User login
Jeff Evans has been editor of Rheumatology News/MDedge Rheumatology and the EULAR Congress News since 2013. He started at Frontline Medical Communications in 2001 and was a reporter for 8 years before serving as editor of Clinical Neurology News and World Neurology, and briefly as editor of GI & Hepatology News. He graduated cum laude from Cornell University (New York) with a BA in biological sciences, concentrating in neurobiology and behavior.
Fludarabine added to interferon hints at benefits for breakthrough MS
Relapsing-remitting multiple sclerosis (MS) patients who experienced breakthrough disease despite treatment with interferon beta-1a required less acute corticosteroids during relapses and had better responses on several MRI outcomes with the addition of fludarabine, compared with monthly methylprednisolone, in a small, prospective, randomized, open-label study.
Investigators led by Dr. Steven J. Greenberg of AbbVie, North Chicago, chose to test fludarabine in the proof-of-concept, pilot study because of its immunosuppressive properties and effectiveness in treating disorders involving immune dysregulation, most notably lymphoproliferative disorders and hematologic malignancies.
Fludarabine is a purine nucleoside analog prodrug that upon phosphorylation is toxic to dividing and quiescent lymphocytes and monocytes, according to the researchers, and exerts its effects through DNA synthesis interference and apoptosis. Methylprednisolone was used as an add-on comparator because of its common use in multiple sclerosis.
In addition to weekly intramuscular interferon beta-1a (Avonex), all 18 patients in the study initially received IV methylprednisolone 1 g once daily for 3 consecutive days, and then 1 week later were randomized to receive fludarabine 25 mg/m2 IV once daily for 5 consecutive days per 4-week cycle for 3 consecutive cycles or methylprednisolone 1 g IV 1 day per 4-week cycle for 3 consecutive cycles (Ther Adv Neurol Disord. 2016 Jan 21. doi: 10.1177/1756285615626049).
Treatment-emergent adverse events occurred with similar frequency in each group over 12 months of follow-up, with infection being the most common AE (three with fludarabine and two with methylprednisolone). Grade 3 or grade 2 leukopenia that had not normalized within 28 days after treatment occurred in three fludarabine patients and one methylprednisolone patient, and took significantly longer resolve for those taking fludarabine (3.75 months vs. 0.17 months).
Over 12 months of follow-up, fludarabine-treated patients experienced numerically, but not significantly, fewer mean relapses (0.5 vs. 0.8) and longer median time to relapse (10.5 months vs. 8.5 months). However, fludarabine led to significantly fewer mean cycles of corticosteroids (0.5 vs. 0.8).
Expanded Disability Status Scale scores declined from baseline to 12 months by a mean of –0.2 in the fludarabine group but increased in the methylprednisolone group by 0.5. Both groups achieved slight improvements in MS Functional Composite scores.
Fludarabine-treated patients had significant declines from baseline to 12 months in gadolinium-positive lesion volume (–98.3%) and number (–93.3%), but no significant differences were recorded in either group for changes in FLAIR lesion volume, T1-hypointense lesion volume or number, or brain parenchymal fraction.
Two outlier patients in the fludarabine group who had 21 and 17 gadolinium-positive lesions, respectively, at baseline were examined in separate analyses and results for the fludarabine group were analyzed both with and without them. None of the results appreciably changed when they were included or excluded, except for gadolinium-positive lesion volume and number, which were not significantly changed without the two patients. The two outlier patients had 100% mean reductions in gadolinium-positive lesion number and volume and a 19.4% mean reduction in FLAIR lesion volume.
The investigators cautioned that “the long-term safety of repetitive use has not been established by this study, which is a critical consideration for a chronic disease like MS. We emphasize that our results should be considered preliminary and would await confirmation in a larger-scale trial.”
This study was supported in part by an investigator-initiated study grant provided by Biogen. Berlex Laboratories provided fludarabine. Dr. Greenberg is an employee of AbbVie, and two coauthors reported financial ties to companies marketing MS drugs.
Relapsing-remitting multiple sclerosis (MS) patients who experienced breakthrough disease despite treatment with interferon beta-1a required less acute corticosteroids during relapses and had better responses on several MRI outcomes with the addition of fludarabine, compared with monthly methylprednisolone, in a small, prospective, randomized, open-label study.
Investigators led by Dr. Steven J. Greenberg of AbbVie, North Chicago, chose to test fludarabine in the proof-of-concept, pilot study because of its immunosuppressive properties and effectiveness in treating disorders involving immune dysregulation, most notably lymphoproliferative disorders and hematologic malignancies.
Fludarabine is a purine nucleoside analog prodrug that upon phosphorylation is toxic to dividing and quiescent lymphocytes and monocytes, according to the researchers, and exerts its effects through DNA synthesis interference and apoptosis. Methylprednisolone was used as an add-on comparator because of its common use in multiple sclerosis.
In addition to weekly intramuscular interferon beta-1a (Avonex), all 18 patients in the study initially received IV methylprednisolone 1 g once daily for 3 consecutive days, and then 1 week later were randomized to receive fludarabine 25 mg/m2 IV once daily for 5 consecutive days per 4-week cycle for 3 consecutive cycles or methylprednisolone 1 g IV 1 day per 4-week cycle for 3 consecutive cycles (Ther Adv Neurol Disord. 2016 Jan 21. doi: 10.1177/1756285615626049).
Treatment-emergent adverse events occurred with similar frequency in each group over 12 months of follow-up, with infection being the most common AE (three with fludarabine and two with methylprednisolone). Grade 3 or grade 2 leukopenia that had not normalized within 28 days after treatment occurred in three fludarabine patients and one methylprednisolone patient, and took significantly longer resolve for those taking fludarabine (3.75 months vs. 0.17 months).
Over 12 months of follow-up, fludarabine-treated patients experienced numerically, but not significantly, fewer mean relapses (0.5 vs. 0.8) and longer median time to relapse (10.5 months vs. 8.5 months). However, fludarabine led to significantly fewer mean cycles of corticosteroids (0.5 vs. 0.8).
Expanded Disability Status Scale scores declined from baseline to 12 months by a mean of –0.2 in the fludarabine group but increased in the methylprednisolone group by 0.5. Both groups achieved slight improvements in MS Functional Composite scores.
Fludarabine-treated patients had significant declines from baseline to 12 months in gadolinium-positive lesion volume (–98.3%) and number (–93.3%), but no significant differences were recorded in either group for changes in FLAIR lesion volume, T1-hypointense lesion volume or number, or brain parenchymal fraction.
Two outlier patients in the fludarabine group who had 21 and 17 gadolinium-positive lesions, respectively, at baseline were examined in separate analyses and results for the fludarabine group were analyzed both with and without them. None of the results appreciably changed when they were included or excluded, except for gadolinium-positive lesion volume and number, which were not significantly changed without the two patients. The two outlier patients had 100% mean reductions in gadolinium-positive lesion number and volume and a 19.4% mean reduction in FLAIR lesion volume.
The investigators cautioned that “the long-term safety of repetitive use has not been established by this study, which is a critical consideration for a chronic disease like MS. We emphasize that our results should be considered preliminary and would await confirmation in a larger-scale trial.”
This study was supported in part by an investigator-initiated study grant provided by Biogen. Berlex Laboratories provided fludarabine. Dr. Greenberg is an employee of AbbVie, and two coauthors reported financial ties to companies marketing MS drugs.
Relapsing-remitting multiple sclerosis (MS) patients who experienced breakthrough disease despite treatment with interferon beta-1a required less acute corticosteroids during relapses and had better responses on several MRI outcomes with the addition of fludarabine, compared with monthly methylprednisolone, in a small, prospective, randomized, open-label study.
Investigators led by Dr. Steven J. Greenberg of AbbVie, North Chicago, chose to test fludarabine in the proof-of-concept, pilot study because of its immunosuppressive properties and effectiveness in treating disorders involving immune dysregulation, most notably lymphoproliferative disorders and hematologic malignancies.
Fludarabine is a purine nucleoside analog prodrug that upon phosphorylation is toxic to dividing and quiescent lymphocytes and monocytes, according to the researchers, and exerts its effects through DNA synthesis interference and apoptosis. Methylprednisolone was used as an add-on comparator because of its common use in multiple sclerosis.
In addition to weekly intramuscular interferon beta-1a (Avonex), all 18 patients in the study initially received IV methylprednisolone 1 g once daily for 3 consecutive days, and then 1 week later were randomized to receive fludarabine 25 mg/m2 IV once daily for 5 consecutive days per 4-week cycle for 3 consecutive cycles or methylprednisolone 1 g IV 1 day per 4-week cycle for 3 consecutive cycles (Ther Adv Neurol Disord. 2016 Jan 21. doi: 10.1177/1756285615626049).
Treatment-emergent adverse events occurred with similar frequency in each group over 12 months of follow-up, with infection being the most common AE (three with fludarabine and two with methylprednisolone). Grade 3 or grade 2 leukopenia that had not normalized within 28 days after treatment occurred in three fludarabine patients and one methylprednisolone patient, and took significantly longer resolve for those taking fludarabine (3.75 months vs. 0.17 months).
Over 12 months of follow-up, fludarabine-treated patients experienced numerically, but not significantly, fewer mean relapses (0.5 vs. 0.8) and longer median time to relapse (10.5 months vs. 8.5 months). However, fludarabine led to significantly fewer mean cycles of corticosteroids (0.5 vs. 0.8).
Expanded Disability Status Scale scores declined from baseline to 12 months by a mean of –0.2 in the fludarabine group but increased in the methylprednisolone group by 0.5. Both groups achieved slight improvements in MS Functional Composite scores.
Fludarabine-treated patients had significant declines from baseline to 12 months in gadolinium-positive lesion volume (–98.3%) and number (–93.3%), but no significant differences were recorded in either group for changes in FLAIR lesion volume, T1-hypointense lesion volume or number, or brain parenchymal fraction.
Two outlier patients in the fludarabine group who had 21 and 17 gadolinium-positive lesions, respectively, at baseline were examined in separate analyses and results for the fludarabine group were analyzed both with and without them. None of the results appreciably changed when they were included or excluded, except for gadolinium-positive lesion volume and number, which were not significantly changed without the two patients. The two outlier patients had 100% mean reductions in gadolinium-positive lesion number and volume and a 19.4% mean reduction in FLAIR lesion volume.
The investigators cautioned that “the long-term safety of repetitive use has not been established by this study, which is a critical consideration for a chronic disease like MS. We emphasize that our results should be considered preliminary and would await confirmation in a larger-scale trial.”
This study was supported in part by an investigator-initiated study grant provided by Biogen. Berlex Laboratories provided fludarabine. Dr. Greenberg is an employee of AbbVie, and two coauthors reported financial ties to companies marketing MS drugs.
FROM THERAPEUTIC ADVANCES IN NEUROLOGICAL DISORDERS
Key clinical point: Preliminary evidence suggests that fludarabine added to interferon beta-1a for breakthrough disease in relapsing-remitting MS patients may be a safe and well-tolerated adjunct with some hints of ability to reduce disease activity.
Major finding: Fludarabine-treated patients had significant declines from baseline to 12 months in gadolinium-positive lesion volume (–98.3%) and number (–93.3%), but no significant differences were recorded in either group for changes in FLAIR lesion volume, T1-hypointense lesion volume or number, or brain parenchymal fraction.
Data source: A prospective, randomized, open-label study of 18 relapsing-remitting MS patients.
Disclosures: This study was supported in part by an investigator-initiated study grant provided by Biogen. Berlex Laboratories provided fludarabine. Dr. Greenberg is an employee of AbbVie, and two coauthors reported financial ties to companies marketing MS drugs.
MRI findings beyond sacroiliitis not necessary for classifying nonradiographic axial SpA
Current recommendations for identifying sacroiliitis on MRI to classify patients with nonradiographic axial spondyloarthritis should still depend on the presence of subchondral bone marrow edema, but additional evidence of structural lesions can be taken into account to define the presence of inflammatory lesions, according to a consensus review by experts from the Assessment in SpondyloArthritis International Society MRI working group.
The additional information provided by structural lesions, such as erosions, detected via MRI of the sacroiliac (SI) joint or spine is not necessary for the definition, but “may enhance confidence in the classification of axial SpA [spondyloarthritis],” said the panel of 16 rheumatologists, 4 radiologists, and 1 research fellow, who presented their summary and draft proposal at the January 2014 annual assembly of the Assessment in SpondyloArthritis International Society (ASAS), where members unanimously approved it (Ann Rheum Dis. 2016 Jan 14. doi: 10.1136/annrheumdis-2015-208642).
The group’s goal was to examine whether new data published on axial SpA in the 5 years following the 2009 publication of the ASAS recommendations were “sufficient to merit a change in the MRI definition of a positive MRI and clarify any misunderstanding of the existing definition.”
Overall, the working group determined that the addition of “structural damage changes of the SI joints and the addition of features on MRI of the spine for classification purposes is not yet clear and this continues to be an important research agenda.”
