocrine Society.
“I separate these things out into ‘front-end’ and ‘back-end,’ work,” said Dr. Anderson of the University of Wisconsin-Madison’s aging and caloric restriction program. She explained that the caloric restriction she researches is back-end work to support the rapidly evolving field of nutritional modulation of aging.
When the basic science builds the framework, physicians and scientists can turn to front-end research, looking at humans to see which dietary manipulations are effective – and which are achievable.
“Take a paradigm that works, and then try to understand how it works,” said Dr. Anderson. “So [for example], we have this paradigm, and it’s tremendously effective in rodents. It’s effective in flies, in worms, in yeast, in spiders, in dogs – and in nonhuman primates.” Then, she and her team try to pull out clues “about the biology of aging itself, and what creates disease vulnerability as a function of age,” she said.
“The most important thing of all is that we can modify aging. This is not a foregone conclusion – no one would have believed it. But even in a primate species, we can change how they age. And the way in which we change is through nutrition.”
Dr Anderson added that “the paradigm of caloric restriction is tremendously effective, but [in reality], people are not going to do it.” It’s simply not practical to ask individuals to restrict calories by 30% or more over a lifespan, so “.”
Dr. Anderson reported no relevant conflicts of interest or disclosures.
NEW ORLEANS – Patients ask their doctors whether dietary manipulation can extend lifespan and promote healthy aging. Right now, basic scientists and clinicians from many disciplines are teaming up under the broad umbrella of the field of geroscience to try to answer these and other concerns relevant to an aging population.
“The idea here is that, instead of going after each disease one at a time, as we do ... [we] instead go after disease vulnerability – and this is something that is shared, as a function of age,” Rozalyn Anderson, PhD, said of this new discipline. The work touches on disparate diseases such as cancer, dementia, and diabetes, she pointed out during a video interview at the annual meeting of the Endocrine Society.
“I separate these things out into ‘front-end’ and ‘back-end,’ work,” said Dr. Anderson of the University of Wisconsin-Madison’s aging and caloric restriction program. She explained that the caloric restriction she researches is back-end work to support the rapidly evolving field of nutritional modulation of aging.
When the basic science builds the framework, physicians and scientists can turn to front-end research, looking at humans to see which dietary manipulations are effective – and which are achievable.
“Take a paradigm that works, and then try to understand how it works,” said Dr. Anderson. “So [for example], we have this paradigm, and it’s tremendously effective in rodents. It’s effective in flies, in worms, in yeast, in spiders, in dogs – and in nonhuman primates.” Then, she and her team try to pull out clues “about the biology of aging itself, and what creates disease vulnerability as a function of age,” she said.
“The most important thing of all is that we can modify aging. This is not a foregone conclusion – no one would have believed it. But even in a primate species, we can change how they age. And the way in which we change is through nutrition.”
Dr Anderson added that “the paradigm of caloric restriction is tremendously effective, but [in reality], people are not going to do it.” It’s simply not practical to ask individuals to restrict calories by 30% or more over a lifespan, so “.”
Dr. Anderson reported no relevant conflicts of interest or disclosures.
REPORTING FROM ENDO 2019
Intermittent, but prolonged, calorie restriction may improve metabolic markers
NEW ORLEANS – Can a physician-supervised, intermittent fasting strategy improve metabolic risk? Yes, according to Valter Longo, PhD.
Dr. Longo is a proponent of 5 days of reduced calories, performed once monthly or even less frequently for at-risk individuals. He calls this the “fasting-mimicking diet.”
“If somebody is obese or overweight, and has high cholesterol, high fasting glucose, and is perhaps prediabetic, then a doctor may decide to do the diet once a month for 5 days, and for the rest of the month, the person can go back to whatever it is that they do,” he said in a video interview at the annual meeting of the Endocrine Society.
“We think we are going to see more and more of this approach in the future,” said Dr. Longo, the Edna M. Jones Professor of Gerontology at the University of Southern California, Los Angeles.
Dr. Longo sees two chief practical benefits from the diet. First, patients “don’t feel they are being pushed to revolutionize their lives” because they aren’t asked to make radical lifestyle changes that have to be adhered to on a daily basis, and second, “we are starting to see that the patient slowly moves in the direction of a better diet without being asked to do it.”
which includes some healthy fats from olive oil and nuts. Fasting blood glucose, blood pressure, and insulinlike growth factor 1 levels and other metabolic markers were all reduced in the randomized crossover trial after 3 months of the diet plan.
Dr. Longo noted that in the clinical trial, effects were more pronounced for individuals with a higher risk for disease.
Dr. Longo has a majority stake in L-Nutra, which markets a commercially available fasting-mimicking diet package. He donates his proceeds to a nonprofit corporation he founded.
NEW ORLEANS – Can a physician-supervised, intermittent fasting strategy improve metabolic risk? Yes, according to Valter Longo, PhD.
Dr. Longo is a proponent of 5 days of reduced calories, performed once monthly or even less frequently for at-risk individuals. He calls this the “fasting-mimicking diet.”
“If somebody is obese or overweight, and has high cholesterol, high fasting glucose, and is perhaps prediabetic, then a doctor may decide to do the diet once a month for 5 days, and for the rest of the month, the person can go back to whatever it is that they do,” he said in a video interview at the annual meeting of the Endocrine Society.
“We think we are going to see more and more of this approach in the future,” said Dr. Longo, the Edna M. Jones Professor of Gerontology at the University of Southern California, Los Angeles.
Dr. Longo sees two chief practical benefits from the diet. First, patients “don’t feel they are being pushed to revolutionize their lives” because they aren’t asked to make radical lifestyle changes that have to be adhered to on a daily basis, and second, “we are starting to see that the patient slowly moves in the direction of a better diet without being asked to do it.”
which includes some healthy fats from olive oil and nuts. Fasting blood glucose, blood pressure, and insulinlike growth factor 1 levels and other metabolic markers were all reduced in the randomized crossover trial after 3 months of the diet plan.
Dr. Longo noted that in the clinical trial, effects were more pronounced for individuals with a higher risk for disease.
Dr. Longo has a majority stake in L-Nutra, which markets a commercially available fasting-mimicking diet package. He donates his proceeds to a nonprofit corporation he founded.
