User login
Don't rule out liver transplant grafts from octogenarians
Donors aged 80 years or older are not necessarily inferior for a liver transplantation (LT) graft, compared with young ideal donors (aged 18-39 years), according to an analysis of the perioperative LT period.
While “the potential risks and benefits associated with the use of livers from octogenarian donors must be closely weighed, with careful donor evaluation, selective donor-to-recipient matching and skilled perioperative care, octogenarian grafts do not affect the short-term course of patients undergoing LT,” concluded Gianni Biancofiore, MD, of Azienda Ospedaliera-Universitaria Pisana, Pisa, Italy, and his coauthors (Dig Liver Dis. 2017. doi: 10.1016/j.dld.2017.01.149).
Perioperative differences were insubstantial in terms of cardiovascular complications (P = .2), respiratory complications (P = 1.0), coagulopathy (P = .5), and incidence of perfusion syndrome (P = .3). Median ICU length of stay of the two groups was identical (P = .4). No differences in terms of death or retransplant were observed during the ICU stay.
“Accordingly, anesthesiologists and intensivists should not label liver allografts from donors aged 80 years [or older] as ‘unusable’ or ‘high risk’ ” based on age alone, the authors concluded.
The authors declared no sources of funding and no conflicts of interest.
Donors aged 80 years or older are not necessarily inferior for a liver transplantation (LT) graft, compared with young ideal donors (aged 18-39 years), according to an analysis of the perioperative LT period.
While “the potential risks and benefits associated with the use of livers from octogenarian donors must be closely weighed, with careful donor evaluation, selective donor-to-recipient matching and skilled perioperative care, octogenarian grafts do not affect the short-term course of patients undergoing LT,” concluded Gianni Biancofiore, MD, of Azienda Ospedaliera-Universitaria Pisana, Pisa, Italy, and his coauthors (Dig Liver Dis. 2017. doi: 10.1016/j.dld.2017.01.149).
Perioperative differences were insubstantial in terms of cardiovascular complications (P = .2), respiratory complications (P = 1.0), coagulopathy (P = .5), and incidence of perfusion syndrome (P = .3). Median ICU length of stay of the two groups was identical (P = .4). No differences in terms of death or retransplant were observed during the ICU stay.
“Accordingly, anesthesiologists and intensivists should not label liver allografts from donors aged 80 years [or older] as ‘unusable’ or ‘high risk’ ” based on age alone, the authors concluded.
The authors declared no sources of funding and no conflicts of interest.
Donors aged 80 years or older are not necessarily inferior for a liver transplantation (LT) graft, compared with young ideal donors (aged 18-39 years), according to an analysis of the perioperative LT period.
While “the potential risks and benefits associated with the use of livers from octogenarian donors must be closely weighed, with careful donor evaluation, selective donor-to-recipient matching and skilled perioperative care, octogenarian grafts do not affect the short-term course of patients undergoing LT,” concluded Gianni Biancofiore, MD, of Azienda Ospedaliera-Universitaria Pisana, Pisa, Italy, and his coauthors (Dig Liver Dis. 2017. doi: 10.1016/j.dld.2017.01.149).
Perioperative differences were insubstantial in terms of cardiovascular complications (P = .2), respiratory complications (P = 1.0), coagulopathy (P = .5), and incidence of perfusion syndrome (P = .3). Median ICU length of stay of the two groups was identical (P = .4). No differences in terms of death or retransplant were observed during the ICU stay.
“Accordingly, anesthesiologists and intensivists should not label liver allografts from donors aged 80 years [or older] as ‘unusable’ or ‘high risk’ ” based on age alone, the authors concluded.
The authors declared no sources of funding and no conflicts of interest.
FROM DIGESTIVE AND LIVER DISEASE
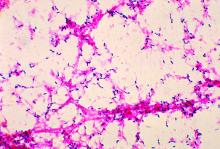
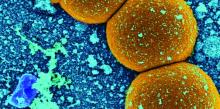
In ICU, pair MRSA testing method with isolation protocol
An ICU’s method of testing for methicillin-resistant Staphylococcus aureus (MRSA) should be paired with its patient isolation policy, according to researchers at the University of Colorado at Denver.
In an ICU with all patients preemptively isolated, it is worth the added expense to opt for the polymerase chain reaction (PCR) test – which generates results in a few hours – so that patients negative for the infection can be moved out of isolation more quickly, wrote Melanie D. Whittington, PhD, and her coauthors. But if the ICU is only isolating MRSA-positive patients, the authors instead recommend the less expensive but slower chromogenic agar 24-hour testing.
The other two MRSA tests the researchers assessed – conventional culture and chromogenic agar 48-hour testing – are less expensive. But when paired with either ICU isolation policy, those tests lead to excessive inappropriate isolation costs while waiting for the results, the study investigators cautioned (Am J Infect Control. 2017 Jan 23. doi: 10.1016/j.ajic.2016.12.014).
Adding together the cost per patient of the test, the “appropriate isolation costs,” and “inappropriate isolation costs,” the universal isolation policy is least expensive per patient with PCR, at $82.51 per patient. With conventional culture, which can take several days, this cost ballooned to $290.11 per patient, with high inappropriate isolation costs.
Doing the same math with the more targeted isolation policy, the least expensive screening method was the 24-hour chromogenic agar, at $8.54 per patient, while the expense of the PCR test made it the most expensive method when paired with this isolation policy, at $30.95 per patient.
“With knowledge of the screening test that minimizes inappropriate and total costs, hospitals can maximize the efficiency of their resource use and improve the health of their patients,” Dr. Whittington and her coauthors wrote.
The authors reported no conflicts of interest.
An ICU’s method of testing for methicillin-resistant Staphylococcus aureus (MRSA) should be paired with its patient isolation policy, according to researchers at the University of Colorado at Denver.
In an ICU with all patients preemptively isolated, it is worth the added expense to opt for the polymerase chain reaction (PCR) test – which generates results in a few hours – so that patients negative for the infection can be moved out of isolation more quickly, wrote Melanie D. Whittington, PhD, and her coauthors. But if the ICU is only isolating MRSA-positive patients, the authors instead recommend the less expensive but slower chromogenic agar 24-hour testing.
The other two MRSA tests the researchers assessed – conventional culture and chromogenic agar 48-hour testing – are less expensive. But when paired with either ICU isolation policy, those tests lead to excessive inappropriate isolation costs while waiting for the results, the study investigators cautioned (Am J Infect Control. 2017 Jan 23. doi: 10.1016/j.ajic.2016.12.014).
