User login
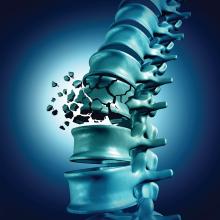
Multiple myeloma treatment produces a similar survival benefit in very elderly patients
More than a third of patients diagnosed with multiple myeloma (MM) are over the age of 80, and yet most treatment successes have been reported in younger patients. However, patients over the age of 80 years received similar benefits as younger patients from MM treatment, according to a study reported online in the Journal of Geriatric Oncology.
Researchers identified 2,155 patients diagnosed with MM at age 80 years or older in the Surveillance, Epidemiology, and End Results Program (SEER)–Medicare database from 2007 to 2013. A cohort of 2,933 similar patients diagnosed with myeloma at age 70-79 was used for comparison.
The researcher found that the number of patients receiving treatment for myeloma within 6 months of diagnosis was significantly lower in the 80 years and older group, compared with the 70-79 years group. Only 51% of patients in the 80 years and older cohort received systemic treatment within 6 months following diagnosis, compared with 71% of patients in the 70-79 years cohort received systemic treatment in the same timeframe (P < .001)
The analysis showed that treatment was associated with an overall 26% decrease in hazard for death, independent of age, race, gender, poverty, comorbidities, and proxy measures of performance status. There was no statistically significant difference in treatment benefit based on age cohort (P = .610).
The median overall survival for patients diagnosed at age 80 years or older was 13.4 months, with those patients receiving systemic treatment having a median overall survival of 21.4 months, compared with 6.4 months for those not receiving treatment. In comparison, patients between ages 70 and 79 years had a median overall survival of 30.1 months with treatment.
The population over 80, when myeloma incidence peaks, is projected to triple over the next few decades, according to the researchers. “Antimyeloma treatment in the era of novel therapies seems to have a similar improvement on survival for the oldest-old, those beyond 80 years, as other patients. With growing knowledge of and experience with novel agents in older patients with myeloma, treatment rates have increased, which have in turn improved survival,” they concluded.
The study was funded by the National Cancer Institute. One author reported research funding from Janssen. The other authors had no relevant conflicts of interest.
SOURCE: Fiala MA et al. J Geriatric Oncol. 2020 Mar 10. doi.org/10.1016/j.jgo.2020.03.005.
More than a third of patients diagnosed with multiple myeloma (MM) are over the age of 80, and yet most treatment successes have been reported in younger patients. However, patients over the age of 80 years received similar benefits as younger patients from MM treatment, according to a study reported online in the Journal of Geriatric Oncology.
Researchers identified 2,155 patients diagnosed with MM at age 80 years or older in the Surveillance, Epidemiology, and End Results Program (SEER)–Medicare database from 2007 to 2013. A cohort of 2,933 similar patients diagnosed with myeloma at age 70-79 was used for comparison.
The researcher found that the number of patients receiving treatment for myeloma within 6 months of diagnosis was significantly lower in the 80 years and older group, compared with the 70-79 years group. Only 51% of patients in the 80 years and older cohort received systemic treatment within 6 months following diagnosis, compared with 71% of patients in the 70-79 years cohort received systemic treatment in the same timeframe (P < .001)
The analysis showed that treatment was associated with an overall 26% decrease in hazard for death, independent of age, race, gender, poverty, comorbidities, and proxy measures of performance status. There was no statistically significant difference in treatment benefit based on age cohort (P = .610).
The median overall survival for patients diagnosed at age 80 years or older was 13.4 months, with those patients receiving systemic treatment having a median overall survival of 21.4 months, compared with 6.4 months for those not receiving treatment. In comparison, patients between ages 70 and 79 years had a median overall survival of 30.1 months with treatment.
The population over 80, when myeloma incidence peaks, is projected to triple over the next few decades, according to the researchers. “Antimyeloma treatment in the era of novel therapies seems to have a similar improvement on survival for the oldest-old, those beyond 80 years, as other patients. With growing knowledge of and experience with novel agents in older patients with myeloma, treatment rates have increased, which have in turn improved survival,” they concluded.
The study was funded by the National Cancer Institute. One author reported research funding from Janssen. The other authors had no relevant conflicts of interest.
SOURCE: Fiala MA et al. J Geriatric Oncol. 2020 Mar 10. doi.org/10.1016/j.jgo.2020.03.005.
More than a third of patients diagnosed with multiple myeloma (MM) are over the age of 80, and yet most treatment successes have been reported in younger patients. However, patients over the age of 80 years received similar benefits as younger patients from MM treatment, according to a study reported online in the Journal of Geriatric Oncology.
Researchers identified 2,155 patients diagnosed with MM at age 80 years or older in the Surveillance, Epidemiology, and End Results Program (SEER)–Medicare database from 2007 to 2013. A cohort of 2,933 similar patients diagnosed with myeloma at age 70-79 was used for comparison.
The researcher found that the number of patients receiving treatment for myeloma within 6 months of diagnosis was significantly lower in the 80 years and older group, compared with the 70-79 years group. Only 51% of patients in the 80 years and older cohort received systemic treatment within 6 months following diagnosis, compared with 71% of patients in the 70-79 years cohort received systemic treatment in the same timeframe (P < .001)
The analysis showed that treatment was associated with an overall 26% decrease in hazard for death, independent of age, race, gender, poverty, comorbidities, and proxy measures of performance status. There was no statistically significant difference in treatment benefit based on age cohort (P = .610).
The median overall survival for patients diagnosed at age 80 years or older was 13.4 months, with those patients receiving systemic treatment having a median overall survival of 21.4 months, compared with 6.4 months for those not receiving treatment. In comparison, patients between ages 70 and 79 years had a median overall survival of 30.1 months with treatment.
The population over 80, when myeloma incidence peaks, is projected to triple over the next few decades, according to the researchers. “Antimyeloma treatment in the era of novel therapies seems to have a similar improvement on survival for the oldest-old, those beyond 80 years, as other patients. With growing knowledge of and experience with novel agents in older patients with myeloma, treatment rates have increased, which have in turn improved survival,” they concluded.
The study was funded by the National Cancer Institute. One author reported research funding from Janssen. The other authors had no relevant conflicts of interest.
SOURCE: Fiala MA et al. J Geriatric Oncol. 2020 Mar 10. doi.org/10.1016/j.jgo.2020.03.005.
FROM THE JOURNAL OF GERIATRIC ONCOLOGY
CLL and breast cancer differ in the expression of regulatory microRNAs
Expression of three microRNAs (miR-155, miR-29a, and miR-27b) was detectable in patients with chronic lymphocytic leukemia (CLL) and in breast cancer (BC) patients, but not in healthy subjects, according to a molecular analysis of patients reported in Molecular Therapy Oncolytics. In addition, circulating microarrays were found to be able to differentiate between both CLL and BC patients and healthy subjects.
The researchers obtained blood samples from 15 CLL patients and tissue samples from 15 BC patients, all from a single center.
The use of quantitative reverse transcription polymerase chain reaction (qRT-PCR) demonstrated a significant increase in the expression of all three miRNAs in patients with BC and CLL, compared with respective healthy groups (P less than .001).
In BC patients, there was a significant difference between the expression of miR-155 and miR-29a (P less than .05), miR-155 and miR-27b (P less than .01), and miR-27b and miR-29a (P less than .001). In CLL patients, the qRT-PCR results showed a significant difference between expression of both miR-27b and miR-29a, compared with expression of miR-155 (P less than .001). In addition, there was a significant association between miR-155 and prevascular invasion (P = .013), but no significant association with other clinical variables (age, tumor grade, nuclear grade, tumor stage, tumor size, area of invasive component, tumor side, margin, or preneural invasion), according to the researchers.
Results also showed that elevated circulating miRNAs were BC specific and could differentiate BC tissues from the controls, and comparing expression of miRNAs between BC and CLL patients, there was also a significant difference for all miRNAs (P less than .001) between them.
“Our results suggest that miR-27b, miR-29a, and miR-155 could be potential new biomarkers for diagnosis, as well as a therapeutic target for CLL and BC,” the researchers concluded.
The authors reported that they had no competing interests.
SOURCE: Raeisi F et al. Mol Ther Oncolytics. 2020;16:230-7.
Expression of three microRNAs (miR-155, miR-29a, and miR-27b) was detectable in patients with chronic lymphocytic leukemia (CLL) and in breast cancer (BC) patients, but not in healthy subjects, according to a molecular analysis of patients reported in Molecular Therapy Oncolytics. In addition, circulating microarrays were found to be able to differentiate between both CLL and BC patients and healthy subjects.
The researchers obtained blood samples from 15 CLL patients and tissue samples from 15 BC patients, all from a single center.
The use of quantitative reverse transcription polymerase chain reaction (qRT-PCR) demonstrated a significant increase in the expression of all three miRNAs in patients with BC and CLL, compared with respective healthy groups (P less than .001).
In BC patients, there was a significant difference between the expression of miR-155 and miR-29a (P less than .05), miR-155 and miR-27b (P less than .01), and miR-27b and miR-29a (P less than .001). In CLL patients, the qRT-PCR results showed a significant difference between expression of both miR-27b and miR-29a, compared with expression of miR-155 (P less than .001). In addition, there was a significant association between miR-155 and prevascular invasion (P = .013), but no significant association with other clinical variables (age, tumor grade, nuclear grade, tumor stage, tumor size, area of invasive component, tumor side, margin, or preneural invasion), according to the researchers.
Results also showed that elevated circulating miRNAs were BC specific and could differentiate BC tissues from the controls, and comparing expression of miRNAs between BC and CLL patients, there was also a significant difference for all miRNAs (P less than .001) between them.
“Our results suggest that miR-27b, miR-29a, and miR-155 could be potential new biomarkers for diagnosis, as well as a therapeutic target for CLL and BC,” the researchers concluded.
The authors reported that they had no competing interests.
SOURCE: Raeisi F et al. Mol Ther Oncolytics. 2020;16:230-7.
Expression of three microRNAs (miR-155, miR-29a, and miR-27b) was detectable in patients with chronic lymphocytic leukemia (CLL) and in breast cancer (BC) patients, but not in healthy subjects, according to a molecular analysis of patients reported in Molecular Therapy Oncolytics. In addition, circulating microarrays were found to be able to differentiate between both CLL and BC patients and healthy subjects.
The researchers obtained blood samples from 15 CLL patients and tissue samples from 15 BC patients, all from a single center.
The use of quantitative reverse transcription polymerase chain reaction (qRT-PCR) demonstrated a significant increase in the expression of all three miRNAs in patients with BC and CLL, compared with respective healthy groups (P less than .001).
In BC patients, there was a significant difference between the expression of miR-155 and miR-29a (P less than .05), miR-155 and miR-27b (P less than .01), and miR-27b and miR-29a (P less than .001). In CLL patients, the qRT-PCR results showed a significant difference between expression of both miR-27b and miR-29a, compared with expression of miR-155 (P less than .001). In addition, there was a significant association between miR-155 and prevascular invasion (P = .013), but no significant association with other clinical variables (age, tumor grade, nuclear grade, tumor stage, tumor size, area of invasive component, tumor side, margin, or preneural invasion), according to the researchers.
Results also showed that elevated circulating miRNAs were BC specific and could differentiate BC tissues from the controls, and comparing expression of miRNAs between BC and CLL patients, there was also a significant difference for all miRNAs (P less than .001) between them.
“Our results suggest that miR-27b, miR-29a, and miR-155 could be potential new biomarkers for diagnosis, as well as a therapeutic target for CLL and BC,” the researchers concluded.
