User login
Topical Therapy for Acne in Women: Is There a Role for Clindamycin Phosphate–Benzoyl Peroxide Gel?
The management of acne vulgaris (AV) in women has been the subject of considerable attention over the last few years. It has become increasingly recognized that a greater number of patient encounters in dermatology offices involve women with AV who are beyond their adolescent years. Overall, it is estimated that up to approximately 22% of women in the United States are affected by AV, with approximately half of women in their 20s and one-third of women in their 30s reporting some degree of AV.1-4 Among women, the disease shows no predilection for certain skin types or ethnicities, can start during the preteenaged or adolescent years, can persist or recur in adulthood (persistent acne, 75%), or can start in adulthood (late-onset acne, 25%) in females with minimal or no history of AV occurring earlier in life.3,5-7 In the subpopulation of adult women, AV occurs at a time when many expect to be far beyond this “teenage affliction.” Women who are affected commonly express feeling embarrassed and frustrated.5-8
Most of the emphasis in the literature and in presentations at dermatology meetings regarding the management of AV in adult women has focused on excluding underlying disorders that cause excess androgens (eg, polycystic ovary syndrome, congenital adrenal hyperplasia, tumors, exogenous sources) as well as the use of systemic therapies such as oral contraceptives (OCs) and spironolactone.5-7,9,10 Little attention has been given to the selection of topical therapies in this patient population, especially with regard to evidence from clinical studies. To date, results from published study analyses using topical agents specifically for adult females with facial AV have only included adapalene gel 0.3% applied once daily and dapsone gel 5% applied twice daily.11-13 Both agents have been evaluated in subset analysis comparisons of outcomes in women aged 18 years and older versus adolescents aged 12 to 17 years based on data from 12-week phase 3 pivotal trials.14-16
Are there clinically relevant differences between AV in adult versus adolescent females?
Although much has been written about AV in women, epidemiology, demographics, assessment of clinical presentation, and correlation of clinical presentation with excess androgens have not been emphasized,1-3,5-10,17 likely due to marketing campaigns that emphasize AV as a disorder that predominantly affects teenagers as well as the focus on optimal use of oral spironolactone and/or OCs in the management of AV in the adult female population. Attention to spironolactone use is important because it is not approved by the US Food and Drug Administration for the treatment of AV. Spironolactone carries certain black-box warnings that may not be clinically relevant in all patients but still require attention. It also is associated with risks if taken during pregnancy, and it is a potassium-sparing diuretic with potential for hyperkalemia, especially in patients with reduced renal function or those who are taking potassium supplements or certain other medications.6,9,11,17 Use of OCs to treat AV also is not without potential risks, with specific warnings and relative contraindications reported, especially in relation to increased risks for cardiac complications, stroke, and thromboembolism.6,9,11,12 Because adult females are in a different stage of life than teenagers, there are defined psychosocial and medical considerations in managing AV in these patients compared with adolescents.5-8,17 Importantly for both clinicians and patients, addressing these differences and considerations can have a major impact on whether or not women with AV experience successful treatment outcomes.1-3,5,6,8,10,13 Skin color and ethnicity also can affect the psychosocial and physical factors that influence the overall management of adult female patients with AV, including selection of therapies and handling long-term visible sequelae that occur in some AV patients, such as dyschromia (eg, persistent or postinflammatory erythema or hyperpigmentation) and acne scarring.5-8,13,17-20
Psychosocial Considerations
With regard to psychosocial, emotional, and attitudinal considerations in women with AV, common findings include concern or frustration regarding the presence of AV beyond adolescence; anxiety; symptoms of depression; decreased self-confidence; increased self-consciousness, especially during public interactions or intimate situations; and interference with steady concentration at work or school.5,6,8,13 Long-term complications of AV, such as dyschromia and acne scarring, are more likely to be encountered in adult patients, especially if they had AV as a teenager, with women reporting that they remain conscious of these adverse sequelae.8 It is estimated that approximately three-fourths of women with AV also had AV as teenagers; therefore, most of them have already used many over-the-counter and prescription therapies and are likely to want treatments that are newer, well-tolerated, safe, and known to be effective in adult women.8,16,17 Convenience and simplicity are vital components of treatment selection and regimen design, as many women with AV frequently face time constraints in their daily routines due to family, social, employment, and home-related demands and responsibilities.6-8,17
Medical Considerations
It is apparent from reports in the literature as well as from clinical experience that some women with AV present with a U-shaped pattern of involvement on the face,5-7,10,13,17 which refers to the presence of predominantly inflammatory papules (many of them deep) and some nodules on the lower face, jawline, and anterolateral neck region, with comedones often sparse or absent.5-7 It often is perceived and may be true that women who present with this pattern of distribution are more androgen sensitive despite having normal serum androgen levels or in some cases exhibit detectable excess androgens (eg, in the setting of polycystic ovary syndrome) and may be more likely to respond to hormonal therapies (eg, spironolactone, OCs) than those with mixed facial AV (ie, multiple comedonal and inflammatory acne lesions, not limited to a U-shaped pattern, similar to adolescent AV), but data are limited to support differentiation between the U-shaped pattern group and the conventional mixed facial AV group.5-7,17 Adult and adolescent females in both groups sometimes report perimenstrual flares and frequent persistent papular AV that tends to concentrate on the perioral and chin area.
It is also important to consider that the current literature suggests approximately three-fourths of women with AV report that they also had AV as a teenager, with many indicating the same clinical pattern of AV and approximately one-third reporting AV that is more severe in adulthood than adolescence.5-8,17 The available literature on topical and oral therapies used to treat AV in both adolescent and adult females predominantly focuses on inclusion of both inflammatory and noninflammatory (comedonal) facial AV lesions, does not specifically address or include the U-shaped pattern of AV in adult women for inclusion in studies that evaluate efficacy in this subgroup, and does not include AV involving the neck region and below the jawline margin as part of any study protocols and/or discussions about therapy.5-7,9-12,17,21-26 Involvement of the neck and lower jawline is common in women presenting with the U-shaped pattern of AV, and available studies only evaluate AV involving the face and do not include AV lesions present below the jawline margin. As a result, there is a considerable need for well-designed studies with laboratory assessments to include or exclude underlying detectable excess androgens and to assess the efficacy, tolerability, and safety of specific therapeutic agents both alone and in combination in adult women who present with a U-shaped pattern of AV.17
Other medical considerations that can influence treatment selection and are more likely to be present in adult versus adolescent females include underlying chronic medical disorders; concomitant medications that may interact with other oral agents; potential for pregnancy; age, particularly when prescribing OCs; and the potential desire to stop taking OCs if already used over a prolonged period.6,7
Age-Related Differentiation of Female Subgroups With AV
The age-based dividing line that defines AV in adults versus adolescent females has been described in the literature; however, the basis for published definitions of female subgroups with AV is not well-supported by strong scientific evidence.1-3,5-7,17 The conventional dividing line that was originally selected to define adult females with AV was 25 years of age or older; persistent acne is present both during adolescence and at or after 25 years of age, while late-onset acne is described as AV that first presents at 25 years of age or older.3,5-7
More recently, a range of 18 years or older has been used to classify adult female AV and a range of 12 to 17 years for adolescent female AV in subset analyses that evaluated treatment outcomes in both patient populations from phase 3 pivotal trials completed with adapalene gel 0.3% applied once daily and dapsone gel 5% applied twice daily.14-16 These subanalyses included participants with facial AV that was predominantly moderate in severity, mandated specific lesion count ranges for both comedonal and inflammatory lesions, and included only facial AV that was above the mandibular (jawline) margin.15,16,21,26 Therefore, patients with AV presenting in a U-shaped pattern with involvement below the jawline and on the neck were not included in these study analyses, as these patients were excluded from the phase 3 trials on which the analyses were based. The outcomes of these analyses apply to treatment in women who present with both inflammatory and noninflammatory facial AV lesions, which supports the observation that AV in this patient population is not always predominantly inflammatory and does not always present in a U-shaped distribution.14-16 In fact, a U-shaped pattern of distribution appears to be less common in women with AV than a mixed inflammatory and comedonal distribution that involves the face more diffusely, though more data are needed from well-designed and large-scale epidemiologic and demographic studies.5,14,17
Are there data available on the use of benzoyl peroxide with or without a topical antibiotic in women with AV?
There is a conspicuous absence of prospective clinical trials and retrospective analyses evaluating the specific use of individual AV therapies in adult females, with a particular lack of studies with topical agents (eg, benzoyl peroxide [BP]).14 Subset analyses have been completed for adapalene gel 0.3% and dapsone gel 5%.15,16 Additionally, an age-based subset analysis in females with facial AV also has been completed with clindamycin phosphate (CP) 1.2%–BP 2.5% gel once daily, with data presented but not yet fully published.14
Two identical phase 3, double-blind, randomized, 12-week, 4-arm trials compared treatment outcomes in groups treated with an aqueous-based combination gel formulation containing BP 2.5% and CP 1.2% (n=797), active monad gels (BP [n=809] or CP [n=812]), or vehicle gel (n=395), all applied once daily in patients with facial AV.22 Participants were 12 years or older (mean age range, 19.1–19.6 years; age range, 12.1–70.2 years), were of either gender (approximately 50% split in each study arm), and presented with moderate (approximately 80% of participants) or severe AV (approximately 20% of participants) at baseline. The entry criteria for lesion types and number of lesions were 17 to 40 inflammatory lesions (ie, papules, pustules, <2 nodules)(range of mean number of lesions, 25.8–26.4) and 20 to 100 noninflammatory lesions (ie, closed comedones, open comedones)(range of mean number of lesions, 44.0–47.4). Participant demographics included white (73.9%–77.5%), black/African American (16.1%–20.4%), and Asian (2.1%–3.3%), with the remaining participants distributed among a variety of other ethnic groups such as Native Hawaiian/Native Pacific Islander and Native American Indian/Native Alaskan (collectively <5% in each study arm). Therefore, approximately 1 of every 4 patients had skin of color, which provided good diversity of patients considering the large study size (N=2813). Data analysis included dichotomization of participants by severity rating (moderate or severe based on evaluator global severity score) and skin phototype (Fitzpatrick skin types I–III or IV–VI).22
The pooled results from both studies completed at 68 investigative sites demonstrated that CP 1.2%–BP 2.5% gel was superior in efficacy to each individual monad and to the vehicle in inflammatory, noninflammatory, and total lesion reductions as early as week 4 (P<.001) and at week 12, which was the study end point (P<.001), with superiority also demonstrated in achieving treatment success (defined as a >2 grade improvement according to the evaluator global severity score) compared to the 3 other study arms (P<.001).22 Subject assessments also were consistent with outcomes noted by the investigators. Cutaneous tolerability was favorable and comparable in all 4 study arms with less than 1% of participants discontinuing treatment due to adverse events.22
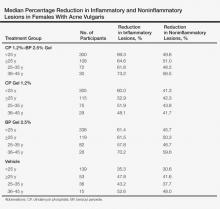
A subset analysis of the data from the phase 3 pivotal trials with CP 1.2%–BP 2.5% gel was completed to compare reductions in both inflammatory and noninflammatory lesions in female participants who were younger than 25 years and 25 years of age or older in all 4 study arms. This information has been presented14,17 but has not been previously published. Based on the overall results reported in the phase 3 studies, there were no differentiations in skin tolerability or safety based on participant age, gender, or skin type.22 The subanalysis included a total of 1080 females who were younger than 25 years and 395 females who were 25 years of age or older. The lesion reduction outcomes of this subanalysis are presented in the Table. Statistical analyses of the results among these age groups in the 4 study arms were not completed because the objective was to determine if there were any major or obvious differences in reduction of AV lesions based on the conventional dividing line of 25 years of age in adult women as compared to adolescent females treated with CP 1.2%–BP 2.5% gel. In addition, the large difference in numbers of female participants between the 2 age groups (>25 years of age, n=395; <25 years of age, n=1080) at least partially confounds both statistical and observational analysis. Among the women who were 25 years of age or older who were included in the subanalysis, 67.0% and 25.8% were between the ages of 25 to 35 years and 36 to 45 years, respectively. Based on the outcomes reported in the phase 3 trials and in this subgroup analysis, CP 1.2%–BP 2.5% gel applied once daily over a 12-week period appeared overall to be comparably effective in females regardless of age and with no apparent adverse events regarding differences in skin tolerability or safety.14,22 One observation that was noted was the possible trend of greater reduction in both lesion types in women older than 35 years versus younger females with the use of the combination gel or BP alone; however, the number of female participants who were older than 35 years of age was substantially less (n=102) than those who were 35 years of age or younger (n=1345), thus precluding support for any definitive conclusions about this possible trend.22
How can CP 1.2%–BP 2.5% gel be incorporated into a treatment regimen for women with facial AV?
The incorporation of CP 1.2%–BP 2.5% gel into a treatment regimen for women with facial AV is similar to the general use of BP-containing formulations in the overall management of AV.9,14,27,28 Because women with AV commonly present with facial inflammatory lesions and many also with facial comedones, CP 1.2%–BP 2.5% gel is best used once daily in the morning in combination with a topical retinoid in the evening,9,27 which can be achieved with use of CP 1.2%–BP 2.5% gel in the morning and a topical retinoid (ie, tretinoin, adapalene, tazarotene) in the evening or CP 1.2%–tretinoin 0.025% gel in the evening. It is important to note that cutaneous irritation may be more likely if neck lesions are present; the potential for bleaching of colored fabric by BP also is a practical concern.28 In addition, CP 1.2%–BP 2.5% gel may also be used in combination with topical dapsone, but both products should be applied separately at different times of the day to avoid temporary orange discoloration of the skin, which appears to be an uncommon side effect but remains a possibility based on the product information for dapsone gel 5% with regard to its concomitant use with BP.29,30
1. Perkins AC, Maglione J, Hillebrand GG, et al. Acne vulgaris in women: prevalence across the life span. J Womens Health. 2012;21:223-230.
2. Zeichner J. Evaluating and treating the adult female patient with acne. J Drugs Dermatol. 2013;12:1416-1427.
3. Goulden V, Stables GI, Cunliffe WJ. Prevalence of facial acne in adults. J Am Acad Dermatol. 1999;41:577-580.
4. Collier CN, Harper J, Cafardi JA, et al. The prevalence of acne in adults 20 years and older. J Am Acad Dermatol. 2008;58:56-59.
5. Dreno B, Layton A, Zouboulis CC, et al. Adult female acne: a new paradigm. J Eur Acad Dermatol Venereol. 2013;27:1063-1070.
6. Kim GK, Del Rosso JQ. Oral spironolactone in post-teenage female patients with acne vulgaris: practical considerations for the clinician based on current data and clinical experience. J Clin Aesthet Dermatol. 2012;5:37-50.
7. Kim GK, Michaels BB. Post-adolescent acne in women: more common and more clinical considerations. J Drugs Dermatol. 2012;11:708-713.
