User login
MOC will be focus for new ABIM president
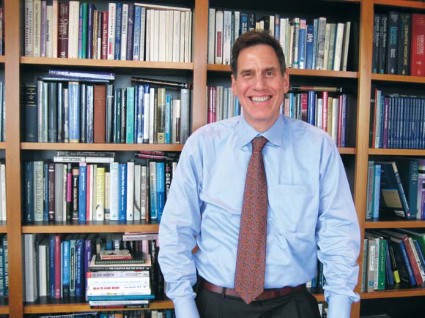
Dr. Richard Baron remembers meeting a friend of his parents many years ago and hearing how the man – an internist – briefly went AWOL from the army during World War II so he could take his board exam.
The story goes that the young doctor was helping transport a patient with tuberculosis from Florida to upstate New York and jumped off the train in Philadelphia to take the exam.
Dr. Baron, who will become president and CEO of the American Board of Internal Medicine (ABIM) and the ABIM Foundation in June, said he thinks internists still take that kind of pride in board certification.
"Here’s somebody who says, ‘I want to demonstrate to myself, to my patients, that I have what it takes to do this very hard, very important work,’ " Dr. Baron said in an interview. "I think that impulse is alive and well in most internists in America."
As Dr. Baron takes over the top job at the ABIM, his first priority will be revising maintenance of certification (MOC) to make it a more continuous process.
"A 10-year cycle is simply not credible," Dr. Baron said.
Currently, physicians who wish to recertify through the ABIM must take an exam, engage in continuing medical education, and complete a series of self-evaluation modules over a 10-year period.
Other certifying boards have already taken steps toward a more continuous process. The American Board of Pediatrics, the American Board of Family Medicine, the American Board of Psychiatry and Neurology, and the American Board of Radiology have all eliminated specific "end dates" for their board-certified physicians.
The ABIM will be announcing revisions to their process over the next year.
While the move toward continuous MOC may sound daunting to some physicians, it could help the ABIM forge agreements that would ultimately reduce some of the demands on physician time, Dr. Baron said. For instance, the ABIM has been working over the last few years to make the work put into MOC count toward other quality reporting programs.
Last July, the ABIM and the Centers for Medicare and Medicaid Services announced that physicians would be able to earn bonus payments from the federal government by participating in a new voluntary program called the Physician Quality Reporting System (PQRS) Maintenance of Certification Program Incentive.
And 20 health plans now allow physicians to use their participation in MOC to qualify for the plans’ quality recognition programs.
"Part of making the credential rewarding and relevant is having it do double duty and triple duty for a variety of other initiatives and programs that are interested in gauging the performance and abilities of physicians," Dr. Baron said.
The ABIM is also working with state licensing boards to see if participation in MOC can be part of that process as well – but that’s still a work in progress, Dr. Baron said.
Fulfilling the goal of making MOC count in as many ways as possible will be one of Dr. Baron’s biggest challenges, said Dr. Steven Weinberger, the executive vice president and chief executive officer of the American College of Physicians.
"In the same way that we look to continuous quality improvement on the practice side, I think we should be looking to continuous quality improvement on the certification side and on the maintenance of certification side," he said.
Another challenge is that the U.S. health care system is running out of money, said Dr. Robert M. Wachter, chair of the ABIM board of directors.
Dr. Baron and the ABIM board will need to revise the MOC process in an era when it’s not just important to assess the quality of care, but the efficiency as well, Dr. Wachter said.
"What it looks like to be a good doctor today has to include stewardship," said Dr. Wachter, who is also the chief of hospital medicine at the University of California, San Francisco.
Dr. Baron has had plenty of experience looking at how to improve efficiency of care. In the late 1980s and early 1990s, at the height of the managed care era, Dr. Baron served as chief medical officer for Health Partners, a not-for-profit Medicaid HMO. And recently, he ran the Seamless Care Models group at the CMS Innovation Center, where he worked on models for Accountable Care Organizations.
But Dr. Baron’s primary care roots also run deep. He spent most of his nearly 30-year career practicing general internal medicine and geriatrics.
He began his career with the National Health Service Corps in the early 1980s in rural Tennessee. Later, while working for the Medical College of Pennsylvania, he established a community-based satellite practice. And in 1989, he opened his own primary care practice in Philadelphia. That practice, Greenhouse Internists, grew into a seven-physician practice with more than 10,000 patients.
For Dr. Baron, it was a laboratory for innovative practice. Greenhouse was one of the first practices recognized by the National Committee for Quality Assurance (NCQA) as a level 3 patient-centered medical home, and it became a leader in the adoption of comprehensive electronic health records.
"I was passionate about practice and wanting to test new things in practice," Dr. Baron said.
His real-world focus was one of the big things that appealed to the ABIM board when selecting Dr. Baron for the job.
"He’s a real doctor," Dr. Wachter said. "In that practice, he saw what people go through in trying to provide high quality and safe and efficient care. That was extremely attractive to us ... someone who really understood the practice environment."
Dr. Richard Baron remembers meeting a friend of his parents many years ago and hearing how the man – an internist – briefly went AWOL from the army during World War II so he could take his board exam.
The story goes that the young doctor was helping transport a patient with tuberculosis from Florida to upstate New York and jumped off the train in Philadelphia to take the exam.
Dr. Baron, who will become president and CEO of the American Board of Internal Medicine (ABIM) and the ABIM Foundation in June, said he thinks internists still take that kind of pride in board certification.
"Here’s somebody who says, ‘I want to demonstrate to myself, to my patients, that I have what it takes to do this very hard, very important work,’ " Dr. Baron said in an interview. "I think that impulse is alive and well in most internists in America."
As Dr. Baron takes over the top job at the ABIM, his first priority will be revising maintenance of certification (MOC) to make it a more continuous process.
"A 10-year cycle is simply not credible," Dr. Baron said.
Currently, physicians who wish to recertify through the ABIM must take an exam, engage in continuing medical education, and complete a series of self-evaluation modules over a 10-year period.
Other certifying boards have already taken steps toward a more continuous process. The American Board of Pediatrics, the American Board of Family Medicine, the American Board of Psychiatry and Neurology, and the American Board of Radiology have all eliminated specific "end dates" for their board-certified physicians.
The ABIM will be announcing revisions to their process over the next year.
While the move toward continuous MOC may sound daunting to some physicians, it could help the ABIM forge agreements that would ultimately reduce some of the demands on physician time, Dr. Baron said. For instance, the ABIM has been working over the last few years to make the work put into MOC count toward other quality reporting programs.
Last July, the ABIM and the Centers for Medicare and Medicaid Services announced that physicians would be able to earn bonus payments from the federal government by participating in a new voluntary program called the Physician Quality Reporting System (PQRS) Maintenance of Certification Program Incentive.
And 20 health plans now allow physicians to use their participation in MOC to qualify for the plans’ quality recognition programs.
"Part of making the credential rewarding and relevant is having it do double duty and triple duty for a variety of other initiatives and programs that are interested in gauging the performance and abilities of physicians," Dr. Baron said.
The ABIM is also working with state licensing boards to see if participation in MOC can be part of that process as well – but that’s still a work in progress, Dr. Baron said.
Fulfilling the goal of making MOC count in as many ways as possible will be one of Dr. Baron’s biggest challenges, said Dr. Steven Weinberger, the executive vice president and chief executive officer of the American College of Physicians.
"In the same way that we look to continuous quality improvement on the practice side, I think we should be looking to continuous quality improvement on the certification side and on the maintenance of certification side," he said.
Another challenge is that the U.S. health care system is running out of money, said Dr. Robert M. Wachter, chair of the ABIM board of directors.
Dr. Baron and the ABIM board will need to revise the MOC process in an era when it’s not just important to assess the quality of care, but the efficiency as well, Dr. Wachter said.
"What it looks like to be a good doctor today has to include stewardship," said Dr. Wachter, who is also the chief of hospital medicine at the University of California, San Francisco.
Dr. Baron has had plenty of experience looking at how to improve efficiency of care. In the late 1980s and early 1990s, at the height of the managed care era, Dr. Baron served as chief medical officer for Health Partners, a not-for-profit Medicaid HMO. And recently, he ran the Seamless Care Models group at the CMS Innovation Center, where he worked on models for Accountable Care Organizations.
But Dr. Baron’s primary care roots also run deep. He spent most of his nearly 30-year career practicing general internal medicine and geriatrics.
He began his career with the National Health Service Corps in the early 1980s in rural Tennessee. Later, while working for the Medical College of Pennsylvania, he established a community-based satellite practice. And in 1989, he opened his own primary care practice in Philadelphia. That practice, Greenhouse Internists, grew into a seven-physician practice with more than 10,000 patients.
For Dr. Baron, it was a laboratory for innovative practice. Greenhouse was one of the first practices recognized by the National Committee for Quality Assurance (NCQA) as a level 3 patient-centered medical home, and it became a leader in the adoption of comprehensive electronic health records.
"I was passionate about practice and wanting to test new things in practice," Dr. Baron said.
His real-world focus was one of the big things that appealed to the ABIM board when selecting Dr. Baron for the job.
"He’s a real doctor," Dr. Wachter said. "In that practice, he saw what people go through in trying to provide high quality and safe and efficient care. That was extremely attractive to us ... someone who really understood the practice environment."
Dr. Richard Baron remembers meeting a friend of his parents many years ago and hearing how the man – an internist – briefly went AWOL from the army during World War II so he could take his board exam.
The story goes that the young doctor was helping transport a patient with tuberculosis from Florida to upstate New York and jumped off the train in Philadelphia to take the exam.
Dr. Baron, who will become president and CEO of the American Board of Internal Medicine (ABIM) and the ABIM Foundation in June, said he thinks internists still take that kind of pride in board certification.
"Here’s somebody who says, ‘I want to demonstrate to myself, to my patients, that I have what it takes to do this very hard, very important work,’ " Dr. Baron said in an interview. "I think that impulse is alive and well in most internists in America."
As Dr. Baron takes over the top job at the ABIM, his first priority will be revising maintenance of certification (MOC) to make it a more continuous process.
"A 10-year cycle is simply not credible," Dr. Baron said.
Currently, physicians who wish to recertify through the ABIM must take an exam, engage in continuing medical education, and complete a series of self-evaluation modules over a 10-year period.
Other certifying boards have already taken steps toward a more continuous process. The American Board of Pediatrics, the American Board of Family Medicine, the American Board of Psychiatry and Neurology, and the American Board of Radiology have all eliminated specific "end dates" for their board-certified physicians.
The ABIM will be announcing revisions to their process over the next year.
While the move toward continuous MOC may sound daunting to some physicians, it could help the ABIM forge agreements that would ultimately reduce some of the demands on physician time, Dr. Baron said. For instance, the ABIM has been working over the last few years to make the work put into MOC count toward other quality reporting programs.
Last July, the ABIM and the Centers for Medicare and Medicaid Services announced that physicians would be able to earn bonus payments from the federal government by participating in a new voluntary program called the Physician Quality Reporting System (PQRS) Maintenance of Certification Program Incentive.
And 20 health plans now allow physicians to use their participation in MOC to qualify for the plans’ quality recognition programs.
"Part of making the credential rewarding and relevant is having it do double duty and triple duty for a variety of other initiatives and programs that are interested in gauging the performance and abilities of physicians," Dr. Baron said.
The ABIM is also working with state licensing boards to see if participation in MOC can be part of that process as well – but that’s still a work in progress, Dr. Baron said.
Fulfilling the goal of making MOC count in as many ways as possible will be one of Dr. Baron’s biggest challenges, said Dr. Steven Weinberger, the executive vice president and chief executive officer of the American College of Physicians.
"In the same way that we look to continuous quality improvement on the practice side, I think we should be looking to continuous quality improvement on the certification side and on the maintenance of certification side," he said.
Another challenge is that the U.S. health care system is running out of money, said Dr. Robert M. Wachter, chair of the ABIM board of directors.
Dr. Baron and the ABIM board will need to revise the MOC process in an era when it’s not just important to assess the quality of care, but the efficiency as well, Dr. Wachter said.
"What it looks like to be a good doctor today has to include stewardship," said Dr. Wachter, who is also the chief of hospital medicine at the University of California, San Francisco.
