User login
Pediatric questionnaire sorts out psychosocial effects of skin conditions
MINNEAPOLIS – A new screening tool may help dermatologists address the psychosocial issues relating to appearance and body image in children and adolescents.
The Pediatric Dermatology Psychosocial Screen (PDPS), is being developed as a standardized tool to evaluate psychosocial stress related to birthmarks, skin diseases, and conditions affecting pigmentation or hair growth. Elizabeth Tocci, MD, and her colleagues, who have been involved with the development of the PDPS, envision it as a useful tool to provide support for pediatric dermatology patients and to help dermatologists decide when mental health consults are warranted in their pediatric patients.
Dr. Tocci, a resident in dermatology at Roger Williams Medical Center, Providence, R.I., and her colleagues described the tool and initial testing results in a poster session at the annual meeting of the Society for Pediatric Dermatology.
The PDPS is a refinement of a pilot survey, created by the coauthors in consultation with experts in neurodermatitis and body dysmorphic disorder (BDD). Following preliminary validity analysis of the pilot questionnaire, a revised PDPS was administered to 105 children, aged 8-19 years, who were patients at a pediatric dermatology clinic. In addition to completing the PDPS, they also filled out psychological questionnaires that assessed for depression, self-esteem, and social problems.
The PDPS asks general questions about the skin diagnosis and any treatments the patient may have used, such as over-the-counter products, prescription medications, and procedures, as well as the use of makeup. In addition, the PDPS asks what social and psychological supports or online resources the patient might have tried, including support groups and appointments with school counselors or mental health providers.
Psychosocial aspects of the skin condition are explored by asking how upset patients are about social sequelae of having a visible skin condition, and whether they are asked about the condition and whether they are made fun of, stared at, or avoided because of the condition. Other questions pertain to whether they notice others’ skin, are hyperobservant of their own skin condition, or feel their popularity and their willingness to date are affected by their skin condition.
Respondent resiliency as it relates to the skin condition is explored by asking whether the respondent found it difficult to move on after a negative social interaction related to the skin condition, and how long the feeling of upset persisted after a negative incident.
Of the 105 surveys, 87 were complete enough to allow analysis. The analysis showed that higher self-reported resiliency was associated with higher positive scores on other psychosocial factors, such as self-esteem, body image, fewer negative and more positive social supports, less self-consciousness, less negative affect, and less BDD. “Self-reported resilience was a significant predictor and determinant of all the psychosocial factors measured,” Dr. Tocci and her associates wrote.
Results indicate that the PDPS is useful to evaluate children and teens in a busy clinic setting, and is “an excellent self-reporting tool for measuring resilience versus psychosocial distress,” they added.
The test is not yet available; the next steps include refining the length and wording of the PDPS, with further validation and testing.
Dr. Tocci and her collaborators reported no conflicts of interest.
On Twitter @karioakes
MINNEAPOLIS – A new screening tool may help dermatologists address the psychosocial issues relating to appearance and body image in children and adolescents.
The Pediatric Dermatology Psychosocial Screen (PDPS), is being developed as a standardized tool to evaluate psychosocial stress related to birthmarks, skin diseases, and conditions affecting pigmentation or hair growth. Elizabeth Tocci, MD, and her colleagues, who have been involved with the development of the PDPS, envision it as a useful tool to provide support for pediatric dermatology patients and to help dermatologists decide when mental health consults are warranted in their pediatric patients.
Dr. Tocci, a resident in dermatology at Roger Williams Medical Center, Providence, R.I., and her colleagues described the tool and initial testing results in a poster session at the annual meeting of the Society for Pediatric Dermatology.
The PDPS is a refinement of a pilot survey, created by the coauthors in consultation with experts in neurodermatitis and body dysmorphic disorder (BDD). Following preliminary validity analysis of the pilot questionnaire, a revised PDPS was administered to 105 children, aged 8-19 years, who were patients at a pediatric dermatology clinic. In addition to completing the PDPS, they also filled out psychological questionnaires that assessed for depression, self-esteem, and social problems.
The PDPS asks general questions about the skin diagnosis and any treatments the patient may have used, such as over-the-counter products, prescription medications, and procedures, as well as the use of makeup. In addition, the PDPS asks what social and psychological supports or online resources the patient might have tried, including support groups and appointments with school counselors or mental health providers.
Psychosocial aspects of the skin condition are explored by asking how upset patients are about social sequelae of having a visible skin condition, and whether they are asked about the condition and whether they are made fun of, stared at, or avoided because of the condition. Other questions pertain to whether they notice others’ skin, are hyperobservant of their own skin condition, or feel their popularity and their willingness to date are affected by their skin condition.
Respondent resiliency as it relates to the skin condition is explored by asking whether the respondent found it difficult to move on after a negative social interaction related to the skin condition, and how long the feeling of upset persisted after a negative incident.
Of the 105 surveys, 87 were complete enough to allow analysis. The analysis showed that higher self-reported resiliency was associated with higher positive scores on other psychosocial factors, such as self-esteem, body image, fewer negative and more positive social supports, less self-consciousness, less negative affect, and less BDD. “Self-reported resilience was a significant predictor and determinant of all the psychosocial factors measured,” Dr. Tocci and her associates wrote.
Results indicate that the PDPS is useful to evaluate children and teens in a busy clinic setting, and is “an excellent self-reporting tool for measuring resilience versus psychosocial distress,” they added.
The test is not yet available; the next steps include refining the length and wording of the PDPS, with further validation and testing.
Dr. Tocci and her collaborators reported no conflicts of interest.
On Twitter @karioakes
MINNEAPOLIS – A new screening tool may help dermatologists address the psychosocial issues relating to appearance and body image in children and adolescents.
The Pediatric Dermatology Psychosocial Screen (PDPS), is being developed as a standardized tool to evaluate psychosocial stress related to birthmarks, skin diseases, and conditions affecting pigmentation or hair growth. Elizabeth Tocci, MD, and her colleagues, who have been involved with the development of the PDPS, envision it as a useful tool to provide support for pediatric dermatology patients and to help dermatologists decide when mental health consults are warranted in their pediatric patients.
Dr. Tocci, a resident in dermatology at Roger Williams Medical Center, Providence, R.I., and her colleagues described the tool and initial testing results in a poster session at the annual meeting of the Society for Pediatric Dermatology.
The PDPS is a refinement of a pilot survey, created by the coauthors in consultation with experts in neurodermatitis and body dysmorphic disorder (BDD). Following preliminary validity analysis of the pilot questionnaire, a revised PDPS was administered to 105 children, aged 8-19 years, who were patients at a pediatric dermatology clinic. In addition to completing the PDPS, they also filled out psychological questionnaires that assessed for depression, self-esteem, and social problems.
The PDPS asks general questions about the skin diagnosis and any treatments the patient may have used, such as over-the-counter products, prescription medications, and procedures, as well as the use of makeup. In addition, the PDPS asks what social and psychological supports or online resources the patient might have tried, including support groups and appointments with school counselors or mental health providers.
Psychosocial aspects of the skin condition are explored by asking how upset patients are about social sequelae of having a visible skin condition, and whether they are asked about the condition and whether they are made fun of, stared at, or avoided because of the condition. Other questions pertain to whether they notice others’ skin, are hyperobservant of their own skin condition, or feel their popularity and their willingness to date are affected by their skin condition.
Respondent resiliency as it relates to the skin condition is explored by asking whether the respondent found it difficult to move on after a negative social interaction related to the skin condition, and how long the feeling of upset persisted after a negative incident.
Of the 105 surveys, 87 were complete enough to allow analysis. The analysis showed that higher self-reported resiliency was associated with higher positive scores on other psychosocial factors, such as self-esteem, body image, fewer negative and more positive social supports, less self-consciousness, less negative affect, and less BDD. “Self-reported resilience was a significant predictor and determinant of all the psychosocial factors measured,” Dr. Tocci and her associates wrote.
Results indicate that the PDPS is useful to evaluate children and teens in a busy clinic setting, and is “an excellent self-reporting tool for measuring resilience versus psychosocial distress,” they added.
The test is not yet available; the next steps include refining the length and wording of the PDPS, with further validation and testing.
Dr. Tocci and her collaborators reported no conflicts of interest.
On Twitter @karioakes
EXPERT ANALYSIS FROM THE SPD ANNUAL MEETING
Combined OCs remain a good choice for teen acne
MINNEAPOLIS – Whether a young female patient has a refractory flare of inflammatory acne, or has a condition that can predispose to androgen excess, using a hormonal approach can be an effective management tool for controlling adolescent acne.
During a presentation at the annual meeting of the Society for Pediatric Dermatology, Dr. Diane Thiboutot outlined tips and tricks for optimizing hormonal therapy for acne in teens, and referred to the new acne treatment guidelines from the American Academy of Dermatology, which clarify when to treat with hormones, which to choose, and when further testing might be indicated.
The full range of hormonal therapy options for acne can include oral contraceptives, which block ovarian hormone production; antiandrogens such as spironolactone, and the less commonly used flutamide, which blocks the effects of androgen on the skin; and glucocorticoids, which block adrenal production.
The 2016 guidelines recommend oral contraceptives as an effective treatment for inflammatory acne in females (J Am Acad Dermatol. 2016 May;74[5]; 945-973.e33). Combined oral contraceptives (COCs) reduce serum androgens, and reduce free testosterone by increasing sex hormone binding globulin production, thus reducing sebum production. “The only things that really decrease sebum are oral contraceptives in women, and isotretinoin,” said Dr. Thiboutot, professor of dermatology at Penn State University, Hershey.
For most female adolescents with acne, hormonal testing is not indicated. The AAD guidelines recommend laboratory evaluation for younger patients with acne who have clinical signs of androgen excess, such as early onset body odor and axillary and/or pubic hair, accelerated growth, advanced bone age, or early genital maturation. Just obtaining a hand film for bone age and mapping growth against a growth chart can be a good initial screening tool when considering whether to perform hormonal testing, she noted.
For postpubertal females in whom polycystic ovary syndrome (PCOS) or other hyperandrogenic states are suspected, hormonal testing is indicated in the presence of the clinical signs of infrequent menses and infertility, hirsutism, truncal obesity, androgenetic alopecia, polycystic ovaries, or clitoromegaly.
In searching for an endocrine disorder, Dr. Thiboutot recommends checking total and free testosterone, luteinizing hormone/follicle stimulating hormone ratio, 17-hydroxyprogesterone levels, and dehydroepiandrosterone (DHEA-S) levels. These tests should be performed at least 6 weeks after the patient has been off hormonal contraception, and should be done during the menstrual period, or during the week prior to menses, in order to avoid ovulation-related hormonal changes.
Lab findings consistent with congenital adrenal hyperplasia include elevated serum DHEA-S, together with elevated 17-hydroxyprogesterone or testosterone. A PCOS diagnosis can be made in adolescent females if there is clinical or laboratory evidence of hyperandrogenism with concomitant persistent oligomenorrhea.
Acne related to hyperandrogenism may respond well to oral contraceptives, but COCs can also be an effective alternative to repeated courses of isotretinoin and antibiotics, as well as an effective adjunct to topical therapy, Dr. Thiboutot said.
When beginning a patient on oral contraceptives, it’s not necessary to perform a pelvic exam or obtain a Pap smear before initiating the COC, but it is important to obtain a thorough medical history and an accurate blood pressure measurement at the outset, she noted. The World Health Organization (WHO) has established recommendations outlining contraindications to COC use, also identifying populations in whom COCs should be used with caution, and who should be monitored.