Adding together the cost per patient of the test, the “appropriate isolation costs,” and “inappropriate isolation costs,” the universal isolation policy is least expensive per patient with PCR, at $82.51 per patient. With conventional culture, which can take several days, this cost ballooned to $290.11 per patient, with high inappropriate isolation costs.
Doing the same math with the more targeted isolation policy, the least expensive screening method was the 24-hour chromogenic agar, at $8.54 per patient, while the expense of the PCR test made it the most expensive method when paired with this isolation policy, at $30.95 per patient.
“With knowledge of the screening test that minimizes inappropriate and total costs, hospitals can maximize the efficiency of their resource use and improve the health of their patients,” Dr. Whittington and her coauthors wrote.
The authors reported no conflicts of interest.
An ICU’s method of testing for methicillin-resistant Staphylococcus aureus (MRSA) should be paired with its patient isolation policy, according to researchers at the University of Colorado at Denver.
In an ICU with all patients preemptively isolated, it is worth the added expense to opt for the polymerase chain reaction (PCR) test – which generates results in a few hours – so that patients negative for the infection can be moved out of isolation more quickly, wrote Melanie D. Whittington, PhD, and her coauthors. But if the ICU is only isolating MRSA-positive patients, the authors instead recommend the less expensive but slower chromogenic agar 24-hour testing.
The other two MRSA tests the researchers assessed – conventional culture and chromogenic agar 48-hour testing – are less expensive. But when paired with either ICU isolation policy, those tests lead to excessive inappropriate isolation costs while waiting for the results, the study investigators cautioned (Am J Infect Control. 2017 Jan 23. doi: 10.1016/j.ajic.2016.12.014).
Adding together the cost per patient of the test, the “appropriate isolation costs,” and “inappropriate isolation costs,” the universal isolation policy is least expensive per patient with PCR, at $82.51 per patient. With conventional culture, which can take several days, this cost ballooned to $290.11 per patient, with high inappropriate isolation costs.
Doing the same math with the more targeted isolation policy, the least expensive screening method was the 24-hour chromogenic agar, at $8.54 per patient, while the expense of the PCR test made it the most expensive method when paired with this isolation policy, at $30.95 per patient.
“With knowledge of the screening test that minimizes inappropriate and total costs, hospitals can maximize the efficiency of their resource use and improve the health of their patients,” Dr. Whittington and her coauthors wrote.
The authors reported no conflicts of interest.
Researchers find ‘feedback loop’ key to reducing high blood pressure
Research with mice and rats in Germany may have found a new way to treat high blood pressure.
Using epifluorescence intravital video microscopy imaging, researchers examined mice to whom they had given angiotensin II hormones to induce arterial hypertension.
They determined that the mice with low levels of thrombin-driven factor XI (FXI) – either naturally or inhibited by antisense oligonucleotides – had healthier endothelium.
“Specificity of the effects of FXI depletion was confirmed by continuous in vivo supplementation with human FXI,” wrote Sabine Kossmann, PhD, of the Center for Thrombosis and Hemostasis, University Medical Center, Mainz (Germany), and her coauthors (Sci Transl Med. 2017 Feb 1. doi: 10.1126/scitranslmed.aah4923).
Targeting the “feedback loop” between the FXI and a receptor that helps thrombin propagate on platelets reduced both vascular inflammation and blood pressure.
“Our findings suggest that inhibiting the ... thrombin-FXI–amplifying loop may provide added cardiovascular benefits that are synergistic with those of established platelet inhibitors,” the authors wrote.
This work was supported by grants from the Stiftung Pathobiochemie und Molekulare Diagnostik and the Federal Ministry of Education and Research. The authors disclosed funding and grants from the German Research Society, the European Research Council, NIH, and other sources. One of the researchers is inventor of five patents related to the FXI inhibitor and equity holder in Aronora, and may have financial interest in the findings of the research.
Research with mice and rats in Germany may have found a new way to treat high blood pressure.
Using epifluorescence intravital video microscopy imaging, researchers examined mice to whom they had given angiotensin II hormones to induce arterial hypertension.
They determined that the mice with low levels of thrombin-driven factor XI (FXI) – either naturally or inhibited by antisense oligonucleotides – had healthier endothelium.
“Specificity of the effects of FXI depletion was confirmed by continuous in vivo supplementation with human FXI,” wrote Sabine Kossmann, PhD, of the Center for Thrombosis and Hemostasis, University Medical Center, Mainz (Germany), and her coauthors (Sci Transl Med. 2017 Feb 1. doi: 10.1126/scitranslmed.aah4923).
Targeting the “feedback loop” between the FXI and a receptor that helps thrombin propagate on platelets reduced both vascular inflammation and blood pressure.
“Our findings suggest that inhibiting the ... thrombin-FXI–amplifying loop may provide added cardiovascular benefits that are synergistic with those of established platelet inhibitors,” the authors wrote.
This work was supported by grants from the Stiftung Pathobiochemie und Molekulare Diagnostik and the Federal Ministry of Education and Research. The authors disclosed funding and grants from the German Research Society, the European Research Council, NIH, and other sources. One of the researchers is inventor of five patents related to the FXI inhibitor and equity holder in Aronora, and may have financial interest in the findings of the research.
Research with mice and rats in Germany may have found a new way to treat high blood pressure.
Using epifluorescence intravital video microscopy imaging, researchers examined mice to whom they had given angiotensin II hormones to induce arterial hypertension.
They determined that the mice with low levels of thrombin-driven factor XI (FXI) – either naturally or inhibited by antisense oligonucleotides – had healthier endothelium.
“Specificity of the effects of FXI depletion was confirmed by continuous in vivo supplementation with human FXI,” wrote Sabine Kossmann, PhD, of the Center for Thrombosis and Hemostasis, University Medical Center, Mainz (Germany), and her coauthors (Sci Transl Med. 2017 Feb 1. doi: 10.1126/scitranslmed.aah4923).
Targeting the “feedback loop” between the FXI and a receptor that helps thrombin propagate on platelets reduced both vascular inflammation and blood pressure.
“Our findings suggest that inhibiting the ... thrombin-FXI–amplifying loop may provide added cardiovascular benefits that are synergistic with those of established platelet inhibitors,” the authors wrote.
This work was supported by grants from the Stiftung Pathobiochemie und Molekulare Diagnostik and the Federal Ministry of Education and Research. The authors disclosed funding and grants from the German Research Society, the European Research Council, NIH, and other sources. One of the researchers is inventor of five patents related to the FXI inhibitor and equity holder in Aronora, and may have financial interest in the findings of the research.
