User login
July 2017: Click for Credit
Here are 6 articles in the July issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. High-dose Oral Vitamin D3 Significantly Reduced Effects of Sunburn
To take the posttest, go to: http://bit.ly/2tmDiKc
Expires May 23, 2018
2. Women Less Likely to Be Diagnosed With Sleep Disorders
To take the posttest, go to: http://bit.ly/2rgLdne
Expires May 30, 2018
3. RA Treatment Delays Raise Risk for Long-term Disability
To take the posttest, go to: http://bit.ly/2tC0IGF
Expires May 30, 2018
4. Target Self-medication of Mood and Anxiety Symptoms
To take the posttest, go to: http://bit.ly/2vy5jel
Expires May 2, 2018
5. Two New Biomarkers for Breast Cancer Show Validity
To take the posttest, go to: http://bit.ly/2ve9H2L
Expires May 2, 2018
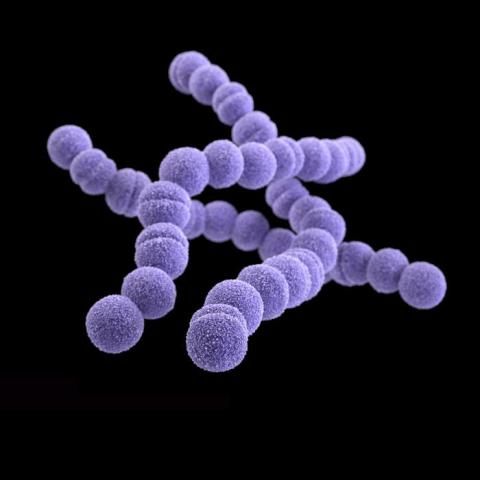
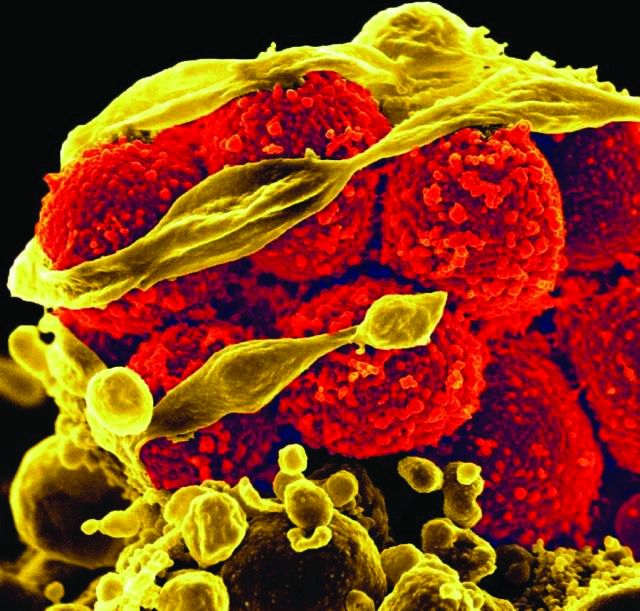
6. Time to Therapy for Gram-positive Bacteremia Reduced From 60 Hours to 4 Hours
To take the posttest, go to: http://bit.ly/2ssacIf
Expires May 25, 2018
Here are 6 articles in the July issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. High-dose Oral Vitamin D3 Significantly Reduced Effects of Sunburn
To take the posttest, go to: http://bit.ly/2tmDiKc
Expires May 23, 2018
2. Women Less Likely to Be Diagnosed With Sleep Disorders
To take the posttest, go to: http://bit.ly/2rgLdne
Expires May 30, 2018
3. RA Treatment Delays Raise Risk for Long-term Disability
To take the posttest, go to: http://bit.ly/2tC0IGF
Expires May 30, 2018
4. Target Self-medication of Mood and Anxiety Symptoms
To take the posttest, go to: http://bit.ly/2vy5jel
Expires May 2, 2018
5. Two New Biomarkers for Breast Cancer Show Validity
To take the posttest, go to: http://bit.ly/2ve9H2L
Expires May 2, 2018
6. Time to Therapy for Gram-positive Bacteremia Reduced From 60 Hours to 4 Hours
To take the posttest, go to: http://bit.ly/2ssacIf
Expires May 25, 2018
Here are 6 articles in the July issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. High-dose Oral Vitamin D3 Significantly Reduced Effects of Sunburn
To take the posttest, go to: http://bit.ly/2tmDiKc
Expires May 23, 2018
2. Women Less Likely to Be Diagnosed With Sleep Disorders
To take the posttest, go to: http://bit.ly/2rgLdne
Expires May 30, 2018
3. RA Treatment Delays Raise Risk for Long-term Disability
To take the posttest, go to: http://bit.ly/2tC0IGF
Expires May 30, 2018
4. Target Self-medication of Mood and Anxiety Symptoms
To take the posttest, go to: http://bit.ly/2vy5jel
Expires May 2, 2018
5. Two New Biomarkers for Breast Cancer Show Validity
To take the posttest, go to: http://bit.ly/2ve9H2L
Expires May 2, 2018
6. Time to Therapy for Gram-positive Bacteremia Reduced From 60 Hours to 4 Hours
To take the posttest, go to: http://bit.ly/2ssacIf
Expires May 25, 2018
Study validates EULAR definition of arthralgia suspicious for progression to RA
Results of a longitudinal study have confirmed that the recently established EULAR definition of arthralgia suspicious for progression to rheumatoid arthritis can help to distinguish patients who are at highest risk for progression from those who do not progress to RA.
Patients clinically suspected of arthralgia who met the definition for arthralgia suspicious for progression to RA displayed an increased risk for arthritis development, compared with patients who did not meet the EULAR definition (hazard ratio, 2.1; 95% confidence interval, 0.9-4.7). The approach had a sensitivity of 83% and positive predictive value of 30%, study head Annette van der Helm–van Mil, MD, reported at the European Congress of Rheumatology in Madrid.
The findings should help investigators looking at early arthritis progression to design better clinical trials by enabling more homogeneous populations of patients to be included, said Dr. van der Helm–van Mil, professor of rheumatology at Leiden University Medical Center and at Erasmus Medical Center in Rotterdam, both in the Netherlands.
“Previous data have shown that rheumatologists do recognize patients at risk for RA based on their clinical expertise and pattern recognition. So, they do recognize patients who have a combination of clinical characteristics that characterize the symptomatic prearthritis stage of RA. (This pattern is also called clinically suspect arthralgia,)” Dr. van der Helm–van Mil said in an interview.
However, the disadvantage of rheumatologists’ use of pattern recognition to identify patients at risk for RA is that it can be subjective, she said.
Several proof-of-concept trials are testing the hypothesis that the disease is more susceptible to disease-modifying treatment in the symptomatic prearthritis phase and that such early treatment might even prevent progression to chronic RA. But, selecting the “correct symptomatic patient” for early treatment with disease-modifying antirheumatic drugs is important, she said. Such a patient does not have clinical arthritis but is truly at risk for RA. Not all arthralgia patients are similar, and the type of arthralgia that is the hallmark for a heightened risk of progression to RA had not been defined formally prior to the EULAR definition.
A EULAR task force sought to provide some objective clarity by defining arthralgia at risk for RA (Ann Rheum Dis. 2017;76:491-6). The process relied on clinical expertise at all stages. However, until now, the definition had not been validated longitudinally. The current study used progression from arthralgia to clinical arthritis or RA as the outcome.
The definition of arthralgia at risk for RA hinges on seven parameters: symptom duration less than 1 year, symptoms in metacarpophalangeal joints, morning stiffness lasting an hour or more, symptoms that are worst in the morning, family history of RA, difficulty forming a fist, and positive squeeze test of metacarpophalangeal joints.
The researchers used those seven parameters to follow 241 Dutch patients considered likely to develop RA and 113 patients with recent-onset arthralgia in small joints who had not been evaluated by rheumatologists and who were referred to secondary care.
“The EULAR definition was developed for use in scientific studies and this definition is immediately applicable for this purpose,” Dr. van der Helm–van Mil said.
“With regards to application in daily practice, the clinical definition should be combined with results of additional investigations to accurately identify imminent RA in the phase of arthralgia. Which combination of markers yields the best accuracy is a subject for further studies,” Dr. van der Helm–van Mil said.
An important aspect of the task force’s definition is that rheumatologists should use it in patients in whom they consider imminent RA more likely than other diagnoses. The definition was not discriminative for RA when the investigators of the current study ignored this entry criterion, leading to a sensitivity of just 10% and positive predictive value of 3%.
“This suggests that the definition should be used in secondary care but may not be useful in primary care. However, more research is needed here,” Dr. van der Helm–van Mil said.
The authors reported no disclosures of interest.
Results of a longitudinal study have confirmed that the recently established EULAR definition of arthralgia suspicious for progression to rheumatoid arthritis can help to distinguish patients who are at highest risk for progression from those who do not progress to RA.
Patients clinically suspected of arthralgia who met the definition for arthralgia suspicious for progression to RA displayed an increased risk for arthritis development, compared with patients who did not meet the EULAR definition (hazard ratio, 2.1; 95% confidence interval, 0.9-4.7). The approach had a sensitivity of 83% and positive predictive value of 30%, study head Annette van der Helm–van Mil, MD, reported at the European Congress of Rheumatology in Madrid.
The findings should help investigators looking at early arthritis progression to design better clinical trials by enabling more homogeneous populations of patients to be included, said Dr. van der Helm–van Mil, professor of rheumatology at Leiden University Medical Center and at Erasmus Medical Center in Rotterdam, both in the Netherlands.
“Previous data have shown that rheumatologists do recognize patients at risk for RA based on their clinical expertise and pattern recognition. So, they do recognize patients who have a combination of clinical characteristics that characterize the symptomatic prearthritis stage of RA. (This pattern is also called clinically suspect arthralgia,)” Dr. van der Helm–van Mil said in an interview.
However, the disadvantage of rheumatologists’ use of pattern recognition to identify patients at risk for RA is that it can be subjective, she said.
Several proof-of-concept trials are testing the hypothesis that the disease is more susceptible to disease-modifying treatment in the symptomatic prearthritis phase and that such early treatment might even prevent progression to chronic RA. But, selecting the “correct symptomatic patient” for early treatment with disease-modifying antirheumatic drugs is important, she said. Such a patient does not have clinical arthritis but is truly at risk for RA. Not all arthralgia patients are similar, and the type of arthralgia that is the hallmark for a heightened risk of progression to RA had not been defined formally prior to the EULAR definition.
A EULAR task force sought to provide some objective clarity by defining arthralgia at risk for RA (Ann Rheum Dis. 2017;76:491-6). The process relied on clinical expertise at all stages. However, until now, the definition had not been validated longitudinally. The current study used progression from arthralgia to clinical arthritis or RA as the outcome.
The definition of arthralgia at risk for RA hinges on seven parameters: symptom duration less than 1 year, symptoms in metacarpophalangeal joints, morning stiffness lasting an hour or more, symptoms that are worst in the morning, family history of RA, difficulty forming a fist, and positive squeeze test of metacarpophalangeal joints.
The researchers used those seven parameters to follow 241 Dutch patients considered likely to develop RA and 113 patients with recent-onset arthralgia in small joints who had not been evaluated by rheumatologists and who were referred to secondary care.
“The EULAR definition was developed for use in scientific studies and this definition is immediately applicable for this purpose,” Dr. van der Helm–van Mil said.
“With regards to application in daily practice, the clinical definition should be combined with results of additional investigations to accurately identify imminent RA in the phase of arthralgia. Which combination of markers yields the best accuracy is a subject for further studies,” Dr. van der Helm–van Mil said.
An important aspect of the task force’s definition is that rheumatologists should use it in patients in whom they consider imminent RA more likely than other diagnoses. The definition was not discriminative for RA when the investigators of the current study ignored this entry criterion, leading to a sensitivity of just 10% and positive predictive value of 3%.
“This suggests that the definition should be used in secondary care but may not be useful in primary care. However, more research is needed here,” Dr. van der Helm–van Mil said.
The authors reported no disclosures of interest.
Results of a longitudinal study have confirmed that the recently established EULAR definition of arthralgia suspicious for progression to rheumatoid arthritis can help to distinguish patients who are at highest risk for progression from those who do not progress to RA.
Patients clinically suspected of arthralgia who met the definition for arthralgia suspicious for progression to RA displayed an increased risk for arthritis development, compared with patients who did not meet the EULAR definition (hazard ratio, 2.1; 95% confidence interval, 0.9-4.7). The approach had a sensitivity of 83% and positive predictive value of 30%, study head Annette van der Helm–van Mil, MD, reported at the European Congress of Rheumatology in Madrid.
