User login
Antibiotics overprescribed during asthma-related hospitalizations
Antibiotics are overprescribed in asthma-related hospitalizations, even though guidelines recommend against prescribing antibiotics during exacerbations of asthma in the absence of concurrent infection, reported Peter K. Lindenauer, MD, MSc, of Baystate Medical Center in Springfield, Mass., and his colleagues.
They examined the hospitalization records of 51,951 individuals admitted to 577 hospitals in the United States between 2013 and 2014 with a principal diagnosis of either asthma or acute respiratory failure combined with asthma as a secondary diagnosis. Each patient type and the timing of antibiotic therapy was noted.
A total of 30,226 of the 51,951 patients (58.2%) were prescribed antibiotics at some point during their hospitalization, while 21,248 (40.9%) were prescribed antibiotics on the first day of hospitalization, without “documentation of an indication for antibiotic therapy.”
Macrolides were most commonly prescribed, given to 9,633 (18.5%) of patients, followed by quinolones (8,632, 16.1%), third-generation cephalosporins (4,420, 8.5%), and tetracyclines (1,858, 3.6%). After adjustment for risk variables, chronic obstructive asthma hospitalizations were found to be those most highly associated with receiving antibiotics (odds ratio 1.6, 95% confidence interval 1.5-1.7).
“Possible explanations for this high rate of potentially inappropriate treatment include the challenge of differentiating bacterial from nonbacterial infections, distinguishing asthma from chronic obstructive pulmonary disease in the acute care setting, and gaps in knowledge about the benefits of antibiotic therapy,” the authors posited, adding that these findings “suggest a significant opportunity to improve patient safety, reduce the spread of resistance, and lower spending through greater adherence to guideline recommendations.”
The National Heart, Lung, and Blood Institute and Veterans Affairs Health Services Research and Development funded the study. Dr. Lindenauer and his coauthors did not report any relevant financial disclosures.
Antibiotics are overprescribed in asthma-related hospitalizations, even though guidelines recommend against prescribing antibiotics during exacerbations of asthma in the absence of concurrent infection, reported Peter K. Lindenauer, MD, MSc, of Baystate Medical Center in Springfield, Mass., and his colleagues.
They examined the hospitalization records of 51,951 individuals admitted to 577 hospitals in the United States between 2013 and 2014 with a principal diagnosis of either asthma or acute respiratory failure combined with asthma as a secondary diagnosis. Each patient type and the timing of antibiotic therapy was noted.
A total of 30,226 of the 51,951 patients (58.2%) were prescribed antibiotics at some point during their hospitalization, while 21,248 (40.9%) were prescribed antibiotics on the first day of hospitalization, without “documentation of an indication for antibiotic therapy.”
Macrolides were most commonly prescribed, given to 9,633 (18.5%) of patients, followed by quinolones (8,632, 16.1%), third-generation cephalosporins (4,420, 8.5%), and tetracyclines (1,858, 3.6%). After adjustment for risk variables, chronic obstructive asthma hospitalizations were found to be those most highly associated with receiving antibiotics (odds ratio 1.6, 95% confidence interval 1.5-1.7).
“Possible explanations for this high rate of potentially inappropriate treatment include the challenge of differentiating bacterial from nonbacterial infections, distinguishing asthma from chronic obstructive pulmonary disease in the acute care setting, and gaps in knowledge about the benefits of antibiotic therapy,” the authors posited, adding that these findings “suggest a significant opportunity to improve patient safety, reduce the spread of resistance, and lower spending through greater adherence to guideline recommendations.”
The National Heart, Lung, and Blood Institute and Veterans Affairs Health Services Research and Development funded the study. Dr. Lindenauer and his coauthors did not report any relevant financial disclosures.
Antibiotics are overprescribed in asthma-related hospitalizations, even though guidelines recommend against prescribing antibiotics during exacerbations of asthma in the absence of concurrent infection, reported Peter K. Lindenauer, MD, MSc, of Baystate Medical Center in Springfield, Mass., and his colleagues.
They examined the hospitalization records of 51,951 individuals admitted to 577 hospitals in the United States between 2013 and 2014 with a principal diagnosis of either asthma or acute respiratory failure combined with asthma as a secondary diagnosis. Each patient type and the timing of antibiotic therapy was noted.
A total of 30,226 of the 51,951 patients (58.2%) were prescribed antibiotics at some point during their hospitalization, while 21,248 (40.9%) were prescribed antibiotics on the first day of hospitalization, without “documentation of an indication for antibiotic therapy.”
Macrolides were most commonly prescribed, given to 9,633 (18.5%) of patients, followed by quinolones (8,632, 16.1%), third-generation cephalosporins (4,420, 8.5%), and tetracyclines (1,858, 3.6%). After adjustment for risk variables, chronic obstructive asthma hospitalizations were found to be those most highly associated with receiving antibiotics (odds ratio 1.6, 95% confidence interval 1.5-1.7).
“Possible explanations for this high rate of potentially inappropriate treatment include the challenge of differentiating bacterial from nonbacterial infections, distinguishing asthma from chronic obstructive pulmonary disease in the acute care setting, and gaps in knowledge about the benefits of antibiotic therapy,” the authors posited, adding that these findings “suggest a significant opportunity to improve patient safety, reduce the spread of resistance, and lower spending through greater adherence to guideline recommendations.”
The National Heart, Lung, and Blood Institute and Veterans Affairs Health Services Research and Development funded the study. Dr. Lindenauer and his coauthors did not report any relevant financial disclosures.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Antibiotics are overprescribed in asthma-related hospitalizations.
Major finding: Among patients hospitalized for asthma, 58.2% had received antibiotics without any documentation or indication for such therapy.
Data source: Retrospective study of 51,951 patients in 577 U.S. hospitals from 2013 to 2014.
Disclosures: The National Heart, Lung, and Blood Institute and Veterans Affairs Health Services Research and Development funded the study. The researchers reported no relevant financial disclosures.
Remission of lupus often short-lasting and variable
The time it takes for patients with systemic lupus erythematosus to achieve remission greatly depends on how remission is defined, and such episodes are usually short-lasting, according to an analysis of more than 2,000 patients in the Hopkins Lupus Cohort.
“Our results concerning durability of remission show the relapsing-remitting nature of SLE [systemic lupus erythematosus]. The median duration of remission was only about 3 months for all [four] definitions [used in the study]. This was the time to the next quarterly cohort visit. Even though achieving remission was frequent, durable remission was rare,” wrote the authors, led by Theresa R. Wilhelm, MD, of Johns Hopkins University in Baltimore.
Dr. Wilhelm and her coauthors chose to examine remission in SLE based on four DORIS (Definitions Of Remission In SLE) working group clinical definitions: clinical remission, complete remission, clinical ROT (Remission on Treatment), and complete ROT. To define them, a clinical SLE Disease Activity Index (cSLEDAI) score of 0 and a Physician Global Assessment of less than 0.5 were applicable to all definitions. Zero prednisone was applicable to clinical and complete remission, while clinical ROT and complete ROT allowed for 5 mg or less daily. Immunosuppressive drugs were not allowed for a patient to be deemed in either clinical or complete remission, but were allowed for both ROT definitions. Serologically negative results were deemed permissible for both complete remission and ROT, but not for clinical remission or clinical ROT (Ann Rheum Dis. 2016 Aug 24. doi: 10.1136/annrheumdis-2016-209489).
For a total of 2,307 SLE patients who were enrolled into the Hopkins Lupus Cohort during 1987-2014, the median time for clinical remission to be achieved was 8.7 years, while complete remission took 11.0 years, clinical ROT took 1.8 years, and complete ROT took 3.1 years. These Kaplan-Meier estimates of the distribution of time to remission after entry into the cohort did not include patients who had a gap in their follow-up or dropped out before satisfying the definition of remission.
However, across all four definitions, the median length of remission was only 3 months, as sustained remission proved elusive. Those with high disease activity and greater treatment had longer median times to achieve remission than did those with low disease activity and less treatment.
“Not surprisingly, we found that the level of baseline treatment and baseline disease activity were strongly associated with the time to remission for all definitions,” Dr. Wilhelm and her coauthors noted.
“Testing definitions of remission is of great relevance for clinical practice, as much as for clinical trials,” the authors concluded. “Our future goal is to find out which definitions are most successful in predicting the best possible outcome for our patients.”
The Hopkins Lupus Cohort receives funding from the National Institutes of Health. Dr. Wilhelm and her coauthors did not report any relevant financial disclosures.
The time it takes for patients with systemic lupus erythematosus to achieve remission greatly depends on how remission is defined, and such episodes are usually short-lasting, according to an analysis of more than 2,000 patients in the Hopkins Lupus Cohort.
“Our results concerning durability of remission show the relapsing-remitting nature of SLE [systemic lupus erythematosus]. The median duration of remission was only about 3 months for all [four] definitions [used in the study]. This was the time to the next quarterly cohort visit. Even though achieving remission was frequent, durable remission was rare,” wrote the authors, led by Theresa R. Wilhelm, MD, of Johns Hopkins University in Baltimore.
Dr. Wilhelm and her coauthors chose to examine remission in SLE based on four DORIS (Definitions Of Remission In SLE) working group clinical definitions: clinical remission, complete remission, clinical ROT (Remission on Treatment), and complete ROT. To define them, a clinical SLE Disease Activity Index (cSLEDAI) score of 0 and a Physician Global Assessment of less than 0.5 were applicable to all definitions. Zero prednisone was applicable to clinical and complete remission, while clinical ROT and complete ROT allowed for 5 mg or less daily. Immunosuppressive drugs were not allowed for a patient to be deemed in either clinical or complete remission, but were allowed for both ROT definitions. Serologically negative results were deemed permissible for both complete remission and ROT, but not for clinical remission or clinical ROT (Ann Rheum Dis. 2016 Aug 24. doi: 10.1136/annrheumdis-2016-209489).
For a total of 2,307 SLE patients who were enrolled into the Hopkins Lupus Cohort during 1987-2014, the median time for clinical remission to be achieved was 8.7 years, while complete remission took 11.0 years, clinical ROT took 1.8 years, and complete ROT took 3.1 years. These Kaplan-Meier estimates of the distribution of time to remission after entry into the cohort did not include patients who had a gap in their follow-up or dropped out before satisfying the definition of remission.
However, across all four definitions, the median length of remission was only 3 months, as sustained remission proved elusive. Those with high disease activity and greater treatment had longer median times to achieve remission than did those with low disease activity and less treatment.
“Not surprisingly, we found that the level of baseline treatment and baseline disease activity were strongly associated with the time to remission for all definitions,” Dr. Wilhelm and her coauthors noted.
“Testing definitions of remission is of great relevance for clinical practice, as much as for clinical trials,” the authors concluded. “Our future goal is to find out which definitions are most successful in predicting the best possible outcome for our patients.”
The Hopkins Lupus Cohort receives funding from the National Institutes of Health. Dr. Wilhelm and her coauthors did not report any relevant financial disclosures.