FROM SCIENCE TRANSLATIONAL MEDICINE
Older women with remitted depression show attention bias for negative information
Older women with a history of major depressive disorder are more likely to direct their attention to negative images than women without history of MDD, researchers report. The findings follow previous research showing that individuals currently depressed or at-risk show a similar attention bias.
The current study examined 33 postmenopausal women aged 45-75 years with an emotion dot probe (EDP) task combined with fMRI scans, in addition to cognitive and depression history screening and several self-rated measures.
“We examined resting-state functional connectivity before the EDP task to assess differences in intrinsic amygdala functional connections to other brain areas between the groups,” wrote Kimberly Albert, PhD, of Vanderbilt University, Nashville, Tenn., and her coauthors (J Affect Disord. 2017 Mar 1;210:49-52).
The women in the study with a history of MDD showed greater attention facilitation to negative images, greater amygdala activity, and greater amygdala-hippocampal functional connectivity than women without a history of MDD.
“Attention bias for negative information can be seen in individuals with past MDD without inducing a negative mood state. Attention bias for negative information may be an ongoing vulnerability for MDD recurrence independent of mood state,” Dr. Albert and her coauthors wrote.
Older women with a history of major depressive disorder are more likely to direct their attention to negative images than women without history of MDD, researchers report. The findings follow previous research showing that individuals currently depressed or at-risk show a similar attention bias.
The current study examined 33 postmenopausal women aged 45-75 years with an emotion dot probe (EDP) task combined with fMRI scans, in addition to cognitive and depression history screening and several self-rated measures.
“We examined resting-state functional connectivity before the EDP task to assess differences in intrinsic amygdala functional connections to other brain areas between the groups,” wrote Kimberly Albert, PhD, of Vanderbilt University, Nashville, Tenn., and her coauthors (J Affect Disord. 2017 Mar 1;210:49-52).
The women in the study with a history of MDD showed greater attention facilitation to negative images, greater amygdala activity, and greater amygdala-hippocampal functional connectivity than women without a history of MDD.
“Attention bias for negative information can be seen in individuals with past MDD without inducing a negative mood state. Attention bias for negative information may be an ongoing vulnerability for MDD recurrence independent of mood state,” Dr. Albert and her coauthors wrote.
Older women with a history of major depressive disorder are more likely to direct their attention to negative images than women without history of MDD, researchers report. The findings follow previous research showing that individuals currently depressed or at-risk show a similar attention bias.
The current study examined 33 postmenopausal women aged 45-75 years with an emotion dot probe (EDP) task combined with fMRI scans, in addition to cognitive and depression history screening and several self-rated measures.
“We examined resting-state functional connectivity before the EDP task to assess differences in intrinsic amygdala functional connections to other brain areas between the groups,” wrote Kimberly Albert, PhD, of Vanderbilt University, Nashville, Tenn., and her coauthors (J Affect Disord. 2017 Mar 1;210:49-52).
The women in the study with a history of MDD showed greater attention facilitation to negative images, greater amygdala activity, and greater amygdala-hippocampal functional connectivity than women without a history of MDD.
“Attention bias for negative information can be seen in individuals with past MDD without inducing a negative mood state. Attention bias for negative information may be an ongoing vulnerability for MDD recurrence independent of mood state,” Dr. Albert and her coauthors wrote.
FROM THE JOURNAL OF AFFECTIVE DISORDERS
Don’t delay pneumococcal conjugate vaccine for preterm infants
There should be no hesitation in administering the routine vaccination schedule for 13-valent pneumococcal conjugate vaccine (PCV13) on account of gestational age or birth weight in preterm infants, researchers concluded.
In a phase IV study, researchers compared 100 term with 100 preterm infants; both groups were vaccinated on the routine schedule at ages 2, 3, 4, and 12 months. After the 12-month (toddler) dose of the PCV13, the infants were evaluated for serum antibody persistence at 12 and 24 months. “To date, no studies have examined the long-term persistence of immune responses to PCV13 in formerly preterm infants,” noted Federico Martinón-Torres, MD, PhD, of Hospital Clínico Universitario de Santiago de Compostela, Spain, and his coauthors.
In the study, at six sites in Spain and five sites in Poland between October 2010 and January 2014, both groups were checked for geometric mean concentrations of serotype-specific anticapsular immunoglobulin G binding antibodies and for opsonophagocytic activity. All 200 subjects were white and were generally healthy; the preterm infants were grouped by gestational age at birth of less than 29 weeks (n = 25), 29 weeks to less than 32 weeks (n = 50), or 32 weeks to less than 37 weeks (n = 25). Twelve subjects dropped out of the study by the first year’s evaluation, and another eight of the term subjects and seven of preterm subjects dropped out by the second year’s evaluation (Ped Infect Dis J. 2017. doi: 10.1097/INF.0000000000001428).
At both follow-up time points, no discernible patterns were observed in IgG GMCs for any serotype or in opsonophagocytic activity geometric mean titers across preterm subgroups based on gestational age.
“The vaccination phase of the study demonstrated that preterm infants are able to generate an immune response to PCV13 that is likely to protect against invasive pneumococcal disease. However, IgG GMCs were lower in preterm than term infants for nearly half of the serotypes at all time points. Antipneumococcal IgG levels in preterm infants were generally lower than in term infants, but fewer differences in opsonophagocytic activity were seen between the groups,” Dr. Martinón-Torres and his associates reported.
Pfizer funded the study. Dr. Martinón-Torres reported receiving research grants and/or honoraria as a consultant/adviser and/or speaker and for conducting vaccine trials for GlaxoSmithKline, MedImmune, Merck, Novartis, Pfizer/Wyeth, Sanofi Pasteur, and the Carlos III Health Institute. Several coauthors disclosed ties with pharmaceutical companies; four are stock-holding employees of Pfizer and another is an employee of a company contracted by Pfizer.
There should be no hesitation in administering the routine vaccination schedule for 13-valent pneumococcal conjugate vaccine (PCV13) on account of gestational age or birth weight in preterm infants, researchers concluded.
In a phase IV study, researchers compared 100 term with 100 preterm infants; both groups were vaccinated on the routine schedule at ages 2, 3, 4, and 12 months. After the 12-month (toddler) dose of the PCV13, the infants were evaluated for serum antibody persistence at 12 and 24 months. “To date, no studies have examined the long-term persistence of immune responses to PCV13 in formerly preterm infants,” noted Federico Martinón-Torres, MD, PhD, of Hospital Clínico Universitario de Santiago de Compostela, Spain, and his coauthors.
