User login
Progesterone Therapy Ineffective in Women With Recurrent Miscarriages
Women with histories of miscarriage do not experience any significant increase in successful births by undergoing progesterone therapy during the first trimester of pregnancy, according to a new study published Nov. 25 in the New England Journal of Medicine.
“Our results do not support earlier findings of a Cochrane analysis that suggested a benefit of progesterone therapy in the first trimester of pregnancy,” wrote Dr. Arri Coomarasamy, professor of gynecology at the University of Birmingham in Edgbaston, England, and his associates, referencing the 2013 review of 2,158 women across 14 randomized trials, which found that progesterone therapy administered in the first trimester can increase the likelihood of having a successful birth without risk of adverse effects on either the mother or infant.
For the current study, known as the PROMISE trial, the investigators randomized 836 women into cohorts of 404 (progesterone therapy) and 432 (placebo). The progesterone therapy regimen consisted of vaginal suppositories of 400 mg micronized progesterone, inserted twice daily, through 12 weeks of gestation. Those in the placebo cohort also were given vaginal suppositories twice a day for the same duration of the pregnancy (N Engl J Med. 2015;373:2141-8).
Of these women, 826 (98.8%) had follow-up interviews – 398 in the progesterone cohort and 428 in the placebo cohort. Primary outcome (live birth after at least 24 weeks of gestation) occurred in 262 (65.8%) of the women in the progesterone cohort and 271 (63.3%) of the women in the placebo cohort (P = .045). Investigators concluded that there was no significant statistical difference in outcomes between progesterone therapy and placebo based on these results.
The PROMISE study was funded by the United Kingdom National Institute of Health Research. Dr. Coomarasamy did not report any relevant financial disclosures.
Women with histories of miscarriage do not experience any significant increase in successful births by undergoing progesterone therapy during the first trimester of pregnancy, according to a new study published Nov. 25 in the New England Journal of Medicine.
“Our results do not support earlier findings of a Cochrane analysis that suggested a benefit of progesterone therapy in the first trimester of pregnancy,” wrote Dr. Arri Coomarasamy, professor of gynecology at the University of Birmingham in Edgbaston, England, and his associates, referencing the 2013 review of 2,158 women across 14 randomized trials, which found that progesterone therapy administered in the first trimester can increase the likelihood of having a successful birth without risk of adverse effects on either the mother or infant.
For the current study, known as the PROMISE trial, the investigators randomized 836 women into cohorts of 404 (progesterone therapy) and 432 (placebo). The progesterone therapy regimen consisted of vaginal suppositories of 400 mg micronized progesterone, inserted twice daily, through 12 weeks of gestation. Those in the placebo cohort also were given vaginal suppositories twice a day for the same duration of the pregnancy (N Engl J Med. 2015;373:2141-8).
Of these women, 826 (98.8%) had follow-up interviews – 398 in the progesterone cohort and 428 in the placebo cohort. Primary outcome (live birth after at least 24 weeks of gestation) occurred in 262 (65.8%) of the women in the progesterone cohort and 271 (63.3%) of the women in the placebo cohort (P = .045). Investigators concluded that there was no significant statistical difference in outcomes between progesterone therapy and placebo based on these results.
The PROMISE study was funded by the United Kingdom National Institute of Health Research. Dr. Coomarasamy did not report any relevant financial disclosures.
Women with histories of miscarriage do not experience any significant increase in successful births by undergoing progesterone therapy during the first trimester of pregnancy, according to a new study published Nov. 25 in the New England Journal of Medicine.
“Our results do not support earlier findings of a Cochrane analysis that suggested a benefit of progesterone therapy in the first trimester of pregnancy,” wrote Dr. Arri Coomarasamy, professor of gynecology at the University of Birmingham in Edgbaston, England, and his associates, referencing the 2013 review of 2,158 women across 14 randomized trials, which found that progesterone therapy administered in the first trimester can increase the likelihood of having a successful birth without risk of adverse effects on either the mother or infant.
For the current study, known as the PROMISE trial, the investigators randomized 836 women into cohorts of 404 (progesterone therapy) and 432 (placebo). The progesterone therapy regimen consisted of vaginal suppositories of 400 mg micronized progesterone, inserted twice daily, through 12 weeks of gestation. Those in the placebo cohort also were given vaginal suppositories twice a day for the same duration of the pregnancy (N Engl J Med. 2015;373:2141-8).
Of these women, 826 (98.8%) had follow-up interviews – 398 in the progesterone cohort and 428 in the placebo cohort. Primary outcome (live birth after at least 24 weeks of gestation) occurred in 262 (65.8%) of the women in the progesterone cohort and 271 (63.3%) of the women in the placebo cohort (P = .045). Investigators concluded that there was no significant statistical difference in outcomes between progesterone therapy and placebo based on these results.
The PROMISE study was funded by the United Kingdom National Institute of Health Research. Dr. Coomarasamy did not report any relevant financial disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Progesterone therapy ineffective in women with recurrent miscarriages
Women with histories of miscarriage do not experience any significant increase in successful births by undergoing progesterone therapy during the first trimester of pregnancy, according to a new study published Nov. 25 in the New England Journal of Medicine.
“Our results do not support earlier findings of a Cochrane analysis that suggested a benefit of progesterone therapy in the first trimester of pregnancy,” wrote Dr. Arri Coomarasamy, professor of gynecology at the University of Birmingham in Edgbaston, England, and his associates, referencing the 2013 review of 2,158 women across 14 randomized trials, which found that progesterone therapy administered in the first trimester can increase the likelihood of having a successful birth without risk of adverse effects on either the mother or infant.
For the current study, known as the PROMISE trial, the investigators randomized 836 women into cohorts of 404 (progesterone therapy) and 432 (placebo). The progesterone therapy regimen consisted of vaginal suppositories of 400 mg micronized progesterone, inserted twice daily, through 12 weeks of gestation. Those in the placebo cohort also were given vaginal suppositories twice a day for the same duration of the pregnancy (N Engl J Med. 2015;373:2141-8).
Of these women, 826 (98.8%) had follow-up interviews – 398 in the progesterone cohort and 428 in the placebo cohort. Primary outcome (live birth after at least 24 weeks of gestation) occurred in 262 (65.8%) of the women in the progesterone cohort and 271 (63.3%) of the women in the placebo cohort (P = .045). Investigators concluded that there was no significant statistical difference in outcomes between progesterone therapy and placebo based on these results.
The PROMISE study was funded by the United Kingdom National Institute of Health Research. Dr. Coomarasamy did not report any relevant financial disclosures.
Women with histories of miscarriage do not experience any significant increase in successful births by undergoing progesterone therapy during the first trimester of pregnancy, according to a new study published Nov. 25 in the New England Journal of Medicine.
“Our results do not support earlier findings of a Cochrane analysis that suggested a benefit of progesterone therapy in the first trimester of pregnancy,” wrote Dr. Arri Coomarasamy, professor of gynecology at the University of Birmingham in Edgbaston, England, and his associates, referencing the 2013 review of 2,158 women across 14 randomized trials, which found that progesterone therapy administered in the first trimester can increase the likelihood of having a successful birth without risk of adverse effects on either the mother or infant.
For the current study, known as the PROMISE trial, the investigators randomized 836 women into cohorts of 404 (progesterone therapy) and 432 (placebo). The progesterone therapy regimen consisted of vaginal suppositories of 400 mg micronized progesterone, inserted twice daily, through 12 weeks of gestation. Those in the placebo cohort also were given vaginal suppositories twice a day for the same duration of the pregnancy (N Engl J Med. 2015;373:2141-8).
Of these women, 826 (98.8%) had follow-up interviews – 398 in the progesterone cohort and 428 in the placebo cohort. Primary outcome (live birth after at least 24 weeks of gestation) occurred in 262 (65.8%) of the women in the progesterone cohort and 271 (63.3%) of the women in the placebo cohort (P = .045). Investigators concluded that there was no significant statistical difference in outcomes between progesterone therapy and placebo based on these results.
The PROMISE study was funded by the United Kingdom National Institute of Health Research. Dr. Coomarasamy did not report any relevant financial disclosures.
Women with histories of miscarriage do not experience any significant increase in successful births by undergoing progesterone therapy during the first trimester of pregnancy, according to a new study published Nov. 25 in the New England Journal of Medicine.
“Our results do not support earlier findings of a Cochrane analysis that suggested a benefit of progesterone therapy in the first trimester of pregnancy,” wrote Dr. Arri Coomarasamy, professor of gynecology at the University of Birmingham in Edgbaston, England, and his associates, referencing the 2013 review of 2,158 women across 14 randomized trials, which found that progesterone therapy administered in the first trimester can increase the likelihood of having a successful birth without risk of adverse effects on either the mother or infant.
For the current study, known as the PROMISE trial, the investigators randomized 836 women into cohorts of 404 (progesterone therapy) and 432 (placebo). The progesterone therapy regimen consisted of vaginal suppositories of 400 mg micronized progesterone, inserted twice daily, through 12 weeks of gestation. Those in the placebo cohort also were given vaginal suppositories twice a day for the same duration of the pregnancy (N Engl J Med. 2015;373:2141-8).
Of these women, 826 (98.8%) had follow-up interviews – 398 in the progesterone cohort and 428 in the placebo cohort. Primary outcome (live birth after at least 24 weeks of gestation) occurred in 262 (65.8%) of the women in the progesterone cohort and 271 (63.3%) of the women in the placebo cohort (P = .045). Investigators concluded that there was no significant statistical difference in outcomes between progesterone therapy and placebo based on these results.
The PROMISE study was funded by the United Kingdom National Institute of Health Research. Dr. Coomarasamy did not report any relevant financial disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Women who have experienced previous recurrent miscarriages are not significantly more likely to have a successful birth if they undergo progesterone therapy during the first trimester of their pregnancy.
Major finding: Of 398 women in the progesterone cohort, 262 (65.8%) had live births; in the placebo cohort, 271 of the 428 women (63.3%) had live births, indicating no significant difference between the two.
Data source: A multicenter, double-blind, placebo-controlled, randomized trial of 826 pregnant women with history of recurrent miscarriages.
Disclosures: The study was funded by the United Kingdom National Institute of Health Research. Dr. Coomarasamy did not report any relevant financial disclosures.
New ACOG recommendations encourage exercise during pregnancy
Women with uncomplicated pregnancies should be encouraged to engage in aerobic and strength-conditioning exercises, including running, stationary cycling, and modified yoga, according to new recommendations from the American College of Obstetricians and Gynecologists.
Even women who were not active before becoming pregnant can start exercising during pregnancy, provided they consult with their physicians and ramp up their exercise gradually.
“Pregnancy should not be looked at as a state of confinement,” Dr. Raul Artal, chairman emeritus of the department of ob.gyn. at Saint Louis University and the lead author of the ACOG recommendations, said in a statement. “In fact, it is an ideal time for lifestyle modification. That is because more than any other time in her life, a pregnant woman has the most available access to medical care and supervision.”
The opinion from ACOG’s Committee on Obstetric Practice, which was released on Nov. 23, outlines safe and unsafe exercises during pregnancy and in the postpartum period, updating recommendations previously issued in 2002 and reaffirmed in 2009.
The updated recommendations differ from the relatively limited ones published by ACOG in 2002. Previously, ACOG recommended exercise only for women who were recreational or competitive athletes prior to pregnancy. And even in those cases, women were cautioned to “modify their usual exercise routines as medically indicated” and to avoid strenuous exercise in the second and third trimesters, especially women with “a history of or risk for preterm labor or fetal growth restriction.” Women who were not regularly physically active prior to their pregnancies were advised to consult with their physicians before beginning any exercise regimen (Obstet Gynecol 2002;99:171-3).
Now, women are encouraged to engage in some amount of physical activity during pregnancy, but physicians should conduct a thorough clinical evaluation before prescribing a specific exercise program to ensure the patient doesn’t have a medical reason to avoid exercise, according to ACOG.
The updated opinion advises that women should have an eventual goal of moderate-intensity exercise for at least 20-30 minutes per day on most or all days of the week. The “talk test” – whether a woman can carry on a conversation while exercising – is a good way to ensure that the exercise is not too intense.
In the updated recommendations, ACOG designates walking, swimming, stationary cycling, low-impact aerobics, modified yoga or pilates, running, jogging, racquet sports, and strength training as “safe” during pregnancy. But pregnant women should avoid contact sports, scuba diving, sky diving, “hot yoga” or “hot pilates,” and “activities with a high risk of falling” such as gymnastics and skiing, among others (Obstet Gynecol. 2015;126:e135-42).
Some absolute contraindications to aerobic exercise during pregnancy include hemodynamically significant heart disease, restrictive lung disease, incompetent cervix or cerclage, and multiple gestation at risk of premature labor, among others.
Obesity in pregnancy
ACOG also released updated clinical management guidelines for obesity in pregnancy, calling on ob.gyns. to calculate body mass index at the first prenatal visit and offer diet and exercise counseling.
The guidelines advise that obese women can have improved pregnancy outcomes by losing even just a little bit of weight prior to pregnancy, and losing weight between pregnancies can decrease the chances of obese women having “large-for-gestational-age neonates in a subsequent pregnancy” (Obstet Gynecol 2015;126:e112-26).
In addition, ACOG advises physicians to consider allowing a longer first stage of labor in obese women before performing a cesarean delivery for labor arrest. Mechanical thromboprophylaxis is recommended both before and after a cesarean in obese women.
While stillbirth rates are higher in obese pregnant women, ACOG did not make a recommendation for or against routine antenatal fetal surveillance in these women because of a lack of evidence showing clear improvement in pregnancy outcomes with surveillance.
Women with uncomplicated pregnancies should be encouraged to engage in aerobic and strength-conditioning exercises, including running, stationary cycling, and modified yoga, according to new recommendations from the American College of Obstetricians and Gynecologists.
Even women who were not active before becoming pregnant can start exercising during pregnancy, provided they consult with their physicians and ramp up their exercise gradually.
