User login
A multimodal treatment for vestibulodynia: TENS plus diazepam
and with placebo in a randomized, double-blind, placebo-controlled trial.
In the TENS/diazepam and TENS/placebo groups, participants reported significant improvements from baseline in pain and sexual functioning by questionnaire and visual analog scale. They also improved in measurements of pelvic floor muscle tone and vestibular nerve fiber current perception threshold.
The study had two groups of 21 women each, all aged 18 years or older and diagnosed (by physical exam) with moderate or severe pelvic floor hypertonic dysfunction. The diazepam was a tablet inserted vaginally daily before bed.
The TENS therapy was also self-administered (after six or seven supervised trial sessions), a recommended three times per week. The device is a 20-mm diameter plastic vaginal probe with gold metallic transversal rings as electrodes, inserted 20 mm, with 30 minutes of electrical stimulation increased slowly until sensation “reached a level described as the maximum tolerable without experiencing pain.” Vulvar pain was assessed on a on a 10-cm visual analog scale and dyspareunia on the Marinoff dyspareunia scale.
At the primary endpoint, the mean change from baseline to 60 days, the diazepam combination improved from 7.5 on the visual scale to 4.7, while the placebo combination improved from 7.2 to 4.3 (P not significant between the groups). Marinoff dyspareunia scores, however, improved from 2.5 to 1.6 and from 2.0 to 1.3, respectively (P less than .01).
Though “very few statistically significant differences in outcomes between the two groups were observed ... our results indicate that diazepam is able to positively change the functions of the pelvic floor muscle often highlighted” in women with vestibulodynia, reported Filippo Murina, MD, of the University of Milan and his coauthors. This conclusion followed from the Marinoff scores and from vaginal surface electromyography. In the latter measure, the diazepam group showed a significantly greater ability to relax the pelvic floor muscle after contraction (3.8 vs. 2.4 microvolts; P = .01), compared with the placebo group.
“We also observed that TENS itself is essential in reducing vulvar pain and the action of diazepam is useful but not decisive. ... It is possible that vaginal diazepam alone is insufficient to resolve the symptoms related to pelvic floor muscle dysfunction, while vaginal diazepam and TENS together provide a synergistic benefit in vestibulodynia patients,” wrote Dr. Murina and his coauthors.
This study was supported by the Associazione Italiana Vulvodinia. The authors declared no conflicts of interest.
SOURCE: Murina F et al. Eur J Obstet Gynecol Reprod Biol. 2018 Jun;228:148-53.
and with placebo in a randomized, double-blind, placebo-controlled trial.
In the TENS/diazepam and TENS/placebo groups, participants reported significant improvements from baseline in pain and sexual functioning by questionnaire and visual analog scale. They also improved in measurements of pelvic floor muscle tone and vestibular nerve fiber current perception threshold.
The study had two groups of 21 women each, all aged 18 years or older and diagnosed (by physical exam) with moderate or severe pelvic floor hypertonic dysfunction. The diazepam was a tablet inserted vaginally daily before bed.
The TENS therapy was also self-administered (after six or seven supervised trial sessions), a recommended three times per week. The device is a 20-mm diameter plastic vaginal probe with gold metallic transversal rings as electrodes, inserted 20 mm, with 30 minutes of electrical stimulation increased slowly until sensation “reached a level described as the maximum tolerable without experiencing pain.” Vulvar pain was assessed on a on a 10-cm visual analog scale and dyspareunia on the Marinoff dyspareunia scale.
At the primary endpoint, the mean change from baseline to 60 days, the diazepam combination improved from 7.5 on the visual scale to 4.7, while the placebo combination improved from 7.2 to 4.3 (P not significant between the groups). Marinoff dyspareunia scores, however, improved from 2.5 to 1.6 and from 2.0 to 1.3, respectively (P less than .01).
Though “very few statistically significant differences in outcomes between the two groups were observed ... our results indicate that diazepam is able to positively change the functions of the pelvic floor muscle often highlighted” in women with vestibulodynia, reported Filippo Murina, MD, of the University of Milan and his coauthors. This conclusion followed from the Marinoff scores and from vaginal surface electromyography. In the latter measure, the diazepam group showed a significantly greater ability to relax the pelvic floor muscle after contraction (3.8 vs. 2.4 microvolts; P = .01), compared with the placebo group.
“We also observed that TENS itself is essential in reducing vulvar pain and the action of diazepam is useful but not decisive. ... It is possible that vaginal diazepam alone is insufficient to resolve the symptoms related to pelvic floor muscle dysfunction, while vaginal diazepam and TENS together provide a synergistic benefit in vestibulodynia patients,” wrote Dr. Murina and his coauthors.
This study was supported by the Associazione Italiana Vulvodinia. The authors declared no conflicts of interest.
SOURCE: Murina F et al. Eur J Obstet Gynecol Reprod Biol. 2018 Jun;228:148-53.
and with placebo in a randomized, double-blind, placebo-controlled trial.
In the TENS/diazepam and TENS/placebo groups, participants reported significant improvements from baseline in pain and sexual functioning by questionnaire and visual analog scale. They also improved in measurements of pelvic floor muscle tone and vestibular nerve fiber current perception threshold.
The study had two groups of 21 women each, all aged 18 years or older and diagnosed (by physical exam) with moderate or severe pelvic floor hypertonic dysfunction. The diazepam was a tablet inserted vaginally daily before bed.
The TENS therapy was also self-administered (after six or seven supervised trial sessions), a recommended three times per week. The device is a 20-mm diameter plastic vaginal probe with gold metallic transversal rings as electrodes, inserted 20 mm, with 30 minutes of electrical stimulation increased slowly until sensation “reached a level described as the maximum tolerable without experiencing pain.” Vulvar pain was assessed on a on a 10-cm visual analog scale and dyspareunia on the Marinoff dyspareunia scale.
At the primary endpoint, the mean change from baseline to 60 days, the diazepam combination improved from 7.5 on the visual scale to 4.7, while the placebo combination improved from 7.2 to 4.3 (P not significant between the groups). Marinoff dyspareunia scores, however, improved from 2.5 to 1.6 and from 2.0 to 1.3, respectively (P less than .01).
Though “very few statistically significant differences in outcomes between the two groups were observed ... our results indicate that diazepam is able to positively change the functions of the pelvic floor muscle often highlighted” in women with vestibulodynia, reported Filippo Murina, MD, of the University of Milan and his coauthors. This conclusion followed from the Marinoff scores and from vaginal surface electromyography. In the latter measure, the diazepam group showed a significantly greater ability to relax the pelvic floor muscle after contraction (3.8 vs. 2.4 microvolts; P = .01), compared with the placebo group.
“We also observed that TENS itself is essential in reducing vulvar pain and the action of diazepam is useful but not decisive. ... It is possible that vaginal diazepam alone is insufficient to resolve the symptoms related to pelvic floor muscle dysfunction, while vaginal diazepam and TENS together provide a synergistic benefit in vestibulodynia patients,” wrote Dr. Murina and his coauthors.
This study was supported by the Associazione Italiana Vulvodinia. The authors declared no conflicts of interest.
SOURCE: Murina F et al. Eur J Obstet Gynecol Reprod Biol. 2018 Jun;228:148-53.
FROM THE EUROPEAN JOURNAL OF OBSTETRICS & GYNECOLOGY AND REPRODUCTIVE BIOLOGY
Treat chronic endometritis to improve implantation rates
In a meta-analysis of five studies of chronic endometritis (CE), women cured of the condition had significantly higher rates of pregnancies, live births, and successful implantations compared with women who had persistent CE.
“These findings potentially suggest that CE is a reversible factor of infertility, whose recognition and therapy may provide better chances at subsequent [in vitro fertilization] attempts,” wrote Amerigo Vitagliano, MD, of the University of Padua (Italy), and his coauthors.
They sought to examine the effect of CE treatment on implantation for women with recurrent implantation failure. While CE is correlated with infertility, prior studies have not resolved the question of whether curing CE would restore fertility. The condition is cured in as many of 80% of cases with a single cycle of antibiotics.
The systematic review found five studies with a total of 796 patients with recurrent implantation failure in Argentina, China, Italy, Japan, and the United States. Two studies compared cured CE with persistent CE, and three studies compared cured CE with patients not affected by CE.
Only one of the studies evaluated CE patients receiving antibiotics with CE patients not receiving antibiotics. The study showed that there was no difference between those two groups in clinical pregnancy rate, ongoing (12 or more weeks’ gestation) pregnancy rate/live birth rate, or implantation rate.
The significant result was the difference between cured and persistent CE. Those numbers worked out to a higher ongoing pregnancy rate/live birth rate (odds ratio, 6.81; 95% confidence interval, 2.08-22.24; P = .001), clinical pregnancy rate (OR, 4.98; 95% CI, 1.72-14.43; P = .003), and implantation rate (OR, 3.24; 95% CI, 1.33-7.88; P = .01), with no difference in the miscarriage rate (P = .30).
The authors recommend further research in the form of randomized controlled trials to confirm whether completed CE treatment will improve in vitro fertilization success, and whether routine CE screening is advisable for all patients with recurrent implantation failure. At present, they recommend that diagnosed cases of CE be resolved before continuing with fertility treatment.
“If our results are confirmed, CE may represent a new therapeutic target for women suffering from [recurrent implantation failure], with affordable access (diagnosed through a simple endometrial biopsy and treated by oral antibiotics),” they wrote.
The authors reported having no financial disclosures.
SOURCE: Vitagliano A et al. Fertil Steril. 2018 Jun. doi: 10.1016/j.fertnstert.2018.03.017.