NEW ORLEANS – Can a physician-supervised, intermittent fasting strategy improve metabolic risk? Yes, according to Valter Longo, PhD.
Dr. Longo is a proponent of 5 days of reduced calories, performed once monthly or even less frequently for at-risk individuals. He calls this the “fasting-mimicking diet.”
“If somebody is obese or overweight, and has high cholesterol, high fasting glucose, and is perhaps prediabetic, then a doctor may decide to do the diet once a month for 5 days, and for the rest of the month, the person can go back to whatever it is that they do,” he said in a video interview at the annual meeting of the Endocrine Society.
“We think we are going to see more and more of this approach in the future,” said Dr. Longo, the Edna M. Jones Professor of Gerontology at the University of Southern California, Los Angeles.
Dr. Longo sees two chief practical benefits from the diet. First, patients “don’t feel they are being pushed to revolutionize their lives” because they aren’t asked to make radical lifestyle changes that have to be adhered to on a daily basis, and second, “we are starting to see that the patient slowly moves in the direction of a better diet without being asked to do it.”
which includes some healthy fats from olive oil and nuts. Fasting blood glucose, blood pressure, and insulinlike growth factor 1 levels and other metabolic markers were all reduced in the randomized crossover trial after 3 months of the diet plan.
Dr. Longo noted that in the clinical trial, effects were more pronounced for individuals with a higher risk for disease.
Dr. Longo has a majority stake in L-Nutra, which markets a commercially available fasting-mimicking diet package. He donates his proceeds to a nonprofit corporation he founded.
REPORTING FROM ENDO 2019
Expert gives tips on timing, managing lupus pregnancies
SAN FRANCISCO – Not that many years ago, women with systemic lupus erythematosus were told not to get pregnant. It was just one more lupus heartbreak.
Times have changed, according to Lisa Sammaritano, MD, a lupus specialist and associate professor of clinical medicine at Weill Cornell Medical College, New York.
While lupus certainly complicates pregnancy, it by no means rules it out these days. With careful management, the dream of motherhood can become a reality for many women. Dr. Sammaritano shared her insights about timing and treatment at an international congress on systemic lupus erythematosus.
It’s important that the disease is under control as much as possible; that means that timing – and contraception – are key. Antiphospholipid antibodies, common in lupus, complicate matters, but there are workarounds, she said.
SAN FRANCISCO – Not that many years ago, women with systemic lupus erythematosus were told not to get pregnant. It was just one more lupus heartbreak.
Times have changed, according to Lisa Sammaritano, MD, a lupus specialist and associate professor of clinical medicine at Weill Cornell Medical College, New York.
While lupus certainly complicates pregnancy, it by no means rules it out these days. With careful management, the dream of motherhood can become a reality for many women. Dr. Sammaritano shared her insights about timing and treatment at an international congress on systemic lupus erythematosus.
It’s important that the disease is under control as much as possible; that means that timing – and contraception – are key. Antiphospholipid antibodies, common in lupus, complicate matters, but there are workarounds, she said.
SAN FRANCISCO – Not that many years ago, women with systemic lupus erythematosus were told not to get pregnant. It was just one more lupus heartbreak.
Times have changed, according to Lisa Sammaritano, MD, a lupus specialist and associate professor of clinical medicine at Weill Cornell Medical College, New York.
While lupus certainly complicates pregnancy, it by no means rules it out these days. With careful management, the dream of motherhood can become a reality for many women. Dr. Sammaritano shared her insights about timing and treatment at an international congress on systemic lupus erythematosus.
It’s important that the disease is under control as much as possible; that means that timing – and contraception – are key. Antiphospholipid antibodies, common in lupus, complicate matters, but there are workarounds, she said.
AT LUPUS 2019
Oxytocin dampens the brain’s food-related reward circuitry
NEW ORLEANS – Oxytocin shows promise as a weight-loss medication, with encouraging results in animal models and small human studies. Now, in a calorie-rich environment.
“It is clear by now that obesity is a very serious health concern,” Liya Kerem, MD, said in a video interview at the annual meeting of the Endocrine Society. “The most adopted strategy, which is lifestyle modification, does not help [with losing or maintaining] weight in many cases, so we really need to find new treatments for obesity.”
Functional magnetic resonance imaging (fMRI) is a good tool for investigating the neurobiologic basis of overeating, said Dr. Kerem, a pediatric endocrinology fellow at Massachusetts General Hospital, Boston. In previous studies, fMRI has shown that “individuals with obesity have hyperactivation of the reward circuitry in the brain.”
Oxytocin is produced in the hypothalamus and is active in many brain areas associated with reward processing, said Dr. Kerem. Animal studies have shown a decrease in food intake and weight gain with oxytocin administration.
The hormone, which is generally seen as very safe, has had limited study in humans as a weight-loss strategy. Findings from one small study have shown that in men, a single intranasal dose of 24 IU of oxytocin resulted in less hunger-driven eating as well as lower consumption of a postmeal palatable snack, with the latter representing hedonic eating, said Dr. Kerem. A second small pilot study showed that significant weight loss occurred in obese humans after 8 weeks of daily oxytocin administration.
Findings from another study showed that participants who were overweight or obese, unlike their normal-weight counterparts, had reduced activation in the ventral tegmental area (VTA) after oxytocin administration. The VTA is an important region in the brain’s reward network, explained Dr. Kerem.
She and her colleagues used fMRI to probe dynamic changes in brain reward circuitry under the effect of oxytocin. They wanted to understand how oxytocin would “change the dialog between the VTA and the key brain areas involved in processing visual food stimuli.”
The hypothesis was that oxytocin would reduce functional connectivity between the VTA and other brain areas that are important for food reward and sensory processing when the participants were exposed to pictures of high-calorie food.
To test that hypothesis, the researchers showed the participants 100 each of four different kinds of images: high-calorie foods, low-calorie foods, nonfood images, and “fixation” images, used for calibration. The 10 participants had a mean body mass index of 29 kg/m2, and the mean age was 31 years.
Oxytocin did indeed attenuate functional connectivity between the VTA and several brain regions that are “key food motivation areas,” said Dr. Kerem. In particular, connections between the VTA and the insula were reduced with oxytocin. The insula is the “gustatory hub of the brain, key to subjective perception of food stimuli,” she explained.