Adding any single lesion or combination of lesions to the current classification criteria for nonradiographic axial spondyloarthritis (nr-axSpA) did not increase the sensitivity of the MRI definition without losing specificity in one cohort, whereas there was an unclear benefit to adding SI erosion to the definition in another cohort. The evaluation of these lesions on MRI depended on the use of T1 weighting and fat-suppression techniques, as well as the contextual interpretation of MRI, which currently add too much complexity to the definition of a positive SI joint MRI to be useful in achieving a “consensus for definitions for each MRI structural damage lesion and the setting of thresholds for any defined lesion or combination of lesions,” the working group wrote.
The panelists found that there was no consistent beneficial effect of adding features of SpA on spine MRI to the definition. Spine MRI added incremental sensitivity in other analyses, but also increased false-positive SpA diagnoses.
In a commentary reviewing the controversy and evidence for classifying diseases within the spectrum of axial SpA, Dr. Atul Deodhar of Oregon Health and Science University, Portland, and his colleagues noted that “there is no need to differentiate between a diagnosis of nr-axSpA and that of [ankylosing spondylitis] in clinical practice, since the only purpose for having these two labels is classification.” They said the need for formal distinction between nr-axSpA and ankylosing spondylitis may require some exceptions, such as when it is necessary “to specify an approved indication for TNFi [tumor necrosis factor inhibitor] therapy, when off-label use of biologics must be avoided ... and to clarify the presence of structural changes that are required for patients to receive coverage from their insurance carrier to use a TNFi” (Ann. Rheum Dis. 2016 Jan 14. doi: 10.1136/annrheumdis-2015-208852).
The working panel and commentary authors declared having no competing interests.
Current recommendations for identifying sacroiliitis on MRI to classify patients with nonradiographic axial spondyloarthritis should still depend on the presence of subchondral bone marrow edema, but additional evidence of structural lesions can be taken into account to define the presence of inflammatory lesions, according to a consensus review by experts from the Assessment in SpondyloArthritis International Society MRI working group.
The additional information provided by structural lesions, such as erosions, detected via MRI of the sacroiliac (SI) joint or spine is not necessary for the definition, but “may enhance confidence in the classification of axial SpA [spondyloarthritis],” said the panel of 16 rheumatologists, 4 radiologists, and 1 research fellow, who presented their summary and draft proposal at the January 2014 annual assembly of the Assessment in SpondyloArthritis International Society (ASAS), where members unanimously approved it (Ann Rheum Dis. 2016 Jan 14. doi: 10.1136/annrheumdis-2015-208642).
The group’s goal was to examine whether new data published on axial SpA in the 5 years following the 2009 publication of the ASAS recommendations were “sufficient to merit a change in the MRI definition of a positive MRI and clarify any misunderstanding of the existing definition.”
Overall, the working group determined that the addition of “structural damage changes of the SI joints and the addition of features on MRI of the spine for classification purposes is not yet clear and this continues to be an important research agenda.”
Adding any single lesion or combination of lesions to the current classification criteria for nonradiographic axial spondyloarthritis (nr-axSpA) did not increase the sensitivity of the MRI definition without losing specificity in one cohort, whereas there was an unclear benefit to adding SI erosion to the definition in another cohort. The evaluation of these lesions on MRI depended on the use of T1 weighting and fat-suppression techniques, as well as the contextual interpretation of MRI, which currently add too much complexity to the definition of a positive SI joint MRI to be useful in achieving a “consensus for definitions for each MRI structural damage lesion and the setting of thresholds for any defined lesion or combination of lesions,” the working group wrote.
The panelists found that there was no consistent beneficial effect of adding features of SpA on spine MRI to the definition. Spine MRI added incremental sensitivity in other analyses, but also increased false-positive SpA diagnoses.
In a commentary reviewing the controversy and evidence for classifying diseases within the spectrum of axial SpA, Dr. Atul Deodhar of Oregon Health and Science University, Portland, and his colleagues noted that “there is no need to differentiate between a diagnosis of nr-axSpA and that of [ankylosing spondylitis] in clinical practice, since the only purpose for having these two labels is classification.” They said the need for formal distinction between nr-axSpA and ankylosing spondylitis may require some exceptions, such as when it is necessary “to specify an approved indication for TNFi [tumor necrosis factor inhibitor] therapy, when off-label use of biologics must be avoided ... and to clarify the presence of structural changes that are required for patients to receive coverage from their insurance carrier to use a TNFi” (Ann. Rheum Dis. 2016 Jan 14. doi: 10.1136/annrheumdis-2015-208852).
The working panel and commentary authors declared having no competing interests.
Current recommendations for identifying sacroiliitis on MRI to classify patients with nonradiographic axial spondyloarthritis should still depend on the presence of subchondral bone marrow edema, but additional evidence of structural lesions can be taken into account to define the presence of inflammatory lesions, according to a consensus review by experts from the Assessment in SpondyloArthritis International Society MRI working group.
The additional information provided by structural lesions, such as erosions, detected via MRI of the sacroiliac (SI) joint or spine is not necessary for the definition, but “may enhance confidence in the classification of axial SpA [spondyloarthritis],” said the panel of 16 rheumatologists, 4 radiologists, and 1 research fellow, who presented their summary and draft proposal at the January 2014 annual assembly of the Assessment in SpondyloArthritis International Society (ASAS), where members unanimously approved it (Ann Rheum Dis. 2016 Jan 14. doi: 10.1136/annrheumdis-2015-208642).
The group’s goal was to examine whether new data published on axial SpA in the 5 years following the 2009 publication of the ASAS recommendations were “sufficient to merit a change in the MRI definition of a positive MRI and clarify any misunderstanding of the existing definition.”
Overall, the working group determined that the addition of “structural damage changes of the SI joints and the addition of features on MRI of the spine for classification purposes is not yet clear and this continues to be an important research agenda.”
Adding any single lesion or combination of lesions to the current classification criteria for nonradiographic axial spondyloarthritis (nr-axSpA) did not increase the sensitivity of the MRI definition without losing specificity in one cohort, whereas there was an unclear benefit to adding SI erosion to the definition in another cohort. The evaluation of these lesions on MRI depended on the use of T1 weighting and fat-suppression techniques, as well as the contextual interpretation of MRI, which currently add too much complexity to the definition of a positive SI joint MRI to be useful in achieving a “consensus for definitions for each MRI structural damage lesion and the setting of thresholds for any defined lesion or combination of lesions,” the working group wrote.
The panelists found that there was no consistent beneficial effect of adding features of SpA on spine MRI to the definition. Spine MRI added incremental sensitivity in other analyses, but also increased false-positive SpA diagnoses.
In a commentary reviewing the controversy and evidence for classifying diseases within the spectrum of axial SpA, Dr. Atul Deodhar of Oregon Health and Science University, Portland, and his colleagues noted that “there is no need to differentiate between a diagnosis of nr-axSpA and that of [ankylosing spondylitis] in clinical practice, since the only purpose for having these two labels is classification.” They said the need for formal distinction between nr-axSpA and ankylosing spondylitis may require some exceptions, such as when it is necessary “to specify an approved indication for TNFi [tumor necrosis factor inhibitor] therapy, when off-label use of biologics must be avoided ... and to clarify the presence of structural changes that are required for patients to receive coverage from their insurance carrier to use a TNFi” (Ann. Rheum Dis. 2016 Jan 14. doi: 10.1136/annrheumdis-2015-208852).
The working panel and commentary authors declared having no competing interests.
FROM ANNALS OF THE RHEUMATIC DISEASES
Glatiramer acetate didn’t affect birth outcomes in women with multiple sclerosis
Glatiramer acetate exposure during the first trimester of pregnancy appears safe and was not associated with a teratogenic effect in a nationwide German Multiple Sclerosis and Pregnancy registry.
In the second largest study of the safety of glatiramer acetate exposure during early pregnancy in multiple sclerosis patients, Sandra Herbstritt, Pharm.D., and her colleagues at Ruhr University Bochum (Germany) reported that exposure to the drug in 151 women with multiple sclerosis was not associated with significant differences in pregnancy or birth outcomes when compared with 95 controls without exposure to disease-modifying therapy (DMT) during pregnancy. All but three of the patients who took glatiramer acetate stopped it in the first trimester (median duration of 31 days; range, 0-154 days). Pregnancies were considered exposed to glatiramer acetate if the last injection was administered after the last menstrual period (Mult Scler. 2016 Jan 11. doi: 10.1177/1352458515623366).
Significantly more relapses occurred in women who did not take a DMT during pregnancy than in women who took glatiramer acetate (28 vs. 18, respectively), particularly in the first and third trimesters. A total of 224 live births occurred, including 136 with exposure to glatiramer acetate and 88 without DMT exposure. All but 3 of the 22 pregnancies that did not result in live births were spontaneous abortions in the first trimester.
The only early neonatal death among women who took glatiramer acetate involved an infant who died 30 minutes after birth in gestational week 24 because of a maternal infection. According to the investigators, “the mother received glatiramer acetate for 8 months prior to pregnancy, stopped treatment in the second [gestational week], and was not exposed to other substances during pregnancy.”
A total of nine congenital abnormalities (eight major, one minor) were observed without any specific pattern and included three in glatiramer acetate–exposed neonates and six in unexposed neonates.
No safety signals were reported for glatiramer acetate on the outcome of pregnancy, labor, or delivery in a previous meta-analysis of 97 pregnancies in eight studies. Glatiramer acetate’s manufacturer, Teva, reported no adverse outcomes in a conference abstract of 245 pregnancies exposed to glatiramer acetate, but the company has not published its postmarketing surveillance data in manuscript form, the authors wrote.
“Our results of a lacking adverse effect of glatiramer acetate during early pregnancy exposure are biologically plausible as it is very unlikely that glatiramer acetate passes the placental barrier,” the investigators wrote, because it is not permeable for a large heterogeneous mixture of polypeptides such as glatiramer acetate, which have molecular weights of 5,000-9,000 d.
The German Multiple Sclerosis and Pregnancy registry was partly supported by Bayer Healthcare, Biogen Idec Germany, Merck Serono, Novartis Pharma, Teva Pharma, and Sanofi-Aventis Genzyme Pharmaceuticals, but the sponsors had no role in the registry design, data collection, analyses, or dissemination of results. Two authors reported financial ties to numerous pharmaceutical companies that market MS drugs, and two reported support from the German Research Council. Another author is the site principal investigator for two industry-sponsored randomized clinical trials.
Glatiramer acetate exposure during the first trimester of pregnancy appears safe and was not associated with a teratogenic effect in a nationwide German Multiple Sclerosis and Pregnancy registry.
In the second largest study of the safety of glatiramer acetate exposure during early pregnancy in multiple sclerosis patients, Sandra Herbstritt, Pharm.D., and her colleagues at Ruhr University Bochum (Germany) reported that exposure to the drug in 151 women with multiple sclerosis was not associated with significant differences in pregnancy or birth outcomes when compared with 95 controls without exposure to disease-modifying therapy (DMT) during pregnancy. All but three of the patients who took glatiramer acetate stopped it in the first trimester (median duration of 31 days; range, 0-154 days). Pregnancies were considered exposed to glatiramer acetate if the last injection was administered after the last menstrual period (Mult Scler. 2016 Jan 11. doi: 10.1177/1352458515623366).
Significantly more relapses occurred in women who did not take a DMT during pregnancy than in women who took glatiramer acetate (28 vs. 18, respectively), particularly in the first and third trimesters. A total of 224 live births occurred, including 136 with exposure to glatiramer acetate and 88 without DMT exposure. All but 3 of the 22 pregnancies that did not result in live births were spontaneous abortions in the first trimester.
The only early neonatal death among women who took glatiramer acetate involved an infant who died 30 minutes after birth in gestational week 24 because of a maternal infection. According to the investigators, “the mother received glatiramer acetate for 8 months prior to pregnancy, stopped treatment in the second [gestational week], and was not exposed to other substances during pregnancy.”
A total of nine congenital abnormalities (eight major, one minor) were observed without any specific pattern and included three in glatiramer acetate–exposed neonates and six in unexposed neonates.
No safety signals were reported for glatiramer acetate on the outcome of pregnancy, labor, or delivery in a previous meta-analysis of 97 pregnancies in eight studies. Glatiramer acetate’s manufacturer, Teva, reported no adverse outcomes in a conference abstract of 245 pregnancies exposed to glatiramer acetate, but the company has not published its postmarketing surveillance data in manuscript form, the authors wrote.
“Our results of a lacking adverse effect of glatiramer acetate during early pregnancy exposure are biologically plausible as it is very unlikely that glatiramer acetate passes the placental barrier,” the investigators wrote, because it is not permeable for a large heterogeneous mixture of polypeptides such as glatiramer acetate, which have molecular weights of 5,000-9,000 d.