The authors reported that they had no competing interests.
SOURCE: Raeisi F et al. Mol Ther Oncolytics. 2020;16:230-7.
FROM MOLECULAR THERAPY ONCOLYTICS
Webinar confronts unique issues for the bleeding disorders community facing COVID-19
In a webinar conducted on March 20, Leonard Valentino, MD, president and CEO of the National Hemophilia Foundation (NHF), provided
Overall, the risk of comorbidities is no different in the bleeding disorders population than in the general population, and similar precautions should be maintained, Dr. Valentino stated. He listed some of the at-risk populations as designated by the Centers for Disease Control and Prevention.
In particular, he pointed out that, when the CDC referred to a greater risk of COVID-19 to individuals with bleeding disorders, the organization was referring to patients with HIV and sickle cell disease. The CDC was not referring to patients with other forms of bleeding disorders, such as hemophilia, Dr. Valentino stated.
All individuals should be following CDC and state and federal recommendations with regard to social distancing and hygiene. However, with regard to immunocompromised individuals, “the two populations we [in the bleeding disorders community] have to be concerned about are those in gene therapy clinical trials and those with inhibitors,” said Dr. Valentino.
Patients in a gene therapy clinical trial should exercise additional precautions because the use of steroids, common in these trials. “Steroids are an immunosuppressive drug, and this would increase one’s risk of infection, including COVID-19,” according to Dr. Valentino.
In addition, “I will say, if you have hemophilia and an inhibitor [an antibody to clotting factor treatment], that may alter the immune system, and we don’t know what the implication of that is in terms of coronavirus infection and COVID-19 disease. So people with an inhibitor should take special precautions to limit their exposures.”
Patients with a port should not need to have extra concerns regarding COVID-19, but they should continue to exercise the good hygiene that has always been essential, according to Dr. Valentino.
Dr. Valentino asked: Are patients with a bleeding disorder who become infected with COVID-19 more susceptible to a bleed? “You shouldn’t be more susceptible to bleeding except if you have severe cough, and that cough could result in bleeding to the head,” he answered.
If a patient needs to go to the emergency department for a bleed or possible COVID-19 infection, they should wear a face mask if they are sick to prevent spreading of disease. “This is really the only instance where a face mask may be beneficial” in that it limits other people’s exposure to your infection. It is especially important to call ahead before visiting the doctor or going to the emergency department. “Make sure that they’re aware that you’re coming.”
Of particular concern to patients is the amount of factor product they should have on hand. The current CDC recommendation is a 30-day supply of medicines, but that is misleading, because it refers to general medications, such as high-blood pressure medicine, and not factor products. “The current MASAC [NHF’s Medical and Scientific Advisory Council] recommendation is to have a 14-day supply of factor products available to you,” said Dr. Valentino, “and one should reorder when you have a 1-week supply.”
MASAC has issued a letter on the crisis on the NHF website.
These recommendations should not be exceeded in order to ensure that there is enough factor available to all patients, he added. Hoarding is discouraged, and there are no concerns as yet of factor running out. “We have had conversations with manufacturers and … the supply chain is robust.” The greater concern is with regard to ancillary supplies in the hospital that a hemophilia patient may require during treatment.
Patients and practitioners should consult the COVID-19 pages of both the NHF and Hemophilia Federation of America (HFA) websites. This includes a Health and Wellness update by Dr. Valentino.
With regard to financial issues, he and Sharon Meyers, CEO and president of the HFA, spoke, stating that both NHF and HFA have advocacy for patients seeking to deal with insurance issues or in paying for their products, urging people to go to the organizational websites and to also use their emails: [email protected] and [email protected].
She also announced that the annual meeting of the HFA was being postponed to Aug. 24-26 at the Hilton Inner Harbor Baltimore, Md.
Dr. Valentino and Ms. Meyers did not provide any disclosure information.
In a webinar conducted on March 20, Leonard Valentino, MD, president and CEO of the National Hemophilia Foundation (NHF), provided
Overall, the risk of comorbidities is no different in the bleeding disorders population than in the general population, and similar precautions should be maintained, Dr. Valentino stated. He listed some of the at-risk populations as designated by the Centers for Disease Control and Prevention.
In particular, he pointed out that, when the CDC referred to a greater risk of COVID-19 to individuals with bleeding disorders, the organization was referring to patients with HIV and sickle cell disease. The CDC was not referring to patients with other forms of bleeding disorders, such as hemophilia, Dr. Valentino stated.
All individuals should be following CDC and state and federal recommendations with regard to social distancing and hygiene. However, with regard to immunocompromised individuals, “the two populations we [in the bleeding disorders community] have to be concerned about are those in gene therapy clinical trials and those with inhibitors,” said Dr. Valentino.
Patients in a gene therapy clinical trial should exercise additional precautions because the use of steroids, common in these trials. “Steroids are an immunosuppressive drug, and this would increase one’s risk of infection, including COVID-19,” according to Dr. Valentino.
In addition, “I will say, if you have hemophilia and an inhibitor [an antibody to clotting factor treatment], that may alter the immune system, and we don’t know what the implication of that is in terms of coronavirus infection and COVID-19 disease. So people with an inhibitor should take special precautions to limit their exposures.”
Patients with a port should not need to have extra concerns regarding COVID-19, but they should continue to exercise the good hygiene that has always been essential, according to Dr. Valentino.
Dr. Valentino asked: Are patients with a bleeding disorder who become infected with COVID-19 more susceptible to a bleed? “You shouldn’t be more susceptible to bleeding except if you have severe cough, and that cough could result in bleeding to the head,” he answered.
If a patient needs to go to the emergency department for a bleed or possible COVID-19 infection, they should wear a face mask if they are sick to prevent spreading of disease. “This is really the only instance where a face mask may be beneficial” in that it limits other people’s exposure to your infection. It is especially important to call ahead before visiting the doctor or going to the emergency department. “Make sure that they’re aware that you’re coming.”
Of particular concern to patients is the amount of factor product they should have on hand. The current CDC recommendation is a 30-day supply of medicines, but that is misleading, because it refers to general medications, such as high-blood pressure medicine, and not factor products. “The current MASAC [NHF’s Medical and Scientific Advisory Council] recommendation is to have a 14-day supply of factor products available to you,” said Dr. Valentino, “and one should reorder when you have a 1-week supply.”
MASAC has issued a letter on the crisis on the NHF website.
These recommendations should not be exceeded in order to ensure that there is enough factor available to all patients, he added. Hoarding is discouraged, and there are no concerns as yet of factor running out. “We have had conversations with manufacturers and … the supply chain is robust.” The greater concern is with regard to ancillary supplies in the hospital that a hemophilia patient may require during treatment.
Patients and practitioners should consult the COVID-19 pages of both the NHF and Hemophilia Federation of America (HFA) websites. This includes a Health and Wellness update by Dr. Valentino.
With regard to financial issues, he and Sharon Meyers, CEO and president of the HFA, spoke, stating that both NHF and HFA have advocacy for patients seeking to deal with insurance issues or in paying for their products, urging people to go to the organizational websites and to also use their emails: [email protected] and [email protected].
She also announced that the annual meeting of the HFA was being postponed to Aug. 24-26 at the Hilton Inner Harbor Baltimore, Md.
Dr. Valentino and Ms. Meyers did not provide any disclosure information.
In a webinar conducted on March 20, Leonard Valentino, MD, president and CEO of the National Hemophilia Foundation (NHF), provided
Overall, the risk of comorbidities is no different in the bleeding disorders population than in the general population, and similar precautions should be maintained, Dr. Valentino stated. He listed some of the at-risk populations as designated by the Centers for Disease Control and Prevention.
In particular, he pointed out that, when the CDC referred to a greater risk of COVID-19 to individuals with bleeding disorders, the organization was referring to patients with HIV and sickle cell disease. The CDC was not referring to patients with other forms of bleeding disorders, such as hemophilia, Dr. Valentino stated.
All individuals should be following CDC and state and federal recommendations with regard to social distancing and hygiene. However, with regard to immunocompromised individuals, “the two populations we [in the bleeding disorders community] have to be concerned about are those in gene therapy clinical trials and those with inhibitors,” said Dr. Valentino.
Patients in a gene therapy clinical trial should exercise additional precautions because the use of steroids, common in these trials. “Steroids are an immunosuppressive drug, and this would increase one’s risk of infection, including COVID-19,” according to Dr. Valentino.
In addition, “I will say, if you have hemophilia and an inhibitor [an antibody to clotting factor treatment], that may alter the immune system, and we don’t know what the implication of that is in terms of coronavirus infection and COVID-19 disease. So people with an inhibitor should take special precautions to limit their exposures.”
Patients with a port should not need to have extra concerns regarding COVID-19, but they should continue to exercise the good hygiene that has always been essential, according to Dr. Valentino.
Dr. Valentino asked: Are patients with a bleeding disorder who become infected with COVID-19 more susceptible to a bleed? “You shouldn’t be more susceptible to bleeding except if you have severe cough, and that cough could result in bleeding to the head,” he answered.
If a patient needs to go to the emergency department for a bleed or possible COVID-19 infection, they should wear a face mask if they are sick to prevent spreading of disease. “This is really the only instance where a face mask may be beneficial” in that it limits other people’s exposure to your infection. It is especially important to call ahead before visiting the doctor or going to the emergency department. “Make sure that they’re aware that you’re coming.”
Of particular concern to patients is the amount of factor product they should have on hand. The current CDC recommendation is a 30-day supply of medicines, but that is misleading, because it refers to general medications, such as high-blood pressure medicine, and not factor products. “The current MASAC [NHF’s Medical and Scientific Advisory Council] recommendation is to have a 14-day supply of factor products available to you,” said Dr. Valentino, “and one should reorder when you have a 1-week supply.”
MASAC has issued a letter on the crisis on the NHF website.
These recommendations should not be exceeded in order to ensure that there is enough factor available to all patients, he added. Hoarding is discouraged, and there are no concerns as yet of factor running out. “We have had conversations with manufacturers and … the supply chain is robust.” The greater concern is with regard to ancillary supplies in the hospital that a hemophilia patient may require during treatment.
Patients and practitioners should consult the COVID-19 pages of both the NHF and Hemophilia Federation of America (HFA) websites. This includes a Health and Wellness update by Dr. Valentino.
With regard to financial issues, he and Sharon Meyers, CEO and president of the HFA, spoke, stating that both NHF and HFA have advocacy for patients seeking to deal with insurance issues or in paying for their products, urging people to go to the organizational websites and to also use their emails: [email protected] and [email protected].
She also announced that the annual meeting of the HFA was being postponed to Aug. 24-26 at the Hilton Inner Harbor Baltimore, Md.
Dr. Valentino and Ms. Meyers did not provide any disclosure information.
AGA and colleague societies issue clinical insights for COVID-19
Amid the growing SARS-CoV-2 pandemic, currently in its expansive growth phase in the United States, the American Gastroenterological Association (AGA), the American Association for the Study of Liver Diseases (AASLD), the American College of Gastroenterology (ACG), and the American Society for Gastrointestinal Endoscopy (ASGE) have jointly released “COVID-19 Clinical Insights for Our Community of Gastroenterologists and Gastroenterology Care Providers,” which can be found on the websites of the various societies.
“The purpose of this communication is to jointly provide you with up to date COVID-19 information in order to maintain the highest level of health and safety for our patients, staff, community, and ourselves,” according to the AGA website announcement.
In particular, the societies point out that there is recent evidence suggesting the potential for coronavirus transmission through droplets and perhaps fecal shedding, which pose potential risks in particular during endoscopy and colonoscopy procedures to other patients, endoscopy personnel, and practitioners.
