User login
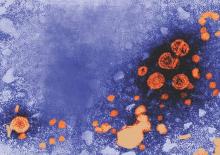
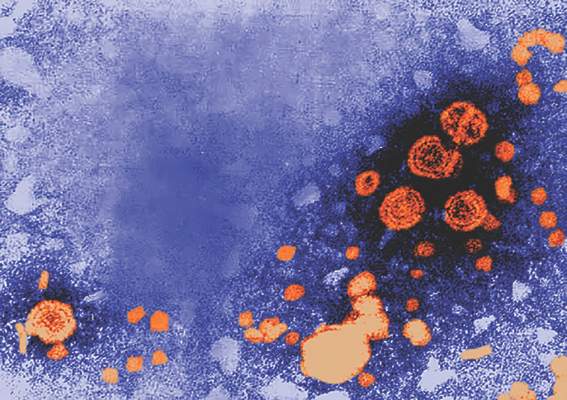
Hepatitis B vaccine in infancy provides long-term protection into adolescence
Pediatric doses of hepatitis B vaccine can provide long-term protection against hepatitis B up to 15-16 years, and also can produce strong immune memory, according to Dr. Olivier Van Der Meeren of GlaxoSmithKline Vaccines, Wavre, Belgium, and his associates.
The researchers looked at 303 healthy adolescents who had received three doses of monovalent pediatric hepatitis B vaccine (containing 10 mcg hepatitis B surface antigen, HBsAg) in infancy. Of the 293 patients analyzed, 71% were seropositive (anti-HBs antibodies greater than or equal to 6.2 mIU/mL) before the challenge dose and 65% remained seroprotected (anti-HBs antibodies greater than or equal to 10 mIU/mL) after challenge. One month after the challenge dose, the percentage of seroprotected subjects increased to 99%, and 91% of those patients had anti-HBs antibody concentrations greater than or equal to 100 mIU/mL.
The study also looked at safety and reactogenicity. The researchers stated that it was well tolerated, with pain and fatigue the most frequently reported adverse effects.
“Despite declining levels of circulating anti-HBs antibodies, the vast majority of subjects in our study were able to mount a rapid and robust anamnestic response after a challenge dose (more than 150-fold increase in GMC [geometric mean concentration]) regardless of their pre-challenge serostatus,” the researchers concluded. “This confirms that maintaining anti-HBs antibody concentrations greater than 10 mIU/mL may not be essential for protection against clinically significant breakthrough hepatitis B infection.”
Find the study in Vaccine (doi:10.1016/j.vaccine.2016.04.013).
Pediatric doses of hepatitis B vaccine can provide long-term protection against hepatitis B up to 15-16 years, and also can produce strong immune memory, according to Dr. Olivier Van Der Meeren of GlaxoSmithKline Vaccines, Wavre, Belgium, and his associates.
The researchers looked at 303 healthy adolescents who had received three doses of monovalent pediatric hepatitis B vaccine (containing 10 mcg hepatitis B surface antigen, HBsAg) in infancy. Of the 293 patients analyzed, 71% were seropositive (anti-HBs antibodies greater than or equal to 6.2 mIU/mL) before the challenge dose and 65% remained seroprotected (anti-HBs antibodies greater than or equal to 10 mIU/mL) after challenge. One month after the challenge dose, the percentage of seroprotected subjects increased to 99%, and 91% of those patients had anti-HBs antibody concentrations greater than or equal to 100 mIU/mL.
The study also looked at safety and reactogenicity. The researchers stated that it was well tolerated, with pain and fatigue the most frequently reported adverse effects.
“Despite declining levels of circulating anti-HBs antibodies, the vast majority of subjects in our study were able to mount a rapid and robust anamnestic response after a challenge dose (more than 150-fold increase in GMC [geometric mean concentration]) regardless of their pre-challenge serostatus,” the researchers concluded. “This confirms that maintaining anti-HBs antibody concentrations greater than 10 mIU/mL may not be essential for protection against clinically significant breakthrough hepatitis B infection.”
Find the study in Vaccine (doi:10.1016/j.vaccine.2016.04.013).
Pediatric doses of hepatitis B vaccine can provide long-term protection against hepatitis B up to 15-16 years, and also can produce strong immune memory, according to Dr. Olivier Van Der Meeren of GlaxoSmithKline Vaccines, Wavre, Belgium, and his associates.
The researchers looked at 303 healthy adolescents who had received three doses of monovalent pediatric hepatitis B vaccine (containing 10 mcg hepatitis B surface antigen, HBsAg) in infancy. Of the 293 patients analyzed, 71% were seropositive (anti-HBs antibodies greater than or equal to 6.2 mIU/mL) before the challenge dose and 65% remained seroprotected (anti-HBs antibodies greater than or equal to 10 mIU/mL) after challenge. One month after the challenge dose, the percentage of seroprotected subjects increased to 99%, and 91% of those patients had anti-HBs antibody concentrations greater than or equal to 100 mIU/mL.
The study also looked at safety and reactogenicity. The researchers stated that it was well tolerated, with pain and fatigue the most frequently reported adverse effects.
“Despite declining levels of circulating anti-HBs antibodies, the vast majority of subjects in our study were able to mount a rapid and robust anamnestic response after a challenge dose (more than 150-fold increase in GMC [geometric mean concentration]) regardless of their pre-challenge serostatus,” the researchers concluded. “This confirms that maintaining anti-HBs antibody concentrations greater than 10 mIU/mL may not be essential for protection against clinically significant breakthrough hepatitis B infection.”