“Pregnancy should not be looked at as a state of confinement,” Dr. Raul Artal, chairman emeritus of the department of ob.gyn. at Saint Louis University and the lead author of the ACOG recommendations, said in a statement. “In fact, it is an ideal time for lifestyle modification. That is because more than any other time in her life, a pregnant woman has the most available access to medical care and supervision.”
The opinion from ACOG’s Committee on Obstetric Practice, which was released on Nov. 23, outlines safe and unsafe exercises during pregnancy and in the postpartum period, updating recommendations previously issued in 2002 and reaffirmed in 2009.
The updated recommendations differ from the relatively limited ones published by ACOG in 2002. Previously, ACOG recommended exercise only for women who were recreational or competitive athletes prior to pregnancy. And even in those cases, women were cautioned to “modify their usual exercise routines as medically indicated” and to avoid strenuous exercise in the second and third trimesters, especially women with “a history of or risk for preterm labor or fetal growth restriction.” Women who were not regularly physically active prior to their pregnancies were advised to consult with their physicians before beginning any exercise regimen (Obstet Gynecol 2002;99:171-3).
Now, women are encouraged to engage in some amount of physical activity during pregnancy, but physicians should conduct a thorough clinical evaluation before prescribing a specific exercise program to ensure the patient doesn’t have a medical reason to avoid exercise, according to ACOG.
The updated opinion advises that women should have an eventual goal of moderate-intensity exercise for at least 20-30 minutes per day on most or all days of the week. The “talk test” – whether a woman can carry on a conversation while exercising – is a good way to ensure that the exercise is not too intense.
In the updated recommendations, ACOG designates walking, swimming, stationary cycling, low-impact aerobics, modified yoga or pilates, running, jogging, racquet sports, and strength training as “safe” during pregnancy. But pregnant women should avoid contact sports, scuba diving, sky diving, “hot yoga” or “hot pilates,” and “activities with a high risk of falling” such as gymnastics and skiing, among others (Obstet Gynecol. 2015;126:e135-42).
Some absolute contraindications to aerobic exercise during pregnancy include hemodynamically significant heart disease, restrictive lung disease, incompetent cervix or cerclage, and multiple gestation at risk of premature labor, among others.
Obesity in pregnancy
ACOG also released updated clinical management guidelines for obesity in pregnancy, calling on ob.gyns. to calculate body mass index at the first prenatal visit and offer diet and exercise counseling.
The guidelines advise that obese women can have improved pregnancy outcomes by losing even just a little bit of weight prior to pregnancy, and losing weight between pregnancies can decrease the chances of obese women having “large-for-gestational-age neonates in a subsequent pregnancy” (Obstet Gynecol 2015;126:e112-26).
In addition, ACOG advises physicians to consider allowing a longer first stage of labor in obese women before performing a cesarean delivery for labor arrest. Mechanical thromboprophylaxis is recommended both before and after a cesarean in obese women.
While stillbirth rates are higher in obese pregnant women, ACOG did not make a recommendation for or against routine antenatal fetal surveillance in these women because of a lack of evidence showing clear improvement in pregnancy outcomes with surveillance.
Women with uncomplicated pregnancies should be encouraged to engage in aerobic and strength-conditioning exercises, including running, stationary cycling, and modified yoga, according to new recommendations from the American College of Obstetricians and Gynecologists.
Even women who were not active before becoming pregnant can start exercising during pregnancy, provided they consult with their physicians and ramp up their exercise gradually.
“Pregnancy should not be looked at as a state of confinement,” Dr. Raul Artal, chairman emeritus of the department of ob.gyn. at Saint Louis University and the lead author of the ACOG recommendations, said in a statement. “In fact, it is an ideal time for lifestyle modification. That is because more than any other time in her life, a pregnant woman has the most available access to medical care and supervision.”
The opinion from ACOG’s Committee on Obstetric Practice, which was released on Nov. 23, outlines safe and unsafe exercises during pregnancy and in the postpartum period, updating recommendations previously issued in 2002 and reaffirmed in 2009.
The updated recommendations differ from the relatively limited ones published by ACOG in 2002. Previously, ACOG recommended exercise only for women who were recreational or competitive athletes prior to pregnancy. And even in those cases, women were cautioned to “modify their usual exercise routines as medically indicated” and to avoid strenuous exercise in the second and third trimesters, especially women with “a history of or risk for preterm labor or fetal growth restriction.” Women who were not regularly physically active prior to their pregnancies were advised to consult with their physicians before beginning any exercise regimen (Obstet Gynecol 2002;99:171-3).
Now, women are encouraged to engage in some amount of physical activity during pregnancy, but physicians should conduct a thorough clinical evaluation before prescribing a specific exercise program to ensure the patient doesn’t have a medical reason to avoid exercise, according to ACOG.
The updated opinion advises that women should have an eventual goal of moderate-intensity exercise for at least 20-30 minutes per day on most or all days of the week. The “talk test” – whether a woman can carry on a conversation while exercising – is a good way to ensure that the exercise is not too intense.
In the updated recommendations, ACOG designates walking, swimming, stationary cycling, low-impact aerobics, modified yoga or pilates, running, jogging, racquet sports, and strength training as “safe” during pregnancy. But pregnant women should avoid contact sports, scuba diving, sky diving, “hot yoga” or “hot pilates,” and “activities with a high risk of falling” such as gymnastics and skiing, among others (Obstet Gynecol. 2015;126:e135-42).
Some absolute contraindications to aerobic exercise during pregnancy include hemodynamically significant heart disease, restrictive lung disease, incompetent cervix or cerclage, and multiple gestation at risk of premature labor, among others.
Obesity in pregnancy
ACOG also released updated clinical management guidelines for obesity in pregnancy, calling on ob.gyns. to calculate body mass index at the first prenatal visit and offer diet and exercise counseling.
The guidelines advise that obese women can have improved pregnancy outcomes by losing even just a little bit of weight prior to pregnancy, and losing weight between pregnancies can decrease the chances of obese women having “large-for-gestational-age neonates in a subsequent pregnancy” (Obstet Gynecol 2015;126:e112-26).
In addition, ACOG advises physicians to consider allowing a longer first stage of labor in obese women before performing a cesarean delivery for labor arrest. Mechanical thromboprophylaxis is recommended both before and after a cesarean in obese women.
While stillbirth rates are higher in obese pregnant women, ACOG did not make a recommendation for or against routine antenatal fetal surveillance in these women because of a lack of evidence showing clear improvement in pregnancy outcomes with surveillance.
FROM OBSTETRICS AND GYNECOLOGY
FDA approves first naloxone nasal spray for opioid overdose
The Food and Drug Administration has approved the first nasal spray variant of the opioid-overdose drug naloxone hydrochloride.
Marketed in the United States as Narcan by Adapt Pharma, a partner of Lightlake Therapeutics, the nasal spray is known to stop or, in some cases, reverse the effects of opioid overdosing in patients. Narcan is the first naloxone hydrochloride nasal spray approved by the FDA.
“Combating the opioid abuse epidemic is a top priority for the FDA,” Dr. Stephen Ostroff, FDA acting commissioner, said in a statement released with the Nov. 18 approval announcement. “We cannot stand by while Americans are dying. While naloxone will not solve the underlying problems of the opioid epidemic, we are speeding to review new formulations that will ultimately save lives that might otherwise be lost to drug addiction and overdose.”
The nasal spray itself is available only with a prescription, and is safe for use by both adults and children, according to the FDA.
The spray delivers a dose of 4 mg naloxone in a single 0.1-mL nasal spray, which comes in a ready-to-use, needle-free device, according to Adapt Pharma. Dosage varies for each individual and should be determined by physicians.
Administration of Narcan, which is sprayed into one nostril while the patient is lying on his or her back, does not require special training and can be performed by anyone.
Narcan’s approval comes less than 4 months after the FDA granted the medication a fast-track designation and priority review status, both of which are meant to expedite the review and approval processes for drugs that “demonstrate the potential to address an unmet medical need” and “offer a significant improvement in the safety or effectiveness of the treatment, prevention, or diagnosis of a serious condition,” according to the FDA’s approval statement.
Adverse events associated with opiate withdrawal have been noted in Narcan patients. Specifically, the FDA warned that body aches, diarrhea, tachycardia, fever, piloerection, nausea, nervousness, abdominal cramps, weakness, and increased blood pressure, among other conditions, are all possible side effects of Narcan.
“Opioid overdose is responsible for the deaths of thousands of Americans in communities throughout the country, leaving a trail of devastation for friends and families,” Seamus Mulligan, Adapt Pharma’s chairman and CEO, said in a statement. “This new device makes naloxone readily available for emergency use by a friend, family member, or caregiver, as well as offering an alternative treatment option for first responders and health care providers.”
Narcan’s approval is one step of many that must be taken to adequately address and ultimately end the problem of opioid abuse in the United States, cautioned Dr. Peter Friedmann, chief research officer at Baystate Health in Springfield, Mass.
“[Narcan] is just addressing overdose; we need more and better medications for treating addiction, we need more physicians and clinicians who are skilled in using these medications,” said Dr. Friedmann. “Given the ongoing crisis of deaths from opioid overuse, this expands the options that physicians, pharmacies, and community distribution programs can use to reduce these deaths.”
Dr. Friedmann also voiced his concern regarding the pricing of Narcan. Making the drug affordable is crucial to its success at successfully treating opioid overuse, he said.
“Right now, nasal atomizers with syringes are used off label, and the prices have been going up with increasing demand,” he said. “But [Narcan] is a commercial product based around what is essentially a generic medication, so [I] hope it’s priced at a price point that’s accessible to the great majority of patients and their families who are facing addiction, many of whom don’t have huge means.”
Dr. Friedmann said that he hopes addiction medicine becomes a more attractive field for medical students and residents. It’s important for future physicians to know how to properly treat patients of addiction and administer drugs safely and effectively, he said.
“Addiction medicine is on the cusp of full recognition as a medical specialty, and we need people to go into that field to teach patients, medical students, and residents how to treat people with addiction,” Dr. Friedmann said. At the current rate, “we’re never going to have enough, so we need generalists to take this on.”
The Food and Drug Administration has approved the first nasal spray variant of the opioid-overdose drug naloxone hydrochloride.
Marketed in the United States as Narcan by Adapt Pharma, a partner of Lightlake Therapeutics, the nasal spray is known to stop or, in some cases, reverse the effects of opioid overdosing in patients. Narcan is the first naloxone hydrochloride nasal spray approved by the FDA.
“Combating the opioid abuse epidemic is a top priority for the FDA,” Dr. Stephen Ostroff, FDA acting commissioner, said in a statement released with the Nov. 18 approval announcement. “We cannot stand by while Americans are dying. While naloxone will not solve the underlying problems of the opioid epidemic, we are speeding to review new formulations that will ultimately save lives that might otherwise be lost to drug addiction and overdose.”
The nasal spray itself is available only with a prescription, and is safe for use by both adults and children, according to the FDA.
The spray delivers a dose of 4 mg naloxone in a single 0.1-mL nasal spray, which comes in a ready-to-use, needle-free device, according to Adapt Pharma. Dosage varies for each individual and should be determined by physicians.
Administration of Narcan, which is sprayed into one nostril while the patient is lying on his or her back, does not require special training and can be performed by anyone.
Narcan’s approval comes less than 4 months after the FDA granted the medication a fast-track designation and priority review status, both of which are meant to expedite the review and approval processes for drugs that “demonstrate the potential to address an unmet medical need” and “offer a significant improvement in the safety or effectiveness of the treatment, prevention, or diagnosis of a serious condition,” according to the FDA’s approval statement.
Adverse events associated with opiate withdrawal have been noted in Narcan patients. Specifically, the FDA warned that body aches, diarrhea, tachycardia, fever, piloerection, nausea, nervousness, abdominal cramps, weakness, and increased blood pressure, among other conditions, are all possible side effects of Narcan.
“Opioid overdose is responsible for the deaths of thousands of Americans in communities throughout the country, leaving a trail of devastation for friends and families,” Seamus Mulligan, Adapt Pharma’s chairman and CEO, said in a statement. “This new device makes naloxone readily available for emergency use by a friend, family member, or caregiver, as well as offering an alternative treatment option for first responders and health care providers.”
Narcan’s approval is one step of many that must be taken to adequately address and ultimately end the problem of opioid abuse in the United States, cautioned Dr. Peter Friedmann, chief research officer at Baystate Health in Springfield, Mass.
“[Narcan] is just addressing overdose; we need more and better medications for treating addiction, we need more physicians and clinicians who are skilled in using these medications,” said Dr. Friedmann. “Given the ongoing crisis of deaths from opioid overuse, this expands the options that physicians, pharmacies, and community distribution programs can use to reduce these deaths.”
Dr. Friedmann also voiced his concern regarding the pricing of Narcan. Making the drug affordable is crucial to its success at successfully treating opioid overuse, he said.
“Right now, nasal atomizers with syringes are used off label, and the prices have been going up with increasing demand,” he said. “But [Narcan] is a commercial product based around what is essentially a generic medication, so [I] hope it’s priced at a price point that’s accessible to the great majority of patients and their families who are facing addiction, many of whom don’t have huge means.”
Dr. Friedmann said that he hopes addiction medicine becomes a more attractive field for medical students and residents. It’s important for future physicians to know how to properly treat patients of addiction and administer drugs safely and effectively, he said.
“Addiction medicine is on the cusp of full recognition as a medical specialty, and we need people to go into that field to teach patients, medical students, and residents how to treat people with addiction,” Dr. Friedmann said. At the current rate, “we’re never going to have enough, so we need generalists to take this on.”
The Food and Drug Administration has approved the first nasal spray variant of the opioid-overdose drug naloxone hydrochloride.
Marketed in the United States as Narcan by Adapt Pharma, a partner of Lightlake Therapeutics, the nasal spray is known to stop or, in some cases, reverse the effects of opioid overdosing in patients. Narcan is the first naloxone hydrochloride nasal spray approved by the FDA.