Relevant clinical factors related to COVID-19 are discussed, including the fact that asymptomatic spread can occur during the prodromal phase (the mean incubation period is approximately 5 days, with a range of 0-14 days), with viral shedding greatest when symptoms begin.
Between 20% and 30% of patients with COVID-19 infection show abnormal liver enzymes. In addition, COVID-19 patients show drops in their leukocyte counts, and elevated white blood cell counts is a poor prognostic sign, according to the release.
The Centers for Disease Control and Prevention lists vulnerable populations at the greatest risk for more serious outcomes; these include the elderly and those with severe chronic health conditions, such as heart disease, lung disease, diabetes, decompensated cirrhosis, HIV with low CD4 counts, and immunosuppression (including liver and other solid organ transplant recipients), are at higher risk of developing more serious illness. In addition pregnancy may provide added risk.
Specific advice for the gastroenterology profession
The joint statement urges that practitioners strongly consider rescheduling elective nonurgent endoscopic procedures, although some nonurgent procedures are higher priority and may need to be performed, including cancer evaluations, prosthetic removals, and evaluation of significant symptoms. “Of note, the Surgeon General on 3/14/20 advised hospitals to postpone all elective surgeries,” the document states.
Patient concerns
In all cases, patients should be prescreened for high-risk exposure or symptoms. This includes asking about history of fever or respiratory symptoms, family members or close contacts with similar symptoms, any contact with a confirmed case of COVID-19, and recent travel to a high-risk area. “Avoid bringing patients (or their escorts) into the medical facility who are over age 65 or have one of the CDC recognized risks listed above,” the societies advise.
Check body temperature of the patient upon arrival at endoscopy unit or clinic, and keep all patients at an appropriate distance from each other (6 feet is recommended) throughout the entire time in the endoscopy unit.
“For COVID-19 positive patients, or those awaiting test results, isolation precautions should be taken with procedures performed in negative pressure rooms,” according to the statement.
In addition, use telemedicine where possible in elective cases, and consider phone follow-up after any procedures at 7 and 14 days to ask about new diagnosis of COVID-19 or development of its symptoms, .
Those patients who are on immunosuppressive drugs for inflammatory bowel disease and autoimmune hepatitis should continue taking their medications because the risk of disease flare outweighs the chance of contracting coronavirus, according to the document. In addition, these patients should be advised to follow CDC guidelines for at-risk groups by avoiding crowds and limiting travel.
Protection of practitioners
Key factors in ensuring practitioner safety and maintaining practice functionality are discussed by the joint document. In particular, appropriate personal protective equipment (PPE) should be worn by all members of the endoscopy team: gloves, mask, eye shield/goggles, face shields, and gown, but practitioners should also be aware of how to put on and take off PPE appropriately.
“Conservation of PPE is critical. Only essential personnel should be present in cases. Consider extended use or reuse of surgical masks and eye protection in accordance with hospital policies,” the document recommends.
“It is important to address our collective staff needs and institute policies that protect our workforce.” To that end, the document recommends that centers should strategically assign available personnel in order to minimize concomitant exposure of those with similar or unique skill sets. This includes the use of nonphysician practitioners and fellows that cannot participate in cases for screening and triaging patients, or performing virtual visits.
Coming at a time of pandemic, when gastrointestinal symptoms have been recognized as a more common symptom of COVID-19 than previously expected and liver damage has been noted as a potential repercussion of SARS-CoV-2 infection, these clinical insights provide a template for gastroenterologists and related professionals for dealing with their patients and keeping themselves safe under dramatically changed circumstances.
The partnered organizations, AASLD, ACG, AGA, and ASGE, are committed to providing updated COVID-19 information as appropriate. However: “Given the evolving and fluid nature of the situation, institutions, hospitals and clinics have also been formulating their own local guidelines, so we urge you to follow the evolving CDC recommendations and your local requirements,” according to the AGA website announcement.
In addition to the joint communication, the society websites each offer additional COVID-19 information. The AGA practice updates on the COVID-19 webpage provides information about announcements, such as the cancellation of Digestive Disease Week® in May, a location for AGA members to discuss their COVID-19 experiences and share advice, and links to the CDC COVID-19 updates.
SOURCE: American Gastroenterological Association et al. March 2020, COVID-19 Clinical Insights for Our Community of Gastroenterologists and Gastroenterology Care Providers.
Amid the growing SARS-CoV-2 pandemic, currently in its expansive growth phase in the United States, the American Gastroenterological Association (AGA), the American Association for the Study of Liver Diseases (AASLD), the American College of Gastroenterology (ACG), and the American Society for Gastrointestinal Endoscopy (ASGE) have jointly released “COVID-19 Clinical Insights for Our Community of Gastroenterologists and Gastroenterology Care Providers,” which can be found on the websites of the various societies.
“The purpose of this communication is to jointly provide you with up to date COVID-19 information in order to maintain the highest level of health and safety for our patients, staff, community, and ourselves,” according to the AGA website announcement.
In particular, the societies point out that there is recent evidence suggesting the potential for coronavirus transmission through droplets and perhaps fecal shedding, which pose potential risks in particular during endoscopy and colonoscopy procedures to other patients, endoscopy personnel, and practitioners.
Relevant clinical factors related to COVID-19 are discussed, including the fact that asymptomatic spread can occur during the prodromal phase (the mean incubation period is approximately 5 days, with a range of 0-14 days), with viral shedding greatest when symptoms begin.
Between 20% and 30% of patients with COVID-19 infection show abnormal liver enzymes. In addition, COVID-19 patients show drops in their leukocyte counts, and elevated white blood cell counts is a poor prognostic sign, according to the release.
The Centers for Disease Control and Prevention lists vulnerable populations at the greatest risk for more serious outcomes; these include the elderly and those with severe chronic health conditions, such as heart disease, lung disease, diabetes, decompensated cirrhosis, HIV with low CD4 counts, and immunosuppression (including liver and other solid organ transplant recipients), are at higher risk of developing more serious illness. In addition pregnancy may provide added risk.
Specific advice for the gastroenterology profession
The joint statement urges that practitioners strongly consider rescheduling elective nonurgent endoscopic procedures, although some nonurgent procedures are higher priority and may need to be performed, including cancer evaluations, prosthetic removals, and evaluation of significant symptoms. “Of note, the Surgeon General on 3/14/20 advised hospitals to postpone all elective surgeries,” the document states.
Patient concerns
In all cases, patients should be prescreened for high-risk exposure or symptoms. This includes asking about history of fever or respiratory symptoms, family members or close contacts with similar symptoms, any contact with a confirmed case of COVID-19, and recent travel to a high-risk area. “Avoid bringing patients (or their escorts) into the medical facility who are over age 65 or have one of the CDC recognized risks listed above,” the societies advise.
Check body temperature of the patient upon arrival at endoscopy unit or clinic, and keep all patients at an appropriate distance from each other (6 feet is recommended) throughout the entire time in the endoscopy unit.
“For COVID-19 positive patients, or those awaiting test results, isolation precautions should be taken with procedures performed in negative pressure rooms,” according to the statement.
In addition, use telemedicine where possible in elective cases, and consider phone follow-up after any procedures at 7 and 14 days to ask about new diagnosis of COVID-19 or development of its symptoms, .
Those patients who are on immunosuppressive drugs for inflammatory bowel disease and autoimmune hepatitis should continue taking their medications because the risk of disease flare outweighs the chance of contracting coronavirus, according to the document. In addition, these patients should be advised to follow CDC guidelines for at-risk groups by avoiding crowds and limiting travel.
Protection of practitioners
Key factors in ensuring practitioner safety and maintaining practice functionality are discussed by the joint document. In particular, appropriate personal protective equipment (PPE) should be worn by all members of the endoscopy team: gloves, mask, eye shield/goggles, face shields, and gown, but practitioners should also be aware of how to put on and take off PPE appropriately.
“Conservation of PPE is critical. Only essential personnel should be present in cases. Consider extended use or reuse of surgical masks and eye protection in accordance with hospital policies,” the document recommends.
“It is important to address our collective staff needs and institute policies that protect our workforce.” To that end, the document recommends that centers should strategically assign available personnel in order to minimize concomitant exposure of those with similar or unique skill sets. This includes the use of nonphysician practitioners and fellows that cannot participate in cases for screening and triaging patients, or performing virtual visits.
Coming at a time of pandemic, when gastrointestinal symptoms have been recognized as a more common symptom of COVID-19 than previously expected and liver damage has been noted as a potential repercussion of SARS-CoV-2 infection, these clinical insights provide a template for gastroenterologists and related professionals for dealing with their patients and keeping themselves safe under dramatically changed circumstances.
The partnered organizations, AASLD, ACG, AGA, and ASGE, are committed to providing updated COVID-19 information as appropriate. However: “Given the evolving and fluid nature of the situation, institutions, hospitals and clinics have also been formulating their own local guidelines, so we urge you to follow the evolving CDC recommendations and your local requirements,” according to the AGA website announcement.
In addition to the joint communication, the society websites each offer additional COVID-19 information. The AGA practice updates on the COVID-19 webpage provides information about announcements, such as the cancellation of Digestive Disease Week® in May, a location for AGA members to discuss their COVID-19 experiences and share advice, and links to the CDC COVID-19 updates.
SOURCE: American Gastroenterological Association et al. March 2020, COVID-19 Clinical Insights for Our Community of Gastroenterologists and Gastroenterology Care Providers.
Amid the growing SARS-CoV-2 pandemic, currently in its expansive growth phase in the United States, the American Gastroenterological Association (AGA), the American Association for the Study of Liver Diseases (AASLD), the American College of Gastroenterology (ACG), and the American Society for Gastrointestinal Endoscopy (ASGE) have jointly released “COVID-19 Clinical Insights for Our Community of Gastroenterologists and Gastroenterology Care Providers,” which can be found on the websites of the various societies.
“The purpose of this communication is to jointly provide you with up to date COVID-19 information in order to maintain the highest level of health and safety for our patients, staff, community, and ourselves,” according to the AGA website announcement.
In particular, the societies point out that there is recent evidence suggesting the potential for coronavirus transmission through droplets and perhaps fecal shedding, which pose potential risks in particular during endoscopy and colonoscopy procedures to other patients, endoscopy personnel, and practitioners.
Relevant clinical factors related to COVID-19 are discussed, including the fact that asymptomatic spread can occur during the prodromal phase (the mean incubation period is approximately 5 days, with a range of 0-14 days), with viral shedding greatest when symptoms begin.
Between 20% and 30% of patients with COVID-19 infection show abnormal liver enzymes. In addition, COVID-19 patients show drops in their leukocyte counts, and elevated white blood cell counts is a poor prognostic sign, according to the release.
The Centers for Disease Control and Prevention lists vulnerable populations at the greatest risk for more serious outcomes; these include the elderly and those with severe chronic health conditions, such as heart disease, lung disease, diabetes, decompensated cirrhosis, HIV with low CD4 counts, and immunosuppression (including liver and other solid organ transplant recipients), are at higher risk of developing more serious illness. In addition pregnancy may provide added risk.
Specific advice for the gastroenterology profession
The joint statement urges that practitioners strongly consider rescheduling elective nonurgent endoscopic procedures, although some nonurgent procedures are higher priority and may need to be performed, including cancer evaluations, prosthetic removals, and evaluation of significant symptoms. “Of note, the Surgeon General on 3/14/20 advised hospitals to postpone all elective surgeries,” the document states.