The findings should help investigators looking at early arthritis progression to design better clinical trials by enabling more homogeneous populations of patients to be included, said Dr. van der Helm–van Mil, professor of rheumatology at Leiden University Medical Center and at Erasmus Medical Center in Rotterdam, both in the Netherlands.
“Previous data have shown that rheumatologists do recognize patients at risk for RA based on their clinical expertise and pattern recognition. So, they do recognize patients who have a combination of clinical characteristics that characterize the symptomatic prearthritis stage of RA. (This pattern is also called clinically suspect arthralgia,)” Dr. van der Helm–van Mil said in an interview.
However, the disadvantage of rheumatologists’ use of pattern recognition to identify patients at risk for RA is that it can be subjective, she said.
Several proof-of-concept trials are testing the hypothesis that the disease is more susceptible to disease-modifying treatment in the symptomatic prearthritis phase and that such early treatment might even prevent progression to chronic RA. But, selecting the “correct symptomatic patient” for early treatment with disease-modifying antirheumatic drugs is important, she said. Such a patient does not have clinical arthritis but is truly at risk for RA. Not all arthralgia patients are similar, and the type of arthralgia that is the hallmark for a heightened risk of progression to RA had not been defined formally prior to the EULAR definition.
A EULAR task force sought to provide some objective clarity by defining arthralgia at risk for RA (Ann Rheum Dis. 2017;76:491-6). The process relied on clinical expertise at all stages. However, until now, the definition had not been validated longitudinally. The current study used progression from arthralgia to clinical arthritis or RA as the outcome.
The definition of arthralgia at risk for RA hinges on seven parameters: symptom duration less than 1 year, symptoms in metacarpophalangeal joints, morning stiffness lasting an hour or more, symptoms that are worst in the morning, family history of RA, difficulty forming a fist, and positive squeeze test of metacarpophalangeal joints.
The researchers used those seven parameters to follow 241 Dutch patients considered likely to develop RA and 113 patients with recent-onset arthralgia in small joints who had not been evaluated by rheumatologists and who were referred to secondary care.
“The EULAR definition was developed for use in scientific studies and this definition is immediately applicable for this purpose,” Dr. van der Helm–van Mil said.
“With regards to application in daily practice, the clinical definition should be combined with results of additional investigations to accurately identify imminent RA in the phase of arthralgia. Which combination of markers yields the best accuracy is a subject for further studies,” Dr. van der Helm–van Mil said.
An important aspect of the task force’s definition is that rheumatologists should use it in patients in whom they consider imminent RA more likely than other diagnoses. The definition was not discriminative for RA when the investigators of the current study ignored this entry criterion, leading to a sensitivity of just 10% and positive predictive value of 3%.
“This suggests that the definition should be used in secondary care but may not be useful in primary care. However, more research is needed here,” Dr. van der Helm–van Mil said.
The authors reported no disclosures of interest.
FROM THE EULAR 2017 CONGRESS
Key clinical point:
Major finding: Patients clinically suspected of arthralgia who met the EULAR definition were twice as likely to develop RA at 2 years than were those who did not meet the definition (hazard ratio, 2.1; 95% confidence interval, 0.9–4.7).
Data source: Longitudinal study of 241 patients considered likely to develop RA and 113 patients with recent-onset arthralgia in small joints who had not been evaluated by rheumatologists and who were referred to secondary care.
Disclosures: The authors reported no disclosures of interest.
Ustekinumab trumps TNF-blockade for enthesitis in patients with psoriatic arthritis
MADRID – The anti-IL-23 antibody ustekinumab cleared enthesitis significantly better than did TNF-blockade in a small, open-label trial of patients with psoriatic arthritis
After 6 months on the drug, 71% of those taking the antibody achieved a score of 0 on the Spondyloarthritis Research Consortium of Canada (SPARCC) scale, representing a complete absence of enthesitis, Elizabeth Araujo, MD, said at the European Congress of Rheumatology. Just 38% of those on TNF-inhibitors achieved that score.
Enthesitis is often more bothersome to arthritis patients than their primary disease, said Dr. Araujo of the Centre of Internal Medicine, Universitätsklinikum Erlangen, Germany.
“Despite being a hallmark of PsA patients, enthesitis still receives rather peripheral attention as an outcome, especially when compared with ‘classical’ arthritis. Nonetheless, in clinical practice, enthesitis is an important factor for PsA-associated pain in many patients,” explained Dr. Araujo.
Yet it’s frequently ignored or under-treated. When it is addressed, enthesitis is often treated using TNF-inhibitors. But recent increases in the treatment options for PsA patients got Dr. Araujo thinking that PsA patients with enthesitis might respond better to a different therapy.
She investigated this with the open-label ECLIPSA trial, which randomized 51 PsA patients (47 with active enthesitis) to a 6-month treatment regimen of ustekinumab or a TNF-inhibitor. The primary endpoint of the observational study was a SPARCC score of 0.
Patients were a mean of 61 years, with a mean disease duration of 2.5 years. The mean baseline SPARCC score was 4. The mean Psoriatic Area and Severity Score (PASI) was 3.
Patients’ arthritis symptoms responded equally well to both drugs, with similar marked decreases in tender and swollen joint counts. But there was a clear, significant between-group separation on the SPARCC score, with 71% of the ustekinumab group reaching a 0 compared to 38% of the TNF-inhibition group.
Ustekinumab also effected better skin clearance than TNF-inhibition, she said. Among the TNF-inhibition group, about 20% achieved a PASI 90 and 20%, a PASI 100. Among those taking ustekinumab, about 80% achieved a PASI 90 and 55% a PASI 100.
The data point the way to more stratified treatment approaches for PsA patients, where PsA that predominantly involves enthesitis is treated by drugs like ustekinumab, Dr. Araujo said. Since both TNF-inhibitors and ustekinumab are approved for treatment of PsA, treatment could be tailored.
“Stratification of PsA patients according to clinical features (enthesitis driven vs. arthritis driven) appears within reach and will allow a more selective use of cytokine-blocking agents in PsA in the future,” said Dr. Araujo.
“More attention on enthesial-driven PsA patients is needed in the future as this patient group is well known to clinicians working in the PsA field but is massively underrepresented in clinical studies. Comparative studies of biological [disease-modifying antirheumatic drugs] in PsA need to take into account the differences in the clinical profile of PsA patients and should not be confined to the traditional polyarticular arthritis–driven disease population,” she added.
Dr. Araujo had no financial disclosures.
[email protected]
On Twitter @Alz_gal
MADRID – The anti-IL-23 antibody ustekinumab cleared enthesitis significantly better than did TNF-blockade in a small, open-label trial of patients with psoriatic arthritis
After 6 months on the drug, 71% of those taking the antibody achieved a score of 0 on the Spondyloarthritis Research Consortium of Canada (SPARCC) scale, representing a complete absence of enthesitis, Elizabeth Araujo, MD, said at the European Congress of Rheumatology. Just 38% of those on TNF-inhibitors achieved that score.
Enthesitis is often more bothersome to arthritis patients than their primary disease, said Dr. Araujo of the Centre of Internal Medicine, Universitätsklinikum Erlangen, Germany.
“Despite being a hallmark of PsA patients, enthesitis still receives rather peripheral attention as an outcome, especially when compared with ‘classical’ arthritis. Nonetheless, in clinical practice, enthesitis is an important factor for PsA-associated pain in many patients,” explained Dr. Araujo.
Yet it’s frequently ignored or under-treated. When it is addressed, enthesitis is often treated using TNF-inhibitors. But recent increases in the treatment options for PsA patients got Dr. Araujo thinking that PsA patients with enthesitis might respond better to a different therapy.
She investigated this with the open-label ECLIPSA trial, which randomized 51 PsA patients (47 with active enthesitis) to a 6-month treatment regimen of ustekinumab or a TNF-inhibitor. The primary endpoint of the observational study was a SPARCC score of 0.
Patients were a mean of 61 years, with a mean disease duration of 2.5 years. The mean baseline SPARCC score was 4. The mean Psoriatic Area and Severity Score (PASI) was 3.
Patients’ arthritis symptoms responded equally well to both drugs, with similar marked decreases in tender and swollen joint counts. But there was a clear, significant between-group separation on the SPARCC score, with 71% of the ustekinumab group reaching a 0 compared to 38% of the TNF-inhibition group.
Ustekinumab also effected better skin clearance than TNF-inhibition, she said. Among the TNF-inhibition group, about 20% achieved a PASI 90 and 20%, a PASI 100. Among those taking ustekinumab, about 80% achieved a PASI 90 and 55% a PASI 100.
The data point the way to more stratified treatment approaches for PsA patients, where PsA that predominantly involves enthesitis is treated by drugs like ustekinumab, Dr. Araujo said. Since both TNF-inhibitors and ustekinumab are approved for treatment of PsA, treatment could be tailored.
“Stratification of PsA patients according to clinical features (enthesitis driven vs. arthritis driven) appears within reach and will allow a more selective use of cytokine-blocking agents in PsA in the future,” said Dr. Araujo.
“More attention on enthesial-driven PsA patients is needed in the future as this patient group is well known to clinicians working in the PsA field but is massively underrepresented in clinical studies. Comparative studies of biological [disease-modifying antirheumatic drugs] in PsA need to take into account the differences in the clinical profile of PsA patients and should not be confined to the traditional polyarticular arthritis–driven disease population,” she added.
Dr. Araujo had no financial disclosures.
[email protected]
On Twitter @Alz_gal
MADRID – The anti-IL-23 antibody ustekinumab cleared enthesitis significantly better than did TNF-blockade in a small, open-label trial of patients with psoriatic arthritis
After 6 months on the drug, 71% of those taking the antibody achieved a score of 0 on the Spondyloarthritis Research Consortium of Canada (SPARCC) scale, representing a complete absence of enthesitis, Elizabeth Araujo, MD, said at the European Congress of Rheumatology. Just 38% of those on TNF-inhibitors achieved that score.
Enthesitis is often more bothersome to arthritis patients than their primary disease, said Dr. Araujo of the Centre of Internal Medicine, Universitätsklinikum Erlangen, Germany.
“Despite being a hallmark of PsA patients, enthesitis still receives rather peripheral attention as an outcome, especially when compared with ‘classical’ arthritis. Nonetheless, in clinical practice, enthesitis is an important factor for PsA-associated pain in many patients,” explained Dr. Araujo.
Yet it’s frequently ignored or under-treated. When it is addressed, enthesitis is often treated using TNF-inhibitors. But recent increases in the treatment options for PsA patients got Dr. Araujo thinking that PsA patients with enthesitis might respond better to a different therapy.
She investigated this with the open-label ECLIPSA trial, which randomized 51 PsA patients (47 with active enthesitis) to a 6-month treatment regimen of ustekinumab or a TNF-inhibitor. The primary endpoint of the observational study was a SPARCC score of 0.
Patients were a mean of 61 years, with a mean disease duration of 2.5 years. The mean baseline SPARCC score was 4. The mean Psoriatic Area and Severity Score (PASI) was 3.
Patients’ arthritis symptoms responded equally well to both drugs, with similar marked decreases in tender and swollen joint counts. But there was a clear, significant between-group separation on the SPARCC score, with 71% of the ustekinumab group reaching a 0 compared to 38% of the TNF-inhibition group.
Ustekinumab also effected better skin clearance than TNF-inhibition, she said. Among the TNF-inhibition group, about 20% achieved a PASI 90 and 20%, a PASI 100. Among those taking ustekinumab, about 80% achieved a PASI 90 and 55% a PASI 100.
The data point the way to more stratified treatment approaches for PsA patients, where PsA that predominantly involves enthesitis is treated by drugs like ustekinumab, Dr. Araujo said. Since both TNF-inhibitors and ustekinumab are approved for treatment of PsA, treatment could be tailored.
“Stratification of PsA patients according to clinical features (enthesitis driven vs. arthritis driven) appears within reach and will allow a more selective use of cytokine-blocking agents in PsA in the future,” said Dr. Araujo.
“More attention on enthesial-driven PsA patients is needed in the future as this patient group is well known to clinicians working in the PsA field but is massively underrepresented in clinical studies. Comparative studies of biological [disease-modifying antirheumatic drugs] in PsA need to take into account the differences in the clinical profile of PsA patients and should not be confined to the traditional polyarticular arthritis–driven disease population,” she added.
Dr. Araujo had no financial disclosures.