“Combating the opioid abuse epidemic is a top priority for the FDA,” Dr. Stephen Ostroff, FDA acting commissioner, said in a statement released with the Nov. 18 approval announcement. “We cannot stand by while Americans are dying. While naloxone will not solve the underlying problems of the opioid epidemic, we are speeding to review new formulations that will ultimately save lives that might otherwise be lost to drug addiction and overdose.”
The nasal spray itself is available only with a prescription, and is safe for use by both adults and children, according to the FDA.
The spray delivers a dose of 4 mg naloxone in a single 0.1-mL nasal spray, which comes in a ready-to-use, needle-free device, according to Adapt Pharma. Dosage varies for each individual and should be determined by physicians.
Administration of Narcan, which is sprayed into one nostril while the patient is lying on his or her back, does not require special training and can be performed by anyone.
Narcan’s approval comes less than 4 months after the FDA granted the medication a fast-track designation and priority review status, both of which are meant to expedite the review and approval processes for drugs that “demonstrate the potential to address an unmet medical need” and “offer a significant improvement in the safety or effectiveness of the treatment, prevention, or diagnosis of a serious condition,” according to the FDA’s approval statement.
Adverse events associated with opiate withdrawal have been noted in Narcan patients. Specifically, the FDA warned that body aches, diarrhea, tachycardia, fever, piloerection, nausea, nervousness, abdominal cramps, weakness, and increased blood pressure, among other conditions, are all possible side effects of Narcan.
“Opioid overdose is responsible for the deaths of thousands of Americans in communities throughout the country, leaving a trail of devastation for friends and families,” Seamus Mulligan, Adapt Pharma’s chairman and CEO, said in a statement. “This new device makes naloxone readily available for emergency use by a friend, family member, or caregiver, as well as offering an alternative treatment option for first responders and health care providers.”
Narcan’s approval is one step of many that must be taken to adequately address and ultimately end the problem of opioid abuse in the United States, cautioned Dr. Peter Friedmann, chief research officer at Baystate Health in Springfield, Mass.
“[Narcan] is just addressing overdose; we need more and better medications for treating addiction, we need more physicians and clinicians who are skilled in using these medications,” said Dr. Friedmann. “Given the ongoing crisis of deaths from opioid overuse, this expands the options that physicians, pharmacies, and community distribution programs can use to reduce these deaths.”
Dr. Friedmann also voiced his concern regarding the pricing of Narcan. Making the drug affordable is crucial to its success at successfully treating opioid overuse, he said.
“Right now, nasal atomizers with syringes are used off label, and the prices have been going up with increasing demand,” he said. “But [Narcan] is a commercial product based around what is essentially a generic medication, so [I] hope it’s priced at a price point that’s accessible to the great majority of patients and their families who are facing addiction, many of whom don’t have huge means.”
Dr. Friedmann said that he hopes addiction medicine becomes a more attractive field for medical students and residents. It’s important for future physicians to know how to properly treat patients of addiction and administer drugs safely and effectively, he said.
“Addiction medicine is on the cusp of full recognition as a medical specialty, and we need people to go into that field to teach patients, medical students, and residents how to treat people with addiction,” Dr. Friedmann said. At the current rate, “we’re never going to have enough, so we need generalists to take this on.”
Mild and moderate OSAS often resolves in children
Mild to moderate obstructive sleep apnea syndrome (OSAS) resolves spontaneously in many children in as few as 7 months, based on polysomnography results from the control arm of the Childhood Adenotonsillectomy Trial (CHAT).
Symptomatic improvement in snoring, however, was less common. Nonetheless, “watchful waiting may be a reasonable option in children with low OSAS symptom burden and, especially, little snoring, who also have low AHIs [apnea/hypopnea indexes] and do not have central obesity,” markers that were most likely to be associated with resolution, wrote Dr. Ronald D. Chervin of the University of Michigan, Ann Arbor, and his colleagues. “Without surgery, habitual snoring resolves in one-half to two-thirds of affected children within 1-3 years.”
The study enrolled 453 children, aged 5-9, with an AHI of at least 2 events per hour of sleep, or an obstructive apnea index (OHI) of at least 1. All children were recruited from pediatric sleep clinics and otolaryngology practices. The study did not include children with severe OSAS, which was defined as having an apnea/hypopnea index of greater than 30, an obstructive apnea index greater than 20, or oxygen saturation less than 90% for at least 2% of total sleep time. None of the study participants had recurrent tonsillitis, had a BMI z-score of at least 3, or were taking medication for attention-deficit/hyperactivity disorder, the investigators reported (Chest. 2015;148[5]:1204-13).
Among 453 children randomized in CHAT, 194 in the control arm had complete follow-up, remained untreated surgically, and provided data for the current analyses. Mean AHI at baseline was 6.7 (range, 1.1-29.3), mean oxygen saturation at baseline was 88.8% (range, 59%-97%), and mean score on the Pediatric Sleep Questionnaire Sleep-Related Breathing Disorder (PSQ-SRBD) scale at baseline was 0.48 (range, 0.05-0.90).
Primary endpoints based on polysomnography results at 7-month follow-up were reaching an AHI of less than 2 and an obstructive apnea index of less than 1. In addition, researchers defined “substantive resolution” of symptoms related to OSAS as a total PSQ-SRBD score of 0.33 or more at baseline that declined below 0.33 and was at least 25% below the baseline value at 7-month follow-up.
At 7 months, OSAS had spontaneously resolved by polysomnography measures in 82 of the 194 children based on achieving an AHI less than 2 and an OAI less than 1. The results did not differ by sex.
However, symptomatic improvement was less common. Of 167 children with PSQ-SRBD scores of at least 0.33 at baseline, only 25 children (15%) had scores less than 0.33 and at least a 25% reduction in PSQ-SRBD score at 7 months. Of the 25, 17 were girls and 8 were boys, indicating a higher rate of spontaneous resolution in girls than in boys (P = .033). In addition, only 20 children (12%) showed both polysomnographic and symptomatic resolution of symptoms at 7 months.
“Symptoms often matter more to patients and families than do laboratory results,” the authors wrote. “In our cohort, 34 of 147 habitual snorers (23%) were no longer habitual snorers at follow-up.”
The CHAT Study was supported by the National Institutes of Health. Dr. Chervin disclosed that he is named in or has developed, patented, and copyrighted materials owned by the University of Michigan and designed to assist with assessment or treatment of sleep disorders, including the Pediatric Sleep Questionnaire Sleep-Related Breathing Disorder scale used in this study. He also has received support for research and education from Philips Respironics and Fisher & Paykel Healthcare, and has consulted for MC3 and Zansors.
Because polysomnography is expensive, time consuming, and often unavailable, otolaryngologists will often perform an adenotonsillectomy based on a strong clinical history and parental observation in a child with snoring and chronically enlarged adenoids and tonsils. The findings of this study challenge that approach. Surgery may not be the treatment of choice for children who have a low symptom burden, little snoring, low apnea/hypopnea indexes, and no central obesity. For these children, mild OSAS resolves as they grow and a period of watchful waiting makes sense.
Admittedly, adenotonsillectomy is relatively safe, but even relatively safe surgical procedures can have complications. Further, the financial impact associated with professional fees, facility fees, medications, and parental lost time at work is substantial.
We need to better understand who requires surgery and who does not. Encouraging empirical evidence suggests anti-inflammatory agents may be effective in treating mild to moderate OSAS. As we learn more about who is affected by this disorder, new treatments will likely emerge. In the meantime, we can feel comfortable that watchful waiting can be an appropriate strategy for many children.
Dr. Ian Nathanson is a pediatric pulmonologist in Maitland, Fla. He made his comments in an editorial that accompanied the article (Chest. 2015;148[5]:1129-1130).
Because polysomnography is expensive, time consuming, and often unavailable, otolaryngologists will often perform an adenotonsillectomy based on a strong clinical history and parental observation in a child with snoring and chronically enlarged adenoids and tonsils. The findings of this study challenge that approach. Surgery may not be the treatment of choice for children who have a low symptom burden, little snoring, low apnea/hypopnea indexes, and no central obesity. For these children, mild OSAS resolves as they grow and a period of watchful waiting makes sense.
Admittedly, adenotonsillectomy is relatively safe, but even relatively safe surgical procedures can have complications. Further, the financial impact associated with professional fees, facility fees, medications, and parental lost time at work is substantial.
We need to better understand who requires surgery and who does not. Encouraging empirical evidence suggests anti-inflammatory agents may be effective in treating mild to moderate OSAS. As we learn more about who is affected by this disorder, new treatments will likely emerge. In the meantime, we can feel comfortable that watchful waiting can be an appropriate strategy for many children.
Dr. Ian Nathanson is a pediatric pulmonologist in Maitland, Fla. He made his comments in an editorial that accompanied the article (Chest. 2015;148[5]:1129-1130).
Because polysomnography is expensive, time consuming, and often unavailable, otolaryngologists will often perform an adenotonsillectomy based on a strong clinical history and parental observation in a child with snoring and chronically enlarged adenoids and tonsils. The findings of this study challenge that approach. Surgery may not be the treatment of choice for children who have a low symptom burden, little snoring, low apnea/hypopnea indexes, and no central obesity. For these children, mild OSAS resolves as they grow and a period of watchful waiting makes sense.
Admittedly, adenotonsillectomy is relatively safe, but even relatively safe surgical procedures can have complications. Further, the financial impact associated with professional fees, facility fees, medications, and parental lost time at work is substantial.
We need to better understand who requires surgery and who does not. Encouraging empirical evidence suggests anti-inflammatory agents may be effective in treating mild to moderate OSAS. As we learn more about who is affected by this disorder, new treatments will likely emerge. In the meantime, we can feel comfortable that watchful waiting can be an appropriate strategy for many children.
Dr. Ian Nathanson is a pediatric pulmonologist in Maitland, Fla. He made his comments in an editorial that accompanied the article (Chest. 2015;148[5]:1129-1130).
Mild to moderate obstructive sleep apnea syndrome (OSAS) resolves spontaneously in many children in as few as 7 months, based on polysomnography results from the control arm of the Childhood Adenotonsillectomy Trial (CHAT).
Symptomatic improvement in snoring, however, was less common. Nonetheless, “watchful waiting may be a reasonable option in children with low OSAS symptom burden and, especially, little snoring, who also have low AHIs [apnea/hypopnea indexes] and do not have central obesity,” markers that were most likely to be associated with resolution, wrote Dr. Ronald D. Chervin of the University of Michigan, Ann Arbor, and his colleagues. “Without surgery, habitual snoring resolves in one-half to two-thirds of affected children within 1-3 years.”
The study enrolled 453 children, aged 5-9, with an AHI of at least 2 events per hour of sleep, or an obstructive apnea index (OHI) of at least 1. All children were recruited from pediatric sleep clinics and otolaryngology practices. The study did not include children with severe OSAS, which was defined as having an apnea/hypopnea index of greater than 30, an obstructive apnea index greater than 20, or oxygen saturation less than 90% for at least 2% of total sleep time. None of the study participants had recurrent tonsillitis, had a BMI z-score of at least 3, or were taking medication for attention-deficit/hyperactivity disorder, the investigators reported (Chest. 2015;148[5]:1204-13).
Among 453 children randomized in CHAT, 194 in the control arm had complete follow-up, remained untreated surgically, and provided data for the current analyses. Mean AHI at baseline was 6.7 (range, 1.1-29.3), mean oxygen saturation at baseline was 88.8% (range, 59%-97%), and mean score on the Pediatric Sleep Questionnaire Sleep-Related Breathing Disorder (PSQ-SRBD) scale at baseline was 0.48 (range, 0.05-0.90).
Primary endpoints based on polysomnography results at 7-month follow-up were reaching an AHI of less than 2 and an obstructive apnea index of less than 1. In addition, researchers defined “substantive resolution” of symptoms related to OSAS as a total PSQ-SRBD score of 0.33 or more at baseline that declined below 0.33 and was at least 25% below the baseline value at 7-month follow-up.
At 7 months, OSAS had spontaneously resolved by polysomnography measures in 82 of the 194 children based on achieving an AHI less than 2 and an OAI less than 1. The results did not differ by sex.
However, symptomatic improvement was less common. Of 167 children with PSQ-SRBD scores of at least 0.33 at baseline, only 25 children (15%) had scores less than 0.33 and at least a 25% reduction in PSQ-SRBD score at 7 months. Of the 25, 17 were girls and 8 were boys, indicating a higher rate of spontaneous resolution in girls than in boys (P = .033). In addition, only 20 children (12%) showed both polysomnographic and symptomatic resolution of symptoms at 7 months.
“Symptoms often matter more to patients and families than do laboratory results,” the authors wrote. “In our cohort, 34 of 147 habitual snorers (23%) were no longer habitual snorers at follow-up.”
The CHAT Study was supported by the National Institutes of Health. Dr. Chervin disclosed that he is named in or has developed, patented, and copyrighted materials owned by the University of Michigan and designed to assist with assessment or treatment of sleep disorders, including the Pediatric Sleep Questionnaire Sleep-Related Breathing Disorder scale used in this study. He also has received support for research and education from Philips Respironics and Fisher & Paykel Healthcare, and has consulted for MC3 and Zansors.
Mild to moderate obstructive sleep apnea syndrome (OSAS) resolves spontaneously in many children in as few as 7 months, based on polysomnography results from the control arm of the Childhood Adenotonsillectomy Trial (CHAT).
Symptomatic improvement in snoring, however, was less common. Nonetheless, “watchful waiting may be a reasonable option in children with low OSAS symptom burden and, especially, little snoring, who also have low AHIs [apnea/hypopnea indexes] and do not have central obesity,” markers that were most likely to be associated with resolution, wrote Dr. Ronald D. Chervin of the University of Michigan, Ann Arbor, and his colleagues. “Without surgery, habitual snoring resolves in one-half to two-thirds of affected children within 1-3 years.”