8. Tanghetti EA, Kawata AK, Daniels SR, et al. Understanding the burden of adult female acne. J Clin Aesthet Dermatol. 2014;7:22-30.
9. Gollnick H, Cunliffe W, Berson D, et al. Management of acne: a report from a Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol. 2003;49(suppl 1):1-37.
10. Thiboutot DM. Endocrinological evaluation and hormonal therapy for women with difficult acne. J Eur Acad Dermatol Venereol. 2001;15(suppl 3):57-61.
11. Sawaya ME, Samani N. Antiandrogens and androgen receptors. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. Philadelphia, PA: Saunders-Elsevier; 2012:361-374.
12. Harper JC. Should dermatologists prescribe hormonal contraceptives for acne? Dermatol Ther. 2009;22:452-457.
13. Preneau S, Dreno B. Female acne: a different subtype of teenager acne? J Eur Acad Dermatol Venereol. 2012;26:277-282.
14. Del Rosso JQ, Zeichner JA. What’s new in the medicine cabinet?: a panoramic review of clinically relevant information for the busy dermatologist. J Clin Aesthet Dermatol. 2014;7:26-30.
15. Berson D, Alexis A. Adapalene 0.3% for the treatment of acne in women. J Clin Aesthet Dermatol. 2013;6:32-35.
16. Del Rosso JQ, Kircik L, Gallagher C. Facing up to adult women with acne vulgaris: an analysis of pivotal trial data on dapsone 5% gel in the adult female population. Poster presented at: Fall Clinical Dermatology; October 2013; Las Vegas, NV.
17. Del Rosso JQ. Management of acne with oral spironolactone. Presented at: American Academy of Dermatology Summer Meeting; August 2013; Boston, MA.
18. Davis EC, Callender VD. A review of acne in ethnic skin: pathogenesis, clinical manifestations, and management strategies. J Clin Aesthet Dermatol. 2010;3:24-38.
19. Davis SA, Narahari S, Feldman SR, et al. Top dermatologic conditions in patients of color: an analysis of nationally representative data. J Drugs Dermatol. 2012;11:466-473.
20. Perkins AC, Cheng CE, Hillebrand GG, et al. Comparison of the epidemiology of acne vulgaris among Caucasian, Asian, Continental Indian and African American women. J Eur Acad Dermatol Venereol. 2011;25:1054-1060.
21. Draelos ZD, Carter E, Maloney JM, et al. Two randomized studies demonstrate the efficacy and safety of dapsone gel, 5% for the treatment of acne vulgaris [published online ahead of print January 17, 2007]. J Am Acad Dermatol. 2007;56:439.e1-439.e10.
22. Thiboutot D, Zaenglein A, Weiss J, et al. An aqueous gel fixed combination of clindamycin phosphate 1.2% and benzoyl peroxide 2.5% for the once-daily treatment of moderate to severe acne vulgaris: assessment of efficacy and safety in 2813 patients. J Am Acad Dermatol. 2008;59:792-800.
23. Schlessinger J, Menter A, Gold M, et al. Clinical safety and efficacy studies of a novel formulation combining
1.2% clindamycin phosphate and 0.025% tretinoin for the treatment of acne vulgaris. J Drugs Dermatol. 2007;6:607-615.
24. Fleischer AB Jr, Dinehart S, Stough D, et al. Safety and efficacy of a new extended-release formulation of minocycline. Cutis. 2006;78(suppl 4):21-31.
25. Gollnick HP, Draelos Z, Glenn MJ, et al. Adapalene-benzoyl peroxide, a unique fixed-dose combination topical gel for the treatment of acne vulgaris: a transatlantic, randomized, double-blind, controlled study in 1670 patients. Br J Dermatol. 2009;161:1180-1189.
26. Thiboutot D, Arsonnaud S, Soto P. Efficacy and tolerability of adapalene 0.3% gel compared to tazarotene 0.1% gel in the treatment of acne vulgaris. J Drugs Dermatol. 2008;7(suppl 6):3-10.
27. Zeichner JA. Optimizing topical combination therapy for the treatment of acne vulgaris. J Drugs Dermatol. 2012;11:313-317.
28. Tanghetti EA, Popp KF. A current review of topical benzoyl peroxide: new perspectives on formulation and utilization. Dermatol Clin. 2009;27:17-24.
29. Fleischer AB, Shalita A, Eichenfield LF. Dapsone gel 5% in combination with adapalene gel 0.1%, benzoyl peroxide gel 4% or moisturizer for the treatment of acne vulgaris: a 12-week, randomized, double-blind study. J Drugs Dermatol. 2010;9:33-40.
30. Aczone (dapsone gel 5%) [package insert]. Irvine, CA: Allergan, Inc; 2013.
The management of acne vulgaris (AV) in women has been the subject of considerable attention over the last few years. It has become increasingly recognized that a greater number of patient encounters in dermatology offices involve women with AV who are beyond their adolescent years. Overall, it is estimated that up to approximately 22% of women in the United States are affected by AV, with approximately half of women in their 20s and one-third of women in their 30s reporting some degree of AV.1-4 Among women, the disease shows no predilection for certain skin types or ethnicities, can start during the preteenaged or adolescent years, can persist or recur in adulthood (persistent acne, 75%), or can start in adulthood (late-onset acne, 25%) in females with minimal or no history of AV occurring earlier in life.3,5-7 In the subpopulation of adult women, AV occurs at a time when many expect to be far beyond this “teenage affliction.” Women who are affected commonly express feeling embarrassed and frustrated.5-8
Most of the emphasis in the literature and in presentations at dermatology meetings regarding the management of AV in adult women has focused on excluding underlying disorders that cause excess androgens (eg, polycystic ovary syndrome, congenital adrenal hyperplasia, tumors, exogenous sources) as well as the use of systemic therapies such as oral contraceptives (OCs) and spironolactone.5-7,9,10 Little attention has been given to the selection of topical therapies in this patient population, especially with regard to evidence from clinical studies. To date, results from published study analyses using topical agents specifically for adult females with facial AV have only included adapalene gel 0.3% applied once daily and dapsone gel 5% applied twice daily.11-13 Both agents have been evaluated in subset analysis comparisons of outcomes in women aged 18 years and older versus adolescents aged 12 to 17 years based on data from 12-week phase 3 pivotal trials.14-16
Are there clinically relevant differences between AV in adult versus adolescent females?
Although much has been written about AV in women, epidemiology, demographics, assessment of clinical presentation, and correlation of clinical presentation with excess androgens have not been emphasized,1-3,5-10,17 likely due to marketing campaigns that emphasize AV as a disorder that predominantly affects teenagers as well as the focus on optimal use of oral spironolactone and/or OCs in the management of AV in the adult female population. Attention to spironolactone use is important because it is not approved by the US Food and Drug Administration for the treatment of AV. Spironolactone carries certain black-box warnings that may not be clinically relevant in all patients but still require attention. It also is associated with risks if taken during pregnancy, and it is a potassium-sparing diuretic with potential for hyperkalemia, especially in patients with reduced renal function or those who are taking potassium supplements or certain other medications.6,9,11,17 Use of OCs to treat AV also is not without potential risks, with specific warnings and relative contraindications reported, especially in relation to increased risks for cardiac complications, stroke, and thromboembolism.6,9,11,12 Because adult females are in a different stage of life than teenagers, there are defined psychosocial and medical considerations in managing AV in these patients compared with adolescents.5-8,17 Importantly for both clinicians and patients, addressing these differences and considerations can have a major impact on whether or not women with AV experience successful treatment outcomes.1-3,5,6,8,10,13 Skin color and ethnicity also can affect the psychosocial and physical factors that influence the overall management of adult female patients with AV, including selection of therapies and handling long-term visible sequelae that occur in some AV patients, such as dyschromia (eg, persistent or postinflammatory erythema or hyperpigmentation) and acne scarring.5-8,13,17-20
Psychosocial Considerations
With regard to psychosocial, emotional, and attitudinal considerations in women with AV, common findings include concern or frustration regarding the presence of AV beyond adolescence; anxiety; symptoms of depression; decreased self-confidence; increased self-consciousness, especially during public interactions or intimate situations; and interference with steady concentration at work or school.5,6,8,13 Long-term complications of AV, such as dyschromia and acne scarring, are more likely to be encountered in adult patients, especially if they had AV as a teenager, with women reporting that they remain conscious of these adverse sequelae.8 It is estimated that approximately three-fourths of women with AV also had AV as teenagers; therefore, most of them have already used many over-the-counter and prescription therapies and are likely to want treatments that are newer, well-tolerated, safe, and known to be effective in adult women.8,16,17 Convenience and simplicity are vital components of treatment selection and regimen design, as many women with AV frequently face time constraints in their daily routines due to family, social, employment, and home-related demands and responsibilities.6-8,17
Medical Considerations
It is apparent from reports in the literature as well as from clinical experience that some women with AV present with a U-shaped pattern of involvement on the face,5-7,10,13,17 which refers to the presence of predominantly inflammatory papules (many of them deep) and some nodules on the lower face, jawline, and anterolateral neck region, with comedones often sparse or absent.5-7 It often is perceived and may be true that women who present with this pattern of distribution are more androgen sensitive despite having normal serum androgen levels or in some cases exhibit detectable excess androgens (eg, in the setting of polycystic ovary syndrome) and may be more likely to respond to hormonal therapies (eg, spironolactone, OCs) than those with mixed facial AV (ie, multiple comedonal and inflammatory acne lesions, not limited to a U-shaped pattern, similar to adolescent AV), but data are limited to support differentiation between the U-shaped pattern group and the conventional mixed facial AV group.5-7,17 Adult and adolescent females in both groups sometimes report perimenstrual flares and frequent persistent papular AV that tends to concentrate on the perioral and chin area.
It is also important to consider that the current literature suggests approximately three-fourths of women with AV report that they also had AV as a teenager, with many indicating the same clinical pattern of AV and approximately one-third reporting AV that is more severe in adulthood than adolescence.5-8,17 The available literature on topical and oral therapies used to treat AV in both adolescent and adult females predominantly focuses on inclusion of both inflammatory and noninflammatory (comedonal) facial AV lesions, does not specifically address or include the U-shaped pattern of AV in adult women for inclusion in studies that evaluate efficacy in this subgroup, and does not include AV involving the neck region and below the jawline margin as part of any study protocols and/or discussions about therapy.5-7,9-12,17,21-26 Involvement of the neck and lower jawline is common in women presenting with the U-shaped pattern of AV, and available studies only evaluate AV involving the face and do not include AV lesions present below the jawline margin. As a result, there is a considerable need for well-designed studies with laboratory assessments to include or exclude underlying detectable excess androgens and to assess the efficacy, tolerability, and safety of specific therapeutic agents both alone and in combination in adult women who present with a U-shaped pattern of AV.17
Other medical considerations that can influence treatment selection and are more likely to be present in adult versus adolescent females include underlying chronic medical disorders; concomitant medications that may interact with other oral agents; potential for pregnancy; age, particularly when prescribing OCs; and the potential desire to stop taking OCs if already used over a prolonged period.6,7
Age-Related Differentiation of Female Subgroups With AV
The age-based dividing line that defines AV in adults versus adolescent females has been described in the literature; however, the basis for published definitions of female subgroups with AV is not well-supported by strong scientific evidence.1-3,5-7,17 The conventional dividing line that was originally selected to define adult females with AV was 25 years of age or older; persistent acne is present both during adolescence and at or after 25 years of age, while late-onset acne is described as AV that first presents at 25 years of age or older.3,5-7
More recently, a range of 18 years or older has been used to classify adult female AV and a range of 12 to 17 years for adolescent female AV in subset analyses that evaluated treatment outcomes in both patient populations from phase 3 pivotal trials completed with adapalene gel 0.3% applied once daily and dapsone gel 5% applied twice daily.14-16 These subanalyses included participants with facial AV that was predominantly moderate in severity, mandated specific lesion count ranges for both comedonal and inflammatory lesions, and included only facial AV that was above the mandibular (jawline) margin.15,16,21,26 Therefore, patients with AV presenting in a U-shaped pattern with involvement below the jawline and on the neck were not included in these study analyses, as these patients were excluded from the phase 3 trials on which the analyses were based. The outcomes of these analyses apply to treatment in women who present with both inflammatory and noninflammatory facial AV lesions, which supports the observation that AV in this patient population is not always predominantly inflammatory and does not always present in a U-shaped distribution.14-16 In fact, a U-shaped pattern of distribution appears to be less common in women with AV than a mixed inflammatory and comedonal distribution that involves the face more diffusely, though more data are needed from well-designed and large-scale epidemiologic and demographic studies.5,14,17
Are there data available on the use of benzoyl peroxide with or without a topical antibiotic in women with AV?
There is a conspicuous absence of prospective clinical trials and retrospective analyses evaluating the specific use of individual AV therapies in adult females, with a particular lack of studies with topical agents (eg, benzoyl peroxide [BP]).14 Subset analyses have been completed for adapalene gel 0.3% and dapsone gel 5%.15,16 Additionally, an age-based subset analysis in females with facial AV also has been completed with clindamycin phosphate (CP) 1.2%–BP 2.5% gel once daily, with data presented but not yet fully published.14
Two identical phase 3, double-blind, randomized, 12-week, 4-arm trials compared treatment outcomes in groups treated with an aqueous-based combination gel formulation containing BP 2.5% and CP 1.2% (n=797), active monad gels (BP [n=809] or CP [n=812]), or vehicle gel (n=395), all applied once daily in patients with facial AV.22 Participants were 12 years or older (mean age range, 19.1–19.6 years; age range, 12.1–70.2 years), were of either gender (approximately 50% split in each study arm), and presented with moderate (approximately 80% of participants) or severe AV (approximately 20% of participants) at baseline. The entry criteria for lesion types and number of lesions were 17 to 40 inflammatory lesions (ie, papules, pustules, <2 nodules)(range of mean number of lesions, 25.8–26.4) and 20 to 100 noninflammatory lesions (ie, closed comedones, open comedones)(range of mean number of lesions, 44.0–47.4). Participant demographics included white (73.9%–77.5%), black/African American (16.1%–20.4%), and Asian (2.1%–3.3%), with the remaining participants distributed among a variety of other ethnic groups such as Native Hawaiian/Native Pacific Islander and Native American Indian/Native Alaskan (collectively <5% in each study arm). Therefore, approximately 1 of every 4 patients had skin of color, which provided good diversity of patients considering the large study size (N=2813). Data analysis included dichotomization of participants by severity rating (moderate or severe based on evaluator global severity score) and skin phototype (Fitzpatrick skin types I–III or IV–VI).22
The pooled results from both studies completed at 68 investigative sites demonstrated that CP 1.2%–BP 2.5% gel was superior in efficacy to each individual monad and to the vehicle in inflammatory, noninflammatory, and total lesion reductions as early as week 4 (P<.001) and at week 12, which was the study end point (P<.001), with superiority also demonstrated in achieving treatment success (defined as a >2 grade improvement according to the evaluator global severity score) compared to the 3 other study arms (P<.001).22 Subject assessments also were consistent with outcomes noted by the investigators. Cutaneous tolerability was favorable and comparable in all 4 study arms with less than 1% of participants discontinuing treatment due to adverse events.22
A subset analysis of the data from the phase 3 pivotal trials with CP 1.2%–BP 2.5% gel was completed to compare reductions in both inflammatory and noninflammatory lesions in female participants who were younger than 25 years and 25 years of age or older in all 4 study arms. This information has been presented14,17 but has not been previously published. Based on the overall results reported in the phase 3 studies, there were no differentiations in skin tolerability or safety based on participant age, gender, or skin type.22 The subanalysis included a total of 1080 females who were younger than 25 years and 395 females who were 25 years of age or older. The lesion reduction outcomes of this subanalysis are presented in the Table. Statistical analyses of the results among these age groups in the 4 study arms were not completed because the objective was to determine if there were any major or obvious differences in reduction of AV lesions based on the conventional dividing line of 25 years of age in adult women as compared to adolescent females treated with CP 1.2%–BP 2.5% gel. In addition, the large difference in numbers of female participants between the 2 age groups (>25 years of age, n=395; <25 years of age, n=1080) at least partially confounds both statistical and observational analysis. Among the women who were 25 years of age or older who were included in the subanalysis, 67.0% and 25.8% were between the ages of 25 to 35 years and 36 to 45 years, respectively. Based on the outcomes reported in the phase 3 trials and in this subgroup analysis, CP 1.2%–BP 2.5% gel applied once daily over a 12-week period appeared overall to be comparably effective in females regardless of age and with no apparent adverse events regarding differences in skin tolerability or safety.14,22 One observation that was noted was the possible trend of greater reduction in both lesion types in women older than 35 years versus younger females with the use of the combination gel or BP alone; however, the number of female participants who were older than 35 years of age was substantially less (n=102) than those who were 35 years of age or younger (n=1345), thus precluding support for any definitive conclusions about this possible trend.22
How can CP 1.2%–BP 2.5% gel be incorporated into a treatment regimen for women with facial AV?
