User login
Dementia costs top cancer, heart disease
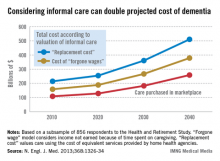
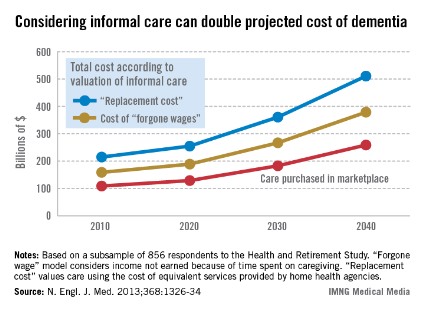
Dementia cost the United States economy between $159 billion and $215 billion in 2010, making it a greater financial burden than either cancer or heart disease, according to a study published April 3 in the New England Journal of Medicine.
With the aging of the population, that number could climb to between $379 billion and $511 billion annually by 2040, depending on how caregiver costs are estimated. Already, the direct cost of dementia care purchased in the marketplace ($109 billion) is greater than what is spent on either heart disease ($102 billion) or cancer ($77 billion).
"We’re going to see an increasing fraction of our resources devoted to this disease," said Michael D. Hurd, Ph.D., a study author and the director of the RAND Center for the Study of Aging in Santa Monica, Calif.
The investigators relied on a subset of 856 patients who had undergone a detailed in-home clinical dementia assessment as part of the Health and Retirement Study to estimate both the prevalence and cost of dementia in the United States. Dr. Hurd and his associates extrapolated the data to estimate the probability of dementia for all study respondents older than 70 years from 2000 through 2008 (N. Engl. J. Med. 2013;368:1326-34).
Estimates of the societal costs of dementia are based on the yearly per-person cost of dementia ($41,000-$56,000) and an estimated prevalence of 14.7% among Americans older than age 70.
Most of the costs associated with dementia are for home-based care or care in a long-term care facility, not for other medical services, the researchers found.
Dr. Hurd said the use of technology offers some promise for reducing those costs in the future. For example, better telemedicine might allow for lower staffing levels at long-term care facilities. And home assistance devices that could help caregivers to handle physically demanding tasks, he said.
"The role of technology could be quite important in this even if we cannot find medical advances that would delay the onset [of dementia]," he said.
The researchers presented the costs in a range to reflect the different ways to estimate the value of in-home care provided by unpaid caregivers.
Under the higher estimates, unpaid caregiver costs are calculated by determining how much it would cost to purchase comparable care from a home health agency. The lower estimates are based on the value of the caregiver’s time in the labor market. In the case of an elderly caregiver who is out of the workforce, that number would be quite low, Dr. Hurd said.
The findings also offer a message to policymakers: Invest in dementia research. "If you’re a coldhearted person who doesn’t care about the emotional side, here’s something on the economic side that you can look at and say, ‘This really is costing us a lot of money, and we ought to put some dollars into seeing what we can do about it,’ " Dr. Hurd said.
The study was supported by a grant from the National Institute on Aging (NIA). The Health and Retirement Study is conducted by the University of Michigan and is supported by grants from the NIA and the Social Security Administration.
Dementia cost the United States economy between $159 billion and $215 billion in 2010, making it a greater financial burden than either cancer or heart disease, according to a study published April 3 in the New England Journal of Medicine.
With the aging of the population, that number could climb to between $379 billion and $511 billion annually by 2040, depending on how caregiver costs are estimated. Already, the direct cost of dementia care purchased in the marketplace ($109 billion) is greater than what is spent on either heart disease ($102 billion) or cancer ($77 billion).
"We’re going to see an increasing fraction of our resources devoted to this disease," said Michael D. Hurd, Ph.D., a study author and the director of the RAND Center for the Study of Aging in Santa Monica, Calif.
The investigators relied on a subset of 856 patients who had undergone a detailed in-home clinical dementia assessment as part of the Health and Retirement Study to estimate both the prevalence and cost of dementia in the United States. Dr. Hurd and his associates extrapolated the data to estimate the probability of dementia for all study respondents older than 70 years from 2000 through 2008 (N. Engl. J. Med. 2013;368:1326-34).
Estimates of the societal costs of dementia are based on the yearly per-person cost of dementia ($41,000-$56,000) and an estimated prevalence of 14.7% among Americans older than age 70.
Most of the costs associated with dementia are for home-based care or care in a long-term care facility, not for other medical services, the researchers found.
Dr. Hurd said the use of technology offers some promise for reducing those costs in the future. For example, better telemedicine might allow for lower staffing levels at long-term care facilities. And home assistance devices that could help caregivers to handle physically demanding tasks, he said.
"The role of technology could be quite important in this even if we cannot find medical advances that would delay the onset [of dementia]," he said.
The researchers presented the costs in a range to reflect the different ways to estimate the value of in-home care provided by unpaid caregivers.
Under the higher estimates, unpaid caregiver costs are calculated by determining how much it would cost to purchase comparable care from a home health agency. The lower estimates are based on the value of the caregiver’s time in the labor market. In the case of an elderly caregiver who is out of the workforce, that number would be quite low, Dr. Hurd said.
The findings also offer a message to policymakers: Invest in dementia research. "If you’re a coldhearted person who doesn’t care about the emotional side, here’s something on the economic side that you can look at and say, ‘This really is costing us a lot of money, and we ought to put some dollars into seeing what we can do about it,’ " Dr. Hurd said.
The study was supported by a grant from the National Institute on Aging (NIA). The Health and Retirement Study is conducted by the University of Michigan and is supported by grants from the NIA and the Social Security Administration.
Dementia cost the United States economy between $159 billion and $215 billion in 2010, making it a greater financial burden than either cancer or heart disease, according to a study published April 3 in the New England Journal of Medicine.
With the aging of the population, that number could climb to between $379 billion and $511 billion annually by 2040, depending on how caregiver costs are estimated. Already, the direct cost of dementia care purchased in the marketplace ($109 billion) is greater than what is spent on either heart disease ($102 billion) or cancer ($77 billion).
"We’re going to see an increasing fraction of our resources devoted to this disease," said Michael D. Hurd, Ph.D., a study author and the director of the RAND Center for the Study of Aging in Santa Monica, Calif.
The investigators relied on a subset of 856 patients who had undergone a detailed in-home clinical dementia assessment as part of the Health and Retirement Study to estimate both the prevalence and cost of dementia in the United States. Dr. Hurd and his associates extrapolated the data to estimate the probability of dementia for all study respondents older than 70 years from 2000 through 2008 (N. Engl. J. Med. 2013;368:1326-34).
Estimates of the societal costs of dementia are based on the yearly per-person cost of dementia ($41,000-$56,000) and an estimated prevalence of 14.7% among Americans older than age 70.
Most of the costs associated with dementia are for home-based care or care in a long-term care facility, not for other medical services, the researchers found.
Dr. Hurd said the use of technology offers some promise for reducing those costs in the future. For example, better telemedicine might allow for lower staffing levels at long-term care facilities. And home assistance devices that could help caregivers to handle physically demanding tasks, he said.
"The role of technology could be quite important in this even if we cannot find medical advances that would delay the onset [of dementia]," he said.
The researchers presented the costs in a range to reflect the different ways to estimate the value of in-home care provided by unpaid caregivers.
Under the higher estimates, unpaid caregiver costs are calculated by determining how much it would cost to purchase comparable care from a home health agency. The lower estimates are based on the value of the caregiver’s time in the labor market. In the case of an elderly caregiver who is out of the workforce, that number would be quite low, Dr. Hurd said.
The findings also offer a message to policymakers: Invest in dementia research. "If you’re a coldhearted person who doesn’t care about the emotional side, here’s something on the economic side that you can look at and say, ‘This really is costing us a lot of money, and we ought to put some dollars into seeing what we can do about it,’ " Dr. Hurd said.
The study was supported by a grant from the National Institute on Aging (NIA). The Health and Retirement Study is conducted by the University of Michigan and is supported by grants from the NIA and the Social Security Administration.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major finding: The total cost of dementia to the U.S. economy ranged from $159 billion to $215 billion in 2010.
Data source: An 856-person subset of the Health and Retirement Survey.
Disclosures: The study was supported by a grant from the National Institute on Aging. The Health and Retirement Study is conducted by the University of Michigan and is supported by grants from NIA and the Social Security Administration.
Bill would waive Medicare copays for polyp removal
Legislation in Congress aims to eliminate cost sharing for Medicare beneficiaries who have polyps removed during a colonoscopy.
Under the Affordable Care Act, preventive care services – including screening colonoscopy – are covered with no copayment or coinsurance to the patients. Under Medicare, however, colonoscopies are reclassified as "therapeutic" if polyps are removed during the procedure. In that case, patients must pay coinsurance of 20% of the Medicare approved charge. Changing the Medicare policy requires action by Congress.
Sen. Ben Cardin (D-Md.) introduced S.608, the Supporting Colorectal Examination and Education Now (SCREEN) Act, in March. The bill would waive cost sharing for Medicare beneficiaries if polyps were removed during a colonoscopy. The proposed legislation also calls for notifying all Medicare beneficiaries about the screening benefit and would cover a prescreening visit under Medicare.
Rep. Richard Neal (D-Mass.) introduced companion legislation n the House (H.R. 1320).
The SCREEN Act also would give physicians a chance to earn higher payments for providing colonoscopies. The legislation would create a preventive services payment modifier for colorectal cancer screening. Under the bill, physicians could earn incentive payments by meeting national colorectal cancer screening goals and minimum standards for knowledge, training, continuing education, and documentation.
At press time, the companion bills had been referred to committee; no other action had been taken.
Legislation in Congress aims to eliminate cost sharing for Medicare beneficiaries who have polyps removed during a colonoscopy.
Under the Affordable Care Act, preventive care services – including screening colonoscopy – are covered with no copayment or coinsurance to the patients. Under Medicare, however, colonoscopies are reclassified as "therapeutic" if polyps are removed during the procedure. In that case, patients must pay coinsurance of 20% of the Medicare approved charge. Changing the Medicare policy requires action by Congress.
