User login
Management of bow legs in children: A primary care protocol
ABSTRACT
Objective To reduce unnecessary orthopedic referrals by developing a protocol for managing physiologic bow legs in the primary care environment through the use of a noninvasive technique that simultaneously tracks normal varus progression and screens for potential pathologic bowing requiring an orthopedic referral.
Methods Retrospective study of 155 patients with physiologic genu varum and 10 with infantile Blount’s disease. We used fingerbreadth measurements to document progression or resolution of bow legs. Final diagnoses were made by one orthopedic surgeon using clinical and radiographic evidence. We divided genu varum patients into 3 groups: patients presenting with bow legs before 18 months of age (MOA), patients presenting between 18 and 23 MOA, and patients presenting at 24 MOA or older for analyses relevant to the development of the follow-up protocol.
Results Physiologic genu varum patients walked earlier than average infants (10 months vs 12-15 months; P<.001). Physiologic genu varum patients presenting before 18 MOA demonstrated initial signs of correction between 18 and 24 MOA and resolution by 30 MOA. Physiologic genu varum patients presenting between 18 and 23 MOA demonstrated initial signs of correction between 24 MOA and 30 MOA and resolution by 36 MOA.
Conclusion Primary care physicians can manage most children presenting with bow legs. Management focuses on following the progression or resolution of varus with regular follow-up. For patients presenting with bow legs, we recommend a follow-up protocol using mainly well-child checkups and a simple clinical assessment to monitor varus progression and screen for pathologic bowing.
Bow legs in young children can be a concern for parents.1,2 By far, the most common reason for bow legs is physiologic genu varum,3-5 a nonprogressive stage of normal development in young children that generally resolves spontaneously without treatment.1,6-11 Normally developing children undergo a varus phase between birth and 18 to 24 months of age (MOA), at which time there is usually a transition in alignment from varus to straight to valgus (knock knees), which will correct to straight or mild valgus throughout adolescence.1,6,7,9,10,12-17
The most common form of pathologic bow legs is Blount’s disease, also known as tibia vara, which must be differentiated from physiologic genu varum.8-10,15,18-24 The progressive varus deformity of Blount’s disease usually requires orthopedic intervention.1,10,23-26 Early diagnosis may spare patients complex interventions, improve prognosis, and limit complications that include gait abnormalities,4,8,10,27 knee joint instability,4,24,27 osteoarthritis,9,20,27 meniscal tears,27 and degenerative joint disease.19,20,27
Although variables such as walking age, race, weight, and gender have been suggested as risk factors for Blount’s disease, they have not been useful in differentiating between Blount’s pathology and physiologic genu varum.1,4,5,7,10,20,28 In the primary care setting, distinguishing physiologic from pathologic forms of bow legs is possible with a thorough history and physical exam and with radiographs, as warranted.1,2,15 More than 40% of genu varum/genu valgum cases referred for orthopedic consultation turn out to be the physiologic form,2 suggesting a need for guidelines in the primary care setting to help direct referral and follow-up. The purpose of this study was to provide recommendations to family physicians for evaluating and managing children with bow legs.
Materials and methods
This study, approved by the Internal Review Board of Akron Children’s Hospital, is a retrospective review of children seen by a single pediatric orthopedic surgeon (DSW) from 1970 to 2012. Four-hundred twenty-four children were received for evaluation of bow legs. Excluded from our final analysis were 220 subjects seen only once for this specific referral and 39 subjects diagnosed with a condition other than genu varum or Blount’s disease (ie, rickets, skeletal dysplasia, sequelae of trauma, or infection). Ten subjects with Blount’s disease and 155 subjects with physiologic genu varum were included in the final data analysis.
In addition to noting the age at which a patient walked independently, at each visit we documented age and the fingerbreadth (varus) distance between the medial femoral condyles with the child’s ankles held together. Parents reported age of independent walking for just 3 children with Blount’s disease and for 134 children with physiologic genu varum. Study variables for the genu varum data analysis were age of walking, age at presentation, age at varus correction, age at varus resolution, time between presentation and varus correction, and time between presentation and varus resolution. Varus correction is defined as any decrease in varus angulation since presentation. Varus resolution is defined as varus correction to less than or equal to half of the varus angulation at presentation. For inclusion in the age-at-resolution analysis, a child must have been evaluated at regular follow-up visits (all rechecks within 8 months).
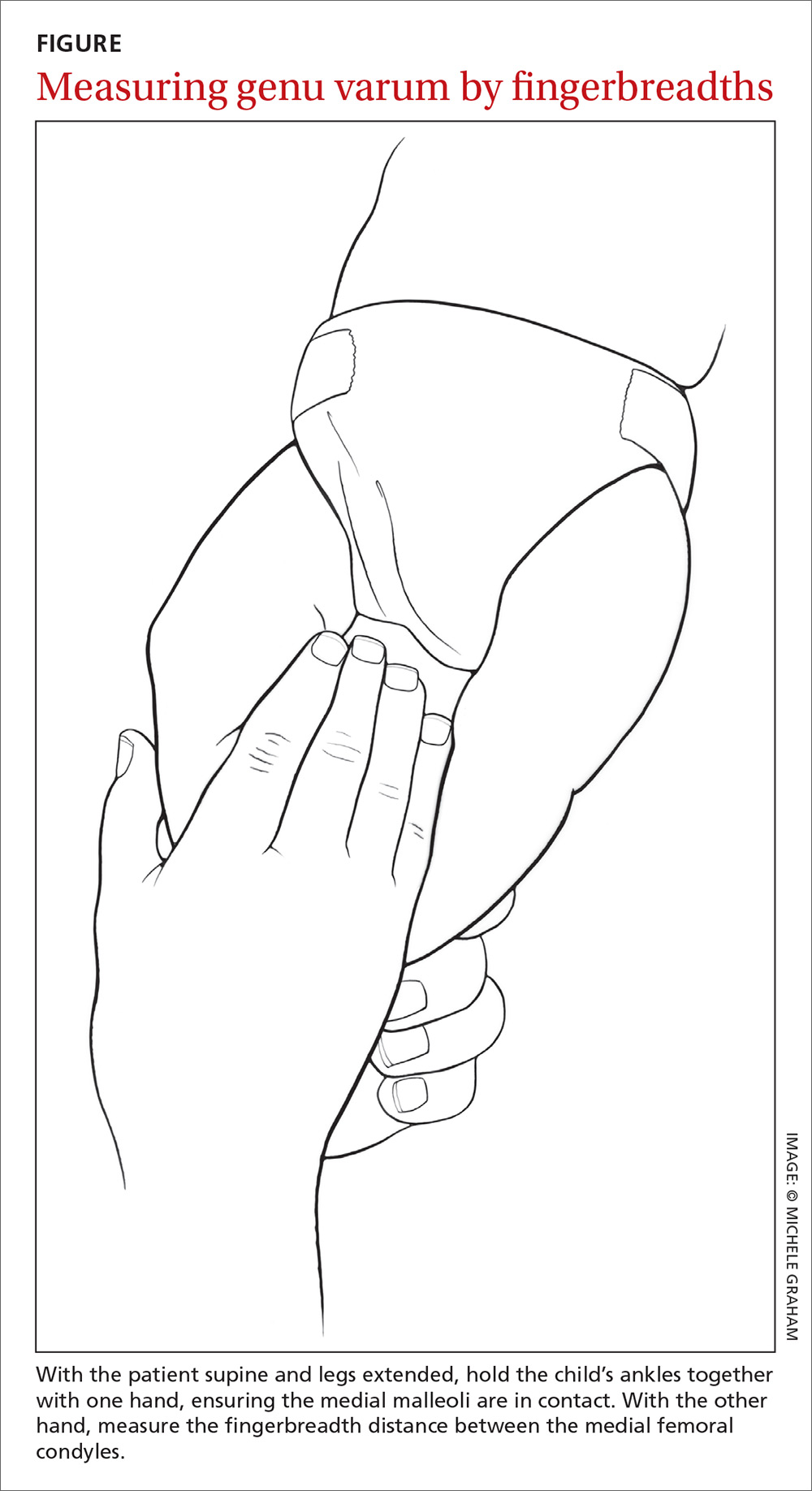
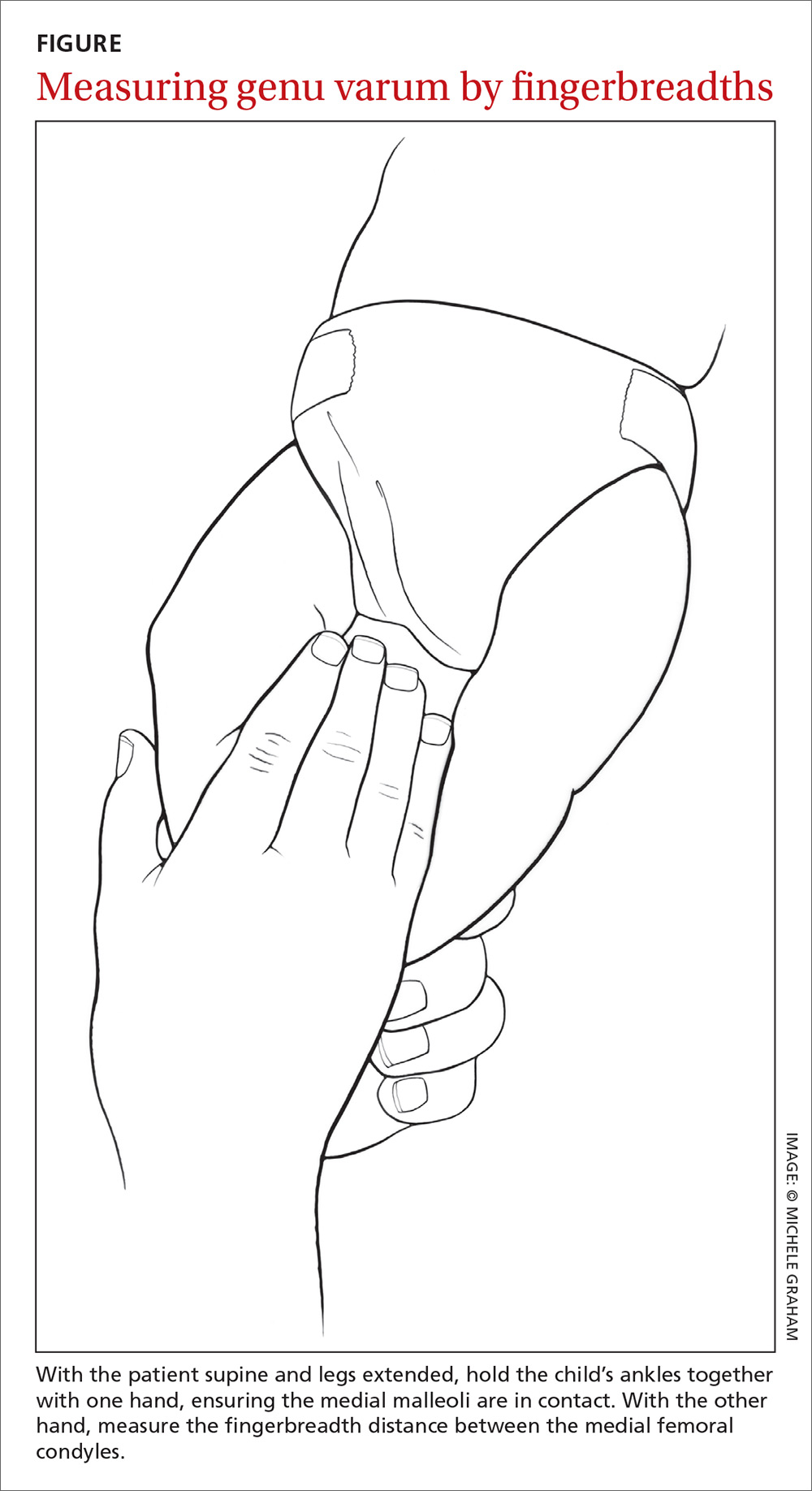
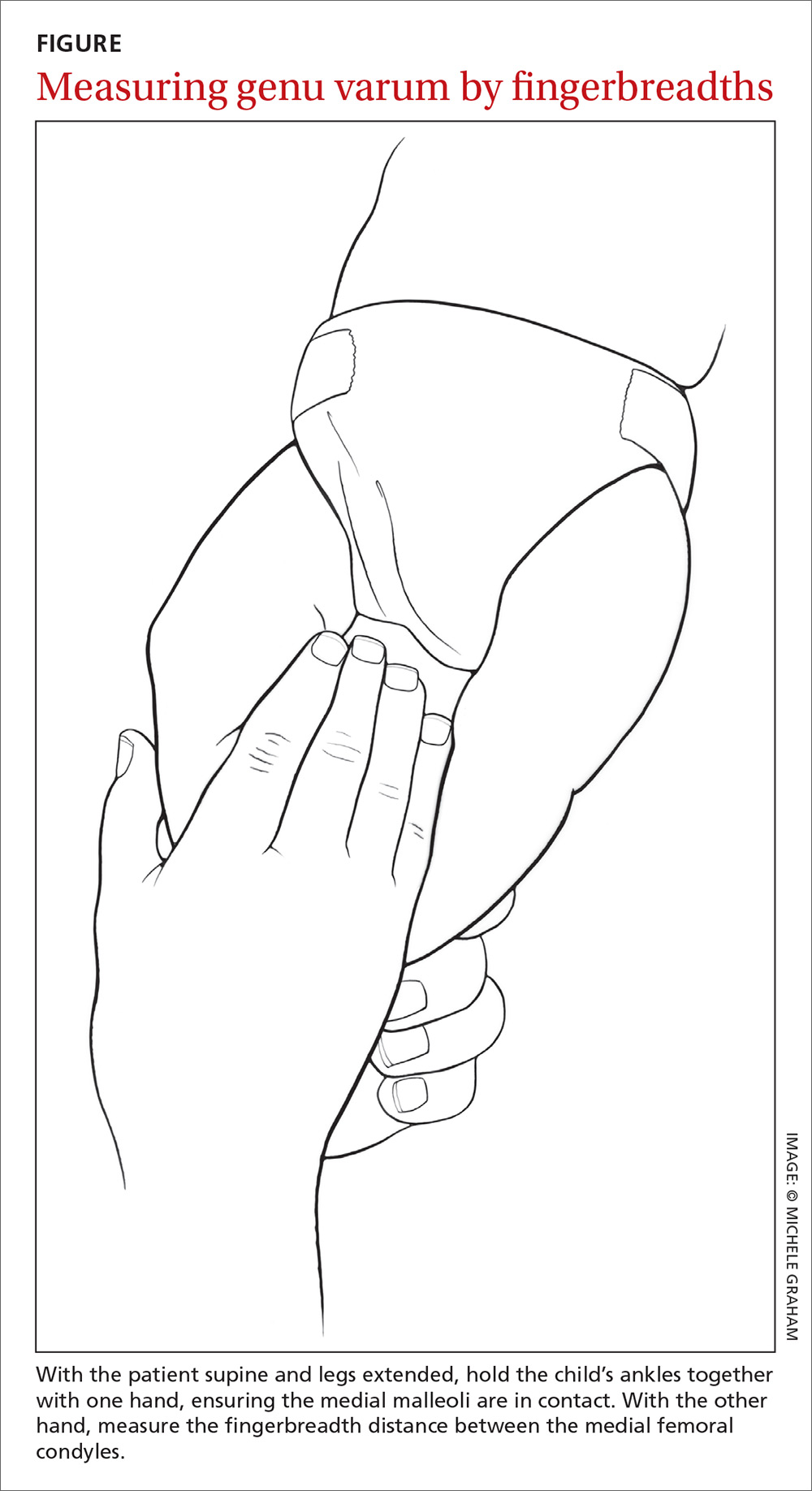
To measure varus distance, we used the fingerbreadth method described by Weiner in a study of 600 cases (FIGURE).6 This simple technique, which requires no special equipment, accurately detected differences in varus angulation and tracked the normal pattern of lower limb angular development. The patient should be supine on the examination table with legs extended. With one hand, the examiner holds the child’s ankles together, ensuring the medial malleoli are in contact. With the other hand, the examiner measures the fingerbreadth distance between the medial femoral condyles. Alternatively, a ruler may be used to measure the distance. This latter method may be especially useful in practices where the patient is likely to see more than one provider for well child care.
