User login
Providers need protocols in place to better treat transgender youth
WASHINGTON – Practices and clinics should implement cultural humility training and gender protocols for dealing with transgender youth because many of these youth and their parents find health care experiences to be difficult when procedures for treating and interacting with transgender youth are confusing or nonexistent.
The study is part of an ongoing effort to “provide high-quality, respectful health care for transgender youth [because] these youth are at greatly increased risk of issues including substance abuse, depression, anxiety, homelessness, and suicide,” explained Julia M. Crouch of Seattle Children’s Research Institute.
“A growing body of evidence shows improved health outcomes for transgender youth who received support from family, schools, and providers, and there are now an increasing number of multidisciplinary gender clinics throughout the country [that] have been demonstrated to be a feasible and effective way to provide coordinated care to this population,” Ms. Crouch said at the annual meeting of the Society for Adolescent Health and Medicine.
Ms. Crouch and her coinvestigators recruited transgender youth between the ages of 14 and 22 years, along with parents of transgender youth, all of whom were evaluated and enrolled from the Seattle metropolitan area. Both parents and youth were given the option of participating in either a semistructured interview or a focus group discussion, during which investigators learned about the concerns and experiences of both youth and parents when visiting their health care clinics (J Adolesc Health. 2011 Apr;48[4]:351-7; J Adolesc Health. 2011 Apr;48(4):351-7)..
In total, 13 youth and 16 parents – the latter of whom were not made up of 8 pairs of parents, but rather 16 individual parents of transgender youth who were not necessarily the same 13 youth recruited for the study – were eventually selected for inclusion. The parents split evenly between opting for interviews and focus groups, while four of the youth chose interviews and the remaining nine chose focus groups. Seven youth identified themselves as male, three identified as female, and the remaining three identified as “genderqueer or gender fluid.”
Analysis of interview and focus group conversations identified six key “barriers to care” that Ms. Crouch and her coauthors call necessary to rectify in order to improve the quality of health care provided to transgender youth. These are:
• The dearth of health care providers with sufficient knowledge and interest in working with transgender youth.
• The lack of access to pubertal blockers and cross-sex hormones.
• Doctors and their staff who are unable or unwilling to use the names and pronouns that youths prefer to go by.
• Patients being made to feel uncomfortable or “not normal” by health care providers,
• The lack of a set protocol or treatment methodology for dealing with transgender youth.
• The lack of coordination between health care providers and specialties on treating transgender youth – specifically, a lack of cohesive care between mental and medical health care.
“ ‘It was hard enough to find providers who were accepting new patients, worked with adolescents and my insurance, [and] on top of it, finding someone who was transfriendly made it all but impossible,’ ” Ms. Crouch recalled one transgender youth saying during the study.
Ms. Crouch also recounted that providers’ inability to consistently use the correct pronoun when talking about or to a transgender patient was harmful, and despite most instances being dismissed as unintentional, several were said to be intentional and malicious.
“For example, one parent told us [their] doctor said, ‘her, her, her,’ and [her] son, who was 10 years old, said, ‘him, him, him,’ and the doctor got mad, became dismissive and irritated, and kept saying ‘her,’ ” said Ms. Crouch.
The average age of the youth was 18 years, and of the parents was 49 years. The parents were 88% white and 75% female, with 44% holding at least a college degree. Most of the youth were white (69%), and 77% had either completed high school or some college. Youth and parents were recruited in 2015 from local clinics in the Seattle area, as well as through local and national listservs. Thirty-three percent of the parents were from outside the state of Washington.
The study was funded by the Center for Diversity and Health Equity, and the Clinical and Translational Research Faculty Research Support Fund, at Seattle Children’s Research Institute. Ms. Crouch did not report any relevant financial disclosures.
WASHINGTON – Practices and clinics should implement cultural humility training and gender protocols for dealing with transgender youth because many of these youth and their parents find health care experiences to be difficult when procedures for treating and interacting with transgender youth are confusing or nonexistent.
The study is part of an ongoing effort to “provide high-quality, respectful health care for transgender youth [because] these youth are at greatly increased risk of issues including substance abuse, depression, anxiety, homelessness, and suicide,” explained Julia M. Crouch of Seattle Children’s Research Institute.
“A growing body of evidence shows improved health outcomes for transgender youth who received support from family, schools, and providers, and there are now an increasing number of multidisciplinary gender clinics throughout the country [that] have been demonstrated to be a feasible and effective way to provide coordinated care to this population,” Ms. Crouch said at the annual meeting of the Society for Adolescent Health and Medicine.
Ms. Crouch and her coinvestigators recruited transgender youth between the ages of 14 and 22 years, along with parents of transgender youth, all of whom were evaluated and enrolled from the Seattle metropolitan area. Both parents and youth were given the option of participating in either a semistructured interview or a focus group discussion, during which investigators learned about the concerns and experiences of both youth and parents when visiting their health care clinics (J Adolesc Health. 2011 Apr;48[4]:351-7; J Adolesc Health. 2011 Apr;48(4):351-7)..
In total, 13 youth and 16 parents – the latter of whom were not made up of 8 pairs of parents, but rather 16 individual parents of transgender youth who were not necessarily the same 13 youth recruited for the study – were eventually selected for inclusion. The parents split evenly between opting for interviews and focus groups, while four of the youth chose interviews and the remaining nine chose focus groups. Seven youth identified themselves as male, three identified as female, and the remaining three identified as “genderqueer or gender fluid.”
Analysis of interview and focus group conversations identified six key “barriers to care” that Ms. Crouch and her coauthors call necessary to rectify in order to improve the quality of health care provided to transgender youth. These are:
• The dearth of health care providers with sufficient knowledge and interest in working with transgender youth.
• The lack of access to pubertal blockers and cross-sex hormones.
• Doctors and their staff who are unable or unwilling to use the names and pronouns that youths prefer to go by.
• Patients being made to feel uncomfortable or “not normal” by health care providers,
• The lack of a set protocol or treatment methodology for dealing with transgender youth.
• The lack of coordination between health care providers and specialties on treating transgender youth – specifically, a lack of cohesive care between mental and medical health care.
“ ‘It was hard enough to find providers who were accepting new patients, worked with adolescents and my insurance, [and] on top of it, finding someone who was transfriendly made it all but impossible,’ ” Ms. Crouch recalled one transgender youth saying during the study.
Ms. Crouch also recounted that providers’ inability to consistently use the correct pronoun when talking about or to a transgender patient was harmful, and despite most instances being dismissed as unintentional, several were said to be intentional and malicious.
“For example, one parent told us [their] doctor said, ‘her, her, her,’ and [her] son, who was 10 years old, said, ‘him, him, him,’ and the doctor got mad, became dismissive and irritated, and kept saying ‘her,’ ” said Ms. Crouch.
The average age of the youth was 18 years, and of the parents was 49 years. The parents were 88% white and 75% female, with 44% holding at least a college degree. Most of the youth were white (69%), and 77% had either completed high school or some college. Youth and parents were recruited in 2015 from local clinics in the Seattle area, as well as through local and national listservs. Thirty-three percent of the parents were from outside the state of Washington.
The study was funded by the Center for Diversity and Health Equity, and the Clinical and Translational Research Faculty Research Support Fund, at Seattle Children’s Research Institute. Ms. Crouch did not report any relevant financial disclosures.
WASHINGTON – Practices and clinics should implement cultural humility training and gender protocols for dealing with transgender youth because many of these youth and their parents find health care experiences to be difficult when procedures for treating and interacting with transgender youth are confusing or nonexistent.
The study is part of an ongoing effort to “provide high-quality, respectful health care for transgender youth [because] these youth are at greatly increased risk of issues including substance abuse, depression, anxiety, homelessness, and suicide,” explained Julia M. Crouch of Seattle Children’s Research Institute.
“A growing body of evidence shows improved health outcomes for transgender youth who received support from family, schools, and providers, and there are now an increasing number of multidisciplinary gender clinics throughout the country [that] have been demonstrated to be a feasible and effective way to provide coordinated care to this population,” Ms. Crouch said at the annual meeting of the Society for Adolescent Health and Medicine.
Ms. Crouch and her coinvestigators recruited transgender youth between the ages of 14 and 22 years, along with parents of transgender youth, all of whom were evaluated and enrolled from the Seattle metropolitan area. Both parents and youth were given the option of participating in either a semistructured interview or a focus group discussion, during which investigators learned about the concerns and experiences of both youth and parents when visiting their health care clinics (J Adolesc Health. 2011 Apr;48[4]:351-7; J Adolesc Health. 2011 Apr;48(4):351-7)..
In total, 13 youth and 16 parents – the latter of whom were not made up of 8 pairs of parents, but rather 16 individual parents of transgender youth who were not necessarily the same 13 youth recruited for the study – were eventually selected for inclusion. The parents split evenly between opting for interviews and focus groups, while four of the youth chose interviews and the remaining nine chose focus groups. Seven youth identified themselves as male, three identified as female, and the remaining three identified as “genderqueer or gender fluid.”
Analysis of interview and focus group conversations identified six key “barriers to care” that Ms. Crouch and her coauthors call necessary to rectify in order to improve the quality of health care provided to transgender youth. These are:
• The dearth of health care providers with sufficient knowledge and interest in working with transgender youth.
• The lack of access to pubertal blockers and cross-sex hormones.
• Doctors and their staff who are unable or unwilling to use the names and pronouns that youths prefer to go by.
• Patients being made to feel uncomfortable or “not normal” by health care providers,
• The lack of a set protocol or treatment methodology for dealing with transgender youth.
• The lack of coordination between health care providers and specialties on treating transgender youth – specifically, a lack of cohesive care between mental and medical health care.
“ ‘It was hard enough to find providers who were accepting new patients, worked with adolescents and my insurance, [and] on top of it, finding someone who was transfriendly made it all but impossible,’ ” Ms. Crouch recalled one transgender youth saying during the study.
Ms. Crouch also recounted that providers’ inability to consistently use the correct pronoun when talking about or to a transgender patient was harmful, and despite most instances being dismissed as unintentional, several were said to be intentional and malicious.
“For example, one parent told us [their] doctor said, ‘her, her, her,’ and [her] son, who was 10 years old, said, ‘him, him, him,’ and the doctor got mad, became dismissive and irritated, and kept saying ‘her,’ ” said Ms. Crouch.
The average age of the youth was 18 years, and of the parents was 49 years. The parents were 88% white and 75% female, with 44% holding at least a college degree. Most of the youth were white (69%), and 77% had either completed high school or some college. Youth and parents were recruited in 2015 from local clinics in the Seattle area, as well as through local and national listservs. Thirty-three percent of the parents were from outside the state of Washington.
The study was funded by the Center for Diversity and Health Equity, and the Clinical and Translational Research Faculty Research Support Fund, at Seattle Children’s Research Institute. Ms. Crouch did not report any relevant financial disclosures.
AT SAHM 16
Key clinical point: Cultural humility training and gender protocols should be adopted for all centers handling transgender youth.
Major finding: A small group of transgender youth and parents of transgender youth outlined six specific protocols that should be adopted by clinicians to improve the treatment of transgender youth.
Data source: A study of 13 transgender youth and 16 parents via interview and focus group discussions.
Disclosures: The study was funded by the Center for Diversity and Health Equity, and the Clinical and Translational Research Faculty Research Support Fund, at Seattle Children’s Research Institute. Ms. Crouch did not report any relevant financial disclosures.
VIDEO: Eight new quality measures key to performance of esophageal manometry
Health care providers performing esophageal manometry should keep in mind eight new quality measures listed and validated in a recent study published in the April issue of Clinical Gastroenterology and Hepatology (Clin Gastroenterol Hepatol. 2015 Oct 20. doi: 10.1016/j.cgh.2015.10.006), which researchers believe will significantly improve the performance of esophageal manometry and interpretation of data culled from such procedures.
“Despite its critical importance in the diagnosis and management of esophageal motility disorders, features of a high-quality esophageal manometry [study] have not been formally defined,” said the study authors, led by Dr. Rena Yadlapati of Northwestern University in Chicago. “Standardizing key aspects of esophageal manometry is imperative to ensure the delivery of high-quality care.”
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Dr. Yadlapati and her coinvestigators carried out the study in accordance with guidelines set out by the RAND/UCLA Appropriateness Method (RAM), They began by recruiting a panel of 15 esophageal manometry experts with leadership, geographical diversity, and a wide range of practice settings being the key criteria in their selection.
Investigators then conducted a literature review, selecting the 30 most relevant randomized, controlled trials, retrospective studies, and systematic reviews from the past 10 years. From this review, investigators created a list of 30 possible quality measures, all of which were then sent to each member of the expert panel via email for them to rank on a 9-point interval scale, and modify if necessary.
Those rankings were then used to determine the appropriateness of each proposed quality measure at a face-to-face meeting among the investigators and the 15-member expert panel, at which 17 quality measures were determined to be appropriate. In all, 2 measures dealt with competency, 2 pertained to assessment before procedure, 3 were regarding performance of the procedure itself, and 10 were about interpretation of data obtained from esophageal manometry; the 10 measures concerning interpretation of data were compiled into 1 measure, leaving a total of 8 that were ultimately approved.
The quality measures for competency are as follows:
• “If esophageal manometry is performed, then the technician must be competent to perform esophageal manometry.”
• “If a physician is considered competent to interpret esophageal manometry, then the physician must interpret a minimum number of esophageal manometry studies annually.”
For assessment before procedure, the measures state the following:
• “If a patient is referred for esophageal manometry, then the patient should have undergone an evaluation for structural abnormalities before manometry.”
• “If an esophageal manometry is performed, then informed consent must be obtained and documented.”
Quality measures regarding the procedure itself state the following:
• “If an esophageal manometry study is performed, then a time interval of at least 30 seconds should occur between swallows.”
• “If an esophageal manometry study is performed, then at least 10 wet swallows should be attempted.”
• “If an esophageal manometry study is performed, then at least seven evaluable wet swallows should be included.”
Finally, regarding interpretation of data, the single quality measures states that “If an esophageal manometry study is interpreted, then a complete procedure report should document the following:
• “Reason for referral.”
• “Clinical diagnosis.”
• “Diagnosis according to formally validated classification scheme.”
• “Documentation of formally validated classification scheme used.”
• “Summary of results”
• “Tabulated results including upper esophageal sphincter activity, interpretation of esophagogastric junction relaxation, documentation of pressure inversion point if technically feasible, pressurization pattern and contractile pattern.”
• “Technical limitation (if applicable).”
• “Communication to referring provider.”
“These eight appropriate quality measures are considered absolutely necessary in the performance and interpretation of esophageal manometry,” the authors concluded. “In particular, measures 3-8 are clinically feasible and measurable, and should serve as an initial framework to benchmark quality and reduce variability in esophageal manometry practices.”
This study was funded by the Alumnae of Northwestern University, and a grant to Dr. Yadlapati (T32 DK101363-02). Five coinvestigators disclosed consultancy and speaking relationships with Boston Scientific, Cook Endoscopy, EndoStim, Given Imaging, Covidien, and Sandhill Scientific.
Health care providers performing esophageal manometry should keep in mind eight new quality measures listed and validated in a recent study published in the April issue of Clinical Gastroenterology and Hepatology (Clin Gastroenterol Hepatol. 2015 Oct 20. doi: 10.1016/j.cgh.2015.10.006), which researchers believe will significantly improve the performance of esophageal manometry and interpretation of data culled from such procedures.
“Despite its critical importance in the diagnosis and management of esophageal motility disorders, features of a high-quality esophageal manometry [study] have not been formally defined,” said the study authors, led by Dr. Rena Yadlapati of Northwestern University in Chicago. “Standardizing key aspects of esophageal manometry is imperative to ensure the delivery of high-quality care.”