The time it takes for patients with systemic lupus erythematosus to achieve remission greatly depends on how remission is defined, and such episodes are usually short-lasting, according to an analysis of more than 2,000 patients in the Hopkins Lupus Cohort.
“Our results concerning durability of remission show the relapsing-remitting nature of SLE [systemic lupus erythematosus]. The median duration of remission was only about 3 months for all [four] definitions [used in the study]. This was the time to the next quarterly cohort visit. Even though achieving remission was frequent, durable remission was rare,” wrote the authors, led by Theresa R. Wilhelm, MD, of Johns Hopkins University in Baltimore.
Dr. Wilhelm and her coauthors chose to examine remission in SLE based on four DORIS (Definitions Of Remission In SLE) working group clinical definitions: clinical remission, complete remission, clinical ROT (Remission on Treatment), and complete ROT. To define them, a clinical SLE Disease Activity Index (cSLEDAI) score of 0 and a Physician Global Assessment of less than 0.5 were applicable to all definitions. Zero prednisone was applicable to clinical and complete remission, while clinical ROT and complete ROT allowed for 5 mg or less daily. Immunosuppressive drugs were not allowed for a patient to be deemed in either clinical or complete remission, but were allowed for both ROT definitions. Serologically negative results were deemed permissible for both complete remission and ROT, but not for clinical remission or clinical ROT (Ann Rheum Dis. 2016 Aug 24. doi: 10.1136/annrheumdis-2016-209489).
For a total of 2,307 SLE patients who were enrolled into the Hopkins Lupus Cohort during 1987-2014, the median time for clinical remission to be achieved was 8.7 years, while complete remission took 11.0 years, clinical ROT took 1.8 years, and complete ROT took 3.1 years. These Kaplan-Meier estimates of the distribution of time to remission after entry into the cohort did not include patients who had a gap in their follow-up or dropped out before satisfying the definition of remission.
However, across all four definitions, the median length of remission was only 3 months, as sustained remission proved elusive. Those with high disease activity and greater treatment had longer median times to achieve remission than did those with low disease activity and less treatment.
“Not surprisingly, we found that the level of baseline treatment and baseline disease activity were strongly associated with the time to remission for all definitions,” Dr. Wilhelm and her coauthors noted.
“Testing definitions of remission is of great relevance for clinical practice, as much as for clinical trials,” the authors concluded. “Our future goal is to find out which definitions are most successful in predicting the best possible outcome for our patients.”
The Hopkins Lupus Cohort receives funding from the National Institutes of Health. Dr. Wilhelm and her coauthors did not report any relevant financial disclosures.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point: Sustained remission in systemic lupus erythematosus patients varies considerably according to different definitions and is less likely than previously believed.
Major finding: The median times for remission were 8.7 years (clinical remission), 11.0 years (complete remission), 1.8 years (clinical remission on treatment), and 3.1 years (complete remission on treatment), while median duration of remission was 3 months across all four definitions.
Data source: Prospective clinical cohort study of 2,307 patients enrolled during 1987-2014.
Disclosures: The Hopkins Lupus Cohort receives funding from the National Institutes of Health. The authors reported no relevant financial disclosures.
CDC reports asymptomatic Zika transmission; FDA begins universal blood testing
Officials at the Centers for Disease Control and Prevention have confirmed a case of Zika virus infection in a nonpregnant Maryland woman who likely contracted the virus through sexual intercourse with her asymptomatic male partner.
“To date, only one other case has been reported in which a man without symptoms might have sexually transmitted Zika virus to his female partner,” Richard B. Brooks, MD, and his colleagues wrote Aug. 26 in the Morbidity and Mortality Weekly Report (doi:10.15585/mmwr.mm6534e2). “However, in that reported case, both the man and the woman had traveled to a country with ongoing Zika virus transmission where they were likely exposed to mosquitoes.”
In the current case, the couple had condomless vaginal sex 10 days and 14 days after his return from the Dominican Republic, along with oral sex on day 14. Two days after the last encounter, the woman began exhibiting symptoms of Zika virus infection, namely, a maculopapular rash and a fever. She sought medical care 3 days later (19 days after her partner returned to the United States). She had no other sexual partners during this time. Meanwhile, the male sex partner reported no symptoms of a Zika virus infection, other than simply being tired from his recent travel.
“The findings in this report indicate that it might be appropriate to consider persons who have condomless sex with partners returning from areas with ongoing Zika virus transmission as exposed to Zika virus, regardless of whether the returning traveler reports symptoms of Zika virus infection,” the researchers wrote.
Transmission of Zika virus through blood transfusions is also a growing concern, particularly if an asymptomatic individual donated blood.
On Aug. 26, the Food and Drug Administration announced recommendations to test all donated blood and blood components across the United States and its territories for the Zika virus, to mitigate the chances of transmitting the virus through transfusions. In February, the FDA first issued guidance recommending that only areas with active Zika virus transmission screen donated blood.
“As new scientific and epidemiological information regarding Zika virus has become available, it’s clear that additional precautionary measures are necessary,” Luciana Borio, MD, FDA’s acting chief scientist, said in a statement. “We are issuing revised guidance for immediate implementation in order to help maintain the safety of the U.S. blood supply.”
In a conference call with reporters, Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said that while there have not yet been any confirmed cases of such transmission, donors and health care workers must be vigilant. “Given the frequency of travel of individuals within the United States, there is the risk that people without symptoms who are infected with Zika virus could potentially donate blood and thereby transmit Zika virus,” he said.
The CDC also published new numbers on Guillain-Barré syndrome (GBS), which has been on the rise in countries affected by Zika virus.
Individuals who began exhibiting any neurologic symptoms between Jan. 1, 2016, and July 31, 2016, and were suspected of possible GBS total 56. Of those 56 patients, 34 (61%) were found to have evidence of either Zika or another related flavivirus. Ten (18%) of those 56 were confirmed to have Zika virus, and 1 patient who received treatment for GBS died of septic shock. Thirty (88%) of the 34 found to have evidence of flavivirus also reported having an acute illness of some kind before the onset of neurologic symptoms. The figures come from the GBS Passive Surveillance System (MMWR. 2016 Aug 26. doi:10.15585/mmwr.mm6534e1).
“Persons with signs or symptoms consistent with GBS should promptly seek medical attention,” the CDC urged. “Health care providers who evaluate patients with neurologic illnesses should consider GBS and report suspected cases to public health authorities. Residents of and travelers to Puerto Rico are advised to follow existing recommendations for prevention of Zika virus infection.”
Officials at the Centers for Disease Control and Prevention have confirmed a case of Zika virus infection in a nonpregnant Maryland woman who likely contracted the virus through sexual intercourse with her asymptomatic male partner.
“To date, only one other case has been reported in which a man without symptoms might have sexually transmitted Zika virus to his female partner,” Richard B. Brooks, MD, and his colleagues wrote Aug. 26 in the Morbidity and Mortality Weekly Report (doi:10.15585/mmwr.mm6534e2). “However, in that reported case, both the man and the woman had traveled to a country with ongoing Zika virus transmission where they were likely exposed to mosquitoes.”
In the current case, the couple had condomless vaginal sex 10 days and 14 days after his return from the Dominican Republic, along with oral sex on day 14. Two days after the last encounter, the woman began exhibiting symptoms of Zika virus infection, namely, a maculopapular rash and a fever. She sought medical care 3 days later (19 days after her partner returned to the United States). She had no other sexual partners during this time. Meanwhile, the male sex partner reported no symptoms of a Zika virus infection, other than simply being tired from his recent travel.
“The findings in this report indicate that it might be appropriate to consider persons who have condomless sex with partners returning from areas with ongoing Zika virus transmission as exposed to Zika virus, regardless of whether the returning traveler reports symptoms of Zika virus infection,” the researchers wrote.
Transmission of Zika virus through blood transfusions is also a growing concern, particularly if an asymptomatic individual donated blood.
On Aug. 26, the Food and Drug Administration announced recommendations to test all donated blood and blood components across the United States and its territories for the Zika virus, to mitigate the chances of transmitting the virus through transfusions. In February, the FDA first issued guidance recommending that only areas with active Zika virus transmission screen donated blood.
“As new scientific and epidemiological information regarding Zika virus has become available, it’s clear that additional precautionary measures are necessary,” Luciana Borio, MD, FDA’s acting chief scientist, said in a statement. “We are issuing revised guidance for immediate implementation in order to help maintain the safety of the U.S. blood supply.”
In a conference call with reporters, Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said that while there have not yet been any confirmed cases of such transmission, donors and health care workers must be vigilant. “Given the frequency of travel of individuals within the United States, there is the risk that people without symptoms who are infected with Zika virus could potentially donate blood and thereby transmit Zika virus,” he said.
The CDC also published new numbers on Guillain-Barré syndrome (GBS), which has been on the rise in countries affected by Zika virus.
Individuals who began exhibiting any neurologic symptoms between Jan. 1, 2016, and July 31, 2016, and were suspected of possible GBS total 56. Of those 56 patients, 34 (61%) were found to have evidence of either Zika or another related flavivirus. Ten (18%) of those 56 were confirmed to have Zika virus, and 1 patient who received treatment for GBS died of septic shock. Thirty (88%) of the 34 found to have evidence of flavivirus also reported having an acute illness of some kind before the onset of neurologic symptoms. The figures come from the GBS Passive Surveillance System (MMWR. 2016 Aug 26. doi:10.15585/mmwr.mm6534e1).
“Persons with signs or symptoms consistent with GBS should promptly seek medical attention,” the CDC urged. “Health care providers who evaluate patients with neurologic illnesses should consider GBS and report suspected cases to public health authorities. Residents of and travelers to Puerto Rico are advised to follow existing recommendations for prevention of Zika virus infection.”
Officials at the Centers for Disease Control and Prevention have confirmed a case of Zika virus infection in a nonpregnant Maryland woman who likely contracted the virus through sexual intercourse with her asymptomatic male partner.
“To date, only one other case has been reported in which a man without symptoms might have sexually transmitted Zika virus to his female partner,” Richard B. Brooks, MD, and his colleagues wrote Aug. 26 in the Morbidity and Mortality Weekly Report (doi:10.15585/mmwr.mm6534e2). “However, in that reported case, both the man and the woman had traveled to a country with ongoing Zika virus transmission where they were likely exposed to mosquitoes.”
In the current case, the couple had condomless vaginal sex 10 days and 14 days after his return from the Dominican Republic, along with oral sex on day 14. Two days after the last encounter, the woman began exhibiting symptoms of Zika virus infection, namely, a maculopapular rash and a fever. She sought medical care 3 days later (19 days after her partner returned to the United States). She had no other sexual partners during this time. Meanwhile, the male sex partner reported no symptoms of a Zika virus infection, other than simply being tired from his recent travel.
“The findings in this report indicate that it might be appropriate to consider persons who have condomless sex with partners returning from areas with ongoing Zika virus transmission as exposed to Zika virus, regardless of whether the returning traveler reports symptoms of Zika virus infection,” the researchers wrote.