Headaches are a condition frequently seen among healthy teens and young women, and one for which the WHO advises caution. There are concerns that women with migraines may be at increased risk of stroke if they take COCs, but the overall risk is low, and the American College of Obstetricians and Gynecologists (ACOG) advises that COCs can be considered for women younger than 35 with migraines if they have no focal neurologic signs, are nonsmokers, and are otherwise healthy, Dr. Thiboutot added.
A large Food and Drug Administration–sponsored retrospective cohort study examined the risk of venous thromboembolism in contraceptive users. In April 2012, the FDA concluded that though the risk of blood clots may be higher for those on hormonal contraception methods than for those who are not using them, the risk of blood clots during pregnancy and the postpartum period is higher than the thromboembolism risk for contraceptive users.
Regarding the potential for antibiotics to reduce contraceptive efficacy, Dr. Thiboutot said,“it’s okay to use oral contraceptives with antibiotics. There’s a lot of misunderstanding about antibiotics and combined oral contraceptives.” She cited an ACOG practice bulletin that reported that only rifampin has been shown to reduce serum steroid levels when taken with oral contraceptives (Obstet Gynecol. 2006 Jun;107[6]:1453-72).
According to the 2016 AAD guidelines, the use of oral glucocorticoids may be appropriate over the short term when initiating therapy for severe inflammatory acne. “Pharmacokinetic studies have not demonstrated decreased oral contraceptive levels with common antibiotics,” Dr. Thiboutot said.
Spironolactone, according to the new guidelines, is useful for acne in select females. Spironolactone is an androgen receptor and 5a-reductase blocker, and its antiandrogen effects can improve acne. Many patients do well with 25-50 mg twice daily, though breast tenderness and menstrual irregularities are commonly seen side effects, she noted. If a woman taking spironolactone becomes pregnant, there’s a risk of hypospadias for a male fetus.
Though spironolactone carries a boxed warning because of tumorigenicity observed in animal studies, Dr. Thiboutot said that a large Danish study searched for any association between breast, uterine, or ovarian cancers and spironolactone use. Among the 2.3 million women studied, no increased association was seen (Cancer Epidemiol. 2013 Dec;37:870-5).
She also noted that there’s “low usefulness in monitoring potassium levels in young healthy women on spironolactone.” She cited a study that compared 974 healthy young women taking spironolactone with 1,165 women who were not on spironolactone, which found that the hyperkalemia rate of 0.72% among those on spironolactone was equivalent to the 0.76% baseline rate of hyperkalemia in the young, healthy female population (JAMA Dermatol. 2015;151[9];941-944).
Oral corticosteroids for acne, Dr. Thiboutot said, should be reserved to quiet a severe bout of inflammatory acne while standard therapies are being initiated.
She reported being an investigator or a consultant for a number of pharmaceutical companies.
On Twitter @karioakes
MINNEAPOLIS – Whether a young female patient has a refractory flare of inflammatory acne, or has a condition that can predispose to androgen excess, using a hormonal approach can be an effective management tool for controlling adolescent acne.
During a presentation at the annual meeting of the Society for Pediatric Dermatology, Dr. Diane Thiboutot outlined tips and tricks for optimizing hormonal therapy for acne in teens, and referred to the new acne treatment guidelines from the American Academy of Dermatology, which clarify when to treat with hormones, which to choose, and when further testing might be indicated.
The full range of hormonal therapy options for acne can include oral contraceptives, which block ovarian hormone production; antiandrogens such as spironolactone, and the less commonly used flutamide, which blocks the effects of androgen on the skin; and glucocorticoids, which block adrenal production.
The 2016 guidelines recommend oral contraceptives as an effective treatment for inflammatory acne in females (J Am Acad Dermatol. 2016 May;74[5]; 945-973.e33). Combined oral contraceptives (COCs) reduce serum androgens, and reduce free testosterone by increasing sex hormone binding globulin production, thus reducing sebum production. “The only things that really decrease sebum are oral contraceptives in women, and isotretinoin,” said Dr. Thiboutot, professor of dermatology at Penn State University, Hershey.
For most female adolescents with acne, hormonal testing is not indicated. The AAD guidelines recommend laboratory evaluation for younger patients with acne who have clinical signs of androgen excess, such as early onset body odor and axillary and/or pubic hair, accelerated growth, advanced bone age, or early genital maturation. Just obtaining a hand film for bone age and mapping growth against a growth chart can be a good initial screening tool when considering whether to perform hormonal testing, she noted.
For postpubertal females in whom polycystic ovary syndrome (PCOS) or other hyperandrogenic states are suspected, hormonal testing is indicated in the presence of the clinical signs of infrequent menses and infertility, hirsutism, truncal obesity, androgenetic alopecia, polycystic ovaries, or clitoromegaly.
In searching for an endocrine disorder, Dr. Thiboutot recommends checking total and free testosterone, luteinizing hormone/follicle stimulating hormone ratio, 17-hydroxyprogesterone levels, and dehydroepiandrosterone (DHEA-S) levels. These tests should be performed at least 6 weeks after the patient has been off hormonal contraception, and should be done during the menstrual period, or during the week prior to menses, in order to avoid ovulation-related hormonal changes.
Lab findings consistent with congenital adrenal hyperplasia include elevated serum DHEA-S, together with elevated 17-hydroxyprogesterone or testosterone. A PCOS diagnosis can be made in adolescent females if there is clinical or laboratory evidence of hyperandrogenism with concomitant persistent oligomenorrhea.
Acne related to hyperandrogenism may respond well to oral contraceptives, but COCs can also be an effective alternative to repeated courses of isotretinoin and antibiotics, as well as an effective adjunct to topical therapy, Dr. Thiboutot said.
When beginning a patient on oral contraceptives, it’s not necessary to perform a pelvic exam or obtain a Pap smear before initiating the COC, but it is important to obtain a thorough medical history and an accurate blood pressure measurement at the outset, she noted. The World Health Organization (WHO) has established recommendations outlining contraindications to COC use, also identifying populations in whom COCs should be used with caution, and who should be monitored.
Headaches are a condition frequently seen among healthy teens and young women, and one for which the WHO advises caution. There are concerns that women with migraines may be at increased risk of stroke if they take COCs, but the overall risk is low, and the American College of Obstetricians and Gynecologists (ACOG) advises that COCs can be considered for women younger than 35 with migraines if they have no focal neurologic signs, are nonsmokers, and are otherwise healthy, Dr. Thiboutot added.
A large Food and Drug Administration–sponsored retrospective cohort study examined the risk of venous thromboembolism in contraceptive users. In April 2012, the FDA concluded that though the risk of blood clots may be higher for those on hormonal contraception methods than for those who are not using them, the risk of blood clots during pregnancy and the postpartum period is higher than the thromboembolism risk for contraceptive users.
Regarding the potential for antibiotics to reduce contraceptive efficacy, Dr. Thiboutot said,“it’s okay to use oral contraceptives with antibiotics. There’s a lot of misunderstanding about antibiotics and combined oral contraceptives.” She cited an ACOG practice bulletin that reported that only rifampin has been shown to reduce serum steroid levels when taken with oral contraceptives (Obstet Gynecol. 2006 Jun;107[6]:1453-72).
According to the 2016 AAD guidelines, the use of oral glucocorticoids may be appropriate over the short term when initiating therapy for severe inflammatory acne. “Pharmacokinetic studies have not demonstrated decreased oral contraceptive levels with common antibiotics,” Dr. Thiboutot said.
Spironolactone, according to the new guidelines, is useful for acne in select females. Spironolactone is an androgen receptor and 5a-reductase blocker, and its antiandrogen effects can improve acne. Many patients do well with 25-50 mg twice daily, though breast tenderness and menstrual irregularities are commonly seen side effects, she noted. If a woman taking spironolactone becomes pregnant, there’s a risk of hypospadias for a male fetus.
Though spironolactone carries a boxed warning because of tumorigenicity observed in animal studies, Dr. Thiboutot said that a large Danish study searched for any association between breast, uterine, or ovarian cancers and spironolactone use. Among the 2.3 million women studied, no increased association was seen (Cancer Epidemiol. 2013 Dec;37:870-5).
She also noted that there’s “low usefulness in monitoring potassium levels in young healthy women on spironolactone.” She cited a study that compared 974 healthy young women taking spironolactone with 1,165 women who were not on spironolactone, which found that the hyperkalemia rate of 0.72% among those on spironolactone was equivalent to the 0.76% baseline rate of hyperkalemia in the young, healthy female population (JAMA Dermatol. 2015;151[9];941-944).
Oral corticosteroids for acne, Dr. Thiboutot said, should be reserved to quiet a severe bout of inflammatory acne while standard therapies are being initiated.
She reported being an investigator or a consultant for a number of pharmaceutical companies.
On Twitter @karioakes
MINNEAPOLIS – Whether a young female patient has a refractory flare of inflammatory acne, or has a condition that can predispose to androgen excess, using a hormonal approach can be an effective management tool for controlling adolescent acne.
During a presentation at the annual meeting of the Society for Pediatric Dermatology, Dr. Diane Thiboutot outlined tips and tricks for optimizing hormonal therapy for acne in teens, and referred to the new acne treatment guidelines from the American Academy of Dermatology, which clarify when to treat with hormones, which to choose, and when further testing might be indicated.
The full range of hormonal therapy options for acne can include oral contraceptives, which block ovarian hormone production; antiandrogens such as spironolactone, and the less commonly used flutamide, which blocks the effects of androgen on the skin; and glucocorticoids, which block adrenal production.
The 2016 guidelines recommend oral contraceptives as an effective treatment for inflammatory acne in females (J Am Acad Dermatol. 2016 May;74[5]; 945-973.e33). Combined oral contraceptives (COCs) reduce serum androgens, and reduce free testosterone by increasing sex hormone binding globulin production, thus reducing sebum production. “The only things that really decrease sebum are oral contraceptives in women, and isotretinoin,” said Dr. Thiboutot, professor of dermatology at Penn State University, Hershey.
For most female adolescents with acne, hormonal testing is not indicated. The AAD guidelines recommend laboratory evaluation for younger patients with acne who have clinical signs of androgen excess, such as early onset body odor and axillary and/or pubic hair, accelerated growth, advanced bone age, or early genital maturation. Just obtaining a hand film for bone age and mapping growth against a growth chart can be a good initial screening tool when considering whether to perform hormonal testing, she noted.
For postpubertal females in whom polycystic ovary syndrome (PCOS) or other hyperandrogenic states are suspected, hormonal testing is indicated in the presence of the clinical signs of infrequent menses and infertility, hirsutism, truncal obesity, androgenetic alopecia, polycystic ovaries, or clitoromegaly.
In searching for an endocrine disorder, Dr. Thiboutot recommends checking total and free testosterone, luteinizing hormone/follicle stimulating hormone ratio, 17-hydroxyprogesterone levels, and dehydroepiandrosterone (DHEA-S) levels. These tests should be performed at least 6 weeks after the patient has been off hormonal contraception, and should be done during the menstrual period, or during the week prior to menses, in order to avoid ovulation-related hormonal changes.
Lab findings consistent with congenital adrenal hyperplasia include elevated serum DHEA-S, together with elevated 17-hydroxyprogesterone or testosterone. A PCOS diagnosis can be made in adolescent females if there is clinical or laboratory evidence of hyperandrogenism with concomitant persistent oligomenorrhea.
Acne related to hyperandrogenism may respond well to oral contraceptives, but COCs can also be an effective alternative to repeated courses of isotretinoin and antibiotics, as well as an effective adjunct to topical therapy, Dr. Thiboutot said.
When beginning a patient on oral contraceptives, it’s not necessary to perform a pelvic exam or obtain a Pap smear before initiating the COC, but it is important to obtain a thorough medical history and an accurate blood pressure measurement at the outset, she noted. The World Health Organization (WHO) has established recommendations outlining contraindications to COC use, also identifying populations in whom COCs should be used with caution, and who should be monitored.