The incorporation of CP 1.2%–BP 2.5% gel into a treatment regimen for women with facial AV is similar to the general use of BP-containing formulations in the overall management of AV.9,14,27,28 Because women with AV commonly present with facial inflammatory lesions and many also with facial comedones, CP 1.2%–BP 2.5% gel is best used once daily in the morning in combination with a topical retinoid in the evening,9,27 which can be achieved with use of CP 1.2%–BP 2.5% gel in the morning and a topical retinoid (ie, tretinoin, adapalene, tazarotene) in the evening or CP 1.2%–tretinoin 0.025% gel in the evening. It is important to note that cutaneous irritation may be more likely if neck lesions are present; the potential for bleaching of colored fabric by BP also is a practical concern.28 In addition, CP 1.2%–BP 2.5% gel may also be used in combination with topical dapsone, but both products should be applied separately at different times of the day to avoid temporary orange discoloration of the skin, which appears to be an uncommon side effect but remains a possibility based on the product information for dapsone gel 5% with regard to its concomitant use with BP.29,30
The management of acne vulgaris (AV) in women has been the subject of considerable attention over the last few years. It has become increasingly recognized that a greater number of patient encounters in dermatology offices involve women with AV who are beyond their adolescent years. Overall, it is estimated that up to approximately 22% of women in the United States are affected by AV, with approximately half of women in their 20s and one-third of women in their 30s reporting some degree of AV.1-4 Among women, the disease shows no predilection for certain skin types or ethnicities, can start during the preteenaged or adolescent years, can persist or recur in adulthood (persistent acne, 75%), or can start in adulthood (late-onset acne, 25%) in females with minimal or no history of AV occurring earlier in life.3,5-7 In the subpopulation of adult women, AV occurs at a time when many expect to be far beyond this “teenage affliction.” Women who are affected commonly express feeling embarrassed and frustrated.5-8
Most of the emphasis in the literature and in presentations at dermatology meetings regarding the management of AV in adult women has focused on excluding underlying disorders that cause excess androgens (eg, polycystic ovary syndrome, congenital adrenal hyperplasia, tumors, exogenous sources) as well as the use of systemic therapies such as oral contraceptives (OCs) and spironolactone.5-7,9,10 Little attention has been given to the selection of topical therapies in this patient population, especially with regard to evidence from clinical studies. To date, results from published study analyses using topical agents specifically for adult females with facial AV have only included adapalene gel 0.3% applied once daily and dapsone gel 5% applied twice daily.11-13 Both agents have been evaluated in subset analysis comparisons of outcomes in women aged 18 years and older versus adolescents aged 12 to 17 years based on data from 12-week phase 3 pivotal trials.14-16
Are there clinically relevant differences between AV in adult versus adolescent females?
Although much has been written about AV in women, epidemiology, demographics, assessment of clinical presentation, and correlation of clinical presentation with excess androgens have not been emphasized,1-3,5-10,17 likely due to marketing campaigns that emphasize AV as a disorder that predominantly affects teenagers as well as the focus on optimal use of oral spironolactone and/or OCs in the management of AV in the adult female population. Attention to spironolactone use is important because it is not approved by the US Food and Drug Administration for the treatment of AV. Spironolactone carries certain black-box warnings that may not be clinically relevant in all patients but still require attention. It also is associated with risks if taken during pregnancy, and it is a potassium-sparing diuretic with potential for hyperkalemia, especially in patients with reduced renal function or those who are taking potassium supplements or certain other medications.6,9,11,17 Use of OCs to treat AV also is not without potential risks, with specific warnings and relative contraindications reported, especially in relation to increased risks for cardiac complications, stroke, and thromboembolism.6,9,11,12 Because adult females are in a different stage of life than teenagers, there are defined psychosocial and medical considerations in managing AV in these patients compared with adolescents.5-8,17 Importantly for both clinicians and patients, addressing these differences and considerations can have a major impact on whether or not women with AV experience successful treatment outcomes.1-3,5,6,8,10,13 Skin color and ethnicity also can affect the psychosocial and physical factors that influence the overall management of adult female patients with AV, including selection of therapies and handling long-term visible sequelae that occur in some AV patients, such as dyschromia (eg, persistent or postinflammatory erythema or hyperpigmentation) and acne scarring.5-8,13,17-20
Psychosocial Considerations
With regard to psychosocial, emotional, and attitudinal considerations in women with AV, common findings include concern or frustration regarding the presence of AV beyond adolescence; anxiety; symptoms of depression; decreased self-confidence; increased self-consciousness, especially during public interactions or intimate situations; and interference with steady concentration at work or school.5,6,8,13 Long-term complications of AV, such as dyschromia and acne scarring, are more likely to be encountered in adult patients, especially if they had AV as a teenager, with women reporting that they remain conscious of these adverse sequelae.8 It is estimated that approximately three-fourths of women with AV also had AV as teenagers; therefore, most of them have already used many over-the-counter and prescription therapies and are likely to want treatments that are newer, well-tolerated, safe, and known to be effective in adult women.8,16,17 Convenience and simplicity are vital components of treatment selection and regimen design, as many women with AV frequently face time constraints in their daily routines due to family, social, employment, and home-related demands and responsibilities.6-8,17
Medical Considerations
It is apparent from reports in the literature as well as from clinical experience that some women with AV present with a U-shaped pattern of involvement on the face,5-7,10,13,17 which refers to the presence of predominantly inflammatory papules (many of them deep) and some nodules on the lower face, jawline, and anterolateral neck region, with comedones often sparse or absent.5-7 It often is perceived and may be true that women who present with this pattern of distribution are more androgen sensitive despite having normal serum androgen levels or in some cases exhibit detectable excess androgens (eg, in the setting of polycystic ovary syndrome) and may be more likely to respond to hormonal therapies (eg, spironolactone, OCs) than those with mixed facial AV (ie, multiple comedonal and inflammatory acne lesions, not limited to a U-shaped pattern, similar to adolescent AV), but data are limited to support differentiation between the U-shaped pattern group and the conventional mixed facial AV group.5-7,17 Adult and adolescent females in both groups sometimes report perimenstrual flares and frequent persistent papular AV that tends to concentrate on the perioral and chin area.
It is also important to consider that the current literature suggests approximately three-fourths of women with AV report that they also had AV as a teenager, with many indicating the same clinical pattern of AV and approximately one-third reporting AV that is more severe in adulthood than adolescence.5-8,17 The available literature on topical and oral therapies used to treat AV in both adolescent and adult females predominantly focuses on inclusion of both inflammatory and noninflammatory (comedonal) facial AV lesions, does not specifically address or include the U-shaped pattern of AV in adult women for inclusion in studies that evaluate efficacy in this subgroup, and does not include AV involving the neck region and below the jawline margin as part of any study protocols and/or discussions about therapy.5-7,9-12,17,21-26 Involvement of the neck and lower jawline is common in women presenting with the U-shaped pattern of AV, and available studies only evaluate AV involving the face and do not include AV lesions present below the jawline margin. As a result, there is a considerable need for well-designed studies with laboratory assessments to include or exclude underlying detectable excess androgens and to assess the efficacy, tolerability, and safety of specific therapeutic agents both alone and in combination in adult women who present with a U-shaped pattern of AV.17
Other medical considerations that can influence treatment selection and are more likely to be present in adult versus adolescent females include underlying chronic medical disorders; concomitant medications that may interact with other oral agents; potential for pregnancy; age, particularly when prescribing OCs; and the potential desire to stop taking OCs if already used over a prolonged period.6,7
Age-Related Differentiation of Female Subgroups With AV
The age-based dividing line that defines AV in adults versus adolescent females has been described in the literature; however, the basis for published definitions of female subgroups with AV is not well-supported by strong scientific evidence.1-3,5-7,17 The conventional dividing line that was originally selected to define adult females with AV was 25 years of age or older; persistent acne is present both during adolescence and at or after 25 years of age, while late-onset acne is described as AV that first presents at 25 years of age or older.3,5-7
More recently, a range of 18 years or older has been used to classify adult female AV and a range of 12 to 17 years for adolescent female AV in subset analyses that evaluated treatment outcomes in both patient populations from phase 3 pivotal trials completed with adapalene gel 0.3% applied once daily and dapsone gel 5% applied twice daily.14-16 These subanalyses included participants with facial AV that was predominantly moderate in severity, mandated specific lesion count ranges for both comedonal and inflammatory lesions, and included only facial AV that was above the mandibular (jawline) margin.15,16,21,26 Therefore, patients with AV presenting in a U-shaped pattern with involvement below the jawline and on the neck were not included in these study analyses, as these patients were excluded from the phase 3 trials on which the analyses were based. The outcomes of these analyses apply to treatment in women who present with both inflammatory and noninflammatory facial AV lesions, which supports the observation that AV in this patient population is not always predominantly inflammatory and does not always present in a U-shaped distribution.14-16 In fact, a U-shaped pattern of distribution appears to be less common in women with AV than a mixed inflammatory and comedonal distribution that involves the face more diffusely, though more data are needed from well-designed and large-scale epidemiologic and demographic studies.5,14,17
Are there data available on the use of benzoyl peroxide with or without a topical antibiotic in women with AV?
There is a conspicuous absence of prospective clinical trials and retrospective analyses evaluating the specific use of individual AV therapies in adult females, with a particular lack of studies with topical agents (eg, benzoyl peroxide [BP]).14 Subset analyses have been completed for adapalene gel 0.3% and dapsone gel 5%.15,16 Additionally, an age-based subset analysis in females with facial AV also has been completed with clindamycin phosphate (CP) 1.2%–BP 2.5% gel once daily, with data presented but not yet fully published.14
Two identical phase 3, double-blind, randomized, 12-week, 4-arm trials compared treatment outcomes in groups treated with an aqueous-based combination gel formulation containing BP 2.5% and CP 1.2% (n=797), active monad gels (BP [n=809] or CP [n=812]), or vehicle gel (n=395), all applied once daily in patients with facial AV.22 Participants were 12 years or older (mean age range, 19.1–19.6 years; age range, 12.1–70.2 years), were of either gender (approximately 50% split in each study arm), and presented with moderate (approximately 80% of participants) or severe AV (approximately 20% of participants) at baseline. The entry criteria for lesion types and number of lesions were 17 to 40 inflammatory lesions (ie, papules, pustules, <2 nodules)(range of mean number of lesions, 25.8–26.4) and 20 to 100 noninflammatory lesions (ie, closed comedones, open comedones)(range of mean number of lesions, 44.0–47.4). Participant demographics included white (73.9%–77.5%), black/African American (16.1%–20.4%), and Asian (2.1%–3.3%), with the remaining participants distributed among a variety of other ethnic groups such as Native Hawaiian/Native Pacific Islander and Native American Indian/Native Alaskan (collectively <5% in each study arm). Therefore, approximately 1 of every 4 patients had skin of color, which provided good diversity of patients considering the large study size (N=2813). Data analysis included dichotomization of participants by severity rating (moderate or severe based on evaluator global severity score) and skin phototype (Fitzpatrick skin types I–III or IV–VI).22
The pooled results from both studies completed at 68 investigative sites demonstrated that CP 1.2%–BP 2.5% gel was superior in efficacy to each individual monad and to the vehicle in inflammatory, noninflammatory, and total lesion reductions as early as week 4 (P<.001) and at week 12, which was the study end point (P<.001), with superiority also demonstrated in achieving treatment success (defined as a >2 grade improvement according to the evaluator global severity score) compared to the 3 other study arms (P<.001).22 Subject assessments also were consistent with outcomes noted by the investigators. Cutaneous tolerability was favorable and comparable in all 4 study arms with less than 1% of participants discontinuing treatment due to adverse events.22
A subset analysis of the data from the phase 3 pivotal trials with CP 1.2%–BP 2.5% gel was completed to compare reductions in both inflammatory and noninflammatory lesions in female participants who were younger than 25 years and 25 years of age or older in all 4 study arms. This information has been presented14,17 but has not been previously published. Based on the overall results reported in the phase 3 studies, there were no differentiations in skin tolerability or safety based on participant age, gender, or skin type.22 The subanalysis included a total of 1080 females who were younger than 25 years and 395 females who were 25 years of age or older. The lesion reduction outcomes of this subanalysis are presented in the Table. Statistical analyses of the results among these age groups in the 4 study arms were not completed because the objective was to determine if there were any major or obvious differences in reduction of AV lesions based on the conventional dividing line of 25 years of age in adult women as compared to adolescent females treated with CP 1.2%–BP 2.5% gel. In addition, the large difference in numbers of female participants between the 2 age groups (>25 years of age, n=395; <25 years of age, n=1080) at least partially confounds both statistical and observational analysis. Among the women who were 25 years of age or older who were included in the subanalysis, 67.0% and 25.8% were between the ages of 25 to 35 years and 36 to 45 years, respectively. Based on the outcomes reported in the phase 3 trials and in this subgroup analysis, CP 1.2%–BP 2.5% gel applied once daily over a 12-week period appeared overall to be comparably effective in females regardless of age and with no apparent adverse events regarding differences in skin tolerability or safety.14,22 One observation that was noted was the possible trend of greater reduction in both lesion types in women older than 35 years versus younger females with the use of the combination gel or BP alone; however, the number of female participants who were older than 35 years of age was substantially less (n=102) than those who were 35 years of age or younger (n=1345), thus precluding support for any definitive conclusions about this possible trend.22
How can CP 1.2%–BP 2.5% gel be incorporated into a treatment regimen for women with facial AV?