[email protected]
On Twitter @Alz_gal
AT EULAR 2017
Key clinical point:
Major finding: After 6 months, 71% of those taking ustekinumab and 38% of those taking TNF-blockers achieved total enthesitis clearance.
Data source: The open-label trial randomized 51 patients - 47 of whom had active enthesitis.
Disclosures: Dr. Araujo had no financial disclosures.
Early literacy assessment tool shows promise for screening preschool children
SAN FRANCISCO – The 10-item Early Literary Assessment Tool (ELSAT) used during regular pediatrician appointments in the first 4 years of life has shown promise in screening preschool children for delayed literacy skills that could result in later reading problems, based on a pilot study conducted in the preschool setting.
ELSAT “can be completed by a clinician [in the primary care setting] in less than a minute and can be incorporated into the Reach Out and Read intervention. An important next step in our research is to study the feasibility of the ELSAT within primary care visits and obtain feedback from clinicians about the ease of administration and value to their practice,” said Sai N. Iyer, MD, a developmental-behavioral pediatric fellow at the University of California, San Diego.
The initial 40-item ELSAT addressed three key domains of early literacy skills: knowledge and awareness of printed words, knowledge of letters, and recognition of word sounds. The observational study had two phases. ELSAT was developed and refined in the pilot phase, with validation against three aforementioned reference measures in the validation phase. The process whittled the test down to 10 items, with the same three domains represented. Comparisons were between the individual measures and a composite of the three.
The 10-item ELSAT correlated with each of the reference measures and with the composite of the three measures of early literacy (Pearson’s correlation, 810; P less than .01; Cronbach’s alpha [a measure of internal consistency] of .852). A cut-off ELSAT score of less than or equal to 5 predicted a “below average” score in any of the three reference measures and identified delayed literacy with a sensitivity of 92% and an acceptable specificity of 64%, Dr. Iyer explained during her presentation at the Pediatric Academic Societies meeting.
Language skills acquired during the first few years of life in the home and preschool settings lay the path for the development of more sophisticated reading skills, including decoding and comprehension beginning in grade 1. “Research has shown that about 40% of children enter kindergarten behind their peers in important early literacy skills. This gap widens with time, and the cost of catching them up far exceeds the cost of screening and early intervention. Many studies have demonstrated that effective early interventions improve the long-term outcomes for children who are at risk for later reading failure. Children who are reading at a below grade level by 4th grade are unlikely to catch up. Low levels of literacy have an impact on later educational and employment opportunities and set up a cycle of social and economic disadvantage that can have transgenerational effects,” Dr. Iyer said.
While parent-completed questionnaires are a convenient way to perform developmental screening, they are limited by the health literacy of the parents and other factors. Furthermore, while some preschools perform assessments, not all children attend preschools. This prompted Dr. Iyer and colleagues to think about developing a more objective screening strategy, with which a clinician could do the brief assessment. “All preschool children do see their pediatrician/primary care provider for vaccinations that are required before kindergarten. This makes the primary care setting an ideal opportunity to screen these children,” said Dr. Iyer.
During the question-and-answer session, an attendee described the data concerning the dichotomy in the test results between the public and private preschools as “some of the most impressive and depressing I’ve seen in this area.”
In a later interview, Dr. Iyer commented that, while the results in the study were not entirely new or surprising, “it was remarkable that we were able to demonstrate such significant differences in a sample of children enrolled in a high-quality preschool. Without specific screening and intervention, these early literacy delays would go unrecognized and increase the risk of poor academic outcomes for these high-risk children. The children were all in some type of preschool environment. Throughout the country, there are many children from low-income families who are not able to access preschool education. Although we did not test these children in our study, it is likely that the gaps between these children and their more advantaged peers are even higher. The pediatrician’s office may be the only place for these children to receive early literacy screening and anticipatory guidance on reading readiness.”
The sponsor of the study was the University of California, San Diego. The study was funded by the 2015 Academic Pediatric Association Young Investigator Award and by Reach Out and Read. Dr. Iyer had no relevant financial disclosures to report.
SAN FRANCISCO – The 10-item Early Literary Assessment Tool (ELSAT) used during regular pediatrician appointments in the first 4 years of life has shown promise in screening preschool children for delayed literacy skills that could result in later reading problems, based on a pilot study conducted in the preschool setting.
ELSAT “can be completed by a clinician [in the primary care setting] in less than a minute and can be incorporated into the Reach Out and Read intervention. An important next step in our research is to study the feasibility of the ELSAT within primary care visits and obtain feedback from clinicians about the ease of administration and value to their practice,” said Sai N. Iyer, MD, a developmental-behavioral pediatric fellow at the University of California, San Diego.
The initial 40-item ELSAT addressed three key domains of early literacy skills: knowledge and awareness of printed words, knowledge of letters, and recognition of word sounds. The observational study had two phases. ELSAT was developed and refined in the pilot phase, with validation against three aforementioned reference measures in the validation phase. The process whittled the test down to 10 items, with the same three domains represented. Comparisons were between the individual measures and a composite of the three.
The 10-item ELSAT correlated with each of the reference measures and with the composite of the three measures of early literacy (Pearson’s correlation, 810; P less than .01; Cronbach’s alpha [a measure of internal consistency] of .852). A cut-off ELSAT score of less than or equal to 5 predicted a “below average” score in any of the three reference measures and identified delayed literacy with a sensitivity of 92% and an acceptable specificity of 64%, Dr. Iyer explained during her presentation at the Pediatric Academic Societies meeting.
Language skills acquired during the first few years of life in the home and preschool settings lay the path for the development of more sophisticated reading skills, including decoding and comprehension beginning in grade 1. “Research has shown that about 40% of children enter kindergarten behind their peers in important early literacy skills. This gap widens with time, and the cost of catching them up far exceeds the cost of screening and early intervention. Many studies have demonstrated that effective early interventions improve the long-term outcomes for children who are at risk for later reading failure. Children who are reading at a below grade level by 4th grade are unlikely to catch up. Low levels of literacy have an impact on later educational and employment opportunities and set up a cycle of social and economic disadvantage that can have transgenerational effects,” Dr. Iyer said.
While parent-completed questionnaires are a convenient way to perform developmental screening, they are limited by the health literacy of the parents and other factors. Furthermore, while some preschools perform assessments, not all children attend preschools. This prompted Dr. Iyer and colleagues to think about developing a more objective screening strategy, with which a clinician could do the brief assessment. “All preschool children do see their pediatrician/primary care provider for vaccinations that are required before kindergarten. This makes the primary care setting an ideal opportunity to screen these children,” said Dr. Iyer.
During the question-and-answer session, an attendee described the data concerning the dichotomy in the test results between the public and private preschools as “some of the most impressive and depressing I’ve seen in this area.”
In a later interview, Dr. Iyer commented that, while the results in the study were not entirely new or surprising, “it was remarkable that we were able to demonstrate such significant differences in a sample of children enrolled in a high-quality preschool. Without specific screening and intervention, these early literacy delays would go unrecognized and increase the risk of poor academic outcomes for these high-risk children. The children were all in some type of preschool environment. Throughout the country, there are many children from low-income families who are not able to access preschool education. Although we did not test these children in our study, it is likely that the gaps between these children and their more advantaged peers are even higher. The pediatrician’s office may be the only place for these children to receive early literacy screening and anticipatory guidance on reading readiness.”
The sponsor of the study was the University of California, San Diego. The study was funded by the 2015 Academic Pediatric Association Young Investigator Award and by Reach Out and Read. Dr. Iyer had no relevant financial disclosures to report.
SAN FRANCISCO – The 10-item Early Literary Assessment Tool (ELSAT) used during regular pediatrician appointments in the first 4 years of life has shown promise in screening preschool children for delayed literacy skills that could result in later reading problems, based on a pilot study conducted in the preschool setting.
ELSAT “can be completed by a clinician [in the primary care setting] in less than a minute and can be incorporated into the Reach Out and Read intervention. An important next step in our research is to study the feasibility of the ELSAT within primary care visits and obtain feedback from clinicians about the ease of administration and value to their practice,” said Sai N. Iyer, MD, a developmental-behavioral pediatric fellow at the University of California, San Diego.
The initial 40-item ELSAT addressed three key domains of early literacy skills: knowledge and awareness of printed words, knowledge of letters, and recognition of word sounds. The observational study had two phases. ELSAT was developed and refined in the pilot phase, with validation against three aforementioned reference measures in the validation phase. The process whittled the test down to 10 items, with the same three domains represented. Comparisons were between the individual measures and a composite of the three.
The 10-item ELSAT correlated with each of the reference measures and with the composite of the three measures of early literacy (Pearson’s correlation, 810; P less than .01; Cronbach’s alpha [a measure of internal consistency] of .852). A cut-off ELSAT score of less than or equal to 5 predicted a “below average” score in any of the three reference measures and identified delayed literacy with a sensitivity of 92% and an acceptable specificity of 64%, Dr. Iyer explained during her presentation at the Pediatric Academic Societies meeting.
Language skills acquired during the first few years of life in the home and preschool settings lay the path for the development of more sophisticated reading skills, including decoding and comprehension beginning in grade 1. “Research has shown that about 40% of children enter kindergarten behind their peers in important early literacy skills. This gap widens with time, and the cost of catching them up far exceeds the cost of screening and early intervention. Many studies have demonstrated that effective early interventions improve the long-term outcomes for children who are at risk for later reading failure. Children who are reading at a below grade level by 4th grade are unlikely to catch up. Low levels of literacy have an impact on later educational and employment opportunities and set up a cycle of social and economic disadvantage that can have transgenerational effects,” Dr. Iyer said.
While parent-completed questionnaires are a convenient way to perform developmental screening, they are limited by the health literacy of the parents and other factors. Furthermore, while some preschools perform assessments, not all children attend preschools. This prompted Dr. Iyer and colleagues to think about developing a more objective screening strategy, with which a clinician could do the brief assessment. “All preschool children do see their pediatrician/primary care provider for vaccinations that are required before kindergarten. This makes the primary care setting an ideal opportunity to screen these children,” said Dr. Iyer.
During the question-and-answer session, an attendee described the data concerning the dichotomy in the test results between the public and private preschools as “some of the most impressive and depressing I’ve seen in this area.”
In a later interview, Dr. Iyer commented that, while the results in the study were not entirely new or surprising, “it was remarkable that we were able to demonstrate such significant differences in a sample of children enrolled in a high-quality preschool. Without specific screening and intervention, these early literacy delays would go unrecognized and increase the risk of poor academic outcomes for these high-risk children. The children were all in some type of preschool environment. Throughout the country, there are many children from low-income families who are not able to access preschool education. Although we did not test these children in our study, it is likely that the gaps between these children and their more advantaged peers are even higher. The pediatrician’s office may be the only place for these children to receive early literacy screening and anticipatory guidance on reading readiness.”
The sponsor of the study was the University of California, San Diego. The study was funded by the 2015 Academic Pediatric Association Young Investigator Award and by Reach Out and Read. Dr. Iyer had no relevant financial disclosures to report.
AT PAS 2017
Key clinical point:
Major finding: The 10-item ELSAT correlated with each of the reference measures and with the composite of the three measures of early literacy (Pearson’s correlation, 810; P less than .01; Cronbach’s alpha [a measure of internal consistency] of .852).
Data source: An observational study of 54-month-old children in five public preschools (n = 61) and two private preschools (n = 35) in San Diego.
Disclosures: The sponsor of the study was the University of California, San Diego. The study was funded by the 2015 Academic Pediatric Association Young Investigator Award and by Reach Out and Read. Dr. Iyer had no relevant financial disclosures to report.
Caffeine therapy of VLBW neonates reduces later motor impairment
SAN FRANCISCO – The 11-year follow-up results of the Caffeine for Apnea of Prematurity randomized, placebo-controlled trial has established the benefits of methylated xanthine therapy in the form of caffeine for very-low-birth-weight (VLBW) neonates in lessening the risk of motor impairment.
“The latest findings bolster the value of caffeine therapy to address apnea of prematurity in VLBW neonates. The CAP trial has provided compelling evidence for the use of caffeine even before this latest finding of improved motor function at age 11 years,” said presenter and the CAP trial’s principal investigator Barbara Schmidt, MD, of McMaster University, Hamilton, Ont.
At least 5 of every 1,000 live-born babies are very premature with a VLBW. Up of 40% die or survive with lasting disabilities. One cause of mortality or disability is apnea. Apnea can be lessened by treatment with methylxanthines such as caffeine, she noted. However, at the time the CAP trial began, it was unclear whether the therapy posed a danger by worsening the damage caused by lack of oxygen.
