User login
Half of newly detected antimicrobial antibodies do not lead to PBC
Nearly half of newly detected antimitochondrial antibodies (AMAs) in clinical practice do not lead to a diagnosis of primary biliary cholangitis (PBC), according to a prospective study.
Geraldine Dahlqvist, MD, and her associates examined 720 patients whose AMA tests were registered during a 1-year census period. They were divided into groups according to whether they were newly diagnosed (275), were previously diagnosed (216), or had a nonestablished diagnosis (229) of PBC. Results showed the prevalence of AMA-positive patients without evidence of PBC was 16.1 per 100,000 inhabitants. It was four (all AMA-positive patients) to six (PBC patients) times higher in women than in men. The median age was 58 years, with the median AMA titer at 1:16. Normal serum alkaline phosphatases (ALP) were 74%, and were 1.5 times above the upper limit of normal in 13% of patients, while cirrhosis was found in 6%. Among the patients with normal ALP and no evidence of cirrhosis, the 5-year incidence rate of PBC was 16%.
It was noted that no patients died officially from PBC in this study. The 1-, 3-, and 5-year rates of survival were 95%, 90%, and 75% (95% CI, 63-87), respectively, compared with 90% in the control group.
“The younger age and lower autoantibody titer of these patients, together with the frequent mild abnormalities of their biochemical liver tests, supports a very early, presymptomatic precholestatic stage of the disease,” Dr. Dahlqvist, of Catholic University of Louvain (Belgium), and her colleagues noted. “The incidence of clinical manifestations of PBC seems, however, much lower than previously reported.”
Find the full story in Hepatology (doi: 10.1002/hep.28559).
Nearly half of newly detected antimitochondrial antibodies (AMAs) in clinical practice do not lead to a diagnosis of primary biliary cholangitis (PBC), according to a prospective study.
Geraldine Dahlqvist, MD, and her associates examined 720 patients whose AMA tests were registered during a 1-year census period. They were divided into groups according to whether they were newly diagnosed (275), were previously diagnosed (216), or had a nonestablished diagnosis (229) of PBC. Results showed the prevalence of AMA-positive patients without evidence of PBC was 16.1 per 100,000 inhabitants. It was four (all AMA-positive patients) to six (PBC patients) times higher in women than in men. The median age was 58 years, with the median AMA titer at 1:16. Normal serum alkaline phosphatases (ALP) were 74%, and were 1.5 times above the upper limit of normal in 13% of patients, while cirrhosis was found in 6%. Among the patients with normal ALP and no evidence of cirrhosis, the 5-year incidence rate of PBC was 16%.
It was noted that no patients died officially from PBC in this study. The 1-, 3-, and 5-year rates of survival were 95%, 90%, and 75% (95% CI, 63-87), respectively, compared with 90% in the control group.
“The younger age and lower autoantibody titer of these patients, together with the frequent mild abnormalities of their biochemical liver tests, supports a very early, presymptomatic precholestatic stage of the disease,” Dr. Dahlqvist, of Catholic University of Louvain (Belgium), and her colleagues noted. “The incidence of clinical manifestations of PBC seems, however, much lower than previously reported.”
Find the full story in Hepatology (doi: 10.1002/hep.28559).
Nearly half of newly detected antimitochondrial antibodies (AMAs) in clinical practice do not lead to a diagnosis of primary biliary cholangitis (PBC), according to a prospective study.
Geraldine Dahlqvist, MD, and her associates examined 720 patients whose AMA tests were registered during a 1-year census period. They were divided into groups according to whether they were newly diagnosed (275), were previously diagnosed (216), or had a nonestablished diagnosis (229) of PBC. Results showed the prevalence of AMA-positive patients without evidence of PBC was 16.1 per 100,000 inhabitants. It was four (all AMA-positive patients) to six (PBC patients) times higher in women than in men. The median age was 58 years, with the median AMA titer at 1:16. Normal serum alkaline phosphatases (ALP) were 74%, and were 1.5 times above the upper limit of normal in 13% of patients, while cirrhosis was found in 6%. Among the patients with normal ALP and no evidence of cirrhosis, the 5-year incidence rate of PBC was 16%.
It was noted that no patients died officially from PBC in this study. The 1-, 3-, and 5-year rates of survival were 95%, 90%, and 75% (95% CI, 63-87), respectively, compared with 90% in the control group.
“The younger age and lower autoantibody titer of these patients, together with the frequent mild abnormalities of their biochemical liver tests, supports a very early, presymptomatic precholestatic stage of the disease,” Dr. Dahlqvist, of Catholic University of Louvain (Belgium), and her colleagues noted. “The incidence of clinical manifestations of PBC seems, however, much lower than previously reported.”
Find the full story in Hepatology (doi: 10.1002/hep.28559).
FROM HEPATOLOGY
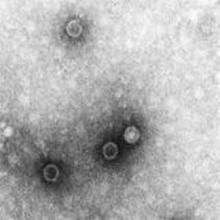
IPV boost after initial OPV offers sustained protection to at least 11 months
Protection against the poliovirus is lower at 1 month but remains sustained at 6 and 11 months after an inactivated poliovirus vaccine (IPV) boost following initial oral poliovirus vaccination (OPV), according to Jacob John, MD, of Christian Medical College, Vellore, Tamil Nadu, India, and his associates.
