User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Physiotherapy Found to Have Short-Term Benefit in Parkinson's
Existing data support the use of physiotherapy in the treatment of Parkinson’s disease in the short term, but larger, randomized controlled trials of longer duration are needed to better define the benefit of the intervention.
That’s the overall conclusion from a systematic review intended to assess the effectiveness of physiotherapy compared with no intervention in patients with Parkinson’s disease.
"In recent years, supportive evidence for the inclusion of physiotherapy in the management of Parkinson’s disease has grown, due to the increased number of trials, particularly in the past 5 years," researchers led by Claire L. Tomlinson, Ph.D., reported. Recent management guidelines, such as those from the U.K. National Institute for Health and Clinical Excellence and the Royal Dutch Society of Physical Therapy, have supported physiotherapy. "This has led to an increased number of referrals, with a survey by Parkinson’s U.K. in 2008 reporting that 54% of the 13,000 members surveyed had seen a physiotherapist," Dr. Tomlinson and her associates wrote.
Dr. Tomlinson, a systematic reviewer with the clinical trials unit at the University of Birmingham (England), and her associates searched existing databases of medical literature to find randomized, controlled trials of patients with Parkinson’s disease that compared a physiotherapy intervention with no intervention or placebo control. This included trials of general physiotherapy, exercise, treadmill training, cueing, dance, and martial arts versus no intervention (BMJ 2012 Aug. 6 [doi:10.1136/bmj.e5004]).
The final analysis included 39 randomized controlled trials involving 1,827 patients. Collectively, information was available for 44 comparisons within the six defined physiotherapy interventions. The methodologic quality of the trials varied widely. For example, less than half described the randomization used, blinded assessors were used in 62% of studies, and only nine trials stated intention to treat as the primary method of analysis. There were 18 outcomes of interest, including measures of gait, functional mobility and balance, falls, clinician-rated impairment and disability measures, patient-rated quality of life, adverse events, compliance, and economics of the intervention.
Dr. Tomlinson and her associates observed a significant benefit from physiotherapy for 9 of 18 outcomes measured. Significant outcomes, which they described as possibly having clinical importance, were speed (0.04 m/sec, P less than .001); Berg balance scale scores (3.71 points, P less than .001); and scores on the Unified Parkinson’s Disease Rating Scale (total score of –6.15 points, P less than .001, and two UPDRS subscores: activities of daily living (–1.36, P = .01) and motor (–5.01, P less than .001).
"We saw no evidence of an improvement in patient-rated quality of life after physiotherapy, and the observed differences in the nine significant outcomes were relatively small," the researchers wrote. "Their relevance and benefit to patients with Parkinson’s disease must be put into context, in terms of what is considered a recommended minimally important difference. Little good-quality evidence is available for minimal clinically important differences in these outcome measures."
No differences in the treatment effect between the different interventions were found, but the researchers pointed out that data for each type of physiotherapy "were limited and these comparisons were based on indirect comparisons, which should be interpreted with caution. Therefore, physiotherapy interventions should be compared against each other within rigorous trial designs to determine which, if any, are effective. This analysis could provide therapists with a menu of treatment strategies from which they can devise individualized interventions."
They acknowledged certain limitations of the meta-analysis, including the fact that most of the trials were small and compared the effect of physiotherapy vs. no intervention over a time period that was shorter than 3 months. "Three trials followed up their patients for 3 months or longer, but all used different follow-up periods, the longest being 6 months," the researchers wrote. "With such limited data, no meaningful meta-analysis could be performed on these longer-term data to assess the duration of any improvement after therapy."
The study was funded by Parkinson’s U.K. and by the U.K. Department of Health. The authors reported no relevant financial disclosures.
Existing data support the use of physiotherapy in the treatment of Parkinson’s disease in the short term, but larger, randomized controlled trials of longer duration are needed to better define the benefit of the intervention.
That’s the overall conclusion from a systematic review intended to assess the effectiveness of physiotherapy compared with no intervention in patients with Parkinson’s disease.
"In recent years, supportive evidence for the inclusion of physiotherapy in the management of Parkinson’s disease has grown, due to the increased number of trials, particularly in the past 5 years," researchers led by Claire L. Tomlinson, Ph.D., reported. Recent management guidelines, such as those from the U.K. National Institute for Health and Clinical Excellence and the Royal Dutch Society of Physical Therapy, have supported physiotherapy. "This has led to an increased number of referrals, with a survey by Parkinson’s U.K. in 2008 reporting that 54% of the 13,000 members surveyed had seen a physiotherapist," Dr. Tomlinson and her associates wrote.
Dr. Tomlinson, a systematic reviewer with the clinical trials unit at the University of Birmingham (England), and her associates searched existing databases of medical literature to find randomized, controlled trials of patients with Parkinson’s disease that compared a physiotherapy intervention with no intervention or placebo control. This included trials of general physiotherapy, exercise, treadmill training, cueing, dance, and martial arts versus no intervention (BMJ 2012 Aug. 6 [doi:10.1136/bmj.e5004]).
The final analysis included 39 randomized controlled trials involving 1,827 patients. Collectively, information was available for 44 comparisons within the six defined physiotherapy interventions. The methodologic quality of the trials varied widely. For example, less than half described the randomization used, blinded assessors were used in 62% of studies, and only nine trials stated intention to treat as the primary method of analysis. There were 18 outcomes of interest, including measures of gait, functional mobility and balance, falls, clinician-rated impairment and disability measures, patient-rated quality of life, adverse events, compliance, and economics of the intervention.
Dr. Tomlinson and her associates observed a significant benefit from physiotherapy for 9 of 18 outcomes measured. Significant outcomes, which they described as possibly having clinical importance, were speed (0.04 m/sec, P less than .001); Berg balance scale scores (3.71 points, P less than .001); and scores on the Unified Parkinson’s Disease Rating Scale (total score of –6.15 points, P less than .001, and two UPDRS subscores: activities of daily living (–1.36, P = .01) and motor (–5.01, P less than .001).
"We saw no evidence of an improvement in patient-rated quality of life after physiotherapy, and the observed differences in the nine significant outcomes were relatively small," the researchers wrote. "Their relevance and benefit to patients with Parkinson’s disease must be put into context, in terms of what is considered a recommended minimally important difference. Little good-quality evidence is available for minimal clinically important differences in these outcome measures."
No differences in the treatment effect between the different interventions were found, but the researchers pointed out that data for each type of physiotherapy "were limited and these comparisons were based on indirect comparisons, which should be interpreted with caution. Therefore, physiotherapy interventions should be compared against each other within rigorous trial designs to determine which, if any, are effective. This analysis could provide therapists with a menu of treatment strategies from which they can devise individualized interventions."
They acknowledged certain limitations of the meta-analysis, including the fact that most of the trials were small and compared the effect of physiotherapy vs. no intervention over a time period that was shorter than 3 months. "Three trials followed up their patients for 3 months or longer, but all used different follow-up periods, the longest being 6 months," the researchers wrote. "With such limited data, no meaningful meta-analysis could be performed on these longer-term data to assess the duration of any improvement after therapy."
The study was funded by Parkinson’s U.K. and by the U.K. Department of Health. The authors reported no relevant financial disclosures.
Existing data support the use of physiotherapy in the treatment of Parkinson’s disease in the short term, but larger, randomized controlled trials of longer duration are needed to better define the benefit of the intervention.
That’s the overall conclusion from a systematic review intended to assess the effectiveness of physiotherapy compared with no intervention in patients with Parkinson’s disease.
"In recent years, supportive evidence for the inclusion of physiotherapy in the management of Parkinson’s disease has grown, due to the increased number of trials, particularly in the past 5 years," researchers led by Claire L. Tomlinson, Ph.D., reported. Recent management guidelines, such as those from the U.K. National Institute for Health and Clinical Excellence and the Royal Dutch Society of Physical Therapy, have supported physiotherapy. "This has led to an increased number of referrals, with a survey by Parkinson’s U.K. in 2008 reporting that 54% of the 13,000 members surveyed had seen a physiotherapist," Dr. Tomlinson and her associates wrote.
Dr. Tomlinson, a systematic reviewer with the clinical trials unit at the University of Birmingham (England), and her associates searched existing databases of medical literature to find randomized, controlled trials of patients with Parkinson’s disease that compared a physiotherapy intervention with no intervention or placebo control. This included trials of general physiotherapy, exercise, treadmill training, cueing, dance, and martial arts versus no intervention (BMJ 2012 Aug. 6 [doi:10.1136/bmj.e5004]).
The final analysis included 39 randomized controlled trials involving 1,827 patients. Collectively, information was available for 44 comparisons within the six defined physiotherapy interventions. The methodologic quality of the trials varied widely. For example, less than half described the randomization used, blinded assessors were used in 62% of studies, and only nine trials stated intention to treat as the primary method of analysis. There were 18 outcomes of interest, including measures of gait, functional mobility and balance, falls, clinician-rated impairment and disability measures, patient-rated quality of life, adverse events, compliance, and economics of the intervention.
Dr. Tomlinson and her associates observed a significant benefit from physiotherapy for 9 of 18 outcomes measured. Significant outcomes, which they described as possibly having clinical importance, were speed (0.04 m/sec, P less than .001); Berg balance scale scores (3.71 points, P less than .001); and scores on the Unified Parkinson’s Disease Rating Scale (total score of –6.15 points, P less than .001, and two UPDRS subscores: activities of daily living (–1.36, P = .01) and motor (–5.01, P less than .001).
"We saw no evidence of an improvement in patient-rated quality of life after physiotherapy, and the observed differences in the nine significant outcomes were relatively small," the researchers wrote. "Their relevance and benefit to patients with Parkinson’s disease must be put into context, in terms of what is considered a recommended minimally important difference. Little good-quality evidence is available for minimal clinically important differences in these outcome measures."
No differences in the treatment effect between the different interventions were found, but the researchers pointed out that data for each type of physiotherapy "were limited and these comparisons were based on indirect comparisons, which should be interpreted with caution. Therefore, physiotherapy interventions should be compared against each other within rigorous trial designs to determine which, if any, are effective. This analysis could provide therapists with a menu of treatment strategies from which they can devise individualized interventions."
They acknowledged certain limitations of the meta-analysis, including the fact that most of the trials were small and compared the effect of physiotherapy vs. no intervention over a time period that was shorter than 3 months. "Three trials followed up their patients for 3 months or longer, but all used different follow-up periods, the longest being 6 months," the researchers wrote. "With such limited data, no meaningful meta-analysis could be performed on these longer-term data to assess the duration of any improvement after therapy."
The study was funded by Parkinson’s U.K. and by the U.K. Department of Health. The authors reported no relevant financial disclosures.
FROM BMJ
Major Finding: Compared with Parkinson’s patients who received no intervention, those who received physiotherapy had significant improvements in speed (0.04 m/sec, P less than .001); Berg balance scale scores (3.71 points, P less than .001); and scores on the Unified Parkinson’s Disease Rating Scale (total score of –6.15 points, P less than .001).
Data Source: A meta-analysis of 39 randomized trials involving 1,827 patients was conducted.
Disclosures: The study was funded by Parkinson’s U.K. and by the U.K. Department of Health. The investigators reported no relevant financial disclosures.
LCZ696 Promising in Subset of Heart Failure Patients
Heart failure patients with preserved ejection who received an investigational agent LCA696 experienced a significant reduction of NT-proBNP at 12 weeks, compared with those who received valsartan, a randomized, multicenter, phase II trial demonstrated.
In addition, a reduction in left atrial size at 36 weeks was observed in patients in the LCA696 group, compared with those who received the angiotensin receptor blocker, researchers led by Dr. Scott Solomon of the cardiovascular division at Brigham and Women’s Hospital, Boston, reported in a study published online Aug. 26, 2012, in the Lancet. The study was simultaneously presented at the annual congress of the European Society of Cardiology.
"Present treatment of heart failure with preserved ejection fraction remains both symptom based and empiric, with no specific treatment approved for this indication," the researchers wrote. "Although ACE inhibitors and ARBs have been associated with symptom improvement, increased functional capacity, and reduction in admission to hospital in these patients, existing guidelines state that no treatment has convincingly been shown to reduce morbidity or mortality.
In a phase II trial known as PARAMOUNT, Dr. Solomon and his associates at 65 centers in 13 countries set out to assess the efficacy and safety of LCZ696 in 301 heart failure patients with preserved ejection fraction. LCZ696 is a first-in-class angiotensin receptor neprilysin inhibitor that includes valsartan. The researchers hypothesized that LCA696 works by augmenting the active natriuretic peptides to improve myocardial relaxation and reduce hypertrophy. They recruited patients from November 2009 through March 2011.
Patients were eligible for PARAMOUNT if they were at least 40 years of age, had New York Heart Association class II-III heart failure, a left ventricular ejection fraction (LVEF) of 45% or higher, and an NT-proBNP greater than 400 pg/mL (Lancet 2012 Aug. 26 [http://dx.doi.org/10.1016/S0140-6736(12)61227-6]).
After randomization, 149 patients were started on 50 mg LCZ696 twice daily and 152 were started on 40 mg valsartan twice daily and titrated to their final doses of 200 mg LCZ696 twice daily or 160 mg valsartan twice daily over a period of 2-4 weeks. All patients were treated for 36 weeks; the primary end point was change in NT-proBNP from baseline to 12 weeks. This end point was selected "because raised natriuretic peptide concentrations are associated with adverse outcomes in patients with heart failure, including those with preserved ejection fraction, and reductions in NT-proBNP have been associated with improved outcomes in heart failure," the researchers explained.
Dr. Solomon and his associates reported complete data from 134 patients in the LCZ696 group and 132 patients in the valsartan group. The mean age of patients in both groups was 71 years and more than half (57%) were women. The change in NT-proBNP from baseline to week 12 was significantly reduced in patients in the LCZ696 group (from 783 to 605 pg/mL), compared with patients in the valsartan group (from 862 to 835 pg/mL). This translated into a significant ratio of change between the two treatment groups of 0.77. By week 36, the differences in NT-proBNP between the two groups were no longer significant.
After 36 weeks of treatment, patients in the LCZ696 group experienced significant reductions in left atrial volume and in left atrial dimension, compared with their counterparts in the valsartan group. "Left atrial size has been one of the most powerful predictors of outcome in heart failure, including heart failure with preserved ejection fraction," the researchers wrote. "The reported reduction in left atrial size offers support to the notion that LCZ696 had a sustained physiological benefit to 36 weeks."
LCZ696 was well tolerated and the proportion of patients who experienced one or more serious adverse events was similar between the two groups (15% among those in the LCZ696 group vs. 20% among those in the valsartan group).
Novartis funded the study. Dr. Solomon and six of his coauthors disclosed having received research support from, and have consulted for, Novartis, which is developing LCZ696. Three other coauthors are employed by the company.
