User login
Rhinovirus most often caused HA-VRIs in two hospitals
Health care–associated viral respiratory infections (HA-VRIs) were common in two pediatric hospitals, with rhinovirus the most frequent cause of the infections in a 3-year analysis.
The incidence rate of laboratory-confirmed HA-VRIs was 1.29/1,000 patient-days in an examination of the hospitals’ patient data. Forty-eight percent of all 323 HA-VRI cases were caused by rhinovirus, with an overall incidence rate of 0.72/1,000 patient-days. Additionally, rhinovirus was the most frequently identified virus in cases of HA-VRI in all units of both hospitals, followed by parainfluenza virus and respiratory syncytial virus. An exception was the medical/surgical ward of Steven and Alexandra Cohen Children’s Medical Center (CCMC) of New York; in this unit of the CCMC, the incidence rate of parainfluenza virus was higher than that of rhinovirus (0.21/1,000 patient-days vs. 0.15/1,000 patient-days) (J Ped Inf Dis. 2016. doi: 10.1093/jpids/piw072).
The researchers used infection prevention and control surveillance databases from Montreal Children’s Hospital (MCH) in Quebec and the CCMC to identify HA-VRIs that occurred between April 1, 2010, and March 31, 2013, In both hospitals, HAIs were attributed to the unit to which the patient was admitted at the time of transmission. Both hospitals used a multiplex nucleic acid amplification test for respiratory virus detection on nasopharyngeal swabs or aspirates.
“An HA-VRI with an onset of symptoms after hospital discharge would be detected and included only for patients who presented to the emergency department or were readmitted for VRI and tested,” according to Caroline Quach, MD, of the Montreal Children’s Hospital, McGill University Health Centre, Quebec, and her colleagues.
The HA-VRI rate was 1.91/1,000 patient-days at Montreal Children’s Hospital, compared with 0.80/1,000 patient-days at the CCMC (P less than .0001). At the CCMC, the HA-VRI incidence rate was lowest in the neonatal ICU, but at Montgomery Children’s Hospital, the hematology/oncology ward had the lowest rate of HA-VRI.
Having less than 50% single rooms in a given unit was associated with a statistically significantly higher rate of HA-VRI, after the investigators adjusted for unit type and took the correlation of HA-VRI rates within a hospital into consideration. The study authors’ model predicted that units with less than 50% single rooms have 1.33 times higher HA-VRI rates than units with at least 50% single rooms, regardless of unit type.
Dr. Quach has received funding from GlaxoSmithKline, Pfizer, Sage, and AbbVie for an unrelated research project, while the other authors disclosed no financial relationships.
Health care–associated viral respiratory infections (HA-VRIs) were common in two pediatric hospitals, with rhinovirus the most frequent cause of the infections in a 3-year analysis.
The incidence rate of laboratory-confirmed HA-VRIs was 1.29/1,000 patient-days in an examination of the hospitals’ patient data. Forty-eight percent of all 323 HA-VRI cases were caused by rhinovirus, with an overall incidence rate of 0.72/1,000 patient-days. Additionally, rhinovirus was the most frequently identified virus in cases of HA-VRI in all units of both hospitals, followed by parainfluenza virus and respiratory syncytial virus. An exception was the medical/surgical ward of Steven and Alexandra Cohen Children’s Medical Center (CCMC) of New York; in this unit of the CCMC, the incidence rate of parainfluenza virus was higher than that of rhinovirus (0.21/1,000 patient-days vs. 0.15/1,000 patient-days) (J Ped Inf Dis. 2016. doi: 10.1093/jpids/piw072).
The researchers used infection prevention and control surveillance databases from Montreal Children’s Hospital (MCH) in Quebec and the CCMC to identify HA-VRIs that occurred between April 1, 2010, and March 31, 2013, In both hospitals, HAIs were attributed to the unit to which the patient was admitted at the time of transmission. Both hospitals used a multiplex nucleic acid amplification test for respiratory virus detection on nasopharyngeal swabs or aspirates.
“An HA-VRI with an onset of symptoms after hospital discharge would be detected and included only for patients who presented to the emergency department or were readmitted for VRI and tested,” according to Caroline Quach, MD, of the Montreal Children’s Hospital, McGill University Health Centre, Quebec, and her colleagues.
The HA-VRI rate was 1.91/1,000 patient-days at Montreal Children’s Hospital, compared with 0.80/1,000 patient-days at the CCMC (P less than .0001). At the CCMC, the HA-VRI incidence rate was lowest in the neonatal ICU, but at Montgomery Children’s Hospital, the hematology/oncology ward had the lowest rate of HA-VRI.
Having less than 50% single rooms in a given unit was associated with a statistically significantly higher rate of HA-VRI, after the investigators adjusted for unit type and took the correlation of HA-VRI rates within a hospital into consideration. The study authors’ model predicted that units with less than 50% single rooms have 1.33 times higher HA-VRI rates than units with at least 50% single rooms, regardless of unit type.
Dr. Quach has received funding from GlaxoSmithKline, Pfizer, Sage, and AbbVie for an unrelated research project, while the other authors disclosed no financial relationships.
Health care–associated viral respiratory infections (HA-VRIs) were common in two pediatric hospitals, with rhinovirus the most frequent cause of the infections in a 3-year analysis.
The incidence rate of laboratory-confirmed HA-VRIs was 1.29/1,000 patient-days in an examination of the hospitals’ patient data. Forty-eight percent of all 323 HA-VRI cases were caused by rhinovirus, with an overall incidence rate of 0.72/1,000 patient-days. Additionally, rhinovirus was the most frequently identified virus in cases of HA-VRI in all units of both hospitals, followed by parainfluenza virus and respiratory syncytial virus. An exception was the medical/surgical ward of Steven and Alexandra Cohen Children’s Medical Center (CCMC) of New York; in this unit of the CCMC, the incidence rate of parainfluenza virus was higher than that of rhinovirus (0.21/1,000 patient-days vs. 0.15/1,000 patient-days) (J Ped Inf Dis. 2016. doi: 10.1093/jpids/piw072).
The researchers used infection prevention and control surveillance databases from Montreal Children’s Hospital (MCH) in Quebec and the CCMC to identify HA-VRIs that occurred between April 1, 2010, and March 31, 2013, In both hospitals, HAIs were attributed to the unit to which the patient was admitted at the time of transmission. Both hospitals used a multiplex nucleic acid amplification test for respiratory virus detection on nasopharyngeal swabs or aspirates.
“An HA-VRI with an onset of symptoms after hospital discharge would be detected and included only for patients who presented to the emergency department or were readmitted for VRI and tested,” according to Caroline Quach, MD, of the Montreal Children’s Hospital, McGill University Health Centre, Quebec, and her colleagues.
The HA-VRI rate was 1.91/1,000 patient-days at Montreal Children’s Hospital, compared with 0.80/1,000 patient-days at the CCMC (P less than .0001). At the CCMC, the HA-VRI incidence rate was lowest in the neonatal ICU, but at Montgomery Children’s Hospital, the hematology/oncology ward had the lowest rate of HA-VRI.
Having less than 50% single rooms in a given unit was associated with a statistically significantly higher rate of HA-VRI, after the investigators adjusted for unit type and took the correlation of HA-VRI rates within a hospital into consideration. The study authors’ model predicted that units with less than 50% single rooms have 1.33 times higher HA-VRI rates than units with at least 50% single rooms, regardless of unit type.
Dr. Quach has received funding from GlaxoSmithKline, Pfizer, Sage, and AbbVie for an unrelated research project, while the other authors disclosed no financial relationships.
FROM THE JOURNAL OF THE PEDIATRIC INFECTIOUS DISEASES SOCIETY
Key clinical point:
Major finding: The incidence rate of HA-VRIs was 1.29/1,000 patient-days in an examination of two pediatric hospitals’ patient data between April 1, 2010, and March 31, 2013.
Data source: A retrospective comparison of two hospitals’ 3 years of infection prevention and control surveillance data.
Disclosures: Dr. Quach has received funding from GlaxoSmithKline, Pfizer, Sage, and AbbVie for an unrelated research project, while the other authors disclosed no relevant financial relationships.
Streptococcal pneumonia’s resistance to macrolides increasing
The incidence of resistance of Streptococcus pneumoniae to the macrolide azithromycin – one of the most commonly prescribed antibiotics for treating pneumonia – was almost 50% in 2014, according to a report by Kara Keedy, PhD, executive director of microbiology at Cempra Pharmaceuticals, and her colleagues.
The researchers prospectively collected and investigated 4,567 nonreplicative community-acquired bacterial pneumonia (CABP) S. pneumoniae isolates between 2008 and 2014 in the United States, according to the report presented as a poster at IDWeek 2016. The isolates were tested for susceptibility by broth microdilution methods, according to Clinical and Laboratory Standards Institute breakpoint criteria. Macrolide resistance rates were based on azithromycin and/or clarithromycin minimal inhibitory concentrations as available, with only data on azithromycin having been collected in 2014.
The overall resistance of S. pneumoniae to azithromycin exceeded 30% in all of the nine geographical divisions of the Centers for Disease Control and Prevention (CDC), with the high-level resistance of this bacterial cause of CABP to azithromycin having been greater than 25% in eight of the CDC divisions.
The co-resistance of S. pneumoniae to azithromycin and penicillin was highest in the CDC’s East South Central division in 2014. The regions with the largest percentages of isolates with high-level macrolide resistance were the East South Central (43.2%), the West South Central (38.1%), and the Mid-Atlantic (35.0%). The regions with the largest percentages of overall macrolide resistance were the West South Central (62.9%), the East South Central (56.8%), and the South Atlantic (53.2%).
The analysis also determined that the 2014 overall rate of macrolide resistance in S. pneumoniae in the United States of 48.4% is higher than it was for any of the four earlier years examined. In 2008, 2009, 2010, and 2011, those macrolide resistance rates were 39.7%, 40.2%, 37.1%, and 44.3%, respectively.
The researchers concluded that S. pneumoniae is the most common bacterial cause of CABP and that antibiotic resistance to it is “a significant clinical challenge as highlighted by” the CDC having listed it as a threatening pathogen in the urgent category. Dr. Keedy and her associates noted that in the United States, macrolides, amoxicillin/clavulanate, and respiratory fluoroquinolones are the most frequent agents prescribed to treat almost all community-acquired respiratory infections.
“Macrolide resistance in S. pneumoniae is continuing to increase in the U.S.,” the researchers reported in the poster. “Both low- and high-level macrolide resistance have been reported to cause clinical failures and other negative outcomes including longer hospital stays and higher costs.”
The study also examined the abilities of several other drugs, including the fourth-generation macrolide solithromycin, to inhibit S. pneumoniae isolates. Solithromycin does not yet have approved Clinical and Laboratory Standards Institute breakpoints, so only minimum inhibitory concentrations (MICs) were presented.
According to the study, more than 50% of S. pneumoniae isolates were inhibited by 0.008 mcg/mL solithromycin. Additionally, solithromycin had one of the lowest MICs against S. pneumoniae of all of the drugs tested in the study. The higher end of the MICs against S. pneumoniae for solithromycin and moxifloxacin was 0.25, which was lower than the higher end of the MICs for any of the other drugs tested against S. pneumoniae isolates.
Solithromycin is the first fluoroketolide in Phase III clinical development. It “shows activity against all macrolide-resistant strains of S. pneumoniae isolates, irrespective of the location in the U.S.,” according to the poster.
The data included in the poster was extracted from a global study by JMI Laboratories. Cempra funded this study. Dr. Keedy and the other authors of the poster are employees of Cempra.
How many of us have heard that line? How many of us have done that ourselves? Did you do that today? Dr. Keedy and her colleagues report that in all geographic areas in the US, resistance to azithromycin for S pneumoniae now exceeds 30%. On average, 48.4% of S pneumoniae isolates display resistance in the US. Without antibiotic stewardship by all of us, azithromycin, along with other antibiotics, will become an expensive placebo.
How many of us have heard that line? How many of us have done that ourselves? Did you do that today? Dr. Keedy and her colleagues report that in all geographic areas in the US, resistance to azithromycin for S pneumoniae now exceeds 30%. On average, 48.4% of S pneumoniae isolates display resistance in the US. Without antibiotic stewardship by all of us, azithromycin, along with other antibiotics, will become an expensive placebo.
How many of us have heard that line? How many of us have done that ourselves? Did you do that today? Dr. Keedy and her colleagues report that in all geographic areas in the US, resistance to azithromycin for S pneumoniae now exceeds 30%. On average, 48.4% of S pneumoniae isolates display resistance in the US. Without antibiotic stewardship by all of us, azithromycin, along with other antibiotics, will become an expensive placebo.
The incidence of resistance of Streptococcus pneumoniae to the macrolide azithromycin – one of the most commonly prescribed antibiotics for treating pneumonia – was almost 50% in 2014, according to a report by Kara Keedy, PhD, executive director of microbiology at Cempra Pharmaceuticals, and her colleagues.
The researchers prospectively collected and investigated 4,567 nonreplicative community-acquired bacterial pneumonia (CABP) S. pneumoniae isolates between 2008 and 2014 in the United States, according to the report presented as a poster at IDWeek 2016. The isolates were tested for susceptibility by broth microdilution methods, according to Clinical and Laboratory Standards Institute breakpoint criteria. Macrolide resistance rates were based on azithromycin and/or clarithromycin minimal inhibitory concentrations as available, with only data on azithromycin having been collected in 2014.