We divided the genu varum subject group into 3 subgroups by age at presentation: 103 subjects were younger than 18 months; 47 were 18 to 23 months; and 5 were 24 months or older. We used the data analysis toolkit in Microsoft Excel 2013 to perform a statistical analysis of study variables. We assumed the genu varum population is a normally distributed population. We used a 95% confidence level (α=0.05) for all calculations of confidence intervals (CIs), student t-tests, and tolerance intervals. Based on the data analysis results, we developed a series of follow-up and referral guidelines for practitioners.
Results
The mean walking age for those diagnosed with physiologic genu varum was 10 months (95% CI, 9.8-10.4), which is significantly younger than the 12 months of age (at the earliest) typical of toddlers in general (P<.001). There was no significant difference between the walking age of male and female children diagnosed with genu varum (P=.37).
Of the children presenting with the primary complaint of bow legs, 6% subsequently developed Blount’s disease. These patients presented at a mean age of 20.9 months and were diagnosed at a mean age of 23.9 months. Following the Blount’s disease diagnosis, we initiated therapy in all cases (3 surgical, 7 bracing).
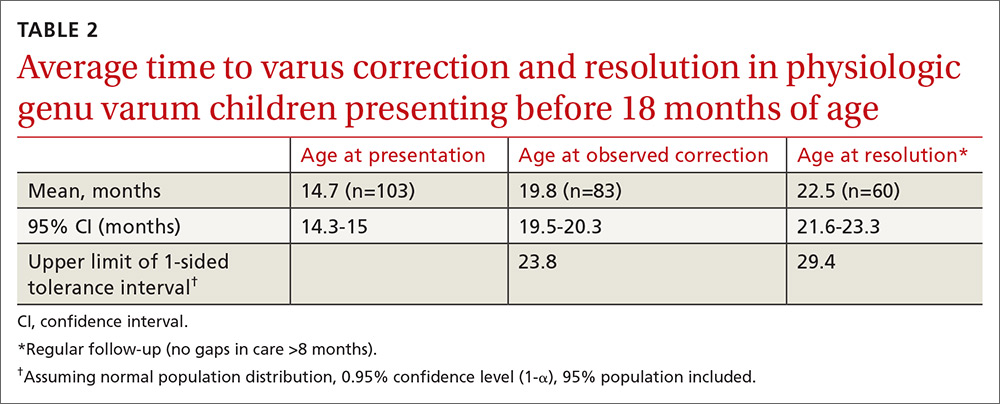
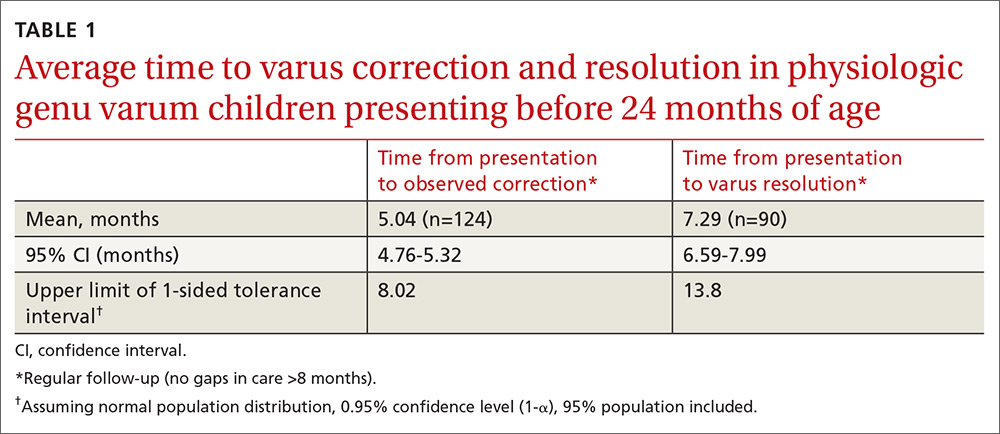
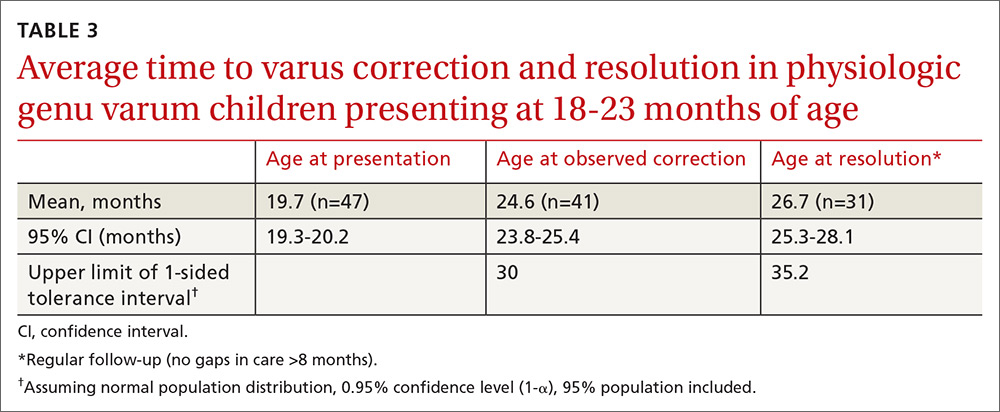
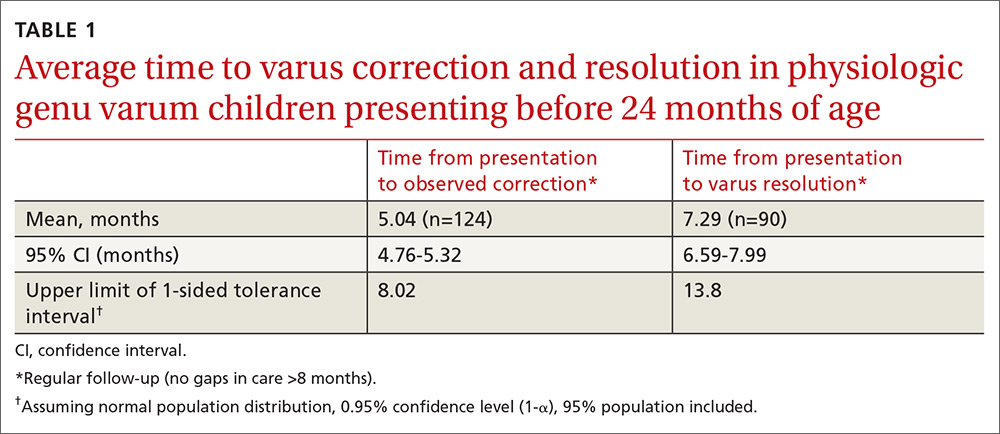
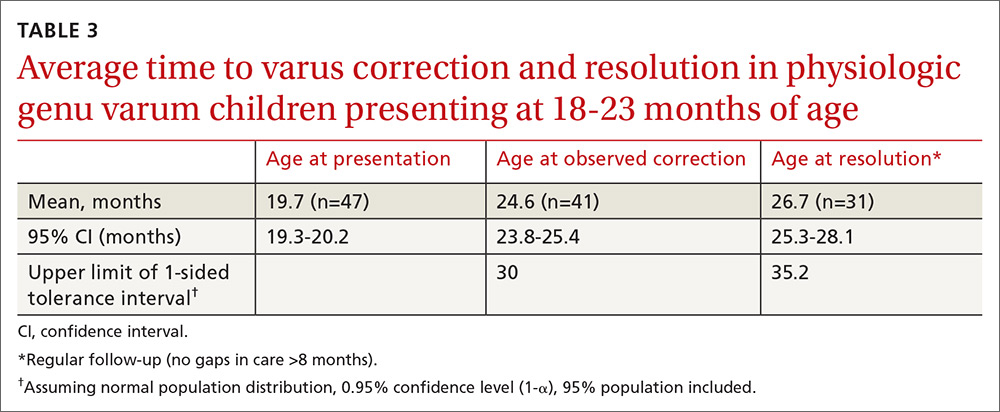
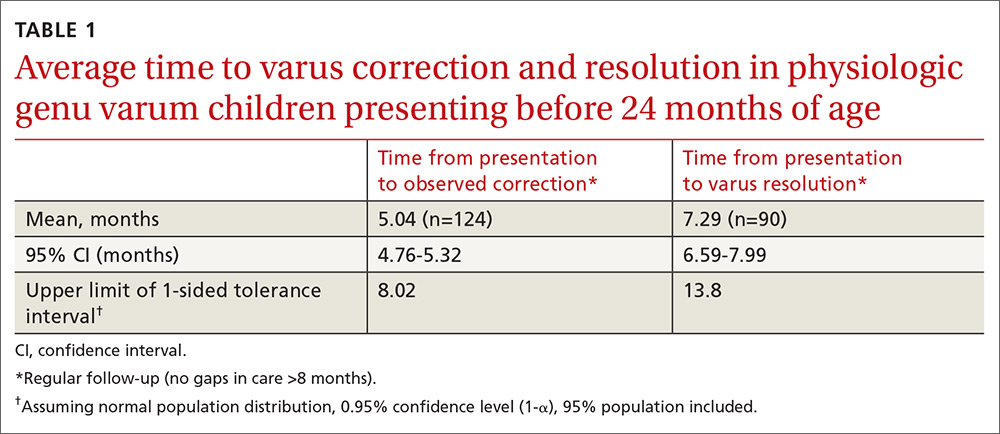
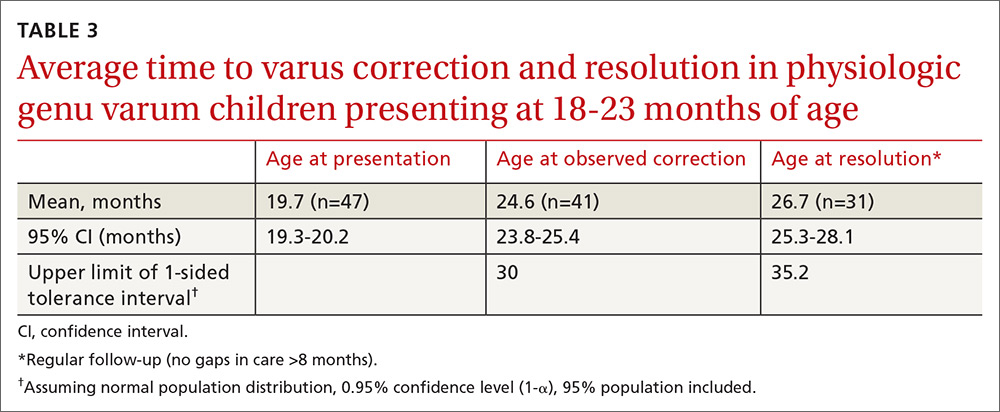
Physiologic genu varum patients presented at a mean age of 16.4 months, with only 3.23% presenting at older than 23 months. On average, physiologic genu varum patients presenting before 24 months of age showed measurable varus correction 5 months after presentation and achieved varus resolution 7.3 months after presentation (TABLE 1). Assuming the patient population is normally distributed, we can be 95% confident that 95% of physiologic genu varum patients presenting before 18 months of age will show measurable varus correction by 24 months and will resolve without intervention by 30 months (TABLE 2). Patients presenting between 18 and 23 months of age should show measurable varus correction by 30 months and resolution by 36 months (TABLE 3).