In a randomized controlled trial from Nov. 4 and Dec. 17, 2014, 900 healthy children from ages 1 to 4 years were randomly assigned between three study groups. The groups had the children receive IPV boost at 5 months (arm A), at enrollment (arm B), or no vaccine (arm C). Poliovirus shedding in stool 7 days after challenge, determined by Fisher’s exact test, was significantly lower in arms A and B, compared with C (risk ratio, 0.68; P = .003, RR, 0.70; P = .006 for arm A vs. C and B vs. C, respectively). The reduction in shedding was more marked for serotype 3 (RR, 0.60; P = .004, RR, 0.54; P = .001 respectively) than for serotype 1 (RR, 0.72; P = .057, RR, 0.80; P = .215, respectively).
It was noted that 41 serious adverse events (11 in arm A, 17 in arm B, and 13 in arm C), including 2 deaths in arm A, were reported during the trial. However, the reported adverse events were classified as unrelated, and the deaths were from leukemia and from viral hemorrhagic fever.
“The boost to intestinal immunity against poliovirus that results from administration of IPV to OPV-vaccinated children is sustained at 6 and 11 months. It is clear that IPV is playing an increasingly important role in the polio endgame as the world transitions away from the use of OPV,” the researchers concluded. “Every effort needs to be made to ensure supply of this vaccine to meet this expanding role.”
Find the full study in the Journal of Infectious Diseases 2016. doi: 10.1093/infdis/jiw595.
Protection against the poliovirus is lower at 1 month but remains sustained at 6 and 11 months after an inactivated poliovirus vaccine (IPV) boost following initial oral poliovirus vaccination (OPV), according to Jacob John, MD, of Christian Medical College, Vellore, Tamil Nadu, India, and his associates.
In a randomized controlled trial from Nov. 4 and Dec. 17, 2014, 900 healthy children from ages 1 to 4 years were randomly assigned between three study groups. The groups had the children receive IPV boost at 5 months (arm A), at enrollment (arm B), or no vaccine (arm C). Poliovirus shedding in stool 7 days after challenge, determined by Fisher’s exact test, was significantly lower in arms A and B, compared with C (risk ratio, 0.68; P = .003, RR, 0.70; P = .006 for arm A vs. C and B vs. C, respectively). The reduction in shedding was more marked for serotype 3 (RR, 0.60; P = .004, RR, 0.54; P = .001 respectively) than for serotype 1 (RR, 0.72; P = .057, RR, 0.80; P = .215, respectively).
It was noted that 41 serious adverse events (11 in arm A, 17 in arm B, and 13 in arm C), including 2 deaths in arm A, were reported during the trial. However, the reported adverse events were classified as unrelated, and the deaths were from leukemia and from viral hemorrhagic fever.
“The boost to intestinal immunity against poliovirus that results from administration of IPV to OPV-vaccinated children is sustained at 6 and 11 months. It is clear that IPV is playing an increasingly important role in the polio endgame as the world transitions away from the use of OPV,” the researchers concluded. “Every effort needs to be made to ensure supply of this vaccine to meet this expanding role.”
Find the full study in the Journal of Infectious Diseases 2016. doi: 10.1093/infdis/jiw595.
Protection against the poliovirus is lower at 1 month but remains sustained at 6 and 11 months after an inactivated poliovirus vaccine (IPV) boost following initial oral poliovirus vaccination (OPV), according to Jacob John, MD, of Christian Medical College, Vellore, Tamil Nadu, India, and his associates.
In a randomized controlled trial from Nov. 4 and Dec. 17, 2014, 900 healthy children from ages 1 to 4 years were randomly assigned between three study groups. The groups had the children receive IPV boost at 5 months (arm A), at enrollment (arm B), or no vaccine (arm C). Poliovirus shedding in stool 7 days after challenge, determined by Fisher’s exact test, was significantly lower in arms A and B, compared with C (risk ratio, 0.68; P = .003, RR, 0.70; P = .006 for arm A vs. C and B vs. C, respectively). The reduction in shedding was more marked for serotype 3 (RR, 0.60; P = .004, RR, 0.54; P = .001 respectively) than for serotype 1 (RR, 0.72; P = .057, RR, 0.80; P = .215, respectively).
It was noted that 41 serious adverse events (11 in arm A, 17 in arm B, and 13 in arm C), including 2 deaths in arm A, were reported during the trial. However, the reported adverse events were classified as unrelated, and the deaths were from leukemia and from viral hemorrhagic fever.
“The boost to intestinal immunity against poliovirus that results from administration of IPV to OPV-vaccinated children is sustained at 6 and 11 months. It is clear that IPV is playing an increasingly important role in the polio endgame as the world transitions away from the use of OPV,” the researchers concluded. “Every effort needs to be made to ensure supply of this vaccine to meet this expanding role.”
Find the full study in the Journal of Infectious Diseases 2016. doi: 10.1093/infdis/jiw595.
FROM THE JOURNAL OF INFECTIOUS DISEASES
Mesh fixation method had no impact on chronic postop pain in TAPP
WASHINGTON – Mesh fixation technique is not a factor in persistent pain after transabdominal preperitoneal (TAPP) groin hernia surgery, a study showed.
“Persistent pain is a well-known phenomenon after groin hernia surgery,” said Jakob Burcharth, MD, of University Hospital of Sjaelland Koge (Denmark). “The way that we fixate the mesh in laparoscopic surgery has been hypothesized to have an [impact] on the risk of persistent pain.”
In a study presented by Dr. Burcharth and his associates at the American College of Surgeons Clinical Congress, a total of 1,421 patients were examined. Each patient completed a validated pain questionnaire through the Danish Hernia Database from 2009 to 2012. The patients were divided into two groups: Group 1 had spray fibrin sealant (34%) for mesh fixation, and group 2 had tacks (66%). The results showed no difference between the groups in terms of pain in getting up from a chair, sitting or standing for more than 30 minutes, walking stairs, driving a car, or exercising, or in the need for postoperative analgesics or postoperative sick leave (all P greater than .20).