The overall resistance of S. pneumoniae to azithromycin exceeded 30% in all of the nine geographical divisions of the Centers for Disease Control and Prevention (CDC), with the high-level resistance of this bacterial cause of CABP to azithromycin having been greater than 25% in eight of the CDC divisions.
The co-resistance of S. pneumoniae to azithromycin and penicillin was highest in the CDC’s East South Central division in 2014. The regions with the largest percentages of isolates with high-level macrolide resistance were the East South Central (43.2%), the West South Central (38.1%), and the Mid-Atlantic (35.0%). The regions with the largest percentages of overall macrolide resistance were the West South Central (62.9%), the East South Central (56.8%), and the South Atlantic (53.2%).
The analysis also determined that the 2014 overall rate of macrolide resistance in S. pneumoniae in the United States of 48.4% is higher than it was for any of the four earlier years examined. In 2008, 2009, 2010, and 2011, those macrolide resistance rates were 39.7%, 40.2%, 37.1%, and 44.3%, respectively.
The researchers concluded that S. pneumoniae is the most common bacterial cause of CABP and that antibiotic resistance to it is “a significant clinical challenge as highlighted by” the CDC having listed it as a threatening pathogen in the urgent category. Dr. Keedy and her associates noted that in the United States, macrolides, amoxicillin/clavulanate, and respiratory fluoroquinolones are the most frequent agents prescribed to treat almost all community-acquired respiratory infections.
“Macrolide resistance in S. pneumoniae is continuing to increase in the U.S.,” the researchers reported in the poster. “Both low- and high-level macrolide resistance have been reported to cause clinical failures and other negative outcomes including longer hospital stays and higher costs.”
The study also examined the abilities of several other drugs, including the fourth-generation macrolide solithromycin, to inhibit S. pneumoniae isolates. Solithromycin does not yet have approved Clinical and Laboratory Standards Institute breakpoints, so only minimum inhibitory concentrations (MICs) were presented.
According to the study, more than 50% of S. pneumoniae isolates were inhibited by 0.008 mcg/mL solithromycin. Additionally, solithromycin had one of the lowest MICs against S. pneumoniae of all of the drugs tested in the study. The higher end of the MICs against S. pneumoniae for solithromycin and moxifloxacin was 0.25, which was lower than the higher end of the MICs for any of the other drugs tested against S. pneumoniae isolates.
Solithromycin is the first fluoroketolide in Phase III clinical development. It “shows activity against all macrolide-resistant strains of S. pneumoniae isolates, irrespective of the location in the U.S.,” according to the poster.
The data included in the poster was extracted from a global study by JMI Laboratories. Cempra funded this study. Dr. Keedy and the other authors of the poster are employees of Cempra.
The incidence of resistance of Streptococcus pneumoniae to the macrolide azithromycin – one of the most commonly prescribed antibiotics for treating pneumonia – was almost 50% in 2014, according to a report by Kara Keedy, PhD, executive director of microbiology at Cempra Pharmaceuticals, and her colleagues.
The researchers prospectively collected and investigated 4,567 nonreplicative community-acquired bacterial pneumonia (CABP) S. pneumoniae isolates between 2008 and 2014 in the United States, according to the report presented as a poster at IDWeek 2016. The isolates were tested for susceptibility by broth microdilution methods, according to Clinical and Laboratory Standards Institute breakpoint criteria. Macrolide resistance rates were based on azithromycin and/or clarithromycin minimal inhibitory concentrations as available, with only data on azithromycin having been collected in 2014.
The overall resistance of S. pneumoniae to azithromycin exceeded 30% in all of the nine geographical divisions of the Centers for Disease Control and Prevention (CDC), with the high-level resistance of this bacterial cause of CABP to azithromycin having been greater than 25% in eight of the CDC divisions.
The co-resistance of S. pneumoniae to azithromycin and penicillin was highest in the CDC’s East South Central division in 2014. The regions with the largest percentages of isolates with high-level macrolide resistance were the East South Central (43.2%), the West South Central (38.1%), and the Mid-Atlantic (35.0%). The regions with the largest percentages of overall macrolide resistance were the West South Central (62.9%), the East South Central (56.8%), and the South Atlantic (53.2%).
The analysis also determined that the 2014 overall rate of macrolide resistance in S. pneumoniae in the United States of 48.4% is higher than it was for any of the four earlier years examined. In 2008, 2009, 2010, and 2011, those macrolide resistance rates were 39.7%, 40.2%, 37.1%, and 44.3%, respectively.
The researchers concluded that S. pneumoniae is the most common bacterial cause of CABP and that antibiotic resistance to it is “a significant clinical challenge as highlighted by” the CDC having listed it as a threatening pathogen in the urgent category. Dr. Keedy and her associates noted that in the United States, macrolides, amoxicillin/clavulanate, and respiratory fluoroquinolones are the most frequent agents prescribed to treat almost all community-acquired respiratory infections.
“Macrolide resistance in S. pneumoniae is continuing to increase in the U.S.,” the researchers reported in the poster. “Both low- and high-level macrolide resistance have been reported to cause clinical failures and other negative outcomes including longer hospital stays and higher costs.”
The study also examined the abilities of several other drugs, including the fourth-generation macrolide solithromycin, to inhibit S. pneumoniae isolates. Solithromycin does not yet have approved Clinical and Laboratory Standards Institute breakpoints, so only minimum inhibitory concentrations (MICs) were presented.
According to the study, more than 50% of S. pneumoniae isolates were inhibited by 0.008 mcg/mL solithromycin. Additionally, solithromycin had one of the lowest MICs against S. pneumoniae of all of the drugs tested in the study. The higher end of the MICs against S. pneumoniae for solithromycin and moxifloxacin was 0.25, which was lower than the higher end of the MICs for any of the other drugs tested against S. pneumoniae isolates.
Solithromycin is the first fluoroketolide in Phase III clinical development. It “shows activity against all macrolide-resistant strains of S. pneumoniae isolates, irrespective of the location in the U.S.,” according to the poster.
The data included in the poster was extracted from a global study by JMI Laboratories. Cempra funded this study. Dr. Keedy and the other authors of the poster are employees of Cempra.
FROM IDWEEK 2016
Key clinical point:
Major finding: S. pneumoniae isolates’ average resistance to the macrolide azithromycin was 48.4% in 2014.
Data source: A prospective collection and investigation of 4,567 non-replicative community-acquired bacterial pneumonia isolates.
Disclosures: The data included in the poster was extracted from a global study by JMI Laboratories. Cempra funded this study. Dr. Keedy and the other authors of the poster are employees of Cempra.
Initial outcomes of PERT at Cleveland Clinic
LOS ANGELES – Initial outcomes measures are beginning to emerge from Pulmonary Embolism Response Teams.
Members of the Cleveland Clinic’s PERT, which was established in 2014, presented some of their preliminary data during a presentation at the CHEST annual meeting.
The concept behind the PERT is to rapidly mobilize a team with varied expertise helpful for treating patients with pulmonary embolisms (PEs). While the PERT “can be activated by any (clinician) for any patient, even low-risk patients ... those with submassive and massive PEs [intermediate- and high-risk patients]” are the target patients, said Dr. Mahar of the Cleveland Clinic.
The first PERT was created at Massachusetts General Hospital in Boston in 2012, according to the National Consortium of Pulmonary Embolism Response Team’s website. As of May 2015, the PERT model has been adopted by physicians and health care professionals from more than 40 institutions.
Dr. Mahar reported that the Cleveland Clinic’s PERT is activated through a single pager that resides with a vascular medicine fellow during the day and a critical care fellow at night. When paged, the fellow promptly evaluates the patient and ensures a complete basic work-up, which includes an ECG, cardiac enzymes, N-terminal pro b-type natriuretic peptide, lower-extremity deep vein thrombosis scans, transthoracic echocardiogram, and confirmatory CT/PE protocol or ventilation/perfusion scan.
Based on the simplified Pulmonary Embolism Severity Index and Bova scores, the patient is risk stratified and the patient’s indications, and relative and absolute contraindications to advanced therapies are reviewed. The fellow next sends a group notification to the PERT via email and text message. The team then convenes online for a virtual meeting and case presentation that includes sharing of lab and test results and images.
The process sounds complex, but the surgeon, interventional radiologist, vascular medicine specialist, and cardiologist are on call and simultaneously get the message and respond, Dr. Mahar said. With a team approach, the decision to use advanced therapies – systemic lytics, surgery, catheter-directed lysis and extracorporeal membrane oxygenation – is expedited. “For example, over the last 2 years, four out of four patients who underwent surgical embolectomies had good outcomes without any deaths,” he said.
Based on a retrospective chart review from October 2014 through August 2016, Cleveland Clinic’s PERT had been activated for 134 patients, 112 of whom were found to have PEs, Dr. Mahar said during his presentation at the annual meeting of the American College of Chest Physicians (CHEST).
The number of low risk, submassive, and massive PEs were 14 (12%), 76 (68%), and 22 (20%), respectively. Just over half of the PE patients, 55% (60 patients), were treated with anticoagulation therapy alone. Inferior vena cava filters were placed in 32 patients (29%); 14 patients received catheter-directed thrombolysis, 3 received a suction thrombectomy, and 4 received a surgical embolectomy.
The 30-day all-cause mortality rate was 9%; the deaths occurred in six patients who had massive PEs, three patients with submassive PEs, and one patient with a low-risk PE. Six of the patients who died had been treated with anticoagulation, two had received catheter-directed thrombolysis, and one had received a full dose of systemic thrombolysis.
Bleeding complications occurred in 10 patients, 6 of whom were treated with anticoagulation alone and 4 of whom underwent catheter-directed thrombolysis.
Cleveland Clinic is a large entity with multiple resources, but the principles of PERT can be applied in smaller facilities, as well, according to Gustavo A. Heresi-Davila, MD, medical director of the Cleveland Clinic’s pulmonary thromboendarterectomy program and the lead researcher for the PERT project at the clinic. “I would emphasize the notion that a PERT has to be multidisciplinary, as people with different backgrounds and expertise bring complementary talent to the discussion of each case. I would not minimize the challenges of assembling such a team,” he said during an interview following the meeting.
The moderator of the meeting session, Robert Schilz, DO, PhD, noted, that the goal of PERT is to determine the best approach for an individual patient based on available resources. To establish a PERT, “you don’t have to be able to put a patient on ECMO [extracorporeal membrane oxygenation] in 15 minutes, and you don’t have to be able to do endarterectomies, embolectomies, and all the catheter-drive techniques emergently. But you do need to have the disposition to have efficient and standardized care, and the solutions may need to be very geographic. What hospital A may do may be very different from hospital B.”
Small hospitals can draw on their available resources, added Dr. Schilz, director of pulmonary vascular disease and lung transplantation at Case Western Reserve University, Cleveland. “Most hospitals have cardiologists on call 24/7, and many have some flavor of interventional radiology; others have clear referral and transfer schemes. Emergency department personnel at small rural hospitals can rapidly identify patients appropriate for transfer.”
Dr. Mahar added that PERTs are already being utilized in smaller hospitals and that he thinks that, in the next 5 years, having a PERT will be the standard protocol.
Dr. Mahar reported no disclosures.
Mary Jo Dales contributed to this report.
LOS ANGELES – Initial outcomes measures are beginning to emerge from Pulmonary Embolism Response Teams.
Members of the Cleveland Clinic’s PERT, which was established in 2014, presented some of their preliminary data during a presentation at the CHEST annual meeting.
The concept behind the PERT is to rapidly mobilize a team with varied expertise helpful for treating patients with pulmonary embolisms (PEs). While the PERT “can be activated by any (clinician) for any patient, even low-risk patients ... those with submassive and massive PEs [intermediate- and high-risk patients]” are the target patients, said Dr. Mahar of the Cleveland Clinic.
The first PERT was created at Massachusetts General Hospital in Boston in 2012, according to the National Consortium of Pulmonary Embolism Response Team’s website. As of May 2015, the PERT model has been adopted by physicians and health care professionals from more than 40 institutions.
Dr. Mahar reported that the Cleveland Clinic’s PERT is activated through a single pager that resides with a vascular medicine fellow during the day and a critical care fellow at night. When paged, the fellow promptly evaluates the patient and ensures a complete basic work-up, which includes an ECG, cardiac enzymes, N-terminal pro b-type natriuretic peptide, lower-extremity deep vein thrombosis scans, transthoracic echocardiogram, and confirmatory CT/PE protocol or ventilation/perfusion scan.
Based on the simplified Pulmonary Embolism Severity Index and Bova scores, the patient is risk stratified and the patient’s indications, and relative and absolute contraindications to advanced therapies are reviewed. The fellow next sends a group notification to the PERT via email and text message. The team then convenes online for a virtual meeting and case presentation that includes sharing of lab and test results and images.
The process sounds complex, but the surgeon, interventional radiologist, vascular medicine specialist, and cardiologist are on call and simultaneously get the message and respond, Dr. Mahar said. With a team approach, the decision to use advanced therapies – systemic lytics, surgery, catheter-directed lysis and extracorporeal membrane oxygenation – is expedited. “For example, over the last 2 years, four out of four patients who underwent surgical embolectomies had good outcomes without any deaths,” he said.