Other attenuated associations included the oral area of the somatosensory cortex; the operculum, which shows fMRI activation to taste; the temporal gyrus, which is important for sensory processing; and, importantly, both the amygdala and hippocampus, known to be important for stimulus-reward learning, said Dr. Kerem. “We found that oxytocin targets exactly that hyperactivation in an overweight and obese population.”
It “reduced the functional connectivity between the VTA, a key hedonic brain region that drives efforts to obtain desired foods, and multiple brain areas involved in the cognitive, sensory, and emotional processing of food cues in men with overweight and obesity,” she said at a press conference highlighting the research. She emphasized that the effect was seen only with exposure to high-calorie food images. “Targeting hyperactivation of reward areas with oxytocin may inhibit overeating behavior,” she added.
Dr. Kerem and her colleagues are currently enrolling men and women for a larger clinical trial of oxytocin for weight loss.
Dr. Kerem reported no conflicts of interest. One of the study’s coauthors is a consultant for OXT Therapeutics, which is investigating obesity-related uses for oxytocin.
NEW ORLEANS – Oxytocin shows promise as a weight-loss medication, with encouraging results in animal models and small human studies. Now, in a calorie-rich environment.
“It is clear by now that obesity is a very serious health concern,” Liya Kerem, MD, said in a video interview at the annual meeting of the Endocrine Society. “The most adopted strategy, which is lifestyle modification, does not help [with losing or maintaining] weight in many cases, so we really need to find new treatments for obesity.”
Functional magnetic resonance imaging (fMRI) is a good tool for investigating the neurobiologic basis of overeating, said Dr. Kerem, a pediatric endocrinology fellow at Massachusetts General Hospital, Boston. In previous studies, fMRI has shown that “individuals with obesity have hyperactivation of the reward circuitry in the brain.”
Oxytocin is produced in the hypothalamus and is active in many brain areas associated with reward processing, said Dr. Kerem. Animal studies have shown a decrease in food intake and weight gain with oxytocin administration.
The hormone, which is generally seen as very safe, has had limited study in humans as a weight-loss strategy. Findings from one small study have shown that in men, a single intranasal dose of 24 IU of oxytocin resulted in less hunger-driven eating as well as lower consumption of a postmeal palatable snack, with the latter representing hedonic eating, said Dr. Kerem. A second small pilot study showed that significant weight loss occurred in obese humans after 8 weeks of daily oxytocin administration.
Findings from another study showed that participants who were overweight or obese, unlike their normal-weight counterparts, had reduced activation in the ventral tegmental area (VTA) after oxytocin administration. The VTA is an important region in the brain’s reward network, explained Dr. Kerem.
She and her colleagues used fMRI to probe dynamic changes in brain reward circuitry under the effect of oxytocin. They wanted to understand how oxytocin would “change the dialog between the VTA and the key brain areas involved in processing visual food stimuli.”
The hypothesis was that oxytocin would reduce functional connectivity between the VTA and other brain areas that are important for food reward and sensory processing when the participants were exposed to pictures of high-calorie food.
To test that hypothesis, the researchers showed the participants 100 each of four different kinds of images: high-calorie foods, low-calorie foods, nonfood images, and “fixation” images, used for calibration. The 10 participants had a mean body mass index of 29 kg/m2, and the mean age was 31 years.
Oxytocin did indeed attenuate functional connectivity between the VTA and several brain regions that are “key food motivation areas,” said Dr. Kerem. In particular, connections between the VTA and the insula were reduced with oxytocin. The insula is the “gustatory hub of the brain, key to subjective perception of food stimuli,” she explained.
Other attenuated associations included the oral area of the somatosensory cortex; the operculum, which shows fMRI activation to taste; the temporal gyrus, which is important for sensory processing; and, importantly, both the amygdala and hippocampus, known to be important for stimulus-reward learning, said Dr. Kerem. “We found that oxytocin targets exactly that hyperactivation in an overweight and obese population.”
It “reduced the functional connectivity between the VTA, a key hedonic brain region that drives efforts to obtain desired foods, and multiple brain areas involved in the cognitive, sensory, and emotional processing of food cues in men with overweight and obesity,” she said at a press conference highlighting the research. She emphasized that the effect was seen only with exposure to high-calorie food images. “Targeting hyperactivation of reward areas with oxytocin may inhibit overeating behavior,” she added.
Dr. Kerem and her colleagues are currently enrolling men and women for a larger clinical trial of oxytocin for weight loss.
Dr. Kerem reported no conflicts of interest. One of the study’s coauthors is a consultant for OXT Therapeutics, which is investigating obesity-related uses for oxytocin.
NEW ORLEANS – Oxytocin shows promise as a weight-loss medication, with encouraging results in animal models and small human studies. Now, in a calorie-rich environment.
“It is clear by now that obesity is a very serious health concern,” Liya Kerem, MD, said in a video interview at the annual meeting of the Endocrine Society. “The most adopted strategy, which is lifestyle modification, does not help [with losing or maintaining] weight in many cases, so we really need to find new treatments for obesity.”
Functional magnetic resonance imaging (fMRI) is a good tool for investigating the neurobiologic basis of overeating, said Dr. Kerem, a pediatric endocrinology fellow at Massachusetts General Hospital, Boston. In previous studies, fMRI has shown that “individuals with obesity have hyperactivation of the reward circuitry in the brain.”
Oxytocin is produced in the hypothalamus and is active in many brain areas associated with reward processing, said Dr. Kerem. Animal studies have shown a decrease in food intake and weight gain with oxytocin administration.
The hormone, which is generally seen as very safe, has had limited study in humans as a weight-loss strategy. Findings from one small study have shown that in men, a single intranasal dose of 24 IU of oxytocin resulted in less hunger-driven eating as well as lower consumption of a postmeal palatable snack, with the latter representing hedonic eating, said Dr. Kerem. A second small pilot study showed that significant weight loss occurred in obese humans after 8 weeks of daily oxytocin administration.
Findings from another study showed that participants who were overweight or obese, unlike their normal-weight counterparts, had reduced activation in the ventral tegmental area (VTA) after oxytocin administration. The VTA is an important region in the brain’s reward network, explained Dr. Kerem.
She and her colleagues used fMRI to probe dynamic changes in brain reward circuitry under the effect of oxytocin. They wanted to understand how oxytocin would “change the dialog between the VTA and the key brain areas involved in processing visual food stimuli.”