Patient concerns
In all cases, patients should be prescreened for high-risk exposure or symptoms. This includes asking about history of fever or respiratory symptoms, family members or close contacts with similar symptoms, any contact with a confirmed case of COVID-19, and recent travel to a high-risk area. “Avoid bringing patients (or their escorts) into the medical facility who are over age 65 or have one of the CDC recognized risks listed above,” the societies advise.
Check body temperature of the patient upon arrival at endoscopy unit or clinic, and keep all patients at an appropriate distance from each other (6 feet is recommended) throughout the entire time in the endoscopy unit.
“For COVID-19 positive patients, or those awaiting test results, isolation precautions should be taken with procedures performed in negative pressure rooms,” according to the statement.
In addition, use telemedicine where possible in elective cases, and consider phone follow-up after any procedures at 7 and 14 days to ask about new diagnosis of COVID-19 or development of its symptoms, .
Those patients who are on immunosuppressive drugs for inflammatory bowel disease and autoimmune hepatitis should continue taking their medications because the risk of disease flare outweighs the chance of contracting coronavirus, according to the document. In addition, these patients should be advised to follow CDC guidelines for at-risk groups by avoiding crowds and limiting travel.
Protection of practitioners
Key factors in ensuring practitioner safety and maintaining practice functionality are discussed by the joint document. In particular, appropriate personal protective equipment (PPE) should be worn by all members of the endoscopy team: gloves, mask, eye shield/goggles, face shields, and gown, but practitioners should also be aware of how to put on and take off PPE appropriately.
“Conservation of PPE is critical. Only essential personnel should be present in cases. Consider extended use or reuse of surgical masks and eye protection in accordance with hospital policies,” the document recommends.
“It is important to address our collective staff needs and institute policies that protect our workforce.” To that end, the document recommends that centers should strategically assign available personnel in order to minimize concomitant exposure of those with similar or unique skill sets. This includes the use of nonphysician practitioners and fellows that cannot participate in cases for screening and triaging patients, or performing virtual visits.
Coming at a time of pandemic, when gastrointestinal symptoms have been recognized as a more common symptom of COVID-19 than previously expected and liver damage has been noted as a potential repercussion of SARS-CoV-2 infection, these clinical insights provide a template for gastroenterologists and related professionals for dealing with their patients and keeping themselves safe under dramatically changed circumstances.
The partnered organizations, AASLD, ACG, AGA, and ASGE, are committed to providing updated COVID-19 information as appropriate. However: “Given the evolving and fluid nature of the situation, institutions, hospitals and clinics have also been formulating their own local guidelines, so we urge you to follow the evolving CDC recommendations and your local requirements,” according to the AGA website announcement.
In addition to the joint communication, the society websites each offer additional COVID-19 information. The AGA practice updates on the COVID-19 webpage provides information about announcements, such as the cancellation of Digestive Disease Week® in May, a location for AGA members to discuss their COVID-19 experiences and share advice, and links to the CDC COVID-19 updates.
SOURCE: American Gastroenterological Association et al. March 2020, COVID-19 Clinical Insights for Our Community of Gastroenterologists and Gastroenterology Care Providers.
Follicular lymphoma treatment can benefit patients 80 years and older
Follicular lymphoma (FL) treatment was associated with improved survival among patients diagnosed with FL at aged 80 years and older, according to the results of a large, retrospective database cohort study.
Researchers used the linked Surveillance, Epidemiology, and End Results–Medicare dataset to identify patients 80 years of age and older, diagnosed with FL between 2000 and 2013, identifying FL-directed treatments based on published guidelines. They used a propensity-score matched sample to compare treated and untreated patient cohorts who had similar observed characteristics.
They assessed 3,705 older patients with FL and a mean age of 84 years). Over a median follow-up of 2.9 years, 68% of the sample received FL-directed therapy and the most common regimen was rituximab monotherapy, which 21% (768 patients) received.
The median overall survival for the treated group was 4.31 years (95% confidence interval [CI], 4.00-4.61) vs. 2.86 years (95% CI, 2.59-3.16) for the untreated group, according to the report, published in the Journal of Geriatric Oncology.
The 3-year restricted mean survival time for the treated group was 2.36 years (95% CI, 2.30-2.41), vs. 2.05 years (95% CI, 1.98-2.11) for the untreated group. Treatment was associated with a 23% reduction in the hazard of death (HR: 0.77; P < .001).
Multivariable analysis showed that older age and a Charlson Comorbidity Index score of two or higher, and a proxy indicator for poor performance status, were inversely associated with receiving treatment. “These factors are expected to discourage physicians from providing FL-directed therapy,” the researchers suggested.
“We observed that, in a cohort of FL patients aged 80 years or older, FL-directed therapy was associated with an overall survival benefit, which persisted in important subgroups,” the researchers concluded.
Financial support for this study was provided by Bayer. One of the authors is employed by Bayer.
SOURCE: Albarmawi H et al. J Geriatric Oncol. 2020;11:55-61.
Follicular lymphoma (FL) treatment was associated with improved survival among patients diagnosed with FL at aged 80 years and older, according to the results of a large, retrospective database cohort study.
Researchers used the linked Surveillance, Epidemiology, and End Results–Medicare dataset to identify patients 80 years of age and older, diagnosed with FL between 2000 and 2013, identifying FL-directed treatments based on published guidelines. They used a propensity-score matched sample to compare treated and untreated patient cohorts who had similar observed characteristics.
They assessed 3,705 older patients with FL and a mean age of 84 years). Over a median follow-up of 2.9 years, 68% of the sample received FL-directed therapy and the most common regimen was rituximab monotherapy, which 21% (768 patients) received.
The median overall survival for the treated group was 4.31 years (95% confidence interval [CI], 4.00-4.61) vs. 2.86 years (95% CI, 2.59-3.16) for the untreated group, according to the report, published in the Journal of Geriatric Oncology.
The 3-year restricted mean survival time for the treated group was 2.36 years (95% CI, 2.30-2.41), vs. 2.05 years (95% CI, 1.98-2.11) for the untreated group. Treatment was associated with a 23% reduction in the hazard of death (HR: 0.77; P < .001).
Multivariable analysis showed that older age and a Charlson Comorbidity Index score of two or higher, and a proxy indicator for poor performance status, were inversely associated with receiving treatment. “These factors are expected to discourage physicians from providing FL-directed therapy,” the researchers suggested.
“We observed that, in a cohort of FL patients aged 80 years or older, FL-directed therapy was associated with an overall survival benefit, which persisted in important subgroups,” the researchers concluded.
Financial support for this study was provided by Bayer. One of the authors is employed by Bayer.
SOURCE: Albarmawi H et al. J Geriatric Oncol. 2020;11:55-61.
Follicular lymphoma (FL) treatment was associated with improved survival among patients diagnosed with FL at aged 80 years and older, according to the results of a large, retrospective database cohort study.
Researchers used the linked Surveillance, Epidemiology, and End Results–Medicare dataset to identify patients 80 years of age and older, diagnosed with FL between 2000 and 2013, identifying FL-directed treatments based on published guidelines. They used a propensity-score matched sample to compare treated and untreated patient cohorts who had similar observed characteristics.
They assessed 3,705 older patients with FL and a mean age of 84 years). Over a median follow-up of 2.9 years, 68% of the sample received FL-directed therapy and the most common regimen was rituximab monotherapy, which 21% (768 patients) received.
The median overall survival for the treated group was 4.31 years (95% confidence interval [CI], 4.00-4.61) vs. 2.86 years (95% CI, 2.59-3.16) for the untreated group, according to the report, published in the Journal of Geriatric Oncology.
The 3-year restricted mean survival time for the treated group was 2.36 years (95% CI, 2.30-2.41), vs. 2.05 years (95% CI, 1.98-2.11) for the untreated group. Treatment was associated with a 23% reduction in the hazard of death (HR: 0.77; P < .001).
Multivariable analysis showed that older age and a Charlson Comorbidity Index score of two or higher, and a proxy indicator for poor performance status, were inversely associated with receiving treatment. “These factors are expected to discourage physicians from providing FL-directed therapy,” the researchers suggested.
“We observed that, in a cohort of FL patients aged 80 years or older, FL-directed therapy was associated with an overall survival benefit, which persisted in important subgroups,” the researchers concluded.
Financial support for this study was provided by Bayer. One of the authors is employed by Bayer.
SOURCE: Albarmawi H et al. J Geriatric Oncol. 2020;11:55-61.
FROM THE JOURNAL OF GERIATRIC ONCOLOGY
COVID-19: ASTCT provides interim guidelines for transplantation
The American Society for Transplantation and Cellular Therapy (ASTCT) has released interim guidelines for the care of hematopoietic cell transplantation (HCT) and cellular therapy patients in the light of the global SARS-CoV-2 pandemic.
The guidelines, summarized briefly below, focus on diagnostic and treatment considerations, evaluation of patients prior to initializing HCT and cellular therapy, and cell donor evaluation. Much of the guideline relies upon recommendations developed by the European Society for Blood and Marrow Transplantation (ESBMT). These guidelines were updated on March 16.
The ASTCT document focuses on patient-treatment specifics and does not cover specific infection-prevention policies and procedures, instead suggesting that local and institutional guidelines, such as those from the Centers for Disease Control and Prevention, should be followed. They did recommend that, in the local presence of COVID-19, “clinic visits that are not critical should be either deferred or substituted with telemedicine visits if deemed appropriate and feasible.”
Diagnostic considerations
In any patient with upper or lower respiratory symptoms, obtain polymerase chain reaction (PCR) testing for SARS-CoV-2, where possible, in addition to other respiratory virus PCR testing from any respiratory sample obtained, following CDC recommendations for sample collection and processing, which are continuously being updated on the CDC website.
These recommendations include nasal sampling, rather than oral sampling, and the discouraging of nasal washes where avoidable. If nasal washing is performed, it should be done with appropriate personal protective equipment as described by the CDC. The CDC has also provided additional infection prevention and control information for known and suspected COVID-19 patients in health care settings.
In patients positive for SARS-CoV-2 in an upper respiratory tract sample, chest imaging should be considered.
Preliminary reports suggest that there may be a discrepancy between upper- and lower-tract specimen positivity. Therefore, even when SARS-CoV-2 is not detected in an upper respiratory sample, the ASTCT recommends that chest imaging should be considered for lower respiratory tract infection when clinical symptoms of lower respiratory tract infection are present, including shortness of breath, hypoxia, and tachypnea.
With regard to routine bronchoalveolar lavage, the ASTCT recommends against it if a patient tests positive for SARS-CoV-2 given the risk of transmission among health care workers. The exception is in the case of suspected coinfection based on abnormal chest imaging and in patients for whom it is clinically indicated (for example, those receiving invasive mechanical ventilation). In addition to testing bronchoalveolar lavage samples for SARS-CoV-2, “copathogens should be evaluated and treated.”
Treatment considerations
“At this point no recommendations can be made on specific therapies due to limited data and unknown risk versus benefit; additional recommendations will be forthcoming. Even less data is available for pediatric patients. Treatment for viral, bacterial, and fungal copathogens should be optimized,” according to the ASTCT.
However, the society lists several therapies currently under consideration, which may be available through compassionate-use programs and are being investigated in current clinical trials in several countries, “including lopinavir/ritonavir, ribavirin, hydroxychloroquine, darunavir/cobicistat, and interferons-alpha and -beta.” Remdesivir, in particular, is being evaluated in a National Institutes of Health–sponsored, placebo-controlled clinical trial (NCT04280705).