Transmission of Zika virus through blood transfusions is also a growing concern, particularly if an asymptomatic individual donated blood.
On Aug. 26, the Food and Drug Administration announced recommendations to test all donated blood and blood components across the United States and its territories for the Zika virus, to mitigate the chances of transmitting the virus through transfusions. In February, the FDA first issued guidance recommending that only areas with active Zika virus transmission screen donated blood.
“As new scientific and epidemiological information regarding Zika virus has become available, it’s clear that additional precautionary measures are necessary,” Luciana Borio, MD, FDA’s acting chief scientist, said in a statement. “We are issuing revised guidance for immediate implementation in order to help maintain the safety of the U.S. blood supply.”
In a conference call with reporters, Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said that while there have not yet been any confirmed cases of such transmission, donors and health care workers must be vigilant. “Given the frequency of travel of individuals within the United States, there is the risk that people without symptoms who are infected with Zika virus could potentially donate blood and thereby transmit Zika virus,” he said.
The CDC also published new numbers on Guillain-Barré syndrome (GBS), which has been on the rise in countries affected by Zika virus.
Individuals who began exhibiting any neurologic symptoms between Jan. 1, 2016, and July 31, 2016, and were suspected of possible GBS total 56. Of those 56 patients, 34 (61%) were found to have evidence of either Zika or another related flavivirus. Ten (18%) of those 56 were confirmed to have Zika virus, and 1 patient who received treatment for GBS died of septic shock. Thirty (88%) of the 34 found to have evidence of flavivirus also reported having an acute illness of some kind before the onset of neurologic symptoms. The figures come from the GBS Passive Surveillance System (MMWR. 2016 Aug 26. doi:10.15585/mmwr.mm6534e1).
“Persons with signs or symptoms consistent with GBS should promptly seek medical attention,” the CDC urged. “Health care providers who evaluate patients with neurologic illnesses should consider GBS and report suspected cases to public health authorities. Residents of and travelers to Puerto Rico are advised to follow existing recommendations for prevention of Zika virus infection.”
Zika virus persists in serum for more than 2 months in newborns
Zika virus infections can persist for more than 2 months after birth in congenitally infected infants, indicating that viral shedding of Zika can take several weeks, according to an Aug. 24, 2016 research letter to the New England Journal of Medicine.
The case study described in the letter involves a male child born after 40 weeks’ gestation in Brazil to a mother who presented with Zika-like symptoms during the 26th week of pregnancy. The child was born with microcephaly – head circumference of 32.5 centimeters – but no signs of neurological abnormalities during the initial postnatal physical examination. Additionally, cerebrospinal fluid, ophthalmologic, and otoacoustic analyses were all deemed normal.
However, low brain parenchyma in the frontal and parietal lobes, along with calcification in the subcortical area and compensatory dilatation of the infratentorial supraventricular system was found via MRI. Furthermore, testing of serum, saliva, and urine at 54 days of age via quantitative real-time polymerase chain reaction assay came back positive for Zika virus. Serum tested at 67 days postbirth also was positive for Zika virus. Testing at day 216, however, showed no signs of Zika virus in serum.
“When the infant was examined on day 54, he had no obvious illness or evidence of any immunocompromising condition,” wrote lead author Danielle B.L. Oliveira, PhD, of the Universidade de São Paulo and her colleagues. “However, by 6 months of age, he showed neuropsychomotor developmental delay, with global hypertonia and spastic hemiplegia, with the right dominant side more severely affected.”
The report comes on the heels of a Florida Department of Health (DOH) announcement that the Zika virus has been found in a pregnant woman residing in Pinellas County, the first such case in that area, making it the third region of Florida in which Zika virus infection has been discovered. As of now, it is the only case of Zika virus in that area.
“DOH has begun door-to-door outreach in Pinellas County and mosquito abatement and reduction activities are also taking place,” the DOH announced in a statement. “DOH still believes ongoing transmission is only taking place within the small identified areas in Wynwood and Miami Beach in Miami-Dade County.”
Zika virus infections can persist for more than 2 months after birth in congenitally infected infants, indicating that viral shedding of Zika can take several weeks, according to an Aug. 24, 2016 research letter to the New England Journal of Medicine.
The case study described in the letter involves a male child born after 40 weeks’ gestation in Brazil to a mother who presented with Zika-like symptoms during the 26th week of pregnancy. The child was born with microcephaly – head circumference of 32.5 centimeters – but no signs of neurological abnormalities during the initial postnatal physical examination. Additionally, cerebrospinal fluid, ophthalmologic, and otoacoustic analyses were all deemed normal.
However, low brain parenchyma in the frontal and parietal lobes, along with calcification in the subcortical area and compensatory dilatation of the infratentorial supraventricular system was found via MRI. Furthermore, testing of serum, saliva, and urine at 54 days of age via quantitative real-time polymerase chain reaction assay came back positive for Zika virus. Serum tested at 67 days postbirth also was positive for Zika virus. Testing at day 216, however, showed no signs of Zika virus in serum.
“When the infant was examined on day 54, he had no obvious illness or evidence of any immunocompromising condition,” wrote lead author Danielle B.L. Oliveira, PhD, of the Universidade de São Paulo and her colleagues. “However, by 6 months of age, he showed neuropsychomotor developmental delay, with global hypertonia and spastic hemiplegia, with the right dominant side more severely affected.”
The report comes on the heels of a Florida Department of Health (DOH) announcement that the Zika virus has been found in a pregnant woman residing in Pinellas County, the first such case in that area, making it the third region of Florida in which Zika virus infection has been discovered. As of now, it is the only case of Zika virus in that area.
“DOH has begun door-to-door outreach in Pinellas County and mosquito abatement and reduction activities are also taking place,” the DOH announced in a statement. “DOH still believes ongoing transmission is only taking place within the small identified areas in Wynwood and Miami Beach in Miami-Dade County.”
Zika virus infections can persist for more than 2 months after birth in congenitally infected infants, indicating that viral shedding of Zika can take several weeks, according to an Aug. 24, 2016 research letter to the New England Journal of Medicine.
The case study described in the letter involves a male child born after 40 weeks’ gestation in Brazil to a mother who presented with Zika-like symptoms during the 26th week of pregnancy. The child was born with microcephaly – head circumference of 32.5 centimeters – but no signs of neurological abnormalities during the initial postnatal physical examination. Additionally, cerebrospinal fluid, ophthalmologic, and otoacoustic analyses were all deemed normal.
However, low brain parenchyma in the frontal and parietal lobes, along with calcification in the subcortical area and compensatory dilatation of the infratentorial supraventricular system was found via MRI. Furthermore, testing of serum, saliva, and urine at 54 days of age via quantitative real-time polymerase chain reaction assay came back positive for Zika virus. Serum tested at 67 days postbirth also was positive for Zika virus. Testing at day 216, however, showed no signs of Zika virus in serum.
“When the infant was examined on day 54, he had no obvious illness or evidence of any immunocompromising condition,” wrote lead author Danielle B.L. Oliveira, PhD, of the Universidade de São Paulo and her colleagues. “However, by 6 months of age, he showed neuropsychomotor developmental delay, with global hypertonia and spastic hemiplegia, with the right dominant side more severely affected.”
The report comes on the heels of a Florida Department of Health (DOH) announcement that the Zika virus has been found in a pregnant woman residing in Pinellas County, the first such case in that area, making it the third region of Florida in which Zika virus infection has been discovered. As of now, it is the only case of Zika virus in that area.
“DOH has begun door-to-door outreach in Pinellas County and mosquito abatement and reduction activities are also taking place,” the DOH announced in a statement. “DOH still believes ongoing transmission is only taking place within the small identified areas in Wynwood and Miami Beach in Miami-Dade County.”
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
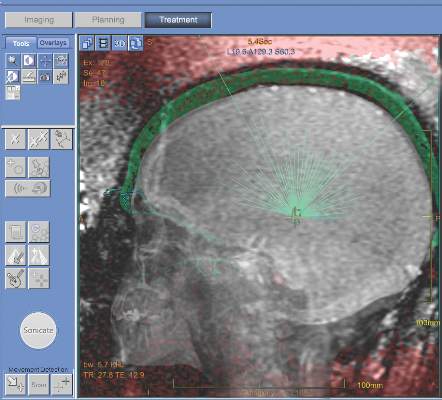
MRI-guided thalamotomy significantly reduces hand tremors
MRI-guided focused ultrasound thalamotomy can significantly mitigate the severity of hand tremors in patients suffering from essential tremor, the most common type of movement disorder, according to a new study published in the New England Journal of Medicine.
“The use of ultrasound energy for the creation of discrete intracranial lesions... has been of interest since the middle of the 20th century,” wrote the investigators, led by W. Jeffrey Elias, MD, of the University of Virginia, Charlottesville. “Prospective pilot trials of focused ultrasound thalamotomy with magnetic resonance imaging (MRI) guidance in patients with essential tremor have shown reductions in hand tremor, improvements in quality of life, and minimal procedural morbidity.”
The trial enrolled a total of 76 patients with a mean age of 71 years and mean disease duration of nearly 17 years; 68% were men and 75% were white. At a 3:1 ratio, they were randomized into one of two cohorts: one underwent thalamotomy and the other received a “sham” procedure. The subjects were unaware which they received for the first 3 months. The Clinical Rating Scale for Tremor (CRST) and the Quality of Life in Essential Tremor Questionnaire (QUEST) was used to determine the severity of tremors at baseline, and at follow-ups conducted at 1, 3, 6, and 12 months post-procedure (N Engl J Med. 2016;375[8]:730-9).
The trial’s primary outcome of between-group difference in the change in tremor score from baseline to 3 months significantly favored thalamotomy (8.5-point improvement, from 18.1 to 9.6) over the sham procedure (0.2-point improvement, from 16.0 to 15.8). The mean between-group difference in the change in score of 8.3 points at 3 months decreased slightly to 7.2 points at 12 months. The tremor score (range, 0-32) was derived from part A of the CRST (three items: resting, postural, and action or intention components of hand tremor), and part B of the CRST (five tasks involving handwriting, drawing, and pouring), in the hand contralateral to the thalamotomy.
Thalamotomy patients also reported 46% better quality of life on QUEST at 3 months, compared with 3% better among sham-procedure patients.
There were adverse events in the thalamotomy cohort. At the 3-month follow-up, 36% of subjects experienced gait disturbance, 38% experienced paresthesias or some kind of numbness. The rates of these adverse events dropped to 9% and 14%, respectively, at the 12-month follow-up.
“Deep-brain stimulation is currently the surgical standard for medication-refractory essential tremor [but] a control group of patients undergoing deep-brain stimulation was not included in this trial; the two technologies were not compared,” the authors noted, indicating that such comparison could potentially be the next step for this research.
This study was supported by InSightec, the Focused Ultrasound Foundation, and the Binational Industrial Research and Development Foundation. Dr. Elias disclosed receiving grant support from InSightec and the Focused Ultrasound Foundation. Other coauthors disclosed receiving similar support.
