User login
South Florida simulation center makes its mark
High-tech computer and robotic simulators are changing the way that obstetricians and gynecologists learn and maintain their skills. Now a new state-of-the-art simulation center in Tampa is changing the way academic medical centers offer this training.
With its modern architecture and gleaming glass exterior, the Center for Advanced Medical Learning and Simulation, located in downtown Tampa, looks like the type of building that houses cutting-edge technology.
The 90,000 square-foot-facility includes a surgical skills lab with more than 30 operating stations, an on-site tissue bank, a robotics suite with two da Vinci robots (S and Si), a synthetic cadaver, a 64-slice CT scanner, and a hybrid operating room. And those are just some of the offerings in the Surgical and Interventional Training Center.
The Center for Advanced Medical Learning and Simulation (CAMLS), which is affiliated with the University of South Florida, houses three other centers: the Virtual Patient Care Center, the Education Center, and the Tampa Bay Research and Innovation Center.
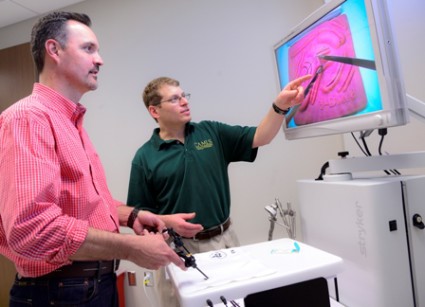
But it’s not the technology alone that sets CAMLS apart, said Dr. Stuart Hart, an ob.gyn. and urogynecologist who is the medical director for the Tampa Bay Research and Innovation Center.
"What makes it so unique is the tight integration among the various centers at CAMLS," he said.
The center, which opened in February 2012, has a lot of overlap among its education, training, and simulation programs. Anyone who comes to CAMLS for continuing medical education can get a sense of that integration, said Dr. Hart, who also oversees the minimally invasive gynecologic surgery courses.
For instance, ob.gyns. might have the chance to practice their skills on a synthetic cadaver in the Surgical and Interventional Training Center. Then they could take a trip upstairs to the Virtual Patient Care Center, where they could continue working on high-fidelity human patient simulators and laparoscopic surgical simulators.
"That’s what makes us so exciting," Dr. Hart said.
Dr. Robert W. Yelverton, an ob.gyn. in Tampa, first became involved with CAMLS while the center was still under construction. Dr. Yelverton, who at the time was the chief medical officer for a large ob.gyn. group in central Florida, was looking for a place where his physicians could get simulator training to improve the quality and safety of robotic and minimally invasive gynecological procedures.
For example, some of their physicians hadn’t received training during residency on how to examine the bladder with a cystoscope following a gynecologic procedure. In the past, urologists had typically been the ones performing cystoscopy, so many ob.gyns weren’t trained. But with those roles changing, Dr. Yelverton wanted his physicians to be able to learn and perfect the procedure on a simulator, rather than on real patients in the operating room. With the bladder simulator at CAMLS, physicians were able to perform cystoscopy hundreds of times and see virtually every abnormal legion in a realistic fashion, he said.
"This is a huge attraction for physicians who really are looking for improvement in ways that they can perfect their surgical skills, particularly those that were introduced after they were in training," Dr. Yelverton said.
Dr. Yelverton, who is the chairman for the American Congress of Obstetricians and Gynecologists District XII, is continuing to work with CAMLS to set up training for ACOG’s Florida fellows as part of their educational meetings.
He said he expects many local physicians, and even some from other parts of the country, will want to try out the center. One of the attractions, he said, is the ability to conduct team training. For instance, a team of obstetricians and nurses can simulate emergencies, from shoulder dystocia to postpartum hemorrhage, in a mock labor and delivery suite.
Practicing physicians aren’t the only ones who can hone their skills at CAMLS. The center is also available for medical students and residents, as well as pharmacy and nursing students. The certified registered nurse anesthetist program is permanently housed in the building.
Even graduate business and engineering students drop in at CAMLS as part of their work with the Tampa Bay Research and Innovation Center. Coming to CAMLS means that engineering and business students get the chance to sit down with physicians and learn about the clinical problems driving the need for new technologies and devices, Dr. Hart said.
As part of the innovation work, Dr. Hart often presents a problem to the engineering students and then brings them to the operating room to see a simulated surgery first hand. The students then come up ideas for different devices that could help solve the problem.
"We go in with problems," he said. "We don’t go in and say, ‘I have an idea for a medical device.’ That’s actually the last thing we want to do."
As part of that process, Dr. Hart and his colleagues also work closely with industry on device development and commercialization. And the device and pharmaceutical industry is also a presence in other parts of CAMLS. Medical device and pharmaceutical companies come to the center to train their sales forces and their clients, said Deborah Sutherland, Ph.D., the CEO of CAMLS.
One of the reasons that CAMLS is able to offer its services to groups and individuals who are not affiliated with the University of South Florida is that the center is part of a not-for-profit corporation that includes USF Health.
CAMLS is run on a business model, not a traditional academic model, Dr. Sutherland said. CAMLS does not receive any financial support from the University of South Florida. All of the revenue comes instead from user fees.
"That is very unique because most simulation centers that you see nationally are supported by a clinical department," she said.
That type of approach may make CAMLS the envy of other simulation centers around the country, said Dr. Carol A. Aschenbrener, the chief medical education officer at the Association of American Medical Colleges.
Running a simulation center is costly, with the annual price tag ranging anywhere between $50,000 and $2.5 million, depending on the scope of the center and the staffing levels, she said. A 2010 survey conducted by the AAMC shows that most of these centers are funded either by a medical school or a teaching hospital. With those organizations under significant financial pressure, many are looking carefully at other ways to pay the bills. A handful of centers are actively developing new business models, she said, but it’s early on in the process. "So people are watching the South Florida center very closely," Dr. Aschenbrener said.
High-tech computer and robotic simulators are changing the way that obstetricians and gynecologists learn and maintain their skills. Now a new state-of-the-art simulation center in Tampa is changing the way academic medical centers offer this training.
With its modern architecture and gleaming glass exterior, the Center for Advanced Medical Learning and Simulation, located in downtown Tampa, looks like the type of building that houses cutting-edge technology.
The 90,000 square-foot-facility includes a surgical skills lab with more than 30 operating stations, an on-site tissue bank, a robotics suite with two da Vinci robots (S and Si), a synthetic cadaver, a 64-slice CT scanner, and a hybrid operating room. And those are just some of the offerings in the Surgical and Interventional Training Center.
The Center for Advanced Medical Learning and Simulation (CAMLS), which is affiliated with the University of South Florida, houses three other centers: the Virtual Patient Care Center, the Education Center, and the Tampa Bay Research and Innovation Center.
But it’s not the technology alone that sets CAMLS apart, said Dr. Stuart Hart, an ob.gyn. and urogynecologist who is the medical director for the Tampa Bay Research and Innovation Center.
"What makes it so unique is the tight integration among the various centers at CAMLS," he said.
The center, which opened in February 2012, has a lot of overlap among its education, training, and simulation programs. Anyone who comes to CAMLS for continuing medical education can get a sense of that integration, said Dr. Hart, who also oversees the minimally invasive gynecologic surgery courses.
For instance, ob.gyns. might have the chance to practice their skills on a synthetic cadaver in the Surgical and Interventional Training Center. Then they could take a trip upstairs to the Virtual Patient Care Center, where they could continue working on high-fidelity human patient simulators and laparoscopic surgical simulators.
"That’s what makes us so exciting," Dr. Hart said.
Dr. Robert W. Yelverton, an ob.gyn. in Tampa, first became involved with CAMLS while the center was still under construction. Dr. Yelverton, who at the time was the chief medical officer for a large ob.gyn. group in central Florida, was looking for a place where his physicians could get simulator training to improve the quality and safety of robotic and minimally invasive gynecological procedures.
For example, some of their physicians hadn’t received training during residency on how to examine the bladder with a cystoscope following a gynecologic procedure. In the past, urologists had typically been the ones performing cystoscopy, so many ob.gyns weren’t trained. But with those roles changing, Dr. Yelverton wanted his physicians to be able to learn and perfect the procedure on a simulator, rather than on real patients in the operating room. With the bladder simulator at CAMLS, physicians were able to perform cystoscopy hundreds of times and see virtually every abnormal legion in a realistic fashion, he said.
"This is a huge attraction for physicians who really are looking for improvement in ways that they can perfect their surgical skills, particularly those that were introduced after they were in training," Dr. Yelverton said.
Dr. Yelverton, who is the chairman for the American Congress of Obstetricians and Gynecologists District XII, is continuing to work with CAMLS to set up training for ACOG’s Florida fellows as part of their educational meetings.
He said he expects many local physicians, and even some from other parts of the country, will want to try out the center. One of the attractions, he said, is the ability to conduct team training. For instance, a team of obstetricians and nurses can simulate emergencies, from shoulder dystocia to postpartum hemorrhage, in a mock labor and delivery suite.
Practicing physicians aren’t the only ones who can hone their skills at CAMLS. The center is also available for medical students and residents, as well as pharmacy and nursing students. The certified registered nurse anesthetist program is permanently housed in the building.
Even graduate business and engineering students drop in at CAMLS as part of their work with the Tampa Bay Research and Innovation Center. Coming to CAMLS means that engineering and business students get the chance to sit down with physicians and learn about the clinical problems driving the need for new technologies and devices, Dr. Hart said.
As part of the innovation work, Dr. Hart often presents a problem to the engineering students and then brings them to the operating room to see a simulated surgery first hand. The students then come up ideas for different devices that could help solve the problem.
"We go in with problems," he said. "We don’t go in and say, ‘I have an idea for a medical device.’ That’s actually the last thing we want to do."
As part of that process, Dr. Hart and his colleagues also work closely with industry on device development and commercialization. And the device and pharmaceutical industry is also a presence in other parts of CAMLS. Medical device and pharmaceutical companies come to the center to train their sales forces and their clients, said Deborah Sutherland, Ph.D., the CEO of CAMLS.
One of the reasons that CAMLS is able to offer its services to groups and individuals who are not affiliated with the University of South Florida is that the center is part of a not-for-profit corporation that includes USF Health.
CAMLS is run on a business model, not a traditional academic model, Dr. Sutherland said. CAMLS does not receive any financial support from the University of South Florida. All of the revenue comes instead from user fees.
"That is very unique because most simulation centers that you see nationally are supported by a clinical department," she said.
That type of approach may make CAMLS the envy of other simulation centers around the country, said Dr. Carol A. Aschenbrener, the chief medical education officer at the Association of American Medical Colleges.
Running a simulation center is costly, with the annual price tag ranging anywhere between $50,000 and $2.5 million, depending on the scope of the center and the staffing levels, she said. A 2010 survey conducted by the AAMC shows that most of these centers are funded either by a medical school or a teaching hospital. With those organizations under significant financial pressure, many are looking carefully at other ways to pay the bills. A handful of centers are actively developing new business models, she said, but it’s early on in the process. "So people are watching the South Florida center very closely," Dr. Aschenbrener said.
High-tech computer and robotic simulators are changing the way that obstetricians and gynecologists learn and maintain their skills. Now a new state-of-the-art simulation center in Tampa is changing the way academic medical centers offer this training.
With its modern architecture and gleaming glass exterior, the Center for Advanced Medical Learning and Simulation, located in downtown Tampa, looks like the type of building that houses cutting-edge technology.
The 90,000 square-foot-facility includes a surgical skills lab with more than 30 operating stations, an on-site tissue bank, a robotics suite with two da Vinci robots (S and Si), a synthetic cadaver, a 64-slice CT scanner, and a hybrid operating room. And those are just some of the offerings in the Surgical and Interventional Training Center.
The Center for Advanced Medical Learning and Simulation (CAMLS), which is affiliated with the University of South Florida, houses three other centers: the Virtual Patient Care Center, the Education Center, and the Tampa Bay Research and Innovation Center.