In a meta-analysis of five studies of chronic endometritis (CE), women cured of the condition had significantly higher rates of pregnancies, live births, and successful implantations compared with women who had persistent CE.
“These findings potentially suggest that CE is a reversible factor of infertility, whose recognition and therapy may provide better chances at subsequent [in vitro fertilization] attempts,” wrote Amerigo Vitagliano, MD, of the University of Padua (Italy), and his coauthors.
They sought to examine the effect of CE treatment on implantation for women with recurrent implantation failure. While CE is correlated with infertility, prior studies have not resolved the question of whether curing CE would restore fertility. The condition is cured in as many of 80% of cases with a single cycle of antibiotics.
The systematic review found five studies with a total of 796 patients with recurrent implantation failure in Argentina, China, Italy, Japan, and the United States. Two studies compared cured CE with persistent CE, and three studies compared cured CE with patients not affected by CE.
Only one of the studies evaluated CE patients receiving antibiotics with CE patients not receiving antibiotics. The study showed that there was no difference between those two groups in clinical pregnancy rate, ongoing (12 or more weeks’ gestation) pregnancy rate/live birth rate, or implantation rate.
The significant result was the difference between cured and persistent CE. Those numbers worked out to a higher ongoing pregnancy rate/live birth rate (odds ratio, 6.81; 95% confidence interval, 2.08-22.24; P = .001), clinical pregnancy rate (OR, 4.98; 95% CI, 1.72-14.43; P = .003), and implantation rate (OR, 3.24; 95% CI, 1.33-7.88; P = .01), with no difference in the miscarriage rate (P = .30).
The authors recommend further research in the form of randomized controlled trials to confirm whether completed CE treatment will improve in vitro fertilization success, and whether routine CE screening is advisable for all patients with recurrent implantation failure. At present, they recommend that diagnosed cases of CE be resolved before continuing with fertility treatment.
“If our results are confirmed, CE may represent a new therapeutic target for women suffering from [recurrent implantation failure], with affordable access (diagnosed through a simple endometrial biopsy and treated by oral antibiotics),” they wrote.
The authors reported having no financial disclosures.
SOURCE: Vitagliano A et al. Fertil Steril. 2018 Jun. doi: 10.1016/j.fertnstert.2018.03.017.
In a meta-analysis of five studies of chronic endometritis (CE), women cured of the condition had significantly higher rates of pregnancies, live births, and successful implantations compared with women who had persistent CE.
“These findings potentially suggest that CE is a reversible factor of infertility, whose recognition and therapy may provide better chances at subsequent [in vitro fertilization] attempts,” wrote Amerigo Vitagliano, MD, of the University of Padua (Italy), and his coauthors.
They sought to examine the effect of CE treatment on implantation for women with recurrent implantation failure. While CE is correlated with infertility, prior studies have not resolved the question of whether curing CE would restore fertility. The condition is cured in as many of 80% of cases with a single cycle of antibiotics.
The systematic review found five studies with a total of 796 patients with recurrent implantation failure in Argentina, China, Italy, Japan, and the United States. Two studies compared cured CE with persistent CE, and three studies compared cured CE with patients not affected by CE.
Only one of the studies evaluated CE patients receiving antibiotics with CE patients not receiving antibiotics. The study showed that there was no difference between those two groups in clinical pregnancy rate, ongoing (12 or more weeks’ gestation) pregnancy rate/live birth rate, or implantation rate.
The significant result was the difference between cured and persistent CE. Those numbers worked out to a higher ongoing pregnancy rate/live birth rate (odds ratio, 6.81; 95% confidence interval, 2.08-22.24; P = .001), clinical pregnancy rate (OR, 4.98; 95% CI, 1.72-14.43; P = .003), and implantation rate (OR, 3.24; 95% CI, 1.33-7.88; P = .01), with no difference in the miscarriage rate (P = .30).
The authors recommend further research in the form of randomized controlled trials to confirm whether completed CE treatment will improve in vitro fertilization success, and whether routine CE screening is advisable for all patients with recurrent implantation failure. At present, they recommend that diagnosed cases of CE be resolved before continuing with fertility treatment.
“If our results are confirmed, CE may represent a new therapeutic target for women suffering from [recurrent implantation failure], with affordable access (diagnosed through a simple endometrial biopsy and treated by oral antibiotics),” they wrote.
The authors reported having no financial disclosures.
SOURCE: Vitagliano A et al. Fertil Steril. 2018 Jun. doi: 10.1016/j.fertnstert.2018.03.017.
FROM FERTILITY & STERILITY
NSAID use early in pregnancy increases miscarriage risk
and a statistically significant dose-response relationship in which the risk increased at a greater duration of exposure was established in a case-control study published in the American Journal of Obstetrics and Gynecology.
The cohorts in the study were NSAID users, acetaminophen-only users, and controls exposed to neither NSAIDs or acetaminophen. The reasoning for including the acetaminophen cohort is that the drug has a similar indication but does not inhibit prostaglandin biosynthesis, as NSAIDs do. Prostaglandin is important for implantation in early pregnancy. The basic facts of what NSAIDs do and how implantation works have led to theories about miscarriage risk, but previous studies have not been conclusive, said De-Kun Li, MD, PhD, of Kaiser Permanente, and his coauthors.
Participants were women in the Kaiser Permanente Northern California database with positive pregnancy test results, questioned by interviewers and compared with pharmacy records when available. The total was 241 women exposed to NSAIDs, 391 exposed to acetaminophen, and 465 unexposed controls.
The adjusted hazard ratio for miscarriage was 1.59 for NSAID users of any timing and any duration, compared with 1.10 for acetaminophen users. If the NSAID exposure first occurred within the first 2 weeks of gestational age, that risk was a 1.89 hazard ratio, and increased to 2.10 when the duration of the near-conception exposure was greater than 14 days. The risk of miscarriage associated with NSAIDs had statistical significance within the first 8 weeks of gestational age, but not later.
“The timing of NSAID use (around conception) and the timing of miscarriage (early miscarriage only) are consistent with the underlying mechanism of the association,” wrote Dr. Li and his associates. The results “provide consistent findings as well as a coherent biological mechanism for the observation.”
The authors warned that the risk “remains largely ignored by both pregnant women and clinicians,” as NSAIDs are still widely prescribed and used.
“The risk was largely confined to women who were not overweight (body mass index less than 25). In contrast, there was little evidence of increased risk of miscarriage due to NSAID use among women who were overweight (body mass index greater than or equal to 25), thus indicating a potential mitigating effect of being overweight,” although this findings requires confirmation, Dr. Li and his associates said.
The study was funded by the National Institute of Child Health and Human Development. The authors reported no conflicts of interest.
SOURCE: Li DK et al. Am J Obstet Gynecol. 2018 Jun. doi: 10.1016/j.ajog.2018.06.002.
and a statistically significant dose-response relationship in which the risk increased at a greater duration of exposure was established in a case-control study published in the American Journal of Obstetrics and Gynecology.
The cohorts in the study were NSAID users, acetaminophen-only users, and controls exposed to neither NSAIDs or acetaminophen. The reasoning for including the acetaminophen cohort is that the drug has a similar indication but does not inhibit prostaglandin biosynthesis, as NSAIDs do. Prostaglandin is important for implantation in early pregnancy. The basic facts of what NSAIDs do and how implantation works have led to theories about miscarriage risk, but previous studies have not been conclusive, said De-Kun Li, MD, PhD, of Kaiser Permanente, and his coauthors.
Participants were women in the Kaiser Permanente Northern California database with positive pregnancy test results, questioned by interviewers and compared with pharmacy records when available. The total was 241 women exposed to NSAIDs, 391 exposed to acetaminophen, and 465 unexposed controls.
The adjusted hazard ratio for miscarriage was 1.59 for NSAID users of any timing and any duration, compared with 1.10 for acetaminophen users. If the NSAID exposure first occurred within the first 2 weeks of gestational age, that risk was a 1.89 hazard ratio, and increased to 2.10 when the duration of the near-conception exposure was greater than 14 days. The risk of miscarriage associated with NSAIDs had statistical significance within the first 8 weeks of gestational age, but not later.
“The timing of NSAID use (around conception) and the timing of miscarriage (early miscarriage only) are consistent with the underlying mechanism of the association,” wrote Dr. Li and his associates. The results “provide consistent findings as well as a coherent biological mechanism for the observation.”
The authors warned that the risk “remains largely ignored by both pregnant women and clinicians,” as NSAIDs are still widely prescribed and used.
“The risk was largely confined to women who were not overweight (body mass index less than 25). In contrast, there was little evidence of increased risk of miscarriage due to NSAID use among women who were overweight (body mass index greater than or equal to 25), thus indicating a potential mitigating effect of being overweight,” although this findings requires confirmation, Dr. Li and his associates said.
The study was funded by the National Institute of Child Health and Human Development. The authors reported no conflicts of interest.
SOURCE: Li DK et al. Am J Obstet Gynecol. 2018 Jun. doi: 10.1016/j.ajog.2018.06.002.
and a statistically significant dose-response relationship in which the risk increased at a greater duration of exposure was established in a case-control study published in the American Journal of Obstetrics and Gynecology.
The cohorts in the study were NSAID users, acetaminophen-only users, and controls exposed to neither NSAIDs or acetaminophen. The reasoning for including the acetaminophen cohort is that the drug has a similar indication but does not inhibit prostaglandin biosynthesis, as NSAIDs do. Prostaglandin is important for implantation in early pregnancy. The basic facts of what NSAIDs do and how implantation works have led to theories about miscarriage risk, but previous studies have not been conclusive, said De-Kun Li, MD, PhD, of Kaiser Permanente, and his coauthors.