The incorporation of CP 1.2%–BP 2.5% gel into a treatment regimen for women with facial AV is similar to the general use of BP-containing formulations in the overall management of AV.9,14,27,28 Because women with AV commonly present with facial inflammatory lesions and many also with facial comedones, CP 1.2%–BP 2.5% gel is best used once daily in the morning in combination with a topical retinoid in the evening,9,27 which can be achieved with use of CP 1.2%–BP 2.5% gel in the morning and a topical retinoid (ie, tretinoin, adapalene, tazarotene) in the evening or CP 1.2%–tretinoin 0.025% gel in the evening. It is important to note that cutaneous irritation may be more likely if neck lesions are present; the potential for bleaching of colored fabric by BP also is a practical concern.28 In addition, CP 1.2%–BP 2.5% gel may also be used in combination with topical dapsone, but both products should be applied separately at different times of the day to avoid temporary orange discoloration of the skin, which appears to be an uncommon side effect but remains a possibility based on the product information for dapsone gel 5% with regard to its concomitant use with BP.29,30
1. Perkins AC, Maglione J, Hillebrand GG, et al. Acne vulgaris in women: prevalence across the life span. J Womens Health. 2012;21:223-230.
2. Zeichner J. Evaluating and treating the adult female patient with acne. J Drugs Dermatol. 2013;12:1416-1427.
3. Goulden V, Stables GI, Cunliffe WJ. Prevalence of facial acne in adults. J Am Acad Dermatol. 1999;41:577-580.
4. Collier CN, Harper J, Cafardi JA, et al. The prevalence of acne in adults 20 years and older. J Am Acad Dermatol. 2008;58:56-59.
5. Dreno B, Layton A, Zouboulis CC, et al. Adult female acne: a new paradigm. J Eur Acad Dermatol Venereol. 2013;27:1063-1070.
6. Kim GK, Del Rosso JQ. Oral spironolactone in post-teenage female patients with acne vulgaris: practical considerations for the clinician based on current data and clinical experience. J Clin Aesthet Dermatol. 2012;5:37-50.
7. Kim GK, Michaels BB. Post-adolescent acne in women: more common and more clinical considerations. J Drugs Dermatol. 2012;11:708-713.
8. Tanghetti EA, Kawata AK, Daniels SR, et al. Understanding the burden of adult female acne. J Clin Aesthet Dermatol. 2014;7:22-30.
9. Gollnick H, Cunliffe W, Berson D, et al. Management of acne: a report from a Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol. 2003;49(suppl 1):1-37.
10. Thiboutot DM. Endocrinological evaluation and hormonal therapy for women with difficult acne. J Eur Acad Dermatol Venereol. 2001;15(suppl 3):57-61.
11. Sawaya ME, Samani N. Antiandrogens and androgen receptors. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. Philadelphia, PA: Saunders-Elsevier; 2012:361-374.
12. Harper JC. Should dermatologists prescribe hormonal contraceptives for acne? Dermatol Ther. 2009;22:452-457.
13. Preneau S, Dreno B. Female acne: a different subtype of teenager acne? J Eur Acad Dermatol Venereol. 2012;26:277-282.
14. Del Rosso JQ, Zeichner JA. What’s new in the medicine cabinet?: a panoramic review of clinically relevant information for the busy dermatologist. J Clin Aesthet Dermatol. 2014;7:26-30.
15. Berson D, Alexis A. Adapalene 0.3% for the treatment of acne in women. J Clin Aesthet Dermatol. 2013;6:32-35.
16. Del Rosso JQ, Kircik L, Gallagher C. Facing up to adult women with acne vulgaris: an analysis of pivotal trial data on dapsone 5% gel in the adult female population. Poster presented at: Fall Clinical Dermatology; October 2013; Las Vegas, NV.
17. Del Rosso JQ. Management of acne with oral spironolactone. Presented at: American Academy of Dermatology Summer Meeting; August 2013; Boston, MA.
18. Davis EC, Callender VD. A review of acne in ethnic skin: pathogenesis, clinical manifestations, and management strategies. J Clin Aesthet Dermatol. 2010;3:24-38.
19. Davis SA, Narahari S, Feldman SR, et al. Top dermatologic conditions in patients of color: an analysis of nationally representative data. J Drugs Dermatol. 2012;11:466-473.
20. Perkins AC, Cheng CE, Hillebrand GG, et al. Comparison of the epidemiology of acne vulgaris among Caucasian, Asian, Continental Indian and African American women. J Eur Acad Dermatol Venereol. 2011;25:1054-1060.
21. Draelos ZD, Carter E, Maloney JM, et al. Two randomized studies demonstrate the efficacy and safety of dapsone gel, 5% for the treatment of acne vulgaris [published online ahead of print January 17, 2007]. J Am Acad Dermatol. 2007;56:439.e1-439.e10.
22. Thiboutot D, Zaenglein A, Weiss J, et al. An aqueous gel fixed combination of clindamycin phosphate 1.2% and benzoyl peroxide 2.5% for the once-daily treatment of moderate to severe acne vulgaris: assessment of efficacy and safety in 2813 patients. J Am Acad Dermatol. 2008;59:792-800.
23. Schlessinger J, Menter A, Gold M, et al. Clinical safety and efficacy studies of a novel formulation combining
1.2% clindamycin phosphate and 0.025% tretinoin for the treatment of acne vulgaris. J Drugs Dermatol. 2007;6:607-615.
24. Fleischer AB Jr, Dinehart S, Stough D, et al. Safety and efficacy of a new extended-release formulation of minocycline. Cutis. 2006;78(suppl 4):21-31.
25. Gollnick HP, Draelos Z, Glenn MJ, et al. Adapalene-benzoyl peroxide, a unique fixed-dose combination topical gel for the treatment of acne vulgaris: a transatlantic, randomized, double-blind, controlled study in 1670 patients. Br J Dermatol. 2009;161:1180-1189.
26. Thiboutot D, Arsonnaud S, Soto P. Efficacy and tolerability of adapalene 0.3% gel compared to tazarotene 0.1% gel in the treatment of acne vulgaris. J Drugs Dermatol. 2008;7(suppl 6):3-10.
27. Zeichner JA. Optimizing topical combination therapy for the treatment of acne vulgaris. J Drugs Dermatol. 2012;11:313-317.
28. Tanghetti EA, Popp KF. A current review of topical benzoyl peroxide: new perspectives on formulation and utilization. Dermatol Clin. 2009;27:17-24.
29. Fleischer AB, Shalita A, Eichenfield LF. Dapsone gel 5% in combination with adapalene gel 0.1%, benzoyl peroxide gel 4% or moisturizer for the treatment of acne vulgaris: a 12-week, randomized, double-blind study. J Drugs Dermatol. 2010;9:33-40.
30. Aczone (dapsone gel 5%) [package insert]. Irvine, CA: Allergan, Inc; 2013.
1. Perkins AC, Maglione J, Hillebrand GG, et al. Acne vulgaris in women: prevalence across the life span. J Womens Health. 2012;21:223-230.
2. Zeichner J. Evaluating and treating the adult female patient with acne. J Drugs Dermatol. 2013;12:1416-1427.
3. Goulden V, Stables GI, Cunliffe WJ. Prevalence of facial acne in adults. J Am Acad Dermatol. 1999;41:577-580.
4. Collier CN, Harper J, Cafardi JA, et al. The prevalence of acne in adults 20 years and older. J Am Acad Dermatol. 2008;58:56-59.
5. Dreno B, Layton A, Zouboulis CC, et al. Adult female acne: a new paradigm. J Eur Acad Dermatol Venereol. 2013;27:1063-1070.
6. Kim GK, Del Rosso JQ. Oral spironolactone in post-teenage female patients with acne vulgaris: practical considerations for the clinician based on current data and clinical experience. J Clin Aesthet Dermatol. 2012;5:37-50.
7. Kim GK, Michaels BB. Post-adolescent acne in women: more common and more clinical considerations. J Drugs Dermatol. 2012;11:708-713.
8. Tanghetti EA, Kawata AK, Daniels SR, et al. Understanding the burden of adult female acne. J Clin Aesthet Dermatol. 2014;7:22-30.
9. Gollnick H, Cunliffe W, Berson D, et al. Management of acne: a report from a Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol. 2003;49(suppl 1):1-37.
10. Thiboutot DM. Endocrinological evaluation and hormonal therapy for women with difficult acne. J Eur Acad Dermatol Venereol. 2001;15(suppl 3):57-61.
11. Sawaya ME, Samani N. Antiandrogens and androgen receptors. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. Philadelphia, PA: Saunders-Elsevier; 2012:361-374.
12. Harper JC. Should dermatologists prescribe hormonal contraceptives for acne? Dermatol Ther. 2009;22:452-457.
13. Preneau S, Dreno B. Female acne: a different subtype of teenager acne? J Eur Acad Dermatol Venereol. 2012;26:277-282.
14. Del Rosso JQ, Zeichner JA. What’s new in the medicine cabinet?: a panoramic review of clinically relevant information for the busy dermatologist. J Clin Aesthet Dermatol. 2014;7:26-30.
15. Berson D, Alexis A. Adapalene 0.3% for the treatment of acne in women. J Clin Aesthet Dermatol. 2013;6:32-35.
16. Del Rosso JQ, Kircik L, Gallagher C. Facing up to adult women with acne vulgaris: an analysis of pivotal trial data on dapsone 5% gel in the adult female population. Poster presented at: Fall Clinical Dermatology; October 2013; Las Vegas, NV.
17. Del Rosso JQ. Management of acne with oral spironolactone. Presented at: American Academy of Dermatology Summer Meeting; August 2013; Boston, MA.
18. Davis EC, Callender VD. A review of acne in ethnic skin: pathogenesis, clinical manifestations, and management strategies. J Clin Aesthet Dermatol. 2010;3:24-38.
19. Davis SA, Narahari S, Feldman SR, et al. Top dermatologic conditions in patients of color: an analysis of nationally representative data. J Drugs Dermatol. 2012;11:466-473.
20. Perkins AC, Cheng CE, Hillebrand GG, et al. Comparison of the epidemiology of acne vulgaris among Caucasian, Asian, Continental Indian and African American women. J Eur Acad Dermatol Venereol. 2011;25:1054-1060.
21. Draelos ZD, Carter E, Maloney JM, et al. Two randomized studies demonstrate the efficacy and safety of dapsone gel, 5% for the treatment of acne vulgaris [published online ahead of print January 17, 2007]. J Am Acad Dermatol. 2007;56:439.e1-439.e10.
22. Thiboutot D, Zaenglein A, Weiss J, et al. An aqueous gel fixed combination of clindamycin phosphate 1.2% and benzoyl peroxide 2.5% for the once-daily treatment of moderate to severe acne vulgaris: assessment of efficacy and safety in 2813 patients. J Am Acad Dermatol. 2008;59:792-800.
23. Schlessinger J, Menter A, Gold M, et al. Clinical safety and efficacy studies of a novel formulation combining
1.2% clindamycin phosphate and 0.025% tretinoin for the treatment of acne vulgaris. J Drugs Dermatol. 2007;6:607-615.
24. Fleischer AB Jr, Dinehart S, Stough D, et al. Safety and efficacy of a new extended-release formulation of minocycline. Cutis. 2006;78(suppl 4):21-31.
25. Gollnick HP, Draelos Z, Glenn MJ, et al. Adapalene-benzoyl peroxide, a unique fixed-dose combination topical gel for the treatment of acne vulgaris: a transatlantic, randomized, double-blind, controlled study in 1670 patients. Br J Dermatol. 2009;161:1180-1189.
26. Thiboutot D, Arsonnaud S, Soto P. Efficacy and tolerability of adapalene 0.3% gel compared to tazarotene 0.1% gel in the treatment of acne vulgaris. J Drugs Dermatol. 2008;7(suppl 6):3-10.
27. Zeichner JA. Optimizing topical combination therapy for the treatment of acne vulgaris. J Drugs Dermatol. 2012;11:313-317.
28. Tanghetti EA, Popp KF. A current review of topical benzoyl peroxide: new perspectives on formulation and utilization. Dermatol Clin. 2009;27:17-24.
29. Fleischer AB, Shalita A, Eichenfield LF. Dapsone gel 5% in combination with adapalene gel 0.1%, benzoyl peroxide gel 4% or moisturizer for the treatment of acne vulgaris: a 12-week, randomized, double-blind study. J Drugs Dermatol. 2010;9:33-40.
30. Aczone (dapsone gel 5%) [package insert]. Irvine, CA: Allergan, Inc; 2013.
Practice Points
- Adult women with acne vulgaris (AV) can present with a U-shaped pattern of predominantly inflammatory papules, pustules, and nodules involving the lower face, jawline region, and anterior and lateral neck; however, many women present with mixed comedonal and inflammatory acne involving the face more diffusely with a presentation similar to what is typically seen in adolescent AV.
- Topical therapy for adult women with acne has been evaluated in subanalyses of data from phase 3 studies with good efficacy and favorable tolerability shown with adapalene gel 0.3% once daily, dapsone gel 5% twice daily, and clindamycin phosphate 1.2%–benzoyl peroxide (BP) 2.5% gel once daily. The latter agent requires cautious use below the jawline margin, as BP can bleach colored fabric of clothing such as shirts, blouses, and sweaters. These topical agents may be used in combination based on the clinical situation, including with systemic therapies for AV.