Dr. Baron has had plenty of experience looking at how to improve efficiency of care. In the late 1980s and early 1990s, at the height of the managed care era, Dr. Baron served as chief medical officer for Health Partners, a not-for-profit Medicaid HMO. And recently, he ran the Seamless Care Models group at the CMS Innovation Center, where he worked on models for Accountable Care Organizations.
But Dr. Baron’s primary care roots also run deep. He spent most of his nearly 30-year career practicing general internal medicine and geriatrics.
He began his career with the National Health Service Corps in the early 1980s in rural Tennessee. Later, while working for the Medical College of Pennsylvania, he established a community-based satellite practice. And in 1989, he opened his own primary care practice in Philadelphia. That practice, Greenhouse Internists, grew into a seven-physician practice with more than 10,000 patients.
For Dr. Baron, it was a laboratory for innovative practice. Greenhouse was one of the first practices recognized by the National Committee for Quality Assurance (NCQA) as a level 3 patient-centered medical home, and it became a leader in the adoption of comprehensive electronic health records.
"I was passionate about practice and wanting to test new things in practice," Dr. Baron said.
His real-world focus was one of the big things that appealed to the ABIM board when selecting Dr. Baron for the job.
"He’s a real doctor," Dr. Wachter said. "In that practice, he saw what people go through in trying to provide high quality and safe and efficient care. That was extremely attractive to us ... someone who really understood the practice environment."
New concussion guidelines stress individualized approach
Any athlete with a possible concussion should be immediately removed from play pending an evaluation by a licensed health care provider trained in assessing concussions and traumatic brain injury, according to a new guideline from the American Academy of Neurology.
The guideline for evaluating and managing athletes with concussion was published online in the journal Neurology on March 18 (doi:10.1212/WNL.0b013e31828d57dd) in conjunction with the annual meeting of the AAN. The guideline replaces the Academy’s 1997 recommendations, which stressed using a grading system to try to predict concussion outcomes.
The new guideline takes a more individualized and conservative approach, especially for younger athletes. The new approach comes as many states have enacted legislation regulating when young athletes can return to play following a concussion.
"If in doubt, sit it out," Dr. Jeffrey S. Kutcher, coauthor of the guideline and a neurologist at the University of Michigan in Ann Arbor, said in a statement. "Being seen by a trained professional is extremely important after a concussion. If headaches or other symptoms return with the start of exercise, stop the activity and consult a doctor. You only get one brain; treat it well."
The new guideline calls for athletes to stay off the field until they are asymptomatic off medication. High school athletes and younger players with a concussion should be managed more conservatively since they take longer to recover than older athletes, according to the AAN.
But there is not enough evidence to support complete rest after a concussion. Activities that do not worsen symptoms and don’t pose a risk of another concussion can be part of the management of the injury, according to the guideline.
"We’re moved away from the concussion grading systems we first established in 1997 and are now recommending concussion and return to play be assessed in each athlete individually," Dr. Christopher C. Giza, the co–lead guideline author and a neurologist at Mattel Children’s Hospital at the University of California, Los Angeles, said in a statement. "There is no set timeline for safe return to play."
The AAN expert panel recommends that sideline providers use symptom checklists such as the Standardized Assessment of Concussion to help identify suspected concussion and that the scores be shared with the physicians involved in the athletes’ care off the field. But these checklists should not be the only tool used in making a diagnosis, according to the guidelines. Also, the checklist scores may be more useful if they are compared against preinjury individual scores, especially in younger athletes and those with prior concussions.
CT imaging should not be used to diagnose a suspected sport-related concussion, according to the guideline. But imaging might be used to rule out more serious traumatic brain injuries, such as intracranial hemorrhage in athletes with a suspected concussion who also have a loss of consciousness, posttraumatic amnesia, persistently altered mental status, focal neurologic deficit, evidence of skull fracture, or signs of clinical deterioration.
Athletes are at greater risk of concussion if they have a history of concussion. The first 10 days after a concussion pose the greatest risk for a repeat injury.
The AAN advises physicians to be on the lookout for ongoing symptoms that are linked to a longer recovery, such as continued headache or fogginess. Athletes with a history of concussions and younger players also tend to have a longer recovery.
The guideline also include level C recommendations stating that health care providers "might" develop individualized graded plans for returning to physical and cognitive activity. They might also provide cognitive restructuring counseling in an effort to shorten the duration of symptoms and the likelihood of developing chronic post-concussion syndrome, according to the guideline.
The guideline also included a number of recommendations on areas for future research, including studies of pre–high school age athletes to determine the natural history of concussion and recovery time for this age group, as well as the best assessment tools. The expert panel also called for clinical trials of different postconcussion management strategies and return-to-play protocols.
The guidelines were developed by a multidisciplinary expert committee that included representatives from neurology, athletic training, neuropsychology, epidemiology and biostatistics, neurosurgery, physical medicine and rehabilitation, and sports medicine. Many of the authors reported serving as consultants for professional sports associations, receiving honoraria and funding for travel for lectures on sports concussion, receiving research support from various foundations and organizations, and providing expert testimony in legal cases involving traumatic brain injury or concussion.
One of the most important statements in the new guideline
is that providers should not rely on a single diagnostic test when evaluating
an athlete, said Dr. Barry Jordan, the assistant medical director and attending
neurologist at the Burke Rehabilitation Hospital in White Plains, N.Y. Dr.
Jordan, who is an expert on sports concussions, said he’s seen too many
providers using a single computerized screening tool to assess whether an
athlete is well enough to return to play.
The new
guideline calls on providers to combine screening checklists with clinical
findings when making the determination about whether an athlete is well enough
to return to the field. Dr. Jordan
said this comprehensive approach is the way to go. And physicians who are
knowledgeable about concussions must be involved with that evaluation, he said.
 |
| Dr. Barry Jordan |
The new guideline is an important update reflecting
the movement away from grading concussions to a more individualized approach. "You can't grade the severity until the concussion is over," he said.
Dr. Jordan
said the AAN guideline is "clear and easy to follow" and will results in better
care if followed.
Dr.
Barry Jordan is the director of the Brain Injury Program at Burke
Rehabilitation Hospital in White Plains, N.Y. He works with several sports
organizations including the New York State Athletic Commission, U.S.A. Boxing, and the National
Football League Players Association. He also writes a bimonthly column for
Clinical Neurology News called “On the Sidelines.”
One of the most important statements in the new guideline
is that providers should not rely on a single diagnostic test when evaluating
an athlete, said Dr. Barry Jordan, the assistant medical director and attending
neurologist at the Burke Rehabilitation Hospital in White Plains, N.Y. Dr.
Jordan, who is an expert on sports concussions, said he’s seen too many
providers using a single computerized screening tool to assess whether an
athlete is well enough to return to play.
The new
guideline calls on providers to combine screening checklists with clinical
findings when making the determination about whether an athlete is well enough
to return to the field. Dr. Jordan
said this comprehensive approach is the way to go. And physicians who are
knowledgeable about concussions must be involved with that evaluation, he said.
 |
| Dr. Barry Jordan |
The new guideline is an important update reflecting
the movement away from grading concussions to a more individualized approach. "You can't grade the severity until the concussion is over," he said.
Dr. Jordan
said the AAN guideline is "clear and easy to follow" and will results in better
care if followed.
Dr.
Barry Jordan is the director of the Brain Injury Program at Burke
Rehabilitation Hospital in White Plains, N.Y. He works with several sports
organizations including the New York State Athletic Commission, U.S.A. Boxing, and the National
Football League Players Association. He also writes a bimonthly column for
Clinical Neurology News called “On the Sidelines.”
One of the most important statements in the new guideline
is that providers should not rely on a single diagnostic test when evaluating
an athlete, said Dr. Barry Jordan, the assistant medical director and attending
neurologist at the Burke Rehabilitation Hospital in White Plains, N.Y. Dr.
Jordan, who is an expert on sports concussions, said he’s seen too many
providers using a single computerized screening tool to assess whether an
athlete is well enough to return to play.
The new
guideline calls on providers to combine screening checklists with clinical
findings when making the determination about whether an athlete is well enough
to return to the field. Dr. Jordan
said this comprehensive approach is the way to go. And physicians who are
knowledgeable about concussions must be involved with that evaluation, he said.
 |
| Dr. Barry Jordan |
The new guideline is an important update reflecting
the movement away from grading concussions to a more individualized approach. "You can't grade the severity until the concussion is over," he said.
Dr. Jordan
said the AAN guideline is "clear and easy to follow" and will results in better
care if followed.
Dr.
Barry Jordan is the director of the Brain Injury Program at Burke
Rehabilitation Hospital in White Plains, N.Y. He works with several sports
organizations including the New York State Athletic Commission, U.S.A. Boxing, and the National
Football League Players Association. He also writes a bimonthly column for
Clinical Neurology News called “On the Sidelines.”
Any athlete with a possible concussion should be immediately removed from play pending an evaluation by a licensed health care provider trained in assessing concussions and traumatic brain injury, according to a new guideline from the American Academy of Neurology.
The guideline for evaluating and managing athletes with concussion was published online in the journal Neurology on March 18 (doi:10.1212/WNL.0b013e31828d57dd) in conjunction with the annual meeting of the AAN. The guideline replaces the Academy’s 1997 recommendations, which stressed using a grading system to try to predict concussion outcomes.
The new guideline takes a more individualized and conservative approach, especially for younger athletes. The new approach comes as many states have enacted legislation regulating when young athletes can return to play following a concussion.
"If in doubt, sit it out," Dr. Jeffrey S. Kutcher, coauthor of the guideline and a neurologist at the University of Michigan in Ann Arbor, said in a statement. "Being seen by a trained professional is extremely important after a concussion. If headaches or other symptoms return with the start of exercise, stop the activity and consult a doctor. You only get one brain; treat it well."
The new guideline calls for athletes to stay off the field until they are asymptomatic off medication. High school athletes and younger players with a concussion should be managed more conservatively since they take longer to recover than older athletes, according to the AAN.
But there is not enough evidence to support complete rest after a concussion. Activities that do not worsen symptoms and don’t pose a risk of another concussion can be part of the management of the injury, according to the guideline.
"We’re moved away from the concussion grading systems we first established in 1997 and are now recommending concussion and return to play be assessed in each athlete individually," Dr. Christopher C. Giza, the co–lead guideline author and a neurologist at Mattel Children’s Hospital at the University of California, Los Angeles, said in a statement. "There is no set timeline for safe return to play."
The AAN expert panel recommends that sideline providers use symptom checklists such as the Standardized Assessment of Concussion to help identify suspected concussion and that the scores be shared with the physicians involved in the athletes’ care off the field. But these checklists should not be the only tool used in making a diagnosis, according to the guidelines. Also, the checklist scores may be more useful if they are compared against preinjury individual scores, especially in younger athletes and those with prior concussions.
CT imaging should not be used to diagnose a suspected sport-related concussion, according to the guideline. But imaging might be used to rule out more serious traumatic brain injuries, such as intracranial hemorrhage in athletes with a suspected concussion who also have a loss of consciousness, posttraumatic amnesia, persistently altered mental status, focal neurologic deficit, evidence of skull fracture, or signs of clinical deterioration.
Athletes are at greater risk of concussion if they have a history of concussion. The first 10 days after a concussion pose the greatest risk for a repeat injury.
The AAN advises physicians to be on the lookout for ongoing symptoms that are linked to a longer recovery, such as continued headache or fogginess. Athletes with a history of concussions and younger players also tend to have a longer recovery.
The guideline also include level C recommendations stating that health care providers "might" develop individualized graded plans for returning to physical and cognitive activity. They might also provide cognitive restructuring counseling in an effort to shorten the duration of symptoms and the likelihood of developing chronic post-concussion syndrome, according to the guideline.
The guideline also included a number of recommendations on areas for future research, including studies of pre–high school age athletes to determine the natural history of concussion and recovery time for this age group, as well as the best assessment tools. The expert panel also called for clinical trials of different postconcussion management strategies and return-to-play protocols.