Based on a retrospective chart review from October 2014 through August 2016, Cleveland Clinic’s PERT had been activated for 134 patients, 112 of whom were found to have PEs, Dr. Mahar said during his presentation at the annual meeting of the American College of Chest Physicians (CHEST).
The number of low risk, submassive, and massive PEs were 14 (12%), 76 (68%), and 22 (20%), respectively. Just over half of the PE patients, 55% (60 patients), were treated with anticoagulation therapy alone. Inferior vena cava filters were placed in 32 patients (29%); 14 patients received catheter-directed thrombolysis, 3 received a suction thrombectomy, and 4 received a surgical embolectomy.
The 30-day all-cause mortality rate was 9%; the deaths occurred in six patients who had massive PEs, three patients with submassive PEs, and one patient with a low-risk PE. Six of the patients who died had been treated with anticoagulation, two had received catheter-directed thrombolysis, and one had received a full dose of systemic thrombolysis.
Bleeding complications occurred in 10 patients, 6 of whom were treated with anticoagulation alone and 4 of whom underwent catheter-directed thrombolysis.
Cleveland Clinic is a large entity with multiple resources, but the principles of PERT can be applied in smaller facilities, as well, according to Gustavo A. Heresi-Davila, MD, medical director of the Cleveland Clinic’s pulmonary thromboendarterectomy program and the lead researcher for the PERT project at the clinic. “I would emphasize the notion that a PERT has to be multidisciplinary, as people with different backgrounds and expertise bring complementary talent to the discussion of each case. I would not minimize the challenges of assembling such a team,” he said during an interview following the meeting.
The moderator of the meeting session, Robert Schilz, DO, PhD, noted, that the goal of PERT is to determine the best approach for an individual patient based on available resources. To establish a PERT, “you don’t have to be able to put a patient on ECMO [extracorporeal membrane oxygenation] in 15 minutes, and you don’t have to be able to do endarterectomies, embolectomies, and all the catheter-drive techniques emergently. But you do need to have the disposition to have efficient and standardized care, and the solutions may need to be very geographic. What hospital A may do may be very different from hospital B.”
Small hospitals can draw on their available resources, added Dr. Schilz, director of pulmonary vascular disease and lung transplantation at Case Western Reserve University, Cleveland. “Most hospitals have cardiologists on call 24/7, and many have some flavor of interventional radiology; others have clear referral and transfer schemes. Emergency department personnel at small rural hospitals can rapidly identify patients appropriate for transfer.”
Dr. Mahar added that PERTs are already being utilized in smaller hospitals and that he thinks that, in the next 5 years, having a PERT will be the standard protocol.
Dr. Mahar reported no disclosures.
Mary Jo Dales contributed to this report.
LOS ANGELES – Initial outcomes measures are beginning to emerge from Pulmonary Embolism Response Teams.
Members of the Cleveland Clinic’s PERT, which was established in 2014, presented some of their preliminary data during a presentation at the CHEST annual meeting.
The concept behind the PERT is to rapidly mobilize a team with varied expertise helpful for treating patients with pulmonary embolisms (PEs). While the PERT “can be activated by any (clinician) for any patient, even low-risk patients ... those with submassive and massive PEs [intermediate- and high-risk patients]” are the target patients, said Dr. Mahar of the Cleveland Clinic.
The first PERT was created at Massachusetts General Hospital in Boston in 2012, according to the National Consortium of Pulmonary Embolism Response Team’s website. As of May 2015, the PERT model has been adopted by physicians and health care professionals from more than 40 institutions.
Dr. Mahar reported that the Cleveland Clinic’s PERT is activated through a single pager that resides with a vascular medicine fellow during the day and a critical care fellow at night. When paged, the fellow promptly evaluates the patient and ensures a complete basic work-up, which includes an ECG, cardiac enzymes, N-terminal pro b-type natriuretic peptide, lower-extremity deep vein thrombosis scans, transthoracic echocardiogram, and confirmatory CT/PE protocol or ventilation/perfusion scan.
Based on the simplified Pulmonary Embolism Severity Index and Bova scores, the patient is risk stratified and the patient’s indications, and relative and absolute contraindications to advanced therapies are reviewed. The fellow next sends a group notification to the PERT via email and text message. The team then convenes online for a virtual meeting and case presentation that includes sharing of lab and test results and images.
The process sounds complex, but the surgeon, interventional radiologist, vascular medicine specialist, and cardiologist are on call and simultaneously get the message and respond, Dr. Mahar said. With a team approach, the decision to use advanced therapies – systemic lytics, surgery, catheter-directed lysis and extracorporeal membrane oxygenation – is expedited. “For example, over the last 2 years, four out of four patients who underwent surgical embolectomies had good outcomes without any deaths,” he said.
Based on a retrospective chart review from October 2014 through August 2016, Cleveland Clinic’s PERT had been activated for 134 patients, 112 of whom were found to have PEs, Dr. Mahar said during his presentation at the annual meeting of the American College of Chest Physicians (CHEST).
The number of low risk, submassive, and massive PEs were 14 (12%), 76 (68%), and 22 (20%), respectively. Just over half of the PE patients, 55% (60 patients), were treated with anticoagulation therapy alone. Inferior vena cava filters were placed in 32 patients (29%); 14 patients received catheter-directed thrombolysis, 3 received a suction thrombectomy, and 4 received a surgical embolectomy.
The 30-day all-cause mortality rate was 9%; the deaths occurred in six patients who had massive PEs, three patients with submassive PEs, and one patient with a low-risk PE. Six of the patients who died had been treated with anticoagulation, two had received catheter-directed thrombolysis, and one had received a full dose of systemic thrombolysis.
Bleeding complications occurred in 10 patients, 6 of whom were treated with anticoagulation alone and 4 of whom underwent catheter-directed thrombolysis.
Cleveland Clinic is a large entity with multiple resources, but the principles of PERT can be applied in smaller facilities, as well, according to Gustavo A. Heresi-Davila, MD, medical director of the Cleveland Clinic’s pulmonary thromboendarterectomy program and the lead researcher for the PERT project at the clinic. “I would emphasize the notion that a PERT has to be multidisciplinary, as people with different backgrounds and expertise bring complementary talent to the discussion of each case. I would not minimize the challenges of assembling such a team,” he said during an interview following the meeting.
The moderator of the meeting session, Robert Schilz, DO, PhD, noted, that the goal of PERT is to determine the best approach for an individual patient based on available resources. To establish a PERT, “you don’t have to be able to put a patient on ECMO [extracorporeal membrane oxygenation] in 15 minutes, and you don’t have to be able to do endarterectomies, embolectomies, and all the catheter-drive techniques emergently. But you do need to have the disposition to have efficient and standardized care, and the solutions may need to be very geographic. What hospital A may do may be very different from hospital B.”
Small hospitals can draw on their available resources, added Dr. Schilz, director of pulmonary vascular disease and lung transplantation at Case Western Reserve University, Cleveland. “Most hospitals have cardiologists on call 24/7, and many have some flavor of interventional radiology; others have clear referral and transfer schemes. Emergency department personnel at small rural hospitals can rapidly identify patients appropriate for transfer.”
Dr. Mahar added that PERTs are already being utilized in smaller hospitals and that he thinks that, in the next 5 years, having a PERT will be the standard protocol.
Dr. Mahar reported no disclosures.
Mary Jo Dales contributed to this report.
FROM CHEST 2016
Home oxygen upped survival in PAH with severely impaired DLCO
LOS ANGELES – Pulmonary arterial hypertension (PAH) patients with severely impaired diffusing capacity of the lung for carbon monoxide (DLCO) were much more likely to survive when they received home oxygen therapy, according to a disease registry analysis.
“We all know that supplemental oxygen is widely used with PAH,” said Harrison W. Farber, MD, director of the pulmonary hypertension center at Boston University. But there are practically no data showing that it is successful, and there are even fewer data for patients with PAH who have very low diffusion capacity, he added.
That knowledge gap prompted Dr. Farber and his colleagues to analyze data from the Registry to Evaluate Early and Long-Term PAH Disease Management (REVEAL), the largest disease registry in the world of patients with PAH.
“Patients in that group – the severe DLCO group – who got oxygen had poorer prognostic features but improved overall survival relative to those who didn’t,” Dr. Farber explained during a presentation at the annual meeting of the American College of Chest Physicians. “Based on this, it makes us think that home oxygen, supplemental oxygen treatment, is associated with improved survival in patients, especially those with severe DLCO and PAH.”
The 3,046 patients analyzed by Dr. Farber and his colleagues had World Health Organization Group 1 PAH with right heart catheterization hemodynamic criteria: a mean pulmonary artery pressure greater than 25 mm Hg, a pulmonary capillary wedge pressure less than or equal to 15 mm Hg, and a pulmonary vascular resistance of at least 3 Wood units (WU). Patients were at least 18 years of age and grouped by oxygen use, which was defined as any use at any time from study enrollment to the end of follow-up, and by DLCO group.
A total of 57% of the patients (1,734) received oxygen, and the remaining 43% of the patients (1,312) did not receive oxygen. Among the patients who received oxygen, 71% (1,227) received the therapy continuously, and 24% (408) received oxygen at night only.
The 424 patients with a DLCO of less than 40% were considered to have a severe DLCO impairment. The other two groups comprised 505 patients with a moderate DLCO impairment (at least 40%, but less than 60%) and 844 patients with a mild to normal DLCO (at least 60%). The DLCOs of 1,273 patients analyzed were unknown.
Among those patients with severe DLCO impairment, the risk of death was significantly lower in those who received oxygen, compared with those who did not receive oxygen (hazard ratio, 0.56; P = .0033). Oxygen use was associated with significant improvements in overall survival in both the newly diagnosed (HR, 0.47; P = .029) and previously diagnosed (HR, 0.59; P = .026) severe DLCO cohorts, Dr. Farber said.
Patients receiving oxygen were more likely to be treated with PAH-specific medications, regardless of their DLCO group.
Among the analysis’s limitations was that the lengths of time patients had been undergoing oxygen treatment were unknown. That prevented adjustments for duration of oxygen treatment, according to Dr. Farber.
Dr. Farber disclosed serving on the steering committees or advisory boards for Actelion, Bayer, Bellerophon, Gilead, and United Therapeutics. He has received research support from Actelion, Gilead, and United Therapeutics, and has been a speaker for Actelion, Bayer, and Gilead.
LOS ANGELES – Pulmonary arterial hypertension (PAH) patients with severely impaired diffusing capacity of the lung for carbon monoxide (DLCO) were much more likely to survive when they received home oxygen therapy, according to a disease registry analysis.
“We all know that supplemental oxygen is widely used with PAH,” said Harrison W. Farber, MD, director of the pulmonary hypertension center at Boston University. But there are practically no data showing that it is successful, and there are even fewer data for patients with PAH who have very low diffusion capacity, he added.
That knowledge gap prompted Dr. Farber and his colleagues to analyze data from the Registry to Evaluate Early and Long-Term PAH Disease Management (REVEAL), the largest disease registry in the world of patients with PAH.
“Patients in that group – the severe DLCO group – who got oxygen had poorer prognostic features but improved overall survival relative to those who didn’t,” Dr. Farber explained during a presentation at the annual meeting of the American College of Chest Physicians. “Based on this, it makes us think that home oxygen, supplemental oxygen treatment, is associated with improved survival in patients, especially those with severe DLCO and PAH.”
The 3,046 patients analyzed by Dr. Farber and his colleagues had World Health Organization Group 1 PAH with right heart catheterization hemodynamic criteria: a mean pulmonary artery pressure greater than 25 mm Hg, a pulmonary capillary wedge pressure less than or equal to 15 mm Hg, and a pulmonary vascular resistance of at least 3 Wood units (WU). Patients were at least 18 years of age and grouped by oxygen use, which was defined as any use at any time from study enrollment to the end of follow-up, and by DLCO group.
A total of 57% of the patients (1,734) received oxygen, and the remaining 43% of the patients (1,312) did not receive oxygen. Among the patients who received oxygen, 71% (1,227) received the therapy continuously, and 24% (408) received oxygen at night only.
The 424 patients with a DLCO of less than 40% were considered to have a severe DLCO impairment. The other two groups comprised 505 patients with a moderate DLCO impairment (at least 40%, but less than 60%) and 844 patients with a mild to normal DLCO (at least 60%). The DLCOs of 1,273 patients analyzed were unknown.
Among those patients with severe DLCO impairment, the risk of death was significantly lower in those who received oxygen, compared with those who did not receive oxygen (hazard ratio, 0.56; P = .0033). Oxygen use was associated with significant improvements in overall survival in both the newly diagnosed (HR, 0.47; P = .029) and previously diagnosed (HR, 0.59; P = .026) severe DLCO cohorts, Dr. Farber said.
Patients receiving oxygen were more likely to be treated with PAH-specific medications, regardless of their DLCO group.
Among the analysis’s limitations was that the lengths of time patients had been undergoing oxygen treatment were unknown. That prevented adjustments for duration of oxygen treatment, according to Dr. Farber.