The hypothesis was that oxytocin would reduce functional connectivity between the VTA and other brain areas that are important for food reward and sensory processing when the participants were exposed to pictures of high-calorie food.
To test that hypothesis, the researchers showed the participants 100 each of four different kinds of images: high-calorie foods, low-calorie foods, nonfood images, and “fixation” images, used for calibration. The 10 participants had a mean body mass index of 29 kg/m2, and the mean age was 31 years.
Oxytocin did indeed attenuate functional connectivity between the VTA and several brain regions that are “key food motivation areas,” said Dr. Kerem. In particular, connections between the VTA and the insula were reduced with oxytocin. The insula is the “gustatory hub of the brain, key to subjective perception of food stimuli,” she explained.
Other attenuated associations included the oral area of the somatosensory cortex; the operculum, which shows fMRI activation to taste; the temporal gyrus, which is important for sensory processing; and, importantly, both the amygdala and hippocampus, known to be important for stimulus-reward learning, said Dr. Kerem. “We found that oxytocin targets exactly that hyperactivation in an overweight and obese population.”
It “reduced the functional connectivity between the VTA, a key hedonic brain region that drives efforts to obtain desired foods, and multiple brain areas involved in the cognitive, sensory, and emotional processing of food cues in men with overweight and obesity,” she said at a press conference highlighting the research. She emphasized that the effect was seen only with exposure to high-calorie food images. “Targeting hyperactivation of reward areas with oxytocin may inhibit overeating behavior,” she added.
Dr. Kerem and her colleagues are currently enrolling men and women for a larger clinical trial of oxytocin for weight loss.
Dr. Kerem reported no conflicts of interest. One of the study’s coauthors is a consultant for OXT Therapeutics, which is investigating obesity-related uses for oxytocin.
REPORTING FROM ENDO 2019
Preclinical findings highlight value of Lynch syndrome for cancer vaccine development
ATLANTA – Lynch syndrome serves as an excellent platform for the development of immunoprevention cancer vaccines, and findings from a preclinical Lynch syndrome mouse model support ongoing research, according to Steven M. Lipkin, MD, PhD.
A novel vaccine, which included peptides encoding four intestinal cancer frameshift peptide (FSP) neoantigens derived from coding microsatellite (cMS) mutations in the genes Nacad, Maz, Xirp1, and Senp6 elicited strong antigen-specific cellular immune responses in the model, Dr. Lipkin, the Gladys and Roland Harriman Professor of Medicine and vice chair for research in the Sanford and Joan Weill Department of Medicine, Weill Cornell Medical College, New York, reported at the annual meeting of the American Association for Cancer Research.
CD4-specific T cell responses were detected for Maz, Nacad, and Senp6, and CD8-positive T cells were detected for Xirp1 and Nacad, he noted, explaining that the findings come in the wake of a recently completed clinical phase 1/2a trial that successfully demonstrated safety and immunogenicity of an FSP neoantigen-based vaccine in microsatellite unstable (MSI) colorectal cancer patients.
The current effort to further develop a cancer preventive vaccine against MSI cancers in Lynch syndrome using a preclinical mouse model involved a systematic database search to identify cMS sequences in the murine genome. Intestinal tumors obtained from Lynch syndrome mice were evaluated for mutations affecting these candidate cMS, and of 13 with a mutation frequency of 15% or higher, the 4 FSP neoantigens ultimately included in the vaccine elicited strong antigen-specific cellular immune responses.
Vaccination with peptides encoding these four intestinal cancer FSP neoantigens promoted antineoantigen immunity, reduced intestinal tumorigenicity, and prolonged overall survival, Dr. Lipkin said.
Further, based on preclinical data suggesting that naproxen in this setting might provide better risk-reducing effects, compared with aspirin (which has previously been shown to reduce colorectal cancer risk in Lynch syndrome patients), its addition to the vaccine did, indeed, improve response, he noted, explaining that naproxen worked as “sort of a super-aspirin,” that improved overall survival, compared with vaccine alone or nonsteroidal anti-inflammatory agents alone.
In a video interview, Dr. Lipkin describes his research and its potential implications for the immunoprevention of Lynch syndrome and other cancers.
Vaccination with as few as four mutations that occur across Lynch syndrome tumors induced complete cures in some mice and delays in disease onset in others, he said.
“[This is] a very simple approach, very effective,” he added, noting that the T cells are now being studied to better understand the biology of the effects. “The idea of immunoprevention ... is actually very exciting and ... can be expanded beyond this.”
Lynch syndrome is a “great place to start,” because of the high rate of mutations, which are the most immunogenic types of mutations, he said.
“If we can get this basic paradigm to work, I think we can expand it to other types of mutations – for example, KRAS or BRAF, which are seen frequently in lung cancers, colon cancers, stomach cancers, pancreatic cancers, and others,” he said, noting that a proposal for a phase 1 clinical trial has been submitted.
ATLANTA – Lynch syndrome serves as an excellent platform for the development of immunoprevention cancer vaccines, and findings from a preclinical Lynch syndrome mouse model support ongoing research, according to Steven M. Lipkin, MD, PhD.
A novel vaccine, which included peptides encoding four intestinal cancer frameshift peptide (FSP) neoantigens derived from coding microsatellite (cMS) mutations in the genes Nacad, Maz, Xirp1, and Senp6 elicited strong antigen-specific cellular immune responses in the model, Dr. Lipkin, the Gladys and Roland Harriman Professor of Medicine and vice chair for research in the Sanford and Joan Weill Department of Medicine, Weill Cornell Medical College, New York, reported at the annual meeting of the American Association for Cancer Research.
CD4-specific T cell responses were detected for Maz, Nacad, and Senp6, and CD8-positive T cells were detected for Xirp1 and Nacad, he noted, explaining that the findings come in the wake of a recently completed clinical phase 1/2a trial that successfully demonstrated safety and immunogenicity of an FSP neoantigen-based vaccine in microsatellite unstable (MSI) colorectal cancer patients.
The current effort to further develop a cancer preventive vaccine against MSI cancers in Lynch syndrome using a preclinical mouse model involved a systematic database search to identify cMS sequences in the murine genome. Intestinal tumors obtained from Lynch syndrome mice were evaluated for mutations affecting these candidate cMS, and of 13 with a mutation frequency of 15% or higher, the 4 FSP neoantigens ultimately included in the vaccine elicited strong antigen-specific cellular immune responses.