Sen. Ben Cardin (D-Md.) introduced S.608, the Supporting Colorectal Examination and Education Now (SCREEN) Act, in March. The bill would waive cost sharing for Medicare beneficiaries if polyps were removed during a colonoscopy. The proposed legislation also calls for notifying all Medicare beneficiaries about the screening benefit and would cover a prescreening visit under Medicare.
Rep. Richard Neal (D-Mass.) introduced companion legislation n the House (H.R. 1320).
The SCREEN Act also would give physicians a chance to earn higher payments for providing colonoscopies. The legislation would create a preventive services payment modifier for colorectal cancer screening. Under the bill, physicians could earn incentive payments by meeting national colorectal cancer screening goals and minimum standards for knowledge, training, continuing education, and documentation.
At press time, the companion bills had been referred to committee; no other action had been taken.
Legislation in Congress aims to eliminate cost sharing for Medicare beneficiaries who have polyps removed during a colonoscopy.
Under the Affordable Care Act, preventive care services – including screening colonoscopy – are covered with no copayment or coinsurance to the patients. Under Medicare, however, colonoscopies are reclassified as "therapeutic" if polyps are removed during the procedure. In that case, patients must pay coinsurance of 20% of the Medicare approved charge. Changing the Medicare policy requires action by Congress.
Sen. Ben Cardin (D-Md.) introduced S.608, the Supporting Colorectal Examination and Education Now (SCREEN) Act, in March. The bill would waive cost sharing for Medicare beneficiaries if polyps were removed during a colonoscopy. The proposed legislation also calls for notifying all Medicare beneficiaries about the screening benefit and would cover a prescreening visit under Medicare.
Rep. Richard Neal (D-Mass.) introduced companion legislation n the House (H.R. 1320).
The SCREEN Act also would give physicians a chance to earn higher payments for providing colonoscopies. The legislation would create a preventive services payment modifier for colorectal cancer screening. Under the bill, physicians could earn incentive payments by meeting national colorectal cancer screening goals and minimum standards for knowledge, training, continuing education, and documentation.
At press time, the companion bills had been referred to committee; no other action had been taken.
CancerLinQ prototype leverages 'Big Data'
The American Society of Clinical Oncology has unveiled its prototype for an ambitious computer network that allows physicians to search patient records and clinical evidence in real time.
The network, called CancerLinQ, promises to ultimately give oncologists access to millions of patient records, expert guidelines, and scientific literature all through a single computer interface.
The development of CancerLinQ comes as more oncologists are embracing health information technology. A recent ASCO survey shows that more than 60% of oncologists are using advanced electronic health records. Only 8% of the oncologists surveyed by ASCO said they aren’t using an EHR now and don’t plan to implement a system.
The prototype, which is the first major step in developing CancerLinQ, focuses on breast cancer. Through the prototype, oncologists are using their EHR systems to contribute everything from genomic data to physician notes related to their breast cancer patients. They can then search CancerLinQ’s database of about 130,000 de-identified patient records to look for trends and associations in treatment responses or patient characteristics.
The prototype also allows physicians to get individualized treatment advice based on breast cancer guidelines and to measure their performance against quality measures in ASCO’s Quality Oncology Practice Initiative (QOPI).
Once complete, the CancerLinQ system will include patients with all types of cancers.
"We’re developing a knowledge-generating computer network that will help us unlock that 97% of data that [are] currently beyond our reach," Dr. Sandra M. Swain, ASCO president, said during a demo of the CancerLinQ network on March 27.
Currently, about 3% of cancer patients participate in clinical trials, leaving the rest of the patient experience untapped for research purposes, Dr. Swain said. The development of CancerLinQ aims to bring that information directly to physicians.
For instance, if an oncologist is planning to start a patient on an aromatase inhibitor to treat a hormone-sensitive breast cancer, they might want to know how long similar patients stay on the treatment. CancerLinQ allows physicians to generate reports showing the typical treatment duration in patients with similar characteristics and to see what their outcomes were at various durations.
For individual patients and physicians, CancerLinQ will be "like having the whole medical community available for an opinion," Dr. Swain said. "It redefines what a second opinion is."
And the health care system as a whole could benefit, too. CancerLinQ has the potential to reduce fragmentation of care, decrease duplicative testing, and reduce costs, she said.
"The result will be higher-quality, higher-value care with better outcomes for patients," said Dr. Swain, who is medical director of the Washington Cancer Institute at MedStar Washington Hospital Center.
ASCO developed the prototype as a "proof of concept" that this type of "learning health system" could be developed, said Dr. Clifford A. Hudis, ASCO president-elect and an oncologist at Memorial Sloan-Kettering Cancer Center in New York. The prototype uses mostly open source software, along with some proprietary programs. But the prototype is able to import and aggregate information from a wide variety of electronic health record systems, he said.
Over the next year, ASCO officials will publish a series of white papers on their experience with the prototype. At the same time, they will continue to develop the system for an eventual rollout that will include patient data across all types of cancer. But that will be a multiyear effort, Dr. Hudis said. "This (demonstration) proves that what we want to do can be done."
Dr. W. Charles Penley, director of ASCO’s Conquer Cancer Foundation and an oncologist at a large group practice in Nashville, Tenn., has been participating in testing of the prototype. The process of linking to the prototype was fairly simple, he said. It took only about a day of work by the practice’s IT staff in to connect their EHR to the CancerLinQ system.
Lynn Etheredge, director of the Rapid Learning Project at George Washington University, Washington, and a member of the Institute of Medicine committee that proposed the concept of the "learning health care system," praised ASCO officials for their leadership in developing the CancerLinQ system and in helping to get better information into the hands of physicians.
"For the last 20 years roughly, we’ve been missing physician leadership," Mr. Etheredge said. "I want to credit ASCO with regaining leadership by physicians for what physicians and patients know needs to be the center of health policy."
CancerLinQ is supported by the Conquer Cancer Foundation, which has received funding from Susan G. Komen for the Cure, Helsinn Group, and by Genentech.
Twitter @MaryEllenNY
The American Society of Clinical Oncology has unveiled its prototype for an ambitious computer network that allows physicians to search patient records and clinical evidence in real time.
The network, called CancerLinQ, promises to ultimately give oncologists access to millions of patient records, expert guidelines, and scientific literature all through a single computer interface.
The development of CancerLinQ comes as more oncologists are embracing health information technology. A recent ASCO survey shows that more than 60% of oncologists are using advanced electronic health records. Only 8% of the oncologists surveyed by ASCO said they aren’t using an EHR now and don’t plan to implement a system.
The prototype, which is the first major step in developing CancerLinQ, focuses on breast cancer. Through the prototype, oncologists are using their EHR systems to contribute everything from genomic data to physician notes related to their breast cancer patients. They can then search CancerLinQ’s database of about 130,000 de-identified patient records to look for trends and associations in treatment responses or patient characteristics.
The prototype also allows physicians to get individualized treatment advice based on breast cancer guidelines and to measure their performance against quality measures in ASCO’s Quality Oncology Practice Initiative (QOPI).
Once complete, the CancerLinQ system will include patients with all types of cancers.
"We’re developing a knowledge-generating computer network that will help us unlock that 97% of data that [are] currently beyond our reach," Dr. Sandra M. Swain, ASCO president, said during a demo of the CancerLinQ network on March 27.
Currently, about 3% of cancer patients participate in clinical trials, leaving the rest of the patient experience untapped for research purposes, Dr. Swain said. The development of CancerLinQ aims to bring that information directly to physicians.
For instance, if an oncologist is planning to start a patient on an aromatase inhibitor to treat a hormone-sensitive breast cancer, they might want to know how long similar patients stay on the treatment. CancerLinQ allows physicians to generate reports showing the typical treatment duration in patients with similar characteristics and to see what their outcomes were at various durations.
For individual patients and physicians, CancerLinQ will be "like having the whole medical community available for an opinion," Dr. Swain said. "It redefines what a second opinion is."
And the health care system as a whole could benefit, too. CancerLinQ has the potential to reduce fragmentation of care, decrease duplicative testing, and reduce costs, she said.
"The result will be higher-quality, higher-value care with better outcomes for patients," said Dr. Swain, who is medical director of the Washington Cancer Institute at MedStar Washington Hospital Center.
ASCO developed the prototype as a "proof of concept" that this type of "learning health system" could be developed, said Dr. Clifford A. Hudis, ASCO president-elect and an oncologist at Memorial Sloan-Kettering Cancer Center in New York. The prototype uses mostly open source software, along with some proprietary programs. But the prototype is able to import and aggregate information from a wide variety of electronic health record systems, he said.
Over the next year, ASCO officials will publish a series of white papers on their experience with the prototype. At the same time, they will continue to develop the system for an eventual rollout that will include patient data across all types of cancer. But that will be a multiyear effort, Dr. Hudis said. "This (demonstration) proves that what we want to do can be done."
Dr. W. Charles Penley, director of ASCO’s Conquer Cancer Foundation and an oncologist at a large group practice in Nashville, Tenn., has been participating in testing of the prototype. The process of linking to the prototype was fairly simple, he said. It took only about a day of work by the practice’s IT staff in to connect their EHR to the CancerLinQ system.
Lynn Etheredge, director of the Rapid Learning Project at George Washington University, Washington, and a member of the Institute of Medicine committee that proposed the concept of the "learning health care system," praised ASCO officials for their leadership in developing the CancerLinQ system and in helping to get better information into the hands of physicians.
"For the last 20 years roughly, we’ve been missing physician leadership," Mr. Etheredge said. "I want to credit ASCO with regaining leadership by physicians for what physicians and patients know needs to be the center of health policy."
CancerLinQ is supported by the Conquer Cancer Foundation, which has received funding from Susan G. Komen for the Cure, Helsinn Group, and by Genentech.
Twitter @MaryEllenNY
The American Society of Clinical Oncology has unveiled its prototype for an ambitious computer network that allows physicians to search patient records and clinical evidence in real time.
The network, called CancerLinQ, promises to ultimately give oncologists access to millions of patient records, expert guidelines, and scientific literature all through a single computer interface.
The development of CancerLinQ comes as more oncologists are embracing health information technology. A recent ASCO survey shows that more than 60% of oncologists are using advanced electronic health records. Only 8% of the oncologists surveyed by ASCO said they aren’t using an EHR now and don’t plan to implement a system.