The positive signals from PARAMOUNT will surely trigger a definitive trial. However, what will the comparator be? Valsartan, a drug not known to be effective for heart failure with preserved ejection fraction? This comparison would show whether there was an advantage to adding a neprilysin inhibitor, but would not provide evidence that valsartan was useful in patients with heart failure with preserved ejection fraction. ACE inhibitors, which seem to have some effect in disease with preserved ejection fraction? An increase in diuretic dose – perhaps the best method of improving symptoms in a congested patient? Or simply placebo? A placebo-controlled design would be the easiest to interpret, but could be confounded by the widespread use of rennin-angiotensin-aldosterone system antagonists in patients with heart failure with preserved ejection fraction, often for problems such as hypertension and peripheral edema. Such background treatment might not easily be withdrawn, rendering enrollment difficult.
Another trial, in patients with heart failure with reduced ejection fraction and raised plasma natriuretic peptides, will show whether LCZ696 is superior to enalapril. If trials in disease with both preserved and reduced ejection fraction are positive (and use the same comparator), cardiac phenotype could become less important than plasma concentration of natriuretic peptides for management of heart failure. However, if LCZ696 proves ineffective in heart failure with preserved ejection fraction, then more attention should be paid to targeting of comorbid disease, to the individual phenotypes, to the causes underlying disease with preserved ejection fraction, or to the aging process itself, which could be the ultimate determinant of prognosis in these patients.
Dr. John G.F. Cleland and Dr. Andrew L. Clark are with the department of cardiology at Castle Hill Hospital in Kingston-Upon-Hull, United Kingdom. These remarks were adapted from a editorial accompanying the PARAMOUNT report (Lancet 2012 Aug. 26 [ http://dx.doi.org/10.1016/ S0140-6736(12)61349-X ]). Dr. Cleland disclosed that he has received honoraria from Novartis. Dr. Clark stated that he has no relevant financial conflicts of interest.
The positive signals from PARAMOUNT will surely trigger a definitive trial. However, what will the comparator be? Valsartan, a drug not known to be effective for heart failure with preserved ejection fraction? This comparison would show whether there was an advantage to adding a neprilysin inhibitor, but would not provide evidence that valsartan was useful in patients with heart failure with preserved ejection fraction. ACE inhibitors, which seem to have some effect in disease with preserved ejection fraction? An increase in diuretic dose – perhaps the best method of improving symptoms in a congested patient? Or simply placebo? A placebo-controlled design would be the easiest to interpret, but could be confounded by the widespread use of rennin-angiotensin-aldosterone system antagonists in patients with heart failure with preserved ejection fraction, often for problems such as hypertension and peripheral edema. Such background treatment might not easily be withdrawn, rendering enrollment difficult.
Another trial, in patients with heart failure with reduced ejection fraction and raised plasma natriuretic peptides, will show whether LCZ696 is superior to enalapril. If trials in disease with both preserved and reduced ejection fraction are positive (and use the same comparator), cardiac phenotype could become less important than plasma concentration of natriuretic peptides for management of heart failure. However, if LCZ696 proves ineffective in heart failure with preserved ejection fraction, then more attention should be paid to targeting of comorbid disease, to the individual phenotypes, to the causes underlying disease with preserved ejection fraction, or to the aging process itself, which could be the ultimate determinant of prognosis in these patients.
Dr. John G.F. Cleland and Dr. Andrew L. Clark are with the department of cardiology at Castle Hill Hospital in Kingston-Upon-Hull, United Kingdom. These remarks were adapted from a editorial accompanying the PARAMOUNT report (Lancet 2012 Aug. 26 [ http://dx.doi.org/10.1016/ S0140-6736(12)61349-X ]). Dr. Cleland disclosed that he has received honoraria from Novartis. Dr. Clark stated that he has no relevant financial conflicts of interest.
The positive signals from PARAMOUNT will surely trigger a definitive trial. However, what will the comparator be? Valsartan, a drug not known to be effective for heart failure with preserved ejection fraction? This comparison would show whether there was an advantage to adding a neprilysin inhibitor, but would not provide evidence that valsartan was useful in patients with heart failure with preserved ejection fraction. ACE inhibitors, which seem to have some effect in disease with preserved ejection fraction? An increase in diuretic dose – perhaps the best method of improving symptoms in a congested patient? Or simply placebo? A placebo-controlled design would be the easiest to interpret, but could be confounded by the widespread use of rennin-angiotensin-aldosterone system antagonists in patients with heart failure with preserved ejection fraction, often for problems such as hypertension and peripheral edema. Such background treatment might not easily be withdrawn, rendering enrollment difficult.
Another trial, in patients with heart failure with reduced ejection fraction and raised plasma natriuretic peptides, will show whether LCZ696 is superior to enalapril. If trials in disease with both preserved and reduced ejection fraction are positive (and use the same comparator), cardiac phenotype could become less important than plasma concentration of natriuretic peptides for management of heart failure. However, if LCZ696 proves ineffective in heart failure with preserved ejection fraction, then more attention should be paid to targeting of comorbid disease, to the individual phenotypes, to the causes underlying disease with preserved ejection fraction, or to the aging process itself, which could be the ultimate determinant of prognosis in these patients.
Dr. John G.F. Cleland and Dr. Andrew L. Clark are with the department of cardiology at Castle Hill Hospital in Kingston-Upon-Hull, United Kingdom. These remarks were adapted from a editorial accompanying the PARAMOUNT report (Lancet 2012 Aug. 26 [ http://dx.doi.org/10.1016/ S0140-6736(12)61349-X ]). Dr. Cleland disclosed that he has received honoraria from Novartis. Dr. Clark stated that he has no relevant financial conflicts of interest.
Heart failure patients with preserved ejection who received an investigational agent LCA696 experienced a significant reduction of NT-proBNP at 12 weeks, compared with those who received valsartan, a randomized, multicenter, phase II trial demonstrated.
In addition, a reduction in left atrial size at 36 weeks was observed in patients in the LCA696 group, compared with those who received the angiotensin receptor blocker, researchers led by Dr. Scott Solomon of the cardiovascular division at Brigham and Women’s Hospital, Boston, reported in a study published online Aug. 26, 2012, in the Lancet. The study was simultaneously presented at the annual congress of the European Society of Cardiology.
"Present treatment of heart failure with preserved ejection fraction remains both symptom based and empiric, with no specific treatment approved for this indication," the researchers wrote. "Although ACE inhibitors and ARBs have been associated with symptom improvement, increased functional capacity, and reduction in admission to hospital in these patients, existing guidelines state that no treatment has convincingly been shown to reduce morbidity or mortality.
In a phase II trial known as PARAMOUNT, Dr. Solomon and his associates at 65 centers in 13 countries set out to assess the efficacy and safety of LCZ696 in 301 heart failure patients with preserved ejection fraction. LCZ696 is a first-in-class angiotensin receptor neprilysin inhibitor that includes valsartan. The researchers hypothesized that LCA696 works by augmenting the active natriuretic peptides to improve myocardial relaxation and reduce hypertrophy. They recruited patients from November 2009 through March 2011.
Patients were eligible for PARAMOUNT if they were at least 40 years of age, had New York Heart Association class II-III heart failure, a left ventricular ejection fraction (LVEF) of 45% or higher, and an NT-proBNP greater than 400 pg/mL (Lancet 2012 Aug. 26 [http://dx.doi.org/10.1016/S0140-6736(12)61227-6]).
After randomization, 149 patients were started on 50 mg LCZ696 twice daily and 152 were started on 40 mg valsartan twice daily and titrated to their final doses of 200 mg LCZ696 twice daily or 160 mg valsartan twice daily over a period of 2-4 weeks. All patients were treated for 36 weeks; the primary end point was change in NT-proBNP from baseline to 12 weeks. This end point was selected "because raised natriuretic peptide concentrations are associated with adverse outcomes in patients with heart failure, including those with preserved ejection fraction, and reductions in NT-proBNP have been associated with improved outcomes in heart failure," the researchers explained.
Dr. Solomon and his associates reported complete data from 134 patients in the LCZ696 group and 132 patients in the valsartan group. The mean age of patients in both groups was 71 years and more than half (57%) were women. The change in NT-proBNP from baseline to week 12 was significantly reduced in patients in the LCZ696 group (from 783 to 605 pg/mL), compared with patients in the valsartan group (from 862 to 835 pg/mL). This translated into a significant ratio of change between the two treatment groups of 0.77. By week 36, the differences in NT-proBNP between the two groups were no longer significant.
After 36 weeks of treatment, patients in the LCZ696 group experienced significant reductions in left atrial volume and in left atrial dimension, compared with their counterparts in the valsartan group. "Left atrial size has been one of the most powerful predictors of outcome in heart failure, including heart failure with preserved ejection fraction," the researchers wrote. "The reported reduction in left atrial size offers support to the notion that LCZ696 had a sustained physiological benefit to 36 weeks."
LCZ696 was well tolerated and the proportion of patients who experienced one or more serious adverse events was similar between the two groups (15% among those in the LCZ696 group vs. 20% among those in the valsartan group).
Novartis funded the study. Dr. Solomon and six of his coauthors disclosed having received research support from, and have consulted for, Novartis, which is developing LCZ696. Three other coauthors are employed by the company.
Heart failure patients with preserved ejection who received an investigational agent LCA696 experienced a significant reduction of NT-proBNP at 12 weeks, compared with those who received valsartan, a randomized, multicenter, phase II trial demonstrated.
In addition, a reduction in left atrial size at 36 weeks was observed in patients in the LCA696 group, compared with those who received the angiotensin receptor blocker, researchers led by Dr. Scott Solomon of the cardiovascular division at Brigham and Women’s Hospital, Boston, reported in a study published online Aug. 26, 2012, in the Lancet. The study was simultaneously presented at the annual congress of the European Society of Cardiology.
"Present treatment of heart failure with preserved ejection fraction remains both symptom based and empiric, with no specific treatment approved for this indication," the researchers wrote. "Although ACE inhibitors and ARBs have been associated with symptom improvement, increased functional capacity, and reduction in admission to hospital in these patients, existing guidelines state that no treatment has convincingly been shown to reduce morbidity or mortality.
In a phase II trial known as PARAMOUNT, Dr. Solomon and his associates at 65 centers in 13 countries set out to assess the efficacy and safety of LCZ696 in 301 heart failure patients with preserved ejection fraction. LCZ696 is a first-in-class angiotensin receptor neprilysin inhibitor that includes valsartan. The researchers hypothesized that LCA696 works by augmenting the active natriuretic peptides to improve myocardial relaxation and reduce hypertrophy. They recruited patients from November 2009 through March 2011.
Patients were eligible for PARAMOUNT if they were at least 40 years of age, had New York Heart Association class II-III heart failure, a left ventricular ejection fraction (LVEF) of 45% or higher, and an NT-proBNP greater than 400 pg/mL (Lancet 2012 Aug. 26 [http://dx.doi.org/10.1016/S0140-6736(12)61227-6]).
After randomization, 149 patients were started on 50 mg LCZ696 twice daily and 152 were started on 40 mg valsartan twice daily and titrated to their final doses of 200 mg LCZ696 twice daily or 160 mg valsartan twice daily over a period of 2-4 weeks. All patients were treated for 36 weeks; the primary end point was change in NT-proBNP from baseline to 12 weeks. This end point was selected "because raised natriuretic peptide concentrations are associated with adverse outcomes in patients with heart failure, including those with preserved ejection fraction, and reductions in NT-proBNP have been associated with improved outcomes in heart failure," the researchers explained.
Dr. Solomon and his associates reported complete data from 134 patients in the LCZ696 group and 132 patients in the valsartan group. The mean age of patients in both groups was 71 years and more than half (57%) were women. The change in NT-proBNP from baseline to week 12 was significantly reduced in patients in the LCZ696 group (from 783 to 605 pg/mL), compared with patients in the valsartan group (from 862 to 835 pg/mL). This translated into a significant ratio of change between the two treatment groups of 0.77. By week 36, the differences in NT-proBNP between the two groups were no longer significant.
After 36 weeks of treatment, patients in the LCZ696 group experienced significant reductions in left atrial volume and in left atrial dimension, compared with their counterparts in the valsartan group. "Left atrial size has been one of the most powerful predictors of outcome in heart failure, including heart failure with preserved ejection fraction," the researchers wrote. "The reported reduction in left atrial size offers support to the notion that LCZ696 had a sustained physiological benefit to 36 weeks."
LCZ696 was well tolerated and the proportion of patients who experienced one or more serious adverse events was similar between the two groups (15% among those in the LCZ696 group vs. 20% among those in the valsartan group).
Novartis funded the study. Dr. Solomon and six of his coauthors disclosed having received research support from, and have consulted for, Novartis, which is developing LCZ696. Three other coauthors are employed by the company.
FROM THE LANCET
Major Finding: The change in NT-proBNP from baseline to week 12 was significantly reduced in patients in the LCZ696 group (from 783 to 605 pg/mL), compared with patients in the valsartan group (from 862 to 835 pg/mL). This translated into a ratio of change of 0.77.
Data Source: Data are from a phase II randomized trial of 301 heart failure patients with preserved ejection fraction that compared the angiotensin receptor neprilysin inhibitor LCZ696 with valsartan.
Disclosures: Novartis funded the study. Dr. Solomon and six of his coauthors disclosed having received research support from, and have consulted for, Novartis. Three other coauthors are employed by the company.
Spinal Cord Stimulation an Option for Chronic Pain
SAN DIEGO – Sometimes the only relief for a patient who presents with chronic and recalcitrant pain comes from a course of spinal cord stimulation.
"I consider spinal cord stimulation a real home run," Dr. Allan L. Brook said at the annual meeting of the Society of Neurointerventional Surgery. "You can really help patients who have no other method of pain relief."
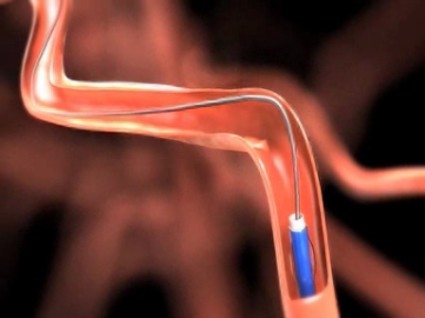
Spinal cord stimulation is a form of neuromodulation that masks the pain signals by delivering pulses of electricity via an electrode directly to the spinal cord, leading to parasthesias along the desired path. The procedure has Food and Drug Administration clearance for treating neuropathic, intractable pain in the extremities and trunk.
In describing its proposed mechanism of action, Dr. Brook, director of neurointerventional neuroradiology at Montefiore Medical Center in the Bronx, N.Y., said that the noxious afferent stimulus is masked by nonnoxious sensations produced by stimulation. This results in a conductance blockade of the spinothalamic sensory system, which in turn activates supraspinal pain-relieving centers. Stimulation also causes blockage of supraspinal or segmental autonomic nervous systems, and alters the way neurotransmitters are released.
"I consider spinal cord stimulation a real home run."