Find the study in Vaccine (doi:10.1016/j.vaccine.2016.04.013).
FROM VACCINE
FDA: Olanzapine Can Cause Serious Skin Reaction
Olanzapine can cause a rare but serious skin reaction that can affect other parts of the body, according to a Food and Drug Administration safety alert released May 10.
The condition linked to all products containing the second-generation antipsychotic is called Drug Reaction with Eosinophilia and Systemic Symptoms, or DRESS. Symptoms of DRESS include a rash that can spread to all parts of the body, fever, swollen lymph nodes, and swelling. In addition, DRESS can result in injury to the liver, kidneys, lungs, heart, or pancreas, and it also can lead to death. The mortality tied to DRESS can reach 10%, the FDA said.
The FDA Adverse Event Reporting System database has identified 23 cases worldwide of DRESS resulting from olanzapine since 1996, including one patient who died. Currently, the only way to treat DRESS is to withdraw the drug promptly. “Health care professionals should immediately stop treatment with olanzapine if DRESS is suspected,” the safety alert states. “The important ways to manage DRESS are early recognition of the syndrome, discontinuation of the offending agent as soon as possible, and supportive care.”
Olanzapine, used to treat schizophrenia and manic episodes of bipolar disorder, is available in generic versions. The medication also is available under the brand names Zyprexa, Zyprexa Zydis, Zyprexa Relprevv, and Symbyax. The agency said it would add a warning describing DRESS to the labels of drugs containing olanzapine.
Read the full safety alert on the FDA website.
Olanzapine can cause a rare but serious skin reaction that can affect other parts of the body, according to a Food and Drug Administration safety alert released May 10.
The condition linked to all products containing the second-generation antipsychotic is called Drug Reaction with Eosinophilia and Systemic Symptoms, or DRESS. Symptoms of DRESS include a rash that can spread to all parts of the body, fever, swollen lymph nodes, and swelling. In addition, DRESS can result in injury to the liver, kidneys, lungs, heart, or pancreas, and it also can lead to death. The mortality tied to DRESS can reach 10%, the FDA said.
The FDA Adverse Event Reporting System database has identified 23 cases worldwide of DRESS resulting from olanzapine since 1996, including one patient who died. Currently, the only way to treat DRESS is to withdraw the drug promptly. “Health care professionals should immediately stop treatment with olanzapine if DRESS is suspected,” the safety alert states. “The important ways to manage DRESS are early recognition of the syndrome, discontinuation of the offending agent as soon as possible, and supportive care.”
Olanzapine, used to treat schizophrenia and manic episodes of bipolar disorder, is available in generic versions. The medication also is available under the brand names Zyprexa, Zyprexa Zydis, Zyprexa Relprevv, and Symbyax. The agency said it would add a warning describing DRESS to the labels of drugs containing olanzapine.
Read the full safety alert on the FDA website.
Olanzapine can cause a rare but serious skin reaction that can affect other parts of the body, according to a Food and Drug Administration safety alert released May 10.
The condition linked to all products containing the second-generation antipsychotic is called Drug Reaction with Eosinophilia and Systemic Symptoms, or DRESS. Symptoms of DRESS include a rash that can spread to all parts of the body, fever, swollen lymph nodes, and swelling. In addition, DRESS can result in injury to the liver, kidneys, lungs, heart, or pancreas, and it also can lead to death. The mortality tied to DRESS can reach 10%, the FDA said.
The FDA Adverse Event Reporting System database has identified 23 cases worldwide of DRESS resulting from olanzapine since 1996, including one patient who died. Currently, the only way to treat DRESS is to withdraw the drug promptly. “Health care professionals should immediately stop treatment with olanzapine if DRESS is suspected,” the safety alert states. “The important ways to manage DRESS are early recognition of the syndrome, discontinuation of the offending agent as soon as possible, and supportive care.”
Olanzapine, used to treat schizophrenia and manic episodes of bipolar disorder, is available in generic versions. The medication also is available under the brand names Zyprexa, Zyprexa Zydis, Zyprexa Relprevv, and Symbyax. The agency said it would add a warning describing DRESS to the labels of drugs containing olanzapine.
Read the full safety alert on the FDA website.
FDA: Olanzapine can cause serious skin reaction
Olanzapine can cause a rare but serious skin reaction that can affect other parts of the body, according to a Food and Drug Administration safety alert released May 10.
The condition linked to all products containing the second-generation antipsychotic is called Drug Reaction with Eosinophilia and Systemic Symptoms, or DRESS. Symptoms of DRESS include a rash that can spread to all parts of the body, fever, swollen lymph nodes, and swelling. In addition, DRESS can result in injury to the liver, kidneys, lungs, heart, or pancreas, and it also can lead to death. The mortality tied to DRESS can reach 10%, the FDA said.
The FDA Adverse Event Reporting System database has identified 23 cases worldwide of DRESS resulting from olanzapine since 1996, including one patient who died. Currently, the only way to treat DRESS is to withdraw the drug promptly. “Health care professionals should immediately stop treatment with olanzapine if DRESS is suspected,” the safety alert states. “The important ways to manage DRESS are early recognition of the syndrome, discontinuation of the offending agent as soon as possible, and supportive care.”