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Dr. Yadlapati and her coinvestigators carried out the study in accordance with guidelines set out by the RAND/UCLA Appropriateness Method (RAM), They began by recruiting a panel of 15 esophageal manometry experts with leadership, geographical diversity, and a wide range of practice settings being the key criteria in their selection.
Investigators then conducted a literature review, selecting the 30 most relevant randomized, controlled trials, retrospective studies, and systematic reviews from the past 10 years. From this review, investigators created a list of 30 possible quality measures, all of which were then sent to each member of the expert panel via email for them to rank on a 9-point interval scale, and modify if necessary.
Those rankings were then used to determine the appropriateness of each proposed quality measure at a face-to-face meeting among the investigators and the 15-member expert panel, at which 17 quality measures were determined to be appropriate. In all, 2 measures dealt with competency, 2 pertained to assessment before procedure, 3 were regarding performance of the procedure itself, and 10 were about interpretation of data obtained from esophageal manometry; the 10 measures concerning interpretation of data were compiled into 1 measure, leaving a total of 8 that were ultimately approved.
The quality measures for competency are as follows:
• “If esophageal manometry is performed, then the technician must be competent to perform esophageal manometry.”
• “If a physician is considered competent to interpret esophageal manometry, then the physician must interpret a minimum number of esophageal manometry studies annually.”
For assessment before procedure, the measures state the following:
• “If a patient is referred for esophageal manometry, then the patient should have undergone an evaluation for structural abnormalities before manometry.”
• “If an esophageal manometry is performed, then informed consent must be obtained and documented.”
Quality measures regarding the procedure itself state the following:
• “If an esophageal manometry study is performed, then a time interval of at least 30 seconds should occur between swallows.”
• “If an esophageal manometry study is performed, then at least 10 wet swallows should be attempted.”
• “If an esophageal manometry study is performed, then at least seven evaluable wet swallows should be included.”
Finally, regarding interpretation of data, the single quality measures states that “If an esophageal manometry study is interpreted, then a complete procedure report should document the following:
• “Reason for referral.”
• “Clinical diagnosis.”
• “Diagnosis according to formally validated classification scheme.”
• “Documentation of formally validated classification scheme used.”
• “Summary of results”
• “Tabulated results including upper esophageal sphincter activity, interpretation of esophagogastric junction relaxation, documentation of pressure inversion point if technically feasible, pressurization pattern and contractile pattern.”
• “Technical limitation (if applicable).”
• “Communication to referring provider.”
“These eight appropriate quality measures are considered absolutely necessary in the performance and interpretation of esophageal manometry,” the authors concluded. “In particular, measures 3-8 are clinically feasible and measurable, and should serve as an initial framework to benchmark quality and reduce variability in esophageal manometry practices.”
This study was funded by the Alumnae of Northwestern University, and a grant to Dr. Yadlapati (T32 DK101363-02). Five coinvestigators disclosed consultancy and speaking relationships with Boston Scientific, Cook Endoscopy, EndoStim, Given Imaging, Covidien, and Sandhill Scientific.
Health care providers performing esophageal manometry should keep in mind eight new quality measures listed and validated in a recent study published in the April issue of Clinical Gastroenterology and Hepatology (Clin Gastroenterol Hepatol. 2015 Oct 20. doi: 10.1016/j.cgh.2015.10.006), which researchers believe will significantly improve the performance of esophageal manometry and interpretation of data culled from such procedures.
“Despite its critical importance in the diagnosis and management of esophageal motility disorders, features of a high-quality esophageal manometry [study] have not been formally defined,” said the study authors, led by Dr. Rena Yadlapati of Northwestern University in Chicago. “Standardizing key aspects of esophageal manometry is imperative to ensure the delivery of high-quality care.”
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Dr. Yadlapati and her coinvestigators carried out the study in accordance with guidelines set out by the RAND/UCLA Appropriateness Method (RAM), They began by recruiting a panel of 15 esophageal manometry experts with leadership, geographical diversity, and a wide range of practice settings being the key criteria in their selection.
Investigators then conducted a literature review, selecting the 30 most relevant randomized, controlled trials, retrospective studies, and systematic reviews from the past 10 years. From this review, investigators created a list of 30 possible quality measures, all of which were then sent to each member of the expert panel via email for them to rank on a 9-point interval scale, and modify if necessary.
Those rankings were then used to determine the appropriateness of each proposed quality measure at a face-to-face meeting among the investigators and the 15-member expert panel, at which 17 quality measures were determined to be appropriate. In all, 2 measures dealt with competency, 2 pertained to assessment before procedure, 3 were regarding performance of the procedure itself, and 10 were about interpretation of data obtained from esophageal manometry; the 10 measures concerning interpretation of data were compiled into 1 measure, leaving a total of 8 that were ultimately approved.
The quality measures for competency are as follows:
• “If esophageal manometry is performed, then the technician must be competent to perform esophageal manometry.”
• “If a physician is considered competent to interpret esophageal manometry, then the physician must interpret a minimum number of esophageal manometry studies annually.”
For assessment before procedure, the measures state the following:
• “If a patient is referred for esophageal manometry, then the patient should have undergone an evaluation for structural abnormalities before manometry.”
• “If an esophageal manometry is performed, then informed consent must be obtained and documented.”
Quality measures regarding the procedure itself state the following:
• “If an esophageal manometry study is performed, then a time interval of at least 30 seconds should occur between swallows.”
• “If an esophageal manometry study is performed, then at least 10 wet swallows should be attempted.”
• “If an esophageal manometry study is performed, then at least seven evaluable wet swallows should be included.”
Finally, regarding interpretation of data, the single quality measures states that “If an esophageal manometry study is interpreted, then a complete procedure report should document the following:
• “Reason for referral.”
• “Clinical diagnosis.”
• “Diagnosis according to formally validated classification scheme.”
• “Documentation of formally validated classification scheme used.”
• “Summary of results”
• “Tabulated results including upper esophageal sphincter activity, interpretation of esophagogastric junction relaxation, documentation of pressure inversion point if technically feasible, pressurization pattern and contractile pattern.”
• “Technical limitation (if applicable).”
• “Communication to referring provider.”
“These eight appropriate quality measures are considered absolutely necessary in the performance and interpretation of esophageal manometry,” the authors concluded. “In particular, measures 3-8 are clinically feasible and measurable, and should serve as an initial framework to benchmark quality and reduce variability in esophageal manometry practices.”
This study was funded by the Alumnae of Northwestern University, and a grant to Dr. Yadlapati (T32 DK101363-02). Five coinvestigators disclosed consultancy and speaking relationships with Boston Scientific, Cook Endoscopy, EndoStim, Given Imaging, Covidien, and Sandhill Scientific.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Health care providers should consider eight new validated quality measures when performing and interpreting esophageal manometry data.
Major finding: Of 30 possible measures, 10 regarding interpretation of data were compiled into a single quality measure, 2 were classified as competency measures, 2 were classified as assessments necessary prior to an esophageal manometry procedure, and 3 were classified as integral to the procedure of esophageal manometry, for a total of 8.
Data source: Survey of existing literature and expert interviews on validated quality measures on the basis of the RAM.
Disclosures: Study was partly funded by a grant from the Alumnae of Northwestern University; five coauthors reported financial disclosures.
VIDEO: Rectal indomethacin does not prevent pancreatitis post ERCP
Patients who receive rectal indomethacin after undergoing endoscopic retrograde cholangiopancreatography (ERCP) are not any less likely to develop pancreatitis than individuals who don’t, according to the findings of a recent study published in Gastroenterology (2016 Jan 9. doi: 10.1053/j.gastro.2015.12.018).
“These results are in contrast to recent studies highlighting the benefit of rectal NSAIDS to prevent PEP [post-ECRP pancreatitis] in high-risk patients [and] counter the guidelines espoused by the European Society for Gastrointestinal Endoscopy, which recently recommended giving rectal indomethacin to prevent PEP in all patients undergoing ERCP,” said the study authors, led by Dr. John M. Levenick of Penn State University in Hershey, Pa.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Dr. Levenick and his coinvestigators screened 604 consecutive patients undergoing ERCP, with and without endoscopic ultrasound, at the Dartmouth-Hitchcock Medical Center between March 2013 and December 2014, eventually enrolling and randomizing 449 subjects into two cohorts: one in which subjects were given indomethacin after undergoing ERCP (n = 223), and one in which subjects were simply given a placebo (n = 226). Randomization happened after subjects’ major papilla had been reached, and cannulation attempts were started.
Individuals were excluded if they had active acute pancreatitis or had undergone ERCP to treat or diagnose acute pancreatitis, if they had any contraindications or allergies to NSAIDs, or were younger than 18 years of age, among other factors. The mean age of the indomethacin cohort was 64.9 years, with 118 (52.9%) females; in the placebo cohort, mean age was 64.3 years and 118 (52.2%) were female.
Pancreatitis occurred in 27 subjects overall, 16 (7.2%) of whom were in the indomethacin cohort and the other 11 (4.9%) were on placebo followed ERCP (P = .33). No subjects receiving indomethacin had severe or moderately severe PEP, but one subject had severe PEP and one had moderately severe PEP in the placebo cohort (P = 1.0). There was no necrotizing pancreatitis in either cohort, nor were there any significant differences in gastrointestinal bleeding (P = .75), death (P = .25), or 30-day hospital readmission (P = .1) between the two cohorts.
“Prophylactic rectal indomethacin did not reduce the incidence or severity of PEP in consecutive patients undergoing ERCP,” Dr. Levenick and his coauthors concluded, adding that “guidelines that recommend the administration of rectal indomethacin in all patients undergoing ERCP should be reconsidered.”
This study was funded by the National Pancreas Foundation and a grant from the National Institutes of Health. Dr. Levenick and his coauthors did not report any financial disclosures.
Acute pancreatitis is the most common and feared complication of endoscopic retrograde cholangiopancreatography (ERCP). The incidence of post-ERCP pancreatitis is around 10% with a mortality of 0.7% (Gastrointest Endosc. 2015;81:143-9). Recent advances in noninvasive pancreaticobiliary imaging, risk stratification before ERCP, prophylactic pancreatic stent placement, and administration of nonsteroidal anti-inflammatory drugs (NSAIDs) have improved the overall risk benefit ratio of ERCP.
NSAIDs are potent inhibitors of phospholipase A2, cyclooxygenase, and of the activation of platelets and endothelium, all of which play a central role in the pathogenesis of post-ERCP pancreatitis. NSAIDs constitute an attractive option in clinical practice, because they are inexpensive and widely available with a favorable risk profile. A recent multicenter randomized controlled trial (RCT) of 602 patients at high-risk for post-ERCP pancreatitis showed that rectal indomethacin is associated with a 7.7% absolute and a 46% relative risk reduction of post-ERCP pancreatitis (N Engl J Med. 2012;366:1414-22). These findings have been broadly adapted in endoscopic practice in the United States.

|
| Dr. Georgios Papachristou |
The presented RCT by Dr. Levenick and his colleagues evaluated the efficacy of rectal indomethacin in preventing post-ERCP pancreatitis among consecutive patients undergoing ERCP in a single U.S. center. This study was a well designed and conducted RCT following the CONSORT guidelines and utilizing an independent data and safety monitoring board.
The authors reported that rectal indomethacin did not result in reduction of post-ERCP pancreatitis (7.2%) when compared with placebo (4.9%). Of importance, 70% of patients included were at average risk for post-ERCP pancreatitis. Furthermore, despite a calculated sample size of 1,398 patients, the study was terminated early after enrolling only 449 patients based on the interim analysis showing futility to reach a statistically different outcome.
This well executed RCT reports no benefit in administering rectal indomethacin in all patients undergoing ERCP. Evidence strongly supports that rectal indomethacin remains an important advancement in preventing post-ERCP pancreatitis. However, its benefit is likely limited to a selected group of patients, those at high-risk for post-ERCP pancreatitis. Further studies are under way to clarify whether rectal indomethacin alone vs. indomethacin plus prophylactic pancreatic stenting is more effective in preventing post-ERCP pancreatitis in high-risk patients.
Dr. Georgios Papachristou is associate professor of medicine at the University of Pittsburgh. He is a consultant for Shire and has received funding from the National Institutes of Health and the VA Health System.
Acute pancreatitis is the most common and feared complication of endoscopic retrograde cholangiopancreatography (ERCP). The incidence of post-ERCP pancreatitis is around 10% with a mortality of 0.7% (Gastrointest Endosc. 2015;81:143-9). Recent advances in noninvasive pancreaticobiliary imaging, risk stratification before ERCP, prophylactic pancreatic stent placement, and administration of nonsteroidal anti-inflammatory drugs (NSAIDs) have improved the overall risk benefit ratio of ERCP.
NSAIDs are potent inhibitors of phospholipase A2, cyclooxygenase, and of the activation of platelets and endothelium, all of which play a central role in the pathogenesis of post-ERCP pancreatitis. NSAIDs constitute an attractive option in clinical practice, because they are inexpensive and widely available with a favorable risk profile. A recent multicenter randomized controlled trial (RCT) of 602 patients at high-risk for post-ERCP pancreatitis showed that rectal indomethacin is associated with a 7.7% absolute and a 46% relative risk reduction of post-ERCP pancreatitis (N Engl J Med. 2012;366:1414-22). These findings have been broadly adapted in endoscopic practice in the United States.

|
| Dr. Georgios Papachristou |
The presented RCT by Dr. Levenick and his colleagues evaluated the efficacy of rectal indomethacin in preventing post-ERCP pancreatitis among consecutive patients undergoing ERCP in a single U.S. center. This study was a well designed and conducted RCT following the CONSORT guidelines and utilizing an independent data and safety monitoring board.
The authors reported that rectal indomethacin did not result in reduction of post-ERCP pancreatitis (7.2%) when compared with placebo (4.9%). Of importance, 70% of patients included were at average risk for post-ERCP pancreatitis. Furthermore, despite a calculated sample size of 1,398 patients, the study was terminated early after enrolling only 449 patients based on the interim analysis showing futility to reach a statistically different outcome.
This well executed RCT reports no benefit in administering rectal indomethacin in all patients undergoing ERCP. Evidence strongly supports that rectal indomethacin remains an important advancement in preventing post-ERCP pancreatitis. However, its benefit is likely limited to a selected group of patients, those at high-risk for post-ERCP pancreatitis. Further studies are under way to clarify whether rectal indomethacin alone vs. indomethacin plus prophylactic pancreatic stenting is more effective in preventing post-ERCP pancreatitis in high-risk patients.
Dr. Georgios Papachristou is associate professor of medicine at the University of Pittsburgh. He is a consultant for Shire and has received funding from the National Institutes of Health and the VA Health System.
Acute pancreatitis is the most common and feared complication of endoscopic retrograde cholangiopancreatography (ERCP). The incidence of post-ERCP pancreatitis is around 10% with a mortality of 0.7% (Gastrointest Endosc. 2015;81:143-9). Recent advances in noninvasive pancreaticobiliary imaging, risk stratification before ERCP, prophylactic pancreatic stent placement, and administration of nonsteroidal anti-inflammatory drugs (NSAIDs) have improved the overall risk benefit ratio of ERCP.
NSAIDs are potent inhibitors of phospholipase A2, cyclooxygenase, and of the activation of platelets and endothelium, all of which play a central role in the pathogenesis of post-ERCP pancreatitis. NSAIDs constitute an attractive option in clinical practice, because they are inexpensive and widely available with a favorable risk profile. A recent multicenter randomized controlled trial (RCT) of 602 patients at high-risk for post-ERCP pancreatitis showed that rectal indomethacin is associated with a 7.7% absolute and a 46% relative risk reduction of post-ERCP pancreatitis (N Engl J Med. 2012;366:1414-22). These findings have been broadly adapted in endoscopic practice in the United States.