There are several important concerns about this study. Its 12-month follow-up period is relatively short, so the sustained benefit at 2 years, 3 years, and 5 or more years is unknown. The tremor score of patients who underwent focused ultrasound thalamotomy increased by 23% from 1 month to 12 months, and it’s unclear whether this loss of efficacy is due to disease progression or tolerance. The typical estimates of the rate of disease progression in essential tremor make tolerance less likely. The loss of efficacy is also seen to some extent with deep-brain stimulation. Furthermore, some patients who underwent thalamotomy did not achieve large improvements in tremor. The percentage change was less than 20% in 9 of 56 patients.
It’s also worthwhile to note that focused ultrasound thalamotomy creates a fixed brain lesion, whereas with deep-brain stimulation there is the potential to adjust stimulator settings in order to obtain further therapeutic gains. The procedure also is not suitable for all patients, such as those with particularly thick skulls. The most common side effect involved altered sensation, which remained permanent in 14% of patients.
The procedure will take its place among other surgical procedures for medically refractory essential tremor. A head-to-head comparison with deep-brain stimulation would facilitate the direct comparison of the two approaches.
Elan D. Louis, MD, is the chief of the division of movement disorders and professor of neurology and epidemiology (chronic diseases) at Yale University, New Haven, Conn. His comments were taken from his editorial accompanying the report by Dr. Elias and his colleagues (N Engl J Med. 2016;375[8]:792-3).
There are several important concerns about this study. Its 12-month follow-up period is relatively short, so the sustained benefit at 2 years, 3 years, and 5 or more years is unknown. The tremor score of patients who underwent focused ultrasound thalamotomy increased by 23% from 1 month to 12 months, and it’s unclear whether this loss of efficacy is due to disease progression or tolerance. The typical estimates of the rate of disease progression in essential tremor make tolerance less likely. The loss of efficacy is also seen to some extent with deep-brain stimulation. Furthermore, some patients who underwent thalamotomy did not achieve large improvements in tremor. The percentage change was less than 20% in 9 of 56 patients.
It’s also worthwhile to note that focused ultrasound thalamotomy creates a fixed brain lesion, whereas with deep-brain stimulation there is the potential to adjust stimulator settings in order to obtain further therapeutic gains. The procedure also is not suitable for all patients, such as those with particularly thick skulls. The most common side effect involved altered sensation, which remained permanent in 14% of patients.
The procedure will take its place among other surgical procedures for medically refractory essential tremor. A head-to-head comparison with deep-brain stimulation would facilitate the direct comparison of the two approaches.
Elan D. Louis, MD, is the chief of the division of movement disorders and professor of neurology and epidemiology (chronic diseases) at Yale University, New Haven, Conn. His comments were taken from his editorial accompanying the report by Dr. Elias and his colleagues (N Engl J Med. 2016;375[8]:792-3).
There are several important concerns about this study. Its 12-month follow-up period is relatively short, so the sustained benefit at 2 years, 3 years, and 5 or more years is unknown. The tremor score of patients who underwent focused ultrasound thalamotomy increased by 23% from 1 month to 12 months, and it’s unclear whether this loss of efficacy is due to disease progression or tolerance. The typical estimates of the rate of disease progression in essential tremor make tolerance less likely. The loss of efficacy is also seen to some extent with deep-brain stimulation. Furthermore, some patients who underwent thalamotomy did not achieve large improvements in tremor. The percentage change was less than 20% in 9 of 56 patients.
It’s also worthwhile to note that focused ultrasound thalamotomy creates a fixed brain lesion, whereas with deep-brain stimulation there is the potential to adjust stimulator settings in order to obtain further therapeutic gains. The procedure also is not suitable for all patients, such as those with particularly thick skulls. The most common side effect involved altered sensation, which remained permanent in 14% of patients.
The procedure will take its place among other surgical procedures for medically refractory essential tremor. A head-to-head comparison with deep-brain stimulation would facilitate the direct comparison of the two approaches.
Elan D. Louis, MD, is the chief of the division of movement disorders and professor of neurology and epidemiology (chronic diseases) at Yale University, New Haven, Conn. His comments were taken from his editorial accompanying the report by Dr. Elias and his colleagues (N Engl J Med. 2016;375[8]:792-3).
MRI-guided focused ultrasound thalamotomy can significantly mitigate the severity of hand tremors in patients suffering from essential tremor, the most common type of movement disorder, according to a new study published in the New England Journal of Medicine.
“The use of ultrasound energy for the creation of discrete intracranial lesions... has been of interest since the middle of the 20th century,” wrote the investigators, led by W. Jeffrey Elias, MD, of the University of Virginia, Charlottesville. “Prospective pilot trials of focused ultrasound thalamotomy with magnetic resonance imaging (MRI) guidance in patients with essential tremor have shown reductions in hand tremor, improvements in quality of life, and minimal procedural morbidity.”
The trial enrolled a total of 76 patients with a mean age of 71 years and mean disease duration of nearly 17 years; 68% were men and 75% were white. At a 3:1 ratio, they were randomized into one of two cohorts: one underwent thalamotomy and the other received a “sham” procedure. The subjects were unaware which they received for the first 3 months. The Clinical Rating Scale for Tremor (CRST) and the Quality of Life in Essential Tremor Questionnaire (QUEST) was used to determine the severity of tremors at baseline, and at follow-ups conducted at 1, 3, 6, and 12 months post-procedure (N Engl J Med. 2016;375[8]:730-9).
The trial’s primary outcome of between-group difference in the change in tremor score from baseline to 3 months significantly favored thalamotomy (8.5-point improvement, from 18.1 to 9.6) over the sham procedure (0.2-point improvement, from 16.0 to 15.8). The mean between-group difference in the change in score of 8.3 points at 3 months decreased slightly to 7.2 points at 12 months. The tremor score (range, 0-32) was derived from part A of the CRST (three items: resting, postural, and action or intention components of hand tremor), and part B of the CRST (five tasks involving handwriting, drawing, and pouring), in the hand contralateral to the thalamotomy.
Thalamotomy patients also reported 46% better quality of life on QUEST at 3 months, compared with 3% better among sham-procedure patients.
There were adverse events in the thalamotomy cohort. At the 3-month follow-up, 36% of subjects experienced gait disturbance, 38% experienced paresthesias or some kind of numbness. The rates of these adverse events dropped to 9% and 14%, respectively, at the 12-month follow-up.
“Deep-brain stimulation is currently the surgical standard for medication-refractory essential tremor [but] a control group of patients undergoing deep-brain stimulation was not included in this trial; the two technologies were not compared,” the authors noted, indicating that such comparison could potentially be the next step for this research.
This study was supported by InSightec, the Focused Ultrasound Foundation, and the Binational Industrial Research and Development Foundation. Dr. Elias disclosed receiving grant support from InSightec and the Focused Ultrasound Foundation. Other coauthors disclosed receiving similar support.
MRI-guided focused ultrasound thalamotomy can significantly mitigate the severity of hand tremors in patients suffering from essential tremor, the most common type of movement disorder, according to a new study published in the New England Journal of Medicine.
“The use of ultrasound energy for the creation of discrete intracranial lesions... has been of interest since the middle of the 20th century,” wrote the investigators, led by W. Jeffrey Elias, MD, of the University of Virginia, Charlottesville. “Prospective pilot trials of focused ultrasound thalamotomy with magnetic resonance imaging (MRI) guidance in patients with essential tremor have shown reductions in hand tremor, improvements in quality of life, and minimal procedural morbidity.”
The trial enrolled a total of 76 patients with a mean age of 71 years and mean disease duration of nearly 17 years; 68% were men and 75% were white. At a 3:1 ratio, they were randomized into one of two cohorts: one underwent thalamotomy and the other received a “sham” procedure. The subjects were unaware which they received for the first 3 months. The Clinical Rating Scale for Tremor (CRST) and the Quality of Life in Essential Tremor Questionnaire (QUEST) was used to determine the severity of tremors at baseline, and at follow-ups conducted at 1, 3, 6, and 12 months post-procedure (N Engl J Med. 2016;375[8]:730-9).
The trial’s primary outcome of between-group difference in the change in tremor score from baseline to 3 months significantly favored thalamotomy (8.5-point improvement, from 18.1 to 9.6) over the sham procedure (0.2-point improvement, from 16.0 to 15.8). The mean between-group difference in the change in score of 8.3 points at 3 months decreased slightly to 7.2 points at 12 months. The tremor score (range, 0-32) was derived from part A of the CRST (three items: resting, postural, and action or intention components of hand tremor), and part B of the CRST (five tasks involving handwriting, drawing, and pouring), in the hand contralateral to the thalamotomy.
Thalamotomy patients also reported 46% better quality of life on QUEST at 3 months, compared with 3% better among sham-procedure patients.
There were adverse events in the thalamotomy cohort. At the 3-month follow-up, 36% of subjects experienced gait disturbance, 38% experienced paresthesias or some kind of numbness. The rates of these adverse events dropped to 9% and 14%, respectively, at the 12-month follow-up.
“Deep-brain stimulation is currently the surgical standard for medication-refractory essential tremor [but] a control group of patients undergoing deep-brain stimulation was not included in this trial; the two technologies were not compared,” the authors noted, indicating that such comparison could potentially be the next step for this research.
This study was supported by InSightec, the Focused Ultrasound Foundation, and the Binational Industrial Research and Development Foundation. Dr. Elias disclosed receiving grant support from InSightec and the Focused Ultrasound Foundation. Other coauthors disclosed receiving similar support.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: The severity of hand tremors in patients with essential tremor can be significantly reduced via use of MRI-guided focused ultrasound thalamotomy.
Major finding: Greater improvement was observed in the ultrasound thalamotomy cohort than in the control (sham treatment) cohort: 18.1 to 9.6 hand tremor score vs. 16.0 to 15.8, respectively.
Data source: A double-blind, randomized, sham-controlled cohort study of 76 patients with moderate-to-severe essential tremor.
Disclosures: Study supported by InSightec, the Focused Ultrasound Foundation, and the Binational Industrial Research and Development Foundation. Some coauthors reported potentially relevant disclosures.
Local Zika virus transmission identified in second area of Miami
The Centers for Disease Control and Prevention has confirmed that a new pocket of local Zika virus transmission has emerged in Miami Beach, adding yet another area in southern Florida for travelers to avoid.
“We now recommend [that] pregnant women should avoid travel to the designated area of Miami Beach, in addition to the designated area of Wynwood,” CDC Director Tom Frieden, MD, MPH, said during a conference call.
The announcement of a second Miami neighborhood experiencing ongoing local transmission came within 24 hours of the Miami Beach area being identified as a potential hazard, according to Dr. Frieden. Public health officials notified the public in late July about Zika virus transmission in the Wynwood neighborhood; in addition, there have been at least four other cases of independent mosquito-borne transmission of the Zika virus, but the CDC noted that these are not indicative of the disease spreading or becoming locally transmitted to a significant extent.