The guidelines were developed by a multidisciplinary expert committee that included representatives from neurology, athletic training, neuropsychology, epidemiology and biostatistics, neurosurgery, physical medicine and rehabilitation, and sports medicine. Many of the authors reported serving as consultants for professional sports associations, receiving honoraria and funding for travel for lectures on sports concussion, receiving research support from various foundations and organizations, and providing expert testimony in legal cases involving traumatic brain injury or concussion.
Any athlete with a possible concussion should be immediately removed from play pending an evaluation by a licensed health care provider trained in assessing concussions and traumatic brain injury, according to a new guideline from the American Academy of Neurology.
The guideline for evaluating and managing athletes with concussion was published online in the journal Neurology on March 18 (doi:10.1212/WNL.0b013e31828d57dd) in conjunction with the annual meeting of the AAN. The guideline replaces the Academy’s 1997 recommendations, which stressed using a grading system to try to predict concussion outcomes.
The new guideline takes a more individualized and conservative approach, especially for younger athletes. The new approach comes as many states have enacted legislation regulating when young athletes can return to play following a concussion.
"If in doubt, sit it out," Dr. Jeffrey S. Kutcher, coauthor of the guideline and a neurologist at the University of Michigan in Ann Arbor, said in a statement. "Being seen by a trained professional is extremely important after a concussion. If headaches or other symptoms return with the start of exercise, stop the activity and consult a doctor. You only get one brain; treat it well."
The new guideline calls for athletes to stay off the field until they are asymptomatic off medication. High school athletes and younger players with a concussion should be managed more conservatively since they take longer to recover than older athletes, according to the AAN.
But there is not enough evidence to support complete rest after a concussion. Activities that do not worsen symptoms and don’t pose a risk of another concussion can be part of the management of the injury, according to the guideline.
"We’re moved away from the concussion grading systems we first established in 1997 and are now recommending concussion and return to play be assessed in each athlete individually," Dr. Christopher C. Giza, the co–lead guideline author and a neurologist at Mattel Children’s Hospital at the University of California, Los Angeles, said in a statement. "There is no set timeline for safe return to play."
The AAN expert panel recommends that sideline providers use symptom checklists such as the Standardized Assessment of Concussion to help identify suspected concussion and that the scores be shared with the physicians involved in the athletes’ care off the field. But these checklists should not be the only tool used in making a diagnosis, according to the guidelines. Also, the checklist scores may be more useful if they are compared against preinjury individual scores, especially in younger athletes and those with prior concussions.
CT imaging should not be used to diagnose a suspected sport-related concussion, according to the guideline. But imaging might be used to rule out more serious traumatic brain injuries, such as intracranial hemorrhage in athletes with a suspected concussion who also have a loss of consciousness, posttraumatic amnesia, persistently altered mental status, focal neurologic deficit, evidence of skull fracture, or signs of clinical deterioration.
Athletes are at greater risk of concussion if they have a history of concussion. The first 10 days after a concussion pose the greatest risk for a repeat injury.
The AAN advises physicians to be on the lookout for ongoing symptoms that are linked to a longer recovery, such as continued headache or fogginess. Athletes with a history of concussions and younger players also tend to have a longer recovery.
The guideline also include level C recommendations stating that health care providers "might" develop individualized graded plans for returning to physical and cognitive activity. They might also provide cognitive restructuring counseling in an effort to shorten the duration of symptoms and the likelihood of developing chronic post-concussion syndrome, according to the guideline.
The guideline also included a number of recommendations on areas for future research, including studies of pre–high school age athletes to determine the natural history of concussion and recovery time for this age group, as well as the best assessment tools. The expert panel also called for clinical trials of different postconcussion management strategies and return-to-play protocols.
The guidelines were developed by a multidisciplinary expert committee that included representatives from neurology, athletic training, neuropsychology, epidemiology and biostatistics, neurosurgery, physical medicine and rehabilitation, and sports medicine. Many of the authors reported serving as consultants for professional sports associations, receiving honoraria and funding for travel for lectures on sports concussion, receiving research support from various foundations and organizations, and providing expert testimony in legal cases involving traumatic brain injury or concussion.
FROM NEUROLOGY
Proposal eases path for early-stage Alzheimer's approvals
The Food and Drug Administration is looking to make it easier to bring early-stage Alzheimer’s disease treatments to market.
In an article in the New England Journal of Medicine, which appeared online March 13, two physicians in the FDA’s Center for Drug Evaluation and Research outlined how treatments targeting patients at the very early stages of the disease could be reviewed under an accelerated approval pathway that allows drugs that address an unmet medical need to be approved on the basis of an intermediate clinical endpoint. The approval would be made on the condition that postapproval studies must be conducted to verify the clinical benefit of the drug (N. Engl. J. Med. 2013 March 13 [doi:10.1056/NEJMp1302513]).
Under this proposal, the FDA would consider the impact of a drug based on cognitive outcomes alone. This is a significant departure from the current regulatory framework, which requires any claims of improved cognition to include evidence of improvement in function. In early Alzheimer’s disease patients who have yet to experience the onset of overt dementia, it’s often impossible to show a functional improvement.
"As the focus of drug development has shifted to earlier stages of Alzheimer’s disease, many new and challenging scientific questions have emerged, and the regulatory framework under which such therapies are evaluated should evolve accordingly," Dr. Nicholas Kozauer and Dr. Russell Katz of the FDA wrote.
The agency recently issued draft guidance to the drug industry on how to conduct clinical trials involving early-stage Alzheimer’s patients who do not present with dementia. In the guidance, the FDA suggested evaluating early-stage disease patients using a single scale that combines assessment of cognition and function. For instance, the Clinical Dementia Rating–Sum of Boxes score is a good tool that evaluates patients based on six domains of cognition and daily functioning, according to the FDA.
On Twitter @MaryEllenNY
The Food and Drug Administration is looking to make it easier to bring early-stage Alzheimer’s disease treatments to market.
In an article in the New England Journal of Medicine, which appeared online March 13, two physicians in the FDA’s Center for Drug Evaluation and Research outlined how treatments targeting patients at the very early stages of the disease could be reviewed under an accelerated approval pathway that allows drugs that address an unmet medical need to be approved on the basis of an intermediate clinical endpoint. The approval would be made on the condition that postapproval studies must be conducted to verify the clinical benefit of the drug (N. Engl. J. Med. 2013 March 13 [doi:10.1056/NEJMp1302513]).
Under this proposal, the FDA would consider the impact of a drug based on cognitive outcomes alone. This is a significant departure from the current regulatory framework, which requires any claims of improved cognition to include evidence of improvement in function. In early Alzheimer’s disease patients who have yet to experience the onset of overt dementia, it’s often impossible to show a functional improvement.
"As the focus of drug development has shifted to earlier stages of Alzheimer’s disease, many new and challenging scientific questions have emerged, and the regulatory framework under which such therapies are evaluated should evolve accordingly," Dr. Nicholas Kozauer and Dr. Russell Katz of the FDA wrote.
The agency recently issued draft guidance to the drug industry on how to conduct clinical trials involving early-stage Alzheimer’s patients who do not present with dementia. In the guidance, the FDA suggested evaluating early-stage disease patients using a single scale that combines assessment of cognition and function. For instance, the Clinical Dementia Rating–Sum of Boxes score is a good tool that evaluates patients based on six domains of cognition and daily functioning, according to the FDA.
On Twitter @MaryEllenNY
The Food and Drug Administration is looking to make it easier to bring early-stage Alzheimer’s disease treatments to market.
In an article in the New England Journal of Medicine, which appeared online March 13, two physicians in the FDA’s Center for Drug Evaluation and Research outlined how treatments targeting patients at the very early stages of the disease could be reviewed under an accelerated approval pathway that allows drugs that address an unmet medical need to be approved on the basis of an intermediate clinical endpoint. The approval would be made on the condition that postapproval studies must be conducted to verify the clinical benefit of the drug (N. Engl. J. Med. 2013 March 13 [doi:10.1056/NEJMp1302513]).
Under this proposal, the FDA would consider the impact of a drug based on cognitive outcomes alone. This is a significant departure from the current regulatory framework, which requires any claims of improved cognition to include evidence of improvement in function. In early Alzheimer’s disease patients who have yet to experience the onset of overt dementia, it’s often impossible to show a functional improvement.
"As the focus of drug development has shifted to earlier stages of Alzheimer’s disease, many new and challenging scientific questions have emerged, and the regulatory framework under which such therapies are evaluated should evolve accordingly," Dr. Nicholas Kozauer and Dr. Russell Katz of the FDA wrote.
The agency recently issued draft guidance to the drug industry on how to conduct clinical trials involving early-stage Alzheimer’s patients who do not present with dementia. In the guidance, the FDA suggested evaluating early-stage disease patients using a single scale that combines assessment of cognition and function. For instance, the Clinical Dementia Rating–Sum of Boxes score is a good tool that evaluates patients based on six domains of cognition and daily functioning, according to the FDA.
On Twitter @MaryEllenNY
NEW ENGLAND JOURNAL OF MEDICINE
Preparing residents for the real world of hospital medicine
Dr. Anjala V. Tess, a hospitalist at the Beth Israel Deaconess Medical Center in Boston, spends about 70% of her time teaching about quality improvement and patient safety. She’s the director of quality and safety for graduate medical education at BIDMC and she helped create the Stoneman Elective on Quality Improvement, which serves as a sort of mandatory patient safety boot camp for residents.
But Dr. Tess also wanted her residents to understand how hospital medicine practices are run, from where the money comes from to how the schedules get made. So about a decade ago, she started teaching the hospital medicine elective, a 2- to 3-week course that covers the history of hospital medicine, the different practice models, how hospitals and hospitalists get paid, and the literature on quality improvement. The 10 residents who complete the course each year visit other hospitals to see how various hospital medicine practices are run.
In an interview, Dr. Tess explained why she started the course at BIDMC and how it has changed over time.
Question: How did the hospital medicine elective get started?
Dr. Tess: One day, I found myself as a member of a practice and all of a sudden I was learning about billing and hearing about how budgets were "neutral" or "positive" or "negative." I had no idea what any of that meant. At the same time, we had more and more residents coming through [internal medicine training] who were interested in hospital medicine as a whole. So I got permission to pull together an elective that was broadly titled, "the Hospital Medicine Elective." Residents, as it is, spend a lot of time in the inpatient setting, so putting together another clinical elective wouldn’t necessarily augment their learning. I decided to try to teach them a little bit about the practice of hospital medicine because the field is much more than just inpatient medicine.
Question: Residents must complete a project as part of the elective. What do they work on?
Dr. Tess: The residents are divided into two groups and I give them a fictional case – a hospital medicine group that’s been established for about 4-5 years, but it’s a mess. It’s falling apart and they can’t keep providers on staff. The hospital is upset, and the nursing staff feels like the hospitalists aren’t engaged anymore. I give the residents information on the current census, billings, and salaries. At the end of the rotation, the two groups make a pitch to redesign the program. It brings the tutorials and readings to life because they have to understand the concept of bringing value as a hospitalist. The presentations usually come down to who makes the best value argument and who can come up with the most innovative way to bring value from this new group to the hospital.
Question: What surprises the residents as they go through the course?
Dr. Tess: For most of them, they are surprised by the layers of bureaucracy around payment and how complicated it is to build a budget. They always tell me that the hardest part is building the schedule. They’re asked to take care of 50 patients a day and when they try to staff the service with a limited number of physicians, they realize that it is very challenging to do that and still come up with a job description that someone would be willing to take.
Question: Is this type of course an essential part of preparing to be a hospitalist?
Dr. Tess: I think it is mission critical for everybody to see patients well and safely on graduation. The clinical training that residents receive is more important, but I do think that this type of elective helps the newer graduates understand what they are getting into. It also helps people when they are applying for jobs. They are able to ask much more appropriate questions. I’ve heard anecdotally from some of the local folks who interview our residents that the ones who went through the hospital medicine elective ask questions that demonstrate a better understanding of what it’s like to be in a hospital medicine practice. They are no longer thinking about just themselves and their job, but about themselves as a member of a practice.
Question: How have you changed the course over the years?