In case of known or suspected COVID-19 with normal imaging and no or mild symptoms, no therapy is recommended. However, if symptoms progress or imaging is abnormal, an infectious disease specialist or department should be consulted, according to the ASTCT.
Evaluation prior to HCT or cellular therapy
“There is sufficient concern that COVID-19 could have a significant impact on posttransplant or posttherapy outcomes,” according to the guidelines, and the ASTCT provided the following recommendations to be considered in known or suspected COVID-19 patients. In particular, practitioners need to weigh the risk of delaying or altering therapy plans with the risk of progression of underlying disease.
If SARS-CoV-2 is detected in a respiratory specimen, HCT or cellular therapy procedures should be deferred. Therapy should also be deferred in HCT and cellular therapy candidates with close contact with a person infected with SARS-CoV-2 and in those patients who have traveled to a high-risk area or had close contact with a person traveling from an area at high risk for COVID-19.
In the case of a patient in a community with widespread disease, “all HCT and cellular therapy candidates should undergo screening for SARS-CoV-2 infection by PCR in respiratory specimens at the time of initial evaluation and 2 days prior to conditioning/lymphodepletion, regardless of the presence of symptoms, if testing is available.”
Procedures to be deferred include peripheral blood stem cell mobilization, bone marrow harvest, T-cell collections, and conditioning/lymphodepletion. These should not be performed for at least 14 days (preferably 21 days) from the day of last contact, according to the ASTCT. Two consecutive negative PCR tests each approximately 1 week apart (deferral for 14 days minimum), should be obtained, if available.
In areas with high community spread, the guidelines also state that “interim treatment and/or longer deferral of definite therapy should be considered when feasible (for example, multiple myeloma, germ cell tumors, consolidative transplants).”
Similar considerations should be afforded to potential cellular donors. Donors with SARS-CoV-2 detected in a respiratory sample are considered ineligible. Those meeting exposure criteria for patients, as listed above, should be excluded from donation for at least 28 days. “In individual circumstances, a donor may be considered eligible if respiratory samples are negative for SARS-CoV-2 by PCR and donor is asymptomatic. Donor should be closely monitored for COVID-19.”
In the case of unrelated donors, the ASTCT recommends referral to the National Marrow Donor Program (NMDP) guidelines for updated guidance, but points out that, according to the NMDP, the Food and Drug Administration reports that there have been no reported or suspected cases of transfusion-transmitted COVID-19 to date and that “no cases of transfusion-transmission were ever reported for the other two coronaviruses that emerged during the past 2 decades [SARS, the severe acute respiratory syndrome coronavirus, and MERS-CoV, which causes Mideast respiratory syndrome].”
In the updated ESBMT guidelines, this recommendation was made in reference to the greater spread of COVID-19: “It is therefore strongly recommended to have secured stem cell product access by freezing the product before start of conditioning and, in situations when this is not possible, to have an alternative donor as a backup. For low-risk patients, it is recommended to postpone the start of the transplant procedure if deemed to be safe to do so. This includes both allogeneic and autologous transplant procedures.”
In a recent webinar, Pavan Reddy, MD, of the University of Michigan, Ann Arbor, and ASTCT President; Alpana Waghmare, MD, of the Fred Hutchinson Cancer Research Center, Seattle; and Roy Chemaly, MD, of the MD Anderson Cancer Center, Houston, and chair of the ASTCT Transplant Infectious Disease Special Interest Group, discussed the guidelines and provided some updated information.
Dr. Reddy stated that, at the University of Michigan, they were delaying all nonurgent transplants, largely for myeloma, and are postponing even allotransplants. “The transplants we are not delaying are the high-risk AMLs … and in cases where we truly cannot delay transplants because of patient condition or, in some cases, the donor situation.”
Dr. Chemaly and Dr. Waghmare both agreed that their centers were following a similar approach.
With regard to patient testing, all three institution have recently moved to testing everyone a few days before transplant regardless of symptoms.
They also pointed out that essentially all clinical trials were being put on hold during the crisis, except for those few where patients would be put in danger if the trial were interrupted.
The guidelines discuss in depth the rationale, toxicity, and dosages for use of select agents, including remdesivir, chloroquine/hydroxychloroquine, ribavirin, and tocilizumab. There was some concern expressed about shortages developing in these drugs, which serve a number of other patient communities, in particular the possibility of a tocilizumab shortage was of concern.
Steroids and intravenous immunoglobulins are not are not recommended, according to the guidelines, which also stated that adjunctive therapies such as antibiotics should be considered.
Dr. Chemaly, Dr. Reddy, and Dr. Waghmare did not provide disclosure in the webinar.
The ASTCT recommends following the World Health Organization and CDC COVID-19 pages for continued updates and information on other aspects of the pandemic.
This article was updated 3/26/20.
SOURCE: ASTCT Response to COVID-19. 2020. www.astct.org/connect/astct-response-to-covid-19.
There is emerging data regarding coinfection of SARS-CoV-2 with other viruses including infleunza. Immunocompromised hosts, especially transplantation and cellular therapy (TCT) recipients, are known to frequently have more than one pathogen present, especially in pulmonary infections. As the community spread increases, it would be reasonable to obtain concomitant testing for respiratory viruses along with SARS-CoV-2 as recommended. In addition, viral infection can cause secondary bacterial and fungal infections (especially Aspergillus). In the presence of SARS-CoV-2, where it is recommended to avoid bronchoalveolar lavage, we have to keep a high clinical suspicion based on patients’ risk factors.
Acute Respiratory Distress Syndrome (ARDS) caused by an intense inflammatory response is the main cause of death in COVID-19. Early reports on the use of tocilizumab (an IL-6 receptor blocker) for ARDS to block cytokine mediated injury to the lung should be a consideration early in the course of COVID-19 pneumonitis, especially in setting of high risk for ARDS mortality.
We are considering other IL-6–blocking agents like siltuximab in case of a shortage of tocilizumab while centers scramble to get these agents. It is important to note that any such usages for COVID-19 would be considered off-label.
TCT candidates should of course be practicing social distancing in days leading to transplant to reduce their risk of exposure regardless of state or federal recommendations. Household members of TCT candidates should practice similar caution because transmission has been reported by asymptomatic individuals.
Zainab Shahid, MD, is the medical director of Bone Marrow Transplant Infectious Diseases at the Levine Cancer Institute/Atrium Health and a clinical associate professor of medicine at University of North Carolina at Chapel Hill. She reported that she had no relevant disclosures.
There is emerging data regarding coinfection of SARS-CoV-2 with other viruses including infleunza. Immunocompromised hosts, especially transplantation and cellular therapy (TCT) recipients, are known to frequently have more than one pathogen present, especially in pulmonary infections. As the community spread increases, it would be reasonable to obtain concomitant testing for respiratory viruses along with SARS-CoV-2 as recommended. In addition, viral infection can cause secondary bacterial and fungal infections (especially Aspergillus). In the presence of SARS-CoV-2, where it is recommended to avoid bronchoalveolar lavage, we have to keep a high clinical suspicion based on patients’ risk factors.
Acute Respiratory Distress Syndrome (ARDS) caused by an intense inflammatory response is the main cause of death in COVID-19. Early reports on the use of tocilizumab (an IL-6 receptor blocker) for ARDS to block cytokine mediated injury to the lung should be a consideration early in the course of COVID-19 pneumonitis, especially in setting of high risk for ARDS mortality.
We are considering other IL-6–blocking agents like siltuximab in case of a shortage of tocilizumab while centers scramble to get these agents. It is important to note that any such usages for COVID-19 would be considered off-label.
TCT candidates should of course be practicing social distancing in days leading to transplant to reduce their risk of exposure regardless of state or federal recommendations. Household members of TCT candidates should practice similar caution because transmission has been reported by asymptomatic individuals.
Zainab Shahid, MD, is the medical director of Bone Marrow Transplant Infectious Diseases at the Levine Cancer Institute/Atrium Health and a clinical associate professor of medicine at University of North Carolina at Chapel Hill. She reported that she had no relevant disclosures.
There is emerging data regarding coinfection of SARS-CoV-2 with other viruses including infleunza. Immunocompromised hosts, especially transplantation and cellular therapy (TCT) recipients, are known to frequently have more than one pathogen present, especially in pulmonary infections. As the community spread increases, it would be reasonable to obtain concomitant testing for respiratory viruses along with SARS-CoV-2 as recommended. In addition, viral infection can cause secondary bacterial and fungal infections (especially Aspergillus). In the presence of SARS-CoV-2, where it is recommended to avoid bronchoalveolar lavage, we have to keep a high clinical suspicion based on patients’ risk factors.
Acute Respiratory Distress Syndrome (ARDS) caused by an intense inflammatory response is the main cause of death in COVID-19. Early reports on the use of tocilizumab (an IL-6 receptor blocker) for ARDS to block cytokine mediated injury to the lung should be a consideration early in the course of COVID-19 pneumonitis, especially in setting of high risk for ARDS mortality.
We are considering other IL-6–blocking agents like siltuximab in case of a shortage of tocilizumab while centers scramble to get these agents. It is important to note that any such usages for COVID-19 would be considered off-label.
TCT candidates should of course be practicing social distancing in days leading to transplant to reduce their risk of exposure regardless of state or federal recommendations. Household members of TCT candidates should practice similar caution because transmission has been reported by asymptomatic individuals.
Zainab Shahid, MD, is the medical director of Bone Marrow Transplant Infectious Diseases at the Levine Cancer Institute/Atrium Health and a clinical associate professor of medicine at University of North Carolina at Chapel Hill. She reported that she had no relevant disclosures.
The American Society for Transplantation and Cellular Therapy (ASTCT) has released interim guidelines for the care of hematopoietic cell transplantation (HCT) and cellular therapy patients in the light of the global SARS-CoV-2 pandemic.
The guidelines, summarized briefly below, focus on diagnostic and treatment considerations, evaluation of patients prior to initializing HCT and cellular therapy, and cell donor evaluation. Much of the guideline relies upon recommendations developed by the European Society for Blood and Marrow Transplantation (ESBMT). These guidelines were updated on March 16.
The ASTCT document focuses on patient-treatment specifics and does not cover specific infection-prevention policies and procedures, instead suggesting that local and institutional guidelines, such as those from the Centers for Disease Control and Prevention, should be followed. They did recommend that, in the local presence of COVID-19, “clinic visits that are not critical should be either deferred or substituted with telemedicine visits if deemed appropriate and feasible.”
Diagnostic considerations
In any patient with upper or lower respiratory symptoms, obtain polymerase chain reaction (PCR) testing for SARS-CoV-2, where possible, in addition to other respiratory virus PCR testing from any respiratory sample obtained, following CDC recommendations for sample collection and processing, which are continuously being updated on the CDC website.
These recommendations include nasal sampling, rather than oral sampling, and the discouraging of nasal washes where avoidable. If nasal washing is performed, it should be done with appropriate personal protective equipment as described by the CDC. The CDC has also provided additional infection prevention and control information for known and suspected COVID-19 patients in health care settings.
In patients positive for SARS-CoV-2 in an upper respiratory tract sample, chest imaging should be considered.
Preliminary reports suggest that there may be a discrepancy between upper- and lower-tract specimen positivity. Therefore, even when SARS-CoV-2 is not detected in an upper respiratory sample, the ASTCT recommends that chest imaging should be considered for lower respiratory tract infection when clinical symptoms of lower respiratory tract infection are present, including shortness of breath, hypoxia, and tachypnea.