For those living in or near the affected areas, Dr. Frieden urged that they “do everything they can to prevent mosquito bites,” including wearing clothing that covers as much of the body as possible and using bug repellent, among other things. Those who traveled to the Miami area on or after July 14 of this year should use protection while having sex with their partners to prevent transmitting the virus that way. Women should wait until at least 8 weeks after onset of Zika virus symptoms before attempting to get pregnant.
“More broadly and not just with respect to Florida, all pregnant women anywhere in the U.S. should be evaluated for possible Zika virus exposure during each prenatal care visit,” said Dr. Frieden. “These evaluations should include an assessment of the symptoms of Zika virus disease such as fever, rash, arthralgia, and conjunctivitis, their travel history, and their potential partners’ exposure to Zika virus.”
Dr. Frieden said that the CDC will continue monitoring the situation on a daily basis and make any further announcements, along with changes to current guidelines and recommendations, as necessary.
The Centers for Disease Control and Prevention has confirmed that a new pocket of local Zika virus transmission has emerged in Miami Beach, adding yet another area in southern Florida for travelers to avoid.
“We now recommend [that] pregnant women should avoid travel to the designated area of Miami Beach, in addition to the designated area of Wynwood,” CDC Director Tom Frieden, MD, MPH, said during a conference call.
The announcement of a second Miami neighborhood experiencing ongoing local transmission came within 24 hours of the Miami Beach area being identified as a potential hazard, according to Dr. Frieden. Public health officials notified the public in late July about Zika virus transmission in the Wynwood neighborhood; in addition, there have been at least four other cases of independent mosquito-borne transmission of the Zika virus, but the CDC noted that these are not indicative of the disease spreading or becoming locally transmitted to a significant extent.
For those living in or near the affected areas, Dr. Frieden urged that they “do everything they can to prevent mosquito bites,” including wearing clothing that covers as much of the body as possible and using bug repellent, among other things. Those who traveled to the Miami area on or after July 14 of this year should use protection while having sex with their partners to prevent transmitting the virus that way. Women should wait until at least 8 weeks after onset of Zika virus symptoms before attempting to get pregnant.
“More broadly and not just with respect to Florida, all pregnant women anywhere in the U.S. should be evaluated for possible Zika virus exposure during each prenatal care visit,” said Dr. Frieden. “These evaluations should include an assessment of the symptoms of Zika virus disease such as fever, rash, arthralgia, and conjunctivitis, their travel history, and their potential partners’ exposure to Zika virus.”
Dr. Frieden said that the CDC will continue monitoring the situation on a daily basis and make any further announcements, along with changes to current guidelines and recommendations, as necessary.
The Centers for Disease Control and Prevention has confirmed that a new pocket of local Zika virus transmission has emerged in Miami Beach, adding yet another area in southern Florida for travelers to avoid.
“We now recommend [that] pregnant women should avoid travel to the designated area of Miami Beach, in addition to the designated area of Wynwood,” CDC Director Tom Frieden, MD, MPH, said during a conference call.
The announcement of a second Miami neighborhood experiencing ongoing local transmission came within 24 hours of the Miami Beach area being identified as a potential hazard, according to Dr. Frieden. Public health officials notified the public in late July about Zika virus transmission in the Wynwood neighborhood; in addition, there have been at least four other cases of independent mosquito-borne transmission of the Zika virus, but the CDC noted that these are not indicative of the disease spreading or becoming locally transmitted to a significant extent.
For those living in or near the affected areas, Dr. Frieden urged that they “do everything they can to prevent mosquito bites,” including wearing clothing that covers as much of the body as possible and using bug repellent, among other things. Those who traveled to the Miami area on or after July 14 of this year should use protection while having sex with their partners to prevent transmitting the virus that way. Women should wait until at least 8 weeks after onset of Zika virus symptoms before attempting to get pregnant.
“More broadly and not just with respect to Florida, all pregnant women anywhere in the U.S. should be evaluated for possible Zika virus exposure during each prenatal care visit,” said Dr. Frieden. “These evaluations should include an assessment of the symptoms of Zika virus disease such as fever, rash, arthralgia, and conjunctivitis, their travel history, and their potential partners’ exposure to Zika virus.”
Dr. Frieden said that the CDC will continue monitoring the situation on a daily basis and make any further announcements, along with changes to current guidelines and recommendations, as necessary.
FASD diagnostic guidelines updated at key time
A newly published set of clinical guidelines for the diagnosis of fetal alcohol spectrum disorder (FASD), the first such update to the guidelines since 2005, will help health care providers better diagnose children exposed to alcohol during gestation.
“These new guidelines will be a valuable resource for clinicians to accurately diagnose infants and children who were affected by alcohol exposure before birth,” George F. Koob, PhD, director of the National Institute on Alcohol Abuse and Alcoholism, said in a statement. “They represent the most data-driven diagnostic criteria for fetal alcohol syndrome and fetal alcohol spectrum disorder produced to date.”
The guidelines call for a multidisciplinary approach to FASD diagnosis, which would require children suspected of FASD to be evaluated by either a pediatrician or a clinical geneticist/dysmorphologist, along with undergoing a neuropsychological and behavioral assessment. Children also should be assessed by speech pathologists, occupational therapists, physical therapists, audiologists, psychiatrists, and ophthalmologists on a case-by-case basis, if needed (Pediatrics. 2016;138[2]:e20154256).
“[FASD], the umbrella term for the range of disabilities that can result from prenatal alcohol exposure, represents the leading cause of preventable developmental disabilities in the world,” according to an NIH statement. “As a result of alcohol exposure in the womb, children can have lower IQ, restricted growth resulting in shorter height/lower weight, small head size, a characteristic pattern of facial deformities, and behavioral issues such as attention deficit, poor impulse control, and the inability to regulate mood/behavior.”
As a first step outlined in the diagnostic algorithm in the guidelines, the mothers should be assessed to determine how much prenatal alcohol was consumed; there is a table with a definition of documented prenatal alcohol exposure as it applies to the four definitions. The guidelines stress that no amount of alcohol consumption during pregnancy can be considered safe; therefore, the amount and frequency of alcohol consumption, along with any possible drug use, is critical to determining the severity of FASD in the child.
The four diagnostic categories into which FASD has been divided have not been changed in the update, although the criteria for each have been updated. These four categories, which were created by the Institute of Medicine in 1996, are: fetal alcohol syndrome (FAS), which applies to the most severely affected children; partial FAS (PFAS), which applies to children who display some, but not all, of the full spectrum of FAS characteristics; alcohol-related neurodevelopmental disorder (ARND), which applies to children who have no physical signs of FAS but do display cognitive or behavioral impairment; and alcohol-related birth defects (ARBD), which applies to children with no FAS symptoms aside from a physical malformation brought on by prenatal alcohol consumption.
“These four diagnostic categories remain the most apt descriptors of the range of disabilities observed within the continuum of FASD,” guidelines coauthor Kenneth R. Warren, MD, said in a statement. “We have refined the guidelines to reflect our collective expertise gained through the evaluation of more than 10,000 children in domestic and international venues.”
There is an extensive chart in the guidelines article documenting the updated criteria for the four diagnostic criteria.
After determining maternal alcohol consumption during pregnancy, characteristic structural features should be evaluated in the child. Typical physical signs of FASD include short palpebral fissures, a smooth philtrum, and a vermilion border of the upper lip that may be thinner than normal, along with midface hypoplasia. There is a new lip/philtrum guide for the white population, incorporating a 45-degree view in the guidelines.
From there, neurodevelopmental assessments and neuropsychological evaluations should be conducted to identify any cognitive impairments, keeping in mind that these will progress as the child ages. Finally, a multidisciplinary case conference should be held to discuss whether or not FASD should be diagnosed or not.
“These updated guidelines reflect consensus among a large and experienced cadre of FASD investigators in the fields of dysmorphology, epidemiology, neurology, psychology, developmental/ behavioral pediatrics, and educational diagnostics,” wrote the authors of the guidelines, led by H. Eugene Hoyme, MD of the University of South Dakota in Sioux Falls. “The improved specificity of these guidelines will aid clinicians in assignment of more accurate diagnoses of alcohol-exposed infants and children, thereby leading to more widespread early intervention and improved prevention efforts.”
The authors reported no relevant financial disclosures.
These updated diagnostic guidelines for fetal alcohol spectrum disorders (FASD) are being published and made available to clinicians at a very important time in the history of research on this disorder.
With National Institutes of Health–National Institute on Alcohol Abuse and Alcoholism support, a multidisciplinary group of investigators under the Collaboration to Establish Fetal Alcohol Spectrum Disorders Prevalence (CoFASP) is now compiling the first regionally based prevalence estimates for the disorders in the United States, which are thought to be on the order of 2%-5% of first grade children in the general population. These estimates exceed that of other common developmental disabilities such as autism spectrum disorders, and highlight the tremendous importance of this public health issue.

|
Dr. Christina D. Chambers |
The updated diagnostic guidelines expand upon the previous criteria published more than 10 years ago by Hoyme et al. Now on the basis of experience with evaluating more than 10,000 children in the United States, the authors’ consensus guidelines add more detailed information about the type and severity of neurobehavioral deficits commonly seen in alcohol-affected children, specify the quantity and frequency of alcohol reported by the mother that can be used to help define prenatal alcohol exposure, and incorporate emerging biomarkers of exposure that do not rely solely on maternal report, among other improvements and clarifications.
One of the major barriers to identification of FASD-affected children is pediatricians’ lack of confidence in their ability to recognize affected children. This set of guidelines should improve the ability of clinicians to better identify those children who may be affected by alcohol and might otherwise be misdiagnosed or not diagnosed at all, and can help standardize the pediatrician’s approach to doing this.
Christina Chambers, PhD, MPH, a professor of pediatrics at University of California, San Diego, and director of clinical research for the department of pediatrics at UCSD and Rady Children’s Hospital, commented in an interview. She is also a coauthor of, and helped to develop, the guidelines. Dr. Chambers said she had no relevant financial disclosures.
These updated diagnostic guidelines for fetal alcohol spectrum disorders (FASD) are being published and made available to clinicians at a very important time in the history of research on this disorder.
With National Institutes of Health–National Institute on Alcohol Abuse and Alcoholism support, a multidisciplinary group of investigators under the Collaboration to Establish Fetal Alcohol Spectrum Disorders Prevalence (CoFASP) is now compiling the first regionally based prevalence estimates for the disorders in the United States, which are thought to be on the order of 2%-5% of first grade children in the general population. These estimates exceed that of other common developmental disabilities such as autism spectrum disorders, and highlight the tremendous importance of this public health issue.

|
Dr. Christina D. Chambers |
The updated diagnostic guidelines expand upon the previous criteria published more than 10 years ago by Hoyme et al. Now on the basis of experience with evaluating more than 10,000 children in the United States, the authors’ consensus guidelines add more detailed information about the type and severity of neurobehavioral deficits commonly seen in alcohol-affected children, specify the quantity and frequency of alcohol reported by the mother that can be used to help define prenatal alcohol exposure, and incorporate emerging biomarkers of exposure that do not rely solely on maternal report, among other improvements and clarifications.