Dr. Farber disclosed serving on the steering committees or advisory boards for Actelion, Bayer, Bellerophon, Gilead, and United Therapeutics. He has received research support from Actelion, Gilead, and United Therapeutics, and has been a speaker for Actelion, Bayer, and Gilead.
LOS ANGELES – Pulmonary arterial hypertension (PAH) patients with severely impaired diffusing capacity of the lung for carbon monoxide (DLCO) were much more likely to survive when they received home oxygen therapy, according to a disease registry analysis.
“We all know that supplemental oxygen is widely used with PAH,” said Harrison W. Farber, MD, director of the pulmonary hypertension center at Boston University. But there are practically no data showing that it is successful, and there are even fewer data for patients with PAH who have very low diffusion capacity, he added.
That knowledge gap prompted Dr. Farber and his colleagues to analyze data from the Registry to Evaluate Early and Long-Term PAH Disease Management (REVEAL), the largest disease registry in the world of patients with PAH.
“Patients in that group – the severe DLCO group – who got oxygen had poorer prognostic features but improved overall survival relative to those who didn’t,” Dr. Farber explained during a presentation at the annual meeting of the American College of Chest Physicians. “Based on this, it makes us think that home oxygen, supplemental oxygen treatment, is associated with improved survival in patients, especially those with severe DLCO and PAH.”
The 3,046 patients analyzed by Dr. Farber and his colleagues had World Health Organization Group 1 PAH with right heart catheterization hemodynamic criteria: a mean pulmonary artery pressure greater than 25 mm Hg, a pulmonary capillary wedge pressure less than or equal to 15 mm Hg, and a pulmonary vascular resistance of at least 3 Wood units (WU). Patients were at least 18 years of age and grouped by oxygen use, which was defined as any use at any time from study enrollment to the end of follow-up, and by DLCO group.
A total of 57% of the patients (1,734) received oxygen, and the remaining 43% of the patients (1,312) did not receive oxygen. Among the patients who received oxygen, 71% (1,227) received the therapy continuously, and 24% (408) received oxygen at night only.
The 424 patients with a DLCO of less than 40% were considered to have a severe DLCO impairment. The other two groups comprised 505 patients with a moderate DLCO impairment (at least 40%, but less than 60%) and 844 patients with a mild to normal DLCO (at least 60%). The DLCOs of 1,273 patients analyzed were unknown.
Among those patients with severe DLCO impairment, the risk of death was significantly lower in those who received oxygen, compared with those who did not receive oxygen (hazard ratio, 0.56; P = .0033). Oxygen use was associated with significant improvements in overall survival in both the newly diagnosed (HR, 0.47; P = .029) and previously diagnosed (HR, 0.59; P = .026) severe DLCO cohorts, Dr. Farber said.
Patients receiving oxygen were more likely to be treated with PAH-specific medications, regardless of their DLCO group.
Among the analysis’s limitations was that the lengths of time patients had been undergoing oxygen treatment were unknown. That prevented adjustments for duration of oxygen treatment, according to Dr. Farber.
Dr. Farber disclosed serving on the steering committees or advisory boards for Actelion, Bayer, Bellerophon, Gilead, and United Therapeutics. He has received research support from Actelion, Gilead, and United Therapeutics, and has been a speaker for Actelion, Bayer, and Gilead.
Key clinical point:
Major finding: PAH patients with severe DLCO impairment who received oxygen had a significantly higher probability of survival than those who didn’t receive oxygen (HR, 0.56; P = .0033).
Data source: An analysis of 3,046 patients in the U.S. multicenter, observational REVEAL disease registry.
Disclosures: Dr. Farber disclosed serving on the steering committees or advisory boards for Actelion, Bayer, Bellerophon, Gilead, and United Therapeutics. He has received research support from Actelion, Gilead, and United Therapeutics, and has been a speaker for Actelion, Bayer, and Gilead.
Pediatric OSA improved with oral montelukast
The majority of children with obstructive sleep apnea (OSA) who took oral montelukast showed reductions in their apnea-hypopnea index (AHI) scores, in a randomized, double-blind placebo-controlled study.
Typically, OSA in children is treated by adenotonsillectomy, according to Leila Kheirandish-Gozal, MD, director of clinical sleep research at the University of Chicago, and her colleagues. Prior to this study, only one randomized controlled trial had showed that children with mild OSA “responded favorably” to the leukotriene modifier montelukast (Pediatrics. 2012 Aug 31. doi: 10.1542/peds.2012-0310).
Twenty (71%) of the children who received montelukast had fewer AHI events per hour of total sleep time at the end of the study. The average number of such events for these patients was 4.2 plus or minus 2.8 after taking the drug, compared with 9.2 plus or minus 4.1 at the beginning of the study (P less than .0001). Only two (6.9%) of the patients who took the placebo had lower AHI scores at the end of the study, with the average AHI score for the placebo group having been 8.7 plus or minus 4.9 events per hour of total sleep time. At baseline, the average score for patients in the placebo group was 8.2 plus or minus 5.0 AHI events per hour of total sleep time at baseline.
Another improvement seen by patients who received the drug was a decrease in the number of 3% reductions in arterial oxygen saturation per hour of sleep. At the beginning of the study, these patients had 7.2 plus or minus 3.1 of these events; by the end of the study, the number of these events was down to 2.8 plus or minus 1.8 (P less than .001). No significant decrease in the number of these events was seen among patients in the placebo group.
In this study, “montelukast emerges as favorably reducing the severity of OSA short term in children 2-10 years of age. These findings add to the existing evidence supporting a therapeutic role for anti-inflammatory approaches in the management of this highly prevalent condition in children, and clearly justify future studies targeting the long-term benefits of these approaches in children with OSA,” the researchers wrote.
All patients participated in overnight sleep studies following a referral to one of two sleep clinics by their primary care pediatrician or pediatric otolaryngologist, at the beginning of the study. Children who had been diagnosed with symptomatic snoring and had an AHI score of greater than 2 events per hour of total sleep time, and for whom adenotonsillectomy was contemplated, were included in the study.
Central, obstructive, mixed apneic events were counted and hypopneas were assessed. OSA was defined “as the absence of airflow with continued chest wall and abdominal movement for a duration of at least two breaths,” the investigators said. Hypopneas were defined “as a decrease in oronasal flow greater than 50% on either the thermistor or nasal pressure transducer signal. with a corresponding decrease in arterial oxygen saturation greater than 3% or arousal,” Dr. Kheirandish-Gozal and her coauthors said.
Patients were excluded from the study for a variety of reasons, including having severe OSA requiring early surgical intervention.
Adverse events included headache in two children, one from the experimental group and one from the placebo group, and nausea in two subjects from the placebo group and in one from the montelukast group.
Merck provided tablets used in this study. Dr. Kheirandish-Gozal reported grants from Merck and the National Institutes of Health during the conduct of the study. David Gozal, MD, is supported by the Herbert T. Abelson Chair in Pediatrics at the University of Chicago.
The majority of children with obstructive sleep apnea (OSA) who took oral montelukast showed reductions in their apnea-hypopnea index (AHI) scores, in a randomized, double-blind placebo-controlled study.
Typically, OSA in children is treated by adenotonsillectomy, according to Leila Kheirandish-Gozal, MD, director of clinical sleep research at the University of Chicago, and her colleagues. Prior to this study, only one randomized controlled trial had showed that children with mild OSA “responded favorably” to the leukotriene modifier montelukast (Pediatrics. 2012 Aug 31. doi: 10.1542/peds.2012-0310).
Twenty (71%) of the children who received montelukast had fewer AHI events per hour of total sleep time at the end of the study. The average number of such events for these patients was 4.2 plus or minus 2.8 after taking the drug, compared with 9.2 plus or minus 4.1 at the beginning of the study (P less than .0001). Only two (6.9%) of the patients who took the placebo had lower AHI scores at the end of the study, with the average AHI score for the placebo group having been 8.7 plus or minus 4.9 events per hour of total sleep time. At baseline, the average score for patients in the placebo group was 8.2 plus or minus 5.0 AHI events per hour of total sleep time at baseline.
Another improvement seen by patients who received the drug was a decrease in the number of 3% reductions in arterial oxygen saturation per hour of sleep. At the beginning of the study, these patients had 7.2 plus or minus 3.1 of these events; by the end of the study, the number of these events was down to 2.8 plus or minus 1.8 (P less than .001). No significant decrease in the number of these events was seen among patients in the placebo group.
In this study, “montelukast emerges as favorably reducing the severity of OSA short term in children 2-10 years of age. These findings add to the existing evidence supporting a therapeutic role for anti-inflammatory approaches in the management of this highly prevalent condition in children, and clearly justify future studies targeting the long-term benefits of these approaches in children with OSA,” the researchers wrote.
All patients participated in overnight sleep studies following a referral to one of two sleep clinics by their primary care pediatrician or pediatric otolaryngologist, at the beginning of the study. Children who had been diagnosed with symptomatic snoring and had an AHI score of greater than 2 events per hour of total sleep time, and for whom adenotonsillectomy was contemplated, were included in the study.
Central, obstructive, mixed apneic events were counted and hypopneas were assessed. OSA was defined “as the absence of airflow with continued chest wall and abdominal movement for a duration of at least two breaths,” the investigators said. Hypopneas were defined “as a decrease in oronasal flow greater than 50% on either the thermistor or nasal pressure transducer signal. with a corresponding decrease in arterial oxygen saturation greater than 3% or arousal,” Dr. Kheirandish-Gozal and her coauthors said.
Patients were excluded from the study for a variety of reasons, including having severe OSA requiring early surgical intervention.
Adverse events included headache in two children, one from the experimental group and one from the placebo group, and nausea in two subjects from the placebo group and in one from the montelukast group.
Merck provided tablets used in this study. Dr. Kheirandish-Gozal reported grants from Merck and the National Institutes of Health during the conduct of the study. David Gozal, MD, is supported by the Herbert T. Abelson Chair in Pediatrics at the University of Chicago.
The majority of children with obstructive sleep apnea (OSA) who took oral montelukast showed reductions in their apnea-hypopnea index (AHI) scores, in a randomized, double-blind placebo-controlled study.
Typically, OSA in children is treated by adenotonsillectomy, according to Leila Kheirandish-Gozal, MD, director of clinical sleep research at the University of Chicago, and her colleagues. Prior to this study, only one randomized controlled trial had showed that children with mild OSA “responded favorably” to the leukotriene modifier montelukast (Pediatrics. 2012 Aug 31. doi: 10.1542/peds.2012-0310).
Twenty (71%) of the children who received montelukast had fewer AHI events per hour of total sleep time at the end of the study. The average number of such events for these patients was 4.2 plus or minus 2.8 after taking the drug, compared with 9.2 plus or minus 4.1 at the beginning of the study (P less than .0001). Only two (6.9%) of the patients who took the placebo had lower AHI scores at the end of the study, with the average AHI score for the placebo group having been 8.7 plus or minus 4.9 events per hour of total sleep time. At baseline, the average score for patients in the placebo group was 8.2 plus or minus 5.0 AHI events per hour of total sleep time at baseline.
Another improvement seen by patients who received the drug was a decrease in the number of 3% reductions in arterial oxygen saturation per hour of sleep. At the beginning of the study, these patients had 7.2 plus or minus 3.1 of these events; by the end of the study, the number of these events was down to 2.8 plus or minus 1.8 (P less than .001). No significant decrease in the number of these events was seen among patients in the placebo group.
In this study, “montelukast emerges as favorably reducing the severity of OSA short term in children 2-10 years of age. These findings add to the existing evidence supporting a therapeutic role for anti-inflammatory approaches in the management of this highly prevalent condition in children, and clearly justify future studies targeting the long-term benefits of these approaches in children with OSA,” the researchers wrote.
All patients participated in overnight sleep studies following a referral to one of two sleep clinics by their primary care pediatrician or pediatric otolaryngologist, at the beginning of the study. Children who had been diagnosed with symptomatic snoring and had an AHI score of greater than 2 events per hour of total sleep time, and for whom adenotonsillectomy was contemplated, were included in the study.
Central, obstructive, mixed apneic events were counted and hypopneas were assessed. OSA was defined “as the absence of airflow with continued chest wall and abdominal movement for a duration of at least two breaths,” the investigators said. Hypopneas were defined “as a decrease in oronasal flow greater than 50% on either the thermistor or nasal pressure transducer signal. with a corresponding decrease in arterial oxygen saturation greater than 3% or arousal,” Dr. Kheirandish-Gozal and her coauthors said.
Patients were excluded from the study for a variety of reasons, including having severe OSA requiring early surgical intervention.
Adverse events included headache in two children, one from the experimental group and one from the placebo group, and nausea in two subjects from the placebo group and in one from the montelukast group.
Merck provided tablets used in this study. Dr. Kheirandish-Gozal reported grants from Merck and the National Institutes of Health during the conduct of the study. David Gozal, MD, is supported by the Herbert T. Abelson Chair in Pediatrics at the University of Chicago.
Key clinical point:
Major finding: 71% of patients who took montelukast had a significant reduction in AHI events per hour of total sleep time (P less than .0001).
Data source: A prospective, randomized, double-blind placebo-controlled study of 57 children with obstructive sleep apnea.