But it’s not the technology alone that sets CAMLS apart, said Dr. Stuart Hart, an ob.gyn. and urogynecologist who is the medical director for the Tampa Bay Research and Innovation Center.
"What makes it so unique is the tight integration among the various centers at CAMLS," he said.
The center, which opened in February 2012, has a lot of overlap among its education, training, and simulation programs. Anyone who comes to CAMLS for continuing medical education can get a sense of that integration, said Dr. Hart, who also oversees the minimally invasive gynecologic surgery courses.
For instance, ob.gyns. might have the chance to practice their skills on a synthetic cadaver in the Surgical and Interventional Training Center. Then they could take a trip upstairs to the Virtual Patient Care Center, where they could continue working on high-fidelity human patient simulators and laparoscopic surgical simulators.
"That’s what makes us so exciting," Dr. Hart said.
Dr. Robert W. Yelverton, an ob.gyn. in Tampa, first became involved with CAMLS while the center was still under construction. Dr. Yelverton, who at the time was the chief medical officer for a large ob.gyn. group in central Florida, was looking for a place where his physicians could get simulator training to improve the quality and safety of robotic and minimally invasive gynecological procedures.
For example, some of their physicians hadn’t received training during residency on how to examine the bladder with a cystoscope following a gynecologic procedure. In the past, urologists had typically been the ones performing cystoscopy, so many ob.gyns weren’t trained. But with those roles changing, Dr. Yelverton wanted his physicians to be able to learn and perfect the procedure on a simulator, rather than on real patients in the operating room. With the bladder simulator at CAMLS, physicians were able to perform cystoscopy hundreds of times and see virtually every abnormal legion in a realistic fashion, he said.
"This is a huge attraction for physicians who really are looking for improvement in ways that they can perfect their surgical skills, particularly those that were introduced after they were in training," Dr. Yelverton said.
Dr. Yelverton, who is the chairman for the American Congress of Obstetricians and Gynecologists District XII, is continuing to work with CAMLS to set up training for ACOG’s Florida fellows as part of their educational meetings.
He said he expects many local physicians, and even some from other parts of the country, will want to try out the center. One of the attractions, he said, is the ability to conduct team training. For instance, a team of obstetricians and nurses can simulate emergencies, from shoulder dystocia to postpartum hemorrhage, in a mock labor and delivery suite.
Practicing physicians aren’t the only ones who can hone their skills at CAMLS. The center is also available for medical students and residents, as well as pharmacy and nursing students. The certified registered nurse anesthetist program is permanently housed in the building.
Even graduate business and engineering students drop in at CAMLS as part of their work with the Tampa Bay Research and Innovation Center. Coming to CAMLS means that engineering and business students get the chance to sit down with physicians and learn about the clinical problems driving the need for new technologies and devices, Dr. Hart said.
As part of the innovation work, Dr. Hart often presents a problem to the engineering students and then brings them to the operating room to see a simulated surgery first hand. The students then come up ideas for different devices that could help solve the problem.
"We go in with problems," he said. "We don’t go in and say, ‘I have an idea for a medical device.’ That’s actually the last thing we want to do."
As part of that process, Dr. Hart and his colleagues also work closely with industry on device development and commercialization. And the device and pharmaceutical industry is also a presence in other parts of CAMLS. Medical device and pharmaceutical companies come to the center to train their sales forces and their clients, said Deborah Sutherland, Ph.D., the CEO of CAMLS.
One of the reasons that CAMLS is able to offer its services to groups and individuals who are not affiliated with the University of South Florida is that the center is part of a not-for-profit corporation that includes USF Health.
CAMLS is run on a business model, not a traditional academic model, Dr. Sutherland said. CAMLS does not receive any financial support from the University of South Florida. All of the revenue comes instead from user fees.
"That is very unique because most simulation centers that you see nationally are supported by a clinical department," she said.
That type of approach may make CAMLS the envy of other simulation centers around the country, said Dr. Carol A. Aschenbrener, the chief medical education officer at the Association of American Medical Colleges.
Running a simulation center is costly, with the annual price tag ranging anywhere between $50,000 and $2.5 million, depending on the scope of the center and the staffing levels, she said. A 2010 survey conducted by the AAMC shows that most of these centers are funded either by a medical school or a teaching hospital. With those organizations under significant financial pressure, many are looking carefully at other ways to pay the bills. A handful of centers are actively developing new business models, she said, but it’s early on in the process. "So people are watching the South Florida center very closely," Dr. Aschenbrener said.
Implementing Health Reform: Boosting clinical trial participation
Following the lead of Medicare and several states, the Affordable Care Act guarantees insurance coverage for individuals participating in clinical trials for the treatment of cancer and other life-threatening diseases.
Under the 2010 health law, health plans offering individual or group coverage cannot bar participation in clinical trials and cannot discriminate against patients who take part in trials. Health plans must cover the routine patient costs associated with participation in certain clinical trials. The plans do not, however, need to cover the investigational drug or device or services provided solely to satisfy data collection and analysis needs.
The policy applies to all phase I-IV clinical trials that are conducted for the prevention, detection, or treatment of cancer or other life-threatening diseases, including federally funded trials, investigational new drug applications reviewed by the Food and Drug Administration, or drug trials that are exempt from having an investigational new drug application.
The new federal policy, which takes effect on Jan. 1, 2014, sets a minimum standard of coverage and permits more expansive state coverage laws to continue.
Dr. Sandra M. Swain, president of the American Society of Clinical Oncology (ASCO), is an expert in the field of inflammatory breast cancer treatment and has led more than 20 clinical trials. She explained how the policy change is likely to impact clinical trial participation.
Question: How many states already mandate coverage of clinical trials and do the laws vary?
Dr. Swain: Twenty-nine states and the District of Columbia have laws and six states have voluntary agreements with insurers to provide coverage. The laws vary tremendously. The laws and agreements do not cover plans for self-insured, large-employer plans (or so-called ERISA plans) because they are regulated by federal, not state law.
Question: Will this new federal policy follow Medicare’s example and covering the treatment of complications in clinical trials?
Dr. Swain: The ACA statute does not specifically mention coverage of complications. ASCO led a coalition of 19 cancer organizations in advocating for the Centers for Medicare and Medicaid Services (CMS) – the federal agency in charge of drafting the implementing regulations – to require in those regulations that insurers cover complications. The coalition submitted proposed regulatory language on this and a number of other issues and met with CMS. We are waiting on the draft regulations.
Question: Is the current lack of insurance coverage for clinical trials a significant barrier to participation?
Dr. Swain: Our members have cited this as a major concern. Health plans do not always deny coverage, but they often don’t make coverage explicit and there is a lot of paperwork and time delays. This can make it difficult for patients to enroll in trials in a timely manner. Some patients also choose not to consider trial participation when they learn that their health plan may not provide coverage. An analysis from Johns Hopkins University, Baltimore, provides the most recent data.
Question: Since this doesn’t apply to grandfathered health plans, how much of an impact is it likely to have?
Dr. Swain: When the Office of Management and Budget released a rule on grandfathered plans in June 2010, it also estimated how many plans would relinquish their grandfathered status by 2013. The conservative estimate is 39% while the high-end estimate is 69%. As time goes on, the number of plans that lose their status will increase, thereby also increasing the effect of the provision.
Question: What will the impact be on cancer research and patients?
Dr. Swain: We’re hoping it will help make it easier to participate in clinical trials. Perhaps our outreach to ASCO members and patients about the provision will increase awareness. Anything that makes it easier to participate in research will ultimately help bring new treatments to our patients.
Question: What will need to be addressed when the Department of Health and Human Services issues regulations on this provision?
Dr. Swain: The statutory language about which trials are covered is very clear. Federally funded trials (including those funded by Cooperative Groups and National Cancer Institute–designated oncology centers) for the prevention, detection, or treatment of cancer are covered – including all phases of trials (I-IV). In addition, these same types of trials that are privately sponsored are covered if they are regulated by the FDA under an investigational new drug (INDA) application or if they meet requirements to be INDA exempt. We are working with the federal government to make the coverage process as timely and straightforward as possible. We developed a standard form that could be sent to any insurer to confirm that a trial meets the coverage requirements. We are hopeful that the federal government will promote use of this type of streamlined process. It is crucial that we help patients obtain a clear coverage answer as quickly as possible.
Dr. Swain is the president of ASCO and the medical director of the Washington Cancer Institute at the MedStar Washington Hospital Center.
Following the lead of Medicare and several states, the Affordable Care Act guarantees insurance coverage for individuals participating in clinical trials for the treatment of cancer and other life-threatening diseases.
Under the 2010 health law, health plans offering individual or group coverage cannot bar participation in clinical trials and cannot discriminate against patients who take part in trials. Health plans must cover the routine patient costs associated with participation in certain clinical trials. The plans do not, however, need to cover the investigational drug or device or services provided solely to satisfy data collection and analysis needs.
The policy applies to all phase I-IV clinical trials that are conducted for the prevention, detection, or treatment of cancer or other life-threatening diseases, including federally funded trials, investigational new drug applications reviewed by the Food and Drug Administration, or drug trials that are exempt from having an investigational new drug application.
The new federal policy, which takes effect on Jan. 1, 2014, sets a minimum standard of coverage and permits more expansive state coverage laws to continue.
Dr. Sandra M. Swain, president of the American Society of Clinical Oncology (ASCO), is an expert in the field of inflammatory breast cancer treatment and has led more than 20 clinical trials. She explained how the policy change is likely to impact clinical trial participation.
Question: How many states already mandate coverage of clinical trials and do the laws vary?
Dr. Swain: Twenty-nine states and the District of Columbia have laws and six states have voluntary agreements with insurers to provide coverage. The laws vary tremendously. The laws and agreements do not cover plans for self-insured, large-employer plans (or so-called ERISA plans) because they are regulated by federal, not state law.
Question: Will this new federal policy follow Medicare’s example and covering the treatment of complications in clinical trials?
Dr. Swain: The ACA statute does not specifically mention coverage of complications. ASCO led a coalition of 19 cancer organizations in advocating for the Centers for Medicare and Medicaid Services (CMS) – the federal agency in charge of drafting the implementing regulations – to require in those regulations that insurers cover complications. The coalition submitted proposed regulatory language on this and a number of other issues and met with CMS. We are waiting on the draft regulations.
Question: Is the current lack of insurance coverage for clinical trials a significant barrier to participation?
Dr. Swain: Our members have cited this as a major concern. Health plans do not always deny coverage, but they often don’t make coverage explicit and there is a lot of paperwork and time delays. This can make it difficult for patients to enroll in trials in a timely manner. Some patients also choose not to consider trial participation when they learn that their health plan may not provide coverage. An analysis from Johns Hopkins University, Baltimore, provides the most recent data.
Question: Since this doesn’t apply to grandfathered health plans, how much of an impact is it likely to have?
Dr. Swain: When the Office of Management and Budget released a rule on grandfathered plans in June 2010, it also estimated how many plans would relinquish their grandfathered status by 2013. The conservative estimate is 39% while the high-end estimate is 69%. As time goes on, the number of plans that lose their status will increase, thereby also increasing the effect of the provision.
Question: What will the impact be on cancer research and patients?
Dr. Swain: We’re hoping it will help make it easier to participate in clinical trials. Perhaps our outreach to ASCO members and patients about the provision will increase awareness. Anything that makes it easier to participate in research will ultimately help bring new treatments to our patients.
Question: What will need to be addressed when the Department of Health and Human Services issues regulations on this provision?
Dr. Swain: The statutory language about which trials are covered is very clear. Federally funded trials (including those funded by Cooperative Groups and National Cancer Institute–designated oncology centers) for the prevention, detection, or treatment of cancer are covered – including all phases of trials (I-IV). In addition, these same types of trials that are privately sponsored are covered if they are regulated by the FDA under an investigational new drug (INDA) application or if they meet requirements to be INDA exempt. We are working with the federal government to make the coverage process as timely and straightforward as possible. We developed a standard form that could be sent to any insurer to confirm that a trial meets the coverage requirements. We are hopeful that the federal government will promote use of this type of streamlined process. It is crucial that we help patients obtain a clear coverage answer as quickly as possible.