The German Multiple Sclerosis and Pregnancy registry was partly supported by Bayer Healthcare, Biogen Idec Germany, Merck Serono, Novartis Pharma, Teva Pharma, and Sanofi-Aventis Genzyme Pharmaceuticals, but the sponsors had no role in the registry design, data collection, analyses, or dissemination of results. Two authors reported financial ties to numerous pharmaceutical companies that market MS drugs, and two reported support from the German Research Council. Another author is the site principal investigator for two industry-sponsored randomized clinical trials.
Glatiramer acetate exposure during the first trimester of pregnancy appears safe and was not associated with a teratogenic effect in a nationwide German Multiple Sclerosis and Pregnancy registry.
In the second largest study of the safety of glatiramer acetate exposure during early pregnancy in multiple sclerosis patients, Sandra Herbstritt, Pharm.D., and her colleagues at Ruhr University Bochum (Germany) reported that exposure to the drug in 151 women with multiple sclerosis was not associated with significant differences in pregnancy or birth outcomes when compared with 95 controls without exposure to disease-modifying therapy (DMT) during pregnancy. All but three of the patients who took glatiramer acetate stopped it in the first trimester (median duration of 31 days; range, 0-154 days). Pregnancies were considered exposed to glatiramer acetate if the last injection was administered after the last menstrual period (Mult Scler. 2016 Jan 11. doi: 10.1177/1352458515623366).
Significantly more relapses occurred in women who did not take a DMT during pregnancy than in women who took glatiramer acetate (28 vs. 18, respectively), particularly in the first and third trimesters. A total of 224 live births occurred, including 136 with exposure to glatiramer acetate and 88 without DMT exposure. All but 3 of the 22 pregnancies that did not result in live births were spontaneous abortions in the first trimester.
The only early neonatal death among women who took glatiramer acetate involved an infant who died 30 minutes after birth in gestational week 24 because of a maternal infection. According to the investigators, “the mother received glatiramer acetate for 8 months prior to pregnancy, stopped treatment in the second [gestational week], and was not exposed to other substances during pregnancy.”
A total of nine congenital abnormalities (eight major, one minor) were observed without any specific pattern and included three in glatiramer acetate–exposed neonates and six in unexposed neonates.
No safety signals were reported for glatiramer acetate on the outcome of pregnancy, labor, or delivery in a previous meta-analysis of 97 pregnancies in eight studies. Glatiramer acetate’s manufacturer, Teva, reported no adverse outcomes in a conference abstract of 245 pregnancies exposed to glatiramer acetate, but the company has not published its postmarketing surveillance data in manuscript form, the authors wrote.
“Our results of a lacking adverse effect of glatiramer acetate during early pregnancy exposure are biologically plausible as it is very unlikely that glatiramer acetate passes the placental barrier,” the investigators wrote, because it is not permeable for a large heterogeneous mixture of polypeptides such as glatiramer acetate, which have molecular weights of 5,000-9,000 d.
The German Multiple Sclerosis and Pregnancy registry was partly supported by Bayer Healthcare, Biogen Idec Germany, Merck Serono, Novartis Pharma, Teva Pharma, and Sanofi-Aventis Genzyme Pharmaceuticals, but the sponsors had no role in the registry design, data collection, analyses, or dissemination of results. Two authors reported financial ties to numerous pharmaceutical companies that market MS drugs, and two reported support from the German Research Council. Another author is the site principal investigator for two industry-sponsored randomized clinical trials.
FROM MULTIPLE SCLEROSIS JOURNAL
Key clinical point: Glatiramer acetate is not associated with adverse maternal or neonatal outcomes, but nonuse of any disease-modifying therapy raises the risk of having more disease relapses.
Major finding: Exposure to glatiramer acetate in 151 women with multiple sclerosis was not associated with significant differences in pregnancy or birth outcomes when compared with 95 controls without exposure to disease-modifying therapy.
Data source: A cohort study of 246 women with multiple sclerosis who became pregnant and enrolled in a German registry.
Disclosures: The German Multiple Sclerosis and Pregnancy registry was partly supported by Bayer Healthcare, Biogen Idec Germany, Merck Serono, Novartis Pharma, Teva Pharma, and Sanofi-Aventis Genzyme Pharmaceuticals, but the sponsors had no role in the registry design, data collection, analyses, or dissemination of results. Two authors reported financial ties to numerous pharmaceutical companies that market MS drugs, and two reported support from the German Research Council. Another author is the site principal investigator for two industry-sponsored randomized clinical trials.
Secukinumab receives FDA approval for psoriatic arthritis, ankylosing spondylitis
The Food and Drug Administration approved two new indications for the interleukin-17A inhibitor secukinumab (Cosentyx) – psoriatic arthritis in adults and ankylosing spondylitis in adults – on Jan. 15. These join the approval for moderate to severe plaque psoriasis in adults it received in January 2015, according to an announcement from the drug’s manufacturer, Novartis.
The approvals are based on the efficacy and safety outcomes from four placebo-controlled, phase III studies, which included more than 1,500 adult patients with ankylosing spondylitis (AS) or psoriatic arthritis (PsA) who were biologic treatment naive or had an inadequate response or were intolerant to anti-TNF agents.
Pivotal phase III studies in the secukinumab clinical trial program, which provided key data for the submission, were MEASURE 1 and MEASURE 2 involving 590 patients with AS, and FUTURE 1 and FUTURE 2 involving 1,003 patients with PsA. Novartis continues to investigate the fully human monoclonal antibody against IL-17A for its potential in preventing radiographic progression of spinal and joint structural damage in AS and PsA patients, respectively.
The European Medicines Agency approved secukinumab for PsA and AS in November 2015.
The Food and Drug Administration approved two new indications for the interleukin-17A inhibitor secukinumab (Cosentyx) – psoriatic arthritis in adults and ankylosing spondylitis in adults – on Jan. 15. These join the approval for moderate to severe plaque psoriasis in adults it received in January 2015, according to an announcement from the drug’s manufacturer, Novartis.
The approvals are based on the efficacy and safety outcomes from four placebo-controlled, phase III studies, which included more than 1,500 adult patients with ankylosing spondylitis (AS) or psoriatic arthritis (PsA) who were biologic treatment naive or had an inadequate response or were intolerant to anti-TNF agents.
Pivotal phase III studies in the secukinumab clinical trial program, which provided key data for the submission, were MEASURE 1 and MEASURE 2 involving 590 patients with AS, and FUTURE 1 and FUTURE 2 involving 1,003 patients with PsA. Novartis continues to investigate the fully human monoclonal antibody against IL-17A for its potential in preventing radiographic progression of spinal and joint structural damage in AS and PsA patients, respectively.
The European Medicines Agency approved secukinumab for PsA and AS in November 2015.
The Food and Drug Administration approved two new indications for the interleukin-17A inhibitor secukinumab (Cosentyx) – psoriatic arthritis in adults and ankylosing spondylitis in adults – on Jan. 15. These join the approval for moderate to severe plaque psoriasis in adults it received in January 2015, according to an announcement from the drug’s manufacturer, Novartis.
The approvals are based on the efficacy and safety outcomes from four placebo-controlled, phase III studies, which included more than 1,500 adult patients with ankylosing spondylitis (AS) or psoriatic arthritis (PsA) who were biologic treatment naive or had an inadequate response or were intolerant to anti-TNF agents.
Pivotal phase III studies in the secukinumab clinical trial program, which provided key data for the submission, were MEASURE 1 and MEASURE 2 involving 590 patients with AS, and FUTURE 1 and FUTURE 2 involving 1,003 patients with PsA. Novartis continues to investigate the fully human monoclonal antibody against IL-17A for its potential in preventing radiographic progression of spinal and joint structural damage in AS and PsA patients, respectively.
The European Medicines Agency approved secukinumab for PsA and AS in November 2015.
FDA rejects antisense oligonucleotide drug for Duchenne muscular dystrophy
The Food and Drug Administration has decided against approving the exon 51-skipping antisense oligonucleotide drug drisapersen for forms of Duchenne muscular dystrophy amenable to exon skipping.
The agency’s complete response letter to BioMarin Pharmaceutical, the developer of drisapersen (Kyndrisa), said that the standard of substantial evidence of effectiveness had not been met, according to a written statement from the company on Jan. 14.
In a Nov. 24, 2015, meeting of the FDA’s Peripheral and Central Nervous System Drugs Advisory Committee, panel members generally felt that drisapersen’s efficacy data were not persuasive enough for an approval.
Drisapersen targets frame-disrupting mutations found in exon 51 of the dystrophin gene, which produces a nonfunctional protein in individuals with a certain form of Duchenne, by restoring expression of the mutated dystrophin gene. There are currently no FDA-approved drugs to treat Duchenne, which affects approximately 1 in every 3,500 to 1 in 5,000 male children, making it the most common fatal genetic disorder diagnosed in childhood.
BioMarin said that extension studies of drisapersen will continue as the company determines the next steps in its new drug application, as will the ongoing clinical trials for other exon-skipping oligonucleotides it is developing. The drug is still under review by the European Medicines Agency.
The Food and Drug Administration has decided against approving the exon 51-skipping antisense oligonucleotide drug drisapersen for forms of Duchenne muscular dystrophy amenable to exon skipping.
The agency’s complete response letter to BioMarin Pharmaceutical, the developer of drisapersen (Kyndrisa), said that the standard of substantial evidence of effectiveness had not been met, according to a written statement from the company on Jan. 14.
In a Nov. 24, 2015, meeting of the FDA’s Peripheral and Central Nervous System Drugs Advisory Committee, panel members generally felt that drisapersen’s efficacy data were not persuasive enough for an approval.
Drisapersen targets frame-disrupting mutations found in exon 51 of the dystrophin gene, which produces a nonfunctional protein in individuals with a certain form of Duchenne, by restoring expression of the mutated dystrophin gene. There are currently no FDA-approved drugs to treat Duchenne, which affects approximately 1 in every 3,500 to 1 in 5,000 male children, making it the most common fatal genetic disorder diagnosed in childhood.
BioMarin said that extension studies of drisapersen will continue as the company determines the next steps in its new drug application, as will the ongoing clinical trials for other exon-skipping oligonucleotides it is developing. The drug is still under review by the European Medicines Agency.
The Food and Drug Administration has decided against approving the exon 51-skipping antisense oligonucleotide drug drisapersen for forms of Duchenne muscular dystrophy amenable to exon skipping.
The agency’s complete response letter to BioMarin Pharmaceutical, the developer of drisapersen (Kyndrisa), said that the standard of substantial evidence of effectiveness had not been met, according to a written statement from the company on Jan. 14.
In a Nov. 24, 2015, meeting of the FDA’s Peripheral and Central Nervous System Drugs Advisory Committee, panel members generally felt that drisapersen’s efficacy data were not persuasive enough for an approval.
Drisapersen targets frame-disrupting mutations found in exon 51 of the dystrophin gene, which produces a nonfunctional protein in individuals with a certain form of Duchenne, by restoring expression of the mutated dystrophin gene. There are currently no FDA-approved drugs to treat Duchenne, which affects approximately 1 in every 3,500 to 1 in 5,000 male children, making it the most common fatal genetic disorder diagnosed in childhood.
BioMarin said that extension studies of drisapersen will continue as the company determines the next steps in its new drug application, as will the ongoing clinical trials for other exon-skipping oligonucleotides it is developing. The drug is still under review by the European Medicines Agency.
Study bolsters argument for sodium channel role in MS cerebellar dysfunction
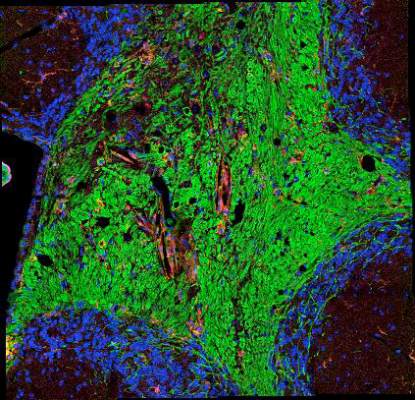
Specific polymorphisms of the SCN10A gene affect motor coordination and functional status in relapsing-onset multiple sclerosis (MS) patients via the abnormal expression of the voltage-gated Nav1.8 sodium channel in cerebellar Purkinje neurons, causing dysfunctional cerebellothalamic circuitry, according to findings from a prospective cohort study.
The clinical effects of abnormally expressed Nav1.8 in cerebellar Purkinje neurons and the polymorphisms’ effect on the activity of the channels in affected patients suggests that “SCN10A genotype may predict an MS subphenotype with significantly greater deficit in motor coordination and cognition and compromised cerebellothalamic functional integrity. This study further supports previous evidence that Nav1.8 channelopathy is involved in the pathophysiology of cerebellar dysfunction in MS,” Dr. Tina Roostaei of the Tehran (Iran) University of Medical Sciences and her colleagues reported (Neurology. 2016 Jan 6. doi: 10.1212/WNL.0000000000002326). The authors noted that “unlike other clinical abnormalities in MS that tend to be remitting, cerebellar dysfunction tends to become persistent early in the course of the illness and is refractory to either disease-modifying or symptomatic therapy.”