Olanzapine, used to treat schizophrenia and manic episodes of bipolar disorder, is available in generic versions. The medication also is available under the brand names Zyprexa, Zyprexa Zydis, Zyprexa Relprevv, and Symbyax. The agency said it would add a warning describing DRESS to the labels of drugs containing olanzapine.
Read the full safety alert on the FDA website.
Olanzapine can cause a rare but serious skin reaction that can affect other parts of the body, according to a Food and Drug Administration safety alert released May 10.
The condition linked to all products containing the second-generation antipsychotic is called Drug Reaction with Eosinophilia and Systemic Symptoms, or DRESS. Symptoms of DRESS include a rash that can spread to all parts of the body, fever, swollen lymph nodes, and swelling. In addition, DRESS can result in injury to the liver, kidneys, lungs, heart, or pancreas, and it also can lead to death. The mortality tied to DRESS can reach 10%, the FDA said.
The FDA Adverse Event Reporting System database has identified 23 cases worldwide of DRESS resulting from olanzapine since 1996, including one patient who died. Currently, the only way to treat DRESS is to withdraw the drug promptly. “Health care professionals should immediately stop treatment with olanzapine if DRESS is suspected,” the safety alert states. “The important ways to manage DRESS are early recognition of the syndrome, discontinuation of the offending agent as soon as possible, and supportive care.”
Olanzapine, used to treat schizophrenia and manic episodes of bipolar disorder, is available in generic versions. The medication also is available under the brand names Zyprexa, Zyprexa Zydis, Zyprexa Relprevv, and Symbyax. The agency said it would add a warning describing DRESS to the labels of drugs containing olanzapine.
Read the full safety alert on the FDA website.
Olanzapine can cause a rare but serious skin reaction that can affect other parts of the body, according to a Food and Drug Administration safety alert released May 10.
The condition linked to all products containing the second-generation antipsychotic is called Drug Reaction with Eosinophilia and Systemic Symptoms, or DRESS. Symptoms of DRESS include a rash that can spread to all parts of the body, fever, swollen lymph nodes, and swelling. In addition, DRESS can result in injury to the liver, kidneys, lungs, heart, or pancreas, and it also can lead to death. The mortality tied to DRESS can reach 10%, the FDA said.
The FDA Adverse Event Reporting System database has identified 23 cases worldwide of DRESS resulting from olanzapine since 1996, including one patient who died. Currently, the only way to treat DRESS is to withdraw the drug promptly. “Health care professionals should immediately stop treatment with olanzapine if DRESS is suspected,” the safety alert states. “The important ways to manage DRESS are early recognition of the syndrome, discontinuation of the offending agent as soon as possible, and supportive care.”
Olanzapine, used to treat schizophrenia and manic episodes of bipolar disorder, is available in generic versions. The medication also is available under the brand names Zyprexa, Zyprexa Zydis, Zyprexa Relprevv, and Symbyax. The agency said it would add a warning describing DRESS to the labels of drugs containing olanzapine.
Read the full safety alert on the FDA website.
USPSTF recommends daily folic acid supplements for women of childbearing age
All women who are capable of getting pregnant should take a daily supplement containing 400-800 micrograms of folic acid to prevent neural tube defects in early pregnancy, according to a draft recommendation from the U.S. Preventive Services Task Force.
The grade A draft recommendation, issued May 10, reaffirms the Task Force’s 2009 recommendation on folic acid supplementation in women of childbearing age.
The critical period for supplementation occurs 1 month before conception and continues through the first 2-3 months of pregnancy, according to the draft recommendation. Although folic acid is found naturally in many fruits and vegetables, and many cereals and breads are fortified with folic acid, most women still fall short of the daily recommended dose of 400 micrograms of folic acid.
In the evidence review, the USPSTF evaluated one randomized controlled trial, two cohort studies, and eight case-control studies for evidence of effectiveness of folic acid supplementation. The Task Force found no substantial new evidence on benefits and harms from folic acid supplementation to change its 2009 recommendation.
“The USPSTF concludes with high certainty that the net benefit of daily folic acid supplementation to prevent neural tube defects in the developing fetus is substantial for women who are planning or capable of pregnancy,” the statement noted.
The draft recommendation is open for public comment on the USPSTF website until June 6.
All women who are capable of getting pregnant should take a daily supplement containing 400-800 micrograms of folic acid to prevent neural tube defects in early pregnancy, according to a draft recommendation from the U.S. Preventive Services Task Force.
The grade A draft recommendation, issued May 10, reaffirms the Task Force’s 2009 recommendation on folic acid supplementation in women of childbearing age.
The critical period for supplementation occurs 1 month before conception and continues through the first 2-3 months of pregnancy, according to the draft recommendation. Although folic acid is found naturally in many fruits and vegetables, and many cereals and breads are fortified with folic acid, most women still fall short of the daily recommended dose of 400 micrograms of folic acid.
In the evidence review, the USPSTF evaluated one randomized controlled trial, two cohort studies, and eight case-control studies for evidence of effectiveness of folic acid supplementation. The Task Force found no substantial new evidence on benefits and harms from folic acid supplementation to change its 2009 recommendation.
“The USPSTF concludes with high certainty that the net benefit of daily folic acid supplementation to prevent neural tube defects in the developing fetus is substantial for women who are planning or capable of pregnancy,” the statement noted.