Discussion
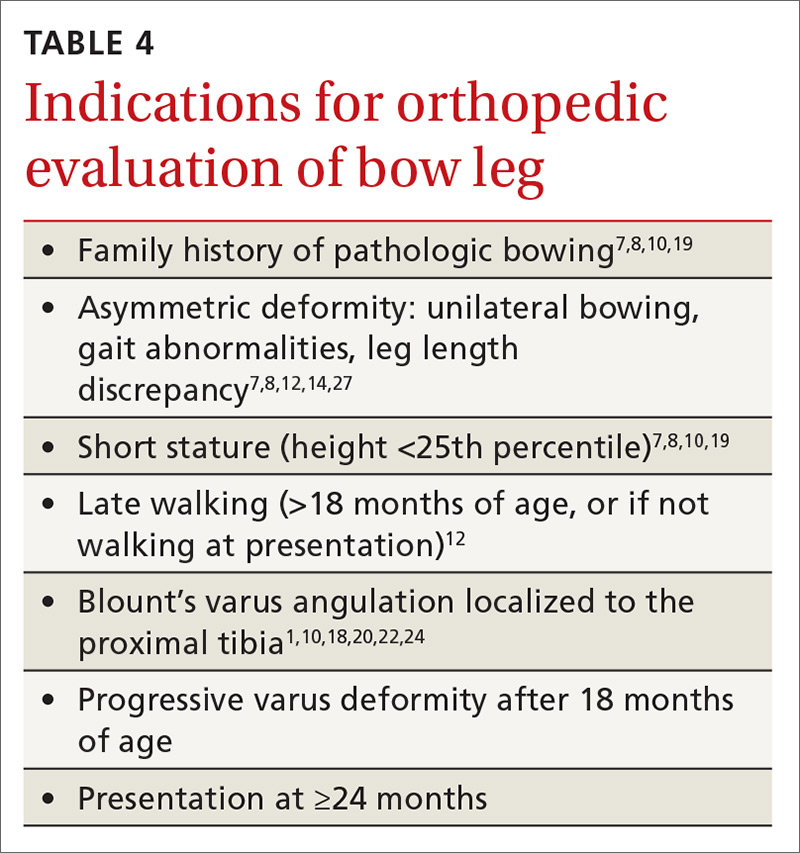
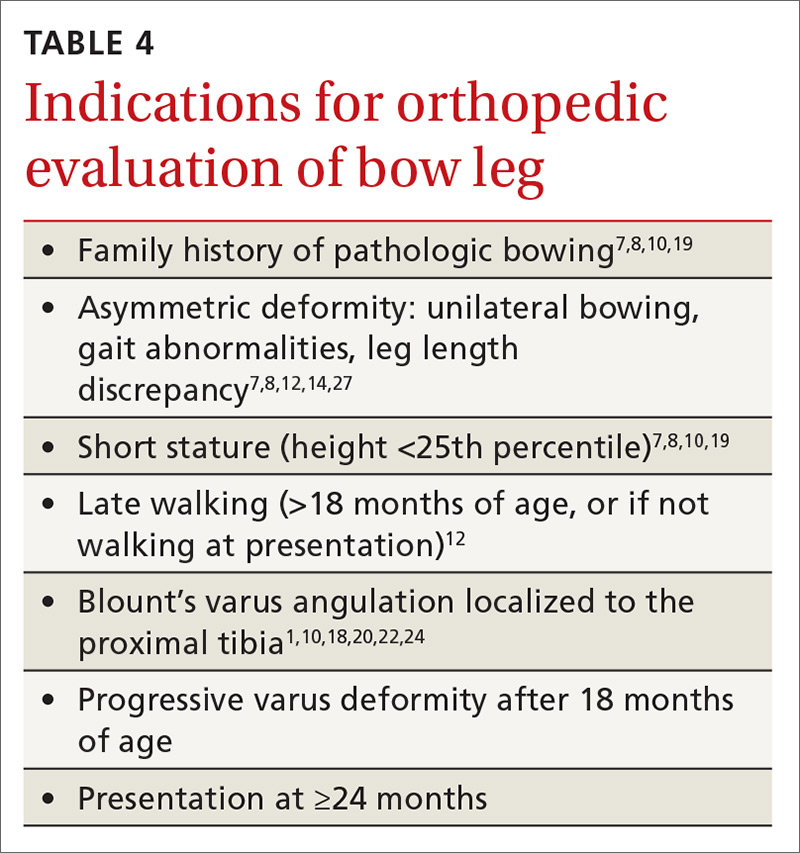
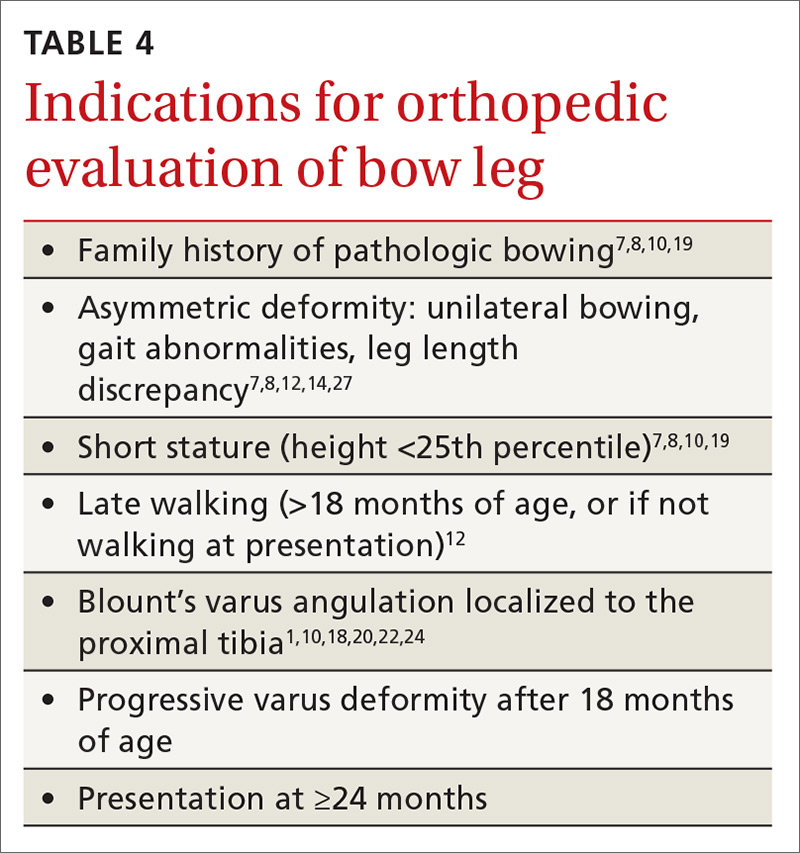
Primary care physicians have the ability to differentiate physiologic genu varum from pathologic forms of bow legs with a thorough history, physical exam, and radiographic examination, if necessary1,2,13 (TABLE 41,7,8,10,12,14,18-20,22,24,27). Several approaches to differentiating Blount’s disease and physiologic genu varum have been described in the literature.1,4,7,8,10,14,22,23
The average age at which children begin to walk independently is between 13 and 15 months.5,18,29-31 Recently, it has been suggested that the range be expanded to include 12 months of age.30 The association between early walking (at 10-11 months)12,20,22 and Blount’s disease is generally accepted in the orthopedic literature.1,4,7,10,19-22 However, some authors have suggested early walking also contributes to genu varum.1,5,8,10,18,28 The mean age of independent walking for children with physiologic genu varum suggested in the literature (10 months) was confirmed in our study and found to be significantly younger than the average for toddlers generally.1,22 Early walking is clearly associated with both physiologic genu varum and Blount’s disease, but no direct causation has been identified in either case. An alternative means of differentiating these entities is needed.
Radiographic examination of the knee is essential to the diagnosis of Blount’s disease as well as other, less common causes of pathologic bow legs (skeletal dysplasia, rickets, traumatic growth plate insults, infections, neoplasms).1,8,14,19 The common radiologic classification of staging for Blount’s disease is the Langenskiöld staging system, which involves identification of characteristic radiographic changes at the tibial physis.5,8,14,15,18,22,24
Sequential measurement of genu varum is most useful in differentiating between physiologic and pathologic processes. Physiologic genu varum, an exaggeration of the normal developmental pattern, characteristically resolves and evolves into physiologic genu valgum by 3 years of age.1,6-11 The pathophysiology of Blount’s disease is believed to be related to biomechanical overloading of the posteromedial proximal tibia during gait with the knee in a varus orientation. Excess loading on the proximal medial physis contributes to varus progression.4,10,14,20,25,27 Patients with Blount’s disease progress with varus and concomitant internal tibial torsion associated with growth plate irregularities and eventually exhibit premature closure.1,10,14,18,20,23,24,26 In the months prior to Blount’s disease diagnosis, increasing varus has been reported.4,7,10,19 Varus progression that differs from the expected pattern indicates possible pathologic bow legs and should prompt radiologic evaluation and, often, an orthopedic referral.3,4,7-9,12,13,21
In our study, only 3% of children with physiologic genu varum presented at 24 months of age or older, compared with 20% of Blount’s disease patients. We recommend considering orthopedic referral for any patient presenting with bow legs at 24 months of age or older. Additionally, consider orthopedic referral for any patient whose varus has not begun to correct within 8 months or has not resolved within 14 months of presentation, as more than 95% of patients with physiologic genu varum are expected to meet these milestones (TABLE 1). And do not hesitate to refer patients at any stage of follow-up if you suspect pathology or if parents are anxious.
If no sign of pathology is immediately identified, we recommend the following course of action:
- Record a reference fingerbreadth or ruler measurement at the initial presentation.
- Re-examine the knee varus at the next regular well-child visit (TABLE 5).
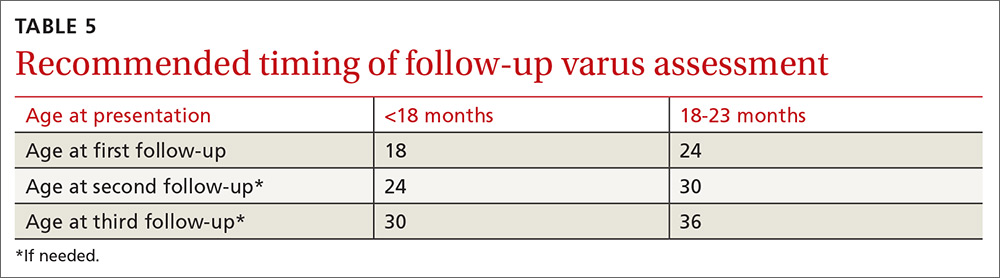
Re-examining the patient prior to the next well-child visit is unnecessary, as some degree of bowing is typical until age 18 to 24 months.1,6,7,9,12,13,17 Recommend orthopedic referral for any patient with varus that has progressed since initial presentation. Without signs of pathology, repeat varus assessment at the next well-child visit. This schedule minimizes the need for additional physician appointments by integrating follow-up into the typical well-child visits at 18, 24, 30, and 36 months of age.32 The 6-month follow-up interval was a feature of our study and is recommended in the related literature.12
- Consider orthopedic referral for patients whose varus has not corrected by the second follow-up appointment, as more than 95% of patients should have measurable varus correction at this visit. Most patients will have exhibited varus resolution by this time and will not require additional follow-up. For patients with observable correction who do not yet meet the criteria for resolution, we recommend a third, final follow-up appointment in another 6 months.
- Refer any patient whose varus has not resolved by the third follow-up appointment, as more than 95% of genu varum cases should have resolved by this time. This finding is echoed in the literature; any varus beyond 36 months of age is considered abnormal and suggestive of pathology.5,7,8,13,14 If evidence of Blount’s or skeletal dysplasia is identified, orthopedic management will likely consist of bracing (orthotics) or surgical management.
CORRESPONDENCE
Dennis S. Weiner, MD, Department of Orthopedic Surgery, Akron Children’s Hospital, 300 Locust Street, Suite 250, Akron, OH, 44302; [email protected].
ACKNOWLEDGEMENTS
The authors thank Meadow Newton, BS, assistant research coordinator, Akron Children’s Hospital, for her editing and technical assistance and Richard Steiner, PhD, The University of Akron, for his statistical review.
1. Weiner DS. Pediatric orthopedics for primary care physicians. 2nd ed. Jones K, ed. Cambridge, United Kingdom: Cambridge University Press; 2004.
2. Carli A, Saran N, Kruijt J, et al. Physiological referrals for paediatric musculoskeletal complaints: a costly problem that needs to be addressed. Paediatr Child Health. 2012;17:e93-e97.
3. Fabry G. Clinical practice. Static, axial, and rotational deformities of the lower extremities in children. Eur J Pediatr. 2010;169:529-534.
4. Davids JR, Blackhurst DW, Allen Jr BL. Clinical evaluation of bowed legs in children. J Pediatr Orthop B. 2000;9:278-284.
5. Bateson EM. The relationship between Blount’s disease and bow legs. Br J Radiol. 1968;41:107-114.
6. Weiner DS. The natural history of “bow legs” and “knock knees” in childhood. Orthopedics. 1981;4:156-160.
7. Greene WB. Genu varum and genu valgum in children: differential diagnosis and guidelines for evaluation. Compr Ther. 1996;22:22-29.
8. Do TT. Clinical and radiographic evaluation of bowlegs. Curr Opin Pediatr. 2001;13:42-46.
9. Bleck EE. Developmental orthopaedics. III: Toddlers. Dev Med Child Neurol. 1982;24:533-555.
10. Brooks WC, Gross RH. Genu Varum in Children: Diagnosis and Treatment. J Am Acad Orthop Surg. 1995;3:326-335.
11. Greenberg LA, Swartz AA. Genu varum and genu valgum. Another look. Am J Dis Child. 1971;121:219-221.
12. Scherl SA. Common lower extremity problems in children. Pediatr Rev. 2004;25:52-62.
13. Wall EJ. Practical primary pediatric orthopedics. Nurs Clin North Am. 2000;35:95-113.
14. Cheema JI, Grissom LE, Harcke HT. Radiographic characteristics of lower-extremity bowing in children. Radiographics. 2003;23:871-880.
15. McCarthy JJ, Betz RR, Kim A, et al. Early radiographic differentiation of infantile tibia vara from physiologic bowing using the femoral-tibial ratio. J Pediatr Orthop. 2001;21:545-548.
16. Salenius P, Vankka E. The development of the tibiofemoral angle in children. J Bone Joint Surg Am. 1975;57:259-261.
17. Engel GM, Staheli LT. The natural history of torsion and other factors influencing gait in childhood. A study of the angle of gait, tibial torsion, knee angle, hip rotation, and development of the arch in normal children. Clin Orthop Relat Res. 1974;99:12-17.
18. Golding J, Bateson E, McNeil-Smith G. Infantile tibia vara. In: The Growth Plate and Its Disorders. Rang M, ed. Baltimore, MD: Williams and Wilkins; 1969:109-119.
19. Greene WB. Infantile tibia vara. J Bone Joint Surg Am. 1993;75:130-143.
20. Golding J, McNeil-Smith JDG. Observations on the etiology of tibia vara. J Bone Joint Surg Br. 1963;45-B:320-325.
21. Eggert P, Viemann M. Physiological bowlegs or infantile Blount’s disease. Some new aspects on an old problem. Pediatr Radiol. 1996;26:349-352.
22. Levine AM, Drennan JC. Physiological bowing and tibia vara. The metaphyseal-diaphyseal angle in the measurement of bowleg deformities. J Bone Joint Surg Am. 1982;64:1158-1163.