The prototype, which is the first major step in developing CancerLinQ, focuses on breast cancer. Through the prototype, oncologists are using their EHR systems to contribute everything from genomic data to physician notes related to their breast cancer patients. They can then search CancerLinQ’s database of about 130,000 de-identified patient records to look for trends and associations in treatment responses or patient characteristics.
The prototype also allows physicians to get individualized treatment advice based on breast cancer guidelines and to measure their performance against quality measures in ASCO’s Quality Oncology Practice Initiative (QOPI).
Once complete, the CancerLinQ system will include patients with all types of cancers.
"We’re developing a knowledge-generating computer network that will help us unlock that 97% of data that [are] currently beyond our reach," Dr. Sandra M. Swain, ASCO president, said during a demo of the CancerLinQ network on March 27.
Currently, about 3% of cancer patients participate in clinical trials, leaving the rest of the patient experience untapped for research purposes, Dr. Swain said. The development of CancerLinQ aims to bring that information directly to physicians.
For instance, if an oncologist is planning to start a patient on an aromatase inhibitor to treat a hormone-sensitive breast cancer, they might want to know how long similar patients stay on the treatment. CancerLinQ allows physicians to generate reports showing the typical treatment duration in patients with similar characteristics and to see what their outcomes were at various durations.
For individual patients and physicians, CancerLinQ will be "like having the whole medical community available for an opinion," Dr. Swain said. "It redefines what a second opinion is."
And the health care system as a whole could benefit, too. CancerLinQ has the potential to reduce fragmentation of care, decrease duplicative testing, and reduce costs, she said.
"The result will be higher-quality, higher-value care with better outcomes for patients," said Dr. Swain, who is medical director of the Washington Cancer Institute at MedStar Washington Hospital Center.
ASCO developed the prototype as a "proof of concept" that this type of "learning health system" could be developed, said Dr. Clifford A. Hudis, ASCO president-elect and an oncologist at Memorial Sloan-Kettering Cancer Center in New York. The prototype uses mostly open source software, along with some proprietary programs. But the prototype is able to import and aggregate information from a wide variety of electronic health record systems, he said.
Over the next year, ASCO officials will publish a series of white papers on their experience with the prototype. At the same time, they will continue to develop the system for an eventual rollout that will include patient data across all types of cancer. But that will be a multiyear effort, Dr. Hudis said. "This (demonstration) proves that what we want to do can be done."
Dr. W. Charles Penley, director of ASCO’s Conquer Cancer Foundation and an oncologist at a large group practice in Nashville, Tenn., has been participating in testing of the prototype. The process of linking to the prototype was fairly simple, he said. It took only about a day of work by the practice’s IT staff in to connect their EHR to the CancerLinQ system.
Lynn Etheredge, director of the Rapid Learning Project at George Washington University, Washington, and a member of the Institute of Medicine committee that proposed the concept of the "learning health care system," praised ASCO officials for their leadership in developing the CancerLinQ system and in helping to get better information into the hands of physicians.
"For the last 20 years roughly, we’ve been missing physician leadership," Mr. Etheredge said. "I want to credit ASCO with regaining leadership by physicians for what physicians and patients know needs to be the center of health policy."
CancerLinQ is supported by the Conquer Cancer Foundation, which has received funding from Susan G. Komen for the Cure, Helsinn Group, and by Genentech.
Twitter @MaryEllenNY
Commission proposes shifting away from fee-for-service to alternatives
The fee-for-service payment system has contributed to high health care costs and inconsistent quality of care and should be replaced with a blended payment model that includes fixed payments, according to a new report released by a panel of physicians and health care experts.
In a recently published report, the National Commission on Physician Payment Reform recommended phasing out the current fee-for-service system over 5 years in favor of bundled payments, capitation, and increased financial risk-sharing.
"We can’t control runaway medical spending without changing how doctors get paid," Dr. Bill Frist, honorary chair of the commission and former Senate majority leader, said in a statement.
"This is a bipartisan issue. We all want to get the most from our health care dollars and that requires rethinking the way we pay for health care."
But the 14-member commission predicted that fee-for-service would continue to play a large role. By the end of the decade, they called for a blended system of fee-for-service, fixed payments, and salary.
The commission also recommended eliminating the Sustainable Growth Rate (SGR) formula, which ties Medicare physician payments to changes in the gross domestic product (GDP). The Congressional Budget Office (CBO) recently estimated the price of eliminating the SGR at $138 billion over 10 years, which the commission said could be paid for by reducing the overutilization of Medicare services and cutting down on fraud.
The commission, which was convened by the Society of General Internal Medicine last March, is chaired by Dr. Steven A. Schroeder, former president of the Robert Wood Johnson Foundation.
The other members include physicians from various specialties, as well as experts in health care policy. The commission is funded in part by the Robert Wood Johnson Foundation and the California HealthCare Foundation.
Some of the commission’s other recommendations include:
• Increasing payments for evaluation and management codes, while freezing procedural diagnosis codes for 3 years.
• Eliminating higher payments for facility-based services that can be performed in lower-cost settings of care.
• Incorporating quality metrics into fee-for-service contracts.
• Using fixed payment models in areas such as the management of multiple chronic diseases and in-hospital procedures and follow-up.
• Changing the membership of the Relative Value Scale Update Committee (RUC) to make it more representative of the medical profession.
The fee-for-service payment system has contributed to high health care costs and inconsistent quality of care and should be replaced with a blended payment model that includes fixed payments, according to a new report released by a panel of physicians and health care experts.
In a recently published report, the National Commission on Physician Payment Reform recommended phasing out the current fee-for-service system over 5 years in favor of bundled payments, capitation, and increased financial risk-sharing.
"We can’t control runaway medical spending without changing how doctors get paid," Dr. Bill Frist, honorary chair of the commission and former Senate majority leader, said in a statement.
"This is a bipartisan issue. We all want to get the most from our health care dollars and that requires rethinking the way we pay for health care."
But the 14-member commission predicted that fee-for-service would continue to play a large role. By the end of the decade, they called for a blended system of fee-for-service, fixed payments, and salary.
The commission also recommended eliminating the Sustainable Growth Rate (SGR) formula, which ties Medicare physician payments to changes in the gross domestic product (GDP). The Congressional Budget Office (CBO) recently estimated the price of eliminating the SGR at $138 billion over 10 years, which the commission said could be paid for by reducing the overutilization of Medicare services and cutting down on fraud.
The commission, which was convened by the Society of General Internal Medicine last March, is chaired by Dr. Steven A. Schroeder, former president of the Robert Wood Johnson Foundation.
The other members include physicians from various specialties, as well as experts in health care policy. The commission is funded in part by the Robert Wood Johnson Foundation and the California HealthCare Foundation.
Some of the commission’s other recommendations include:
• Increasing payments for evaluation and management codes, while freezing procedural diagnosis codes for 3 years.
• Eliminating higher payments for facility-based services that can be performed in lower-cost settings of care.
• Incorporating quality metrics into fee-for-service contracts.
• Using fixed payment models in areas such as the management of multiple chronic diseases and in-hospital procedures and follow-up.
• Changing the membership of the Relative Value Scale Update Committee (RUC) to make it more representative of the medical profession.
The fee-for-service payment system has contributed to high health care costs and inconsistent quality of care and should be replaced with a blended payment model that includes fixed payments, according to a new report released by a panel of physicians and health care experts.
In a recently published report, the National Commission on Physician Payment Reform recommended phasing out the current fee-for-service system over 5 years in favor of bundled payments, capitation, and increased financial risk-sharing.
"We can’t control runaway medical spending without changing how doctors get paid," Dr. Bill Frist, honorary chair of the commission and former Senate majority leader, said in a statement.
"This is a bipartisan issue. We all want to get the most from our health care dollars and that requires rethinking the way we pay for health care."
But the 14-member commission predicted that fee-for-service would continue to play a large role. By the end of the decade, they called for a blended system of fee-for-service, fixed payments, and salary.
The commission also recommended eliminating the Sustainable Growth Rate (SGR) formula, which ties Medicare physician payments to changes in the gross domestic product (GDP). The Congressional Budget Office (CBO) recently estimated the price of eliminating the SGR at $138 billion over 10 years, which the commission said could be paid for by reducing the overutilization of Medicare services and cutting down on fraud.
The commission, which was convened by the Society of General Internal Medicine last March, is chaired by Dr. Steven A. Schroeder, former president of the Robert Wood Johnson Foundation.
The other members include physicians from various specialties, as well as experts in health care policy. The commission is funded in part by the Robert Wood Johnson Foundation and the California HealthCare Foundation.
Some of the commission’s other recommendations include:
• Increasing payments for evaluation and management codes, while freezing procedural diagnosis codes for 3 years.
• Eliminating higher payments for facility-based services that can be performed in lower-cost settings of care.
• Incorporating quality metrics into fee-for-service contracts.
• Using fixed payment models in areas such as the management of multiple chronic diseases and in-hospital procedures and follow-up.
• Changing the membership of the Relative Value Scale Update Committee (RUC) to make it more representative of the medical profession.
ACOG: Balance risks when considering early deliveries
The American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine are urging obstetricians to avoid delivering women with uncomplicated pregnancies before 39 weeks’ gestation, but also not to hesitate to perform early inductions when medically necessary.
In a set of policy statements published in Obstetrics & Gynecology in April, the two organizations laid out the best evidence for when early delivery is medically necessary and when it is not (Obstet. Gynecol. 2013;121:908-10;Obstet. Gynecol. 2013;121:911-5).
"For women who aren’t having any complications with their pregnancy, delivery at or after 39 weeks is the best thing to do," said Dr. George A. Macones, chair of the ACOG Committee on Obstetric Practice and chair of obstetrics and gynecology at Washington University in St. Louis. "But the flip side is we don’t want doctors not to deliver patients early who would benefit from that."
Over the last several years, the number of nonmedically indicated deliveries performed before 39 weeks was on the rise, prompting some patient advocates and quality experts to push for the elimination of early elective deliveries. The March of Dimes, the Joint Commission, and the Leapfrog Group have all called on physicians to do more to curb early elective deliveries to avoid adverse outcomes for neonates.
The ACOG and SMFM statement #561 echoes those concerns, noting the greater rates of morbidity and mortality for neonates and infants delivered at 37 and 38 weeks, compared with those delivered at 39 and 40 weeks’ gestation.