Calcipotriene–Betamethasone Dipropionate Topical Suspension in the Management of Psoriasis: A Status Report on Available Data With an Overview of Practical Clinical Application
Psoriasis is a common inflammatory skin disorder that appears to be induced by multifactorial pathophysiologic processes associated with immunologic dysregulation.1 It can affect patients of any age, gender, and ethnicity, and it presents clinically with a variety of visible manifestations. The disease course and severity of psoriasis varies among affected patients.1 Chronic plaque psoriasis (PP), also referred to as psoriasis vulgaris, is the most common clinical presentation.1,2 Although many patients are affected by psoriasis that is widespread and in some cases severe, the majority of affected patients exhibit localized involvement that usually affects less than 2% to 5% of the body surface area. Although the skin at any anatomic location can be affected, commonly involved sites are described by the mnemonic term SNAKES (scalp, nails, anogenital region, knees, elbows, sacral region).2,3
Because the majority of patients with PP present with localized disease, topical therapy is the foundation of treatment in most cases. Topical corticosteroids (TCs) are the most commonly utilized agents, supported by a long track record of favorable efficacy and safety over approximately 6 decades.4,5 However, optimal management of PP with TCs requires use of a formulation that is of adequate potency, is adaptable for application to the affected body sites, and is properly monitored and adjusted to avoid potential TC-induced adverse effects.4-6 Nonsteroidal topical therapies such as vitamin D analogues (eg, calcipotriene) and retinoids (eg, tazarotene) are commonly integrated into topical regimens to reduce the application frequency and duration of TC use as well as to sustain efficacy.5,7,8 Plaque psoriasis is characteristically a chronic disease associated with periods of persistence and episodes of flaring; therefore, intermittent use of TC therapy along with concurrent or sequential use of a nonsteroidal topical agent are commonly employed to achieve and sustain control of the disorder.7-9
In the last decade, several advances have revolutionized the management of psoriasis, especially for PP patients with extensive involvement who require systemic therapy and/or phototherapy as well as for those with psoriatic arthritis.10,11 The availability of biologic agents such as tumor necrosis factor a inhibitors and certain interleukin inhibitors (eg, IL-12/IL-23) have been at the forefront of major advances in PP treatment, with some agents also blocking the progression of joint destruction associated with psoriatic arthritis.10-12 However, even when patients with PP respond favorably to biologic therapy, it is not uncommon for them to still be affected by some persistent PP. In these cases, although much of the chronic PP may clear with use of the biologic agent, persistence of psoriatic plaques may involve the lower extremities, scalp, and/or trunk, with topical therapy often added to augment the therapeutic response.13-15
This article provides a review of a patented topical suspension combination formulation that contains calcipotriene hydrate 0.005%, a vitamin D analogue, and betamethasone dipropio-nate (Bd) 0.064%, a high-potency TC. In 2008, the US Food and Drug Administration approved the once-daily application of calcipotriene 0.005%–Bd 0.064% topical suspension (C/Bd-TS) for the treatment of PP; this formulation is approved for use on the scalp and body in patients 18 years of age and older. According to the product insert, the recommended maximum duration of treatment with C/Bd-TS once daily is 8 weeks, and patients may not exceed a maximum weekly dose of 100 g.16 It is important to note that the terms calcipotriene and calcipotriol refer to the same molecule and are used interchangeably in the literature. Formulation characteristics of C/Bd-TS, perspectives on modes of action, outcomes from pivotal trials, and efficacy and safety data reported from additional studies are discussed in this article.
What are the formulation characteristics of C/Bd-TS?
Each gram of C/Bd-TS contains 52.18 mg of calcipotriene hydrate (equivalent to 50 µg of calcipotriene) and 0.643 µg of Bd (equivalent to 0.5 mg of betamethasone), formulated together in a viscous, nearly odorless, almost clear to slightly off-white suspension. The excipients are hydrogenated castor oil, polypropylene glycol 11 stearyl ether, α-tocopherol, butylhydroxytoluene, and mineral oil, collectively producing a gel base in which both active ingredients are suspended.16 Although the viscous quality of the suspension warrants some additional effort for removal during hair washing, the tenacious gel-like viscosity assists in removing scale on psoriatic plaques, which is often adherent, especially on the scalp. Additionally, it is important that C/Bd-TS be shaken well before use.16 Initially, C/Bd-TS was studied and marketed in the United States for treatment of scalp psoriasis; however, the indication was expanded to include treatment of PP on the rest of the body, supported by evidence from randomized controlled trials (RCTs).16-23
Vitamin D analogues (eg, calcipotriene/calcitriol) have been shown to be photolabile when exposed to UV light, especially UVA. They also have been shown to be chemically incompatible and less stable when admixed with a variety of other active ingredients and/or vehicles used to treat PP, including hydrocortisone valerate ointment 0.2%, ammonium lactate lotion 12%, and salicylic acid compound ointment 6%.24-26 As a result, it is important for clinicians to consider avoidance of concomitant topical calcipotriene application with use of a TC unless the stability of the active ingredients has been tested when the formulations are combined. Calcipotriene 0.005%/Bd 0.064% topical suspension utilizes vehicle technology that maintains the stability and activity of both calcipotriene and Bd within the suspension formulation.16,26
What is the rationale behind combining calcipotriene and Bd in a single formulation for the treatment of PP?
The potential advantages of C/Bd-TS include the combined modes of action of 2 different active ingredients used for treatment of PP, complementary immunomodulatory effects as compared to use of a TC or vitamin D analogue alone, ease of use with a single product applied once daily, adaptability of the vehicle for use on scalp and/or body skin, and improvement in quality-of-life (QOL) measures.27-34
Combined Modes of Action
Calcipotriene 0.005%–Bd 0.064% topical suspension combines the modes of action of a high-potency topical suspension and a vitamin D analogue for the treatment of PP in a single stable gel formulation that is approved in the United States for treatment of PP in adults.16 The multiple anti-inflammatory properties of corticosteroids as well as the efficacy and safety of TC therapy for psoriasis have been well described.4,6,7,9,27 The antiproliferative and anti-inflammatory properties of vitamin D analogues that appear to correlate with therapeutic effects in the treatment of PP also have been discussed in the literature.28
Complementary Immunomodulatory Effects
More recent studies using various research assays have provided further evidence supporting relevant immunomodulatory properties of calcipotriene alone and in combination with Bd that favorably modify immune dysregulation pathways described more recently in the pathogenesis of PP.1,29,30 Treatment of psoriatic plaques with calcipotriene has been shown to suppress the increased production of peptide alarmins (psoriasin and koebnerisin) in psoriatic skin and their TH17-mediated regulation in epidermal ke-ratinocytes, thus interfering with the S100 amplification loop that appears to produce inflammation in psoriasis.29 In T-lymphocyte cultures evaluating exposure to calcipotriene and Bd both alone and as a combined therapy, calcipotriene inhibited IFN-g, IL-8, IL-17, and IL-22 expression, and it reversed the corticosteroid-induced suppression of IL-4, IL-5, IL-10, and IL-13; Bd inhibited both IL-6 and tumor necrosis factor α expression. The outcomes demonstrated that the combination of calcipotriene and Bd inhibited the endogenous release of TH1- and TH17-associated cytokines that are associated with psoriatic inflammation and together induced a more favorable anti-inflammatory cytokine profile.30 Although the broad range of anti-inflammatory effects provided by a TC of adequate potency, such as Bd, can clear or markedly improve PP, the concurrent use of calcipotriene was shown to provide additional immunomodulatory effects that suppressed the key TH17/TH1 pathophysiologic mediators of psoriatic inflammation and simultaneously induced a TH2/T regulatory response that is believed to provide therapeutic benefit.29,30
Ease of Use and Vehicle Adaptability
A once-daily regimen and a vehicle formulation adaptable for use on both the scalp and body are advantageous in enhancing the potential for greater patient adherence.31,32 The adaptability of the C/Bd-TS for use on the scalp and/or body is supported by several studies encompassing a large number of actively treated subjects. Calcipotriene 0.005%–Bd 0.064% topical suspension has been extensively studied in patients with PP on the scalp and/or body as evidenced by a pooled analysis of 9 eight-week RCTs (scalp, n=6; body, n=3) that encompassed 2777 total subjects treated once daily for PP (scalp, n=1953; body, n=824).23 Additionally, C/Bd-TS applied once daily was evaluated in an open-label, single-arm, 8-week, phase 2 study of adolescents (N=78; age range, 12–17 years [mean age, 14.6 years]) with scalp psoriasis (mean affected scalp area, 43.7%). The investigator global assessment of treatment success (clear or almost clear) and the patient global assessment of treatment success (clear or very mild) were essentially identical among participants and investigators with 85% and 87% reported after 8 weeks, respectively; approximately 50% of participants achieved treatment success after 2 weeks based on both the investigator global assessment and patient global assessment.33
Improvement in QOL Measures
Quality-of-life measures were compared in an 8-week RCT of participants with at least moderate scalp psoriasis treated with C/Bd-TS once daily (n=207) or calcipotriene solution twice daily (n=107). Significantly greater improvement in QOL scores compared to baseline were noted at all time points using the Skindex-16 questionnaire in participants treated with C/Bd-TS compared to calcipotriene solution (total score, P<.001 at weeks 2 and 4 and P=.008 at week 8; symptoms score, P<.001 at weeks 2 and 4 and P=.004 at week 8; emotions score, P<.001 at weeks 2 and 4 and P=.005 at week 8).34 A 4-week, open-label, noninterventional cohort, postmarketing (“real life”) study of 721 patients treated at 333 dermatology centers with C/Bd-TS showed a 69.5% improvement in the scalp life quality index score compared to baseline (P<.0001), with 89.5% and 90.4% of participants reporting that C/Bd-TS was better/much better than previously used therapies for scalp psoriasis and easy/very easy to use, respectively.35 An 8-week RCT trial evaluated C/Bd-TS once daily compared to calcipotriene alone, betamethasone dipropionate alone, and vehicle in 1152 participants with mild to moderate PP involving the trunk and extremities. Participants treated with C/Bd-TS (n=442) demonstrated superior reductions in QOL scores using the dermatology life quality index at weeks 4 and 8 compared to those treated with Bd alone (n=418) or vehicle (n=77) but not compared to calcipotriene alone (n=80).19
What data are available on the efficacy and safety of C/Bd-TS?
Several clinical studies have evaluated the efficacy, tolerability, and safety of C/Bd-TS applied once daily for PP of the scalp and body (ie, trunk, extremities). Most studies were completed over a duration of 8 weeks in adults16-23; however, studies also have been performed in adolescents,33 in adults treated for up to 52 weeks,36 and in a subgroup of Hispanic/Latino and black/African American patients with scalp psoriasis.37 The Table provides a detailed summary of primary efficacy data along with important tolerability and safety considerations based on study outcomes.
What practical recommendations can be made regarding the use of C/Bd-TS for PP?
Calcipotriene 0.005%–Bd 0.064% topical suspension applied once daily provides a formulation that allows for treatment of PP involving both the scalp and body using a single product, which provides an element of convenience and is likely to enhance compliance and reduce costs compared with the use of 2 separate products. The efficacy and safety of C/Bd-TS has been well established in several studies,16-23,37 including a 52-week trial in patients with scalp psoriasis.36 The combination of calcipotriene and Bd appears to favorably address the pathophysiologic pathways involved in psoriasis.29,30 Calcipotriene 0.005%–Bd 0.064% topical suspension is a rational option for the treatment of PP in patients with localized disease or in patients treated systemically or with phototherapy for more extensive disease who exhibit persistence or recurrence of scattered areas of PP.6-9,14,15 Appropriate use of C/Bd-TS is likely to achieve favorable efficacy with a low risk of tolerability reactions and a very low risk of major adverse drug reactions.16-23,36-38
1. Guttman-Yassky E, Krueger JG. Psoriasis: evolution of pathogenic concepts and new therapies through phases of translational research. Br J Dermatol. 2007;157:1103-1115.
2. Menter MA. An overview of psoriasis. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:1-21.
3. Sandoval LF, Feldman SR. General approach to psoriasis treatment. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:3-8.
4. Zeichner JA, Lebwohl MG, Menter A, et al. Optimizing topical therapies for treating psoriasis: a consensus conference. Cutis. 2010;(3 suppl):5-31.
5. American Academy of Dermatology Work Group, Menter A, Korman NJ, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 6. guidelines of care for the treatment of psoriasis and psoriatic arthritis: case-based presentations and evidence-based conclusions [published online ahead of print February 8, 2011]. J Am Acad Dermatol. 2011;65:137-174.
6. Del Rosso J, Friedlander SF. Corticosteroids: options in the era of steroid-sparing therapy. J Am Acad Dermatol. 2005;53(1, suppl 1):S50-S58.
7. Menter A, Korman NJ, Elmets CA, et al; American Academy of Dermatology. Guidelines of care for the management of psoriasis and psoriatic arthritis. section 3. guidelines of care for the management and treatment of psoriasis with topical therapies [published online ahead of print February 13, 2009]. J Am Acad Dermatol. 2009;60:643-659.
8. Koo J. New developments in topical sequential therapy for psoriasis. Skin Therapy Lett. 2005;10:1-4.
9. Mason AR, Mason J, Cork M, et al. Topical treatments for chronic plaque psoriasis. Cochrane Database Syst Rev. 2009;2:CD005028.
10. Belge K, Brück J, Ghoreschi K. Advances in treating psoriasis. F1000Prime Rep. 2014;6:4.
11. Mease PJ, Armstrong AW. Managing patients with psoriatic disease: the diagnosis and pharmacologic treatment of psoriatic arthritis in patients with psoriasis. Drugs. 2014;74:423-441.
12. Boehncke WH, Qureshi A, Merola JF, et al. Diagnosing and treating psoriatic arthritis: an update. Br J Dermatol. 2014;170:772-786.
13. Feldman SR. Effectiveness of clobetasol propionate spray 0.05% added to other stable treatments: add-on therapy in the COBRA trial. Cutis. 2007;80(suppl 5):20-28.
14. Feldman SR, Gelfand JM, Stein Gold L, et al. The role of topical therapy for patients with extensive psoriasis. Cutis. 2007;79(suppl 1[ii]):18-31.
15. Kircik L. Topical calcipotriene 0.005% and betamethasone dipropionate 0.064% maintains efficacy of etanercept after step-down dose in patients with moderate-to-severe plaque psoriasis: results of an open label trial. J Drugs Dermatol. 2011;10:878-882.
16. Taclonex [product insert]. Parsippany, NJ: LEO Pharma Inc; 2014.
17. Buckley C, Hoffmann V, Shapiro J, et al. Calcipotriol plus betamethasone dipropionate scalp formulation is effective and well tolerated in the treatment of scalp psoriasis: a phase II study. Dermatology. 2008;217:107-113.
18. Fleming C, Ganslandt C, Guenther L, et al. Calcipotriol plus betamethasone dipropionate gel compared with its active components in the same vehicle and the vehicle alone in the treatment of psoriasis vulgaris: a randomized, parallel group, double-blind, exploratory study. Eur J Dermatol. 2010;20:465-471.
19. Menter A, Stein Gold L, Bukhalo M, et al. Calcipotriene plus betamethasone dipropionate topical suspension for the treatment of mild to moderate psoriasis vulgaris on the body: a randomized, double-blind, vehicle-controlled trial. J Drugs Dermatol. 2013;12:92-98.
20. Jemec GBE, Ganslandt C, Ortonne JP, et al. A new scalp formulation of calcipotriene plus betamethasone compared with its active ingredients and the vehicle in the treatment of scalp psoriasis: a randomized, double-blind, controlled trial. J Am Acad Dermatol. 2008;59:455-463.
21. van de Kerkhof PC, Hoffmann V, Anstey A, et al. A new scalp formulation of calcipotriol plus betamethasone dipropionate compared with each of its active ingredients in the same vehicle for the treatment of scalp psoriasis: a randomized, double-blind, controlled trial. Br J Dermatol. 2009;160:170-176.