23. Kessel L. Annotations on the etiology and treatment of tibia vara. J Bone Joint Surg Br. 1970;52:93-99.
24. Blount WP. Tibia vara: osteochondrosis deformans tibiae. J Bone Joint Surg Am. 1937;19:1-29.
25. Davids JR, Blackhurst DW, Allen BL Jr. Radiographic evaluation of bowed legs in children. J Pediatr Orthop. 2001;21:257-263.
26. Cook SD, Lavernia CJ, Burke SW, et al. A biomechanical analysis of the etiology of tibia vara. J Pediatr Orthop. 1983;3:449-454.
27. Birch JG. Blount disease. J Am Acad Orthop Surg. 2013;21:408-418.
28. Bateson EM. Non-rachitic bow leg and knock-knee deformities in young Jamaican children. Br J Radiol. 1966;39:92-101.
29. Grantham-McGregor SM, Back EH. Gross motor development in Jamaican infants. Dev Med Child Neurol. 1971;13:79-87.
30. Størvold GV, Aarethun K, Bratberg GH. Age for onset of walking and prewalking strategies. Early Hum Dev. 2013;89:655-659.
31. Garrett M, McElroy AM, Staines A. Locomotor milestones and babywalkers: cross sectional study. BMJ. 2002;324:1494.
32. Simon GR, Baker C, Barden GA 3rd, et al; Committee on Practice and Ambulatory Medicine, Curry ES, Dunca PM, Hagan JF Jr, et al; Bright Futures Periodicity Schedule Workgroup. 2014 recommendations for pediatric preventive health care. Pediatrics. 2014;133:568-570.
ABSTRACT
Objective To reduce unnecessary orthopedic referrals by developing a protocol for managing physiologic bow legs in the primary care environment through the use of a noninvasive technique that simultaneously tracks normal varus progression and screens for potential pathologic bowing requiring an orthopedic referral.
Methods Retrospective study of 155 patients with physiologic genu varum and 10 with infantile Blount’s disease. We used fingerbreadth measurements to document progression or resolution of bow legs. Final diagnoses were made by one orthopedic surgeon using clinical and radiographic evidence. We divided genu varum patients into 3 groups: patients presenting with bow legs before 18 months of age (MOA), patients presenting between 18 and 23 MOA, and patients presenting at 24 MOA or older for analyses relevant to the development of the follow-up protocol.
Results Physiologic genu varum patients walked earlier than average infants (10 months vs 12-15 months; P<.001). Physiologic genu varum patients presenting before 18 MOA demonstrated initial signs of correction between 18 and 24 MOA and resolution by 30 MOA. Physiologic genu varum patients presenting between 18 and 23 MOA demonstrated initial signs of correction between 24 MOA and 30 MOA and resolution by 36 MOA.
Conclusion Primary care physicians can manage most children presenting with bow legs. Management focuses on following the progression or resolution of varus with regular follow-up. For patients presenting with bow legs, we recommend a follow-up protocol using mainly well-child checkups and a simple clinical assessment to monitor varus progression and screen for pathologic bowing.
Bow legs in young children can be a concern for parents.1,2 By far, the most common reason for bow legs is physiologic genu varum,3-5 a nonprogressive stage of normal development in young children that generally resolves spontaneously without treatment.1,6-11 Normally developing children undergo a varus phase between birth and 18 to 24 months of age (MOA), at which time there is usually a transition in alignment from varus to straight to valgus (knock knees), which will correct to straight or mild valgus throughout adolescence.1,6,7,9,10,12-17
The most common form of pathologic bow legs is Blount’s disease, also known as tibia vara, which must be differentiated from physiologic genu varum.8-10,15,18-24 The progressive varus deformity of Blount’s disease usually requires orthopedic intervention.1,10,23-26 Early diagnosis may spare patients complex interventions, improve prognosis, and limit complications that include gait abnormalities,4,8,10,27 knee joint instability,4,24,27 osteoarthritis,9,20,27 meniscal tears,27 and degenerative joint disease.19,20,27
Although variables such as walking age, race, weight, and gender have been suggested as risk factors for Blount’s disease, they have not been useful in differentiating between Blount’s pathology and physiologic genu varum.1,4,5,7,10,20,28 In the primary care setting, distinguishing physiologic from pathologic forms of bow legs is possible with a thorough history and physical exam and with radiographs, as warranted.1,2,15 More than 40% of genu varum/genu valgum cases referred for orthopedic consultation turn out to be the physiologic form,2 suggesting a need for guidelines in the primary care setting to help direct referral and follow-up. The purpose of this study was to provide recommendations to family physicians for evaluating and managing children with bow legs.
Materials and methods
This study, approved by the Internal Review Board of Akron Children’s Hospital, is a retrospective review of children seen by a single pediatric orthopedic surgeon (DSW) from 1970 to 2012. Four-hundred twenty-four children were received for evaluation of bow legs. Excluded from our final analysis were 220 subjects seen only once for this specific referral and 39 subjects diagnosed with a condition other than genu varum or Blount’s disease (ie, rickets, skeletal dysplasia, sequelae of trauma, or infection). Ten subjects with Blount’s disease and 155 subjects with physiologic genu varum were included in the final data analysis.
In addition to noting the age at which a patient walked independently, at each visit we documented age and the fingerbreadth (varus) distance between the medial femoral condyles with the child’s ankles held together. Parents reported age of independent walking for just 3 children with Blount’s disease and for 134 children with physiologic genu varum. Study variables for the genu varum data analysis were age of walking, age at presentation, age at varus correction, age at varus resolution, time between presentation and varus correction, and time between presentation and varus resolution. Varus correction is defined as any decrease in varus angulation since presentation. Varus resolution is defined as varus correction to less than or equal to half of the varus angulation at presentation. For inclusion in the age-at-resolution analysis, a child must have been evaluated at regular follow-up visits (all rechecks within 8 months).
To measure varus distance, we used the fingerbreadth method described by Weiner in a study of 600 cases (FIGURE).6 This simple technique, which requires no special equipment, accurately detected differences in varus angulation and tracked the normal pattern of lower limb angular development. The patient should be supine on the examination table with legs extended. With one hand, the examiner holds the child’s ankles together, ensuring the medial malleoli are in contact. With the other hand, the examiner measures the fingerbreadth distance between the medial femoral condyles. Alternatively, a ruler may be used to measure the distance. This latter method may be especially useful in practices where the patient is likely to see more than one provider for well child care.
We divided the genu varum subject group into 3 subgroups by age at presentation: 103 subjects were younger than 18 months; 47 were 18 to 23 months; and 5 were 24 months or older. We used the data analysis toolkit in Microsoft Excel 2013 to perform a statistical analysis of study variables. We assumed the genu varum population is a normally distributed population. We used a 95% confidence level (α=0.05) for all calculations of confidence intervals (CIs), student t-tests, and tolerance intervals. Based on the data analysis results, we developed a series of follow-up and referral guidelines for practitioners.
Results
The mean walking age for those diagnosed with physiologic genu varum was 10 months (95% CI, 9.8-10.4), which is significantly younger than the 12 months of age (at the earliest) typical of toddlers in general (P<.001). There was no significant difference between the walking age of male and female children diagnosed with genu varum (P=.37).
Of the children presenting with the primary complaint of bow legs, 6% subsequently developed Blount’s disease. These patients presented at a mean age of 20.9 months and were diagnosed at a mean age of 23.9 months. Following the Blount’s disease diagnosis, we initiated therapy in all cases (3 surgical, 7 bracing).
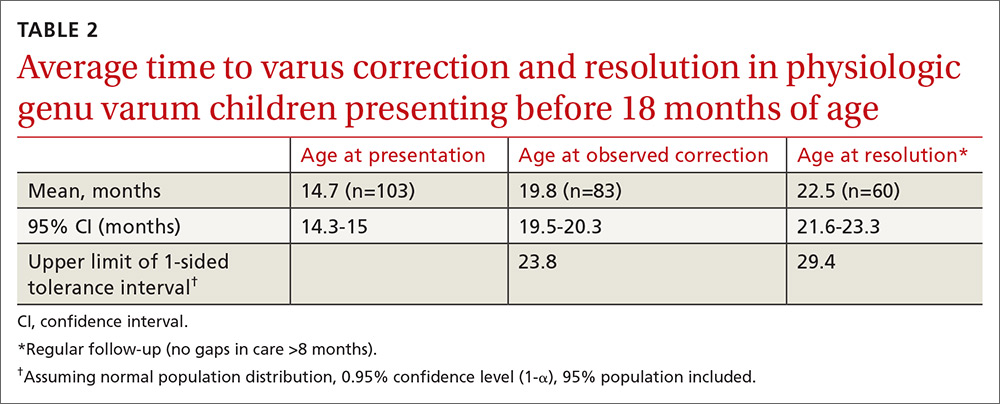
Physiologic genu varum patients presented at a mean age of 16.4 months, with only 3.23% presenting at older than 23 months. On average, physiologic genu varum patients presenting before 24 months of age showed measurable varus correction 5 months after presentation and achieved varus resolution 7.3 months after presentation (TABLE 1). Assuming the patient population is normally distributed, we can be 95% confident that 95% of physiologic genu varum patients presenting before 18 months of age will show measurable varus correction by 24 months and will resolve without intervention by 30 months (TABLE 2). Patients presenting between 18 and 23 months of age should show measurable varus correction by 30 months and resolution by 36 months (TABLE 3).
Discussion
Primary care physicians have the ability to differentiate physiologic genu varum from pathologic forms of bow legs with a thorough history, physical exam, and radiographic examination, if necessary1,2,13 (TABLE 41,7,8,10,12,14,18-20,22,24,27). Several approaches to differentiating Blount’s disease and physiologic genu varum have been described in the literature.1,4,7,8,10,14,22,23
The average age at which children begin to walk independently is between 13 and 15 months.5,18,29-31 Recently, it has been suggested that the range be expanded to include 12 months of age.30 The association between early walking (at 10-11 months)12,20,22 and Blount’s disease is generally accepted in the orthopedic literature.1,4,7,10,19-22 However, some authors have suggested early walking also contributes to genu varum.1,5,8,10,18,28 The mean age of independent walking for children with physiologic genu varum suggested in the literature (10 months) was confirmed in our study and found to be significantly younger than the average for toddlers generally.1,22 Early walking is clearly associated with both physiologic genu varum and Blount’s disease, but no direct causation has been identified in either case. An alternative means of differentiating these entities is needed.
Radiographic examination of the knee is essential to the diagnosis of Blount’s disease as well as other, less common causes of pathologic bow legs (skeletal dysplasia, rickets, traumatic growth plate insults, infections, neoplasms).1,8,14,19 The common radiologic classification of staging for Blount’s disease is the Langenskiöld staging system, which involves identification of characteristic radiographic changes at the tibial physis.5,8,14,15,18,22,24
Sequential measurement of genu varum is most useful in differentiating between physiologic and pathologic processes. Physiologic genu varum, an exaggeration of the normal developmental pattern, characteristically resolves and evolves into physiologic genu valgum by 3 years of age.1,6-11 The pathophysiology of Blount’s disease is believed to be related to biomechanical overloading of the posteromedial proximal tibia during gait with the knee in a varus orientation. Excess loading on the proximal medial physis contributes to varus progression.4,10,14,20,25,27 Patients with Blount’s disease progress with varus and concomitant internal tibial torsion associated with growth plate irregularities and eventually exhibit premature closure.1,10,14,18,20,23,24,26 In the months prior to Blount’s disease diagnosis, increasing varus has been reported.4,7,10,19 Varus progression that differs from the expected pattern indicates possible pathologic bow legs and should prompt radiologic evaluation and, often, an orthopedic referral.3,4,7-9,12,13,21
In our study, only 3% of children with physiologic genu varum presented at 24 months of age or older, compared with 20% of Blount’s disease patients. We recommend considering orthopedic referral for any patient presenting with bow legs at 24 months of age or older. Additionally, consider orthopedic referral for any patient whose varus has not begun to correct within 8 months or has not resolved within 14 months of presentation, as more than 95% of patients with physiologic genu varum are expected to meet these milestones (TABLE 1). And do not hesitate to refer patients at any stage of follow-up if you suspect pathology or if parents are anxious.
If no sign of pathology is immediately identified, we recommend the following course of action:
- Record a reference fingerbreadth or ruler measurement at the initial presentation.
- Re-examine the knee varus at the next regular well-child visit (TABLE 5).
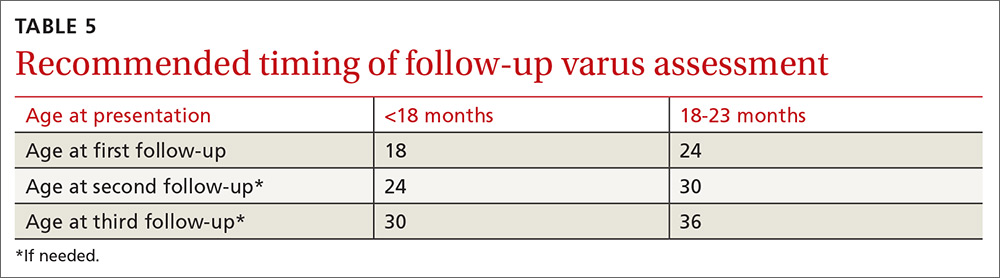
Re-examining the patient prior to the next well-child visit is unnecessary, as some degree of bowing is typical until age 18 to 24 months.1,6,7,9,12,13,17 Recommend orthopedic referral for any patient with varus that has progressed since initial presentation. Without signs of pathology, repeat varus assessment at the next well-child visit. This schedule minimizes the need for additional physician appointments by integrating follow-up into the typical well-child visits at 18, 24, 30, and 36 months of age.32 The 6-month follow-up interval was a feature of our study and is recommended in the related literature.12
- Consider orthopedic referral for patients whose varus has not corrected by the second follow-up appointment, as more than 95% of patients should have measurable varus correction at this visit. Most patients will have exhibited varus resolution by this time and will not require additional follow-up. For patients with observable correction who do not yet meet the criteria for resolution, we recommend a third, final follow-up appointment in another 6 months.
- Refer any patient whose varus has not resolved by the third follow-up appointment, as more than 95% of genu varum cases should have resolved by this time. This finding is echoed in the literature; any varus beyond 36 months of age is considered abnormal and suggestive of pathology.5,7,8,13,14 If evidence of Blount’s or skeletal dysplasia is identified, orthopedic management will likely consist of bracing (orthotics) or surgical management.