Dr. Swain is the president of ASCO and the medical director of the Washington Cancer Institute at the MedStar Washington Hospital Center.
Following the lead of Medicare and several states, the Affordable Care Act guarantees insurance coverage for individuals participating in clinical trials for the treatment of cancer and other life-threatening diseases.
Under the 2010 health law, health plans offering individual or group coverage cannot bar participation in clinical trials and cannot discriminate against patients who take part in trials. Health plans must cover the routine patient costs associated with participation in certain clinical trials. The plans do not, however, need to cover the investigational drug or device or services provided solely to satisfy data collection and analysis needs.
The policy applies to all phase I-IV clinical trials that are conducted for the prevention, detection, or treatment of cancer or other life-threatening diseases, including federally funded trials, investigational new drug applications reviewed by the Food and Drug Administration, or drug trials that are exempt from having an investigational new drug application.
The new federal policy, which takes effect on Jan. 1, 2014, sets a minimum standard of coverage and permits more expansive state coverage laws to continue.
Dr. Sandra M. Swain, president of the American Society of Clinical Oncology (ASCO), is an expert in the field of inflammatory breast cancer treatment and has led more than 20 clinical trials. She explained how the policy change is likely to impact clinical trial participation.
Question: How many states already mandate coverage of clinical trials and do the laws vary?
Dr. Swain: Twenty-nine states and the District of Columbia have laws and six states have voluntary agreements with insurers to provide coverage. The laws vary tremendously. The laws and agreements do not cover plans for self-insured, large-employer plans (or so-called ERISA plans) because they are regulated by federal, not state law.
Question: Will this new federal policy follow Medicare’s example and covering the treatment of complications in clinical trials?
Dr. Swain: The ACA statute does not specifically mention coverage of complications. ASCO led a coalition of 19 cancer organizations in advocating for the Centers for Medicare and Medicaid Services (CMS) – the federal agency in charge of drafting the implementing regulations – to require in those regulations that insurers cover complications. The coalition submitted proposed regulatory language on this and a number of other issues and met with CMS. We are waiting on the draft regulations.
Question: Is the current lack of insurance coverage for clinical trials a significant barrier to participation?
Dr. Swain: Our members have cited this as a major concern. Health plans do not always deny coverage, but they often don’t make coverage explicit and there is a lot of paperwork and time delays. This can make it difficult for patients to enroll in trials in a timely manner. Some patients also choose not to consider trial participation when they learn that their health plan may not provide coverage. An analysis from Johns Hopkins University, Baltimore, provides the most recent data.
Question: Since this doesn’t apply to grandfathered health plans, how much of an impact is it likely to have?
Dr. Swain: When the Office of Management and Budget released a rule on grandfathered plans in June 2010, it also estimated how many plans would relinquish their grandfathered status by 2013. The conservative estimate is 39% while the high-end estimate is 69%. As time goes on, the number of plans that lose their status will increase, thereby also increasing the effect of the provision.
Question: What will the impact be on cancer research and patients?
Dr. Swain: We’re hoping it will help make it easier to participate in clinical trials. Perhaps our outreach to ASCO members and patients about the provision will increase awareness. Anything that makes it easier to participate in research will ultimately help bring new treatments to our patients.
Question: What will need to be addressed when the Department of Health and Human Services issues regulations on this provision?
Dr. Swain: The statutory language about which trials are covered is very clear. Federally funded trials (including those funded by Cooperative Groups and National Cancer Institute–designated oncology centers) for the prevention, detection, or treatment of cancer are covered – including all phases of trials (I-IV). In addition, these same types of trials that are privately sponsored are covered if they are regulated by the FDA under an investigational new drug (INDA) application or if they meet requirements to be INDA exempt. We are working with the federal government to make the coverage process as timely and straightforward as possible. We developed a standard form that could be sent to any insurer to confirm that a trial meets the coverage requirements. We are hopeful that the federal government will promote use of this type of streamlined process. It is crucial that we help patients obtain a clear coverage answer as quickly as possible.
Dr. Swain is the president of ASCO and the medical director of the Washington Cancer Institute at the MedStar Washington Hospital Center.
Feds get specific on ACA individual mandate rules
After years of legal wrangling and a showdown in front of the Supreme Court, the federal government has finally begun to implement the Affordable Care Act’s controversial individual insurance mandate.
Starting on Jan. 1, 2014, Americans will have a choice: Buy basic health insurance, qualify for an exemption, or pay a penalty when filing federal income taxes, according to proposed regulations issued Jan. 30 by the Treasury Department and the Health and Human Services Department.
Individuals will be able to meet the requirement to for "minimum essential coverage" through a government-sponsored program, an employer-sponsored plan, an individual health plan, or a grandfathered health plan. HHS also is working on regulations to designate other coverage options, according to the proposed regulation.
Individuals will not have to pay a penalty if they can’t find affordable insurance or if they spend less than 3 consecutive months without coverage. The federal government will offer "hardship" exemptions for individuals who would be eligible for Medicaid under the expansion outlined in the Affordable Care Act (ACA) and who live in states that are not expanding eligibility.
Under the Treasury department proposed regulation, individuals would be considered covered for a month as long as they were covered for a single day in that month.
The federal government also proposes to grant exemptions for people with religious objections, members of Indian tribes, taxpayers with income below the income tax filing threshold, members of a health care sharing ministry, and the incarcerated.
The proposed rules are aimed at ensuring that only a "limited group of taxpayers who choose to spend a substantial period of time without coverage despite having ready access to affordable coverage" will have to pay the penalty, according to an HHS fact sheet.
Based on data from the Congressional Budget Office, HHS officials estimate that less than 2% of Americans actually will be required to pay a penalty.
Comments on the proposed regulation from the Treasury Department are due by May 2. Comments on the HHS proposal are due by March 18. Both proposed regulations reference a public meeting on the proposals to be held on May 29.
After years of legal wrangling and a showdown in front of the Supreme Court, the federal government has finally begun to implement the Affordable Care Act’s controversial individual insurance mandate.
Starting on Jan. 1, 2014, Americans will have a choice: Buy basic health insurance, qualify for an exemption, or pay a penalty when filing federal income taxes, according to proposed regulations issued Jan. 30 by the Treasury Department and the Health and Human Services Department.
Individuals will be able to meet the requirement to for "minimum essential coverage" through a government-sponsored program, an employer-sponsored plan, an individual health plan, or a grandfathered health plan. HHS also is working on regulations to designate other coverage options, according to the proposed regulation.
Individuals will not have to pay a penalty if they can’t find affordable insurance or if they spend less than 3 consecutive months without coverage. The federal government will offer "hardship" exemptions for individuals who would be eligible for Medicaid under the expansion outlined in the Affordable Care Act (ACA) and who live in states that are not expanding eligibility.
Under the Treasury department proposed regulation, individuals would be considered covered for a month as long as they were covered for a single day in that month.
The federal government also proposes to grant exemptions for people with religious objections, members of Indian tribes, taxpayers with income below the income tax filing threshold, members of a health care sharing ministry, and the incarcerated.
The proposed rules are aimed at ensuring that only a "limited group of taxpayers who choose to spend a substantial period of time without coverage despite having ready access to affordable coverage" will have to pay the penalty, according to an HHS fact sheet.
Based on data from the Congressional Budget Office, HHS officials estimate that less than 2% of Americans actually will be required to pay a penalty.
Comments on the proposed regulation from the Treasury Department are due by May 2. Comments on the HHS proposal are due by March 18. Both proposed regulations reference a public meeting on the proposals to be held on May 29.
After years of legal wrangling and a showdown in front of the Supreme Court, the federal government has finally begun to implement the Affordable Care Act’s controversial individual insurance mandate.
Starting on Jan. 1, 2014, Americans will have a choice: Buy basic health insurance, qualify for an exemption, or pay a penalty when filing federal income taxes, according to proposed regulations issued Jan. 30 by the Treasury Department and the Health and Human Services Department.
Individuals will be able to meet the requirement to for "minimum essential coverage" through a government-sponsored program, an employer-sponsored plan, an individual health plan, or a grandfathered health plan. HHS also is working on regulations to designate other coverage options, according to the proposed regulation.
Individuals will not have to pay a penalty if they can’t find affordable insurance or if they spend less than 3 consecutive months without coverage. The federal government will offer "hardship" exemptions for individuals who would be eligible for Medicaid under the expansion outlined in the Affordable Care Act (ACA) and who live in states that are not expanding eligibility.
Under the Treasury department proposed regulation, individuals would be considered covered for a month as long as they were covered for a single day in that month.
The federal government also proposes to grant exemptions for people with religious objections, members of Indian tribes, taxpayers with income below the income tax filing threshold, members of a health care sharing ministry, and the incarcerated.
The proposed rules are aimed at ensuring that only a "limited group of taxpayers who choose to spend a substantial period of time without coverage despite having ready access to affordable coverage" will have to pay the penalty, according to an HHS fact sheet.
Based on data from the Congressional Budget Office, HHS officials estimate that less than 2% of Americans actually will be required to pay a penalty.
Comments on the proposed regulation from the Treasury Department are due by May 2. Comments on the HHS proposal are due by March 18. Both proposed regulations reference a public meeting on the proposals to be held on May 29.
Poll: Public doesn't see cancer as a death sentence
People are optimistic about their chances of surviving cancer, according to a poll conducted in the United States and five other wealthy nations.
Among respondents in all six countries, 48% said they did not believe that cancer always leads to death, while 32% said they see cancer as a death sentence; the remainder did not know or didn’t have an opinion. Those polled in the United States had the sunniest outlook. About 65% of U.S. respondents said they do not believe that cancer always leads to death.
The survey, which was commissioned by Lilly Oncology, polled the general public, cancer patients, and caregivers in the United States, France, Germany, Italy, Japan, and the United Kingdom, on their knowledge and attitudes about cancer. The telephone survey included responses from 4,341 adults, with 3,009 from the general public, 663 from cancer patients, and 669 from caregivers.
The finding that the public sees cancer as a disease that can be beat was both surprising and encouraging, Newton F. Crenshaw, vice president of Lilly Oncology, said during a press briefing Jan. 30.
"We know that there have been important advances in cancer care across the varieties of cancer." Mr. Crenshaw said. "But in many cases, we’re seeing cancer not become a death sentence, but move more toward a chronic disease, something that can be managed over time."
While patients may be optimistic, they aren’t always well informed about the disease or what goes into producing treatments.
For example, a sizable minority (43%) across the six countries surveyed said they think that cancer is a single disease; 51% correctly answered that cancer is many different diseases that can appear in different parts of the body.
The public also tends to underestimate the time and money required to bring new cancer drugs to the market.
On average, across the six countries surveyed, 44% of respondents said they believe it takes less than 10 years to bring a cancer drug to market, 28% think that it takes exactly 10 years, and only 18% said that it takes more than 10 years. In fact, industry experts say that it takes on average 10-15 years to bring a new drug to market and that many fail during the process.
The same is true with the cost. Two-thirds or more in each country surveyed underestimated the cost of bringing a new cancer drug to the marketplace, she said. For instance, in the United States, 74% of those surveyed said that it costs $100 million or less to develop a new cancer drug, while industry estimates put that figure closer to $1.2 billion.
But the public has a "relatively nuanced understanding" of how cancer treatment works, the survey found. About 62% of the public across the six countries surveyed said that cancer medication results can differ by individual, even when patients have similar diagnoses.
When it comes to clinical trials to test new medicines, the public appears willing to participate, especially if it will give them better access to treatments. For instance, in the United States, 74% of respondents said they would participate in a clinical trial if it would improve the hope of receiving life-extending treatment. Seventy-two percent said they would participate if it would improve the likelihood of helping future patients. But willingness to take part in a clinical trial declined when it became inconvenient or costly, according to the survey results.