|
| Dr. Georgios Papachristou |
The presented RCT by Dr. Levenick and his colleagues evaluated the efficacy of rectal indomethacin in preventing post-ERCP pancreatitis among consecutive patients undergoing ERCP in a single U.S. center. This study was a well designed and conducted RCT following the CONSORT guidelines and utilizing an independent data and safety monitoring board.
The authors reported that rectal indomethacin did not result in reduction of post-ERCP pancreatitis (7.2%) when compared with placebo (4.9%). Of importance, 70% of patients included were at average risk for post-ERCP pancreatitis. Furthermore, despite a calculated sample size of 1,398 patients, the study was terminated early after enrolling only 449 patients based on the interim analysis showing futility to reach a statistically different outcome.
This well executed RCT reports no benefit in administering rectal indomethacin in all patients undergoing ERCP. Evidence strongly supports that rectal indomethacin remains an important advancement in preventing post-ERCP pancreatitis. However, its benefit is likely limited to a selected group of patients, those at high-risk for post-ERCP pancreatitis. Further studies are under way to clarify whether rectal indomethacin alone vs. indomethacin plus prophylactic pancreatic stenting is more effective in preventing post-ERCP pancreatitis in high-risk patients.
Dr. Georgios Papachristou is associate professor of medicine at the University of Pittsburgh. He is a consultant for Shire and has received funding from the National Institutes of Health and the VA Health System.
Patients who receive rectal indomethacin after undergoing endoscopic retrograde cholangiopancreatography (ERCP) are not any less likely to develop pancreatitis than individuals who don’t, according to the findings of a recent study published in Gastroenterology (2016 Jan 9. doi: 10.1053/j.gastro.2015.12.018).
“These results are in contrast to recent studies highlighting the benefit of rectal NSAIDS to prevent PEP [post-ECRP pancreatitis] in high-risk patients [and] counter the guidelines espoused by the European Society for Gastrointestinal Endoscopy, which recently recommended giving rectal indomethacin to prevent PEP in all patients undergoing ERCP,” said the study authors, led by Dr. John M. Levenick of Penn State University in Hershey, Pa.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Dr. Levenick and his coinvestigators screened 604 consecutive patients undergoing ERCP, with and without endoscopic ultrasound, at the Dartmouth-Hitchcock Medical Center between March 2013 and December 2014, eventually enrolling and randomizing 449 subjects into two cohorts: one in which subjects were given indomethacin after undergoing ERCP (n = 223), and one in which subjects were simply given a placebo (n = 226). Randomization happened after subjects’ major papilla had been reached, and cannulation attempts were started.
Individuals were excluded if they had active acute pancreatitis or had undergone ERCP to treat or diagnose acute pancreatitis, if they had any contraindications or allergies to NSAIDs, or were younger than 18 years of age, among other factors. The mean age of the indomethacin cohort was 64.9 years, with 118 (52.9%) females; in the placebo cohort, mean age was 64.3 years and 118 (52.2%) were female.
Pancreatitis occurred in 27 subjects overall, 16 (7.2%) of whom were in the indomethacin cohort and the other 11 (4.9%) were on placebo followed ERCP (P = .33). No subjects receiving indomethacin had severe or moderately severe PEP, but one subject had severe PEP and one had moderately severe PEP in the placebo cohort (P = 1.0). There was no necrotizing pancreatitis in either cohort, nor were there any significant differences in gastrointestinal bleeding (P = .75), death (P = .25), or 30-day hospital readmission (P = .1) between the two cohorts.
“Prophylactic rectal indomethacin did not reduce the incidence or severity of PEP in consecutive patients undergoing ERCP,” Dr. Levenick and his coauthors concluded, adding that “guidelines that recommend the administration of rectal indomethacin in all patients undergoing ERCP should be reconsidered.”
This study was funded by the National Pancreas Foundation and a grant from the National Institutes of Health. Dr. Levenick and his coauthors did not report any financial disclosures.
Patients who receive rectal indomethacin after undergoing endoscopic retrograde cholangiopancreatography (ERCP) are not any less likely to develop pancreatitis than individuals who don’t, according to the findings of a recent study published in Gastroenterology (2016 Jan 9. doi: 10.1053/j.gastro.2015.12.018).
“These results are in contrast to recent studies highlighting the benefit of rectal NSAIDS to prevent PEP [post-ECRP pancreatitis] in high-risk patients [and] counter the guidelines espoused by the European Society for Gastrointestinal Endoscopy, which recently recommended giving rectal indomethacin to prevent PEP in all patients undergoing ERCP,” said the study authors, led by Dr. John M. Levenick of Penn State University in Hershey, Pa.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Dr. Levenick and his coinvestigators screened 604 consecutive patients undergoing ERCP, with and without endoscopic ultrasound, at the Dartmouth-Hitchcock Medical Center between March 2013 and December 2014, eventually enrolling and randomizing 449 subjects into two cohorts: one in which subjects were given indomethacin after undergoing ERCP (n = 223), and one in which subjects were simply given a placebo (n = 226). Randomization happened after subjects’ major papilla had been reached, and cannulation attempts were started.
Individuals were excluded if they had active acute pancreatitis or had undergone ERCP to treat or diagnose acute pancreatitis, if they had any contraindications or allergies to NSAIDs, or were younger than 18 years of age, among other factors. The mean age of the indomethacin cohort was 64.9 years, with 118 (52.9%) females; in the placebo cohort, mean age was 64.3 years and 118 (52.2%) were female.
Pancreatitis occurred in 27 subjects overall, 16 (7.2%) of whom were in the indomethacin cohort and the other 11 (4.9%) were on placebo followed ERCP (P = .33). No subjects receiving indomethacin had severe or moderately severe PEP, but one subject had severe PEP and one had moderately severe PEP in the placebo cohort (P = 1.0). There was no necrotizing pancreatitis in either cohort, nor were there any significant differences in gastrointestinal bleeding (P = .75), death (P = .25), or 30-day hospital readmission (P = .1) between the two cohorts.
“Prophylactic rectal indomethacin did not reduce the incidence or severity of PEP in consecutive patients undergoing ERCP,” Dr. Levenick and his coauthors concluded, adding that “guidelines that recommend the administration of rectal indomethacin in all patients undergoing ERCP should be reconsidered.”
This study was funded by the National Pancreas Foundation and a grant from the National Institutes of Health. Dr. Levenick and his coauthors did not report any financial disclosures.
FROM GASTROENTEROLOGY
Key clinical point: Rectal indomethacin does not prevent pancreatitis in patients who undergo endoscopic retrograde cholangiopancreatography (ERCP).
Major finding: 7.2% of subjects on indomethacin and 4.9% on placebo developed post-ERCP pancreatitis, indicating no significant difference between the two cohorts (P = .33).
Data source: Prospective, double-blind, placebo-controlled study of 449 ERCP patients between March 2013 and December 2014.
Disclosures: Study funded by National Pancreas Foundation and National Institutes of Health. Dr. Levenick and his coauthors did not report any relevant financial disclosures.
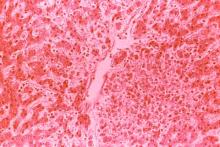
VIDEO: Newer MRI hardware, software significantly better at detecting pancreatic cysts
As magnetic resonance imaging technology continues to advance year after year, so does MRI’s ability to accurately detect pancreatic cysts, according to a new study published in the April issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2015.08.038).
“To our knowledge, this is the first study to analyze the relationship between the technical improvements in imaging techniques (specifically, MRI) and the presence of incidentally found PCLs [pancreatic cystic lesions],” said the study authors, led by Dr. Michael B. Wallace of the Mayo Clinic in Jacksonville, Fla.
Dr. Wallace and his coinvestigators launched this retrospective descriptive study selecting the first 50 consecutive abdominal MRI patients at the Jacksonville Mayo Clinic during January and February of each year from 2005 through 2014, for a total of 500 cases who met inclusion criteria included in the study. Patients were excluded if they had preexisting symptomatic or asymptomatic pancreatitis, either acute or chronic, pancreatic masses, pancreatic cysts, pancreatic surgery, pancreatic symptoms, or any pancreas-related indications found by MRI.
The clinic underwent periodic MRI updates over the course of the 10-year study, along with requisite software updates to “take advantage of the new hardware technology,” the study explains. Major hardware improvements, provided by Siemens Medical Solutions USA, were Symphony/Sonata, Espree/Avanto, and Aera/Skyra, while software updates corresponding to each hardware update were VA, VB, and VD, respectively.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Furthermore, each software update had other, smaller upgrades, leading to a total of 20 combinations of MRI hardware and software on which MRIs were performed over the 10 years. Every MRI taken included “an axial and a coronal T2-weighted single-shot (HASTE) pulse sequence [with] TR 1400-1500 ms, TE 82-99 ms, and slice thickness 5-7 mm (gap, 0.5-0.7 mm).” Each MRI was analyzed by a pancreatic MRI specialist to find incidental cysts.
The number of patients found with pancreatic cysts increased incrementally from 2005 to 2014, with 2010 being the year with the highest number. A total of 208 subjects (41.6%) were found to have incidental cysts, but only 44 of these cases were discovered in the original MRI. The presence of cysts was associated with older age in patients who had them; only 20% of all subjects under 50 years of age had cysts, compared to 32.4% of those between 50 and 60 years, 54.9% of those between 60 and 70 years, and 61.5% of those over the age of 70 years (P less than .01).
Additionally, 56.4% of all subjects with diabetes (P less than .01), 59.0% of subjects with nonmelanoma skin cancer (P less than .03), and 58.1% of those with hepatocarcinoma (P less than .02) were also found to have cysts. Most striking, however, is that newer hardware and software permutations were able to detect cysts in 56.3% (Skyra) of patients who had them, compared with only 30.3% (Symphony) of patients who underwent MRI on older technology.
“The variable field strength” (1.5 T vs. 3 T) was not significantly related to the presence of PCLs,” Dr. Wallace and his coauthors concluded. “We believe this may be secondary to the lack of power of the analysis, because only 6% of the examinations were 3-T studies. Therefore, we speculate that this relationship may be confirmed if the number of 3-T studies increased.”
Males and females each made up roughly 50% of the study population, with a median age of 60 years and 85% being white. Additionally, 4% of subjects had a family history of pancreatic cancer, 12% had a personal history of solid organ transplant, and 53% had a personal history of smoking.
This study was funded by the Mayo Clinic. Dr. Wallace disclosed that he has received grant funding from Olympus, Boston Scientific, and Cosmo Pharmaceuticals, and travel support from Olympus. No other authors reported any financial disclosures.
The increasing prevalence of pancreatic cystic lesions on MRI scanning may provide an important opportunity for detection of early precursors of pancreatic cancer – or may represent just another insignificant incidental finding. What is the implication of a small asymptomatic cyst?
MRI scanning of the pancreas has revolutionized our ability to detect early cystic neoplasms of the pancreas. Pancreatic cysts appear as well-defined, small, round fluid-filled structures within the pancreas. The inner structures – such as septations, nodules, and adjacent masses – offer clues as to the type of cyst and the risk of malignancy. But the real strength of pancreatic MRI scanning is the ability to detect and portray small cysts and the adjacent main pancreatic duct.
The size, number, and distribution of cysts over time can be tracked with MRI surveillance. By tracking the diameter of cysts and calculating the rate of growth of cysts, clinicians may be able to predict the development of malignancy in intraductal papillary mucinous neoplasms.
How should these patients be managed clinically? Once a cyst has been identified, are clinicians obligated to notify the patient, monitor the cyst with an established surveillance program, or biopsy the cyst? If the cyst is very small and benign appearing, can the clinician ignore the finding and perhaps not notify the patient?
Once again, we are watching dilemmas unfold as technology outstrips our understanding of diseases and their management. We are going to need some good correlations between imaging and tissue of pancreatic cystic lesions. In the meantime, it is important to reserve the use of pancreatic MRI scanning to high-risk patients or patients with CT scan abnormalities.
Dr. William R. Brugge, AGAF, is professor of medicine, Harvard Medical School, and director, Pancreas Biliary Center, Massachusetts General Hospital, both in Boston. He is a consultant with Boston Scientific.
The increasing prevalence of pancreatic cystic lesions on MRI scanning may provide an important opportunity for detection of early precursors of pancreatic cancer – or may represent just another insignificant incidental finding. What is the implication of a small asymptomatic cyst?
MRI scanning of the pancreas has revolutionized our ability to detect early cystic neoplasms of the pancreas. Pancreatic cysts appear as well-defined, small, round fluid-filled structures within the pancreas. The inner structures – such as septations, nodules, and adjacent masses – offer clues as to the type of cyst and the risk of malignancy. But the real strength of pancreatic MRI scanning is the ability to detect and portray small cysts and the adjacent main pancreatic duct.
The size, number, and distribution of cysts over time can be tracked with MRI surveillance. By tracking the diameter of cysts and calculating the rate of growth of cysts, clinicians may be able to predict the development of malignancy in intraductal papillary mucinous neoplasms.
How should these patients be managed clinically? Once a cyst has been identified, are clinicians obligated to notify the patient, monitor the cyst with an established surveillance program, or biopsy the cyst? If the cyst is very small and benign appearing, can the clinician ignore the finding and perhaps not notify the patient?
Once again, we are watching dilemmas unfold as technology outstrips our understanding of diseases and their management. We are going to need some good correlations between imaging and tissue of pancreatic cystic lesions. In the meantime, it is important to reserve the use of pancreatic MRI scanning to high-risk patients or patients with CT scan abnormalities.
Dr. William R. Brugge, AGAF, is professor of medicine, Harvard Medical School, and director, Pancreas Biliary Center, Massachusetts General Hospital, both in Boston. He is a consultant with Boston Scientific.
The increasing prevalence of pancreatic cystic lesions on MRI scanning may provide an important opportunity for detection of early precursors of pancreatic cancer – or may represent just another insignificant incidental finding. What is the implication of a small asymptomatic cyst?
MRI scanning of the pancreas has revolutionized our ability to detect early cystic neoplasms of the pancreas. Pancreatic cysts appear as well-defined, small, round fluid-filled structures within the pancreas. The inner structures – such as septations, nodules, and adjacent masses – offer clues as to the type of cyst and the risk of malignancy. But the real strength of pancreatic MRI scanning is the ability to detect and portray small cysts and the adjacent main pancreatic duct.
The size, number, and distribution of cysts over time can be tracked with MRI surveillance. By tracking the diameter of cysts and calculating the rate of growth of cysts, clinicians may be able to predict the development of malignancy in intraductal papillary mucinous neoplasms.
How should these patients be managed clinically? Once a cyst has been identified, are clinicians obligated to notify the patient, monitor the cyst with an established surveillance program, or biopsy the cyst? If the cyst is very small and benign appearing, can the clinician ignore the finding and perhaps not notify the patient?
Once again, we are watching dilemmas unfold as technology outstrips our understanding of diseases and their management. We are going to need some good correlations between imaging and tissue of pancreatic cystic lesions. In the meantime, it is important to reserve the use of pancreatic MRI scanning to high-risk patients or patients with CT scan abnormalities.
Dr. William R. Brugge, AGAF, is professor of medicine, Harvard Medical School, and director, Pancreas Biliary Center, Massachusetts General Hospital, both in Boston. He is a consultant with Boston Scientific.
As magnetic resonance imaging technology continues to advance year after year, so does MRI’s ability to accurately detect pancreatic cysts, according to a new study published in the April issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2015.08.038).