The most common indication for spinal cord stimulation is failed back surgery syndromes. "There are many fusion surgeries out there with poor results," said Dr. Brook, who is also professor of clinical radiology and neurosurgery at Albert Einstein College of Medicine, New York. "Causes may include arachnoiditis, recurrent or residual disk herniation, epidural fibrosis, and radiculopathy from any cause."
Other indications include complex regional pain syndrome type I, CRPS type II, ischemic limb pain, refractory angina, peripheral neuropathy, abdominal pain, brachial plexus/cervical pain, interstitial cystitis, phantom limb pain, postherpetic neuralgia, headache/facial pain, and chronic pain that fails medical therapy.
Contraindications for spinal cord stimulation include patients with an infection, those in whom standard pain therapy works, those with coagulation issues, those who are mentally incompetent, and those who lack health insurance, as each device costs about $20,000. Psychological exclusion criteria include patients with active psychosis or those who are suicidal, and those with major depression, mood problems, or substance abuse problems. "Insurance companies require a psychological evaluation for this procedure," Dr. Brook said.
Orientation of the pain drives placement of the stimulator’s lead tip. For example, the lead tip is positioned on C2-C5 for pain in the upper extremity, on T11-L1 for foot pain, on T9-T10 for lower extremity pain, on T8-T10 for low back pain, on T1-T2 for chest pain, on C1-C2 for occipital neuralgia, and on S2-S4 for pelvic pain.
The least invasive initial approach is to temporarily position the spinal cord stimulator for several days so that the proximal lead portion is secured to skin. If the pain relief exceeds 50% during this trial period, then a permanent spine stimulator can be placed surgically.
The main drawback to permanent placement is that patients can’t undergo an MRI, but Dr. Brook said that an MRI-compatible device is currently being developed. Complications can rarely occur, including nerve injury, epidural hematoma, wound infection, and lead migration. "All of these can be prevented with good techniques," he said.
Researchers who conducted a 20-year retrospective review of 51 studies of spinal cord stimulation concluded that the procedure had a positive effect on chronic low back pain, severe limb ischemia, refractory angina, and peripheral neuropathy (J. Neurosurg. 2004;100:254-67).
A randomized, prospective, controlled trial of spinal cord stimulation in patients who had reflex sympathetic dystrophy (now called CRPS type I) for at least 6 months found a significant benefit of decreased pain and improved function, with a P value less than .001 (N. Engl. J. Med. 2000;343:618-24).
Another trial found that neurostimulation for failed back surgery syndrome resulted in a cost savings after 2.5 years, compared with conventional medical management (Neurosurgery 2002;51:106-16).
"This is a reversible, minimally invasive procedure," Dr. Brook said of spinal cord stimulation. "It’s nondestructive, compared with neuroablation; it reduces the abuse of narcotics; and it can improve a patient’s ability to perform activities of daily living."
Dr. Brook said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Sometimes the only relief for a patient who presents with chronic and recalcitrant pain comes from a course of spinal cord stimulation.
"I consider spinal cord stimulation a real home run," Dr. Allan L. Brook said at the annual meeting of the Society of Neurointerventional Surgery. "You can really help patients who have no other method of pain relief."
Spinal cord stimulation is a form of neuromodulation that masks the pain signals by delivering pulses of electricity via an electrode directly to the spinal cord, leading to parasthesias along the desired path. The procedure has Food and Drug Administration clearance for treating neuropathic, intractable pain in the extremities and trunk.
In describing its proposed mechanism of action, Dr. Brook, director of neurointerventional neuroradiology at Montefiore Medical Center in the Bronx, N.Y., said that the noxious afferent stimulus is masked by nonnoxious sensations produced by stimulation. This results in a conductance blockade of the spinothalamic sensory system, which in turn activates supraspinal pain-relieving centers. Stimulation also causes blockage of supraspinal or segmental autonomic nervous systems, and alters the way neurotransmitters are released.
"I consider spinal cord stimulation a real home run."
The most common indication for spinal cord stimulation is failed back surgery syndromes. "There are many fusion surgeries out there with poor results," said Dr. Brook, who is also professor of clinical radiology and neurosurgery at Albert Einstein College of Medicine, New York. "Causes may include arachnoiditis, recurrent or residual disk herniation, epidural fibrosis, and radiculopathy from any cause."
Other indications include complex regional pain syndrome type I, CRPS type II, ischemic limb pain, refractory angina, peripheral neuropathy, abdominal pain, brachial plexus/cervical pain, interstitial cystitis, phantom limb pain, postherpetic neuralgia, headache/facial pain, and chronic pain that fails medical therapy.
Contraindications for spinal cord stimulation include patients with an infection, those in whom standard pain therapy works, those with coagulation issues, those who are mentally incompetent, and those who lack health insurance, as each device costs about $20,000. Psychological exclusion criteria include patients with active psychosis or those who are suicidal, and those with major depression, mood problems, or substance abuse problems. "Insurance companies require a psychological evaluation for this procedure," Dr. Brook said.
Orientation of the pain drives placement of the stimulator’s lead tip. For example, the lead tip is positioned on C2-C5 for pain in the upper extremity, on T11-L1 for foot pain, on T9-T10 for lower extremity pain, on T8-T10 for low back pain, on T1-T2 for chest pain, on C1-C2 for occipital neuralgia, and on S2-S4 for pelvic pain.
The least invasive initial approach is to temporarily position the spinal cord stimulator for several days so that the proximal lead portion is secured to skin. If the pain relief exceeds 50% during this trial period, then a permanent spine stimulator can be placed surgically.
The main drawback to permanent placement is that patients can’t undergo an MRI, but Dr. Brook said that an MRI-compatible device is currently being developed. Complications can rarely occur, including nerve injury, epidural hematoma, wound infection, and lead migration. "All of these can be prevented with good techniques," he said.
Researchers who conducted a 20-year retrospective review of 51 studies of spinal cord stimulation concluded that the procedure had a positive effect on chronic low back pain, severe limb ischemia, refractory angina, and peripheral neuropathy (J. Neurosurg. 2004;100:254-67).
A randomized, prospective, controlled trial of spinal cord stimulation in patients who had reflex sympathetic dystrophy (now called CRPS type I) for at least 6 months found a significant benefit of decreased pain and improved function, with a P value less than .001 (N. Engl. J. Med. 2000;343:618-24).
Another trial found that neurostimulation for failed back surgery syndrome resulted in a cost savings after 2.5 years, compared with conventional medical management (Neurosurgery 2002;51:106-16).
"This is a reversible, minimally invasive procedure," Dr. Brook said of spinal cord stimulation. "It’s nondestructive, compared with neuroablation; it reduces the abuse of narcotics; and it can improve a patient’s ability to perform activities of daily living."
Dr. Brook said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Sometimes the only relief for a patient who presents with chronic and recalcitrant pain comes from a course of spinal cord stimulation.
"I consider spinal cord stimulation a real home run," Dr. Allan L. Brook said at the annual meeting of the Society of Neurointerventional Surgery. "You can really help patients who have no other method of pain relief."
Spinal cord stimulation is a form of neuromodulation that masks the pain signals by delivering pulses of electricity via an electrode directly to the spinal cord, leading to parasthesias along the desired path. The procedure has Food and Drug Administration clearance for treating neuropathic, intractable pain in the extremities and trunk.
In describing its proposed mechanism of action, Dr. Brook, director of neurointerventional neuroradiology at Montefiore Medical Center in the Bronx, N.Y., said that the noxious afferent stimulus is masked by nonnoxious sensations produced by stimulation. This results in a conductance blockade of the spinothalamic sensory system, which in turn activates supraspinal pain-relieving centers. Stimulation also causes blockage of supraspinal or segmental autonomic nervous systems, and alters the way neurotransmitters are released.
"I consider spinal cord stimulation a real home run."
The most common indication for spinal cord stimulation is failed back surgery syndromes. "There are many fusion surgeries out there with poor results," said Dr. Brook, who is also professor of clinical radiology and neurosurgery at Albert Einstein College of Medicine, New York. "Causes may include arachnoiditis, recurrent or residual disk herniation, epidural fibrosis, and radiculopathy from any cause."
Other indications include complex regional pain syndrome type I, CRPS type II, ischemic limb pain, refractory angina, peripheral neuropathy, abdominal pain, brachial plexus/cervical pain, interstitial cystitis, phantom limb pain, postherpetic neuralgia, headache/facial pain, and chronic pain that fails medical therapy.
Contraindications for spinal cord stimulation include patients with an infection, those in whom standard pain therapy works, those with coagulation issues, those who are mentally incompetent, and those who lack health insurance, as each device costs about $20,000. Psychological exclusion criteria include patients with active psychosis or those who are suicidal, and those with major depression, mood problems, or substance abuse problems. "Insurance companies require a psychological evaluation for this procedure," Dr. Brook said.
Orientation of the pain drives placement of the stimulator’s lead tip. For example, the lead tip is positioned on C2-C5 for pain in the upper extremity, on T11-L1 for foot pain, on T9-T10 for lower extremity pain, on T8-T10 for low back pain, on T1-T2 for chest pain, on C1-C2 for occipital neuralgia, and on S2-S4 for pelvic pain.
The least invasive initial approach is to temporarily position the spinal cord stimulator for several days so that the proximal lead portion is secured to skin. If the pain relief exceeds 50% during this trial period, then a permanent spine stimulator can be placed surgically.
The main drawback to permanent placement is that patients can’t undergo an MRI, but Dr. Brook said that an MRI-compatible device is currently being developed. Complications can rarely occur, including nerve injury, epidural hematoma, wound infection, and lead migration. "All of these can be prevented with good techniques," he said.
Researchers who conducted a 20-year retrospective review of 51 studies of spinal cord stimulation concluded that the procedure had a positive effect on chronic low back pain, severe limb ischemia, refractory angina, and peripheral neuropathy (J. Neurosurg. 2004;100:254-67).
A randomized, prospective, controlled trial of spinal cord stimulation in patients who had reflex sympathetic dystrophy (now called CRPS type I) for at least 6 months found a significant benefit of decreased pain and improved function, with a P value less than .001 (N. Engl. J. Med. 2000;343:618-24).
Another trial found that neurostimulation for failed back surgery syndrome resulted in a cost savings after 2.5 years, compared with conventional medical management (Neurosurgery 2002;51:106-16).
"This is a reversible, minimally invasive procedure," Dr. Brook said of spinal cord stimulation. "It’s nondestructive, compared with neuroablation; it reduces the abuse of narcotics; and it can improve a patient’s ability to perform activities of daily living."
Dr. Brook said that he had no relevant financial conflicts to disclose.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE SOCIETY OF NEUROINTERVENTIONAL SURGERY
CT Perfusion Findings Drive Mechanical Thrombectomy for Stroke
SAN DIEGO – An approach that uses CT perfusion findings to select patients for mechanical thrombectomy resulted in effective, safe treatment of stroke patients beyond the traditional 7- to 8-hour treatment window, results from a single-center study demonstrated.
"CT perfusion–based patient selection for endovascular therapy enables us to treat patients who would otherwise have not received such therapy based on time criteria," Jordan Magarik said at the annual meeting of the Society of Neurointerventional Surgery. "We have seen improved outcomes over historical controls and improved safety as well. The bottom line is that patient selection is paramount. When patients are selected based solely on CT perfusion imaging, we are finding very similar rates of good functional outcome regardless of when they were treated, whether it’s 8 or 18 hours after symptom onset."
When the Medical University of South Carolina (MUSC) in Charleston launched its Comprehensive Stroke Center in 2008, clinicians there devised an alternate method of selecting patients solely based on the CT perfusion findings, regardless of their time from symptom onset. For the current study, Mr. Magarik, who is a medical student at MUSC, and his associates reviewed the records of 140 stroke patients who were treated at the stroke center from 2008 to 2011. The mean age of the patients was 67 years. Data of interest included age, concurrent administration of IV tissue plasminogen activator (TPA), time to treatment, presenting National Institutes of Health Stroke Scale (NIHSS) score, 90-day modified Rankin score (mRS), and angiographic recanalization rates. The primary intra-arterial device used was the Penumbra System.
All 140 patients underwent mechanical thrombectomy; 54 received IV TPA in addition to mechanical thrombectomy and 86 only underwent mechanical thrombectomy. The mean NIHSS score was 16.2, and the mean time to treatment was 11.3 hours, which is well beyond the traditional 7- to 8-hour time window used in mechanical device trials, said Mr. Magarik.
The majority of patients (87%) achieved a partial or full recanalization and 10% of patients suffered symptomatic intracranial hemorrhage, which is consistent with previous trials.
More than one-third of patients (38%) achieved a 90-day mRS of 0-2, and 53% achieved a 90-day mRS of 0-3. The mortality rate was 25%, which is consistent with previous trials.
When the researchers divided patients on the basis of mean time from symptom onset to treatment, they observed no statistically significant differences in the rates of patients with mRS of 0-2 (31% among those treated within a 7-hour window vs. 42% among those treated beyond a 7-hour window) or mRS of 0-3 (49% among those treated within a 7-hour window vs. 55% among those treated beyond a 7-hour window).
"Many patients in the later time group are presenting 15 or 18 hours out from symptom onset, yet they are still achieving a very similar rate of good functional outcome," Mr. Magarik said. "We believe this is because they were selected based on their CT perfusion findings."
Mr. Magarik said that he had no relevant financial disclosures to make.
SAN DIEGO – An approach that uses CT perfusion findings to select patients for mechanical thrombectomy resulted in effective, safe treatment of stroke patients beyond the traditional 7- to 8-hour treatment window, results from a single-center study demonstrated.
"CT perfusion–based patient selection for endovascular therapy enables us to treat patients who would otherwise have not received such therapy based on time criteria," Jordan Magarik said at the annual meeting of the Society of Neurointerventional Surgery. "We have seen improved outcomes over historical controls and improved safety as well. The bottom line is that patient selection is paramount. When patients are selected based solely on CT perfusion imaging, we are finding very similar rates of good functional outcome regardless of when they were treated, whether it’s 8 or 18 hours after symptom onset."
When the Medical University of South Carolina (MUSC) in Charleston launched its Comprehensive Stroke Center in 2008, clinicians there devised an alternate method of selecting patients solely based on the CT perfusion findings, regardless of their time from symptom onset. For the current study, Mr. Magarik, who is a medical student at MUSC, and his associates reviewed the records of 140 stroke patients who were treated at the stroke center from 2008 to 2011. The mean age of the patients was 67 years. Data of interest included age, concurrent administration of IV tissue plasminogen activator (TPA), time to treatment, presenting National Institutes of Health Stroke Scale (NIHSS) score, 90-day modified Rankin score (mRS), and angiographic recanalization rates. The primary intra-arterial device used was the Penumbra System.
All 140 patients underwent mechanical thrombectomy; 54 received IV TPA in addition to mechanical thrombectomy and 86 only underwent mechanical thrombectomy. The mean NIHSS score was 16.2, and the mean time to treatment was 11.3 hours, which is well beyond the traditional 7- to 8-hour time window used in mechanical device trials, said Mr. Magarik.