Disclosures: Merck provided tablets used in this study. Dr. Kheirandish-Gozal reported grants from Merck and the National Institutes of Health during the conduct of the study. David Gozal, MD, is supported by the Herbert T. Abelson Chair in Pediatrics at the University of Chicago.
IPF Patient Registry will expand
The number of patients enrolled in the Idiopathic Pulmonary Fibrosis–Prospective Outcomes (IPF-PRO) Registry will be increased to 1,500, Boehringer Ingelheim Pharmaceuticals and the Duke Clinical Research Institute have announced.
The organizations plan to accomplish this goal by increasing the number of sites they use to gather IPF patient data, according to a statement; the patients enrolled in the registry will now come from 45 sites instead of 18 sites.
IPF-PRO, which was launched in June 2014, is the first multicenter longitudinal disease state registry in the United States focused specifically on IPF. It was designed for the purpose of studying the progression of IPF and the effectiveness of various treatment approaches for the disease. The registry includes a biorepository that stores blood samples that provide patient genetic material.
“In collecting data from a larger, more diverse group of patients ... this registry will allow us to better assess the impact of the disease over time on clinical and patient-centered outcomes,” said Scott M. Palmer, MD, director of pulmonary research at the Duke Clinical Research Institute, Durham, N.C., in the statement.
More information on the registry is available at clinicaltrials.gov/ct2/show/NCT01915511.
The number of patients enrolled in the Idiopathic Pulmonary Fibrosis–Prospective Outcomes (IPF-PRO) Registry will be increased to 1,500, Boehringer Ingelheim Pharmaceuticals and the Duke Clinical Research Institute have announced.
The organizations plan to accomplish this goal by increasing the number of sites they use to gather IPF patient data, according to a statement; the patients enrolled in the registry will now come from 45 sites instead of 18 sites.
IPF-PRO, which was launched in June 2014, is the first multicenter longitudinal disease state registry in the United States focused specifically on IPF. It was designed for the purpose of studying the progression of IPF and the effectiveness of various treatment approaches for the disease. The registry includes a biorepository that stores blood samples that provide patient genetic material.
“In collecting data from a larger, more diverse group of patients ... this registry will allow us to better assess the impact of the disease over time on clinical and patient-centered outcomes,” said Scott M. Palmer, MD, director of pulmonary research at the Duke Clinical Research Institute, Durham, N.C., in the statement.
More information on the registry is available at clinicaltrials.gov/ct2/show/NCT01915511.
The number of patients enrolled in the Idiopathic Pulmonary Fibrosis–Prospective Outcomes (IPF-PRO) Registry will be increased to 1,500, Boehringer Ingelheim Pharmaceuticals and the Duke Clinical Research Institute have announced.
The organizations plan to accomplish this goal by increasing the number of sites they use to gather IPF patient data, according to a statement; the patients enrolled in the registry will now come from 45 sites instead of 18 sites.
IPF-PRO, which was launched in June 2014, is the first multicenter longitudinal disease state registry in the United States focused specifically on IPF. It was designed for the purpose of studying the progression of IPF and the effectiveness of various treatment approaches for the disease. The registry includes a biorepository that stores blood samples that provide patient genetic material.
“In collecting data from a larger, more diverse group of patients ... this registry will allow us to better assess the impact of the disease over time on clinical and patient-centered outcomes,” said Scott M. Palmer, MD, director of pulmonary research at the Duke Clinical Research Institute, Durham, N.C., in the statement.
More information on the registry is available at clinicaltrials.gov/ct2/show/NCT01915511.
Teams boost confidence in IPF diagnoses
The accuracy of idiopathic pulmonary fibrosis (IPF) diagnoses is improving with the use of multidisciplinary team meetings and updated guidelines, based on the findings of a study that compared diagnostic agreement of individual clinicians and teams evaluating patients with interstitial lung disease.
Pulmonologists who participate in multidisciplinary team meetings said the findings validate the team approach.
“The [study’s] data confirm what we see in clinical practice ... it takes a multidisciplinary – and perhaps often multiple pulmonologists – to review these cases,” Marilyn K. Glassberg, MD,professor of medicine and surgery and director of the interstitial lung disease program at the University of Miami Health System, said in an interview.“This study demonstrates the importance of multiple perspectives when evaluating a patient and coming to a diagnosis at a time when reliable biomarkers are not available.”
The study, published in The Lancet Respiratory Medicine (2016;4[7]:557-65), is the first evaluation of multidisciplinary team agreement on diagnosis of interstitial lung disease since updated guidelines were published, according to Simon L. F. Walsh, MD, of Kings College Hospital NHS Foundation Trust, London, and his colleagues.
In 2015, the American Thoracic Society (ATS), European Respiratory Society (ERS), Japanese Respiratory Society (JRS), and Latin American Thoracic Association (ALTA) adopted joint guidelines for the treatment of IPF. In 2013, the ATS and ERS updated guidelines for the classification and terminology for idiopathic interstitial pneumonias.
“Our study shows ... in [IPF], MDTMs (multidisciplinary team meetings) have a higher level of agreement on diagnoses, assign diagnoses with higher confidence more frequently, and provide diagnoses that have non-significant greater prognostic separation than do clinicians or radiologists in most cases,” the researchers wrote.
Before MDTMs were initiated, the clinicians, radiologists, and pathologists who would be participating in them independently reviewed each patient’s case without consulting other specialists and provided up to five diagnoses with diagnostic likelihoods for each patient.
For the study, 70 patients were evaluated and the level of diagnostic agreement was assessed at seven international centers for the diagnosis of interstitial lung disease (diffuse parenchymal lung disease). Following independent reviews of the 70 cases, the clinician, radiologist, and pathologist from each center met as a multidisciplinary team to review the same cases together and give up to five diagnoses with diagnostic likelihoods.
All clinical information supplied in the first stage of the study, including pulmonary function test results, high-resolution CT at presentation, and digitalized surgical lung biopsy slides, were available to the multidisciplinary team. The patients’ outcomes were used to validate the diagnoses. The survival period for each patient was calculated based on the date of referral to the host institution to the minimum date of death, date patient was last known to be alive, or June 1, 2015 – the end of the study period.
The inter-MDTM agreement was better than interobserver agreement for all diagnoses (unweighted kappa value (K) = 0.50), and inter-MDTM agreement was highest for IPF (K = 0.60) and connective tissue disease-related interstitial lung disease (K = 0.64).
“We have shown an acceptable level [based on a K of greater than 0.40 being deemed clinically acceptable] of diagnostic agreement exists between multidisciplinary teams in the setting of diffuse parenchymal lung disease. Additionally, we showed that this agreement was validated by the nonsignificant increases toward greater prognostic separation of an IPF diagnosis made by multidisciplinary teams than by individual clinicians or radiologists,” the researchers wrote.
The weighted kappa (KW) values for estimation of diagnostic likelihood for diagnoses of IPF were 0.72 (0.67-0.76) for clinicians, 0.60 (0.46-0.66) for radiologists, 0.58 (0.45-0.66) for pathologists and 0.71 (0.64-0.77) for MDTMs.
For connective tissue disease–related interstitial lung diseases, the KW for estimation of diagnostic likelihood for diagnoses for MDTMs were 0.73 (0.68-0.78), compared with 0.76 (0.70-0.78) for clinicians, 0.17 (0.08-0.31) for radiologists, and 0.21 (0.06-0.36) for pathologists.
Krishna Thavarajah, MD,, who sees patients with interstitial lung disease within the Henry Ford Health System in Detroit, has been participating in MDTMs for nearly 6 years.
“The accuracies of diagnoses for patients with IPF are much better than even 10 years ago,” she said in an interview. “I think this is because of the improvement in consistency in diagnostic criteria based on the updated guidelines in IPF. Among the MDTMs that participated in the study, the agreement about diagnoses was highest for IPF. The interobserver agreement for clinicians was also pretty high for IPF.”
In her work within an academic center, Dr. Glassberg sees patients in an IPF clinic and in a separate autoimmune disorders clinic. For each clinic, there is a multidisciplinary team. In the IPF clinic, there are three pulmonologists and a radiologist, and when there is a biopsy, there are two pathologists. Dr. Glassberg’s IPF team also includes four pulmonary radiologists.
During her MDTMs, Dr. Thavarajah, a radiologist, and a pathologist will examine a patient’s chest imaging and pathology slides. They sit together until they become confident of their diagnosis in the absence of a biopsy.
There are times when the team tells a patient the probable diagnosis and acknowledges the small chance of an alternative diagnosis. “It was comforting to me that, in the Lancet study, there was a good level of agreement in diagnosis of IPF among multidisciplinary teams, whether the patients had undergone a biopsy or not,” said Dr. Thavarajah. “The mortality of patients given a diagnosis of IPF was worse than those given a diagnosis of non-IPF to validate the IPF diagnosis.”
Establishing and implementing MDTMs is challenging, though, said Dr. Glassberg.
“[We] need to address how multidisciplinary teams could work for doctors who are in smaller cities or who are not in academic centers. We need to utilize existing channels to create new avenues for these colleagues to present their cases – particularly challenging ones or patients who need to be referred – to be evaluated by an interdisciplinary team. The Internet may offer these opportunities for networking and decision making, said Dr. Glassberg.
The study was funded by the National Institute of Health Research, Imperial College London. Several of the study’s authors declared receiving personal fees, grants, or research support from a variety of sources, but had no financial disclosures relevant to this study.
Daniel R. Ouellette, MD, FCCP, comments: “Recommendations have been that multidisciplinary teams add to the accuracy of the diagnosis of IPF. The value of this study is that it provides objective data that this is so.”
Daniel R. Ouellette, MD, FCCP, comments: “Recommendations have been that multidisciplinary teams add to the accuracy of the diagnosis of IPF. The value of this study is that it provides objective data that this is so.”
Daniel R. Ouellette, MD, FCCP, comments: “Recommendations have been that multidisciplinary teams add to the accuracy of the diagnosis of IPF. The value of this study is that it provides objective data that this is so.”
The accuracy of idiopathic pulmonary fibrosis (IPF) diagnoses is improving with the use of multidisciplinary team meetings and updated guidelines, based on the findings of a study that compared diagnostic agreement of individual clinicians and teams evaluating patients with interstitial lung disease.
Pulmonologists who participate in multidisciplinary team meetings said the findings validate the team approach.
“The [study’s] data confirm what we see in clinical practice ... it takes a multidisciplinary – and perhaps often multiple pulmonologists – to review these cases,” Marilyn K. Glassberg, MD,professor of medicine and surgery and director of the interstitial lung disease program at the University of Miami Health System, said in an interview.“This study demonstrates the importance of multiple perspectives when evaluating a patient and coming to a diagnosis at a time when reliable biomarkers are not available.”
The study, published in The Lancet Respiratory Medicine (2016;4[7]:557-65), is the first evaluation of multidisciplinary team agreement on diagnosis of interstitial lung disease since updated guidelines were published, according to Simon L. F. Walsh, MD, of Kings College Hospital NHS Foundation Trust, London, and his colleagues.
In 2015, the American Thoracic Society (ATS), European Respiratory Society (ERS), Japanese Respiratory Society (JRS), and Latin American Thoracic Association (ALTA) adopted joint guidelines for the treatment of IPF. In 2013, the ATS and ERS updated guidelines for the classification and terminology for idiopathic interstitial pneumonias.
“Our study shows ... in [IPF], MDTMs (multidisciplinary team meetings) have a higher level of agreement on diagnoses, assign diagnoses with higher confidence more frequently, and provide diagnoses that have non-significant greater prognostic separation than do clinicians or radiologists in most cases,” the researchers wrote.
Before MDTMs were initiated, the clinicians, radiologists, and pathologists who would be participating in them independently reviewed each patient’s case without consulting other specialists and provided up to five diagnoses with diagnostic likelihoods for each patient.
For the study, 70 patients were evaluated and the level of diagnostic agreement was assessed at seven international centers for the diagnosis of interstitial lung disease (diffuse parenchymal lung disease). Following independent reviews of the 70 cases, the clinician, radiologist, and pathologist from each center met as a multidisciplinary team to review the same cases together and give up to five diagnoses with diagnostic likelihoods.
All clinical information supplied in the first stage of the study, including pulmonary function test results, high-resolution CT at presentation, and digitalized surgical lung biopsy slides, were available to the multidisciplinary team. The patients’ outcomes were used to validate the diagnoses. The survival period for each patient was calculated based on the date of referral to the host institution to the minimum date of death, date patient was last known to be alive, or June 1, 2015 – the end of the study period.
The inter-MDTM agreement was better than interobserver agreement for all diagnoses (unweighted kappa value (K) = 0.50), and inter-MDTM agreement was highest for IPF (K = 0.60) and connective tissue disease-related interstitial lung disease (K = 0.64).
“We have shown an acceptable level [based on a K of greater than 0.40 being deemed clinically acceptable] of diagnostic agreement exists between multidisciplinary teams in the setting of diffuse parenchymal lung disease. Additionally, we showed that this agreement was validated by the nonsignificant increases toward greater prognostic separation of an IPF diagnosis made by multidisciplinary teams than by individual clinicians or radiologists,” the researchers wrote.
The weighted kappa (KW) values for estimation of diagnostic likelihood for diagnoses of IPF were 0.72 (0.67-0.76) for clinicians, 0.60 (0.46-0.66) for radiologists, 0.58 (0.45-0.66) for pathologists and 0.71 (0.64-0.77) for MDTMs.