Dr. Tess: One of the major changes that I made was changing the case. We went from cases trying to establish hospital medicine programs to trying to fix a troubled program. In the last 5 or 6 years, I’ve changed the slant on it so that the hospital isn’t happy with some of the quality metrics. In the past, I’ve used catheter-associated urinary tract infections or the poor deep vein thrombosis compliance rates. Lately, I’ve used readmissions because they are a little more topical. And as the role of hospitalists in partnering with primary care providers around Accountable Care Organizations gets sorted out, for example, I need to start to bring that into the cases as well.
Take us to your leader. Nominate a hospitalist whose work inspires you. E-mail suggestions to [email protected].
Dr. Anjala V. Tess, a hospitalist at the Beth Israel Deaconess Medical Center in Boston, spends about 70% of her time teaching about quality improvement and patient safety. She’s the director of quality and safety for graduate medical education at BIDMC and she helped create the Stoneman Elective on Quality Improvement, which serves as a sort of mandatory patient safety boot camp for residents.
But Dr. Tess also wanted her residents to understand how hospital medicine practices are run, from where the money comes from to how the schedules get made. So about a decade ago, she started teaching the hospital medicine elective, a 2- to 3-week course that covers the history of hospital medicine, the different practice models, how hospitals and hospitalists get paid, and the literature on quality improvement. The 10 residents who complete the course each year visit other hospitals to see how various hospital medicine practices are run.
In an interview, Dr. Tess explained why she started the course at BIDMC and how it has changed over time.
Question: How did the hospital medicine elective get started?
Dr. Tess: One day, I found myself as a member of a practice and all of a sudden I was learning about billing and hearing about how budgets were "neutral" or "positive" or "negative." I had no idea what any of that meant. At the same time, we had more and more residents coming through [internal medicine training] who were interested in hospital medicine as a whole. So I got permission to pull together an elective that was broadly titled, "the Hospital Medicine Elective." Residents, as it is, spend a lot of time in the inpatient setting, so putting together another clinical elective wouldn’t necessarily augment their learning. I decided to try to teach them a little bit about the practice of hospital medicine because the field is much more than just inpatient medicine.
Question: Residents must complete a project as part of the elective. What do they work on?
Dr. Tess: The residents are divided into two groups and I give them a fictional case – a hospital medicine group that’s been established for about 4-5 years, but it’s a mess. It’s falling apart and they can’t keep providers on staff. The hospital is upset, and the nursing staff feels like the hospitalists aren’t engaged anymore. I give the residents information on the current census, billings, and salaries. At the end of the rotation, the two groups make a pitch to redesign the program. It brings the tutorials and readings to life because they have to understand the concept of bringing value as a hospitalist. The presentations usually come down to who makes the best value argument and who can come up with the most innovative way to bring value from this new group to the hospital.
Question: What surprises the residents as they go through the course?
Dr. Tess: For most of them, they are surprised by the layers of bureaucracy around payment and how complicated it is to build a budget. They always tell me that the hardest part is building the schedule. They’re asked to take care of 50 patients a day and when they try to staff the service with a limited number of physicians, they realize that it is very challenging to do that and still come up with a job description that someone would be willing to take.
Question: Is this type of course an essential part of preparing to be a hospitalist?
Dr. Tess: I think it is mission critical for everybody to see patients well and safely on graduation. The clinical training that residents receive is more important, but I do think that this type of elective helps the newer graduates understand what they are getting into. It also helps people when they are applying for jobs. They are able to ask much more appropriate questions. I’ve heard anecdotally from some of the local folks who interview our residents that the ones who went through the hospital medicine elective ask questions that demonstrate a better understanding of what it’s like to be in a hospital medicine practice. They are no longer thinking about just themselves and their job, but about themselves as a member of a practice.
Question: How have you changed the course over the years?
Dr. Tess: One of the major changes that I made was changing the case. We went from cases trying to establish hospital medicine programs to trying to fix a troubled program. In the last 5 or 6 years, I’ve changed the slant on it so that the hospital isn’t happy with some of the quality metrics. In the past, I’ve used catheter-associated urinary tract infections or the poor deep vein thrombosis compliance rates. Lately, I’ve used readmissions because they are a little more topical. And as the role of hospitalists in partnering with primary care providers around Accountable Care Organizations gets sorted out, for example, I need to start to bring that into the cases as well.
Take us to your leader. Nominate a hospitalist whose work inspires you. E-mail suggestions to [email protected].
Dr. Anjala V. Tess, a hospitalist at the Beth Israel Deaconess Medical Center in Boston, spends about 70% of her time teaching about quality improvement and patient safety. She’s the director of quality and safety for graduate medical education at BIDMC and she helped create the Stoneman Elective on Quality Improvement, which serves as a sort of mandatory patient safety boot camp for residents.
But Dr. Tess also wanted her residents to understand how hospital medicine practices are run, from where the money comes from to how the schedules get made. So about a decade ago, she started teaching the hospital medicine elective, a 2- to 3-week course that covers the history of hospital medicine, the different practice models, how hospitals and hospitalists get paid, and the literature on quality improvement. The 10 residents who complete the course each year visit other hospitals to see how various hospital medicine practices are run.
In an interview, Dr. Tess explained why she started the course at BIDMC and how it has changed over time.
Question: How did the hospital medicine elective get started?
Dr. Tess: One day, I found myself as a member of a practice and all of a sudden I was learning about billing and hearing about how budgets were "neutral" or "positive" or "negative." I had no idea what any of that meant. At the same time, we had more and more residents coming through [internal medicine training] who were interested in hospital medicine as a whole. So I got permission to pull together an elective that was broadly titled, "the Hospital Medicine Elective." Residents, as it is, spend a lot of time in the inpatient setting, so putting together another clinical elective wouldn’t necessarily augment their learning. I decided to try to teach them a little bit about the practice of hospital medicine because the field is much more than just inpatient medicine.
Question: Residents must complete a project as part of the elective. What do they work on?
Dr. Tess: The residents are divided into two groups and I give them a fictional case – a hospital medicine group that’s been established for about 4-5 years, but it’s a mess. It’s falling apart and they can’t keep providers on staff. The hospital is upset, and the nursing staff feels like the hospitalists aren’t engaged anymore. I give the residents information on the current census, billings, and salaries. At the end of the rotation, the two groups make a pitch to redesign the program. It brings the tutorials and readings to life because they have to understand the concept of bringing value as a hospitalist. The presentations usually come down to who makes the best value argument and who can come up with the most innovative way to bring value from this new group to the hospital.
Question: What surprises the residents as they go through the course?
Dr. Tess: For most of them, they are surprised by the layers of bureaucracy around payment and how complicated it is to build a budget. They always tell me that the hardest part is building the schedule. They’re asked to take care of 50 patients a day and when they try to staff the service with a limited number of physicians, they realize that it is very challenging to do that and still come up with a job description that someone would be willing to take.
Question: Is this type of course an essential part of preparing to be a hospitalist?
Dr. Tess: I think it is mission critical for everybody to see patients well and safely on graduation. The clinical training that residents receive is more important, but I do think that this type of elective helps the newer graduates understand what they are getting into. It also helps people when they are applying for jobs. They are able to ask much more appropriate questions. I’ve heard anecdotally from some of the local folks who interview our residents that the ones who went through the hospital medicine elective ask questions that demonstrate a better understanding of what it’s like to be in a hospital medicine practice. They are no longer thinking about just themselves and their job, but about themselves as a member of a practice.
Question: How have you changed the course over the years?
Dr. Tess: One of the major changes that I made was changing the case. We went from cases trying to establish hospital medicine programs to trying to fix a troubled program. In the last 5 or 6 years, I’ve changed the slant on it so that the hospital isn’t happy with some of the quality metrics. In the past, I’ve used catheter-associated urinary tract infections or the poor deep vein thrombosis compliance rates. Lately, I’ve used readmissions because they are a little more topical. And as the role of hospitalists in partnering with primary care providers around Accountable Care Organizations gets sorted out, for example, I need to start to bring that into the cases as well.
Take us to your leader. Nominate a hospitalist whose work inspires you. E-mail suggestions to [email protected].
Rabies death follows infected organ transplant
A Maryland man recently died of rabies more than a year after receiving an infected organ in a transplant, according to the Centers for Disease Control and Prevention.
Officials at the CDC and the Maryland Department of Health and Mental Hygiene confirmed that the man died from rabies contracted through an organ transplant performed in 2011. After an investigation found that the Maryland man had no reported animal exposures, health officials began looking into the possibility that the infection was transmitted during his transplant.
Tissue testing of the organ donor and recipient revealed that they both had a raccoon type of rabies virus, which can infect raccoons as well as other wild and domestic animals. Only one other person is reported to have died from a raccoon-type rabies virus in the United States, according to the CDC.
Three other people who received organs from the infected donor have been identified and are receiving immune globulin and antirabies vaccination. In addition, the CDC is working with health officials in Florida, Georgia, Illinois, Maryland, and North Carolina to identify anyone who was in close contact with either the initial organ donor or the four recipients since they may also need postexposure rabies treatment.
At the time of the organ donor’s death in 2011, rabies was not suspected as the cause. Investigators are still trying to piece together how the donor first contracted rabies.
Although all potential organ donors in the United States are screened for infectious diseases such as HIV and hepatitis, rabies is not part of the standard screening process. The CDC estimates that there are only one to three cases of human rabies diagnosed each year in the United States. Because cases are so rare, screening for rabies is not routinely performed unless it is suspected based on interviews with family and friends or a physical examination, according to the CDC.
Maryland Department of Health and Mental Hygiene, infection
A Maryland man recently died of rabies more than a year after receiving an infected organ in a transplant, according to the Centers for Disease Control and Prevention.
Officials at the CDC and the Maryland Department of Health and Mental Hygiene confirmed that the man died from rabies contracted through an organ transplant performed in 2011. After an investigation found that the Maryland man had no reported animal exposures, health officials began looking into the possibility that the infection was transmitted during his transplant.
Tissue testing of the organ donor and recipient revealed that they both had a raccoon type of rabies virus, which can infect raccoons as well as other wild and domestic animals. Only one other person is reported to have died from a raccoon-type rabies virus in the United States, according to the CDC.
Three other people who received organs from the infected donor have been identified and are receiving immune globulin and antirabies vaccination. In addition, the CDC is working with health officials in Florida, Georgia, Illinois, Maryland, and North Carolina to identify anyone who was in close contact with either the initial organ donor or the four recipients since they may also need postexposure rabies treatment.
At the time of the organ donor’s death in 2011, rabies was not suspected as the cause. Investigators are still trying to piece together how the donor first contracted rabies.
Although all potential organ donors in the United States are screened for infectious diseases such as HIV and hepatitis, rabies is not part of the standard screening process. The CDC estimates that there are only one to three cases of human rabies diagnosed each year in the United States. Because cases are so rare, screening for rabies is not routinely performed unless it is suspected based on interviews with family and friends or a physical examination, according to the CDC.
A Maryland man recently died of rabies more than a year after receiving an infected organ in a transplant, according to the Centers for Disease Control and Prevention.
Officials at the CDC and the Maryland Department of Health and Mental Hygiene confirmed that the man died from rabies contracted through an organ transplant performed in 2011. After an investigation found that the Maryland man had no reported animal exposures, health officials began looking into the possibility that the infection was transmitted during his transplant.
Tissue testing of the organ donor and recipient revealed that they both had a raccoon type of rabies virus, which can infect raccoons as well as other wild and domestic animals. Only one other person is reported to have died from a raccoon-type rabies virus in the United States, according to the CDC.
Three other people who received organs from the infected donor have been identified and are receiving immune globulin and antirabies vaccination. In addition, the CDC is working with health officials in Florida, Georgia, Illinois, Maryland, and North Carolina to identify anyone who was in close contact with either the initial organ donor or the four recipients since they may also need postexposure rabies treatment.
At the time of the organ donor’s death in 2011, rabies was not suspected as the cause. Investigators are still trying to piece together how the donor first contracted rabies.
Although all potential organ donors in the United States are screened for infectious diseases such as HIV and hepatitis, rabies is not part of the standard screening process. The CDC estimates that there are only one to three cases of human rabies diagnosed each year in the United States. Because cases are so rare, screening for rabies is not routinely performed unless it is suspected based on interviews with family and friends or a physical examination, according to the CDC.