Vaccination with peptides encoding these four intestinal cancer FSP neoantigens promoted antineoantigen immunity, reduced intestinal tumorigenicity, and prolonged overall survival, Dr. Lipkin said.
Further, based on preclinical data suggesting that naproxen in this setting might provide better risk-reducing effects, compared with aspirin (which has previously been shown to reduce colorectal cancer risk in Lynch syndrome patients), its addition to the vaccine did, indeed, improve response, he noted, explaining that naproxen worked as “sort of a super-aspirin,” that improved overall survival, compared with vaccine alone or nonsteroidal anti-inflammatory agents alone.
In a video interview, Dr. Lipkin describes his research and its potential implications for the immunoprevention of Lynch syndrome and other cancers.
Vaccination with as few as four mutations that occur across Lynch syndrome tumors induced complete cures in some mice and delays in disease onset in others, he said.
“[This is] a very simple approach, very effective,” he added, noting that the T cells are now being studied to better understand the biology of the effects. “The idea of immunoprevention ... is actually very exciting and ... can be expanded beyond this.”
Lynch syndrome is a “great place to start,” because of the high rate of mutations, which are the most immunogenic types of mutations, he said.
“If we can get this basic paradigm to work, I think we can expand it to other types of mutations – for example, KRAS or BRAF, which are seen frequently in lung cancers, colon cancers, stomach cancers, pancreatic cancers, and others,” he said, noting that a proposal for a phase 1 clinical trial has been submitted.
ATLANTA – Lynch syndrome serves as an excellent platform for the development of immunoprevention cancer vaccines, and findings from a preclinical Lynch syndrome mouse model support ongoing research, according to Steven M. Lipkin, MD, PhD.
A novel vaccine, which included peptides encoding four intestinal cancer frameshift peptide (FSP) neoantigens derived from coding microsatellite (cMS) mutations in the genes Nacad, Maz, Xirp1, and Senp6 elicited strong antigen-specific cellular immune responses in the model, Dr. Lipkin, the Gladys and Roland Harriman Professor of Medicine and vice chair for research in the Sanford and Joan Weill Department of Medicine, Weill Cornell Medical College, New York, reported at the annual meeting of the American Association for Cancer Research.
CD4-specific T cell responses were detected for Maz, Nacad, and Senp6, and CD8-positive T cells were detected for Xirp1 and Nacad, he noted, explaining that the findings come in the wake of a recently completed clinical phase 1/2a trial that successfully demonstrated safety and immunogenicity of an FSP neoantigen-based vaccine in microsatellite unstable (MSI) colorectal cancer patients.
The current effort to further develop a cancer preventive vaccine against MSI cancers in Lynch syndrome using a preclinical mouse model involved a systematic database search to identify cMS sequences in the murine genome. Intestinal tumors obtained from Lynch syndrome mice were evaluated for mutations affecting these candidate cMS, and of 13 with a mutation frequency of 15% or higher, the 4 FSP neoantigens ultimately included in the vaccine elicited strong antigen-specific cellular immune responses.
Vaccination with peptides encoding these four intestinal cancer FSP neoantigens promoted antineoantigen immunity, reduced intestinal tumorigenicity, and prolonged overall survival, Dr. Lipkin said.
Further, based on preclinical data suggesting that naproxen in this setting might provide better risk-reducing effects, compared with aspirin (which has previously been shown to reduce colorectal cancer risk in Lynch syndrome patients), its addition to the vaccine did, indeed, improve response, he noted, explaining that naproxen worked as “sort of a super-aspirin,” that improved overall survival, compared with vaccine alone or nonsteroidal anti-inflammatory agents alone.
In a video interview, Dr. Lipkin describes his research and its potential implications for the immunoprevention of Lynch syndrome and other cancers.
Vaccination with as few as four mutations that occur across Lynch syndrome tumors induced complete cures in some mice and delays in disease onset in others, he said.
“[This is] a very simple approach, very effective,” he added, noting that the T cells are now being studied to better understand the biology of the effects. “The idea of immunoprevention ... is actually very exciting and ... can be expanded beyond this.”
Lynch syndrome is a “great place to start,” because of the high rate of mutations, which are the most immunogenic types of mutations, he said.
“If we can get this basic paradigm to work, I think we can expand it to other types of mutations – for example, KRAS or BRAF, which are seen frequently in lung cancers, colon cancers, stomach cancers, pancreatic cancers, and others,” he said, noting that a proposal for a phase 1 clinical trial has been submitted.
REPORTING FROM AACR 2019
HM19: Lessons from the Update in Hospital Medicine session

In the second of two episodes, Amith Skandhan, MD, FHM, of Southeast Alabama Medical Center, Dothan, Ala., and Raman Palabindala, MD, SFHM, of the University of Mississippi Medical Center, Jackson, Miss., discuss more of their favorite lessons from the annual meeting of the Society of Hospital Medicine. Dr. Skandhan and Dr. Palabindala share practice-changing takeaways from the Update in Hospital Medicine session.

In the second of two episodes, Amith Skandhan, MD, FHM, of Southeast Alabama Medical Center, Dothan, Ala., and Raman Palabindala, MD, SFHM, of the University of Mississippi Medical Center, Jackson, Miss., discuss more of their favorite lessons from the annual meeting of the Society of Hospital Medicine. Dr. Skandhan and Dr. Palabindala share practice-changing takeaways from the Update in Hospital Medicine session.

In the second of two episodes, Amith Skandhan, MD, FHM, of Southeast Alabama Medical Center, Dothan, Ala., and Raman Palabindala, MD, SFHM, of the University of Mississippi Medical Center, Jackson, Miss., discuss more of their favorite lessons from the annual meeting of the Society of Hospital Medicine. Dr. Skandhan and Dr. Palabindala share practice-changing takeaways from the Update in Hospital Medicine session.
REPORTING FROM HM19
HM19: Key takeaways on quality and innovation

In the first of two episodes, Amith Skandhan, MD, FHM, of Southeast Alabama Medical Center, Dothan, Ala., and Raman Palabindala, MD, SFHM, of the University of Mississippi Medical Center, Jackson, Miss., discuss their favorite lessons from the annual meeting of the Society of Hospital Medicine. Dr. Skandhan and Dr. Palabindala review key points from sessions on quality and patient safety, caring for the complex medically ill, using data analytics to drive clinical change, and the best studies from the Research and Innovation poster competition.