The draft recommendation is open for public comment on the USPSTF website until June 6.
All women who are capable of getting pregnant should take a daily supplement containing 400-800 micrograms of folic acid to prevent neural tube defects in early pregnancy, according to a draft recommendation from the U.S. Preventive Services Task Force.
The grade A draft recommendation, issued May 10, reaffirms the Task Force’s 2009 recommendation on folic acid supplementation in women of childbearing age.
The critical period for supplementation occurs 1 month before conception and continues through the first 2-3 months of pregnancy, according to the draft recommendation. Although folic acid is found naturally in many fruits and vegetables, and many cereals and breads are fortified with folic acid, most women still fall short of the daily recommended dose of 400 micrograms of folic acid.
In the evidence review, the USPSTF evaluated one randomized controlled trial, two cohort studies, and eight case-control studies for evidence of effectiveness of folic acid supplementation. The Task Force found no substantial new evidence on benefits and harms from folic acid supplementation to change its 2009 recommendation.
“The USPSTF concludes with high certainty that the net benefit of daily folic acid supplementation to prevent neural tube defects in the developing fetus is substantial for women who are planning or capable of pregnancy,” the statement noted.
The draft recommendation is open for public comment on the USPSTF website until June 6.
Phone coaching adds limited benefits in knee osteoarthritis
Adding telephone coaching to a home-based physiotherapist-prescribed activity program does not increase the pain and function benefits of such a program alone in knee osteoarthritis, a randomized controlled trial shows.
Kim L. Bennell, Ph.D., and her associates recruited volunteers who were aged 50 years and older, had knee pain rated at 4 or higher on an 11-point scale, and were classified as sedentary. One group participated in both coaching and the home-based physiotherapy program; the other participated in the home-based physiotherapy program alone.
Overall,142 (85%), 136 (81%), and 128 (76%) participants completed 6-, 12-, and 18-month measurements. In the 6-month outcomes, no significance differences were found between the two groups in average pain (mean difference, 0.4 units) or in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) function (1.8 units). In addition, there was no change between group differences observed at either 12 or 18 months. At 6 months, however, both groups showed large significant and clinically important improvements from baseline in the primary outcomes of pain and function, reported Dr. Bennell of the Centre for Health, Exercise and Sports Medicine at the University of Melbourne.
Reseachers also examined secondary outcomes and found there was no significant difference for change in numeric rating scale walking pain, WOMAC pain, or quality-of-life scores at any time.
“Improving exercise adherence was an aim of our coaching intervention given that adherence is positively linked to clinical outcomes in knee OA,” the reseachers concluded. “Our study provides novel information about the effects of telephone coaching alongside a physiotherapy prescribed physical activity and exercise program and extends the limited research in telephone coaching for OA.”
Read the full study in Arthritis Care & Research (doi: 10.1002/acr.22915).
Adding telephone coaching to a home-based physiotherapist-prescribed activity program does not increase the pain and function benefits of such a program alone in knee osteoarthritis, a randomized controlled trial shows.
Kim L. Bennell, Ph.D., and her associates recruited volunteers who were aged 50 years and older, had knee pain rated at 4 or higher on an 11-point scale, and were classified as sedentary. One group participated in both coaching and the home-based physiotherapy program; the other participated in the home-based physiotherapy program alone.
Overall,142 (85%), 136 (81%), and 128 (76%) participants completed 6-, 12-, and 18-month measurements. In the 6-month outcomes, no significance differences were found between the two groups in average pain (mean difference, 0.4 units) or in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) function (1.8 units). In addition, there was no change between group differences observed at either 12 or 18 months. At 6 months, however, both groups showed large significant and clinically important improvements from baseline in the primary outcomes of pain and function, reported Dr. Bennell of the Centre for Health, Exercise and Sports Medicine at the University of Melbourne.
Reseachers also examined secondary outcomes and found there was no significant difference for change in numeric rating scale walking pain, WOMAC pain, or quality-of-life scores at any time.
“Improving exercise adherence was an aim of our coaching intervention given that adherence is positively linked to clinical outcomes in knee OA,” the reseachers concluded. “Our study provides novel information about the effects of telephone coaching alongside a physiotherapy prescribed physical activity and exercise program and extends the limited research in telephone coaching for OA.”
Read the full study in Arthritis Care & Research (doi: 10.1002/acr.22915).
Adding telephone coaching to a home-based physiotherapist-prescribed activity program does not increase the pain and function benefits of such a program alone in knee osteoarthritis, a randomized controlled trial shows.
Kim L. Bennell, Ph.D., and her associates recruited volunteers who were aged 50 years and older, had knee pain rated at 4 or higher on an 11-point scale, and were classified as sedentary. One group participated in both coaching and the home-based physiotherapy program; the other participated in the home-based physiotherapy program alone.
Overall,142 (85%), 136 (81%), and 128 (76%) participants completed 6-, 12-, and 18-month measurements. In the 6-month outcomes, no significance differences were found between the two groups in average pain (mean difference, 0.4 units) or in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) function (1.8 units). In addition, there was no change between group differences observed at either 12 or 18 months. At 6 months, however, both groups showed large significant and clinically important improvements from baseline in the primary outcomes of pain and function, reported Dr. Bennell of the Centre for Health, Exercise and Sports Medicine at the University of Melbourne.
Reseachers also examined secondary outcomes and found there was no significant difference for change in numeric rating scale walking pain, WOMAC pain, or quality-of-life scores at any time.