The study enrolled 453 children, aged 5-9, with an AHI of at least 2 events per hour of sleep, or an obstructive apnea index (OHI) of at least 1. All children were recruited from pediatric sleep clinics and otolaryngology practices. The study did not include children with severe OSAS, which was defined as having an apnea/hypopnea index of greater than 30, an obstructive apnea index greater than 20, or oxygen saturation less than 90% for at least 2% of total sleep time. None of the study participants had recurrent tonsillitis, had a BMI z-score of at least 3, or were taking medication for attention-deficit/hyperactivity disorder, the investigators reported (Chest. 2015;148[5]:1204-13).
Among 453 children randomized in CHAT, 194 in the control arm had complete follow-up, remained untreated surgically, and provided data for the current analyses. Mean AHI at baseline was 6.7 (range, 1.1-29.3), mean oxygen saturation at baseline was 88.8% (range, 59%-97%), and mean score on the Pediatric Sleep Questionnaire Sleep-Related Breathing Disorder (PSQ-SRBD) scale at baseline was 0.48 (range, 0.05-0.90).
Primary endpoints based on polysomnography results at 7-month follow-up were reaching an AHI of less than 2 and an obstructive apnea index of less than 1. In addition, researchers defined “substantive resolution” of symptoms related to OSAS as a total PSQ-SRBD score of 0.33 or more at baseline that declined below 0.33 and was at least 25% below the baseline value at 7-month follow-up.
At 7 months, OSAS had spontaneously resolved by polysomnography measures in 82 of the 194 children based on achieving an AHI less than 2 and an OAI less than 1. The results did not differ by sex.
However, symptomatic improvement was less common. Of 167 children with PSQ-SRBD scores of at least 0.33 at baseline, only 25 children (15%) had scores less than 0.33 and at least a 25% reduction in PSQ-SRBD score at 7 months. Of the 25, 17 were girls and 8 were boys, indicating a higher rate of spontaneous resolution in girls than in boys (P = .033). In addition, only 20 children (12%) showed both polysomnographic and symptomatic resolution of symptoms at 7 months.
“Symptoms often matter more to patients and families than do laboratory results,” the authors wrote. “In our cohort, 34 of 147 habitual snorers (23%) were no longer habitual snorers at follow-up.”
The CHAT Study was supported by the National Institutes of Health. Dr. Chervin disclosed that he is named in or has developed, patented, and copyrighted materials owned by the University of Michigan and designed to assist with assessment or treatment of sleep disorders, including the Pediatric Sleep Questionnaire Sleep-Related Breathing Disorder scale used in this study. He also has received support for research and education from Philips Respironics and Fisher & Paykel Healthcare, and has consulted for MC3 and Zansors.
FROM CHEST
Key clinical point: Advise parents that moderate obstructive sleep apnea syndrome can spontaneously resolve in children with a low baseline apnea/hypopnea index and a normal waist circumference, or if they have a low Pediatric Sleep Questionnaire and snoring score.
Major finding: After 7 months, 82 of 194 children no longer met polysomnographic criteria for OSAS; 25 of 167 children with baseline PSQ scores of at least 0.33 still had symptoms after 7 months.
Data source: A prospective cohort study of 194 children, aged 5-9 years.
Disclosures: The study was supported by the National Institutes of Health; Dr. Chervin disclosed that he is named in or has developed, patented, and copyrighted materials owned by the University of Michigan and designed to assist with assessment or treatment of sleep disorders, including the Pediatric Sleep Questionnaire Sleep-Related Breathing Disorder scale used in this study.
Heroin smoking linked to emphysema
Inhalation or smoking of heroin can lead to early onset chronic obstructive pulmonary disease (COPD), according to Dr. Paul P. Walker and his colleagues from the University Hospital Aintree and the University of Liverpool, England.
“We believe that we have accumulated sufficient evidence of both physiologic impairment and structural damage to identify a discrete form of early onset COPD, commonly involving emphysema, which can be attributed to inhaled opiate use,” the researchers wrote. “The widespread use of opiates as recreational drugs in some communities means that we are likely to see more obstructive lung disease in the future.”
Recreational use of opiates has been linked to asthma, but there has not been a definitive link to airway disease. “Little is known about the association between heroin inhalation and COPD beyond a study by Buster et al. [and] no previous study has examined measures of emphysema, such as detailed lung function testing or CT scan,” the researchers wrote (Chest. 2015 Nov;148[5]:1156-1163).
The researchers studied 73 individuals who were aged 40 years or younger when they developed symptoms, were diagnosed with COPD, and smoked heroin regularly within the last 2 years. The mean history of smoking heroin was 14 years. The study participants additionally were regular smokers for at least 5 years, most were heavy smokers, and did not have a primary clinical diagnosis of asthma. All had completed spirometry on at least one occasion when clinically stable.
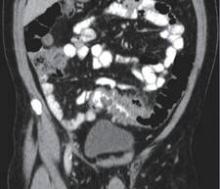
Data was collected during 2005-2013, via lung function testing done when subjects were both clinically stable and a minimum of 4 weeks postexacerbation. Lung function testing was done in 12 subjects via spirometry, either prebronchodilator or postbronchodilator. High-resolution CT scans (slice thickness was no greater than 2 mm) were performed in 32 subjects each analyzed by two thoracic radiologists. Emphysema was scored on a scale of 1-5 based on guidelines produced by Sakai et al., which requires examination of a cranial level taken 1 cm above the superior margin of the aortic arch, a middle level taken 1 cm below the carina, and a caudal level taken about 3 cm above the top of the diaphragm.
Data were available from 44 of the initial 73 subjects. In the 32 who had high-resolution CT scans, their mean score – taking into account the scans of the upper, middle, and lower lung – was 2.3, indicating a 5%-25% chance of emphysema; 15 of 32 individuals had a score greater than 3, indicating a 25%-50% likelihood of emphysema, in the upper lung alone.
In the 12 subjects who underwent lung function testing, the range of the diffusing capacity of the lung for carbon monoxide was 35.5-63.0, with a median of 48.0 and a mean of 50.7. Eleven of these subjects (92%) had score that qualified as “abnormal.”
As a result of “lifestyle and varying motivation” not all subjects completed the planned sequence of the investigation or returned for follow-up spirometric measurement, the researchers wrote. “Taking a history of inhaled drug use is important in patients with early-onset COPD, as is the provision of appropriate education about this new hazard of opiate use among drug users and their caretakers. In some areas and populations there may be a role for case finding using spirometry.”
Dr. Walker and his coauthors did not report any relevant financial disclosures.
This case series of heroin smokers who developed early-onset emphysema may offer insights into the development of COPD and emphysema in cigarette smokers who don’t smoke opiates.
How might narcotic use contribute to the development of COPD and emphysema? There are several possible explanations. Smokers of heroin and other illicit substances typically take a deep inhalation, combined with a Valsalva maneuver to enhance absorption of the drug into the body. This behavior has been described previously in heroin users and users of other smoked substances. In addition, these agents often burn at a very high temperature, with the potential to cause damage deep within the lung.
The depth of inhalation, dynamic hyperinflation, and barotrauma may be important factors in some patients who develop emphysema related to cigarette smoking or other factors, as well. Physicians should be aware of this problem, and the public must be educated about the dangers associated with the inhalation of these and other burned substances.
Dr. David M. Mannino is the chair of preventative medicine and environmental health in the department of epidemiology at the University of Kentucky in Lexington. He disclosed having served as a consultant for Boehringer Ingelheim GmbH, GlaxoSmithKline, AstraZeneca, Novartis AG, Merck, and Forest Pharmaceuticals, and has received research grants from GSK, Novartis, Boehringer Ingelheim, Forest Pharmaceuticals, and Pfizer. He is also compensated by Up-to-Date, has served as an expert in tobacco-related cases, and is on the board of the COPD Foundation. He made his remarks in an editorial published with the study.
This case series of heroin smokers who developed early-onset emphysema may offer insights into the development of COPD and emphysema in cigarette smokers who don’t smoke opiates.
How might narcotic use contribute to the development of COPD and emphysema? There are several possible explanations. Smokers of heroin and other illicit substances typically take a deep inhalation, combined with a Valsalva maneuver to enhance absorption of the drug into the body. This behavior has been described previously in heroin users and users of other smoked substances. In addition, these agents often burn at a very high temperature, with the potential to cause damage deep within the lung.
The depth of inhalation, dynamic hyperinflation, and barotrauma may be important factors in some patients who develop emphysema related to cigarette smoking or other factors, as well. Physicians should be aware of this problem, and the public must be educated about the dangers associated with the inhalation of these and other burned substances.
Dr. David M. Mannino is the chair of preventative medicine and environmental health in the department of epidemiology at the University of Kentucky in Lexington. He disclosed having served as a consultant for Boehringer Ingelheim GmbH, GlaxoSmithKline, AstraZeneca, Novartis AG, Merck, and Forest Pharmaceuticals, and has received research grants from GSK, Novartis, Boehringer Ingelheim, Forest Pharmaceuticals, and Pfizer. He is also compensated by Up-to-Date, has served as an expert in tobacco-related cases, and is on the board of the COPD Foundation. He made his remarks in an editorial published with the study.
This case series of heroin smokers who developed early-onset emphysema may offer insights into the development of COPD and emphysema in cigarette smokers who don’t smoke opiates.
How might narcotic use contribute to the development of COPD and emphysema? There are several possible explanations. Smokers of heroin and other illicit substances typically take a deep inhalation, combined with a Valsalva maneuver to enhance absorption of the drug into the body. This behavior has been described previously in heroin users and users of other smoked substances. In addition, these agents often burn at a very high temperature, with the potential to cause damage deep within the lung.
The depth of inhalation, dynamic hyperinflation, and barotrauma may be important factors in some patients who develop emphysema related to cigarette smoking or other factors, as well. Physicians should be aware of this problem, and the public must be educated about the dangers associated with the inhalation of these and other burned substances.
Dr. David M. Mannino is the chair of preventative medicine and environmental health in the department of epidemiology at the University of Kentucky in Lexington. He disclosed having served as a consultant for Boehringer Ingelheim GmbH, GlaxoSmithKline, AstraZeneca, Novartis AG, Merck, and Forest Pharmaceuticals, and has received research grants from GSK, Novartis, Boehringer Ingelheim, Forest Pharmaceuticals, and Pfizer. He is also compensated by Up-to-Date, has served as an expert in tobacco-related cases, and is on the board of the COPD Foundation. He made his remarks in an editorial published with the study.
Inhalation or smoking of heroin can lead to early onset chronic obstructive pulmonary disease (COPD), according to Dr. Paul P. Walker and his colleagues from the University Hospital Aintree and the University of Liverpool, England.
“We believe that we have accumulated sufficient evidence of both physiologic impairment and structural damage to identify a discrete form of early onset COPD, commonly involving emphysema, which can be attributed to inhaled opiate use,” the researchers wrote. “The widespread use of opiates as recreational drugs in some communities means that we are likely to see more obstructive lung disease in the future.”
Recreational use of opiates has been linked to asthma, but there has not been a definitive link to airway disease. “Little is known about the association between heroin inhalation and COPD beyond a study by Buster et al. [and] no previous study has examined measures of emphysema, such as detailed lung function testing or CT scan,” the researchers wrote (Chest. 2015 Nov;148[5]:1156-1163).
The researchers studied 73 individuals who were aged 40 years or younger when they developed symptoms, were diagnosed with COPD, and smoked heroin regularly within the last 2 years. The mean history of smoking heroin was 14 years. The study participants additionally were regular smokers for at least 5 years, most were heavy smokers, and did not have a primary clinical diagnosis of asthma. All had completed spirometry on at least one occasion when clinically stable.
Data was collected during 2005-2013, via lung function testing done when subjects were both clinically stable and a minimum of 4 weeks postexacerbation. Lung function testing was done in 12 subjects via spirometry, either prebronchodilator or postbronchodilator. High-resolution CT scans (slice thickness was no greater than 2 mm) were performed in 32 subjects each analyzed by two thoracic radiologists. Emphysema was scored on a scale of 1-5 based on guidelines produced by Sakai et al., which requires examination of a cranial level taken 1 cm above the superior margin of the aortic arch, a middle level taken 1 cm below the carina, and a caudal level taken about 3 cm above the top of the diaphragm.
Data were available from 44 of the initial 73 subjects. In the 32 who had high-resolution CT scans, their mean score – taking into account the scans of the upper, middle, and lower lung – was 2.3, indicating a 5%-25% chance of emphysema; 15 of 32 individuals had a score greater than 3, indicating a 25%-50% likelihood of emphysema, in the upper lung alone.
In the 12 subjects who underwent lung function testing, the range of the diffusing capacity of the lung for carbon monoxide was 35.5-63.0, with a median of 48.0 and a mean of 50.7. Eleven of these subjects (92%) had score that qualified as “abnormal.”
As a result of “lifestyle and varying motivation” not all subjects completed the planned sequence of the investigation or returned for follow-up spirometric measurement, the researchers wrote. “Taking a history of inhaled drug use is important in patients with early-onset COPD, as is the provision of appropriate education about this new hazard of opiate use among drug users and their caretakers. In some areas and populations there may be a role for case finding using spirometry.”
Dr. Walker and his coauthors did not report any relevant financial disclosures.
Inhalation or smoking of heroin can lead to early onset chronic obstructive pulmonary disease (COPD), according to Dr. Paul P. Walker and his colleagues from the University Hospital Aintree and the University of Liverpool, England.
“We believe that we have accumulated sufficient evidence of both physiologic impairment and structural damage to identify a discrete form of early onset COPD, commonly involving emphysema, which can be attributed to inhaled opiate use,” the researchers wrote. “The widespread use of opiates as recreational drugs in some communities means that we are likely to see more obstructive lung disease in the future.”
Recreational use of opiates has been linked to asthma, but there has not been a definitive link to airway disease. “Little is known about the association between heroin inhalation and COPD beyond a study by Buster et al. [and] no previous study has examined measures of emphysema, such as detailed lung function testing or CT scan,” the researchers wrote (Chest. 2015 Nov;148[5]:1156-1163).
The researchers studied 73 individuals who were aged 40 years or younger when they developed symptoms, were diagnosed with COPD, and smoked heroin regularly within the last 2 years. The mean history of smoking heroin was 14 years. The study participants additionally were regular smokers for at least 5 years, most were heavy smokers, and did not have a primary clinical diagnosis of asthma. All had completed spirometry on at least one occasion when clinically stable.