“To our knowledge, this is the first study to analyze the relationship between the technical improvements in imaging techniques (specifically, MRI) and the presence of incidentally found PCLs [pancreatic cystic lesions],” said the study authors, led by Dr. Michael B. Wallace of the Mayo Clinic in Jacksonville, Fla.
Dr. Wallace and his coinvestigators launched this retrospective descriptive study selecting the first 50 consecutive abdominal MRI patients at the Jacksonville Mayo Clinic during January and February of each year from 2005 through 2014, for a total of 500 cases who met inclusion criteria included in the study. Patients were excluded if they had preexisting symptomatic or asymptomatic pancreatitis, either acute or chronic, pancreatic masses, pancreatic cysts, pancreatic surgery, pancreatic symptoms, or any pancreas-related indications found by MRI.
The clinic underwent periodic MRI updates over the course of the 10-year study, along with requisite software updates to “take advantage of the new hardware technology,” the study explains. Major hardware improvements, provided by Siemens Medical Solutions USA, were Symphony/Sonata, Espree/Avanto, and Aera/Skyra, while software updates corresponding to each hardware update were VA, VB, and VD, respectively.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Furthermore, each software update had other, smaller upgrades, leading to a total of 20 combinations of MRI hardware and software on which MRIs were performed over the 10 years. Every MRI taken included “an axial and a coronal T2-weighted single-shot (HASTE) pulse sequence [with] TR 1400-1500 ms, TE 82-99 ms, and slice thickness 5-7 mm (gap, 0.5-0.7 mm).” Each MRI was analyzed by a pancreatic MRI specialist to find incidental cysts.
The number of patients found with pancreatic cysts increased incrementally from 2005 to 2014, with 2010 being the year with the highest number. A total of 208 subjects (41.6%) were found to have incidental cysts, but only 44 of these cases were discovered in the original MRI. The presence of cysts was associated with older age in patients who had them; only 20% of all subjects under 50 years of age had cysts, compared to 32.4% of those between 50 and 60 years, 54.9% of those between 60 and 70 years, and 61.5% of those over the age of 70 years (P less than .01).
Additionally, 56.4% of all subjects with diabetes (P less than .01), 59.0% of subjects with nonmelanoma skin cancer (P less than .03), and 58.1% of those with hepatocarcinoma (P less than .02) were also found to have cysts. Most striking, however, is that newer hardware and software permutations were able to detect cysts in 56.3% (Skyra) of patients who had them, compared with only 30.3% (Symphony) of patients who underwent MRI on older technology.
“The variable field strength” (1.5 T vs. 3 T) was not significantly related to the presence of PCLs,” Dr. Wallace and his coauthors concluded. “We believe this may be secondary to the lack of power of the analysis, because only 6% of the examinations were 3-T studies. Therefore, we speculate that this relationship may be confirmed if the number of 3-T studies increased.”
Males and females each made up roughly 50% of the study population, with a median age of 60 years and 85% being white. Additionally, 4% of subjects had a family history of pancreatic cancer, 12% had a personal history of solid organ transplant, and 53% had a personal history of smoking.
This study was funded by the Mayo Clinic. Dr. Wallace disclosed that he has received grant funding from Olympus, Boston Scientific, and Cosmo Pharmaceuticals, and travel support from Olympus. No other authors reported any financial disclosures.
As magnetic resonance imaging technology continues to advance year after year, so does MRI’s ability to accurately detect pancreatic cysts, according to a new study published in the April issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2015.08.038).
“To our knowledge, this is the first study to analyze the relationship between the technical improvements in imaging techniques (specifically, MRI) and the presence of incidentally found PCLs [pancreatic cystic lesions],” said the study authors, led by Dr. Michael B. Wallace of the Mayo Clinic in Jacksonville, Fla.
Dr. Wallace and his coinvestigators launched this retrospective descriptive study selecting the first 50 consecutive abdominal MRI patients at the Jacksonville Mayo Clinic during January and February of each year from 2005 through 2014, for a total of 500 cases who met inclusion criteria included in the study. Patients were excluded if they had preexisting symptomatic or asymptomatic pancreatitis, either acute or chronic, pancreatic masses, pancreatic cysts, pancreatic surgery, pancreatic symptoms, or any pancreas-related indications found by MRI.
The clinic underwent periodic MRI updates over the course of the 10-year study, along with requisite software updates to “take advantage of the new hardware technology,” the study explains. Major hardware improvements, provided by Siemens Medical Solutions USA, were Symphony/Sonata, Espree/Avanto, and Aera/Skyra, while software updates corresponding to each hardware update were VA, VB, and VD, respectively.
SOURCE: AMERICAN GASTROENTEROLOGICAL ASSOCIATION
Furthermore, each software update had other, smaller upgrades, leading to a total of 20 combinations of MRI hardware and software on which MRIs were performed over the 10 years. Every MRI taken included “an axial and a coronal T2-weighted single-shot (HASTE) pulse sequence [with] TR 1400-1500 ms, TE 82-99 ms, and slice thickness 5-7 mm (gap, 0.5-0.7 mm).” Each MRI was analyzed by a pancreatic MRI specialist to find incidental cysts.
The number of patients found with pancreatic cysts increased incrementally from 2005 to 2014, with 2010 being the year with the highest number. A total of 208 subjects (41.6%) were found to have incidental cysts, but only 44 of these cases were discovered in the original MRI. The presence of cysts was associated with older age in patients who had them; only 20% of all subjects under 50 years of age had cysts, compared to 32.4% of those between 50 and 60 years, 54.9% of those between 60 and 70 years, and 61.5% of those over the age of 70 years (P less than .01).
Additionally, 56.4% of all subjects with diabetes (P less than .01), 59.0% of subjects with nonmelanoma skin cancer (P less than .03), and 58.1% of those with hepatocarcinoma (P less than .02) were also found to have cysts. Most striking, however, is that newer hardware and software permutations were able to detect cysts in 56.3% (Skyra) of patients who had them, compared with only 30.3% (Symphony) of patients who underwent MRI on older technology.
“The variable field strength” (1.5 T vs. 3 T) was not significantly related to the presence of PCLs,” Dr. Wallace and his coauthors concluded. “We believe this may be secondary to the lack of power of the analysis, because only 6% of the examinations were 3-T studies. Therefore, we speculate that this relationship may be confirmed if the number of 3-T studies increased.”
Males and females each made up roughly 50% of the study population, with a median age of 60 years and 85% being white. Additionally, 4% of subjects had a family history of pancreatic cancer, 12% had a personal history of solid organ transplant, and 53% had a personal history of smoking.
This study was funded by the Mayo Clinic. Dr. Wallace disclosed that he has received grant funding from Olympus, Boston Scientific, and Cosmo Pharmaceuticals, and travel support from Olympus. No other authors reported any financial disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Newer MRI technology is more effective at detecting pancreatic cysts, particularly in patients with diabetes or advanced age.
Major finding: Newer MRI hardware and software detected pancreatic cysts in 56.3% of patients, compared with only 30.3% on older MRI hardware and software.
Data source: Retrospective, descriptive study of 500 patients undergoing MRI for nonpancreatic indications during January and February of 2005-2014.
Disclosures: Study funded by the Mayo Clinic. Dr. Michael B. Wallace disclosed relationships with Olympus, Boston Scientific, and Cosmo Pharmaceuticals.
VIDEO: Anesthesia services during colonoscopy increase risk of near-term complications
Receiving anesthesia services while undergoing a colonoscopy may not be in your patients’ best interest, as doing so could significantly increase the likelihood of patients experiencing serious complications within 30 days of the procedure.
This is according to a new study published in the April issue of Gastroenterology, in which Dr. Karen J. Wernli and her coinvestigators analyzed claims data, collected from the Truven Health MarketScan Research Database, related to 3,168,228 colonoscopy procedures that took place between 2008 and 2011, to determine whether patients who received anesthesia were at a higher risk of developing complications after the procedure (doi: 10.1053/j.gastro.2015.12.018).
Source: American Gastroenterological Association
“The involvement of anesthesia services for colonoscopy sedation, mainly to administer propofol, has increased accordingly, from 11.0% of colonoscopies in 2001 to 23.4% in 2006, with projections of more than 50% in 2015,” wrote Dr. Wernli of the Group Health Research Institute in Seattle, and her coauthors. “Whether the use of propofol is associated with higher rates of short-term complications compared with standard sedation is not well understood.”
Men and women whose data was included in the study were between 40 and 64 years of age; men accounted for 46.8% of those receiving standard sedation (53.2% women) and 46.5% of those receiving anesthesia services (53.5% women). A total of 4,939,993 individuals were initially screened for enrollment, with 39,784 excluded because of a previous colorectal cancer diagnosis, 240,038 for “noncancer exclusions,” and 1,491,943 for being enrolled in the study less than 1 year.
Standard sedation was done in 2,079,784 (65.6%) of the procedures included in the study, while the other 1,088,444 (34.4%) colonoscopies involved anesthesia services. Use of anesthesia services resulted in a 13% increase in likelihood for patients to experience some kind of complication within 30 days of colonoscopy (95% confidence interval, 1.12-1.14). The most common complications were perforation (odds ratio, 1.07; 95% CI, 1.00-1.15), hemorrhage (OR, 1.28; 95% CI, 1.27-1.30), abdominal pain (OR, 1.07; 95% CI, 1.05-1.08), complications secondary to anesthesia (OR, 1.15; 95% CI, 1.05-1.28), and “stroke and other central nervous system events” (OR, 1.04; 95% CI, 1.00-1.08).
Analysis of geographic distribution of colonoscopies performed with and without anesthesia services showed that all areas of the United States had a higher likelihood of postcolonoscopy complications associated with anesthesia except in the Southeast, where there was no association between the two. Additionally, in the western U.S., use of anesthesia services was less common than in any other geographic area, but was associated with a staggering 60% higher chance of complication within 30 days for patients who did opt for it.
“Although the use of anesthesia agents can directly impact colonoscopy outcomes, it is not solely the anesthesia agent that could lead to additional complications,” the study authors wrote. “In the absence of patient feedback, increased colonic-wall tension from colonoscopy pressure may not be identified by the endoscopist, and, consistent with our results, could lead to increased risks of colonic complications, such as perforation and abdominal pain.”
Dr. Wernli and her coauthors did not report any relevant financial disclosures.
We are approaching a time when half of all colonoscopies are performed with anesthesia assistance, most using propofol. Undeniably, some patients require anesthesia support for medical reasons, or because they do not sedate adequately with opiate-benzodiazepine combinations endoscopists can administer. The popularity of propofol-based anesthesia for routine colonoscopy, however, is based on several perceived benefits: patient demand for a discomfort-free procedure, rapid sedation followed by quick recovery, and good reimbursement for the anesthesia service itself, added to the benefits of faster overall procedure turnaround time. And presently, there is no disincentive — financial or otherwise — to continuing or expanding this practice. Colonoscopy with anesthesia looks like a win-win for both patient and endoscopist, as long as the added cost of anesthesia can be justified.
However, while anesthesia-assisted colonoscopy appears to possess several advantages, growing evidence suggests that a lower risk of complications is not one of them.
A smaller study (165,000 colonoscopies) using NCI SEER registry data suggested that adding anesthesia to colonoscopy may increase some adverse events. Cooper et al. (JAMA Intern Med. 2013;173:551-6) showed an increase in overall complications and, specifically, aspiration, although not in technical complications of colonoscopy, including perforation and splenic rupture. However, this study did not include patients who underwent polypectomy. Wernli, et al. now show evidence derived from over 3 million patients demonstrating that adding anesthesia to colonoscopy increases complications significantly — not only aspiration, but also technical aspects of colonoscopy, including perforation, bleeding, and abdominal pain.
Colonoscopy is extremely safe, so complications are infrequent. Thus, data sets of colonoscopy complications large enough to be statistically meaningful for studies of this type require an extraordinarily large patient pool. For this prospective, observational cohort study, the authors obtained the large sample size by mining administrative claims data for 3 years, not through examining clinical data. As a result, several assumptions were made. These 3 million colonoscopies represented all indications — not just colorectal cancer screening. Billing claims for anesthesia represented surrogate markers for administration of propofol-based anesthesia. While anesthesia assistance was associated with increased risk of perforation, hemorrhage, abdominal pain, anesthesia complications, and stroke; risk of perforation associated with anesthesia was increased only in patients who underwent polypectomy.
Study methodology and confounding variables aside, it is hard to ignore the core message here: a large body of data analyzed rigorously demonstrate that anesthesia support for colonoscopy increases risk of procedure-related complications.
Patients who are ill, have certain cardiopulmonary issues, or do not sedate adequately with moderate sedation benefit from anesthesia assistance for colonoscopy. But for patients undergoing routine colonoscopy, without such issues, who could safely undergo colonoscopy under moderate sedation without unreasonable discomfort, we must now ask ourselves and discuss with our patients honestly, not only whether the added cost of anesthesia is reasonable — but also whether the apparent added risk of anesthesia justifies perceived benefits.
Dr. John A. Martin is senior associate consultant and associate professor, associate chair for endoscopy, Mayo Clinic, Rochester, Minn. He has no conflicts of interest to disclose.
We are approaching a time when half of all colonoscopies are performed with anesthesia assistance, most using propofol. Undeniably, some patients require anesthesia support for medical reasons, or because they do not sedate adequately with opiate-benzodiazepine combinations endoscopists can administer. The popularity of propofol-based anesthesia for routine colonoscopy, however, is based on several perceived benefits: patient demand for a discomfort-free procedure, rapid sedation followed by quick recovery, and good reimbursement for the anesthesia service itself, added to the benefits of faster overall procedure turnaround time. And presently, there is no disincentive — financial or otherwise — to continuing or expanding this practice. Colonoscopy with anesthesia looks like a win-win for both patient and endoscopist, as long as the added cost of anesthesia can be justified.
However, while anesthesia-assisted colonoscopy appears to possess several advantages, growing evidence suggests that a lower risk of complications is not one of them.
A smaller study (165,000 colonoscopies) using NCI SEER registry data suggested that adding anesthesia to colonoscopy may increase some adverse events. Cooper et al. (JAMA Intern Med. 2013;173:551-6) showed an increase in overall complications and, specifically, aspiration, although not in technical complications of colonoscopy, including perforation and splenic rupture. However, this study did not include patients who underwent polypectomy. Wernli, et al. now show evidence derived from over 3 million patients demonstrating that adding anesthesia to colonoscopy increases complications significantly — not only aspiration, but also technical aspects of colonoscopy, including perforation, bleeding, and abdominal pain.
Colonoscopy is extremely safe, so complications are infrequent. Thus, data sets of colonoscopy complications large enough to be statistically meaningful for studies of this type require an extraordinarily large patient pool. For this prospective, observational cohort study, the authors obtained the large sample size by mining administrative claims data for 3 years, not through examining clinical data. As a result, several assumptions were made. These 3 million colonoscopies represented all indications — not just colorectal cancer screening. Billing claims for anesthesia represented surrogate markers for administration of propofol-based anesthesia. While anesthesia assistance was associated with increased risk of perforation, hemorrhage, abdominal pain, anesthesia complications, and stroke; risk of perforation associated with anesthesia was increased only in patients who underwent polypectomy.
Study methodology and confounding variables aside, it is hard to ignore the core message here: a large body of data analyzed rigorously demonstrate that anesthesia support for colonoscopy increases risk of procedure-related complications.
Patients who are ill, have certain cardiopulmonary issues, or do not sedate adequately with moderate sedation benefit from anesthesia assistance for colonoscopy. But for patients undergoing routine colonoscopy, without such issues, who could safely undergo colonoscopy under moderate sedation without unreasonable discomfort, we must now ask ourselves and discuss with our patients honestly, not only whether the added cost of anesthesia is reasonable — but also whether the apparent added risk of anesthesia justifies perceived benefits.