“Improving exercise adherence was an aim of our coaching intervention given that adherence is positively linked to clinical outcomes in knee OA,” the reseachers concluded. “Our study provides novel information about the effects of telephone coaching alongside a physiotherapy prescribed physical activity and exercise program and extends the limited research in telephone coaching for OA.”
Read the full study in Arthritis Care & Research (doi: 10.1002/acr.22915).
FROM ARTHRITIS CARE & RESEARCH
High-risk siblings of ASD children show lower levels of initiating joint attention
High-risk siblings of children with autism spectrum disorder (ASD) show lower levels of initiating joint attention (IJA) than do low-risk siblings of children without ASD, according to Devon N. Gangi, Ph.D., and his associates.
“Early deficits in [IJA], a form of referential communication involving the use of gaze and gesture to coordinate attention between social partners and objects, are a core feature of ASD,” the researchers noted.
“We aimed to refine our understanding of heterogeneity in early behavior relevant to ASD by examining the role of common genetic variants,” they wrote. “To our knowledge, this is the first investigation of these genetic variants in relation to joint attention in siblings at risk for ASD.”
In the preliminary analysis, among the children with 7-repeat allele in the DRD4 genotype, high-risk siblings exhibited lower levels of IJA (M = –0.52, SD = 0.75) than did low-risk siblings (M = 0.73, SD = 1.01), (t [24] = 3.62, P = .001). Also, in the DRD2 genotype, there was a main effect of group status, (P = .01), with high-risk siblings (M = –0.13, SD = 0.84) exhibiting lower levels of IJA than those of low-risk siblings (M = 0.29, SD = 0.86), the researchers wrote.
“Among high-risk siblings, early behavior often predicts diagnosis, but these patterns of prediction are not clear,” they noted.
The study also examined dopamine scores in both high- and low-risk siblings in correlation with IJA. Read the study in Autism Research (doi: 10.1002/aur.1623).
High-risk siblings of children with autism spectrum disorder (ASD) show lower levels of initiating joint attention (IJA) than do low-risk siblings of children without ASD, according to Devon N. Gangi, Ph.D., and his associates.
“Early deficits in [IJA], a form of referential communication involving the use of gaze and gesture to coordinate attention between social partners and objects, are a core feature of ASD,” the researchers noted.
“We aimed to refine our understanding of heterogeneity in early behavior relevant to ASD by examining the role of common genetic variants,” they wrote. “To our knowledge, this is the first investigation of these genetic variants in relation to joint attention in siblings at risk for ASD.”
In the preliminary analysis, among the children with 7-repeat allele in the DRD4 genotype, high-risk siblings exhibited lower levels of IJA (M = –0.52, SD = 0.75) than did low-risk siblings (M = 0.73, SD = 1.01), (t [24] = 3.62, P = .001). Also, in the DRD2 genotype, there was a main effect of group status, (P = .01), with high-risk siblings (M = –0.13, SD = 0.84) exhibiting lower levels of IJA than those of low-risk siblings (M = 0.29, SD = 0.86), the researchers wrote.
“Among high-risk siblings, early behavior often predicts diagnosis, but these patterns of prediction are not clear,” they noted.
The study also examined dopamine scores in both high- and low-risk siblings in correlation with IJA. Read the study in Autism Research (doi: 10.1002/aur.1623).
High-risk siblings of children with autism spectrum disorder (ASD) show lower levels of initiating joint attention (IJA) than do low-risk siblings of children without ASD, according to Devon N. Gangi, Ph.D., and his associates.
“Early deficits in [IJA], a form of referential communication involving the use of gaze and gesture to coordinate attention between social partners and objects, are a core feature of ASD,” the researchers noted.
“We aimed to refine our understanding of heterogeneity in early behavior relevant to ASD by examining the role of common genetic variants,” they wrote. “To our knowledge, this is the first investigation of these genetic variants in relation to joint attention in siblings at risk for ASD.”
In the preliminary analysis, among the children with 7-repeat allele in the DRD4 genotype, high-risk siblings exhibited lower levels of IJA (M = –0.52, SD = 0.75) than did low-risk siblings (M = 0.73, SD = 1.01), (t [24] = 3.62, P = .001). Also, in the DRD2 genotype, there was a main effect of group status, (P = .01), with high-risk siblings (M = –0.13, SD = 0.84) exhibiting lower levels of IJA than those of low-risk siblings (M = 0.29, SD = 0.86), the researchers wrote.
“Among high-risk siblings, early behavior often predicts diagnosis, but these patterns of prediction are not clear,” they noted.
The study also examined dopamine scores in both high- and low-risk siblings in correlation with IJA. Read the study in Autism Research (doi: 10.1002/aur.1623).
FROM AUTISM RESEARCH
FDA Approves First Drug to Treat Hallucinations in Parkinson’s Psychosis
Pimavanserin on April 29 became the first drug to receive approval from the Food and Drug Administration for the indication of hallucinations and delusions associated with psychosis in Parkinson’s disease.
The drug, to be marketed under the brand name Nuplazid by Acadia Pharmaceuticals, was shown in a 6-week clinical trial of 199 participants to be superior to placebo in decreasing the frequency and/or severity of hallucinations and delusions without worsening the primary motor symptoms of Parkinson’s disease.