Genotyping for four potentially functional SCN10A polymorphisms in 161 patients with relapsing-onset MS and 94 healthy controls revealed two polymorphisms that proved significantly related to performance on the Multiple Sclerosis Functional Composite and all its subscores, with carriers of one polymorphism (rs6795970AA) performing worse than carriers of rs6795970G, regardless of Expanded Disability Status Scale score or cerebellar atrophy. However, carriers of rs6795970AA did not have significant gross ataxia as indexed by the Scale for the Assessment and Rating of Ataxia and cerebellar functional system score. The poor-performing carriers showed significantly diminished cerebellar functional connectivity with the thalami and midbrain on functional MRI. Similar results occurred for analyses of a separate polymorphism (rs6801957) that was in high-linkage disequilibrium with rs6795970. The effects of the polymorphisms were not seen in the healthy controls.
The effects of abnormal Nav1.8 channel expression on Purkinje cells is thought to alter their activity because Nav1.8 channels are normally found on unmyelinated sensory neurons of the dorsal root ganglia and peripheral nerve axons and support their repetitive firing by rapidly recovering from inactivation at depolarized membrane potentials.
The study by Dr. Roostaei and her colleagues and previous research suggests that it may be possible to reverse cerebellar manifestations of MS by blocking Nav1.8 with drugs currently in development for treating pain caused by pain-signaling cells in dorsal root ganglion neurons, which have been shown to improve clinical function in animal models of MS, wrote Dr. Stephen G. Waxman of Yale University, New Haven, Conn., and Dr. Orhun H. Kantarci of the Mayo Clinic, Rochester, Minn., in an accompanying editorial (Neurology. 2016 Jan 6. doi: 10.1212/WNL.0000000000002338). Additional work needs to be done with higher-resolution tests of cerebellar function to determine the effects of the abnormal presence of Nav1.8 on Purkinje cells in the cerebellum of MS patients, as well as further experiments to “understand the triggers that lead to upregulation of Nav1.8 expression in the cerebellum in MS.”
The study was supported by the Tehran University of Medical Sciences and the MS Society of Iran. One author reported receiving financial compensation from Biogen, Merck Serono, Bayer-Schering, Novartis, and CinnaGen for consulting and speaking services. Dr. Waxman reported holding a patent for invention of sodium channel Nav1.9, serving on the advisory board of SiteOne Therapeutics, and consulting for a variety of pharmaceutical companies. Dr. Kantarci reported receiving funding for travel and/or speaker honoraria from Novartis; research support from the European Regional Development Fund, National Multiple Sclerosis Society, Mayo Foundation, and Hilton Foundation; and participating in grant review for the National Multiple Sclerosis Society.
Specific polymorphisms of the SCN10A gene affect motor coordination and functional status in relapsing-onset multiple sclerosis (MS) patients via the abnormal expression of the voltage-gated Nav1.8 sodium channel in cerebellar Purkinje neurons, causing dysfunctional cerebellothalamic circuitry, according to findings from a prospective cohort study.
The clinical effects of abnormally expressed Nav1.8 in cerebellar Purkinje neurons and the polymorphisms’ effect on the activity of the channels in affected patients suggests that “SCN10A genotype may predict an MS subphenotype with significantly greater deficit in motor coordination and cognition and compromised cerebellothalamic functional integrity. This study further supports previous evidence that Nav1.8 channelopathy is involved in the pathophysiology of cerebellar dysfunction in MS,” Dr. Tina Roostaei of the Tehran (Iran) University of Medical Sciences and her colleagues reported (Neurology. 2016 Jan 6. doi: 10.1212/WNL.0000000000002326). The authors noted that “unlike other clinical abnormalities in MS that tend to be remitting, cerebellar dysfunction tends to become persistent early in the course of the illness and is refractory to either disease-modifying or symptomatic therapy.”
Genotyping for four potentially functional SCN10A polymorphisms in 161 patients with relapsing-onset MS and 94 healthy controls revealed two polymorphisms that proved significantly related to performance on the Multiple Sclerosis Functional Composite and all its subscores, with carriers of one polymorphism (rs6795970AA) performing worse than carriers of rs6795970G, regardless of Expanded Disability Status Scale score or cerebellar atrophy. However, carriers of rs6795970AA did not have significant gross ataxia as indexed by the Scale for the Assessment and Rating of Ataxia and cerebellar functional system score. The poor-performing carriers showed significantly diminished cerebellar functional connectivity with the thalami and midbrain on functional MRI. Similar results occurred for analyses of a separate polymorphism (rs6801957) that was in high-linkage disequilibrium with rs6795970. The effects of the polymorphisms were not seen in the healthy controls.
The effects of abnormal Nav1.8 channel expression on Purkinje cells is thought to alter their activity because Nav1.8 channels are normally found on unmyelinated sensory neurons of the dorsal root ganglia and peripheral nerve axons and support their repetitive firing by rapidly recovering from inactivation at depolarized membrane potentials.
The study by Dr. Roostaei and her colleagues and previous research suggests that it may be possible to reverse cerebellar manifestations of MS by blocking Nav1.8 with drugs currently in development for treating pain caused by pain-signaling cells in dorsal root ganglion neurons, which have been shown to improve clinical function in animal models of MS, wrote Dr. Stephen G. Waxman of Yale University, New Haven, Conn., and Dr. Orhun H. Kantarci of the Mayo Clinic, Rochester, Minn., in an accompanying editorial (Neurology. 2016 Jan 6. doi: 10.1212/WNL.0000000000002338). Additional work needs to be done with higher-resolution tests of cerebellar function to determine the effects of the abnormal presence of Nav1.8 on Purkinje cells in the cerebellum of MS patients, as well as further experiments to “understand the triggers that lead to upregulation of Nav1.8 expression in the cerebellum in MS.”
The study was supported by the Tehran University of Medical Sciences and the MS Society of Iran. One author reported receiving financial compensation from Biogen, Merck Serono, Bayer-Schering, Novartis, and CinnaGen for consulting and speaking services. Dr. Waxman reported holding a patent for invention of sodium channel Nav1.9, serving on the advisory board of SiteOne Therapeutics, and consulting for a variety of pharmaceutical companies. Dr. Kantarci reported receiving funding for travel and/or speaker honoraria from Novartis; research support from the European Regional Development Fund, National Multiple Sclerosis Society, Mayo Foundation, and Hilton Foundation; and participating in grant review for the National Multiple Sclerosis Society.
Specific polymorphisms of the SCN10A gene affect motor coordination and functional status in relapsing-onset multiple sclerosis (MS) patients via the abnormal expression of the voltage-gated Nav1.8 sodium channel in cerebellar Purkinje neurons, causing dysfunctional cerebellothalamic circuitry, according to findings from a prospective cohort study.
The clinical effects of abnormally expressed Nav1.8 in cerebellar Purkinje neurons and the polymorphisms’ effect on the activity of the channels in affected patients suggests that “SCN10A genotype may predict an MS subphenotype with significantly greater deficit in motor coordination and cognition and compromised cerebellothalamic functional integrity. This study further supports previous evidence that Nav1.8 channelopathy is involved in the pathophysiology of cerebellar dysfunction in MS,” Dr. Tina Roostaei of the Tehran (Iran) University of Medical Sciences and her colleagues reported (Neurology. 2016 Jan 6. doi: 10.1212/WNL.0000000000002326). The authors noted that “unlike other clinical abnormalities in MS that tend to be remitting, cerebellar dysfunction tends to become persistent early in the course of the illness and is refractory to either disease-modifying or symptomatic therapy.”
Genotyping for four potentially functional SCN10A polymorphisms in 161 patients with relapsing-onset MS and 94 healthy controls revealed two polymorphisms that proved significantly related to performance on the Multiple Sclerosis Functional Composite and all its subscores, with carriers of one polymorphism (rs6795970AA) performing worse than carriers of rs6795970G, regardless of Expanded Disability Status Scale score or cerebellar atrophy. However, carriers of rs6795970AA did not have significant gross ataxia as indexed by the Scale for the Assessment and Rating of Ataxia and cerebellar functional system score. The poor-performing carriers showed significantly diminished cerebellar functional connectivity with the thalami and midbrain on functional MRI. Similar results occurred for analyses of a separate polymorphism (rs6801957) that was in high-linkage disequilibrium with rs6795970. The effects of the polymorphisms were not seen in the healthy controls.
The effects of abnormal Nav1.8 channel expression on Purkinje cells is thought to alter their activity because Nav1.8 channels are normally found on unmyelinated sensory neurons of the dorsal root ganglia and peripheral nerve axons and support their repetitive firing by rapidly recovering from inactivation at depolarized membrane potentials.
The study by Dr. Roostaei and her colleagues and previous research suggests that it may be possible to reverse cerebellar manifestations of MS by blocking Nav1.8 with drugs currently in development for treating pain caused by pain-signaling cells in dorsal root ganglion neurons, which have been shown to improve clinical function in animal models of MS, wrote Dr. Stephen G. Waxman of Yale University, New Haven, Conn., and Dr. Orhun H. Kantarci of the Mayo Clinic, Rochester, Minn., in an accompanying editorial (Neurology. 2016 Jan 6. doi: 10.1212/WNL.0000000000002338). Additional work needs to be done with higher-resolution tests of cerebellar function to determine the effects of the abnormal presence of Nav1.8 on Purkinje cells in the cerebellum of MS patients, as well as further experiments to “understand the triggers that lead to upregulation of Nav1.8 expression in the cerebellum in MS.”
The study was supported by the Tehran University of Medical Sciences and the MS Society of Iran. One author reported receiving financial compensation from Biogen, Merck Serono, Bayer-Schering, Novartis, and CinnaGen for consulting and speaking services. Dr. Waxman reported holding a patent for invention of sodium channel Nav1.9, serving on the advisory board of SiteOne Therapeutics, and consulting for a variety of pharmaceutical companies. Dr. Kantarci reported receiving funding for travel and/or speaker honoraria from Novartis; research support from the European Regional Development Fund, National Multiple Sclerosis Society, Mayo Foundation, and Hilton Foundation; and participating in grant review for the National Multiple Sclerosis Society.
FROM NEUROLOGY
Key clinical point: New evidence further supports previous evidence that Nav1.8 channelopathy is involved in the pathophysiology of cerebellar dysfunction in MS.
Major finding: Two polymorphisms in the SCN10A gene were associated with worse performance on the Multiple Sclerosis Functional Composite and all its subscores, regardless of Expanded Disability Status Scale score or cerebellar atrophy.
Data source: A prospective cohort study of 161 patients with relapsing-onset MS and 94 healthy controls.
Disclosures: The study was supported by the Tehran University of Medical Sciences and the MS Society of Iran. One author reported receiving financial compensation from Biogen, Merck Serono, Bayer-Schering, Novartis, and CinnaGen for consulting and speaking services. Dr. Waxman reported holding a patent for invention of sodium channel Nav1.9, serving on the advisory board of SiteOne Therapeutics, and consulting for a variety of pharmaceutical companies. Dr. Kantarci reported receiving funding for travel and/or speaker honoraria from Novartis; research support from the European Regional Development Fund, National Multiple Sclerosis Society, Mayo Foundation, and Hilton Foundation; and participating in grant review for the National Multiple Sclerosis Society.
Anti-SPAG16 antibodies could be prognostic marker in primary progressive MS
The recently identified autoantibody target in multiple sclerosis, sperm-associated antigen 16 (SPAG16), occurred most often in patients with primary progressive disease and was associated with faster-progressing disease in a case-control cohort study of Belgian and Spanish patients.
Anti-SPAG16 antibody reactivity to the autoantigen, which occurred in 22% of 374 multiple sclerosis (MS) patients overall in the study, was highest among patients with primary progressive MS (PPMS, 34% of 61), followed by secondary progressive MS (SPMS, 26% of 39) and relapsing-remitting MS (RRMS, 19% of 274). Patients with PPMS also had the highest anti-SPAG16 antibody levels, and seropositive PPMS patients had greater worsening of disease over time, judging from a significantly increased progression index relative to seronegative PPMS patients, Laura de Bock of Hasselt University, Diepenbeek, Belgium, and her colleagues reported (Eur J Neurol. 2015 Dec 26. doi: 10.1111/ene.12925).
Anti-SPAG16 antibody seropositivity had a 93% specificity for MS. A total of 7 out of 106 healthy controls were seropositive, based on a cutoff of 70 arbitrary units (AU) for seropositivity using enzyme-linked immunosorbent assay testing. While the mean anti-SPAG16 antibody levels were 58.7 AU in MS patients overall and 16.6 AU in healthy controls, PPMS patients had significantly higher mean levels than did RRMS patients (77.9 vs. 53.2 AU). However, anti-SPAG16 antibody levels in SPMS patients (67.5 AU) did not differ significantly from the other MS groups. The investigators suggested that the “increase in anti-SPAG16 antibody levels [in PPMS patients] is probably due to the significantly increased proportion of PPMS patients (34%) positive for anti-SPAG16 antibodies compared to RRMS patients (19%)” and that anti-SPAG16 antibody seropositivity overall “is possibly linked to disease stage and pathological subtype.”