For instance, a retrospective cohort study that included more than 200,000 births found higher rates of respiratory failure and ventilator use for infants delivered at 37 weeks, compared with those delivered at 39 weeks, regardless of the indication for delivery. Those infants delivered at 37 weeks’ gestation also had higher rates of respiratory distress syndrome, transient tachypnea of the newborn, pneumonia, and surfactant and oscillator use, compared with infants delivered at 39 weeks (JAMA 2010;304:419-25).
Mortality rates are also significantly higher for infants delivered at 37 and 38 weeks’ gestation, compared with infants who are delivered at 39 weeks, according to the statement.
The ACOG and SMFM also cautioned obstetricians not use fetal pulmonary maturity testing to justify an early elective delivery because even though the testing may help identify a fetus at risk for respiratory distress syndrome, it may not be able to predict other adverse outcomes.
But the ACOG and SMFM also have concerns that some efforts to eliminate early deliveries may be going too far. For instance, at least one state Medicaid agency has stopped paying physicians for non-indicated deliveries before 39 weeks’ gestation, they wrote in the policy statement.
"That’s a problem," Dr. Macones said in an interview. "When insurance companies start to try to regulate medical care, that’s where we can get into some trouble."
These types of blanket payment policies, which typically rely on chart abstractions and billing codes, can overlook real medical indications for an early delivery, said Dr. Jeffrey L. Ecker, vice chair of the ACOG Committee on Obstetric Practice and a maternal-fetal medicine specialist at Massachusetts General Hospital in Boston. "There’s particular concern that good medicine sometimes doesn’t appear in documentation or in billing codes," he said in an interview.
It’s critical, Dr. Ecker said, that these policies don’t give physicians the message that they should never perform deliveries before 39 weeks.
The ACOG and the SMFM also issued a policy statement (#560) that offers general and specific recommendations on the timing of deliveries for several conditions that may require early delivery in either late-preterm (34 through 36 weeks) or early-term (37 through 38 weeks) periods. The conditions include placenta previa, prior classical cesarean, prior myomectomy, fetal growth restriction, chronic hypertension, diabetes, and preterm premature rupture of membranes (PPROM). The list is not meant to be all-inclusive, but gives physicians a sense of the most common indications for early delivery.
"We hope the list will make it easier for physicians to justify their actions to hospital leaders and insurers who may have strict policies about early deliveries," Dr. Macones said.
In a related policy statement (#559), ACOG also addressed the issue of cesarean delivery on maternal request (Obstet. Gynecol. 2013;121:904-7). The Committee on Obstetric Practice stated that physicians should recommend a vaginal delivery unless there are maternal or fetal indications for a cesarean. The committee specifically recommended against cesarean delivery on maternal request for women who plan to have several children because the risks of placenta previa, placenta accreta, and gravid hysterectomy increase with each cesarean delivery.
However, in cases were a cesarean on maternal request is planned, it should not be performed before 39 weeks, the committee wrote. In counseling patients, the ACOG committee also urged physicians not to let the decision to proceed with a cesarean be based on the patient\'s fears about managing pain during a vaginal delivery.
On Twitter @MaryEllenNY
The American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine are urging obstetricians to avoid delivering women with uncomplicated pregnancies before 39 weeks’ gestation, but also not to hesitate to perform early inductions when medically necessary.
In a set of policy statements published in Obstetrics & Gynecology in April, the two organizations laid out the best evidence for when early delivery is medically necessary and when it is not (Obstet. Gynecol. 2013;121:908-10;Obstet. Gynecol. 2013;121:911-5).
"For women who aren’t having any complications with their pregnancy, delivery at or after 39 weeks is the best thing to do," said Dr. George A. Macones, chair of the ACOG Committee on Obstetric Practice and chair of obstetrics and gynecology at Washington University in St. Louis. "But the flip side is we don’t want doctors not to deliver patients early who would benefit from that."
Over the last several years, the number of nonmedically indicated deliveries performed before 39 weeks was on the rise, prompting some patient advocates and quality experts to push for the elimination of early elective deliveries. The March of Dimes, the Joint Commission, and the Leapfrog Group have all called on physicians to do more to curb early elective deliveries to avoid adverse outcomes for neonates.
The ACOG and SMFM statement #561 echoes those concerns, noting the greater rates of morbidity and mortality for neonates and infants delivered at 37 and 38 weeks, compared with those delivered at 39 and 40 weeks’ gestation.
For instance, a retrospective cohort study that included more than 200,000 births found higher rates of respiratory failure and ventilator use for infants delivered at 37 weeks, compared with those delivered at 39 weeks, regardless of the indication for delivery. Those infants delivered at 37 weeks’ gestation also had higher rates of respiratory distress syndrome, transient tachypnea of the newborn, pneumonia, and surfactant and oscillator use, compared with infants delivered at 39 weeks (JAMA 2010;304:419-25).
Mortality rates are also significantly higher for infants delivered at 37 and 38 weeks’ gestation, compared with infants who are delivered at 39 weeks, according to the statement.
The ACOG and SMFM also cautioned obstetricians not use fetal pulmonary maturity testing to justify an early elective delivery because even though the testing may help identify a fetus at risk for respiratory distress syndrome, it may not be able to predict other adverse outcomes.
But the ACOG and SMFM also have concerns that some efforts to eliminate early deliveries may be going too far. For instance, at least one state Medicaid agency has stopped paying physicians for non-indicated deliveries before 39 weeks’ gestation, they wrote in the policy statement.
"That’s a problem," Dr. Macones said in an interview. "When insurance companies start to try to regulate medical care, that’s where we can get into some trouble."
These types of blanket payment policies, which typically rely on chart abstractions and billing codes, can overlook real medical indications for an early delivery, said Dr. Jeffrey L. Ecker, vice chair of the ACOG Committee on Obstetric Practice and a maternal-fetal medicine specialist at Massachusetts General Hospital in Boston. "There’s particular concern that good medicine sometimes doesn’t appear in documentation or in billing codes," he said in an interview.
It’s critical, Dr. Ecker said, that these policies don’t give physicians the message that they should never perform deliveries before 39 weeks.
The ACOG and the SMFM also issued a policy statement (#560) that offers general and specific recommendations on the timing of deliveries for several conditions that may require early delivery in either late-preterm (34 through 36 weeks) or early-term (37 through 38 weeks) periods. The conditions include placenta previa, prior classical cesarean, prior myomectomy, fetal growth restriction, chronic hypertension, diabetes, and preterm premature rupture of membranes (PPROM). The list is not meant to be all-inclusive, but gives physicians a sense of the most common indications for early delivery.
"We hope the list will make it easier for physicians to justify their actions to hospital leaders and insurers who may have strict policies about early deliveries," Dr. Macones said.
In a related policy statement (#559), ACOG also addressed the issue of cesarean delivery on maternal request (Obstet. Gynecol. 2013;121:904-7). The Committee on Obstetric Practice stated that physicians should recommend a vaginal delivery unless there are maternal or fetal indications for a cesarean. The committee specifically recommended against cesarean delivery on maternal request for women who plan to have several children because the risks of placenta previa, placenta accreta, and gravid hysterectomy increase with each cesarean delivery.
However, in cases were a cesarean on maternal request is planned, it should not be performed before 39 weeks, the committee wrote. In counseling patients, the ACOG committee also urged physicians not to let the decision to proceed with a cesarean be based on the patient\'s fears about managing pain during a vaginal delivery.
On Twitter @MaryEllenNY
The American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine are urging obstetricians to avoid delivering women with uncomplicated pregnancies before 39 weeks’ gestation, but also not to hesitate to perform early inductions when medically necessary.
In a set of policy statements published in Obstetrics & Gynecology in April, the two organizations laid out the best evidence for when early delivery is medically necessary and when it is not (Obstet. Gynecol. 2013;121:908-10;Obstet. Gynecol. 2013;121:911-5).
"For women who aren’t having any complications with their pregnancy, delivery at or after 39 weeks is the best thing to do," said Dr. George A. Macones, chair of the ACOG Committee on Obstetric Practice and chair of obstetrics and gynecology at Washington University in St. Louis. "But the flip side is we don’t want doctors not to deliver patients early who would benefit from that."
Over the last several years, the number of nonmedically indicated deliveries performed before 39 weeks was on the rise, prompting some patient advocates and quality experts to push for the elimination of early elective deliveries. The March of Dimes, the Joint Commission, and the Leapfrog Group have all called on physicians to do more to curb early elective deliveries to avoid adverse outcomes for neonates.
The ACOG and SMFM statement #561 echoes those concerns, noting the greater rates of morbidity and mortality for neonates and infants delivered at 37 and 38 weeks, compared with those delivered at 39 and 40 weeks’ gestation.
For instance, a retrospective cohort study that included more than 200,000 births found higher rates of respiratory failure and ventilator use for infants delivered at 37 weeks, compared with those delivered at 39 weeks, regardless of the indication for delivery. Those infants delivered at 37 weeks’ gestation also had higher rates of respiratory distress syndrome, transient tachypnea of the newborn, pneumonia, and surfactant and oscillator use, compared with infants delivered at 39 weeks (JAMA 2010;304:419-25).
Mortality rates are also significantly higher for infants delivered at 37 and 38 weeks’ gestation, compared with infants who are delivered at 39 weeks, according to the statement.
The ACOG and SMFM also cautioned obstetricians not use fetal pulmonary maturity testing to justify an early elective delivery because even though the testing may help identify a fetus at risk for respiratory distress syndrome, it may not be able to predict other adverse outcomes.
But the ACOG and SMFM also have concerns that some efforts to eliminate early deliveries may be going too far. For instance, at least one state Medicaid agency has stopped paying physicians for non-indicated deliveries before 39 weeks’ gestation, they wrote in the policy statement.
"That’s a problem," Dr. Macones said in an interview. "When insurance companies start to try to regulate medical care, that’s where we can get into some trouble."
These types of blanket payment policies, which typically rely on chart abstractions and billing codes, can overlook real medical indications for an early delivery, said Dr. Jeffrey L. Ecker, vice chair of the ACOG Committee on Obstetric Practice and a maternal-fetal medicine specialist at Massachusetts General Hospital in Boston. "There’s particular concern that good medicine sometimes doesn’t appear in documentation or in billing codes," he said in an interview.