Participants were women in the Kaiser Permanente Northern California database with positive pregnancy test results, questioned by interviewers and compared with pharmacy records when available. The total was 241 women exposed to NSAIDs, 391 exposed to acetaminophen, and 465 unexposed controls.
The adjusted hazard ratio for miscarriage was 1.59 for NSAID users of any timing and any duration, compared with 1.10 for acetaminophen users. If the NSAID exposure first occurred within the first 2 weeks of gestational age, that risk was a 1.89 hazard ratio, and increased to 2.10 when the duration of the near-conception exposure was greater than 14 days. The risk of miscarriage associated with NSAIDs had statistical significance within the first 8 weeks of gestational age, but not later.
“The timing of NSAID use (around conception) and the timing of miscarriage (early miscarriage only) are consistent with the underlying mechanism of the association,” wrote Dr. Li and his associates. The results “provide consistent findings as well as a coherent biological mechanism for the observation.”
The authors warned that the risk “remains largely ignored by both pregnant women and clinicians,” as NSAIDs are still widely prescribed and used.
“The risk was largely confined to women who were not overweight (body mass index less than 25). In contrast, there was little evidence of increased risk of miscarriage due to NSAID use among women who were overweight (body mass index greater than or equal to 25), thus indicating a potential mitigating effect of being overweight,” although this findings requires confirmation, Dr. Li and his associates said.
The study was funded by the National Institute of Child Health and Human Development. The authors reported no conflicts of interest.
SOURCE: Li DK et al. Am J Obstet Gynecol. 2018 Jun. doi: 10.1016/j.ajog.2018.06.002.
FROM THE AMERICAN JOURNAL OF OBSTETRICS AND GYNECOLOGY
Key clinical point: A cohort study in California showed a dose-response relationship between NSAID use early in pregnancy and risk of miscarriage.
Major finding: The adjusted hazard ratio for miscarriage was 1.59 for NSAID users of any timing and any duration, compared with 1.10 for acetaminophen users.
Study details: The study comprised 241 women exposed to NSAIDs, 391 exposed to acetaminophen, and 465 unexposed controls, drawn from the Kaiser Permanente Northern California database.
Disclosures: The National Institute of Child Health and Human Development funded the work. The authors reported no conflicts of interest.
Source: Li DK et al. Am J Obstet Gynecol. 2018 Jun. doi: 10.1016/j.ajog.2018.06.002.
SLN mapping is most cost-effective in low-risk endometrial carcinoma
Researchers conducting a cost-utility analysis of sentinel lymph node (SLN) mapping and lymph node dissection (LND), both selective and routine, for low-risk endometrial carcinoma (clinical stage 1 disease with grade 1-2 endometrioid histology on preoperative endometrial biopsy), found that the SLN mapping had the lowest costs and the highest quality-adjusted survival of the three strategies.
Between the two strategies of LND, selective LND based on intraoperative frozen section was more cost-effective than routine LND.
The researchers created a model using data from past studies and clinical estimates. “Our biggest assumption was that sentinel lymph node mapping is associated with a decreased risk of lymphedema compared with lymph node dissection ... [from] several studies showing that having less than five lymph nodes excised was associated with a much smaller risk of developing lymphedema,” wrote Rudy S. Suidan, MD, of the MD Anderson Cancer Center, Houston, and his coauthors. Lymphedema was the main factor affecting quality of life in the analysis.
The analysis included estimates of rates of lymphadenectomy, bilateral mapping, and unilateral mapping, 3-year disease-specific survival, and overall survival, all of which were compared with third-party reimbursement costs at 2016 Medicare rates.
SLN mapping cost $16,401 per patient, while selective LND cost $17,036 per patient and routine LND cost $18,041 per patient. These strategies had quality-adjusted life years of 2.87, 2.81, and 2.79, respectively.
The superior cost-effectiveness of SLN mapping held, even when the researchers altered several of the variables in the model, including assuming open surgery instead of minimally invasive, and altering the assumed risk of lymphedema.
In addition to the possible limitation of making assumptions about SLN mapping and lymphedema, the researchers also pointed to the 3-year survival rates as shorter-term than preferable, driven by the available literature. The quality-adjusted life years did not differ much between the strategies because “most patients with low-risk cancer tend to have good clinical outcomes,” they wrote.
“This adds to the body of literature evaluating the clinical benefits of this strategy and may help health care providers in the decision-making process as they consider which approach to use,” the researchers wrote.
Dr. Suidan is supported by an NIH grant. Three coauthors reported other grants and fellowships. Five coauthors reported research support from AstraZeneca, Bayer, Clovis Oncology, and several other companies.
SOURCE: Suidan RS et al. Obstet Gynecol. 2018 Jun 11;132:52-8.
Researchers conducting a cost-utility analysis of sentinel lymph node (SLN) mapping and lymph node dissection (LND), both selective and routine, for low-risk endometrial carcinoma (clinical stage 1 disease with grade 1-2 endometrioid histology on preoperative endometrial biopsy), found that the SLN mapping had the lowest costs and the highest quality-adjusted survival of the three strategies.
Between the two strategies of LND, selective LND based on intraoperative frozen section was more cost-effective than routine LND.
The researchers created a model using data from past studies and clinical estimates. “Our biggest assumption was that sentinel lymph node mapping is associated with a decreased risk of lymphedema compared with lymph node dissection ... [from] several studies showing that having less than five lymph nodes excised was associated with a much smaller risk of developing lymphedema,” wrote Rudy S. Suidan, MD, of the MD Anderson Cancer Center, Houston, and his coauthors. Lymphedema was the main factor affecting quality of life in the analysis.
The analysis included estimates of rates of lymphadenectomy, bilateral mapping, and unilateral mapping, 3-year disease-specific survival, and overall survival, all of which were compared with third-party reimbursement costs at 2016 Medicare rates.
SLN mapping cost $16,401 per patient, while selective LND cost $17,036 per patient and routine LND cost $18,041 per patient. These strategies had quality-adjusted life years of 2.87, 2.81, and 2.79, respectively.
The superior cost-effectiveness of SLN mapping held, even when the researchers altered several of the variables in the model, including assuming open surgery instead of minimally invasive, and altering the assumed risk of lymphedema.
In addition to the possible limitation of making assumptions about SLN mapping and lymphedema, the researchers also pointed to the 3-year survival rates as shorter-term than preferable, driven by the available literature. The quality-adjusted life years did not differ much between the strategies because “most patients with low-risk cancer tend to have good clinical outcomes,” they wrote.
“This adds to the body of literature evaluating the clinical benefits of this strategy and may help health care providers in the decision-making process as they consider which approach to use,” the researchers wrote.
Dr. Suidan is supported by an NIH grant. Three coauthors reported other grants and fellowships. Five coauthors reported research support from AstraZeneca, Bayer, Clovis Oncology, and several other companies.
SOURCE: Suidan RS et al. Obstet Gynecol. 2018 Jun 11;132:52-8.
Researchers conducting a cost-utility analysis of sentinel lymph node (SLN) mapping and lymph node dissection (LND), both selective and routine, for low-risk endometrial carcinoma (clinical stage 1 disease with grade 1-2 endometrioid histology on preoperative endometrial biopsy), found that the SLN mapping had the lowest costs and the highest quality-adjusted survival of the three strategies.
Between the two strategies of LND, selective LND based on intraoperative frozen section was more cost-effective than routine LND.
The researchers created a model using data from past studies and clinical estimates. “Our biggest assumption was that sentinel lymph node mapping is associated with a decreased risk of lymphedema compared with lymph node dissection ... [from] several studies showing that having less than five lymph nodes excised was associated with a much smaller risk of developing lymphedema,” wrote Rudy S. Suidan, MD, of the MD Anderson Cancer Center, Houston, and his coauthors. Lymphedema was the main factor affecting quality of life in the analysis.
The analysis included estimates of rates of lymphadenectomy, bilateral mapping, and unilateral mapping, 3-year disease-specific survival, and overall survival, all of which were compared with third-party reimbursement costs at 2016 Medicare rates.
SLN mapping cost $16,401 per patient, while selective LND cost $17,036 per patient and routine LND cost $18,041 per patient. These strategies had quality-adjusted life years of 2.87, 2.81, and 2.79, respectively.
The superior cost-effectiveness of SLN mapping held, even when the researchers altered several of the variables in the model, including assuming open surgery instead of minimally invasive, and altering the assumed risk of lymphedema.
In addition to the possible limitation of making assumptions about SLN mapping and lymphedema, the researchers also pointed to the 3-year survival rates as shorter-term than preferable, driven by the available literature. The quality-adjusted life years did not differ much between the strategies because “most patients with low-risk cancer tend to have good clinical outcomes,” they wrote.
“This adds to the body of literature evaluating the clinical benefits of this strategy and may help health care providers in the decision-making process as they consider which approach to use,” the researchers wrote.
Dr. Suidan is supported by an NIH grant. Three coauthors reported other grants and fellowships. Five coauthors reported research support from AstraZeneca, Bayer, Clovis Oncology, and several other companies.
SOURCE: Suidan RS et al. Obstet Gynecol. 2018 Jun 11;132:52-8.