Headaches are a condition frequently seen among healthy teens and young women, and one for which the WHO advises caution. There are concerns that women with migraines may be at increased risk of stroke if they take COCs, but the overall risk is low, and the American College of Obstetricians and Gynecologists (ACOG) advises that COCs can be considered for women younger than 35 with migraines if they have no focal neurologic signs, are nonsmokers, and are otherwise healthy, Dr. Thiboutot added.
A large Food and Drug Administration–sponsored retrospective cohort study examined the risk of venous thromboembolism in contraceptive users. In April 2012, the FDA concluded that though the risk of blood clots may be higher for those on hormonal contraception methods than for those who are not using them, the risk of blood clots during pregnancy and the postpartum period is higher than the thromboembolism risk for contraceptive users.
Regarding the potential for antibiotics to reduce contraceptive efficacy, Dr. Thiboutot said,“it’s okay to use oral contraceptives with antibiotics. There’s a lot of misunderstanding about antibiotics and combined oral contraceptives.” She cited an ACOG practice bulletin that reported that only rifampin has been shown to reduce serum steroid levels when taken with oral contraceptives (Obstet Gynecol. 2006 Jun;107[6]:1453-72).
According to the 2016 AAD guidelines, the use of oral glucocorticoids may be appropriate over the short term when initiating therapy for severe inflammatory acne. “Pharmacokinetic studies have not demonstrated decreased oral contraceptive levels with common antibiotics,” Dr. Thiboutot said.
Spironolactone, according to the new guidelines, is useful for acne in select females. Spironolactone is an androgen receptor and 5a-reductase blocker, and its antiandrogen effects can improve acne. Many patients do well with 25-50 mg twice daily, though breast tenderness and menstrual irregularities are commonly seen side effects, she noted. If a woman taking spironolactone becomes pregnant, there’s a risk of hypospadias for a male fetus.
Though spironolactone carries a boxed warning because of tumorigenicity observed in animal studies, Dr. Thiboutot said that a large Danish study searched for any association between breast, uterine, or ovarian cancers and spironolactone use. Among the 2.3 million women studied, no increased association was seen (Cancer Epidemiol. 2013 Dec;37:870-5).
She also noted that there’s “low usefulness in monitoring potassium levels in young healthy women on spironolactone.” She cited a study that compared 974 healthy young women taking spironolactone with 1,165 women who were not on spironolactone, which found that the hyperkalemia rate of 0.72% among those on spironolactone was equivalent to the 0.76% baseline rate of hyperkalemia in the young, healthy female population (JAMA Dermatol. 2015;151[9];941-944).
Oral corticosteroids for acne, Dr. Thiboutot said, should be reserved to quiet a severe bout of inflammatory acne while standard therapies are being initiated.
She reported being an investigator or a consultant for a number of pharmaceutical companies.
On Twitter @karioakes
EXPERT ANALYSIS FROM THE SPD ANNUAL MEETING
Candida auris in Venezuela outbreak is triazole-resistant, opportunistic
BOSTON – An investigation into 18 nosocomial Candida auris infections at a tertiary care center in Venezuela showed that isolates of the emerging fungal pathogen obtained during the outbreak were resistant to fluconazole and voriconazole. However, the isolates were intermediately susceptible to amphotericin B and susceptible to 5-fluorocitosine, and demonstrated high susceptibility to the candin antifungal anidulafungin.
Dr. Belinda Calvo, an infectious disease specialist at the University of Maracaibo, Venezuela, and her collaborators reported these findings, related to a 2012-2013 C. auris outbreak at the hospital. Dr. Calvo and her coinvestigators noted that other invasive C. auris outbreaks have been reported in India, Korea, and South Africa, but that “the real prevalence of this organism may be underestimated,” since common rapid microbial identification techniques may misidentify the species.
In a poster session at the annual meeting of the American Society of Microbiology, Dr. Calvo and her collaborators reported that the 18 patients involved in the Venezuelan outbreak were critically ill, of whom 11 were pediatric, and all had central venous catheter placement. All but two of the pediatric patients were neonates, and all had serious underlying morbidities; several had significant congenital anomalies. The median patient age was 26 days (range, 2 days to 72 years), reflecting the high number of neonates affected. One of the adult patients had esophageal carcinoma. Overall, 10/18 patients (56%) had undergone surgical procedures, and all had received antibiotics.
As has been reported in other C. auris outbreaks, isolates from blood cultures of affected individuals were initially reported as C. haemulonii by the Vitek 2 C automated microbial identification system. Molecular identification was completed by sequencing the internal transcribed spacer (ITS) of the rDNA gene, with analysis aided by the National Institutes of Health’s GenBank and the Netherland’s CBS Fungal Diversity Centre , in order to confirm the identity of the fungal isolates as C. auris. Dr. Calvo and her associates were able to generate a dendrogram of the 18 isolates, showing high clonality, a trait shared with other nosocomial C. auris outbreaks.
Susceptibility testing of the C. auris cultured from blood samples of the affected patients showed that fluconazole had a minimum inhibitory concentration to inhibit the growth of 50% of the organisms (MIC50) of greater than 64 mcg/mL. For fluconazole, the MIC90, range, and geometric mean were all also above 64 mcg/mL, indicating a high level of resistance. For voriconazole, the MICs, range, and mean were all 4 mcg/mL. For amphotericin B, the MIC50 was 1 mcg/mL, the MIC90 was 2 mcg/mL, the range was 1-2, and the geometric mean was 1.414 mcg/mL.
The high number of pediatric patients affected, as well as early pathogen identification with speedy and appropriate antifungal therapy and prompt removal of central venous catheters, likely contributed to the relatively low 30-day crude mortality rate of 28%, said Dr. Calvo and her coauthors.
“C. auris should be considered an emergent multiresistant species,” wrote Dr. Calbo and her collaborators, noting that the opportunistic pathogen has a “high potential for nosocomial horizontal transmission.”
In June 2016, the Centers for Disease Control issued a clinical alert to U.S. healthcare facilities regarding the global emergence of invasive infections caused by C. auris.
The study authors reported no external sources of funding and no conflicts of interest.
On Twitter @karioakes
BOSTON – An investigation into 18 nosocomial Candida auris infections at a tertiary care center in Venezuela showed that isolates of the emerging fungal pathogen obtained during the outbreak were resistant to fluconazole and voriconazole. However, the isolates were intermediately susceptible to amphotericin B and susceptible to 5-fluorocitosine, and demonstrated high susceptibility to the candin antifungal anidulafungin.
Dr. Belinda Calvo, an infectious disease specialist at the University of Maracaibo, Venezuela, and her collaborators reported these findings, related to a 2012-2013 C. auris outbreak at the hospital. Dr. Calvo and her coinvestigators noted that other invasive C. auris outbreaks have been reported in India, Korea, and South Africa, but that “the real prevalence of this organism may be underestimated,” since common rapid microbial identification techniques may misidentify the species.
In a poster session at the annual meeting of the American Society of Microbiology, Dr. Calvo and her collaborators reported that the 18 patients involved in the Venezuelan outbreak were critically ill, of whom 11 were pediatric, and all had central venous catheter placement. All but two of the pediatric patients were neonates, and all had serious underlying morbidities; several had significant congenital anomalies. The median patient age was 26 days (range, 2 days to 72 years), reflecting the high number of neonates affected. One of the adult patients had esophageal carcinoma. Overall, 10/18 patients (56%) had undergone surgical procedures, and all had received antibiotics.
As has been reported in other C. auris outbreaks, isolates from blood cultures of affected individuals were initially reported as C. haemulonii by the Vitek 2 C automated microbial identification system. Molecular identification was completed by sequencing the internal transcribed spacer (ITS) of the rDNA gene, with analysis aided by the National Institutes of Health’s GenBank and the Netherland’s CBS Fungal Diversity Centre , in order to confirm the identity of the fungal isolates as C. auris. Dr. Calvo and her associates were able to generate a dendrogram of the 18 isolates, showing high clonality, a trait shared with other nosocomial C. auris outbreaks.
Susceptibility testing of the C. auris cultured from blood samples of the affected patients showed that fluconazole had a minimum inhibitory concentration to inhibit the growth of 50% of the organisms (MIC50) of greater than 64 mcg/mL. For fluconazole, the MIC90, range, and geometric mean were all also above 64 mcg/mL, indicating a high level of resistance. For voriconazole, the MICs, range, and mean were all 4 mcg/mL. For amphotericin B, the MIC50 was 1 mcg/mL, the MIC90 was 2 mcg/mL, the range was 1-2, and the geometric mean was 1.414 mcg/mL.
The high number of pediatric patients affected, as well as early pathogen identification with speedy and appropriate antifungal therapy and prompt removal of central venous catheters, likely contributed to the relatively low 30-day crude mortality rate of 28%, said Dr. Calvo and her coauthors.
“C. auris should be considered an emergent multiresistant species,” wrote Dr. Calbo and her collaborators, noting that the opportunistic pathogen has a “high potential for nosocomial horizontal transmission.”
In June 2016, the Centers for Disease Control issued a clinical alert to U.S. healthcare facilities regarding the global emergence of invasive infections caused by C. auris.
The study authors reported no external sources of funding and no conflicts of interest.
On Twitter @karioakes
BOSTON – An investigation into 18 nosocomial Candida auris infections at a tertiary care center in Venezuela showed that isolates of the emerging fungal pathogen obtained during the outbreak were resistant to fluconazole and voriconazole. However, the isolates were intermediately susceptible to amphotericin B and susceptible to 5-fluorocitosine, and demonstrated high susceptibility to the candin antifungal anidulafungin.
Dr. Belinda Calvo, an infectious disease specialist at the University of Maracaibo, Venezuela, and her collaborators reported these findings, related to a 2012-2013 C. auris outbreak at the hospital. Dr. Calvo and her coinvestigators noted that other invasive C. auris outbreaks have been reported in India, Korea, and South Africa, but that “the real prevalence of this organism may be underestimated,” since common rapid microbial identification techniques may misidentify the species.
In a poster session at the annual meeting of the American Society of Microbiology, Dr. Calvo and her collaborators reported that the 18 patients involved in the Venezuelan outbreak were critically ill, of whom 11 were pediatric, and all had central venous catheter placement. All but two of the pediatric patients were neonates, and all had serious underlying morbidities; several had significant congenital anomalies. The median patient age was 26 days (range, 2 days to 72 years), reflecting the high number of neonates affected. One of the adult patients had esophageal carcinoma. Overall, 10/18 patients (56%) had undergone surgical procedures, and all had received antibiotics.
As has been reported in other C. auris outbreaks, isolates from blood cultures of affected individuals were initially reported as C. haemulonii by the Vitek 2 C automated microbial identification system. Molecular identification was completed by sequencing the internal transcribed spacer (ITS) of the rDNA gene, with analysis aided by the National Institutes of Health’s GenBank and the Netherland’s CBS Fungal Diversity Centre , in order to confirm the identity of the fungal isolates as C. auris. Dr. Calvo and her associates were able to generate a dendrogram of the 18 isolates, showing high clonality, a trait shared with other nosocomial C. auris outbreaks.
Susceptibility testing of the C. auris cultured from blood samples of the affected patients showed that fluconazole had a minimum inhibitory concentration to inhibit the growth of 50% of the organisms (MIC50) of greater than 64 mcg/mL. For fluconazole, the MIC90, range, and geometric mean were all also above 64 mcg/mL, indicating a high level of resistance. For voriconazole, the MICs, range, and mean were all 4 mcg/mL. For amphotericin B, the MIC50 was 1 mcg/mL, the MIC90 was 2 mcg/mL, the range was 1-2, and the geometric mean was 1.414 mcg/mL.