With regard to routine bronchoalveolar lavage, the ASTCT recommends against it if a patient tests positive for SARS-CoV-2 given the risk of transmission among health care workers. The exception is in the case of suspected coinfection based on abnormal chest imaging and in patients for whom it is clinically indicated (for example, those receiving invasive mechanical ventilation). In addition to testing bronchoalveolar lavage samples for SARS-CoV-2, “copathogens should be evaluated and treated.”
Treatment considerations
“At this point no recommendations can be made on specific therapies due to limited data and unknown risk versus benefit; additional recommendations will be forthcoming. Even less data is available for pediatric patients. Treatment for viral, bacterial, and fungal copathogens should be optimized,” according to the ASTCT.
However, the society lists several therapies currently under consideration, which may be available through compassionate-use programs and are being investigated in current clinical trials in several countries, “including lopinavir/ritonavir, ribavirin, hydroxychloroquine, darunavir/cobicistat, and interferons-alpha and -beta.” Remdesivir, in particular, is being evaluated in a National Institutes of Health–sponsored, placebo-controlled clinical trial (NCT04280705).
In case of known or suspected COVID-19 with normal imaging and no or mild symptoms, no therapy is recommended. However, if symptoms progress or imaging is abnormal, an infectious disease specialist or department should be consulted, according to the ASTCT.
Evaluation prior to HCT or cellular therapy
“There is sufficient concern that COVID-19 could have a significant impact on posttransplant or posttherapy outcomes,” according to the guidelines, and the ASTCT provided the following recommendations to be considered in known or suspected COVID-19 patients. In particular, practitioners need to weigh the risk of delaying or altering therapy plans with the risk of progression of underlying disease.
If SARS-CoV-2 is detected in a respiratory specimen, HCT or cellular therapy procedures should be deferred. Therapy should also be deferred in HCT and cellular therapy candidates with close contact with a person infected with SARS-CoV-2 and in those patients who have traveled to a high-risk area or had close contact with a person traveling from an area at high risk for COVID-19.
In the case of a patient in a community with widespread disease, “all HCT and cellular therapy candidates should undergo screening for SARS-CoV-2 infection by PCR in respiratory specimens at the time of initial evaluation and 2 days prior to conditioning/lymphodepletion, regardless of the presence of symptoms, if testing is available.”
Procedures to be deferred include peripheral blood stem cell mobilization, bone marrow harvest, T-cell collections, and conditioning/lymphodepletion. These should not be performed for at least 14 days (preferably 21 days) from the day of last contact, according to the ASTCT. Two consecutive negative PCR tests each approximately 1 week apart (deferral for 14 days minimum), should be obtained, if available.
In areas with high community spread, the guidelines also state that “interim treatment and/or longer deferral of definite therapy should be considered when feasible (for example, multiple myeloma, germ cell tumors, consolidative transplants).”
Similar considerations should be afforded to potential cellular donors. Donors with SARS-CoV-2 detected in a respiratory sample are considered ineligible. Those meeting exposure criteria for patients, as listed above, should be excluded from donation for at least 28 days. “In individual circumstances, a donor may be considered eligible if respiratory samples are negative for SARS-CoV-2 by PCR and donor is asymptomatic. Donor should be closely monitored for COVID-19.”
In the case of unrelated donors, the ASTCT recommends referral to the National Marrow Donor Program (NMDP) guidelines for updated guidance, but points out that, according to the NMDP, the Food and Drug Administration reports that there have been no reported or suspected cases of transfusion-transmitted COVID-19 to date and that “no cases of transfusion-transmission were ever reported for the other two coronaviruses that emerged during the past 2 decades [SARS, the severe acute respiratory syndrome coronavirus, and MERS-CoV, which causes Mideast respiratory syndrome].”
In the updated ESBMT guidelines, this recommendation was made in reference to the greater spread of COVID-19: “It is therefore strongly recommended to have secured stem cell product access by freezing the product before start of conditioning and, in situations when this is not possible, to have an alternative donor as a backup. For low-risk patients, it is recommended to postpone the start of the transplant procedure if deemed to be safe to do so. This includes both allogeneic and autologous transplant procedures.”
In a recent webinar, Pavan Reddy, MD, of the University of Michigan, Ann Arbor, and ASTCT President; Alpana Waghmare, MD, of the Fred Hutchinson Cancer Research Center, Seattle; and Roy Chemaly, MD, of the MD Anderson Cancer Center, Houston, and chair of the ASTCT Transplant Infectious Disease Special Interest Group, discussed the guidelines and provided some updated information.
Dr. Reddy stated that, at the University of Michigan, they were delaying all nonurgent transplants, largely for myeloma, and are postponing even allotransplants. “The transplants we are not delaying are the high-risk AMLs … and in cases where we truly cannot delay transplants because of patient condition or, in some cases, the donor situation.”
Dr. Chemaly and Dr. Waghmare both agreed that their centers were following a similar approach.
With regard to patient testing, all three institution have recently moved to testing everyone a few days before transplant regardless of symptoms.
They also pointed out that essentially all clinical trials were being put on hold during the crisis, except for those few where patients would be put in danger if the trial were interrupted.
The guidelines discuss in depth the rationale, toxicity, and dosages for use of select agents, including remdesivir, chloroquine/hydroxychloroquine, ribavirin, and tocilizumab. There was some concern expressed about shortages developing in these drugs, which serve a number of other patient communities, in particular the possibility of a tocilizumab shortage was of concern.
Steroids and intravenous immunoglobulins are not are not recommended, according to the guidelines, which also stated that adjunctive therapies such as antibiotics should be considered.
Dr. Chemaly, Dr. Reddy, and Dr. Waghmare did not provide disclosure in the webinar.
The ASTCT recommends following the World Health Organization and CDC COVID-19 pages for continued updates and information on other aspects of the pandemic.
This article was updated 3/26/20.
SOURCE: ASTCT Response to COVID-19. 2020. www.astct.org/connect/astct-response-to-covid-19.
The American Society for Transplantation and Cellular Therapy (ASTCT) has released interim guidelines for the care of hematopoietic cell transplantation (HCT) and cellular therapy patients in the light of the global SARS-CoV-2 pandemic.
The guidelines, summarized briefly below, focus on diagnostic and treatment considerations, evaluation of patients prior to initializing HCT and cellular therapy, and cell donor evaluation. Much of the guideline relies upon recommendations developed by the European Society for Blood and Marrow Transplantation (ESBMT). These guidelines were updated on March 16.
The ASTCT document focuses on patient-treatment specifics and does not cover specific infection-prevention policies and procedures, instead suggesting that local and institutional guidelines, such as those from the Centers for Disease Control and Prevention, should be followed. They did recommend that, in the local presence of COVID-19, “clinic visits that are not critical should be either deferred or substituted with telemedicine visits if deemed appropriate and feasible.”
Diagnostic considerations
In any patient with upper or lower respiratory symptoms, obtain polymerase chain reaction (PCR) testing for SARS-CoV-2, where possible, in addition to other respiratory virus PCR testing from any respiratory sample obtained, following CDC recommendations for sample collection and processing, which are continuously being updated on the CDC website.
These recommendations include nasal sampling, rather than oral sampling, and the discouraging of nasal washes where avoidable. If nasal washing is performed, it should be done with appropriate personal protective equipment as described by the CDC. The CDC has also provided additional infection prevention and control information for known and suspected COVID-19 patients in health care settings.
In patients positive for SARS-CoV-2 in an upper respiratory tract sample, chest imaging should be considered.
Preliminary reports suggest that there may be a discrepancy between upper- and lower-tract specimen positivity. Therefore, even when SARS-CoV-2 is not detected in an upper respiratory sample, the ASTCT recommends that chest imaging should be considered for lower respiratory tract infection when clinical symptoms of lower respiratory tract infection are present, including shortness of breath, hypoxia, and tachypnea.
With regard to routine bronchoalveolar lavage, the ASTCT recommends against it if a patient tests positive for SARS-CoV-2 given the risk of transmission among health care workers. The exception is in the case of suspected coinfection based on abnormal chest imaging and in patients for whom it is clinically indicated (for example, those receiving invasive mechanical ventilation). In addition to testing bronchoalveolar lavage samples for SARS-CoV-2, “copathogens should be evaluated and treated.”
Treatment considerations
“At this point no recommendations can be made on specific therapies due to limited data and unknown risk versus benefit; additional recommendations will be forthcoming. Even less data is available for pediatric patients. Treatment for viral, bacterial, and fungal copathogens should be optimized,” according to the ASTCT.
However, the society lists several therapies currently under consideration, which may be available through compassionate-use programs and are being investigated in current clinical trials in several countries, “including lopinavir/ritonavir, ribavirin, hydroxychloroquine, darunavir/cobicistat, and interferons-alpha and -beta.” Remdesivir, in particular, is being evaluated in a National Institutes of Health–sponsored, placebo-controlled clinical trial (NCT04280705).
In case of known or suspected COVID-19 with normal imaging and no or mild symptoms, no therapy is recommended. However, if symptoms progress or imaging is abnormal, an infectious disease specialist or department should be consulted, according to the ASTCT.
Evaluation prior to HCT or cellular therapy
“There is sufficient concern that COVID-19 could have a significant impact on posttransplant or posttherapy outcomes,” according to the guidelines, and the ASTCT provided the following recommendations to be considered in known or suspected COVID-19 patients. In particular, practitioners need to weigh the risk of delaying or altering therapy plans with the risk of progression of underlying disease.
If SARS-CoV-2 is detected in a respiratory specimen, HCT or cellular therapy procedures should be deferred. Therapy should also be deferred in HCT and cellular therapy candidates with close contact with a person infected with SARS-CoV-2 and in those patients who have traveled to a high-risk area or had close contact with a person traveling from an area at high risk for COVID-19.
In the case of a patient in a community with widespread disease, “all HCT and cellular therapy candidates should undergo screening for SARS-CoV-2 infection by PCR in respiratory specimens at the time of initial evaluation and 2 days prior to conditioning/lymphodepletion, regardless of the presence of symptoms, if testing is available.”
Procedures to be deferred include peripheral blood stem cell mobilization, bone marrow harvest, T-cell collections, and conditioning/lymphodepletion. These should not be performed for at least 14 days (preferably 21 days) from the day of last contact, according to the ASTCT. Two consecutive negative PCR tests each approximately 1 week apart (deferral for 14 days minimum), should be obtained, if available.
In areas with high community spread, the guidelines also state that “interim treatment and/or longer deferral of definite therapy should be considered when feasible (for example, multiple myeloma, germ cell tumors, consolidative transplants).”
Similar considerations should be afforded to potential cellular donors. Donors with SARS-CoV-2 detected in a respiratory sample are considered ineligible. Those meeting exposure criteria for patients, as listed above, should be excluded from donation for at least 28 days. “In individual circumstances, a donor may be considered eligible if respiratory samples are negative for SARS-CoV-2 by PCR and donor is asymptomatic. Donor should be closely monitored for COVID-19.”
In the case of unrelated donors, the ASTCT recommends referral to the National Marrow Donor Program (NMDP) guidelines for updated guidance, but points out that, according to the NMDP, the Food and Drug Administration reports that there have been no reported or suspected cases of transfusion-transmitted COVID-19 to date and that “no cases of transfusion-transmission were ever reported for the other two coronaviruses that emerged during the past 2 decades [SARS, the severe acute respiratory syndrome coronavirus, and MERS-CoV, which causes Mideast respiratory syndrome].”
In the updated ESBMT guidelines, this recommendation was made in reference to the greater spread of COVID-19: “It is therefore strongly recommended to have secured stem cell product access by freezing the product before start of conditioning and, in situations when this is not possible, to have an alternative donor as a backup. For low-risk patients, it is recommended to postpone the start of the transplant procedure if deemed to be safe to do so. This includes both allogeneic and autologous transplant procedures.”