In the first of two episodes, Amith Skandhan, MD, FHM, of Southeast Alabama Medical Center, Dothan, Ala., and Raman Palabindala, MD, SFHM, of the University of Mississippi Medical Center, Jackson, Miss., discuss their favorite lessons from the annual meeting of the Society of Hospital Medicine. Dr. Skandhan and Dr. Palabindala review key points from sessions on quality and patient safety, caring for the complex medically ill, using data analytics to drive clinical change, and the best studies from the Research and Innovation poster competition.

In the first of two episodes, Amith Skandhan, MD, FHM, of Southeast Alabama Medical Center, Dothan, Ala., and Raman Palabindala, MD, SFHM, of the University of Mississippi Medical Center, Jackson, Miss., discuss their favorite lessons from the annual meeting of the Society of Hospital Medicine. Dr. Skandhan and Dr. Palabindala review key points from sessions on quality and patient safety, caring for the complex medically ill, using data analytics to drive clinical change, and the best studies from the Research and Innovation poster competition.
REPORTING FROM HM19
Laparoscopic bilateral salpingo-oophorectomy via minilaparotomy assistance for the massively enlarged adnexal mass

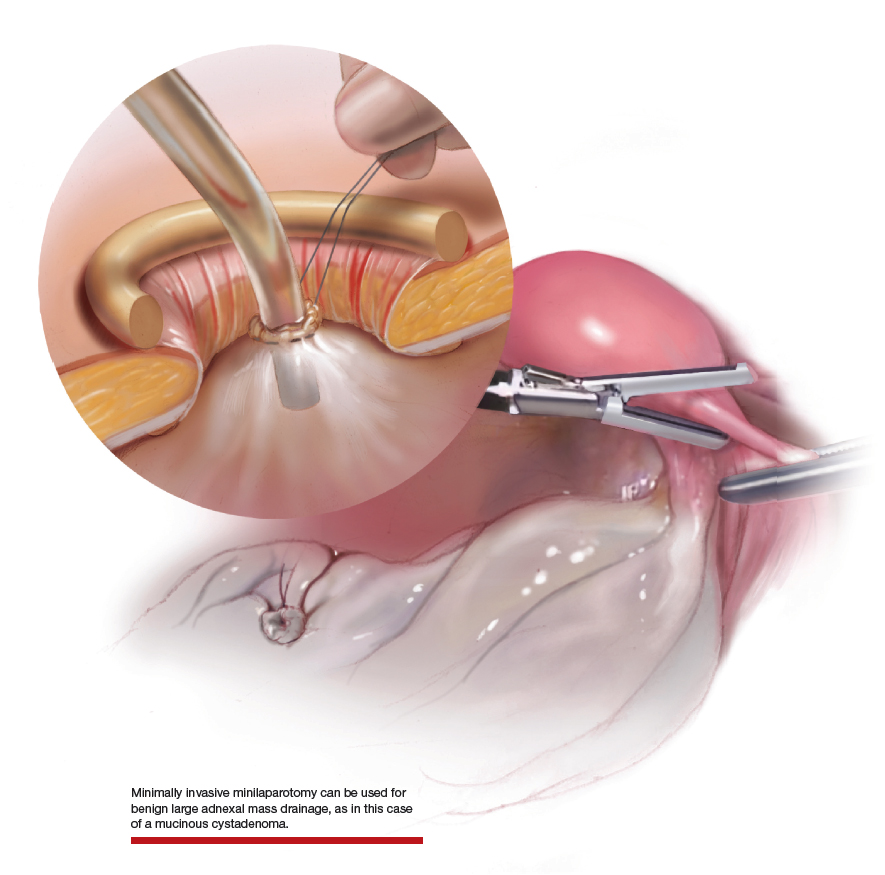
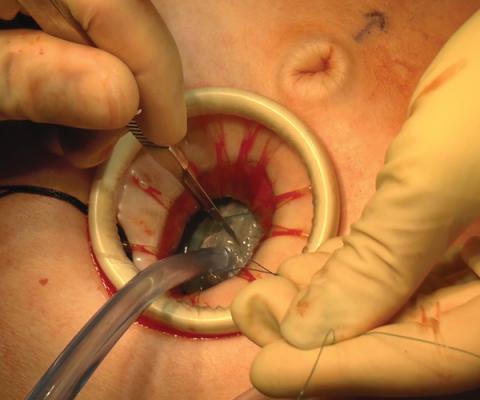
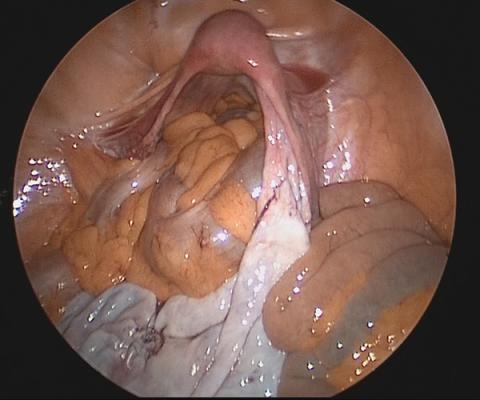
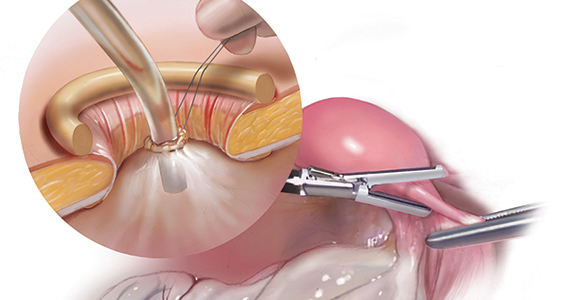
Large adnexal masses traditionally are removed surgically via laparotomy through a midline vertical incision to achieve adequate exposure and to avoid spillage of cyst contents. However, large laparotomies carry significant morbidity compared with minimally invasive techniques. Minilaparotomy is a minimally invasive approach that is associated with shorter operating times and lower estimated blood loss compared with laparoscopy in gynecologic surgery.1 The procedure also provides adequate exposure and can be used for carefully selected patients with a large adnexal mass.2,3 Preoperative assessment for the risk of malignancy typically includes an evaluation of risk factors, physical examination, imaging, and tumor markers.4
In this video, we illustrate a minimally invasive technique for the removal of a massively enlarged adnexal mass through laparoscopic bilateral salpingo-oophorectomy with minilaparotomy assistance. We conclude that this procedure is a safe and feasible option for women with a large benign adnexal mass, such as the highlighted patient whose final pathology resulted in a mucinous cystadenoma. Careful patient selection and preoperative assessment of malignancy risk is critical.5,6
We hope that you find this innovative approach useful in your clinical practice.