The most common side effects reported from the clinical trial included peripheral edema, nausea, and confused state of mind.
“Nuplazid represents an important treatment for people with Parkinson’s disease who experience these symptoms,” said Dr. Mitchell Mathis, director of the Division of Psychiatry Products in the FDA’s Center for Drug Evaluation and Research.
The FDA gave pimavanserin a Boxed Warning in relation to the general increased risk of death associated with the use of atypical antipsychotic drugs to treat older people with dementia-related psychosis. No other drug atypical antipsychotic drug has been approved to treat patients with dementia-related psychosis.
Read the agency’s full statement on the FDA website.
Pimavanserin on April 29 became the first drug to receive approval from the Food and Drug Administration for the indication of hallucinations and delusions associated with psychosis in Parkinson’s disease.
The drug, to be marketed under the brand name Nuplazid by Acadia Pharmaceuticals, was shown in a 6-week clinical trial of 199 participants to be superior to placebo in decreasing the frequency and/or severity of hallucinations and delusions without worsening the primary motor symptoms of Parkinson’s disease.
The most common side effects reported from the clinical trial included peripheral edema, nausea, and confused state of mind.
“Nuplazid represents an important treatment for people with Parkinson’s disease who experience these symptoms,” said Dr. Mitchell Mathis, director of the Division of Psychiatry Products in the FDA’s Center for Drug Evaluation and Research.
The FDA gave pimavanserin a Boxed Warning in relation to the general increased risk of death associated with the use of atypical antipsychotic drugs to treat older people with dementia-related psychosis. No other drug atypical antipsychotic drug has been approved to treat patients with dementia-related psychosis.
Read the agency’s full statement on the FDA website.
Pimavanserin on April 29 became the first drug to receive approval from the Food and Drug Administration for the indication of hallucinations and delusions associated with psychosis in Parkinson’s disease.
The drug, to be marketed under the brand name Nuplazid by Acadia Pharmaceuticals, was shown in a 6-week clinical trial of 199 participants to be superior to placebo in decreasing the frequency and/or severity of hallucinations and delusions without worsening the primary motor symptoms of Parkinson’s disease.
The most common side effects reported from the clinical trial included peripheral edema, nausea, and confused state of mind.
“Nuplazid represents an important treatment for people with Parkinson’s disease who experience these symptoms,” said Dr. Mitchell Mathis, director of the Division of Psychiatry Products in the FDA’s Center for Drug Evaluation and Research.
The FDA gave pimavanserin a Boxed Warning in relation to the general increased risk of death associated with the use of atypical antipsychotic drugs to treat older people with dementia-related psychosis. No other drug atypical antipsychotic drug has been approved to treat patients with dementia-related psychosis.
Read the agency’s full statement on the FDA website.
FDA approves first drug to treat hallucinations in Parkinson’s psychosis
Pimavanserin on April 29 became the first drug to receive approval from the Food and Drug Administration for the indication of hallucinations and delusions associated with psychosis in Parkinson’s disease.
The drug, to be marketed under the brand name Nuplazid by Acadia Pharmaceuticals, was shown in a 6-week clinical trial of 199 participants to be superior to placebo in decreasing the frequency and/or severity of hallucinations and delusions without worsening the primary motor symptoms of Parkinson’s disease.
The most common side effects reported from the clinical trial included peripheral edema, nausea, and confused state of mind.
“Nuplazid represents an important treatment for people with Parkinson’s disease who experience these symptoms,” said Dr. Mitchell Mathis, director of the Division of Psychiatry Products in the FDA’s Center for Drug Evaluation and Research.
The FDA gave pimavanserin a Boxed Warning in relation to the general increased risk of death associated with the use of atypical antipsychotic drugs to treat older people with dementia-related psychosis. No other drug atypical antipsychotic drug has been approved to treat patients with dementia-related psychosis.
Read the agency’s full statement on the FDA website.
Pimavanserin on April 29 became the first drug to receive approval from the Food and Drug Administration for the indication of hallucinations and delusions associated with psychosis in Parkinson’s disease.
The drug, to be marketed under the brand name Nuplazid by Acadia Pharmaceuticals, was shown in a 6-week clinical trial of 199 participants to be superior to placebo in decreasing the frequency and/or severity of hallucinations and delusions without worsening the primary motor symptoms of Parkinson’s disease.
The most common side effects reported from the clinical trial included peripheral edema, nausea, and confused state of mind.
“Nuplazid represents an important treatment for people with Parkinson’s disease who experience these symptoms,” said Dr. Mitchell Mathis, director of the Division of Psychiatry Products in the FDA’s Center for Drug Evaluation and Research.
The FDA gave pimavanserin a Boxed Warning in relation to the general increased risk of death associated with the use of atypical antipsychotic drugs to treat older people with dementia-related psychosis. No other drug atypical antipsychotic drug has been approved to treat patients with dementia-related psychosis.
Read the agency’s full statement on the FDA website.
Pimavanserin on April 29 became the first drug to receive approval from the Food and Drug Administration for the indication of hallucinations and delusions associated with psychosis in Parkinson’s disease.
The drug, to be marketed under the brand name Nuplazid by Acadia Pharmaceuticals, was shown in a 6-week clinical trial of 199 participants to be superior to placebo in decreasing the frequency and/or severity of hallucinations and delusions without worsening the primary motor symptoms of Parkinson’s disease.