FROM OBSTETRICS & GYNECOLOGY
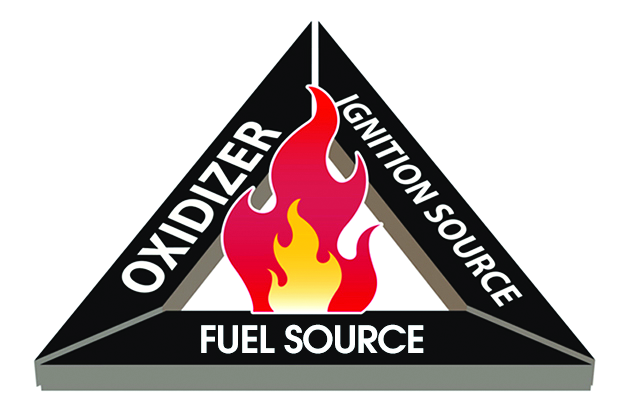
FDA issues recommendations to avoid surgical fires
The Food and Drug Administration on May 29 issued a set of recommendations to medical professionals and health care facility staff to reduce the occurrence of surgical fires on or near a patient.
Surgical fires most often occur when there is an oxygen-enriched environment (a concentration of greater than 30%). In addition to an oxygen source, the other two necessary elements of the “fire triangle” are an ignition source and a fuel source.
The recommendations discuss the safe use of devices or items that may serve as a source of any one of those three elements.
Oxygen: Evaluate if supplemental oxygen is needed. If it is, titrate to the minimum concentration needed for adequate saturation. Closed oxygen delivery systems (such as a laryngeal mask or endotracheal tube) are safer than open oxygen delivery systems (such as a nasal cannula or mask). If you must use an open system, take additional precautions to exclude oxygen and flammable/combustible gases from the operative field, such as draping techniques that avoid accumulation of oxygen.
Ignition sources: Consider alternatives to using an ignition source for surgery of the head, neck, and upper chest if high concentrations of supplemental oxygen are being delivered. Check for insulation failure before use, and keep devices clean of char and tissue. When not in use, place the devices safely away from the patient and drapes. Devices are safer to use if you can allow time for the oxygen concentration in the room to decrease.
Fuel sources: Ensure dry conditions prior to draping, avoiding pooling of alcohol-based antiseptics during skin preparation. Use the appropriate-sized applicator for the surgical site. Be aware of products that may serve as a fuel source, such as oxygen-trapping gauze, plastic laryngeal masks, and aware of potential patient sources such as hair or gastrointestinal gases.
Training should include how to manage fires that do occur – stop the ignition source, then extinguish the fire – and evacuation procedures.
Read the full recommendations here.
The Food and Drug Administration on May 29 issued a set of recommendations to medical professionals and health care facility staff to reduce the occurrence of surgical fires on or near a patient.
Surgical fires most often occur when there is an oxygen-enriched environment (a concentration of greater than 30%). In addition to an oxygen source, the other two necessary elements of the “fire triangle” are an ignition source and a fuel source.
The recommendations discuss the safe use of devices or items that may serve as a source of any one of those three elements.
Oxygen: Evaluate if supplemental oxygen is needed. If it is, titrate to the minimum concentration needed for adequate saturation. Closed oxygen delivery systems (such as a laryngeal mask or endotracheal tube) are safer than open oxygen delivery systems (such as a nasal cannula or mask). If you must use an open system, take additional precautions to exclude oxygen and flammable/combustible gases from the operative field, such as draping techniques that avoid accumulation of oxygen.
Ignition sources: Consider alternatives to using an ignition source for surgery of the head, neck, and upper chest if high concentrations of supplemental oxygen are being delivered. Check for insulation failure before use, and keep devices clean of char and tissue. When not in use, place the devices safely away from the patient and drapes. Devices are safer to use if you can allow time for the oxygen concentration in the room to decrease.
Fuel sources: Ensure dry conditions prior to draping, avoiding pooling of alcohol-based antiseptics during skin preparation. Use the appropriate-sized applicator for the surgical site. Be aware of products that may serve as a fuel source, such as oxygen-trapping gauze, plastic laryngeal masks, and aware of potential patient sources such as hair or gastrointestinal gases.
Training should include how to manage fires that do occur – stop the ignition source, then extinguish the fire – and evacuation procedures.
Read the full recommendations here.
The Food and Drug Administration on May 29 issued a set of recommendations to medical professionals and health care facility staff to reduce the occurrence of surgical fires on or near a patient.
Surgical fires most often occur when there is an oxygen-enriched environment (a concentration of greater than 30%). In addition to an oxygen source, the other two necessary elements of the “fire triangle” are an ignition source and a fuel source.
The recommendations discuss the safe use of devices or items that may serve as a source of any one of those three elements.
Oxygen: Evaluate if supplemental oxygen is needed. If it is, titrate to the minimum concentration needed for adequate saturation. Closed oxygen delivery systems (such as a laryngeal mask or endotracheal tube) are safer than open oxygen delivery systems (such as a nasal cannula or mask). If you must use an open system, take additional precautions to exclude oxygen and flammable/combustible gases from the operative field, such as draping techniques that avoid accumulation of oxygen.
Ignition sources: Consider alternatives to using an ignition source for surgery of the head, neck, and upper chest if high concentrations of supplemental oxygen are being delivered. Check for insulation failure before use, and keep devices clean of char and tissue. When not in use, place the devices safely away from the patient and drapes. Devices are safer to use if you can allow time for the oxygen concentration in the room to decrease.
Fuel sources: Ensure dry conditions prior to draping, avoiding pooling of alcohol-based antiseptics during skin preparation. Use the appropriate-sized applicator for the surgical site. Be aware of products that may serve as a fuel source, such as oxygen-trapping gauze, plastic laryngeal masks, and aware of potential patient sources such as hair or gastrointestinal gases.
Training should include how to manage fires that do occur – stop the ignition source, then extinguish the fire – and evacuation procedures.
Read the full recommendations here.
Mifepristone, then misoprostol is best in early pregnancy loss
In a randomized trial of women with early pregnancy loss, pretreatment with mifepristone before misoprostol was superior to misoprostol alone at achieving gestational sac expulsion by the time of the first follow-up visit without additional intervention.
“Women generally prefer active management; the ability to have control over the management of miscarriage may relieve some of the emotional burden that accompanies first trimester pregnancy loss,” Courtney A. Schreiber, MD, of the University of Pennsylvania, Philadelphia, and her coauthors wrote in the New England Journal of Medicine. But misoprostol (Cytotec) alone for women with a closed cervical os can require a second dose or intervention.
The trial enrolled 300 participants. Each had an ultrasound showing a nonviable intrauterine pregnancy of 5-12 weeks’ gestation. Women with an incomplete or inevitable abortion (that is, the absence of a gestational sac, an open cervical os, or both) were excluded, as misoprostol alone is effective for management of that diagnosis.
After randomization, 149 participants received 200 mg of oral mifepristone (Mifeprex), with 800 mcg misoprostol administered approximately 24 hours later. The other 151 participants received the standard 800 mcg dose of misoprostol alone. In both groups, the misoprostol was self-administered vaginally at home by inserting four 200-mcg tablets.
Follow-up came 24 hours to 4 days after misoprostol administration. The primary outcome was a gestational sac expulsion by the time of this follow-up, and no additional surgical or medical intervention within 30 days. If the gestational sac was present at follow-up, participants chose either expectant management, surgical management, or a second misoprostol dose.
The primary outcome was achieved in 124 of 148 women (83.8%; 95% confidence interval, 76.8-89.3) in the mifepristone-pretreatment group and in 100 of 149 women (67.1%; 95% CI, 59.0-74.6) in the misoprostol-alone group for a relative risk of 1.25 (95% CI, 1.09 to 1.43). Two women were lost to follow-up and one who was declared ineligible because of a possible ectopic pregnancy.
At 30 days’ follow-up, the cumulative rate of gestational sac expulsion with up to two doses of misoprostol was 91.2% (95% CI, 85.4-95.2) in the mifepristone-pretreatment group and 75.8% (95% CI, 68.2%-82.5%) in the misoprostol-alone group. Also by 30 days’ follow-up, 13 women in the mifepristone-pretreatment group and 35 women in the misoprostol-alone group had undergone uterine aspiration (relative risk, 0.37; 95% CI, 0.21-0.68).
Serious adverse events were rare in both groups, and both groups had matching mean scores for bleeding intensity and pain.
“Pretreatment with mifepristone followed by treatment with misoprostol resulted in a significantly higher rate of complete gestational sac expulsion by approximately 2 days after treatment ... [and] a significantly lower rate of uterine aspiration than misoprostol use alone,” wrote Dr. Schreiber and her coauthors. Patient satisfaction was similar between the two groups (89.4% vs. 87.4%, respectively, described their experience overall as either “good” or “neutral”).
The trial was funded by the National Institute of Child Health and Human Development. Two coauthors reported grants from the National Institutes of Health during the study and another reported personal fees from Danco Laboratories, which markets mifepristone, outside the submitted work.
SOURCE: Schreiber CA et al. N Engl J Med. 2018;378:2161-70.
The results of this study provide strong evidence that the sequential regimen of mifepristone followed by misoprostol is safe and superior to misoprostol alone in achieving treatment success and avoiding an aspiration procedure, wrote Carolyn L. Westhoff, MD, in an editorial accompanying the article.
In addition to its greater efficacy, the mifepristone treatment is quicker, which is more desirable for patients and reduces costs, inconvenience, and patient anxiety. Some women still will need prompt access to aspiration.
The mifepristone-pretreatment regimen should be the standard of care, Dr. Westhoff writes, but access to mifepristone is limited by the FDA’s Risk Evaluation and Mitigation Strategy restriction, which requires that the oral drug be taken in the doctor’s office rather than obtained at a retail pharmacy. “Extensive clinical experience with mifepristone indicates that there is no need for such restrictions,” she wrote.