People are optimistic about their chances of surviving cancer, according to a poll conducted in the United States and five other wealthy nations.
Among respondents in all six countries, 48% said they did not believe that cancer always leads to death, while 32% said they see cancer as a death sentence; the remainder did not know or didn’t have an opinion. Those polled in the United States had the sunniest outlook. About 65% of U.S. respondents said they do not believe that cancer always leads to death.
The survey, which was commissioned by Lilly Oncology, polled the general public, cancer patients, and caregivers in the United States, France, Germany, Italy, Japan, and the United Kingdom, on their knowledge and attitudes about cancer. The telephone survey included responses from 4,341 adults, with 3,009 from the general public, 663 from cancer patients, and 669 from caregivers.
The finding that the public sees cancer as a disease that can be beat was both surprising and encouraging, Newton F. Crenshaw, vice president of Lilly Oncology, said during a press briefing Jan. 30.
"We know that there have been important advances in cancer care across the varieties of cancer." Mr. Crenshaw said. "But in many cases, we’re seeing cancer not become a death sentence, but move more toward a chronic disease, something that can be managed over time."
While patients may be optimistic, they aren’t always well informed about the disease or what goes into producing treatments.
For example, a sizable minority (43%) across the six countries surveyed said they think that cancer is a single disease; 51% correctly answered that cancer is many different diseases that can appear in different parts of the body.
The public also tends to underestimate the time and money required to bring new cancer drugs to the market.
On average, across the six countries surveyed, 44% of respondents said they believe it takes less than 10 years to bring a cancer drug to market, 28% think that it takes exactly 10 years, and only 18% said that it takes more than 10 years. In fact, industry experts say that it takes on average 10-15 years to bring a new drug to market and that many fail during the process.
The same is true with the cost. Two-thirds or more in each country surveyed underestimated the cost of bringing a new cancer drug to the marketplace, she said. For instance, in the United States, 74% of those surveyed said that it costs $100 million or less to develop a new cancer drug, while industry estimates put that figure closer to $1.2 billion.
But the public has a "relatively nuanced understanding" of how cancer treatment works, the survey found. About 62% of the public across the six countries surveyed said that cancer medication results can differ by individual, even when patients have similar diagnoses.
When it comes to clinical trials to test new medicines, the public appears willing to participate, especially if it will give them better access to treatments. For instance, in the United States, 74% of respondents said they would participate in a clinical trial if it would improve the hope of receiving life-extending treatment. Seventy-two percent said they would participate if it would improve the likelihood of helping future patients. But willingness to take part in a clinical trial declined when it became inconvenient or costly, according to the survey results.
People are optimistic about their chances of surviving cancer, according to a poll conducted in the United States and five other wealthy nations.
Among respondents in all six countries, 48% said they did not believe that cancer always leads to death, while 32% said they see cancer as a death sentence; the remainder did not know or didn’t have an opinion. Those polled in the United States had the sunniest outlook. About 65% of U.S. respondents said they do not believe that cancer always leads to death.
The survey, which was commissioned by Lilly Oncology, polled the general public, cancer patients, and caregivers in the United States, France, Germany, Italy, Japan, and the United Kingdom, on their knowledge and attitudes about cancer. The telephone survey included responses from 4,341 adults, with 3,009 from the general public, 663 from cancer patients, and 669 from caregivers.
The finding that the public sees cancer as a disease that can be beat was both surprising and encouraging, Newton F. Crenshaw, vice president of Lilly Oncology, said during a press briefing Jan. 30.
"We know that there have been important advances in cancer care across the varieties of cancer." Mr. Crenshaw said. "But in many cases, we’re seeing cancer not become a death sentence, but move more toward a chronic disease, something that can be managed over time."
While patients may be optimistic, they aren’t always well informed about the disease or what goes into producing treatments.
For example, a sizable minority (43%) across the six countries surveyed said they think that cancer is a single disease; 51% correctly answered that cancer is many different diseases that can appear in different parts of the body.
The public also tends to underestimate the time and money required to bring new cancer drugs to the market.
On average, across the six countries surveyed, 44% of respondents said they believe it takes less than 10 years to bring a cancer drug to market, 28% think that it takes exactly 10 years, and only 18% said that it takes more than 10 years. In fact, industry experts say that it takes on average 10-15 years to bring a new drug to market and that many fail during the process.
The same is true with the cost. Two-thirds or more in each country surveyed underestimated the cost of bringing a new cancer drug to the marketplace, she said. For instance, in the United States, 74% of those surveyed said that it costs $100 million or less to develop a new cancer drug, while industry estimates put that figure closer to $1.2 billion.
But the public has a "relatively nuanced understanding" of how cancer treatment works, the survey found. About 62% of the public across the six countries surveyed said that cancer medication results can differ by individual, even when patients have similar diagnoses.
When it comes to clinical trials to test new medicines, the public appears willing to participate, especially if it will give them better access to treatments. For instance, in the United States, 74% of respondents said they would participate in a clinical trial if it would improve the hope of receiving life-extending treatment. Seventy-two percent said they would participate if it would improve the likelihood of helping future patients. But willingness to take part in a clinical trial declined when it became inconvenient or costly, according to the survey results.
ACC and AHA Release Electronic Data Standards
The American College of Cardiology and the American Heart Association are releasing a set of electronic data standards for managing acute coronary syndromes and coronary artery disease with the goal of making it easier to compare data across research studies and share data between electronic health record systems.
The new document includes a series of standardized terms and definitions across seven categories:
• Demographic and admission: patient’s sex, date of birth, race, source of admission, and payment type.
• History and risk factors: history of prior angina, previous history of heart failure, and date of prior coronary artery bypass grafting.
• Clinical presentation: date and time of symptom onset, heart rate, systolic blood pressure on first medical contact, height, and weight.
• Diagnostic procedure: rhythm determined by electrocardiography (ECG), site where first ECG was obtained, LDL value, HDL value, and glucose.
• Invasive therapeutic intervention: type of pacemaker implanted, data of noninvasive stress testing, artery responsible for acute coronary syndromes, percent of stenosis in the left main coronary artery.
• Medication: dose of anticoagulant administered, administration of beta-blocker in the first 24 hours, and prescription of aspirin at hospital discharge.
• Outcomes: death during hospitalization, occurrence of reinfarction, surgical intervention required for bleeding, and transfusion.
"We hope that these data definitions can advance research and clinical care, to increase the adoption of both proven old therapies and new innovations in cardiology," Dr. Christopher Cannon, chair of the writing committee and a cardiologist at Brigham and Women’s Hospital in Boston, said in a statement. "This advancement can support our ultimate goal – to improve outcomes for patients with cardiovascular disease."
The "2013 ACCF/AHA Key Elements and Data Definitions for Measuring the Clinical Management and Outcomes of Patients with Acute Coronary Syndromes and Coronary Artery Disease" was developed by a writing committee of physicians. Their work was supported by the ACC, the AHA, and 13 other medical organizations. There was no commercial support for the project.
The document will be published in the March 5 issue of the Journal of the American College of Cardiology and is available on the websites of both the ACC and the AHA.
The American College of Cardiology and the American Heart Association are releasing a set of electronic data standards for managing acute coronary syndromes and coronary artery disease with the goal of making it easier to compare data across research studies and share data between electronic health record systems.
The new document includes a series of standardized terms and definitions across seven categories:
• Demographic and admission: patient’s sex, date of birth, race, source of admission, and payment type.
• History and risk factors: history of prior angina, previous history of heart failure, and date of prior coronary artery bypass grafting.
• Clinical presentation: date and time of symptom onset, heart rate, systolic blood pressure on first medical contact, height, and weight.
• Diagnostic procedure: rhythm determined by electrocardiography (ECG), site where first ECG was obtained, LDL value, HDL value, and glucose.
• Invasive therapeutic intervention: type of pacemaker implanted, data of noninvasive stress testing, artery responsible for acute coronary syndromes, percent of stenosis in the left main coronary artery.
• Medication: dose of anticoagulant administered, administration of beta-blocker in the first 24 hours, and prescription of aspirin at hospital discharge.
• Outcomes: death during hospitalization, occurrence of reinfarction, surgical intervention required for bleeding, and transfusion.
"We hope that these data definitions can advance research and clinical care, to increase the adoption of both proven old therapies and new innovations in cardiology," Dr. Christopher Cannon, chair of the writing committee and a cardiologist at Brigham and Women’s Hospital in Boston, said in a statement. "This advancement can support our ultimate goal – to improve outcomes for patients with cardiovascular disease."
The "2013 ACCF/AHA Key Elements and Data Definitions for Measuring the Clinical Management and Outcomes of Patients with Acute Coronary Syndromes and Coronary Artery Disease" was developed by a writing committee of physicians. Their work was supported by the ACC, the AHA, and 13 other medical organizations. There was no commercial support for the project.
The document will be published in the March 5 issue of the Journal of the American College of Cardiology and is available on the websites of both the ACC and the AHA.
The American College of Cardiology and the American Heart Association are releasing a set of electronic data standards for managing acute coronary syndromes and coronary artery disease with the goal of making it easier to compare data across research studies and share data between electronic health record systems.
The new document includes a series of standardized terms and definitions across seven categories:
• Demographic and admission: patient’s sex, date of birth, race, source of admission, and payment type.
• History and risk factors: history of prior angina, previous history of heart failure, and date of prior coronary artery bypass grafting.
• Clinical presentation: date and time of symptom onset, heart rate, systolic blood pressure on first medical contact, height, and weight.
• Diagnostic procedure: rhythm determined by electrocardiography (ECG), site where first ECG was obtained, LDL value, HDL value, and glucose.
• Invasive therapeutic intervention: type of pacemaker implanted, data of noninvasive stress testing, artery responsible for acute coronary syndromes, percent of stenosis in the left main coronary artery.
• Medication: dose of anticoagulant administered, administration of beta-blocker in the first 24 hours, and prescription of aspirin at hospital discharge.
• Outcomes: death during hospitalization, occurrence of reinfarction, surgical intervention required for bleeding, and transfusion.
"We hope that these data definitions can advance research and clinical care, to increase the adoption of both proven old therapies and new innovations in cardiology," Dr. Christopher Cannon, chair of the writing committee and a cardiologist at Brigham and Women’s Hospital in Boston, said in a statement. "This advancement can support our ultimate goal – to improve outcomes for patients with cardiovascular disease."
The "2013 ACCF/AHA Key Elements and Data Definitions for Measuring the Clinical Management and Outcomes of Patients with Acute Coronary Syndromes and Coronary Artery Disease" was developed by a writing committee of physicians. Their work was supported by the ACC, the AHA, and 13 other medical organizations. There was no commercial support for the project.
The document will be published in the March 5 issue of the Journal of the American College of Cardiology and is available on the websites of both the ACC and the AHA.
Calif. hospitals support feds in quality goals
Nearly 400 California hospitals have pledged to lower preventable hospital-acquired conditions and hospital readmissions as part of a federal quality initiative.
More Golden State hospitals have agreed to participate in the federal Partnership for Patients initiative than any other state in the nation. The project, which is being led by the Centers for Medicare and Medicaid Services, aims to decrease preventable hospital-acquired conditions by 40% and hospital readmissions by 20% by the end of 2013. Officials at CMS estimate that achieving these goals will prevent more than 3.4 million injuries and complications nationwide.
"Under the Partnership for Patients initiative, we are providing support to help hospitals provide high-quality care and keep their patients healthy," Dr. Richard Gilfillan, director of the Center for Medicare and Medicaid Innovation, said in a statement. "Participating in this initiative will help California hospitals improve health outcomes and reduce complications for their patients."