It’s critical, Dr. Ecker said, that these policies don’t give physicians the message that they should never perform deliveries before 39 weeks.
The ACOG and the SMFM also issued a policy statement (#560) that offers general and specific recommendations on the timing of deliveries for several conditions that may require early delivery in either late-preterm (34 through 36 weeks) or early-term (37 through 38 weeks) periods. The conditions include placenta previa, prior classical cesarean, prior myomectomy, fetal growth restriction, chronic hypertension, diabetes, and preterm premature rupture of membranes (PPROM). The list is not meant to be all-inclusive, but gives physicians a sense of the most common indications for early delivery.
"We hope the list will make it easier for physicians to justify their actions to hospital leaders and insurers who may have strict policies about early deliveries," Dr. Macones said.
In a related policy statement (#559), ACOG also addressed the issue of cesarean delivery on maternal request (Obstet. Gynecol. 2013;121:904-7). The Committee on Obstetric Practice stated that physicians should recommend a vaginal delivery unless there are maternal or fetal indications for a cesarean. The committee specifically recommended against cesarean delivery on maternal request for women who plan to have several children because the risks of placenta previa, placenta accreta, and gravid hysterectomy increase with each cesarean delivery.
However, in cases were a cesarean on maternal request is planned, it should not be performed before 39 weeks, the committee wrote. In counseling patients, the ACOG committee also urged physicians not to let the decision to proceed with a cesarean be based on the patient\'s fears about managing pain during a vaginal delivery.
On Twitter @MaryEllenNY
NCQA offers medical home recognition to specialists
The National Committee for Quality Assurance has launched a new program to recognize the role of specialists in the patient-centered medical home.
The program, which launched March 25, evaluates how well specialists do in ensuring access, communication, and care coordination for their patients. The "Patient-Centered Specialty Practice Recognition" program is based on the concept of the medical home "neighbor" – first developed by the American College of Physicians – and follows the same model as the NCQA’s patient-centered medical home recognition program for primary care physicians.
Most patients see multiple physicians, so a program to help specialists see how they are doing on care coordination is essential, Margaret E. O’Kane, NCQA president, said during a press conference.
NCQA estimates that the typical primary care physician coordinates with 229 physicians across 117 different practices. And the average Medicare beneficiary sees seven physicians and fills more than 20 prescriptions each year.
"The opportunity for gaps to emerge among all those complex relationships – or for things to happen that really are in conflict with each other – obviously is great," Ms. O’Kane said.
Specialists who take on a key management role for patients, including oncologists, cardiologists, and endocrinologists would be prime candidates for the recognition, according to NCQA.
Under the program, specialists will be required to meet several standards for care coordination and information sharing:
• Track and coordinate referrals. Specialists will be required to create referral arrangements and care plans with primary care practices. They will also need to monitor the communication to make sure information is being received and that it meets the needs of all the providers.
• Provide access and communication. Specialists need to provide 24/7 access, either through in-person visits or electronically.
• Identify and coordinate care for patient populations. Specialists must track their patients over time and across clinical encounters.
• Plan and manage care. This standard includes previsit planning, creation of care plans, and medication management and reconciliation.
• Track and coordinate care. This involves tracking laboratory and radiology tests, hospitalizations, and emergency department visits.
• Measure and improve performance. This standard measures clinical quality, utilization, care coordination, and patient experience.
The program requires specialists to complete an online survey and submit documentation on their ability to meet the standards.
The NCQA offers three levels of recognition. Level 1 is awarded to practices that meet the minimum score of 25 points out of 100 and all of the "must pass" standards. Practices who score higher can qualify for higher levels of recognition. The recognition status lasts for 3 years.
Dr. John Cox, a Dallas oncologist and member of the NCQA advisory council that developed the standards, said his practice interacts with more than 500 referring physicians each year and too often does not have necessary information from other providers when they sit down to work out care plans with their patients.
"We do a terrible job of really coordinating our efforts," he said.
Dr. Cox said he and other specialists are eager for the kind of tool the NCQA is offering.
"I think a lot of specialists are somewhat thirsty for having an external yardstick by which we can measure and aspire to get our practices up to speed," he said.
NCQA officials foresee that specialists who achieve this recognition potentially could see a financial benefit. Ms. O’Kane said payers might use the NCQA recognition as the basis for offering care coordination payments to specialists as part of pay-for-performance programs.
The National Committee for Quality Assurance has launched a new program to recognize the role of specialists in the patient-centered medical home.
The program, which launched March 25, evaluates how well specialists do in ensuring access, communication, and care coordination for their patients. The "Patient-Centered Specialty Practice Recognition" program is based on the concept of the medical home "neighbor" – first developed by the American College of Physicians – and follows the same model as the NCQA’s patient-centered medical home recognition program for primary care physicians.
Most patients see multiple physicians, so a program to help specialists see how they are doing on care coordination is essential, Margaret E. O’Kane, NCQA president, said during a press conference.
NCQA estimates that the typical primary care physician coordinates with 229 physicians across 117 different practices. And the average Medicare beneficiary sees seven physicians and fills more than 20 prescriptions each year.
"The opportunity for gaps to emerge among all those complex relationships – or for things to happen that really are in conflict with each other – obviously is great," Ms. O’Kane said.
Specialists who take on a key management role for patients, including oncologists, cardiologists, and endocrinologists would be prime candidates for the recognition, according to NCQA.
Under the program, specialists will be required to meet several standards for care coordination and information sharing:
• Track and coordinate referrals. Specialists will be required to create referral arrangements and care plans with primary care practices. They will also need to monitor the communication to make sure information is being received and that it meets the needs of all the providers.
• Provide access and communication. Specialists need to provide 24/7 access, either through in-person visits or electronically.
• Identify and coordinate care for patient populations. Specialists must track their patients over time and across clinical encounters.
• Plan and manage care. This standard includes previsit planning, creation of care plans, and medication management and reconciliation.
• Track and coordinate care. This involves tracking laboratory and radiology tests, hospitalizations, and emergency department visits.
• Measure and improve performance. This standard measures clinical quality, utilization, care coordination, and patient experience.
The program requires specialists to complete an online survey and submit documentation on their ability to meet the standards.
The NCQA offers three levels of recognition. Level 1 is awarded to practices that meet the minimum score of 25 points out of 100 and all of the "must pass" standards. Practices who score higher can qualify for higher levels of recognition. The recognition status lasts for 3 years.
Dr. John Cox, a Dallas oncologist and member of the NCQA advisory council that developed the standards, said his practice interacts with more than 500 referring physicians each year and too often does not have necessary information from other providers when they sit down to work out care plans with their patients.
"We do a terrible job of really coordinating our efforts," he said.
Dr. Cox said he and other specialists are eager for the kind of tool the NCQA is offering.
"I think a lot of specialists are somewhat thirsty for having an external yardstick by which we can measure and aspire to get our practices up to speed," he said.
NCQA officials foresee that specialists who achieve this recognition potentially could see a financial benefit. Ms. O’Kane said payers might use the NCQA recognition as the basis for offering care coordination payments to specialists as part of pay-for-performance programs.
The National Committee for Quality Assurance has launched a new program to recognize the role of specialists in the patient-centered medical home.
The program, which launched March 25, evaluates how well specialists do in ensuring access, communication, and care coordination for their patients. The "Patient-Centered Specialty Practice Recognition" program is based on the concept of the medical home "neighbor" – first developed by the American College of Physicians – and follows the same model as the NCQA’s patient-centered medical home recognition program for primary care physicians.
Most patients see multiple physicians, so a program to help specialists see how they are doing on care coordination is essential, Margaret E. O’Kane, NCQA president, said during a press conference.
NCQA estimates that the typical primary care physician coordinates with 229 physicians across 117 different practices. And the average Medicare beneficiary sees seven physicians and fills more than 20 prescriptions each year.
"The opportunity for gaps to emerge among all those complex relationships – or for things to happen that really are in conflict with each other – obviously is great," Ms. O’Kane said.
Specialists who take on a key management role for patients, including oncologists, cardiologists, and endocrinologists would be prime candidates for the recognition, according to NCQA.
Under the program, specialists will be required to meet several standards for care coordination and information sharing:
• Track and coordinate referrals. Specialists will be required to create referral arrangements and care plans with primary care practices. They will also need to monitor the communication to make sure information is being received and that it meets the needs of all the providers.
• Provide access and communication. Specialists need to provide 24/7 access, either through in-person visits or electronically.
• Identify and coordinate care for patient populations. Specialists must track their patients over time and across clinical encounters.
• Plan and manage care. This standard includes previsit planning, creation of care plans, and medication management and reconciliation.
• Track and coordinate care. This involves tracking laboratory and radiology tests, hospitalizations, and emergency department visits.
• Measure and improve performance. This standard measures clinical quality, utilization, care coordination, and patient experience.
The program requires specialists to complete an online survey and submit documentation on their ability to meet the standards.
The NCQA offers three levels of recognition. Level 1 is awarded to practices that meet the minimum score of 25 points out of 100 and all of the "must pass" standards. Practices who score higher can qualify for higher levels of recognition. The recognition status lasts for 3 years.
Dr. John Cox, a Dallas oncologist and member of the NCQA advisory council that developed the standards, said his practice interacts with more than 500 referring physicians each year and too often does not have necessary information from other providers when they sit down to work out care plans with their patients.
"We do a terrible job of really coordinating our efforts," he said.
Dr. Cox said he and other specialists are eager for the kind of tool the NCQA is offering.
"I think a lot of specialists are somewhat thirsty for having an external yardstick by which we can measure and aspire to get our practices up to speed," he said.
NCQA officials foresee that specialists who achieve this recognition potentially could see a financial benefit. Ms. O’Kane said payers might use the NCQA recognition as the basis for offering care coordination payments to specialists as part of pay-for-performance programs.
Seven-question tool aims to prevent readmissions
Seven data points may help predict which discharged patients are at risk for readmission in the next 30 days – critical information now that Medicare penalizes hospitals with excess readmissions.
The HOSPITAL score assesses factors that independently contribute to readmission: hemoglobin at discharge; discharge from an oncology service; sodium level at discharge; procedures employed during index admission; type of index admission; number of admissions in the last 12 months; and length of stay.