In a recent webinar, Pavan Reddy, MD, of the University of Michigan, Ann Arbor, and ASTCT President; Alpana Waghmare, MD, of the Fred Hutchinson Cancer Research Center, Seattle; and Roy Chemaly, MD, of the MD Anderson Cancer Center, Houston, and chair of the ASTCT Transplant Infectious Disease Special Interest Group, discussed the guidelines and provided some updated information.
Dr. Reddy stated that, at the University of Michigan, they were delaying all nonurgent transplants, largely for myeloma, and are postponing even allotransplants. “The transplants we are not delaying are the high-risk AMLs … and in cases where we truly cannot delay transplants because of patient condition or, in some cases, the donor situation.”
Dr. Chemaly and Dr. Waghmare both agreed that their centers were following a similar approach.
With regard to patient testing, all three institution have recently moved to testing everyone a few days before transplant regardless of symptoms.
They also pointed out that essentially all clinical trials were being put on hold during the crisis, except for those few where patients would be put in danger if the trial were interrupted.
The guidelines discuss in depth the rationale, toxicity, and dosages for use of select agents, including remdesivir, chloroquine/hydroxychloroquine, ribavirin, and tocilizumab. There was some concern expressed about shortages developing in these drugs, which serve a number of other patient communities, in particular the possibility of a tocilizumab shortage was of concern.
Steroids and intravenous immunoglobulins are not are not recommended, according to the guidelines, which also stated that adjunctive therapies such as antibiotics should be considered.
Dr. Chemaly, Dr. Reddy, and Dr. Waghmare did not provide disclosure in the webinar.
The ASTCT recommends following the World Health Organization and CDC COVID-19 pages for continued updates and information on other aspects of the pandemic.
This article was updated 3/26/20.
SOURCE: ASTCT Response to COVID-19. 2020. www.astct.org/connect/astct-response-to-covid-19.
Sickle cell patients with vitamin D deficiency prone to more ED visits, longer stays
Patients with sickle cell disease (SCD) plus vitamin D deficiency were found to have more hospitalization outcomes, including number of emergency department (ED) visits, the number of hospital admissions for pain crisis, and the length of hospital admission, according to a study published online by researchers from New York-Presbyterian Brooklyn Methodist Hospital.
The researchers performed a retrospective chart review of all 134 pediatric patients with SCD (aged 1-21 years) from January 2015 to January 2016 in an urban-based hospital setting. Ninety patients with at least one reported vitamin D level who maintained follow-up during the time studied were enrolled. Hospitalization rates were compared between vitamin D deficiency (< 20 ng/mL) and sufficiency (> 20 ng/mL) patients.
When compared to patients with SCD and sufficient vitamin D levels, patients with both SCD and vitamin D deficiency were more likely to have at least one ED visit (P < .01), at least one admission for pain crisis (P < .01), and a longer length of admission (P < .0001), the researchers found.
“Screening and treatment for vitamin D deficiency is generally cost effective and readily available, potentially having a significant impact on the quality of life for those living with sickle cell disease,” the researchers concluded.
The authors reported that there was no study funding and that they had no conflicts of interest.
SOURCE: Brown B et al. Blood Cells Mol Dis. 2020. doi: 10.1016/j.bcmd.2020.102415.
Patients with sickle cell disease (SCD) plus vitamin D deficiency were found to have more hospitalization outcomes, including number of emergency department (ED) visits, the number of hospital admissions for pain crisis, and the length of hospital admission, according to a study published online by researchers from New York-Presbyterian Brooklyn Methodist Hospital.
The researchers performed a retrospective chart review of all 134 pediatric patients with SCD (aged 1-21 years) from January 2015 to January 2016 in an urban-based hospital setting. Ninety patients with at least one reported vitamin D level who maintained follow-up during the time studied were enrolled. Hospitalization rates were compared between vitamin D deficiency (< 20 ng/mL) and sufficiency (> 20 ng/mL) patients.
When compared to patients with SCD and sufficient vitamin D levels, patients with both SCD and vitamin D deficiency were more likely to have at least one ED visit (P < .01), at least one admission for pain crisis (P < .01), and a longer length of admission (P < .0001), the researchers found.
“Screening and treatment for vitamin D deficiency is generally cost effective and readily available, potentially having a significant impact on the quality of life for those living with sickle cell disease,” the researchers concluded.
The authors reported that there was no study funding and that they had no conflicts of interest.
SOURCE: Brown B et al. Blood Cells Mol Dis. 2020. doi: 10.1016/j.bcmd.2020.102415.
Patients with sickle cell disease (SCD) plus vitamin D deficiency were found to have more hospitalization outcomes, including number of emergency department (ED) visits, the number of hospital admissions for pain crisis, and the length of hospital admission, according to a study published online by researchers from New York-Presbyterian Brooklyn Methodist Hospital.
The researchers performed a retrospective chart review of all 134 pediatric patients with SCD (aged 1-21 years) from January 2015 to January 2016 in an urban-based hospital setting. Ninety patients with at least one reported vitamin D level who maintained follow-up during the time studied were enrolled. Hospitalization rates were compared between vitamin D deficiency (< 20 ng/mL) and sufficiency (> 20 ng/mL) patients.
When compared to patients with SCD and sufficient vitamin D levels, patients with both SCD and vitamin D deficiency were more likely to have at least one ED visit (P < .01), at least one admission for pain crisis (P < .01), and a longer length of admission (P < .0001), the researchers found.
“Screening and treatment for vitamin D deficiency is generally cost effective and readily available, potentially having a significant impact on the quality of life for those living with sickle cell disease,” the researchers concluded.
The authors reported that there was no study funding and that they had no conflicts of interest.
SOURCE: Brown B et al. Blood Cells Mol Dis. 2020. doi: 10.1016/j.bcmd.2020.102415.
FROM BLOOD CELLS, MOLECULES, AND DISEASES
Accelerated fetal growth in boys associated with development of AML
Accelerated fetal growth was associated with acute myeloid leukemia (AML), especially in infant boys and those with minimally differentiated leukemia, according to researchers from the Childhood Leukemia International Consortium (CLIC).
They assessed data from 22 studies involving a total of 3,564 cases to determine if there was an association between fetal growth and AML. The researchers also examined whether this association might vary by age, sex and disease subtype, according to their report published in the European Journal of Cancer.
The researchers calculated pooled estimates by age, sex and overall for harmonized fetal growth markers in association with AML. They used data from 17 International Fetal and Newborn Growth Consortium for the 21st Century Project studies and performed meta-analyses on 5 more studies. They also did subanalyses based on AML subtype.
They found a nearly 50% increased risk of AML among large-for-gestational-age infant boys (odds ratio [OR]: 1.49, 95% confidence interval [CI]: 1.03-2.14), reduced to 34% in boys aged less than 2 years (OR: 1.34, 95% CI: 1.05-1.71) and 25% in boys aged 0-14 years (OR: 1.25, 95% CI: 1.06-1.46). The association of large for gestational age was stronger in boys with the M0/M1 subtype (OR: 1.80, 95% CI: 1.15-2.83). In addition, large birth length for gestational age was also positively associated with AML (OR: 1.38, 95% CI: 1.00-1.92) in boys. By contrast, there, none of these factors were associated with AML in girls, nor were there associates for girls with respect to decelerated fetal growth markers.
“Although the absolute risk seems to be low at a population level, given the rarity of childhood AML, it would be worth exploring whether modifiable factors leading to macrosomia may also affect AML risk to stimulate future monitoring and preventive interventions before and during pregnancy,” the researchers suggested.
The authors reported that they had no conflicts of interest.
SOURCE: Karalexi MA et al. Eur J Canc. 2020;130:1-11.
Accelerated fetal growth was associated with acute myeloid leukemia (AML), especially in infant boys and those with minimally differentiated leukemia, according to researchers from the Childhood Leukemia International Consortium (CLIC).
They assessed data from 22 studies involving a total of 3,564 cases to determine if there was an association between fetal growth and AML. The researchers also examined whether this association might vary by age, sex and disease subtype, according to their report published in the European Journal of Cancer.
The researchers calculated pooled estimates by age, sex and overall for harmonized fetal growth markers in association with AML. They used data from 17 International Fetal and Newborn Growth Consortium for the 21st Century Project studies and performed meta-analyses on 5 more studies. They also did subanalyses based on AML subtype.
They found a nearly 50% increased risk of AML among large-for-gestational-age infant boys (odds ratio [OR]: 1.49, 95% confidence interval [CI]: 1.03-2.14), reduced to 34% in boys aged less than 2 years (OR: 1.34, 95% CI: 1.05-1.71) and 25% in boys aged 0-14 years (OR: 1.25, 95% CI: 1.06-1.46). The association of large for gestational age was stronger in boys with the M0/M1 subtype (OR: 1.80, 95% CI: 1.15-2.83). In addition, large birth length for gestational age was also positively associated with AML (OR: 1.38, 95% CI: 1.00-1.92) in boys. By contrast, there, none of these factors were associated with AML in girls, nor were there associates for girls with respect to decelerated fetal growth markers.
“Although the absolute risk seems to be low at a population level, given the rarity of childhood AML, it would be worth exploring whether modifiable factors leading to macrosomia may also affect AML risk to stimulate future monitoring and preventive interventions before and during pregnancy,” the researchers suggested.
The authors reported that they had no conflicts of interest.
SOURCE: Karalexi MA et al. Eur J Canc. 2020;130:1-11.
Accelerated fetal growth was associated with acute myeloid leukemia (AML), especially in infant boys and those with minimally differentiated leukemia, according to researchers from the Childhood Leukemia International Consortium (CLIC).
They assessed data from 22 studies involving a total of 3,564 cases to determine if there was an association between fetal growth and AML. The researchers also examined whether this association might vary by age, sex and disease subtype, according to their report published in the European Journal of Cancer.
The researchers calculated pooled estimates by age, sex and overall for harmonized fetal growth markers in association with AML. They used data from 17 International Fetal and Newborn Growth Consortium for the 21st Century Project studies and performed meta-analyses on 5 more studies. They also did subanalyses based on AML subtype.
They found a nearly 50% increased risk of AML among large-for-gestational-age infant boys (odds ratio [OR]: 1.49, 95% confidence interval [CI]: 1.03-2.14), reduced to 34% in boys aged less than 2 years (OR: 1.34, 95% CI: 1.05-1.71) and 25% in boys aged 0-14 years (OR: 1.25, 95% CI: 1.06-1.46). The association of large for gestational age was stronger in boys with the M0/M1 subtype (OR: 1.80, 95% CI: 1.15-2.83). In addition, large birth length for gestational age was also positively associated with AML (OR: 1.38, 95% CI: 1.00-1.92) in boys. By contrast, there, none of these factors were associated with AML in girls, nor were there associates for girls with respect to decelerated fetal growth markers.
“Although the absolute risk seems to be low at a population level, given the rarity of childhood AML, it would be worth exploring whether modifiable factors leading to macrosomia may also affect AML risk to stimulate future monitoring and preventive interventions before and during pregnancy,” the researchers suggested.
The authors reported that they had no conflicts of interest.
SOURCE: Karalexi MA et al. Eur J Canc. 2020;130:1-11.
FROM THE EUROPEAN JOURNAL OF CANCER
Fracture risk for MM patients remains higher despite improvements in treatments, survival
Bone lesions are one of the primary symptoms in multiple myeloma (MM), and approximately 80% of patients experience a pathological fracture at initial presentation or during the course of the disease, according to the authors of a study published online in Bone.