“Very few studies have followed more recent cohorts of very preterm infants to middle school age. Therefore, it was difficult to anticipate actual rates of functional impairment, and the possible effect of caffeine on those rates,” said Dr. Schmidt.
As reported about a decade ago, the CAP trial involving VLBW infants randomized to caffeine therapy or placebo established the short-term safety and effectiveness of the therapy in terms of reducing cerebral palsy and cognitive delay (N Engl J Med. 2007;357:1893-902).
Follow-ups at 18 months and 5 years revealed the benefits of caffeine therapy in reducing the rates of bronchopulmonary dysplasia, severe retinopathy, and neurodevelopmental disability. The present follow-up data assessed academic performance, motor function, and behavior in 1,202 children with a median age of 11 years. Of these, 602 had received caffeine therapy and 600 had been randomized to the placebo group. Data at age 11 years was available for 457 and 463 of the children randomized to caffeine therapy or placebo, respectively.
The primary outcome was functional impairment, which was indicated by at least one of poor academic performance (with at least one standard score more than two standard deviations below the mean on the Wide Range Achievement Test, 4th edition), motor impairment (percentile rank of 5 or less on the Movement Assessment Battery for Children, Second Edition), and behavior problems (Total Problem T score more than two standard deviations above the mean on the Child Behavior Checklist).
Functional impairment was evident in 145 the 457 (32%) children who had received caffeine therapy and 174 of the 463 (38%) who had not. The rates of 32% and 38% were statistically similar (P = .07). In the individual functional outcomes, the caffeine and placebo groups also were similar in terms of poor academic performance (14% vs. 13%; P = .58) and behavior (11% vs. 8%, respectively; P = .22).
However, caffeine therapy was associated with a reduced risk of motor impairment at age 11 years, compared with those in the placebo group (20% vs. 28%, respectively; odds ratio [OR], 0.66; 95% confidence interval [CI], 0.48-0.90; P = .009). The number of children needed to treat to lessen motor impairment in one child was 13 (95% CI, 8-42).
“Caffeine therapy for apnea of prematurity did not significantly reduce the combined rate of academic, motor, and behavioral impairments at age 11 years. However, caffeine therapy reduced the risk of motor impairment 11 years later,” said Dr. Schmidt. Whether caffeine therapy using higher doses or longer treatment duration is equally risk free is uncertain and further studies, which are not planned, would be needed, she said.
These 11-year follow-up findings of the CAP trial were published online in JAMA Pediatrics (2017, Apr 24. doi: 10.1001/jamapediatrics.2017.0238).
The sponsor of study was McMaster University. The study was funded by the Canadian Institutes of Health Research and the National Health and Medical Research Council of Australia. Dr. Schmidt had no relevant financial disclosures to report.
SAN FRANCISCO – The 11-year follow-up results of the Caffeine for Apnea of Prematurity randomized, placebo-controlled trial has established the benefits of methylated xanthine therapy in the form of caffeine for very-low-birth-weight (VLBW) neonates in lessening the risk of motor impairment.
“The latest findings bolster the value of caffeine therapy to address apnea of prematurity in VLBW neonates. The CAP trial has provided compelling evidence for the use of caffeine even before this latest finding of improved motor function at age 11 years,” said presenter and the CAP trial’s principal investigator Barbara Schmidt, MD, of McMaster University, Hamilton, Ont.
At least 5 of every 1,000 live-born babies are very premature with a VLBW. Up of 40% die or survive with lasting disabilities. One cause of mortality or disability is apnea. Apnea can be lessened by treatment with methylxanthines such as caffeine, she noted. However, at the time the CAP trial began, it was unclear whether the therapy posed a danger by worsening the damage caused by lack of oxygen.
“Very few studies have followed more recent cohorts of very preterm infants to middle school age. Therefore, it was difficult to anticipate actual rates of functional impairment, and the possible effect of caffeine on those rates,” said Dr. Schmidt.
As reported about a decade ago, the CAP trial involving VLBW infants randomized to caffeine therapy or placebo established the short-term safety and effectiveness of the therapy in terms of reducing cerebral palsy and cognitive delay (N Engl J Med. 2007;357:1893-902).
Follow-ups at 18 months and 5 years revealed the benefits of caffeine therapy in reducing the rates of bronchopulmonary dysplasia, severe retinopathy, and neurodevelopmental disability. The present follow-up data assessed academic performance, motor function, and behavior in 1,202 children with a median age of 11 years. Of these, 602 had received caffeine therapy and 600 had been randomized to the placebo group. Data at age 11 years was available for 457 and 463 of the children randomized to caffeine therapy or placebo, respectively.
The primary outcome was functional impairment, which was indicated by at least one of poor academic performance (with at least one standard score more than two standard deviations below the mean on the Wide Range Achievement Test, 4th edition), motor impairment (percentile rank of 5 or less on the Movement Assessment Battery for Children, Second Edition), and behavior problems (Total Problem T score more than two standard deviations above the mean on the Child Behavior Checklist).
Functional impairment was evident in 145 the 457 (32%) children who had received caffeine therapy and 174 of the 463 (38%) who had not. The rates of 32% and 38% were statistically similar (P = .07). In the individual functional outcomes, the caffeine and placebo groups also were similar in terms of poor academic performance (14% vs. 13%; P = .58) and behavior (11% vs. 8%, respectively; P = .22).
However, caffeine therapy was associated with a reduced risk of motor impairment at age 11 years, compared with those in the placebo group (20% vs. 28%, respectively; odds ratio [OR], 0.66; 95% confidence interval [CI], 0.48-0.90; P = .009). The number of children needed to treat to lessen motor impairment in one child was 13 (95% CI, 8-42).
“Caffeine therapy for apnea of prematurity did not significantly reduce the combined rate of academic, motor, and behavioral impairments at age 11 years. However, caffeine therapy reduced the risk of motor impairment 11 years later,” said Dr. Schmidt. Whether caffeine therapy using higher doses or longer treatment duration is equally risk free is uncertain and further studies, which are not planned, would be needed, she said.
These 11-year follow-up findings of the CAP trial were published online in JAMA Pediatrics (2017, Apr 24. doi: 10.1001/jamapediatrics.2017.0238).
The sponsor of study was McMaster University. The study was funded by the Canadian Institutes of Health Research and the National Health and Medical Research Council of Australia. Dr. Schmidt had no relevant financial disclosures to report.
SAN FRANCISCO – The 11-year follow-up results of the Caffeine for Apnea of Prematurity randomized, placebo-controlled trial has established the benefits of methylated xanthine therapy in the form of caffeine for very-low-birth-weight (VLBW) neonates in lessening the risk of motor impairment.
“The latest findings bolster the value of caffeine therapy to address apnea of prematurity in VLBW neonates. The CAP trial has provided compelling evidence for the use of caffeine even before this latest finding of improved motor function at age 11 years,” said presenter and the CAP trial’s principal investigator Barbara Schmidt, MD, of McMaster University, Hamilton, Ont.
At least 5 of every 1,000 live-born babies are very premature with a VLBW. Up of 40% die or survive with lasting disabilities. One cause of mortality or disability is apnea. Apnea can be lessened by treatment with methylxanthines such as caffeine, she noted. However, at the time the CAP trial began, it was unclear whether the therapy posed a danger by worsening the damage caused by lack of oxygen.
“Very few studies have followed more recent cohorts of very preterm infants to middle school age. Therefore, it was difficult to anticipate actual rates of functional impairment, and the possible effect of caffeine on those rates,” said Dr. Schmidt.
As reported about a decade ago, the CAP trial involving VLBW infants randomized to caffeine therapy or placebo established the short-term safety and effectiveness of the therapy in terms of reducing cerebral palsy and cognitive delay (N Engl J Med. 2007;357:1893-902).
Follow-ups at 18 months and 5 years revealed the benefits of caffeine therapy in reducing the rates of bronchopulmonary dysplasia, severe retinopathy, and neurodevelopmental disability. The present follow-up data assessed academic performance, motor function, and behavior in 1,202 children with a median age of 11 years. Of these, 602 had received caffeine therapy and 600 had been randomized to the placebo group. Data at age 11 years was available for 457 and 463 of the children randomized to caffeine therapy or placebo, respectively.
The primary outcome was functional impairment, which was indicated by at least one of poor academic performance (with at least one standard score more than two standard deviations below the mean on the Wide Range Achievement Test, 4th edition), motor impairment (percentile rank of 5 or less on the Movement Assessment Battery for Children, Second Edition), and behavior problems (Total Problem T score more than two standard deviations above the mean on the Child Behavior Checklist).
Functional impairment was evident in 145 the 457 (32%) children who had received caffeine therapy and 174 of the 463 (38%) who had not. The rates of 32% and 38% were statistically similar (P = .07). In the individual functional outcomes, the caffeine and placebo groups also were similar in terms of poor academic performance (14% vs. 13%; P = .58) and behavior (11% vs. 8%, respectively; P = .22).
However, caffeine therapy was associated with a reduced risk of motor impairment at age 11 years, compared with those in the placebo group (20% vs. 28%, respectively; odds ratio [OR], 0.66; 95% confidence interval [CI], 0.48-0.90; P = .009). The number of children needed to treat to lessen motor impairment in one child was 13 (95% CI, 8-42).
“Caffeine therapy for apnea of prematurity did not significantly reduce the combined rate of academic, motor, and behavioral impairments at age 11 years. However, caffeine therapy reduced the risk of motor impairment 11 years later,” said Dr. Schmidt. Whether caffeine therapy using higher doses or longer treatment duration is equally risk free is uncertain and further studies, which are not planned, would be needed, she said.
These 11-year follow-up findings of the CAP trial were published online in JAMA Pediatrics (2017, Apr 24. doi: 10.1001/jamapediatrics.2017.0238).
The sponsor of study was McMaster University. The study was funded by the Canadian Institutes of Health Research and the National Health and Medical Research Council of Australia. Dr. Schmidt had no relevant financial disclosures to report.
AT PAS 17
Key clinical point:
Major finding: At the 11-year follow-up, motor impairment was identified in 20% of those who received caffeine therapy versus 28% of those in the placebo group (P = .009).
Data source: Multicenter, randomized, placebo-controlled trial (NCT00182312).
Disclosures: The sponsor of study was McMaster University. The study was funded by the Canadian Institutes of Health Research and the National Health and Medical Research Council of Australia. Dr. Schmidt had no relevant financial disclosures to report.
Drainage, irrigation, and fibrinolytic therapy held safe, effective for PHVD
SAN FRANCISCO – The 10-year follow-up of neonates treated for posthemorrhagic ventricular dilatation (PHVD) has demonstrated the long-term success of drainage, irrigation, and fibrinolytic therapy (DRIFT), with a cognitive advantage in the now school-age children evident, compared with those neonates who had not received the therapy.
“Children in the DRIFT group had a 23-point cognitive quotient advantage and were nine times more likely to be alive without severe cognitive disability at 10 years,” presenter and DRIFT investigator Karen Luyt, MBChB, PhD, of the University of Bristol and St. Michael’s Hospital, Bristol, England, said at the Pediatric Academic Societies meeting.
PHVD carries a high risk of disabilities in cognition and movement. DRIFT was developed as a way to wash out the ventricles in the brain to clear the effects of bleeding, with the goal of reducing neurodevelopmental disability. In the technique, catheters are inserted into the affected ventricles and are used to deliver an anti-clotting agent (alteplase) and to drain the bloody fluid. The catheters remain in place for a time as a conduit for artificial cerebrospinal fluid (CSF) containing antibiotics.
In the DRIFT trial, 77 preterm infants were randomized to DRIFT (n = 39) or the standard treatment of siphoning off cerebrospinal fluid to restrict brain expansion (n = 38). At 2 years, the DRIFT group displayed fewer cases of severe disability and cognitive disability, and death (Pediatrics. 2010 Apr;125[4]:e852-8).
Dr. Luyt summarized the final 10-year data from 52 school-age children (28 treated using DRIFT and 24 treated in the standard manner). The primary outcomes in the school-age children were cognitive quotient (CQ) and survival without severe cognitive disability. Secondary outcomes included visual function, sensory and motor disabilities, and emotional or behavior problems.
The age at the time of treatment randomization was 19 days in the DRIFT group and 19 days in the standard group. The DRIFT group was composed of more males (79% vs. 63%) and newborns with lower birth weight (336 vs. 535 grams). The gestational age and the prevalence of grade 4 intraventricular hemorrhage were similar between the groups.