The tool scores risk on a 0-13 scale. Patients who score 0-4 points are considered at low risk for a readmission, those with scores of 5-6 are at intermediate risk, and those with scores of 7 or more are considered high risk, according to a study published March 25 in JAMA Internal Medicine (2013 [doi:10.1001/jamainternmed.2013.3023]).
"The use of this simple score before discharge may help target transitional care for patients who might benefit the most and consequently reduce the rate of avoidable readmission," wrote the researchers from Brigham and Women’s Hospital in Boston and the Bern (Switzerland) University Hospital.
The tool does not include functional status, health literacy, degree of social support, or previous medication adherence – all of which are predictors of potentially avoidable readmission, the researchers wrote. They said that they chose not to include these data points because they are infrequently measured and difficult to obtain.
"The study’s goal was to derive a model that could be easily and widely used," they wrote.
To develop the tool, the researchers performed a retrospective cohort study of consecutive adult patient discharges from all of the medical services at the Brigham and Women’s Hospital between July 1, 2009, and June 30, 2010. They compared patients with a potentially avoidable readmission to those who were not readmitted at 30 days. They excluded unavoidable readmissions, such as planned readmissions for any reason, and readmissions for newly developed, unrelated conditions.
Two-thirds of the admissions were randomized into a derivation set (6,141) and one-third was included in a validation set (3,071). The validation set showed good calibration. The Hosmer-Lemeshow goodness-of-fit statistics were P = .28 and P = .15 in the derivation and validation sets, respectively. Nonsignificant P values on the test indicate a "good fit."
The discriminatory power of the HOSPITAL score was considered fair, with a cross-validated C statistic of 0.69 in the derivation set and 0.71 in the validation set.
For instance, in the derivation set, 18.7% of admissions were observed to be at high risk for readmission, compared with 18.3% estimated by the HOSPITAL score. Similar results were found in the validation set. The proportion of admissions at high-risk for return in 30 days was 18.2%, compared to 18.0% estimated by the HOSPITAL score.
The study was supported in part by grants from the Swiss Science National Foundation and the SICPA Foundation.
Seven data points may help predict which discharged patients are at risk for readmission in the next 30 days – critical information now that Medicare penalizes hospitals with excess readmissions.
The HOSPITAL score assesses factors that independently contribute to readmission: hemoglobin at discharge; discharge from an oncology service; sodium level at discharge; procedures employed during index admission; type of index admission; number of admissions in the last 12 months; and length of stay.
The tool scores risk on a 0-13 scale. Patients who score 0-4 points are considered at low risk for a readmission, those with scores of 5-6 are at intermediate risk, and those with scores of 7 or more are considered high risk, according to a study published March 25 in JAMA Internal Medicine (2013 [doi:10.1001/jamainternmed.2013.3023]).
"The use of this simple score before discharge may help target transitional care for patients who might benefit the most and consequently reduce the rate of avoidable readmission," wrote the researchers from Brigham and Women’s Hospital in Boston and the Bern (Switzerland) University Hospital.
The tool does not include functional status, health literacy, degree of social support, or previous medication adherence – all of which are predictors of potentially avoidable readmission, the researchers wrote. They said that they chose not to include these data points because they are infrequently measured and difficult to obtain.
"The study’s goal was to derive a model that could be easily and widely used," they wrote.
To develop the tool, the researchers performed a retrospective cohort study of consecutive adult patient discharges from all of the medical services at the Brigham and Women’s Hospital between July 1, 2009, and June 30, 2010. They compared patients with a potentially avoidable readmission to those who were not readmitted at 30 days. They excluded unavoidable readmissions, such as planned readmissions for any reason, and readmissions for newly developed, unrelated conditions.
Two-thirds of the admissions were randomized into a derivation set (6,141) and one-third was included in a validation set (3,071). The validation set showed good calibration. The Hosmer-Lemeshow goodness-of-fit statistics were P = .28 and P = .15 in the derivation and validation sets, respectively. Nonsignificant P values on the test indicate a "good fit."
The discriminatory power of the HOSPITAL score was considered fair, with a cross-validated C statistic of 0.69 in the derivation set and 0.71 in the validation set.
For instance, in the derivation set, 18.7% of admissions were observed to be at high risk for readmission, compared with 18.3% estimated by the HOSPITAL score. Similar results were found in the validation set. The proportion of admissions at high-risk for return in 30 days was 18.2%, compared to 18.0% estimated by the HOSPITAL score.
The study was supported in part by grants from the Swiss Science National Foundation and the SICPA Foundation.
Seven data points may help predict which discharged patients are at risk for readmission in the next 30 days – critical information now that Medicare penalizes hospitals with excess readmissions.
The HOSPITAL score assesses factors that independently contribute to readmission: hemoglobin at discharge; discharge from an oncology service; sodium level at discharge; procedures employed during index admission; type of index admission; number of admissions in the last 12 months; and length of stay.
The tool scores risk on a 0-13 scale. Patients who score 0-4 points are considered at low risk for a readmission, those with scores of 5-6 are at intermediate risk, and those with scores of 7 or more are considered high risk, according to a study published March 25 in JAMA Internal Medicine (2013 [doi:10.1001/jamainternmed.2013.3023]).
"The use of this simple score before discharge may help target transitional care for patients who might benefit the most and consequently reduce the rate of avoidable readmission," wrote the researchers from Brigham and Women’s Hospital in Boston and the Bern (Switzerland) University Hospital.
The tool does not include functional status, health literacy, degree of social support, or previous medication adherence – all of which are predictors of potentially avoidable readmission, the researchers wrote. They said that they chose not to include these data points because they are infrequently measured and difficult to obtain.
"The study’s goal was to derive a model that could be easily and widely used," they wrote.
To develop the tool, the researchers performed a retrospective cohort study of consecutive adult patient discharges from all of the medical services at the Brigham and Women’s Hospital between July 1, 2009, and June 30, 2010. They compared patients with a potentially avoidable readmission to those who were not readmitted at 30 days. They excluded unavoidable readmissions, such as planned readmissions for any reason, and readmissions for newly developed, unrelated conditions.
Two-thirds of the admissions were randomized into a derivation set (6,141) and one-third was included in a validation set (3,071). The validation set showed good calibration. The Hosmer-Lemeshow goodness-of-fit statistics were P = .28 and P = .15 in the derivation and validation sets, respectively. Nonsignificant P values on the test indicate a "good fit."
The discriminatory power of the HOSPITAL score was considered fair, with a cross-validated C statistic of 0.69 in the derivation set and 0.71 in the validation set.
For instance, in the derivation set, 18.7% of admissions were observed to be at high risk for readmission, compared with 18.3% estimated by the HOSPITAL score. Similar results were found in the validation set. The proportion of admissions at high-risk for return in 30 days was 18.2%, compared to 18.0% estimated by the HOSPITAL score.
The study was supported in part by grants from the Swiss Science National Foundation and the SICPA Foundation.
FROM JAMA INTERNAL MEDICINE
Major finding: The HOSPITAL score had fair discriminatory power with a cross-validated C statistic of 0.69 in the derivation set and 0.71 in the validation set. The score had good calibration with Hosmer-Lemeshow goodness-of-fit statistics of P = .28 in the derivation set and P = .15 in the validation set.
Data source: Retrospective cohort study of 9,212 hospital admissions.
Disclosures: The study was supported in part by grants from the Swiss Science National Foundation and the SICPA Foundation.
Match Day- Surgery remains most popular, primary care rising
Surgery residencies are still the top choice for U.S. medical students, but the number choosing primary care continues to rise.
The 2013 Match Day results show that dermatology, emergency medicine, medicine-pediatrics, neurological surgery, orthopedic surgery, otolaryngology, radiation oncology, general surgery, and plastic surgery are the top choices for medical students. Residency programs in these specialties filled at least 80% of their positions with U.S. seniors.
Nearly 400 more U.S. medical students chose primary care residencies in this year’s Main Residency Match than did in 2012, according to data from the National Resident Matching Program.
The number of U.S. medical students choosing residency positions in internal medicine, family medicine, and pediatrics all rose in 2013, with internal medicine getting the biggest boost. The number of U.S. seniors matching to internal medicine rose by 194, while pediatric matches with U.S. seniors increased by 105 and family medicine rose by 33.
The results point to an increased interest in primary care that has been percolating over the last few years.
Mona M. Signer, executive director of the National Resident Matching Program (NRMP), said the 2010 Affordable Care Act may be driving some of the interest.
"There is a lot of talk about the fact that the Affordable Care Act is going to create demand for more physicians, in particular more primary care physicians. Perhaps that is finally starting to resonate with U.S. seniors," Ms. Signer said in an interview.
With the Match program becoming more competitive, medical school seniors may also be getting more realistic about their matching chances. Ms. Signer said the NRMP produces a report called "Charting Outcomes in the Match" (2011 data) that shows the test scores, the number of research publications, and other characteristics of previous successful candidates for each specialty. Applicants and their medical school advisors are looking at the online report, she said, and getting savvier about the specialties in which they are most likely to be competitive.
In internal medicine, 6,277 positions were offered this year, an increase of 1,000 over 2012. Of those, 99.4% were filled, with 49.9% taken by U.S. medical graduates.
In 2013, 3,037 family medicine residency positions were offered. Of those, 95.9% were filled, with 44.6% filled by U.S. medical graduates.
In pediatrics, 99.6% of the total 2,616 positions offered were filled. U.S. medical graduates filled 70.2% of the pediatric positions.
Though the match rate for U.S. graduates stayed about the same in pediatrics this year as in 2012, it was down somewhat in internal medicine and family medicine. The reason, Ms. Signer said, is that there were just so many more positions offered in those specialties than in previous years.
This year marked the first Match held under the NRMP’s new "all-in" policy, which requires programs participating in the Match to register and attempt to fill all of their available positions within the Match. Previously, some programs had offered positions outside of the Match process and the NRMP board of directors concluded that the practice placed too much pressure on students to accept these positions rather than to take their chances in the Match. The practice of offering positions outside the Match primarily affected osteopathic students, prior-year graduates of U.S. allopathic schools, and international medical graduates, Ms. Signer said.
As a result of the all-in policy, there were 1,000 more internal medicine positions in the Match, 297 more family medicine positions, and 141 positions in pediatrics, according to NRMP.