The majority of patients (87%) achieved a partial or full recanalization and 10% of patients suffered symptomatic intracranial hemorrhage, which is consistent with previous trials.
More than one-third of patients (38%) achieved a 90-day mRS of 0-2, and 53% achieved a 90-day mRS of 0-3. The mortality rate was 25%, which is consistent with previous trials.
When the researchers divided patients on the basis of mean time from symptom onset to treatment, they observed no statistically significant differences in the rates of patients with mRS of 0-2 (31% among those treated within a 7-hour window vs. 42% among those treated beyond a 7-hour window) or mRS of 0-3 (49% among those treated within a 7-hour window vs. 55% among those treated beyond a 7-hour window).
"Many patients in the later time group are presenting 15 or 18 hours out from symptom onset, yet they are still achieving a very similar rate of good functional outcome," Mr. Magarik said. "We believe this is because they were selected based on their CT perfusion findings."
Mr. Magarik said that he had no relevant financial disclosures to make.
SAN DIEGO – An approach that uses CT perfusion findings to select patients for mechanical thrombectomy resulted in effective, safe treatment of stroke patients beyond the traditional 7- to 8-hour treatment window, results from a single-center study demonstrated.
"CT perfusion–based patient selection for endovascular therapy enables us to treat patients who would otherwise have not received such therapy based on time criteria," Jordan Magarik said at the annual meeting of the Society of Neurointerventional Surgery. "We have seen improved outcomes over historical controls and improved safety as well. The bottom line is that patient selection is paramount. When patients are selected based solely on CT perfusion imaging, we are finding very similar rates of good functional outcome regardless of when they were treated, whether it’s 8 or 18 hours after symptom onset."
When the Medical University of South Carolina (MUSC) in Charleston launched its Comprehensive Stroke Center in 2008, clinicians there devised an alternate method of selecting patients solely based on the CT perfusion findings, regardless of their time from symptom onset. For the current study, Mr. Magarik, who is a medical student at MUSC, and his associates reviewed the records of 140 stroke patients who were treated at the stroke center from 2008 to 2011. The mean age of the patients was 67 years. Data of interest included age, concurrent administration of IV tissue plasminogen activator (TPA), time to treatment, presenting National Institutes of Health Stroke Scale (NIHSS) score, 90-day modified Rankin score (mRS), and angiographic recanalization rates. The primary intra-arterial device used was the Penumbra System.
All 140 patients underwent mechanical thrombectomy; 54 received IV TPA in addition to mechanical thrombectomy and 86 only underwent mechanical thrombectomy. The mean NIHSS score was 16.2, and the mean time to treatment was 11.3 hours, which is well beyond the traditional 7- to 8-hour time window used in mechanical device trials, said Mr. Magarik.
The majority of patients (87%) achieved a partial or full recanalization and 10% of patients suffered symptomatic intracranial hemorrhage, which is consistent with previous trials.
More than one-third of patients (38%) achieved a 90-day mRS of 0-2, and 53% achieved a 90-day mRS of 0-3. The mortality rate was 25%, which is consistent with previous trials.
When the researchers divided patients on the basis of mean time from symptom onset to treatment, they observed no statistically significant differences in the rates of patients with mRS of 0-2 (31% among those treated within a 7-hour window vs. 42% among those treated beyond a 7-hour window) or mRS of 0-3 (49% among those treated within a 7-hour window vs. 55% among those treated beyond a 7-hour window).
"Many patients in the later time group are presenting 15 or 18 hours out from symptom onset, yet they are still achieving a very similar rate of good functional outcome," Mr. Magarik said. "We believe this is because they were selected based on their CT perfusion findings."
Mr. Magarik said that he had no relevant financial disclosures to make.
AT THE ANNUAL MEETING OF THE SOCIETY OF NEUROINTERVENTIONAL SURGERY
Solitaire Clot Remover Effective for Large Artery Stroke
SAN DIEGO – When used as a first-line choice for the treatment of acute ischemic stroke secondary to large artery occlusion, the Solitaire FR revascularization device was safe and offered good recanalization rates and clinical outcomes, a multicenter study showed.
The Solitaire FR device, which mechanically removes blood clots from blocked vessels, received CE Mark approval in Europe and has been commercialized internationally by Covidien since November 2009. The Solitaire FR device was cleared in March of 2012 by the Food and Drug Administration.
At the annual meeting of the Society of Neurointerventional Surgery, Dr. Vitor Mendes Pereira presented findings from 141 consecutive patients with acute ischemic stroke who were treated with the Solitaire FR device as first-line treatment to restore blood flow at clinical centers located in Geneva; Barcelona; Essen, Germany; Montpellier, France; Stockholm; and Bern, Switzerland, between March 2009 and July 2010. The researchers used an independent clinical lab to evaluate Thrombolysis in Cerebral Infarction (TICI) scores on pre- and postprocedural angiograms.
Dr. Pereira, one of the investigators who heads the section of interventional neuroradiology at University Hospital of Geneva, said that complete recanalization was defined as TICI 2b or 3 post treatment. He and his associates defined good early neurologic outcome as a National Institutes of Health Stroke Scale (NIHSS) score improvement of 10 or more points or a NIHSS score of 0 or 1 at hospital discharge. They defined favorable outcome as a modified Rankin Scale score of 2 or less at day 90.
The mean age of the 141 patients was 66 years; 44% were women. Their median NIHSS score was 18, and 52% of patients were treated after previous treatment using intravenous tissue plasminogen activator (TPA). Most of the occlusions were located in the anterior circulation (86%), and 46% corresponded to M1 occlusions.
Dr. Pereira reported successful revascularization in 85% of patients with a TICI of 2b or greater, 96% for those with a Thrombolysis in Myocardial Infarction (TIMI) score of 2 or greater, and 83% for those with an Arterial Occlusive Lesion (AOL) score of 3.
Nearly three-quarters of cases (74%) were performed using a balloon-guided catheter. Technical success was achieved in 97.8% of patients, and the median time to groin puncture was 40 minutes. The mean number of passes was 1.8, and 77% of patients achieved recanalization success with up to two passes. Rescue therapy was required in seven cases (4.9%).
Nearly one-third of patients (32%) achieved a good neurologic outcome at hospital discharge and 55% had a modified Rankin Scale score of 2 or less at 90 days. The rate of death at 90 days was 26%, and 6% experienced intracranial hemorrhage.
The study was funded by Covidien. Dr. Pereira disclosed that he is a consultant for Covidien and is the principal investigator for two studies funded by the company.
SAN DIEGO – When used as a first-line choice for the treatment of acute ischemic stroke secondary to large artery occlusion, the Solitaire FR revascularization device was safe and offered good recanalization rates and clinical outcomes, a multicenter study showed.
The Solitaire FR device, which mechanically removes blood clots from blocked vessels, received CE Mark approval in Europe and has been commercialized internationally by Covidien since November 2009. The Solitaire FR device was cleared in March of 2012 by the Food and Drug Administration.
At the annual meeting of the Society of Neurointerventional Surgery, Dr. Vitor Mendes Pereira presented findings from 141 consecutive patients with acute ischemic stroke who were treated with the Solitaire FR device as first-line treatment to restore blood flow at clinical centers located in Geneva; Barcelona; Essen, Germany; Montpellier, France; Stockholm; and Bern, Switzerland, between March 2009 and July 2010. The researchers used an independent clinical lab to evaluate Thrombolysis in Cerebral Infarction (TICI) scores on pre- and postprocedural angiograms.
Dr. Pereira, one of the investigators who heads the section of interventional neuroradiology at University Hospital of Geneva, said that complete recanalization was defined as TICI 2b or 3 post treatment. He and his associates defined good early neurologic outcome as a National Institutes of Health Stroke Scale (NIHSS) score improvement of 10 or more points or a NIHSS score of 0 or 1 at hospital discharge. They defined favorable outcome as a modified Rankin Scale score of 2 or less at day 90.
The mean age of the 141 patients was 66 years; 44% were women. Their median NIHSS score was 18, and 52% of patients were treated after previous treatment using intravenous tissue plasminogen activator (TPA). Most of the occlusions were located in the anterior circulation (86%), and 46% corresponded to M1 occlusions.
Dr. Pereira reported successful revascularization in 85% of patients with a TICI of 2b or greater, 96% for those with a Thrombolysis in Myocardial Infarction (TIMI) score of 2 or greater, and 83% for those with an Arterial Occlusive Lesion (AOL) score of 3.
Nearly three-quarters of cases (74%) were performed using a balloon-guided catheter. Technical success was achieved in 97.8% of patients, and the median time to groin puncture was 40 minutes. The mean number of passes was 1.8, and 77% of patients achieved recanalization success with up to two passes. Rescue therapy was required in seven cases (4.9%).
Nearly one-third of patients (32%) achieved a good neurologic outcome at hospital discharge and 55% had a modified Rankin Scale score of 2 or less at 90 days. The rate of death at 90 days was 26%, and 6% experienced intracranial hemorrhage.
The study was funded by Covidien. Dr. Pereira disclosed that he is a consultant for Covidien and is the principal investigator for two studies funded by the company.
SAN DIEGO – When used as a first-line choice for the treatment of acute ischemic stroke secondary to large artery occlusion, the Solitaire FR revascularization device was safe and offered good recanalization rates and clinical outcomes, a multicenter study showed.
The Solitaire FR device, which mechanically removes blood clots from blocked vessels, received CE Mark approval in Europe and has been commercialized internationally by Covidien since November 2009. The Solitaire FR device was cleared in March of 2012 by the Food and Drug Administration.
At the annual meeting of the Society of Neurointerventional Surgery, Dr. Vitor Mendes Pereira presented findings from 141 consecutive patients with acute ischemic stroke who were treated with the Solitaire FR device as first-line treatment to restore blood flow at clinical centers located in Geneva; Barcelona; Essen, Germany; Montpellier, France; Stockholm; and Bern, Switzerland, between March 2009 and July 2010. The researchers used an independent clinical lab to evaluate Thrombolysis in Cerebral Infarction (TICI) scores on pre- and postprocedural angiograms.
Dr. Pereira, one of the investigators who heads the section of interventional neuroradiology at University Hospital of Geneva, said that complete recanalization was defined as TICI 2b or 3 post treatment. He and his associates defined good early neurologic outcome as a National Institutes of Health Stroke Scale (NIHSS) score improvement of 10 or more points or a NIHSS score of 0 or 1 at hospital discharge. They defined favorable outcome as a modified Rankin Scale score of 2 or less at day 90.
The mean age of the 141 patients was 66 years; 44% were women. Their median NIHSS score was 18, and 52% of patients were treated after previous treatment using intravenous tissue plasminogen activator (TPA). Most of the occlusions were located in the anterior circulation (86%), and 46% corresponded to M1 occlusions.
Dr. Pereira reported successful revascularization in 85% of patients with a TICI of 2b or greater, 96% for those with a Thrombolysis in Myocardial Infarction (TIMI) score of 2 or greater, and 83% for those with an Arterial Occlusive Lesion (AOL) score of 3.
Nearly three-quarters of cases (74%) were performed using a balloon-guided catheter. Technical success was achieved in 97.8% of patients, and the median time to groin puncture was 40 minutes. The mean number of passes was 1.8, and 77% of patients achieved recanalization success with up to two passes. Rescue therapy was required in seven cases (4.9%).
Nearly one-third of patients (32%) achieved a good neurologic outcome at hospital discharge and 55% had a modified Rankin Scale score of 2 or less at 90 days. The rate of death at 90 days was 26%, and 6% experienced intracranial hemorrhage.
The study was funded by Covidien. Dr. Pereira disclosed that he is a consultant for Covidien and is the principal investigator for two studies funded by the company.
AT THE ANNUAL MEETING OF THE SOCIETY OF NEUROINTERVENTIONAL SURGERY
Major Finding: Nearly one-third of patients (32%) achieved a good neurological outcome and 55% had a modified Rankin Scale score of 2 or less at 90 days.
Data Source: The analysis involved 141 consecutive patients with acute ischemic stroke who were treated with the Solitaire FR device as first-line treatment to restore blood flow at six clinical centers in Europe.
Disclosures: The study was funded by Covidien. Dr. Pereira disclosed that he is a consultant for Covidien and is the principal investigator for two studies funded by the company.
MRI Profile Helps Target Candidates for Endovascular Treatment
SAN DIEGO – Stroke patients who are likely to benefit from endovascular reperfusion can be identified on the basis of their MRI profile, results from a multicenter study demonstrated.
"These results are largely independent of stroke onset time," Dr. Michael P. Marks said at the annual meeting of the Society of Neurointerventional Surgery. "Our belief is that if the right patients are identified, it can be shown that endovascular therapy will be of benefit in the treatment of their acute strokes."
Endovascular treatment is increasingly used in the management of acute stroke, said Dr. Marks, an interventional neuroradiologist at Stanford (Calif.) University. "A randomized trial has shown benefit for intra-arterial thrombolytic agents in this setting," he said (JAMA 1999;282:2003-11). "Single-armed prospective studies have shown that thrombectomy devices improve outcome in patients when reperfusion is successfully attained. Nevertheless, tremendous controversy exists because there is an absence of any study with randomized data and concurrent controls. In addition, many questions remain as to which candidates are best suited for revascularization and whether imaging can help identify those patients," Dr. Marks said.
Against this backdrop, he and his associates at nine clinical sites carried out the DEFUSE-2 (Diffusion and Perfusion Imaging Evaluation for Understanding Stroke Evolution Study-2) to identify patients who might fit into a randomized controlled trial. DEFUSE-2 is a prospective study of acute stroke patients who underwent endovascular therapy following MRI. The primary hypothesis was that a target mismatch profile (TMM) could be identified where patients had a relatively small area of injured tissue as seen on diffusion-weighted imaging (DWI) relative to a larger volume of ischemic tissue that was still salvageable as identified by perfusion-weighted imaging (PWI); and that patients with a TMM would respond more favorably to endovascular reperfusion therapy than patients without a TMM.
To be eligible for the trial, patients had to have endovascular therapy started within 12 hours of an anterior circulation stroke. They underwent a baseline MRI within 90 minutes of endovascular therapy, a second MRI following reperfusion in the catheter lab, and a third MRI at 5 days to assess infarct volume. This was followed by clinical assessments at day 30 and day 90 using the National Institutes of Health Stroke Scale (NIHSS) and the modified Rankin Scale (mRS).
A TMM was defined as PWI volume over the DWI volume of 1.8 or greater, when the PWI volume had a Tmax of more than 6 seconds. PWI reperfusion was defined as a reduction in PWI lesion volume of greater than 50% between baseline and follow-up.