Dr. Burcharth concluded that a high number of patients reported persistent pain regardless of mesh fixation technique, which emphasizes the need for preoperative information.
Dr. Burcharth reported having no relevant financial disclosures.
WASHINGTON – Mesh fixation technique is not a factor in persistent pain after transabdominal preperitoneal (TAPP) groin hernia surgery, a study showed.
“Persistent pain is a well-known phenomenon after groin hernia surgery,” said Jakob Burcharth, MD, of University Hospital of Sjaelland Koge (Denmark). “The way that we fixate the mesh in laparoscopic surgery has been hypothesized to have an [impact] on the risk of persistent pain.”
In a study presented by Dr. Burcharth and his associates at the American College of Surgeons Clinical Congress, a total of 1,421 patients were examined. Each patient completed a validated pain questionnaire through the Danish Hernia Database from 2009 to 2012. The patients were divided into two groups: Group 1 had spray fibrin sealant (34%) for mesh fixation, and group 2 had tacks (66%). The results showed no difference between the groups in terms of pain in getting up from a chair, sitting or standing for more than 30 minutes, walking stairs, driving a car, or exercising, or in the need for postoperative analgesics or postoperative sick leave (all P greater than .20).
Dr. Burcharth concluded that a high number of patients reported persistent pain regardless of mesh fixation technique, which emphasizes the need for preoperative information.
Dr. Burcharth reported having no relevant financial disclosures.
WASHINGTON – Mesh fixation technique is not a factor in persistent pain after transabdominal preperitoneal (TAPP) groin hernia surgery, a study showed.
“Persistent pain is a well-known phenomenon after groin hernia surgery,” said Jakob Burcharth, MD, of University Hospital of Sjaelland Koge (Denmark). “The way that we fixate the mesh in laparoscopic surgery has been hypothesized to have an [impact] on the risk of persistent pain.”
In a study presented by Dr. Burcharth and his associates at the American College of Surgeons Clinical Congress, a total of 1,421 patients were examined. Each patient completed a validated pain questionnaire through the Danish Hernia Database from 2009 to 2012. The patients were divided into two groups: Group 1 had spray fibrin sealant (34%) for mesh fixation, and group 2 had tacks (66%). The results showed no difference between the groups in terms of pain in getting up from a chair, sitting or standing for more than 30 minutes, walking stairs, driving a car, or exercising, or in the need for postoperative analgesics or postoperative sick leave (all P greater than .20).
Dr. Burcharth concluded that a high number of patients reported persistent pain regardless of mesh fixation technique, which emphasizes the need for preoperative information.
Dr. Burcharth reported having no relevant financial disclosures.
Key clinical point:
Major finding: There was no difference between the groups in terms of pain in getting up from a chair, sitting or standing for more than 30 minutes, walking stairs, driving a car, or doing exercise, or in the need for postoperative analgesics or postoperative sick leave (all P greater than .20).
Data source: 1,421 patients who were examined and completed a validated pain questionnaire.
Disclosures: Dr. Burcharth reported having no relevant financial disclosures.
Light and heavy mesh deliver similar outcomes and QOL for lap inguinal repair
WASHINGTON – The weight of mesh used in laparoscopic inguinal hernia repairs was not a significant factor in postoperative outcomes and quality of life, in a large, long-term study.
“There are approximately 700,000 inguinal hernia repairs annually,” said Steve Groene, MD, of the Carolinas Medical Center, Charlotte, N.C. “The goal of our study was to utilize a large sample size of long-term follow-up and compare surgical and quality of life outcomes between light-weight and heavy-weight mesh in laparoscopic inguinal hernia repairs.”
The rates of postoperative complications such as surgical infection, urinary retention, and recurrence in the two groups were similar. Although the LW mesh group had a significantly higher rate of hematoma and seroma, that difference vanished with a multivariate analysis that accounted for confounding factors such as smoking, elective vs. emergent surgery, and surgical technique, Dr. Groene said at the annual clinical congress of the American College of Surgeons.
Quality of life (QOL) was measured with the Carolina Comfort Scale before surgery and at the 2-week, 1-month, 6-month, 12-month, 24-month, and 36-month follow-ups. The investigators looked at pain, movement limitation, and mesh sensation for outcomes and symptoms. There were no other statistically significant differences in QOL between the groups at any of the follow-up time points.
When asked during the discussion about the experience of the investigators in getting patients to continue through a 36-month follow-up, Dr. Groene said that “at 1 month, we were about 60%, [and] at 1 year about 40%; having about 40%-42% of people following up at 1 month is very good.”
Dr. Groene concluded that surgeons should continue to use the type of mesh they feel most comfortable with for laparoscopic inguinal hernia repair and expect to have similar outcomes.
He reported having no relevant financial disclosures.
WASHINGTON – The weight of mesh used in laparoscopic inguinal hernia repairs was not a significant factor in postoperative outcomes and quality of life, in a large, long-term study.
“There are approximately 700,000 inguinal hernia repairs annually,” said Steve Groene, MD, of the Carolinas Medical Center, Charlotte, N.C. “The goal of our study was to utilize a large sample size of long-term follow-up and compare surgical and quality of life outcomes between light-weight and heavy-weight mesh in laparoscopic inguinal hernia repairs.”