In the study, at six sites in Spain and five sites in Poland between October 2010 and January 2014, both groups were checked for geometric mean concentrations of serotype-specific anticapsular immunoglobulin G binding antibodies and for opsonophagocytic activity. All 200 subjects were white and were generally healthy; the preterm infants were grouped by gestational age at birth of less than 29 weeks (n = 25), 29 weeks to less than 32 weeks (n = 50), or 32 weeks to less than 37 weeks (n = 25). Twelve subjects dropped out of the study by the first year’s evaluation, and another eight of the term subjects and seven of preterm subjects dropped out by the second year’s evaluation (Ped Infect Dis J. 2017. doi: 10.1097/INF.0000000000001428).
At both follow-up time points, no discernible patterns were observed in IgG GMCs for any serotype or in opsonophagocytic activity geometric mean titers across preterm subgroups based on gestational age.
“The vaccination phase of the study demonstrated that preterm infants are able to generate an immune response to PCV13 that is likely to protect against invasive pneumococcal disease. However, IgG GMCs were lower in preterm than term infants for nearly half of the serotypes at all time points. Antipneumococcal IgG levels in preterm infants were generally lower than in term infants, but fewer differences in opsonophagocytic activity were seen between the groups,” Dr. Martinón-Torres and his associates reported.
Pfizer funded the study. Dr. Martinón-Torres reported receiving research grants and/or honoraria as a consultant/adviser and/or speaker and for conducting vaccine trials for GlaxoSmithKline, MedImmune, Merck, Novartis, Pfizer/Wyeth, Sanofi Pasteur, and the Carlos III Health Institute. Several coauthors disclosed ties with pharmaceutical companies; four are stock-holding employees of Pfizer and another is an employee of a company contracted by Pfizer.
There should be no hesitation in administering the routine vaccination schedule for 13-valent pneumococcal conjugate vaccine (PCV13) on account of gestational age or birth weight in preterm infants, researchers concluded.
In a phase IV study, researchers compared 100 term with 100 preterm infants; both groups were vaccinated on the routine schedule at ages 2, 3, 4, and 12 months. After the 12-month (toddler) dose of the PCV13, the infants were evaluated for serum antibody persistence at 12 and 24 months. “To date, no studies have examined the long-term persistence of immune responses to PCV13 in formerly preterm infants,” noted Federico Martinón-Torres, MD, PhD, of Hospital Clínico Universitario de Santiago de Compostela, Spain, and his coauthors.
In the study, at six sites in Spain and five sites in Poland between October 2010 and January 2014, both groups were checked for geometric mean concentrations of serotype-specific anticapsular immunoglobulin G binding antibodies and for opsonophagocytic activity. All 200 subjects were white and were generally healthy; the preterm infants were grouped by gestational age at birth of less than 29 weeks (n = 25), 29 weeks to less than 32 weeks (n = 50), or 32 weeks to less than 37 weeks (n = 25). Twelve subjects dropped out of the study by the first year’s evaluation, and another eight of the term subjects and seven of preterm subjects dropped out by the second year’s evaluation (Ped Infect Dis J. 2017. doi: 10.1097/INF.0000000000001428).
At both follow-up time points, no discernible patterns were observed in IgG GMCs for any serotype or in opsonophagocytic activity geometric mean titers across preterm subgroups based on gestational age.
“The vaccination phase of the study demonstrated that preterm infants are able to generate an immune response to PCV13 that is likely to protect against invasive pneumococcal disease. However, IgG GMCs were lower in preterm than term infants for nearly half of the serotypes at all time points. Antipneumococcal IgG levels in preterm infants were generally lower than in term infants, but fewer differences in opsonophagocytic activity were seen between the groups,” Dr. Martinón-Torres and his associates reported.
Pfizer funded the study. Dr. Martinón-Torres reported receiving research grants and/or honoraria as a consultant/adviser and/or speaker and for conducting vaccine trials for GlaxoSmithKline, MedImmune, Merck, Novartis, Pfizer/Wyeth, Sanofi Pasteur, and the Carlos III Health Institute. Several coauthors disclosed ties with pharmaceutical companies; four are stock-holding employees of Pfizer and another is an employee of a company contracted by Pfizer.
Key clinical point:
Major finding: IgG GMCs were lower in preterm than term infants for nearly half of the serotypes at all time points. Antipneumococcal IgG levels in preterm infants were generally lower than in term infants, but fewer differences in opsonophagocytic activity were seen between the groups.
Data source: In a phase IV study, 100 term and 100 preterm infants were evaluated for serum antibody persistence at 12 and 24 months.
Disclosures: Pfizer funded the study. Dr. Martinón-Torres reported receiving research grants and/or honoraria as a consultant/adviser and/or speaker and for conducting vaccine trials for GlaxoSmithKline, MedImmune, Merck, Novartis, Pfizer/Wyeth, Sanofi Pasteur, and the Carlos III Health Institute. Several coauthors disclosed ties with pharmaceutical companies; four are stock-holding employees of Pfizer and another is an employee of a company contracted by Pfizer.
FDA approves Trulance for chronic idiopathic constipation
Trulance, a once-daily oral medication for chronic idiopathic constipation, has been approved by the Food and Drug Administration for adult patients as of Jan. 19.
Manufactured by Synergy Pharmaceuticals, Trulance (plecanatide) stimulates intestinal fluid secretion in the upper GI tract. Its efficacy and safety were determined to be sufficient in two 12-week placebo-controlled trials (NCT01982240 and NCT02122471). Participants taking Trulance were more likely than were those taking placebo to have improved bowel function and stool.
The FDA’s statement noted that “an estimated 42 million people are affected by constipation. Chronic idiopathic constipation is a diagnosis given to those who experience persistent constipation and for whom there is no structural or biochemical explanation.”
Trulance, a once-daily oral medication for chronic idiopathic constipation, has been approved by the Food and Drug Administration for adult patients as of Jan. 19.
Manufactured by Synergy Pharmaceuticals, Trulance (plecanatide) stimulates intestinal fluid secretion in the upper GI tract. Its efficacy and safety were determined to be sufficient in two 12-week placebo-controlled trials (NCT01982240 and NCT02122471). Participants taking Trulance were more likely than were those taking placebo to have improved bowel function and stool.
The FDA’s statement noted that “an estimated 42 million people are affected by constipation. Chronic idiopathic constipation is a diagnosis given to those who experience persistent constipation and for whom there is no structural or biochemical explanation.”
Trulance, a once-daily oral medication for chronic idiopathic constipation, has been approved by the Food and Drug Administration for adult patients as of Jan. 19.