The investigators defined reperfusion as a Thrombolysis in Cerebral Infarction (TICI) score of 2b or 3. In this study, TICI 1 was defined as perfusion past the initial obstruction but little or slow distal perfusion with limited branch filling. TICI 2a was defined as partial perfusion of less than half of the vascular distribution of the occluded artery, TICI 2b was defined as partial perfusion of half or more of the vascular distribution of the occluded artery, and TICI 3 was defined as full perfusion filling of all distal branches.
Dr. Marks reported on outcomes from 78 patients who had a target mismatch and 21 who did not have a target mismatch. The researchers found that reperfusion was associated with a significantly increased odds of a favorable clinical response (odds ratio, 2.8), which was defined as an improvement in NIHSS score between baseline and day 30 of 8 points or more, or an NIHSS score of 0-1 at day 30. This outcome was driven by the target mismatch group, which had significantly greater odds of a favorable response to reperfusion than the no target mismatch group (OR, 5.0 vs. 0.2; P = .004).
A significantly higher percentage of patients in the target mismatch group achieved a 90-day mRS of 0-2 when there was reperfusion, compared with their counterparts in the no target mismatch group (57% vs. 25%), as well as when there was no reperfusion (31% vs. 22%).
The median time to the onset of vascular therapy was 6 hours. "When we divided patients into those started less than 6 hours versus those started greater than 6 hours, the results were very comparable," he said.
Dr. Marks also reported that by day 90, 29% of patients a TICI score of 0-1 achieved an mRS score of 0-2, compared with 25% of patients with a TICI score of 2a, 61% of patients with a score of 2b, and 50% of those with a score of 3. "This was driven by having a target mismatch," he said.
Dr. Marks and his associates are proposing a randomized controlled trial in which the primary hypothesis is that treatment with an approved thrombectomy device within 18-24 hours is more likely to result in a good clinical outcome at 90 days when patients are selected on the basis of a favorable MRI profile.
"The time is right to do this study, because current stentrievers have a high rate of recanalization," Dr. Marks said. "Physiologic imaging can identify patients who will benefit from recanalization in an extended time period."
DEFUSE-2 was funded by the National Institute of Neurological Disorders and Stroke. Dr. Marks said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Stroke patients who are likely to benefit from endovascular reperfusion can be identified on the basis of their MRI profile, results from a multicenter study demonstrated.
"These results are largely independent of stroke onset time," Dr. Michael P. Marks said at the annual meeting of the Society of Neurointerventional Surgery. "Our belief is that if the right patients are identified, it can be shown that endovascular therapy will be of benefit in the treatment of their acute strokes."
Endovascular treatment is increasingly used in the management of acute stroke, said Dr. Marks, an interventional neuroradiologist at Stanford (Calif.) University. "A randomized trial has shown benefit for intra-arterial thrombolytic agents in this setting," he said (JAMA 1999;282:2003-11). "Single-armed prospective studies have shown that thrombectomy devices improve outcome in patients when reperfusion is successfully attained. Nevertheless, tremendous controversy exists because there is an absence of any study with randomized data and concurrent controls. In addition, many questions remain as to which candidates are best suited for revascularization and whether imaging can help identify those patients," Dr. Marks said.
Against this backdrop, he and his associates at nine clinical sites carried out the DEFUSE-2 (Diffusion and Perfusion Imaging Evaluation for Understanding Stroke Evolution Study-2) to identify patients who might fit into a randomized controlled trial. DEFUSE-2 is a prospective study of acute stroke patients who underwent endovascular therapy following MRI. The primary hypothesis was that a target mismatch profile (TMM) could be identified where patients had a relatively small area of injured tissue as seen on diffusion-weighted imaging (DWI) relative to a larger volume of ischemic tissue that was still salvageable as identified by perfusion-weighted imaging (PWI); and that patients with a TMM would respond more favorably to endovascular reperfusion therapy than patients without a TMM.
To be eligible for the trial, patients had to have endovascular therapy started within 12 hours of an anterior circulation stroke. They underwent a baseline MRI within 90 minutes of endovascular therapy, a second MRI following reperfusion in the catheter lab, and a third MRI at 5 days to assess infarct volume. This was followed by clinical assessments at day 30 and day 90 using the National Institutes of Health Stroke Scale (NIHSS) and the modified Rankin Scale (mRS).
A TMM was defined as PWI volume over the DWI volume of 1.8 or greater, when the PWI volume had a Tmax of more than 6 seconds. PWI reperfusion was defined as a reduction in PWI lesion volume of greater than 50% between baseline and follow-up.
The investigators defined reperfusion as a Thrombolysis in Cerebral Infarction (TICI) score of 2b or 3. In this study, TICI 1 was defined as perfusion past the initial obstruction but little or slow distal perfusion with limited branch filling. TICI 2a was defined as partial perfusion of less than half of the vascular distribution of the occluded artery, TICI 2b was defined as partial perfusion of half or more of the vascular distribution of the occluded artery, and TICI 3 was defined as full perfusion filling of all distal branches.
Dr. Marks reported on outcomes from 78 patients who had a target mismatch and 21 who did not have a target mismatch. The researchers found that reperfusion was associated with a significantly increased odds of a favorable clinical response (odds ratio, 2.8), which was defined as an improvement in NIHSS score between baseline and day 30 of 8 points or more, or an NIHSS score of 0-1 at day 30. This outcome was driven by the target mismatch group, which had significantly greater odds of a favorable response to reperfusion than the no target mismatch group (OR, 5.0 vs. 0.2; P = .004).
A significantly higher percentage of patients in the target mismatch group achieved a 90-day mRS of 0-2 when there was reperfusion, compared with their counterparts in the no target mismatch group (57% vs. 25%), as well as when there was no reperfusion (31% vs. 22%).
The median time to the onset of vascular therapy was 6 hours. "When we divided patients into those started less than 6 hours versus those started greater than 6 hours, the results were very comparable," he said.
Dr. Marks also reported that by day 90, 29% of patients a TICI score of 0-1 achieved an mRS score of 0-2, compared with 25% of patients with a TICI score of 2a, 61% of patients with a score of 2b, and 50% of those with a score of 3. "This was driven by having a target mismatch," he said.
Dr. Marks and his associates are proposing a randomized controlled trial in which the primary hypothesis is that treatment with an approved thrombectomy device within 18-24 hours is more likely to result in a good clinical outcome at 90 days when patients are selected on the basis of a favorable MRI profile.
"The time is right to do this study, because current stentrievers have a high rate of recanalization," Dr. Marks said. "Physiologic imaging can identify patients who will benefit from recanalization in an extended time period."
DEFUSE-2 was funded by the National Institute of Neurological Disorders and Stroke. Dr. Marks said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Stroke patients who are likely to benefit from endovascular reperfusion can be identified on the basis of their MRI profile, results from a multicenter study demonstrated.
"These results are largely independent of stroke onset time," Dr. Michael P. Marks said at the annual meeting of the Society of Neurointerventional Surgery. "Our belief is that if the right patients are identified, it can be shown that endovascular therapy will be of benefit in the treatment of their acute strokes."
Endovascular treatment is increasingly used in the management of acute stroke, said Dr. Marks, an interventional neuroradiologist at Stanford (Calif.) University. "A randomized trial has shown benefit for intra-arterial thrombolytic agents in this setting," he said (JAMA 1999;282:2003-11). "Single-armed prospective studies have shown that thrombectomy devices improve outcome in patients when reperfusion is successfully attained. Nevertheless, tremendous controversy exists because there is an absence of any study with randomized data and concurrent controls. In addition, many questions remain as to which candidates are best suited for revascularization and whether imaging can help identify those patients," Dr. Marks said.
Against this backdrop, he and his associates at nine clinical sites carried out the DEFUSE-2 (Diffusion and Perfusion Imaging Evaluation for Understanding Stroke Evolution Study-2) to identify patients who might fit into a randomized controlled trial. DEFUSE-2 is a prospective study of acute stroke patients who underwent endovascular therapy following MRI. The primary hypothesis was that a target mismatch profile (TMM) could be identified where patients had a relatively small area of injured tissue as seen on diffusion-weighted imaging (DWI) relative to a larger volume of ischemic tissue that was still salvageable as identified by perfusion-weighted imaging (PWI); and that patients with a TMM would respond more favorably to endovascular reperfusion therapy than patients without a TMM.
To be eligible for the trial, patients had to have endovascular therapy started within 12 hours of an anterior circulation stroke. They underwent a baseline MRI within 90 minutes of endovascular therapy, a second MRI following reperfusion in the catheter lab, and a third MRI at 5 days to assess infarct volume. This was followed by clinical assessments at day 30 and day 90 using the National Institutes of Health Stroke Scale (NIHSS) and the modified Rankin Scale (mRS).
A TMM was defined as PWI volume over the DWI volume of 1.8 or greater, when the PWI volume had a Tmax of more than 6 seconds. PWI reperfusion was defined as a reduction in PWI lesion volume of greater than 50% between baseline and follow-up.
The investigators defined reperfusion as a Thrombolysis in Cerebral Infarction (TICI) score of 2b or 3. In this study, TICI 1 was defined as perfusion past the initial obstruction but little or slow distal perfusion with limited branch filling. TICI 2a was defined as partial perfusion of less than half of the vascular distribution of the occluded artery, TICI 2b was defined as partial perfusion of half or more of the vascular distribution of the occluded artery, and TICI 3 was defined as full perfusion filling of all distal branches.
Dr. Marks reported on outcomes from 78 patients who had a target mismatch and 21 who did not have a target mismatch. The researchers found that reperfusion was associated with a significantly increased odds of a favorable clinical response (odds ratio, 2.8), which was defined as an improvement in NIHSS score between baseline and day 30 of 8 points or more, or an NIHSS score of 0-1 at day 30. This outcome was driven by the target mismatch group, which had significantly greater odds of a favorable response to reperfusion than the no target mismatch group (OR, 5.0 vs. 0.2; P = .004).
A significantly higher percentage of patients in the target mismatch group achieved a 90-day mRS of 0-2 when there was reperfusion, compared with their counterparts in the no target mismatch group (57% vs. 25%), as well as when there was no reperfusion (31% vs. 22%).
The median time to the onset of vascular therapy was 6 hours. "When we divided patients into those started less than 6 hours versus those started greater than 6 hours, the results were very comparable," he said.
Dr. Marks also reported that by day 90, 29% of patients a TICI score of 0-1 achieved an mRS score of 0-2, compared with 25% of patients with a TICI score of 2a, 61% of patients with a score of 2b, and 50% of those with a score of 3. "This was driven by having a target mismatch," he said.
Dr. Marks and his associates are proposing a randomized controlled trial in which the primary hypothesis is that treatment with an approved thrombectomy device within 18-24 hours is more likely to result in a good clinical outcome at 90 days when patients are selected on the basis of a favorable MRI profile.
"The time is right to do this study, because current stentrievers have a high rate of recanalization," Dr. Marks said. "Physiologic imaging can identify patients who will benefit from recanalization in an extended time period."
DEFUSE-2 was funded by the National Institute of Neurological Disorders and Stroke. Dr. Marks said that he had no relevant financial conflicts to disclose.
AT THE ANNUAL MEETING OF THE SOCIETY OF NEUROINTERVENTIONAL SURGERY
Pain Scales: What to Ponder When Making Your Pick
SAN DIEGO – Of the many scales at a clinician’s disposal to measure acute pain, the three most commonly used are the Numerical Rating Scale, the Verbal Rating Scale, and the Visual Analog Scale, Dr. Jeffrey A. Stone said at the annual meeting of the Society of Neurointerventional Surgery.
"All of these scales have been shown to be statistically reliable and valid," said Dr. Stone, associate professor of neurointerventional surgery in the radiology department at the Mayo Clinic, Jacksonville, Fla. In his clinical experience, most patients prefer the Numerical Rating Scale (NRS) and the Verbal Rating Scale (VRS) because they are easy to use. "The other advantage is that these can be conducted by telephone or electronic diaries," he said.
The NRS is a familiar and commonly used 0-10 scale, where 0 = no pain, 1-3 = mild pain, 4-6 = moderate pain, and 7-10 = severe pain. "If patients tell you, ‘I’m a 5 out of 10,’ that can be difficult to gauge, particularly in the elderly," Dr. Stone said. "The VRS, a four-scale system ranging from no pain up to severe pain, is somewhat simpler and correlates well with the NRS."
With the Visual Analog Scale, patients are asked to make a vertical slash on a 100-mm line to denote their level of pain. "I use this scale a lot, but it can be cumbersome, particularly with follow-up," he said.
Factors to consider in the backdrop of pain intensity include rescue analgesics, which may be prescribed by other physicians for sleep or anxiety, or may be used to prevent pain from increased activity or to treat unrelated pain. "Another factor is concomitant pain treatments, such as acupuncture and chiropractic treatments," Dr. Stone said. "In addition, patients enrolled in the placebo group of a clinical trial are generally expected to have more pain medication use compared with those in an efficacious treatment group."
Other distinct components of pain include pain sensation and pain affect. Pain sensation "is the quality of the pain, such as burning, throbbing, or sharp pain versus dull pain," Dr. Stone said. "There are also temporal aspects to pain, such as variability of intensity over time; time to onset of meaningful pain relief; durability of pain relief; and the frequency, duration, and intensity of pain episodes. Pain affect is the mental distress caused by the pain."
Global pain assessments for pain sensation and pain affect include a modification of the McGill Pain Questionnaire (MPQ), known as the short-form MPQ, and the Brief Pain Inventory (BPI), which was adapted from the Wisconsin Brief Pain Questionnaire. The short-form MPQ contains 15 sensory and affective descriptors, while the BPI "does a much better job measuring the temporal aspect of pain and is often used in conjunction with the short-form MPQ," Dr. Stone said.
Two other core pain outcome domains are physical function and emotional function. Effective outcome measures for these domains include the Oswestry Disability Index (ODI), the Short Form-36 (SF-36), the Roland-Morris Disability Questionnaire (RMQ) and the Pain Disability Index (PDI).
The ODI, a 10-item questionnaire, "has been used in many pain trials," he said. "It looks at pain intensity but also other things such as lifting, the ability to walk, social life, sexual activity, and sleep cycle. It is a very accurate way to look at a patient’s global disability from pain."
He described the SF-36 as "a little bit more cumbersome for patients to complete" in measuring physical and emotional function. This tool provides an eight-scale profile of functional health and well-being scores, as well as a psychometric-based physical and mental health summary.
The 24-item RMQ consists of yes/no questions intended to measure self-perceived disability, while the 7-question PDI measures pain interference in physical and psychosocial role performance.
In a later interview, Dr. Stone said that the NRS, VRS, and VAS instruments can be used in hospitalized patients. Outcome measures such as the ODI and the RMQ "would not be very useful, as they ask many functional questions such as sex life [and] activity level, which would not be applicable to a hospitalized patient."
Dr. Stone said that he had no relevant financial disclosures to make.