Data was collected during 2005-2013, via lung function testing done when subjects were both clinically stable and a minimum of 4 weeks postexacerbation. Lung function testing was done in 12 subjects via spirometry, either prebronchodilator or postbronchodilator. High-resolution CT scans (slice thickness was no greater than 2 mm) were performed in 32 subjects each analyzed by two thoracic radiologists. Emphysema was scored on a scale of 1-5 based on guidelines produced by Sakai et al., which requires examination of a cranial level taken 1 cm above the superior margin of the aortic arch, a middle level taken 1 cm below the carina, and a caudal level taken about 3 cm above the top of the diaphragm.
Data were available from 44 of the initial 73 subjects. In the 32 who had high-resolution CT scans, their mean score – taking into account the scans of the upper, middle, and lower lung – was 2.3, indicating a 5%-25% chance of emphysema; 15 of 32 individuals had a score greater than 3, indicating a 25%-50% likelihood of emphysema, in the upper lung alone.
In the 12 subjects who underwent lung function testing, the range of the diffusing capacity of the lung for carbon monoxide was 35.5-63.0, with a median of 48.0 and a mean of 50.7. Eleven of these subjects (92%) had score that qualified as “abnormal.”
As a result of “lifestyle and varying motivation” not all subjects completed the planned sequence of the investigation or returned for follow-up spirometric measurement, the researchers wrote. “Taking a history of inhaled drug use is important in patients with early-onset COPD, as is the provision of appropriate education about this new hazard of opiate use among drug users and their caretakers. In some areas and populations there may be a role for case finding using spirometry.”
Dr. Walker and his coauthors did not report any relevant financial disclosures.
FROM CHEST
Key clinical point: Recreational smoking of heroin is associated with a higher risk of developing early-onset emphysema.
Major finding: Overall high-resolution CT scan emphysema score averaged across the upper, middle, and lower part of the lung was 2.3 (5%-25% emphysema), with 47% subjects having an upper lobe emphysema score 3 (25%-50% emphysema).
Data source: Cohort study of 73 heroin smokers with clinician-diagnosed and spirometrically confirmed COPD, whose symptoms developed before age 40 years.
Disclosures: The authors did not report any relevant financial disclosures.
PrEP effective in preventing HIV acquisition in MSM and transgender women
Use of pre-exposure prophylaxis (PrEP) by homosexual men and transgender women, even those who already have sexually transmitted infections (STIs), can significantly decrease the likelihood of contracting or spreading STIs among their partners, particularly HIV.
This is according to a prospective study, known as the Demonstration or “Demo” study, published by JAMA Internal Medicine, which examined HIV incidence rates among homosexual men and transgender women in San Francisco, Miami, and Washington for 48 weeks, between Oct. 1, 2012 and Jan. 23, 2014, with a final follow-up on Feb.10, 2015. (2015 Nov 16. doi: 10.1001/jamainternmed.2015.4683)
“Men who have sex with men [MSM] account for more than two-thirds of new HIV infections in the United States and are the only risk group in whom infection rates are rising,” says the study, led by Dr. Albert Y. Liu of the San Francisco Department of Public Health, adding that previous work in this field – namely, the 2010 iPrEx (Pre-Exposure Prophylaxis Initiative) trial – found that tenofovir disoproxil fumarate and emtricitabine led to an overall 44% reduction in HIV acquisition among the aforementioned demographic groups.
A total of 557 participants enrolled, of which 437 (78.5%) were also measured through 48 weeks of follow-up. Participants were given access to a PrEP regimen of daily, oral tenofovir disoproxil fumarate and emtricitabine during clinical visits at 4, 12, 24, 36, and 48 weeks. HIV and STI testing and clinical monitoring were also done during these follow-up visits.
Eligible individuals had to be male at birth, at least 18 years old, have a negative rapid HIV antibody test result at enrollment and a negative fourth-generation antibody-antigen test result at screening, creatinine clearance rate of at least 60 mL/min, and a urine dipstick test with negative or trace findings of protein.
Additionally, all participants were asked to report if they had engaged in condomless anal sex with at least two male or transgender female partners; at least two episodes of anal sex with at least one HIV-infected partner; or sex with a male or transgender female partner and having a diagnosis of syphilis, rectal gonorrhea, or chlamydia in the 12 months prior to enrollment. During the study period, PrEP was discontinued for subjects who underwent seroconversion, and for those who received counseling, partner services, and linkage to HIV primary care.
Of the original 557 who enrolled, 294 (52.8%) ultimately had their tenofovir diphosphate levels measured. Between 80.0% and 85.6% had protective levels of at least four doses per week, indicating high protective levels. However, significant disparity was seen in subjects who were African American (56.8%; P = .03) and those living in the Miami area (65.1%; P less than .01); subjects who had at least two condomless anal sex partners (88.6%; P = .01) and those with stable housing (86.8%; P = .02) were more likely to have high protective levels. Furthermore, the mean number of anal sex partners declined from 10.9 at baseline to 9.3 at the 48 weeks’ follow-up, but the rate of participants engaging in condomless receptive anal sex remained at 65.5% at baseline and at follow-up at 48 weeks.
Regarding acquisition of HIV, only two individuals contracted HIV over the 48 weeks of study, leading to an incidence rate 0.43/100 person-years (95% confidence interval, 0.05-1.54). This is significantly lower than the 90/100 person-years incidence rate of STIs measured by participants at baseline. Both individuals who contracted HIV had tenofovir diphosphate levels indicating that they took fewer than two doses of PrEP per week, and therefore had lower protective levels.
Among the 557 enrolled participants, 25 (4.5%) had no follow-up visits, whereas 383 (68.8%) completed all five visits. Total follow-up was 481 person-years, and after researchers adjusted for each individual site, prior PrEP knowledge and reporting of condomless receptive anal sex at baseline were associated with being retained in the study.
“Adherence was higher among those participants with more reported risk behaviors,” Dr. Liu and his coauthors conclude, adding that “These results provide support for expanding PrEP implementation in MSM in similar clinical settings and highlight the urgent need to increase PrEP awareness and engagement and to develop effective adherence support for highly affected African American and transgender populations.”
To that end, a separate study, also published by JAMA Internal Medicine, looked at “real-world PrEP use” by young, homosexual black men in Chicago. According to a JAMA press release accompanying the release of the uConnect study, “Young black men who have sex with men (YBMSM) are the only group in the United States where HIV incidence has increased over the past decade with effective clinic-based HIV preventions that target YBMSM virtually nonexistent.” (JAMA Intern Med. Nov 16. doi: 10.1001/jamainternmed.2015.6536)
A total of 622 YBMSM – mean age of 23 years, 39% with high school or equivalent level of education, 79% of whom reported annual income of less than $20,000, and only half of whom were both HIV-negative and reported having health coverage – were enrolled, based on eligibility requirements that they self-identified as African American or black, were born male, were between 16 and 29 years of age, and reported oral or anal sex with a male within the 24 months prior to enrollment.
PrEP of daily oral tenofovir disoproxil fumarate and emtricitabine was administered between June 2013 and July 2014. Baseline levels of PrEP awareness – 40.5% of participants knew about PrEP, and 12.1% knew of someone who had used PrEP – remained unchanged significantly at follow-up. Just over 72% of participants were not infected with HIV during the study period; only 3.6% of these individuals had previously used PrEP prior to enrollment.
“Ongoing work should include scientific assessment of strategies to mobilize networks of YBMSM around PrEP as part of a comprehensive health care program. Concomitantly, efforts to mitigate the structural barriers that prevent PrEP uptake among YBMSM may greatly improve the public health effect potential of this promising HIV prevention intervention,” conclude the authors, led by Dr. John A. Schneider of the University of Chicago.
The Demo Study was supported by the NIH’s National Institute for Allergies and Infectious Diseases, National Institute for Mental Health, the Miami Center for AIDS Research, and the Gladstone Institute of Virology & Immunology–University of California, San Francisco. Gilead Sciences supplied the study drugs and support for pharmacokinetic and resistance testing. Dr. Liu disclosed leading other trials in which study drugs were supplied by Gilead Sciences, but no other conflicts of interest. Several other coauthors reported potential conflicts of interest.
The uConnect study was supported by the NIH’s National Institutes of Health. Neither Dr. Schneider nor any coauthors reported any potential conflicts of interest.
Data show that PrEP is effective in preventing HIV infections in men who have sex with men (MSM), as well as in heterosexually active men and women. In intention-to-treat analyses, these studies showed reductions of infections between 44% and 75%, although compliance with daily therapy did not appear to be high. When investigators restricted the analysis to persons with detectable drug levels, effectiveness rates were greater than 90%. An open label extension study in follow-up to the iPrEX (Iniciativa Profilaxis Pre-Exposición) trial found100% protection for those who had sustained adherence at the level of four or more doses per week.
Whether adherence to daily or near-daily dosing can be achieved in real-world settings has been questioned. Moreover, there has been concern that PrEP will lead to increases in condomless sex with attendant risk of other sexually transmitted infections.
Overall, the news concerning PrEP dissemination is good, but there are sobering lessons. Of the 557 enrolled in the Demo Study, 78% were retained over the 48 weeks of follow-up. African Americans and participants from the Miami site were less likely to be retained, as were those with lower socioeconomic status and the uninsured. In an attempt to mimic clinical settings, missing participants were contacted only a maximum of three times in response to a missed visit, and incentives for visit attendance were nominal, although the drug was free.
Realizing the benefits of PrEP requires an optimal cascade of events that is remarkably similar to the Gardner Cascade of engagement in care for those infected with HIV. The so-called PrEP cascade requires identification of at-risk individuals, promotion of interest and knowledge of PrEP, linkage to PrEP-knowledgeable clinics, and PrEP initiation, persistence, and adherence. The benefits of PrEP will fully be realized only when we can identify ways of successfully moving persons at a high risk of HIV infection through this cascade.
Dr. Raphael J. Landovitz is the codirector of the Combination Prevention Core at the Center for HIV Identification, Prevention, and Treatment Services, and is currently at the UCLA Medical Center in Los Angeles. Dr. Landovitz disclosed having previously served as a consultant to Gilead Sciences, which supplied the study drug for the Demo Study.
Data show that PrEP is effective in preventing HIV infections in men who have sex with men (MSM), as well as in heterosexually active men and women. In intention-to-treat analyses, these studies showed reductions of infections between 44% and 75%, although compliance with daily therapy did not appear to be high. When investigators restricted the analysis to persons with detectable drug levels, effectiveness rates were greater than 90%. An open label extension study in follow-up to the iPrEX (Iniciativa Profilaxis Pre-Exposición) trial found100% protection for those who had sustained adherence at the level of four or more doses per week.
Whether adherence to daily or near-daily dosing can be achieved in real-world settings has been questioned. Moreover, there has been concern that PrEP will lead to increases in condomless sex with attendant risk of other sexually transmitted infections.
Overall, the news concerning PrEP dissemination is good, but there are sobering lessons. Of the 557 enrolled in the Demo Study, 78% were retained over the 48 weeks of follow-up. African Americans and participants from the Miami site were less likely to be retained, as were those with lower socioeconomic status and the uninsured. In an attempt to mimic clinical settings, missing participants were contacted only a maximum of three times in response to a missed visit, and incentives for visit attendance were nominal, although the drug was free.
Realizing the benefits of PrEP requires an optimal cascade of events that is remarkably similar to the Gardner Cascade of engagement in care for those infected with HIV. The so-called PrEP cascade requires identification of at-risk individuals, promotion of interest and knowledge of PrEP, linkage to PrEP-knowledgeable clinics, and PrEP initiation, persistence, and adherence. The benefits of PrEP will fully be realized only when we can identify ways of successfully moving persons at a high risk of HIV infection through this cascade.
Dr. Raphael J. Landovitz is the codirector of the Combination Prevention Core at the Center for HIV Identification, Prevention, and Treatment Services, and is currently at the UCLA Medical Center in Los Angeles. Dr. Landovitz disclosed having previously served as a consultant to Gilead Sciences, which supplied the study drug for the Demo Study.
Data show that PrEP is effective in preventing HIV infections in men who have sex with men (MSM), as well as in heterosexually active men and women. In intention-to-treat analyses, these studies showed reductions of infections between 44% and 75%, although compliance with daily therapy did not appear to be high. When investigators restricted the analysis to persons with detectable drug levels, effectiveness rates were greater than 90%. An open label extension study in follow-up to the iPrEX (Iniciativa Profilaxis Pre-Exposición) trial found100% protection for those who had sustained adherence at the level of four or more doses per week.
Whether adherence to daily or near-daily dosing can be achieved in real-world settings has been questioned. Moreover, there has been concern that PrEP will lead to increases in condomless sex with attendant risk of other sexually transmitted infections.
Overall, the news concerning PrEP dissemination is good, but there are sobering lessons. Of the 557 enrolled in the Demo Study, 78% were retained over the 48 weeks of follow-up. African Americans and participants from the Miami site were less likely to be retained, as were those with lower socioeconomic status and the uninsured. In an attempt to mimic clinical settings, missing participants were contacted only a maximum of three times in response to a missed visit, and incentives for visit attendance were nominal, although the drug was free.
Realizing the benefits of PrEP requires an optimal cascade of events that is remarkably similar to the Gardner Cascade of engagement in care for those infected with HIV. The so-called PrEP cascade requires identification of at-risk individuals, promotion of interest and knowledge of PrEP, linkage to PrEP-knowledgeable clinics, and PrEP initiation, persistence, and adherence. The benefits of PrEP will fully be realized only when we can identify ways of successfully moving persons at a high risk of HIV infection through this cascade.
Dr. Raphael J. Landovitz is the codirector of the Combination Prevention Core at the Center for HIV Identification, Prevention, and Treatment Services, and is currently at the UCLA Medical Center in Los Angeles. Dr. Landovitz disclosed having previously served as a consultant to Gilead Sciences, which supplied the study drug for the Demo Study.