22. Langley RG, Gupta A, Papp K, et al. Calcipotriol plus betamethasone dipropionate gel compared with tacalcitol ointment and the gel vehicle alone in patients with psoriasis vulgaris: a randomized, controlled clinical trial. Dermatology. 2011;222:148-156.
23. Kragballe K, van de Kerkhof P. Pooled safety analysis of calcipotriol plus betamethasone dipropionate gel for the treatment of psoriasis on the body and scalp. J Eur Acad Dermatol Venereol. 2014;28:10-21.
24. Lebwohl MG, Corvari L. Compatibility of topical therapies for psoriasis: challenges and innovations. Cutis. 2007;79(suppl 1[ii]):5-10.
25. Patel B, Siskin S, Krazmien R, et al. Compatibility of calcipotriene with other topical medications. J Am Acad Dermatol. 1998;38(6, pt 1):1010-1011.
26. Traulsen J. Bioavailability of betamethasone dipropionate when combined with calcipotriol. Int J Dermatol. 2004;43:611-617.
27. Sandoval LF, Feldman SR. Topical corticosteroids. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:21-36.
28. deShazo R, Krueger GG, Duffin KC. Topical agents. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:41-65.
29. Hegyi Z, Zwicker S, Bureik D, et al. Vitamin D analog calcipotriol suppresses the Th17 cytokine-induced proinflammatory S100 “alarmins” psoriasin (S100A7) and koebnerisin (S100A15) in psoriasis. J Invest Dermatol. 2012;132:1416-1424.
30. Lovato P, Norsgaard H, Ropke M. Key immunomodulatory effects exerted by calcipotriol in combination with corticosteroid on human cells. Poster presented at: 21st European Academy of Dermatology and Venereology Congress; September 27-30, 2012; Prague, Czech Republic.
31. Renton C. Diagnosis and treatment of adults with scalp psoriasis. Nurs Stand. 2014;28:35-39.
32. Feldman SR, Housman TS. Patients’ vehicle preference for corticosteroid treatments of scalp psoriasis. Am J Clin Dermatol. 2003;4:221-224.
33. Gooderham M, Debarre JM, Keddy-Grant J, et al. Safety and efficacy of calcipotriene plus betamethasone dipropionate topical suspension in adolescents with scalp psoriasis: an open, non-controlled, 8-week trial. Poster presented at: American Academy of Dermatology 72nd Annual Meeting; March 21-25, 2014; Denver, CO.
34. Ortonne JP, Tan J, Nordin P, et al. Quality of life of patients with scalp psoriasis treated with calcipotriene plus betamethasone dipropionate gel compared to calcipotriene solution. J Am Academy Dermatol. 2008;58(2, suppl 2):AB134.
35. Mrowietz U, Macheleidt O, Eicke C. Effective treatment and improvement of quality of life in patients with scalp psoriasis by topical use of calcipotriol/betamethasone (Xamiol®-gel): results [in German]. J Dtsch Dermatol Ges. 2011;9:825-831.
36. Luger TA, Cambazard F, Larsen FG, et al. A study of the safety and efficacy of calcipotriol and betamethasone dipropionate scalp formulation in the long-term management of scalp psoriasis. Dermatology. 2008;217:321-328.
37. Tyring S, Mendoza N, Appell M, et al. A calcipotriene/betamethasone dipropionate two-compound scalp formulation in the treatment of scalp psoriasis in Hispanic/Latino and Black/African American patients: results of the randomized, 8-week, double-blind phase of a clinical trial. Int J Dermatol. 2010;49:1328-1333.
38. Silver S, Tuppal R, Gupta AK, et al. Effect of calcipotriene plus betamethasone dipropionate topical suspension on the hypothalamic-pituitary-adrenal axis and calcium homeostasis in subjects with extensive psoriasis vulgaris: an open, non-controlled, 8-week trial. J Drugs Dermatol. 2013;12:882-888.
Psoriasis is a common inflammatory skin disorder that appears to be induced by multifactorial pathophysiologic processes associated with immunologic dysregulation.1 It can affect patients of any age, gender, and ethnicity, and it presents clinically with a variety of visible manifestations. The disease course and severity of psoriasis varies among affected patients.1 Chronic plaque psoriasis (PP), also referred to as psoriasis vulgaris, is the most common clinical presentation.1,2 Although many patients are affected by psoriasis that is widespread and in some cases severe, the majority of affected patients exhibit localized involvement that usually affects less than 2% to 5% of the body surface area. Although the skin at any anatomic location can be affected, commonly involved sites are described by the mnemonic term SNAKES (scalp, nails, anogenital region, knees, elbows, sacral region).2,3
Because the majority of patients with PP present with localized disease, topical therapy is the foundation of treatment in most cases. Topical corticosteroids (TCs) are the most commonly utilized agents, supported by a long track record of favorable efficacy and safety over approximately 6 decades.4,5 However, optimal management of PP with TCs requires use of a formulation that is of adequate potency, is adaptable for application to the affected body sites, and is properly monitored and adjusted to avoid potential TC-induced adverse effects.4-6 Nonsteroidal topical therapies such as vitamin D analogues (eg, calcipotriene) and retinoids (eg, tazarotene) are commonly integrated into topical regimens to reduce the application frequency and duration of TC use as well as to sustain efficacy.5,7,8 Plaque psoriasis is characteristically a chronic disease associated with periods of persistence and episodes of flaring; therefore, intermittent use of TC therapy along with concurrent or sequential use of a nonsteroidal topical agent are commonly employed to achieve and sustain control of the disorder.7-9
In the last decade, several advances have revolutionized the management of psoriasis, especially for PP patients with extensive involvement who require systemic therapy and/or phototherapy as well as for those with psoriatic arthritis.10,11 The availability of biologic agents such as tumor necrosis factor a inhibitors and certain interleukin inhibitors (eg, IL-12/IL-23) have been at the forefront of major advances in PP treatment, with some agents also blocking the progression of joint destruction associated with psoriatic arthritis.10-12 However, even when patients with PP respond favorably to biologic therapy, it is not uncommon for them to still be affected by some persistent PP. In these cases, although much of the chronic PP may clear with use of the biologic agent, persistence of psoriatic plaques may involve the lower extremities, scalp, and/or trunk, with topical therapy often added to augment the therapeutic response.13-15
This article provides a review of a patented topical suspension combination formulation that contains calcipotriene hydrate 0.005%, a vitamin D analogue, and betamethasone dipropio-nate (Bd) 0.064%, a high-potency TC. In 2008, the US Food and Drug Administration approved the once-daily application of calcipotriene 0.005%–Bd 0.064% topical suspension (C/Bd-TS) for the treatment of PP; this formulation is approved for use on the scalp and body in patients 18 years of age and older. According to the product insert, the recommended maximum duration of treatment with C/Bd-TS once daily is 8 weeks, and patients may not exceed a maximum weekly dose of 100 g.16 It is important to note that the terms calcipotriene and calcipotriol refer to the same molecule and are used interchangeably in the literature. Formulation characteristics of C/Bd-TS, perspectives on modes of action, outcomes from pivotal trials, and efficacy and safety data reported from additional studies are discussed in this article.
What are the formulation characteristics of C/Bd-TS?
Each gram of C/Bd-TS contains 52.18 mg of calcipotriene hydrate (equivalent to 50 µg of calcipotriene) and 0.643 µg of Bd (equivalent to 0.5 mg of betamethasone), formulated together in a viscous, nearly odorless, almost clear to slightly off-white suspension. The excipients are hydrogenated castor oil, polypropylene glycol 11 stearyl ether, α-tocopherol, butylhydroxytoluene, and mineral oil, collectively producing a gel base in which both active ingredients are suspended.16 Although the viscous quality of the suspension warrants some additional effort for removal during hair washing, the tenacious gel-like viscosity assists in removing scale on psoriatic plaques, which is often adherent, especially on the scalp. Additionally, it is important that C/Bd-TS be shaken well before use.16 Initially, C/Bd-TS was studied and marketed in the United States for treatment of scalp psoriasis; however, the indication was expanded to include treatment of PP on the rest of the body, supported by evidence from randomized controlled trials (RCTs).16-23
Vitamin D analogues (eg, calcipotriene/calcitriol) have been shown to be photolabile when exposed to UV light, especially UVA. They also have been shown to be chemically incompatible and less stable when admixed with a variety of other active ingredients and/or vehicles used to treat PP, including hydrocortisone valerate ointment 0.2%, ammonium lactate lotion 12%, and salicylic acid compound ointment 6%.24-26 As a result, it is important for clinicians to consider avoidance of concomitant topical calcipotriene application with use of a TC unless the stability of the active ingredients has been tested when the formulations are combined. Calcipotriene 0.005%/Bd 0.064% topical suspension utilizes vehicle technology that maintains the stability and activity of both calcipotriene and Bd within the suspension formulation.16,26
What is the rationale behind combining calcipotriene and Bd in a single formulation for the treatment of PP?
The potential advantages of C/Bd-TS include the combined modes of action of 2 different active ingredients used for treatment of PP, complementary immunomodulatory effects as compared to use of a TC or vitamin D analogue alone, ease of use with a single product applied once daily, adaptability of the vehicle for use on scalp and/or body skin, and improvement in quality-of-life (QOL) measures.27-34
Combined Modes of Action
Calcipotriene 0.005%–Bd 0.064% topical suspension combines the modes of action of a high-potency topical suspension and a vitamin D analogue for the treatment of PP in a single stable gel formulation that is approved in the United States for treatment of PP in adults.16 The multiple anti-inflammatory properties of corticosteroids as well as the efficacy and safety of TC therapy for psoriasis have been well described.4,6,7,9,27 The antiproliferative and anti-inflammatory properties of vitamin D analogues that appear to correlate with therapeutic effects in the treatment of PP also have been discussed in the literature.28
Complementary Immunomodulatory Effects
More recent studies using various research assays have provided further evidence supporting relevant immunomodulatory properties of calcipotriene alone and in combination with Bd that favorably modify immune dysregulation pathways described more recently in the pathogenesis of PP.1,29,30 Treatment of psoriatic plaques with calcipotriene has been shown to suppress the increased production of peptide alarmins (psoriasin and koebnerisin) in psoriatic skin and their TH17-mediated regulation in epidermal ke-ratinocytes, thus interfering with the S100 amplification loop that appears to produce inflammation in psoriasis.29 In T-lymphocyte cultures evaluating exposure to calcipotriene and Bd both alone and as a combined therapy, calcipotriene inhibited IFN-g, IL-8, IL-17, and IL-22 expression, and it reversed the corticosteroid-induced suppression of IL-4, IL-5, IL-10, and IL-13; Bd inhibited both IL-6 and tumor necrosis factor α expression. The outcomes demonstrated that the combination of calcipotriene and Bd inhibited the endogenous release of TH1- and TH17-associated cytokines that are associated with psoriatic inflammation and together induced a more favorable anti-inflammatory cytokine profile.30 Although the broad range of anti-inflammatory effects provided by a TC of adequate potency, such as Bd, can clear or markedly improve PP, the concurrent use of calcipotriene was shown to provide additional immunomodulatory effects that suppressed the key TH17/TH1 pathophysiologic mediators of psoriatic inflammation and simultaneously induced a TH2/T regulatory response that is believed to provide therapeutic benefit.29,30
Ease of Use and Vehicle Adaptability
A once-daily regimen and a vehicle formulation adaptable for use on both the scalp and body are advantageous in enhancing the potential for greater patient adherence.31,32 The adaptability of the C/Bd-TS for use on the scalp and/or body is supported by several studies encompassing a large number of actively treated subjects. Calcipotriene 0.005%–Bd 0.064% topical suspension has been extensively studied in patients with PP on the scalp and/or body as evidenced by a pooled analysis of 9 eight-week RCTs (scalp, n=6; body, n=3) that encompassed 2777 total subjects treated once daily for PP (scalp, n=1953; body, n=824).23 Additionally, C/Bd-TS applied once daily was evaluated in an open-label, single-arm, 8-week, phase 2 study of adolescents (N=78; age range, 12–17 years [mean age, 14.6 years]) with scalp psoriasis (mean affected scalp area, 43.7%). The investigator global assessment of treatment success (clear or almost clear) and the patient global assessment of treatment success (clear or very mild) were essentially identical among participants and investigators with 85% and 87% reported after 8 weeks, respectively; approximately 50% of participants achieved treatment success after 2 weeks based on both the investigator global assessment and patient global assessment.33
Improvement in QOL Measures
Quality-of-life measures were compared in an 8-week RCT of participants with at least moderate scalp psoriasis treated with C/Bd-TS once daily (n=207) or calcipotriene solution twice daily (n=107). Significantly greater improvement in QOL scores compared to baseline were noted at all time points using the Skindex-16 questionnaire in participants treated with C/Bd-TS compared to calcipotriene solution (total score, P<.001 at weeks 2 and 4 and P=.008 at week 8; symptoms score, P<.001 at weeks 2 and 4 and P=.004 at week 8; emotions score, P<.001 at weeks 2 and 4 and P=.005 at week 8).34 A 4-week, open-label, noninterventional cohort, postmarketing (“real life”) study of 721 patients treated at 333 dermatology centers with C/Bd-TS showed a 69.5% improvement in the scalp life quality index score compared to baseline (P<.0001), with 89.5% and 90.4% of participants reporting that C/Bd-TS was better/much better than previously used therapies for scalp psoriasis and easy/very easy to use, respectively.35 An 8-week RCT trial evaluated C/Bd-TS once daily compared to calcipotriene alone, betamethasone dipropionate alone, and vehicle in 1152 participants with mild to moderate PP involving the trunk and extremities. Participants treated with C/Bd-TS (n=442) demonstrated superior reductions in QOL scores using the dermatology life quality index at weeks 4 and 8 compared to those treated with Bd alone (n=418) or vehicle (n=77) but not compared to calcipotriene alone (n=80).19
What data are available on the efficacy and safety of C/Bd-TS?
Several clinical studies have evaluated the efficacy, tolerability, and safety of C/Bd-TS applied once daily for PP of the scalp and body (ie, trunk, extremities). Most studies were completed over a duration of 8 weeks in adults16-23; however, studies also have been performed in adolescents,33 in adults treated for up to 52 weeks,36 and in a subgroup of Hispanic/Latino and black/African American patients with scalp psoriasis.37 The Table provides a detailed summary of primary efficacy data along with important tolerability and safety considerations based on study outcomes.
What practical recommendations can be made regarding the use of C/Bd-TS for PP?