CORRESPONDENCE
Dennis S. Weiner, MD, Department of Orthopedic Surgery, Akron Children’s Hospital, 300 Locust Street, Suite 250, Akron, OH, 44302; [email protected].
ACKNOWLEDGEMENTS
The authors thank Meadow Newton, BS, assistant research coordinator, Akron Children’s Hospital, for her editing and technical assistance and Richard Steiner, PhD, The University of Akron, for his statistical review.
ABSTRACT
Objective To reduce unnecessary orthopedic referrals by developing a protocol for managing physiologic bow legs in the primary care environment through the use of a noninvasive technique that simultaneously tracks normal varus progression and screens for potential pathologic bowing requiring an orthopedic referral.
Methods Retrospective study of 155 patients with physiologic genu varum and 10 with infantile Blount’s disease. We used fingerbreadth measurements to document progression or resolution of bow legs. Final diagnoses were made by one orthopedic surgeon using clinical and radiographic evidence. We divided genu varum patients into 3 groups: patients presenting with bow legs before 18 months of age (MOA), patients presenting between 18 and 23 MOA, and patients presenting at 24 MOA or older for analyses relevant to the development of the follow-up protocol.
Results Physiologic genu varum patients walked earlier than average infants (10 months vs 12-15 months; P<.001). Physiologic genu varum patients presenting before 18 MOA demonstrated initial signs of correction between 18 and 24 MOA and resolution by 30 MOA. Physiologic genu varum patients presenting between 18 and 23 MOA demonstrated initial signs of correction between 24 MOA and 30 MOA and resolution by 36 MOA.
Conclusion Primary care physicians can manage most children presenting with bow legs. Management focuses on following the progression or resolution of varus with regular follow-up. For patients presenting with bow legs, we recommend a follow-up protocol using mainly well-child checkups and a simple clinical assessment to monitor varus progression and screen for pathologic bowing.
Bow legs in young children can be a concern for parents.1,2 By far, the most common reason for bow legs is physiologic genu varum,3-5 a nonprogressive stage of normal development in young children that generally resolves spontaneously without treatment.1,6-11 Normally developing children undergo a varus phase between birth and 18 to 24 months of age (MOA), at which time there is usually a transition in alignment from varus to straight to valgus (knock knees), which will correct to straight or mild valgus throughout adolescence.1,6,7,9,10,12-17
The most common form of pathologic bow legs is Blount’s disease, also known as tibia vara, which must be differentiated from physiologic genu varum.8-10,15,18-24 The progressive varus deformity of Blount’s disease usually requires orthopedic intervention.1,10,23-26 Early diagnosis may spare patients complex interventions, improve prognosis, and limit complications that include gait abnormalities,4,8,10,27 knee joint instability,4,24,27 osteoarthritis,9,20,27 meniscal tears,27 and degenerative joint disease.19,20,27
Although variables such as walking age, race, weight, and gender have been suggested as risk factors for Blount’s disease, they have not been useful in differentiating between Blount’s pathology and physiologic genu varum.1,4,5,7,10,20,28 In the primary care setting, distinguishing physiologic from pathologic forms of bow legs is possible with a thorough history and physical exam and with radiographs, as warranted.1,2,15 More than 40% of genu varum/genu valgum cases referred for orthopedic consultation turn out to be the physiologic form,2 suggesting a need for guidelines in the primary care setting to help direct referral and follow-up. The purpose of this study was to provide recommendations to family physicians for evaluating and managing children with bow legs.
Materials and methods
This study, approved by the Internal Review Board of Akron Children’s Hospital, is a retrospective review of children seen by a single pediatric orthopedic surgeon (DSW) from 1970 to 2012. Four-hundred twenty-four children were received for evaluation of bow legs. Excluded from our final analysis were 220 subjects seen only once for this specific referral and 39 subjects diagnosed with a condition other than genu varum or Blount’s disease (ie, rickets, skeletal dysplasia, sequelae of trauma, or infection). Ten subjects with Blount’s disease and 155 subjects with physiologic genu varum were included in the final data analysis.
In addition to noting the age at which a patient walked independently, at each visit we documented age and the fingerbreadth (varus) distance between the medial femoral condyles with the child’s ankles held together. Parents reported age of independent walking for just 3 children with Blount’s disease and for 134 children with physiologic genu varum. Study variables for the genu varum data analysis were age of walking, age at presentation, age at varus correction, age at varus resolution, time between presentation and varus correction, and time between presentation and varus resolution. Varus correction is defined as any decrease in varus angulation since presentation. Varus resolution is defined as varus correction to less than or equal to half of the varus angulation at presentation. For inclusion in the age-at-resolution analysis, a child must have been evaluated at regular follow-up visits (all rechecks within 8 months).
To measure varus distance, we used the fingerbreadth method described by Weiner in a study of 600 cases (FIGURE).6 This simple technique, which requires no special equipment, accurately detected differences in varus angulation and tracked the normal pattern of lower limb angular development. The patient should be supine on the examination table with legs extended. With one hand, the examiner holds the child’s ankles together, ensuring the medial malleoli are in contact. With the other hand, the examiner measures the fingerbreadth distance between the medial femoral condyles. Alternatively, a ruler may be used to measure the distance. This latter method may be especially useful in practices where the patient is likely to see more than one provider for well child care.
We divided the genu varum subject group into 3 subgroups by age at presentation: 103 subjects were younger than 18 months; 47 were 18 to 23 months; and 5 were 24 months or older. We used the data analysis toolkit in Microsoft Excel 2013 to perform a statistical analysis of study variables. We assumed the genu varum population is a normally distributed population. We used a 95% confidence level (α=0.05) for all calculations of confidence intervals (CIs), student t-tests, and tolerance intervals. Based on the data analysis results, we developed a series of follow-up and referral guidelines for practitioners.
Results
The mean walking age for those diagnosed with physiologic genu varum was 10 months (95% CI, 9.8-10.4), which is significantly younger than the 12 months of age (at the earliest) typical of toddlers in general (P<.001). There was no significant difference between the walking age of male and female children diagnosed with genu varum (P=.37).
Of the children presenting with the primary complaint of bow legs, 6% subsequently developed Blount’s disease. These patients presented at a mean age of 20.9 months and were diagnosed at a mean age of 23.9 months. Following the Blount’s disease diagnosis, we initiated therapy in all cases (3 surgical, 7 bracing).
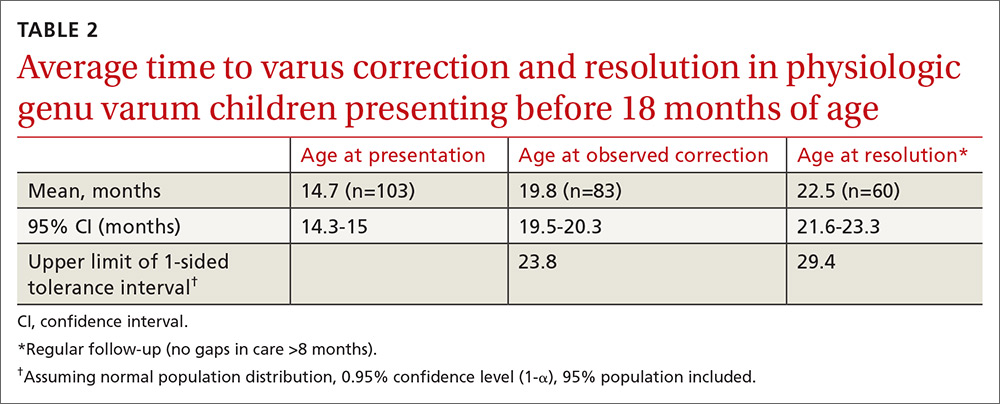
Physiologic genu varum patients presented at a mean age of 16.4 months, with only 3.23% presenting at older than 23 months. On average, physiologic genu varum patients presenting before 24 months of age showed measurable varus correction 5 months after presentation and achieved varus resolution 7.3 months after presentation (TABLE 1). Assuming the patient population is normally distributed, we can be 95% confident that 95% of physiologic genu varum patients presenting before 18 months of age will show measurable varus correction by 24 months and will resolve without intervention by 30 months (TABLE 2). Patients presenting between 18 and 23 months of age should show measurable varus correction by 30 months and resolution by 36 months (TABLE 3).
Discussion
Primary care physicians have the ability to differentiate physiologic genu varum from pathologic forms of bow legs with a thorough history, physical exam, and radiographic examination, if necessary1,2,13 (TABLE 41,7,8,10,12,14,18-20,22,24,27). Several approaches to differentiating Blount’s disease and physiologic genu varum have been described in the literature.1,4,7,8,10,14,22,23
The average age at which children begin to walk independently is between 13 and 15 months.5,18,29-31 Recently, it has been suggested that the range be expanded to include 12 months of age.30 The association between early walking (at 10-11 months)12,20,22 and Blount’s disease is generally accepted in the orthopedic literature.1,4,7,10,19-22 However, some authors have suggested early walking also contributes to genu varum.1,5,8,10,18,28 The mean age of independent walking for children with physiologic genu varum suggested in the literature (10 months) was confirmed in our study and found to be significantly younger than the average for toddlers generally.1,22 Early walking is clearly associated with both physiologic genu varum and Blount’s disease, but no direct causation has been identified in either case. An alternative means of differentiating these entities is needed.
Radiographic examination of the knee is essential to the diagnosis of Blount’s disease as well as other, less common causes of pathologic bow legs (skeletal dysplasia, rickets, traumatic growth plate insults, infections, neoplasms).1,8,14,19 The common radiologic classification of staging for Blount’s disease is the Langenskiöld staging system, which involves identification of characteristic radiographic changes at the tibial physis.5,8,14,15,18,22,24
Sequential measurement of genu varum is most useful in differentiating between physiologic and pathologic processes. Physiologic genu varum, an exaggeration of the normal developmental pattern, characteristically resolves and evolves into physiologic genu valgum by 3 years of age.1,6-11 The pathophysiology of Blount’s disease is believed to be related to biomechanical overloading of the posteromedial proximal tibia during gait with the knee in a varus orientation. Excess loading on the proximal medial physis contributes to varus progression.4,10,14,20,25,27 Patients with Blount’s disease progress with varus and concomitant internal tibial torsion associated with growth plate irregularities and eventually exhibit premature closure.1,10,14,18,20,23,24,26 In the months prior to Blount’s disease diagnosis, increasing varus has been reported.4,7,10,19 Varus progression that differs from the expected pattern indicates possible pathologic bow legs and should prompt radiologic evaluation and, often, an orthopedic referral.3,4,7-9,12,13,21
In our study, only 3% of children with physiologic genu varum presented at 24 months of age or older, compared with 20% of Blount’s disease patients. We recommend considering orthopedic referral for any patient presenting with bow legs at 24 months of age or older. Additionally, consider orthopedic referral for any patient whose varus has not begun to correct within 8 months or has not resolved within 14 months of presentation, as more than 95% of patients with physiologic genu varum are expected to meet these milestones (TABLE 1). And do not hesitate to refer patients at any stage of follow-up if you suspect pathology or if parents are anxious.
If no sign of pathology is immediately identified, we recommend the following course of action:
- Record a reference fingerbreadth or ruler measurement at the initial presentation.
- Re-examine the knee varus at the next regular well-child visit (TABLE 5).
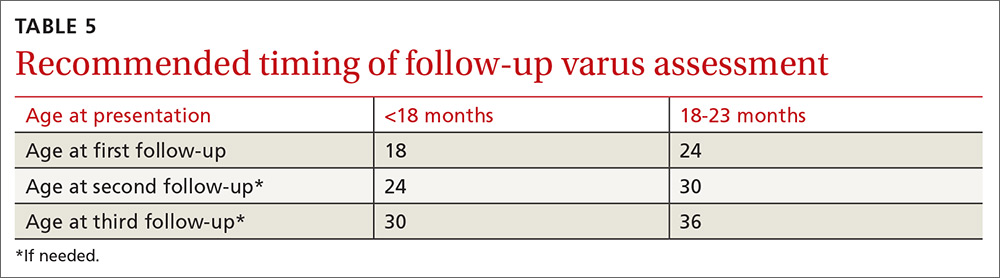
Re-examining the patient prior to the next well-child visit is unnecessary, as some degree of bowing is typical until age 18 to 24 months.1,6,7,9,12,13,17 Recommend orthopedic referral for any patient with varus that has progressed since initial presentation. Without signs of pathology, repeat varus assessment at the next well-child visit. This schedule minimizes the need for additional physician appointments by integrating follow-up into the typical well-child visits at 18, 24, 30, and 36 months of age.32 The 6-month follow-up interval was a feature of our study and is recommended in the related literature.12
- Consider orthopedic referral for patients whose varus has not corrected by the second follow-up appointment, as more than 95% of patients should have measurable varus correction at this visit. Most patients will have exhibited varus resolution by this time and will not require additional follow-up. For patients with observable correction who do not yet meet the criteria for resolution, we recommend a third, final follow-up appointment in another 6 months.
- Refer any patient whose varus has not resolved by the third follow-up appointment, as more than 95% of genu varum cases should have resolved by this time. This finding is echoed in the literature; any varus beyond 36 months of age is considered abnormal and suggestive of pathology.5,7,8,13,14 If evidence of Blount’s or skeletal dysplasia is identified, orthopedic management will likely consist of bracing (orthotics) or surgical management.
CORRESPONDENCE
Dennis S. Weiner, MD, Department of Orthopedic Surgery, Akron Children’s Hospital, 300 Locust Street, Suite 250, Akron, OH, 44302; [email protected].
ACKNOWLEDGEMENTS
The authors thank Meadow Newton, BS, assistant research coordinator, Akron Children’s Hospital, for her editing and technical assistance and Richard Steiner, PhD, The University of Akron, for his statistical review.
1. Weiner DS. Pediatric orthopedics for primary care physicians. 2nd ed. Jones K, ed. Cambridge, United Kingdom: Cambridge University Press; 2004.
2. Carli A, Saran N, Kruijt J, et al. Physiological referrals for paediatric musculoskeletal complaints: a costly problem that needs to be addressed. Paediatr Child Health. 2012;17:e93-e97.
3. Fabry G. Clinical practice. Static, axial, and rotational deformities of the lower extremities in children. Eur J Pediatr. 2010;169:529-534.