Use of pre-exposure prophylaxis (PrEP) by homosexual men and transgender women, even those who already have sexually transmitted infections (STIs), can significantly decrease the likelihood of contracting or spreading STIs among their partners, particularly HIV.
This is according to a prospective study, known as the Demonstration or “Demo” study, published by JAMA Internal Medicine, which examined HIV incidence rates among homosexual men and transgender women in San Francisco, Miami, and Washington for 48 weeks, between Oct. 1, 2012 and Jan. 23, 2014, with a final follow-up on Feb.10, 2015. (2015 Nov 16. doi: 10.1001/jamainternmed.2015.4683)
“Men who have sex with men [MSM] account for more than two-thirds of new HIV infections in the United States and are the only risk group in whom infection rates are rising,” says the study, led by Dr. Albert Y. Liu of the San Francisco Department of Public Health, adding that previous work in this field – namely, the 2010 iPrEx (Pre-Exposure Prophylaxis Initiative) trial – found that tenofovir disoproxil fumarate and emtricitabine led to an overall 44% reduction in HIV acquisition among the aforementioned demographic groups.
A total of 557 participants enrolled, of which 437 (78.5%) were also measured through 48 weeks of follow-up. Participants were given access to a PrEP regimen of daily, oral tenofovir disoproxil fumarate and emtricitabine during clinical visits at 4, 12, 24, 36, and 48 weeks. HIV and STI testing and clinical monitoring were also done during these follow-up visits.
Eligible individuals had to be male at birth, at least 18 years old, have a negative rapid HIV antibody test result at enrollment and a negative fourth-generation antibody-antigen test result at screening, creatinine clearance rate of at least 60 mL/min, and a urine dipstick test with negative or trace findings of protein.
Additionally, all participants were asked to report if they had engaged in condomless anal sex with at least two male or transgender female partners; at least two episodes of anal sex with at least one HIV-infected partner; or sex with a male or transgender female partner and having a diagnosis of syphilis, rectal gonorrhea, or chlamydia in the 12 months prior to enrollment. During the study period, PrEP was discontinued for subjects who underwent seroconversion, and for those who received counseling, partner services, and linkage to HIV primary care.
Of the original 557 who enrolled, 294 (52.8%) ultimately had their tenofovir diphosphate levels measured. Between 80.0% and 85.6% had protective levels of at least four doses per week, indicating high protective levels. However, significant disparity was seen in subjects who were African American (56.8%; P = .03) and those living in the Miami area (65.1%; P less than .01); subjects who had at least two condomless anal sex partners (88.6%; P = .01) and those with stable housing (86.8%; P = .02) were more likely to have high protective levels. Furthermore, the mean number of anal sex partners declined from 10.9 at baseline to 9.3 at the 48 weeks’ follow-up, but the rate of participants engaging in condomless receptive anal sex remained at 65.5% at baseline and at follow-up at 48 weeks.
Regarding acquisition of HIV, only two individuals contracted HIV over the 48 weeks of study, leading to an incidence rate 0.43/100 person-years (95% confidence interval, 0.05-1.54). This is significantly lower than the 90/100 person-years incidence rate of STIs measured by participants at baseline. Both individuals who contracted HIV had tenofovir diphosphate levels indicating that they took fewer than two doses of PrEP per week, and therefore had lower protective levels.
Among the 557 enrolled participants, 25 (4.5%) had no follow-up visits, whereas 383 (68.8%) completed all five visits. Total follow-up was 481 person-years, and after researchers adjusted for each individual site, prior PrEP knowledge and reporting of condomless receptive anal sex at baseline were associated with being retained in the study.
“Adherence was higher among those participants with more reported risk behaviors,” Dr. Liu and his coauthors conclude, adding that “These results provide support for expanding PrEP implementation in MSM in similar clinical settings and highlight the urgent need to increase PrEP awareness and engagement and to develop effective adherence support for highly affected African American and transgender populations.”
To that end, a separate study, also published by JAMA Internal Medicine, looked at “real-world PrEP use” by young, homosexual black men in Chicago. According to a JAMA press release accompanying the release of the uConnect study, “Young black men who have sex with men (YBMSM) are the only group in the United States where HIV incidence has increased over the past decade with effective clinic-based HIV preventions that target YBMSM virtually nonexistent.” (JAMA Intern Med. Nov 16. doi: 10.1001/jamainternmed.2015.6536)
A total of 622 YBMSM – mean age of 23 years, 39% with high school or equivalent level of education, 79% of whom reported annual income of less than $20,000, and only half of whom were both HIV-negative and reported having health coverage – were enrolled, based on eligibility requirements that they self-identified as African American or black, were born male, were between 16 and 29 years of age, and reported oral or anal sex with a male within the 24 months prior to enrollment.
PrEP of daily oral tenofovir disoproxil fumarate and emtricitabine was administered between June 2013 and July 2014. Baseline levels of PrEP awareness – 40.5% of participants knew about PrEP, and 12.1% knew of someone who had used PrEP – remained unchanged significantly at follow-up. Just over 72% of participants were not infected with HIV during the study period; only 3.6% of these individuals had previously used PrEP prior to enrollment.
“Ongoing work should include scientific assessment of strategies to mobilize networks of YBMSM around PrEP as part of a comprehensive health care program. Concomitantly, efforts to mitigate the structural barriers that prevent PrEP uptake among YBMSM may greatly improve the public health effect potential of this promising HIV prevention intervention,” conclude the authors, led by Dr. John A. Schneider of the University of Chicago.
The Demo Study was supported by the NIH’s National Institute for Allergies and Infectious Diseases, National Institute for Mental Health, the Miami Center for AIDS Research, and the Gladstone Institute of Virology & Immunology–University of California, San Francisco. Gilead Sciences supplied the study drugs and support for pharmacokinetic and resistance testing. Dr. Liu disclosed leading other trials in which study drugs were supplied by Gilead Sciences, but no other conflicts of interest. Several other coauthors reported potential conflicts of interest.
The uConnect study was supported by the NIH’s National Institutes of Health. Neither Dr. Schneider nor any coauthors reported any potential conflicts of interest.
Use of pre-exposure prophylaxis (PrEP) by homosexual men and transgender women, even those who already have sexually transmitted infections (STIs), can significantly decrease the likelihood of contracting or spreading STIs among their partners, particularly HIV.
This is according to a prospective study, known as the Demonstration or “Demo” study, published by JAMA Internal Medicine, which examined HIV incidence rates among homosexual men and transgender women in San Francisco, Miami, and Washington for 48 weeks, between Oct. 1, 2012 and Jan. 23, 2014, with a final follow-up on Feb.10, 2015. (2015 Nov 16. doi: 10.1001/jamainternmed.2015.4683)
“Men who have sex with men [MSM] account for more than two-thirds of new HIV infections in the United States and are the only risk group in whom infection rates are rising,” says the study, led by Dr. Albert Y. Liu of the San Francisco Department of Public Health, adding that previous work in this field – namely, the 2010 iPrEx (Pre-Exposure Prophylaxis Initiative) trial – found that tenofovir disoproxil fumarate and emtricitabine led to an overall 44% reduction in HIV acquisition among the aforementioned demographic groups.
A total of 557 participants enrolled, of which 437 (78.5%) were also measured through 48 weeks of follow-up. Participants were given access to a PrEP regimen of daily, oral tenofovir disoproxil fumarate and emtricitabine during clinical visits at 4, 12, 24, 36, and 48 weeks. HIV and STI testing and clinical monitoring were also done during these follow-up visits.
Eligible individuals had to be male at birth, at least 18 years old, have a negative rapid HIV antibody test result at enrollment and a negative fourth-generation antibody-antigen test result at screening, creatinine clearance rate of at least 60 mL/min, and a urine dipstick test with negative or trace findings of protein.
Additionally, all participants were asked to report if they had engaged in condomless anal sex with at least two male or transgender female partners; at least two episodes of anal sex with at least one HIV-infected partner; or sex with a male or transgender female partner and having a diagnosis of syphilis, rectal gonorrhea, or chlamydia in the 12 months prior to enrollment. During the study period, PrEP was discontinued for subjects who underwent seroconversion, and for those who received counseling, partner services, and linkage to HIV primary care.
Of the original 557 who enrolled, 294 (52.8%) ultimately had their tenofovir diphosphate levels measured. Between 80.0% and 85.6% had protective levels of at least four doses per week, indicating high protective levels. However, significant disparity was seen in subjects who were African American (56.8%; P = .03) and those living in the Miami area (65.1%; P less than .01); subjects who had at least two condomless anal sex partners (88.6%; P = .01) and those with stable housing (86.8%; P = .02) were more likely to have high protective levels. Furthermore, the mean number of anal sex partners declined from 10.9 at baseline to 9.3 at the 48 weeks’ follow-up, but the rate of participants engaging in condomless receptive anal sex remained at 65.5% at baseline and at follow-up at 48 weeks.
Regarding acquisition of HIV, only two individuals contracted HIV over the 48 weeks of study, leading to an incidence rate 0.43/100 person-years (95% confidence interval, 0.05-1.54). This is significantly lower than the 90/100 person-years incidence rate of STIs measured by participants at baseline. Both individuals who contracted HIV had tenofovir diphosphate levels indicating that they took fewer than two doses of PrEP per week, and therefore had lower protective levels.
Among the 557 enrolled participants, 25 (4.5%) had no follow-up visits, whereas 383 (68.8%) completed all five visits. Total follow-up was 481 person-years, and after researchers adjusted for each individual site, prior PrEP knowledge and reporting of condomless receptive anal sex at baseline were associated with being retained in the study.
“Adherence was higher among those participants with more reported risk behaviors,” Dr. Liu and his coauthors conclude, adding that “These results provide support for expanding PrEP implementation in MSM in similar clinical settings and highlight the urgent need to increase PrEP awareness and engagement and to develop effective adherence support for highly affected African American and transgender populations.”
To that end, a separate study, also published by JAMA Internal Medicine, looked at “real-world PrEP use” by young, homosexual black men in Chicago. According to a JAMA press release accompanying the release of the uConnect study, “Young black men who have sex with men (YBMSM) are the only group in the United States where HIV incidence has increased over the past decade with effective clinic-based HIV preventions that target YBMSM virtually nonexistent.” (JAMA Intern Med. Nov 16. doi: 10.1001/jamainternmed.2015.6536)
A total of 622 YBMSM – mean age of 23 years, 39% with high school or equivalent level of education, 79% of whom reported annual income of less than $20,000, and only half of whom were both HIV-negative and reported having health coverage – were enrolled, based on eligibility requirements that they self-identified as African American or black, were born male, were between 16 and 29 years of age, and reported oral or anal sex with a male within the 24 months prior to enrollment.
PrEP of daily oral tenofovir disoproxil fumarate and emtricitabine was administered between June 2013 and July 2014. Baseline levels of PrEP awareness – 40.5% of participants knew about PrEP, and 12.1% knew of someone who had used PrEP – remained unchanged significantly at follow-up. Just over 72% of participants were not infected with HIV during the study period; only 3.6% of these individuals had previously used PrEP prior to enrollment.
“Ongoing work should include scientific assessment of strategies to mobilize networks of YBMSM around PrEP as part of a comprehensive health care program. Concomitantly, efforts to mitigate the structural barriers that prevent PrEP uptake among YBMSM may greatly improve the public health effect potential of this promising HIV prevention intervention,” conclude the authors, led by Dr. John A. Schneider of the University of Chicago.
The Demo Study was supported by the NIH’s National Institute for Allergies and Infectious Diseases, National Institute for Mental Health, the Miami Center for AIDS Research, and the Gladstone Institute of Virology & Immunology–University of California, San Francisco. Gilead Sciences supplied the study drugs and support for pharmacokinetic and resistance testing. Dr. Liu disclosed leading other trials in which study drugs were supplied by Gilead Sciences, but no other conflicts of interest. Several other coauthors reported potential conflicts of interest.
The uConnect study was supported by the NIH’s National Institutes of Health. Neither Dr. Schneider nor any coauthors reported any potential conflicts of interest.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Pre-exposure prophylaxis (PrEP) – consisting of daily, oral tenofovir disoproxil fumarate and emtricitabine – was associated with a very low rate of HIV acquisition among homosexual males and transgender women with high rates of STIs.
Major finding: Despite high overall incidence of STIs among participants at baseline (90/100 person-years), only two individuals contracted HIV over the 48 weeks of study (incidence rate 0.43/100 person-years [95% CI, 0.05-1.54]), and both had tenofovir diphosphate levels indicating fewer than two doses per week, or lower protective levels.
Data source: Demonstration project analyzing 557 subjects in three U.S. centers between October 2012 and February 2015.
Disclosures: Study was supported by the NIH’s National Institute for Allergies and Infectious Diseases, National Institute for Mental Health, the Miami Center for AIDS Research, and the Gladstone Institute of Virology & Immunology–University of California, San Francisco; Gilead Sciences supplied the study drugs and support for pharmacokinetic and resistance testing. Several coauthors reported individual disclosures.
Study backs broader use of aspirin to prevent preeclampsia
Prescribing low-dose aspirin to all women at high risk for preeclampsia and women with two or more moderate risk factors is the most cost-beneficial approach to lowering the risk of preeclampsia, according to a new study.
The study, which modeled four approaches to low-dose aspirin prophylaxis in pregnant women, shows that the approach recommended by the U.S. Preventive Services Task Force is superior to the one currently recommended by the American College of Obstetricians and Gynecologists when it comes to lowering the risk of preeclampsia and reducing costs (Obstet Gynecol 2015. doi: 10.1097/AOG.0000000000001115).
Dr. Erika F. Werner and her colleagues at Brown University, Providence, R.I., used a hypothetical cohort of four million U.S. women to analyze the effectiveness of four distinct distribution models for low-dose aspirin prophylaxis: no prophylaxis; following the ACOG recommendations; following the USPSTF recommendations; and universal prophylaxis.