Surgery residencies are still the top choice for U.S. medical students, but the number choosing primary care continues to rise.
The 2013 Match Day results show that dermatology, emergency medicine, medicine-pediatrics, neurological surgery, orthopedic surgery, otolaryngology, radiation oncology, general surgery, and plastic surgery are the top choices for medical students. Residency programs in these specialties filled at least 80% of their positions with U.S. seniors.
Nearly 400 more U.S. medical students chose primary care residencies in this year’s Main Residency Match than did in 2012, according to data from the National Resident Matching Program.
The number of U.S. medical students choosing residency positions in internal medicine, family medicine, and pediatrics all rose in 2013, with internal medicine getting the biggest boost. The number of U.S. seniors matching to internal medicine rose by 194, while pediatric matches with U.S. seniors increased by 105 and family medicine rose by 33.
The results point to an increased interest in primary care that has been percolating over the last few years.
Mona M. Signer, executive director of the National Resident Matching Program (NRMP), said the 2010 Affordable Care Act may be driving some of the interest.
"There is a lot of talk about the fact that the Affordable Care Act is going to create demand for more physicians, in particular more primary care physicians. Perhaps that is finally starting to resonate with U.S. seniors," Ms. Signer said in an interview.
With the Match program becoming more competitive, medical school seniors may also be getting more realistic about their matching chances. Ms. Signer said the NRMP produces a report called "Charting Outcomes in the Match" (2011 data) that shows the test scores, the number of research publications, and other characteristics of previous successful candidates for each specialty. Applicants and their medical school advisors are looking at the online report, she said, and getting savvier about the specialties in which they are most likely to be competitive.
In internal medicine, 6,277 positions were offered this year, an increase of 1,000 over 2012. Of those, 99.4% were filled, with 49.9% taken by U.S. medical graduates.
In 2013, 3,037 family medicine residency positions were offered. Of those, 95.9% were filled, with 44.6% filled by U.S. medical graduates.
In pediatrics, 99.6% of the total 2,616 positions offered were filled. U.S. medical graduates filled 70.2% of the pediatric positions.
Though the match rate for U.S. graduates stayed about the same in pediatrics this year as in 2012, it was down somewhat in internal medicine and family medicine. The reason, Ms. Signer said, is that there were just so many more positions offered in those specialties than in previous years.
This year marked the first Match held under the NRMP’s new "all-in" policy, which requires programs participating in the Match to register and attempt to fill all of their available positions within the Match. Previously, some programs had offered positions outside of the Match process and the NRMP board of directors concluded that the practice placed too much pressure on students to accept these positions rather than to take their chances in the Match. The practice of offering positions outside the Match primarily affected osteopathic students, prior-year graduates of U.S. allopathic schools, and international medical graduates, Ms. Signer said.
As a result of the all-in policy, there were 1,000 more internal medicine positions in the Match, 297 more family medicine positions, and 141 positions in pediatrics, according to NRMP.
Surgery residencies are still the top choice for U.S. medical students, but the number choosing primary care continues to rise.
The 2013 Match Day results show that dermatology, emergency medicine, medicine-pediatrics, neurological surgery, orthopedic surgery, otolaryngology, radiation oncology, general surgery, and plastic surgery are the top choices for medical students. Residency programs in these specialties filled at least 80% of their positions with U.S. seniors.
Nearly 400 more U.S. medical students chose primary care residencies in this year’s Main Residency Match than did in 2012, according to data from the National Resident Matching Program.
The number of U.S. medical students choosing residency positions in internal medicine, family medicine, and pediatrics all rose in 2013, with internal medicine getting the biggest boost. The number of U.S. seniors matching to internal medicine rose by 194, while pediatric matches with U.S. seniors increased by 105 and family medicine rose by 33.
The results point to an increased interest in primary care that has been percolating over the last few years.
Mona M. Signer, executive director of the National Resident Matching Program (NRMP), said the 2010 Affordable Care Act may be driving some of the interest.
"There is a lot of talk about the fact that the Affordable Care Act is going to create demand for more physicians, in particular more primary care physicians. Perhaps that is finally starting to resonate with U.S. seniors," Ms. Signer said in an interview.
With the Match program becoming more competitive, medical school seniors may also be getting more realistic about their matching chances. Ms. Signer said the NRMP produces a report called "Charting Outcomes in the Match" (2011 data) that shows the test scores, the number of research publications, and other characteristics of previous successful candidates for each specialty. Applicants and their medical school advisors are looking at the online report, she said, and getting savvier about the specialties in which they are most likely to be competitive.
In internal medicine, 6,277 positions were offered this year, an increase of 1,000 over 2012. Of those, 99.4% were filled, with 49.9% taken by U.S. medical graduates.
In 2013, 3,037 family medicine residency positions were offered. Of those, 95.9% were filled, with 44.6% filled by U.S. medical graduates.
In pediatrics, 99.6% of the total 2,616 positions offered were filled. U.S. medical graduates filled 70.2% of the pediatric positions.
Though the match rate for U.S. graduates stayed about the same in pediatrics this year as in 2012, it was down somewhat in internal medicine and family medicine. The reason, Ms. Signer said, is that there were just so many more positions offered in those specialties than in previous years.
This year marked the first Match held under the NRMP’s new "all-in" policy, which requires programs participating in the Match to register and attempt to fill all of their available positions within the Match. Previously, some programs had offered positions outside of the Match process and the NRMP board of directors concluded that the practice placed too much pressure on students to accept these positions rather than to take their chances in the Match. The practice of offering positions outside the Match primarily affected osteopathic students, prior-year graduates of U.S. allopathic schools, and international medical graduates, Ms. Signer said.
As a result of the all-in policy, there were 1,000 more internal medicine positions in the Match, 297 more family medicine positions, and 141 positions in pediatrics, according to NRMP.
Autism reports on the rise
The prevalence of autism spectrum disorder among school-age children rose from about 1.2% to 2% over the last 5 years, the Centers for Disease Control and Prevention has reported.
Reports from parents revealed that among children aged 6-17 years, a diagnosis of autism spectrum disorder (ASD) occurred in about 1 in 86 children in 2007. By 2011-2012, parents reported ASD diagnoses for 1 in 50 children in that age group. The results are based on new data from the 2011-2012 National Survey of Children’s Health.
But the increase in prevalence is likely because of an increased awareness of ASD and better diagnosis by physicians, the CDC researchers wrote, rather than a "true" increase. The researchers reached that conclusion in part based on the number of new diagnoses occurring in older children.
"Changes in the ascertainment of ASD could occur because of changes in ASD awareness among parents or health care professionals, increased access to diagnostic services, changes in how screening tests or diagnostic criteria are used, or increased special education placements in the community," they wrote.
The researchers found statistically significant increases in the prevalence of ASD for all age groups and for boys. There was a small increase in ASD prevalence among girls, but it was not statistically significant. During 2011-2012, boys were more than four times as likely as girls aged 6-17 years to have a diagnosis of ASD.
The analysis also examined the severity of ASD diagnoses. Children who were diagnosed in 2008 or later were less likely to have a severe form of ASD. Only about 7% of the new diagnoses were for severe ASD, compared to nearly 17% for children diagnosed in 2007 or earlier.
The prevalence of autism spectrum disorder among school-age children rose from about 1.2% to 2% over the last 5 years, the Centers for Disease Control and Prevention has reported.
Reports from parents revealed that among children aged 6-17 years, a diagnosis of autism spectrum disorder (ASD) occurred in about 1 in 86 children in 2007. By 2011-2012, parents reported ASD diagnoses for 1 in 50 children in that age group. The results are based on new data from the 2011-2012 National Survey of Children’s Health.
But the increase in prevalence is likely because of an increased awareness of ASD and better diagnosis by physicians, the CDC researchers wrote, rather than a "true" increase. The researchers reached that conclusion in part based on the number of new diagnoses occurring in older children.
"Changes in the ascertainment of ASD could occur because of changes in ASD awareness among parents or health care professionals, increased access to diagnostic services, changes in how screening tests or diagnostic criteria are used, or increased special education placements in the community," they wrote.
The researchers found statistically significant increases in the prevalence of ASD for all age groups and for boys. There was a small increase in ASD prevalence among girls, but it was not statistically significant. During 2011-2012, boys were more than four times as likely as girls aged 6-17 years to have a diagnosis of ASD.
The analysis also examined the severity of ASD diagnoses. Children who were diagnosed in 2008 or later were less likely to have a severe form of ASD. Only about 7% of the new diagnoses were for severe ASD, compared to nearly 17% for children diagnosed in 2007 or earlier.
The prevalence of autism spectrum disorder among school-age children rose from about 1.2% to 2% over the last 5 years, the Centers for Disease Control and Prevention has reported.
Reports from parents revealed that among children aged 6-17 years, a diagnosis of autism spectrum disorder (ASD) occurred in about 1 in 86 children in 2007. By 2011-2012, parents reported ASD diagnoses for 1 in 50 children in that age group. The results are based on new data from the 2011-2012 National Survey of Children’s Health.
But the increase in prevalence is likely because of an increased awareness of ASD and better diagnosis by physicians, the CDC researchers wrote, rather than a "true" increase. The researchers reached that conclusion in part based on the number of new diagnoses occurring in older children.
"Changes in the ascertainment of ASD could occur because of changes in ASD awareness among parents or health care professionals, increased access to diagnostic services, changes in how screening tests or diagnostic criteria are used, or increased special education placements in the community," they wrote.
The researchers found statistically significant increases in the prevalence of ASD for all age groups and for boys. There was a small increase in ASD prevalence among girls, but it was not statistically significant. During 2011-2012, boys were more than four times as likely as girls aged 6-17 years to have a diagnosis of ASD.
The analysis also examined the severity of ASD diagnoses. Children who were diagnosed in 2008 or later were less likely to have a severe form of ASD. Only about 7% of the new diagnoses were for severe ASD, compared to nearly 17% for children diagnosed in 2007 or earlier.
AAP supports same-sex marriage
The American Academy of Pediatrics has come out in support of full marriage rights for same-sex couples and is urging the Supreme Court to declare the federal Defense of Marriage Act unconstitutional.
In a new policy statement issued March 21, the largest organization of U.S. pediatricians said that it supports marriage equality for all couples, regardless of gender or sexual orientation, as a way to guarantee the long-term social and economic security of children.