SAN DIEGO – Of the many scales at a clinician’s disposal to measure acute pain, the three most commonly used are the Numerical Rating Scale, the Verbal Rating Scale, and the Visual Analog Scale, Dr. Jeffrey A. Stone said at the annual meeting of the Society of Neurointerventional Surgery.
"All of these scales have been shown to be statistically reliable and valid," said Dr. Stone, associate professor of neurointerventional surgery in the radiology department at the Mayo Clinic, Jacksonville, Fla. In his clinical experience, most patients prefer the Numerical Rating Scale (NRS) and the Verbal Rating Scale (VRS) because they are easy to use. "The other advantage is that these can be conducted by telephone or electronic diaries," he said.
The NRS is a familiar and commonly used 0-10 scale, where 0 = no pain, 1-3 = mild pain, 4-6 = moderate pain, and 7-10 = severe pain. "If patients tell you, ‘I’m a 5 out of 10,’ that can be difficult to gauge, particularly in the elderly," Dr. Stone said. "The VRS, a four-scale system ranging from no pain up to severe pain, is somewhat simpler and correlates well with the NRS."
With the Visual Analog Scale, patients are asked to make a vertical slash on a 100-mm line to denote their level of pain. "I use this scale a lot, but it can be cumbersome, particularly with follow-up," he said.
Factors to consider in the backdrop of pain intensity include rescue analgesics, which may be prescribed by other physicians for sleep or anxiety, or may be used to prevent pain from increased activity or to treat unrelated pain. "Another factor is concomitant pain treatments, such as acupuncture and chiropractic treatments," Dr. Stone said. "In addition, patients enrolled in the placebo group of a clinical trial are generally expected to have more pain medication use compared with those in an efficacious treatment group."
Other distinct components of pain include pain sensation and pain affect. Pain sensation "is the quality of the pain, such as burning, throbbing, or sharp pain versus dull pain," Dr. Stone said. "There are also temporal aspects to pain, such as variability of intensity over time; time to onset of meaningful pain relief; durability of pain relief; and the frequency, duration, and intensity of pain episodes. Pain affect is the mental distress caused by the pain."
Global pain assessments for pain sensation and pain affect include a modification of the McGill Pain Questionnaire (MPQ), known as the short-form MPQ, and the Brief Pain Inventory (BPI), which was adapted from the Wisconsin Brief Pain Questionnaire. The short-form MPQ contains 15 sensory and affective descriptors, while the BPI "does a much better job measuring the temporal aspect of pain and is often used in conjunction with the short-form MPQ," Dr. Stone said.
Two other core pain outcome domains are physical function and emotional function. Effective outcome measures for these domains include the Oswestry Disability Index (ODI), the Short Form-36 (SF-36), the Roland-Morris Disability Questionnaire (RMQ) and the Pain Disability Index (PDI).
The ODI, a 10-item questionnaire, "has been used in many pain trials," he said. "It looks at pain intensity but also other things such as lifting, the ability to walk, social life, sexual activity, and sleep cycle. It is a very accurate way to look at a patient’s global disability from pain."
He described the SF-36 as "a little bit more cumbersome for patients to complete" in measuring physical and emotional function. This tool provides an eight-scale profile of functional health and well-being scores, as well as a psychometric-based physical and mental health summary.
The 24-item RMQ consists of yes/no questions intended to measure self-perceived disability, while the 7-question PDI measures pain interference in physical and psychosocial role performance.
In a later interview, Dr. Stone said that the NRS, VRS, and VAS instruments can be used in hospitalized patients. Outcome measures such as the ODI and the RMQ "would not be very useful, as they ask many functional questions such as sex life [and] activity level, which would not be applicable to a hospitalized patient."
Dr. Stone said that he had no relevant financial disclosures to make.
SAN DIEGO – Of the many scales at a clinician’s disposal to measure acute pain, the three most commonly used are the Numerical Rating Scale, the Verbal Rating Scale, and the Visual Analog Scale, Dr. Jeffrey A. Stone said at the annual meeting of the Society of Neurointerventional Surgery.
"All of these scales have been shown to be statistically reliable and valid," said Dr. Stone, associate professor of neurointerventional surgery in the radiology department at the Mayo Clinic, Jacksonville, Fla. In his clinical experience, most patients prefer the Numerical Rating Scale (NRS) and the Verbal Rating Scale (VRS) because they are easy to use. "The other advantage is that these can be conducted by telephone or electronic diaries," he said.
The NRS is a familiar and commonly used 0-10 scale, where 0 = no pain, 1-3 = mild pain, 4-6 = moderate pain, and 7-10 = severe pain. "If patients tell you, ‘I’m a 5 out of 10,’ that can be difficult to gauge, particularly in the elderly," Dr. Stone said. "The VRS, a four-scale system ranging from no pain up to severe pain, is somewhat simpler and correlates well with the NRS."
With the Visual Analog Scale, patients are asked to make a vertical slash on a 100-mm line to denote their level of pain. "I use this scale a lot, but it can be cumbersome, particularly with follow-up," he said.
Factors to consider in the backdrop of pain intensity include rescue analgesics, which may be prescribed by other physicians for sleep or anxiety, or may be used to prevent pain from increased activity or to treat unrelated pain. "Another factor is concomitant pain treatments, such as acupuncture and chiropractic treatments," Dr. Stone said. "In addition, patients enrolled in the placebo group of a clinical trial are generally expected to have more pain medication use compared with those in an efficacious treatment group."
Other distinct components of pain include pain sensation and pain affect. Pain sensation "is the quality of the pain, such as burning, throbbing, or sharp pain versus dull pain," Dr. Stone said. "There are also temporal aspects to pain, such as variability of intensity over time; time to onset of meaningful pain relief; durability of pain relief; and the frequency, duration, and intensity of pain episodes. Pain affect is the mental distress caused by the pain."
Global pain assessments for pain sensation and pain affect include a modification of the McGill Pain Questionnaire (MPQ), known as the short-form MPQ, and the Brief Pain Inventory (BPI), which was adapted from the Wisconsin Brief Pain Questionnaire. The short-form MPQ contains 15 sensory and affective descriptors, while the BPI "does a much better job measuring the temporal aspect of pain and is often used in conjunction with the short-form MPQ," Dr. Stone said.
Two other core pain outcome domains are physical function and emotional function. Effective outcome measures for these domains include the Oswestry Disability Index (ODI), the Short Form-36 (SF-36), the Roland-Morris Disability Questionnaire (RMQ) and the Pain Disability Index (PDI).
The ODI, a 10-item questionnaire, "has been used in many pain trials," he said. "It looks at pain intensity but also other things such as lifting, the ability to walk, social life, sexual activity, and sleep cycle. It is a very accurate way to look at a patient’s global disability from pain."
He described the SF-36 as "a little bit more cumbersome for patients to complete" in measuring physical and emotional function. This tool provides an eight-scale profile of functional health and well-being scores, as well as a psychometric-based physical and mental health summary.
The 24-item RMQ consists of yes/no questions intended to measure self-perceived disability, while the 7-question PDI measures pain interference in physical and psychosocial role performance.
In a later interview, Dr. Stone said that the NRS, VRS, and VAS instruments can be used in hospitalized patients. Outcome measures such as the ODI and the RMQ "would not be very useful, as they ask many functional questions such as sex life [and] activity level, which would not be applicable to a hospitalized patient."
Dr. Stone said that he had no relevant financial disclosures to make.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE SOCIETY OF NEUROINTERVENTIONAL SURGERY
Treatment Guidelines for Thyroid Dysfunction in Pregnancy Updated
When treating women with thyroid dysfunction during and after pregnancy, clinicians should use caution interpreting serum-free thyroxine levels, use propylthiouracil as the first-line drug during for hyperthyroidism in the first trimester, and advise breastfeeding women to maintain a daily intake of 250 mcg of iodine to ensure breast milk provides 100 mcg of iodine/day to the infant.
These mark some of the changes the Endocrine Society made to its 2007 Clinical Practice Guideline (CPG) for the management of thyroid disease during pregnancy and the postpartum.
"Pregnancy may affect the course of thyroid diseases and conversely, thyroid diseases may affect the course of pregnancy," Dr. Leslie De Groot, lead researcher from the University of Rhode Island, Kingston, said in a prepared statement. "Pregnant women may be under the care of multiple health care professionals including obstetricians, nurse midwives, family practitioners and endocrinologists making the development of guidelines all the more critical."
In order to update the Endocrine Society’s 2007 CPG, Dr. De Groot and a task force of 12 other experts reviewed existing medical literature on the topic and followed the approach of the U.S. Preventive Services Task Force and the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) system to evaluate the strength of each recommendation. The effort, published online in the Aug. 12 issue of the Journal of Clinical Endocrinology & Metabolism, included collaboration with the Asia and Oceania Thyroid Association, European Thyroid Association, and Latin American Thyroid Society (J. Clin. Endocrinol. Metab. 2012 Aug. 1;97:2543-65 [doi: 10.1210/jc.2011-2803]).
"At present, with the exception of studies on iodide nutrition, only a few prospective, randomized intervention trials have been published in this area [of thyroid dysfunction during pregnancy]," the authors wrote. "We are aware of large-scale prospective intervention trials that are ongoing. Nevertheless, in the past decade many high-quality studies have modified older dogmas and profoundly changed the ways in which these patients are managed."
Key recommendations in the 2012 clinical practice guideline that differ from the 2007 version include the following:
• Use caution in the interpretation of serum-free T4 levels during pregnancy. "Each laboratory should establish trimester-specific reference ranges for pregnant women if using a free T4 assay," the authors wrote in a supplemental index in which they summarized changes between the 2007 and 2012 versions of the guideline. "The non-pregnant total T4 range (5-12 mcg/dL or 50-150 nmol/L) can be adapted in the second and third trimesters by multiplying this range by 1.5-fold. Alternatively, the free thyroxine index (‘adjusted T4’) appears to be a reliable assay during pregnancy."
• Use propylthiouracil (PTU), if available, as the first-line drug for treatment of hyperthyroidism during the first trimester. This is because of the possible association of methimazole (MMI) with congenital abnormalities. MMI "may also be prescribed if PTU is not available or if a patient cannot tolerate or has an adverse response to PTU," the authors wrote. "Recent analyses reported by the FDA indicate that PTU may rarely be associated with severe liver toxicity. For this reason, we recommend that clinicians should change treatment of patients from PTU to MMI after the completion of first trimester. Available data indicate that MMI and PTU are equally efficacious in treatment of pregnant women."
• Breastfeeding women should maintain a daily intake of 250 mcg of iodine. This ensures that breast milk provides 100 mcg iodine/day to the infant. "These changes are in response to recent publications indicating that some vitamin-mineral preparations used during pregnancy may not provide adequate iodine intake, and that iodine supplements should be continued during breastfeeding," the authors explained.
• Measure thyroid receptor antibodies (TRAb) before 22 weeks’ gestational age in a subset of mothers. This includes mothers with either current Graves’ disease, a history of Graves’ disease and treatment with 131-I (radioiodine) or thyroidectomy before pregnancy, a previous neonate with Graves’ disease, or previously elevated TRAb. This approach is recommended because thyroid receptor antibodies "freely cross the placenta and can stimulate or inhibit the fetal thyroid," the authors wrote. "Women who have negative TRAb and do not require antithyroid drugs have a very low risk of fetal or neonatal thyroid dysfunction. This change makes more explicit the timing and indications for measurement of TRAb in pregnancy."
The authors could not reach agreement on universal screening recommendations for all newly pregnant women. Some recommend screening of all pregnant women for serum TSH abnormalities by the 9th week or at the time of their first visit while others recommended neither for nor against universal screening of all pregnant women for TSH abnormalities at the time of their first visit.
Despite their differences on universal screening recommendations, the authors unanimously agreed that clinicians should perform targeted screening of high-risk women during the prenatal and perinatal periods. This includes women over age 30 years and those with a family history or autoimmune thyroid disease or hypothyroidism; a goiter; thyroid antibodies, primarily thyroid peroxidase antibodies; symptoms or clinical signs suggestive of thyroid hypofunction; type 1 diabetes mellitus, or other autoimmune disorders; those with infertility; a prior history of preterm delivery; prior therapeutic head or neck irradiation or prior thyroid surgery; and those currently receiving levothyroxine replacement.
No member of the task force disclosed relevant financial conflicts of interest.
When treating women with thyroid dysfunction during and after pregnancy, clinicians should use caution interpreting serum-free thyroxine levels, use propylthiouracil as the first-line drug during for hyperthyroidism in the first trimester, and advise breastfeeding women to maintain a daily intake of 250 mcg of iodine to ensure breast milk provides 100 mcg of iodine/day to the infant.
These mark some of the changes the Endocrine Society made to its 2007 Clinical Practice Guideline (CPG) for the management of thyroid disease during pregnancy and the postpartum.
"Pregnancy may affect the course of thyroid diseases and conversely, thyroid diseases may affect the course of pregnancy," Dr. Leslie De Groot, lead researcher from the University of Rhode Island, Kingston, said in a prepared statement. "Pregnant women may be under the care of multiple health care professionals including obstetricians, nurse midwives, family practitioners and endocrinologists making the development of guidelines all the more critical."
In order to update the Endocrine Society’s 2007 CPG, Dr. De Groot and a task force of 12 other experts reviewed existing medical literature on the topic and followed the approach of the U.S. Preventive Services Task Force and the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) system to evaluate the strength of each recommendation. The effort, published online in the Aug. 12 issue of the Journal of Clinical Endocrinology & Metabolism, included collaboration with the Asia and Oceania Thyroid Association, European Thyroid Association, and Latin American Thyroid Society (J. Clin. Endocrinol. Metab. 2012 Aug. 1;97:2543-65 [doi: 10.1210/jc.2011-2803]).
"At present, with the exception of studies on iodide nutrition, only a few prospective, randomized intervention trials have been published in this area [of thyroid dysfunction during pregnancy]," the authors wrote. "We are aware of large-scale prospective intervention trials that are ongoing. Nevertheless, in the past decade many high-quality studies have modified older dogmas and profoundly changed the ways in which these patients are managed."
Key recommendations in the 2012 clinical practice guideline that differ from the 2007 version include the following:
• Use caution in the interpretation of serum-free T4 levels during pregnancy. "Each laboratory should establish trimester-specific reference ranges for pregnant women if using a free T4 assay," the authors wrote in a supplemental index in which they summarized changes between the 2007 and 2012 versions of the guideline. "The non-pregnant total T4 range (5-12 mcg/dL or 50-150 nmol/L) can be adapted in the second and third trimesters by multiplying this range by 1.5-fold. Alternatively, the free thyroxine index (‘adjusted T4’) appears to be a reliable assay during pregnancy."
• Use propylthiouracil (PTU), if available, as the first-line drug for treatment of hyperthyroidism during the first trimester. This is because of the possible association of methimazole (MMI) with congenital abnormalities. MMI "may also be prescribed if PTU is not available or if a patient cannot tolerate or has an adverse response to PTU," the authors wrote. "Recent analyses reported by the FDA indicate that PTU may rarely be associated with severe liver toxicity. For this reason, we recommend that clinicians should change treatment of patients from PTU to MMI after the completion of first trimester. Available data indicate that MMI and PTU are equally efficacious in treatment of pregnant women."