Maryland Department of Health and Mental Hygiene, infection
Maryland Department of Health and Mental Hygiene, infection
Primary care spots are hot in largest-ever Match Day
Nearly 400 more U.S. medical students chose primary care residencies in this year’s Main Residency Match than did in 2012, according to data from the National Resident Matching Program.
The number of U.S. medical students choosing residency positions in internal medicine, family medicine, and pediatrics all rose in 2013, with internal medicine getting the biggest boost. The number of U.S. seniors matching to internal medicine rose by 194, while pediatric matches with U.S. seniors increased by 105 and family medicine rose by 33.
The results point to an increased interest in primary care that has been percolating over the last few years.
Mona M. Signer, executive director of the National Resident Matching Program (NRMP), said the 2010 Affordable Care Act may be driving some of the interest.
"There is a lot of talk about the fact that the Affordable Care Act is going to create demand for more physicians, in particular more primary care physicians. Perhaps that is finally starting to resonate with U.S. seniors," Ms. Signer said in an interview.
With the Match program becoming more competitive, medical school seniors may also be getting more realistic about their matching chances. Ms. Signer said the NRMP produces a report called "Charting Outcomes in the Match" (2011 data) that shows the test scores, the number of research publications, and other characteristics of previous successful candidates for each specialty. Applicants and their medical school advisors are looking at the online report, she said, and getting savvier about the specialties in which they are most likely to be competitive.
The 2013 Match Day results show that dermatology, emergency medicine, medicine-pediatrics, neurological surgery, orthopedic surgery, otolaryngology, radiation oncology, general surgery, and plastic surgery are the top choices for medical students. Residency programs in these specialties filled at least 80% of their positions with U.S. seniors.
In internal medicine, 6,277 positions were offered this year, an increase of 1,000 over 2012. Of those, 99.4% were filled, with 49.9% taken by U.S. medical graduates.
In 2013, 3,037 family medicine residency positions were offered. Of those, 95.9% were filled, with 44.6% filled by U.S. medical graduates.
In pediatrics, 99.6% of the total 2,616 positions offered were filled. U.S. medical graduates filled 70.2% of the pediatric positions.
Though the match rate for U.S. graduates stayed about the same in pediatrics this year as in 2012, it was down somewhat in internal medicine and family medicine. The reason, Ms. Signer said, is that there were just so many more positions offered in those specialties than in previous years.
This year marked the first Match held under the NRMP’s new "all-in" policy, which requires programs participating in the Match to register and attempt to fill all of their available positions within the Match. Previously, some programs had offered positions outside of the Match process and the NRMP board of directors concluded that the practice placed too much pressure on students to accept these positions rather than to take their chances in the Match. The practice of offering positions outside the Match primarily affected osteopathic students, prior-year graduates of U.S. allopathic schools, and international medical graduates, Ms. Signer said.
As a result of the all-in policy, there were 1,000 more internal medicine positions in the Match, 297 more family medicine positions, and 141 positions in pediatrics, according to NRMP.
On Twitter @MaryEllenNY
Nearly 400 more U.S. medical students chose primary care residencies in this year’s Main Residency Match than did in 2012, according to data from the National Resident Matching Program.
The number of U.S. medical students choosing residency positions in internal medicine, family medicine, and pediatrics all rose in 2013, with internal medicine getting the biggest boost. The number of U.S. seniors matching to internal medicine rose by 194, while pediatric matches with U.S. seniors increased by 105 and family medicine rose by 33.
The results point to an increased interest in primary care that has been percolating over the last few years.
Mona M. Signer, executive director of the National Resident Matching Program (NRMP), said the 2010 Affordable Care Act may be driving some of the interest.
"There is a lot of talk about the fact that the Affordable Care Act is going to create demand for more physicians, in particular more primary care physicians. Perhaps that is finally starting to resonate with U.S. seniors," Ms. Signer said in an interview.
With the Match program becoming more competitive, medical school seniors may also be getting more realistic about their matching chances. Ms. Signer said the NRMP produces a report called "Charting Outcomes in the Match" (2011 data) that shows the test scores, the number of research publications, and other characteristics of previous successful candidates for each specialty. Applicants and their medical school advisors are looking at the online report, she said, and getting savvier about the specialties in which they are most likely to be competitive.
The 2013 Match Day results show that dermatology, emergency medicine, medicine-pediatrics, neurological surgery, orthopedic surgery, otolaryngology, radiation oncology, general surgery, and plastic surgery are the top choices for medical students. Residency programs in these specialties filled at least 80% of their positions with U.S. seniors.
In internal medicine, 6,277 positions were offered this year, an increase of 1,000 over 2012. Of those, 99.4% were filled, with 49.9% taken by U.S. medical graduates.
In 2013, 3,037 family medicine residency positions were offered. Of those, 95.9% were filled, with 44.6% filled by U.S. medical graduates.
In pediatrics, 99.6% of the total 2,616 positions offered were filled. U.S. medical graduates filled 70.2% of the pediatric positions.
Though the match rate for U.S. graduates stayed about the same in pediatrics this year as in 2012, it was down somewhat in internal medicine and family medicine. The reason, Ms. Signer said, is that there were just so many more positions offered in those specialties than in previous years.
This year marked the first Match held under the NRMP’s new "all-in" policy, which requires programs participating in the Match to register and attempt to fill all of their available positions within the Match. Previously, some programs had offered positions outside of the Match process and the NRMP board of directors concluded that the practice placed too much pressure on students to accept these positions rather than to take their chances in the Match. The practice of offering positions outside the Match primarily affected osteopathic students, prior-year graduates of U.S. allopathic schools, and international medical graduates, Ms. Signer said.
As a result of the all-in policy, there were 1,000 more internal medicine positions in the Match, 297 more family medicine positions, and 141 positions in pediatrics, according to NRMP.
On Twitter @MaryEllenNY
Nearly 400 more U.S. medical students chose primary care residencies in this year’s Main Residency Match than did in 2012, according to data from the National Resident Matching Program.
The number of U.S. medical students choosing residency positions in internal medicine, family medicine, and pediatrics all rose in 2013, with internal medicine getting the biggest boost. The number of U.S. seniors matching to internal medicine rose by 194, while pediatric matches with U.S. seniors increased by 105 and family medicine rose by 33.
The results point to an increased interest in primary care that has been percolating over the last few years.
Mona M. Signer, executive director of the National Resident Matching Program (NRMP), said the 2010 Affordable Care Act may be driving some of the interest.
"There is a lot of talk about the fact that the Affordable Care Act is going to create demand for more physicians, in particular more primary care physicians. Perhaps that is finally starting to resonate with U.S. seniors," Ms. Signer said in an interview.
With the Match program becoming more competitive, medical school seniors may also be getting more realistic about their matching chances. Ms. Signer said the NRMP produces a report called "Charting Outcomes in the Match" (2011 data) that shows the test scores, the number of research publications, and other characteristics of previous successful candidates for each specialty. Applicants and their medical school advisors are looking at the online report, she said, and getting savvier about the specialties in which they are most likely to be competitive.
The 2013 Match Day results show that dermatology, emergency medicine, medicine-pediatrics, neurological surgery, orthopedic surgery, otolaryngology, radiation oncology, general surgery, and plastic surgery are the top choices for medical students. Residency programs in these specialties filled at least 80% of their positions with U.S. seniors.
In internal medicine, 6,277 positions were offered this year, an increase of 1,000 over 2012. Of those, 99.4% were filled, with 49.9% taken by U.S. medical graduates.
In 2013, 3,037 family medicine residency positions were offered. Of those, 95.9% were filled, with 44.6% filled by U.S. medical graduates.
In pediatrics, 99.6% of the total 2,616 positions offered were filled. U.S. medical graduates filled 70.2% of the pediatric positions.
Though the match rate for U.S. graduates stayed about the same in pediatrics this year as in 2012, it was down somewhat in internal medicine and family medicine. The reason, Ms. Signer said, is that there were just so many more positions offered in those specialties than in previous years.
This year marked the first Match held under the NRMP’s new "all-in" policy, which requires programs participating in the Match to register and attempt to fill all of their available positions within the Match. Previously, some programs had offered positions outside of the Match process and the NRMP board of directors concluded that the practice placed too much pressure on students to accept these positions rather than to take their chances in the Match. The practice of offering positions outside the Match primarily affected osteopathic students, prior-year graduates of U.S. allopathic schools, and international medical graduates, Ms. Signer said.
As a result of the all-in policy, there were 1,000 more internal medicine positions in the Match, 297 more family medicine positions, and 141 positions in pediatrics, according to NRMP.
On Twitter @MaryEllenNY
CMS rules on reporting physician COI
Federal health officials have finally released the details on how online public reporting of industry payments to physicians will work.
Under the final rule released by the Centers for Medicare and Medicaid Services (CMS), drug, device, and medical supply manufacturers who participate in Medicare, Medicaid, or the Children’s Health Insurance Program will be required to submit annual reports to the federal government on any payments of $10 or more that they made to physicians and teaching hospitals. They also will be required to report on all payments if the payments and transfers of value to a single physician reach $100 in aggregate value for a year.
Manufacturers and group purchasing organizations (GPOs) must also report on physician ownership and investment interests each year. CMS will post the information on a public website. The requirements are mandated under the Affordable Care Act (ACA).
"You should know when your doctor has a financial relationship with the companies that manufacture or supply the medicines or medical devices you may need," Dr. Peter Budetti, CMS deputy administrator for Program Integrity, said in a statement. "Disclosure of these relationships allows patients to have more informed discussions with their doctors."
Manufacturers and GPOs have until Aug. 1 to begin collecting data. They must submit their reports on payments made in 2013 by March 31, 2014. CMS will post the data online by Sept. 30, 2014.
CMS did not meet the deadline set by law for issuing this final regulation: Under the ACA, data collection was supposed to begin in January 2012.
The final rule contains plenty of exceptions, however. For instance, reporting is not required for gifts between individuals with an existing personal relationship. Other exclusions include small payments of less than $10, educational materials that directly benefit patients or are intended for patient use, discounts for rebates for drugs and devices, in-kind items for charity care, and samples.
Indirect payments made to speakers at accredited or certified continuing medical education (CME) events also do not need to be reported as long as the manufacturer doesn’t suggest speakers.
The final rule also clarifies that companies sponsoring large-scale conferences do not need to track and report on small gifts and food items worth less than $10 such as pens and bottles of water. These items also won’t count toward the minimum yearly reporting threshold of $100, according to CMS.
"I think this will make life easier, because it will contribute toward a more relaxed atmosphere at meetings so that attendees won’t have to worry every time they pick up a bottle of water or a granola bar," said Dr. Daniel Carlat, project director for the Pew Prescription Project, which works for greater transparency in physician-industry relationships.
Dr. Carlat said the final rule strikes the right balance between increasing payment transparency and not overburdening physicians with the requirements.
Although the data collection and reporting requirements are on the drug and device industry, physicians are responsible for reviewing their information before publication. Under the final rule, physicians will have 45 days to review the reports and another 15 days to work with the manufacturers to correct any disputed reports. After that, if there are still disputes, the information will be posted publicly but will include a disclaimer that it is disputed, according to the final rule.
The new transparency initiative will likely enhance the public’s trust and confidence in their physicians, Dr. Carlat said. Consumers often hear about the worst-case scenarios, where physicians are taking millions of dollars that may cause conflicts of interest, but the new reporting is likely to show that is rare, he said.
"I think we’ll find with these transparency reports that the vast majority of payments and gifts are of very low value and are the equivalent of $50 to $100 or a few hundred dollars a year," Dr. Carlat said. "I think when patients see these figures, their concerns about relationships between doctors and companies will be to some extent allayed."
Federal health officials have finally released the details on how online public reporting of industry payments to physicians will work.
Under the final rule released by the Centers for Medicare and Medicaid Services (CMS), drug, device, and medical supply manufacturers who participate in Medicare, Medicaid, or the Children’s Health Insurance Program will be required to submit annual reports to the federal government on any payments of $10 or more that they made to physicians and teaching hospitals. They also will be required to report on all payments if the payments and transfers of value to a single physician reach $100 in aggregate value for a year.