>> Dr. Arnold P. Advincula and colleagues
- Kumar A, Pearl M. Mini-laparotomy versus laparoscopy for gynecologic conditions. J Minim Invasive Gynecol. 2014;21:109-114.
- Pelosi MA. A novel minilaparotomy approach for large ovarian cysts. OBG Manag. 2004;16(2):17-30.
- Rhode JM, Advincula AP, Reynolds RK, et al. A minimally invasive technique for management of the large adnexal mass. J Minim Invasive Gynecol. 2006;13:476-479.
- American College of Obstetricians and Gynecologists' Committee on Practice Bulletins--Gynecology. Practice Bulletin No. 174: evaluation and management of adnexal masses. Obstet Gynecol. 2016;128:e210-e226.
- Roman LD, Muderspach LI, Stein SM, et al. Pelvic examination, tumor marker level, and gray-scale and Doppler sonography in the prediction of pelvic cancer. Obstet Gynecol. 1997;89:493-500.
- Dodge JE, Covens AL, Lacchetti C, et al; Gynecology Cancer Disease Site Group. Preoperative identification of a suspicious adnexal mass: a systematic review and meta-analysis. Gynecol Oncol. 2012:126:157-166.

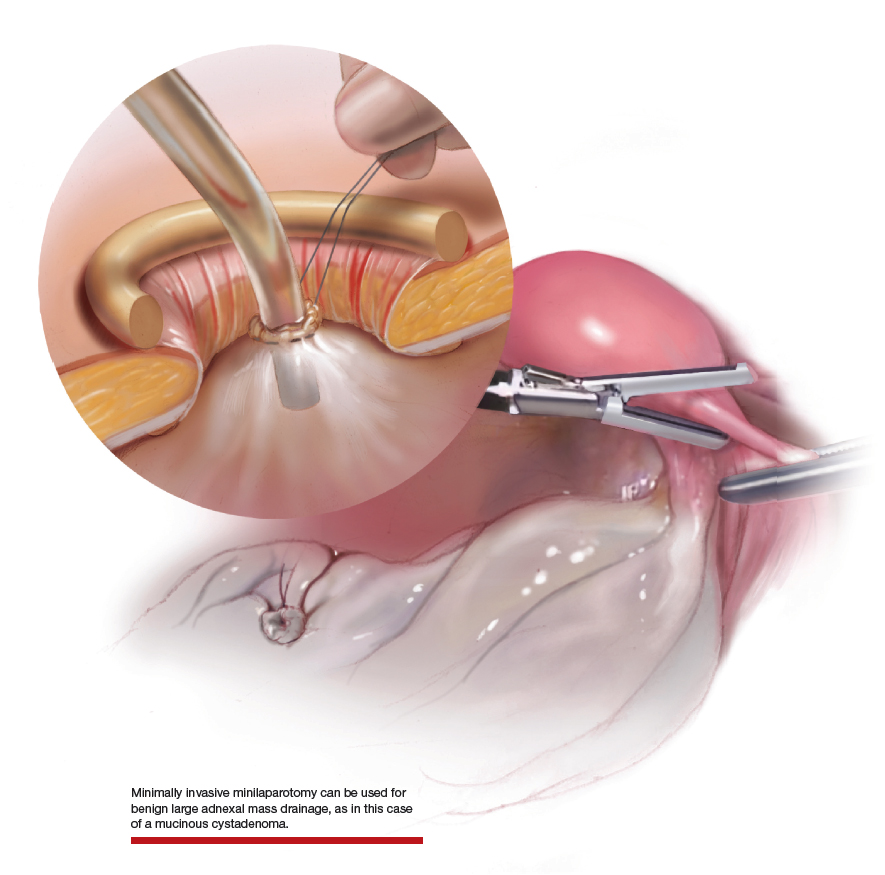
Large adnexal masses traditionally are removed surgically via laparotomy through a midline vertical incision to achieve adequate exposure and to avoid spillage of cyst contents. However, large laparotomies carry significant morbidity compared with minimally invasive techniques. Minilaparotomy is a minimally invasive approach that is associated with shorter operating times and lower estimated blood loss compared with laparoscopy in gynecologic surgery.1 The procedure also provides adequate exposure and can be used for carefully selected patients with a large adnexal mass.2,3 Preoperative assessment for the risk of malignancy typically includes an evaluation of risk factors, physical examination, imaging, and tumor markers.4
In this video, we illustrate a minimally invasive technique for the removal of a massively enlarged adnexal mass through laparoscopic bilateral salpingo-oophorectomy with minilaparotomy assistance. We conclude that this procedure is a safe and feasible option for women with a large benign adnexal mass, such as the highlighted patient whose final pathology resulted in a mucinous cystadenoma. Careful patient selection and preoperative assessment of malignancy risk is critical.5,6
We hope that you find this innovative approach useful in your clinical practice.