Age did not correlate with antibody levels, although PPMS patients were significantly younger than their seronegative counterparts when antibodies were detected (48.4 years vs. 56.0 years), compared with patients with other MS subtypes. The seropositive PPMS patients also had significantly shorter mean disease duration than did seronegative PPMS patients (4.6 years vs. 7.9 years) despite having a similar mean Expanded Disability Status Scale (EDSS) score (4.2 vs. 4.1). This indication of a faster disease progression in seropositive PPMS patients was confirmed by their higher mean progression index, compared with seronegative patients (2.7 vs. 1.0); progression index was also significantly correlated with mean score on the MS severity scale (MSSS). Independent predictors of anti-SPAG16 antibody seropositivity on a logistic regression analysis included female sex (odds ratio, 3.91) and progression index (OR, 1.78).
In the overall cohort of MS patients, seropositivity was associated with a significantly higher mean EDSS score than was seronegative status (2.9 vs. 2.5, respectively), although EDSS did not differ according to serologic status in RRMS and SPMS subtypes. Serologic status in those subtypes also was not influenced by sex, disease duration, progression index, or MSSS score.
“Future follow-up of seropositive and seronegative PPMS patients is essential to conclude whether the presence of anti-SPAG16 antibodies could be a novel prognostic biomarker in PPMS. It would be interesting to investigate anti-SPAG16 antibodies in relation to neurofilament light levels, which have been shown to be higher in PPMS and can be used as a prognostic marker, and to investigate whether anti-SPAG16 antibodies can be used as a biomarker for possible treatment monitoring in PPMS,” the investigators wrote.
SPAG16 is known to be upregulated in astrocytes in MS lesions, the researchers noted. “Interestingly, astrocytes are becoming increasingly recognized as important players in MS progression and targets of autoantibodies in MS. It is possible that anti-SPAG16 antibodies are formed due to cell damage and death of astrocytes which leads to the exposure of intracellular antigens such as SPAG16 (epitope spreading).”
The study received support from the Transnationale Universiteit Limburg, Hasselt University, the Flanders Fund for Scientific Research, the Charcot Foundation (Belgium), and Rotary International. Two authors declared financial relationships with companies marketing MS drugs.
The recently identified autoantibody target in multiple sclerosis, sperm-associated antigen 16 (SPAG16), occurred most often in patients with primary progressive disease and was associated with faster-progressing disease in a case-control cohort study of Belgian and Spanish patients.
Anti-SPAG16 antibody reactivity to the autoantigen, which occurred in 22% of 374 multiple sclerosis (MS) patients overall in the study, was highest among patients with primary progressive MS (PPMS, 34% of 61), followed by secondary progressive MS (SPMS, 26% of 39) and relapsing-remitting MS (RRMS, 19% of 274). Patients with PPMS also had the highest anti-SPAG16 antibody levels, and seropositive PPMS patients had greater worsening of disease over time, judging from a significantly increased progression index relative to seronegative PPMS patients, Laura de Bock of Hasselt University, Diepenbeek, Belgium, and her colleagues reported (Eur J Neurol. 2015 Dec 26. doi: 10.1111/ene.12925).
Anti-SPAG16 antibody seropositivity had a 93% specificity for MS. A total of 7 out of 106 healthy controls were seropositive, based on a cutoff of 70 arbitrary units (AU) for seropositivity using enzyme-linked immunosorbent assay testing. While the mean anti-SPAG16 antibody levels were 58.7 AU in MS patients overall and 16.6 AU in healthy controls, PPMS patients had significantly higher mean levels than did RRMS patients (77.9 vs. 53.2 AU). However, anti-SPAG16 antibody levels in SPMS patients (67.5 AU) did not differ significantly from the other MS groups. The investigators suggested that the “increase in anti-SPAG16 antibody levels [in PPMS patients] is probably due to the significantly increased proportion of PPMS patients (34%) positive for anti-SPAG16 antibodies compared to RRMS patients (19%)” and that anti-SPAG16 antibody seropositivity overall “is possibly linked to disease stage and pathological subtype.”
Age did not correlate with antibody levels, although PPMS patients were significantly younger than their seronegative counterparts when antibodies were detected (48.4 years vs. 56.0 years), compared with patients with other MS subtypes. The seropositive PPMS patients also had significantly shorter mean disease duration than did seronegative PPMS patients (4.6 years vs. 7.9 years) despite having a similar mean Expanded Disability Status Scale (EDSS) score (4.2 vs. 4.1). This indication of a faster disease progression in seropositive PPMS patients was confirmed by their higher mean progression index, compared with seronegative patients (2.7 vs. 1.0); progression index was also significantly correlated with mean score on the MS severity scale (MSSS). Independent predictors of anti-SPAG16 antibody seropositivity on a logistic regression analysis included female sex (odds ratio, 3.91) and progression index (OR, 1.78).
In the overall cohort of MS patients, seropositivity was associated with a significantly higher mean EDSS score than was seronegative status (2.9 vs. 2.5, respectively), although EDSS did not differ according to serologic status in RRMS and SPMS subtypes. Serologic status in those subtypes also was not influenced by sex, disease duration, progression index, or MSSS score.
“Future follow-up of seropositive and seronegative PPMS patients is essential to conclude whether the presence of anti-SPAG16 antibodies could be a novel prognostic biomarker in PPMS. It would be interesting to investigate anti-SPAG16 antibodies in relation to neurofilament light levels, which have been shown to be higher in PPMS and can be used as a prognostic marker, and to investigate whether anti-SPAG16 antibodies can be used as a biomarker for possible treatment monitoring in PPMS,” the investigators wrote.
SPAG16 is known to be upregulated in astrocytes in MS lesions, the researchers noted. “Interestingly, astrocytes are becoming increasingly recognized as important players in MS progression and targets of autoantibodies in MS. It is possible that anti-SPAG16 antibodies are formed due to cell damage and death of astrocytes which leads to the exposure of intracellular antigens such as SPAG16 (epitope spreading).”
The study received support from the Transnationale Universiteit Limburg, Hasselt University, the Flanders Fund for Scientific Research, the Charcot Foundation (Belgium), and Rotary International. Two authors declared financial relationships with companies marketing MS drugs.
The recently identified autoantibody target in multiple sclerosis, sperm-associated antigen 16 (SPAG16), occurred most often in patients with primary progressive disease and was associated with faster-progressing disease in a case-control cohort study of Belgian and Spanish patients.
Anti-SPAG16 antibody reactivity to the autoantigen, which occurred in 22% of 374 multiple sclerosis (MS) patients overall in the study, was highest among patients with primary progressive MS (PPMS, 34% of 61), followed by secondary progressive MS (SPMS, 26% of 39) and relapsing-remitting MS (RRMS, 19% of 274). Patients with PPMS also had the highest anti-SPAG16 antibody levels, and seropositive PPMS patients had greater worsening of disease over time, judging from a significantly increased progression index relative to seronegative PPMS patients, Laura de Bock of Hasselt University, Diepenbeek, Belgium, and her colleagues reported (Eur J Neurol. 2015 Dec 26. doi: 10.1111/ene.12925).
Anti-SPAG16 antibody seropositivity had a 93% specificity for MS. A total of 7 out of 106 healthy controls were seropositive, based on a cutoff of 70 arbitrary units (AU) for seropositivity using enzyme-linked immunosorbent assay testing. While the mean anti-SPAG16 antibody levels were 58.7 AU in MS patients overall and 16.6 AU in healthy controls, PPMS patients had significantly higher mean levels than did RRMS patients (77.9 vs. 53.2 AU). However, anti-SPAG16 antibody levels in SPMS patients (67.5 AU) did not differ significantly from the other MS groups. The investigators suggested that the “increase in anti-SPAG16 antibody levels [in PPMS patients] is probably due to the significantly increased proportion of PPMS patients (34%) positive for anti-SPAG16 antibodies compared to RRMS patients (19%)” and that anti-SPAG16 antibody seropositivity overall “is possibly linked to disease stage and pathological subtype.”
Age did not correlate with antibody levels, although PPMS patients were significantly younger than their seronegative counterparts when antibodies were detected (48.4 years vs. 56.0 years), compared with patients with other MS subtypes. The seropositive PPMS patients also had significantly shorter mean disease duration than did seronegative PPMS patients (4.6 years vs. 7.9 years) despite having a similar mean Expanded Disability Status Scale (EDSS) score (4.2 vs. 4.1). This indication of a faster disease progression in seropositive PPMS patients was confirmed by their higher mean progression index, compared with seronegative patients (2.7 vs. 1.0); progression index was also significantly correlated with mean score on the MS severity scale (MSSS). Independent predictors of anti-SPAG16 antibody seropositivity on a logistic regression analysis included female sex (odds ratio, 3.91) and progression index (OR, 1.78).
In the overall cohort of MS patients, seropositivity was associated with a significantly higher mean EDSS score than was seronegative status (2.9 vs. 2.5, respectively), although EDSS did not differ according to serologic status in RRMS and SPMS subtypes. Serologic status in those subtypes also was not influenced by sex, disease duration, progression index, or MSSS score.
“Future follow-up of seropositive and seronegative PPMS patients is essential to conclude whether the presence of anti-SPAG16 antibodies could be a novel prognostic biomarker in PPMS. It would be interesting to investigate anti-SPAG16 antibodies in relation to neurofilament light levels, which have been shown to be higher in PPMS and can be used as a prognostic marker, and to investigate whether anti-SPAG16 antibodies can be used as a biomarker for possible treatment monitoring in PPMS,” the investigators wrote.
SPAG16 is known to be upregulated in astrocytes in MS lesions, the researchers noted. “Interestingly, astrocytes are becoming increasingly recognized as important players in MS progression and targets of autoantibodies in MS. It is possible that anti-SPAG16 antibodies are formed due to cell damage and death of astrocytes which leads to the exposure of intracellular antigens such as SPAG16 (epitope spreading).”
The study received support from the Transnationale Universiteit Limburg, Hasselt University, the Flanders Fund for Scientific Research, the Charcot Foundation (Belgium), and Rotary International. Two authors declared financial relationships with companies marketing MS drugs.
FROM EUROPEAN JOURNAL OF NEUROLOGY
Key clinical point: The presence of anti-SPAG16 antibodies could be a novel prognostic biomarker in PPMS, but further follow-up is required.
Major finding: Anti-SPAG16 antibody reactivity was highest among patients with PPMS (34% of 61), followed by SPMS (26% of 39) and RRMS (19% of 274).
Data source: A case-control study of 374 MS patients and 106 healthy controls.
Disclosures: The study received support from the Transnationale Universiteit Limburg, Hasselt University, the Flanders Fund for Scientific Research, the Charcot Foundation (Belgium), and Rotary International. Two authors declared financial relationships with companies marketing MS drugs.
T-cell biomarker not viable for detecting PML risk with natalizumab
The expression of l-selectin on specific T cells in peripheral blood from patients with relapsing forms of multiple sclerosis (MS) does not reliably predict risk for progressive multifocal leukoencephalopathy (PML) during natalizumab treatment, according to findings from a Biogen-supported study.
These findings are at odds with those of a previously reported preliminary study that used a different analytical technique. Investigators in the earlier preliminary study had found a drop in the percentage of CD4- and CD3-positive T cells expressing l-selectin (CD62L) at least 4 months and often 2 years prior to PML diagnosis and concluded that measuring the percentage of CD4- and CD3-positive T cells expressing l-selectin (%CD62L) “may improve stratification of patients taking natalizumab who are at risk for developing PML,” according to the study from Biogen, which makes natalizumab (Tysabri).
Biogen investigators, led by Linda A. Lieberman, Ph.D., sought to confirm the findings, enhance the reproducibility of the %CD62L assay, “and potentially enable the deployment of %CD62L as a biomarker for PML in a global setting.” However, the investigators did not find a significant difference in %CD62L in cryopreserved peripheral blood mononuclear cells in 104 patients with relapsing forms of multiple sclerosis (MS) on natalizumab who did not develop PML, compared with 21 who developed PML (Neurology. 2015 Dec 30. doi: 10.1212/WNL.0000000000002314).
In the current study, the investigators detected a large range in %CD62L (0.31%-68.4%) in a subset of natalizumab-treated MS patients without PML at two time points at least 6 months apart. Because CD62L and the chemokine receptor CCR7 are coexpressed on CD4- and CD3-positive T cells, they also checked the level of variation in simultaneous measurements of %CD62L and %CCR7 on the same cells at two separate time points in the same patients. They found that %CD62L expression varied substantially, whereas %CCR7 varied little, and the difference between the two was significant, “signifying that %CD62L is not a stable outcome measure,” they wrote.
Dr. Lieberman and her colleagues also confirmed a positive correlation between lymphocyte viability and %CD62L expression, which highlights the “technique-driven variability of the assay” that was used in the preliminary study.