One of the major barriers to identification of FASD-affected children is pediatricians’ lack of confidence in their ability to recognize affected children. This set of guidelines should improve the ability of clinicians to better identify those children who may be affected by alcohol and might otherwise be misdiagnosed or not diagnosed at all, and can help standardize the pediatrician’s approach to doing this.
Christina Chambers, PhD, MPH, a professor of pediatrics at University of California, San Diego, and director of clinical research for the department of pediatrics at UCSD and Rady Children’s Hospital, commented in an interview. She is also a coauthor of, and helped to develop, the guidelines. Dr. Chambers said she had no relevant financial disclosures.
These updated diagnostic guidelines for fetal alcohol spectrum disorders (FASD) are being published and made available to clinicians at a very important time in the history of research on this disorder.
With National Institutes of Health–National Institute on Alcohol Abuse and Alcoholism support, a multidisciplinary group of investigators under the Collaboration to Establish Fetal Alcohol Spectrum Disorders Prevalence (CoFASP) is now compiling the first regionally based prevalence estimates for the disorders in the United States, which are thought to be on the order of 2%-5% of first grade children in the general population. These estimates exceed that of other common developmental disabilities such as autism spectrum disorders, and highlight the tremendous importance of this public health issue.

|
Dr. Christina D. Chambers |
The updated diagnostic guidelines expand upon the previous criteria published more than 10 years ago by Hoyme et al. Now on the basis of experience with evaluating more than 10,000 children in the United States, the authors’ consensus guidelines add more detailed information about the type and severity of neurobehavioral deficits commonly seen in alcohol-affected children, specify the quantity and frequency of alcohol reported by the mother that can be used to help define prenatal alcohol exposure, and incorporate emerging biomarkers of exposure that do not rely solely on maternal report, among other improvements and clarifications.
One of the major barriers to identification of FASD-affected children is pediatricians’ lack of confidence in their ability to recognize affected children. This set of guidelines should improve the ability of clinicians to better identify those children who may be affected by alcohol and might otherwise be misdiagnosed or not diagnosed at all, and can help standardize the pediatrician’s approach to doing this.
Christina Chambers, PhD, MPH, a professor of pediatrics at University of California, San Diego, and director of clinical research for the department of pediatrics at UCSD and Rady Children’s Hospital, commented in an interview. She is also a coauthor of, and helped to develop, the guidelines. Dr. Chambers said she had no relevant financial disclosures.
A newly published set of clinical guidelines for the diagnosis of fetal alcohol spectrum disorder (FASD), the first such update to the guidelines since 2005, will help health care providers better diagnose children exposed to alcohol during gestation.
“These new guidelines will be a valuable resource for clinicians to accurately diagnose infants and children who were affected by alcohol exposure before birth,” George F. Koob, PhD, director of the National Institute on Alcohol Abuse and Alcoholism, said in a statement. “They represent the most data-driven diagnostic criteria for fetal alcohol syndrome and fetal alcohol spectrum disorder produced to date.”
The guidelines call for a multidisciplinary approach to FASD diagnosis, which would require children suspected of FASD to be evaluated by either a pediatrician or a clinical geneticist/dysmorphologist, along with undergoing a neuropsychological and behavioral assessment. Children also should be assessed by speech pathologists, occupational therapists, physical therapists, audiologists, psychiatrists, and ophthalmologists on a case-by-case basis, if needed (Pediatrics. 2016;138[2]:e20154256).
“[FASD], the umbrella term for the range of disabilities that can result from prenatal alcohol exposure, represents the leading cause of preventable developmental disabilities in the world,” according to an NIH statement. “As a result of alcohol exposure in the womb, children can have lower IQ, restricted growth resulting in shorter height/lower weight, small head size, a characteristic pattern of facial deformities, and behavioral issues such as attention deficit, poor impulse control, and the inability to regulate mood/behavior.”
As a first step outlined in the diagnostic algorithm in the guidelines, the mothers should be assessed to determine how much prenatal alcohol was consumed; there is a table with a definition of documented prenatal alcohol exposure as it applies to the four definitions. The guidelines stress that no amount of alcohol consumption during pregnancy can be considered safe; therefore, the amount and frequency of alcohol consumption, along with any possible drug use, is critical to determining the severity of FASD in the child.
The four diagnostic categories into which FASD has been divided have not been changed in the update, although the criteria for each have been updated. These four categories, which were created by the Institute of Medicine in 1996, are: fetal alcohol syndrome (FAS), which applies to the most severely affected children; partial FAS (PFAS), which applies to children who display some, but not all, of the full spectrum of FAS characteristics; alcohol-related neurodevelopmental disorder (ARND), which applies to children who have no physical signs of FAS but do display cognitive or behavioral impairment; and alcohol-related birth defects (ARBD), which applies to children with no FAS symptoms aside from a physical malformation brought on by prenatal alcohol consumption.
“These four diagnostic categories remain the most apt descriptors of the range of disabilities observed within the continuum of FASD,” guidelines coauthor Kenneth R. Warren, MD, said in a statement. “We have refined the guidelines to reflect our collective expertise gained through the evaluation of more than 10,000 children in domestic and international venues.”
There is an extensive chart in the guidelines article documenting the updated criteria for the four diagnostic criteria.
After determining maternal alcohol consumption during pregnancy, characteristic structural features should be evaluated in the child. Typical physical signs of FASD include short palpebral fissures, a smooth philtrum, and a vermilion border of the upper lip that may be thinner than normal, along with midface hypoplasia. There is a new lip/philtrum guide for the white population, incorporating a 45-degree view in the guidelines.
From there, neurodevelopmental assessments and neuropsychological evaluations should be conducted to identify any cognitive impairments, keeping in mind that these will progress as the child ages. Finally, a multidisciplinary case conference should be held to discuss whether or not FASD should be diagnosed or not.
“These updated guidelines reflect consensus among a large and experienced cadre of FASD investigators in the fields of dysmorphology, epidemiology, neurology, psychology, developmental/ behavioral pediatrics, and educational diagnostics,” wrote the authors of the guidelines, led by H. Eugene Hoyme, MD of the University of South Dakota in Sioux Falls. “The improved specificity of these guidelines will aid clinicians in assignment of more accurate diagnoses of alcohol-exposed infants and children, thereby leading to more widespread early intervention and improved prevention efforts.”
The authors reported no relevant financial disclosures.
A newly published set of clinical guidelines for the diagnosis of fetal alcohol spectrum disorder (FASD), the first such update to the guidelines since 2005, will help health care providers better diagnose children exposed to alcohol during gestation.
“These new guidelines will be a valuable resource for clinicians to accurately diagnose infants and children who were affected by alcohol exposure before birth,” George F. Koob, PhD, director of the National Institute on Alcohol Abuse and Alcoholism, said in a statement. “They represent the most data-driven diagnostic criteria for fetal alcohol syndrome and fetal alcohol spectrum disorder produced to date.”
The guidelines call for a multidisciplinary approach to FASD diagnosis, which would require children suspected of FASD to be evaluated by either a pediatrician or a clinical geneticist/dysmorphologist, along with undergoing a neuropsychological and behavioral assessment. Children also should be assessed by speech pathologists, occupational therapists, physical therapists, audiologists, psychiatrists, and ophthalmologists on a case-by-case basis, if needed (Pediatrics. 2016;138[2]:e20154256).
“[FASD], the umbrella term for the range of disabilities that can result from prenatal alcohol exposure, represents the leading cause of preventable developmental disabilities in the world,” according to an NIH statement. “As a result of alcohol exposure in the womb, children can have lower IQ, restricted growth resulting in shorter height/lower weight, small head size, a characteristic pattern of facial deformities, and behavioral issues such as attention deficit, poor impulse control, and the inability to regulate mood/behavior.”
As a first step outlined in the diagnostic algorithm in the guidelines, the mothers should be assessed to determine how much prenatal alcohol was consumed; there is a table with a definition of documented prenatal alcohol exposure as it applies to the four definitions. The guidelines stress that no amount of alcohol consumption during pregnancy can be considered safe; therefore, the amount and frequency of alcohol consumption, along with any possible drug use, is critical to determining the severity of FASD in the child.
The four diagnostic categories into which FASD has been divided have not been changed in the update, although the criteria for each have been updated. These four categories, which were created by the Institute of Medicine in 1996, are: fetal alcohol syndrome (FAS), which applies to the most severely affected children; partial FAS (PFAS), which applies to children who display some, but not all, of the full spectrum of FAS characteristics; alcohol-related neurodevelopmental disorder (ARND), which applies to children who have no physical signs of FAS but do display cognitive or behavioral impairment; and alcohol-related birth defects (ARBD), which applies to children with no FAS symptoms aside from a physical malformation brought on by prenatal alcohol consumption.
“These four diagnostic categories remain the most apt descriptors of the range of disabilities observed within the continuum of FASD,” guidelines coauthor Kenneth R. Warren, MD, said in a statement. “We have refined the guidelines to reflect our collective expertise gained through the evaluation of more than 10,000 children in domestic and international venues.”
There is an extensive chart in the guidelines article documenting the updated criteria for the four diagnostic criteria.
After determining maternal alcohol consumption during pregnancy, characteristic structural features should be evaluated in the child. Typical physical signs of FASD include short palpebral fissures, a smooth philtrum, and a vermilion border of the upper lip that may be thinner than normal, along with midface hypoplasia. There is a new lip/philtrum guide for the white population, incorporating a 45-degree view in the guidelines.
From there, neurodevelopmental assessments and neuropsychological evaluations should be conducted to identify any cognitive impairments, keeping in mind that these will progress as the child ages. Finally, a multidisciplinary case conference should be held to discuss whether or not FASD should be diagnosed or not.
“These updated guidelines reflect consensus among a large and experienced cadre of FASD investigators in the fields of dysmorphology, epidemiology, neurology, psychology, developmental/ behavioral pediatrics, and educational diagnostics,” wrote the authors of the guidelines, led by H. Eugene Hoyme, MD of the University of South Dakota in Sioux Falls. “The improved specificity of these guidelines will aid clinicians in assignment of more accurate diagnoses of alcohol-exposed infants and children, thereby leading to more widespread early intervention and improved prevention efforts.”
The authors reported no relevant financial disclosures.
FROM PEDIATRICS
CDC updates diagnostic guidelines for congenital Zika virus infection
All infants who either exhibit abnormal clinical or neuroimaging findings consistent with possible Zika infection, or who exhibit normal phenotypes but are born to mothers who are positive for Zika virus infection during pregnancy, should undergo laboratory testing for the virus, according to updated diagnostic guidance from the CDC.
All infants should undergo a comprehensive physical exam at birth, as well as a neurologic examination, postnatal head ultrasound, and standard hearing tests to determine any phenotypic signs of congenital Zika infections (MMWR. ePub: 2016 Aug 19. doi: 10.15585/mmwr.mm6533e2).