DRIFT increased cognitive ability at 10 years (P = .096). Adjustment for gender, birth weight, and grade of intraventricular hemorrhage strengthened this association, with the DRIFT group having an average advantage in CQ score of 23.5 points (P = .009), which translated to a 2.5-year advantage in cognitive ability. When the data was further adjusted by ruling out the three children (two in the DRIFT group and one in the standard treatment group) who died between the 2- and 10-year follow-ups, the CQ score advantage remained (20 points; P = .029).
The other primary outcome of survival without severe cognitive disability also favored DRIFT, with an unadjusted odds ratio (OR) of 3.3 (95% confidence interval [CI] 1.1-10.4 (P = .037) and adjusted (as above) OR of 8.9 (95% CI, 1.9-42.3; P = .006). Fewer children in the DRIFT group were attending schools with an expertise in special needs (OR, 0.27; 95% CI, 0.07-1.05; P = .059). No differences between the groups were evident for the secondary outcomes.
The number needed to treat to prevent death or severe cognitive disability was four.
Dr. Luyt’s recommendation that DRIFT become the standard of care for neonatal intraventricular hemorrhage comes with the caveat of increased secondary bleeding, which caused the trial to be halted after a planned external safety monitoring review. Children who already had been treated were followed up, with no further recruitment. In her response to a question from the audience regarding her endorsement of DRIFT despite the trial’s halt, Dr. Luyt pointed to the comparable safety profiles of the two groups, the superior outcomes in the DRIFT group, and the knowledge that modifications made to the technique in the intervening years have reduced the possibility of secondary bleeds.
The sponsor of study was Dr. Birgit Whitman of the University of Bristol. The study was funded by the National Institute of Health’s Health Technology Assessment Programme. Dr. Luyt disclosed the off-label use of alteplase.
SAN FRANCISCO – The 10-year follow-up of neonates treated for posthemorrhagic ventricular dilatation (PHVD) has demonstrated the long-term success of drainage, irrigation, and fibrinolytic therapy (DRIFT), with a cognitive advantage in the now school-age children evident, compared with those neonates who had not received the therapy.
“Children in the DRIFT group had a 23-point cognitive quotient advantage and were nine times more likely to be alive without severe cognitive disability at 10 years,” presenter and DRIFT investigator Karen Luyt, MBChB, PhD, of the University of Bristol and St. Michael’s Hospital, Bristol, England, said at the Pediatric Academic Societies meeting.
PHVD carries a high risk of disabilities in cognition and movement. DRIFT was developed as a way to wash out the ventricles in the brain to clear the effects of bleeding, with the goal of reducing neurodevelopmental disability. In the technique, catheters are inserted into the affected ventricles and are used to deliver an anti-clotting agent (alteplase) and to drain the bloody fluid. The catheters remain in place for a time as a conduit for artificial cerebrospinal fluid (CSF) containing antibiotics.
In the DRIFT trial, 77 preterm infants were randomized to DRIFT (n = 39) or the standard treatment of siphoning off cerebrospinal fluid to restrict brain expansion (n = 38). At 2 years, the DRIFT group displayed fewer cases of severe disability and cognitive disability, and death (Pediatrics. 2010 Apr;125[4]:e852-8).
Dr. Luyt summarized the final 10-year data from 52 school-age children (28 treated using DRIFT and 24 treated in the standard manner). The primary outcomes in the school-age children were cognitive quotient (CQ) and survival without severe cognitive disability. Secondary outcomes included visual function, sensory and motor disabilities, and emotional or behavior problems.
The age at the time of treatment randomization was 19 days in the DRIFT group and 19 days in the standard group. The DRIFT group was composed of more males (79% vs. 63%) and newborns with lower birth weight (336 vs. 535 grams). The gestational age and the prevalence of grade 4 intraventricular hemorrhage were similar between the groups.
DRIFT increased cognitive ability at 10 years (P = .096). Adjustment for gender, birth weight, and grade of intraventricular hemorrhage strengthened this association, with the DRIFT group having an average advantage in CQ score of 23.5 points (P = .009), which translated to a 2.5-year advantage in cognitive ability. When the data was further adjusted by ruling out the three children (two in the DRIFT group and one in the standard treatment group) who died between the 2- and 10-year follow-ups, the CQ score advantage remained (20 points; P = .029).
The other primary outcome of survival without severe cognitive disability also favored DRIFT, with an unadjusted odds ratio (OR) of 3.3 (95% confidence interval [CI] 1.1-10.4 (P = .037) and adjusted (as above) OR of 8.9 (95% CI, 1.9-42.3; P = .006). Fewer children in the DRIFT group were attending schools with an expertise in special needs (OR, 0.27; 95% CI, 0.07-1.05; P = .059). No differences between the groups were evident for the secondary outcomes.
The number needed to treat to prevent death or severe cognitive disability was four.
Dr. Luyt’s recommendation that DRIFT become the standard of care for neonatal intraventricular hemorrhage comes with the caveat of increased secondary bleeding, which caused the trial to be halted after a planned external safety monitoring review. Children who already had been treated were followed up, with no further recruitment. In her response to a question from the audience regarding her endorsement of DRIFT despite the trial’s halt, Dr. Luyt pointed to the comparable safety profiles of the two groups, the superior outcomes in the DRIFT group, and the knowledge that modifications made to the technique in the intervening years have reduced the possibility of secondary bleeds.
The sponsor of study was Dr. Birgit Whitman of the University of Bristol. The study was funded by the National Institute of Health’s Health Technology Assessment Programme. Dr. Luyt disclosed the off-label use of alteplase.
SAN FRANCISCO – The 10-year follow-up of neonates treated for posthemorrhagic ventricular dilatation (PHVD) has demonstrated the long-term success of drainage, irrigation, and fibrinolytic therapy (DRIFT), with a cognitive advantage in the now school-age children evident, compared with those neonates who had not received the therapy.
“Children in the DRIFT group had a 23-point cognitive quotient advantage and were nine times more likely to be alive without severe cognitive disability at 10 years,” presenter and DRIFT investigator Karen Luyt, MBChB, PhD, of the University of Bristol and St. Michael’s Hospital, Bristol, England, said at the Pediatric Academic Societies meeting.
PHVD carries a high risk of disabilities in cognition and movement. DRIFT was developed as a way to wash out the ventricles in the brain to clear the effects of bleeding, with the goal of reducing neurodevelopmental disability. In the technique, catheters are inserted into the affected ventricles and are used to deliver an anti-clotting agent (alteplase) and to drain the bloody fluid. The catheters remain in place for a time as a conduit for artificial cerebrospinal fluid (CSF) containing antibiotics.
In the DRIFT trial, 77 preterm infants were randomized to DRIFT (n = 39) or the standard treatment of siphoning off cerebrospinal fluid to restrict brain expansion (n = 38). At 2 years, the DRIFT group displayed fewer cases of severe disability and cognitive disability, and death (Pediatrics. 2010 Apr;125[4]:e852-8).
Dr. Luyt summarized the final 10-year data from 52 school-age children (28 treated using DRIFT and 24 treated in the standard manner). The primary outcomes in the school-age children were cognitive quotient (CQ) and survival without severe cognitive disability. Secondary outcomes included visual function, sensory and motor disabilities, and emotional or behavior problems.
The age at the time of treatment randomization was 19 days in the DRIFT group and 19 days in the standard group. The DRIFT group was composed of more males (79% vs. 63%) and newborns with lower birth weight (336 vs. 535 grams). The gestational age and the prevalence of grade 4 intraventricular hemorrhage were similar between the groups.
DRIFT increased cognitive ability at 10 years (P = .096). Adjustment for gender, birth weight, and grade of intraventricular hemorrhage strengthened this association, with the DRIFT group having an average advantage in CQ score of 23.5 points (P = .009), which translated to a 2.5-year advantage in cognitive ability. When the data was further adjusted by ruling out the three children (two in the DRIFT group and one in the standard treatment group) who died between the 2- and 10-year follow-ups, the CQ score advantage remained (20 points; P = .029).
The other primary outcome of survival without severe cognitive disability also favored DRIFT, with an unadjusted odds ratio (OR) of 3.3 (95% confidence interval [CI] 1.1-10.4 (P = .037) and adjusted (as above) OR of 8.9 (95% CI, 1.9-42.3; P = .006). Fewer children in the DRIFT group were attending schools with an expertise in special needs (OR, 0.27; 95% CI, 0.07-1.05; P = .059). No differences between the groups were evident for the secondary outcomes.
The number needed to treat to prevent death or severe cognitive disability was four.
Dr. Luyt’s recommendation that DRIFT become the standard of care for neonatal intraventricular hemorrhage comes with the caveat of increased secondary bleeding, which caused the trial to be halted after a planned external safety monitoring review. Children who already had been treated were followed up, with no further recruitment. In her response to a question from the audience regarding her endorsement of DRIFT despite the trial’s halt, Dr. Luyt pointed to the comparable safety profiles of the two groups, the superior outcomes in the DRIFT group, and the knowledge that modifications made to the technique in the intervening years have reduced the possibility of secondary bleeds.
The sponsor of study was Dr. Birgit Whitman of the University of Bristol. The study was funded by the National Institute of Health’s Health Technology Assessment Programme. Dr. Luyt disclosed the off-label use of alteplase.
AT PAS 17
Key clinical point: The 10-year follow-up data from the Drainage, Irrigation, and Fibrinolytic Therapy (DRIFT) study has confirmed the long-term safety and effectiveness of the intervention in treatment of preterm intraventricular hemorrhage.
Major finding: The DRIFT group had an average advantage in cognitive quotient score of 23.5 points (P = .009), translating to a 2.5 year advantage in cognitive ability.
Data source: Randomized controlled trial of 52 10-year-old children from the DRIFT study.
Disclosures: The sponsor of study was Dr. Birgit Whitman of the University of Bristol. The study was funded by the National Institute of Health’s Health Technology Assessment Programme. Dr. Luyt disclosed the off-label use of alteplase.
GI disorders more prevalent in children with poorly controlled asthma
SAN FRANCISCO – Pediatric patients who have asthma that is poorly controlled may be more likely to have functional gastrointestinal (GI) disorders, which feature chronic GI distress that has several causes, according to a study of patients treated at one hospital.
Female sex and increased anxiety were influential factors.
“This study suggests a high prevalence of functional GI disorders among patients with persistent asthma. Moreover, patients with functional GI disorders had poor asthma control and increased anxiety. Clinicians should consider functional GI disorders in patients with poor asthma control and assess for anxiety as indicated,” Ruben J. Colman, MD, a pediatric resident at SBH Health System, Bronx, N.Y., said at the Pediatric Academic Societies meeting.
Functional GI disorders including functional abdominal pain, irritable bowel syndrome, and functional dyspepsia were evaluated. The study was prompted by the knowledge that these conditions are a common cause of chronic GI symptoms in children, and from the findings of a retrospective study of 30,000 patients in Europe that reported a higher prevalence of asthma in those with functional GI disorders, compared with those without chronic GI distress (Aliment Pharmacol Ther. 2014 Aug;40[40]:382-91). Data are scarce in North America concerning asthma control and functional GI disorders in both pediatric and adult populations.
The validated Questionnaire on Pediatric Gastrointestinal Symptoms–Rome III version was used to assess functional GI disorders. Asthma control was assessed using the childhood Asthma Control Test (ACT) questionnaire, with scores exceeding 30, less than 19, and less than 14 indicating well-controlled, not well-controlled, and poorly controlled asthma, respectively. Anxiety was assessed using the Beck Anxiety Inventory, with increasing scores indicating increasing anxiety.
The 110 enrolled patients had a mean age of 10 years. Age was similar between the 18 patients with functional GI disorders – representing a prevalence rate of 16% – and the 92 without such disorders at 12 and 10 years, respectively. Those with functional GI disorders were predominantly female, compared with the patients without a functional GI disorder (72% vs 45%; P less than .03). The GI distress in the 18 patients comprised 10 cases of abdominal pain disorders and 13 cases of upper GI tract disorders, with 3 patients having an overlap of 2 to 3 functional GI disorders.
Patients with functional GI disorders had a lower mean ACT score, compared with those without (12 vs. 15; P = .03). Functional GI disorders also were associated with higher anxiety scores (34 vs. 14; P less than .01).