Calcipotriene 0.005%–Bd 0.064% topical suspension applied once daily provides a formulation that allows for treatment of PP involving both the scalp and body using a single product, which provides an element of convenience and is likely to enhance compliance and reduce costs compared with the use of 2 separate products. The efficacy and safety of C/Bd-TS has been well established in several studies,16-23,37 including a 52-week trial in patients with scalp psoriasis.36 The combination of calcipotriene and Bd appears to favorably address the pathophysiologic pathways involved in psoriasis.29,30 Calcipotriene 0.005%–Bd 0.064% topical suspension is a rational option for the treatment of PP in patients with localized disease or in patients treated systemically or with phototherapy for more extensive disease who exhibit persistence or recurrence of scattered areas of PP.6-9,14,15 Appropriate use of C/Bd-TS is likely to achieve favorable efficacy with a low risk of tolerability reactions and a very low risk of major adverse drug reactions.16-23,36-38
Psoriasis is a common inflammatory skin disorder that appears to be induced by multifactorial pathophysiologic processes associated with immunologic dysregulation.1 It can affect patients of any age, gender, and ethnicity, and it presents clinically with a variety of visible manifestations. The disease course and severity of psoriasis varies among affected patients.1 Chronic plaque psoriasis (PP), also referred to as psoriasis vulgaris, is the most common clinical presentation.1,2 Although many patients are affected by psoriasis that is widespread and in some cases severe, the majority of affected patients exhibit localized involvement that usually affects less than 2% to 5% of the body surface area. Although the skin at any anatomic location can be affected, commonly involved sites are described by the mnemonic term SNAKES (scalp, nails, anogenital region, knees, elbows, sacral region).2,3
Because the majority of patients with PP present with localized disease, topical therapy is the foundation of treatment in most cases. Topical corticosteroids (TCs) are the most commonly utilized agents, supported by a long track record of favorable efficacy and safety over approximately 6 decades.4,5 However, optimal management of PP with TCs requires use of a formulation that is of adequate potency, is adaptable for application to the affected body sites, and is properly monitored and adjusted to avoid potential TC-induced adverse effects.4-6 Nonsteroidal topical therapies such as vitamin D analogues (eg, calcipotriene) and retinoids (eg, tazarotene) are commonly integrated into topical regimens to reduce the application frequency and duration of TC use as well as to sustain efficacy.5,7,8 Plaque psoriasis is characteristically a chronic disease associated with periods of persistence and episodes of flaring; therefore, intermittent use of TC therapy along with concurrent or sequential use of a nonsteroidal topical agent are commonly employed to achieve and sustain control of the disorder.7-9
In the last decade, several advances have revolutionized the management of psoriasis, especially for PP patients with extensive involvement who require systemic therapy and/or phototherapy as well as for those with psoriatic arthritis.10,11 The availability of biologic agents such as tumor necrosis factor a inhibitors and certain interleukin inhibitors (eg, IL-12/IL-23) have been at the forefront of major advances in PP treatment, with some agents also blocking the progression of joint destruction associated with psoriatic arthritis.10-12 However, even when patients with PP respond favorably to biologic therapy, it is not uncommon for them to still be affected by some persistent PP. In these cases, although much of the chronic PP may clear with use of the biologic agent, persistence of psoriatic plaques may involve the lower extremities, scalp, and/or trunk, with topical therapy often added to augment the therapeutic response.13-15
This article provides a review of a patented topical suspension combination formulation that contains calcipotriene hydrate 0.005%, a vitamin D analogue, and betamethasone dipropio-nate (Bd) 0.064%, a high-potency TC. In 2008, the US Food and Drug Administration approved the once-daily application of calcipotriene 0.005%–Bd 0.064% topical suspension (C/Bd-TS) for the treatment of PP; this formulation is approved for use on the scalp and body in patients 18 years of age and older. According to the product insert, the recommended maximum duration of treatment with C/Bd-TS once daily is 8 weeks, and patients may not exceed a maximum weekly dose of 100 g.16 It is important to note that the terms calcipotriene and calcipotriol refer to the same molecule and are used interchangeably in the literature. Formulation characteristics of C/Bd-TS, perspectives on modes of action, outcomes from pivotal trials, and efficacy and safety data reported from additional studies are discussed in this article.
What are the formulation characteristics of C/Bd-TS?
Each gram of C/Bd-TS contains 52.18 mg of calcipotriene hydrate (equivalent to 50 µg of calcipotriene) and 0.643 µg of Bd (equivalent to 0.5 mg of betamethasone), formulated together in a viscous, nearly odorless, almost clear to slightly off-white suspension. The excipients are hydrogenated castor oil, polypropylene glycol 11 stearyl ether, α-tocopherol, butylhydroxytoluene, and mineral oil, collectively producing a gel base in which both active ingredients are suspended.16 Although the viscous quality of the suspension warrants some additional effort for removal during hair washing, the tenacious gel-like viscosity assists in removing scale on psoriatic plaques, which is often adherent, especially on the scalp. Additionally, it is important that C/Bd-TS be shaken well before use.16 Initially, C/Bd-TS was studied and marketed in the United States for treatment of scalp psoriasis; however, the indication was expanded to include treatment of PP on the rest of the body, supported by evidence from randomized controlled trials (RCTs).16-23
Vitamin D analogues (eg, calcipotriene/calcitriol) have been shown to be photolabile when exposed to UV light, especially UVA. They also have been shown to be chemically incompatible and less stable when admixed with a variety of other active ingredients and/or vehicles used to treat PP, including hydrocortisone valerate ointment 0.2%, ammonium lactate lotion 12%, and salicylic acid compound ointment 6%.24-26 As a result, it is important for clinicians to consider avoidance of concomitant topical calcipotriene application with use of a TC unless the stability of the active ingredients has been tested when the formulations are combined. Calcipotriene 0.005%/Bd 0.064% topical suspension utilizes vehicle technology that maintains the stability and activity of both calcipotriene and Bd within the suspension formulation.16,26
What is the rationale behind combining calcipotriene and Bd in a single formulation for the treatment of PP?
The potential advantages of C/Bd-TS include the combined modes of action of 2 different active ingredients used for treatment of PP, complementary immunomodulatory effects as compared to use of a TC or vitamin D analogue alone, ease of use with a single product applied once daily, adaptability of the vehicle for use on scalp and/or body skin, and improvement in quality-of-life (QOL) measures.27-34
Combined Modes of Action
Calcipotriene 0.005%–Bd 0.064% topical suspension combines the modes of action of a high-potency topical suspension and a vitamin D analogue for the treatment of PP in a single stable gel formulation that is approved in the United States for treatment of PP in adults.16 The multiple anti-inflammatory properties of corticosteroids as well as the efficacy and safety of TC therapy for psoriasis have been well described.4,6,7,9,27 The antiproliferative and anti-inflammatory properties of vitamin D analogues that appear to correlate with therapeutic effects in the treatment of PP also have been discussed in the literature.28
Complementary Immunomodulatory Effects
More recent studies using various research assays have provided further evidence supporting relevant immunomodulatory properties of calcipotriene alone and in combination with Bd that favorably modify immune dysregulation pathways described more recently in the pathogenesis of PP.1,29,30 Treatment of psoriatic plaques with calcipotriene has been shown to suppress the increased production of peptide alarmins (psoriasin and koebnerisin) in psoriatic skin and their TH17-mediated regulation in epidermal ke-ratinocytes, thus interfering with the S100 amplification loop that appears to produce inflammation in psoriasis.29 In T-lymphocyte cultures evaluating exposure to calcipotriene and Bd both alone and as a combined therapy, calcipotriene inhibited IFN-g, IL-8, IL-17, and IL-22 expression, and it reversed the corticosteroid-induced suppression of IL-4, IL-5, IL-10, and IL-13; Bd inhibited both IL-6 and tumor necrosis factor α expression. The outcomes demonstrated that the combination of calcipotriene and Bd inhibited the endogenous release of TH1- and TH17-associated cytokines that are associated with psoriatic inflammation and together induced a more favorable anti-inflammatory cytokine profile.30 Although the broad range of anti-inflammatory effects provided by a TC of adequate potency, such as Bd, can clear or markedly improve PP, the concurrent use of calcipotriene was shown to provide additional immunomodulatory effects that suppressed the key TH17/TH1 pathophysiologic mediators of psoriatic inflammation and simultaneously induced a TH2/T regulatory response that is believed to provide therapeutic benefit.29,30
Ease of Use and Vehicle Adaptability
A once-daily regimen and a vehicle formulation adaptable for use on both the scalp and body are advantageous in enhancing the potential for greater patient adherence.31,32 The adaptability of the C/Bd-TS for use on the scalp and/or body is supported by several studies encompassing a large number of actively treated subjects. Calcipotriene 0.005%–Bd 0.064% topical suspension has been extensively studied in patients with PP on the scalp and/or body as evidenced by a pooled analysis of 9 eight-week RCTs (scalp, n=6; body, n=3) that encompassed 2777 total subjects treated once daily for PP (scalp, n=1953; body, n=824).23 Additionally, C/Bd-TS applied once daily was evaluated in an open-label, single-arm, 8-week, phase 2 study of adolescents (N=78; age range, 12–17 years [mean age, 14.6 years]) with scalp psoriasis (mean affected scalp area, 43.7%). The investigator global assessment of treatment success (clear or almost clear) and the patient global assessment of treatment success (clear or very mild) were essentially identical among participants and investigators with 85% and 87% reported after 8 weeks, respectively; approximately 50% of participants achieved treatment success after 2 weeks based on both the investigator global assessment and patient global assessment.33
Improvement in QOL Measures
Quality-of-life measures were compared in an 8-week RCT of participants with at least moderate scalp psoriasis treated with C/Bd-TS once daily (n=207) or calcipotriene solution twice daily (n=107). Significantly greater improvement in QOL scores compared to baseline were noted at all time points using the Skindex-16 questionnaire in participants treated with C/Bd-TS compared to calcipotriene solution (total score, P<.001 at weeks 2 and 4 and P=.008 at week 8; symptoms score, P<.001 at weeks 2 and 4 and P=.004 at week 8; emotions score, P<.001 at weeks 2 and 4 and P=.005 at week 8).34 A 4-week, open-label, noninterventional cohort, postmarketing (“real life”) study of 721 patients treated at 333 dermatology centers with C/Bd-TS showed a 69.5% improvement in the scalp life quality index score compared to baseline (P<.0001), with 89.5% and 90.4% of participants reporting that C/Bd-TS was better/much better than previously used therapies for scalp psoriasis and easy/very easy to use, respectively.35 An 8-week RCT trial evaluated C/Bd-TS once daily compared to calcipotriene alone, betamethasone dipropionate alone, and vehicle in 1152 participants with mild to moderate PP involving the trunk and extremities. Participants treated with C/Bd-TS (n=442) demonstrated superior reductions in QOL scores using the dermatology life quality index at weeks 4 and 8 compared to those treated with Bd alone (n=418) or vehicle (n=77) but not compared to calcipotriene alone (n=80).19
What data are available on the efficacy and safety of C/Bd-TS?
Several clinical studies have evaluated the efficacy, tolerability, and safety of C/Bd-TS applied once daily for PP of the scalp and body (ie, trunk, extremities). Most studies were completed over a duration of 8 weeks in adults16-23; however, studies also have been performed in adolescents,33 in adults treated for up to 52 weeks,36 and in a subgroup of Hispanic/Latino and black/African American patients with scalp psoriasis.37 The Table provides a detailed summary of primary efficacy data along with important tolerability and safety considerations based on study outcomes.
What practical recommendations can be made regarding the use of C/Bd-TS for PP?
Calcipotriene 0.005%–Bd 0.064% topical suspension applied once daily provides a formulation that allows for treatment of PP involving both the scalp and body using a single product, which provides an element of convenience and is likely to enhance compliance and reduce costs compared with the use of 2 separate products. The efficacy and safety of C/Bd-TS has been well established in several studies,16-23,37 including a 52-week trial in patients with scalp psoriasis.36 The combination of calcipotriene and Bd appears to favorably address the pathophysiologic pathways involved in psoriasis.29,30 Calcipotriene 0.005%–Bd 0.064% topical suspension is a rational option for the treatment of PP in patients with localized disease or in patients treated systemically or with phototherapy for more extensive disease who exhibit persistence or recurrence of scattered areas of PP.6-9,14,15 Appropriate use of C/Bd-TS is likely to achieve favorable efficacy with a low risk of tolerability reactions and a very low risk of major adverse drug reactions.16-23,36-38
1. Guttman-Yassky E, Krueger JG. Psoriasis: evolution of pathogenic concepts and new therapies through phases of translational research. Br J Dermatol. 2007;157:1103-1115.
2. Menter MA. An overview of psoriasis. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:1-21.
3. Sandoval LF, Feldman SR. General approach to psoriasis treatment. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:3-8.
4. Zeichner JA, Lebwohl MG, Menter A, et al. Optimizing topical therapies for treating psoriasis: a consensus conference. Cutis. 2010;(3 suppl):5-31.
5. American Academy of Dermatology Work Group, Menter A, Korman NJ, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 6. guidelines of care for the treatment of psoriasis and psoriatic arthritis: case-based presentations and evidence-based conclusions [published online ahead of print February 8, 2011]. J Am Acad Dermatol. 2011;65:137-174.
6. Del Rosso J, Friedlander SF. Corticosteroids: options in the era of steroid-sparing therapy. J Am Acad Dermatol. 2005;53(1, suppl 1):S50-S58.
7. Menter A, Korman NJ, Elmets CA, et al; American Academy of Dermatology. Guidelines of care for the management of psoriasis and psoriatic arthritis. section 3. guidelines of care for the management and treatment of psoriasis with topical therapies [published online ahead of print February 13, 2009]. J Am Acad Dermatol. 2009;60:643-659.
8. Koo J. New developments in topical sequential therapy for psoriasis. Skin Therapy Lett. 2005;10:1-4.
9. Mason AR, Mason J, Cork M, et al. Topical treatments for chronic plaque psoriasis. Cochrane Database Syst Rev. 2009;2:CD005028.
10. Belge K, Brück J, Ghoreschi K. Advances in treating psoriasis. F1000Prime Rep. 2014;6:4.
11. Mease PJ, Armstrong AW. Managing patients with psoriatic disease: the diagnosis and pharmacologic treatment of psoriatic arthritis in patients with psoriasis. Drugs. 2014;74:423-441.
12. Boehncke WH, Qureshi A, Merola JF, et al. Diagnosing and treating psoriatic arthritis: an update. Br J Dermatol. 2014;170:772-786.
13. Feldman SR. Effectiveness of clobetasol propionate spray 0.05% added to other stable treatments: add-on therapy in the COBRA trial. Cutis. 2007;80(suppl 5):20-28.
14. Feldman SR, Gelfand JM, Stein Gold L, et al. The role of topical therapy for patients with extensive psoriasis. Cutis. 2007;79(suppl 1[ii]):18-31.
15. Kircik L. Topical calcipotriene 0.005% and betamethasone dipropionate 0.064% maintains efficacy of etanercept after step-down dose in patients with moderate-to-severe plaque psoriasis: results of an open label trial. J Drugs Dermatol. 2011;10:878-882.
16. Taclonex [product insert]. Parsippany, NJ: LEO Pharma Inc; 2014.
17. Buckley C, Hoffmann V, Shapiro J, et al. Calcipotriol plus betamethasone dipropionate scalp formulation is effective and well tolerated in the treatment of scalp psoriasis: a phase II study. Dermatology. 2008;217:107-113.