The rates of postoperative complications such as surgical infection, urinary retention, and recurrence in the two groups were similar. Although the LW mesh group had a significantly higher rate of hematoma and seroma, that difference vanished with a multivariate analysis that accounted for confounding factors such as smoking, elective vs. emergent surgery, and surgical technique, Dr. Groene said at the annual clinical congress of the American College of Surgeons.
Quality of life (QOL) was measured with the Carolina Comfort Scale before surgery and at the 2-week, 1-month, 6-month, 12-month, 24-month, and 36-month follow-ups. The investigators looked at pain, movement limitation, and mesh sensation for outcomes and symptoms. There were no other statistically significant differences in QOL between the groups at any of the follow-up time points.
When asked during the discussion about the experience of the investigators in getting patients to continue through a 36-month follow-up, Dr. Groene said that “at 1 month, we were about 60%, [and] at 1 year about 40%; having about 40%-42% of people following up at 1 month is very good.”
Dr. Groene concluded that surgeons should continue to use the type of mesh they feel most comfortable with for laparoscopic inguinal hernia repair and expect to have similar outcomes.
He reported having no relevant financial disclosures.
WASHINGTON – The weight of mesh used in laparoscopic inguinal hernia repairs was not a significant factor in postoperative outcomes and quality of life, in a large, long-term study.
“There are approximately 700,000 inguinal hernia repairs annually,” said Steve Groene, MD, of the Carolinas Medical Center, Charlotte, N.C. “The goal of our study was to utilize a large sample size of long-term follow-up and compare surgical and quality of life outcomes between light-weight and heavy-weight mesh in laparoscopic inguinal hernia repairs.”
The rates of postoperative complications such as surgical infection, urinary retention, and recurrence in the two groups were similar. Although the LW mesh group had a significantly higher rate of hematoma and seroma, that difference vanished with a multivariate analysis that accounted for confounding factors such as smoking, elective vs. emergent surgery, and surgical technique, Dr. Groene said at the annual clinical congress of the American College of Surgeons.
Quality of life (QOL) was measured with the Carolina Comfort Scale before surgery and at the 2-week, 1-month, 6-month, 12-month, 24-month, and 36-month follow-ups. The investigators looked at pain, movement limitation, and mesh sensation for outcomes and symptoms. There were no other statistically significant differences in QOL between the groups at any of the follow-up time points.
When asked during the discussion about the experience of the investigators in getting patients to continue through a 36-month follow-up, Dr. Groene said that “at 1 month, we were about 60%, [and] at 1 year about 40%; having about 40%-42% of people following up at 1 month is very good.”
Dr. Groene concluded that surgeons should continue to use the type of mesh they feel most comfortable with for laparoscopic inguinal hernia repair and expect to have similar outcomes.
He reported having no relevant financial disclosures.
FROM ACS CLINICAL CONGRESS
Key clinical point:
Major finding: For laparoscopic inguinal hernia repair, mesh weight was not a significant factor in postoperative complications or quality of life, as measured by the Carolinas Comfort Scale.
Data source: A prospective study of 1,270 laparoscopic inguinal hernia repair patients from a hernia-specific database.
Disclosures: Dr. Groene reported having no relevant financial disclosures.
E. coli resistant to colistin and carbapenems found in U.S. patient
The first strain of Escherichia coli harboring the antibiotic-resistant genes mcr-1 and blaNDM-5 was isolated in the urine of a U.S. patient, according to a report in mBio.
A 76-year-old man was admitted to a tertiary-care hospital in New Jersey with a fever and flank pain in August 2014. The patient emigrated from India and resided in the United States for 1 year prior to this presentation. He had a history of prostate cancer treated with radiation therapy and subsequently developed recurrent urinary tract infections. He had also experienced bladder perforation requiring bilateral placement of nephrostomy tubes, which were clamped 5 days prior to presentation.
Using molecular analysis, the E. coli isolate from the study case (named MCR1_NJ) was shown to carry both mcr-1 and blaNDM-5 genes. In addition to mcr-1 and blaNDM-5, strain MCR1_NJ was found to harbor resistance genes for aminoglycosides, beta-lactams, chloramphenicol, fluoroquinolones, rifampin, sulfonamides, and tetracycline.
“This strain was isolated in August 2014, highlighting an earlier presence of mcr-1 within the region than previously known and raising the likelihood of ongoing undetected transmission,” wrote José R. Mediavilla, MBS, MPH of the New Jersey Medical School, Rutgers University, Newark, N.J., and his coauthors. “Active surveillance efforts involving all polymyxin- and carbapenem-resistant organisms are imperative in order to determine mcr-1 prevalence and prevent further dissemination.”
Find the full study in mBio (doi: 10.1128/mBio.01191-16).
The first strain of Escherichia coli harboring the antibiotic-resistant genes mcr-1 and blaNDM-5 was isolated in the urine of a U.S. patient, according to a report in mBio.
A 76-year-old man was admitted to a tertiary-care hospital in New Jersey with a fever and flank pain in August 2014. The patient emigrated from India and resided in the United States for 1 year prior to this presentation. He had a history of prostate cancer treated with radiation therapy and subsequently developed recurrent urinary tract infections. He had also experienced bladder perforation requiring bilateral placement of nephrostomy tubes, which were clamped 5 days prior to presentation.
Using molecular analysis, the E. coli isolate from the study case (named MCR1_NJ) was shown to carry both mcr-1 and blaNDM-5 genes. In addition to mcr-1 and blaNDM-5, strain MCR1_NJ was found to harbor resistance genes for aminoglycosides, beta-lactams, chloramphenicol, fluoroquinolones, rifampin, sulfonamides, and tetracycline.