The high number of pediatric patients affected, as well as early pathogen identification with speedy and appropriate antifungal therapy and prompt removal of central venous catheters, likely contributed to the relatively low 30-day crude mortality rate of 28%, said Dr. Calvo and her coauthors.
“C. auris should be considered an emergent multiresistant species,” wrote Dr. Calbo and her collaborators, noting that the opportunistic pathogen has a “high potential for nosocomial horizontal transmission.”
In June 2016, the Centers for Disease Control issued a clinical alert to U.S. healthcare facilities regarding the global emergence of invasive infections caused by C. auris.
The study authors reported no external sources of funding and no conflicts of interest.
On Twitter @karioakes
AT ASM 2016
Key clinical point: Isolates in an outbreak of nosocomially acquired Candida auris were fluconazole-resistant.
Major finding: All C. auris isolates were resistant to fluconazole, with geometric mean minimum inhibitory concentrations greater than 64 mcg/mL.
Data source: Retrospective, single-center study of 18 pediatric and adult patients with C. auris infections at a tertiary care center in Venezuela.
Disclosures: The study investigators reported no outside sources of funding and no disclosures.
Tofacitinib clears pediatric alopecia areata in small study
MINNEAPOLIS – The first study to evaluate tofacitinib’s effectiveness at treating severe alopecia areata in the pediatric population found that the janus kinase inhibitor was effective for more than half of the patients, and well tolerated by all.
Of a case series of 13 pediatric patients who had alopecia areata (AA) and were treated with tofacitinib, 9 (68%) experienced “clinically significant” regrowth of hair, with mean improvement in the Severity of Alopecia Tool (SALT) score of 88% for these responders. The nonresponding group, all of whom had alopecia universalis or totalis, saw essentially no response, with a 1% reduction in SALT score.
Lucy Y. Liu, a medical student at Yale University, New Haven, Conn., presented the findings at the annual meeting of the Society for Pediatric Dermatology.
Ms. Liu and her coinvestigators reported that all of the patients had severe AA by SALT scoring, with an overall mean pretreatment SALT score of 74. Eight of the patients (62%) had alopecia universalis, and two (15%) had alopecia totalis.
The patients ranged in age from 12 to 17 years, with a median age of 15. All but three were male, and patients were an average 9 years old at onset of AA. For patients with alopecia totalis or universalis, the duration of the current episode was a median 1.75 years.
Five patients (38%) had atopic dermatitis, while 1 (8%) had thyroid disease. Three patients (23%) had family members with AA; all but one patient, however, had a family history of autoimmune disease of some sort.
Patients were given tofacitinib 5 mg orally twice daily for 5 months. One patient developed new patches of alopecia during treatment, so the dosing for that patient was increased to 10 mg/5 mg daily.
Adverse events for participants included headaches, upper respiratory infections, and “mild, transient increases in transaminases,” wrote Dr. Lieu and her collaborators. No serious adverse events were reported.
Previous work at Yale had shown that tofacitinib reversed alopecia universalis in a patient who received the medication for plaque psoriasis, and that topical treatment with ruxolitinib, another janus kinase inhibitor, was effective in treating alopecia universalis.
Study limitations included the small sample size and the relatively short duration of follow-up, an important consideration because relapse has been observed after tofacitinib treatment in AA. Still, “Tofacitinib is a promising therapy for the treatment of severe AA in adolescents,” wrote Ms. Liu and her colleagues, recommending randomized clinical trials for further exploration of efficacy and safety in the pediatric population.
On Twitter @karioakes
MINNEAPOLIS – The first study to evaluate tofacitinib’s effectiveness at treating severe alopecia areata in the pediatric population found that the janus kinase inhibitor was effective for more than half of the patients, and well tolerated by all.
Of a case series of 13 pediatric patients who had alopecia areata (AA) and were treated with tofacitinib, 9 (68%) experienced “clinically significant” regrowth of hair, with mean improvement in the Severity of Alopecia Tool (SALT) score of 88% for these responders. The nonresponding group, all of whom had alopecia universalis or totalis, saw essentially no response, with a 1% reduction in SALT score.
Lucy Y. Liu, a medical student at Yale University, New Haven, Conn., presented the findings at the annual meeting of the Society for Pediatric Dermatology.
Ms. Liu and her coinvestigators reported that all of the patients had severe AA by SALT scoring, with an overall mean pretreatment SALT score of 74. Eight of the patients (62%) had alopecia universalis, and two (15%) had alopecia totalis.
The patients ranged in age from 12 to 17 years, with a median age of 15. All but three were male, and patients were an average 9 years old at onset of AA. For patients with alopecia totalis or universalis, the duration of the current episode was a median 1.75 years.
Five patients (38%) had atopic dermatitis, while 1 (8%) had thyroid disease. Three patients (23%) had family members with AA; all but one patient, however, had a family history of autoimmune disease of some sort.
Patients were given tofacitinib 5 mg orally twice daily for 5 months. One patient developed new patches of alopecia during treatment, so the dosing for that patient was increased to 10 mg/5 mg daily.
Adverse events for participants included headaches, upper respiratory infections, and “mild, transient increases in transaminases,” wrote Dr. Lieu and her collaborators. No serious adverse events were reported.
Previous work at Yale had shown that tofacitinib reversed alopecia universalis in a patient who received the medication for plaque psoriasis, and that topical treatment with ruxolitinib, another janus kinase inhibitor, was effective in treating alopecia universalis.
Study limitations included the small sample size and the relatively short duration of follow-up, an important consideration because relapse has been observed after tofacitinib treatment in AA. Still, “Tofacitinib is a promising therapy for the treatment of severe AA in adolescents,” wrote Ms. Liu and her colleagues, recommending randomized clinical trials for further exploration of efficacy and safety in the pediatric population.
On Twitter @karioakes
MINNEAPOLIS – The first study to evaluate tofacitinib’s effectiveness at treating severe alopecia areata in the pediatric population found that the janus kinase inhibitor was effective for more than half of the patients, and well tolerated by all.
Of a case series of 13 pediatric patients who had alopecia areata (AA) and were treated with tofacitinib, 9 (68%) experienced “clinically significant” regrowth of hair, with mean improvement in the Severity of Alopecia Tool (SALT) score of 88% for these responders. The nonresponding group, all of whom had alopecia universalis or totalis, saw essentially no response, with a 1% reduction in SALT score.
Lucy Y. Liu, a medical student at Yale University, New Haven, Conn., presented the findings at the annual meeting of the Society for Pediatric Dermatology.
Ms. Liu and her coinvestigators reported that all of the patients had severe AA by SALT scoring, with an overall mean pretreatment SALT score of 74. Eight of the patients (62%) had alopecia universalis, and two (15%) had alopecia totalis.
The patients ranged in age from 12 to 17 years, with a median age of 15. All but three were male, and patients were an average 9 years old at onset of AA. For patients with alopecia totalis or universalis, the duration of the current episode was a median 1.75 years.
Five patients (38%) had atopic dermatitis, while 1 (8%) had thyroid disease. Three patients (23%) had family members with AA; all but one patient, however, had a family history of autoimmune disease of some sort.
Patients were given tofacitinib 5 mg orally twice daily for 5 months. One patient developed new patches of alopecia during treatment, so the dosing for that patient was increased to 10 mg/5 mg daily.
Adverse events for participants included headaches, upper respiratory infections, and “mild, transient increases in transaminases,” wrote Dr. Lieu and her collaborators. No serious adverse events were reported.
Previous work at Yale had shown that tofacitinib reversed alopecia universalis in a patient who received the medication for plaque psoriasis, and that topical treatment with ruxolitinib, another janus kinase inhibitor, was effective in treating alopecia universalis.
Study limitations included the small sample size and the relatively short duration of follow-up, an important consideration because relapse has been observed after tofacitinib treatment in AA. Still, “Tofacitinib is a promising therapy for the treatment of severe AA in adolescents,” wrote Ms. Liu and her colleagues, recommending randomized clinical trials for further exploration of efficacy and safety in the pediatric population.
On Twitter @karioakes
AT THE SPD ANNUAL MEETING
Key clinical point: The JAK inhibitor tofacitinib resolved alopecia areata in 68% of pediatric patients.
Major finding: Among the responders, the Severity of Alopecia Tool score improved by a mean 88% over 5 months.
Data source: Case series of 13 pediatric patients with severe alopecia areata treated with tofacitinib at a single site.
Disclosures: Ms. Liu and her collaborators reported no conflicts of interest.
Extended pneumococcal vaccination schedule boosts early immunity for preemies
A randomized clinical trial evaluating three dosing strategies for 13-valent pneumococcal vaccine (PCV13) in preterm infants found that more widely spaced priming vaccinations resulted in higher immunoglobulin G (IgG) during the first 12 months of life, but reduced the immune response seen after the 12-month booster was given.
After the primary schedule, the percent of infants lacking seroprotection for more than one half of the serotypes in the PCV13 formulation was 25% on a reduced two-dose schedule, 12% on an accelerated schedule, and 3% on an extended schedule (P less than .001).
Conversely, “A reduced priming schedule of PCV13 resulted in higher post-booster IgG concentrations but lower post-primary concentrations,” wrote Alison Kent, MBChB, and her coinvestigators in the PUNS (Prems Under New Schedule) Study Group (Pediatrics. 2016;138[3]:e20153945).
“Infants who received the extended schedule had lower fold increases in concentrations after booster vaccination than the other groups,” wrote Dr. Kent of the Pediatric Infectious Diseases Research Group and Vaccine Institute, St. George’s, University of London, and her collaborators. Participants receiving the extended schedule had lower geometric mean concentrations (GMCs) of antibodies than did those on the reduced schedule for nine serotypes and those on the accelerated schedule for four serotypes.
The study enrolled 210 premature infants in a phase IV, controlled, open-label trial at 12 sites in the United Kingdom. Infants of less than 35 weeks gestation, and between 7 and 12 weeks of age, were randomly assigned to receive PCV13 on one of three schedules. The reduced schedule gave two priming doses at 2 and 4 months of age; the accelerated schedule gave the doses at 2, 3, and 4 months of age; and the extended schedule gave doses at 2, 4, and 6 months of age. All infants received a booster vaccination at 12 or 13 months of age, and all received a standard suite of childhood immunizations for other diseases. The entire study was completed by 194 patients.
Serotype-specific IgG concentrations were obtained pre-vaccination, 1 month after the primary vaccination, and before and 1 month after the booster vaccination was given. IgG levels were reported for each PCV serotype; “there was considerable variation between serotypes,” ranging from 0.16 ng/mL for serotype 6b on the reduced schedule to 8.49 ng/mL for serotype 14 on the extended schedule, the investigators said.
Dr. Kent and her collaborators also used logistic regression analysis to explore how the vaccine’s effectiveness was affected by a number of factors. These included gestational length, the receipt of blood transfusions or pre- or post-natal steroids, BCG vaccination, early postvaccination acetaminophen, and the presence of chronic lung disease.
Later gestation was associated with increased seroprotection for four serotypes at 2 months of age, and with an increase in post-primary vaccination IgG concentrations for three others (P-values ranging from P less than .001 to P = .021).
No other factors were associated with protective IgG levels at any point, except that receipt of prenatal steroids had a negative association with seroprotection for several serotypes. “At no time points were antenatal steroids associated with higher antibody concentrations,” wrote the investigators.