Manufactured by Synergy Pharmaceuticals, Trulance (plecanatide) stimulates intestinal fluid secretion in the upper GI tract. Its efficacy and safety were determined to be sufficient in two 12-week placebo-controlled trials (NCT01982240 and NCT02122471). Participants taking Trulance were more likely than were those taking placebo to have improved bowel function and stool.
The FDA’s statement noted that “an estimated 42 million people are affected by constipation. Chronic idiopathic constipation is a diagnosis given to those who experience persistent constipation and for whom there is no structural or biochemical explanation.”
VA MRSA Prevention Initiative reports continued health care–associated infection declines
The U.S. Department of Veterans Affairs MRSA Prevention Initiative, implemented in October 2007, has shown progress at limiting health care–associated infections of methicillin-resistant Staphylococcus aureus through 2011 and 2012.
A new report published in the January 2017 issue of the American Journal of Infection Control tracks continued declines in infection through September 2015.
Monthly rates of health care–associated infections fell significantly in all settings from October 2007 to September 2015: an 87% decrease in ICUs, 80.1% in non-ICUs, 80.9% in spinal cord injury units, and 49.4% in long-term care facilities (P for all less than .0001).
“The VA data suggest that active surveillance followed by contact precautions (with or without decolonization) may be most useful when MRSA [health care–associated infection] rates are unacceptably high (as they were in VA facilities during 2007) or to decrease infections in high-risk units such as ICUs,” Dr. Evans and his colleagues concluded.
Details about the implementation of the initiative were previously published in the New England Journal of Medicine in 2011, including the initiative’s goal to promote “a change in the institutional culture whereby infection control would become the responsibility of everyone who had contact with patients” (N Engl J Med. 2011;364:1419-30).
Dr. Evans and his colleagues had no relevant financial disclosures.
The U.S. Department of Veterans Affairs MRSA Prevention Initiative, implemented in October 2007, has shown progress at limiting health care–associated infections of methicillin-resistant Staphylococcus aureus through 2011 and 2012.
A new report published in the January 2017 issue of the American Journal of Infection Control tracks continued declines in infection through September 2015.
Monthly rates of health care–associated infections fell significantly in all settings from October 2007 to September 2015: an 87% decrease in ICUs, 80.1% in non-ICUs, 80.9% in spinal cord injury units, and 49.4% in long-term care facilities (P for all less than .0001).
“The VA data suggest that active surveillance followed by contact precautions (with or without decolonization) may be most useful when MRSA [health care–associated infection] rates are unacceptably high (as they were in VA facilities during 2007) or to decrease infections in high-risk units such as ICUs,” Dr. Evans and his colleagues concluded.
Details about the implementation of the initiative were previously published in the New England Journal of Medicine in 2011, including the initiative’s goal to promote “a change in the institutional culture whereby infection control would become the responsibility of everyone who had contact with patients” (N Engl J Med. 2011;364:1419-30).
Dr. Evans and his colleagues had no relevant financial disclosures.
The U.S. Department of Veterans Affairs MRSA Prevention Initiative, implemented in October 2007, has shown progress at limiting health care–associated infections of methicillin-resistant Staphylococcus aureus through 2011 and 2012.
A new report published in the January 2017 issue of the American Journal of Infection Control tracks continued declines in infection through September 2015.
Monthly rates of health care–associated infections fell significantly in all settings from October 2007 to September 2015: an 87% decrease in ICUs, 80.1% in non-ICUs, 80.9% in spinal cord injury units, and 49.4% in long-term care facilities (P for all less than .0001).
“The VA data suggest that active surveillance followed by contact precautions (with or without decolonization) may be most useful when MRSA [health care–associated infection] rates are unacceptably high (as they were in VA facilities during 2007) or to decrease infections in high-risk units such as ICUs,” Dr. Evans and his colleagues concluded.
Details about the implementation of the initiative were previously published in the New England Journal of Medicine in 2011, including the initiative’s goal to promote “a change in the institutional culture whereby infection control would become the responsibility of everyone who had contact with patients” (N Engl J Med. 2011;364:1419-30).
Dr. Evans and his colleagues had no relevant financial disclosures.
FROM THE AMERICAN JOURNAL OF INFECTION CONTROL
Screen opioid users for depression, study recommends
Depression combined with chronic opioid analgesic use involves more symptoms and comorbidities than depression without chronic opioid use, according to a study of Department of Veterans Affairs patients seen between 2000 and 2012.
“Screening and treatment of depression in non–cancer pain patients may limit risk of persistent mood disorder and subsequent suicidal ideation,” wrote Jeffrey F. Scherrer, PhD, and his coauthors. “Opioid prescribing for pain management should be coupled with careful screening and treatment of emerging depression.”
“Eligible patients were cancer free, HIV free. ... Because we were interested in characterizing severity of new-onset [new depression episodes] and not predictors of NDE, we measured incident substance use and psychiatric comorbidities that occurred at the same time or after NDE. Therefore, eligible patients were free of psychiatric and substance use disorders before NDE. Patients whose opioid use began after NDE and patients without NDE in follow-up were excluded,” wrote Dr. Scherrer of Saint Louis University and his coauthors (J Affect Disord. 2017 Mar 1;210:125-9).
This process left the researchers with a sample size of 4,758 patients. Of those, 4,314 developed NDE without receiving an opioid, while the remaining 444 developed NDE after opioid use of more than 90 days.
Looking at raw figures prior to the application of inverse probability of treatment weighting (IPTW), the opioid use group was more likely than was the nonopioid use group to have comorbid posttraumatic stress disorder (17.3% vs. 11.9%), opioid (4.3% vs. 0.5%) and other drug abuse/dependence (11.3% vs. 4.8%), all pain-related conditions, obesity (48.2% vs. 37.4%), and nicotine abuse/dependence (52.5% vs. 30.5%). The further calculations were made “to assess whether differences between the groups were irrespective of pain-related variables.”
With IPTW adjustments made, the differences in pain-related comorbidities went away. Opioid-using patients had higher depression severity as measured by Patient Health Questionnaire–9 scores (P = .012). They also were more likely to have had antidepressant treatment for at least 12 weeks (P less than .0001). Nonopioid use patients were more likely to have anxiety disorders other than PTSD (P = .014).
Dr. Scherrer had no conflicts of interest. The study received funding support from the National Institute of Mental Health. The views reflected in the article are those of the authors and not necessarily those of the VA, the researchers reported.
Depression combined with chronic opioid analgesic use involves more symptoms and comorbidities than depression without chronic opioid use, according to a study of Department of Veterans Affairs patients seen between 2000 and 2012.