For connective tissue disease–related interstitial lung diseases, the KW for estimation of diagnostic likelihood for diagnoses for MDTMs were 0.73 (0.68-0.78), compared with 0.76 (0.70-0.78) for clinicians, 0.17 (0.08-0.31) for radiologists, and 0.21 (0.06-0.36) for pathologists.
Krishna Thavarajah, MD,, who sees patients with interstitial lung disease within the Henry Ford Health System in Detroit, has been participating in MDTMs for nearly 6 years.
“The accuracies of diagnoses for patients with IPF are much better than even 10 years ago,” she said in an interview. “I think this is because of the improvement in consistency in diagnostic criteria based on the updated guidelines in IPF. Among the MDTMs that participated in the study, the agreement about diagnoses was highest for IPF. The interobserver agreement for clinicians was also pretty high for IPF.”
In her work within an academic center, Dr. Glassberg sees patients in an IPF clinic and in a separate autoimmune disorders clinic. For each clinic, there is a multidisciplinary team. In the IPF clinic, there are three pulmonologists and a radiologist, and when there is a biopsy, there are two pathologists. Dr. Glassberg’s IPF team also includes four pulmonary radiologists.
During her MDTMs, Dr. Thavarajah, a radiologist, and a pathologist will examine a patient’s chest imaging and pathology slides. They sit together until they become confident of their diagnosis in the absence of a biopsy.
There are times when the team tells a patient the probable diagnosis and acknowledges the small chance of an alternative diagnosis. “It was comforting to me that, in the Lancet study, there was a good level of agreement in diagnosis of IPF among multidisciplinary teams, whether the patients had undergone a biopsy or not,” said Dr. Thavarajah. “The mortality of patients given a diagnosis of IPF was worse than those given a diagnosis of non-IPF to validate the IPF diagnosis.”
Establishing and implementing MDTMs is challenging, though, said Dr. Glassberg.
“[We] need to address how multidisciplinary teams could work for doctors who are in smaller cities or who are not in academic centers. We need to utilize existing channels to create new avenues for these colleagues to present their cases – particularly challenging ones or patients who need to be referred – to be evaluated by an interdisciplinary team. The Internet may offer these opportunities for networking and decision making, said Dr. Glassberg.
The study was funded by the National Institute of Health Research, Imperial College London. Several of the study’s authors declared receiving personal fees, grants, or research support from a variety of sources, but had no financial disclosures relevant to this study.
The accuracy of idiopathic pulmonary fibrosis (IPF) diagnoses is improving with the use of multidisciplinary team meetings and updated guidelines, based on the findings of a study that compared diagnostic agreement of individual clinicians and teams evaluating patients with interstitial lung disease.
Pulmonologists who participate in multidisciplinary team meetings said the findings validate the team approach.
“The [study’s] data confirm what we see in clinical practice ... it takes a multidisciplinary – and perhaps often multiple pulmonologists – to review these cases,” Marilyn K. Glassberg, MD,professor of medicine and surgery and director of the interstitial lung disease program at the University of Miami Health System, said in an interview.“This study demonstrates the importance of multiple perspectives when evaluating a patient and coming to a diagnosis at a time when reliable biomarkers are not available.”
The study, published in The Lancet Respiratory Medicine (2016;4[7]:557-65), is the first evaluation of multidisciplinary team agreement on diagnosis of interstitial lung disease since updated guidelines were published, according to Simon L. F. Walsh, MD, of Kings College Hospital NHS Foundation Trust, London, and his colleagues.
In 2015, the American Thoracic Society (ATS), European Respiratory Society (ERS), Japanese Respiratory Society (JRS), and Latin American Thoracic Association (ALTA) adopted joint guidelines for the treatment of IPF. In 2013, the ATS and ERS updated guidelines for the classification and terminology for idiopathic interstitial pneumonias.
“Our study shows ... in [IPF], MDTMs (multidisciplinary team meetings) have a higher level of agreement on diagnoses, assign diagnoses with higher confidence more frequently, and provide diagnoses that have non-significant greater prognostic separation than do clinicians or radiologists in most cases,” the researchers wrote.
Before MDTMs were initiated, the clinicians, radiologists, and pathologists who would be participating in them independently reviewed each patient’s case without consulting other specialists and provided up to five diagnoses with diagnostic likelihoods for each patient.
For the study, 70 patients were evaluated and the level of diagnostic agreement was assessed at seven international centers for the diagnosis of interstitial lung disease (diffuse parenchymal lung disease). Following independent reviews of the 70 cases, the clinician, radiologist, and pathologist from each center met as a multidisciplinary team to review the same cases together and give up to five diagnoses with diagnostic likelihoods.
All clinical information supplied in the first stage of the study, including pulmonary function test results, high-resolution CT at presentation, and digitalized surgical lung biopsy slides, were available to the multidisciplinary team. The patients’ outcomes were used to validate the diagnoses. The survival period for each patient was calculated based on the date of referral to the host institution to the minimum date of death, date patient was last known to be alive, or June 1, 2015 – the end of the study period.
The inter-MDTM agreement was better than interobserver agreement for all diagnoses (unweighted kappa value (K) = 0.50), and inter-MDTM agreement was highest for IPF (K = 0.60) and connective tissue disease-related interstitial lung disease (K = 0.64).
“We have shown an acceptable level [based on a K of greater than 0.40 being deemed clinically acceptable] of diagnostic agreement exists between multidisciplinary teams in the setting of diffuse parenchymal lung disease. Additionally, we showed that this agreement was validated by the nonsignificant increases toward greater prognostic separation of an IPF diagnosis made by multidisciplinary teams than by individual clinicians or radiologists,” the researchers wrote.
The weighted kappa (KW) values for estimation of diagnostic likelihood for diagnoses of IPF were 0.72 (0.67-0.76) for clinicians, 0.60 (0.46-0.66) for radiologists, 0.58 (0.45-0.66) for pathologists and 0.71 (0.64-0.77) for MDTMs.
For connective tissue disease–related interstitial lung diseases, the KW for estimation of diagnostic likelihood for diagnoses for MDTMs were 0.73 (0.68-0.78), compared with 0.76 (0.70-0.78) for clinicians, 0.17 (0.08-0.31) for radiologists, and 0.21 (0.06-0.36) for pathologists.
Krishna Thavarajah, MD,, who sees patients with interstitial lung disease within the Henry Ford Health System in Detroit, has been participating in MDTMs for nearly 6 years.
“The accuracies of diagnoses for patients with IPF are much better than even 10 years ago,” she said in an interview. “I think this is because of the improvement in consistency in diagnostic criteria based on the updated guidelines in IPF. Among the MDTMs that participated in the study, the agreement about diagnoses was highest for IPF. The interobserver agreement for clinicians was also pretty high for IPF.”
In her work within an academic center, Dr. Glassberg sees patients in an IPF clinic and in a separate autoimmune disorders clinic. For each clinic, there is a multidisciplinary team. In the IPF clinic, there are three pulmonologists and a radiologist, and when there is a biopsy, there are two pathologists. Dr. Glassberg’s IPF team also includes four pulmonary radiologists.
During her MDTMs, Dr. Thavarajah, a radiologist, and a pathologist will examine a patient’s chest imaging and pathology slides. They sit together until they become confident of their diagnosis in the absence of a biopsy.
There are times when the team tells a patient the probable diagnosis and acknowledges the small chance of an alternative diagnosis. “It was comforting to me that, in the Lancet study, there was a good level of agreement in diagnosis of IPF among multidisciplinary teams, whether the patients had undergone a biopsy or not,” said Dr. Thavarajah. “The mortality of patients given a diagnosis of IPF was worse than those given a diagnosis of non-IPF to validate the IPF diagnosis.”
Establishing and implementing MDTMs is challenging, though, said Dr. Glassberg.
“[We] need to address how multidisciplinary teams could work for doctors who are in smaller cities or who are not in academic centers. We need to utilize existing channels to create new avenues for these colleagues to present their cases – particularly challenging ones or patients who need to be referred – to be evaluated by an interdisciplinary team. The Internet may offer these opportunities for networking and decision making, said Dr. Glassberg.
The study was funded by the National Institute of Health Research, Imperial College London. Several of the study’s authors declared receiving personal fees, grants, or research support from a variety of sources, but had no financial disclosures relevant to this study.
USPSTF opposes screening for obstructive sleep apnea in draft recommendation
The U.S. Preventive Services Task Force has issued a draft recommendation opposing screening for obstructive sleep apnea (OSA) in adults who are asymptomatic for the breathing disorder.
The USPSTF’s opposition is based on its determination that there is insufficient evidence to assess the balance of benefits and harms of screening for OSA in asymptomatic adults in primary care settings, giving the service an “I” grade. The recommendation and a draft evidence review are available for public comment until July 11 at 8:00 p.m. EST.
The draft recommendation is the first that the USPSTF has ever made about sleep apnea, according to the draft evidence review. The recommendation “applies to asymptomatic adults (aged 18 years and older) and adults with unrecognized symptoms of OSA.” It does not apply to children, adolescents, pregnant women, persons presenting with symptoms of or concerns about OSA, those who are being referred for evaluation or treatment of suspected OSA, and those who have acute conditions that could trigger the onset of OSA.
“Reported estimates of OSA prevalence vary due to differing definitions of OSA, sampling bias, and year of study publication. A 2013 systematic review reported an estimated prevalence of 2%-14% based on four community-based studies, while two U.S.-based studies conducted in the 1990s reported an estimated prevalence of 10% for mild OSA and 3.8%-6.5% for moderate or severe OSA,” according to the recommendation.
The USPSTF was unable to find adequate evidence on the direct harms of screening for OSA or the benefits of screening for OSA in asymptomatic populations, including their magnitude.
Most primary care clinicians do not routinely screen for OSA, according to the recommendation. While the Epworth Sleepiness Scale, STOP Questionnaire, STOPBang Questionnaire, Berlin Questionnaire, and Wisconsin Sleep Questionnaire are potential screening tests for OSA, none of these questionnaires has been validated in a primary care setting.
“There is uncertainty about the clinical utility of all potential screening tools,” and the USPSTF found no studies that prospectively evaluated screening questionnaires or clinical prediction tools to report calibration or clinical utility for improving health outcomes,” the draft evidence review said.
The USPSTF also found no studies evaluating the effect of screening for OSA on health outcomes or that directly evaluated benefits or harms of screening for OSA.
The recommendation calls for further research on the health outcomes of screening for OSA in asymptomatic persons and the role of sleepiness in determining health outcomes. The following are needed:
• The identification of valid and reliable clinical prediction tools that could accurately determine which asymptomatic persons (or persons with unrecognized symptoms) would benefit from further evaluation and testing for OSA.
• Studies that evaluate the effect of OSA treatments or interventions on health outcomes that are adequately powered and have an appropriate length of follow-up.
• Studies that evaluate whether improvement in the apnea-hypopnea index leads to improvement in health outcomes.
• More data on the natural history of mild sleep apnea.
The final evidence review will be used to inform the final USPSTF recommendation statement.

|
| Dr. David Schulman, FCCP |
Dr. David A. Schulman, FCCP, comments: The draft statement from the Preventative Services Task Force recommending against screening asymptomatic patients with standardized OSA questionnaires warrants a careful read. Many sleepy patients may not complain of their fatigue unless specifically asked, choosing to attribute their symptoms to inactivity, age, weight or a lack of exercise instead of a potential underlying sleep disorder.
Assessment of patients’ sleep habits and patterns by primary care physicians remains a critical component of preventative health to improve identification of the twenty-plus million Americans with sleep disordered breathing.

|
| Dr. David Schulman, FCCP |
Dr. David A. Schulman, FCCP, comments: The draft statement from the Preventative Services Task Force recommending against screening asymptomatic patients with standardized OSA questionnaires warrants a careful read. Many sleepy patients may not complain of their fatigue unless specifically asked, choosing to attribute their symptoms to inactivity, age, weight or a lack of exercise instead of a potential underlying sleep disorder.
Assessment of patients’ sleep habits and patterns by primary care physicians remains a critical component of preventative health to improve identification of the twenty-plus million Americans with sleep disordered breathing.

|
| Dr. David Schulman, FCCP |
Dr. David A. Schulman, FCCP, comments: The draft statement from the Preventative Services Task Force recommending against screening asymptomatic patients with standardized OSA questionnaires warrants a careful read. Many sleepy patients may not complain of their fatigue unless specifically asked, choosing to attribute their symptoms to inactivity, age, weight or a lack of exercise instead of a potential underlying sleep disorder.
Assessment of patients’ sleep habits and patterns by primary care physicians remains a critical component of preventative health to improve identification of the twenty-plus million Americans with sleep disordered breathing.
The U.S. Preventive Services Task Force has issued a draft recommendation opposing screening for obstructive sleep apnea (OSA) in adults who are asymptomatic for the breathing disorder.
The USPSTF’s opposition is based on its determination that there is insufficient evidence to assess the balance of benefits and harms of screening for OSA in asymptomatic adults in primary care settings, giving the service an “I” grade. The recommendation and a draft evidence review are available for public comment until July 11 at 8:00 p.m. EST.