The authors performed a study to determine if improved treatment strategies and supportive care over time, including the use of bisphosphonates, reduced the overall fracture risk in MM patients.
Their retrospective case-control study included 1,334 patients with MM in Denmark from the Danish National Health Service, of which 881 sustained a fracture between 1996 and 2011. MM patients were matched to patients from the database without MM.
The researchers found that the risk of any fracture was significantly higher in MM patients, compared with patients without MM at all three time periods examined, and remained high over time: adjusted odds ratio (95% confidence interval) 1996-2000: 1.7 (1.3–2.3); 2001-2006: 1.3 (1.1-1.6); 2007-2011: 1.7 (1.4-2.2)). The risk of vertebral fractures was particularly higher in MM patients and also remained high over time: ORadj (95% CI) 1996-2000: 3.5 (1.4–8.6); 2001-2006: 4.0 (1.9-8.2); 2007-2011: 3.0 (1.6-5.7).
In addition, they found that the risk of any fracture was equally high in men and women MM patients, and in patients aged ≤ 65 or > 65 years.
“New treatment strategies, even if they have a positive impact on overall survival, offer no guarantee for a corresponding reduction in bone lesions,” the authors concluded.
The majority of authors reported having no disclosures. One author reported grants and personal fees from three pharmaceutical companies, outside the submitted work.
SOURCE: Oortgiesen BE et al. Bone. 2020 doi.org/10.1016/j.bone.2020.115299.
Bone lesions are one of the primary symptoms in multiple myeloma (MM), and approximately 80% of patients experience a pathological fracture at initial presentation or during the course of the disease, according to the authors of a study published online in Bone.
The authors performed a study to determine if improved treatment strategies and supportive care over time, including the use of bisphosphonates, reduced the overall fracture risk in MM patients.
Their retrospective case-control study included 1,334 patients with MM in Denmark from the Danish National Health Service, of which 881 sustained a fracture between 1996 and 2011. MM patients were matched to patients from the database without MM.
The researchers found that the risk of any fracture was significantly higher in MM patients, compared with patients without MM at all three time periods examined, and remained high over time: adjusted odds ratio (95% confidence interval) 1996-2000: 1.7 (1.3–2.3); 2001-2006: 1.3 (1.1-1.6); 2007-2011: 1.7 (1.4-2.2)). The risk of vertebral fractures was particularly higher in MM patients and also remained high over time: ORadj (95% CI) 1996-2000: 3.5 (1.4–8.6); 2001-2006: 4.0 (1.9-8.2); 2007-2011: 3.0 (1.6-5.7).
In addition, they found that the risk of any fracture was equally high in men and women MM patients, and in patients aged ≤ 65 or > 65 years.
“New treatment strategies, even if they have a positive impact on overall survival, offer no guarantee for a corresponding reduction in bone lesions,” the authors concluded.
The majority of authors reported having no disclosures. One author reported grants and personal fees from three pharmaceutical companies, outside the submitted work.
SOURCE: Oortgiesen BE et al. Bone. 2020 doi.org/10.1016/j.bone.2020.115299.
Bone lesions are one of the primary symptoms in multiple myeloma (MM), and approximately 80% of patients experience a pathological fracture at initial presentation or during the course of the disease, according to the authors of a study published online in Bone.
The authors performed a study to determine if improved treatment strategies and supportive care over time, including the use of bisphosphonates, reduced the overall fracture risk in MM patients.
Their retrospective case-control study included 1,334 patients with MM in Denmark from the Danish National Health Service, of which 881 sustained a fracture between 1996 and 2011. MM patients were matched to patients from the database without MM.
The researchers found that the risk of any fracture was significantly higher in MM patients, compared with patients without MM at all three time periods examined, and remained high over time: adjusted odds ratio (95% confidence interval) 1996-2000: 1.7 (1.3–2.3); 2001-2006: 1.3 (1.1-1.6); 2007-2011: 1.7 (1.4-2.2)). The risk of vertebral fractures was particularly higher in MM patients and also remained high over time: ORadj (95% CI) 1996-2000: 3.5 (1.4–8.6); 2001-2006: 4.0 (1.9-8.2); 2007-2011: 3.0 (1.6-5.7).
In addition, they found that the risk of any fracture was equally high in men and women MM patients, and in patients aged ≤ 65 or > 65 years.
“New treatment strategies, even if they have a positive impact on overall survival, offer no guarantee for a corresponding reduction in bone lesions,” the authors concluded.
The majority of authors reported having no disclosures. One author reported grants and personal fees from three pharmaceutical companies, outside the submitted work.
SOURCE: Oortgiesen BE et al. Bone. 2020 doi.org/10.1016/j.bone.2020.115299.
FROM BONE
NMA haploidentical allo-BMT plus post-transplant cyclophosphamide deemed safe, effective for CLL
for patients with chronic lymphocytic leukemia (CLL), according to a study published in Biology of Blood and Marrow Transplantation.
The number of patients undergoing haploidentical allo-BMT has increased substantially, with the advent of new graft-versus-host disease (GVHD) prophylaxis strategies, such as posttransplantation cyclophosphamide (PTCy), that reduce the risk of GVHD complications; however there have been few studies assessing the results of this treatment regimen, according to the authors.
The study assessed 64 consecutive patients with CLL between Jan. 2005 and Aug. 2018 who underwent haploidentical allo-BMT. The median age was 59 years; 4 patients (6.2%) underwent allo-BMT after first-line treatment; 20 patients (31.2%) underwent allo-BMT after second-line treatment, and 40 patients (62.5%) underwent allo-BMT after three or more lines of treatment for relapsed and/or refractory disease.
All patients received a nonmyeloablative (NMA) conditioning regimen consisting of fludarabine, cyclophosphamide, and 200 cGy total body irradiation. Patients received PTCy (i.v. 50 mg/kg per day) on days +3 and +4, along with additional GVHD prophylaxis with mycophenolate mofetil between days +5 and +35 and tacrolimus or sirolimus between days +5 and +180.
For all 64 patients, the median duration of follow-up was 4.4 years based on the reverse Kaplan-Meier method. The 4-year overall survival (OS) was 52%, and the 4-year progression-free survival (PFS) was 37%. The 56 patients with less than 20% marrow CLL involvement before undergoing allo-BMT had a 4-year OS of 61%, a 4-year PFS of 43%, and a median OS of 4.8 years, according to the authors.
Regression analysis demonstrated that donor age, stem cell source, IGHV mutation status, or grade II-III acute GVHD did not affect risk of progression or survival.
“The majority of our patients had unfavorable risk factors, and collectively our data show that haploidentical allo-BMT with PTCy in CLL with less than 20% marrow involvement is a safe treatment option carrying a low risk of serious GVHD and other toxicities,” the researchers concluded.
The study was supported by National Institutes of Health, National Cancer Institute grants. The authors reported that they had no disclosures.
SOURCE: Suman P et al. Biol Blood Marrow Transplant. 2020 Mar 1;26:502-8. doi: 10.1016/j.bbmt.2019.11.008
for patients with chronic lymphocytic leukemia (CLL), according to a study published in Biology of Blood and Marrow Transplantation.
The number of patients undergoing haploidentical allo-BMT has increased substantially, with the advent of new graft-versus-host disease (GVHD) prophylaxis strategies, such as posttransplantation cyclophosphamide (PTCy), that reduce the risk of GVHD complications; however there have been few studies assessing the results of this treatment regimen, according to the authors.
The study assessed 64 consecutive patients with CLL between Jan. 2005 and Aug. 2018 who underwent haploidentical allo-BMT. The median age was 59 years; 4 patients (6.2%) underwent allo-BMT after first-line treatment; 20 patients (31.2%) underwent allo-BMT after second-line treatment, and 40 patients (62.5%) underwent allo-BMT after three or more lines of treatment for relapsed and/or refractory disease.
All patients received a nonmyeloablative (NMA) conditioning regimen consisting of fludarabine, cyclophosphamide, and 200 cGy total body irradiation. Patients received PTCy (i.v. 50 mg/kg per day) on days +3 and +4, along with additional GVHD prophylaxis with mycophenolate mofetil between days +5 and +35 and tacrolimus or sirolimus between days +5 and +180.
For all 64 patients, the median duration of follow-up was 4.4 years based on the reverse Kaplan-Meier method. The 4-year overall survival (OS) was 52%, and the 4-year progression-free survival (PFS) was 37%. The 56 patients with less than 20% marrow CLL involvement before undergoing allo-BMT had a 4-year OS of 61%, a 4-year PFS of 43%, and a median OS of 4.8 years, according to the authors.
Regression analysis demonstrated that donor age, stem cell source, IGHV mutation status, or grade II-III acute GVHD did not affect risk of progression or survival.
“The majority of our patients had unfavorable risk factors, and collectively our data show that haploidentical allo-BMT with PTCy in CLL with less than 20% marrow involvement is a safe treatment option carrying a low risk of serious GVHD and other toxicities,” the researchers concluded.
The study was supported by National Institutes of Health, National Cancer Institute grants. The authors reported that they had no disclosures.
SOURCE: Suman P et al. Biol Blood Marrow Transplant. 2020 Mar 1;26:502-8. doi: 10.1016/j.bbmt.2019.11.008
for patients with chronic lymphocytic leukemia (CLL), according to a study published in Biology of Blood and Marrow Transplantation.
The number of patients undergoing haploidentical allo-BMT has increased substantially, with the advent of new graft-versus-host disease (GVHD) prophylaxis strategies, such as posttransplantation cyclophosphamide (PTCy), that reduce the risk of GVHD complications; however there have been few studies assessing the results of this treatment regimen, according to the authors.
The study assessed 64 consecutive patients with CLL between Jan. 2005 and Aug. 2018 who underwent haploidentical allo-BMT. The median age was 59 years; 4 patients (6.2%) underwent allo-BMT after first-line treatment; 20 patients (31.2%) underwent allo-BMT after second-line treatment, and 40 patients (62.5%) underwent allo-BMT after three or more lines of treatment for relapsed and/or refractory disease.
All patients received a nonmyeloablative (NMA) conditioning regimen consisting of fludarabine, cyclophosphamide, and 200 cGy total body irradiation. Patients received PTCy (i.v. 50 mg/kg per day) on days +3 and +4, along with additional GVHD prophylaxis with mycophenolate mofetil between days +5 and +35 and tacrolimus or sirolimus between days +5 and +180.
For all 64 patients, the median duration of follow-up was 4.4 years based on the reverse Kaplan-Meier method. The 4-year overall survival (OS) was 52%, and the 4-year progression-free survival (PFS) was 37%. The 56 patients with less than 20% marrow CLL involvement before undergoing allo-BMT had a 4-year OS of 61%, a 4-year PFS of 43%, and a median OS of 4.8 years, according to the authors.
Regression analysis demonstrated that donor age, stem cell source, IGHV mutation status, or grade II-III acute GVHD did not affect risk of progression or survival.
“The majority of our patients had unfavorable risk factors, and collectively our data show that haploidentical allo-BMT with PTCy in CLL with less than 20% marrow involvement is a safe treatment option carrying a low risk of serious GVHD and other toxicities,” the researchers concluded.
The study was supported by National Institutes of Health, National Cancer Institute grants. The authors reported that they had no disclosures.
SOURCE: Suman P et al. Biol Blood Marrow Transplant. 2020 Mar 1;26:502-8. doi: 10.1016/j.bbmt.2019.11.008
FROM BIOLOGY OF BLOOD AND MARROW TRANSPLANTATION