4. Davids JR, Blackhurst DW, Allen Jr BL. Clinical evaluation of bowed legs in children. J Pediatr Orthop B. 2000;9:278-284.
5. Bateson EM. The relationship between Blount’s disease and bow legs. Br J Radiol. 1968;41:107-114.
6. Weiner DS. The natural history of “bow legs” and “knock knees” in childhood. Orthopedics. 1981;4:156-160.
7. Greene WB. Genu varum and genu valgum in children: differential diagnosis and guidelines for evaluation. Compr Ther. 1996;22:22-29.
8. Do TT. Clinical and radiographic evaluation of bowlegs. Curr Opin Pediatr. 2001;13:42-46.
9. Bleck EE. Developmental orthopaedics. III: Toddlers. Dev Med Child Neurol. 1982;24:533-555.
10. Brooks WC, Gross RH. Genu Varum in Children: Diagnosis and Treatment. J Am Acad Orthop Surg. 1995;3:326-335.
11. Greenberg LA, Swartz AA. Genu varum and genu valgum. Another look. Am J Dis Child. 1971;121:219-221.
12. Scherl SA. Common lower extremity problems in children. Pediatr Rev. 2004;25:52-62.
13. Wall EJ. Practical primary pediatric orthopedics. Nurs Clin North Am. 2000;35:95-113.
14. Cheema JI, Grissom LE, Harcke HT. Radiographic characteristics of lower-extremity bowing in children. Radiographics. 2003;23:871-880.
15. McCarthy JJ, Betz RR, Kim A, et al. Early radiographic differentiation of infantile tibia vara from physiologic bowing using the femoral-tibial ratio. J Pediatr Orthop. 2001;21:545-548.
16. Salenius P, Vankka E. The development of the tibiofemoral angle in children. J Bone Joint Surg Am. 1975;57:259-261.
17. Engel GM, Staheli LT. The natural history of torsion and other factors influencing gait in childhood. A study of the angle of gait, tibial torsion, knee angle, hip rotation, and development of the arch in normal children. Clin Orthop Relat Res. 1974;99:12-17.
18. Golding J, Bateson E, McNeil-Smith G. Infantile tibia vara. In: The Growth Plate and Its Disorders. Rang M, ed. Baltimore, MD: Williams and Wilkins; 1969:109-119.
19. Greene WB. Infantile tibia vara. J Bone Joint Surg Am. 1993;75:130-143.
20. Golding J, McNeil-Smith JDG. Observations on the etiology of tibia vara. J Bone Joint Surg Br. 1963;45-B:320-325.
21. Eggert P, Viemann M. Physiological bowlegs or infantile Blount’s disease. Some new aspects on an old problem. Pediatr Radiol. 1996;26:349-352.
22. Levine AM, Drennan JC. Physiological bowing and tibia vara. The metaphyseal-diaphyseal angle in the measurement of bowleg deformities. J Bone Joint Surg Am. 1982;64:1158-1163.
23. Kessel L. Annotations on the etiology and treatment of tibia vara. J Bone Joint Surg Br. 1970;52:93-99.
24. Blount WP. Tibia vara: osteochondrosis deformans tibiae. J Bone Joint Surg Am. 1937;19:1-29.
25. Davids JR, Blackhurst DW, Allen BL Jr. Radiographic evaluation of bowed legs in children. J Pediatr Orthop. 2001;21:257-263.
26. Cook SD, Lavernia CJ, Burke SW, et al. A biomechanical analysis of the etiology of tibia vara. J Pediatr Orthop. 1983;3:449-454.
27. Birch JG. Blount disease. J Am Acad Orthop Surg. 2013;21:408-418.
28. Bateson EM. Non-rachitic bow leg and knock-knee deformities in young Jamaican children. Br J Radiol. 1966;39:92-101.
29. Grantham-McGregor SM, Back EH. Gross motor development in Jamaican infants. Dev Med Child Neurol. 1971;13:79-87.
30. Størvold GV, Aarethun K, Bratberg GH. Age for onset of walking and prewalking strategies. Early Hum Dev. 2013;89:655-659.
31. Garrett M, McElroy AM, Staines A. Locomotor milestones and babywalkers: cross sectional study. BMJ. 2002;324:1494.
32. Simon GR, Baker C, Barden GA 3rd, et al; Committee on Practice and Ambulatory Medicine, Curry ES, Dunca PM, Hagan JF Jr, et al; Bright Futures Periodicity Schedule Workgroup. 2014 recommendations for pediatric preventive health care. Pediatrics. 2014;133:568-570.
1. Weiner DS. Pediatric orthopedics for primary care physicians. 2nd ed. Jones K, ed. Cambridge, United Kingdom: Cambridge University Press; 2004.
2. Carli A, Saran N, Kruijt J, et al. Physiological referrals for paediatric musculoskeletal complaints: a costly problem that needs to be addressed. Paediatr Child Health. 2012;17:e93-e97.
3. Fabry G. Clinical practice. Static, axial, and rotational deformities of the lower extremities in children. Eur J Pediatr. 2010;169:529-534.
4. Davids JR, Blackhurst DW, Allen Jr BL. Clinical evaluation of bowed legs in children. J Pediatr Orthop B. 2000;9:278-284.
5. Bateson EM. The relationship between Blount’s disease and bow legs. Br J Radiol. 1968;41:107-114.
6. Weiner DS. The natural history of “bow legs” and “knock knees” in childhood. Orthopedics. 1981;4:156-160.
7. Greene WB. Genu varum and genu valgum in children: differential diagnosis and guidelines for evaluation. Compr Ther. 1996;22:22-29.
8. Do TT. Clinical and radiographic evaluation of bowlegs. Curr Opin Pediatr. 2001;13:42-46.
9. Bleck EE. Developmental orthopaedics. III: Toddlers. Dev Med Child Neurol. 1982;24:533-555.
10. Brooks WC, Gross RH. Genu Varum in Children: Diagnosis and Treatment. J Am Acad Orthop Surg. 1995;3:326-335.
11. Greenberg LA, Swartz AA. Genu varum and genu valgum. Another look. Am J Dis Child. 1971;121:219-221.
12. Scherl SA. Common lower extremity problems in children. Pediatr Rev. 2004;25:52-62.
13. Wall EJ. Practical primary pediatric orthopedics. Nurs Clin North Am. 2000;35:95-113.
14. Cheema JI, Grissom LE, Harcke HT. Radiographic characteristics of lower-extremity bowing in children. Radiographics. 2003;23:871-880.
15. McCarthy JJ, Betz RR, Kim A, et al. Early radiographic differentiation of infantile tibia vara from physiologic bowing using the femoral-tibial ratio. J Pediatr Orthop. 2001;21:545-548.
16. Salenius P, Vankka E. The development of the tibiofemoral angle in children. J Bone Joint Surg Am. 1975;57:259-261.
17. Engel GM, Staheli LT. The natural history of torsion and other factors influencing gait in childhood. A study of the angle of gait, tibial torsion, knee angle, hip rotation, and development of the arch in normal children. Clin Orthop Relat Res. 1974;99:12-17.
18. Golding J, Bateson E, McNeil-Smith G. Infantile tibia vara. In: The Growth Plate and Its Disorders. Rang M, ed. Baltimore, MD: Williams and Wilkins; 1969:109-119.
19. Greene WB. Infantile tibia vara. J Bone Joint Surg Am. 1993;75:130-143.
20. Golding J, McNeil-Smith JDG. Observations on the etiology of tibia vara. J Bone Joint Surg Br. 1963;45-B:320-325.
21. Eggert P, Viemann M. Physiological bowlegs or infantile Blount’s disease. Some new aspects on an old problem. Pediatr Radiol. 1996;26:349-352.
22. Levine AM, Drennan JC. Physiological bowing and tibia vara. The metaphyseal-diaphyseal angle in the measurement of bowleg deformities. J Bone Joint Surg Am. 1982;64:1158-1163.
23. Kessel L. Annotations on the etiology and treatment of tibia vara. J Bone Joint Surg Br. 1970;52:93-99.
24. Blount WP. Tibia vara: osteochondrosis deformans tibiae. J Bone Joint Surg Am. 1937;19:1-29.
25. Davids JR, Blackhurst DW, Allen BL Jr. Radiographic evaluation of bowed legs in children. J Pediatr Orthop. 2001;21:257-263.
26. Cook SD, Lavernia CJ, Burke SW, et al. A biomechanical analysis of the etiology of tibia vara. J Pediatr Orthop. 1983;3:449-454.
27. Birch JG. Blount disease. J Am Acad Orthop Surg. 2013;21:408-418.
28. Bateson EM. Non-rachitic bow leg and knock-knee deformities in young Jamaican children. Br J Radiol. 1966;39:92-101.
29. Grantham-McGregor SM, Back EH. Gross motor development in Jamaican infants. Dev Med Child Neurol. 1971;13:79-87.
30. Størvold GV, Aarethun K, Bratberg GH. Age for onset of walking and prewalking strategies. Early Hum Dev. 2013;89:655-659.
31. Garrett M, McElroy AM, Staines A. Locomotor milestones and babywalkers: cross sectional study. BMJ. 2002;324:1494.
32. Simon GR, Baker C, Barden GA 3rd, et al; Committee on Practice and Ambulatory Medicine, Curry ES, Dunca PM, Hagan JF Jr, et al; Bright Futures Periodicity Schedule Workgroup. 2014 recommendations for pediatric preventive health care. Pediatrics. 2014;133:568-570.
Calcaneal apophysitis: Simple diagnosis, simpler treatment
- The true origin of the heel pain of calcaneal apophysitis is a stress microfracture (invisible on x-ray) due to chronic repetitive microtrauma—it’s an overuse syndrome that resolves without surgery in nearly all cases. (C)
- Most patients experience pain relief and can resume full activities while using a simple in-shoe wedge-shaped orthotic. (C)
- The most distinguishing feature on physical exam is the exquisite heel pain produced by lateral and medial compression (“squeezing”) of the heel. (C)
Strength of recommendation (SOR)
- Good quality patient-oriented evidence
- Inconsistent or limited-quality patient-oriented evidence
- Consensus, usual practice, opinion, disease-oriented evidence, case series
Two things about calcaneal “apophysitis” are a bit misleading. The first is its name. Although this common cause of heel pain in adolescents and teenagers was once considered a true osteochondritis, we now know that it’s actually a mechanical overuse pain syndrome with a self-limited, benign prognosis.1-3 The second area of confusion is what you’ll see on x-ray: an increased density and irregular fragmentation that was once viewed with suspicion, but is actually a normal pattern of ossification for this particular apophysis.
Don’t let the x-ray fool you
Primary care physicians can properly manage this common pain condition, given an understanding of the features, natural history, and treatment principles presented here.
Orthopedic referral is indicated for only a few recalcitrant cases.
Shoes aren’t to blame, but activity level is
Adolescents with calcaneal apophysitis—also known as Sever’s disease—will typically come into the office complaining of pain, often in both heels, particularly with mechanical activities such as running, jumping, and long-distance walking. Patients may walk on tiptoe to avoid the pain.4
The condition is common in both boys and girls, although personal experience indicates it’s more common in boys. The typical age of the patient is 8 to 15 years. The condition is most commonly seen in patients who are engaged in athletic endeavors,5,6 including soccer, basketball, and gymnastics,7,8 though no specific athletic endeavor has been directly implicated in the pathogenesis. Likewise, no specific foot structure or type of shoe wear has been directly related to the symptomatology.
An otherwise healthy boy, age 12, walks into your office—on tiptoe. His problem is pain in both heels, especially when running. It’s his first season on his school track team, and he says he’s been practicing hard for the 50-yard dash, “my best event.” his parents express to you their concern about possible sports-related injuries or underlying disease, and their son’s distress about the possibilty of “letting down the team” if he quits. You find no swelling, no skin changes, no erythema, and no other local abnormalities. Symptoms of marked pain are produced by medial and lateral compression (squeezing) of the heel at the site where the calcaneal apophysis attaches to the main body of the os calcis. There is no pain on plantar, posterior, or retrocalcaneal pressure, or adjacent to the Achilles tendon.
Exquisite heel pain produced by medial and lateral compression of the heel is the most distinguishing feature of calcaneal apophysitis
Is this x-ray normal? You order a lateral x-ray of the calcaneus to exclude other pathology. You observe a pattern of increased density and apparent irregular fragmentation on the x-ray. The radiologist reports no abnormal findings. The above x-ray typifies calcaneal apophysitis, an overuse syndrome often seen in children 8 to 15 years of age. The “dense” area is actually a secondary ossification center of the calcaneus, not an indication of pathology.
The ossification of the calcaneus is different from that of the tarsal bones, which are each ossified from a single center. In the case of the calcaneus, a secondary center of ossification typically appears in girls by age 6, and in boys by age 8.14,15 During adolescence, a C-shaped cartilage develops between the metaphyseal bone of the body of the calcaneus and the secondary center (or centers) of ossification. Then, at around age 10 or 11, a more superior tertiary ossification center appears in the apophysis of the calcaneus.
As the calcaneal apophysis progressively ossifies, it presents as a very dense radiographic pattern in an adolescent. For years, this was thought to represent a form of osteochondritis.16 In fact, this is a normal pattern of ossification for this particular apophysis.17-22
What do you tell the patient and parents? You advise an in-shoe orthotic, no limits on physical activity, and no surgery. You explain that the pain is due to recurrent impact (overuse), and that the orthotic will “unload” the heel and permit symtoms to resolve, typically within 60 days. If asked about discomfort, you may advise anti-inflammatories and ice/heat.
Patients typically have no swelling, skin changes, erythema, or other local abnormalities.8 The most characteristic distinguishing feature on physical examination is exquisite pain produced on medial and lateral compression (“squeezing”) of the heel at the site where the calcaneal apophysis attaches to the main body of the os calcis. The pain is not on plantar pressure (as you would see with plantar fasciitis), or posterior, retrocalcaneal, or adjacent to the Achilles tendon (as you would see on Achilles tendinitis), but on medial and lateral compression.3
I’ve noticed a number of trends over the years while caring for patients with calcaneal apophysitis. My chart review of the 227 patients I cared for between 1971 and 1997 revealed the following:
- 60% (137) of patients had bilateral involvement.
- 78% of the patients were male. The reason for the male preponderance remains unclear.
- All but 3 of the 364 feet obtained eventual complete symptom resolution with the prescribed sponge-leather heel orthotic.