“This strain was isolated in August 2014, highlighting an earlier presence of mcr-1 within the region than previously known and raising the likelihood of ongoing undetected transmission,” wrote José R. Mediavilla, MBS, MPH of the New Jersey Medical School, Rutgers University, Newark, N.J., and his coauthors. “Active surveillance efforts involving all polymyxin- and carbapenem-resistant organisms are imperative in order to determine mcr-1 prevalence and prevent further dissemination.”
Find the full study in mBio (doi: 10.1128/mBio.01191-16).
The first strain of Escherichia coli harboring the antibiotic-resistant genes mcr-1 and blaNDM-5 was isolated in the urine of a U.S. patient, according to a report in mBio.
A 76-year-old man was admitted to a tertiary-care hospital in New Jersey with a fever and flank pain in August 2014. The patient emigrated from India and resided in the United States for 1 year prior to this presentation. He had a history of prostate cancer treated with radiation therapy and subsequently developed recurrent urinary tract infections. He had also experienced bladder perforation requiring bilateral placement of nephrostomy tubes, which were clamped 5 days prior to presentation.
Using molecular analysis, the E. coli isolate from the study case (named MCR1_NJ) was shown to carry both mcr-1 and blaNDM-5 genes. In addition to mcr-1 and blaNDM-5, strain MCR1_NJ was found to harbor resistance genes for aminoglycosides, beta-lactams, chloramphenicol, fluoroquinolones, rifampin, sulfonamides, and tetracycline.
“This strain was isolated in August 2014, highlighting an earlier presence of mcr-1 within the region than previously known and raising the likelihood of ongoing undetected transmission,” wrote José R. Mediavilla, MBS, MPH of the New Jersey Medical School, Rutgers University, Newark, N.J., and his coauthors. “Active surveillance efforts involving all polymyxin- and carbapenem-resistant organisms are imperative in order to determine mcr-1 prevalence and prevent further dissemination.”
Find the full study in mBio (doi: 10.1128/mBio.01191-16).
Hypertension in children linked to lower neurocognitive performance
Children with primary hypertension demonstrated significantly lower performance on neurocognitive testing, compared with children without primary hypertension, according to Marc B. Lande, MD, of the University of Rochester (N.Y.), and his associates.
In the study, 75 children with newly diagnosed untreated primary hypertension and 75 normotensive control subjects were examined. Hypertension was linked with worse performances on neurocognitive measures of attention, learning, memory, and fine motor dexterity, compared with the controls. There also was an association between increased disordered sleep and worse executive function. This was more pronounced in children with hypertension than in normotensive children. Hypertension and control groups did not differ significantly in age, sex, maternal education, income, race, ethnicity, obesity, anxiety, depression, cholesterol, glucose, insulin, and C-reactive protein.
“These results suggest that hypertension in youth may have an impact on brain function, and perhaps brain development, in childhood,” the researchers concluded. “Future results from this study will assess the degree to which these effects can be minimized or reversed with antihypertensive therapies.”
Find the full study in the Journal of Pediatrics (2016 Sept 29. doi: 10.1016/j.jpeds.2016.08.076).
Children with primary hypertension demonstrated significantly lower performance on neurocognitive testing, compared with children without primary hypertension, according to Marc B. Lande, MD, of the University of Rochester (N.Y.), and his associates.
In the study, 75 children with newly diagnosed untreated primary hypertension and 75 normotensive control subjects were examined. Hypertension was linked with worse performances on neurocognitive measures of attention, learning, memory, and fine motor dexterity, compared with the controls. There also was an association between increased disordered sleep and worse executive function. This was more pronounced in children with hypertension than in normotensive children. Hypertension and control groups did not differ significantly in age, sex, maternal education, income, race, ethnicity, obesity, anxiety, depression, cholesterol, glucose, insulin, and C-reactive protein.
“These results suggest that hypertension in youth may have an impact on brain function, and perhaps brain development, in childhood,” the researchers concluded. “Future results from this study will assess the degree to which these effects can be minimized or reversed with antihypertensive therapies.”
Find the full study in the Journal of Pediatrics (2016 Sept 29. doi: 10.1016/j.jpeds.2016.08.076).
Children with primary hypertension demonstrated significantly lower performance on neurocognitive testing, compared with children without primary hypertension, according to Marc B. Lande, MD, of the University of Rochester (N.Y.), and his associates.
In the study, 75 children with newly diagnosed untreated primary hypertension and 75 normotensive control subjects were examined. Hypertension was linked with worse performances on neurocognitive measures of attention, learning, memory, and fine motor dexterity, compared with the controls. There also was an association between increased disordered sleep and worse executive function. This was more pronounced in children with hypertension than in normotensive children. Hypertension and control groups did not differ significantly in age, sex, maternal education, income, race, ethnicity, obesity, anxiety, depression, cholesterol, glucose, insulin, and C-reactive protein.
“These results suggest that hypertension in youth may have an impact on brain function, and perhaps brain development, in childhood,” the researchers concluded. “Future results from this study will assess the degree to which these effects can be minimized or reversed with antihypertensive therapies.”
Find the full study in the Journal of Pediatrics (2016 Sept 29. doi: 10.1016/j.jpeds.2016.08.076).