Hospitals are getting some federal support under the initiative. The federal government has awarded $218 million to 26 organizations that are serving as Hospital Engagement Networks. These networks are developing learning collaboratives for hospitals, conducting training programs, providing technical assistance, identifying and disseminating best practices, and establishing systems for tracking and monitoring hospital progress in meeting quality improvement goals.
Nearly 400 California hospitals have pledged to lower preventable hospital-acquired conditions and hospital readmissions as part of a federal quality initiative.
More Golden State hospitals have agreed to participate in the federal Partnership for Patients initiative than any other state in the nation. The project, which is being led by the Centers for Medicare and Medicaid Services, aims to decrease preventable hospital-acquired conditions by 40% and hospital readmissions by 20% by the end of 2013. Officials at CMS estimate that achieving these goals will prevent more than 3.4 million injuries and complications nationwide.
"Under the Partnership for Patients initiative, we are providing support to help hospitals provide high-quality care and keep their patients healthy," Dr. Richard Gilfillan, director of the Center for Medicare and Medicaid Innovation, said in a statement. "Participating in this initiative will help California hospitals improve health outcomes and reduce complications for their patients."
Hospitals are getting some federal support under the initiative. The federal government has awarded $218 million to 26 organizations that are serving as Hospital Engagement Networks. These networks are developing learning collaboratives for hospitals, conducting training programs, providing technical assistance, identifying and disseminating best practices, and establishing systems for tracking and monitoring hospital progress in meeting quality improvement goals.
Nearly 400 California hospitals have pledged to lower preventable hospital-acquired conditions and hospital readmissions as part of a federal quality initiative.
More Golden State hospitals have agreed to participate in the federal Partnership for Patients initiative than any other state in the nation. The project, which is being led by the Centers for Medicare and Medicaid Services, aims to decrease preventable hospital-acquired conditions by 40% and hospital readmissions by 20% by the end of 2013. Officials at CMS estimate that achieving these goals will prevent more than 3.4 million injuries and complications nationwide.
"Under the Partnership for Patients initiative, we are providing support to help hospitals provide high-quality care and keep their patients healthy," Dr. Richard Gilfillan, director of the Center for Medicare and Medicaid Innovation, said in a statement. "Participating in this initiative will help California hospitals improve health outcomes and reduce complications for their patients."
Hospitals are getting some federal support under the initiative. The federal government has awarded $218 million to 26 organizations that are serving as Hospital Engagement Networks. These networks are developing learning collaboratives for hospitals, conducting training programs, providing technical assistance, identifying and disseminating best practices, and establishing systems for tracking and monitoring hospital progress in meeting quality improvement goals.
PCOS panel calls for classification, name changes
The term polycystic ovary syndrome, or PCOS, is confusing and needs to be changed to better explain the metabolic, adrenal, and other complications that are common in the condition, according to an independent panel of experts convened by the National Institutes of Health.
"It focuses on a criteria – namely the polycystic ovarian morphology – that is neither necessary nor sufficient to diagnose the syndrome," Dr. Robert A. Rizza, executive dean for research at the Mayo Clinic in Rochester, Minn., and a member of the panel, said at a teleconference. "We therefore believe it is time to assign a name that reflects the complex metabolic, hypothalamic, pituitary, ovarian, and adrenal interactions that characterize PCOS."
The four-member panel issued a report on Jan. 23 based on evidence presented during a workshop on PCOS held at the NIH last December.
The panel did not recommend a new name for PCOS but said that a broad group of clinicians, researchers, and patients should be able to quickly come up with a new label that is more inclusive. A name change may seem superficial, but a more descriptive label would help to highlight the importance of the syndrome for funding agencies, said Dr. Timothy R.B. Johnson, professor and chair of obstetrics and gynecology at the University of Michigan, Ann Arbor, and a member of the panel.
The expert panel also recommended changes to the criteria used to diagnose PCOS. Currently, clinicians and researchers rely on three different classification systems – the NIH Criteria, the Rotterdam Criteria, and the Androgen Excess and PCOS (AE-PCOS) Society Criteria. The panel instead recommended using the broad, inclusionary diagnostic Rotterdam Criteria to identify the specific phenotypes of PCOS, such as androgen excess plus ovulatory dysfunction, androgen excess plus polycystic ovarian morphology, ovulatory dysfunction plus polycystic ovarian morphology, or androgen excess plus ovulatory dysfunction plus polycystic ovarian morphology.
"The use of multiple classification systems to diagnose PCOS is confusing and delays progress in understanding of the disorder," Dr. Rizza said. "It also hinders the ability of clinicians to partner with women to address and manage the health issues that concern them."
The panel also called for improved methods and criteria to assess androgen excess, ovarian dysfunction, and polycystic ovarian morphology to help improve diagnosis.
The report also includes several recommendations for future research since there are still many unanswered questions about the role of metabolic dysfunction and the underlying pathophysiology of the condition.
The panel called for conducting large, multiethnic studies aimed at establishing the genetic or epigenetic causes of PCOS. Also needed are multiethnic longitudinal studies looking at the role of cardiovascular and diabetic complications. More research is needed to determine if PCOS is associated with endometrial, breast, and ovarian cancers.
Other studies should focus on the role of PCOS in pregnancy by establishing the prevalence of abnormal glucose tolerance in women trying to conceive and determining whether treatment of abnormal glucose tolerance prior to or early after conception alters maternal-fetal outcomes, the panel wrote.
The term polycystic ovary syndrome, or PCOS, is confusing and needs to be changed to better explain the metabolic, adrenal, and other complications that are common in the condition, according to an independent panel of experts convened by the National Institutes of Health.
"It focuses on a criteria – namely the polycystic ovarian morphology – that is neither necessary nor sufficient to diagnose the syndrome," Dr. Robert A. Rizza, executive dean for research at the Mayo Clinic in Rochester, Minn., and a member of the panel, said at a teleconference. "We therefore believe it is time to assign a name that reflects the complex metabolic, hypothalamic, pituitary, ovarian, and adrenal interactions that characterize PCOS."
The four-member panel issued a report on Jan. 23 based on evidence presented during a workshop on PCOS held at the NIH last December.
The panel did not recommend a new name for PCOS but said that a broad group of clinicians, researchers, and patients should be able to quickly come up with a new label that is more inclusive. A name change may seem superficial, but a more descriptive label would help to highlight the importance of the syndrome for funding agencies, said Dr. Timothy R.B. Johnson, professor and chair of obstetrics and gynecology at the University of Michigan, Ann Arbor, and a member of the panel.
The expert panel also recommended changes to the criteria used to diagnose PCOS. Currently, clinicians and researchers rely on three different classification systems – the NIH Criteria, the Rotterdam Criteria, and the Androgen Excess and PCOS (AE-PCOS) Society Criteria. The panel instead recommended using the broad, inclusionary diagnostic Rotterdam Criteria to identify the specific phenotypes of PCOS, such as androgen excess plus ovulatory dysfunction, androgen excess plus polycystic ovarian morphology, ovulatory dysfunction plus polycystic ovarian morphology, or androgen excess plus ovulatory dysfunction plus polycystic ovarian morphology.
"The use of multiple classification systems to diagnose PCOS is confusing and delays progress in understanding of the disorder," Dr. Rizza said. "It also hinders the ability of clinicians to partner with women to address and manage the health issues that concern them."
The panel also called for improved methods and criteria to assess androgen excess, ovarian dysfunction, and polycystic ovarian morphology to help improve diagnosis.
The report also includes several recommendations for future research since there are still many unanswered questions about the role of metabolic dysfunction and the underlying pathophysiology of the condition.
The panel called for conducting large, multiethnic studies aimed at establishing the genetic or epigenetic causes of PCOS. Also needed are multiethnic longitudinal studies looking at the role of cardiovascular and diabetic complications. More research is needed to determine if PCOS is associated with endometrial, breast, and ovarian cancers.
Other studies should focus on the role of PCOS in pregnancy by establishing the prevalence of abnormal glucose tolerance in women trying to conceive and determining whether treatment of abnormal glucose tolerance prior to or early after conception alters maternal-fetal outcomes, the panel wrote.
The term polycystic ovary syndrome, or PCOS, is confusing and needs to be changed to better explain the metabolic, adrenal, and other complications that are common in the condition, according to an independent panel of experts convened by the National Institutes of Health.
"It focuses on a criteria – namely the polycystic ovarian morphology – that is neither necessary nor sufficient to diagnose the syndrome," Dr. Robert A. Rizza, executive dean for research at the Mayo Clinic in Rochester, Minn., and a member of the panel, said at a teleconference. "We therefore believe it is time to assign a name that reflects the complex metabolic, hypothalamic, pituitary, ovarian, and adrenal interactions that characterize PCOS."
The four-member panel issued a report on Jan. 23 based on evidence presented during a workshop on PCOS held at the NIH last December.
The panel did not recommend a new name for PCOS but said that a broad group of clinicians, researchers, and patients should be able to quickly come up with a new label that is more inclusive. A name change may seem superficial, but a more descriptive label would help to highlight the importance of the syndrome for funding agencies, said Dr. Timothy R.B. Johnson, professor and chair of obstetrics and gynecology at the University of Michigan, Ann Arbor, and a member of the panel.
The expert panel also recommended changes to the criteria used to diagnose PCOS. Currently, clinicians and researchers rely on three different classification systems – the NIH Criteria, the Rotterdam Criteria, and the Androgen Excess and PCOS (AE-PCOS) Society Criteria. The panel instead recommended using the broad, inclusionary diagnostic Rotterdam Criteria to identify the specific phenotypes of PCOS, such as androgen excess plus ovulatory dysfunction, androgen excess plus polycystic ovarian morphology, ovulatory dysfunction plus polycystic ovarian morphology, or androgen excess plus ovulatory dysfunction plus polycystic ovarian morphology.
"The use of multiple classification systems to diagnose PCOS is confusing and delays progress in understanding of the disorder," Dr. Rizza said. "It also hinders the ability of clinicians to partner with women to address and manage the health issues that concern them."
The panel also called for improved methods and criteria to assess androgen excess, ovarian dysfunction, and polycystic ovarian morphology to help improve diagnosis.
The report also includes several recommendations for future research since there are still many unanswered questions about the role of metabolic dysfunction and the underlying pathophysiology of the condition.
The panel called for conducting large, multiethnic studies aimed at establishing the genetic or epigenetic causes of PCOS. Also needed are multiethnic longitudinal studies looking at the role of cardiovascular and diabetic complications. More research is needed to determine if PCOS is associated with endometrial, breast, and ovarian cancers.
Other studies should focus on the role of PCOS in pregnancy by establishing the prevalence of abnormal glucose tolerance in women trying to conceive and determining whether treatment of abnormal glucose tolerance prior to or early after conception alters maternal-fetal outcomes, the panel wrote.
2013 outlook: possible SGR action
Could 2013 finally be the year to eliminate the Sustainable Growth Rate formula?
Officials at the American Medical Association say there's a chance that Congress could decide to permanently scrap the unpopular formula, which drives payment under the Medicare physician fee schedule, as part of a larger deal to cut the federal deficit.
"The fact that we've got this big potential deficit-reduction package would make us more optimistic that we can get [the SGR] taken care of this coming year," said Dr. Jeremy A. Lazarus, president of the American Medical Association .
On Jan. 1, lawmakers passed legislation providing a short-term, 1-year delay to the scheduled 26.5% SGR cut. The bill also included a 2-month delay to scheduled tax hikes and federal spending cuts that were planned as part of a deficit reduction process known as sequestration. That gives Congress several weeks to craft a new plan to deal with the nation's debt and the growth in Medicare spending.
It wouldn't be unprecedented for a permanent SGR fix to be considered as part of comprehensive deficit reduction legislation. SGR repeal was included in bipartisan plans created by outside groups several times, including the Simpson-Bowles Commission, the Senate Gang of Six, and others, Dr. Lazarus said.