In patient samples collected at least 6 months prior to PML diagnosis, %CD62L did not discriminate significantly between non-PML and active PML (defined as 0-6 months prior to diagnosis). The median %CD62L varied according to the viability of cryopreserved CD4- and CD3-positive T cells. Median %CD62L was no different between non-PML and pre-PML samples with lymphocyte viability greater than 75% (25.9% vs. 26.3%, respectively) but was significantly lower than with non-PML and pre-PML samples with lymphocyte viability less than 75% (10.55% and 5.41%). There was no difference in lymphocyte viability between non-PML and pre-PML samples.
In a case-control comparison of patients on natalizumab who had multiple pre-PML samples, nine patients who developed PML had %CD62L values that in most samples fell in the range of nine matched control patients without PML.
Examination of samples from non-MS patients demonstrated that %CD62L also could vary significantly in various disease states, such as after influenza vaccination and during hospitalization for total knee replacement surgery or methicillin-resistant Staphylococcus aureus infection, the researchers found.
The expression of l-selectin on specific T cells in peripheral blood from patients with relapsing forms of multiple sclerosis (MS) does not reliably predict risk for progressive multifocal leukoencephalopathy (PML) during natalizumab treatment, according to findings from a Biogen-supported study.
These findings are at odds with those of a previously reported preliminary study that used a different analytical technique. Investigators in the earlier preliminary study had found a drop in the percentage of CD4- and CD3-positive T cells expressing l-selectin (CD62L) at least 4 months and often 2 years prior to PML diagnosis and concluded that measuring the percentage of CD4- and CD3-positive T cells expressing l-selectin (%CD62L) “may improve stratification of patients taking natalizumab who are at risk for developing PML,” according to the study from Biogen, which makes natalizumab (Tysabri).
Biogen investigators, led by Linda A. Lieberman, Ph.D., sought to confirm the findings, enhance the reproducibility of the %CD62L assay, “and potentially enable the deployment of %CD62L as a biomarker for PML in a global setting.” However, the investigators did not find a significant difference in %CD62L in cryopreserved peripheral blood mononuclear cells in 104 patients with relapsing forms of multiple sclerosis (MS) on natalizumab who did not develop PML, compared with 21 who developed PML (Neurology. 2015 Dec 30. doi: 10.1212/WNL.0000000000002314).
In the current study, the investigators detected a large range in %CD62L (0.31%-68.4%) in a subset of natalizumab-treated MS patients without PML at two time points at least 6 months apart. Because CD62L and the chemokine receptor CCR7 are coexpressed on CD4- and CD3-positive T cells, they also checked the level of variation in simultaneous measurements of %CD62L and %CCR7 on the same cells at two separate time points in the same patients. They found that %CD62L expression varied substantially, whereas %CCR7 varied little, and the difference between the two was significant, “signifying that %CD62L is not a stable outcome measure,” they wrote.
Dr. Lieberman and her colleagues also confirmed a positive correlation between lymphocyte viability and %CD62L expression, which highlights the “technique-driven variability of the assay” that was used in the preliminary study.
In patient samples collected at least 6 months prior to PML diagnosis, %CD62L did not discriminate significantly between non-PML and active PML (defined as 0-6 months prior to diagnosis). The median %CD62L varied according to the viability of cryopreserved CD4- and CD3-positive T cells. Median %CD62L was no different between non-PML and pre-PML samples with lymphocyte viability greater than 75% (25.9% vs. 26.3%, respectively) but was significantly lower than with non-PML and pre-PML samples with lymphocyte viability less than 75% (10.55% and 5.41%). There was no difference in lymphocyte viability between non-PML and pre-PML samples.
In a case-control comparison of patients on natalizumab who had multiple pre-PML samples, nine patients who developed PML had %CD62L values that in most samples fell in the range of nine matched control patients without PML.
Examination of samples from non-MS patients demonstrated that %CD62L also could vary significantly in various disease states, such as after influenza vaccination and during hospitalization for total knee replacement surgery or methicillin-resistant Staphylococcus aureus infection, the researchers found.
The expression of l-selectin on specific T cells in peripheral blood from patients with relapsing forms of multiple sclerosis (MS) does not reliably predict risk for progressive multifocal leukoencephalopathy (PML) during natalizumab treatment, according to findings from a Biogen-supported study.
These findings are at odds with those of a previously reported preliminary study that used a different analytical technique. Investigators in the earlier preliminary study had found a drop in the percentage of CD4- and CD3-positive T cells expressing l-selectin (CD62L) at least 4 months and often 2 years prior to PML diagnosis and concluded that measuring the percentage of CD4- and CD3-positive T cells expressing l-selectin (%CD62L) “may improve stratification of patients taking natalizumab who are at risk for developing PML,” according to the study from Biogen, which makes natalizumab (Tysabri).
Biogen investigators, led by Linda A. Lieberman, Ph.D., sought to confirm the findings, enhance the reproducibility of the %CD62L assay, “and potentially enable the deployment of %CD62L as a biomarker for PML in a global setting.” However, the investigators did not find a significant difference in %CD62L in cryopreserved peripheral blood mononuclear cells in 104 patients with relapsing forms of multiple sclerosis (MS) on natalizumab who did not develop PML, compared with 21 who developed PML (Neurology. 2015 Dec 30. doi: 10.1212/WNL.0000000000002314).
In the current study, the investigators detected a large range in %CD62L (0.31%-68.4%) in a subset of natalizumab-treated MS patients without PML at two time points at least 6 months apart. Because CD62L and the chemokine receptor CCR7 are coexpressed on CD4- and CD3-positive T cells, they also checked the level of variation in simultaneous measurements of %CD62L and %CCR7 on the same cells at two separate time points in the same patients. They found that %CD62L expression varied substantially, whereas %CCR7 varied little, and the difference between the two was significant, “signifying that %CD62L is not a stable outcome measure,” they wrote.
Dr. Lieberman and her colleagues also confirmed a positive correlation between lymphocyte viability and %CD62L expression, which highlights the “technique-driven variability of the assay” that was used in the preliminary study.
In patient samples collected at least 6 months prior to PML diagnosis, %CD62L did not discriminate significantly between non-PML and active PML (defined as 0-6 months prior to diagnosis). The median %CD62L varied according to the viability of cryopreserved CD4- and CD3-positive T cells. Median %CD62L was no different between non-PML and pre-PML samples with lymphocyte viability greater than 75% (25.9% vs. 26.3%, respectively) but was significantly lower than with non-PML and pre-PML samples with lymphocyte viability less than 75% (10.55% and 5.41%). There was no difference in lymphocyte viability between non-PML and pre-PML samples.
In a case-control comparison of patients on natalizumab who had multiple pre-PML samples, nine patients who developed PML had %CD62L values that in most samples fell in the range of nine matched control patients without PML.
Examination of samples from non-MS patients demonstrated that %CD62L also could vary significantly in various disease states, such as after influenza vaccination and during hospitalization for total knee replacement surgery or methicillin-resistant Staphylococcus aureus infection, the researchers found.
FROM NEUROLOGY
Key clinical point: Measuring %CD62L does not appear to be a viable method for stratifying PML risk in natalizumab-treated MS patients.
Major finding: Median %CD62L was no different between non-PML and pre-PML samples with lymphocyte viability greater than 75% (25.9% vs. 26.3%, respectively) but was significantly lower than with non-PML and pre-PML samples with lymphocyte viability less than 75% (10.55% and 5.41%).
Data source: A retrospective, case-control study of natalizumab-treated patients with relapsing forms of MS from clinical trials and observational studies.
Disclosures: Biogen manufactures natalizumab and sponsored the study. All authors are employees of Biogen.
Rheumatology trends, research, concerns highlighted for 2016
The coming year in rheumatology brings with it a variety of trends and concerns about how rheumatologists can chart the best course for their practices and patients amid mounting fiscal and regulatory pressures.
Questions also arise as to how rheumatology can improve its attractiveness to students and residents in 2016 with the current level of effort in mentoring, outreach, and competition against higher-paying subspecialties.
There’s also high interest and expectations in the new year for studies on systemic sclerosis and microbiome research, as well as questions about what the future holds for intra-articular hyaluronic acid and over-the-counter topical nonsteroidal anti-inflammatory drugs for osteoarthritis (OA).
Rheumatology News editorial advisory board members gave their thoughts on these areas of rheumatology in 2016.
Insurance and reimbursement problems
The changing landscape in insurance plans, brought about largely by the Affordable Care Act, is having a big impact on patients and physicians, particularly in Florida, where more than 1.5 million people signed up for an ACA federal marketplace plan in 2015. Difficulty in accessing and affording care in 2016 figures to be an even greater problem, said Dr. Norman Gaylis, who is in private practice in Aventura, Fla.
In general, many policies are passing an increased burden onto patients in regard to deductibles, copayments, and costs of medications, he said. “That’s putting tremendous stress on practices. I think this is nationwide, where we’re finding that rheumatology patients are not getting access to the drugs for [several] reasons: they’ve become unaffordable, the various pharmaceutical support programs have run out of money, and the amount of work that practices are now performing in trying to get authorization for the patients far exceeds any type of revenue [it] could be generating or should be generating to cover these increased costs. So essentially there’s a reduction in reimbursement and a reduction in revenue going along at the same time.”
Dr. Gaylis noted that there is “tremendous pressure” from all sides to reduce access to rheumatology drugs, which have rising costs. For instance, the cost of a monthly supply of generic celebrex in his practice’s area is on average $120-$200, “which is almost prohibitive for many of our patients.”
“We’re finding that this year [2015] alone, 20% of patients who are on standard infusion therapy as a routine part of their management of rheumatoid arthritis have basically dropped out,” he said. “If that’s equal across the board, that means a very high number of patients are not getting optimal care.”
The trend for rheumatologists, particularly those in solo practice, to make contracts with fewer insurance companies could accelerate in 2016, Dr. Gaylis said.
Some rheumatologists are beginning to not accept insured patients with coverage from managed care companies or the lower-tier payers, and “that’s a significant trend if it starts evolving because it will create a two-tiered system in that you’ll have the more affluent patient going to one of these practices, and then you’ll have clinics where you’ll have a totally different level of care.” Whether it builds up enough to where rheumatologists begin to develop hybrid concierge practices is a fair question, he said. “It’s very difficult to conceive of a patient paying for both primary care and subspecialist concierge service. But I am starting to see signals where there may well be some integration between concierge primary care and concierge subspecialties.”
Training, mentoring more rheumatologists
Another issue going into 2016 is the lack of mentoring and assistance to medical students and residents to draw them to the subspecialty and keep them there, as well as the viability of rheumatology as an attractive subspecialty. “It’s difficult to see how we can attract medical students and residents to the specialty when the cost of their education leaves them with staggering bills to be paid. You’ve got to be extremely passionate to want to be a rheumatologist,” Dr. Gaylis said.
Dr. Elizabeth Volkmann, clinical instructor in rheumatology at the University of California, Los Angeles, agreed and said she looked forward to seeing how the future of mentoring programs in rheumatology will progress in 2016 and beyond. She noted that the American College of Rheumatology (ACR)/Childhood Arthritis and Rheumatology Research Alliance Mentoring Interest Group (AMIGO), a career-mentoring program that serves most fellows and many junior faculty in pediatric rheumatology across the United States and Canada, recently reported success in establishing mentor contact, suitability of mentor-mentee pairing, as well as benefit with respect to career development, scholarship, and work-life balance, and was especially useful to fellows, compared with junior faculty (Arthritis Care Res. 2015 Sep 28. doi: 10.1002/acr.22732).
Dr. Volkmann expressed interest in seeing how the ACR’s Choose Rheumatology! mentorship program is performing. The program seeks to pair students and residents with rheumatologist mentors who will offer advice and help to guide them. She also pointed to the European League Against Rheumatism’s working group for young rheumatologists, the Emerging EULAR Network (EMEUNET), which seeks to promote the educational, research, and mentoring needs of young clinicians and researchers in rheumatology in Europe. as a potential model for the ACR to use in the United States.
Some of the conference-based resources available to rheumatology fellows include the ACR’s 2016 State-of-the-Art Clinical Symposium, which provides a presymposium course specifically for fellows and has sessions on choosing career paths, and the Rheumatology Research Workshop, which targets rheumatologists interested in pursuing an academic research career. Fellows-in-training travel scholarships are available for both conferences.
New systemic sclerosis and microbiome research
Many new studies in systemic sclerosis will build on results obtained in earlier-phase trials or unanswered questions arising out of treatment comparison studies. “It is a very exciting time in the world of scleroderma,” said Dr. Virginia Steen, professor of medicine at Georgetown University, Washington.
At least four new trials are studying treatments for skin manifestations of systemic sclerosis, noted Dr. Steen. In patients with diffuse cutaneous systemic sclerosis, the phase II ASSET study is testing abatacept (Orencia) against placebo and another phase II study is testing riociguat (Adempas). Roche has started enrolling patients for a phase III trial of tocilizumab (Actemra) on the heels of positive findings from its phase II study. Dr. Steen and colleagues at Johns Hopkins University are also finishing up a pilot study of the effects of intravenous immunoglobulin (Privigen) on skin disease in systemic sclerosis and should have results ready for 2016.