“Screening and treatment of depression in non–cancer pain patients may limit risk of persistent mood disorder and subsequent suicidal ideation,” wrote Jeffrey F. Scherrer, PhD, and his coauthors. “Opioid prescribing for pain management should be coupled with careful screening and treatment of emerging depression.”
“Eligible patients were cancer free, HIV free. ... Because we were interested in characterizing severity of new-onset [new depression episodes] and not predictors of NDE, we measured incident substance use and psychiatric comorbidities that occurred at the same time or after NDE. Therefore, eligible patients were free of psychiatric and substance use disorders before NDE. Patients whose opioid use began after NDE and patients without NDE in follow-up were excluded,” wrote Dr. Scherrer of Saint Louis University and his coauthors (J Affect Disord. 2017 Mar 1;210:125-9).
This process left the researchers with a sample size of 4,758 patients. Of those, 4,314 developed NDE without receiving an opioid, while the remaining 444 developed NDE after opioid use of more than 90 days.
Looking at raw figures prior to the application of inverse probability of treatment weighting (IPTW), the opioid use group was more likely than was the nonopioid use group to have comorbid posttraumatic stress disorder (17.3% vs. 11.9%), opioid (4.3% vs. 0.5%) and other drug abuse/dependence (11.3% vs. 4.8%), all pain-related conditions, obesity (48.2% vs. 37.4%), and nicotine abuse/dependence (52.5% vs. 30.5%). The further calculations were made “to assess whether differences between the groups were irrespective of pain-related variables.”
With IPTW adjustments made, the differences in pain-related comorbidities went away. Opioid-using patients had higher depression severity as measured by Patient Health Questionnaire–9 scores (P = .012). They also were more likely to have had antidepressant treatment for at least 12 weeks (P less than .0001). Nonopioid use patients were more likely to have anxiety disorders other than PTSD (P = .014).
Dr. Scherrer had no conflicts of interest. The study received funding support from the National Institute of Mental Health. The views reflected in the article are those of the authors and not necessarily those of the VA, the researchers reported.
Depression combined with chronic opioid analgesic use involves more symptoms and comorbidities than depression without chronic opioid use, according to a study of Department of Veterans Affairs patients seen between 2000 and 2012.
“Screening and treatment of depression in non–cancer pain patients may limit risk of persistent mood disorder and subsequent suicidal ideation,” wrote Jeffrey F. Scherrer, PhD, and his coauthors. “Opioid prescribing for pain management should be coupled with careful screening and treatment of emerging depression.”
“Eligible patients were cancer free, HIV free. ... Because we were interested in characterizing severity of new-onset [new depression episodes] and not predictors of NDE, we measured incident substance use and psychiatric comorbidities that occurred at the same time or after NDE. Therefore, eligible patients were free of psychiatric and substance use disorders before NDE. Patients whose opioid use began after NDE and patients without NDE in follow-up were excluded,” wrote Dr. Scherrer of Saint Louis University and his coauthors (J Affect Disord. 2017 Mar 1;210:125-9).
This process left the researchers with a sample size of 4,758 patients. Of those, 4,314 developed NDE without receiving an opioid, while the remaining 444 developed NDE after opioid use of more than 90 days.
Looking at raw figures prior to the application of inverse probability of treatment weighting (IPTW), the opioid use group was more likely than was the nonopioid use group to have comorbid posttraumatic stress disorder (17.3% vs. 11.9%), opioid (4.3% vs. 0.5%) and other drug abuse/dependence (11.3% vs. 4.8%), all pain-related conditions, obesity (48.2% vs. 37.4%), and nicotine abuse/dependence (52.5% vs. 30.5%). The further calculations were made “to assess whether differences between the groups were irrespective of pain-related variables.”
With IPTW adjustments made, the differences in pain-related comorbidities went away. Opioid-using patients had higher depression severity as measured by Patient Health Questionnaire–9 scores (P = .012). They also were more likely to have had antidepressant treatment for at least 12 weeks (P less than .0001). Nonopioid use patients were more likely to have anxiety disorders other than PTSD (P = .014).
Dr. Scherrer had no conflicts of interest. The study received funding support from the National Institute of Mental Health. The views reflected in the article are those of the authors and not necessarily those of the VA, the researchers reported.
Meningococcal conjugate vaccination may be associated with increased risk of Bell’s palsy
A postlicensure safety study of a meningococcal conjugate vaccine in Southern California has shown that the vaccine may be associated with an increase in the risk of Bell’s palsy, but only if the vaccine is taken concomitantly with another vaccine.
Researchers set out to evaluate the safety of one quadrivalent meningococcal conjugate vaccine, MenACWY-CRM. Two MenACWY vaccines are currently licensed in the United States; MenACWY-D is the other. The vaccines underwent studies on the road to approval, but researchers saw an absence of data about how the vaccine was faring in routine clinical use.
Researchers looked through the electronic health records of the study population for “26 prespecified events of interest (EOIs) under investigation, including neurologic, rheumatologic, hematologic, endocrine, renal, pediatric, and pediatric infectious disease EOIs. Occurrence of incident episodes of these EOIs was identified during a 1-year observation period after the index vaccination for each individual.”
They identified 4,240 EOIs, but dismissed 3,000 of them as probable preexisting conditions. With what was left, some of the EOIs did not occur at all (such as Guillain-Barré syndrome, myasthenia gravis, or systemic lupus erythematosus). Of transverse myelitis and autoimmune hemolytic anemia, among others, there was only 1 case.
Seizure, iridocyclitis, Hashimoto’s disease, and anaphylaxis initially showed statistically significant risk incidence, but were all ruled out (of the hypothesis of possible cause by vaccination) by further review from a physician investigator.
But in the case of Bell’s palsy, the independent case review committee did not rule out the possibility that the MenACWY-CRM vaccine increased the risk incidence of the condition.
However, the increased risk was present only for subjects who received a concomitant vaccine along with the MenACWY-CRM, such as Tdap, influenza, or human papillomavirus vaccine. “Stratified analyses demonstrated an increased risk for Bell’s palsy in subjects receiving concomitant vaccines (risk incidence, 5.0; 95% confidence interval, 1.4-17.8), and no increased risk for those without concomitant vaccine (RI, 1.1; 95% CI, 0.2-5.5),” Dr. Tseng and his coauthors wrote. All eight cases of Bell’s palsy resolved completely.
They concluded, “we observed a temporal association between occurrence of Bell’s palsy and receipt of MenACWY-CRM concomitantly with other vaccines. The association needs further investigation because it could be due to chance, concomitant vaccination, or underlying medical history predisposing to Bell’s palsy.”