Dr. John A. Martin is senior associate consultant and associate professor, associate chair for endoscopy, Mayo Clinic, Rochester, Minn. He has no conflicts of interest to disclose.
We are approaching a time when half of all colonoscopies are performed with anesthesia assistance, most using propofol. Undeniably, some patients require anesthesia support for medical reasons, or because they do not sedate adequately with opiate-benzodiazepine combinations endoscopists can administer. The popularity of propofol-based anesthesia for routine colonoscopy, however, is based on several perceived benefits: patient demand for a discomfort-free procedure, rapid sedation followed by quick recovery, and good reimbursement for the anesthesia service itself, added to the benefits of faster overall procedure turnaround time. And presently, there is no disincentive — financial or otherwise — to continuing or expanding this practice. Colonoscopy with anesthesia looks like a win-win for both patient and endoscopist, as long as the added cost of anesthesia can be justified.
However, while anesthesia-assisted colonoscopy appears to possess several advantages, growing evidence suggests that a lower risk of complications is not one of them.
A smaller study (165,000 colonoscopies) using NCI SEER registry data suggested that adding anesthesia to colonoscopy may increase some adverse events. Cooper et al. (JAMA Intern Med. 2013;173:551-6) showed an increase in overall complications and, specifically, aspiration, although not in technical complications of colonoscopy, including perforation and splenic rupture. However, this study did not include patients who underwent polypectomy. Wernli, et al. now show evidence derived from over 3 million patients demonstrating that adding anesthesia to colonoscopy increases complications significantly — not only aspiration, but also technical aspects of colonoscopy, including perforation, bleeding, and abdominal pain.
Colonoscopy is extremely safe, so complications are infrequent. Thus, data sets of colonoscopy complications large enough to be statistically meaningful for studies of this type require an extraordinarily large patient pool. For this prospective, observational cohort study, the authors obtained the large sample size by mining administrative claims data for 3 years, not through examining clinical data. As a result, several assumptions were made. These 3 million colonoscopies represented all indications — not just colorectal cancer screening. Billing claims for anesthesia represented surrogate markers for administration of propofol-based anesthesia. While anesthesia assistance was associated with increased risk of perforation, hemorrhage, abdominal pain, anesthesia complications, and stroke; risk of perforation associated with anesthesia was increased only in patients who underwent polypectomy.
Study methodology and confounding variables aside, it is hard to ignore the core message here: a large body of data analyzed rigorously demonstrate that anesthesia support for colonoscopy increases risk of procedure-related complications.
Patients who are ill, have certain cardiopulmonary issues, or do not sedate adequately with moderate sedation benefit from anesthesia assistance for colonoscopy. But for patients undergoing routine colonoscopy, without such issues, who could safely undergo colonoscopy under moderate sedation without unreasonable discomfort, we must now ask ourselves and discuss with our patients honestly, not only whether the added cost of anesthesia is reasonable — but also whether the apparent added risk of anesthesia justifies perceived benefits.
Dr. John A. Martin is senior associate consultant and associate professor, associate chair for endoscopy, Mayo Clinic, Rochester, Minn. He has no conflicts of interest to disclose.
Receiving anesthesia services while undergoing a colonoscopy may not be in your patients’ best interest, as doing so could significantly increase the likelihood of patients experiencing serious complications within 30 days of the procedure.
This is according to a new study published in the April issue of Gastroenterology, in which Dr. Karen J. Wernli and her coinvestigators analyzed claims data, collected from the Truven Health MarketScan Research Database, related to 3,168,228 colonoscopy procedures that took place between 2008 and 2011, to determine whether patients who received anesthesia were at a higher risk of developing complications after the procedure (doi: 10.1053/j.gastro.2015.12.018).
Source: American Gastroenterological Association
“The involvement of anesthesia services for colonoscopy sedation, mainly to administer propofol, has increased accordingly, from 11.0% of colonoscopies in 2001 to 23.4% in 2006, with projections of more than 50% in 2015,” wrote Dr. Wernli of the Group Health Research Institute in Seattle, and her coauthors. “Whether the use of propofol is associated with higher rates of short-term complications compared with standard sedation is not well understood.”
Men and women whose data was included in the study were between 40 and 64 years of age; men accounted for 46.8% of those receiving standard sedation (53.2% women) and 46.5% of those receiving anesthesia services (53.5% women). A total of 4,939,993 individuals were initially screened for enrollment, with 39,784 excluded because of a previous colorectal cancer diagnosis, 240,038 for “noncancer exclusions,” and 1,491,943 for being enrolled in the study less than 1 year.
Standard sedation was done in 2,079,784 (65.6%) of the procedures included in the study, while the other 1,088,444 (34.4%) colonoscopies involved anesthesia services. Use of anesthesia services resulted in a 13% increase in likelihood for patients to experience some kind of complication within 30 days of colonoscopy (95% confidence interval, 1.12-1.14). The most common complications were perforation (odds ratio, 1.07; 95% CI, 1.00-1.15), hemorrhage (OR, 1.28; 95% CI, 1.27-1.30), abdominal pain (OR, 1.07; 95% CI, 1.05-1.08), complications secondary to anesthesia (OR, 1.15; 95% CI, 1.05-1.28), and “stroke and other central nervous system events” (OR, 1.04; 95% CI, 1.00-1.08).
Analysis of geographic distribution of colonoscopies performed with and without anesthesia services showed that all areas of the United States had a higher likelihood of postcolonoscopy complications associated with anesthesia except in the Southeast, where there was no association between the two. Additionally, in the western U.S., use of anesthesia services was less common than in any other geographic area, but was associated with a staggering 60% higher chance of complication within 30 days for patients who did opt for it.
“Although the use of anesthesia agents can directly impact colonoscopy outcomes, it is not solely the anesthesia agent that could lead to additional complications,” the study authors wrote. “In the absence of patient feedback, increased colonic-wall tension from colonoscopy pressure may not be identified by the endoscopist, and, consistent with our results, could lead to increased risks of colonic complications, such as perforation and abdominal pain.”
Dr. Wernli and her coauthors did not report any relevant financial disclosures.
Receiving anesthesia services while undergoing a colonoscopy may not be in your patients’ best interest, as doing so could significantly increase the likelihood of patients experiencing serious complications within 30 days of the procedure.
This is according to a new study published in the April issue of Gastroenterology, in which Dr. Karen J. Wernli and her coinvestigators analyzed claims data, collected from the Truven Health MarketScan Research Database, related to 3,168,228 colonoscopy procedures that took place between 2008 and 2011, to determine whether patients who received anesthesia were at a higher risk of developing complications after the procedure (doi: 10.1053/j.gastro.2015.12.018).
Source: American Gastroenterological Association
“The involvement of anesthesia services for colonoscopy sedation, mainly to administer propofol, has increased accordingly, from 11.0% of colonoscopies in 2001 to 23.4% in 2006, with projections of more than 50% in 2015,” wrote Dr. Wernli of the Group Health Research Institute in Seattle, and her coauthors. “Whether the use of propofol is associated with higher rates of short-term complications compared with standard sedation is not well understood.”
Men and women whose data was included in the study were between 40 and 64 years of age; men accounted for 46.8% of those receiving standard sedation (53.2% women) and 46.5% of those receiving anesthesia services (53.5% women). A total of 4,939,993 individuals were initially screened for enrollment, with 39,784 excluded because of a previous colorectal cancer diagnosis, 240,038 for “noncancer exclusions,” and 1,491,943 for being enrolled in the study less than 1 year.
Standard sedation was done in 2,079,784 (65.6%) of the procedures included in the study, while the other 1,088,444 (34.4%) colonoscopies involved anesthesia services. Use of anesthesia services resulted in a 13% increase in likelihood for patients to experience some kind of complication within 30 days of colonoscopy (95% confidence interval, 1.12-1.14). The most common complications were perforation (odds ratio, 1.07; 95% CI, 1.00-1.15), hemorrhage (OR, 1.28; 95% CI, 1.27-1.30), abdominal pain (OR, 1.07; 95% CI, 1.05-1.08), complications secondary to anesthesia (OR, 1.15; 95% CI, 1.05-1.28), and “stroke and other central nervous system events” (OR, 1.04; 95% CI, 1.00-1.08).
Analysis of geographic distribution of colonoscopies performed with and without anesthesia services showed that all areas of the United States had a higher likelihood of postcolonoscopy complications associated with anesthesia except in the Southeast, where there was no association between the two. Additionally, in the western U.S., use of anesthesia services was less common than in any other geographic area, but was associated with a staggering 60% higher chance of complication within 30 days for patients who did opt for it.
“Although the use of anesthesia agents can directly impact colonoscopy outcomes, it is not solely the anesthesia agent that could lead to additional complications,” the study authors wrote. “In the absence of patient feedback, increased colonic-wall tension from colonoscopy pressure may not be identified by the endoscopist, and, consistent with our results, could lead to increased risks of colonic complications, such as perforation and abdominal pain.”
Dr. Wernli and her coauthors did not report any relevant financial disclosures.
FROM GASTROENTEROLOGY
Key clinical point: Using anesthesia services on individuals receiving colonoscopy increases the overall risk of complications associated with the procedure.
Major finding: Colonoscopy patients who received anesthesia had a 13% higher risk of complication within 30 days, including perforation, hemorrhage, abdominal pain, and stroke.
Data source: A prospective cohort study of claims data from 3,168,228 colonoscopy procedures in the Truven Health MarketScan Research Databases from 2008 to 2011.
Disclosures: Funding provided by the Agency for Healthcare Research and Quality and the National Institutes of Health. Dr. Wernli and her coauthors did not report any relevant financial disclosures.
Gender nonconforming LGBTQ youth more prone to bullying, harassment
WASHINGTON – Lesbian, gay, bisexual, transgender, questioning (LGBTQ) children and adolescents who are gender nonconforming are more susceptible to bullying at school than are those who don’t, so schools should make it a point to integrate LGBTQ outreach into its programs and to combat bullying against this group of students .
“In recent years, there’s been heightened national attention in the United States [on] harassment, bullying, and violence victimization, especially in schools and particularly targeting [LGBT] youth,” explained Allegra R. Gordon, Sc.D., of Boston Children’s Hospital.
“There’s substantial public health literature documenting an array of mental and physical health correlates of such victimization. However, there’s been less focus on discrimination and violence victimization targeting gender expression, broadly, although there is some evidence that this is an area of concern,” said Dr. Gordon, who presented the findings at the annual meeting of the Society for Adolescent Health and Medicine.
Dr. Gordon and her coinvestigators analyzed data on 5,503 public school students in grades 9-12 from four specific school districts in the United States: Los Angeles; San Diego; Chicago; and Broward County, Fla. These school districts were chosen because they had recently added a new question to the survey regarding socially assigned gender expression, making them the first districts in the nation to do so in 2013.
The data accumulated came from the 2013 Youth Risk Behavior Surveillance System, a survey conducted by the Centers for Disease Control and Prevention every 2 years to determine “the prevalence of health risk behaviors [and] assess whether health risk behaviors increase, decrease, or stay the same over time,” among other things.
The primary outcome of the study was to determine if sex and/or sexual orientation was in any way responsible for whether or not a student conformed to a specific gender – if not, the student was marked as GNC, or gender nonconformity – and if there was any association between GNC youths and in-school victimization. Youth who responded as being GNC were categorized as either most conforming, moderately nonconforming, or most noncomforming.
Nonconformity for each subject was defined based on “socially assigned gender expression, which is the extent to which a person is perceived by others as conforming or not conforming to culturally defined ideas of masculine or feminine appearance and behavior,” Dr. Gordon explained.
Results indicated a strong association between youths identifying as GNC and school-based victimization, with incidences of bullying increasing with greater GNC identification. Out of all GNC youth, 14% reported experiencing some form of bullying, 8% reported missing school because they felt unsafe being there, and 6% reported either being threatened or having been physically injured because of their gender identification.
After adjustment, Dr. Gordon and her coinvestigators found that the higher the degree of GNC a subject had, the more likely they would be victims of bullying, with steadily increasing odds ratios as the level of GNC rose: moderately nonconforming, 1.40 (range, 1.18-1.68) and most nonconforming, 2.01 (1.38-2.93). The latter group also had the highest odds of being absent from school, with an OR of 2.06 (2.10-4.44), and being either threatened with injury or actually getting injured having an OR of 2.79 (1.58-4.91).
“A key take-home here as well is given that the majority of the youth in the sample are heterosexual, the majority of youth in that most gender nonconforming group are heterosexual, so these are issues that apply across sexual orientation identities,” said Dr. Gordon.
Dr. Gordon did not report any relevant financial disclosures.
WASHINGTON – Lesbian, gay, bisexual, transgender, questioning (LGBTQ) children and adolescents who are gender nonconforming are more susceptible to bullying at school than are those who don’t, so schools should make it a point to integrate LGBTQ outreach into its programs and to combat bullying against this group of students .
“In recent years, there’s been heightened national attention in the United States [on] harassment, bullying, and violence victimization, especially in schools and particularly targeting [LGBT] youth,” explained Allegra R. Gordon, Sc.D., of Boston Children’s Hospital.
“There’s substantial public health literature documenting an array of mental and physical health correlates of such victimization. However, there’s been less focus on discrimination and violence victimization targeting gender expression, broadly, although there is some evidence that this is an area of concern,” said Dr. Gordon, who presented the findings at the annual meeting of the Society for Adolescent Health and Medicine.
Dr. Gordon and her coinvestigators analyzed data on 5,503 public school students in grades 9-12 from four specific school districts in the United States: Los Angeles; San Diego; Chicago; and Broward County, Fla. These school districts were chosen because they had recently added a new question to the survey regarding socially assigned gender expression, making them the first districts in the nation to do so in 2013.
The data accumulated came from the 2013 Youth Risk Behavior Surveillance System, a survey conducted by the Centers for Disease Control and Prevention every 2 years to determine “the prevalence of health risk behaviors [and] assess whether health risk behaviors increase, decrease, or stay the same over time,” among other things.
The primary outcome of the study was to determine if sex and/or sexual orientation was in any way responsible for whether or not a student conformed to a specific gender – if not, the student was marked as GNC, or gender nonconformity – and if there was any association between GNC youths and in-school victimization. Youth who responded as being GNC were categorized as either most conforming, moderately nonconforming, or most noncomforming.
Nonconformity for each subject was defined based on “socially assigned gender expression, which is the extent to which a person is perceived by others as conforming or not conforming to culturally defined ideas of masculine or feminine appearance and behavior,” Dr. Gordon explained.
Results indicated a strong association between youths identifying as GNC and school-based victimization, with incidences of bullying increasing with greater GNC identification. Out of all GNC youth, 14% reported experiencing some form of bullying, 8% reported missing school because they felt unsafe being there, and 6% reported either being threatened or having been physically injured because of their gender identification.
After adjustment, Dr. Gordon and her coinvestigators found that the higher the degree of GNC a subject had, the more likely they would be victims of bullying, with steadily increasing odds ratios as the level of GNC rose: moderately nonconforming, 1.40 (range, 1.18-1.68) and most nonconforming, 2.01 (1.38-2.93). The latter group also had the highest odds of being absent from school, with an OR of 2.06 (2.10-4.44), and being either threatened with injury or actually getting injured having an OR of 2.79 (1.58-4.91).
“A key take-home here as well is given that the majority of the youth in the sample are heterosexual, the majority of youth in that most gender nonconforming group are heterosexual, so these are issues that apply across sexual orientation identities,” said Dr. Gordon.
Dr. Gordon did not report any relevant financial disclosures.