• Breastfeeding women should maintain a daily intake of 250 mcg of iodine. This ensures that breast milk provides 100 mcg iodine/day to the infant. "These changes are in response to recent publications indicating that some vitamin-mineral preparations used during pregnancy may not provide adequate iodine intake, and that iodine supplements should be continued during breastfeeding," the authors explained.
• Measure thyroid receptor antibodies (TRAb) before 22 weeks’ gestational age in a subset of mothers. This includes mothers with either current Graves’ disease, a history of Graves’ disease and treatment with 131-I (radioiodine) or thyroidectomy before pregnancy, a previous neonate with Graves’ disease, or previously elevated TRAb. This approach is recommended because thyroid receptor antibodies "freely cross the placenta and can stimulate or inhibit the fetal thyroid," the authors wrote. "Women who have negative TRAb and do not require antithyroid drugs have a very low risk of fetal or neonatal thyroid dysfunction. This change makes more explicit the timing and indications for measurement of TRAb in pregnancy."
The authors could not reach agreement on universal screening recommendations for all newly pregnant women. Some recommend screening of all pregnant women for serum TSH abnormalities by the 9th week or at the time of their first visit while others recommended neither for nor against universal screening of all pregnant women for TSH abnormalities at the time of their first visit.
Despite their differences on universal screening recommendations, the authors unanimously agreed that clinicians should perform targeted screening of high-risk women during the prenatal and perinatal periods. This includes women over age 30 years and those with a family history or autoimmune thyroid disease or hypothyroidism; a goiter; thyroid antibodies, primarily thyroid peroxidase antibodies; symptoms or clinical signs suggestive of thyroid hypofunction; type 1 diabetes mellitus, or other autoimmune disorders; those with infertility; a prior history of preterm delivery; prior therapeutic head or neck irradiation or prior thyroid surgery; and those currently receiving levothyroxine replacement.
No member of the task force disclosed relevant financial conflicts of interest.
When treating women with thyroid dysfunction during and after pregnancy, clinicians should use caution interpreting serum-free thyroxine levels, use propylthiouracil as the first-line drug during for hyperthyroidism in the first trimester, and advise breastfeeding women to maintain a daily intake of 250 mcg of iodine to ensure breast milk provides 100 mcg of iodine/day to the infant.
These mark some of the changes the Endocrine Society made to its 2007 Clinical Practice Guideline (CPG) for the management of thyroid disease during pregnancy and the postpartum.
"Pregnancy may affect the course of thyroid diseases and conversely, thyroid diseases may affect the course of pregnancy," Dr. Leslie De Groot, lead researcher from the University of Rhode Island, Kingston, said in a prepared statement. "Pregnant women may be under the care of multiple health care professionals including obstetricians, nurse midwives, family practitioners and endocrinologists making the development of guidelines all the more critical."
In order to update the Endocrine Society’s 2007 CPG, Dr. De Groot and a task force of 12 other experts reviewed existing medical literature on the topic and followed the approach of the U.S. Preventive Services Task Force and the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) system to evaluate the strength of each recommendation. The effort, published online in the Aug. 12 issue of the Journal of Clinical Endocrinology & Metabolism, included collaboration with the Asia and Oceania Thyroid Association, European Thyroid Association, and Latin American Thyroid Society (J. Clin. Endocrinol. Metab. 2012 Aug. 1;97:2543-65 [doi: 10.1210/jc.2011-2803]).
"At present, with the exception of studies on iodide nutrition, only a few prospective, randomized intervention trials have been published in this area [of thyroid dysfunction during pregnancy]," the authors wrote. "We are aware of large-scale prospective intervention trials that are ongoing. Nevertheless, in the past decade many high-quality studies have modified older dogmas and profoundly changed the ways in which these patients are managed."
Key recommendations in the 2012 clinical practice guideline that differ from the 2007 version include the following:
• Use caution in the interpretation of serum-free T4 levels during pregnancy. "Each laboratory should establish trimester-specific reference ranges for pregnant women if using a free T4 assay," the authors wrote in a supplemental index in which they summarized changes between the 2007 and 2012 versions of the guideline. "The non-pregnant total T4 range (5-12 mcg/dL or 50-150 nmol/L) can be adapted in the second and third trimesters by multiplying this range by 1.5-fold. Alternatively, the free thyroxine index (‘adjusted T4’) appears to be a reliable assay during pregnancy."
• Use propylthiouracil (PTU), if available, as the first-line drug for treatment of hyperthyroidism during the first trimester. This is because of the possible association of methimazole (MMI) with congenital abnormalities. MMI "may also be prescribed if PTU is not available or if a patient cannot tolerate or has an adverse response to PTU," the authors wrote. "Recent analyses reported by the FDA indicate that PTU may rarely be associated with severe liver toxicity. For this reason, we recommend that clinicians should change treatment of patients from PTU to MMI after the completion of first trimester. Available data indicate that MMI and PTU are equally efficacious in treatment of pregnant women."
• Breastfeeding women should maintain a daily intake of 250 mcg of iodine. This ensures that breast milk provides 100 mcg iodine/day to the infant. "These changes are in response to recent publications indicating that some vitamin-mineral preparations used during pregnancy may not provide adequate iodine intake, and that iodine supplements should be continued during breastfeeding," the authors explained.
• Measure thyroid receptor antibodies (TRAb) before 22 weeks’ gestational age in a subset of mothers. This includes mothers with either current Graves’ disease, a history of Graves’ disease and treatment with 131-I (radioiodine) or thyroidectomy before pregnancy, a previous neonate with Graves’ disease, or previously elevated TRAb. This approach is recommended because thyroid receptor antibodies "freely cross the placenta and can stimulate or inhibit the fetal thyroid," the authors wrote. "Women who have negative TRAb and do not require antithyroid drugs have a very low risk of fetal or neonatal thyroid dysfunction. This change makes more explicit the timing and indications for measurement of TRAb in pregnancy."
The authors could not reach agreement on universal screening recommendations for all newly pregnant women. Some recommend screening of all pregnant women for serum TSH abnormalities by the 9th week or at the time of their first visit while others recommended neither for nor against universal screening of all pregnant women for TSH abnormalities at the time of their first visit.
Despite their differences on universal screening recommendations, the authors unanimously agreed that clinicians should perform targeted screening of high-risk women during the prenatal and perinatal periods. This includes women over age 30 years and those with a family history or autoimmune thyroid disease or hypothyroidism; a goiter; thyroid antibodies, primarily thyroid peroxidase antibodies; symptoms or clinical signs suggestive of thyroid hypofunction; type 1 diabetes mellitus, or other autoimmune disorders; those with infertility; a prior history of preterm delivery; prior therapeutic head or neck irradiation or prior thyroid surgery; and those currently receiving levothyroxine replacement.
No member of the task force disclosed relevant financial conflicts of interest.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY AND METABOLISM
New Light Shed on Impact of Psychosis Family History
Among first-episode psychosis patients, a family history of the condition negatively affects age at onset, negative symptoms, and the duration of illness and psychosis that are untreated, results from a large study showed.
The study "adds to an existing body of research suggesting that [family history] of psychosis is associated with a younger age at onset of psychosis, and is one of the first to demonstrate that FH acts similarly on age at onset at the prodrome," Michelle L. Esterberg, Ph.D., and her coinvestigator wrote (Psychiatry Res. 2012;197:23-8). "This is especially important given that earlier age at onset has adverse prognostic implications for illness course and outcome."
The investigators examined the impact of FH on the clinical presentation and help-seeking behaviors of 152 first-episode psychosis (FEP) patients who were hospitalized in a psychiatry unit of a large, university-affiliated psychiatry hospital or a suburban county psychiatric crisis stabilization unit. Patients were eligible for the trial if they were aged 18-40 years, could speak English, had an MMSE (Mini-Mental State Examination) score of 23 or greater, and were able to give informed consent.
Scales and measures used in the analysis included an interviewer-administered questionnaire, the SCID-I (Structured Clinical Interview for DSM-IV Axis I Disorders), the SOS (Symptom Onset in Schizophrenia) inventory, and the PANSS (Positive and Negative Syndrome Scale), wrote Dr. Esterberg of the VA Puget Sound Health Care System, Seattle.
The mean age of the study participants was 23 years, 90% were black, 75% were men, and 82% were hospitalized involuntarily. More than half (58%) were diagnosed with schizophrenia, and 15% were determined to have at least one first-degree family member with schizophrenia or another psychotic disorder.
The researchers reported that patients with a first-degree FH of psychosis had a significantly younger age at onset of the prodrome, compared with those who had no such history (mean age, 16 vs. 19 years, respectively; P less than .05), yet they did not differ significantly in duration of the prodromal period. Patients with a first-degree FH of psychosis also had a significantly younger age at onset of psychosis, compared with those who had no such FH (mean age, 18 vs. 22 years, respectively; P less than .01).
The investigators found that FH and sex interacted to influence the severity of negative symptoms, but not positive symptoms. Among patients overall, for example, men showed significantly more severe symptoms, compared with women (22 vs. 20%, respectively; P less than .01). When the analysis was limited to patients with FH, men had significantly more negative symptoms, compared with women (26% vs. 17%, respectively; P less than .01).
No significant difference was found in the duration of untreated illness (DUI) between patients with and without FH of psychosis, but patients with FH of psychosis had a longer duration of untreated psychosis (DUP), compared with patients who did not have FH of psychosis (P less than .05). Once again, sex differences emerged among patients with FH, with men having significantly more negative symptoms than did women (26% vs. 17%; P less than .01).
"It seems that FEP with a FH of psychosis spend a longer period of time with untreated psychosis relative to FEP patients without a FH, but statistically do not have an overall longer [duration of untreated illness]," the authors concluded. "Furthermore, the current findings are the first to show that sex of the patient should be taken into account when examining the relationships between FH and [duration of untreated illness/DUP] in that males with a FH of psychosis had a significantly longer [duration of untreated illness] and DUP relative to males with no FH of psychosis."
The researchers acknowledged certain limitations of the study, including its retrospective design, the fact that "assessing the presence of FH can ... be quite difficult, and [that] data collected from patients alone (without family member informants) may be less reliable. However, we made every effort to interview one or two family members in addition to the patient when possible to ensure that the most accurate data on FH were obtained."
They went on to recommend that "future research should focus on attempting to understand potential mediators and moderators of FH and its influence on the clinical presentation in schizophrenia."
The study was funded by the National Institute of Mental Health. The authors declared no relevant financial conflicts of interest.
Among first-episode psychosis patients, a family history of the condition negatively affects age at onset, negative symptoms, and the duration of illness and psychosis that are untreated, results from a large study showed.
The study "adds to an existing body of research suggesting that [family history] of psychosis is associated with a younger age at onset of psychosis, and is one of the first to demonstrate that FH acts similarly on age at onset at the prodrome," Michelle L. Esterberg, Ph.D., and her coinvestigator wrote (Psychiatry Res. 2012;197:23-8). "This is especially important given that earlier age at onset has adverse prognostic implications for illness course and outcome."
The investigators examined the impact of FH on the clinical presentation and help-seeking behaviors of 152 first-episode psychosis (FEP) patients who were hospitalized in a psychiatry unit of a large, university-affiliated psychiatry hospital or a suburban county psychiatric crisis stabilization unit. Patients were eligible for the trial if they were aged 18-40 years, could speak English, had an MMSE (Mini-Mental State Examination) score of 23 or greater, and were able to give informed consent.
Scales and measures used in the analysis included an interviewer-administered questionnaire, the SCID-I (Structured Clinical Interview for DSM-IV Axis I Disorders), the SOS (Symptom Onset in Schizophrenia) inventory, and the PANSS (Positive and Negative Syndrome Scale), wrote Dr. Esterberg of the VA Puget Sound Health Care System, Seattle.
The mean age of the study participants was 23 years, 90% were black, 75% were men, and 82% were hospitalized involuntarily. More than half (58%) were diagnosed with schizophrenia, and 15% were determined to have at least one first-degree family member with schizophrenia or another psychotic disorder.
The researchers reported that patients with a first-degree FH of psychosis had a significantly younger age at onset of the prodrome, compared with those who had no such history (mean age, 16 vs. 19 years, respectively; P less than .05), yet they did not differ significantly in duration of the prodromal period. Patients with a first-degree FH of psychosis also had a significantly younger age at onset of psychosis, compared with those who had no such FH (mean age, 18 vs. 22 years, respectively; P less than .01).
The investigators found that FH and sex interacted to influence the severity of negative symptoms, but not positive symptoms. Among patients overall, for example, men showed significantly more severe symptoms, compared with women (22 vs. 20%, respectively; P less than .01). When the analysis was limited to patients with FH, men had significantly more negative symptoms, compared with women (26% vs. 17%, respectively; P less than .01).
No significant difference was found in the duration of untreated illness (DUI) between patients with and without FH of psychosis, but patients with FH of psychosis had a longer duration of untreated psychosis (DUP), compared with patients who did not have FH of psychosis (P less than .05). Once again, sex differences emerged among patients with FH, with men having significantly more negative symptoms than did women (26% vs. 17%; P less than .01).
"It seems that FEP with a FH of psychosis spend a longer period of time with untreated psychosis relative to FEP patients without a FH, but statistically do not have an overall longer [duration of untreated illness]," the authors concluded. "Furthermore, the current findings are the first to show that sex of the patient should be taken into account when examining the relationships between FH and [duration of untreated illness/DUP] in that males with a FH of psychosis had a significantly longer [duration of untreated illness] and DUP relative to males with no FH of psychosis."
The researchers acknowledged certain limitations of the study, including its retrospective design, the fact that "assessing the presence of FH can ... be quite difficult, and [that] data collected from patients alone (without family member informants) may be less reliable. However, we made every effort to interview one or two family members in addition to the patient when possible to ensure that the most accurate data on FH were obtained."
They went on to recommend that "future research should focus on attempting to understand potential mediators and moderators of FH and its influence on the clinical presentation in schizophrenia."
The study was funded by the National Institute of Mental Health. The authors declared no relevant financial conflicts of interest.
Among first-episode psychosis patients, a family history of the condition negatively affects age at onset, negative symptoms, and the duration of illness and psychosis that are untreated, results from a large study showed.
The study "adds to an existing body of research suggesting that [family history] of psychosis is associated with a younger age at onset of psychosis, and is one of the first to demonstrate that FH acts similarly on age at onset at the prodrome," Michelle L. Esterberg, Ph.D., and her coinvestigator wrote (Psychiatry Res. 2012;197:23-8). "This is especially important given that earlier age at onset has adverse prognostic implications for illness course and outcome."