Most studies of immunogenicity of infant vaccination schedules have been completed using term infants, with limited knowledge about efficacy in preterm infants. Previous work had shown that preterm infants had lower IgG concentrations after the primary and booster vaccinations for eight serotypes of PCV, compared with term infants. “The lower immunogenicity ... is concerning because premature infants are also less likely to benefit from the protective maternal antibodies transferred during late pregnancy,” Dr. Kent and her coauthors wrote.
The lower booster immunogenicity after the extended schedule is an effect that has been previously observed with other vaccinations and may be related to the formation of immune complexes with previously existing antibodies with the vaccine antigen, said Dr. Kent and her coauthors. The variation in immunogenicity timing for the various priming schedules, they said, will be helpful for those caring for preterm infants, enabling them “to consider this finding in the context of their own immunization programs and epidemiologic situations.”
The study was funded by Pfizer as an investigator-led study, without Pfizer’s input on the conduct of the trial, analysis of data, interpretation of results, or the preparation of this manuscript. Pfizer manufactures Prevnar 13.
On Twitter @karioakes
The needs of varying populations, the prevalence of various serotypes, and other local epidemiologic and economic factors all influence vaccination schedules. For PCV, the present study showed how widely seroprotection varied between serotypes and between different priming schedules.
Invasive pneumococcal disease (IPD) can be devastating in the vulnerable preterm population, as can pneumococcal pneumonia. Though the current vaccination schedule recommendations in the United States takes into account age-related changes in the immune system, truly optimized vaccine delivery for all populations, including this vulnerable one, is still more a goal than a reality.
However, each of the schedules examined in this study have been studied in areas where they are in clinical use, and all are generally protective of IPD. The timing of other vaccinations, as well as economic and logistic realities, will also affect vaccination schedules, and must be taken into account.
The findings of this study show that no one schedule is best for all populations, and also highlight why those making vaccine policy around the globe will continue to arrive at varying answers when considering the needs of their populations.
Mark H. Sawyer, MD, is a professor of pediatrics at the University of California, San Diego. Mobeen Rathore, MD, is director of the University of Florida Center for HIV/AIDS Research, Education and Service. They had no conflicts of interest to declare. Their remarks are drawn from a companion commentary in Pediatrics (Pediatrics. 2016;138[3]:e20160975).
The needs of varying populations, the prevalence of various serotypes, and other local epidemiologic and economic factors all influence vaccination schedules. For PCV, the present study showed how widely seroprotection varied between serotypes and between different priming schedules.
Invasive pneumococcal disease (IPD) can be devastating in the vulnerable preterm population, as can pneumococcal pneumonia. Though the current vaccination schedule recommendations in the United States takes into account age-related changes in the immune system, truly optimized vaccine delivery for all populations, including this vulnerable one, is still more a goal than a reality.
However, each of the schedules examined in this study have been studied in areas where they are in clinical use, and all are generally protective of IPD. The timing of other vaccinations, as well as economic and logistic realities, will also affect vaccination schedules, and must be taken into account.
The findings of this study show that no one schedule is best for all populations, and also highlight why those making vaccine policy around the globe will continue to arrive at varying answers when considering the needs of their populations.
Mark H. Sawyer, MD, is a professor of pediatrics at the University of California, San Diego. Mobeen Rathore, MD, is director of the University of Florida Center for HIV/AIDS Research, Education and Service. They had no conflicts of interest to declare. Their remarks are drawn from a companion commentary in Pediatrics (Pediatrics. 2016;138[3]:e20160975).
The needs of varying populations, the prevalence of various serotypes, and other local epidemiologic and economic factors all influence vaccination schedules. For PCV, the present study showed how widely seroprotection varied between serotypes and between different priming schedules.
Invasive pneumococcal disease (IPD) can be devastating in the vulnerable preterm population, as can pneumococcal pneumonia. Though the current vaccination schedule recommendations in the United States takes into account age-related changes in the immune system, truly optimized vaccine delivery for all populations, including this vulnerable one, is still more a goal than a reality.
However, each of the schedules examined in this study have been studied in areas where they are in clinical use, and all are generally protective of IPD. The timing of other vaccinations, as well as economic and logistic realities, will also affect vaccination schedules, and must be taken into account.
The findings of this study show that no one schedule is best for all populations, and also highlight why those making vaccine policy around the globe will continue to arrive at varying answers when considering the needs of their populations.
Mark H. Sawyer, MD, is a professor of pediatrics at the University of California, San Diego. Mobeen Rathore, MD, is director of the University of Florida Center for HIV/AIDS Research, Education and Service. They had no conflicts of interest to declare. Their remarks are drawn from a companion commentary in Pediatrics (Pediatrics. 2016;138[3]:e20160975).
A randomized clinical trial evaluating three dosing strategies for 13-valent pneumococcal vaccine (PCV13) in preterm infants found that more widely spaced priming vaccinations resulted in higher immunoglobulin G (IgG) during the first 12 months of life, but reduced the immune response seen after the 12-month booster was given.
After the primary schedule, the percent of infants lacking seroprotection for more than one half of the serotypes in the PCV13 formulation was 25% on a reduced two-dose schedule, 12% on an accelerated schedule, and 3% on an extended schedule (P less than .001).
Conversely, “A reduced priming schedule of PCV13 resulted in higher post-booster IgG concentrations but lower post-primary concentrations,” wrote Alison Kent, MBChB, and her coinvestigators in the PUNS (Prems Under New Schedule) Study Group (Pediatrics. 2016;138[3]:e20153945).
“Infants who received the extended schedule had lower fold increases in concentrations after booster vaccination than the other groups,” wrote Dr. Kent of the Pediatric Infectious Diseases Research Group and Vaccine Institute, St. George’s, University of London, and her collaborators. Participants receiving the extended schedule had lower geometric mean concentrations (GMCs) of antibodies than did those on the reduced schedule for nine serotypes and those on the accelerated schedule for four serotypes.
The study enrolled 210 premature infants in a phase IV, controlled, open-label trial at 12 sites in the United Kingdom. Infants of less than 35 weeks gestation, and between 7 and 12 weeks of age, were randomly assigned to receive PCV13 on one of three schedules. The reduced schedule gave two priming doses at 2 and 4 months of age; the accelerated schedule gave the doses at 2, 3, and 4 months of age; and the extended schedule gave doses at 2, 4, and 6 months of age. All infants received a booster vaccination at 12 or 13 months of age, and all received a standard suite of childhood immunizations for other diseases. The entire study was completed by 194 patients.
Serotype-specific IgG concentrations were obtained pre-vaccination, 1 month after the primary vaccination, and before and 1 month after the booster vaccination was given. IgG levels were reported for each PCV serotype; “there was considerable variation between serotypes,” ranging from 0.16 ng/mL for serotype 6b on the reduced schedule to 8.49 ng/mL for serotype 14 on the extended schedule, the investigators said.
Dr. Kent and her collaborators also used logistic regression analysis to explore how the vaccine’s effectiveness was affected by a number of factors. These included gestational length, the receipt of blood transfusions or pre- or post-natal steroids, BCG vaccination, early postvaccination acetaminophen, and the presence of chronic lung disease.
Later gestation was associated with increased seroprotection for four serotypes at 2 months of age, and with an increase in post-primary vaccination IgG concentrations for three others (P-values ranging from P less than .001 to P = .021).
No other factors were associated with protective IgG levels at any point, except that receipt of prenatal steroids had a negative association with seroprotection for several serotypes. “At no time points were antenatal steroids associated with higher antibody concentrations,” wrote the investigators.
Most studies of immunogenicity of infant vaccination schedules have been completed using term infants, with limited knowledge about efficacy in preterm infants. Previous work had shown that preterm infants had lower IgG concentrations after the primary and booster vaccinations for eight serotypes of PCV, compared with term infants. “The lower immunogenicity ... is concerning because premature infants are also less likely to benefit from the protective maternal antibodies transferred during late pregnancy,” Dr. Kent and her coauthors wrote.
The lower booster immunogenicity after the extended schedule is an effect that has been previously observed with other vaccinations and may be related to the formation of immune complexes with previously existing antibodies with the vaccine antigen, said Dr. Kent and her coauthors. The variation in immunogenicity timing for the various priming schedules, they said, will be helpful for those caring for preterm infants, enabling them “to consider this finding in the context of their own immunization programs and epidemiologic situations.”
The study was funded by Pfizer as an investigator-led study, without Pfizer’s input on the conduct of the trial, analysis of data, interpretation of results, or the preparation of this manuscript. Pfizer manufactures Prevnar 13.
On Twitter @karioakes
A randomized clinical trial evaluating three dosing strategies for 13-valent pneumococcal vaccine (PCV13) in preterm infants found that more widely spaced priming vaccinations resulted in higher immunoglobulin G (IgG) during the first 12 months of life, but reduced the immune response seen after the 12-month booster was given.
After the primary schedule, the percent of infants lacking seroprotection for more than one half of the serotypes in the PCV13 formulation was 25% on a reduced two-dose schedule, 12% on an accelerated schedule, and 3% on an extended schedule (P less than .001).
Conversely, “A reduced priming schedule of PCV13 resulted in higher post-booster IgG concentrations but lower post-primary concentrations,” wrote Alison Kent, MBChB, and her coinvestigators in the PUNS (Prems Under New Schedule) Study Group (Pediatrics. 2016;138[3]:e20153945).
“Infants who received the extended schedule had lower fold increases in concentrations after booster vaccination than the other groups,” wrote Dr. Kent of the Pediatric Infectious Diseases Research Group and Vaccine Institute, St. George’s, University of London, and her collaborators. Participants receiving the extended schedule had lower geometric mean concentrations (GMCs) of antibodies than did those on the reduced schedule for nine serotypes and those on the accelerated schedule for four serotypes.
The study enrolled 210 premature infants in a phase IV, controlled, open-label trial at 12 sites in the United Kingdom. Infants of less than 35 weeks gestation, and between 7 and 12 weeks of age, were randomly assigned to receive PCV13 on one of three schedules. The reduced schedule gave two priming doses at 2 and 4 months of age; the accelerated schedule gave the doses at 2, 3, and 4 months of age; and the extended schedule gave doses at 2, 4, and 6 months of age. All infants received a booster vaccination at 12 or 13 months of age, and all received a standard suite of childhood immunizations for other diseases. The entire study was completed by 194 patients.
Serotype-specific IgG concentrations were obtained pre-vaccination, 1 month after the primary vaccination, and before and 1 month after the booster vaccination was given. IgG levels were reported for each PCV serotype; “there was considerable variation between serotypes,” ranging from 0.16 ng/mL for serotype 6b on the reduced schedule to 8.49 ng/mL for serotype 14 on the extended schedule, the investigators said.
Dr. Kent and her collaborators also used logistic regression analysis to explore how the vaccine’s effectiveness was affected by a number of factors. These included gestational length, the receipt of blood transfusions or pre- or post-natal steroids, BCG vaccination, early postvaccination acetaminophen, and the presence of chronic lung disease.
Later gestation was associated with increased seroprotection for four serotypes at 2 months of age, and with an increase in post-primary vaccination IgG concentrations for three others (P-values ranging from P less than .001 to P = .021).
No other factors were associated with protective IgG levels at any point, except that receipt of prenatal steroids had a negative association with seroprotection for several serotypes. “At no time points were antenatal steroids associated with higher antibody concentrations,” wrote the investigators.
Most studies of immunogenicity of infant vaccination schedules have been completed using term infants, with limited knowledge about efficacy in preterm infants. Previous work had shown that preterm infants had lower IgG concentrations after the primary and booster vaccinations for eight serotypes of PCV, compared with term infants. “The lower immunogenicity ... is concerning because premature infants are also less likely to benefit from the protective maternal antibodies transferred during late pregnancy,” Dr. Kent and her coauthors wrote.