WASHINGTON – Lesbian, gay, bisexual, transgender, questioning (LGBTQ) children and adolescents who are gender nonconforming are more susceptible to bullying at school than are those who don’t, so schools should make it a point to integrate LGBTQ outreach into its programs and to combat bullying against this group of students .
“In recent years, there’s been heightened national attention in the United States [on] harassment, bullying, and violence victimization, especially in schools and particularly targeting [LGBT] youth,” explained Allegra R. Gordon, Sc.D., of Boston Children’s Hospital.
“There’s substantial public health literature documenting an array of mental and physical health correlates of such victimization. However, there’s been less focus on discrimination and violence victimization targeting gender expression, broadly, although there is some evidence that this is an area of concern,” said Dr. Gordon, who presented the findings at the annual meeting of the Society for Adolescent Health and Medicine.
Dr. Gordon and her coinvestigators analyzed data on 5,503 public school students in grades 9-12 from four specific school districts in the United States: Los Angeles; San Diego; Chicago; and Broward County, Fla. These school districts were chosen because they had recently added a new question to the survey regarding socially assigned gender expression, making them the first districts in the nation to do so in 2013.
The data accumulated came from the 2013 Youth Risk Behavior Surveillance System, a survey conducted by the Centers for Disease Control and Prevention every 2 years to determine “the prevalence of health risk behaviors [and] assess whether health risk behaviors increase, decrease, or stay the same over time,” among other things.
The primary outcome of the study was to determine if sex and/or sexual orientation was in any way responsible for whether or not a student conformed to a specific gender – if not, the student was marked as GNC, or gender nonconformity – and if there was any association between GNC youths and in-school victimization. Youth who responded as being GNC were categorized as either most conforming, moderately nonconforming, or most noncomforming.
Nonconformity for each subject was defined based on “socially assigned gender expression, which is the extent to which a person is perceived by others as conforming or not conforming to culturally defined ideas of masculine or feminine appearance and behavior,” Dr. Gordon explained.
Results indicated a strong association between youths identifying as GNC and school-based victimization, with incidences of bullying increasing with greater GNC identification. Out of all GNC youth, 14% reported experiencing some form of bullying, 8% reported missing school because they felt unsafe being there, and 6% reported either being threatened or having been physically injured because of their gender identification.
After adjustment, Dr. Gordon and her coinvestigators found that the higher the degree of GNC a subject had, the more likely they would be victims of bullying, with steadily increasing odds ratios as the level of GNC rose: moderately nonconforming, 1.40 (range, 1.18-1.68) and most nonconforming, 2.01 (1.38-2.93). The latter group also had the highest odds of being absent from school, with an OR of 2.06 (2.10-4.44), and being either threatened with injury or actually getting injured having an OR of 2.79 (1.58-4.91).
“A key take-home here as well is given that the majority of the youth in the sample are heterosexual, the majority of youth in that most gender nonconforming group are heterosexual, so these are issues that apply across sexual orientation identities,” said Dr. Gordon.
Dr. Gordon did not report any relevant financial disclosures.
AT THE SAHM ANNUAL MEETING
Key clinical point: Gender identification among LGBTQ youth may predispose them to bullying at school by their peers.
Major finding: Among gender nonconforming youth, 14% reported being bullied, 8% reported missing school, and 6% reported being threatened or injured.
Data source: Retrospective cohort analysis of 5,503 students in grades 9-12 from four counties in the United States, collected in 2013.
Disclosures: Dr. Gordon did not report any relevant disclosures.
Mindfulness, cognitive therapy top conventional care for low back pain
Adults suffering from chronic lower back pain may be better off pursuing mindfulness-based stress reduction or cognitive behavioral therapy rather than more standard, conventional treatments for pain alleviation, according to a new study published in JAMA.
However, the relatively limited availability of cognitive and mindfulness-based approaches to stress reduction in many parts of the country, coupled with the uncertainty about insurance providers covering such treatments, put the viability of such treatments receiving widespread acceptance and use in question.
“Low back pain is a leading cause of disability in the United States, [and] psychosocial factors play important roles in pain and associated physical and psychosocial disability,” said Daniel C. Cherkin, Ph.D., of the Group Health Research Institute in Seattle, and his associates. “Cognitive behavioral therapy [CBT] has demonstrated effectiveness for various chronic pain conditions and is widely recommended for patients with chronic low back pain, [but] patient access to CBT is limited.”
Dr. Cherkin and his coinvestigators recruited subjects from Group Health, an integrated health care system in Washington state, looking for patients between the ages of 20 years and 70 years with low back pain persisting for at least 3 months that was both nonspecific and had not been given a specific diagnosis (JAMA. 2016 Mar;315[12]:1240-9).
Of 1,767 patients evaluated, 342 patients were enrolled and randomized into one of three cohorts: those receiving mindfulness-based stress reduction (MBSR) (116 patients), those receiving CBT (113 patients), and those receiving “usual care,” defined as “whatever care participants received” prior to enrollment (113 patients).
Those randomized to receive usual care received $50 toward whichever pain management option they chose to receive. Those receiving MBSR or CBT were not aware of which they were receiving until they attended the first group session.
A total of 8 sessions, each 2 hours long and offered weekly, were conducted for patients in each cohort, although attendance at each session was not mandatory. Follow-up with patients in each cohort was conducted at 4 weeks (halfway through treatment), 8 weeks (post-treatment), 26 weeks (primary endpoint of the study), and 52 weeks, with the number of patients in each cohort varying at each follow-up; patients who attended follow-up interviews were compensated $20.
Improvements in functional limitations of at least 30% and intensity of back pain were the primary outcomes measured. The former was measured via a modified Roland Disability Questionnaire (RDQ), which assessed patients’ physical limitations brought on by low back pain on a scale of 0-23, with 0 being the least intense and 23 being the most intense. The latter outcome was measured on a simple scale of 0-10, 0 being the least intense and 10 being the most intense.
At 26 weeks, RDQ scores for MBSR and CBT patients were significantly higher than for those patients receiving usual-care treatment options. Mean percentage improvement in the MBSR cohort was 60.5% and 57.7% in the CBT cohort. Comparatively, patients receiving usual care improved by an average of 44.1% (P = .04). MBSR showed the highest percentage improvement at all four follow-up intervals except 8 weeks, when CBT had a higher percentage. However, both were consistently higher than usual care throughout.
When it came to the second primary outcome, MBSR and CBT were again shown to be significantly more effective, registering mean percentage improvements of 43.6% and 44.9% at 26-week follow-up, respectively. The usual care cohort, on the other hand, improved by 26.6% (P = .01).
Regarding study limitations, Dr. Cherkin and his coinvestigators noted that “participants were enrolled in a single health care system and generally highly educated. [Also] the generalizability of findings to other settings and populations is unknown, [and] approximately 20% of participants randomized to the MBSR and CBT groups were lost to follow-up.”
The pressing question, however, is the viability of MBSR and CBT therapies, particularly the former. While treatments such as yoga and meditation are relatively widespread throughout the United States, getting insurance providers to cover such treatments may be a roadblock for doctors looking to prescribe such therapies to their chronic back pain patients.
Because CBT and MBSR have been around for more than 30 years, they are accessible mostly in urban areas of the country, usually through programs run by hospitals, and “reaches [that] are more open to the idea of mindfulness and meditation concepts,” Dr. Cherkin explained in an interview. However, he added, “they are not generally covered [by] insurance, but we’re hoping that studies like ours will help change that.”
The problem, said Dr. Cherkin, is the allocation of resources by insurance and health care providers to certain treatment and therapies that aren’t necessarily the most effective.
“Just because something isn’t covered by insurance doesn’t mean it isn’t helpful and cost effective,” he explained. “And on the opposite side, many things that are covered by insurance are not very helpful.”
Dr. Cherkin cautioned that, while the findings of this study are promising – especially as they relate to the growing desire by both providers and patients to turn away from opioids for chronic pain management – these findings are ultimately just one step along a longer journey.
“Opioids are often resorted to out of desperation by both physicians and patients who both feel there isn’t any alternative, and physicians don’t like to see their patients continuing to suffer,” said Dr. Cherkin. “Things have gotten way out of whack over the years, because there has not been an evidence-based approach to ensuring that what is most helpful for patients is available and offered by insurance.
“If we can look at the most effective treatment options available to patients that have low risks of addiction, death, or other harm and make those available so physicians can include those in their repertoire of what they feel they can offer patients, we’re going to be in much better shape,” Dr. Cherkin noted.
The National Center for Complementary and Integrative Health funded the study. The authors did not report any relevant financial disclosures.
The potential relevance of mind-body interventions for chronic low back pain derives from the tremendous individual and societal burden caused by this disabling, costly, and increasingly prevalent condition.
[Increasingly], chronic pain management demands shifting away from the biomedical disease model focused on cure to a biopsychosocial model in which physicians and other clinicians guide patient-centered care that emphasizes patient engagement in daily self-management using a range of tools.
A critical component of self-management includes home practice and the daily implementation of skills learned. Although it does not appear that this component was assessed in this trial, future studies should examine the relationship of home practice and skill development with clinical outcomes to enhance understanding of how these interventions work and help identify the most appropriate candidates for these treatments.
Dr. Madhav Goyal and Dr. Jennifer A. Haythornthwaite are both at Johns Hopkins University in Baltimore. These remarks come from their editorial accompanying the study (JAMA. 2016 Mar;315[12]:1236-7).
The potential relevance of mind-body interventions for chronic low back pain derives from the tremendous individual and societal burden caused by this disabling, costly, and increasingly prevalent condition.
[Increasingly], chronic pain management demands shifting away from the biomedical disease model focused on cure to a biopsychosocial model in which physicians and other clinicians guide patient-centered care that emphasizes patient engagement in daily self-management using a range of tools.
A critical component of self-management includes home practice and the daily implementation of skills learned. Although it does not appear that this component was assessed in this trial, future studies should examine the relationship of home practice and skill development with clinical outcomes to enhance understanding of how these interventions work and help identify the most appropriate candidates for these treatments.
Dr. Madhav Goyal and Dr. Jennifer A. Haythornthwaite are both at Johns Hopkins University in Baltimore. These remarks come from their editorial accompanying the study (JAMA. 2016 Mar;315[12]:1236-7).
The potential relevance of mind-body interventions for chronic low back pain derives from the tremendous individual and societal burden caused by this disabling, costly, and increasingly prevalent condition.
[Increasingly], chronic pain management demands shifting away from the biomedical disease model focused on cure to a biopsychosocial model in which physicians and other clinicians guide patient-centered care that emphasizes patient engagement in daily self-management using a range of tools.
A critical component of self-management includes home practice and the daily implementation of skills learned. Although it does not appear that this component was assessed in this trial, future studies should examine the relationship of home practice and skill development with clinical outcomes to enhance understanding of how these interventions work and help identify the most appropriate candidates for these treatments.
Dr. Madhav Goyal and Dr. Jennifer A. Haythornthwaite are both at Johns Hopkins University in Baltimore. These remarks come from their editorial accompanying the study (JAMA. 2016 Mar;315[12]:1236-7).
Adults suffering from chronic lower back pain may be better off pursuing mindfulness-based stress reduction or cognitive behavioral therapy rather than more standard, conventional treatments for pain alleviation, according to a new study published in JAMA.
However, the relatively limited availability of cognitive and mindfulness-based approaches to stress reduction in many parts of the country, coupled with the uncertainty about insurance providers covering such treatments, put the viability of such treatments receiving widespread acceptance and use in question.
“Low back pain is a leading cause of disability in the United States, [and] psychosocial factors play important roles in pain and associated physical and psychosocial disability,” said Daniel C. Cherkin, Ph.D., of the Group Health Research Institute in Seattle, and his associates. “Cognitive behavioral therapy [CBT] has demonstrated effectiveness for various chronic pain conditions and is widely recommended for patients with chronic low back pain, [but] patient access to CBT is limited.”
Dr. Cherkin and his coinvestigators recruited subjects from Group Health, an integrated health care system in Washington state, looking for patients between the ages of 20 years and 70 years with low back pain persisting for at least 3 months that was both nonspecific and had not been given a specific diagnosis (JAMA. 2016 Mar;315[12]:1240-9).
Of 1,767 patients evaluated, 342 patients were enrolled and randomized into one of three cohorts: those receiving mindfulness-based stress reduction (MBSR) (116 patients), those receiving CBT (113 patients), and those receiving “usual care,” defined as “whatever care participants received” prior to enrollment (113 patients).
Those randomized to receive usual care received $50 toward whichever pain management option they chose to receive. Those receiving MBSR or CBT were not aware of which they were receiving until they attended the first group session.
A total of 8 sessions, each 2 hours long and offered weekly, were conducted for patients in each cohort, although attendance at each session was not mandatory. Follow-up with patients in each cohort was conducted at 4 weeks (halfway through treatment), 8 weeks (post-treatment), 26 weeks (primary endpoint of the study), and 52 weeks, with the number of patients in each cohort varying at each follow-up; patients who attended follow-up interviews were compensated $20.
Improvements in functional limitations of at least 30% and intensity of back pain were the primary outcomes measured. The former was measured via a modified Roland Disability Questionnaire (RDQ), which assessed patients’ physical limitations brought on by low back pain on a scale of 0-23, with 0 being the least intense and 23 being the most intense. The latter outcome was measured on a simple scale of 0-10, 0 being the least intense and 10 being the most intense.
At 26 weeks, RDQ scores for MBSR and CBT patients were significantly higher than for those patients receiving usual-care treatment options. Mean percentage improvement in the MBSR cohort was 60.5% and 57.7% in the CBT cohort. Comparatively, patients receiving usual care improved by an average of 44.1% (P = .04). MBSR showed the highest percentage improvement at all four follow-up intervals except 8 weeks, when CBT had a higher percentage. However, both were consistently higher than usual care throughout.
When it came to the second primary outcome, MBSR and CBT were again shown to be significantly more effective, registering mean percentage improvements of 43.6% and 44.9% at 26-week follow-up, respectively. The usual care cohort, on the other hand, improved by 26.6% (P = .01).
Regarding study limitations, Dr. Cherkin and his coinvestigators noted that “participants were enrolled in a single health care system and generally highly educated. [Also] the generalizability of findings to other settings and populations is unknown, [and] approximately 20% of participants randomized to the MBSR and CBT groups were lost to follow-up.”
The pressing question, however, is the viability of MBSR and CBT therapies, particularly the former. While treatments such as yoga and meditation are relatively widespread throughout the United States, getting insurance providers to cover such treatments may be a roadblock for doctors looking to prescribe such therapies to their chronic back pain patients.
Because CBT and MBSR have been around for more than 30 years, they are accessible mostly in urban areas of the country, usually through programs run by hospitals, and “reaches [that] are more open to the idea of mindfulness and meditation concepts,” Dr. Cherkin explained in an interview. However, he added, “they are not generally covered [by] insurance, but we’re hoping that studies like ours will help change that.”
The problem, said Dr. Cherkin, is the allocation of resources by insurance and health care providers to certain treatment and therapies that aren’t necessarily the most effective.
“Just because something isn’t covered by insurance doesn’t mean it isn’t helpful and cost effective,” he explained. “And on the opposite side, many things that are covered by insurance are not very helpful.”
Dr. Cherkin cautioned that, while the findings of this study are promising – especially as they relate to the growing desire by both providers and patients to turn away from opioids for chronic pain management – these findings are ultimately just one step along a longer journey.
“Opioids are often resorted to out of desperation by both physicians and patients who both feel there isn’t any alternative, and physicians don’t like to see their patients continuing to suffer,” said Dr. Cherkin. “Things have gotten way out of whack over the years, because there has not been an evidence-based approach to ensuring that what is most helpful for patients is available and offered by insurance.