18. Fleming C, Ganslandt C, Guenther L, et al. Calcipotriol plus betamethasone dipropionate gel compared with its active components in the same vehicle and the vehicle alone in the treatment of psoriasis vulgaris: a randomized, parallel group, double-blind, exploratory study. Eur J Dermatol. 2010;20:465-471.
19. Menter A, Stein Gold L, Bukhalo M, et al. Calcipotriene plus betamethasone dipropionate topical suspension for the treatment of mild to moderate psoriasis vulgaris on the body: a randomized, double-blind, vehicle-controlled trial. J Drugs Dermatol. 2013;12:92-98.
20. Jemec GBE, Ganslandt C, Ortonne JP, et al. A new scalp formulation of calcipotriene plus betamethasone compared with its active ingredients and the vehicle in the treatment of scalp psoriasis: a randomized, double-blind, controlled trial. J Am Acad Dermatol. 2008;59:455-463.
21. van de Kerkhof PC, Hoffmann V, Anstey A, et al. A new scalp formulation of calcipotriol plus betamethasone dipropionate compared with each of its active ingredients in the same vehicle for the treatment of scalp psoriasis: a randomized, double-blind, controlled trial. Br J Dermatol. 2009;160:170-176.
22. Langley RG, Gupta A, Papp K, et al. Calcipotriol plus betamethasone dipropionate gel compared with tacalcitol ointment and the gel vehicle alone in patients with psoriasis vulgaris: a randomized, controlled clinical trial. Dermatology. 2011;222:148-156.
23. Kragballe K, van de Kerkhof P. Pooled safety analysis of calcipotriol plus betamethasone dipropionate gel for the treatment of psoriasis on the body and scalp. J Eur Acad Dermatol Venereol. 2014;28:10-21.
24. Lebwohl MG, Corvari L. Compatibility of topical therapies for psoriasis: challenges and innovations. Cutis. 2007;79(suppl 1[ii]):5-10.
25. Patel B, Siskin S, Krazmien R, et al. Compatibility of calcipotriene with other topical medications. J Am Acad Dermatol. 1998;38(6, pt 1):1010-1011.
26. Traulsen J. Bioavailability of betamethasone dipropionate when combined with calcipotriol. Int J Dermatol. 2004;43:611-617.
27. Sandoval LF, Feldman SR. Topical corticosteroids. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:21-36.
28. deShazo R, Krueger GG, Duffin KC. Topical agents. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:41-65.
29. Hegyi Z, Zwicker S, Bureik D, et al. Vitamin D analog calcipotriol suppresses the Th17 cytokine-induced proinflammatory S100 “alarmins” psoriasin (S100A7) and koebnerisin (S100A15) in psoriasis. J Invest Dermatol. 2012;132:1416-1424.
30. Lovato P, Norsgaard H, Ropke M. Key immunomodulatory effects exerted by calcipotriol in combination with corticosteroid on human cells. Poster presented at: 21st European Academy of Dermatology and Venereology Congress; September 27-30, 2012; Prague, Czech Republic.
31. Renton C. Diagnosis and treatment of adults with scalp psoriasis. Nurs Stand. 2014;28:35-39.
32. Feldman SR, Housman TS. Patients’ vehicle preference for corticosteroid treatments of scalp psoriasis. Am J Clin Dermatol. 2003;4:221-224.
33. Gooderham M, Debarre JM, Keddy-Grant J, et al. Safety and efficacy of calcipotriene plus betamethasone dipropionate topical suspension in adolescents with scalp psoriasis: an open, non-controlled, 8-week trial. Poster presented at: American Academy of Dermatology 72nd Annual Meeting; March 21-25, 2014; Denver, CO.
34. Ortonne JP, Tan J, Nordin P, et al. Quality of life of patients with scalp psoriasis treated with calcipotriene plus betamethasone dipropionate gel compared to calcipotriene solution. J Am Academy Dermatol. 2008;58(2, suppl 2):AB134.
35. Mrowietz U, Macheleidt O, Eicke C. Effective treatment and improvement of quality of life in patients with scalp psoriasis by topical use of calcipotriol/betamethasone (Xamiol®-gel): results [in German]. J Dtsch Dermatol Ges. 2011;9:825-831.
36. Luger TA, Cambazard F, Larsen FG, et al. A study of the safety and efficacy of calcipotriol and betamethasone dipropionate scalp formulation in the long-term management of scalp psoriasis. Dermatology. 2008;217:321-328.
37. Tyring S, Mendoza N, Appell M, et al. A calcipotriene/betamethasone dipropionate two-compound scalp formulation in the treatment of scalp psoriasis in Hispanic/Latino and Black/African American patients: results of the randomized, 8-week, double-blind phase of a clinical trial. Int J Dermatol. 2010;49:1328-1333.
38. Silver S, Tuppal R, Gupta AK, et al. Effect of calcipotriene plus betamethasone dipropionate topical suspension on the hypothalamic-pituitary-adrenal axis and calcium homeostasis in subjects with extensive psoriasis vulgaris: an open, non-controlled, 8-week trial. J Drugs Dermatol. 2013;12:882-888.
1. Guttman-Yassky E, Krueger JG. Psoriasis: evolution of pathogenic concepts and new therapies through phases of translational research. Br J Dermatol. 2007;157:1103-1115.
2. Menter MA. An overview of psoriasis. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:1-21.
3. Sandoval LF, Feldman SR. General approach to psoriasis treatment. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:3-8.
4. Zeichner JA, Lebwohl MG, Menter A, et al. Optimizing topical therapies for treating psoriasis: a consensus conference. Cutis. 2010;(3 suppl):5-31.
5. American Academy of Dermatology Work Group, Menter A, Korman NJ, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 6. guidelines of care for the treatment of psoriasis and psoriatic arthritis: case-based presentations and evidence-based conclusions [published online ahead of print February 8, 2011]. J Am Acad Dermatol. 2011;65:137-174.
6. Del Rosso J, Friedlander SF. Corticosteroids: options in the era of steroid-sparing therapy. J Am Acad Dermatol. 2005;53(1, suppl 1):S50-S58.
7. Menter A, Korman NJ, Elmets CA, et al; American Academy of Dermatology. Guidelines of care for the management of psoriasis and psoriatic arthritis. section 3. guidelines of care for the management and treatment of psoriasis with topical therapies [published online ahead of print February 13, 2009]. J Am Acad Dermatol. 2009;60:643-659.
8. Koo J. New developments in topical sequential therapy for psoriasis. Skin Therapy Lett. 2005;10:1-4.
9. Mason AR, Mason J, Cork M, et al. Topical treatments for chronic plaque psoriasis. Cochrane Database Syst Rev. 2009;2:CD005028.
10. Belge K, Brück J, Ghoreschi K. Advances in treating psoriasis. F1000Prime Rep. 2014;6:4.
11. Mease PJ, Armstrong AW. Managing patients with psoriatic disease: the diagnosis and pharmacologic treatment of psoriatic arthritis in patients with psoriasis. Drugs. 2014;74:423-441.
12. Boehncke WH, Qureshi A, Merola JF, et al. Diagnosing and treating psoriatic arthritis: an update. Br J Dermatol. 2014;170:772-786.
13. Feldman SR. Effectiveness of clobetasol propionate spray 0.05% added to other stable treatments: add-on therapy in the COBRA trial. Cutis. 2007;80(suppl 5):20-28.
14. Feldman SR, Gelfand JM, Stein Gold L, et al. The role of topical therapy for patients with extensive psoriasis. Cutis. 2007;79(suppl 1[ii]):18-31.
15. Kircik L. Topical calcipotriene 0.005% and betamethasone dipropionate 0.064% maintains efficacy of etanercept after step-down dose in patients with moderate-to-severe plaque psoriasis: results of an open label trial. J Drugs Dermatol. 2011;10:878-882.
16. Taclonex [product insert]. Parsippany, NJ: LEO Pharma Inc; 2014.
17. Buckley C, Hoffmann V, Shapiro J, et al. Calcipotriol plus betamethasone dipropionate scalp formulation is effective and well tolerated in the treatment of scalp psoriasis: a phase II study. Dermatology. 2008;217:107-113.
18. Fleming C, Ganslandt C, Guenther L, et al. Calcipotriol plus betamethasone dipropionate gel compared with its active components in the same vehicle and the vehicle alone in the treatment of psoriasis vulgaris: a randomized, parallel group, double-blind, exploratory study. Eur J Dermatol. 2010;20:465-471.
19. Menter A, Stein Gold L, Bukhalo M, et al. Calcipotriene plus betamethasone dipropionate topical suspension for the treatment of mild to moderate psoriasis vulgaris on the body: a randomized, double-blind, vehicle-controlled trial. J Drugs Dermatol. 2013;12:92-98.
20. Jemec GBE, Ganslandt C, Ortonne JP, et al. A new scalp formulation of calcipotriene plus betamethasone compared with its active ingredients and the vehicle in the treatment of scalp psoriasis: a randomized, double-blind, controlled trial. J Am Acad Dermatol. 2008;59:455-463.
21. van de Kerkhof PC, Hoffmann V, Anstey A, et al. A new scalp formulation of calcipotriol plus betamethasone dipropionate compared with each of its active ingredients in the same vehicle for the treatment of scalp psoriasis: a randomized, double-blind, controlled trial. Br J Dermatol. 2009;160:170-176.
22. Langley RG, Gupta A, Papp K, et al. Calcipotriol plus betamethasone dipropionate gel compared with tacalcitol ointment and the gel vehicle alone in patients with psoriasis vulgaris: a randomized, controlled clinical trial. Dermatology. 2011;222:148-156.
23. Kragballe K, van de Kerkhof P. Pooled safety analysis of calcipotriol plus betamethasone dipropionate gel for the treatment of psoriasis on the body and scalp. J Eur Acad Dermatol Venereol. 2014;28:10-21.
24. Lebwohl MG, Corvari L. Compatibility of topical therapies for psoriasis: challenges and innovations. Cutis. 2007;79(suppl 1[ii]):5-10.
25. Patel B, Siskin S, Krazmien R, et al. Compatibility of calcipotriene with other topical medications. J Am Acad Dermatol. 1998;38(6, pt 1):1010-1011.
26. Traulsen J. Bioavailability of betamethasone dipropionate when combined with calcipotriol. Int J Dermatol. 2004;43:611-617.
27. Sandoval LF, Feldman SR. Topical corticosteroids. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:21-36.
28. deShazo R, Krueger GG, Duffin KC. Topical agents. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:41-65.
29. Hegyi Z, Zwicker S, Bureik D, et al. Vitamin D analog calcipotriol suppresses the Th17 cytokine-induced proinflammatory S100 “alarmins” psoriasin (S100A7) and koebnerisin (S100A15) in psoriasis. J Invest Dermatol. 2012;132:1416-1424.
30. Lovato P, Norsgaard H, Ropke M. Key immunomodulatory effects exerted by calcipotriol in combination with corticosteroid on human cells. Poster presented at: 21st European Academy of Dermatology and Venereology Congress; September 27-30, 2012; Prague, Czech Republic.
31. Renton C. Diagnosis and treatment of adults with scalp psoriasis. Nurs Stand. 2014;28:35-39.
32. Feldman SR, Housman TS. Patients’ vehicle preference for corticosteroid treatments of scalp psoriasis. Am J Clin Dermatol. 2003;4:221-224.
33. Gooderham M, Debarre JM, Keddy-Grant J, et al. Safety and efficacy of calcipotriene plus betamethasone dipropionate topical suspension in adolescents with scalp psoriasis: an open, non-controlled, 8-week trial. Poster presented at: American Academy of Dermatology 72nd Annual Meeting; March 21-25, 2014; Denver, CO.
34. Ortonne JP, Tan J, Nordin P, et al. Quality of life of patients with scalp psoriasis treated with calcipotriene plus betamethasone dipropionate gel compared to calcipotriene solution. J Am Academy Dermatol. 2008;58(2, suppl 2):AB134.
35. Mrowietz U, Macheleidt O, Eicke C. Effective treatment and improvement of quality of life in patients with scalp psoriasis by topical use of calcipotriol/betamethasone (Xamiol®-gel): results [in German]. J Dtsch Dermatol Ges. 2011;9:825-831.
36. Luger TA, Cambazard F, Larsen FG, et al. A study of the safety and efficacy of calcipotriol and betamethasone dipropionate scalp formulation in the long-term management of scalp psoriasis. Dermatology. 2008;217:321-328.
37. Tyring S, Mendoza N, Appell M, et al. A calcipotriene/betamethasone dipropionate two-compound scalp formulation in the treatment of scalp psoriasis in Hispanic/Latino and Black/African American patients: results of the randomized, 8-week, double-blind phase of a clinical trial. Int J Dermatol. 2010;49:1328-1333.
38. Silver S, Tuppal R, Gupta AK, et al. Effect of calcipotriene plus betamethasone dipropionate topical suspension on the hypothalamic-pituitary-adrenal axis and calcium homeostasis in subjects with extensive psoriasis vulgaris: an open, non-controlled, 8-week trial. J Drugs Dermatol. 2013;12:882-888.
Practice Points
- Calcipotriene 0.005%–betamethasone dipropionate 0.064% topical suspension (C/Bd-TS) applied once daily has been shown in multiple studies to be effective, well tolerated, and safe for the treatment of plaque psoriasis (PP) involving the scalp and/or other body sites such as the trunk and extremities. Studies have included all severities of PP, with both investigator and subject assessments shown to be favorable overall.
- Most studies were completed in adults over a duration of 8 weeks; however, clinical trials also have been performed with C/Bd-TS in adults treated for up to 52 weeks for scalp psoriasis, in a subgroup of Hispanic/Latino and black/African American adult patients with scalp psoriasis, and in adolescents with scalp psoriasis.
- Studies evaluating application of C/Bd-TS once daily for PP affecting nonscalp sites have primarily involved use on the trunk and extremities.
- The adaptability for scalp and body application allows for use in many cases of a single topical product without needing to prescribe a second leave-on medication specifically for use on the scalp.
Consensus Recommendations From the American Acne & Rosacea Society on the Management of Rosacea, Part 5: A Guide on the Management of Rosacea
Consensus Recommendations From the American Acne & Rosacea Society on the Management of Rosacea, Part 4: A Status Report on Physical Modalities and Devices
Consensus Recommendations From the American Acne & Rosacea Society on the Management of Rosacea, Part 3: A Status Report on Systemic Therapies
Consensus Recommendations From the American Acne & Rosacea Society on the Management of Rosacea, Part 2: A Status Report on Topical Agents
Consensus Recommendations From the American Acne & Rosacea Society on the Management of Rosacea, Part 1: A Status Report on the Disease State, General Measures, and Adjunctive Skin Care
Test your knowledge on consensus recommendations for rosacea with MD-IQ: the medical intelligence quiz. Click here to answer 5 questions.