Although complete SGR repeal carries a 10-year price tag of nearly $300 billion, physicians argue that, since Congress always acts to avert the pay cuts triggered by the formula, the federal government does not save any money by keeping it on the books. The large cost of repeal, however, means that it may be easier to get the SGR fix inserted into a larger bill than to get lawmakers to approve it separately, Dr. Lazarus said.
The AMA is asking Congress to not only repeal the SGR but also to establish a period of stable Medicare payments so that physicians can begin to transition to a new payment system that focuses on quality of care, Dr. Lazarus said. In the meantime, the AMA and other groups have been working on developing new delivery and payment reform options that could offer an alternative to the current fee for service system.
"We do hope we can start changing the equation on reimbursement and going from fee for service to accounting for quality," said Dr. William A. Zoghbi, president of the American College of Cardiology.
ACC officials are eager to move away from the SGR but they are concerned about where the money to do so might come from. Dr. Zoghbi said that he doesn't want to see lawmakers robbing other health care priorities to pay for the fix. For instance, in December, lawmakers considered a proposal to pay for a 1-year SGR fix using money that was slated for increasing Medicaid payments to physicians providing primary care services. Instead, lawmakers financed the one-year SGR fix mainly through cuts to hospital payments.
"These fixes cannot be on the backs of the professionals providing care," Dr. Zoghbi said.
ACA milestones
This year also will see some practice-impacting milestones under the Affordable Care Act.
Federal money now helps pay for preventive services for Medicaid patients, and many primary care services provided under Medicaid now are paid at the higher Medicare rate. Under the ACA, Medicaid payment increases to 100% of Medicare rates for family physicians, internists, and pediatricians when they provide certain primary care services. Subspecialists in these areas are also eligible for increased payments. The pay hike is for 2013 and 2014.
The law also provides an additional 2 years of funding to the Children's Health Insurance Program to continue coverage for those children eligible under the Medicaid program.
The Independent Payment Advisory Board is slated to start work this year, even though its members have yet to be named by President Obama. The controversial 15-member panel is charged with making recommendations on how to reduce Medicare spending. Dr. Lazarus said the AMA will continue to work toward eliminating the IPAB.
Some of the biggest changes under the ACA -- the expansion of Medicaid eligibility and the creation of state-based health insurance exchanges -- are coming in 2014, but physician leaders said that doctors need to start preparing this year.
Exactly how to get ready will vary by state since both the Medicaid expansion and the exchanges will be largely state-run.
The AMA is pushing to give physicians greater say by getting them seats on the boards of state exchanges. But even as physicians await more information on these changes, they can prepare by becoming more familiar with the Medicaid program since they are likely to see more of those patients, said Robert Doherty, senior vice president for governmental affairs and public policy at the American College of Physicians.
Penalties kick in
This year the Physician Quality Reporting System (PQRS) transitions from a pure incentive program to a mixed incentive/disincentive program. Previously, PQRS offered small bonus payments to physicians for successfully reporting on quality measures. Now, physicians who don't participate in the program will be assessed a penalty. The 1.5% cut to Medicare fees won't come until 2015, but it will be based on participation this year. Physicians will see a 2% penalty in 2016 if they don't successfully report data during 2014.
"People don't realize that if they get past 2013, they won't have an opportunity to fix it for the next year," said Dr. Bruce Bagley, medical director for quality improvement at the American Academy of Family Physicians.
There are also penalties coming in Medicare's Electronic Prescribing (eRx) Incentive Program. To avoid a 2% penalty in 2014, physicians must meet Medicare's e-prescribing requirements by June 30, 2013.
Penalties from the Medicare Electronic Health Record (EHR) Incentive Program aren't coming until 2015, but Dr. Bagley said that physicians should take a good look at this program now to try to earn some money to offset the cost of EHR implementation.
"The sooner you get going on this stuff, the better," he said.
A physician who starts participating this year can earn up to $39,000 over 4 years. Start next year and the bonus drops to $24,000. A 1% penalty takes effect in 2015, increasing to 2% the following year.
The transition to the ICD-10 coding set is another requirement that physicians need to keep in mind, ACP's Mr. Doherty said. The Department of Health and Human Services delayed the move to ICD-10 until October 2014, but Mr. Doherty said physicians can't afford to wait that long to prepare.
The ACP is trying to convince federal officials to accept some alternative ways of coding that would both satisfy the ICD-10 requirements and be clinically relevant, he said.
Primary care gets a boost
Overall, the outlook for 2013 will probably vary by specialty. The 2013 Medicare Physician Fee Schedule dealt some tough blows to subspecialists, making deep payment cuts in interventional cardiology, neurology, and oncology.
Coding changes in primary care, though, could bolster that field, experts said.
"There's never been a time when so many people from so many quarters recognize the value of primary care," Dr. Bagley said.
Could 2013 finally be the year to eliminate the Sustainable Growth Rate formula?
Officials at the American Medical Association say there's a chance that Congress could decide to permanently scrap the unpopular formula, which drives payment under the Medicare physician fee schedule, as part of a larger deal to cut the federal deficit.
"The fact that we've got this big potential deficit-reduction package would make us more optimistic that we can get [the SGR] taken care of this coming year," said Dr. Jeremy A. Lazarus, president of the American Medical Association .
On Jan. 1, lawmakers passed legislation providing a short-term, 1-year delay to the scheduled 26.5% SGR cut. The bill also included a 2-month delay to scheduled tax hikes and federal spending cuts that were planned as part of a deficit reduction process known as sequestration. That gives Congress several weeks to craft a new plan to deal with the nation's debt and the growth in Medicare spending.
It wouldn't be unprecedented for a permanent SGR fix to be considered as part of comprehensive deficit reduction legislation. SGR repeal was included in bipartisan plans created by outside groups several times, including the Simpson-Bowles Commission, the Senate Gang of Six, and others, Dr. Lazarus said.
Although complete SGR repeal carries a 10-year price tag of nearly $300 billion, physicians argue that, since Congress always acts to avert the pay cuts triggered by the formula, the federal government does not save any money by keeping it on the books. The large cost of repeal, however, means that it may be easier to get the SGR fix inserted into a larger bill than to get lawmakers to approve it separately, Dr. Lazarus said.
The AMA is asking Congress to not only repeal the SGR but also to establish a period of stable Medicare payments so that physicians can begin to transition to a new payment system that focuses on quality of care, Dr. Lazarus said. In the meantime, the AMA and other groups have been working on developing new delivery and payment reform options that could offer an alternative to the current fee for service system.
"We do hope we can start changing the equation on reimbursement and going from fee for service to accounting for quality," said Dr. William A. Zoghbi, president of the American College of Cardiology.
ACC officials are eager to move away from the SGR but they are concerned about where the money to do so might come from. Dr. Zoghbi said that he doesn't want to see lawmakers robbing other health care priorities to pay for the fix. For instance, in December, lawmakers considered a proposal to pay for a 1-year SGR fix using money that was slated for increasing Medicaid payments to physicians providing primary care services. Instead, lawmakers financed the one-year SGR fix mainly through cuts to hospital payments.
"These fixes cannot be on the backs of the professionals providing care," Dr. Zoghbi said.
ACA milestones
This year also will see some practice-impacting milestones under the Affordable Care Act.
Federal money now helps pay for preventive services for Medicaid patients, and many primary care services provided under Medicaid now are paid at the higher Medicare rate. Under the ACA, Medicaid payment increases to 100% of Medicare rates for family physicians, internists, and pediatricians when they provide certain primary care services. Subspecialists in these areas are also eligible for increased payments. The pay hike is for 2013 and 2014.
The law also provides an additional 2 years of funding to the Children's Health Insurance Program to continue coverage for those children eligible under the Medicaid program.
The Independent Payment Advisory Board is slated to start work this year, even though its members have yet to be named by President Obama. The controversial 15-member panel is charged with making recommendations on how to reduce Medicare spending. Dr. Lazarus said the AMA will continue to work toward eliminating the IPAB.
Some of the biggest changes under the ACA -- the expansion of Medicaid eligibility and the creation of state-based health insurance exchanges -- are coming in 2014, but physician leaders said that doctors need to start preparing this year.
Exactly how to get ready will vary by state since both the Medicaid expansion and the exchanges will be largely state-run.
The AMA is pushing to give physicians greater say by getting them seats on the boards of state exchanges. But even as physicians await more information on these changes, they can prepare by becoming more familiar with the Medicaid program since they are likely to see more of those patients, said Robert Doherty, senior vice president for governmental affairs and public policy at the American College of Physicians.
Penalties kick in
This year the Physician Quality Reporting System (PQRS) transitions from a pure incentive program to a mixed incentive/disincentive program. Previously, PQRS offered small bonus payments to physicians for successfully reporting on quality measures. Now, physicians who don't participate in the program will be assessed a penalty. The 1.5% cut to Medicare fees won't come until 2015, but it will be based on participation this year. Physicians will see a 2% penalty in 2016 if they don't successfully report data during 2014.
"People don't realize that if they get past 2013, they won't have an opportunity to fix it for the next year," said Dr. Bruce Bagley, medical director for quality improvement at the American Academy of Family Physicians.
There are also penalties coming in Medicare's Electronic Prescribing (eRx) Incentive Program. To avoid a 2% penalty in 2014, physicians must meet Medicare's e-prescribing requirements by June 30, 2013.
Penalties from the Medicare Electronic Health Record (EHR) Incentive Program aren't coming until 2015, but Dr. Bagley said that physicians should take a good look at this program now to try to earn some money to offset the cost of EHR implementation.
"The sooner you get going on this stuff, the better," he said.
A physician who starts participating this year can earn up to $39,000 over 4 years. Start next year and the bonus drops to $24,000. A 1% penalty takes effect in 2015, increasing to 2% the following year.
The transition to the ICD-10 coding set is another requirement that physicians need to keep in mind, ACP's Mr. Doherty said. The Department of Health and Human Services delayed the move to ICD-10 until October 2014, but Mr. Doherty said physicians can't afford to wait that long to prepare.
The ACP is trying to convince federal officials to accept some alternative ways of coding that would both satisfy the ICD-10 requirements and be clinically relevant, he said.
Primary care gets a boost
Overall, the outlook for 2013 will probably vary by specialty. The 2013 Medicare Physician Fee Schedule dealt some tough blows to subspecialists, making deep payment cuts in interventional cardiology, neurology, and oncology.
Coding changes in primary care, though, could bolster that field, experts said.
"There's never been a time when so many people from so many quarters recognize the value of primary care," Dr. Bagley said.
Could 2013 finally be the year to eliminate the Sustainable Growth Rate formula?
Officials at the American Medical Association say there's a chance that Congress could decide to permanently scrap the unpopular formula, which drives payment under the Medicare physician fee schedule, as part of a larger deal to cut the federal deficit.
"The fact that we've got this big potential deficit-reduction package would make us more optimistic that we can get [the SGR] taken care of this coming year," said Dr. Jeremy A. Lazarus, president of the American Medical Association .
On Jan. 1, lawmakers passed legislation providing a short-term, 1-year delay to the scheduled 26.5% SGR cut. The bill also included a 2-month delay to scheduled tax hikes and federal spending cuts that were planned as part of a deficit reduction process known as sequestration. That gives Congress several weeks to craft a new plan to deal with the nation's debt and the growth in Medicare spending.
It wouldn't be unprecedented for a permanent SGR fix to be considered as part of comprehensive deficit reduction legislation. SGR repeal was included in bipartisan plans created by outside groups several times, including the Simpson-Bowles Commission, the Senate Gang of Six, and others, Dr. Lazarus said.
Although complete SGR repeal carries a 10-year price tag of nearly $300 billion, physicians argue that, since Congress always acts to avert the pay cuts triggered by the formula, the federal government does not save any money by keeping it on the books. The large cost of repeal, however, means that it may be easier to get the SGR fix inserted into a larger bill than to get lawmakers to approve it separately, Dr. Lazarus said.