The policy also declares AAP support for adoption by single gay and lesbian parents and same-sex couples, as well as for gay and lesbian foster parents. The policy statement, issued by the AAP’s Committee on Psychosocial Aspects of Child and Family Health, will be published in the April issue of Pediatrics (2013;131:827-30 [doi: 10.1542/peds.2013-0376]). A technical report detailing the scientific literature that influenced its policy accompanies the statement (Pediatrics 2013;131:e1374-83 [doi: 10.1542/peds.2013-0377]).
The AAP announced its position just days before the Supreme Court is scheduled to hear oral arguments in two landmark same-sex marriage cases. On March 26, the high court will take up Hollingsworth v. Perry, a challenge to California’s Proposition 8 ban on gay marriage. The next day, the justices will hear U.S. v. Windsor, which challenges the constitutionality of the 1996 Defense of Marriage Act (DOMA).
"I hope that policymakers recognize the needs of children, the health and well-being of children, and the emotional-social development of children," said Dr. Benjamin Siegel, a coauthor of the policy statement and a professor of pediatrics and psychiatry at Boston University. "Families need to be supported to raise their kids, and families ought to be treated equally."
The AAP criticized the DOMA for denying equal access to federal support and legal recognition to children raised in same-sex households. Under that law, same-sex couples – even those legally married under state law – can’t access Social Security disability benefits, housing and food stamp benefits, and military service benefits. Same-sex couples also can’t file joint income tax returns and take advantage of child and dependent care tax credits – benefits that create greater financial security for children, according to the AAP policy.
"Many families [in Massachusetts] are happily married, raising kids, and not getting the same supports from the federal government, both legal and financial, that other married people just have by virtue of their sexual orientation," Dr. Siegel said.
The inability of same-sex couples to marry in most states also means that there are not legal avenues for child custody and financial support in the event of a breakup.
"If you don’t have marriage, you don’t have divorce," said Dr. Ellen C. Perrin, a coauthor of the policy and director of research for the Center for Children with Special Needs at the Floating Hospital for Children at Tufts Medical Center in Boston.
The AAP has supported parenting rights for same-sex couples for more than a decade. In 2002, the AAP issued a policy supporting second-parent and coparent adoption by gay and lesbian parents (Pediatrics 2002;109:339-40). The policy was reaffirmed in 2010. And in 2006, the academy issued a report showing that civil unions and domestic partnerships fall short in terms of providing the legal rights, protections, and benefits to children that are offered by civil marriage (Pediatrics 2006;118:349-64). It was after the release of the 2006 report that AAP leaders began examining the evidence in order to create the new policy, Dr. Perrin said.
The new policy is informed by a large body of scientific research from the last 30 years, according to the academy. Overall, the research shows that children who are raised by same-sex parents fare as well as the children of heterosexual parents in terms of emotional, cognitive, social, and sexual functioning. The adjustment of children has much more to do with the quality of the relationships between children and parents and the availability of economic and socioeconomic resources, according to the AAP.
"We believe that is now pretty well clinched, given how much research has happened and how similar the results are," Dr. Perrin said. "There are many other phenomena in children’s lives that are much more problematic or worrisome than what the gender or sexual orientation of their parents is."
On Twitter @MaryEllenNY
The American Academy of Pediatrics has come out in support of full marriage rights for same-sex couples and is urging the Supreme Court to declare the federal Defense of Marriage Act unconstitutional.
In a new policy statement issued March 21, the largest organization of U.S. pediatricians said that it supports marriage equality for all couples, regardless of gender or sexual orientation, as a way to guarantee the long-term social and economic security of children.
The policy also declares AAP support for adoption by single gay and lesbian parents and same-sex couples, as well as for gay and lesbian foster parents. The policy statement, issued by the AAP’s Committee on Psychosocial Aspects of Child and Family Health, will be published in the April issue of Pediatrics (2013;131:827-30 [doi: 10.1542/peds.2013-0376]). A technical report detailing the scientific literature that influenced its policy accompanies the statement (Pediatrics 2013;131:e1374-83 [doi: 10.1542/peds.2013-0377]).
The AAP announced its position just days before the Supreme Court is scheduled to hear oral arguments in two landmark same-sex marriage cases. On March 26, the high court will take up Hollingsworth v. Perry, a challenge to California’s Proposition 8 ban on gay marriage. The next day, the justices will hear U.S. v. Windsor, which challenges the constitutionality of the 1996 Defense of Marriage Act (DOMA).
"I hope that policymakers recognize the needs of children, the health and well-being of children, and the emotional-social development of children," said Dr. Benjamin Siegel, a coauthor of the policy statement and a professor of pediatrics and psychiatry at Boston University. "Families need to be supported to raise their kids, and families ought to be treated equally."
The AAP criticized the DOMA for denying equal access to federal support and legal recognition to children raised in same-sex households. Under that law, same-sex couples – even those legally married under state law – can’t access Social Security disability benefits, housing and food stamp benefits, and military service benefits. Same-sex couples also can’t file joint income tax returns and take advantage of child and dependent care tax credits – benefits that create greater financial security for children, according to the AAP policy.
"Many families [in Massachusetts] are happily married, raising kids, and not getting the same supports from the federal government, both legal and financial, that other married people just have by virtue of their sexual orientation," Dr. Siegel said.
The inability of same-sex couples to marry in most states also means that there are not legal avenues for child custody and financial support in the event of a breakup.
"If you don’t have marriage, you don’t have divorce," said Dr. Ellen C. Perrin, a coauthor of the policy and director of research for the Center for Children with Special Needs at the Floating Hospital for Children at Tufts Medical Center in Boston.
The AAP has supported parenting rights for same-sex couples for more than a decade. In 2002, the AAP issued a policy supporting second-parent and coparent adoption by gay and lesbian parents (Pediatrics 2002;109:339-40). The policy was reaffirmed in 2010. And in 2006, the academy issued a report showing that civil unions and domestic partnerships fall short in terms of providing the legal rights, protections, and benefits to children that are offered by civil marriage (Pediatrics 2006;118:349-64). It was after the release of the 2006 report that AAP leaders began examining the evidence in order to create the new policy, Dr. Perrin said.
The new policy is informed by a large body of scientific research from the last 30 years, according to the academy. Overall, the research shows that children who are raised by same-sex parents fare as well as the children of heterosexual parents in terms of emotional, cognitive, social, and sexual functioning. The adjustment of children has much more to do with the quality of the relationships between children and parents and the availability of economic and socioeconomic resources, according to the AAP.
"We believe that is now pretty well clinched, given how much research has happened and how similar the results are," Dr. Perrin said. "There are many other phenomena in children’s lives that are much more problematic or worrisome than what the gender or sexual orientation of their parents is."
On Twitter @MaryEllenNY
The American Academy of Pediatrics has come out in support of full marriage rights for same-sex couples and is urging the Supreme Court to declare the federal Defense of Marriage Act unconstitutional.
In a new policy statement issued March 21, the largest organization of U.S. pediatricians said that it supports marriage equality for all couples, regardless of gender or sexual orientation, as a way to guarantee the long-term social and economic security of children.
The policy also declares AAP support for adoption by single gay and lesbian parents and same-sex couples, as well as for gay and lesbian foster parents. The policy statement, issued by the AAP’s Committee on Psychosocial Aspects of Child and Family Health, will be published in the April issue of Pediatrics (2013;131:827-30 [doi: 10.1542/peds.2013-0376]). A technical report detailing the scientific literature that influenced its policy accompanies the statement (Pediatrics 2013;131:e1374-83 [doi: 10.1542/peds.2013-0377]).
The AAP announced its position just days before the Supreme Court is scheduled to hear oral arguments in two landmark same-sex marriage cases. On March 26, the high court will take up Hollingsworth v. Perry, a challenge to California’s Proposition 8 ban on gay marriage. The next day, the justices will hear U.S. v. Windsor, which challenges the constitutionality of the 1996 Defense of Marriage Act (DOMA).
"I hope that policymakers recognize the needs of children, the health and well-being of children, and the emotional-social development of children," said Dr. Benjamin Siegel, a coauthor of the policy statement and a professor of pediatrics and psychiatry at Boston University. "Families need to be supported to raise their kids, and families ought to be treated equally."
The AAP criticized the DOMA for denying equal access to federal support and legal recognition to children raised in same-sex households. Under that law, same-sex couples – even those legally married under state law – can’t access Social Security disability benefits, housing and food stamp benefits, and military service benefits. Same-sex couples also can’t file joint income tax returns and take advantage of child and dependent care tax credits – benefits that create greater financial security for children, according to the AAP policy.
"Many families [in Massachusetts] are happily married, raising kids, and not getting the same supports from the federal government, both legal and financial, that other married people just have by virtue of their sexual orientation," Dr. Siegel said.
The inability of same-sex couples to marry in most states also means that there are not legal avenues for child custody and financial support in the event of a breakup.
"If you don’t have marriage, you don’t have divorce," said Dr. Ellen C. Perrin, a coauthor of the policy and director of research for the Center for Children with Special Needs at the Floating Hospital for Children at Tufts Medical Center in Boston.
The AAP has supported parenting rights for same-sex couples for more than a decade. In 2002, the AAP issued a policy supporting second-parent and coparent adoption by gay and lesbian parents (Pediatrics 2002;109:339-40). The policy was reaffirmed in 2010. And in 2006, the academy issued a report showing that civil unions and domestic partnerships fall short in terms of providing the legal rights, protections, and benefits to children that are offered by civil marriage (Pediatrics 2006;118:349-64). It was after the release of the 2006 report that AAP leaders began examining the evidence in order to create the new policy, Dr. Perrin said.
The new policy is informed by a large body of scientific research from the last 30 years, according to the academy. Overall, the research shows that children who are raised by same-sex parents fare as well as the children of heterosexual parents in terms of emotional, cognitive, social, and sexual functioning. The adjustment of children has much more to do with the quality of the relationships between children and parents and the availability of economic and socioeconomic resources, according to the AAP.
"We believe that is now pretty well clinched, given how much research has happened and how similar the results are," Dr. Perrin said. "There are many other phenomena in children’s lives that are much more problematic or worrisome than what the gender or sexual orientation of their parents is."
On Twitter @MaryEllenNY
FROM PEDIATRICS