The draft recommendation is the first that the USPSTF has ever made about sleep apnea, according to the draft evidence review. The recommendation “applies to asymptomatic adults (aged 18 years and older) and adults with unrecognized symptoms of OSA.” It does not apply to children, adolescents, pregnant women, persons presenting with symptoms of or concerns about OSA, those who are being referred for evaluation or treatment of suspected OSA, and those who have acute conditions that could trigger the onset of OSA.
“Reported estimates of OSA prevalence vary due to differing definitions of OSA, sampling bias, and year of study publication. A 2013 systematic review reported an estimated prevalence of 2%-14% based on four community-based studies, while two U.S.-based studies conducted in the 1990s reported an estimated prevalence of 10% for mild OSA and 3.8%-6.5% for moderate or severe OSA,” according to the recommendation.
The USPSTF was unable to find adequate evidence on the direct harms of screening for OSA or the benefits of screening for OSA in asymptomatic populations, including their magnitude.
Most primary care clinicians do not routinely screen for OSA, according to the recommendation. While the Epworth Sleepiness Scale, STOP Questionnaire, STOPBang Questionnaire, Berlin Questionnaire, and Wisconsin Sleep Questionnaire are potential screening tests for OSA, none of these questionnaires has been validated in a primary care setting.
“There is uncertainty about the clinical utility of all potential screening tools,” and the USPSTF found no studies that prospectively evaluated screening questionnaires or clinical prediction tools to report calibration or clinical utility for improving health outcomes,” the draft evidence review said.
The USPSTF also found no studies evaluating the effect of screening for OSA on health outcomes or that directly evaluated benefits or harms of screening for OSA.
The recommendation calls for further research on the health outcomes of screening for OSA in asymptomatic persons and the role of sleepiness in determining health outcomes. The following are needed:
• The identification of valid and reliable clinical prediction tools that could accurately determine which asymptomatic persons (or persons with unrecognized symptoms) would benefit from further evaluation and testing for OSA.
• Studies that evaluate the effect of OSA treatments or interventions on health outcomes that are adequately powered and have an appropriate length of follow-up.
• Studies that evaluate whether improvement in the apnea-hypopnea index leads to improvement in health outcomes.
• More data on the natural history of mild sleep apnea.
The final evidence review will be used to inform the final USPSTF recommendation statement.
The U.S. Preventive Services Task Force has issued a draft recommendation opposing screening for obstructive sleep apnea (OSA) in adults who are asymptomatic for the breathing disorder.
The USPSTF’s opposition is based on its determination that there is insufficient evidence to assess the balance of benefits and harms of screening for OSA in asymptomatic adults in primary care settings, giving the service an “I” grade. The recommendation and a draft evidence review are available for public comment until July 11 at 8:00 p.m. EST.
The draft recommendation is the first that the USPSTF has ever made about sleep apnea, according to the draft evidence review. The recommendation “applies to asymptomatic adults (aged 18 years and older) and adults with unrecognized symptoms of OSA.” It does not apply to children, adolescents, pregnant women, persons presenting with symptoms of or concerns about OSA, those who are being referred for evaluation or treatment of suspected OSA, and those who have acute conditions that could trigger the onset of OSA.
“Reported estimates of OSA prevalence vary due to differing definitions of OSA, sampling bias, and year of study publication. A 2013 systematic review reported an estimated prevalence of 2%-14% based on four community-based studies, while two U.S.-based studies conducted in the 1990s reported an estimated prevalence of 10% for mild OSA and 3.8%-6.5% for moderate or severe OSA,” according to the recommendation.
The USPSTF was unable to find adequate evidence on the direct harms of screening for OSA or the benefits of screening for OSA in asymptomatic populations, including their magnitude.
Most primary care clinicians do not routinely screen for OSA, according to the recommendation. While the Epworth Sleepiness Scale, STOP Questionnaire, STOPBang Questionnaire, Berlin Questionnaire, and Wisconsin Sleep Questionnaire are potential screening tests for OSA, none of these questionnaires has been validated in a primary care setting.
“There is uncertainty about the clinical utility of all potential screening tools,” and the USPSTF found no studies that prospectively evaluated screening questionnaires or clinical prediction tools to report calibration or clinical utility for improving health outcomes,” the draft evidence review said.
The USPSTF also found no studies evaluating the effect of screening for OSA on health outcomes or that directly evaluated benefits or harms of screening for OSA.
The recommendation calls for further research on the health outcomes of screening for OSA in asymptomatic persons and the role of sleepiness in determining health outcomes. The following are needed:
• The identification of valid and reliable clinical prediction tools that could accurately determine which asymptomatic persons (or persons with unrecognized symptoms) would benefit from further evaluation and testing for OSA.
• Studies that evaluate the effect of OSA treatments or interventions on health outcomes that are adequately powered and have an appropriate length of follow-up.
• Studies that evaluate whether improvement in the apnea-hypopnea index leads to improvement in health outcomes.
• More data on the natural history of mild sleep apnea.
The final evidence review will be used to inform the final USPSTF recommendation statement.
Diffuse alveolar damage ups death risk in acute respiratory distress syndrome
Among patients with acute respiratory distress syndrome (ARDS), those who are also diagnosed with diffuse alveolar damage (DAD) via an open lung biopsy face nearly twice as high a mortality risk as did those without DAD, according to a systematic review and a meta-analysis by Dr. Pablo Cardinal-Fernandez and his colleagues.
The results of this and other studies “support the hypothesis that ARDS with DAD is a specific clinicopathological entity different from ARDS without DAD,” said Dr. Cardinal-Fernandez of the department of genetic medicine, Cornell University, New York, and his colleagues (CHEST 2016 149:1155-64.).
“Our meta-analysis underscores the need for less-invasive approaches to individualize therapy for patients with ARDS, including the development of biomarkers for predicting responses to treatments.”
The researchers analyzed studies identified using MEDLINE, EMBASE, Cochrane Register of Controlled Trials, LILACS, and citation review from Jan. 1, 1967, to Sept. 1, 2015. Eight studies involving 350 patients satisfied the researchers’ criteria for inclusion in the review. All of such studies included patients who received an open lung biopsy after being diagnosed with ARDS, histologic results indicating the presence or absence of DAD based on the open lung biopsy, and the mortalities of both a group of patients diagnosed with DAD and a group of patients not diagnosed with DAD. Studies were excluded from the review if they included fewer than five participants.
The pooled odds ratio for mortality in patients who had ARDS with DAD, compared with patients with ARDs who did not have DAD was 1.81.
At the time of ARDS diagnosis, the meta-differences for sequential organ failure assessment scores and the index of hypoxemia (PaO2/FiO2) ratio between the patients who had DAD and those who did not were 0.26 and 4.36, respectively. On the day of open lung biopsy, the meta-differences for the sequential organ failure assessment score and the PaO2/FiO2 ratio between the two patient groups were also small; the meta-difference for sequential organ failure was 0.45 and the meta-difference for the PaO2/FiO2 ratio was –8.63.
The higher mortality risk in the group of patients with DAD – despite patients in both groups having similar severities of illness – suggests that “the presence of DAD confers additional prognostic information,” according to the researchers.
“The mortality heterogeneity of this meta-analysis was low, suggesting that no other variables affect the results (that is, the observed effect depends mainly on the presence of DAD). Conditions that were identified in patients without DAD included pneumonia, pulmonary embolism, edema, or no pathologic abnormality. It appears that these subsets of patients have a different and better prognosis than did patients with ARDS and DAD, perhaps as a result of favorable responses to specific treatments, with the possible exception of lower tidal volume, which appears to be beneficial in all subgroups,” the researchers said.
No financial or nonfinancial disclosures were declared.
Among patients with acute respiratory distress syndrome (ARDS), those who are also diagnosed with diffuse alveolar damage (DAD) via an open lung biopsy face nearly twice as high a mortality risk as did those without DAD, according to a systematic review and a meta-analysis by Dr. Pablo Cardinal-Fernandez and his colleagues.
The results of this and other studies “support the hypothesis that ARDS with DAD is a specific clinicopathological entity different from ARDS without DAD,” said Dr. Cardinal-Fernandez of the department of genetic medicine, Cornell University, New York, and his colleagues (CHEST 2016 149:1155-64.).
“Our meta-analysis underscores the need for less-invasive approaches to individualize therapy for patients with ARDS, including the development of biomarkers for predicting responses to treatments.”
The researchers analyzed studies identified using MEDLINE, EMBASE, Cochrane Register of Controlled Trials, LILACS, and citation review from Jan. 1, 1967, to Sept. 1, 2015. Eight studies involving 350 patients satisfied the researchers’ criteria for inclusion in the review. All of such studies included patients who received an open lung biopsy after being diagnosed with ARDS, histologic results indicating the presence or absence of DAD based on the open lung biopsy, and the mortalities of both a group of patients diagnosed with DAD and a group of patients not diagnosed with DAD. Studies were excluded from the review if they included fewer than five participants.
The pooled odds ratio for mortality in patients who had ARDS with DAD, compared with patients with ARDs who did not have DAD was 1.81.
At the time of ARDS diagnosis, the meta-differences for sequential organ failure assessment scores and the index of hypoxemia (PaO2/FiO2) ratio between the patients who had DAD and those who did not were 0.26 and 4.36, respectively. On the day of open lung biopsy, the meta-differences for the sequential organ failure assessment score and the PaO2/FiO2 ratio between the two patient groups were also small; the meta-difference for sequential organ failure was 0.45 and the meta-difference for the PaO2/FiO2 ratio was –8.63.
The higher mortality risk in the group of patients with DAD – despite patients in both groups having similar severities of illness – suggests that “the presence of DAD confers additional prognostic information,” according to the researchers.
“The mortality heterogeneity of this meta-analysis was low, suggesting that no other variables affect the results (that is, the observed effect depends mainly on the presence of DAD). Conditions that were identified in patients without DAD included pneumonia, pulmonary embolism, edema, or no pathologic abnormality. It appears that these subsets of patients have a different and better prognosis than did patients with ARDS and DAD, perhaps as a result of favorable responses to specific treatments, with the possible exception of lower tidal volume, which appears to be beneficial in all subgroups,” the researchers said.
No financial or nonfinancial disclosures were declared.
Among patients with acute respiratory distress syndrome (ARDS), those who are also diagnosed with diffuse alveolar damage (DAD) via an open lung biopsy face nearly twice as high a mortality risk as did those without DAD, according to a systematic review and a meta-analysis by Dr. Pablo Cardinal-Fernandez and his colleagues.
The results of this and other studies “support the hypothesis that ARDS with DAD is a specific clinicopathological entity different from ARDS without DAD,” said Dr. Cardinal-Fernandez of the department of genetic medicine, Cornell University, New York, and his colleagues (CHEST 2016 149:1155-64.).
“Our meta-analysis underscores the need for less-invasive approaches to individualize therapy for patients with ARDS, including the development of biomarkers for predicting responses to treatments.”
The researchers analyzed studies identified using MEDLINE, EMBASE, Cochrane Register of Controlled Trials, LILACS, and citation review from Jan. 1, 1967, to Sept. 1, 2015. Eight studies involving 350 patients satisfied the researchers’ criteria for inclusion in the review. All of such studies included patients who received an open lung biopsy after being diagnosed with ARDS, histologic results indicating the presence or absence of DAD based on the open lung biopsy, and the mortalities of both a group of patients diagnosed with DAD and a group of patients not diagnosed with DAD. Studies were excluded from the review if they included fewer than five participants.
The pooled odds ratio for mortality in patients who had ARDS with DAD, compared with patients with ARDs who did not have DAD was 1.81.
At the time of ARDS diagnosis, the meta-differences for sequential organ failure assessment scores and the index of hypoxemia (PaO2/FiO2) ratio between the patients who had DAD and those who did not were 0.26 and 4.36, respectively. On the day of open lung biopsy, the meta-differences for the sequential organ failure assessment score and the PaO2/FiO2 ratio between the two patient groups were also small; the meta-difference for sequential organ failure was 0.45 and the meta-difference for the PaO2/FiO2 ratio was –8.63.
The higher mortality risk in the group of patients with DAD – despite patients in both groups having similar severities of illness – suggests that “the presence of DAD confers additional prognostic information,” according to the researchers.
“The mortality heterogeneity of this meta-analysis was low, suggesting that no other variables affect the results (that is, the observed effect depends mainly on the presence of DAD). Conditions that were identified in patients without DAD included pneumonia, pulmonary embolism, edema, or no pathologic abnormality. It appears that these subsets of patients have a different and better prognosis than did patients with ARDS and DAD, perhaps as a result of favorable responses to specific treatments, with the possible exception of lower tidal volume, which appears to be beneficial in all subgroups,” the researchers said.
No financial or nonfinancial disclosures were declared.
FROM CHEST
Key clinical point: Among patients with ARDS, those who are also diagnosed with DAD faced nearly twice as high a mortality risk as did those without DAD.
Major finding: The pooled odds ratio for mortality in patients who had acute respiratory distress syndrome with diffuse alveolar damage, compared with patients with ARDs who did not have DAD was 1.81.
Data source: A systematic review and meta-analysis of eight studies, including 350 patients, published between 1967 and 2015.
Disclosures: No financial or nonfinancial disclosures were declared.