Asthma control significantly predicted the presence of functional GI disorders in univariate analysis (odds ratio, 0.9; 95% confidence interval, 0.80-0.99; P = .03). However, this significance was lost in a multivariate analysis that adjusted for asthma control, anxiety, and sex. The multivariate analysis revealed continued significant associations between functional GI disorders and anxiety (OR, 1.1; 95% CI, 1.01-1.10; P less than .01) and female sex (OR, 3.3; 95% CI, 1.00-10.56; P less than .05).
Dr. Colman speculated that the apparent association of asthma with chronic GI distress could reflect asthma-related inflammation that exacerbates the GI disorders. Future research should examine if improving the control of asthma and lessening anxiety can decrease symptoms of functional GI disorders.
SAN FRANCISCO – Pediatric patients who have asthma that is poorly controlled may be more likely to have functional gastrointestinal (GI) disorders, which feature chronic GI distress that has several causes, according to a study of patients treated at one hospital.
Female sex and increased anxiety were influential factors.
“This study suggests a high prevalence of functional GI disorders among patients with persistent asthma. Moreover, patients with functional GI disorders had poor asthma control and increased anxiety. Clinicians should consider functional GI disorders in patients with poor asthma control and assess for anxiety as indicated,” Ruben J. Colman, MD, a pediatric resident at SBH Health System, Bronx, N.Y., said at the Pediatric Academic Societies meeting.
Functional GI disorders including functional abdominal pain, irritable bowel syndrome, and functional dyspepsia were evaluated. The study was prompted by the knowledge that these conditions are a common cause of chronic GI symptoms in children, and from the findings of a retrospective study of 30,000 patients in Europe that reported a higher prevalence of asthma in those with functional GI disorders, compared with those without chronic GI distress (Aliment Pharmacol Ther. 2014 Aug;40[40]:382-91). Data are scarce in North America concerning asthma control and functional GI disorders in both pediatric and adult populations.
The validated Questionnaire on Pediatric Gastrointestinal Symptoms–Rome III version was used to assess functional GI disorders. Asthma control was assessed using the childhood Asthma Control Test (ACT) questionnaire, with scores exceeding 30, less than 19, and less than 14 indicating well-controlled, not well-controlled, and poorly controlled asthma, respectively. Anxiety was assessed using the Beck Anxiety Inventory, with increasing scores indicating increasing anxiety.
The 110 enrolled patients had a mean age of 10 years. Age was similar between the 18 patients with functional GI disorders – representing a prevalence rate of 16% – and the 92 without such disorders at 12 and 10 years, respectively. Those with functional GI disorders were predominantly female, compared with the patients without a functional GI disorder (72% vs 45%; P less than .03). The GI distress in the 18 patients comprised 10 cases of abdominal pain disorders and 13 cases of upper GI tract disorders, with 3 patients having an overlap of 2 to 3 functional GI disorders.
Patients with functional GI disorders had a lower mean ACT score, compared with those without (12 vs. 15; P = .03). Functional GI disorders also were associated with higher anxiety scores (34 vs. 14; P less than .01).
Asthma control significantly predicted the presence of functional GI disorders in univariate analysis (odds ratio, 0.9; 95% confidence interval, 0.80-0.99; P = .03). However, this significance was lost in a multivariate analysis that adjusted for asthma control, anxiety, and sex. The multivariate analysis revealed continued significant associations between functional GI disorders and anxiety (OR, 1.1; 95% CI, 1.01-1.10; P less than .01) and female sex (OR, 3.3; 95% CI, 1.00-10.56; P less than .05).
Dr. Colman speculated that the apparent association of asthma with chronic GI distress could reflect asthma-related inflammation that exacerbates the GI disorders. Future research should examine if improving the control of asthma and lessening anxiety can decrease symptoms of functional GI disorders.
SAN FRANCISCO – Pediatric patients who have asthma that is poorly controlled may be more likely to have functional gastrointestinal (GI) disorders, which feature chronic GI distress that has several causes, according to a study of patients treated at one hospital.
Female sex and increased anxiety were influential factors.
“This study suggests a high prevalence of functional GI disorders among patients with persistent asthma. Moreover, patients with functional GI disorders had poor asthma control and increased anxiety. Clinicians should consider functional GI disorders in patients with poor asthma control and assess for anxiety as indicated,” Ruben J. Colman, MD, a pediatric resident at SBH Health System, Bronx, N.Y., said at the Pediatric Academic Societies meeting.
Functional GI disorders including functional abdominal pain, irritable bowel syndrome, and functional dyspepsia were evaluated. The study was prompted by the knowledge that these conditions are a common cause of chronic GI symptoms in children, and from the findings of a retrospective study of 30,000 patients in Europe that reported a higher prevalence of asthma in those with functional GI disorders, compared with those without chronic GI distress (Aliment Pharmacol Ther. 2014 Aug;40[40]:382-91). Data are scarce in North America concerning asthma control and functional GI disorders in both pediatric and adult populations.
The validated Questionnaire on Pediatric Gastrointestinal Symptoms–Rome III version was used to assess functional GI disorders. Asthma control was assessed using the childhood Asthma Control Test (ACT) questionnaire, with scores exceeding 30, less than 19, and less than 14 indicating well-controlled, not well-controlled, and poorly controlled asthma, respectively. Anxiety was assessed using the Beck Anxiety Inventory, with increasing scores indicating increasing anxiety.
The 110 enrolled patients had a mean age of 10 years. Age was similar between the 18 patients with functional GI disorders – representing a prevalence rate of 16% – and the 92 without such disorders at 12 and 10 years, respectively. Those with functional GI disorders were predominantly female, compared with the patients without a functional GI disorder (72% vs 45%; P less than .03). The GI distress in the 18 patients comprised 10 cases of abdominal pain disorders and 13 cases of upper GI tract disorders, with 3 patients having an overlap of 2 to 3 functional GI disorders.
Patients with functional GI disorders had a lower mean ACT score, compared with those without (12 vs. 15; P = .03). Functional GI disorders also were associated with higher anxiety scores (34 vs. 14; P less than .01).
Asthma control significantly predicted the presence of functional GI disorders in univariate analysis (odds ratio, 0.9; 95% confidence interval, 0.80-0.99; P = .03). However, this significance was lost in a multivariate analysis that adjusted for asthma control, anxiety, and sex. The multivariate analysis revealed continued significant associations between functional GI disorders and anxiety (OR, 1.1; 95% CI, 1.01-1.10; P less than .01) and female sex (OR, 3.3; 95% CI, 1.00-10.56; P less than .05).
Dr. Colman speculated that the apparent association of asthma with chronic GI distress could reflect asthma-related inflammation that exacerbates the GI disorders. Future research should examine if improving the control of asthma and lessening anxiety can decrease symptoms of functional GI disorders.
AT PAS 17
Key clinical point: The prevalence of functional gastrointestinal disorders is high in pediatric patients with poorly controlled asthma.
Major finding:
Data source: Prospective cross-sectional study at one institution.
Disclosures: The sponsor of the study was SBH Health System. The study was not funded. Dr. Colman had no conflicts to report.
Immunization requirements, availability vary in U.S. universities
SAN FRANCISCO – in the enrollment process and vaccine availability through on-campus student health.
The policies of the institutions usually reflected the policies of the particular state or district.
The cross-sectional study surveyed two private and two publicly-funded 4-year degree-granting colleges or universities in each state and the District of Columbia – 216 institutions in total. The institutions were randomly selected to reflect the diversities in size, religious affiliations, and type of institution. The institutions’ websites were scrutinized for information on immunization requirements, vaccinations needed prior to enrollment, vaccination options available on-campus, and consequence of failure to obtain the necessary vaccinations.
A wide variation in vaccine requirements and on-campus availability was evident. MMR vaccination was an admission requirement of about 82% of the schools surveyed. Vaccination was best done prior to arrival on campus, as only 42% of the surveyed colleges and universities offered the vaccine through student health. Vaccination for hepatitis B was required by only 31% of colleges/universities, with 44% offering the vaccine through student health. Vaccination for hepatitis A was required by only about 1% of the surveyed institutions, although the vaccine was available on one-third of the campuses, Dr. Feemster said at the Pediatric Academic Societies annual meeting.
Meningococcal B (MenB) vaccination was required by 25 schools, of which 6 (24%) had experienced MenB illness outbreaks. Of the 191 schools that did not have a requirement for MenB vaccination, only 4 (2.0%) had experienced a MenB outbreak.
Of contemporary concern, vaccination for human papillomavirus was offered by one-third of the colleges/universities, but this vaccination was not a requirement for admission to any of the surveyed institutions. Vaccination for influenza, another disease with a high propensity to spread, also was not required by any school, with only 37% having influenza vaccination available as part of student health care.
Compliance with immunization requirements was enforced by 67% of the schools, with course registration not finalized until the necessary vaccinations had been received and documented. Of the 17% of schools that did not have an enforcement policy, 61% cited the vaccine requirements of their particular state, the assumption being that the incoming students from that state would have received the necessary vaccinations, reflecting a more reactive than proactive stance, according to Dr. Feemster. There was no difference in enforcement strategy between the public or private institutions.
Of the surveyed vaccines, at least some were available at just over 91% of the public institutions and at 76% of the private institutions
“The variation in requirements and enforcement suggest inconsistent vaccine uptake. Next steps include a mixed-methods study to measure attitudes, beliefs, and behaviors related to school vaccine policy among a national sample of college students and to identify facilitators and barriers to school vaccine policy implementation among school health administrators and providers,” said Dr. Feemster.
“The ultimate goal is to identify the best practices for implementation of college vaccine policies to optimize vaccine uptake and increase positive attitudes, beliefs, and future intentions about vaccines,” she added.
The sponsor of study was the Children’s Hospital of Philadelphia. The study was not funded. Dr. Feemster had no conflicts to disclose.
SAN FRANCISCO – in the enrollment process and vaccine availability through on-campus student health.
The policies of the institutions usually reflected the policies of the particular state or district.
The cross-sectional study surveyed two private and two publicly-funded 4-year degree-granting colleges or universities in each state and the District of Columbia – 216 institutions in total. The institutions were randomly selected to reflect the diversities in size, religious affiliations, and type of institution. The institutions’ websites were scrutinized for information on immunization requirements, vaccinations needed prior to enrollment, vaccination options available on-campus, and consequence of failure to obtain the necessary vaccinations.
A wide variation in vaccine requirements and on-campus availability was evident. MMR vaccination was an admission requirement of about 82% of the schools surveyed. Vaccination was best done prior to arrival on campus, as only 42% of the surveyed colleges and universities offered the vaccine through student health. Vaccination for hepatitis B was required by only 31% of colleges/universities, with 44% offering the vaccine through student health. Vaccination for hepatitis A was required by only about 1% of the surveyed institutions, although the vaccine was available on one-third of the campuses, Dr. Feemster said at the Pediatric Academic Societies annual meeting.
Meningococcal B (MenB) vaccination was required by 25 schools, of which 6 (24%) had experienced MenB illness outbreaks. Of the 191 schools that did not have a requirement for MenB vaccination, only 4 (2.0%) had experienced a MenB outbreak.
Of contemporary concern, vaccination for human papillomavirus was offered by one-third of the colleges/universities, but this vaccination was not a requirement for admission to any of the surveyed institutions. Vaccination for influenza, another disease with a high propensity to spread, also was not required by any school, with only 37% having influenza vaccination available as part of student health care.
Compliance with immunization requirements was enforced by 67% of the schools, with course registration not finalized until the necessary vaccinations had been received and documented. Of the 17% of schools that did not have an enforcement policy, 61% cited the vaccine requirements of their particular state, the assumption being that the incoming students from that state would have received the necessary vaccinations, reflecting a more reactive than proactive stance, according to Dr. Feemster. There was no difference in enforcement strategy between the public or private institutions.
Of the surveyed vaccines, at least some were available at just over 91% of the public institutions and at 76% of the private institutions
“The variation in requirements and enforcement suggest inconsistent vaccine uptake. Next steps include a mixed-methods study to measure attitudes, beliefs, and behaviors related to school vaccine policy among a national sample of college students and to identify facilitators and barriers to school vaccine policy implementation among school health administrators and providers,” said Dr. Feemster.
“The ultimate goal is to identify the best practices for implementation of college vaccine policies to optimize vaccine uptake and increase positive attitudes, beliefs, and future intentions about vaccines,” she added.
The sponsor of study was the Children’s Hospital of Philadelphia. The study was not funded. Dr. Feemster had no conflicts to disclose.
SAN FRANCISCO – in the enrollment process and vaccine availability through on-campus student health.
The policies of the institutions usually reflected the policies of the particular state or district.