Manufacturers and group purchasing organizations (GPOs) must also report on physician ownership and investment interests each year. CMS will post the information on a public website. The requirements are mandated under the Affordable Care Act (ACA).
"You should know when your doctor has a financial relationship with the companies that manufacture or supply the medicines or medical devices you may need," Dr. Peter Budetti, CMS deputy administrator for Program Integrity, said in a statement. "Disclosure of these relationships allows patients to have more informed discussions with their doctors."
Manufacturers and GPOs have until Aug. 1 to begin collecting data. They must submit their reports on payments made in 2013 by March 31, 2014. CMS will post the data online by Sept. 30, 2014.
CMS did not meet the deadline set by law for issuing this final regulation: Under the ACA, data collection was supposed to begin in January 2012.
The final rule contains plenty of exceptions, however. For instance, reporting is not required for gifts between individuals with an existing personal relationship. Other exclusions include small payments of less than $10, educational materials that directly benefit patients or are intended for patient use, discounts for rebates for drugs and devices, in-kind items for charity care, and samples.
Indirect payments made to speakers at accredited or certified continuing medical education (CME) events also do not need to be reported as long as the manufacturer doesn’t suggest speakers.
The final rule also clarifies that companies sponsoring large-scale conferences do not need to track and report on small gifts and food items worth less than $10 such as pens and bottles of water. These items also won’t count toward the minimum yearly reporting threshold of $100, according to CMS.
"I think this will make life easier, because it will contribute toward a more relaxed atmosphere at meetings so that attendees won’t have to worry every time they pick up a bottle of water or a granola bar," said Dr. Daniel Carlat, project director for the Pew Prescription Project, which works for greater transparency in physician-industry relationships.
Dr. Carlat said the final rule strikes the right balance between increasing payment transparency and not overburdening physicians with the requirements.
Although the data collection and reporting requirements are on the drug and device industry, physicians are responsible for reviewing their information before publication. Under the final rule, physicians will have 45 days to review the reports and another 15 days to work with the manufacturers to correct any disputed reports. After that, if there are still disputes, the information will be posted publicly but will include a disclaimer that it is disputed, according to the final rule.
The new transparency initiative will likely enhance the public’s trust and confidence in their physicians, Dr. Carlat said. Consumers often hear about the worst-case scenarios, where physicians are taking millions of dollars that may cause conflicts of interest, but the new reporting is likely to show that is rare, he said.
"I think we’ll find with these transparency reports that the vast majority of payments and gifts are of very low value and are the equivalent of $50 to $100 or a few hundred dollars a year," Dr. Carlat said. "I think when patients see these figures, their concerns about relationships between doctors and companies will be to some extent allayed."
Federal health officials have finally released the details on how online public reporting of industry payments to physicians will work.
Under the final rule released by the Centers for Medicare and Medicaid Services (CMS), drug, device, and medical supply manufacturers who participate in Medicare, Medicaid, or the Children’s Health Insurance Program will be required to submit annual reports to the federal government on any payments of $10 or more that they made to physicians and teaching hospitals. They also will be required to report on all payments if the payments and transfers of value to a single physician reach $100 in aggregate value for a year.
Manufacturers and group purchasing organizations (GPOs) must also report on physician ownership and investment interests each year. CMS will post the information on a public website. The requirements are mandated under the Affordable Care Act (ACA).
"You should know when your doctor has a financial relationship with the companies that manufacture or supply the medicines or medical devices you may need," Dr. Peter Budetti, CMS deputy administrator for Program Integrity, said in a statement. "Disclosure of these relationships allows patients to have more informed discussions with their doctors."
Manufacturers and GPOs have until Aug. 1 to begin collecting data. They must submit their reports on payments made in 2013 by March 31, 2014. CMS will post the data online by Sept. 30, 2014.
CMS did not meet the deadline set by law for issuing this final regulation: Under the ACA, data collection was supposed to begin in January 2012.
The final rule contains plenty of exceptions, however. For instance, reporting is not required for gifts between individuals with an existing personal relationship. Other exclusions include small payments of less than $10, educational materials that directly benefit patients or are intended for patient use, discounts for rebates for drugs and devices, in-kind items for charity care, and samples.
Indirect payments made to speakers at accredited or certified continuing medical education (CME) events also do not need to be reported as long as the manufacturer doesn’t suggest speakers.
The final rule also clarifies that companies sponsoring large-scale conferences do not need to track and report on small gifts and food items worth less than $10 such as pens and bottles of water. These items also won’t count toward the minimum yearly reporting threshold of $100, according to CMS.
"I think this will make life easier, because it will contribute toward a more relaxed atmosphere at meetings so that attendees won’t have to worry every time they pick up a bottle of water or a granola bar," said Dr. Daniel Carlat, project director for the Pew Prescription Project, which works for greater transparency in physician-industry relationships.
Dr. Carlat said the final rule strikes the right balance between increasing payment transparency and not overburdening physicians with the requirements.
Although the data collection and reporting requirements are on the drug and device industry, physicians are responsible for reviewing their information before publication. Under the final rule, physicians will have 45 days to review the reports and another 15 days to work with the manufacturers to correct any disputed reports. After that, if there are still disputes, the information will be posted publicly but will include a disclaimer that it is disputed, according to the final rule.
The new transparency initiative will likely enhance the public’s trust and confidence in their physicians, Dr. Carlat said. Consumers often hear about the worst-case scenarios, where physicians are taking millions of dollars that may cause conflicts of interest, but the new reporting is likely to show that is rare, he said.
"I think we’ll find with these transparency reports that the vast majority of payments and gifts are of very low value and are the equivalent of $50 to $100 or a few hundred dollars a year," Dr. Carlat said. "I think when patients see these figures, their concerns about relationships between doctors and companies will be to some extent allayed."
PCPs drive reduction in Cleveland hospitalizations
Doctors in Cleveland are offering proof that a robust primary care system is the way to reduce health care costs.
Better Health Greater Cleveland – a group of 55 primary care practices across eight health systems – reduced hospitalizations for patients with diabetes, hypertension, angina, or heart failure by 10% between 2009 and 2011 by improving the quality of primary care in the region.
Over this 3-year period, residents in Cuyahoga County, the area served by Better Health Greater Cleveland, experienced 2,624 fewer hospital stays than expected based on trends in the next five largest Ohio counties. The coalition estimates that the reduction saved nearly $20 million during that time.
It’s a different way to preserve health care resources, said Dr. Randall D. Cebul, director and president of Better Health.
Previously, "we spent a lot of money and a lot of time trying to change hospitals, and we felt as though that wasn’t our sweet spot," said Dr. Cebul, who is also a professor of medicine at Case Western Reserve University in Cleveland. "We’re ... essentially demanding better transitions of care when patients are hospitalized unavoidably, but we feel that avoiding hospitalizations is mostly our responsibility and the patient’s."
The group’s results show that primary care offices, staffed by a team of doctors, nurses, and allied health professionals, will be at the center of health care going forward, said Dr. Ronald Adams, senior physician for population health at Kaiser Permanente Ohio and a learning instructor for Better Health.
There’s already physical proof of this in Northeast Ohio, where new hospitals are few but Kaiser – a coalition member – has built several new primary care centers.
"Hospitals really are going to have a challenge because as we continue to do this good work, the number of people who are going to roll through [hospital] doors is going to decrease," Dr. Adams said. "They’re going to have to rethink which services they provide."
Better Health, which was established in 2007 and began its major activities in 2008, relies on a few key strategies: the use of electronic health records (EHRs), public reporting of performance measures, and sharing of best practices.
The coalition also provides practice coaches who provide free on-site technical support on everything from getting the most out of an EHR to submitting data for patient-centered medical home recognition.
The assistance is supported by a grant from the Robert Wood Johnson Foundation, membership fees, local businesses, and philanthropy. Better Health is one of 16 communities chosen to be part of the RWJF’s Aligning Forces for Quality initiative.
EHR use, public reporting
As of 2012, all groups within Better Health Greater Cleveland were using EHRs to target their treatment of diabetes, heart failure, and hypertension. EHRs also collect performance data on the three conditions, which are publicly reported twice a year. The reports, which can be viewed at www.betterhealthcleveland.org, show the performance of individual practices, regional performance, and change over time.
While they don’t know if patients are using the data, Dr. Cebul said, physicians certainly are. "They care as a point of pride, if nothing else, about doing better."
For physicians and other health care providers at the Louis Stokes Cleveland Veterans Affairs Medical Center, the ability to benchmark their performance against the local community was a big draw to participate in the collaborative, said Dr. Brook Watts, the Cleveland VAMC’s chief quality officer. Having data on the local health care environment was an important addition to national benchmarking data, she said.
And the data sharing was done in a nonthreatening way, she said. "We all agreed to put our data out there, and we’re not using it to point fingers," Dr. Watts said. "People have been very willing to share what they’re doing to try to improve the care of others."
Sharing ideas across systems
To share best practices, representatives from all the primary care practices gather twice a year to highlight what is working for the top performers.
"We are teaching one another how to do things smartly," Dr. Cebul said.
Even the world-renowned Cleveland Clinic has learned a few things from being part of the Better Health collaborative.
Dr. Michael Rabovsky, interim chairman of the Cleveland Clinic’s family medicine department, said he’s heard some great ideas while attending the learning sessions, whether it’s a protocol for improving pneumococcal vaccination rates or the successful hypertension control guidelines developed by Kaiser Permanente Ohio. And Cleveland Clinic providers have shared their expertise too. Dr. Rabovsky and his colleagues have provided insight on patient-centered medical home accreditation as well as strategies for improving care transitions.
The Cleveland Clinic’s 17 family medicine sites also have used the practice coaches to assist with their quality improvement projects, said Dr. Rabovsky, who chairs Better Health’s Clinical Advisory Committee.
Dr. Corinna Falck-Ytter, director of the Diabetes Group Clinic at MetroHealth Medical Center, part of Case Western Reserve University, said the practice coaches helped her improve group educational sessions at her clinic.
Since she started the clinic years before on a tight budget, she and her team never had formal training in group dynamics or on motivational interviewing. The practice coach helped them learn how to get the most out of the teaching sessions, she said.
Paying for improvement
So far, Better Health’s success has come without offering bonuses or other financial incentives to physicians for improved performance. But Dr. Cebul said the improvement would be faster if the payment system encouraged physicians to provide patient-centered primary care rather than just office visits.
For instance, having a nurse call patients if they miss a test or fail to fill a medication leads to better patient care, Dr. Cebul said, but it’s not paid for by insurance. And if those reminder calls help keep patients healthy and out of the office in the future, that only costs the practice more money under the fee-for-service system.
"The payment system is screwed up, and we’re getting exactly what we pay for – too many tests, too many visits, and too many treatments without regard to outcomes," Dr. Cebul said.
Doctors in Cleveland are offering proof that a robust primary care system is the way to reduce health care costs.
Better Health Greater Cleveland – a group of 55 primary care practices across eight health systems – reduced hospitalizations for patients with diabetes, hypertension, angina, or heart failure by 10% between 2009 and 2011 by improving the quality of primary care in the region.
Over this 3-year period, residents in Cuyahoga County, the area served by Better Health Greater Cleveland, experienced 2,624 fewer hospital stays than expected based on trends in the next five largest Ohio counties. The coalition estimates that the reduction saved nearly $20 million during that time.
It’s a different way to preserve health care resources, said Dr. Randall D. Cebul, director and president of Better Health.
Previously, "we spent a lot of money and a lot of time trying to change hospitals, and we felt as though that wasn’t our sweet spot," said Dr. Cebul, who is also a professor of medicine at Case Western Reserve University in Cleveland. "We’re ... essentially demanding better transitions of care when patients are hospitalized unavoidably, but we feel that avoiding hospitalizations is mostly our responsibility and the patient’s."
The group’s results show that primary care offices, staffed by a team of doctors, nurses, and allied health professionals, will be at the center of health care going forward, said Dr. Ronald Adams, senior physician for population health at Kaiser Permanente Ohio and a learning instructor for Better Health.
There’s already physical proof of this in Northeast Ohio, where new hospitals are few but Kaiser – a coalition member – has built several new primary care centers.