The lower booster immunogenicity after the extended schedule is an effect that has been previously observed with other vaccinations and may be related to the formation of immune complexes with previously existing antibodies with the vaccine antigen, said Dr. Kent and her coauthors. The variation in immunogenicity timing for the various priming schedules, they said, will be helpful for those caring for preterm infants, enabling them “to consider this finding in the context of their own immunization programs and epidemiologic situations.”
The study was funded by Pfizer as an investigator-led study, without Pfizer’s input on the conduct of the trial, analysis of data, interpretation of results, or the preparation of this manuscript. Pfizer manufactures Prevnar 13.
On Twitter @karioakes
FROM PEDIATRICS
Key clinical point: More widely-spaced pneumococcal vaccinations boosted early immunity but reduced the effectiveness of a 12-month booster in preterm infants.
Major finding: Of preterm infants on an extended pneumococcal conjugate vaccine (PCV13) schedule, just 3% lacked seroprotection for over half of the serotypes.
Data source: Randomized, placebo-controlled, open-label study of 210 preterm infants receiving PCV13vaccination on one of three dosing schedules.
Disclosures: The study was funded by Pfizer as an investigator-led study, without Pfizer’s input on the conduct of the trial, analysis of data, interpretation of results, or the preparation of this manuscript. Pfizer manufactures Prevnar 13.
Clindamycin Confers No Extra Benefit for Kids With SSSS
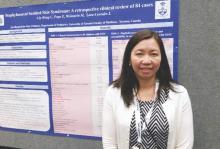
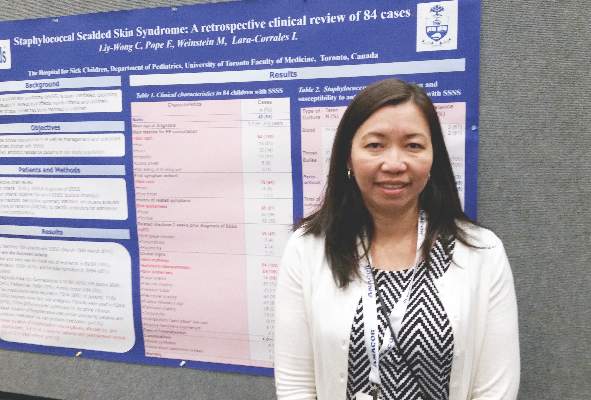
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
AT THE SPD ANNUAL MEETING
Clindamycin confers no extra benefit for kids with SSSS
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
On Twitter @karioakes
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
On Twitter @karioakes
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
On Twitter @karioakes
AT THE SPD ANNUAL MEETING
Key clinical point: Clindamycin did not benefit hospitalized children with staphylococcal scalded skin syndrome (SSSS).
Major finding: Clindamycin conferred no benefit in length of hospital stay compared with non-antitoxin antibiotics for SSSS (P = .63).
Data source: A retrospective chart review of 84 pediatric patients meeting SSSS criteria at a single children’s hospital.
Disclosures: Dr. Liy-Wong and her colleagues reported no external sources of funding, and no relevant disclosures.
Common Allergic Dermatitis Culprits Are Hiding in Plain Sight
MINNEAPOLIS – When it comes to allergic contact dermatitis in children, the answer is sometimes hiding in plain sight. Cleansers, moisturizers, shampoos, detergents – all can contain ingredients that provoke significant reactions, yet many of these ingredients are not on the most common testing panels.
Erin Warshaw, MD, professor of dermatology at the University of Minnesota, reviewed common but often unsuspected causes of allergic dermatitis in the pediatric population at the annual meeting of the Society for Pediatric Dermatology.
Even some hypoallergenic and frequently recommended products can contain preservatives and other ingredients that provoke allergic reactions, according to Dr. Warshaw. A chief culprit is methylisothiazolinone (MI), a preservative that came into common use as formaldehyde has been gradually phased out.
“If there’s anything I could emphasize from this talk, it’s MI, MI, MI. This is the major epidemic of our time in the contact dermatitis world,” Dr. Warshaw said. Upcoming publications, she added, will place MI in the top five most common contact allergens. “MI is in everything, including things you would think would be hypoallergenic,” she said. She recommended looking at ingredient labels with a keen eye when making testing decisions.
Despite MI’s status as a frequent culprit, it’s not an allergen that appears on common test kits, Dr. Warshaw pointed out. For example, it’s absent from one of the most commonly used test kits, the Thin-Layer Rapid Use Epicutaneous Patch (T.R.U.E. test).
The T.R.U.E. test, said Dr. Warshaw, has reasonable sensitivity – it can detect 71% of relevant positive patch tests (RPPTs) in children. However, she added, a recent study showed that about 23% of children reacted to a supplemental allergen. “That’s significant. One quarter of these individuals only reacted to a preservative … or a sunscreen, or an acrylate. These aren’t on the T.R.U.E. test.”
Decyl glucoside is another frequent culprit that is not included in commercial patch test kits. “It’s really an important emerging allergen,” said Dr. Warshaw, noting that it commonly cross-reacts with coco and lauryl glucoside, frequently found in fragrance-free products. “It’s always humbling when we find the allergen in the product we’ve recommended to our patients.”
Other important allergens not on the T.R.U.E. test include propolis, tocopherol, oxybenzone, and many surfactants and botanicals.
In order to avoid a confounding reaction to aluminum, Dr. Warshaw recommends testing using plastic-backed test chambers, such as IQ chambers, rather than Finn chambers, which are aluminum backed.
When working with families to track down allergens in the pediatric population, Dr. Warshaw adjusts her approach from what she would use for adults.
“What do I do differently in kids? First of all, I set expectations for children and parents,” she said. Some of the most frequent parental questions deal with food allergies, so she allots time to explain the rationale for not testing for food allergens when allergic contact dermatitis is suspected.
For many patients, “I try and frame that there is probably baseline eczema, and our goal is to try to figure out if there is an allergy in addition to that that is contributing to the flares,” she said. She makes sure to convey that “all it takes is one exposure every 3 weeks; that will keep this reaction going.”
However, she’s judicious in interpreting equivocal results. “I feel a responsibility not to label children with an allergy” if results are unclear. Finally, providing enough time is key, said Dr. Warshaw, who allots an hour for reviewing final testing results.
The take-home points? It’s worthwhile to patch test children, since over half of children will have at least one RPPT. Also, contact dermatitis can be an overlay on preexisting allergic dermatitis, so patch testing can still be helpful for these children. Supplemental allergens are important in patch testing, “especially in children with a negative test to a screening series,” Dr. Warshaw said.
She recommended accessing the Contact Allergen Management Program (CAMP) database, found on the American Contact Dermatitis Society website. The list is a searchable database that generates a list of “safe” products that don’t contain a given allergen. This resource is available for society members, but a member’s access code can be shared among faculty members at academic institutions, she said. Patients can also be given unique codes that will give them access for life, so they can use the CAMP database on a computer or via a smartphone app.
Dr. Warshaw reported no relevant financial disclosures.
MINNEAPOLIS – When it comes to allergic contact dermatitis in children, the answer is sometimes hiding in plain sight. Cleansers, moisturizers, shampoos, detergents – all can contain ingredients that provoke significant reactions, yet many of these ingredients are not on the most common testing panels.
Erin Warshaw, MD, professor of dermatology at the University of Minnesota, reviewed common but often unsuspected causes of allergic dermatitis in the pediatric population at the annual meeting of the Society for Pediatric Dermatology.
Even some hypoallergenic and frequently recommended products can contain preservatives and other ingredients that provoke allergic reactions, according to Dr. Warshaw. A chief culprit is methylisothiazolinone (MI), a preservative that came into common use as formaldehyde has been gradually phased out.
“If there’s anything I could emphasize from this talk, it’s MI, MI, MI. This is the major epidemic of our time in the contact dermatitis world,” Dr. Warshaw said. Upcoming publications, she added, will place MI in the top five most common contact allergens. “MI is in everything, including things you would think would be hypoallergenic,” she said. She recommended looking at ingredient labels with a keen eye when making testing decisions.
Despite MI’s status as a frequent culprit, it’s not an allergen that appears on common test kits, Dr. Warshaw pointed out. For example, it’s absent from one of the most commonly used test kits, the Thin-Layer Rapid Use Epicutaneous Patch (T.R.U.E. test).
The T.R.U.E. test, said Dr. Warshaw, has reasonable sensitivity – it can detect 71% of relevant positive patch tests (RPPTs) in children. However, she added, a recent study showed that about 23% of children reacted to a supplemental allergen. “That’s significant. One quarter of these individuals only reacted to a preservative … or a sunscreen, or an acrylate. These aren’t on the T.R.U.E. test.”
Decyl glucoside is another frequent culprit that is not included in commercial patch test kits. “It’s really an important emerging allergen,” said Dr. Warshaw, noting that it commonly cross-reacts with coco and lauryl glucoside, frequently found in fragrance-free products. “It’s always humbling when we find the allergen in the product we’ve recommended to our patients.”
Other important allergens not on the T.R.U.E. test include propolis, tocopherol, oxybenzone, and many surfactants and botanicals.
In order to avoid a confounding reaction to aluminum, Dr. Warshaw recommends testing using plastic-backed test chambers, such as IQ chambers, rather than Finn chambers, which are aluminum backed.
When working with families to track down allergens in the pediatric population, Dr. Warshaw adjusts her approach from what she would use for adults.
“What do I do differently in kids? First of all, I set expectations for children and parents,” she said. Some of the most frequent parental questions deal with food allergies, so she allots time to explain the rationale for not testing for food allergens when allergic contact dermatitis is suspected.
For many patients, “I try and frame that there is probably baseline eczema, and our goal is to try to figure out if there is an allergy in addition to that that is contributing to the flares,” she said. She makes sure to convey that “all it takes is one exposure every 3 weeks; that will keep this reaction going.”
However, she’s judicious in interpreting equivocal results. “I feel a responsibility not to label children with an allergy” if results are unclear. Finally, providing enough time is key, said Dr. Warshaw, who allots an hour for reviewing final testing results.
The take-home points? It’s worthwhile to patch test children, since over half of children will have at least one RPPT. Also, contact dermatitis can be an overlay on preexisting allergic dermatitis, so patch testing can still be helpful for these children. Supplemental allergens are important in patch testing, “especially in children with a negative test to a screening series,” Dr. Warshaw said.
She recommended accessing the Contact Allergen Management Program (CAMP) database, found on the American Contact Dermatitis Society website. The list is a searchable database that generates a list of “safe” products that don’t contain a given allergen. This resource is available for society members, but a member’s access code can be shared among faculty members at academic institutions, she said. Patients can also be given unique codes that will give them access for life, so they can use the CAMP database on a computer or via a smartphone app.
Dr. Warshaw reported no relevant financial disclosures.
MINNEAPOLIS – When it comes to allergic contact dermatitis in children, the answer is sometimes hiding in plain sight. Cleansers, moisturizers, shampoos, detergents – all can contain ingredients that provoke significant reactions, yet many of these ingredients are not on the most common testing panels.
Erin Warshaw, MD, professor of dermatology at the University of Minnesota, reviewed common but often unsuspected causes of allergic dermatitis in the pediatric population at the annual meeting of the Society for Pediatric Dermatology.
Even some hypoallergenic and frequently recommended products can contain preservatives and other ingredients that provoke allergic reactions, according to Dr. Warshaw. A chief culprit is methylisothiazolinone (MI), a preservative that came into common use as formaldehyde has been gradually phased out.