Laboratory samples should be collected within 2 days of birth. Molecular testing should be done via a real-time reverse transcription–polymerase chain reaction (rRT-PCR), while serologic testing should be carried out via IgM. If the former test is positive, then the infant is Zika positive; however, if the rRT-PCR is negative but the IgM is positive, then the conclusion can only be a “probable” congenital Zika infection.
For infants with laboratory-confirmed or probable congenital Zika infection, the CDC recommends outpatient management and follow-up. For those who are found negative for Zika despite having other symptoms consistent with infection, the CDC advises continued evaluation to determine the cause of any congenital anomalies.
If an infant has no overt symptoms of Zika virus but is found to have laboratory-confirmed or probable Zika, they should be given routine newborn care along with auditory brainstem response (ABR) testing and an opthalmology examination within 1 month of birth. Infants with no overt signs of Zika and a lab-confirmed negative result can resume standard newborn care with no additional monitoring.
Outpatient care should begin with clear establishment of a medical home, followed by monitoring the child’s growth and developmental screenings at every well child visit, according to the CDC. Vision screening should be repeated at all well child visits; ABR should be repeated 4-6 months after initial testing.
“Use a standardized, validated developmental screening tool at 9 months as currently recommended, or earlier for any parental or provider concerns,” according to lead author Kate Russell, MD, of the CDC’s Epidemic Intelligence Service, and her coauthors.
Cranial ultrasound should be performed on all infants, regardless of how normal any prenatal cranial ultrasounds were. Previously, the CDC advised that if a third trimester prenatal cranial ultrasound showed no abnormalities, a postnatal cranial ultrasound was not needed.
The CDC continues to advise that a multidisciplinary approach be taken to evaluation, diagnosis, and potential treatment of infants with congenital Zika virus infection.
“Because the types of services needed to care for infants with congenital Zika syndrome are complex, CDC recommends coordinated care through a multidisciplinary team and established medical home,” according to the guidance. “As a critical component of patient care and early identification of any delays, families should be empowered to be active participants in their child’s monitoring and care.”
All infants who either exhibit abnormal clinical or neuroimaging findings consistent with possible Zika infection, or who exhibit normal phenotypes but are born to mothers who are positive for Zika virus infection during pregnancy, should undergo laboratory testing for the virus, according to updated diagnostic guidance from the CDC.
All infants should undergo a comprehensive physical exam at birth, as well as a neurologic examination, postnatal head ultrasound, and standard hearing tests to determine any phenotypic signs of congenital Zika infections (MMWR. ePub: 2016 Aug 19. doi: 10.15585/mmwr.mm6533e2).
Laboratory samples should be collected within 2 days of birth. Molecular testing should be done via a real-time reverse transcription–polymerase chain reaction (rRT-PCR), while serologic testing should be carried out via IgM. If the former test is positive, then the infant is Zika positive; however, if the rRT-PCR is negative but the IgM is positive, then the conclusion can only be a “probable” congenital Zika infection.
For infants with laboratory-confirmed or probable congenital Zika infection, the CDC recommends outpatient management and follow-up. For those who are found negative for Zika despite having other symptoms consistent with infection, the CDC advises continued evaluation to determine the cause of any congenital anomalies.
If an infant has no overt symptoms of Zika virus but is found to have laboratory-confirmed or probable Zika, they should be given routine newborn care along with auditory brainstem response (ABR) testing and an opthalmology examination within 1 month of birth. Infants with no overt signs of Zika and a lab-confirmed negative result can resume standard newborn care with no additional monitoring.
Outpatient care should begin with clear establishment of a medical home, followed by monitoring the child’s growth and developmental screenings at every well child visit, according to the CDC. Vision screening should be repeated at all well child visits; ABR should be repeated 4-6 months after initial testing.
“Use a standardized, validated developmental screening tool at 9 months as currently recommended, or earlier for any parental or provider concerns,” according to lead author Kate Russell, MD, of the CDC’s Epidemic Intelligence Service, and her coauthors.
Cranial ultrasound should be performed on all infants, regardless of how normal any prenatal cranial ultrasounds were. Previously, the CDC advised that if a third trimester prenatal cranial ultrasound showed no abnormalities, a postnatal cranial ultrasound was not needed.
The CDC continues to advise that a multidisciplinary approach be taken to evaluation, diagnosis, and potential treatment of infants with congenital Zika virus infection.
“Because the types of services needed to care for infants with congenital Zika syndrome are complex, CDC recommends coordinated care through a multidisciplinary team and established medical home,” according to the guidance. “As a critical component of patient care and early identification of any delays, families should be empowered to be active participants in their child’s monitoring and care.”
All infants who either exhibit abnormal clinical or neuroimaging findings consistent with possible Zika infection, or who exhibit normal phenotypes but are born to mothers who are positive for Zika virus infection during pregnancy, should undergo laboratory testing for the virus, according to updated diagnostic guidance from the CDC.
All infants should undergo a comprehensive physical exam at birth, as well as a neurologic examination, postnatal head ultrasound, and standard hearing tests to determine any phenotypic signs of congenital Zika infections (MMWR. ePub: 2016 Aug 19. doi: 10.15585/mmwr.mm6533e2).
Laboratory samples should be collected within 2 days of birth. Molecular testing should be done via a real-time reverse transcription–polymerase chain reaction (rRT-PCR), while serologic testing should be carried out via IgM. If the former test is positive, then the infant is Zika positive; however, if the rRT-PCR is negative but the IgM is positive, then the conclusion can only be a “probable” congenital Zika infection.
For infants with laboratory-confirmed or probable congenital Zika infection, the CDC recommends outpatient management and follow-up. For those who are found negative for Zika despite having other symptoms consistent with infection, the CDC advises continued evaluation to determine the cause of any congenital anomalies.
If an infant has no overt symptoms of Zika virus but is found to have laboratory-confirmed or probable Zika, they should be given routine newborn care along with auditory brainstem response (ABR) testing and an opthalmology examination within 1 month of birth. Infants with no overt signs of Zika and a lab-confirmed negative result can resume standard newborn care with no additional monitoring.
Outpatient care should begin with clear establishment of a medical home, followed by monitoring the child’s growth and developmental screenings at every well child visit, according to the CDC. Vision screening should be repeated at all well child visits; ABR should be repeated 4-6 months after initial testing.
“Use a standardized, validated developmental screening tool at 9 months as currently recommended, or earlier for any parental or provider concerns,” according to lead author Kate Russell, MD, of the CDC’s Epidemic Intelligence Service, and her coauthors.
Cranial ultrasound should be performed on all infants, regardless of how normal any prenatal cranial ultrasounds were. Previously, the CDC advised that if a third trimester prenatal cranial ultrasound showed no abnormalities, a postnatal cranial ultrasound was not needed.
The CDC continues to advise that a multidisciplinary approach be taken to evaluation, diagnosis, and potential treatment of infants with congenital Zika virus infection.
“Because the types of services needed to care for infants with congenital Zika syndrome are complex, CDC recommends coordinated care through a multidisciplinary team and established medical home,” according to the guidance. “As a critical component of patient care and early identification of any delays, families should be empowered to be active participants in their child’s monitoring and care.”
FROM MMWR
Gallstone disease boosts heart disease risk
Gallstone disease is associated with a 23% higher risk of developing coronary heart disease, according to an analysis published Aug. 18 in Arteriosclerosis, Thrombosis, and Vascular Biology.
“Our results suggest that patients with gallstone disease should be monitored closely based on a careful assessment of both gallstone and heart disease risk factors,” senior author Lu Qi, MD, PhD, said in a statement.
Dr. Qi, professor of epidemiology at Tulane University in New Orleans, and his coinvestigators conducted a meta-analysis of seven distinct studies, which involved a total of 842,553 patients and 51,123 cases of coronary heart disease. Patients with coronary heart disease were investigated further to determine if there was any history of gallstone disease.
Results showed that there was a 23% higher likelihood of coronary heart disease in patients who had gallstone disease, compared with those who did not, with a range of 15%-33% across the studies; the adjusted hazard ratio was 1.23 (95% confidence interval, 1.15-1.33).
Additionally, a separate prospective analysis of three of the included studies was conducted to determine individual risk factors that may contribute to the association between gallstone disease and coronary heart disease. These studies were the Nurses’ Health Study, conducted from 1980 to 2010, the Nurses’ Health Study II, which took place during 1989-2011, and the Health Professionals Follow-up Study, from 1986 through 2010, involving 112,520 women, 112,919 women, and 43,703 men, respectively.
This analysis revealed a 17% increase in coronary heart disease risk (aHR, 1.17; 95% CI, 1.09-1.26). Furthermore, the investigators noted that individuals with a history of gallstone disease who were otherwise healthy – in other words, had no history of obesity, high blood pressure, diabetes, or other disorders commonly associated with coronary heart disease – still stood a higher chance of developing coronary heart disease than individuals with no history of gallstone disease (Arterioscler Thromb Vasc Biol. 2016 Aug 18. doi: 10.1161/atvbaha.116.307507).
“Preventing gallstone disease may also benefit heart health,” Dr. Qi said.
“The potential mechanisms for the association of gallstone diseases with [coronary heart disease] may, at least, include the primary metabolic pathway and the bacterial pathway,” Dr. Qi and his coinvestigators posited, explaining that “among patients with gallstones, especially those with cholesterol gallstones, their bile acid and lecithin secretion rates tend to be depressed and cholesterol secretion rates elevated, which could indicate enhanced cholesterol synthesis and therefore increase cardiovascular disease risk.”
This study was supported by funding from the National Institutes of Health, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. The authors had no relevant financial disclosures.
Gallstone disease is associated with a 23% higher risk of developing coronary heart disease, according to an analysis published Aug. 18 in Arteriosclerosis, Thrombosis, and Vascular Biology.
“Our results suggest that patients with gallstone disease should be monitored closely based on a careful assessment of both gallstone and heart disease risk factors,” senior author Lu Qi, MD, PhD, said in a statement.
Dr. Qi, professor of epidemiology at Tulane University in New Orleans, and his coinvestigators conducted a meta-analysis of seven distinct studies, which involved a total of 842,553 patients and 51,123 cases of coronary heart disease. Patients with coronary heart disease were investigated further to determine if there was any history of gallstone disease.
Results showed that there was a 23% higher likelihood of coronary heart disease in patients who had gallstone disease, compared with those who did not, with a range of 15%-33% across the studies; the adjusted hazard ratio was 1.23 (95% confidence interval, 1.15-1.33).
Additionally, a separate prospective analysis of three of the included studies was conducted to determine individual risk factors that may contribute to the association between gallstone disease and coronary heart disease. These studies were the Nurses’ Health Study, conducted from 1980 to 2010, the Nurses’ Health Study II, which took place during 1989-2011, and the Health Professionals Follow-up Study, from 1986 through 2010, involving 112,520 women, 112,919 women, and 43,703 men, respectively.