Carolyn L. Westhoff, MD, is a professor of epidemiology and population and family health at Columbia University in New York. Her remarks are adapted from an accompanying editorial (N Engl J Med. 2018;378:2232-3). She reported personal fees from Planned Parenthood, Bayer, Agile Therapeutics, Cooper Surgical, Allergan, Elsevier, and personal fees and nonfinancial support from Merck.
The results of this study provide strong evidence that the sequential regimen of mifepristone followed by misoprostol is safe and superior to misoprostol alone in achieving treatment success and avoiding an aspiration procedure, wrote Carolyn L. Westhoff, MD, in an editorial accompanying the article.
In addition to its greater efficacy, the mifepristone treatment is quicker, which is more desirable for patients and reduces costs, inconvenience, and patient anxiety. Some women still will need prompt access to aspiration.
The mifepristone-pretreatment regimen should be the standard of care, Dr. Westhoff writes, but access to mifepristone is limited by the FDA’s Risk Evaluation and Mitigation Strategy restriction, which requires that the oral drug be taken in the doctor’s office rather than obtained at a retail pharmacy. “Extensive clinical experience with mifepristone indicates that there is no need for such restrictions,” she wrote.
Carolyn L. Westhoff, MD, is a professor of epidemiology and population and family health at Columbia University in New York. Her remarks are adapted from an accompanying editorial (N Engl J Med. 2018;378:2232-3). She reported personal fees from Planned Parenthood, Bayer, Agile Therapeutics, Cooper Surgical, Allergan, Elsevier, and personal fees and nonfinancial support from Merck.
The results of this study provide strong evidence that the sequential regimen of mifepristone followed by misoprostol is safe and superior to misoprostol alone in achieving treatment success and avoiding an aspiration procedure, wrote Carolyn L. Westhoff, MD, in an editorial accompanying the article.
In addition to its greater efficacy, the mifepristone treatment is quicker, which is more desirable for patients and reduces costs, inconvenience, and patient anxiety. Some women still will need prompt access to aspiration.
The mifepristone-pretreatment regimen should be the standard of care, Dr. Westhoff writes, but access to mifepristone is limited by the FDA’s Risk Evaluation and Mitigation Strategy restriction, which requires that the oral drug be taken in the doctor’s office rather than obtained at a retail pharmacy. “Extensive clinical experience with mifepristone indicates that there is no need for such restrictions,” she wrote.
Carolyn L. Westhoff, MD, is a professor of epidemiology and population and family health at Columbia University in New York. Her remarks are adapted from an accompanying editorial (N Engl J Med. 2018;378:2232-3). She reported personal fees from Planned Parenthood, Bayer, Agile Therapeutics, Cooper Surgical, Allergan, Elsevier, and personal fees and nonfinancial support from Merck.
In a randomized trial of women with early pregnancy loss, pretreatment with mifepristone before misoprostol was superior to misoprostol alone at achieving gestational sac expulsion by the time of the first follow-up visit without additional intervention.
“Women generally prefer active management; the ability to have control over the management of miscarriage may relieve some of the emotional burden that accompanies first trimester pregnancy loss,” Courtney A. Schreiber, MD, of the University of Pennsylvania, Philadelphia, and her coauthors wrote in the New England Journal of Medicine. But misoprostol (Cytotec) alone for women with a closed cervical os can require a second dose or intervention.
The trial enrolled 300 participants. Each had an ultrasound showing a nonviable intrauterine pregnancy of 5-12 weeks’ gestation. Women with an incomplete or inevitable abortion (that is, the absence of a gestational sac, an open cervical os, or both) were excluded, as misoprostol alone is effective for management of that diagnosis.
After randomization, 149 participants received 200 mg of oral mifepristone (Mifeprex), with 800 mcg misoprostol administered approximately 24 hours later. The other 151 participants received the standard 800 mcg dose of misoprostol alone. In both groups, the misoprostol was self-administered vaginally at home by inserting four 200-mcg tablets.
Follow-up came 24 hours to 4 days after misoprostol administration. The primary outcome was a gestational sac expulsion by the time of this follow-up, and no additional surgical or medical intervention within 30 days. If the gestational sac was present at follow-up, participants chose either expectant management, surgical management, or a second misoprostol dose.
The primary outcome was achieved in 124 of 148 women (83.8%; 95% confidence interval, 76.8-89.3) in the mifepristone-pretreatment group and in 100 of 149 women (67.1%; 95% CI, 59.0-74.6) in the misoprostol-alone group for a relative risk of 1.25 (95% CI, 1.09 to 1.43). Two women were lost to follow-up and one who was declared ineligible because of a possible ectopic pregnancy.
At 30 days’ follow-up, the cumulative rate of gestational sac expulsion with up to two doses of misoprostol was 91.2% (95% CI, 85.4-95.2) in the mifepristone-pretreatment group and 75.8% (95% CI, 68.2%-82.5%) in the misoprostol-alone group. Also by 30 days’ follow-up, 13 women in the mifepristone-pretreatment group and 35 women in the misoprostol-alone group had undergone uterine aspiration (relative risk, 0.37; 95% CI, 0.21-0.68).
Serious adverse events were rare in both groups, and both groups had matching mean scores for bleeding intensity and pain.
“Pretreatment with mifepristone followed by treatment with misoprostol resulted in a significantly higher rate of complete gestational sac expulsion by approximately 2 days after treatment ... [and] a significantly lower rate of uterine aspiration than misoprostol use alone,” wrote Dr. Schreiber and her coauthors. Patient satisfaction was similar between the two groups (89.4% vs. 87.4%, respectively, described their experience overall as either “good” or “neutral”).
The trial was funded by the National Institute of Child Health and Human Development. Two coauthors reported grants from the National Institutes of Health during the study and another reported personal fees from Danco Laboratories, which markets mifepristone, outside the submitted work.
SOURCE: Schreiber CA et al. N Engl J Med. 2018;378:2161-70.
In a randomized trial of women with early pregnancy loss, pretreatment with mifepristone before misoprostol was superior to misoprostol alone at achieving gestational sac expulsion by the time of the first follow-up visit without additional intervention.
“Women generally prefer active management; the ability to have control over the management of miscarriage may relieve some of the emotional burden that accompanies first trimester pregnancy loss,” Courtney A. Schreiber, MD, of the University of Pennsylvania, Philadelphia, and her coauthors wrote in the New England Journal of Medicine. But misoprostol (Cytotec) alone for women with a closed cervical os can require a second dose or intervention.
The trial enrolled 300 participants. Each had an ultrasound showing a nonviable intrauterine pregnancy of 5-12 weeks’ gestation. Women with an incomplete or inevitable abortion (that is, the absence of a gestational sac, an open cervical os, or both) were excluded, as misoprostol alone is effective for management of that diagnosis.
After randomization, 149 participants received 200 mg of oral mifepristone (Mifeprex), with 800 mcg misoprostol administered approximately 24 hours later. The other 151 participants received the standard 800 mcg dose of misoprostol alone. In both groups, the misoprostol was self-administered vaginally at home by inserting four 200-mcg tablets.
Follow-up came 24 hours to 4 days after misoprostol administration. The primary outcome was a gestational sac expulsion by the time of this follow-up, and no additional surgical or medical intervention within 30 days. If the gestational sac was present at follow-up, participants chose either expectant management, surgical management, or a second misoprostol dose.
The primary outcome was achieved in 124 of 148 women (83.8%; 95% confidence interval, 76.8-89.3) in the mifepristone-pretreatment group and in 100 of 149 women (67.1%; 95% CI, 59.0-74.6) in the misoprostol-alone group for a relative risk of 1.25 (95% CI, 1.09 to 1.43). Two women were lost to follow-up and one who was declared ineligible because of a possible ectopic pregnancy.
At 30 days’ follow-up, the cumulative rate of gestational sac expulsion with up to two doses of misoprostol was 91.2% (95% CI, 85.4-95.2) in the mifepristone-pretreatment group and 75.8% (95% CI, 68.2%-82.5%) in the misoprostol-alone group. Also by 30 days’ follow-up, 13 women in the mifepristone-pretreatment group and 35 women in the misoprostol-alone group had undergone uterine aspiration (relative risk, 0.37; 95% CI, 0.21-0.68).
Serious adverse events were rare in both groups, and both groups had matching mean scores for bleeding intensity and pain.
“Pretreatment with mifepristone followed by treatment with misoprostol resulted in a significantly higher rate of complete gestational sac expulsion by approximately 2 days after treatment ... [and] a significantly lower rate of uterine aspiration than misoprostol use alone,” wrote Dr. Schreiber and her coauthors. Patient satisfaction was similar between the two groups (89.4% vs. 87.4%, respectively, described their experience overall as either “good” or “neutral”).
The trial was funded by the National Institute of Child Health and Human Development. Two coauthors reported grants from the National Institutes of Health during the study and another reported personal fees from Danco Laboratories, which markets mifepristone, outside the submitted work.
SOURCE: Schreiber CA et al. N Engl J Med. 2018;378:2161-70.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: Gestational sac expulsion was achieved in 83.8% of the mifepristone pretreatment group and in 67.1% of the misoprostol-only group.
Study details: A randomized trial of 300 women who experienced early pregnancy loss.
Disclosures: The trial was funded by the National Institute of Child Health and Human Development. Two coauthors reported grants from the National Institutes of Health during the study and another reported personal fees from Danco Laboratories, outside the submitted work.
Source: Schreiber CA et al. N Engl J Med 2018;378:2161-70.
Trachelectomy rate for early-stage cervical cancer rises to 17% in younger women
based on a recent analysis of the National Cancer Database.