"Hospitals really are going to have a challenge because as we continue to do this good work, the number of people who are going to roll through [hospital] doors is going to decrease," Dr. Adams said. "They’re going to have to rethink which services they provide."
Better Health, which was established in 2007 and began its major activities in 2008, relies on a few key strategies: the use of electronic health records (EHRs), public reporting of performance measures, and sharing of best practices.
The coalition also provides practice coaches who provide free on-site technical support on everything from getting the most out of an EHR to submitting data for patient-centered medical home recognition.
The assistance is supported by a grant from the Robert Wood Johnson Foundation, membership fees, local businesses, and philanthropy. Better Health is one of 16 communities chosen to be part of the RWJF’s Aligning Forces for Quality initiative.
EHR use, public reporting
As of 2012, all groups within Better Health Greater Cleveland were using EHRs to target their treatment of diabetes, heart failure, and hypertension. EHRs also collect performance data on the three conditions, which are publicly reported twice a year. The reports, which can be viewed at www.betterhealthcleveland.org, show the performance of individual practices, regional performance, and change over time.
While they don’t know if patients are using the data, Dr. Cebul said, physicians certainly are. "They care as a point of pride, if nothing else, about doing better."
For physicians and other health care providers at the Louis Stokes Cleveland Veterans Affairs Medical Center, the ability to benchmark their performance against the local community was a big draw to participate in the collaborative, said Dr. Brook Watts, the Cleveland VAMC’s chief quality officer. Having data on the local health care environment was an important addition to national benchmarking data, she said.
And the data sharing was done in a nonthreatening way, she said. "We all agreed to put our data out there, and we’re not using it to point fingers," Dr. Watts said. "People have been very willing to share what they’re doing to try to improve the care of others."
Sharing ideas across systems
To share best practices, representatives from all the primary care practices gather twice a year to highlight what is working for the top performers.
"We are teaching one another how to do things smartly," Dr. Cebul said.
Even the world-renowned Cleveland Clinic has learned a few things from being part of the Better Health collaborative.
Dr. Michael Rabovsky, interim chairman of the Cleveland Clinic’s family medicine department, said he’s heard some great ideas while attending the learning sessions, whether it’s a protocol for improving pneumococcal vaccination rates or the successful hypertension control guidelines developed by Kaiser Permanente Ohio. And Cleveland Clinic providers have shared their expertise too. Dr. Rabovsky and his colleagues have provided insight on patient-centered medical home accreditation as well as strategies for improving care transitions.
The Cleveland Clinic’s 17 family medicine sites also have used the practice coaches to assist with their quality improvement projects, said Dr. Rabovsky, who chairs Better Health’s Clinical Advisory Committee.
Dr. Corinna Falck-Ytter, director of the Diabetes Group Clinic at MetroHealth Medical Center, part of Case Western Reserve University, said the practice coaches helped her improve group educational sessions at her clinic.
Since she started the clinic years before on a tight budget, she and her team never had formal training in group dynamics or on motivational interviewing. The practice coach helped them learn how to get the most out of the teaching sessions, she said.
Paying for improvement
So far, Better Health’s success has come without offering bonuses or other financial incentives to physicians for improved performance. But Dr. Cebul said the improvement would be faster if the payment system encouraged physicians to provide patient-centered primary care rather than just office visits.
For instance, having a nurse call patients if they miss a test or fail to fill a medication leads to better patient care, Dr. Cebul said, but it’s not paid for by insurance. And if those reminder calls help keep patients healthy and out of the office in the future, that only costs the practice more money under the fee-for-service system.
"The payment system is screwed up, and we’re getting exactly what we pay for – too many tests, too many visits, and too many treatments without regard to outcomes," Dr. Cebul said.
Doctors in Cleveland are offering proof that a robust primary care system is the way to reduce health care costs.
Better Health Greater Cleveland – a group of 55 primary care practices across eight health systems – reduced hospitalizations for patients with diabetes, hypertension, angina, or heart failure by 10% between 2009 and 2011 by improving the quality of primary care in the region.
Over this 3-year period, residents in Cuyahoga County, the area served by Better Health Greater Cleveland, experienced 2,624 fewer hospital stays than expected based on trends in the next five largest Ohio counties. The coalition estimates that the reduction saved nearly $20 million during that time.
It’s a different way to preserve health care resources, said Dr. Randall D. Cebul, director and president of Better Health.
Previously, "we spent a lot of money and a lot of time trying to change hospitals, and we felt as though that wasn’t our sweet spot," said Dr. Cebul, who is also a professor of medicine at Case Western Reserve University in Cleveland. "We’re ... essentially demanding better transitions of care when patients are hospitalized unavoidably, but we feel that avoiding hospitalizations is mostly our responsibility and the patient’s."
The group’s results show that primary care offices, staffed by a team of doctors, nurses, and allied health professionals, will be at the center of health care going forward, said Dr. Ronald Adams, senior physician for population health at Kaiser Permanente Ohio and a learning instructor for Better Health.
There’s already physical proof of this in Northeast Ohio, where new hospitals are few but Kaiser – a coalition member – has built several new primary care centers.
"Hospitals really are going to have a challenge because as we continue to do this good work, the number of people who are going to roll through [hospital] doors is going to decrease," Dr. Adams said. "They’re going to have to rethink which services they provide."
Better Health, which was established in 2007 and began its major activities in 2008, relies on a few key strategies: the use of electronic health records (EHRs), public reporting of performance measures, and sharing of best practices.
The coalition also provides practice coaches who provide free on-site technical support on everything from getting the most out of an EHR to submitting data for patient-centered medical home recognition.
The assistance is supported by a grant from the Robert Wood Johnson Foundation, membership fees, local businesses, and philanthropy. Better Health is one of 16 communities chosen to be part of the RWJF’s Aligning Forces for Quality initiative.
EHR use, public reporting
As of 2012, all groups within Better Health Greater Cleveland were using EHRs to target their treatment of diabetes, heart failure, and hypertension. EHRs also collect performance data on the three conditions, which are publicly reported twice a year. The reports, which can be viewed at www.betterhealthcleveland.org, show the performance of individual practices, regional performance, and change over time.
While they don’t know if patients are using the data, Dr. Cebul said, physicians certainly are. "They care as a point of pride, if nothing else, about doing better."
For physicians and other health care providers at the Louis Stokes Cleveland Veterans Affairs Medical Center, the ability to benchmark their performance against the local community was a big draw to participate in the collaborative, said Dr. Brook Watts, the Cleveland VAMC’s chief quality officer. Having data on the local health care environment was an important addition to national benchmarking data, she said.
And the data sharing was done in a nonthreatening way, she said. "We all agreed to put our data out there, and we’re not using it to point fingers," Dr. Watts said. "People have been very willing to share what they’re doing to try to improve the care of others."
Sharing ideas across systems
To share best practices, representatives from all the primary care practices gather twice a year to highlight what is working for the top performers.
"We are teaching one another how to do things smartly," Dr. Cebul said.
Even the world-renowned Cleveland Clinic has learned a few things from being part of the Better Health collaborative.
Dr. Michael Rabovsky, interim chairman of the Cleveland Clinic’s family medicine department, said he’s heard some great ideas while attending the learning sessions, whether it’s a protocol for improving pneumococcal vaccination rates or the successful hypertension control guidelines developed by Kaiser Permanente Ohio. And Cleveland Clinic providers have shared their expertise too. Dr. Rabovsky and his colleagues have provided insight on patient-centered medical home accreditation as well as strategies for improving care transitions.
The Cleveland Clinic’s 17 family medicine sites also have used the practice coaches to assist with their quality improvement projects, said Dr. Rabovsky, who chairs Better Health’s Clinical Advisory Committee.
Dr. Corinna Falck-Ytter, director of the Diabetes Group Clinic at MetroHealth Medical Center, part of Case Western Reserve University, said the practice coaches helped her improve group educational sessions at her clinic.
Since she started the clinic years before on a tight budget, she and her team never had formal training in group dynamics or on motivational interviewing. The practice coach helped them learn how to get the most out of the teaching sessions, she said.
Paying for improvement
So far, Better Health’s success has come without offering bonuses or other financial incentives to physicians for improved performance. But Dr. Cebul said the improvement would be faster if the payment system encouraged physicians to provide patient-centered primary care rather than just office visits.
For instance, having a nurse call patients if they miss a test or fail to fill a medication leads to better patient care, Dr. Cebul said, but it’s not paid for by insurance. And if those reminder calls help keep patients healthy and out of the office in the future, that only costs the practice more money under the fee-for-service system.
"The payment system is screwed up, and we’re getting exactly what we pay for – too many tests, too many visits, and too many treatments without regard to outcomes," Dr. Cebul said.
Readmission rates still poor, vary by region
Hospital readmission rates continue to hover at around 16% for medical discharges and 12% for surgical conditions, despite the existence of several proven protocols for improving the discharge process.
A new analysis of Medicare data conducted by the Dartmouth Atlas Project, and supported by the Robert Wood Johnson Foundation, shows that readmission rates are virtually unchanged between 2008 and 2010. This follows an earlier report from the Dartmouth Atlas Project showing that readmission rates failed to improve between 2004 and 2009.
"We still have a very persistent problem," Dr. Risa Lavizzo-Mourey, president and CEO of the Robert Wood Johnson Foundation, said during a panel discussion on the report on Feb. 13 in Washington.
The national rate for 30-day readmissions for medical conditions was 16.2% in 2008 and 15.9% in 2010. Similarly, the 30-day surgical readmission rates were 12.7% in 2008 and 12.4% in 2010. The same trends hold true when looking at readmission rates for heart failure, acute myocardial infarction, and pneumonia, the conditions that held accountable for as part of a new Medicare readmissions penalty that went into effect in October 2012.
Readmission rates for heart failure were dipped slightly from 21.4% in 2008 to 21.1% in 2010. Acute myocardial infarction readmissions went from 18.7% to 18.1% during the same time period. And pneumonia readmission rates stayed at 15.3% in both 2008 and 2010.
The researchers called the progress on readmissions "slow and inconsistent." But while there has been little change nationally among the Medicare population, there is widespread regional variation, according to the analysis.
For instance, 30-day readmission rates following medical discharge ranged from a low of 11.4% in Ogden, Utah, to a high of 18.1% in the Bronx, N.Y., in 2010. There was even greater variation in readmissions following surgery. Surgical readmission rates ranged from 7.6% in Bend, Oregon, to 18.3% in the New York.
"People who have the same illness often have very different chances of being readmitted depending on where they live," Dr. Lavizzo-Mourey said.
Many patients are readmitted simply because their local hospital is the community’s main source of care, the researchers wrote. This trend results in both higher initial hospital admissions and readmissions, they wrote.
But while the report highlights the lack of progress, there are some success stories, Dr. Lavizzo-Mourey said. For instance, some hospitals are establishing 24-hour pharmacies so that patients can get their prescriptions no matter what time they are discharged. Others are setting up clinics to specialize in the care of patients with heart failure, a condition with a high rate of bounce-back to the hospital. And other hospitals are working with community organizations to ensure patients have the care and support they need when they go home, she said.
"This issue of readmissions is firmly on the radar screen of our health care providers," Dr. Lavizzo-Mourey said.
Dr. Eric Coleman, who runs the Care Transitions Program aimed at improving the safety of hand-offs, said one of the issues that leads to readmissions is the poor engagement of patients and family members before discharge.
At the University of Colorado, Denver, where he heads the division of health care policy and research, Dr. Coleman said they try to avoid simply dumping information on patients and families and instead use a process called "skill transfer" to train them to be able to handle their own care at home without the help of health care providers.
But many of the causes of readmissions are beyond the control of the hospital, Dr. Coleman said. He encourages physicians to go the bedside and ask patients why they think they were readmitted to the hospital. The answers are often about a lack of transportation to appointments, struggles to afford medicine and care, or family caregivers who are burning out.
"It may be that hospitals don’t have the resources to address this but a lot of their community partners, such as the area agencies on aging do have that opportunity," Dr. Coleman said.
Hospital readmission rates continue to hover at around 16% for medical discharges and 12% for surgical conditions, despite the existence of several proven protocols for improving the discharge process.