Dr. Tseng and numerous coauthors reported receiving research support from Novartis Vaccines, the sponsor of the study. Three coauthors were employees of Novartis at the time of the study.
A postlicensure safety study of a meningococcal conjugate vaccine in Southern California has shown that the vaccine may be associated with an increase in the risk of Bell’s palsy, but only if the vaccine is taken concomitantly with another vaccine.
Researchers set out to evaluate the safety of one quadrivalent meningococcal conjugate vaccine, MenACWY-CRM. Two MenACWY vaccines are currently licensed in the United States; MenACWY-D is the other. The vaccines underwent studies on the road to approval, but researchers saw an absence of data about how the vaccine was faring in routine clinical use.
Researchers looked through the electronic health records of the study population for “26 prespecified events of interest (EOIs) under investigation, including neurologic, rheumatologic, hematologic, endocrine, renal, pediatric, and pediatric infectious disease EOIs. Occurrence of incident episodes of these EOIs was identified during a 1-year observation period after the index vaccination for each individual.”
They identified 4,240 EOIs, but dismissed 3,000 of them as probable preexisting conditions. With what was left, some of the EOIs did not occur at all (such as Guillain-Barré syndrome, myasthenia gravis, or systemic lupus erythematosus). Of transverse myelitis and autoimmune hemolytic anemia, among others, there was only 1 case.
Seizure, iridocyclitis, Hashimoto’s disease, and anaphylaxis initially showed statistically significant risk incidence, but were all ruled out (of the hypothesis of possible cause by vaccination) by further review from a physician investigator.
But in the case of Bell’s palsy, the independent case review committee did not rule out the possibility that the MenACWY-CRM vaccine increased the risk incidence of the condition.
However, the increased risk was present only for subjects who received a concomitant vaccine along with the MenACWY-CRM, such as Tdap, influenza, or human papillomavirus vaccine. “Stratified analyses demonstrated an increased risk for Bell’s palsy in subjects receiving concomitant vaccines (risk incidence, 5.0; 95% confidence interval, 1.4-17.8), and no increased risk for those without concomitant vaccine (RI, 1.1; 95% CI, 0.2-5.5),” Dr. Tseng and his coauthors wrote. All eight cases of Bell’s palsy resolved completely.
They concluded, “we observed a temporal association between occurrence of Bell’s palsy and receipt of MenACWY-CRM concomitantly with other vaccines. The association needs further investigation because it could be due to chance, concomitant vaccination, or underlying medical history predisposing to Bell’s palsy.”
Dr. Tseng and numerous coauthors reported receiving research support from Novartis Vaccines, the sponsor of the study. Three coauthors were employees of Novartis at the time of the study.
A postlicensure safety study of a meningococcal conjugate vaccine in Southern California has shown that the vaccine may be associated with an increase in the risk of Bell’s palsy, but only if the vaccine is taken concomitantly with another vaccine.
Researchers set out to evaluate the safety of one quadrivalent meningococcal conjugate vaccine, MenACWY-CRM. Two MenACWY vaccines are currently licensed in the United States; MenACWY-D is the other. The vaccines underwent studies on the road to approval, but researchers saw an absence of data about how the vaccine was faring in routine clinical use.
Researchers looked through the electronic health records of the study population for “26 prespecified events of interest (EOIs) under investigation, including neurologic, rheumatologic, hematologic, endocrine, renal, pediatric, and pediatric infectious disease EOIs. Occurrence of incident episodes of these EOIs was identified during a 1-year observation period after the index vaccination for each individual.”
They identified 4,240 EOIs, but dismissed 3,000 of them as probable preexisting conditions. With what was left, some of the EOIs did not occur at all (such as Guillain-Barré syndrome, myasthenia gravis, or systemic lupus erythematosus). Of transverse myelitis and autoimmune hemolytic anemia, among others, there was only 1 case.
Seizure, iridocyclitis, Hashimoto’s disease, and anaphylaxis initially showed statistically significant risk incidence, but were all ruled out (of the hypothesis of possible cause by vaccination) by further review from a physician investigator.
But in the case of Bell’s palsy, the independent case review committee did not rule out the possibility that the MenACWY-CRM vaccine increased the risk incidence of the condition.
However, the increased risk was present only for subjects who received a concomitant vaccine along with the MenACWY-CRM, such as Tdap, influenza, or human papillomavirus vaccine. “Stratified analyses demonstrated an increased risk for Bell’s palsy in subjects receiving concomitant vaccines (risk incidence, 5.0; 95% confidence interval, 1.4-17.8), and no increased risk for those without concomitant vaccine (RI, 1.1; 95% CI, 0.2-5.5),” Dr. Tseng and his coauthors wrote. All eight cases of Bell’s palsy resolved completely.
They concluded, “we observed a temporal association between occurrence of Bell’s palsy and receipt of MenACWY-CRM concomitantly with other vaccines. The association needs further investigation because it could be due to chance, concomitant vaccination, or underlying medical history predisposing to Bell’s palsy.”
Dr. Tseng and numerous coauthors reported receiving research support from Novartis Vaccines, the sponsor of the study. Three coauthors were employees of Novartis at the time of the study.
More evidence shows ties between early inflammation, schizophrenia risk in adulthood
Increases in inflammatory markers during acute psychosis suggest that higher C-reactive protein levels in adolescence may play an important role in subsequent schizophrenia by age 27, but more study is needed, results from a longitudinal study suggest.
“Inflammatory pathways may offer important new prevention and intervention targets for schizophrenia,” wrote Stephen A. Metcalf of the University of Cambridge (England) and his coauthors, most of whom are based in Finland (Brain Behav Immun. 2017 Jan;59:253-9).
The birth cohort consisted of 99% of the live births in two northern Finland provinces between July 1985 and June 1986. Investigators studied 6,362 individuals within the cohort who had gone on to have their blood sampled at age 15 or 16 years and measured for levels of serum C-reactive protein (CRP).
Increased levels of CRP are associated with antipsychotic-naive first-episode psychosis and acute psychotic relapse. However, “it is difficult to ascertain the direction of association between inflammation and schizophrenia from cross-sectional data. Longitudinal studies of inflammatory markers and subsequent psychotic illness are scarce but are necessary to establish whether the increase in circulating inflammatory markers is a cause or consequence of illness,” wrote Mr. Metcalf and his coauthors.