This analysis revealed a 17% increase in coronary heart disease risk (aHR, 1.17; 95% CI, 1.09-1.26). Furthermore, the investigators noted that individuals with a history of gallstone disease who were otherwise healthy – in other words, had no history of obesity, high blood pressure, diabetes, or other disorders commonly associated with coronary heart disease – still stood a higher chance of developing coronary heart disease than individuals with no history of gallstone disease (Arterioscler Thromb Vasc Biol. 2016 Aug 18. doi: 10.1161/atvbaha.116.307507).
“Preventing gallstone disease may also benefit heart health,” Dr. Qi said.
“The potential mechanisms for the association of gallstone diseases with [coronary heart disease] may, at least, include the primary metabolic pathway and the bacterial pathway,” Dr. Qi and his coinvestigators posited, explaining that “among patients with gallstones, especially those with cholesterol gallstones, their bile acid and lecithin secretion rates tend to be depressed and cholesterol secretion rates elevated, which could indicate enhanced cholesterol synthesis and therefore increase cardiovascular disease risk.”
This study was supported by funding from the National Institutes of Health, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. The authors had no relevant financial disclosures.
Gallstone disease is associated with a 23% higher risk of developing coronary heart disease, according to an analysis published Aug. 18 in Arteriosclerosis, Thrombosis, and Vascular Biology.
“Our results suggest that patients with gallstone disease should be monitored closely based on a careful assessment of both gallstone and heart disease risk factors,” senior author Lu Qi, MD, PhD, said in a statement.
Dr. Qi, professor of epidemiology at Tulane University in New Orleans, and his coinvestigators conducted a meta-analysis of seven distinct studies, which involved a total of 842,553 patients and 51,123 cases of coronary heart disease. Patients with coronary heart disease were investigated further to determine if there was any history of gallstone disease.
Results showed that there was a 23% higher likelihood of coronary heart disease in patients who had gallstone disease, compared with those who did not, with a range of 15%-33% across the studies; the adjusted hazard ratio was 1.23 (95% confidence interval, 1.15-1.33).
Additionally, a separate prospective analysis of three of the included studies was conducted to determine individual risk factors that may contribute to the association between gallstone disease and coronary heart disease. These studies were the Nurses’ Health Study, conducted from 1980 to 2010, the Nurses’ Health Study II, which took place during 1989-2011, and the Health Professionals Follow-up Study, from 1986 through 2010, involving 112,520 women, 112,919 women, and 43,703 men, respectively.
This analysis revealed a 17% increase in coronary heart disease risk (aHR, 1.17; 95% CI, 1.09-1.26). Furthermore, the investigators noted that individuals with a history of gallstone disease who were otherwise healthy – in other words, had no history of obesity, high blood pressure, diabetes, or other disorders commonly associated with coronary heart disease – still stood a higher chance of developing coronary heart disease than individuals with no history of gallstone disease (Arterioscler Thromb Vasc Biol. 2016 Aug 18. doi: 10.1161/atvbaha.116.307507).
“Preventing gallstone disease may also benefit heart health,” Dr. Qi said.
“The potential mechanisms for the association of gallstone diseases with [coronary heart disease] may, at least, include the primary metabolic pathway and the bacterial pathway,” Dr. Qi and his coinvestigators posited, explaining that “among patients with gallstones, especially those with cholesterol gallstones, their bile acid and lecithin secretion rates tend to be depressed and cholesterol secretion rates elevated, which could indicate enhanced cholesterol synthesis and therefore increase cardiovascular disease risk.”
This study was supported by funding from the National Institutes of Health, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. The authors had no relevant financial disclosures.
FROM ARTERIOSCLEROSIS, THROMBOSIS, AND VASCULAR BIOLOGY
Key clinical point: Gallstone disease is associated with an increased risk for coronary heart disease; preventing the former can help mitigate chances of developing the latter.
Major finding: A meta-analysis revealed a 23% increased chance of CHD in gallstone disease patients.
Data source: A meta-analysis of seven studies involving 842,553 subjects, and a prospective cohort study of 269,142 participants in three separate studies that took place from 1980 to 2011.
Disclosures: Funding provided by NIH, Boston Obesity Nutrition Research Center, and United States–Israel Binational Science Foundation. The authors had no relevant financial disclosures.
Study identifies link between rosacea and several GI disorders
A Danish population-based cohort study identified a significant association between patients who have rosacea and their risk of having certain other gastrointestinal diseases – specifically, celiac disease, Crohn’s disease, ulcerative colitis, and irritable bowel syndrome.
“While a co-occurrence of rosacea and gastrointestinal disorders has previously been evaluated, the topic remains controversial,” wrote the authors, led by Alexander Egeberg, MD, of the department of dermatology and allergy, Herlev and Gentofte Hospital, Hellerup, Denmark (Br J Dermatol. 2016 Aug 8. doi: 10.1111/bjd.14930).
Dr. Egeberg and his coinvestigators conducted a nationwide cohort study of adults aged 18 years and older from national administrative registers, starting on Jan. 1, 2008, through Dec. 31, 2012. In total, 49,475 rosacea patients were included, with 4,312,213 individuals from the general population who were used as controls. The outcomes were any occurrences of celiac disease (CeD), Crohn’s disease (CD), ulcerative colitis (UC), and irritable bowel syndrome (IBS), Helicobactor pylori (HP) infection, and small intestinal bacterial overgrowth that occurred during the study period, conditions that were chosen “due to their potential mechanistic and pathogenic overlap with rosacea,” they wrote.
At baseline, the prevalence of CeD, CD, UC, HP infection, small intestinal bacterial overgrowth, and IBS was significantly higher among the patients with rosacea, compared with the controls.
Adjusted hazard ratios showed a significant association between patients with rosacea and one of the following GI diagnoses: CeD (Hazard ratio, 1.46), CD (HR, 1.45), UC (HR, 1.19), and IBS (HR, 1.34). However, no significant association was found between rosacea and HP infection or small intestinal bacterial overgrowth.
“The findings from this study raise an important question about the pathogenic overlap between the studied gastrointestinal disorders and rosacea,” Dr. Egeberg and his coauthors wrote. Most of the outcomes examined in the study, they noted, “carry several autoimmune characteristics and, although speculative, it is possible that shared autoimmune susceptibility may provide a link between rosacea and the examined gastrointestinal disorders.”
No funding was received for this study. Dr. Egeberg and his coauthors reported no relevant financial disclosures.
A Danish population-based cohort study identified a significant association between patients who have rosacea and their risk of having certain other gastrointestinal diseases – specifically, celiac disease, Crohn’s disease, ulcerative colitis, and irritable bowel syndrome.
“While a co-occurrence of rosacea and gastrointestinal disorders has previously been evaluated, the topic remains controversial,” wrote the authors, led by Alexander Egeberg, MD, of the department of dermatology and allergy, Herlev and Gentofte Hospital, Hellerup, Denmark (Br J Dermatol. 2016 Aug 8. doi: 10.1111/bjd.14930).
Dr. Egeberg and his coinvestigators conducted a nationwide cohort study of adults aged 18 years and older from national administrative registers, starting on Jan. 1, 2008, through Dec. 31, 2012. In total, 49,475 rosacea patients were included, with 4,312,213 individuals from the general population who were used as controls. The outcomes were any occurrences of celiac disease (CeD), Crohn’s disease (CD), ulcerative colitis (UC), and irritable bowel syndrome (IBS), Helicobactor pylori (HP) infection, and small intestinal bacterial overgrowth that occurred during the study period, conditions that were chosen “due to their potential mechanistic and pathogenic overlap with rosacea,” they wrote.
At baseline, the prevalence of CeD, CD, UC, HP infection, small intestinal bacterial overgrowth, and IBS was significantly higher among the patients with rosacea, compared with the controls.
Adjusted hazard ratios showed a significant association between patients with rosacea and one of the following GI diagnoses: CeD (Hazard ratio, 1.46), CD (HR, 1.45), UC (HR, 1.19), and IBS (HR, 1.34). However, no significant association was found between rosacea and HP infection or small intestinal bacterial overgrowth.
“The findings from this study raise an important question about the pathogenic overlap between the studied gastrointestinal disorders and rosacea,” Dr. Egeberg and his coauthors wrote. Most of the outcomes examined in the study, they noted, “carry several autoimmune characteristics and, although speculative, it is possible that shared autoimmune susceptibility may provide a link between rosacea and the examined gastrointestinal disorders.”
No funding was received for this study. Dr. Egeberg and his coauthors reported no relevant financial disclosures.
A Danish population-based cohort study identified a significant association between patients who have rosacea and their risk of having certain other gastrointestinal diseases – specifically, celiac disease, Crohn’s disease, ulcerative colitis, and irritable bowel syndrome.
“While a co-occurrence of rosacea and gastrointestinal disorders has previously been evaluated, the topic remains controversial,” wrote the authors, led by Alexander Egeberg, MD, of the department of dermatology and allergy, Herlev and Gentofte Hospital, Hellerup, Denmark (Br J Dermatol. 2016 Aug 8. doi: 10.1111/bjd.14930).
Dr. Egeberg and his coinvestigators conducted a nationwide cohort study of adults aged 18 years and older from national administrative registers, starting on Jan. 1, 2008, through Dec. 31, 2012. In total, 49,475 rosacea patients were included, with 4,312,213 individuals from the general population who were used as controls. The outcomes were any occurrences of celiac disease (CeD), Crohn’s disease (CD), ulcerative colitis (UC), and irritable bowel syndrome (IBS), Helicobactor pylori (HP) infection, and small intestinal bacterial overgrowth that occurred during the study period, conditions that were chosen “due to their potential mechanistic and pathogenic overlap with rosacea,” they wrote.
At baseline, the prevalence of CeD, CD, UC, HP infection, small intestinal bacterial overgrowth, and IBS was significantly higher among the patients with rosacea, compared with the controls.
Adjusted hazard ratios showed a significant association between patients with rosacea and one of the following GI diagnoses: CeD (Hazard ratio, 1.46), CD (HR, 1.45), UC (HR, 1.19), and IBS (HR, 1.34). However, no significant association was found between rosacea and HP infection or small intestinal bacterial overgrowth.
“The findings from this study raise an important question about the pathogenic overlap between the studied gastrointestinal disorders and rosacea,” Dr. Egeberg and his coauthors wrote. Most of the outcomes examined in the study, they noted, “carry several autoimmune characteristics and, although speculative, it is possible that shared autoimmune susceptibility may provide a link between rosacea and the examined gastrointestinal disorders.”
No funding was received for this study. Dr. Egeberg and his coauthors reported no relevant financial disclosures.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Key clinical point: There is an association between rosacea and certain gastrointestinal diseases, but the specific link between the two is not clear.
Major finding: People with rosacea had a significantly increased risk of having celiac disease, Crohn’s disease, ulcerative colitis, and irritable bowel syndrome.
Data source: A population-based case-control study in Denmark compared the risks of several GI disorders in 49,475 people with rosacea and 4,312,213 controls without rosacea.
Disclosures: No funding was received for this study. The authors reported no relevant financial disclosures.