“If we can look at the most effective treatment options available to patients that have low risks of addiction, death, or other harm and make those available so physicians can include those in their repertoire of what they feel they can offer patients, we’re going to be in much better shape,” Dr. Cherkin noted.
The National Center for Complementary and Integrative Health funded the study. The authors did not report any relevant financial disclosures.
Adults suffering from chronic lower back pain may be better off pursuing mindfulness-based stress reduction or cognitive behavioral therapy rather than more standard, conventional treatments for pain alleviation, according to a new study published in JAMA.
However, the relatively limited availability of cognitive and mindfulness-based approaches to stress reduction in many parts of the country, coupled with the uncertainty about insurance providers covering such treatments, put the viability of such treatments receiving widespread acceptance and use in question.
“Low back pain is a leading cause of disability in the United States, [and] psychosocial factors play important roles in pain and associated physical and psychosocial disability,” said Daniel C. Cherkin, Ph.D., of the Group Health Research Institute in Seattle, and his associates. “Cognitive behavioral therapy [CBT] has demonstrated effectiveness for various chronic pain conditions and is widely recommended for patients with chronic low back pain, [but] patient access to CBT is limited.”
Dr. Cherkin and his coinvestigators recruited subjects from Group Health, an integrated health care system in Washington state, looking for patients between the ages of 20 years and 70 years with low back pain persisting for at least 3 months that was both nonspecific and had not been given a specific diagnosis (JAMA. 2016 Mar;315[12]:1240-9).
Of 1,767 patients evaluated, 342 patients were enrolled and randomized into one of three cohorts: those receiving mindfulness-based stress reduction (MBSR) (116 patients), those receiving CBT (113 patients), and those receiving “usual care,” defined as “whatever care participants received” prior to enrollment (113 patients).
Those randomized to receive usual care received $50 toward whichever pain management option they chose to receive. Those receiving MBSR or CBT were not aware of which they were receiving until they attended the first group session.
A total of 8 sessions, each 2 hours long and offered weekly, were conducted for patients in each cohort, although attendance at each session was not mandatory. Follow-up with patients in each cohort was conducted at 4 weeks (halfway through treatment), 8 weeks (post-treatment), 26 weeks (primary endpoint of the study), and 52 weeks, with the number of patients in each cohort varying at each follow-up; patients who attended follow-up interviews were compensated $20.
Improvements in functional limitations of at least 30% and intensity of back pain were the primary outcomes measured. The former was measured via a modified Roland Disability Questionnaire (RDQ), which assessed patients’ physical limitations brought on by low back pain on a scale of 0-23, with 0 being the least intense and 23 being the most intense. The latter outcome was measured on a simple scale of 0-10, 0 being the least intense and 10 being the most intense.
At 26 weeks, RDQ scores for MBSR and CBT patients were significantly higher than for those patients receiving usual-care treatment options. Mean percentage improvement in the MBSR cohort was 60.5% and 57.7% in the CBT cohort. Comparatively, patients receiving usual care improved by an average of 44.1% (P = .04). MBSR showed the highest percentage improvement at all four follow-up intervals except 8 weeks, when CBT had a higher percentage. However, both were consistently higher than usual care throughout.
When it came to the second primary outcome, MBSR and CBT were again shown to be significantly more effective, registering mean percentage improvements of 43.6% and 44.9% at 26-week follow-up, respectively. The usual care cohort, on the other hand, improved by 26.6% (P = .01).
Regarding study limitations, Dr. Cherkin and his coinvestigators noted that “participants were enrolled in a single health care system and generally highly educated. [Also] the generalizability of findings to other settings and populations is unknown, [and] approximately 20% of participants randomized to the MBSR and CBT groups were lost to follow-up.”
The pressing question, however, is the viability of MBSR and CBT therapies, particularly the former. While treatments such as yoga and meditation are relatively widespread throughout the United States, getting insurance providers to cover such treatments may be a roadblock for doctors looking to prescribe such therapies to their chronic back pain patients.
Because CBT and MBSR have been around for more than 30 years, they are accessible mostly in urban areas of the country, usually through programs run by hospitals, and “reaches [that] are more open to the idea of mindfulness and meditation concepts,” Dr. Cherkin explained in an interview. However, he added, “they are not generally covered [by] insurance, but we’re hoping that studies like ours will help change that.”
The problem, said Dr. Cherkin, is the allocation of resources by insurance and health care providers to certain treatment and therapies that aren’t necessarily the most effective.
“Just because something isn’t covered by insurance doesn’t mean it isn’t helpful and cost effective,” he explained. “And on the opposite side, many things that are covered by insurance are not very helpful.”
Dr. Cherkin cautioned that, while the findings of this study are promising – especially as they relate to the growing desire by both providers and patients to turn away from opioids for chronic pain management – these findings are ultimately just one step along a longer journey.
“Opioids are often resorted to out of desperation by both physicians and patients who both feel there isn’t any alternative, and physicians don’t like to see their patients continuing to suffer,” said Dr. Cherkin. “Things have gotten way out of whack over the years, because there has not been an evidence-based approach to ensuring that what is most helpful for patients is available and offered by insurance.
“If we can look at the most effective treatment options available to patients that have low risks of addiction, death, or other harm and make those available so physicians can include those in their repertoire of what they feel they can offer patients, we’re going to be in much better shape,” Dr. Cherkin noted.
The National Center for Complementary and Integrative Health funded the study. The authors did not report any relevant financial disclosures.
FROM JAMA
Key clinical point: Undergoing either mindfulness-based stress reduction or cognitive behavioral therapy is more effective at mitigating chronic back pain in adults than conventional treatment options.
Major finding: At 26 weeks, Roland Disability Questionnaire scores were significantly higher for those who received mindfulness-based or cognitive therapy – 60.5% and 57.7%, respectively – than those receiving conventional care (44.1%) (P = .04).
Data source: Randomized, interviewer-blind, clinical trial of 342 individuals age 20-70 years in Washington state from September 2012 to April 2014.
Disclosures: The National Center for Complementary and Integrative Health funded the study. The authors did not report any relevant financial disclosures.
Condom use low among female teens using LARC
WASHINGTON – While use of long-acting reversible contraception (LARC) has steadily been increasing over recent years, a new study shows that adolescent females who use LARC might be neglecting to wear condoms when engaging in sexual intercourse, regardless of their number of partners, thus predisposing them to a high risk of contracting sexually transmitted infections (STIs).
“Like moderately effective methods of contraception, [LARC] does not protect against STIs, and so use of a condom in conjunction with [LARC] is recommended for STI prevention,” lead author Riley J. Steiner of the Centers for Disease Control and Prevention in Atlanta, explained at the annual meeting of the Society for Adolescent Health and Medicine. The study also was published in JAMA Pediatrics (2016 Mar 14. doi:10.1001/jamapediatrics.2016.0007)
She added that, “We really think that establishing a link between LARC and condom use early on, prior to widespread adolescent uptake of LARC, can help provide a useful reference point for future monitoring and, ultimately, inform STI prevention efforts as LARC is brought to scale.”
Ms. Steiner and her coinvestigators used data from the 2013 national Youth Risk Behavior Survey, a self-administered “paper and pencil” questionnaire conducted every 2 years for students in grades 9-12 in public and private high schools across the United States. Analysis of the data – which looked for age, race, and type of contraceptive used – was conducted in July and August of 2015.
Primary outcome of the analysis was to determine the contraceptive method used the most recent time a female had sexual intercourse: either LARC – via an intrauterine device or an implant – oral contraceptives, Depo-Provera, a patch, or a ring. In total, 2,288 females were included in the study; 41% used condoms, 22% used oral contraceptives, 16% used no contraceptive methods whatsoever, 12% used “withdrawal or other method,” 6% used either Depo-Provera, a patch, or a ring, 2% said they were unsure of what contraceptive, if any, they used, and only 2% of females used LARC.
However, of the 2% that used LARC, adjusted odds ratios revealed that they were significantly more likely not to use condoms (adjusted prevalence ratio [aPR], 0.42; 95% confidence interval, 0.21-0.84) as opposed to females on oral contraceptives. There was no significant difference found in condom use between females on LARC versus those on Depo-Provera, a patch, or a ring (aPR = 0.57; 95% CI, 0.26-1.25).
“Health care professionals may be more likely to offer LARC to adolescents who report not using condoms or using them infrequently, as LARC methods are particularly well suited for adolescents who have difficulty adhering to coitally dependent methods,” Ms. Steiner and her associates said, adding that it is currently unknown “whether the association varies by partnership type; it is possible that the observed differences occur largely among adolescents who consider themselves to be in committed partnerships and thus are less concerned about STIs.”
Females included in the study were 57% white, with just over a third of all 2,288 subjects being in the 12th grade. Condom use was most prevalent among 9th graders (47%), while non-Hispanic blacks and Hispanic females tended to use condoms the most (47% and 46%, respectively). LARC use, though low overall, was highest among 12th graders (3%) and non-Hispanic whites (2%).
The study was funded partly by grants from the National Institute of Allergy and Infectious Diseases, and the Centers for Disease Control and Prevention. Ms. Steiner did not report any relevant financial disclosures.
WASHINGTON – While use of long-acting reversible contraception (LARC) has steadily been increasing over recent years, a new study shows that adolescent females who use LARC might be neglecting to wear condoms when engaging in sexual intercourse, regardless of their number of partners, thus predisposing them to a high risk of contracting sexually transmitted infections (STIs).
“Like moderately effective methods of contraception, [LARC] does not protect against STIs, and so use of a condom in conjunction with [LARC] is recommended for STI prevention,” lead author Riley J. Steiner of the Centers for Disease Control and Prevention in Atlanta, explained at the annual meeting of the Society for Adolescent Health and Medicine. The study also was published in JAMA Pediatrics (2016 Mar 14. doi:10.1001/jamapediatrics.2016.0007)
She added that, “We really think that establishing a link between LARC and condom use early on, prior to widespread adolescent uptake of LARC, can help provide a useful reference point for future monitoring and, ultimately, inform STI prevention efforts as LARC is brought to scale.”
Ms. Steiner and her coinvestigators used data from the 2013 national Youth Risk Behavior Survey, a self-administered “paper and pencil” questionnaire conducted every 2 years for students in grades 9-12 in public and private high schools across the United States. Analysis of the data – which looked for age, race, and type of contraceptive used – was conducted in July and August of 2015.
Primary outcome of the analysis was to determine the contraceptive method used the most recent time a female had sexual intercourse: either LARC – via an intrauterine device or an implant – oral contraceptives, Depo-Provera, a patch, or a ring. In total, 2,288 females were included in the study; 41% used condoms, 22% used oral contraceptives, 16% used no contraceptive methods whatsoever, 12% used “withdrawal or other method,” 6% used either Depo-Provera, a patch, or a ring, 2% said they were unsure of what contraceptive, if any, they used, and only 2% of females used LARC.
However, of the 2% that used LARC, adjusted odds ratios revealed that they were significantly more likely not to use condoms (adjusted prevalence ratio [aPR], 0.42; 95% confidence interval, 0.21-0.84) as opposed to females on oral contraceptives. There was no significant difference found in condom use between females on LARC versus those on Depo-Provera, a patch, or a ring (aPR = 0.57; 95% CI, 0.26-1.25).
“Health care professionals may be more likely to offer LARC to adolescents who report not using condoms or using them infrequently, as LARC methods are particularly well suited for adolescents who have difficulty adhering to coitally dependent methods,” Ms. Steiner and her associates said, adding that it is currently unknown “whether the association varies by partnership type; it is possible that the observed differences occur largely among adolescents who consider themselves to be in committed partnerships and thus are less concerned about STIs.”
Females included in the study were 57% white, with just over a third of all 2,288 subjects being in the 12th grade. Condom use was most prevalent among 9th graders (47%), while non-Hispanic blacks and Hispanic females tended to use condoms the most (47% and 46%, respectively). LARC use, though low overall, was highest among 12th graders (3%) and non-Hispanic whites (2%).
The study was funded partly by grants from the National Institute of Allergy and Infectious Diseases, and the Centers for Disease Control and Prevention. Ms. Steiner did not report any relevant financial disclosures.
WASHINGTON – While use of long-acting reversible contraception (LARC) has steadily been increasing over recent years, a new study shows that adolescent females who use LARC might be neglecting to wear condoms when engaging in sexual intercourse, regardless of their number of partners, thus predisposing them to a high risk of contracting sexually transmitted infections (STIs).
“Like moderately effective methods of contraception, [LARC] does not protect against STIs, and so use of a condom in conjunction with [LARC] is recommended for STI prevention,” lead author Riley J. Steiner of the Centers for Disease Control and Prevention in Atlanta, explained at the annual meeting of the Society for Adolescent Health and Medicine. The study also was published in JAMA Pediatrics (2016 Mar 14. doi:10.1001/jamapediatrics.2016.0007)
She added that, “We really think that establishing a link between LARC and condom use early on, prior to widespread adolescent uptake of LARC, can help provide a useful reference point for future monitoring and, ultimately, inform STI prevention efforts as LARC is brought to scale.”
Ms. Steiner and her coinvestigators used data from the 2013 national Youth Risk Behavior Survey, a self-administered “paper and pencil” questionnaire conducted every 2 years for students in grades 9-12 in public and private high schools across the United States. Analysis of the data – which looked for age, race, and type of contraceptive used – was conducted in July and August of 2015.
Primary outcome of the analysis was to determine the contraceptive method used the most recent time a female had sexual intercourse: either LARC – via an intrauterine device or an implant – oral contraceptives, Depo-Provera, a patch, or a ring. In total, 2,288 females were included in the study; 41% used condoms, 22% used oral contraceptives, 16% used no contraceptive methods whatsoever, 12% used “withdrawal or other method,” 6% used either Depo-Provera, a patch, or a ring, 2% said they were unsure of what contraceptive, if any, they used, and only 2% of females used LARC.
However, of the 2% that used LARC, adjusted odds ratios revealed that they were significantly more likely not to use condoms (adjusted prevalence ratio [aPR], 0.42; 95% confidence interval, 0.21-0.84) as opposed to females on oral contraceptives. There was no significant difference found in condom use between females on LARC versus those on Depo-Provera, a patch, or a ring (aPR = 0.57; 95% CI, 0.26-1.25).
“Health care professionals may be more likely to offer LARC to adolescents who report not using condoms or using them infrequently, as LARC methods are particularly well suited for adolescents who have difficulty adhering to coitally dependent methods,” Ms. Steiner and her associates said, adding that it is currently unknown “whether the association varies by partnership type; it is possible that the observed differences occur largely among adolescents who consider themselves to be in committed partnerships and thus are less concerned about STIs.”
Females included in the study were 57% white, with just over a third of all 2,288 subjects being in the 12th grade. Condom use was most prevalent among 9th graders (47%), while non-Hispanic blacks and Hispanic females tended to use condoms the most (47% and 46%, respectively). LARC use, though low overall, was highest among 12th graders (3%) and non-Hispanic whites (2%).
The study was funded partly by grants from the National Institute of Allergy and Infectious Diseases, and the Centers for Disease Control and Prevention. Ms. Steiner did not report any relevant financial disclosures.
AT THE SAHM ANNUAL MEETING
Key clinical point: Adolescent females using LARC to prevent pregnancy often don’t use condoms, even if they have more than one sexual partner, leading to a high risk of contracting and transmitting STIs.
Major finding: 1.8% of sexually active females included in the study used LARC; however, these females were 60% less likely to use condoms, compared with females using oral contraceptives.
Data source: Cross-sectional analysis of data on 2,288 sexually active females from the 2013 national Youth Risk Behavior Survey of U.S. students in grades 9-12.
Disclosures: The study was funded partly by grants from the National Institute of Allergy and Infectious Diseases, and the CDC. Ms. Steiner did not report any relevant financial disclosures.