“If there’s anything I could emphasize from this talk, it’s MI, MI, MI. This is the major epidemic of our time in the contact dermatitis world,” Dr. Warshaw said. Upcoming publications, she added, will place MI in the top five most common contact allergens. “MI is in everything, including things you would think would be hypoallergenic,” she said. She recommended looking at ingredient labels with a keen eye when making testing decisions.
Despite MI’s status as a frequent culprit, it’s not an allergen that appears on common test kits, Dr. Warshaw pointed out. For example, it’s absent from one of the most commonly used test kits, the Thin-Layer Rapid Use Epicutaneous Patch (T.R.U.E. test).
The T.R.U.E. test, said Dr. Warshaw, has reasonable sensitivity – it can detect 71% of relevant positive patch tests (RPPTs) in children. However, she added, a recent study showed that about 23% of children reacted to a supplemental allergen. “That’s significant. One quarter of these individuals only reacted to a preservative … or a sunscreen, or an acrylate. These aren’t on the T.R.U.E. test.”
Decyl glucoside is another frequent culprit that is not included in commercial patch test kits. “It’s really an important emerging allergen,” said Dr. Warshaw, noting that it commonly cross-reacts with coco and lauryl glucoside, frequently found in fragrance-free products. “It’s always humbling when we find the allergen in the product we’ve recommended to our patients.”
Other important allergens not on the T.R.U.E. test include propolis, tocopherol, oxybenzone, and many surfactants and botanicals.
In order to avoid a confounding reaction to aluminum, Dr. Warshaw recommends testing using plastic-backed test chambers, such as IQ chambers, rather than Finn chambers, which are aluminum backed.
When working with families to track down allergens in the pediatric population, Dr. Warshaw adjusts her approach from what she would use for adults.
“What do I do differently in kids? First of all, I set expectations for children and parents,” she said. Some of the most frequent parental questions deal with food allergies, so she allots time to explain the rationale for not testing for food allergens when allergic contact dermatitis is suspected.
For many patients, “I try and frame that there is probably baseline eczema, and our goal is to try to figure out if there is an allergy in addition to that that is contributing to the flares,” she said. She makes sure to convey that “all it takes is one exposure every 3 weeks; that will keep this reaction going.”
However, she’s judicious in interpreting equivocal results. “I feel a responsibility not to label children with an allergy” if results are unclear. Finally, providing enough time is key, said Dr. Warshaw, who allots an hour for reviewing final testing results.
The take-home points? It’s worthwhile to patch test children, since over half of children will have at least one RPPT. Also, contact dermatitis can be an overlay on preexisting allergic dermatitis, so patch testing can still be helpful for these children. Supplemental allergens are important in patch testing, “especially in children with a negative test to a screening series,” Dr. Warshaw said.
She recommended accessing the Contact Allergen Management Program (CAMP) database, found on the American Contact Dermatitis Society website. The list is a searchable database that generates a list of “safe” products that don’t contain a given allergen. This resource is available for society members, but a member’s access code can be shared among faculty members at academic institutions, she said. Patients can also be given unique codes that will give them access for life, so they can use the CAMP database on a computer or via a smartphone app.
Dr. Warshaw reported no relevant financial disclosures.
EXPERT ANALYSIS FROM THE SPD ANNUAL MEETING
Common allergic dermatitis culprits are hiding in plain sight
MINNEAPOLIS – When it comes to allergic contact dermatitis in children, the answer is sometimes hiding in plain sight. Cleansers, moisturizers, shampoos, detergents – all can contain ingredients that provoke significant reactions, yet many of these ingredients are not on the most common testing panels.
Erin Warshaw, MD, professor of dermatology at the University of Minnesota, reviewed common but often unsuspected causes of allergic dermatitis in the pediatric population at the annual meeting of the Society for Pediatric Dermatology.
Even some hypoallergenic and frequently recommended products can contain preservatives and other ingredients that provoke allergic reactions, according to Dr. Warshaw. A chief culprit is methylisothiazolinone (MI), a preservative that came into common use as formaldehyde has been gradually phased out.
“If there’s anything I could emphasize from this talk, it’s MI, MI, MI. This is the major epidemic of our time in the contact dermatitis world,” Dr. Warshaw said. Upcoming publications, she added, will place MI in the top five most common contact allergens. “MI is in everything, including things you would think would be hypoallergenic,” she said. She recommended looking at ingredient labels with a keen eye when making testing decisions.
Despite MI’s status as a frequent culprit, it’s not an allergen that appears on common test kits, Dr. Warshaw pointed out. For example, it’s absent from one of the most commonly used test kits, the Thin-Layer Rapid Use Epicutaneous Patch (T.R.U.E. test).
The T.R.U.E. test, said Dr. Warshaw, has reasonable sensitivity – it can detect 71% of relevant positive patch tests (RPPTs) in children. However, she added, a recent study showed that about 23% of children reacted to a supplemental allergen. “That’s significant. One quarter of these individuals only reacted to a preservative … or a sunscreen, or an acrylate. These aren’t on the T.R.U.E. test.”
Decyl glucoside is another frequent culprit that is not included in commercial patch test kits. “It’s really an important emerging allergen,” said Dr. Warshaw, noting that it commonly cross-reacts with coco and lauryl glucoside, frequently found in fragrance-free products. “It’s always humbling when we find the allergen in the product we’ve recommended to our patients.”
Other important allergens not on the T.R.U.E. test include propolis, tocopherol, oxybenzone, and many surfactants and botanicals.
In order to avoid a confounding reaction to aluminum, Dr. Warshaw recommends testing using plastic-backed test chambers, such as IQ chambers, rather than Finn chambers, which are aluminum backed.
When working with families to track down allergens in the pediatric population, Dr. Warshaw adjusts her approach from what she would use for adults.
“What do I do differently in kids? First of all, I set expectations for children and parents,” she said. Some of the most frequent parental questions deal with food allergies, so she allots time to explain the rationale for not testing for food allergens when allergic contact dermatitis is suspected.
For many patients, “I try and frame that there is probably baseline eczema, and our goal is to try to figure out if there is an allergy in addition to that that is contributing to the flares,” she said. She makes sure to convey that “all it takes is one exposure every 3 weeks; that will keep this reaction going.”
However, she’s judicious in interpreting equivocal results. “I feel a responsibility not to label children with an allergy” if results are unclear. Finally, providing enough time is key, said Dr. Warshaw, who allots an hour for reviewing final testing results.
The take-home points? It’s worthwhile to patch test children, since over half of children will have at least one RPPT. Also, contact dermatitis can be an overlay on preexisting allergic dermatitis, so patch testing can still be helpful for these children. Supplemental allergens are important in patch testing, “especially in children with a negative test to a screening series,” Dr. Warshaw said.
She recommended accessing the Contact Allergen Management Program (CAMP) database, found on the American Contact Dermatitis Society website. The list is a searchable database that generates a list of “safe” products that don’t contain a given allergen. This resource is available for society members, but a member’s access code can be shared among faculty members at academic institutions, she said. Patients can also be given unique codes that will give them access for life, so they can use the CAMP database on a computer or via a smartphone app.
Dr. Warshaw reported no relevant financial disclosures.
On Twitter @karioakes
MINNEAPOLIS – When it comes to allergic contact dermatitis in children, the answer is sometimes hiding in plain sight. Cleansers, moisturizers, shampoos, detergents – all can contain ingredients that provoke significant reactions, yet many of these ingredients are not on the most common testing panels.
Erin Warshaw, MD, professor of dermatology at the University of Minnesota, reviewed common but often unsuspected causes of allergic dermatitis in the pediatric population at the annual meeting of the Society for Pediatric Dermatology.
Even some hypoallergenic and frequently recommended products can contain preservatives and other ingredients that provoke allergic reactions, according to Dr. Warshaw. A chief culprit is methylisothiazolinone (MI), a preservative that came into common use as formaldehyde has been gradually phased out.
“If there’s anything I could emphasize from this talk, it’s MI, MI, MI. This is the major epidemic of our time in the contact dermatitis world,” Dr. Warshaw said. Upcoming publications, she added, will place MI in the top five most common contact allergens. “MI is in everything, including things you would think would be hypoallergenic,” she said. She recommended looking at ingredient labels with a keen eye when making testing decisions.
Despite MI’s status as a frequent culprit, it’s not an allergen that appears on common test kits, Dr. Warshaw pointed out. For example, it’s absent from one of the most commonly used test kits, the Thin-Layer Rapid Use Epicutaneous Patch (T.R.U.E. test).
The T.R.U.E. test, said Dr. Warshaw, has reasonable sensitivity – it can detect 71% of relevant positive patch tests (RPPTs) in children. However, she added, a recent study showed that about 23% of children reacted to a supplemental allergen. “That’s significant. One quarter of these individuals only reacted to a preservative … or a sunscreen, or an acrylate. These aren’t on the T.R.U.E. test.”
Decyl glucoside is another frequent culprit that is not included in commercial patch test kits. “It’s really an important emerging allergen,” said Dr. Warshaw, noting that it commonly cross-reacts with coco and lauryl glucoside, frequently found in fragrance-free products. “It’s always humbling when we find the allergen in the product we’ve recommended to our patients.”
Other important allergens not on the T.R.U.E. test include propolis, tocopherol, oxybenzone, and many surfactants and botanicals.
In order to avoid a confounding reaction to aluminum, Dr. Warshaw recommends testing using plastic-backed test chambers, such as IQ chambers, rather than Finn chambers, which are aluminum backed.
When working with families to track down allergens in the pediatric population, Dr. Warshaw adjusts her approach from what she would use for adults.
“What do I do differently in kids? First of all, I set expectations for children and parents,” she said. Some of the most frequent parental questions deal with food allergies, so she allots time to explain the rationale for not testing for food allergens when allergic contact dermatitis is suspected.
For many patients, “I try and frame that there is probably baseline eczema, and our goal is to try to figure out if there is an allergy in addition to that that is contributing to the flares,” she said. She makes sure to convey that “all it takes is one exposure every 3 weeks; that will keep this reaction going.”
However, she’s judicious in interpreting equivocal results. “I feel a responsibility not to label children with an allergy” if results are unclear. Finally, providing enough time is key, said Dr. Warshaw, who allots an hour for reviewing final testing results.
The take-home points? It’s worthwhile to patch test children, since over half of children will have at least one RPPT. Also, contact dermatitis can be an overlay on preexisting allergic dermatitis, so patch testing can still be helpful for these children. Supplemental allergens are important in patch testing, “especially in children with a negative test to a screening series,” Dr. Warshaw said.
She recommended accessing the Contact Allergen Management Program (CAMP) database, found on the American Contact Dermatitis Society website. The list is a searchable database that generates a list of “safe” products that don’t contain a given allergen. This resource is available for society members, but a member’s access code can be shared among faculty members at academic institutions, she said. Patients can also be given unique codes that will give them access for life, so they can use the CAMP database on a computer or via a smartphone app.
Dr. Warshaw reported no relevant financial disclosures.
On Twitter @karioakes
MINNEAPOLIS – When it comes to allergic contact dermatitis in children, the answer is sometimes hiding in plain sight. Cleansers, moisturizers, shampoos, detergents – all can contain ingredients that provoke significant reactions, yet many of these ingredients are not on the most common testing panels.
Erin Warshaw, MD, professor of dermatology at the University of Minnesota, reviewed common but often unsuspected causes of allergic dermatitis in the pediatric population at the annual meeting of the Society for Pediatric Dermatology.
Even some hypoallergenic and frequently recommended products can contain preservatives and other ingredients that provoke allergic reactions, according to Dr. Warshaw. A chief culprit is methylisothiazolinone (MI), a preservative that came into common use as formaldehyde has been gradually phased out.