The most common side effects reported from the clinical trial included peripheral edema, nausea, and confused state of mind.
“Nuplazid represents an important treatment for people with Parkinson’s disease who experience these symptoms,” said Dr. Mitchell Mathis, director of the Division of Psychiatry Products in the FDA’s Center for Drug Evaluation and Research.
The FDA gave pimavanserin a Boxed Warning in relation to the general increased risk of death associated with the use of atypical antipsychotic drugs to treat older people with dementia-related psychosis. No other drug atypical antipsychotic drug has been approved to treat patients with dementia-related psychosis.
Read the agency’s full statement on the FDA website.
Neuraminidase inhibition titer a better predictor of influenza protection
Neuraminidase inhibition (NAI) titer is a better predictor of protection against influenza infection than hemagglutination inhibition (HAI) titer, according to new research, which could have implications for future flu vaccine development.
Investigators at the National Institute of Allergy and Infectious Diseases (NIAID) and the University of Pennsylvania, Philadelphia, performed a healthy volunteer challenge study with a wild-type 2009 A(H1N1)pdm influenza A challenge virus at the NIH Clinical Center in Bethesda, Md., to evaluate two groups of participants with HAI titers of greater than 1:40 and less than 1:40. The primary objective was to determine whether participants with HAI titers of greater than 1:40 were less likely to develop mild to moderate influenza disease after intranasal inoculation
In a multiple regression analysis, researchers evaluated the independent effects of both HAI and NAI titers on four diseases severity measures. In all measures – duration of shedding (HAI: P = .164; NAI: P less than .001), duration of symptoms (HAI: P = .497; NAI: P = .011), number of symptoms (HAI: P = .533; NAI: P less than .001), and symptom severity score (HAI: P = .906; NAI: P less than .001) – increasing NAI titers showed a statistically significant independent effect of decreasing severity, while HAI titers showed no significant independent effect on any of the disease severity measures examined.
When grouped by baseline NAI titers, those participants with high titers (greater than or equal to 1:40) had only minimal increases in NAI after challenge, but unlike HAI titer, every cohort with a low NAI titer had a rise in NAI titer after challenge, regardless of the outcome.
“These data further suggest that NAI titer may play a more significant role as a correlate of protection than previously thought and that the role of neuraminidase immunity should be considered when studying influenza susceptibility after vaccination and as a critical target in future influenza vaccine platforms,” Dr. Jeffery K. Taubenberger of the NIAID and his coauthors concluded.
This study was the first time the current “gold standard” for evaluating influenza vaccines – a protective HAI titer of greater than 1:40 – has been evaluated in a well-controlled healthy volunteer challenge since the cutoff was established, and the first time NAI titer has been identified in a controlled trial to be an independent predictor of a reduction in all aspects of influenza. The authors declared no conflicts of interest.
Read the full study in mBio (doi: 10.1128/mBio.00417-16).
Neuraminidase inhibition (NAI) titer is a better predictor of protection against influenza infection than hemagglutination inhibition (HAI) titer, according to new research, which could have implications for future flu vaccine development.
Investigators at the National Institute of Allergy and Infectious Diseases (NIAID) and the University of Pennsylvania, Philadelphia, performed a healthy volunteer challenge study with a wild-type 2009 A(H1N1)pdm influenza A challenge virus at the NIH Clinical Center in Bethesda, Md., to evaluate two groups of participants with HAI titers of greater than 1:40 and less than 1:40. The primary objective was to determine whether participants with HAI titers of greater than 1:40 were less likely to develop mild to moderate influenza disease after intranasal inoculation
In a multiple regression analysis, researchers evaluated the independent effects of both HAI and NAI titers on four diseases severity measures. In all measures – duration of shedding (HAI: P = .164; NAI: P less than .001), duration of symptoms (HAI: P = .497; NAI: P = .011), number of symptoms (HAI: P = .533; NAI: P less than .001), and symptom severity score (HAI: P = .906; NAI: P less than .001) – increasing NAI titers showed a statistically significant independent effect of decreasing severity, while HAI titers showed no significant independent effect on any of the disease severity measures examined.
When grouped by baseline NAI titers, those participants with high titers (greater than or equal to 1:40) had only minimal increases in NAI after challenge, but unlike HAI titer, every cohort with a low NAI titer had a rise in NAI titer after challenge, regardless of the outcome.
“These data further suggest that NAI titer may play a more significant role as a correlate of protection than previously thought and that the role of neuraminidase immunity should be considered when studying influenza susceptibility after vaccination and as a critical target in future influenza vaccine platforms,” Dr. Jeffery K. Taubenberger of the NIAID and his coauthors concluded.
This study was the first time the current “gold standard” for evaluating influenza vaccines – a protective HAI titer of greater than 1:40 – has been evaluated in a well-controlled healthy volunteer challenge since the cutoff was established, and the first time NAI titer has been identified in a controlled trial to be an independent predictor of a reduction in all aspects of influenza. The authors declared no conflicts of interest.
Read the full study in mBio (doi: 10.1128/mBio.00417-16).
Neuraminidase inhibition (NAI) titer is a better predictor of protection against influenza infection than hemagglutination inhibition (HAI) titer, according to new research, which could have implications for future flu vaccine development.