Respiratory exacerbations rate high in patients not meeting COPD criteria
The clinical definition of chronic obstructive pulmonary disease (COPD) may need to be revised, based on results from a multicenter observational study of 2,736 individuals.
Respiratory symptoms of COPD were present in 425 of 849 current or former smokers who did not meet the standard spirometry criteria for diagnosing COPD. The 425 study participants who were symptomatic for COPD but were considered to have preserved pulmonary function had a significantly higher rate of respiratory exacerbations, compared with that of the 424 current or former smokers who were asymptomatic for COPD and were not classified as having the disease (0.27 +/- 0.67 events vs. 0.08 +/- 0.31 events; P less than .001).
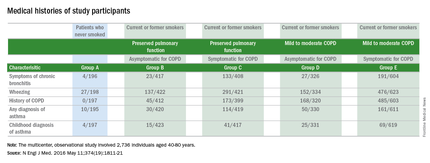
Using spirometry to define who should receive a diagnosis of COPD does not address all people with symptomatic smoking-related lung disease. This large population needs to be studied to better define appropriate treatment strategies, Dr. Prescott G. Woodruff, a professor of medicine at the University of California, San Francisco, and his associates noted (N Engl J Med. 2016 May 11;[19]374:1811-21.).
Study participants were classified as not having COPD if the ratios of their forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) was 0.70 or more after bronchodilator use and if their FVC was above the lower limit of the normal range. During a stable phase of disease, which was defined as greater than six weeks after a respiratory exacerbation, patients participated in the COPD Assessment Test (CAT), an eight-question health status instrument. Patients with a CAT score of greater than or equal to 10 were considered to be symptomatic for COPD and those with CAT scores of less than 10 were considered to be asymptomatic for COPD.
While 963 of the 1,812 study participants who were current or former smokers were classified as having Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage 1 or 2 COPD, half of the current or former smokers who were not classified as having COPD were still symptomatic for the disease. Additionally, among the 199 study participants who had never smoked, 16% had COPD symptoms.
Current or former smokers classified as not having COPD, who were symptomatic for the disease, had elevations in all components of the CAT score, were younger, were more likely to be nonwhite or Hispanic, and had a higher body mass index than those with a CAT score of less than 10. These patients with preserved pulmonary function despite being symptomatic for COPD also were more likely to be current smokers, report symptoms of chronic bronchitis, report a history of wheezing and asthma, and report a previous diagnosis of COPD, compared with the asymptomatic patients with preserved pulmonary function.
From 2010 through 2015, 2,736 individuals, aged 40-80 years, were enrolled in the study. The study participants had either never smoked (defined as having smoked less than or equal to 1 pack-year of tobacco use) or were current or former smokers with a smoking history of more than 20 pack-years. Spirometry was used to determine if study participants had COPD. This was performed before and after four inhalations each of albuterol, at a dose of 90 mcg per inhalation, and ipratropium, at a dose of 18 mcg per inhalation.
Among the other data obtained by the researchers were the patients’ 6-minute walk distances. The average 6-minute walk distance was shorter for patients with symptoms of COPD, compared with those with CAT scores of less than 10.
This study shows that the CAT can identify smokers at risk for exacerbations and provides evidence that individuals with COPD symptoms may have airway disease, according to the researchers.
“Clinical trials are needed to determine whether maintenance therapy with bronchodilators or inhaled glucocorticoids will alleviate symptoms and reduce the rate of respiratory exacerbations in [current or former smokers with elevated respiratory exacerbation rates who do not meet the standard criteria for having COPD],” the researchers said.
This study was supported by grants from the National Heart, Lung, and Blood Institute of the National Institutes of Health and by the Foundation for the National Institutes of Health through contributions made to an external advisory board composed of members from several pharmaceutical companies. The authors’ disclosures are available at NEJM.org.
It is often symptoms that bring patients to seek hospital care. This study points out a split between smoking-related respiratory symptoms and the preserved spirometry that was found in a portion of the study group. Further research may better characterize this population of symptomatic current and former smokers. With identification of effective treatments and improved symptom management, we may be able to promote better respiratory health, thereby reducing hospital utilization.
Dr. Vera De Palo is Editor in Chief of CHEST Physician. She is the Chief Medical Officer at Signature Healthcare in Brockton, Massachusetts.
It is often symptoms that bring patients to seek hospital care. This study points out a split between smoking-related respiratory symptoms and the preserved spirometry that was found in a portion of the study group. Further research may better characterize this population of symptomatic current and former smokers. With identification of effective treatments and improved symptom management, we may be able to promote better respiratory health, thereby reducing hospital utilization.
Dr. Vera De Palo is Editor in Chief of CHEST Physician. She is the Chief Medical Officer at Signature Healthcare in Brockton, Massachusetts.
It is often symptoms that bring patients to seek hospital care. This study points out a split between smoking-related respiratory symptoms and the preserved spirometry that was found in a portion of the study group. Further research may better characterize this population of symptomatic current and former smokers. With identification of effective treatments and improved symptom management, we may be able to promote better respiratory health, thereby reducing hospital utilization.
Dr. Vera De Palo is Editor in Chief of CHEST Physician. She is the Chief Medical Officer at Signature Healthcare in Brockton, Massachusetts.
The clinical definition of chronic obstructive pulmonary disease (COPD) may need to be revised, based on results from a multicenter observational study of 2,736 individuals.
Respiratory symptoms of COPD were present in 425 of 849 current or former smokers who did not meet the standard spirometry criteria for diagnosing COPD. The 425 study participants who were symptomatic for COPD but were considered to have preserved pulmonary function had a significantly higher rate of respiratory exacerbations, compared with that of the 424 current or former smokers who were asymptomatic for COPD and were not classified as having the disease (0.27 +/- 0.67 events vs. 0.08 +/- 0.31 events; P less than .001).
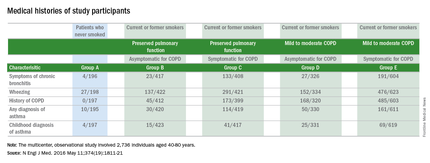
Using spirometry to define who should receive a diagnosis of COPD does not address all people with symptomatic smoking-related lung disease. This large population needs to be studied to better define appropriate treatment strategies, Dr. Prescott G. Woodruff, a professor of medicine at the University of California, San Francisco, and his associates noted (N Engl J Med. 2016 May 11;[19]374:1811-21.).
Study participants were classified as not having COPD if the ratios of their forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) was 0.70 or more after bronchodilator use and if their FVC was above the lower limit of the normal range. During a stable phase of disease, which was defined as greater than six weeks after a respiratory exacerbation, patients participated in the COPD Assessment Test (CAT), an eight-question health status instrument. Patients with a CAT score of greater than or equal to 10 were considered to be symptomatic for COPD and those with CAT scores of less than 10 were considered to be asymptomatic for COPD.
While 963 of the 1,812 study participants who were current or former smokers were classified as having Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage 1 or 2 COPD, half of the current or former smokers who were not classified as having COPD were still symptomatic for the disease. Additionally, among the 199 study participants who had never smoked, 16% had COPD symptoms.
Current or former smokers classified as not having COPD, who were symptomatic for the disease, had elevations in all components of the CAT score, were younger, were more likely to be nonwhite or Hispanic, and had a higher body mass index than those with a CAT score of less than 10. These patients with preserved pulmonary function despite being symptomatic for COPD also were more likely to be current smokers, report symptoms of chronic bronchitis, report a history of wheezing and asthma, and report a previous diagnosis of COPD, compared with the asymptomatic patients with preserved pulmonary function.
From 2010 through 2015, 2,736 individuals, aged 40-80 years, were enrolled in the study. The study participants had either never smoked (defined as having smoked less than or equal to 1 pack-year of tobacco use) or were current or former smokers with a smoking history of more than 20 pack-years. Spirometry was used to determine if study participants had COPD. This was performed before and after four inhalations each of albuterol, at a dose of 90 mcg per inhalation, and ipratropium, at a dose of 18 mcg per inhalation.
Among the other data obtained by the researchers were the patients’ 6-minute walk distances. The average 6-minute walk distance was shorter for patients with symptoms of COPD, compared with those with CAT scores of less than 10.
This study shows that the CAT can identify smokers at risk for exacerbations and provides evidence that individuals with COPD symptoms may have airway disease, according to the researchers.
“Clinical trials are needed to determine whether maintenance therapy with bronchodilators or inhaled glucocorticoids will alleviate symptoms and reduce the rate of respiratory exacerbations in [current or former smokers with elevated respiratory exacerbation rates who do not meet the standard criteria for having COPD],” the researchers said.
This study was supported by grants from the National Heart, Lung, and Blood Institute of the National Institutes of Health and by the Foundation for the National Institutes of Health through contributions made to an external advisory board composed of members from several pharmaceutical companies. The authors’ disclosures are available at NEJM.org.
The clinical definition of chronic obstructive pulmonary disease (COPD) may need to be revised, based on results from a multicenter observational study of 2,736 individuals.
Respiratory symptoms of COPD were present in 425 of 849 current or former smokers who did not meet the standard spirometry criteria for diagnosing COPD. The 425 study participants who were symptomatic for COPD but were considered to have preserved pulmonary function had a significantly higher rate of respiratory exacerbations, compared with that of the 424 current or former smokers who were asymptomatic for COPD and were not classified as having the disease (0.27 +/- 0.67 events vs. 0.08 +/- 0.31 events; P less than .001).
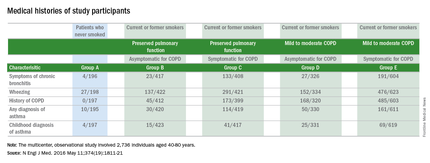
Using spirometry to define who should receive a diagnosis of COPD does not address all people with symptomatic smoking-related lung disease. This large population needs to be studied to better define appropriate treatment strategies, Dr. Prescott G. Woodruff, a professor of medicine at the University of California, San Francisco, and his associates noted (N Engl J Med. 2016 May 11;[19]374:1811-21.).
Study participants were classified as not having COPD if the ratios of their forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) was 0.70 or more after bronchodilator use and if their FVC was above the lower limit of the normal range. During a stable phase of disease, which was defined as greater than six weeks after a respiratory exacerbation, patients participated in the COPD Assessment Test (CAT), an eight-question health status instrument. Patients with a CAT score of greater than or equal to 10 were considered to be symptomatic for COPD and those with CAT scores of less than 10 were considered to be asymptomatic for COPD.
While 963 of the 1,812 study participants who were current or former smokers were classified as having Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage 1 or 2 COPD, half of the current or former smokers who were not classified as having COPD were still symptomatic for the disease. Additionally, among the 199 study participants who had never smoked, 16% had COPD symptoms.
Current or former smokers classified as not having COPD, who were symptomatic for the disease, had elevations in all components of the CAT score, were younger, were more likely to be nonwhite or Hispanic, and had a higher body mass index than those with a CAT score of less than 10. These patients with preserved pulmonary function despite being symptomatic for COPD also were more likely to be current smokers, report symptoms of chronic bronchitis, report a history of wheezing and asthma, and report a previous diagnosis of COPD, compared with the asymptomatic patients with preserved pulmonary function.
From 2010 through 2015, 2,736 individuals, aged 40-80 years, were enrolled in the study. The study participants had either never smoked (defined as having smoked less than or equal to 1 pack-year of tobacco use) or were current or former smokers with a smoking history of more than 20 pack-years. Spirometry was used to determine if study participants had COPD. This was performed before and after four inhalations each of albuterol, at a dose of 90 mcg per inhalation, and ipratropium, at a dose of 18 mcg per inhalation.
Among the other data obtained by the researchers were the patients’ 6-minute walk distances. The average 6-minute walk distance was shorter for patients with symptoms of COPD, compared with those with CAT scores of less than 10.
This study shows that the CAT can identify smokers at risk for exacerbations and provides evidence that individuals with COPD symptoms may have airway disease, according to the researchers.
“Clinical trials are needed to determine whether maintenance therapy with bronchodilators or inhaled glucocorticoids will alleviate symptoms and reduce the rate of respiratory exacerbations in [current or former smokers with elevated respiratory exacerbation rates who do not meet the standard criteria for having COPD],” the researchers said.
This study was supported by grants from the National Heart, Lung, and Blood Institute of the National Institutes of Health and by the Foundation for the National Institutes of Health through contributions made to an external advisory board composed of members from several pharmaceutical companies. The authors’ disclosures are available at NEJM.org.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Respiratory symptoms of COPD were present in 425 of 849 current or former smokers who did not meet the standard spirometry criteria for diagnosing COPD.
Major finding: The 425 study participants who were symptomatic for COPD but did not meet the standard spirometry criteria for diagnosing COPD had a significantly higher rate of respiratory exacerbations, compared with that of the 424 current or former smokers who were asymptomatic for COPD and were not classified as having the disease (0.27 +/- 0.67 events vs. 0.08 +/- 0.31 events; P less than .001).
Data source: Results are from a multicenter observational study that enrolled 2,736 individuals from 2010 to 2015.
Disclosures: This study was supported by grants from the National Heart, Lung, and Blood Institute of the National Institutes of Health and by the Foundation for the National Institutes of Health through contributions made to an external advisory board composed of members from several pharmaceutical companies. The authors’ disclosures are available at NEJM.org.