Of 15,150 patients analyzed, the vast majority (97.1%) underwent hysterectomy, but trachelectomy performance increased from 1.5% (95% confidence interval, 0.8%-2.2%; P less than .001) in 2004 to 3.8% (95% CI, 2.7%-4.8%; P less than .001) by 2014. The increase was mostly seen among women younger than 30 years old. In that group, trachelectomy increased from 4.6% (95% CI, 1.0%-8.2%; P less than .001) in 2004 to 17% (95% CI, 10.2%-23.7%; P less than .001) in 2014. Rates among women aged 30-49 years were relatively stable over the same period.
“A possible explanation for this rise in trachelectomy is the trend in delayed childbearing in women in the United States,” wrote Rosa R. Cui, MD, a resident at Columbia University, New York, and her coauthors.
In the analysis, mortality risk and 5-year survival rates were similar between the two procedures. Overall cohort 5-year survival was nearly identical with hysterectomy and trachelectomy at 92.4% and 92.3%, respectively. For stages IA2, IB1, and IB not specified, tumor stage was not associated with differences in 5-year survival for the two procedures. As few patients with stage IB2 tumors received trachelectomy, that data was excluded from the analysis.
Though increasing tumor size made trachelectomy less likely, 30% of patients in the study who underwent trachelectomy had a tumor greater than 2 cm in diameter, and 4% had a tumor greater than 4 cm in diameter. The researchers noted studies published in the past few years suggest abdominal radical trachelectomy may be a safe option for larger tumors, compared with vaginal trachelectomy. In the current analysis, they did not find a statistically significant decrease in survival for trachelectomy patients with tumors greater than 2 cm in diameter, but the sample size was small.
“The trachelectomy procedure has evolved significantly since it was initially described and now encompasses several approaches,” and can be performed more or less conservatively depending on the diagnosis “without compromising outcomes,” wrote Dr. Cui and her coauthors.
The researchers noted that the National Cancer Database does not have data on fertility outcomes, a possible focus of future studies of trachelectomy.
Two coauthors disclosed grants and a fellowship from the National Cancer Institute, and others disclosed consulting for several pharmaceutical companies including Pfizer, Teva, and Eisai.
SOURCE: Cui RR et al. Obstet Gynecol. 2018 Jun;131(6):1085-94.
based on a recent analysis of the National Cancer Database.
Of 15,150 patients analyzed, the vast majority (97.1%) underwent hysterectomy, but trachelectomy performance increased from 1.5% (95% confidence interval, 0.8%-2.2%; P less than .001) in 2004 to 3.8% (95% CI, 2.7%-4.8%; P less than .001) by 2014. The increase was mostly seen among women younger than 30 years old. In that group, trachelectomy increased from 4.6% (95% CI, 1.0%-8.2%; P less than .001) in 2004 to 17% (95% CI, 10.2%-23.7%; P less than .001) in 2014. Rates among women aged 30-49 years were relatively stable over the same period.
“A possible explanation for this rise in trachelectomy is the trend in delayed childbearing in women in the United States,” wrote Rosa R. Cui, MD, a resident at Columbia University, New York, and her coauthors.
In the analysis, mortality risk and 5-year survival rates were similar between the two procedures. Overall cohort 5-year survival was nearly identical with hysterectomy and trachelectomy at 92.4% and 92.3%, respectively. For stages IA2, IB1, and IB not specified, tumor stage was not associated with differences in 5-year survival for the two procedures. As few patients with stage IB2 tumors received trachelectomy, that data was excluded from the analysis.
Though increasing tumor size made trachelectomy less likely, 30% of patients in the study who underwent trachelectomy had a tumor greater than 2 cm in diameter, and 4% had a tumor greater than 4 cm in diameter. The researchers noted studies published in the past few years suggest abdominal radical trachelectomy may be a safe option for larger tumors, compared with vaginal trachelectomy. In the current analysis, they did not find a statistically significant decrease in survival for trachelectomy patients with tumors greater than 2 cm in diameter, but the sample size was small.
“The trachelectomy procedure has evolved significantly since it was initially described and now encompasses several approaches,” and can be performed more or less conservatively depending on the diagnosis “without compromising outcomes,” wrote Dr. Cui and her coauthors.
The researchers noted that the National Cancer Database does not have data on fertility outcomes, a possible focus of future studies of trachelectomy.
Two coauthors disclosed grants and a fellowship from the National Cancer Institute, and others disclosed consulting for several pharmaceutical companies including Pfizer, Teva, and Eisai.
SOURCE: Cui RR et al. Obstet Gynecol. 2018 Jun;131(6):1085-94.
based on a recent analysis of the National Cancer Database.
Of 15,150 patients analyzed, the vast majority (97.1%) underwent hysterectomy, but trachelectomy performance increased from 1.5% (95% confidence interval, 0.8%-2.2%; P less than .001) in 2004 to 3.8% (95% CI, 2.7%-4.8%; P less than .001) by 2014. The increase was mostly seen among women younger than 30 years old. In that group, trachelectomy increased from 4.6% (95% CI, 1.0%-8.2%; P less than .001) in 2004 to 17% (95% CI, 10.2%-23.7%; P less than .001) in 2014. Rates among women aged 30-49 years were relatively stable over the same period.
“A possible explanation for this rise in trachelectomy is the trend in delayed childbearing in women in the United States,” wrote Rosa R. Cui, MD, a resident at Columbia University, New York, and her coauthors.
In the analysis, mortality risk and 5-year survival rates were similar between the two procedures. Overall cohort 5-year survival was nearly identical with hysterectomy and trachelectomy at 92.4% and 92.3%, respectively. For stages IA2, IB1, and IB not specified, tumor stage was not associated with differences in 5-year survival for the two procedures. As few patients with stage IB2 tumors received trachelectomy, that data was excluded from the analysis.
Though increasing tumor size made trachelectomy less likely, 30% of patients in the study who underwent trachelectomy had a tumor greater than 2 cm in diameter, and 4% had a tumor greater than 4 cm in diameter. The researchers noted studies published in the past few years suggest abdominal radical trachelectomy may be a safe option for larger tumors, compared with vaginal trachelectomy. In the current analysis, they did not find a statistically significant decrease in survival for trachelectomy patients with tumors greater than 2 cm in diameter, but the sample size was small.
“The trachelectomy procedure has evolved significantly since it was initially described and now encompasses several approaches,” and can be performed more or less conservatively depending on the diagnosis “without compromising outcomes,” wrote Dr. Cui and her coauthors.
The researchers noted that the National Cancer Database does not have data on fertility outcomes, a possible focus of future studies of trachelectomy.
Two coauthors disclosed grants and a fellowship from the National Cancer Institute, and others disclosed consulting for several pharmaceutical companies including Pfizer, Teva, and Eisai.
SOURCE: Cui RR et al. Obstet Gynecol. 2018 Jun;131(6):1085-94.
FROM OBSTETRICS & GYNECOLOGY
Bladder injection may improve sexual function
An injection to the bladder may help improve sexual function along with relieving symptoms, according to a recent statistical analysis.
In a prospective observational study, 32 women with wet idiopathic overactive bladder received a 100 U/10 mL injection of onabotulinumtoxinA (onaBoNT-A) to their detrusor muscle while sedated.
The women in the study had overactive bladder syndrome with urgency urinary incontinence that was refractory to more conservative treatments. All were aged 18 years or older, sexually active, and in a relationship with the same partner for more than 3 months.
The researchers sought to distinguish the effect of the injection treatment on sexual function for women with an idiopathic, rather than neurogenic, version of the syndrome. Sexual function was assessed through a 19-item questionnaire, the Female Sexual Function Index (FSFI), before and after the treatment. To determine the efficacy of the treatment, participants kept a 3-day voiding diary, and completed two more forms: an overactive bladder screener questionnaire and the International Consultation on Incontinence Questionnaire Short Form.
Most of the participants (88.2%) saw an improvement in their overactive bladder symptoms. They also reported statistically meaningful improvement in sexual function on the FSFI, and specifically for arousal, lubrication, orgasm, and satisfaction, though not for desire and pain (average FSFI total score before and after treatment, 20.30 vs. 24.91; P = .0008).
“Although voiding diaries and questionnaires on urinary symptoms showed an improvement after onaBoNT-A injection, we documented a significant correlation only between the reduction of episodes of [urgency urinary incontinence] and improvement of FSFI total score. This finding shows that, in our population, the most relevant urinary symptom reducing the sexual function is urgency urinary incontinence,” Matteo Balzarro, MD, of Azienda Ospedaliera Universitaria Integrata of Verona, Italy, and his coauthors wrote in the European Journal of Obstetrics & Gynecology and Reproductive Biology.
The researchers noted that the small sample size resulted from multiple exclusion criteria applied to an already small population of 157 patients. They also remarked that a control group – which was absent from their study – would be difficult to have because of “ethical considerations.”
The researchers reported having no conflicts of interest.
SOURCE: Balzarro M et al. Eur J Obstet Gynecol Reprod Biol. 2018 Jun;225:228-31.
An injection to the bladder may help improve sexual function along with relieving symptoms, according to a recent statistical analysis.
In a prospective observational study, 32 women with wet idiopathic overactive bladder received a 100 U/10 mL injection of onabotulinumtoxinA (onaBoNT-A) to their detrusor muscle while sedated.
The women in the study had overactive bladder syndrome with urgency urinary incontinence that was refractory to more conservative treatments. All were aged 18 years or older, sexually active, and in a relationship with the same partner for more than 3 months.