The cross-sectional study surveyed two private and two publicly-funded 4-year degree-granting colleges or universities in each state and the District of Columbia – 216 institutions in total. The institutions were randomly selected to reflect the diversities in size, religious affiliations, and type of institution. The institutions’ websites were scrutinized for information on immunization requirements, vaccinations needed prior to enrollment, vaccination options available on-campus, and consequence of failure to obtain the necessary vaccinations.
A wide variation in vaccine requirements and on-campus availability was evident. MMR vaccination was an admission requirement of about 82% of the schools surveyed. Vaccination was best done prior to arrival on campus, as only 42% of the surveyed colleges and universities offered the vaccine through student health. Vaccination for hepatitis B was required by only 31% of colleges/universities, with 44% offering the vaccine through student health. Vaccination for hepatitis A was required by only about 1% of the surveyed institutions, although the vaccine was available on one-third of the campuses, Dr. Feemster said at the Pediatric Academic Societies annual meeting.
Meningococcal B (MenB) vaccination was required by 25 schools, of which 6 (24%) had experienced MenB illness outbreaks. Of the 191 schools that did not have a requirement for MenB vaccination, only 4 (2.0%) had experienced a MenB outbreak.
Of contemporary concern, vaccination for human papillomavirus was offered by one-third of the colleges/universities, but this vaccination was not a requirement for admission to any of the surveyed institutions. Vaccination for influenza, another disease with a high propensity to spread, also was not required by any school, with only 37% having influenza vaccination available as part of student health care.
Compliance with immunization requirements was enforced by 67% of the schools, with course registration not finalized until the necessary vaccinations had been received and documented. Of the 17% of schools that did not have an enforcement policy, 61% cited the vaccine requirements of their particular state, the assumption being that the incoming students from that state would have received the necessary vaccinations, reflecting a more reactive than proactive stance, according to Dr. Feemster. There was no difference in enforcement strategy between the public or private institutions.
Of the surveyed vaccines, at least some were available at just over 91% of the public institutions and at 76% of the private institutions
“The variation in requirements and enforcement suggest inconsistent vaccine uptake. Next steps include a mixed-methods study to measure attitudes, beliefs, and behaviors related to school vaccine policy among a national sample of college students and to identify facilitators and barriers to school vaccine policy implementation among school health administrators and providers,” said Dr. Feemster.
“The ultimate goal is to identify the best practices for implementation of college vaccine policies to optimize vaccine uptake and increase positive attitudes, beliefs, and future intentions about vaccines,” she added.
The sponsor of study was the Children’s Hospital of Philadelphia. The study was not funded. Dr. Feemster had no conflicts to disclose.
AT PAS 2017
Key clinical point: A survey of colleges and universities nationwide in the United States has revealed marked variation in vaccination requirements and vaccine availability.
Major finding: Of the two public and two private schools surveyed in each state and the District of Columbia, none require vaccination for human papillomavirus, with only one-third of schools having the vaccine available through student health.
Data source: Cross-sectional survey of 216 U.S. colleges and universities.
Disclosures: The sponsor of the study was the Children’s Hospital of Philadelphia. The study was not funded. Dr. Feemster had no conflicts to disclose.
Molecular tests for GAS pharyngitis could spur overuse of antibiotics
SAN FRANCISCO – The diagnosis of pharyngitis due to infection by group A streptococcus (GAS) based on the detection of nucleic acid is fast and accurate. But this benefit brings the possibility of overuse of antibiotics, with treatment offered to those who, in the era of growth-based detection of the bacteria, would not have received treatment, according to Robert R. Tanz, MD.
Dr. Tanz, professor of pediatrics at Northwestern University, Chicago, delivered this cautionary note at the meeting of the Pediatrics Academics Societies.
“The short turnaround time, high sensitivity, and high specificity of newer molecular tests for GAS will make their use increasingly common. Many of the additional patients identified by molecular testing may not have an illness attributable to GAS. The increase in positive tests will probably be associated with increased antibiotic prescribing. This may not be beneficial, especially in areas with low rates of acute rheumatic fever,” said Dr. Tanz, who practices at Ann & Robert Lurie Children’s Hospital of Chicago.
Nowadays, diagnosis of GAS at Ann & Robert Lurie Children’s Hospital uses the Illumigene system. Its use has been approved by the Food and Drug Administration for diagnosis without the need for backup culture of throat swabs. Results are available in about 1 hour.
Dr. Tanz and his colleagues took a retrospective look at patient records during 2013, when testing was still growth-based, and in 2014 and 2015, after the hospital had shifted to the molecular analysis of throat swabs. The aim was to determine the proportion of tests positive for GAS prior to and after the switch.
The positive detection rate of 9.6% (96 of 997 samples) in 2013 climbed to 17% (152 of 894) in 2014 and 16% (138 of 859) in 2015. The difference was highly significant (P less than .00001).
Sore throats increase in the colder months when people tend to be indoors more often, and this seasonality was evident in 2013. However, detection was more consistent throughout the 12 months in 2014 (2013 vs 2014, P less than .000001) and 2015 (2013 vs 2015, P less than .00001). The detection rates in 2014 and 2015 were similar (P equal to .59), according to Dr. Tanz.
The new era of molecular testing circumvents what is known as the spectrum effect, in which culture-based tests are more often positive in patients with symptoms that are consistent with the infection, he said. In contrast, molecular tests can increase the identification of the target bacterium, here GAS, in patients who have sore throat caused by a viral infection.
Preliminary results presented by Dr. Tanz indicated a significantly greater detection of GAS in children not displaying symptoms of infection. In decades past, these children would not have been treated.
“The increase in positive tests for group A strep is likely associated with increased antibiotic prescribing. This may or may not represent a benefit to patients, as the additional identified patients may not have an illness actually attributable to group A strep,” said Dr. Tanz.
“Our findings support rigorous selectivity in choosing which patients to test, specifically excluding those with overt viral symptoms, as recommended in the guidelines from the [Infectious Diseases Society of America], [American Academy of Pediatrics], and other groups,” he said, adding that clinician guidance on the use of molecular diagnostic tests for pharyngitis caused by group A strep is a prudent step.
Features suggestive of GAS may include sudden onset of sore throat, age 5-15 years, fever, headache, nausea, vomiting, and abdominal pain, tonsillopharyngeal inflammation and patchy tonsillopharyngeal exudates, palatal petechiae, tender nodes, and scarlatiniform rash. Viral pharyngitis features include conjunctivitis, coryza, cough, diarrhea, discrete ulcerative stomatitis, viral exanthema, and hoarseness, according to the 2012 Infectious Diseases Society of American guidelines (Clin Infect Dis. 2012. doi: 10.1093/cid/cis629).
For most people, a sore throat is more of a temporary inconvenience rather than a looming health threat, but GAS easily spreads from person to person and can lead to the more serious condition of acute rheumatic fever, Dr. Tanz said. Hence the concern with diagnosing the cause of sore throat and, when the cause is bacterial, alleviating the infection using antibiotics.
The study was conducted at Ann & Robert H. Lurie Children’s Hospital of Chicago and was not funded. Dr. Tanz reported having received support from Meridian Bioscience, manufacturer of the Illumigene Group A Streptococcus assay. Meridian Bioscience did not support this study.
SAN FRANCISCO – The diagnosis of pharyngitis due to infection by group A streptococcus (GAS) based on the detection of nucleic acid is fast and accurate. But this benefit brings the possibility of overuse of antibiotics, with treatment offered to those who, in the era of growth-based detection of the bacteria, would not have received treatment, according to Robert R. Tanz, MD.
Dr. Tanz, professor of pediatrics at Northwestern University, Chicago, delivered this cautionary note at the meeting of the Pediatrics Academics Societies.
“The short turnaround time, high sensitivity, and high specificity of newer molecular tests for GAS will make their use increasingly common. Many of the additional patients identified by molecular testing may not have an illness attributable to GAS. The increase in positive tests will probably be associated with increased antibiotic prescribing. This may not be beneficial, especially in areas with low rates of acute rheumatic fever,” said Dr. Tanz, who practices at Ann & Robert Lurie Children’s Hospital of Chicago.
Nowadays, diagnosis of GAS at Ann & Robert Lurie Children’s Hospital uses the Illumigene system. Its use has been approved by the Food and Drug Administration for diagnosis without the need for backup culture of throat swabs. Results are available in about 1 hour.
Dr. Tanz and his colleagues took a retrospective look at patient records during 2013, when testing was still growth-based, and in 2014 and 2015, after the hospital had shifted to the molecular analysis of throat swabs. The aim was to determine the proportion of tests positive for GAS prior to and after the switch.
The positive detection rate of 9.6% (96 of 997 samples) in 2013 climbed to 17% (152 of 894) in 2014 and 16% (138 of 859) in 2015. The difference was highly significant (P less than .00001).
Sore throats increase in the colder months when people tend to be indoors more often, and this seasonality was evident in 2013. However, detection was more consistent throughout the 12 months in 2014 (2013 vs 2014, P less than .000001) and 2015 (2013 vs 2015, P less than .00001). The detection rates in 2014 and 2015 were similar (P equal to .59), according to Dr. Tanz.
The new era of molecular testing circumvents what is known as the spectrum effect, in which culture-based tests are more often positive in patients with symptoms that are consistent with the infection, he said. In contrast, molecular tests can increase the identification of the target bacterium, here GAS, in patients who have sore throat caused by a viral infection.
Preliminary results presented by Dr. Tanz indicated a significantly greater detection of GAS in children not displaying symptoms of infection. In decades past, these children would not have been treated.
“The increase in positive tests for group A strep is likely associated with increased antibiotic prescribing. This may or may not represent a benefit to patients, as the additional identified patients may not have an illness actually attributable to group A strep,” said Dr. Tanz.
“Our findings support rigorous selectivity in choosing which patients to test, specifically excluding those with overt viral symptoms, as recommended in the guidelines from the [Infectious Diseases Society of America], [American Academy of Pediatrics], and other groups,” he said, adding that clinician guidance on the use of molecular diagnostic tests for pharyngitis caused by group A strep is a prudent step.
Features suggestive of GAS may include sudden onset of sore throat, age 5-15 years, fever, headache, nausea, vomiting, and abdominal pain, tonsillopharyngeal inflammation and patchy tonsillopharyngeal exudates, palatal petechiae, tender nodes, and scarlatiniform rash. Viral pharyngitis features include conjunctivitis, coryza, cough, diarrhea, discrete ulcerative stomatitis, viral exanthema, and hoarseness, according to the 2012 Infectious Diseases Society of American guidelines (Clin Infect Dis. 2012. doi: 10.1093/cid/cis629).
For most people, a sore throat is more of a temporary inconvenience rather than a looming health threat, but GAS easily spreads from person to person and can lead to the more serious condition of acute rheumatic fever, Dr. Tanz said. Hence the concern with diagnosing the cause of sore throat and, when the cause is bacterial, alleviating the infection using antibiotics.
The study was conducted at Ann & Robert H. Lurie Children’s Hospital of Chicago and was not funded. Dr. Tanz reported having received support from Meridian Bioscience, manufacturer of the Illumigene Group A Streptococcus assay. Meridian Bioscience did not support this study.
SAN FRANCISCO – The diagnosis of pharyngitis due to infection by group A streptococcus (GAS) based on the detection of nucleic acid is fast and accurate. But this benefit brings the possibility of overuse of antibiotics, with treatment offered to those who, in the era of growth-based detection of the bacteria, would not have received treatment, according to Robert R. Tanz, MD.
Dr. Tanz, professor of pediatrics at Northwestern University, Chicago, delivered this cautionary note at the meeting of the Pediatrics Academics Societies.
“The short turnaround time, high sensitivity, and high specificity of newer molecular tests for GAS will make their use increasingly common. Many of the additional patients identified by molecular testing may not have an illness attributable to GAS. The increase in positive tests will probably be associated with increased antibiotic prescribing. This may not be beneficial, especially in areas with low rates of acute rheumatic fever,” said Dr. Tanz, who practices at Ann & Robert Lurie Children’s Hospital of Chicago.
Nowadays, diagnosis of GAS at Ann & Robert Lurie Children’s Hospital uses the Illumigene system. Its use has been approved by the Food and Drug Administration for diagnosis without the need for backup culture of throat swabs. Results are available in about 1 hour.
Dr. Tanz and his colleagues took a retrospective look at patient records during 2013, when testing was still growth-based, and in 2014 and 2015, after the hospital had shifted to the molecular analysis of throat swabs. The aim was to determine the proportion of tests positive for GAS prior to and after the switch.