Prior randomized studies have established that low-dose aspirin prophylaxis lowers the risk of preeclampsia and preterm birth, the authors wrote. “The remaining question over low-dose aspirin use in pregnancy is not a scientific one, but rather a question of health policy: Who should be treated and what are the expected risks, benefits, and costs of one policy, compared with another?”
ACOG recommends that low-dose aspirin be given to pregnant women with a history of preeclampsia necessitating delivery before 34 weeks of gestation and to women with preeclampsia in more than one prior pregnancy. The USPSTF, on the other hand, takes a broader approach, recommending that women with a history of preeclampsia and those with multiple gestation, chronic hypertension, diabetes mellitus, renal disease, or autoimmune disease should receive low-dose aspirin. Women with two or more moderate risk factors such as nulliparity, obesity, African American race, age 35 years or older, a family history of preeclampsia, or a personal history of pregnancy complications should also receive aspirin, according to the USPSTF.
Under the decision model created by the researchers, women were assumed to be 77% compliant with adhering to their aspirin regimen of 81 mg daily.
Without any aspirin prophylaxis, researchers estimated that the rate of preeclampsia in this population would be 4.18%, meaning 167,200 women would develop preeclampsia. If ACOG’s approach were followed, the rate would dip to 4.17% (166,720 women). But following the USPSTF’s recommendations would result in a 3.83% rate of preeclampsia (153,160), while universal administration of low-dose aspirin prophylaxis would result in a rate of 3.81% (152,240).
The more widespread use of aspirin would also reduce preterm births and maternal deaths, but increase significant maternal gastrointestinal bleeding events, placental abruption, and aspirin-exacerbated respiratory disease, according to the study.
In the baseline analysis, the USPSTF approach was the most cost beneficial, with a direct annual medical cost savings of more than $364 million when compared with the ACOG approach.
“Our analysis suggests that the U.S. Preventive Services Task Force approach is the most cost beneficial, achieving 94% of the possible preeclampsia rate reduction that can be obtained with aspirin while exposing only one-fourth of pregnant women to the theoretical risks of aspirin,” the researchers wrote.
When compared with the USPSTF approach, universal administration would require more than 3 million women to take aspirin to prevent 920 cases of preeclampsia, an incremental number needed to treat of 3,325. Even after taking this into account, universal coverage would still be “highly cost-effective” and would maximize reductions in preterm birth and preeclampsia, according to the researchers.
“From the standpoint of parsimony, and minimization of potential aspirin risks, the U.S. Preventive Services Task Force approach is a better approach than universal administration,” the researchers wrote. “However, universal administration, with its ease of implementation and potential to maximize the health benefits of aspirin, may in fact be the more rational and clinically pragmatic approach.”
The researchers reported having no financial disclosures.
Prescribing low-dose aspirin to all women at high risk for preeclampsia and women with two or more moderate risk factors is the most cost-beneficial approach to lowering the risk of preeclampsia, according to a new study.
The study, which modeled four approaches to low-dose aspirin prophylaxis in pregnant women, shows that the approach recommended by the U.S. Preventive Services Task Force is superior to the one currently recommended by the American College of Obstetricians and Gynecologists when it comes to lowering the risk of preeclampsia and reducing costs (Obstet Gynecol 2015. doi: 10.1097/AOG.0000000000001115).
Dr. Erika F. Werner and her colleagues at Brown University, Providence, R.I., used a hypothetical cohort of four million U.S. women to analyze the effectiveness of four distinct distribution models for low-dose aspirin prophylaxis: no prophylaxis; following the ACOG recommendations; following the USPSTF recommendations; and universal prophylaxis.
Prior randomized studies have established that low-dose aspirin prophylaxis lowers the risk of preeclampsia and preterm birth, the authors wrote. “The remaining question over low-dose aspirin use in pregnancy is not a scientific one, but rather a question of health policy: Who should be treated and what are the expected risks, benefits, and costs of one policy, compared with another?”
ACOG recommends that low-dose aspirin be given to pregnant women with a history of preeclampsia necessitating delivery before 34 weeks of gestation and to women with preeclampsia in more than one prior pregnancy. The USPSTF, on the other hand, takes a broader approach, recommending that women with a history of preeclampsia and those with multiple gestation, chronic hypertension, diabetes mellitus, renal disease, or autoimmune disease should receive low-dose aspirin. Women with two or more moderate risk factors such as nulliparity, obesity, African American race, age 35 years or older, a family history of preeclampsia, or a personal history of pregnancy complications should also receive aspirin, according to the USPSTF.
Under the decision model created by the researchers, women were assumed to be 77% compliant with adhering to their aspirin regimen of 81 mg daily.
Without any aspirin prophylaxis, researchers estimated that the rate of preeclampsia in this population would be 4.18%, meaning 167,200 women would develop preeclampsia. If ACOG’s approach were followed, the rate would dip to 4.17% (166,720 women). But following the USPSTF’s recommendations would result in a 3.83% rate of preeclampsia (153,160), while universal administration of low-dose aspirin prophylaxis would result in a rate of 3.81% (152,240).
The more widespread use of aspirin would also reduce preterm births and maternal deaths, but increase significant maternal gastrointestinal bleeding events, placental abruption, and aspirin-exacerbated respiratory disease, according to the study.
In the baseline analysis, the USPSTF approach was the most cost beneficial, with a direct annual medical cost savings of more than $364 million when compared with the ACOG approach.
“Our analysis suggests that the U.S. Preventive Services Task Force approach is the most cost beneficial, achieving 94% of the possible preeclampsia rate reduction that can be obtained with aspirin while exposing only one-fourth of pregnant women to the theoretical risks of aspirin,” the researchers wrote.
When compared with the USPSTF approach, universal administration would require more than 3 million women to take aspirin to prevent 920 cases of preeclampsia, an incremental number needed to treat of 3,325. Even after taking this into account, universal coverage would still be “highly cost-effective” and would maximize reductions in preterm birth and preeclampsia, according to the researchers.
“From the standpoint of parsimony, and minimization of potential aspirin risks, the U.S. Preventive Services Task Force approach is a better approach than universal administration,” the researchers wrote. “However, universal administration, with its ease of implementation and potential to maximize the health benefits of aspirin, may in fact be the more rational and clinically pragmatic approach.”
The researchers reported having no financial disclosures.
Prescribing low-dose aspirin to all women at high risk for preeclampsia and women with two or more moderate risk factors is the most cost-beneficial approach to lowering the risk of preeclampsia, according to a new study.
The study, which modeled four approaches to low-dose aspirin prophylaxis in pregnant women, shows that the approach recommended by the U.S. Preventive Services Task Force is superior to the one currently recommended by the American College of Obstetricians and Gynecologists when it comes to lowering the risk of preeclampsia and reducing costs (Obstet Gynecol 2015. doi: 10.1097/AOG.0000000000001115).
Dr. Erika F. Werner and her colleagues at Brown University, Providence, R.I., used a hypothetical cohort of four million U.S. women to analyze the effectiveness of four distinct distribution models for low-dose aspirin prophylaxis: no prophylaxis; following the ACOG recommendations; following the USPSTF recommendations; and universal prophylaxis.
Prior randomized studies have established that low-dose aspirin prophylaxis lowers the risk of preeclampsia and preterm birth, the authors wrote. “The remaining question over low-dose aspirin use in pregnancy is not a scientific one, but rather a question of health policy: Who should be treated and what are the expected risks, benefits, and costs of one policy, compared with another?”
ACOG recommends that low-dose aspirin be given to pregnant women with a history of preeclampsia necessitating delivery before 34 weeks of gestation and to women with preeclampsia in more than one prior pregnancy. The USPSTF, on the other hand, takes a broader approach, recommending that women with a history of preeclampsia and those with multiple gestation, chronic hypertension, diabetes mellitus, renal disease, or autoimmune disease should receive low-dose aspirin. Women with two or more moderate risk factors such as nulliparity, obesity, African American race, age 35 years or older, a family history of preeclampsia, or a personal history of pregnancy complications should also receive aspirin, according to the USPSTF.
Under the decision model created by the researchers, women were assumed to be 77% compliant with adhering to their aspirin regimen of 81 mg daily.
Without any aspirin prophylaxis, researchers estimated that the rate of preeclampsia in this population would be 4.18%, meaning 167,200 women would develop preeclampsia. If ACOG’s approach were followed, the rate would dip to 4.17% (166,720 women). But following the USPSTF’s recommendations would result in a 3.83% rate of preeclampsia (153,160), while universal administration of low-dose aspirin prophylaxis would result in a rate of 3.81% (152,240).
The more widespread use of aspirin would also reduce preterm births and maternal deaths, but increase significant maternal gastrointestinal bleeding events, placental abruption, and aspirin-exacerbated respiratory disease, according to the study.
In the baseline analysis, the USPSTF approach was the most cost beneficial, with a direct annual medical cost savings of more than $364 million when compared with the ACOG approach.
“Our analysis suggests that the U.S. Preventive Services Task Force approach is the most cost beneficial, achieving 94% of the possible preeclampsia rate reduction that can be obtained with aspirin while exposing only one-fourth of pregnant women to the theoretical risks of aspirin,” the researchers wrote.
When compared with the USPSTF approach, universal administration would require more than 3 million women to take aspirin to prevent 920 cases of preeclampsia, an incremental number needed to treat of 3,325. Even after taking this into account, universal coverage would still be “highly cost-effective” and would maximize reductions in preterm birth and preeclampsia, according to the researchers.
“From the standpoint of parsimony, and minimization of potential aspirin risks, the U.S. Preventive Services Task Force approach is a better approach than universal administration,” the researchers wrote. “However, universal administration, with its ease of implementation and potential to maximize the health benefits of aspirin, may in fact be the more rational and clinically pragmatic approach.”
The researchers reported having no financial disclosures.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: Following the U.S. Preventive Services Task Force’s recommendations for the distribution of low-dose aspirin prophylaxis is the most cost-beneficial solution to significantly reduce morbidity and mortality associated with preeclampsia.
Major finding: The USPSTF approach would result in a preeclampsia rate of 3.83%, compared with a rate of 4.17% if the ACOG recommendations were followed.
Data source: Prospective cohort study of four million women and four decision models of distributing low-dose aspirin to prevent preeclampsia.
Disclosures: The researchers reported having no financial disclosures.
AGA updates guidelines for management of acute diverticulitis
The American Gastroenterological Association (AGA) has announced new guidelines for the management of acute diverticulitis, the first practice guidelines for the disease since 1999, and they appear in the December issue of Gastroenterology.
“The management of acute diverticulitis has undergone meaningful change over the past decade, including a more judicious use of antibiotics and surgery, as well as preliminary and ongoing investigations into medical therapies to decrease symptoms and reduce recurrences,” the AGA noted. “The majority of the evidence currently, however, is of poor quality, and most of our recommendations are therefore conditional.”
The guidelines strongly recommend that patients not use mesalamine after acute uncomplicated diverticulitis, citing “moderate” evidence to this effect and saying that currently available evidence regarding the anti-inflammatory agent often used for ulcerative colitis “does not suggest efficacy in reducing recurrence risk, pain resolution, or need for surgery in this specific population.” All other recommendations, however, are conditional and offer either “low-” or “very low-quality” evidence to support them.
These additional recommendations include the following:
• Antibiotics should be used selectively, rather than routinely, in patients with acute uncomplicated diverticulitis.
• Colonoscopy should be performed after resolution of acute uncomplicated diverticulitis in appropriate candidates to exclude the misdiagnosis of a colonic neoplasm, if a high-quality exam of the colon has not been recently performed.
• Patients with a history of diverticulitis should consume a fiber-rich diet or consider fiber supplementation.
• Patients with diverticular disease should consider vigorous physical activity.
The AGA recommendations also advise against certain practices, all with conditional application and either “low-” or “very low-quality” supportive evidence. These are as follows:
• Elective colonic resection should not be done in patients with an initial episode of acute, uncomplicated diverticulitis; the decision to perform elective prophylactic colonic resection in this setting should be individualized.
• Patients with a history of diverticulitis should not be advised to avoid consumption of seeds, nuts, and popcorn.
• Patients with a history of diverticulitis should not be advised to avoid the use of aspirin.
• Patients with a history of diverticulitis should not be advised to avoid the use of nonselective nonsteroidal anti-inflammatory drugs.
• Do not advise the use of mesalamine after acute uncomplicated diverticulitis.
• Do not advise the use of rifaximin after acute uncomplicated diverticulitis.
• Do not advise the use of probiotics after acute uncomplicated diverticulitis.
“Acute diverticulitis is the third most common inpatient gastrointestinal diagnosis in the United States, costing over $2 billion annually, and is a common outpatient and emergency department diagnosis as well,” stated the AGA recommendations, which were developed by the AGA’s Clinical Guidelines Committee and approved by the AGA Institute Governing Board.
The statement notes that the condition “occurs in approximately 4% of patients with diverticulosis, roughly 15% of whom will have complicated disease, defined as an abscess, perforation, fistula or colon obstruction, and 15%-30% will experience recurrence.”
The new guidelines do not address other forms of diverticular disease, including symptomatic uncomplicated diverticular disease, diverticular bleeding, and segmental colitis associated with diverticulosis. It does not address the prevention of incident diverticulitis or the management of complicated disease.
Areas of further research, advises the AGA, should be in identifying patients who will benefit the most from antibiotics, identifying those in whom antibiotics can be withheld safely, identifying risk factors for recurrent diverticulitis, examining the risks of colonoscopy following acute diverticulitis, and taking a closer looks at anti-inflammatory drugs, antibiotics, probiotics, and dietary interventions as viable therapies.
The American Gastroenterological Association (AGA) has announced new guidelines for the management of acute diverticulitis, the first practice guidelines for the disease since 1999, and they appear in the December issue of Gastroenterology.
“The management of acute diverticulitis has undergone meaningful change over the past decade, including a more judicious use of antibiotics and surgery, as well as preliminary and ongoing investigations into medical therapies to decrease symptoms and reduce recurrences,” the AGA noted. “The majority of the evidence currently, however, is of poor quality, and most of our recommendations are therefore conditional.”