The researchers sought to distinguish the effect of the injection treatment on sexual function for women with an idiopathic, rather than neurogenic, version of the syndrome. Sexual function was assessed through a 19-item questionnaire, the Female Sexual Function Index (FSFI), before and after the treatment. To determine the efficacy of the treatment, participants kept a 3-day voiding diary, and completed two more forms: an overactive bladder screener questionnaire and the International Consultation on Incontinence Questionnaire Short Form.
Most of the participants (88.2%) saw an improvement in their overactive bladder symptoms. They also reported statistically meaningful improvement in sexual function on the FSFI, and specifically for arousal, lubrication, orgasm, and satisfaction, though not for desire and pain (average FSFI total score before and after treatment, 20.30 vs. 24.91; P = .0008).
“Although voiding diaries and questionnaires on urinary symptoms showed an improvement after onaBoNT-A injection, we documented a significant correlation only between the reduction of episodes of [urgency urinary incontinence] and improvement of FSFI total score. This finding shows that, in our population, the most relevant urinary symptom reducing the sexual function is urgency urinary incontinence,” Matteo Balzarro, MD, of Azienda Ospedaliera Universitaria Integrata of Verona, Italy, and his coauthors wrote in the European Journal of Obstetrics & Gynecology and Reproductive Biology.
The researchers noted that the small sample size resulted from multiple exclusion criteria applied to an already small population of 157 patients. They also remarked that a control group – which was absent from their study – would be difficult to have because of “ethical considerations.”
The researchers reported having no conflicts of interest.
SOURCE: Balzarro M et al. Eur J Obstet Gynecol Reprod Biol. 2018 Jun;225:228-31.
An injection to the bladder may help improve sexual function along with relieving symptoms, according to a recent statistical analysis.
In a prospective observational study, 32 women with wet idiopathic overactive bladder received a 100 U/10 mL injection of onabotulinumtoxinA (onaBoNT-A) to their detrusor muscle while sedated.
The women in the study had overactive bladder syndrome with urgency urinary incontinence that was refractory to more conservative treatments. All were aged 18 years or older, sexually active, and in a relationship with the same partner for more than 3 months.
The researchers sought to distinguish the effect of the injection treatment on sexual function for women with an idiopathic, rather than neurogenic, version of the syndrome. Sexual function was assessed through a 19-item questionnaire, the Female Sexual Function Index (FSFI), before and after the treatment. To determine the efficacy of the treatment, participants kept a 3-day voiding diary, and completed two more forms: an overactive bladder screener questionnaire and the International Consultation on Incontinence Questionnaire Short Form.
Most of the participants (88.2%) saw an improvement in their overactive bladder symptoms. They also reported statistically meaningful improvement in sexual function on the FSFI, and specifically for arousal, lubrication, orgasm, and satisfaction, though not for desire and pain (average FSFI total score before and after treatment, 20.30 vs. 24.91; P = .0008).
“Although voiding diaries and questionnaires on urinary symptoms showed an improvement after onaBoNT-A injection, we documented a significant correlation only between the reduction of episodes of [urgency urinary incontinence] and improvement of FSFI total score. This finding shows that, in our population, the most relevant urinary symptom reducing the sexual function is urgency urinary incontinence,” Matteo Balzarro, MD, of Azienda Ospedaliera Universitaria Integrata of Verona, Italy, and his coauthors wrote in the European Journal of Obstetrics & Gynecology and Reproductive Biology.
The researchers noted that the small sample size resulted from multiple exclusion criteria applied to an already small population of 157 patients. They also remarked that a control group – which was absent from their study – would be difficult to have because of “ethical considerations.”
The researchers reported having no conflicts of interest.
SOURCE: Balzarro M et al. Eur J Obstet Gynecol Reprod Biol. 2018 Jun;225:228-31.
FROM THE EUROPEAN JOURNAL OF OBSTETRICS & GYNECOLOGY AND REPRODUCTIVE BIOLOGY
First antidepressant use not tied to first abortion
Women who have had an abortion are more likely to use antidepressants than women who have not had an abortion, but new research suggests that this association is a result of differences in risk factors for depression.
“Thus, policies based on the notion that abortion harms women’s mental health may be misinformed,” wrote Julia R. Steinberg, PhD, and her coauthors in JAMA Psychiatry.
Dr. Steinberg and her coauthors looked at a cohort of Danish women, intending to examine the association between first-time antidepressant use and either first-trimester abortion or first childbirth. “One shortcoming of many studies in the field is their reliance on self-report of both abortion and mental health problems, which is subject to both faulty memory and social desirability in reporting,” wrote Dr. Steinberg of the University of Maryland, College Park, and her coauthors. Using data on abortion, childbirth, and antidepressants from the Danish population registries, which were collected over time, avoided that limitation.
Of the 396,397 women, 17,294 (4.4%) had at least one first-trimester abortion and no children, 72,052 (18.2%) had no abortions and at least one childbirth, 13,540 (3.4%) had at least one abortion and at least one childbirth, and 293,511 (74.1%) had neither an abortion nor a childbirth.
Of 30,834 women who had an abortion and filled at least one antidepressant prescription, 5,705 (18.5%) initiated antidepressant use after a first abortion. Of 85,592 women who gave birth and filled at least one antidepressant prescription, 10,825 (12.7%) initiated antidepressant use after a first childbirth.
The researchers were limited to 2-month increments of incidence rates for patient confidentiality reasons.
While women who had an abortion were more likely than women who had not to obtain an antidepressant prescription, “the rate of new antidepressant use was the same in the year before and year after and decreased with increasing time after the abortion,” the researchers wrote. “ after the abortion.”
The strongest risk factors for initiating antidepressant use were indicators for earlier mental health problems, such as a previous psychiatric contact. The authors speculated that mental health problems may lead women to have unintended pregnancies and therefore abortions, as Kelli Stidham Hall, PhD, and associates discussed (Soc Sci Med. 2014 Jan;0:62-71).
The combination of the absence of a postprocedure increase in antidepressant use, the gradual decrease in their use over time, and the lack of statistical significance of the incidence rate ratios when adjusted for risk factors led Dr. Steinberg and her coauthors to conclude that “compared with women who do not have an abortion, women who have an abortion may be at higher risk of depression after undergoing the procedure because they were at higher risk to begin with.”
Dr. Steinberg disclosed that she has served as a scientific expert on the topic of abortion and mental health in legal cases and has consulted for the Center for Reproductive Rights and Planned Parenthood Federation of America. The study was supported by grants from the Society of Family Planning, the American Foundation for Suicide Prevention, and the Lundbeck Foundation Initiative for Integrative Psychiatric Research.
SOURCE: Steinberg JR et al. JAMA Psychiatry. 2018 May 30. doi: 10.1001/jamapsychiatry.2018.0849.
The study by Julia R. Steinberg, PhD, and her associates adds to the body of evidence showing that abortion is not associated with an increased risk of mental disorders, wrote Nada L. Stotland, MD, and Angela D. Shrestha, MD, in an editorial accompanying the article in JAMA Psychiatry (2018 May 30. doi: 10.1001/jamapsychiatry.2018.0838).
“The authors report that, compared with women who had not had an abortion, women who had a first abortion had a higher risk of first-time antidepressant prescription,” Dr. Stotland and Dr. Shrestha wrote. “However, the risk of first-time antidepressant prescription was similar to the year before and after an abortion. Giving birth was associated with a lower likelihood of a prescription, but this likelihood rose after childbirth and continued to rise for 5 years after delivery.”
Dr. Stotland and Dr. Shrestha also praised the methodology used by Dr. Steinberg and her associates, particularly the decision to make pregnant women who choose to remain pregnant a control group. However, women who opt to continue their pregnancies are more likely to have supportive and healthy circumstances that influence them to make that decision, Dr. Stotland and Dr. Shrestha said.
The decision to have an abortion is fraught with complexities. Ultimately, clinicians must recognize that abortions are indeed significant events for women, and offer them both accurate information and nonjudgmental support, they wrote.
Dr. Stotland is affiliated with Rush University in Chicago and the University of Illinois at Chicago. Dr. Shrestha also is affiliated with the University of Illinois at Chicago. They reported no conflicts of interest.
The study by Julia R. Steinberg, PhD, and her associates adds to the body of evidence showing that abortion is not associated with an increased risk of mental disorders, wrote Nada L. Stotland, MD, and Angela D. Shrestha, MD, in an editorial accompanying the article in JAMA Psychiatry (2018 May 30. doi: 10.1001/jamapsychiatry.2018.0838).
“The authors report that, compared with women who had not had an abortion, women who had a first abortion had a higher risk of first-time antidepressant prescription,” Dr. Stotland and Dr. Shrestha wrote. “However, the risk of first-time antidepressant prescription was similar to the year before and after an abortion. Giving birth was associated with a lower likelihood of a prescription, but this likelihood rose after childbirth and continued to rise for 5 years after delivery.”
Dr. Stotland and Dr. Shrestha also praised the methodology used by Dr. Steinberg and her associates, particularly the decision to make pregnant women who choose to remain pregnant a control group. However, women who opt to continue their pregnancies are more likely to have supportive and healthy circumstances that influence them to make that decision, Dr. Stotland and Dr. Shrestha said.
The decision to have an abortion is fraught with complexities. Ultimately, clinicians must recognize that abortions are indeed significant events for women, and offer them both accurate information and nonjudgmental support, they wrote.
Dr. Stotland is affiliated with Rush University in Chicago and the University of Illinois at Chicago. Dr. Shrestha also is affiliated with the University of Illinois at Chicago. They reported no conflicts of interest.