Investigators at the National Institute of Allergy and Infectious Diseases (NIAID) and the University of Pennsylvania, Philadelphia, performed a healthy volunteer challenge study with a wild-type 2009 A(H1N1)pdm influenza A challenge virus at the NIH Clinical Center in Bethesda, Md., to evaluate two groups of participants with HAI titers of greater than 1:40 and less than 1:40. The primary objective was to determine whether participants with HAI titers of greater than 1:40 were less likely to develop mild to moderate influenza disease after intranasal inoculation
In a multiple regression analysis, researchers evaluated the independent effects of both HAI and NAI titers on four diseases severity measures. In all measures – duration of shedding (HAI: P = .164; NAI: P less than .001), duration of symptoms (HAI: P = .497; NAI: P = .011), number of symptoms (HAI: P = .533; NAI: P less than .001), and symptom severity score (HAI: P = .906; NAI: P less than .001) – increasing NAI titers showed a statistically significant independent effect of decreasing severity, while HAI titers showed no significant independent effect on any of the disease severity measures examined.
When grouped by baseline NAI titers, those participants with high titers (greater than or equal to 1:40) had only minimal increases in NAI after challenge, but unlike HAI titer, every cohort with a low NAI titer had a rise in NAI titer after challenge, regardless of the outcome.
“These data further suggest that NAI titer may play a more significant role as a correlate of protection than previously thought and that the role of neuraminidase immunity should be considered when studying influenza susceptibility after vaccination and as a critical target in future influenza vaccine platforms,” Dr. Jeffery K. Taubenberger of the NIAID and his coauthors concluded.
This study was the first time the current “gold standard” for evaluating influenza vaccines – a protective HAI titer of greater than 1:40 – has been evaluated in a well-controlled healthy volunteer challenge since the cutoff was established, and the first time NAI titer has been identified in a controlled trial to be an independent predictor of a reduction in all aspects of influenza. The authors declared no conflicts of interest.
Read the full study in mBio (doi: 10.1128/mBio.00417-16).
FROM MBIO
FDA Evaluating the Use of Oral Fluconazole in Pregnancy
The Food and Drug Administration is reviewing the results of a Danish study that concludes there is a possible increased risk of miscarriage with the use of oral fluconazole (Diflucan) in pregnancy, according to a safety alert issued April 26.
The current drug label for oral fluconazole states that data from studies in women does not suggest an increased risk of problems during pregnancy or abnormalities in developing babies when women used a single 150-mg dose to treat vaginal yeast infections. However, reports of abnormalities at birth have resulted from high doses (400-800 mg/day) taken during pregnancy for much longer than a single dose. The Danish study had most pregnant women use one or two doses of 150 mg.
Oral fluconazole is used to treat yeast infections of the vaginal area, mouth, and esophagus. It can also be used to treat a fungal infection of the brain and spinal cord.
The FDA is also evaluating additional data and will make recommendations when the review is complete.
“Until FDA’s review is complete and more is understood about this study and other available data, FDA advises cautious prescribing of oral fluconazole in pregnancy,” the safety alert states.
The FDA also noted that the Centers for Disease Control and Prevention recommends using topical antifungal products only when treating pregnant women with vulvovaginal yeast infections.
Read more about the investigation on the FDA website.
The Food and Drug Administration is reviewing the results of a Danish study that concludes there is a possible increased risk of miscarriage with the use of oral fluconazole (Diflucan) in pregnancy, according to a safety alert issued April 26.
The current drug label for oral fluconazole states that data from studies in women does not suggest an increased risk of problems during pregnancy or abnormalities in developing babies when women used a single 150-mg dose to treat vaginal yeast infections. However, reports of abnormalities at birth have resulted from high doses (400-800 mg/day) taken during pregnancy for much longer than a single dose. The Danish study had most pregnant women use one or two doses of 150 mg.
Oral fluconazole is used to treat yeast infections of the vaginal area, mouth, and esophagus. It can also be used to treat a fungal infection of the brain and spinal cord.
The FDA is also evaluating additional data and will make recommendations when the review is complete.
“Until FDA’s review is complete and more is understood about this study and other available data, FDA advises cautious prescribing of oral fluconazole in pregnancy,” the safety alert states.
The FDA also noted that the Centers for Disease Control and Prevention recommends using topical antifungal products only when treating pregnant women with vulvovaginal yeast infections.
Read more about the investigation on the FDA website.
The Food and Drug Administration is reviewing the results of a Danish study that concludes there is a possible increased risk of miscarriage with the use of oral fluconazole (Diflucan) in pregnancy, according to a safety alert issued April 26.
The current drug label for oral fluconazole states that data from studies in women does not suggest an increased risk of problems during pregnancy or abnormalities in developing babies when women used a single 150-mg dose to treat vaginal yeast infections. However, reports of abnormalities at birth have resulted from high doses (400-800 mg/day) taken during pregnancy for much longer than a single dose. The Danish study had most pregnant women use one or two doses of 150 mg.
Oral fluconazole is used to treat yeast infections of the vaginal area, mouth, and esophagus. It can also be used to treat a fungal infection of the brain and spinal cord.
The FDA is also evaluating additional data and will make recommendations when the review is complete.
“Until FDA’s review is complete and more is understood about this study and other available data, FDA advises cautious prescribing of oral fluconazole in pregnancy,” the safety alert states.
The FDA also noted that the Centers for Disease Control and Prevention recommends using topical antifungal products only when treating pregnant women with vulvovaginal yeast infections.
Read more about the investigation on the FDA website.