The AMA is asking Congress to not only repeal the SGR but also to establish a period of stable Medicare payments so that physicians can begin to transition to a new payment system that focuses on quality of care, Dr. Lazarus said. In the meantime, the AMA and other groups have been working on developing new delivery and payment reform options that could offer an alternative to the current fee for service system.
"We do hope we can start changing the equation on reimbursement and going from fee for service to accounting for quality," said Dr. William A. Zoghbi, president of the American College of Cardiology.
ACC officials are eager to move away from the SGR but they are concerned about where the money to do so might come from. Dr. Zoghbi said that he doesn't want to see lawmakers robbing other health care priorities to pay for the fix. For instance, in December, lawmakers considered a proposal to pay for a 1-year SGR fix using money that was slated for increasing Medicaid payments to physicians providing primary care services. Instead, lawmakers financed the one-year SGR fix mainly through cuts to hospital payments.
"These fixes cannot be on the backs of the professionals providing care," Dr. Zoghbi said.
ACA milestones
This year also will see some practice-impacting milestones under the Affordable Care Act.
Federal money now helps pay for preventive services for Medicaid patients, and many primary care services provided under Medicaid now are paid at the higher Medicare rate. Under the ACA, Medicaid payment increases to 100% of Medicare rates for family physicians, internists, and pediatricians when they provide certain primary care services. Subspecialists in these areas are also eligible for increased payments. The pay hike is for 2013 and 2014.
The law also provides an additional 2 years of funding to the Children's Health Insurance Program to continue coverage for those children eligible under the Medicaid program.
The Independent Payment Advisory Board is slated to start work this year, even though its members have yet to be named by President Obama. The controversial 15-member panel is charged with making recommendations on how to reduce Medicare spending. Dr. Lazarus said the AMA will continue to work toward eliminating the IPAB.
Some of the biggest changes under the ACA -- the expansion of Medicaid eligibility and the creation of state-based health insurance exchanges -- are coming in 2014, but physician leaders said that doctors need to start preparing this year.
Exactly how to get ready will vary by state since both the Medicaid expansion and the exchanges will be largely state-run.
The AMA is pushing to give physicians greater say by getting them seats on the boards of state exchanges. But even as physicians await more information on these changes, they can prepare by becoming more familiar with the Medicaid program since they are likely to see more of those patients, said Robert Doherty, senior vice president for governmental affairs and public policy at the American College of Physicians.
Penalties kick in
This year the Physician Quality Reporting System (PQRS) transitions from a pure incentive program to a mixed incentive/disincentive program. Previously, PQRS offered small bonus payments to physicians for successfully reporting on quality measures. Now, physicians who don't participate in the program will be assessed a penalty. The 1.5% cut to Medicare fees won't come until 2015, but it will be based on participation this year. Physicians will see a 2% penalty in 2016 if they don't successfully report data during 2014.
"People don't realize that if they get past 2013, they won't have an opportunity to fix it for the next year," said Dr. Bruce Bagley, medical director for quality improvement at the American Academy of Family Physicians.
There are also penalties coming in Medicare's Electronic Prescribing (eRx) Incentive Program. To avoid a 2% penalty in 2014, physicians must meet Medicare's e-prescribing requirements by June 30, 2013.
Penalties from the Medicare Electronic Health Record (EHR) Incentive Program aren't coming until 2015, but Dr. Bagley said that physicians should take a good look at this program now to try to earn some money to offset the cost of EHR implementation.
"The sooner you get going on this stuff, the better," he said.
A physician who starts participating this year can earn up to $39,000 over 4 years. Start next year and the bonus drops to $24,000. A 1% penalty takes effect in 2015, increasing to 2% the following year.
The transition to the ICD-10 coding set is another requirement that physicians need to keep in mind, ACP's Mr. Doherty said. The Department of Health and Human Services delayed the move to ICD-10 until October 2014, but Mr. Doherty said physicians can't afford to wait that long to prepare.
The ACP is trying to convince federal officials to accept some alternative ways of coding that would both satisfy the ICD-10 requirements and be clinically relevant, he said.
Primary care gets a boost
Overall, the outlook for 2013 will probably vary by specialty. The 2013 Medicare Physician Fee Schedule dealt some tough blows to subspecialists, making deep payment cuts in interventional cardiology, neurology, and oncology.
Coding changes in primary care, though, could bolster that field, experts said.
"There's never been a time when so many people from so many quarters recognize the value of primary care," Dr. Bagley said.
ACOG recommends counseling for prenatal spina bifida surgery
Certain pregnant women who are carrying a fetus with severe spina bifida should be counseled about the potential benefits and risks of maternal-fetal surgery, according to the American College of Obstetricians and Gynecologists.
The ACOG Committee on Obstetric Practice recently recommended counseling about maternal-fetal surgery for myelomeningocele, the most severe form of spina bifida, following promising results from the procedure in an 8-year randomized controlled trial (Obstet. Gynecol. 2013;121:218-9).
In the Management of Myelomeningocele Study (MOMS), prenatal repair before 26 weeks of gestation reduced the need for a shunt at 12 months and also decreased the rate of hindbrain herniation by one-third at 12 months of age. The procedure also doubled the rate of independent walking and produced higher levels of functioning than were expected based on anatomic levels (N. Engl. J. Med. 2011;364:993-1004).
But the study, which was sponsored by the National Institutes of Health, also found significant maternal and fetal risks. For example, the surgery was associated with high rates of preterm birth, fetal bradycardia, oligohydramnios, placental abruption, pulmonary edema, maternal transfusion at delivery, and an increased incidence of uterine thinning.
ACOG cautions that the MOMS trial used stringent inclusion criteria and rigorous requirements for the experience of the surgeons involved. As a result, outcomes from the trial should be considered a "best-case scenario," the committee members wrote. They urged physicians to use the same inclusion criteria as the researchers when considering which women to counsel about the maternal-fetal surgery. The criteria were a singleton pregnancy, myelomeningocele with the upper boundary between T-1 and S-1, evidence of hindbrain herniation, gestational age between 19.0 and 25.9 weeks, and a normal karyotype. The major exclusion criteria included a fetal anomaly unrelated to the myelomeningocele; severe kyphosis; risk of preterm birth; a maternal body mass index of 35 kg/m2 or more; and contraindications to surgery, including previous hysterotomy in the active uterine segment.
Women should also be counseled about the implications of the surgery for future pregnancies, the ACOG committee recommended.
"It is a highly technical procedure with potential for significant morbidity and possibly mortality, even in the best and most experienced hands," they wrote. "Maternal-fetal surgery for myelomeningocele should only be offered at facilities with the expertise, multidisciplinary teams, services, and facilities to provide the intensive care required for these patients."
The study authors declared that they received funding from the National Institutes of Health. One of the authors reported receiving funding from Vanderbilt University in Nashville, Tenn.
Certain pregnant women who are carrying a fetus with severe spina bifida should be counseled about the potential benefits and risks of maternal-fetal surgery, according to the American College of Obstetricians and Gynecologists.
The ACOG Committee on Obstetric Practice recently recommended counseling about maternal-fetal surgery for myelomeningocele, the most severe form of spina bifida, following promising results from the procedure in an 8-year randomized controlled trial (Obstet. Gynecol. 2013;121:218-9).
In the Management of Myelomeningocele Study (MOMS), prenatal repair before 26 weeks of gestation reduced the need for a shunt at 12 months and also decreased the rate of hindbrain herniation by one-third at 12 months of age. The procedure also doubled the rate of independent walking and produced higher levels of functioning than were expected based on anatomic levels (N. Engl. J. Med. 2011;364:993-1004).
But the study, which was sponsored by the National Institutes of Health, also found significant maternal and fetal risks. For example, the surgery was associated with high rates of preterm birth, fetal bradycardia, oligohydramnios, placental abruption, pulmonary edema, maternal transfusion at delivery, and an increased incidence of uterine thinning.
ACOG cautions that the MOMS trial used stringent inclusion criteria and rigorous requirements for the experience of the surgeons involved. As a result, outcomes from the trial should be considered a "best-case scenario," the committee members wrote. They urged physicians to use the same inclusion criteria as the researchers when considering which women to counsel about the maternal-fetal surgery. The criteria were a singleton pregnancy, myelomeningocele with the upper boundary between T-1 and S-1, evidence of hindbrain herniation, gestational age between 19.0 and 25.9 weeks, and a normal karyotype. The major exclusion criteria included a fetal anomaly unrelated to the myelomeningocele; severe kyphosis; risk of preterm birth; a maternal body mass index of 35 kg/m2 or more; and contraindications to surgery, including previous hysterotomy in the active uterine segment.
Women should also be counseled about the implications of the surgery for future pregnancies, the ACOG committee recommended.
"It is a highly technical procedure with potential for significant morbidity and possibly mortality, even in the best and most experienced hands," they wrote. "Maternal-fetal surgery for myelomeningocele should only be offered at facilities with the expertise, multidisciplinary teams, services, and facilities to provide the intensive care required for these patients."
The study authors declared that they received funding from the National Institutes of Health. One of the authors reported receiving funding from Vanderbilt University in Nashville, Tenn.
Certain pregnant women who are carrying a fetus with severe spina bifida should be counseled about the potential benefits and risks of maternal-fetal surgery, according to the American College of Obstetricians and Gynecologists.
The ACOG Committee on Obstetric Practice recently recommended counseling about maternal-fetal surgery for myelomeningocele, the most severe form of spina bifida, following promising results from the procedure in an 8-year randomized controlled trial (Obstet. Gynecol. 2013;121:218-9).
In the Management of Myelomeningocele Study (MOMS), prenatal repair before 26 weeks of gestation reduced the need for a shunt at 12 months and also decreased the rate of hindbrain herniation by one-third at 12 months of age. The procedure also doubled the rate of independent walking and produced higher levels of functioning than were expected based on anatomic levels (N. Engl. J. Med. 2011;364:993-1004).
But the study, which was sponsored by the National Institutes of Health, also found significant maternal and fetal risks. For example, the surgery was associated with high rates of preterm birth, fetal bradycardia, oligohydramnios, placental abruption, pulmonary edema, maternal transfusion at delivery, and an increased incidence of uterine thinning.
ACOG cautions that the MOMS trial used stringent inclusion criteria and rigorous requirements for the experience of the surgeons involved. As a result, outcomes from the trial should be considered a "best-case scenario," the committee members wrote. They urged physicians to use the same inclusion criteria as the researchers when considering which women to counsel about the maternal-fetal surgery. The criteria were a singleton pregnancy, myelomeningocele with the upper boundary between T-1 and S-1, evidence of hindbrain herniation, gestational age between 19.0 and 25.9 weeks, and a normal karyotype. The major exclusion criteria included a fetal anomaly unrelated to the myelomeningocele; severe kyphosis; risk of preterm birth; a maternal body mass index of 35 kg/m2 or more; and contraindications to surgery, including previous hysterotomy in the active uterine segment.
Women should also be counseled about the implications of the surgery for future pregnancies, the ACOG committee recommended.
"It is a highly technical procedure with potential for significant morbidity and possibly mortality, even in the best and most experienced hands," they wrote. "Maternal-fetal surgery for myelomeningocele should only be offered at facilities with the expertise, multidisciplinary teams, services, and facilities to provide the intensive care required for these patients."
The study authors declared that they received funding from the National Institutes of Health. One of the authors reported receiving funding from Vanderbilt University in Nashville, Tenn.
Sanofi discounts cancer drug by 50% after backlash
The drugmaker Sanofi is cutting the price of its new colorectal cancer drug Zaltrap in half after physicians balked at the $11,000-a-month price tag.
Sanofi has not released official documentation detailing the specifics of the change, but in recent conversations with oncology experts, company officials laid out a plan to offer a 50% discount to anyone who purchases ziv-aflibercept (Zaltrap) from them on the wholesale market.
The move follows a New York Times op-ed column in which Dr. Leonard B. Saltz, chief of the gastrointestinal oncology service at Memorial Sloan-Kettering Cancer Center (MSKCC) in New York, and two colleagues announced that they would not use Zaltrap because of its high price. He said in an interview that there are some lingering questions about the newly announced price reduction.