- Symptoms typically resolved within 60 days.
- The 3 cases that were recalcitrant to orthotic treatment required an equinus-type cast for 4 to 6 weeks. Those patients treated with a cast also had resolution of their symptoms.
- Roughly 30% of the cases encountered a recurrence of symptoms with similar resolution with the previously described retreatment. Recurrences were unrelated to gender.
- No case ever required any other treatment type beyond the orthotic or cast.—Dennis Weiner, MD
Researchers found microfractures. Magnetic resonance imaging (MRI) evidence suggests that the true pathogenesis of calcaneal apophysitis is a stress microfracture related to chronic repetitive microtrauma.9 In addition, MRI evidence suggests that the location of the stress microfractures is in the metaphysis of the body of the calcaneus adjacent to—but not directly involving—the apophysis.1,7 This more recent evidence replaces the historical hypotheses that the condition is primarily an inflammatory process. As a consequence of the microtrauma, however, it’s possible that an inflammatory process may occur secondarily.
Should you order x-rays? X-rays are not essential to the diagnosis, though they may be used to rule out other conditions, such as fracture, infection, or a bone cyst. Keep in mind, though, that patients with calcaneal pain will have a normal x-ray.7 What is normal, however, is another matter, and has been the subject of confusion in the past.
Pain stops in a few weeks
Usually, the symptoms of calcaneal apophysitis resolve fairly quickly, and with relatively simple treatment. (The symptoms also disappear as the child gets older and the calcaneal apophysis amalgamates with the main body of the calcaneus.)
Physiotherapy, forced ankle dorsiflexion stretching, gastrocsoleus stretching, ice, heat, heel cups and pads,1,10-13 and anti-inflammatories have all been used in the management of the condition.3,8 Clinicians have also historically restricted the patients’ activity, but this is unnecessary.
An in-shoe soft orthotic is helpful in treating calcaneal apophysitis. The prescription that the lead author writes is for a ⅝″ compressible, sponge-filled leather orthotic that is made in the form of a heel wedge or heel pad. Pain relief is believed to occur as a result of relaxation of the tension on the gastrocsoleus complex inserting onto the calcaneal apophysis and by “cushioning” the impact of heel strike.3 The orthotic, which typically lasts for 3 to 6 months, generally abrogates the need for anti-inflammatories as a primary treatment. However, relief of discomfort during this period may include use of antiflammatories.
For many years, the lead author has utilized a simple in-shoe, wedge-shaped orthotic consisting of a sponge material covered by leather, and compressible down to ⅝″. It raises the heel and cushions the impact of weightbearing. It can be transferred from shoe to shoe, and the patient can resume full activities while wearing the orthotic. Pain relief is generally achieved within 6 weeks to 3 months. Recalcitrant cases may require a 4 to 6 week period of casting in a plantar flexed position. Surgery is not necessary, nor are there any surgical cases reported in the literature. Orthopaedic referral is indicated for recalcitrant cases.
Acknowledgments
The Audio-Visual Department, Children’s Hospital Medical Center, Akron and Adeline Weiner assisted in preparing this paper.
Correspondence
Dennis S. Weiner, MD, 300 Locust Street, Suite 160, Akron, OH 44302-1821. [email protected]
1. Ogden J. Skeletal Injury in the Child. 3rd ed. New York: Springer-Verlag; 2000:1118–1120.
2. Orava S, Virtanen K. Osteochondroses in athletes. Br J Sports Med 1982;16:161-168.
3. Weiner DS. Pediatric Orthopedics for Primary Care Physicians. 2nd ed. Cambridge: Cambridge University Press; 2004.
4. Ishikawa SN. Conditions of the calcaneus in skeletally immature patients. Foot Ankle Clin N Am 2005;10:503-513.
5. Allison N. Apophysitis of the os calcis. J Bone Joint Surg 1924;6:91-94.
6. Brantigan CO. Calcaneal apophysitis. One of the growing pains of adolescence. Rocky Mt Med J 1972;69(8):59-60.
7. Ogden J, Ganey T, Hill JD, Jaakkola JI. Sever’s injury: a stress fracture of the immature calcaneal metaphysis. J Pediatr Orthop 2004;24:488-492.
8. Micheli LJ, Ireland LM. Prevention and management of calcaneal apophysitis in children; an overuse syndrome. J Pediatr Orthop 1987;7:34-38.
9. Liberson A, Lieberson S, Mendes DG, Shajrawi I, Ben Haim Y, Boss JH. Remodeling of the calcaneus apophysis in the growing child. J Pediatr Orthop 1995;4:74-79.
10. Contompasis JP. The management of heel pain in the athlete. Clin Podiatr Med Surg 1986;3:705-711.
11. McKenzie DC, Taunton JE, Clement DB, Smart GW, McNicol KL. Calcaneal epiphysitis in adolescent athletes. Can J Appl Sport Sci 1981;6:123-125.
12. Madden C, Mellion M. Sever’s disease and other causes of heel pain in adolescents. Am Fam Physician 1996;54:1995-2000.
13. Meyerding HW, Stuck WG. Painful heels among children (apophysitis). JAMA 1934;102:1658-1660.
14. Rhine I, Locke R. Apophysitis of the calcaneus. J Am Osteopath Assoc 1952;51:441-447.
15. Ross SE, Caffey J. Ossification of the calcaneal apophysis in healthy children. Stanford Med Bull 1957;15:224-226.
16. Sever JW. Apophysitis of the os calcis. NY State J Med 1912;95:1025-1029.
17. Volpon JB, de Carvalho Filho G. Calcaneal apophysitis a quantitative radiographic evaluation of the secondary ossification center. Arch Orthop Trauma Surg 2002;122:338-341.
18. Hughes ASR. Painful heels in children. Surg Gynecol Obstet 1948;86:64-68.
19. Kohler A, Zimmer EA. Borderlands of the Normal and Early Pathologic and Skeletal Roentgenology. 3rd ed. New York: Grune and Stratton; 1968.
20. Shopfner CE, Coin CG. Effect of weightbearing on the appearance and development of the secondary calcaneal epiphysis. Radiology 1966;86:201-206.
21. Krantz MK. Calcaneal apophysitis a clinical and roentgenologic study. J Am Podiatry Assoc 1965;55:801-807.
22. Lerner LH. Radiographic evaluation of calcaneal apophysitis. J Natl Assoc Chiropodists 1957;47:451-459.
- The true origin of the heel pain of calcaneal apophysitis is a stress microfracture (invisible on x-ray) due to chronic repetitive microtrauma—it’s an overuse syndrome that resolves without surgery in nearly all cases. (C)
- Most patients experience pain relief and can resume full activities while using a simple in-shoe wedge-shaped orthotic. (C)
- The most distinguishing feature on physical exam is the exquisite heel pain produced by lateral and medial compression (“squeezing”) of the heel. (C)
Strength of recommendation (SOR)
- Good quality patient-oriented evidence
- Inconsistent or limited-quality patient-oriented evidence
- Consensus, usual practice, opinion, disease-oriented evidence, case series
Two things about calcaneal “apophysitis” are a bit misleading. The first is its name. Although this common cause of heel pain in adolescents and teenagers was once considered a true osteochondritis, we now know that it’s actually a mechanical overuse pain syndrome with a self-limited, benign prognosis.1-3 The second area of confusion is what you’ll see on x-ray: an increased density and irregular fragmentation that was once viewed with suspicion, but is actually a normal pattern of ossification for this particular apophysis.
Don’t let the x-ray fool you
Primary care physicians can properly manage this common pain condition, given an understanding of the features, natural history, and treatment principles presented here.
Orthopedic referral is indicated for only a few recalcitrant cases.
Shoes aren’t to blame, but activity level is
Adolescents with calcaneal apophysitis—also known as Sever’s disease—will typically come into the office complaining of pain, often in both heels, particularly with mechanical activities such as running, jumping, and long-distance walking. Patients may walk on tiptoe to avoid the pain.4
The condition is common in both boys and girls, although personal experience indicates it’s more common in boys. The typical age of the patient is 8 to 15 years. The condition is most commonly seen in patients who are engaged in athletic endeavors,5,6 including soccer, basketball, and gymnastics,7,8 though no specific athletic endeavor has been directly implicated in the pathogenesis. Likewise, no specific foot structure or type of shoe wear has been directly related to the symptomatology.
An otherwise healthy boy, age 12, walks into your office—on tiptoe. His problem is pain in both heels, especially when running. It’s his first season on his school track team, and he says he’s been practicing hard for the 50-yard dash, “my best event.” his parents express to you their concern about possible sports-related injuries or underlying disease, and their son’s distress about the possibilty of “letting down the team” if he quits. You find no swelling, no skin changes, no erythema, and no other local abnormalities. Symptoms of marked pain are produced by medial and lateral compression (squeezing) of the heel at the site where the calcaneal apophysis attaches to the main body of the os calcis. There is no pain on plantar, posterior, or retrocalcaneal pressure, or adjacent to the Achilles tendon.
Exquisite heel pain produced by medial and lateral compression of the heel is the most distinguishing feature of calcaneal apophysitis
Is this x-ray normal? You order a lateral x-ray of the calcaneus to exclude other pathology. You observe a pattern of increased density and apparent irregular fragmentation on the x-ray. The radiologist reports no abnormal findings. The above x-ray typifies calcaneal apophysitis, an overuse syndrome often seen in children 8 to 15 years of age. The “dense” area is actually a secondary ossification center of the calcaneus, not an indication of pathology.
The ossification of the calcaneus is different from that of the tarsal bones, which are each ossified from a single center. In the case of the calcaneus, a secondary center of ossification typically appears in girls by age 6, and in boys by age 8.14,15 During adolescence, a C-shaped cartilage develops between the metaphyseal bone of the body of the calcaneus and the secondary center (or centers) of ossification. Then, at around age 10 or 11, a more superior tertiary ossification center appears in the apophysis of the calcaneus.
As the calcaneal apophysis progressively ossifies, it presents as a very dense radiographic pattern in an adolescent. For years, this was thought to represent a form of osteochondritis.16 In fact, this is a normal pattern of ossification for this particular apophysis.17-22
What do you tell the patient and parents? You advise an in-shoe orthotic, no limits on physical activity, and no surgery. You explain that the pain is due to recurrent impact (overuse), and that the orthotic will “unload” the heel and permit symtoms to resolve, typically within 60 days. If asked about discomfort, you may advise anti-inflammatories and ice/heat.
Patients typically have no swelling, skin changes, erythema, or other local abnormalities.8 The most characteristic distinguishing feature on physical examination is exquisite pain produced on medial and lateral compression (“squeezing”) of the heel at the site where the calcaneal apophysis attaches to the main body of the os calcis. The pain is not on plantar pressure (as you would see with plantar fasciitis), or posterior, retrocalcaneal, or adjacent to the Achilles tendon (as you would see on Achilles tendinitis), but on medial and lateral compression.3
I’ve noticed a number of trends over the years while caring for patients with calcaneal apophysitis. My chart review of the 227 patients I cared for between 1971 and 1997 revealed the following:
- 60% (137) of patients had bilateral involvement.
- 78% of the patients were male. The reason for the male preponderance remains unclear.
- All but 3 of the 364 feet obtained eventual complete symptom resolution with the prescribed sponge-leather heel orthotic.
- Symptoms typically resolved within 60 days.
- The 3 cases that were recalcitrant to orthotic treatment required an equinus-type cast for 4 to 6 weeks. Those patients treated with a cast also had resolution of their symptoms.
- Roughly 30% of the cases encountered a recurrence of symptoms with similar resolution with the previously described retreatment. Recurrences were unrelated to gender.
- No case ever required any other treatment type beyond the orthotic or cast.—Dennis Weiner, MD
Researchers found microfractures. Magnetic resonance imaging (MRI) evidence suggests that the true pathogenesis of calcaneal apophysitis is a stress microfracture related to chronic repetitive microtrauma.9 In addition, MRI evidence suggests that the location of the stress microfractures is in the metaphysis of the body of the calcaneus adjacent to—but not directly involving—the apophysis.1,7 This more recent evidence replaces the historical hypotheses that the condition is primarily an inflammatory process. As a consequence of the microtrauma, however, it’s possible that an inflammatory process may occur secondarily.
Should you order x-rays? X-rays are not essential to the diagnosis, though they may be used to rule out other conditions, such as fracture, infection, or a bone cyst. Keep in mind, though, that patients with calcaneal pain will have a normal x-ray.7 What is normal, however, is another matter, and has been the subject of confusion in the past.
Pain stops in a few weeks
Usually, the symptoms of calcaneal apophysitis resolve fairly quickly, and with relatively simple treatment. (The symptoms also disappear as the child gets older and the calcaneal apophysis amalgamates with the main body of the calcaneus.)
Physiotherapy, forced ankle dorsiflexion stretching, gastrocsoleus stretching, ice, heat, heel cups and pads,1,10-13 and anti-inflammatories have all been used in the management of the condition.3,8 Clinicians have also historically restricted the patients’ activity, but this is unnecessary.
An in-shoe soft orthotic is helpful in treating calcaneal apophysitis. The prescription that the lead author writes is for a ⅝″ compressible, sponge-filled leather orthotic that is made in the form of a heel wedge or heel pad. Pain relief is believed to occur as a result of relaxation of the tension on the gastrocsoleus complex inserting onto the calcaneal apophysis and by “cushioning” the impact of heel strike.3 The orthotic, which typically lasts for 3 to 6 months, generally abrogates the need for anti-inflammatories as a primary treatment. However, relief of discomfort during this period may include use of antiflammatories.
For many years, the lead author has utilized a simple in-shoe, wedge-shaped orthotic consisting of a sponge material covered by leather, and compressible down to ⅝″. It raises the heel and cushions the impact of weightbearing. It can be transferred from shoe to shoe, and the patient can resume full activities while wearing the orthotic. Pain relief is generally achieved within 6 weeks to 3 months. Recalcitrant cases may require a 4 to 6 week period of casting in a plantar flexed position. Surgery is not necessary, nor are there any surgical cases reported in the literature. Orthopaedic referral is indicated for recalcitrant cases.
Acknowledgments
The Audio-Visual Department, Children’s Hospital Medical Center, Akron and Adeline Weiner assisted in preparing this paper.