The positive detection rate of 9.6% (96 of 997 samples) in 2013 climbed to 17% (152 of 894) in 2014 and 16% (138 of 859) in 2015. The difference was highly significant (P less than .00001).
Sore throats increase in the colder months when people tend to be indoors more often, and this seasonality was evident in 2013. However, detection was more consistent throughout the 12 months in 2014 (2013 vs 2014, P less than .000001) and 2015 (2013 vs 2015, P less than .00001). The detection rates in 2014 and 2015 were similar (P equal to .59), according to Dr. Tanz.
The new era of molecular testing circumvents what is known as the spectrum effect, in which culture-based tests are more often positive in patients with symptoms that are consistent with the infection, he said. In contrast, molecular tests can increase the identification of the target bacterium, here GAS, in patients who have sore throat caused by a viral infection.
Preliminary results presented by Dr. Tanz indicated a significantly greater detection of GAS in children not displaying symptoms of infection. In decades past, these children would not have been treated.
“The increase in positive tests for group A strep is likely associated with increased antibiotic prescribing. This may or may not represent a benefit to patients, as the additional identified patients may not have an illness actually attributable to group A strep,” said Dr. Tanz.
“Our findings support rigorous selectivity in choosing which patients to test, specifically excluding those with overt viral symptoms, as recommended in the guidelines from the [Infectious Diseases Society of America], [American Academy of Pediatrics], and other groups,” he said, adding that clinician guidance on the use of molecular diagnostic tests for pharyngitis caused by group A strep is a prudent step.
Features suggestive of GAS may include sudden onset of sore throat, age 5-15 years, fever, headache, nausea, vomiting, and abdominal pain, tonsillopharyngeal inflammation and patchy tonsillopharyngeal exudates, palatal petechiae, tender nodes, and scarlatiniform rash. Viral pharyngitis features include conjunctivitis, coryza, cough, diarrhea, discrete ulcerative stomatitis, viral exanthema, and hoarseness, according to the 2012 Infectious Diseases Society of American guidelines (Clin Infect Dis. 2012. doi: 10.1093/cid/cis629).
For most people, a sore throat is more of a temporary inconvenience rather than a looming health threat, but GAS easily spreads from person to person and can lead to the more serious condition of acute rheumatic fever, Dr. Tanz said. Hence the concern with diagnosing the cause of sore throat and, when the cause is bacterial, alleviating the infection using antibiotics.
The study was conducted at Ann & Robert H. Lurie Children’s Hospital of Chicago and was not funded. Dr. Tanz reported having received support from Meridian Bioscience, manufacturer of the Illumigene Group A Streptococcus assay. Meridian Bioscience did not support this study.
Key clinical point: The increased molecular-based detection of group A streptococci could led to antibiotic overuse, with prescriptions for patients who do not have bacterial infections.
Major finding: In the most recent year of culture-based testing at Lurie Children’s Hospital, the detection rate of group A streptococci was 9.6%; detection rates were 17.0% and 16.1% in the next 2 years when molecular-based analysis was implemented.
Data source: Quality assessment study involving a retrospective review of hospital electronic medical records.
Disclosures: The study was conducted at Ann & Robert H. Lurie Children’s Hospital of Chicago and was not funded. Dr. Tanz reported having received support from Meridian Bioscience, manufacturer of the Illumigene Group A Streptococcus assay. Meridian Bioscience did not support this study.
Time to therapy for gram-positive bacteremia reduced from 60 hours to 4 hours
SAN FRANCISCO – Implementation of sample testing using a molecular approach, combined with coordinated and multidisciplinary notification of clinicians, has reduced the time to deliver adequate antibiotic therapy for bacteremia caused by gram-positive cocci including methicillin-resistant Staphylococcus aureus (MRSA) from 60 hours to 4 hours.
“We observed a significant decrease in the time to adequate antibiotics, significant decrease in time to first negative blood culture, and decreased variation in both measures,” Michael Tchou, MD, of the division of hospital medicine at Cincinnati Children’s Hospital Medical Center (CCHMC), reported at the Pediatric Academic Societies meeting.
Speeding up the time to delivery of adequate antibiotics is a must, Dr. Tchou emphasized.
CCHMC initiated the use of a multiplex polymerase chain reaction (PCR)–based identification protocol in mid-2013. Multiplex PCR targets specific regions of genetic material. In the protocol, empiric antibiotics are administered. At the same time, multiplex PCR is done. Blood culture and subsequent Gram staining of the bacteria in the colonies that grow also are done. PCR-based species identification and determination of probable antibiotic resistance, which takes about 3 hours, can be used to shift antibiotic therapy to adequate therapy, which is defined as the necessary antimicrobial therapy, even if it is still too broad. The growth-based results available the next day help fine-tune the therapy.
The use of multiplex PCR speeds the time to an “actionable result” – the time to recognize that the empiric antibiotic therapy is not the best, Dr. Tchou said.
At CCHMC, an actionable result is obtained for about 1 of every 40 cases of bloodstream infection determined to be caused by gram-positive cocci. The delay in switching to adequate antibiotic coverage used to average 60 hours.
In an effort to do better, Dr. Tchou and colleagues set a goal of reducing the time to adequate antibiotic therapy for gram-positive bacteremia from 60 to 12 hours within 6 months.
The effort necessitated the coordinated involvement of a multidisciplinary team, with a rapid system of clinician notification, and the real-time software-based monitoring of results. In the system, an actionable result triggers a text message to the on-call antibiotic stewardship contact, who in turn notifies the primary care team.
The multidisciplinary system was rolled out first for MRSA. The effort was even more successful than they hoped for. Delivery of appropriate antibiotics for MRSA infections dropped from about 60 hours to 13 hours within a few months, with a further decrease to 4 hours within another few months. Roll out of the initiative to all gram-positive cocci including coagulase-negative staphylococci, Streptococcus pyogenes, Enterococcus faecalis, and E. faecium similarly achieved the 4-hour target within months.
And preliminary results not presented by Dr. Tchou indicate an earlier resolution of bacteremia.
Next steps include modifying the decision support software to allow direct paging of providers instead of using text messages, expansion of the antibiotic coverage, and achieving similar improved treatment time for gram-negative bloodstream infections.
The study was sponsored by Cincinnati Children’s Hospital and was not funded. Dr. Tchou reported having no relevant financial disclosures.
SAN FRANCISCO – Implementation of sample testing using a molecular approach, combined with coordinated and multidisciplinary notification of clinicians, has reduced the time to deliver adequate antibiotic therapy for bacteremia caused by gram-positive cocci including methicillin-resistant Staphylococcus aureus (MRSA) from 60 hours to 4 hours.
“We observed a significant decrease in the time to adequate antibiotics, significant decrease in time to first negative blood culture, and decreased variation in both measures,” Michael Tchou, MD, of the division of hospital medicine at Cincinnati Children’s Hospital Medical Center (CCHMC), reported at the Pediatric Academic Societies meeting.
Speeding up the time to delivery of adequate antibiotics is a must, Dr. Tchou emphasized.
CCHMC initiated the use of a multiplex polymerase chain reaction (PCR)–based identification protocol in mid-2013. Multiplex PCR targets specific regions of genetic material. In the protocol, empiric antibiotics are administered. At the same time, multiplex PCR is done. Blood culture and subsequent Gram staining of the bacteria in the colonies that grow also are done. PCR-based species identification and determination of probable antibiotic resistance, which takes about 3 hours, can be used to shift antibiotic therapy to adequate therapy, which is defined as the necessary antimicrobial therapy, even if it is still too broad. The growth-based results available the next day help fine-tune the therapy.
The use of multiplex PCR speeds the time to an “actionable result” – the time to recognize that the empiric antibiotic therapy is not the best, Dr. Tchou said.
At CCHMC, an actionable result is obtained for about 1 of every 40 cases of bloodstream infection determined to be caused by gram-positive cocci. The delay in switching to adequate antibiotic coverage used to average 60 hours.
In an effort to do better, Dr. Tchou and colleagues set a goal of reducing the time to adequate antibiotic therapy for gram-positive bacteremia from 60 to 12 hours within 6 months.
The effort necessitated the coordinated involvement of a multidisciplinary team, with a rapid system of clinician notification, and the real-time software-based monitoring of results. In the system, an actionable result triggers a text message to the on-call antibiotic stewardship contact, who in turn notifies the primary care team.
The multidisciplinary system was rolled out first for MRSA. The effort was even more successful than they hoped for. Delivery of appropriate antibiotics for MRSA infections dropped from about 60 hours to 13 hours within a few months, with a further decrease to 4 hours within another few months. Roll out of the initiative to all gram-positive cocci including coagulase-negative staphylococci, Streptococcus pyogenes, Enterococcus faecalis, and E. faecium similarly achieved the 4-hour target within months.
And preliminary results not presented by Dr. Tchou indicate an earlier resolution of bacteremia.
Next steps include modifying the decision support software to allow direct paging of providers instead of using text messages, expansion of the antibiotic coverage, and achieving similar improved treatment time for gram-negative bloodstream infections.
The study was sponsored by Cincinnati Children’s Hospital and was not funded. Dr. Tchou reported having no relevant financial disclosures.
SAN FRANCISCO – Implementation of sample testing using a molecular approach, combined with coordinated and multidisciplinary notification of clinicians, has reduced the time to deliver adequate antibiotic therapy for bacteremia caused by gram-positive cocci including methicillin-resistant Staphylococcus aureus (MRSA) from 60 hours to 4 hours.
“We observed a significant decrease in the time to adequate antibiotics, significant decrease in time to first negative blood culture, and decreased variation in both measures,” Michael Tchou, MD, of the division of hospital medicine at Cincinnati Children’s Hospital Medical Center (CCHMC), reported at the Pediatric Academic Societies meeting.
Speeding up the time to delivery of adequate antibiotics is a must, Dr. Tchou emphasized.
CCHMC initiated the use of a multiplex polymerase chain reaction (PCR)–based identification protocol in mid-2013. Multiplex PCR targets specific regions of genetic material. In the protocol, empiric antibiotics are administered. At the same time, multiplex PCR is done. Blood culture and subsequent Gram staining of the bacteria in the colonies that grow also are done. PCR-based species identification and determination of probable antibiotic resistance, which takes about 3 hours, can be used to shift antibiotic therapy to adequate therapy, which is defined as the necessary antimicrobial therapy, even if it is still too broad. The growth-based results available the next day help fine-tune the therapy.
The use of multiplex PCR speeds the time to an “actionable result” – the time to recognize that the empiric antibiotic therapy is not the best, Dr. Tchou said.
At CCHMC, an actionable result is obtained for about 1 of every 40 cases of bloodstream infection determined to be caused by gram-positive cocci. The delay in switching to adequate antibiotic coverage used to average 60 hours.
In an effort to do better, Dr. Tchou and colleagues set a goal of reducing the time to adequate antibiotic therapy for gram-positive bacteremia from 60 to 12 hours within 6 months.
The effort necessitated the coordinated involvement of a multidisciplinary team, with a rapid system of clinician notification, and the real-time software-based monitoring of results. In the system, an actionable result triggers a text message to the on-call antibiotic stewardship contact, who in turn notifies the primary care team.
The multidisciplinary system was rolled out first for MRSA. The effort was even more successful than they hoped for. Delivery of appropriate antibiotics for MRSA infections dropped from about 60 hours to 13 hours within a few months, with a further decrease to 4 hours within another few months. Roll out of the initiative to all gram-positive cocci including coagulase-negative staphylococci, Streptococcus pyogenes, Enterococcus faecalis, and E. faecium similarly achieved the 4-hour target within months.
And preliminary results not presented by Dr. Tchou indicate an earlier resolution of bacteremia.
Next steps include modifying the decision support software to allow direct paging of providers instead of using text messages, expansion of the antibiotic coverage, and achieving similar improved treatment time for gram-negative bloodstream infections.
The study was sponsored by Cincinnati Children’s Hospital and was not funded. Dr. Tchou reported having no relevant financial disclosures.
AT PAS 2017
Key clinical point: Multiplex PCR and a revamped system of notification reduced the time to deliver adequate antibiotic therapy for bacteremia caused by gram-positive cocci from 60 hours to 4 hours within 6 months of implementation.
Major finding: and other gram-positive cocci-related infections.
Data source: A retrospective review of hospital records including patient data prior to and following implementation of multiplex PCR testing at one hospital.
Disclosures: The study was sponsored by Cincinnati Children’s Hospital and was not funded. Dr. Tchou reported having no relevant financial disclosures.