Two additional trials will be investigating treatments for interstitial lung disease associated with systemic sclerosis: the Scleroderma Lung Study III, testing the use of mycophenolate mofetil in all patients with the addition of pirfenidone (Esbriet) or placebo, and a separate phase III study of nintedanib (Ofev) vs. placebo that just began enrolling patients.
There are also several trials of add-on therapies, including topical nitroglycerin for Raynaud’s phenomenon or riociguat for digital ulcers, and another that is testing autologous adipose–derived regenerative cells for the treatment of hand dysfunction.
In addition to these trials now underway, the expected 2016 publication of the validation of the Combined Response Index for Systemic Sclerosis will hopefully “lead to real movement forward in the treatment of systemic sclerosis,” said Dr. Daniel E. Furst, the Carl Pearson Professor of Medicine at University of California, Los Angeles.
Further examination of the Wnt signaling pathway in systemic sclerosis should also bring better insights into the disease’s pathogenesis and potential for treatment, Dr. Furst noted, as recent experimental results have shown that its activation induces fibroblast activation with subsequent myofibroblast differentiation and excessive collagen release. Small-molecule inhibitors of Wnt signaling in early clinical trials have shown promising results.
Dr. Furst and Dr. Volkmann said they also hope for studies describing better and more specific data regarding the microbiome in rheumatic disease, especially systemic sclerosis and rheumatoid arthritis, both of which have microbiome data linked with clinically meaningful outcomes (Nat Med. 2015 Aug;21[8]:895-905).
An important unanswered question, Dr. Volkmann said, is whether differences found in GI microbial composition between diseases and between different disease subtypes are clinically meaningful.
OA treatments: AAOS guidelines, OTC topical NSAIDs
The repercussions of the American Academy of Orthopaedic Surgeons 2013 clinical practice guideline’s statement on intra-articular hyaluronic acid treatment of knee OA will continue to be felt in 2016, according to Dr. Roy D. Altman, professor emeritus of medicine at University of California, Los Angeles.
The AAOS took a different stance from all other recent treatment guidelines for knee OA by stating: “Intra-articular hyaluronic acid is no longer recommended as a method of treatment for patients with symptomatic osteoarthritis of the knee.” The AAOS’s recommendation didn’t create much confusion with physicians and patients because its use continues to increase, but instead it has contributed to “a plethora of contradictory publications and increasing resistance on coverage by insurance carriers,” Dr. Altman said.
Another unresolved issue in OA treatment is “the resistance of the FDA to approve over-the-counter topical NSAIDs,” Dr. Altman said. The FDA requires a new drug application for OTC topical NSAIDs demonstrating efficacy and safety, “as if they were completely new,” when the safety exceeds presently approved OTC oral NSAIDs and has already been shown for prescription topical NSAIDs, he said.
The coming year in rheumatology brings with it a variety of trends and concerns about how rheumatologists can chart the best course for their practices and patients amid mounting fiscal and regulatory pressures.
Questions also arise as to how rheumatology can improve its attractiveness to students and residents in 2016 with the current level of effort in mentoring, outreach, and competition against higher-paying subspecialties.
There’s also high interest and expectations in the new year for studies on systemic sclerosis and microbiome research, as well as questions about what the future holds for intra-articular hyaluronic acid and over-the-counter topical nonsteroidal anti-inflammatory drugs for osteoarthritis (OA).
Rheumatology News editorial advisory board members gave their thoughts on these areas of rheumatology in 2016.
Insurance and reimbursement problems
The changing landscape in insurance plans, brought about largely by the Affordable Care Act, is having a big impact on patients and physicians, particularly in Florida, where more than 1.5 million people signed up for an ACA federal marketplace plan in 2015. Difficulty in accessing and affording care in 2016 figures to be an even greater problem, said Dr. Norman Gaylis, who is in private practice in Aventura, Fla.
In general, many policies are passing an increased burden onto patients in regard to deductibles, copayments, and costs of medications, he said. “That’s putting tremendous stress on practices. I think this is nationwide, where we’re finding that rheumatology patients are not getting access to the drugs for [several] reasons: they’ve become unaffordable, the various pharmaceutical support programs have run out of money, and the amount of work that practices are now performing in trying to get authorization for the patients far exceeds any type of revenue [it] could be generating or should be generating to cover these increased costs. So essentially there’s a reduction in reimbursement and a reduction in revenue going along at the same time.”
Dr. Gaylis noted that there is “tremendous pressure” from all sides to reduce access to rheumatology drugs, which have rising costs. For instance, the cost of a monthly supply of generic celebrex in his practice’s area is on average $120-$200, “which is almost prohibitive for many of our patients.”
“We’re finding that this year [2015] alone, 20% of patients who are on standard infusion therapy as a routine part of their management of rheumatoid arthritis have basically dropped out,” he said. “If that’s equal across the board, that means a very high number of patients are not getting optimal care.”
The trend for rheumatologists, particularly those in solo practice, to make contracts with fewer insurance companies could accelerate in 2016, Dr. Gaylis said.
Some rheumatologists are beginning to not accept insured patients with coverage from managed care companies or the lower-tier payers, and “that’s a significant trend if it starts evolving because it will create a two-tiered system in that you’ll have the more affluent patient going to one of these practices, and then you’ll have clinics where you’ll have a totally different level of care.” Whether it builds up enough to where rheumatologists begin to develop hybrid concierge practices is a fair question, he said. “It’s very difficult to conceive of a patient paying for both primary care and subspecialist concierge service. But I am starting to see signals where there may well be some integration between concierge primary care and concierge subspecialties.”
Training, mentoring more rheumatologists
Another issue going into 2016 is the lack of mentoring and assistance to medical students and residents to draw them to the subspecialty and keep them there, as well as the viability of rheumatology as an attractive subspecialty. “It’s difficult to see how we can attract medical students and residents to the specialty when the cost of their education leaves them with staggering bills to be paid. You’ve got to be extremely passionate to want to be a rheumatologist,” Dr. Gaylis said.
Dr. Elizabeth Volkmann, clinical instructor in rheumatology at the University of California, Los Angeles, agreed and said she looked forward to seeing how the future of mentoring programs in rheumatology will progress in 2016 and beyond. She noted that the American College of Rheumatology (ACR)/Childhood Arthritis and Rheumatology Research Alliance Mentoring Interest Group (AMIGO), a career-mentoring program that serves most fellows and many junior faculty in pediatric rheumatology across the United States and Canada, recently reported success in establishing mentor contact, suitability of mentor-mentee pairing, as well as benefit with respect to career development, scholarship, and work-life balance, and was especially useful to fellows, compared with junior faculty (Arthritis Care Res. 2015 Sep 28. doi: 10.1002/acr.22732).
Dr. Volkmann expressed interest in seeing how the ACR’s Choose Rheumatology! mentorship program is performing. The program seeks to pair students and residents with rheumatologist mentors who will offer advice and help to guide them. She also pointed to the European League Against Rheumatism’s working group for young rheumatologists, the Emerging EULAR Network (EMEUNET), which seeks to promote the educational, research, and mentoring needs of young clinicians and researchers in rheumatology in Europe. as a potential model for the ACR to use in the United States.
Some of the conference-based resources available to rheumatology fellows include the ACR’s 2016 State-of-the-Art Clinical Symposium, which provides a presymposium course specifically for fellows and has sessions on choosing career paths, and the Rheumatology Research Workshop, which targets rheumatologists interested in pursuing an academic research career. Fellows-in-training travel scholarships are available for both conferences.
New systemic sclerosis and microbiome research
Many new studies in systemic sclerosis will build on results obtained in earlier-phase trials or unanswered questions arising out of treatment comparison studies. “It is a very exciting time in the world of scleroderma,” said Dr. Virginia Steen, professor of medicine at Georgetown University, Washington.
At least four new trials are studying treatments for skin manifestations of systemic sclerosis, noted Dr. Steen. In patients with diffuse cutaneous systemic sclerosis, the phase II ASSET study is testing abatacept (Orencia) against placebo and another phase II study is testing riociguat (Adempas). Roche has started enrolling patients for a phase III trial of tocilizumab (Actemra) on the heels of positive findings from its phase II study. Dr. Steen and colleagues at Johns Hopkins University are also finishing up a pilot study of the effects of intravenous immunoglobulin (Privigen) on skin disease in systemic sclerosis and should have results ready for 2016.
Two additional trials will be investigating treatments for interstitial lung disease associated with systemic sclerosis: the Scleroderma Lung Study III, testing the use of mycophenolate mofetil in all patients with the addition of pirfenidone (Esbriet) or placebo, and a separate phase III study of nintedanib (Ofev) vs. placebo that just began enrolling patients.
There are also several trials of add-on therapies, including topical nitroglycerin for Raynaud’s phenomenon or riociguat for digital ulcers, and another that is testing autologous adipose–derived regenerative cells for the treatment of hand dysfunction.
In addition to these trials now underway, the expected 2016 publication of the validation of the Combined Response Index for Systemic Sclerosis will hopefully “lead to real movement forward in the treatment of systemic sclerosis,” said Dr. Daniel E. Furst, the Carl Pearson Professor of Medicine at University of California, Los Angeles.
Further examination of the Wnt signaling pathway in systemic sclerosis should also bring better insights into the disease’s pathogenesis and potential for treatment, Dr. Furst noted, as recent experimental results have shown that its activation induces fibroblast activation with subsequent myofibroblast differentiation and excessive collagen release. Small-molecule inhibitors of Wnt signaling in early clinical trials have shown promising results.
Dr. Furst and Dr. Volkmann said they also hope for studies describing better and more specific data regarding the microbiome in rheumatic disease, especially systemic sclerosis and rheumatoid arthritis, both of which have microbiome data linked with clinically meaningful outcomes (Nat Med. 2015 Aug;21[8]:895-905).
An important unanswered question, Dr. Volkmann said, is whether differences found in GI microbial composition between diseases and between different disease subtypes are clinically meaningful.
OA treatments: AAOS guidelines, OTC topical NSAIDs
The repercussions of the American Academy of Orthopaedic Surgeons 2013 clinical practice guideline’s statement on intra-articular hyaluronic acid treatment of knee OA will continue to be felt in 2016, according to Dr. Roy D. Altman, professor emeritus of medicine at University of California, Los Angeles.
The AAOS took a different stance from all other recent treatment guidelines for knee OA by stating: “Intra-articular hyaluronic acid is no longer recommended as a method of treatment for patients with symptomatic osteoarthritis of the knee.” The AAOS’s recommendation didn’t create much confusion with physicians and patients because its use continues to increase, but instead it has contributed to “a plethora of contradictory publications and increasing resistance on coverage by insurance carriers,” Dr. Altman said.
Another unresolved issue in OA treatment is “the resistance of the FDA to approve over-the-counter topical NSAIDs,” Dr. Altman said. The FDA requires a new drug application for OTC topical NSAIDs demonstrating efficacy and safety, “as if they were completely new,” when the safety exceeds presently approved OTC oral NSAIDs and has already been shown for prescription topical NSAIDs, he said.
The coming year in rheumatology brings with it a variety of trends and concerns about how rheumatologists can chart the best course for their practices and patients amid mounting fiscal and regulatory pressures.
Questions also arise as to how rheumatology can improve its attractiveness to students and residents in 2016 with the current level of effort in mentoring, outreach, and competition against higher-paying subspecialties.
There’s also high interest and expectations in the new year for studies on systemic sclerosis and microbiome research, as well as questions about what the future holds for intra-articular hyaluronic acid and over-the-counter topical nonsteroidal anti-inflammatory drugs for osteoarthritis (OA).
Rheumatology News editorial advisory board members gave their thoughts on these areas of rheumatology in 2016.
Insurance and reimbursement problems
The changing landscape in insurance plans, brought about largely by the Affordable Care Act, is having a big impact on patients and physicians, particularly in Florida, where more than 1.5 million people signed up for an ACA federal marketplace plan in 2015. Difficulty in accessing and affording care in 2016 figures to be an even greater problem, said Dr. Norman Gaylis, who is in private practice in Aventura, Fla.
In general, many policies are passing an increased burden onto patients in regard to deductibles, copayments, and costs of medications, he said. “That’s putting tremendous stress on practices. I think this is nationwide, where we’re finding that rheumatology patients are not getting access to the drugs for [several] reasons: they’ve become unaffordable, the various pharmaceutical support programs have run out of money, and the amount of work that practices are now performing in trying to get authorization for the patients far exceeds any type of revenue [it] could be generating or should be generating to cover these increased costs. So essentially there’s a reduction in reimbursement and a reduction in revenue going along at the same time.”
Dr. Gaylis noted that there is “tremendous pressure” from all sides to reduce access to rheumatology drugs, which have rising costs. For instance, the cost of a monthly supply of generic celebrex in his practice’s area is on average $120-$200, “which is almost prohibitive for many of our patients.”