Correspondence
Dennis S. Weiner, MD, 300 Locust Street, Suite 160, Akron, OH 44302-1821. [email protected]
- The true origin of the heel pain of calcaneal apophysitis is a stress microfracture (invisible on x-ray) due to chronic repetitive microtrauma—it’s an overuse syndrome that resolves without surgery in nearly all cases. (C)
- Most patients experience pain relief and can resume full activities while using a simple in-shoe wedge-shaped orthotic. (C)
- The most distinguishing feature on physical exam is the exquisite heel pain produced by lateral and medial compression (“squeezing”) of the heel. (C)
Strength of recommendation (SOR)
- Good quality patient-oriented evidence
- Inconsistent or limited-quality patient-oriented evidence
- Consensus, usual practice, opinion, disease-oriented evidence, case series
Two things about calcaneal “apophysitis” are a bit misleading. The first is its name. Although this common cause of heel pain in adolescents and teenagers was once considered a true osteochondritis, we now know that it’s actually a mechanical overuse pain syndrome with a self-limited, benign prognosis.1-3 The second area of confusion is what you’ll see on x-ray: an increased density and irregular fragmentation that was once viewed with suspicion, but is actually a normal pattern of ossification for this particular apophysis.
Don’t let the x-ray fool you
Primary care physicians can properly manage this common pain condition, given an understanding of the features, natural history, and treatment principles presented here.
Orthopedic referral is indicated for only a few recalcitrant cases.
Shoes aren’t to blame, but activity level is
Adolescents with calcaneal apophysitis—also known as Sever’s disease—will typically come into the office complaining of pain, often in both heels, particularly with mechanical activities such as running, jumping, and long-distance walking. Patients may walk on tiptoe to avoid the pain.4
The condition is common in both boys and girls, although personal experience indicates it’s more common in boys. The typical age of the patient is 8 to 15 years. The condition is most commonly seen in patients who are engaged in athletic endeavors,5,6 including soccer, basketball, and gymnastics,7,8 though no specific athletic endeavor has been directly implicated in the pathogenesis. Likewise, no specific foot structure or type of shoe wear has been directly related to the symptomatology.
An otherwise healthy boy, age 12, walks into your office—on tiptoe. His problem is pain in both heels, especially when running. It’s his first season on his school track team, and he says he’s been practicing hard for the 50-yard dash, “my best event.” his parents express to you their concern about possible sports-related injuries or underlying disease, and their son’s distress about the possibilty of “letting down the team” if he quits. You find no swelling, no skin changes, no erythema, and no other local abnormalities. Symptoms of marked pain are produced by medial and lateral compression (squeezing) of the heel at the site where the calcaneal apophysis attaches to the main body of the os calcis. There is no pain on plantar, posterior, or retrocalcaneal pressure, or adjacent to the Achilles tendon.
Exquisite heel pain produced by medial and lateral compression of the heel is the most distinguishing feature of calcaneal apophysitis
Is this x-ray normal? You order a lateral x-ray of the calcaneus to exclude other pathology. You observe a pattern of increased density and apparent irregular fragmentation on the x-ray. The radiologist reports no abnormal findings. The above x-ray typifies calcaneal apophysitis, an overuse syndrome often seen in children 8 to 15 years of age. The “dense” area is actually a secondary ossification center of the calcaneus, not an indication of pathology.
The ossification of the calcaneus is different from that of the tarsal bones, which are each ossified from a single center. In the case of the calcaneus, a secondary center of ossification typically appears in girls by age 6, and in boys by age 8.14,15 During adolescence, a C-shaped cartilage develops between the metaphyseal bone of the body of the calcaneus and the secondary center (or centers) of ossification. Then, at around age 10 or 11, a more superior tertiary ossification center appears in the apophysis of the calcaneus.
As the calcaneal apophysis progressively ossifies, it presents as a very dense radiographic pattern in an adolescent. For years, this was thought to represent a form of osteochondritis.16 In fact, this is a normal pattern of ossification for this particular apophysis.17-22
What do you tell the patient and parents? You advise an in-shoe orthotic, no limits on physical activity, and no surgery. You explain that the pain is due to recurrent impact (overuse), and that the orthotic will “unload” the heel and permit symtoms to resolve, typically within 60 days. If asked about discomfort, you may advise anti-inflammatories and ice/heat.
Patients typically have no swelling, skin changes, erythema, or other local abnormalities.8 The most characteristic distinguishing feature on physical examination is exquisite pain produced on medial and lateral compression (“squeezing”) of the heel at the site where the calcaneal apophysis attaches to the main body of the os calcis. The pain is not on plantar pressure (as you would see with plantar fasciitis), or posterior, retrocalcaneal, or adjacent to the Achilles tendon (as you would see on Achilles tendinitis), but on medial and lateral compression.3
I’ve noticed a number of trends over the years while caring for patients with calcaneal apophysitis. My chart review of the 227 patients I cared for between 1971 and 1997 revealed the following:
- 60% (137) of patients had bilateral involvement.
- 78% of the patients were male. The reason for the male preponderance remains unclear.
- All but 3 of the 364 feet obtained eventual complete symptom resolution with the prescribed sponge-leather heel orthotic.
- Symptoms typically resolved within 60 days.
- The 3 cases that were recalcitrant to orthotic treatment required an equinus-type cast for 4 to 6 weeks. Those patients treated with a cast also had resolution of their symptoms.
- Roughly 30% of the cases encountered a recurrence of symptoms with similar resolution with the previously described retreatment. Recurrences were unrelated to gender.
- No case ever required any other treatment type beyond the orthotic or cast.—Dennis Weiner, MD
Researchers found microfractures. Magnetic resonance imaging (MRI) evidence suggests that the true pathogenesis of calcaneal apophysitis is a stress microfracture related to chronic repetitive microtrauma.9 In addition, MRI evidence suggests that the location of the stress microfractures is in the metaphysis of the body of the calcaneus adjacent to—but not directly involving—the apophysis.1,7 This more recent evidence replaces the historical hypotheses that the condition is primarily an inflammatory process. As a consequence of the microtrauma, however, it’s possible that an inflammatory process may occur secondarily.
Should you order x-rays? X-rays are not essential to the diagnosis, though they may be used to rule out other conditions, such as fracture, infection, or a bone cyst. Keep in mind, though, that patients with calcaneal pain will have a normal x-ray.7 What is normal, however, is another matter, and has been the subject of confusion in the past.
Pain stops in a few weeks
Usually, the symptoms of calcaneal apophysitis resolve fairly quickly, and with relatively simple treatment. (The symptoms also disappear as the child gets older and the calcaneal apophysis amalgamates with the main body of the calcaneus.)
Physiotherapy, forced ankle dorsiflexion stretching, gastrocsoleus stretching, ice, heat, heel cups and pads,1,10-13 and anti-inflammatories have all been used in the management of the condition.3,8 Clinicians have also historically restricted the patients’ activity, but this is unnecessary.
An in-shoe soft orthotic is helpful in treating calcaneal apophysitis. The prescription that the lead author writes is for a ⅝″ compressible, sponge-filled leather orthotic that is made in the form of a heel wedge or heel pad. Pain relief is believed to occur as a result of relaxation of the tension on the gastrocsoleus complex inserting onto the calcaneal apophysis and by “cushioning” the impact of heel strike.3 The orthotic, which typically lasts for 3 to 6 months, generally abrogates the need for anti-inflammatories as a primary treatment. However, relief of discomfort during this period may include use of antiflammatories.
For many years, the lead author has utilized a simple in-shoe, wedge-shaped orthotic consisting of a sponge material covered by leather, and compressible down to ⅝″. It raises the heel and cushions the impact of weightbearing. It can be transferred from shoe to shoe, and the patient can resume full activities while wearing the orthotic. Pain relief is generally achieved within 6 weeks to 3 months. Recalcitrant cases may require a 4 to 6 week period of casting in a plantar flexed position. Surgery is not necessary, nor are there any surgical cases reported in the literature. Orthopaedic referral is indicated for recalcitrant cases.
Acknowledgments
The Audio-Visual Department, Children’s Hospital Medical Center, Akron and Adeline Weiner assisted in preparing this paper.
Correspondence
Dennis S. Weiner, MD, 300 Locust Street, Suite 160, Akron, OH 44302-1821. [email protected]
1. Ogden J. Skeletal Injury in the Child. 3rd ed. New York: Springer-Verlag; 2000:1118–1120.
2. Orava S, Virtanen K. Osteochondroses in athletes. Br J Sports Med 1982;16:161-168.
3. Weiner DS. Pediatric Orthopedics for Primary Care Physicians. 2nd ed. Cambridge: Cambridge University Press; 2004.
4. Ishikawa SN. Conditions of the calcaneus in skeletally immature patients. Foot Ankle Clin N Am 2005;10:503-513.
5. Allison N. Apophysitis of the os calcis. J Bone Joint Surg 1924;6:91-94.
6. Brantigan CO. Calcaneal apophysitis. One of the growing pains of adolescence. Rocky Mt Med J 1972;69(8):59-60.
7. Ogden J, Ganey T, Hill JD, Jaakkola JI. Sever’s injury: a stress fracture of the immature calcaneal metaphysis. J Pediatr Orthop 2004;24:488-492.
8. Micheli LJ, Ireland LM. Prevention and management of calcaneal apophysitis in children; an overuse syndrome. J Pediatr Orthop 1987;7:34-38.
9. Liberson A, Lieberson S, Mendes DG, Shajrawi I, Ben Haim Y, Boss JH. Remodeling of the calcaneus apophysis in the growing child. J Pediatr Orthop 1995;4:74-79.
10. Contompasis JP. The management of heel pain in the athlete. Clin Podiatr Med Surg 1986;3:705-711.
11. McKenzie DC, Taunton JE, Clement DB, Smart GW, McNicol KL. Calcaneal epiphysitis in adolescent athletes. Can J Appl Sport Sci 1981;6:123-125.
12. Madden C, Mellion M. Sever’s disease and other causes of heel pain in adolescents. Am Fam Physician 1996;54:1995-2000.
13. Meyerding HW, Stuck WG. Painful heels among children (apophysitis). JAMA 1934;102:1658-1660.
14. Rhine I, Locke R. Apophysitis of the calcaneus. J Am Osteopath Assoc 1952;51:441-447.
15. Ross SE, Caffey J. Ossification of the calcaneal apophysis in healthy children. Stanford Med Bull 1957;15:224-226.
16. Sever JW. Apophysitis of the os calcis. NY State J Med 1912;95:1025-1029.
17. Volpon JB, de Carvalho Filho G. Calcaneal apophysitis a quantitative radiographic evaluation of the secondary ossification center. Arch Orthop Trauma Surg 2002;122:338-341.
18. Hughes ASR. Painful heels in children. Surg Gynecol Obstet 1948;86:64-68.
19. Kohler A, Zimmer EA. Borderlands of the Normal and Early Pathologic and Skeletal Roentgenology. 3rd ed. New York: Grune and Stratton; 1968.
20. Shopfner CE, Coin CG. Effect of weightbearing on the appearance and development of the secondary calcaneal epiphysis. Radiology 1966;86:201-206.
21. Krantz MK. Calcaneal apophysitis a clinical and roentgenologic study. J Am Podiatry Assoc 1965;55:801-807.
22. Lerner LH. Radiographic evaluation of calcaneal apophysitis. J Natl Assoc Chiropodists 1957;47:451-459.
1. Ogden J. Skeletal Injury in the Child. 3rd ed. New York: Springer-Verlag; 2000:1118–1120.
2. Orava S, Virtanen K. Osteochondroses in athletes. Br J Sports Med 1982;16:161-168.
3. Weiner DS. Pediatric Orthopedics for Primary Care Physicians. 2nd ed. Cambridge: Cambridge University Press; 2004.
4. Ishikawa SN. Conditions of the calcaneus in skeletally immature patients. Foot Ankle Clin N Am 2005;10:503-513.
5. Allison N. Apophysitis of the os calcis. J Bone Joint Surg 1924;6:91-94.
6. Brantigan CO. Calcaneal apophysitis. One of the growing pains of adolescence. Rocky Mt Med J 1972;69(8):59-60.
7. Ogden J, Ganey T, Hill JD, Jaakkola JI. Sever’s injury: a stress fracture of the immature calcaneal metaphysis. J Pediatr Orthop 2004;24:488-492.
8. Micheli LJ, Ireland LM. Prevention and management of calcaneal apophysitis in children; an overuse syndrome. J Pediatr Orthop 1987;7:34-38.
9. Liberson A, Lieberson S, Mendes DG, Shajrawi I, Ben Haim Y, Boss JH. Remodeling of the calcaneus apophysis in the growing child. J Pediatr Orthop 1995;4:74-79.
10. Contompasis JP. The management of heel pain in the athlete. Clin Podiatr Med Surg 1986;3:705-711.
11. McKenzie DC, Taunton JE, Clement DB, Smart GW, McNicol KL. Calcaneal epiphysitis in adolescent athletes. Can J Appl Sport Sci 1981;6:123-125.
12. Madden C, Mellion M. Sever’s disease and other causes of heel pain in adolescents. Am Fam Physician 1996;54:1995-2000.
13. Meyerding HW, Stuck WG. Painful heels among children (apophysitis). JAMA 1934;102:1658-1660.
14. Rhine I, Locke R. Apophysitis of the calcaneus. J Am Osteopath Assoc 1952;51:441-447.
15. Ross SE, Caffey J. Ossification of the calcaneal apophysis in healthy children. Stanford Med Bull 1957;15:224-226.
16. Sever JW. Apophysitis of the os calcis. NY State J Med 1912;95:1025-1029.
17. Volpon JB, de Carvalho Filho G. Calcaneal apophysitis a quantitative radiographic evaluation of the secondary ossification center. Arch Orthop Trauma Surg 2002;122:338-341.
18. Hughes ASR. Painful heels in children. Surg Gynecol Obstet 1948;86:64-68.
19. Kohler A, Zimmer EA. Borderlands of the Normal and Early Pathologic and Skeletal Roentgenology. 3rd ed. New York: Grune and Stratton; 1968.
20. Shopfner CE, Coin CG. Effect of weightbearing on the appearance and development of the secondary calcaneal epiphysis. Radiology 1966;86:201-206.
21. Krantz MK. Calcaneal apophysitis a clinical and roentgenologic study. J Am Podiatry Assoc 1965;55:801-807.
22. Lerner LH. Radiographic evaluation of calcaneal apophysitis. J Natl Assoc Chiropodists 1957;47:451-459.