A new analysis of Medicare data conducted by the Dartmouth Atlas Project, and supported by the Robert Wood Johnson Foundation, shows that readmission rates are virtually unchanged between 2008 and 2010. This follows an earlier report from the Dartmouth Atlas Project showing that readmission rates failed to improve between 2004 and 2009.
"We still have a very persistent problem," Dr. Risa Lavizzo-Mourey, president and CEO of the Robert Wood Johnson Foundation, said during a panel discussion on the report on Feb. 13 in Washington.
The national rate for 30-day readmissions for medical conditions was 16.2% in 2008 and 15.9% in 2010. Similarly, the 30-day surgical readmission rates were 12.7% in 2008 and 12.4% in 2010. The same trends hold true when looking at readmission rates for heart failure, acute myocardial infarction, and pneumonia, the conditions that held accountable for as part of a new Medicare readmissions penalty that went into effect in October 2012.
Readmission rates for heart failure were dipped slightly from 21.4% in 2008 to 21.1% in 2010. Acute myocardial infarction readmissions went from 18.7% to 18.1% during the same time period. And pneumonia readmission rates stayed at 15.3% in both 2008 and 2010.
The researchers called the progress on readmissions "slow and inconsistent." But while there has been little change nationally among the Medicare population, there is widespread regional variation, according to the analysis.
For instance, 30-day readmission rates following medical discharge ranged from a low of 11.4% in Ogden, Utah, to a high of 18.1% in the Bronx, N.Y., in 2010. There was even greater variation in readmissions following surgery. Surgical readmission rates ranged from 7.6% in Bend, Oregon, to 18.3% in the New York.
"People who have the same illness often have very different chances of being readmitted depending on where they live," Dr. Lavizzo-Mourey said.
Many patients are readmitted simply because their local hospital is the community’s main source of care, the researchers wrote. This trend results in both higher initial hospital admissions and readmissions, they wrote.
But while the report highlights the lack of progress, there are some success stories, Dr. Lavizzo-Mourey said. For instance, some hospitals are establishing 24-hour pharmacies so that patients can get their prescriptions no matter what time they are discharged. Others are setting up clinics to specialize in the care of patients with heart failure, a condition with a high rate of bounce-back to the hospital. And other hospitals are working with community organizations to ensure patients have the care and support they need when they go home, she said.
"This issue of readmissions is firmly on the radar screen of our health care providers," Dr. Lavizzo-Mourey said.
Dr. Eric Coleman, who runs the Care Transitions Program aimed at improving the safety of hand-offs, said one of the issues that leads to readmissions is the poor engagement of patients and family members before discharge.
At the University of Colorado, Denver, where he heads the division of health care policy and research, Dr. Coleman said they try to avoid simply dumping information on patients and families and instead use a process called "skill transfer" to train them to be able to handle their own care at home without the help of health care providers.
But many of the causes of readmissions are beyond the control of the hospital, Dr. Coleman said. He encourages physicians to go the bedside and ask patients why they think they were readmitted to the hospital. The answers are often about a lack of transportation to appointments, struggles to afford medicine and care, or family caregivers who are burning out.
"It may be that hospitals don’t have the resources to address this but a lot of their community partners, such as the area agencies on aging do have that opportunity," Dr. Coleman said.
Hospital readmission rates continue to hover at around 16% for medical discharges and 12% for surgical conditions, despite the existence of several proven protocols for improving the discharge process.
A new analysis of Medicare data conducted by the Dartmouth Atlas Project, and supported by the Robert Wood Johnson Foundation, shows that readmission rates are virtually unchanged between 2008 and 2010. This follows an earlier report from the Dartmouth Atlas Project showing that readmission rates failed to improve between 2004 and 2009.
"We still have a very persistent problem," Dr. Risa Lavizzo-Mourey, president and CEO of the Robert Wood Johnson Foundation, said during a panel discussion on the report on Feb. 13 in Washington.
The national rate for 30-day readmissions for medical conditions was 16.2% in 2008 and 15.9% in 2010. Similarly, the 30-day surgical readmission rates were 12.7% in 2008 and 12.4% in 2010. The same trends hold true when looking at readmission rates for heart failure, acute myocardial infarction, and pneumonia, the conditions that held accountable for as part of a new Medicare readmissions penalty that went into effect in October 2012.
Readmission rates for heart failure were dipped slightly from 21.4% in 2008 to 21.1% in 2010. Acute myocardial infarction readmissions went from 18.7% to 18.1% during the same time period. And pneumonia readmission rates stayed at 15.3% in both 2008 and 2010.
The researchers called the progress on readmissions "slow and inconsistent." But while there has been little change nationally among the Medicare population, there is widespread regional variation, according to the analysis.
For instance, 30-day readmission rates following medical discharge ranged from a low of 11.4% in Ogden, Utah, to a high of 18.1% in the Bronx, N.Y., in 2010. There was even greater variation in readmissions following surgery. Surgical readmission rates ranged from 7.6% in Bend, Oregon, to 18.3% in the New York.
"People who have the same illness often have very different chances of being readmitted depending on where they live," Dr. Lavizzo-Mourey said.
Many patients are readmitted simply because their local hospital is the community’s main source of care, the researchers wrote. This trend results in both higher initial hospital admissions and readmissions, they wrote.
But while the report highlights the lack of progress, there are some success stories, Dr. Lavizzo-Mourey said. For instance, some hospitals are establishing 24-hour pharmacies so that patients can get their prescriptions no matter what time they are discharged. Others are setting up clinics to specialize in the care of patients with heart failure, a condition with a high rate of bounce-back to the hospital. And other hospitals are working with community organizations to ensure patients have the care and support they need when they go home, she said.
"This issue of readmissions is firmly on the radar screen of our health care providers," Dr. Lavizzo-Mourey said.
Dr. Eric Coleman, who runs the Care Transitions Program aimed at improving the safety of hand-offs, said one of the issues that leads to readmissions is the poor engagement of patients and family members before discharge.
At the University of Colorado, Denver, where he heads the division of health care policy and research, Dr. Coleman said they try to avoid simply dumping information on patients and families and instead use a process called "skill transfer" to train them to be able to handle their own care at home without the help of health care providers.
But many of the causes of readmissions are beyond the control of the hospital, Dr. Coleman said. He encourages physicians to go the bedside and ask patients why they think they were readmitted to the hospital. The answers are often about a lack of transportation to appointments, struggles to afford medicine and care, or family caregivers who are burning out.
"It may be that hospitals don’t have the resources to address this but a lot of their community partners, such as the area agencies on aging do have that opportunity," Dr. Coleman said.
Commission proposes shift away from fee-for-service
The fee-for-service payment system has contributed to high health care costs and inconsistent quality of care and should be replaced with a blended payment model that includes fixed payments, according to a new report from a panel of physicians and health care experts.
In the report, released March 4, the National Commission on Physician Payment Reform recommended phasing out the current fee-for-service system over 5 years in favor of bundled payments, capitation, and increased financial risk-sharing.
"We can’t control runaway medical spending without changing how doctors get paid," Dr. Bill Frist, honorary chair of the commission and former Senate majority leader, said in a statement. "This is a bipartisan issue. We all want to get the most from our health care dollars and that requires rethinking the way we pay for health care."
But the 14-member commission predicted that fee-for-service would continue to play a large role. By the end of the decade, they called for a blended system of fee-for-service, fixed payments, and salary.
The commission also recommended eliminating the Sustainable Growth Rate (SGR) formula, which ties Medicare physician payments to changes in the gross domestic product (GDP). The Congressional Budget Office (CBO) recently estimated the price of eliminating the SGR at $138 billion over 10 years, which the commission said could be paid for by reducing overutilization of Medicare services and cutting down on fraud.
The commission, which was convened by the Society of General Internal Medicine last March, is chaired by Dr. Steven A. Schroeder, former president of the Robert Wood Johnson Foundation. The other members include physicians from various specialties, as well as experts in health care policy. The commission is funded in part by the Robert Wood Johnson Foundation and the California HealthCare Foundation.
Some of the commission’s other recommendations include:
– Increasing payments for evaluation and management codes, while freezing procedural diagnosis codes for 3 years.
– Eliminating higher payments for facility-based services that can be performed in lower-cost settings of care.
– Incorporating quality metrics into fee-for-service contracts.
– Using fixed payment models in areas such as the management of multiple chronic diseases and in-hospital procedures and follow-up.
– Changing the membership of the Relative Value Scale Update Committee (RUC) to make it more representative of the medical profession.
The fee-for-service payment system has contributed to high health care costs and inconsistent quality of care and should be replaced with a blended payment model that includes fixed payments, according to a new report from a panel of physicians and health care experts.
In the report, released March 4, the National Commission on Physician Payment Reform recommended phasing out the current fee-for-service system over 5 years in favor of bundled payments, capitation, and increased financial risk-sharing.
"We can’t control runaway medical spending without changing how doctors get paid," Dr. Bill Frist, honorary chair of the commission and former Senate majority leader, said in a statement. "This is a bipartisan issue. We all want to get the most from our health care dollars and that requires rethinking the way we pay for health care."
But the 14-member commission predicted that fee-for-service would continue to play a large role. By the end of the decade, they called for a blended system of fee-for-service, fixed payments, and salary.
The commission also recommended eliminating the Sustainable Growth Rate (SGR) formula, which ties Medicare physician payments to changes in the gross domestic product (GDP). The Congressional Budget Office (CBO) recently estimated the price of eliminating the SGR at $138 billion over 10 years, which the commission said could be paid for by reducing overutilization of Medicare services and cutting down on fraud.
The commission, which was convened by the Society of General Internal Medicine last March, is chaired by Dr. Steven A. Schroeder, former president of the Robert Wood Johnson Foundation. The other members include physicians from various specialties, as well as experts in health care policy. The commission is funded in part by the Robert Wood Johnson Foundation and the California HealthCare Foundation.
Some of the commission’s other recommendations include:
– Increasing payments for evaluation and management codes, while freezing procedural diagnosis codes for 3 years.
– Eliminating higher payments for facility-based services that can be performed in lower-cost settings of care.
– Incorporating quality metrics into fee-for-service contracts.
– Using fixed payment models in areas such as the management of multiple chronic diseases and in-hospital procedures and follow-up.
– Changing the membership of the Relative Value Scale Update Committee (RUC) to make it more representative of the medical profession.
The fee-for-service payment system has contributed to high health care costs and inconsistent quality of care and should be replaced with a blended payment model that includes fixed payments, according to a new report from a panel of physicians and health care experts.
In the report, released March 4, the National Commission on Physician Payment Reform recommended phasing out the current fee-for-service system over 5 years in favor of bundled payments, capitation, and increased financial risk-sharing.
"We can’t control runaway medical spending without changing how doctors get paid," Dr. Bill Frist, honorary chair of the commission and former Senate majority leader, said in a statement. "This is a bipartisan issue. We all want to get the most from our health care dollars and that requires rethinking the way we pay for health care."
But the 14-member commission predicted that fee-for-service would continue to play a large role. By the end of the decade, they called for a blended system of fee-for-service, fixed payments, and salary.
The commission also recommended eliminating the Sustainable Growth Rate (SGR) formula, which ties Medicare physician payments to changes in the gross domestic product (GDP). The Congressional Budget Office (CBO) recently estimated the price of eliminating the SGR at $138 billion over 10 years, which the commission said could be paid for by reducing overutilization of Medicare services and cutting down on fraud.
The commission, which was convened by the Society of General Internal Medicine last March, is chaired by Dr. Steven A. Schroeder, former president of the Robert Wood Johnson Foundation. The other members include physicians from various specialties, as well as experts in health care policy. The commission is funded in part by the Robert Wood Johnson Foundation and the California HealthCare Foundation.
Some of the commission’s other recommendations include:
– Increasing payments for evaluation and management codes, while freezing procedural diagnosis codes for 3 years.
– Eliminating higher payments for facility-based services that can be performed in lower-cost settings of care.
– Incorporating quality metrics into fee-for-service contracts.
– Using fixed payment models in areas such as the management of multiple chronic diseases and in-hospital procedures and follow-up.
– Changing the membership of the Relative Value Scale Update Committee (RUC) to make it more representative of the medical profession.