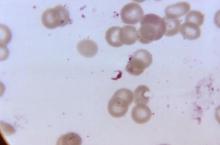
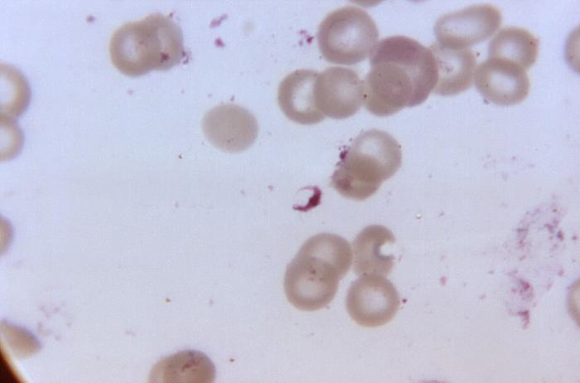
New antimalarial drug proves promising in phase II trial
Recent research suggests the novel antimalarial agent KAF156 is effective without visible safety concerns in adults with uncomplicated Plasmodium vivax or P. falciparum malaria, according to a study published in the New England Journal of Medicine.
From March to August 2013, 21 adults with acute uncomplicated malaria (11 with P. vivax malaria and 10 with P. falciparum malaria) were enrolled in multiple-dose cohorts (400 mg of KAF156 given once daily for 3 days). A third cohort of patients was treated with a single 800-mg dose of KAF156 in order to assess the cure rate at 28 days and the potential for a single-dose cure.
Among the 21 patients with P. falciparum malaria who received the single 800-mg dose and were followed for 28 days, 1 had reinfection and 7 had recrudescent infections (cure rate, 67%). Gametocytemia was detected in two of the patients with P. vivax malaria at baseline and cleared in both patients within 16 hours after receipt of KAF156. In the patients with P. falciparum malaria, one patient had gametocytemia from baseline to 54 hours after receiving the dose and one had intermittent gametocytemia from baseline until 72 hours after dose administration.
The investigators also reported two patients had posttreatment gametocytemia – one had a single positive reading at 24 hours, and the other had positive readings from 12 to 96 hours, at which time sampling finished. Most patients had at least one adverse event, although no grade 4 or serious adverse events were noted. Overall, there were more adverse events after the single 800-mg dose than after multiple 400-mg doses.
“New antimalarial drugs are needed as artemisinin resistance spreads in Southeast Asia and partner-drug resistance follows.” the researchers concluded. “Our study showed that KAF156, a new antimalarial drug, has activity against vivax and falciparum malaria, including artemisinin-resistant parasites.”
Read the full study in the New England Journal of Medicine (2016 Sep. 21. doi: 10.1056/NEJMoa1602250).
Recent research suggests the novel antimalarial agent KAF156 is effective without visible safety concerns in adults with uncomplicated Plasmodium vivax or P. falciparum malaria, according to a study published in the New England Journal of Medicine.
From March to August 2013, 21 adults with acute uncomplicated malaria (11 with P. vivax malaria and 10 with P. falciparum malaria) were enrolled in multiple-dose cohorts (400 mg of KAF156 given once daily for 3 days). A third cohort of patients was treated with a single 800-mg dose of KAF156 in order to assess the cure rate at 28 days and the potential for a single-dose cure.
Among the 21 patients with P. falciparum malaria who received the single 800-mg dose and were followed for 28 days, 1 had reinfection and 7 had recrudescent infections (cure rate, 67%). Gametocytemia was detected in two of the patients with P. vivax malaria at baseline and cleared in both patients within 16 hours after receipt of KAF156. In the patients with P. falciparum malaria, one patient had gametocytemia from baseline to 54 hours after receiving the dose and one had intermittent gametocytemia from baseline until 72 hours after dose administration.
The investigators also reported two patients had posttreatment gametocytemia – one had a single positive reading at 24 hours, and the other had positive readings from 12 to 96 hours, at which time sampling finished. Most patients had at least one adverse event, although no grade 4 or serious adverse events were noted. Overall, there were more adverse events after the single 800-mg dose than after multiple 400-mg doses.
“New antimalarial drugs are needed as artemisinin resistance spreads in Southeast Asia and partner-drug resistance follows.” the researchers concluded. “Our study showed that KAF156, a new antimalarial drug, has activity against vivax and falciparum malaria, including artemisinin-resistant parasites.”
Read the full study in the New England Journal of Medicine (2016 Sep. 21. doi: 10.1056/NEJMoa1602250).
Recent research suggests the novel antimalarial agent KAF156 is effective without visible safety concerns in adults with uncomplicated Plasmodium vivax or P. falciparum malaria, according to a study published in the New England Journal of Medicine.
From March to August 2013, 21 adults with acute uncomplicated malaria (11 with P. vivax malaria and 10 with P. falciparum malaria) were enrolled in multiple-dose cohorts (400 mg of KAF156 given once daily for 3 days). A third cohort of patients was treated with a single 800-mg dose of KAF156 in order to assess the cure rate at 28 days and the potential for a single-dose cure.
Among the 21 patients with P. falciparum malaria who received the single 800-mg dose and were followed for 28 days, 1 had reinfection and 7 had recrudescent infections (cure rate, 67%). Gametocytemia was detected in two of the patients with P. vivax malaria at baseline and cleared in both patients within 16 hours after receipt of KAF156. In the patients with P. falciparum malaria, one patient had gametocytemia from baseline to 54 hours after receiving the dose and one had intermittent gametocytemia from baseline until 72 hours after dose administration.
The investigators also reported two patients had posttreatment gametocytemia – one had a single positive reading at 24 hours, and the other had positive readings from 12 to 96 hours, at which time sampling finished. Most patients had at least one adverse event, although no grade 4 or serious adverse events were noted. Overall, there were more adverse events after the single 800-mg dose than after multiple 400-mg doses.
“New antimalarial drugs are needed as artemisinin resistance spreads in Southeast Asia and partner-drug resistance follows.” the researchers concluded. “Our study showed that KAF156, a new antimalarial drug, has activity against vivax and falciparum malaria, including artemisinin-resistant parasites.”