The investigators examined the impact of FH on the clinical presentation and help-seeking behaviors of 152 first-episode psychosis (FEP) patients who were hospitalized in a psychiatry unit of a large, university-affiliated psychiatry hospital or a suburban county psychiatric crisis stabilization unit. Patients were eligible for the trial if they were aged 18-40 years, could speak English, had an MMSE (Mini-Mental State Examination) score of 23 or greater, and were able to give informed consent.
Scales and measures used in the analysis included an interviewer-administered questionnaire, the SCID-I (Structured Clinical Interview for DSM-IV Axis I Disorders), the SOS (Symptom Onset in Schizophrenia) inventory, and the PANSS (Positive and Negative Syndrome Scale), wrote Dr. Esterberg of the VA Puget Sound Health Care System, Seattle.
The mean age of the study participants was 23 years, 90% were black, 75% were men, and 82% were hospitalized involuntarily. More than half (58%) were diagnosed with schizophrenia, and 15% were determined to have at least one first-degree family member with schizophrenia or another psychotic disorder.
The researchers reported that patients with a first-degree FH of psychosis had a significantly younger age at onset of the prodrome, compared with those who had no such history (mean age, 16 vs. 19 years, respectively; P less than .05), yet they did not differ significantly in duration of the prodromal period. Patients with a first-degree FH of psychosis also had a significantly younger age at onset of psychosis, compared with those who had no such FH (mean age, 18 vs. 22 years, respectively; P less than .01).
The investigators found that FH and sex interacted to influence the severity of negative symptoms, but not positive symptoms. Among patients overall, for example, men showed significantly more severe symptoms, compared with women (22 vs. 20%, respectively; P less than .01). When the analysis was limited to patients with FH, men had significantly more negative symptoms, compared with women (26% vs. 17%, respectively; P less than .01).
No significant difference was found in the duration of untreated illness (DUI) between patients with and without FH of psychosis, but patients with FH of psychosis had a longer duration of untreated psychosis (DUP), compared with patients who did not have FH of psychosis (P less than .05). Once again, sex differences emerged among patients with FH, with men having significantly more negative symptoms than did women (26% vs. 17%; P less than .01).
"It seems that FEP with a FH of psychosis spend a longer period of time with untreated psychosis relative to FEP patients without a FH, but statistically do not have an overall longer [duration of untreated illness]," the authors concluded. "Furthermore, the current findings are the first to show that sex of the patient should be taken into account when examining the relationships between FH and [duration of untreated illness/DUP] in that males with a FH of psychosis had a significantly longer [duration of untreated illness] and DUP relative to males with no FH of psychosis."
The researchers acknowledged certain limitations of the study, including its retrospective design, the fact that "assessing the presence of FH can ... be quite difficult, and [that] data collected from patients alone (without family member informants) may be less reliable. However, we made every effort to interview one or two family members in addition to the patient when possible to ensure that the most accurate data on FH were obtained."
They went on to recommend that "future research should focus on attempting to understand potential mediators and moderators of FH and its influence on the clinical presentation in schizophrenia."
The study was funded by the National Institute of Mental Health. The authors declared no relevant financial conflicts of interest.
FROM PSYCHIATRY RESEARCH
Major Finding: First-episode psychosis patients with a family history of psychosis had a longer duration of untreated psychosis, compared with patients who had no such FH (P less than .05). Among patients with a FH of psychosis, men had significantly more negative symptoms than did women (26% vs. 17%; P less than .01).
Data Source: This was a retrospective study of 152 first-episode psychosis patients.
Disclosures: The study was supported by grants from the National Institute of Mental Health. The authors declared no relevant financial conflicts of interest.
Large-Vessel Stroke May Respond Best to Endovascular Therapy
SAN DIEGO – Patients who presented with acute ischemic stroke secondary to a large-vessel occlusion in the anterior circulation were nearly four times more likely to have a favorable outcome at 90 days if they underwent endovascular therapy than if they underwent intravenous rt-PA therapy in a single-center study.
"Large-vessel occlusions cause almost half of acute ischemic strokes and portend a poor prognosis if untreated," Dr. Ansaar T. Rai said at the annual meeting of the Society of Neurointerventional Surgery. "There are limited data comparing IV rt-PA [recombinant tissue-type plasminogen activator] and endovascular therapy outcomes for large-vessel occlusions. We need evidence to define the target population for endovascular therapy. We need to design meaningful trials around this target population and provide reasonable outcome expectations and information to patients presenting with acute ischemic stroke."
Dr. Rai, an interventional neuroradiologist with West Virginia University, Morgantown, presented findings from a single-center, retrospective study of 223 patients with an intracranial vascular occlusion in the anterior circulation on baseline CT angiography (CTA). The patients had undergone either endovascular therapy (EVT) or IV rt-PA treatment (IVT), but not both. Large-vessel occlusion on admission CTA was defined as involvement of the internal carotid artery terminus (ICA-T), the middle cerebral artery main stem with or without bifurcation involvement (M1), or isolated involvement of the proximal M2 branches.
The primary outcome was 90-day favorable outcome, defined as a modified Rankin score of 0-2, while the safety outcomes were mortality and significant parenchymal hemorrhage.
Dr. Rai reported on results from 100 patients in the IVT group and 123 patients in the EVT group. The mean age of patients was 72 years, 56% were female, and their mean baseline National Institutes of Health Stroke Scale (NIHSS) score was 19.1. Nearly half of the occlusions (48%) involved M1, 32% involved M2, and 20% involved ICA-T.
Among all patients, a favorable outcome occurred in 81 (36.3%), and mortality occurred in 81 (36.3%).
A comparison of baseline characteristics revealed that patients in the EVT group were significantly younger than those in the IVT group (69 vs. 76 years; P = .0002), had significantly more M1 occlusions (56% vs. 38%; P = .007), and had significantly fewer M2 occlusions (20% vs. 46%; P = .0002).
A significantly greater proportion of patients in the EVT group had a favorable outcome compared with those in the IVT group (45% vs. 26%, P = .003; odds ratio, 2.3), yet there were no significant differences between the groups in terms of mortality (32% vs. 42%; P = .10) or in the rate of significant hemorrhage (14% vs. 10%; P = .38).
For all occlusion sites, patients in the EVT group had significantly better outcomes than did patients in the IVT group. For ICA-T occlusions, 27% of patients in the EVT group achieved a good outcome, compared with 0% in the IVT group (P = .004). Similar associations were observed for M1 lesions (41% vs. 11%, respectively; P = .0006) and for M2 lesions (76% vs. 48%; P = .01).
The researchers observed that at all sites of occlusion, a higher proportion of patients younger than 80 years had favorable outcomes, compared with patients aged 80 and older, especially those with proximal occlusions.
Multivariate analysis controlling for age and occlusion site composition demonstrated that patients in the EVT group were 3.9 times more likely to achieve a favorable outcome compared with their counterparts in the IVT group (P = .0004).
"In the last decade, we’ve seen significant technological advancement in our techniques and devices for stroke therapy," Dr. Rai commented. "The number of stroke treatments has not changed significantly. We need a paradigm shift in how we select patients for therapy, an appropriate intervention, and a comprehensive strategy."
Dr. Rai acknowledged certain limitations of the study, including its retrospective design and a bias in selecting EVT patients.
He said that he had no relevant financial disclosures.
SAN DIEGO – Patients who presented with acute ischemic stroke secondary to a large-vessel occlusion in the anterior circulation were nearly four times more likely to have a favorable outcome at 90 days if they underwent endovascular therapy than if they underwent intravenous rt-PA therapy in a single-center study.
"Large-vessel occlusions cause almost half of acute ischemic strokes and portend a poor prognosis if untreated," Dr. Ansaar T. Rai said at the annual meeting of the Society of Neurointerventional Surgery. "There are limited data comparing IV rt-PA [recombinant tissue-type plasminogen activator] and endovascular therapy outcomes for large-vessel occlusions. We need evidence to define the target population for endovascular therapy. We need to design meaningful trials around this target population and provide reasonable outcome expectations and information to patients presenting with acute ischemic stroke."
Dr. Rai, an interventional neuroradiologist with West Virginia University, Morgantown, presented findings from a single-center, retrospective study of 223 patients with an intracranial vascular occlusion in the anterior circulation on baseline CT angiography (CTA). The patients had undergone either endovascular therapy (EVT) or IV rt-PA treatment (IVT), but not both. Large-vessel occlusion on admission CTA was defined as involvement of the internal carotid artery terminus (ICA-T), the middle cerebral artery main stem with or without bifurcation involvement (M1), or isolated involvement of the proximal M2 branches.
The primary outcome was 90-day favorable outcome, defined as a modified Rankin score of 0-2, while the safety outcomes were mortality and significant parenchymal hemorrhage.
Dr. Rai reported on results from 100 patients in the IVT group and 123 patients in the EVT group. The mean age of patients was 72 years, 56% were female, and their mean baseline National Institutes of Health Stroke Scale (NIHSS) score was 19.1. Nearly half of the occlusions (48%) involved M1, 32% involved M2, and 20% involved ICA-T.
Among all patients, a favorable outcome occurred in 81 (36.3%), and mortality occurred in 81 (36.3%).
A comparison of baseline characteristics revealed that patients in the EVT group were significantly younger than those in the IVT group (69 vs. 76 years; P = .0002), had significantly more M1 occlusions (56% vs. 38%; P = .007), and had significantly fewer M2 occlusions (20% vs. 46%; P = .0002).
A significantly greater proportion of patients in the EVT group had a favorable outcome compared with those in the IVT group (45% vs. 26%, P = .003; odds ratio, 2.3), yet there were no significant differences between the groups in terms of mortality (32% vs. 42%; P = .10) or in the rate of significant hemorrhage (14% vs. 10%; P = .38).
For all occlusion sites, patients in the EVT group had significantly better outcomes than did patients in the IVT group. For ICA-T occlusions, 27% of patients in the EVT group achieved a good outcome, compared with 0% in the IVT group (P = .004). Similar associations were observed for M1 lesions (41% vs. 11%, respectively; P = .0006) and for M2 lesions (76% vs. 48%; P = .01).
The researchers observed that at all sites of occlusion, a higher proportion of patients younger than 80 years had favorable outcomes, compared with patients aged 80 and older, especially those with proximal occlusions.
Multivariate analysis controlling for age and occlusion site composition demonstrated that patients in the EVT group were 3.9 times more likely to achieve a favorable outcome compared with their counterparts in the IVT group (P = .0004).
"In the last decade, we’ve seen significant technological advancement in our techniques and devices for stroke therapy," Dr. Rai commented. "The number of stroke treatments has not changed significantly. We need a paradigm shift in how we select patients for therapy, an appropriate intervention, and a comprehensive strategy."
Dr. Rai acknowledged certain limitations of the study, including its retrospective design and a bias in selecting EVT patients.
He said that he had no relevant financial disclosures.
SAN DIEGO – Patients who presented with acute ischemic stroke secondary to a large-vessel occlusion in the anterior circulation were nearly four times more likely to have a favorable outcome at 90 days if they underwent endovascular therapy than if they underwent intravenous rt-PA therapy in a single-center study.
"Large-vessel occlusions cause almost half of acute ischemic strokes and portend a poor prognosis if untreated," Dr. Ansaar T. Rai said at the annual meeting of the Society of Neurointerventional Surgery. "There are limited data comparing IV rt-PA [recombinant tissue-type plasminogen activator] and endovascular therapy outcomes for large-vessel occlusions. We need evidence to define the target population for endovascular therapy. We need to design meaningful trials around this target population and provide reasonable outcome expectations and information to patients presenting with acute ischemic stroke."
Dr. Rai, an interventional neuroradiologist with West Virginia University, Morgantown, presented findings from a single-center, retrospective study of 223 patients with an intracranial vascular occlusion in the anterior circulation on baseline CT angiography (CTA). The patients had undergone either endovascular therapy (EVT) or IV rt-PA treatment (IVT), but not both. Large-vessel occlusion on admission CTA was defined as involvement of the internal carotid artery terminus (ICA-T), the middle cerebral artery main stem with or without bifurcation involvement (M1), or isolated involvement of the proximal M2 branches.
The primary outcome was 90-day favorable outcome, defined as a modified Rankin score of 0-2, while the safety outcomes were mortality and significant parenchymal hemorrhage.
Dr. Rai reported on results from 100 patients in the IVT group and 123 patients in the EVT group. The mean age of patients was 72 years, 56% were female, and their mean baseline National Institutes of Health Stroke Scale (NIHSS) score was 19.1. Nearly half of the occlusions (48%) involved M1, 32% involved M2, and 20% involved ICA-T.
Among all patients, a favorable outcome occurred in 81 (36.3%), and mortality occurred in 81 (36.3%).
A comparison of baseline characteristics revealed that patients in the EVT group were significantly younger than those in the IVT group (69 vs. 76 years; P = .0002), had significantly more M1 occlusions (56% vs. 38%; P = .007), and had significantly fewer M2 occlusions (20% vs. 46%; P = .0002).
A significantly greater proportion of patients in the EVT group had a favorable outcome compared with those in the IVT group (45% vs. 26%, P = .003; odds ratio, 2.3), yet there were no significant differences between the groups in terms of mortality (32% vs. 42%; P = .10) or in the rate of significant hemorrhage (14% vs. 10%; P = .38).
For all occlusion sites, patients in the EVT group had significantly better outcomes than did patients in the IVT group. For ICA-T occlusions, 27% of patients in the EVT group achieved a good outcome, compared with 0% in the IVT group (P = .004). Similar associations were observed for M1 lesions (41% vs. 11%, respectively; P = .0006) and for M2 lesions (76% vs. 48%; P = .01).
The researchers observed that at all sites of occlusion, a higher proportion of patients younger than 80 years had favorable outcomes, compared with patients aged 80 and older, especially those with proximal occlusions.
Multivariate analysis controlling for age and occlusion site composition demonstrated that patients in the EVT group were 3.9 times more likely to achieve a favorable outcome compared with their counterparts in the IVT group (P = .0004).
"In the last decade, we’ve seen significant technological advancement in our techniques and devices for stroke therapy," Dr. Rai commented. "The number of stroke treatments has not changed significantly. We need a paradigm shift in how we select patients for therapy, an appropriate intervention, and a comprehensive strategy."
Dr. Rai acknowledged certain limitations of the study, including its retrospective design and a bias in selecting EVT patients.
He said that he had no relevant financial disclosures.
AT THE ANNUAL MEETING OF THE SOCIETY OF NEUROINTERVENTIONAL SURGERY
Major Finding: Patients
who suffered an acute ischemic stroke secondary to a large-vessel occlusion were
3.9 times more likely to achieve a favorable outcome at 90 days if they
underwent endovascular therapy than if they underwent IV rt-PA treatment (P
= .0004).
Data Source: This
was a single-center study of 223 patients with a mean age of 72 years and a
mean baseline NIHSS score of 19.1.
Disclosures: Dr.
Rai said that he had no relevant financial conflicts.