>> Dr. Arnold P. Advincula and colleagues

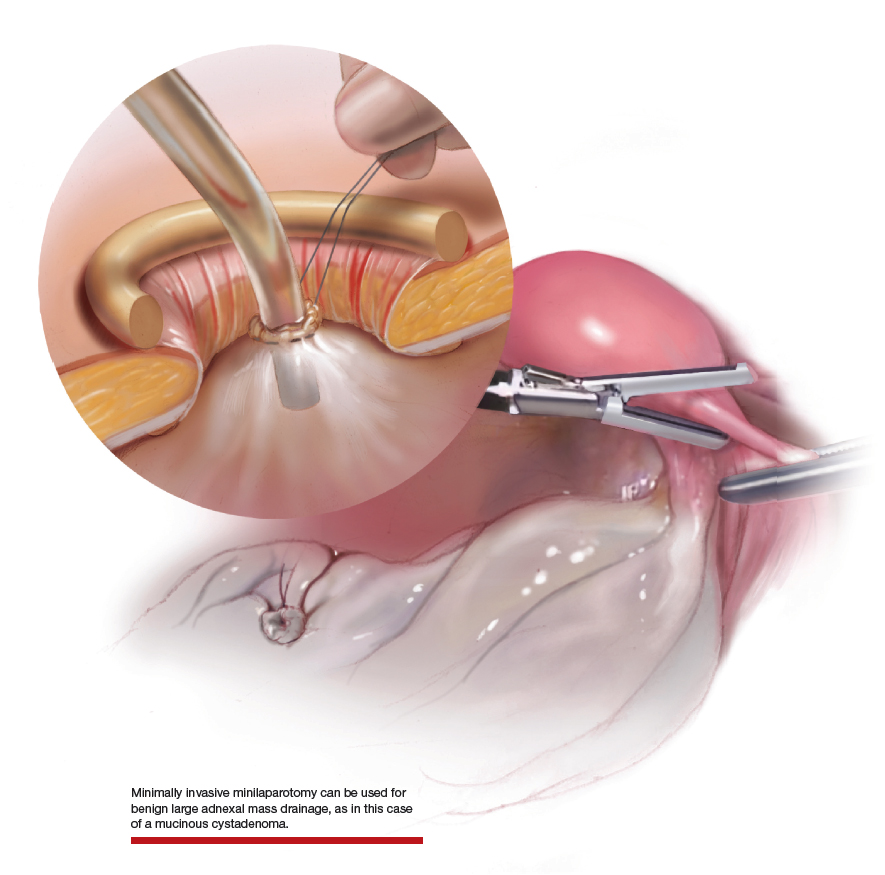
Large adnexal masses traditionally are removed surgically via laparotomy through a midline vertical incision to achieve adequate exposure and to avoid spillage of cyst contents. However, large laparotomies carry significant morbidity compared with minimally invasive techniques. Minilaparotomy is a minimally invasive approach that is associated with shorter operating times and lower estimated blood loss compared with laparoscopy in gynecologic surgery.1 The procedure also provides adequate exposure and can be used for carefully selected patients with a large adnexal mass.2,3 Preoperative assessment for the risk of malignancy typically includes an evaluation of risk factors, physical examination, imaging, and tumor markers.4
In this video, we illustrate a minimally invasive technique for the removal of a massively enlarged adnexal mass through laparoscopic bilateral salpingo-oophorectomy with minilaparotomy assistance. We conclude that this procedure is a safe and feasible option for women with a large benign adnexal mass, such as the highlighted patient whose final pathology resulted in a mucinous cystadenoma. Careful patient selection and preoperative assessment of malignancy risk is critical.5,6
We hope that you find this innovative approach useful in your clinical practice.
>> Dr. Arnold P. Advincula and colleagues
- Kumar A, Pearl M. Mini-laparotomy versus laparoscopy for gynecologic conditions. J Minim Invasive Gynecol. 2014;21:109-114.
- Pelosi MA. A novel minilaparotomy approach for large ovarian cysts. OBG Manag. 2004;16(2):17-30.
- Rhode JM, Advincula AP, Reynolds RK, et al. A minimally invasive technique for management of the large adnexal mass. J Minim Invasive Gynecol. 2006;13:476-479.
- American College of Obstetricians and Gynecologists' Committee on Practice Bulletins--Gynecology. Practice Bulletin No. 174: evaluation and management of adnexal masses. Obstet Gynecol. 2016;128:e210-e226.
- Roman LD, Muderspach LI, Stein SM, et al. Pelvic examination, tumor marker level, and gray-scale and Doppler sonography in the prediction of pelvic cancer. Obstet Gynecol. 1997;89:493-500.
- Dodge JE, Covens AL, Lacchetti C, et al; Gynecology Cancer Disease Site Group. Preoperative identification of a suspicious adnexal mass: a systematic review and meta-analysis. Gynecol Oncol. 2012:126:157-166.
- Kumar A, Pearl M. Mini-laparotomy versus laparoscopy for gynecologic conditions. J Minim Invasive Gynecol. 2014;21:109-114.
- Pelosi MA. A novel minilaparotomy approach for large ovarian cysts. OBG Manag. 2004;16(2):17-30.
- Rhode JM, Advincula AP, Reynolds RK, et al. A minimally invasive technique for management of the large adnexal mass. J Minim Invasive Gynecol. 2006;13:476-479.
- American College of Obstetricians and Gynecologists' Committee on Practice Bulletins--Gynecology. Practice Bulletin No. 174: evaluation and management of adnexal masses. Obstet Gynecol. 2016;128:e210-e226.
- Roman LD, Muderspach LI, Stein SM, et al. Pelvic examination, tumor marker level, and gray-scale and Doppler sonography in the prediction of pelvic cancer. Obstet Gynecol. 1997;89:493-500.
- Dodge JE, Covens AL, Lacchetti C, et al; Gynecology Cancer Disease Site Group. Preoperative identification of a suspicious adnexal mass: a systematic review and meta-analysis. Gynecol Oncol. 2012:126:157-166.
DDNA19: News and advances in IBD

Dr. Stephen Brant and Dr. Nikolaos Pyrsopoulos discuss the latest news and advances in inflammatory bowel disease (IBD) at Digestive Diseases: New Advances, jointly provided by Rutgers and Global Academy for Medical Education.
Global Academy and this news organization are owned by the same company.

Dr. Stephen Brant and Dr. Nikolaos Pyrsopoulos discuss the latest news and advances in inflammatory bowel disease (IBD) at Digestive Diseases: New Advances, jointly provided by Rutgers and Global Academy for Medical Education.
Global Academy and this news organization are owned by the same company.

Dr. Stephen Brant and Dr. Nikolaos Pyrsopoulos discuss the latest news and advances in inflammatory bowel disease (IBD) at Digestive Diseases: New Advances, jointly provided by Rutgers and Global Academy for Medical Education.
Global Academy and this news organization are owned by the same company.
REPORTING FROM DIGESTIVE DISEASES: NEW ADVANCES