Read the full study in the New England Journal of Medicine (2016 Sep. 21. doi: 10.1056/NEJMoa1602250).
FDA provides clearance for new colonoscope system
The U.S Food and Drug Administration provided 510(k) clearance for the new Aer-O-Scope colonoscope system, according to GI View of Ramat Gan, Israel.
The Aer-O-Scope is a self-propelled, disposable colonoscope with a 360-degree view of the colon that is controlled with a joystick.
The new system, which is an improvement on the earlier Aer-O-Scope colonoscope, also FDA approved, will have two working channels in order to provide therapeutic access for standard tools to take biopsies or perform polypectomies. It uses a soft multilumen tube designed to significantly reduce pressure on the colon wall, which may increase patient safety. It is also hydrophilic and reduces the friction between bowel and scope by more than 90%. The system has a self-propelled intubation process, created with balloons and low pressure CO2 gas. And, like all colonoscopes, the Aer-O-Scope provides insufflation, irrigation, and suction.
“The new Aer-O-Scope system with therapeutic access has many significant clinical benefits including enabling physicians to more easily, effectively, and efficiently identify and remove polyps and prevent colon cancer,” said GI View CEO Tal Simchony, PhD, in a press release. “We are now working on U.S. market introduction of the Aer-O-Scope. Postmarket studies are also in the plans.”
Colorectal cancer is one of the biggest causes of cancer death worldwide. It can be prevented by early detection and removal of polyps. Read more about Aer-O-Scope on GI View’s website.
The U.S Food and Drug Administration provided 510(k) clearance for the new Aer-O-Scope colonoscope system, according to GI View of Ramat Gan, Israel.
The Aer-O-Scope is a self-propelled, disposable colonoscope with a 360-degree view of the colon that is controlled with a joystick.
The new system, which is an improvement on the earlier Aer-O-Scope colonoscope, also FDA approved, will have two working channels in order to provide therapeutic access for standard tools to take biopsies or perform polypectomies. It uses a soft multilumen tube designed to significantly reduce pressure on the colon wall, which may increase patient safety. It is also hydrophilic and reduces the friction between bowel and scope by more than 90%. The system has a self-propelled intubation process, created with balloons and low pressure CO2 gas. And, like all colonoscopes, the Aer-O-Scope provides insufflation, irrigation, and suction.
“The new Aer-O-Scope system with therapeutic access has many significant clinical benefits including enabling physicians to more easily, effectively, and efficiently identify and remove polyps and prevent colon cancer,” said GI View CEO Tal Simchony, PhD, in a press release. “We are now working on U.S. market introduction of the Aer-O-Scope. Postmarket studies are also in the plans.”
Colorectal cancer is one of the biggest causes of cancer death worldwide. It can be prevented by early detection and removal of polyps. Read more about Aer-O-Scope on GI View’s website.
The U.S Food and Drug Administration provided 510(k) clearance for the new Aer-O-Scope colonoscope system, according to GI View of Ramat Gan, Israel.
The Aer-O-Scope is a self-propelled, disposable colonoscope with a 360-degree view of the colon that is controlled with a joystick.
The new system, which is an improvement on the earlier Aer-O-Scope colonoscope, also FDA approved, will have two working channels in order to provide therapeutic access for standard tools to take biopsies or perform polypectomies. It uses a soft multilumen tube designed to significantly reduce pressure on the colon wall, which may increase patient safety. It is also hydrophilic and reduces the friction between bowel and scope by more than 90%. The system has a self-propelled intubation process, created with balloons and low pressure CO2 gas. And, like all colonoscopes, the Aer-O-Scope provides insufflation, irrigation, and suction.
“The new Aer-O-Scope system with therapeutic access has many significant clinical benefits including enabling physicians to more easily, effectively, and efficiently identify and remove polyps and prevent colon cancer,” said GI View CEO Tal Simchony, PhD, in a press release. “We are now working on U.S. market introduction of the Aer-O-Scope. Postmarket studies are also in the plans.”
Colorectal cancer is one of the biggest causes of cancer death worldwide. It can be prevented by early detection and removal of polyps. Read more about Aer-O-Scope on GI View’s website.
Reduced rotavirus detection after vaccine licensure tied to herd immunity
Rotavirus detection was found to be diminished after rotavirus vaccine licensure, which is consistent with herd immunity, according to Harvey W. Kaufman, MD, and Zhen Chen.
During the 11-year period, 276,949 specimens were submitted for rotavirus antigen detection. In the prevaccine period, the laboratory performed an average of 31,800 tests for rotavirus antigen detection annually, of which 21% were positive. During the postvaccine period, an average of 20,981 annual tests were performed, with only 6% having a positive result, which represents an 82% reduction in the total number of positive results and a 73% reduction in the positivity rate (P less than .001). In the transition period, the positivity rate for rotavirus antigen detection was 14%, which represents a 27% reduction in the positive number and a 32% reduction in the positivity rate, compared with the prevaccine period (P less than .001).
The study noted that the positivity rate during each of the three periods was nearly identical for boys and girls, with 21.1% for boys and 20.9% for girls during the prevaccine period, 9.8% for boys and 9.6% for girls in the transition period, and 4.9% for boys and 4.6% for girls in the postvaccine period.
“The data support the notion of herd immunity in children unlikely to have been vaccinated,” the researchers concluded. “Although the postvaccination period featured alternating years of higher and lower positivity, the peak seasons have a lower positivity rate than in the prevaccination period.”