Dengue vaccine 100% effective in human challenge trial
A newly developed vaccine, known as TV003, has been shown to induce complete protection against dengue fever in a human challenge model, making it the first-ever such vaccine for the world’s most common mosquito-borne viral disease.
“Control of dengue has certainly been a public health priority for [about a century], but getting there hasn’t really been very easy,” explained Stephen S. Whitehead, Ph.D., of the National Institute of Allergy and Infectious Diseases during a March 15 teleconference held by the American Association for the Advancement of Science. “Dengue virus comes in four different types, or varieties, and a useful vaccine really needs to protect against all four of them at the same time.”
The TV003 vaccine tested in the trial comprised the dengue virus type 1 (DEN1)delta30, DEN2/4delta30, DEN3-3delta30/31-7164, and DEN4delta30 strains. Initially, Dr. Whitehead and his team planned to use rDEN2delta30 as the component for protecting against type 2 dengue virus strains, but “it was not sufficiently attenuated in preclinical studies when compared with its parent virus.” Therefore, it was chosen as the challenge virus to test the protective efficacy of TV003.
Dr. Whitehead and his coinvestigators evaluated 118 individuals for inclusion in the human challenge trial, seeking flavivirus-naive subjects from centers in Burlington, Vt., and Baltimore during November 2013–February 2014. Eventually, 48 subjects were enrolled and randomly assigned to receive the TV003 vaccine or placebo.
After 6 months, subjects were injected with rDEN2delta30, a recombinant strain of dengue virus, to determine the viability of TV003. Of the 48 participants, 41 returned for follow-up: 21 in the TV003 group and 20 in the placebo cohort.
None of the 21 subjects in the TV003 group developed any dengue virus infection after exposure to rDEN2delta30, meaning the candidate vaccine was 100% effective. However, in the placebo group, 100% of the 20 subjects developed viremia, 95% had rDEN2delta30 recovered from blood samples on multiple days, 80% developed a rash consistent with dengue virus infection, and 20% developed neutropenia. Subjects in the TV003 cohort reported an adverse event of a “mild, asymptomatic rash” in 79% of cases.
“The strong protective immunity against DENV-2 induced by TV003 is likely a combination of both a strong homotypic antibody response against DENV-2 that can prevent infection in most of the subjects and a cellular immune response that controls infection if it does occur,” Dr. Whitehead wrote (Sci Transl Med. 2016 Mar 16. doi: 10.1126/scitranslmed.aaf1517). “Under investigation are the roles of both in the protective immune response to dengue to better define a correlate of vaccine efficacy.”
There were no statistical differences between the vaccine and placebo groups in age (29 and 31 years, respectively) sex (54% and 67% male), or race (58% and 63% white).
The study was funded by the National Institutes of Allergy and Infectious Diseases Intramural Research Program. Dr. Whitehead disclosed that he is an inventor of three patents related to components of a dengue virus vaccine. No other authors reported any relevant financial disclosures.
A newly developed vaccine, known as TV003, has been shown to induce complete protection against dengue fever in a human challenge model, making it the first-ever such vaccine for the world’s most common mosquito-borne viral disease.
“Control of dengue has certainly been a public health priority for [about a century], but getting there hasn’t really been very easy,” explained Stephen S. Whitehead, Ph.D., of the National Institute of Allergy and Infectious Diseases during a March 15 teleconference held by the American Association for the Advancement of Science. “Dengue virus comes in four different types, or varieties, and a useful vaccine really needs to protect against all four of them at the same time.”
The TV003 vaccine tested in the trial comprised the dengue virus type 1 (DEN1)delta30, DEN2/4delta30, DEN3-3delta30/31-7164, and DEN4delta30 strains. Initially, Dr. Whitehead and his team planned to use rDEN2delta30 as the component for protecting against type 2 dengue virus strains, but “it was not sufficiently attenuated in preclinical studies when compared with its parent virus.” Therefore, it was chosen as the challenge virus to test the protective efficacy of TV003.
Dr. Whitehead and his coinvestigators evaluated 118 individuals for inclusion in the human challenge trial, seeking flavivirus-naive subjects from centers in Burlington, Vt., and Baltimore during November 2013–February 2014. Eventually, 48 subjects were enrolled and randomly assigned to receive the TV003 vaccine or placebo.
After 6 months, subjects were injected with rDEN2delta30, a recombinant strain of dengue virus, to determine the viability of TV003. Of the 48 participants, 41 returned for follow-up: 21 in the TV003 group and 20 in the placebo cohort.
None of the 21 subjects in the TV003 group developed any dengue virus infection after exposure to rDEN2delta30, meaning the candidate vaccine was 100% effective. However, in the placebo group, 100% of the 20 subjects developed viremia, 95% had rDEN2delta30 recovered from blood samples on multiple days, 80% developed a rash consistent with dengue virus infection, and 20% developed neutropenia. Subjects in the TV003 cohort reported an adverse event of a “mild, asymptomatic rash” in 79% of cases.
“The strong protective immunity against DENV-2 induced by TV003 is likely a combination of both a strong homotypic antibody response against DENV-2 that can prevent infection in most of the subjects and a cellular immune response that controls infection if it does occur,” Dr. Whitehead wrote (Sci Transl Med. 2016 Mar 16. doi: 10.1126/scitranslmed.aaf1517). “Under investigation are the roles of both in the protective immune response to dengue to better define a correlate of vaccine efficacy.”
There were no statistical differences between the vaccine and placebo groups in age (29 and 31 years, respectively) sex (54% and 67% male), or race (58% and 63% white).
The study was funded by the National Institutes of Allergy and Infectious Diseases Intramural Research Program. Dr. Whitehead disclosed that he is an inventor of three patents related to components of a dengue virus vaccine. No other authors reported any relevant financial disclosures.
A newly developed vaccine, known as TV003, has been shown to induce complete protection against dengue fever in a human challenge model, making it the first-ever such vaccine for the world’s most common mosquito-borne viral disease.
“Control of dengue has certainly been a public health priority for [about a century], but getting there hasn’t really been very easy,” explained Stephen S. Whitehead, Ph.D., of the National Institute of Allergy and Infectious Diseases during a March 15 teleconference held by the American Association for the Advancement of Science. “Dengue virus comes in four different types, or varieties, and a useful vaccine really needs to protect against all four of them at the same time.”
The TV003 vaccine tested in the trial comprised the dengue virus type 1 (DEN1)delta30, DEN2/4delta30, DEN3-3delta30/31-7164, and DEN4delta30 strains. Initially, Dr. Whitehead and his team planned to use rDEN2delta30 as the component for protecting against type 2 dengue virus strains, but “it was not sufficiently attenuated in preclinical studies when compared with its parent virus.” Therefore, it was chosen as the challenge virus to test the protective efficacy of TV003.
Dr. Whitehead and his coinvestigators evaluated 118 individuals for inclusion in the human challenge trial, seeking flavivirus-naive subjects from centers in Burlington, Vt., and Baltimore during November 2013–February 2014. Eventually, 48 subjects were enrolled and randomly assigned to receive the TV003 vaccine or placebo.
After 6 months, subjects were injected with rDEN2delta30, a recombinant strain of dengue virus, to determine the viability of TV003. Of the 48 participants, 41 returned for follow-up: 21 in the TV003 group and 20 in the placebo cohort.
None of the 21 subjects in the TV003 group developed any dengue virus infection after exposure to rDEN2delta30, meaning the candidate vaccine was 100% effective. However, in the placebo group, 100% of the 20 subjects developed viremia, 95% had rDEN2delta30 recovered from blood samples on multiple days, 80% developed a rash consistent with dengue virus infection, and 20% developed neutropenia. Subjects in the TV003 cohort reported an adverse event of a “mild, asymptomatic rash” in 79% of cases.
“The strong protective immunity against DENV-2 induced by TV003 is likely a combination of both a strong homotypic antibody response against DENV-2 that can prevent infection in most of the subjects and a cellular immune response that controls infection if it does occur,” Dr. Whitehead wrote (Sci Transl Med. 2016 Mar 16. doi: 10.1126/scitranslmed.aaf1517). “Under investigation are the roles of both in the protective immune response to dengue to better define a correlate of vaccine efficacy.”
There were no statistical differences between the vaccine and placebo groups in age (29 and 31 years, respectively) sex (54% and 67% male), or race (58% and 63% white).
The study was funded by the National Institutes of Allergy and Infectious Diseases Intramural Research Program. Dr. Whitehead disclosed that he is an inventor of three patents related to components of a dengue virus vaccine. No other authors reported any relevant financial disclosures.
FROM AN AAAS TELECON
Key clinical point: TV003, a live attenuated dengue virus vaccine, can induce complete protection against the virus.
Major finding: All of the 21 subjects who received TV003 and were exposed to the rDEN2Delta30 strain of DENV-2 were protected from infection and did not develop dengue fever.
Data source: A randomized, double-blind, placebo-controlled trial of 48 individuals enrolled between November 2013 and February 2014.
Disclosures: Study funded by the National Institutes of Allergy and Infectious Diseases Intramural Research Program; Dr. Whitehead disclosed a potential conflict of interest.
Zika vaccine candidates possible by early 2017
Phase I trials to determine the safety and immunogenicity of a Zika virus vaccine could begin as soon as late summer or early fall of this year, with a candidate vaccine by early 2017.
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases at the U.S. National Institutes of Health, made the announcement during a call with the media on March 10, stating that finding a vaccine to combat the increasingly problematic spread of the Zika virus is a top priority of federal health agencies.
Phase I trials “usually take several months – 3 or 4 months – to get an answer,” said Dr. Fauci, adding that he hopes to have “a candidate or candidates that are safe and can induce an immune response” by early 2017.
Dr. Fauci said that he hopes the vaccine could be selected for an accelerated approval schedule so that it could be manufactured and distributed as quickly as possible. That will, however, depend in large part on the state of the Zika virus outbreak in early 2017, a situation he called “impossible to predict.”
“What I can tell you is that we’ll be testing the vaccine in phase I [by] the early fall,” Dr. Fauci said.
Dr. Tom Frieden, director of the U.S. Centers for Disease Control and Prevention, echoed Dr. Fauci’s concerns about the growing Zika virus outbreak in the Americas.
Having just returned from a trip to Puerto Rico, Dr. Frieden said he is “very concerned that, before the year is out, we could see hundreds of thousands of Zika infections in Puerto Rico, and thousands of infected pregnant women.”
Health officials, however, are making progress. The CDC and the NIH are closer than ever to understanding the links between Zika virus and the neurological conditions that have been associated with the virus, including microcephaly and Guillain-Barré syndrome.
“Never before have we had a mosquito-borne infection that could cause serious birth defects on a large scale,” Dr. Frieden said, adding that “funding from Congress is urgently needed” to adequately attack the growing threat.
Another approach being targeted to fight the Zika virus is controlling the way it is spread – through mosquitoes. To that end, Dr. Frieden outlined a four-pronged approach to reduce exposure to mosquitoes “inside the home, outside the home, at the larval stage, and at the adult mosquito stage,” including using insect repellents and wearing long-sleeve shirts and pants.
“The bottom line here is that [this] is an uphill battle,” Dr. Frieden said. “We know we won’t be able to protect 100% of women, but for every single case of Zika infection in pregnancy we prevent, we’re potentially preventing an individual, personal, and family tragedy.”
Phase I trials to determine the safety and immunogenicity of a Zika virus vaccine could begin as soon as late summer or early fall of this year, with a candidate vaccine by early 2017.
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases at the U.S. National Institutes of Health, made the announcement during a call with the media on March 10, stating that finding a vaccine to combat the increasingly problematic spread of the Zika virus is a top priority of federal health agencies.
Phase I trials “usually take several months – 3 or 4 months – to get an answer,” said Dr. Fauci, adding that he hopes to have “a candidate or candidates that are safe and can induce an immune response” by early 2017.
Dr. Fauci said that he hopes the vaccine could be selected for an accelerated approval schedule so that it could be manufactured and distributed as quickly as possible. That will, however, depend in large part on the state of the Zika virus outbreak in early 2017, a situation he called “impossible to predict.”
“What I can tell you is that we’ll be testing the vaccine in phase I [by] the early fall,” Dr. Fauci said.
Dr. Tom Frieden, director of the U.S. Centers for Disease Control and Prevention, echoed Dr. Fauci’s concerns about the growing Zika virus outbreak in the Americas.
Having just returned from a trip to Puerto Rico, Dr. Frieden said he is “very concerned that, before the year is out, we could see hundreds of thousands of Zika infections in Puerto Rico, and thousands of infected pregnant women.”
Health officials, however, are making progress. The CDC and the NIH are closer than ever to understanding the links between Zika virus and the neurological conditions that have been associated with the virus, including microcephaly and Guillain-Barré syndrome.
“Never before have we had a mosquito-borne infection that could cause serious birth defects on a large scale,” Dr. Frieden said, adding that “funding from Congress is urgently needed” to adequately attack the growing threat.
Another approach being targeted to fight the Zika virus is controlling the way it is spread – through mosquitoes. To that end, Dr. Frieden outlined a four-pronged approach to reduce exposure to mosquitoes “inside the home, outside the home, at the larval stage, and at the adult mosquito stage,” including using insect repellents and wearing long-sleeve shirts and pants.
“The bottom line here is that [this] is an uphill battle,” Dr. Frieden said. “We know we won’t be able to protect 100% of women, but for every single case of Zika infection in pregnancy we prevent, we’re potentially preventing an individual, personal, and family tragedy.”
Phase I trials to determine the safety and immunogenicity of a Zika virus vaccine could begin as soon as late summer or early fall of this year, with a candidate vaccine by early 2017.
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases at the U.S. National Institutes of Health, made the announcement during a call with the media on March 10, stating that finding a vaccine to combat the increasingly problematic spread of the Zika virus is a top priority of federal health agencies.
Phase I trials “usually take several months – 3 or 4 months – to get an answer,” said Dr. Fauci, adding that he hopes to have “a candidate or candidates that are safe and can induce an immune response” by early 2017.
Dr. Fauci said that he hopes the vaccine could be selected for an accelerated approval schedule so that it could be manufactured and distributed as quickly as possible. That will, however, depend in large part on the state of the Zika virus outbreak in early 2017, a situation he called “impossible to predict.”
“What I can tell you is that we’ll be testing the vaccine in phase I [by] the early fall,” Dr. Fauci said.
Dr. Tom Frieden, director of the U.S. Centers for Disease Control and Prevention, echoed Dr. Fauci’s concerns about the growing Zika virus outbreak in the Americas.
Having just returned from a trip to Puerto Rico, Dr. Frieden said he is “very concerned that, before the year is out, we could see hundreds of thousands of Zika infections in Puerto Rico, and thousands of infected pregnant women.”
Health officials, however, are making progress. The CDC and the NIH are closer than ever to understanding the links between Zika virus and the neurological conditions that have been associated with the virus, including microcephaly and Guillain-Barré syndrome.
“Never before have we had a mosquito-borne infection that could cause serious birth defects on a large scale,” Dr. Frieden said, adding that “funding from Congress is urgently needed” to adequately attack the growing threat.
Another approach being targeted to fight the Zika virus is controlling the way it is spread – through mosquitoes. To that end, Dr. Frieden outlined a four-pronged approach to reduce exposure to mosquitoes “inside the home, outside the home, at the larval stage, and at the adult mosquito stage,” including using insect repellents and wearing long-sleeve shirts and pants.
“The bottom line here is that [this] is an uphill battle,” Dr. Frieden said. “We know we won’t be able to protect 100% of women, but for every single case of Zika infection in pregnancy we prevent, we’re potentially preventing an individual, personal, and family tragedy.”