“If there’s anything I could emphasize from this talk, it’s MI, MI, MI. This is the major epidemic of our time in the contact dermatitis world,” Dr. Warshaw said. Upcoming publications, she added, will place MI in the top five most common contact allergens. “MI is in everything, including things you would think would be hypoallergenic,” she said. She recommended looking at ingredient labels with a keen eye when making testing decisions.
Despite MI’s status as a frequent culprit, it’s not an allergen that appears on common test kits, Dr. Warshaw pointed out. For example, it’s absent from one of the most commonly used test kits, the Thin-Layer Rapid Use Epicutaneous Patch (T.R.U.E. test).
The T.R.U.E. test, said Dr. Warshaw, has reasonable sensitivity – it can detect 71% of relevant positive patch tests (RPPTs) in children. However, she added, a recent study showed that about 23% of children reacted to a supplemental allergen. “That’s significant. One quarter of these individuals only reacted to a preservative … or a sunscreen, or an acrylate. These aren’t on the T.R.U.E. test.”
Decyl glucoside is another frequent culprit that is not included in commercial patch test kits. “It’s really an important emerging allergen,” said Dr. Warshaw, noting that it commonly cross-reacts with coco and lauryl glucoside, frequently found in fragrance-free products. “It’s always humbling when we find the allergen in the product we’ve recommended to our patients.”
Other important allergens not on the T.R.U.E. test include propolis, tocopherol, oxybenzone, and many surfactants and botanicals.
In order to avoid a confounding reaction to aluminum, Dr. Warshaw recommends testing using plastic-backed test chambers, such as IQ chambers, rather than Finn chambers, which are aluminum backed.
When working with families to track down allergens in the pediatric population, Dr. Warshaw adjusts her approach from what she would use for adults.
“What do I do differently in kids? First of all, I set expectations for children and parents,” she said. Some of the most frequent parental questions deal with food allergies, so she allots time to explain the rationale for not testing for food allergens when allergic contact dermatitis is suspected.
For many patients, “I try and frame that there is probably baseline eczema, and our goal is to try to figure out if there is an allergy in addition to that that is contributing to the flares,” she said. She makes sure to convey that “all it takes is one exposure every 3 weeks; that will keep this reaction going.”
However, she’s judicious in interpreting equivocal results. “I feel a responsibility not to label children with an allergy” if results are unclear. Finally, providing enough time is key, said Dr. Warshaw, who allots an hour for reviewing final testing results.
The take-home points? It’s worthwhile to patch test children, since over half of children will have at least one RPPT. Also, contact dermatitis can be an overlay on preexisting allergic dermatitis, so patch testing can still be helpful for these children. Supplemental allergens are important in patch testing, “especially in children with a negative test to a screening series,” Dr. Warshaw said.
She recommended accessing the Contact Allergen Management Program (CAMP) database, found on the American Contact Dermatitis Society website. The list is a searchable database that generates a list of “safe” products that don’t contain a given allergen. This resource is available for society members, but a member’s access code can be shared among faculty members at academic institutions, she said. Patients can also be given unique codes that will give them access for life, so they can use the CAMP database on a computer or via a smartphone app.
Dr. Warshaw reported no relevant financial disclosures.
On Twitter @karioakes
EXPERT ANALYSIS FROM THE SPD ANNUAL MEETING
Possible Downside to Cloth Diapers: Bullous Diaper Dermatitis
MINNEAPOLIS – A small study of cloth diaper–wearing toddlers with unusual vesiculobullous and erosive lesions found that the rashes fully resolved with aggressive barrier cream application and a switch to disposable diapers.
The four patients had previously received aggressive work-ups, including biopsy in some cases; all had received systemic antibiotics. Katya L. Harfmann, MD, a pediatric dermatologist at Nationwide Children’s Hospital in Columbus, Ohio, was the lead author in a poster presentation at the annual meeting of the Society for Pediatric Dermatology.
The toddlers, aged 17 months to 2 years, had diaper dermatitis of several weeks’ to several months’ duration, with a presentation of vesicles, bullae, and erosions. All of the children had been placed in cloth diapers since birth. The patients, three of them male, had undergone work-ups that included bacterial culture for three patients, herpes simplex virus (HSV) polymerase chain reaction (PCR) testing for three patients, and blood work for two patients. HSV cultures and viral cultures were each performed on one patient. With the exception of one bacterial culture returning methicillin-sensitive Staphylococcus aureus (MSSA), all results were negative.
Two patients underwent biopsies. One biopsy was reported as “spongiform dermatitis,” while the other was read as a “nonspecific ulcer.”
A variety of treatments had been tried for the children. All of the children had received systemic antibiotics; two received systemic antivirals as well. Two patients each received topical steroids and topical antibacterials, and one patient also received topical dapsone. Many treatments were given “in repetitive courses, without improvement in the lesions,” wrote Dr. Harfmann and her coauthor.
The families were advised to switch to exclusive use of disposable diapers and to begin frequent use of a zinc oxide–based thick diaper paste. For all patients, the diaper dermatitis completely resolved within as little as 2 weeks.
The medical literature documents an increased risk of diaper dermatitis with cloth diaper use. “Despite this knowledge in the medical community, nearly half of cloth diaper–using parents select cloth diapers with the assumption that diaper rash is less frequent with their usage,” the researchers noted.
They pointed out that bullae in the diaper region are often thought to be associated with such infectious conditions as impetigo and herpes simplex infection, and can also be associated with immunobullous disorders. Diaper changes are less frequent in older children, though, giving the opportunity for prolonged contact with the irritating chemicals in feces and urine. This prolonged contact, exacerbated by the moister environment of a cloth diaper, may account for the unusual, severe presentation seen in these cases.
Also, the three boys had vesicular lesions on their testicles and penis. “It is possible that the thinner skin in these areas has a lower irritation threshold or that the redundancy of skin often seen on the penile shaft leads to trapping of irritants with extended diaper use,” they wrote.
“An empiric trial of disposable diapers exclusively with aggressive barrier cream application for several weeks may eliminate the need for more invasive procedures and laboratory tests,” wrote Dr. Harfmann and her coauthor.
They reported no conflicts of interest.
MINNEAPOLIS – A small study of cloth diaper–wearing toddlers with unusual vesiculobullous and erosive lesions found that the rashes fully resolved with aggressive barrier cream application and a switch to disposable diapers.
The four patients had previously received aggressive work-ups, including biopsy in some cases; all had received systemic antibiotics. Katya L. Harfmann, MD, a pediatric dermatologist at Nationwide Children’s Hospital in Columbus, Ohio, was the lead author in a poster presentation at the annual meeting of the Society for Pediatric Dermatology.
The toddlers, aged 17 months to 2 years, had diaper dermatitis of several weeks’ to several months’ duration, with a presentation of vesicles, bullae, and erosions. All of the children had been placed in cloth diapers since birth. The patients, three of them male, had undergone work-ups that included bacterial culture for three patients, herpes simplex virus (HSV) polymerase chain reaction (PCR) testing for three patients, and blood work for two patients. HSV cultures and viral cultures were each performed on one patient. With the exception of one bacterial culture returning methicillin-sensitive Staphylococcus aureus (MSSA), all results were negative.
Two patients underwent biopsies. One biopsy was reported as “spongiform dermatitis,” while the other was read as a “nonspecific ulcer.”
A variety of treatments had been tried for the children. All of the children had received systemic antibiotics; two received systemic antivirals as well. Two patients each received topical steroids and topical antibacterials, and one patient also received topical dapsone. Many treatments were given “in repetitive courses, without improvement in the lesions,” wrote Dr. Harfmann and her coauthor.
The families were advised to switch to exclusive use of disposable diapers and to begin frequent use of a zinc oxide–based thick diaper paste. For all patients, the diaper dermatitis completely resolved within as little as 2 weeks.
The medical literature documents an increased risk of diaper dermatitis with cloth diaper use. “Despite this knowledge in the medical community, nearly half of cloth diaper–using parents select cloth diapers with the assumption that diaper rash is less frequent with their usage,” the researchers noted.
They pointed out that bullae in the diaper region are often thought to be associated with such infectious conditions as impetigo and herpes simplex infection, and can also be associated with immunobullous disorders. Diaper changes are less frequent in older children, though, giving the opportunity for prolonged contact with the irritating chemicals in feces and urine. This prolonged contact, exacerbated by the moister environment of a cloth diaper, may account for the unusual, severe presentation seen in these cases.
Also, the three boys had vesicular lesions on their testicles and penis. “It is possible that the thinner skin in these areas has a lower irritation threshold or that the redundancy of skin often seen on the penile shaft leads to trapping of irritants with extended diaper use,” they wrote.
“An empiric trial of disposable diapers exclusively with aggressive barrier cream application for several weeks may eliminate the need for more invasive procedures and laboratory tests,” wrote Dr. Harfmann and her coauthor.
They reported no conflicts of interest.
MINNEAPOLIS – A small study of cloth diaper–wearing toddlers with unusual vesiculobullous and erosive lesions found that the rashes fully resolved with aggressive barrier cream application and a switch to disposable diapers.
The four patients had previously received aggressive work-ups, including biopsy in some cases; all had received systemic antibiotics. Katya L. Harfmann, MD, a pediatric dermatologist at Nationwide Children’s Hospital in Columbus, Ohio, was the lead author in a poster presentation at the annual meeting of the Society for Pediatric Dermatology.
The toddlers, aged 17 months to 2 years, had diaper dermatitis of several weeks’ to several months’ duration, with a presentation of vesicles, bullae, and erosions. All of the children had been placed in cloth diapers since birth. The patients, three of them male, had undergone work-ups that included bacterial culture for three patients, herpes simplex virus (HSV) polymerase chain reaction (PCR) testing for three patients, and blood work for two patients. HSV cultures and viral cultures were each performed on one patient. With the exception of one bacterial culture returning methicillin-sensitive Staphylococcus aureus (MSSA), all results were negative.
Two patients underwent biopsies. One biopsy was reported as “spongiform dermatitis,” while the other was read as a “nonspecific ulcer.”
A variety of treatments had been tried for the children. All of the children had received systemic antibiotics; two received systemic antivirals as well. Two patients each received topical steroids and topical antibacterials, and one patient also received topical dapsone. Many treatments were given “in repetitive courses, without improvement in the lesions,” wrote Dr. Harfmann and her coauthor.
The families were advised to switch to exclusive use of disposable diapers and to begin frequent use of a zinc oxide–based thick diaper paste. For all patients, the diaper dermatitis completely resolved within as little as 2 weeks.
The medical literature documents an increased risk of diaper dermatitis with cloth diaper use. “Despite this knowledge in the medical community, nearly half of cloth diaper–using parents select cloth diapers with the assumption that diaper rash is less frequent with their usage,” the researchers noted.
They pointed out that bullae in the diaper region are often thought to be associated with such infectious conditions as impetigo and herpes simplex infection, and can also be associated with immunobullous disorders. Diaper changes are less frequent in older children, though, giving the opportunity for prolonged contact with the irritating chemicals in feces and urine. This prolonged contact, exacerbated by the moister environment of a cloth diaper, may account for the unusual, severe presentation seen in these cases.
Also, the three boys had vesicular lesions on their testicles and penis. “It is possible that the thinner skin in these areas has a lower irritation threshold or that the redundancy of skin often seen on the penile shaft leads to trapping of irritants with extended diaper use,” they wrote.
“An empiric trial of disposable diapers exclusively with aggressive barrier cream application for several weeks may eliminate the need for more invasive procedures and laboratory tests,” wrote Dr. Harfmann and her coauthor.
They reported no conflicts of interest.
AT THE SPD ANNUAL MEETING