Find the full study in Pediatrics (2016 Sept. 23. doi: 10.1542/peds.2016-1173).
Rotavirus detection was found to be diminished after rotavirus vaccine licensure, which is consistent with herd immunity, according to Harvey W. Kaufman, MD, and Zhen Chen.
During the 11-year period, 276,949 specimens were submitted for rotavirus antigen detection. In the prevaccine period, the laboratory performed an average of 31,800 tests for rotavirus antigen detection annually, of which 21% were positive. During the postvaccine period, an average of 20,981 annual tests were performed, with only 6% having a positive result, which represents an 82% reduction in the total number of positive results and a 73% reduction in the positivity rate (P less than .001). In the transition period, the positivity rate for rotavirus antigen detection was 14%, which represents a 27% reduction in the positive number and a 32% reduction in the positivity rate, compared with the prevaccine period (P less than .001).
The study noted that the positivity rate during each of the three periods was nearly identical for boys and girls, with 21.1% for boys and 20.9% for girls during the prevaccine period, 9.8% for boys and 9.6% for girls in the transition period, and 4.9% for boys and 4.6% for girls in the postvaccine period.
“The data support the notion of herd immunity in children unlikely to have been vaccinated,” the researchers concluded. “Although the postvaccination period featured alternating years of higher and lower positivity, the peak seasons have a lower positivity rate than in the prevaccination period.”
Find the full study in Pediatrics (2016 Sept. 23. doi: 10.1542/peds.2016-1173).
Rotavirus detection was found to be diminished after rotavirus vaccine licensure, which is consistent with herd immunity, according to Harvey W. Kaufman, MD, and Zhen Chen.
During the 11-year period, 276,949 specimens were submitted for rotavirus antigen detection. In the prevaccine period, the laboratory performed an average of 31,800 tests for rotavirus antigen detection annually, of which 21% were positive. During the postvaccine period, an average of 20,981 annual tests were performed, with only 6% having a positive result, which represents an 82% reduction in the total number of positive results and a 73% reduction in the positivity rate (P less than .001). In the transition period, the positivity rate for rotavirus antigen detection was 14%, which represents a 27% reduction in the positive number and a 32% reduction in the positivity rate, compared with the prevaccine period (P less than .001).
The study noted that the positivity rate during each of the three periods was nearly identical for boys and girls, with 21.1% for boys and 20.9% for girls during the prevaccine period, 9.8% for boys and 9.6% for girls in the transition period, and 4.9% for boys and 4.6% for girls in the postvaccine period.
“The data support the notion of herd immunity in children unlikely to have been vaccinated,” the researchers concluded. “Although the postvaccination period featured alternating years of higher and lower positivity, the peak seasons have a lower positivity rate than in the prevaccination period.”
Find the full study in Pediatrics (2016 Sept. 23. doi: 10.1542/peds.2016-1173).
FROM PEDIATRICS
FDA approves first-line combo therapy for type 2 diabetes
The Food and Drug Administration approved an extended-release combination of canagliflozin and metformin for first-line use as an adjunct to diet and exercise to improve blood glucose control in adults with type 2 diabetes, according to Janssen Pharmaceuticals.
Once-daily Invokamet XR combines canagliflozin (Invokana) and an extended-release formulation of metformin. Studies in healthy adults have shown that Invokamet XR results in the same levels of canagliflozin and metformin in the body as when corresponding dosages of the two medicines are administered as separate tablets.
Phase III studies showed that using canagliflozin and metformin lowered blood sugar and, in prespecified secondary endpoints, was linked to greater reductions in body weight and systolic blood pressure.
Invokamet XR is available with 50 mg or 150 mg of canagliflozin, and 500 mg or 1,000 mg of extended-release metformin. Invokamet XR contains a boxed warning regarding the risk of lactic acidosis.
Read the full company statement here.
The Food and Drug Administration approved an extended-release combination of canagliflozin and metformin for first-line use as an adjunct to diet and exercise to improve blood glucose control in adults with type 2 diabetes, according to Janssen Pharmaceuticals.
Once-daily Invokamet XR combines canagliflozin (Invokana) and an extended-release formulation of metformin. Studies in healthy adults have shown that Invokamet XR results in the same levels of canagliflozin and metformin in the body as when corresponding dosages of the two medicines are administered as separate tablets.
Phase III studies showed that using canagliflozin and metformin lowered blood sugar and, in prespecified secondary endpoints, was linked to greater reductions in body weight and systolic blood pressure.
Invokamet XR is available with 50 mg or 150 mg of canagliflozin, and 500 mg or 1,000 mg of extended-release metformin. Invokamet XR contains a boxed warning regarding the risk of lactic acidosis.
Read the full company statement here.
The Food and Drug Administration approved an extended-release combination of canagliflozin and metformin for first-line use as an adjunct to diet and exercise to improve blood glucose control in adults with type 2 diabetes, according to Janssen Pharmaceuticals.
Once-daily Invokamet XR combines canagliflozin (Invokana) and an extended-release formulation of metformin. Studies in healthy adults have shown that Invokamet XR results in the same levels of canagliflozin and metformin in the body as when corresponding dosages of the two medicines are administered as separate tablets.
Phase III studies showed that using canagliflozin and metformin lowered blood sugar and, in prespecified secondary endpoints, was linked to greater reductions in body weight and systolic blood pressure.
Invokamet XR is available with 50 mg or 150 mg of canagliflozin, and 500 mg or 1,000 mg of extended-release metformin. Invokamet XR contains a boxed warning regarding the risk of lactic acidosis.
Read the full company statement here.