“We’re finding that this year [2015] alone, 20% of patients who are on standard infusion therapy as a routine part of their management of rheumatoid arthritis have basically dropped out,” he said. “If that’s equal across the board, that means a very high number of patients are not getting optimal care.”
The trend for rheumatologists, particularly those in solo practice, to make contracts with fewer insurance companies could accelerate in 2016, Dr. Gaylis said.
Some rheumatologists are beginning to not accept insured patients with coverage from managed care companies or the lower-tier payers, and “that’s a significant trend if it starts evolving because it will create a two-tiered system in that you’ll have the more affluent patient going to one of these practices, and then you’ll have clinics where you’ll have a totally different level of care.” Whether it builds up enough to where rheumatologists begin to develop hybrid concierge practices is a fair question, he said. “It’s very difficult to conceive of a patient paying for both primary care and subspecialist concierge service. But I am starting to see signals where there may well be some integration between concierge primary care and concierge subspecialties.”
Training, mentoring more rheumatologists
Another issue going into 2016 is the lack of mentoring and assistance to medical students and residents to draw them to the subspecialty and keep them there, as well as the viability of rheumatology as an attractive subspecialty. “It’s difficult to see how we can attract medical students and residents to the specialty when the cost of their education leaves them with staggering bills to be paid. You’ve got to be extremely passionate to want to be a rheumatologist,” Dr. Gaylis said.
Dr. Elizabeth Volkmann, clinical instructor in rheumatology at the University of California, Los Angeles, agreed and said she looked forward to seeing how the future of mentoring programs in rheumatology will progress in 2016 and beyond. She noted that the American College of Rheumatology (ACR)/Childhood Arthritis and Rheumatology Research Alliance Mentoring Interest Group (AMIGO), a career-mentoring program that serves most fellows and many junior faculty in pediatric rheumatology across the United States and Canada, recently reported success in establishing mentor contact, suitability of mentor-mentee pairing, as well as benefit with respect to career development, scholarship, and work-life balance, and was especially useful to fellows, compared with junior faculty (Arthritis Care Res. 2015 Sep 28. doi: 10.1002/acr.22732).
Dr. Volkmann expressed interest in seeing how the ACR’s Choose Rheumatology! mentorship program is performing. The program seeks to pair students and residents with rheumatologist mentors who will offer advice and help to guide them. She also pointed to the European League Against Rheumatism’s working group for young rheumatologists, the Emerging EULAR Network (EMEUNET), which seeks to promote the educational, research, and mentoring needs of young clinicians and researchers in rheumatology in Europe. as a potential model for the ACR to use in the United States.
Some of the conference-based resources available to rheumatology fellows include the ACR’s 2016 State-of-the-Art Clinical Symposium, which provides a presymposium course specifically for fellows and has sessions on choosing career paths, and the Rheumatology Research Workshop, which targets rheumatologists interested in pursuing an academic research career. Fellows-in-training travel scholarships are available for both conferences.
New systemic sclerosis and microbiome research
Many new studies in systemic sclerosis will build on results obtained in earlier-phase trials or unanswered questions arising out of treatment comparison studies. “It is a very exciting time in the world of scleroderma,” said Dr. Virginia Steen, professor of medicine at Georgetown University, Washington.
At least four new trials are studying treatments for skin manifestations of systemic sclerosis, noted Dr. Steen. In patients with diffuse cutaneous systemic sclerosis, the phase II ASSET study is testing abatacept (Orencia) against placebo and another phase II study is testing riociguat (Adempas). Roche has started enrolling patients for a phase III trial of tocilizumab (Actemra) on the heels of positive findings from its phase II study. Dr. Steen and colleagues at Johns Hopkins University are also finishing up a pilot study of the effects of intravenous immunoglobulin (Privigen) on skin disease in systemic sclerosis and should have results ready for 2016.
Two additional trials will be investigating treatments for interstitial lung disease associated with systemic sclerosis: the Scleroderma Lung Study III, testing the use of mycophenolate mofetil in all patients with the addition of pirfenidone (Esbriet) or placebo, and a separate phase III study of nintedanib (Ofev) vs. placebo that just began enrolling patients.
There are also several trials of add-on therapies, including topical nitroglycerin for Raynaud’s phenomenon or riociguat for digital ulcers, and another that is testing autologous adipose–derived regenerative cells for the treatment of hand dysfunction.
In addition to these trials now underway, the expected 2016 publication of the validation of the Combined Response Index for Systemic Sclerosis will hopefully “lead to real movement forward in the treatment of systemic sclerosis,” said Dr. Daniel E. Furst, the Carl Pearson Professor of Medicine at University of California, Los Angeles.
Further examination of the Wnt signaling pathway in systemic sclerosis should also bring better insights into the disease’s pathogenesis and potential for treatment, Dr. Furst noted, as recent experimental results have shown that its activation induces fibroblast activation with subsequent myofibroblast differentiation and excessive collagen release. Small-molecule inhibitors of Wnt signaling in early clinical trials have shown promising results.
Dr. Furst and Dr. Volkmann said they also hope for studies describing better and more specific data regarding the microbiome in rheumatic disease, especially systemic sclerosis and rheumatoid arthritis, both of which have microbiome data linked with clinically meaningful outcomes (Nat Med. 2015 Aug;21[8]:895-905).
An important unanswered question, Dr. Volkmann said, is whether differences found in GI microbial composition between diseases and between different disease subtypes are clinically meaningful.
OA treatments: AAOS guidelines, OTC topical NSAIDs
The repercussions of the American Academy of Orthopaedic Surgeons 2013 clinical practice guideline’s statement on intra-articular hyaluronic acid treatment of knee OA will continue to be felt in 2016, according to Dr. Roy D. Altman, professor emeritus of medicine at University of California, Los Angeles.
The AAOS took a different stance from all other recent treatment guidelines for knee OA by stating: “Intra-articular hyaluronic acid is no longer recommended as a method of treatment for patients with symptomatic osteoarthritis of the knee.” The AAOS’s recommendation didn’t create much confusion with physicians and patients because its use continues to increase, but instead it has contributed to “a plethora of contradictory publications and increasing resistance on coverage by insurance carriers,” Dr. Altman said.
Another unresolved issue in OA treatment is “the resistance of the FDA to approve over-the-counter topical NSAIDs,” Dr. Altman said. The FDA requires a new drug application for OTC topical NSAIDs demonstrating efficacy and safety, “as if they were completely new,” when the safety exceeds presently approved OTC oral NSAIDs and has already been shown for prescription topical NSAIDs, he said.
Evidence points to early brain cell death as catalyst for MS inflammation, demyelination
An adaptive autoimmune response against myelin that occurs late after an initial loss of oligodendrocytes in a new mouse model offers evidence in support of the “inside-out” hypothesis for multiple sclerosis pathogenesis in which “certain forms of MS may be caused by primary oligodendrocyte loss or myelin damage that secondarily leads to activation of the permissive adaptive immune system and CNS inflammation,” according to Maria Traka, Ph.D., of the University of Chicago. The report was published Dec. 14 in Nature Neuroscience.
“To our knowledge, this is the first experimental evidence to support the hypothesis that oligodendrocyte loss or myelin degeneration triggers myelin autoimmunity and initiates inflammation and tissue damage in the CNS during MS,” wrote Dr. Traka and her colleagues.
The new mouse model that the investigators used to support the hypothesis undergoes a genetically induced loss of oligodendrocytes and demyelination from which it recovers, but then later in life develops an infiltration of CD4-positive T cells into the CNS that causes a secondary, fatal demyelinating disease that occurs with axonal loss, CNS inflammation, and the presence of myelin oligodendrocyte glycoprotein (MOG)–specific T cells in peripheral lymphoid organs. The investigators found that the transfer of these MOG-specific T cells could induce mild neurological symptoms and inflammatory CNS white matter lesions in recipient, naive mice and that they could block the progression of late-onset disease symptoms and induce immune tolerance to MOG by injecting MOG-specific T cells coupled to nanoparticles at just the right point in time prior to late-onset disease. The investigators concluded that this disease process is “likely to be a T-cell mediated autoimmune response,” consistent with MS.
The researchers suggested that the “development of CNS autoimmunity after oligodendrocyte loss could be a slow process ... [which] might explain the difficulty in observing a correlation between oligodendrocyte loss, whether induced by viral cytotoxicity or other environmental factors, and a myelin immune response in patients with MS.”
A news release from Northwestern University, one of the institutions involved in the research, said that the nanoparticle technology used in the experiments has been licensed to Cour Pharmaceutical Development Company to develop it for human trials in autoimmune disease.
Read the full paper at Nat Neurosci. 2015 Dec 14. doi: 10.1038/nn.4193.
An adaptive autoimmune response against myelin that occurs late after an initial loss of oligodendrocytes in a new mouse model offers evidence in support of the “inside-out” hypothesis for multiple sclerosis pathogenesis in which “certain forms of MS may be caused by primary oligodendrocyte loss or myelin damage that secondarily leads to activation of the permissive adaptive immune system and CNS inflammation,” according to Maria Traka, Ph.D., of the University of Chicago. The report was published Dec. 14 in Nature Neuroscience.
“To our knowledge, this is the first experimental evidence to support the hypothesis that oligodendrocyte loss or myelin degeneration triggers myelin autoimmunity and initiates inflammation and tissue damage in the CNS during MS,” wrote Dr. Traka and her colleagues.
The new mouse model that the investigators used to support the hypothesis undergoes a genetically induced loss of oligodendrocytes and demyelination from which it recovers, but then later in life develops an infiltration of CD4-positive T cells into the CNS that causes a secondary, fatal demyelinating disease that occurs with axonal loss, CNS inflammation, and the presence of myelin oligodendrocyte glycoprotein (MOG)–specific T cells in peripheral lymphoid organs. The investigators found that the transfer of these MOG-specific T cells could induce mild neurological symptoms and inflammatory CNS white matter lesions in recipient, naive mice and that they could block the progression of late-onset disease symptoms and induce immune tolerance to MOG by injecting MOG-specific T cells coupled to nanoparticles at just the right point in time prior to late-onset disease. The investigators concluded that this disease process is “likely to be a T-cell mediated autoimmune response,” consistent with MS.
The researchers suggested that the “development of CNS autoimmunity after oligodendrocyte loss could be a slow process ... [which] might explain the difficulty in observing a correlation between oligodendrocyte loss, whether induced by viral cytotoxicity or other environmental factors, and a myelin immune response in patients with MS.”
A news release from Northwestern University, one of the institutions involved in the research, said that the nanoparticle technology used in the experiments has been licensed to Cour Pharmaceutical Development Company to develop it for human trials in autoimmune disease.
Read the full paper at Nat Neurosci. 2015 Dec 14. doi: 10.1038/nn.4193.
An adaptive autoimmune response against myelin that occurs late after an initial loss of oligodendrocytes in a new mouse model offers evidence in support of the “inside-out” hypothesis for multiple sclerosis pathogenesis in which “certain forms of MS may be caused by primary oligodendrocyte loss or myelin damage that secondarily leads to activation of the permissive adaptive immune system and CNS inflammation,” according to Maria Traka, Ph.D., of the University of Chicago. The report was published Dec. 14 in Nature Neuroscience.
“To our knowledge, this is the first experimental evidence to support the hypothesis that oligodendrocyte loss or myelin degeneration triggers myelin autoimmunity and initiates inflammation and tissue damage in the CNS during MS,” wrote Dr. Traka and her colleagues.
The new mouse model that the investigators used to support the hypothesis undergoes a genetically induced loss of oligodendrocytes and demyelination from which it recovers, but then later in life develops an infiltration of CD4-positive T cells into the CNS that causes a secondary, fatal demyelinating disease that occurs with axonal loss, CNS inflammation, and the presence of myelin oligodendrocyte glycoprotein (MOG)–specific T cells in peripheral lymphoid organs. The investigators found that the transfer of these MOG-specific T cells could induce mild neurological symptoms and inflammatory CNS white matter lesions in recipient, naive mice and that they could block the progression of late-onset disease symptoms and induce immune tolerance to MOG by injecting MOG-specific T cells coupled to nanoparticles at just the right point in time prior to late-onset disease. The investigators concluded that this disease process is “likely to be a T-cell mediated autoimmune response,” consistent with MS.
The researchers suggested that the “development of CNS autoimmunity after oligodendrocyte loss could be a slow process ... [which] might explain the difficulty in observing a correlation between oligodendrocyte loss, whether induced by viral cytotoxicity or other environmental factors, and a myelin immune response in patients with MS.”
A news release from Northwestern University, one of the institutions involved in the research, said that the nanoparticle technology used in the experiments has been licensed to Cour Pharmaceutical Development Company to develop it for human trials in autoimmune disease.
Read the full paper at Nat Neurosci. 2015 Dec 14. doi: 10.1038/nn.4193.
FROM NATURE NEUROSCIENCE