The study by Julia R. Steinberg, PhD, and her associates adds to the body of evidence showing that abortion is not associated with an increased risk of mental disorders, wrote Nada L. Stotland, MD, and Angela D. Shrestha, MD, in an editorial accompanying the article in JAMA Psychiatry (2018 May 30. doi: 10.1001/jamapsychiatry.2018.0838).
“The authors report that, compared with women who had not had an abortion, women who had a first abortion had a higher risk of first-time antidepressant prescription,” Dr. Stotland and Dr. Shrestha wrote. “However, the risk of first-time antidepressant prescription was similar to the year before and after an abortion. Giving birth was associated with a lower likelihood of a prescription, but this likelihood rose after childbirth and continued to rise for 5 years after delivery.”
Dr. Stotland and Dr. Shrestha also praised the methodology used by Dr. Steinberg and her associates, particularly the decision to make pregnant women who choose to remain pregnant a control group. However, women who opt to continue their pregnancies are more likely to have supportive and healthy circumstances that influence them to make that decision, Dr. Stotland and Dr. Shrestha said.
The decision to have an abortion is fraught with complexities. Ultimately, clinicians must recognize that abortions are indeed significant events for women, and offer them both accurate information and nonjudgmental support, they wrote.
Dr. Stotland is affiliated with Rush University in Chicago and the University of Illinois at Chicago. Dr. Shrestha also is affiliated with the University of Illinois at Chicago. They reported no conflicts of interest.
Women who have had an abortion are more likely to use antidepressants than women who have not had an abortion, but new research suggests that this association is a result of differences in risk factors for depression.
“Thus, policies based on the notion that abortion harms women’s mental health may be misinformed,” wrote Julia R. Steinberg, PhD, and her coauthors in JAMA Psychiatry.
Dr. Steinberg and her coauthors looked at a cohort of Danish women, intending to examine the association between first-time antidepressant use and either first-trimester abortion or first childbirth. “One shortcoming of many studies in the field is their reliance on self-report of both abortion and mental health problems, which is subject to both faulty memory and social desirability in reporting,” wrote Dr. Steinberg of the University of Maryland, College Park, and her coauthors. Using data on abortion, childbirth, and antidepressants from the Danish population registries, which were collected over time, avoided that limitation.
Of the 396,397 women, 17,294 (4.4%) had at least one first-trimester abortion and no children, 72,052 (18.2%) had no abortions and at least one childbirth, 13,540 (3.4%) had at least one abortion and at least one childbirth, and 293,511 (74.1%) had neither an abortion nor a childbirth.
Of 30,834 women who had an abortion and filled at least one antidepressant prescription, 5,705 (18.5%) initiated antidepressant use after a first abortion. Of 85,592 women who gave birth and filled at least one antidepressant prescription, 10,825 (12.7%) initiated antidepressant use after a first childbirth.
The researchers were limited to 2-month increments of incidence rates for patient confidentiality reasons.
While women who had an abortion were more likely than women who had not to obtain an antidepressant prescription, “the rate of new antidepressant use was the same in the year before and year after and decreased with increasing time after the abortion,” the researchers wrote. “ after the abortion.”
The strongest risk factors for initiating antidepressant use were indicators for earlier mental health problems, such as a previous psychiatric contact. The authors speculated that mental health problems may lead women to have unintended pregnancies and therefore abortions, as Kelli Stidham Hall, PhD, and associates discussed (Soc Sci Med. 2014 Jan;0:62-71).
The combination of the absence of a postprocedure increase in antidepressant use, the gradual decrease in their use over time, and the lack of statistical significance of the incidence rate ratios when adjusted for risk factors led Dr. Steinberg and her coauthors to conclude that “compared with women who do not have an abortion, women who have an abortion may be at higher risk of depression after undergoing the procedure because they were at higher risk to begin with.”
Dr. Steinberg disclosed that she has served as a scientific expert on the topic of abortion and mental health in legal cases and has consulted for the Center for Reproductive Rights and Planned Parenthood Federation of America. The study was supported by grants from the Society of Family Planning, the American Foundation for Suicide Prevention, and the Lundbeck Foundation Initiative for Integrative Psychiatric Research.
SOURCE: Steinberg JR et al. JAMA Psychiatry. 2018 May 30. doi: 10.1001/jamapsychiatry.2018.0849.
Women who have had an abortion are more likely to use antidepressants than women who have not had an abortion, but new research suggests that this association is a result of differences in risk factors for depression.
“Thus, policies based on the notion that abortion harms women’s mental health may be misinformed,” wrote Julia R. Steinberg, PhD, and her coauthors in JAMA Psychiatry.
Dr. Steinberg and her coauthors looked at a cohort of Danish women, intending to examine the association between first-time antidepressant use and either first-trimester abortion or first childbirth. “One shortcoming of many studies in the field is their reliance on self-report of both abortion and mental health problems, which is subject to both faulty memory and social desirability in reporting,” wrote Dr. Steinberg of the University of Maryland, College Park, and her coauthors. Using data on abortion, childbirth, and antidepressants from the Danish population registries, which were collected over time, avoided that limitation.
Of the 396,397 women, 17,294 (4.4%) had at least one first-trimester abortion and no children, 72,052 (18.2%) had no abortions and at least one childbirth, 13,540 (3.4%) had at least one abortion and at least one childbirth, and 293,511 (74.1%) had neither an abortion nor a childbirth.
Of 30,834 women who had an abortion and filled at least one antidepressant prescription, 5,705 (18.5%) initiated antidepressant use after a first abortion. Of 85,592 women who gave birth and filled at least one antidepressant prescription, 10,825 (12.7%) initiated antidepressant use after a first childbirth.
The researchers were limited to 2-month increments of incidence rates for patient confidentiality reasons.
While women who had an abortion were more likely than women who had not to obtain an antidepressant prescription, “the rate of new antidepressant use was the same in the year before and year after and decreased with increasing time after the abortion,” the researchers wrote. “ after the abortion.”
The strongest risk factors for initiating antidepressant use were indicators for earlier mental health problems, such as a previous psychiatric contact. The authors speculated that mental health problems may lead women to have unintended pregnancies and therefore abortions, as Kelli Stidham Hall, PhD, and associates discussed (Soc Sci Med. 2014 Jan;0:62-71).
The combination of the absence of a postprocedure increase in antidepressant use, the gradual decrease in their use over time, and the lack of statistical significance of the incidence rate ratios when adjusted for risk factors led Dr. Steinberg and her coauthors to conclude that “compared with women who do not have an abortion, women who have an abortion may be at higher risk of depression after undergoing the procedure because they were at higher risk to begin with.”
Dr. Steinberg disclosed that she has served as a scientific expert on the topic of abortion and mental health in legal cases and has consulted for the Center for Reproductive Rights and Planned Parenthood Federation of America. The study was supported by grants from the Society of Family Planning, the American Foundation for Suicide Prevention, and the Lundbeck Foundation Initiative for Integrative Psychiatric Research.
SOURCE: Steinberg JR et al. JAMA Psychiatry. 2018 May 30. doi: 10.1001/jamapsychiatry.2018.0849.
FROM JAMA PSYCHIATRY
FDA approves estradiol vaginal inserts for dyspareunia*
, in a 4-mcg and 10-mcg dose. The 4-mcg dose is a lower dose than any currently available.
The hormone treatment is intended for dyspareunia resulting from menopausal vulvar and vaginal atrophy. The patient places a soft gel capsule in the lower part of the vagina, daily for 2 weeks, then at a reduced rate of twice per week. The capsule dissolves and reintroduces estrogen to the tissue.
The manufacturer of the product, TherapeuticsMD, has committed to conduct a postapproval observational study, as a condition of approval.
Estradiol comes with a boxed warning of risks of endometrial cancer, stroke, deep vein thrombosis, pulmonary embolism, myocardial infarction, breast cancer, and “probable dementia.” The most common adverse reaction to the estradiol vaginal inserts was headache.
Editor's Note: This article has been corrected to state that the 4-mcg dose showed significant improvement in severity of dyspareunia.
[email protected]
, in a 4-mcg and 10-mcg dose. The 4-mcg dose is a lower dose than any currently available.
The hormone treatment is intended for dyspareunia resulting from menopausal vulvar and vaginal atrophy. The patient places a soft gel capsule in the lower part of the vagina, daily for 2 weeks, then at a reduced rate of twice per week. The capsule dissolves and reintroduces estrogen to the tissue.
The manufacturer of the product, TherapeuticsMD, has committed to conduct a postapproval observational study, as a condition of approval.
Estradiol comes with a boxed warning of risks of endometrial cancer, stroke, deep vein thrombosis, pulmonary embolism, myocardial infarction, breast cancer, and “probable dementia.” The most common adverse reaction to the estradiol vaginal inserts was headache.
Editor's Note: This article has been corrected to state that the 4-mcg dose showed significant improvement in severity of dyspareunia.
[email protected]
, in a 4-mcg and 10-mcg dose. The 4-mcg dose is a lower dose than any currently available.
The hormone treatment is intended for dyspareunia resulting from menopausal vulvar and vaginal atrophy. The patient places a soft gel capsule in the lower part of the vagina, daily for 2 weeks, then at a reduced rate of twice per week. The capsule dissolves and reintroduces estrogen to the tissue.
The manufacturer of the product, TherapeuticsMD, has committed to conduct a postapproval observational study, as a condition of approval.
Estradiol comes with a boxed warning of risks of endometrial cancer, stroke, deep vein thrombosis, pulmonary embolism, myocardial infarction, breast cancer, and “probable dementia.” The most common adverse reaction to the estradiol vaginal inserts was headache.
Editor's Note: This article has been corrected to state that the 4-mcg dose showed significant improvement in severity of dyspareunia.
[email protected]