The investigators searched Finnish hospital records for cases and ICD-10 diagnoses of nonaffective psychosis, including schizophrenia, for the years 1994 to 2012 for CRP-measured members of the birth cohort, spanning ages 8-27 years. With the records collected, they sorted the participants for analysis into the following three groups: schizophrenia (n = 22), nonschizophrenia nonaffective psychosis (n = 66), and no psychosis (n = 6,274).
“The adjusted [odds ratio] for schizophrenia by age 27 years for each standard deviation increase in CRP levels at age 15/16 years was 1.25 (95% confidence interval, 1.07-1.46), which was consistent with a linear, dose-response relationship (P = 0.23),” Mr. Metcalf and his coauthors wrote. Participants with high levels of CRP at baseline (greater than 3 mg/L), compared with low levels (less than 1 mg/L), were more likely to develop schizophrenia (adjusted OR, 4.25; 95% CI, 1.30-13.93).
The investigators adjusted their regression models for age, sex, body mass index, maternal education, smoking, and alcohol use. “To exclude reverse causality (i.e., schizophrenia leading to elevated CRP), we repeated the analyses after removing participants who had developed schizophrenia within one year of CRP assay.”
The findings build on those from a longitudinal study in Denmark on increased risks for schizophrenia associated with higher CRP levels (Schizophr Bull. 2014 Sep;40[5]:1117-27). The authors cautioned that the current findings must be replicated elsewhere.
The authors disclosed several individual funding sources, but none played a role in the study.
Increases in inflammatory markers during acute psychosis suggest that higher C-reactive protein levels in adolescence may play an important role in subsequent schizophrenia by age 27, but more study is needed, results from a longitudinal study suggest.
“Inflammatory pathways may offer important new prevention and intervention targets for schizophrenia,” wrote Stephen A. Metcalf of the University of Cambridge (England) and his coauthors, most of whom are based in Finland (Brain Behav Immun. 2017 Jan;59:253-9).
The birth cohort consisted of 99% of the live births in two northern Finland provinces between July 1985 and June 1986. Investigators studied 6,362 individuals within the cohort who had gone on to have their blood sampled at age 15 or 16 years and measured for levels of serum C-reactive protein (CRP).
Increased levels of CRP are associated with antipsychotic-naive first-episode psychosis and acute psychotic relapse. However, “it is difficult to ascertain the direction of association between inflammation and schizophrenia from cross-sectional data. Longitudinal studies of inflammatory markers and subsequent psychotic illness are scarce but are necessary to establish whether the increase in circulating inflammatory markers is a cause or consequence of illness,” wrote Mr. Metcalf and his coauthors.
The investigators searched Finnish hospital records for cases and ICD-10 diagnoses of nonaffective psychosis, including schizophrenia, for the years 1994 to 2012 for CRP-measured members of the birth cohort, spanning ages 8-27 years. With the records collected, they sorted the participants for analysis into the following three groups: schizophrenia (n = 22), nonschizophrenia nonaffective psychosis (n = 66), and no psychosis (n = 6,274).
“The adjusted [odds ratio] for schizophrenia by age 27 years for each standard deviation increase in CRP levels at age 15/16 years was 1.25 (95% confidence interval, 1.07-1.46), which was consistent with a linear, dose-response relationship (P = 0.23),” Mr. Metcalf and his coauthors wrote. Participants with high levels of CRP at baseline (greater than 3 mg/L), compared with low levels (less than 1 mg/L), were more likely to develop schizophrenia (adjusted OR, 4.25; 95% CI, 1.30-13.93).
The investigators adjusted their regression models for age, sex, body mass index, maternal education, smoking, and alcohol use. “To exclude reverse causality (i.e., schizophrenia leading to elevated CRP), we repeated the analyses after removing participants who had developed schizophrenia within one year of CRP assay.”
The findings build on those from a longitudinal study in Denmark on increased risks for schizophrenia associated with higher CRP levels (Schizophr Bull. 2014 Sep;40[5]:1117-27). The authors cautioned that the current findings must be replicated elsewhere.
The authors disclosed several individual funding sources, but none played a role in the study.
Increases in inflammatory markers during acute psychosis suggest that higher C-reactive protein levels in adolescence may play an important role in subsequent schizophrenia by age 27, but more study is needed, results from a longitudinal study suggest.
“Inflammatory pathways may offer important new prevention and intervention targets for schizophrenia,” wrote Stephen A. Metcalf of the University of Cambridge (England) and his coauthors, most of whom are based in Finland (Brain Behav Immun. 2017 Jan;59:253-9).
The birth cohort consisted of 99% of the live births in two northern Finland provinces between July 1985 and June 1986. Investigators studied 6,362 individuals within the cohort who had gone on to have their blood sampled at age 15 or 16 years and measured for levels of serum C-reactive protein (CRP).
Increased levels of CRP are associated with antipsychotic-naive first-episode psychosis and acute psychotic relapse. However, “it is difficult to ascertain the direction of association between inflammation and schizophrenia from cross-sectional data. Longitudinal studies of inflammatory markers and subsequent psychotic illness are scarce but are necessary to establish whether the increase in circulating inflammatory markers is a cause or consequence of illness,” wrote Mr. Metcalf and his coauthors.
The investigators searched Finnish hospital records for cases and ICD-10 diagnoses of nonaffective psychosis, including schizophrenia, for the years 1994 to 2012 for CRP-measured members of the birth cohort, spanning ages 8-27 years. With the records collected, they sorted the participants for analysis into the following three groups: schizophrenia (n = 22), nonschizophrenia nonaffective psychosis (n = 66), and no psychosis (n = 6,274).
“The adjusted [odds ratio] for schizophrenia by age 27 years for each standard deviation increase in CRP levels at age 15/16 years was 1.25 (95% confidence interval, 1.07-1.46), which was consistent with a linear, dose-response relationship (P = 0.23),” Mr. Metcalf and his coauthors wrote. Participants with high levels of CRP at baseline (greater than 3 mg/L), compared with low levels (less than 1 mg/L), were more likely to develop schizophrenia (adjusted OR, 4.25; 95% CI, 1.30-13.93).
The investigators adjusted their regression models for age, sex, body mass index, maternal education, smoking, and alcohol use. “To exclude reverse causality (i.e., schizophrenia leading to elevated CRP), we repeated the analyses after removing participants who had developed schizophrenia within one year of CRP assay.”
The findings build on those from a longitudinal study in Denmark on increased risks for schizophrenia associated with higher CRP levels (Schizophr Bull. 2014 Sep;40[5]:1117-27). The authors cautioned that the current findings must be replicated elsewhere.
The authors disclosed several individual funding sources, but none played a role in the study.
FROM BRAIN, BEHAVIOR, AND IMMUNITY