The guidelines strongly recommend that patients not use mesalamine after acute uncomplicated diverticulitis, citing “moderate” evidence to this effect and saying that currently available evidence regarding the anti-inflammatory agent often used for ulcerative colitis “does not suggest efficacy in reducing recurrence risk, pain resolution, or need for surgery in this specific population.” All other recommendations, however, are conditional and offer either “low-” or “very low-quality” evidence to support them.
These additional recommendations include the following:
• Antibiotics should be used selectively, rather than routinely, in patients with acute uncomplicated diverticulitis.
• Colonoscopy should be performed after resolution of acute uncomplicated diverticulitis in appropriate candidates to exclude the misdiagnosis of a colonic neoplasm, if a high-quality exam of the colon has not been recently performed.
• Patients with a history of diverticulitis should consume a fiber-rich diet or consider fiber supplementation.
• Patients with diverticular disease should consider vigorous physical activity.
The AGA recommendations also advise against certain practices, all with conditional application and either “low-” or “very low-quality” supportive evidence. These are as follows:
• Elective colonic resection should not be done in patients with an initial episode of acute, uncomplicated diverticulitis; the decision to perform elective prophylactic colonic resection in this setting should be individualized.
• Patients with a history of diverticulitis should not be advised to avoid consumption of seeds, nuts, and popcorn.
• Patients with a history of diverticulitis should not be advised to avoid the use of aspirin.
• Patients with a history of diverticulitis should not be advised to avoid the use of nonselective nonsteroidal anti-inflammatory drugs.
• Do not advise the use of mesalamine after acute uncomplicated diverticulitis.
• Do not advise the use of rifaximin after acute uncomplicated diverticulitis.
• Do not advise the use of probiotics after acute uncomplicated diverticulitis.
“Acute diverticulitis is the third most common inpatient gastrointestinal diagnosis in the United States, costing over $2 billion annually, and is a common outpatient and emergency department diagnosis as well,” stated the AGA recommendations, which were developed by the AGA’s Clinical Guidelines Committee and approved by the AGA Institute Governing Board.
The statement notes that the condition “occurs in approximately 4% of patients with diverticulosis, roughly 15% of whom will have complicated disease, defined as an abscess, perforation, fistula or colon obstruction, and 15%-30% will experience recurrence.”
The new guidelines do not address other forms of diverticular disease, including symptomatic uncomplicated diverticular disease, diverticular bleeding, and segmental colitis associated with diverticulosis. It does not address the prevention of incident diverticulitis or the management of complicated disease.
Areas of further research, advises the AGA, should be in identifying patients who will benefit the most from antibiotics, identifying those in whom antibiotics can be withheld safely, identifying risk factors for recurrent diverticulitis, examining the risks of colonoscopy following acute diverticulitis, and taking a closer looks at anti-inflammatory drugs, antibiotics, probiotics, and dietary interventions as viable therapies.
The American Gastroenterological Association (AGA) has announced new guidelines for the management of acute diverticulitis, the first practice guidelines for the disease since 1999, and they appear in the December issue of Gastroenterology.
“The management of acute diverticulitis has undergone meaningful change over the past decade, including a more judicious use of antibiotics and surgery, as well as preliminary and ongoing investigations into medical therapies to decrease symptoms and reduce recurrences,” the AGA noted. “The majority of the evidence currently, however, is of poor quality, and most of our recommendations are therefore conditional.”
The guidelines strongly recommend that patients not use mesalamine after acute uncomplicated diverticulitis, citing “moderate” evidence to this effect and saying that currently available evidence regarding the anti-inflammatory agent often used for ulcerative colitis “does not suggest efficacy in reducing recurrence risk, pain resolution, or need for surgery in this specific population.” All other recommendations, however, are conditional and offer either “low-” or “very low-quality” evidence to support them.
These additional recommendations include the following:
• Antibiotics should be used selectively, rather than routinely, in patients with acute uncomplicated diverticulitis.
• Colonoscopy should be performed after resolution of acute uncomplicated diverticulitis in appropriate candidates to exclude the misdiagnosis of a colonic neoplasm, if a high-quality exam of the colon has not been recently performed.
• Patients with a history of diverticulitis should consume a fiber-rich diet or consider fiber supplementation.
• Patients with diverticular disease should consider vigorous physical activity.
The AGA recommendations also advise against certain practices, all with conditional application and either “low-” or “very low-quality” supportive evidence. These are as follows:
• Elective colonic resection should not be done in patients with an initial episode of acute, uncomplicated diverticulitis; the decision to perform elective prophylactic colonic resection in this setting should be individualized.
• Patients with a history of diverticulitis should not be advised to avoid consumption of seeds, nuts, and popcorn.
• Patients with a history of diverticulitis should not be advised to avoid the use of aspirin.
• Patients with a history of diverticulitis should not be advised to avoid the use of nonselective nonsteroidal anti-inflammatory drugs.
• Do not advise the use of mesalamine after acute uncomplicated diverticulitis.
• Do not advise the use of rifaximin after acute uncomplicated diverticulitis.
• Do not advise the use of probiotics after acute uncomplicated diverticulitis.
“Acute diverticulitis is the third most common inpatient gastrointestinal diagnosis in the United States, costing over $2 billion annually, and is a common outpatient and emergency department diagnosis as well,” stated the AGA recommendations, which were developed by the AGA’s Clinical Guidelines Committee and approved by the AGA Institute Governing Board.
The statement notes that the condition “occurs in approximately 4% of patients with diverticulosis, roughly 15% of whom will have complicated disease, defined as an abscess, perforation, fistula or colon obstruction, and 15%-30% will experience recurrence.”
The new guidelines do not address other forms of diverticular disease, including symptomatic uncomplicated diverticular disease, diverticular bleeding, and segmental colitis associated with diverticulosis. It does not address the prevention of incident diverticulitis or the management of complicated disease.
Areas of further research, advises the AGA, should be in identifying patients who will benefit the most from antibiotics, identifying those in whom antibiotics can be withheld safely, identifying risk factors for recurrent diverticulitis, examining the risks of colonoscopy following acute diverticulitis, and taking a closer looks at anti-inflammatory drugs, antibiotics, probiotics, and dietary interventions as viable therapies.
Legionellosis Cases Continue to Increase Nationwide
Data from the first 3 years of the Center for Disease Control and Prevention’s Active Bacterial Core surveillance (ABCs) program on legionellosis confirm that incidences of disease caused by the bacteria are increasing across the United States, according to the latest Morbidity and Mortality Weekly Report (MMWR. 2015 Oct 30;64[42]:1190-1193).
The ABCs program, which launched in 2011, identified 1,426 cases of legionellosis over the 3-year time span, and incidence rates of 1.3 (2011), 1.1 (2012), and 1.4 (2013) cases per 100,000 individuals in the general population. This corroborates similar findings made by the National Notifiable Diseases Surveillance System (NNDSS) between 2000 and 2011, which reported an increase in the crude incidence rate of legionellosis nationwide from 0.39 to 1.36 cases per 100,000 individuals.
The two main clinical syndromes associated with legionellosis are Legionnaires’ disease, which is a severe form of pneumonia; and Pontiac fever, a milder illness without pneumonia.
“During 2000-2011, passive surveillance for legionellosis in the United States demonstrated a 249% increase in crude incidence, although little was known about the clinical course and method of diagnosis,” says the report, led by Dr. Kathleen I. Dooling of the CDC’s National Center for Immunization and Respiratory Diseases.
The report also states that “ABCs data during 2011-2013 showed that approximately 44% of patients with legionellosis required intensive care, and 9% died.” Furthermore, incidence increased with age among the ABCs program cohort. Those younger than 50 years of age had a 0.4 incidence rate per 100,000 individuals; patients between 50 and 64 years old had a 2.5 per 100,000 incidence rate; those who were 65-79 years old had a 3.6 per 100,000 incidence rate; and individuals 80 years and older had an incidence rate of 4.7 per 100,000 individuals.
“Among cases identified during 2011-2013, 79% occurred in persons aged >50 years, 65% were in males, and 72% of patients were white,” says the report, adding that “1,300 (91%) received a diagnosis of legionellosis on the basis of urine antigen testing, which only detects Lp1 species.”
The ABCs program defined a confirmed case of legionellosis as “the isolation of Legionella from respiratory culture, detection of Legionella antigen in urine, or seroconversion (a more than fourfold rise in antibody titer between acute and convalescent sera) to Lp1.” Unlike NNDSS, ABCs recorded clinical and race data for each patient found to have legionellosis, finding that incidence rates among blacks were higher than among whites per 100,000 individuals: 1.0 vs. 1.5, respectively.
The report concludes by calling for further research into the disparities in legionellosis cases based on race, age, and geography, as well as the need for “more sensitive laboratory tests for legionellosis because proper diagnosis is needed for treatment and public health action.”
This study was supported by the CDC.
Data from the first 3 years of the Center for Disease Control and Prevention’s Active Bacterial Core surveillance (ABCs) program on legionellosis confirm that incidences of disease caused by the bacteria are increasing across the United States, according to the latest Morbidity and Mortality Weekly Report (MMWR. 2015 Oct 30;64[42]:1190-1193).
The ABCs program, which launched in 2011, identified 1,426 cases of legionellosis over the 3-year time span, and incidence rates of 1.3 (2011), 1.1 (2012), and 1.4 (2013) cases per 100,000 individuals in the general population. This corroborates similar findings made by the National Notifiable Diseases Surveillance System (NNDSS) between 2000 and 2011, which reported an increase in the crude incidence rate of legionellosis nationwide from 0.39 to 1.36 cases per 100,000 individuals.
The two main clinical syndromes associated with legionellosis are Legionnaires’ disease, which is a severe form of pneumonia; and Pontiac fever, a milder illness without pneumonia.
“During 2000-2011, passive surveillance for legionellosis in the United States demonstrated a 249% increase in crude incidence, although little was known about the clinical course and method of diagnosis,” says the report, led by Dr. Kathleen I. Dooling of the CDC’s National Center for Immunization and Respiratory Diseases.
The report also states that “ABCs data during 2011-2013 showed that approximately 44% of patients with legionellosis required intensive care, and 9% died.” Furthermore, incidence increased with age among the ABCs program cohort. Those younger than 50 years of age had a 0.4 incidence rate per 100,000 individuals; patients between 50 and 64 years old had a 2.5 per 100,000 incidence rate; those who were 65-79 years old had a 3.6 per 100,000 incidence rate; and individuals 80 years and older had an incidence rate of 4.7 per 100,000 individuals.
“Among cases identified during 2011-2013, 79% occurred in persons aged >50 years, 65% were in males, and 72% of patients were white,” says the report, adding that “1,300 (91%) received a diagnosis of legionellosis on the basis of urine antigen testing, which only detects Lp1 species.”
The ABCs program defined a confirmed case of legionellosis as “the isolation of Legionella from respiratory culture, detection of Legionella antigen in urine, or seroconversion (a more than fourfold rise in antibody titer between acute and convalescent sera) to Lp1.” Unlike NNDSS, ABCs recorded clinical and race data for each patient found to have legionellosis, finding that incidence rates among blacks were higher than among whites per 100,000 individuals: 1.0 vs. 1.5, respectively.
The report concludes by calling for further research into the disparities in legionellosis cases based on race, age, and geography, as well as the need for “more sensitive laboratory tests for legionellosis because proper diagnosis is needed for treatment and public health action.”
This study was supported by the CDC.
Data from the first 3 years of the Center for Disease Control and Prevention’s Active Bacterial Core surveillance (ABCs) program on legionellosis confirm that incidences of disease caused by the bacteria are increasing across the United States, according to the latest Morbidity and Mortality Weekly Report (MMWR. 2015 Oct 30;64[42]:1190-1193).
The ABCs program, which launched in 2011, identified 1,426 cases of legionellosis over the 3-year time span, and incidence rates of 1.3 (2011), 1.1 (2012), and 1.4 (2013) cases per 100,000 individuals in the general population. This corroborates similar findings made by the National Notifiable Diseases Surveillance System (NNDSS) between 2000 and 2011, which reported an increase in the crude incidence rate of legionellosis nationwide from 0.39 to 1.36 cases per 100,000 individuals.
The two main clinical syndromes associated with legionellosis are Legionnaires’ disease, which is a severe form of pneumonia; and Pontiac fever, a milder illness without pneumonia.
“During 2000-2011, passive surveillance for legionellosis in the United States demonstrated a 249% increase in crude incidence, although little was known about the clinical course and method of diagnosis,” says the report, led by Dr. Kathleen I. Dooling of the CDC’s National Center for Immunization and Respiratory Diseases.
The report also states that “ABCs data during 2011-2013 showed that approximately 44% of patients with legionellosis required intensive care, and 9% died.” Furthermore, incidence increased with age among the ABCs program cohort. Those younger than 50 years of age had a 0.4 incidence rate per 100,000 individuals; patients between 50 and 64 years old had a 2.5 per 100,000 incidence rate; those who were 65-79 years old had a 3.6 per 100,000 incidence rate; and individuals 80 years and older had an incidence rate of 4.7 per 100,000 individuals.
“Among cases identified during 2011-2013, 79% occurred in persons aged >50 years, 65% were in males, and 72% of patients were white,” says the report, adding that “1,300 (91%) received a diagnosis of legionellosis on the basis of urine antigen testing, which only detects Lp1 species.”
The ABCs program defined a confirmed case of legionellosis as “the isolation of Legionella from respiratory culture, detection of Legionella antigen in urine, or seroconversion (a more than fourfold rise in antibody titer between acute and convalescent sera) to Lp1.” Unlike NNDSS, ABCs recorded clinical and race data for each patient found to have legionellosis, finding that incidence rates among blacks were higher than among whites per 100,000 individuals: 1.0 vs. 1.5, respectively.
The report concludes by calling for further research into the disparities in legionellosis cases based on race, age, and geography, as well as the need for “more sensitive laboratory tests for legionellosis because proper diagnosis is needed for treatment and public health action.”
This study was supported by the CDC.
FROM MMWR