Discount vs. Price Reduction
For instance, he expressed concern that the 50% discount given to physicians and hospitals may not translate into a reduction in either Medicare reimbursement or copayments for patients, both of which are tied to the wholesale acquisition cost (WAC) of the drug.
Another problem with offering a discount without changing the official price of the drug is that this could inadvertently create a financial inducement for providers to choose that drug, Dr. Saltz said. If the providers are getting a 50% discount but are still being reimbursed at the full price, they would make a significant profit for using Zaltrap.
Dr. Saltz said he and his colleagues at Memorial Sloan-Kettering raised these issues with Sanofi officials but didn’t get an immediate response.
The Oncology Report contacted Sanofi about the Zaltrap price reduction, but company officials declined to comment.
‘A Good Thing for Patients’
Dr. Roy Beveridge, chief medical officer for the US Oncology Network, supported by McKesson Specialty Health, said in an interview that he’s confident that Sanofi made the price reduction in a way that will benefit patients and payers eventually. And he applauded the company’s unprecedented move to slash the price.
"It’s a good thing for patients," Dr. Beveridge said. "It’s a good thing for the system."
At the 1,000-plus physician US Oncology Network, oncologists consider efficacy, toxicity, and price when making determinations about which drugs are placed on its Level I Pathways. If something is more effective, it’s the first choice on the treatment pathway, Dr. Beveridge said. But if treatments are comparable in terms of efficacy and toxicity, then cost is a major consideration.
"We, as oncologists, recognize that increases of 15% per year are just not sustainable," he said.
With Sanofi’s decision to drop the price, Dr. Beveridge said he thinks more companies will be under pressure not to debut drugs with sky-high prices if they don’t offer significant new benefits.
"For those companies that have true innovative products and have something which is completely different and better, you’ll still see cost pressure going up," he said. "But for those that have results that are more comparable to other treatments, there’s going to be huge price pressure to be equal or lower than others."
Zaltrap Compared with Avastin
In October, Dr. Saltz, along with two other physicians at Memorial Sloan-Kettering, penned the op-ed in the New York Times saying that they had decided not to give Zaltrap to their patients because the drug did not provide greater efficacy than Genentech’s bevacizumab (Avastin), which sells for about $5,000 a month or less than half the cost of Zaltrap.
It was a relatively easy decision to make, said Dr. Saltz, who has been a paid consultant for Genentech and an unpaid consultant to Sanofi this year. They found no evidence that Zaltrap offered any benefit over Avastin, which they could get for about half the price. But Dr. Saltz said there needs to be more discussion in the United States about what to do in those more complicated cases where drugs offer fractionally more benefit at substantially increased prices.
There’s been a sense in the country that everything in health care is so important that it’s wrong to discuss costs, Dr. Saltz said, but that attitude has to change.
"We can’t afford that," he said. "It’s a fantasy and it’s untrue. We can’t just say that because we’re talking about health care, money is no object."
In the past decade, advances in the treatment of metastatic colon cancer have improved survival. This advance has been slow and steady and has come as a result of innovative technology, unwavering researchers, brave patients, and funding from pharmaceutical companies and the National Cancer Institute. These advances do not come cheaply.
In 2004, the antiangiogenic agent bevacizumab (Avastin) was approved by the Food and Drug Administration for the treatment of metastatic colorectal cancer, with 5FU, leucovorin, and irinotecan as the first line of therapy. According to a commentary in the New England Journal of Medicine, the cost was estimated at $21,399 for an 8-week treatment course. Bevacizumab was responsible for more than 50% of that cost. The addition of bevacizumab to the standard chemotherapy improved the median overall survival from 15.6 months to 20.3 months.
Through a convoluted series of clinical trials – beyond the scope of this comment – the first line of therapy for the treatment of advanced colorectal cancer in the United States is 5FU, leucovorin, and oxaliplatin with bevacizumab. Second-line therapy is considered at the time of progression, signifying resistance to the first-line agents. What remained unclear is the role of further antiangiogenic therapy with the second-line chemotherapy agents.
Aflibercept (Zaltrap) was developed using a unique technology that "traps" multiple ligands of the vascular endothelial growth factor receptor, a possible improvement in bevacizumab. Rather than compare this agent directly with bevacizumab, a study was conducted in which 1,226 patients were randomized to standard second-line chemotherapy with or without aflibercept. The study showed that with the addition of aflibercept, the median overall survival from the start of second line therapy increased from 12.1 months to 13.5 months. Those patients that received bevacizumab with their first-line of therapy had a marginal benefit from 11.7 months to 12.5 months, while those that did not receive bevacizumab had a benefit from 12.4 months to 13.9 months with the addition of aflibercept.
In a similar study, 884 patients were randomized to receive standard second-line chemotherapy with or without continued bevacizumab. The median overall survival from the start of second-line therapy increased from 9.8 months to 11.2 months with the continuation of bevacizumab.
Dr. Mary Mulcahy |
These studies show us that continuing antiangiogenic therapy with the second-line of chemotherapy may be beneficial. With two agents demonstrating comparable benefit with the second-line of chemotherapy, and with no evidence that one is better than another, cost is certainly an important consideration. With the time, money, and patients invested in new drug development, it is imperative that clear benefits are demonstrated at a cost that our overextended health care system can manage.
Mary F. Mulcahy, M.D., is an associate professor in the division of hematology/oncology at Northwestern University Feinberg School of Medicine, Chicago. She has no relevant disclosures.
In the past decade, advances in the treatment of metastatic colon cancer have improved survival. This advance has been slow and steady and has come as a result of innovative technology, unwavering researchers, brave patients, and funding from pharmaceutical companies and the National Cancer Institute. These advances do not come cheaply.
In 2004, the antiangiogenic agent bevacizumab (Avastin) was approved by the Food and Drug Administration for the treatment of metastatic colorectal cancer, with 5FU, leucovorin, and irinotecan as the first line of therapy. According to a commentary in the New England Journal of Medicine, the cost was estimated at $21,399 for an 8-week treatment course. Bevacizumab was responsible for more than 50% of that cost. The addition of bevacizumab to the standard chemotherapy improved the median overall survival from 15.6 months to 20.3 months.
Through a convoluted series of clinical trials – beyond the scope of this comment – the first line of therapy for the treatment of advanced colorectal cancer in the United States is 5FU, leucovorin, and oxaliplatin with bevacizumab. Second-line therapy is considered at the time of progression, signifying resistance to the first-line agents. What remained unclear is the role of further antiangiogenic therapy with the second-line chemotherapy agents.
Aflibercept (Zaltrap) was developed using a unique technology that "traps" multiple ligands of the vascular endothelial growth factor receptor, a possible improvement in bevacizumab. Rather than compare this agent directly with bevacizumab, a study was conducted in which 1,226 patients were randomized to standard second-line chemotherapy with or without aflibercept. The study showed that with the addition of aflibercept, the median overall survival from the start of second line therapy increased from 12.1 months to 13.5 months. Those patients that received bevacizumab with their first-line of therapy had a marginal benefit from 11.7 months to 12.5 months, while those that did not receive bevacizumab had a benefit from 12.4 months to 13.9 months with the addition of aflibercept.
In a similar study, 884 patients were randomized to receive standard second-line chemotherapy with or without continued bevacizumab. The median overall survival from the start of second-line therapy increased from 9.8 months to 11.2 months with the continuation of bevacizumab.
Dr. Mary Mulcahy |
These studies show us that continuing antiangiogenic therapy with the second-line of chemotherapy may be beneficial. With two agents demonstrating comparable benefit with the second-line of chemotherapy, and with no evidence that one is better than another, cost is certainly an important consideration. With the time, money, and patients invested in new drug development, it is imperative that clear benefits are demonstrated at a cost that our overextended health care system can manage.
Mary F. Mulcahy, M.D., is an associate professor in the division of hematology/oncology at Northwestern University Feinberg School of Medicine, Chicago. She has no relevant disclosures.
In the past decade, advances in the treatment of metastatic colon cancer have improved survival. This advance has been slow and steady and has come as a result of innovative technology, unwavering researchers, brave patients, and funding from pharmaceutical companies and the National Cancer Institute. These advances do not come cheaply.
In 2004, the antiangiogenic agent bevacizumab (Avastin) was approved by the Food and Drug Administration for the treatment of metastatic colorectal cancer, with 5FU, leucovorin, and irinotecan as the first line of therapy. According to a commentary in the New England Journal of Medicine, the cost was estimated at $21,399 for an 8-week treatment course. Bevacizumab was responsible for more than 50% of that cost. The addition of bevacizumab to the standard chemotherapy improved the median overall survival from 15.6 months to 20.3 months.
Through a convoluted series of clinical trials – beyond the scope of this comment – the first line of therapy for the treatment of advanced colorectal cancer in the United States is 5FU, leucovorin, and oxaliplatin with bevacizumab. Second-line therapy is considered at the time of progression, signifying resistance to the first-line agents. What remained unclear is the role of further antiangiogenic therapy with the second-line chemotherapy agents.
Aflibercept (Zaltrap) was developed using a unique technology that "traps" multiple ligands of the vascular endothelial growth factor receptor, a possible improvement in bevacizumab. Rather than compare this agent directly with bevacizumab, a study was conducted in which 1,226 patients were randomized to standard second-line chemotherapy with or without aflibercept. The study showed that with the addition of aflibercept, the median overall survival from the start of second line therapy increased from 12.1 months to 13.5 months. Those patients that received bevacizumab with their first-line of therapy had a marginal benefit from 11.7 months to 12.5 months, while those that did not receive bevacizumab had a benefit from 12.4 months to 13.9 months with the addition of aflibercept.
In a similar study, 884 patients were randomized to receive standard second-line chemotherapy with or without continued bevacizumab. The median overall survival from the start of second-line therapy increased from 9.8 months to 11.2 months with the continuation of bevacizumab.
Dr. Mary Mulcahy |
These studies show us that continuing antiangiogenic therapy with the second-line of chemotherapy may be beneficial. With two agents demonstrating comparable benefit with the second-line of chemotherapy, and with no evidence that one is better than another, cost is certainly an important consideration. With the time, money, and patients invested in new drug development, it is imperative that clear benefits are demonstrated at a cost that our overextended health care system can manage.
Mary F. Mulcahy, M.D., is an associate professor in the division of hematology/oncology at Northwestern University Feinberg School of Medicine, Chicago. She has no relevant disclosures.
The drugmaker Sanofi is cutting the price of its new colorectal cancer drug Zaltrap in half after physicians balked at the $11,000-a-month price tag.
Sanofi has not released official documentation detailing the specifics of the change, but in recent conversations with oncology experts, company officials laid out a plan to offer a 50% discount to anyone who purchases ziv-aflibercept (Zaltrap) from them on the wholesale market.
The move follows a New York Times op-ed column in which Dr. Leonard B. Saltz, chief of the gastrointestinal oncology service at Memorial Sloan-Kettering Cancer Center (MSKCC) in New York, and two colleagues announced that they would not use Zaltrap because of its high price. He said in an interview that there are some lingering questions about the newly announced price reduction.
Discount vs. Price Reduction
For instance, he expressed concern that the 50% discount given to physicians and hospitals may not translate into a reduction in either Medicare reimbursement or copayments for patients, both of which are tied to the wholesale acquisition cost (WAC) of the drug.
Another problem with offering a discount without changing the official price of the drug is that this could inadvertently create a financial inducement for providers to choose that drug, Dr. Saltz said. If the providers are getting a 50% discount but are still being reimbursed at the full price, they would make a significant profit for using Zaltrap.
Dr. Saltz said he and his colleagues at Memorial Sloan-Kettering raised these issues with Sanofi officials but didn’t get an immediate response.
The Oncology Report contacted Sanofi about the Zaltrap price reduction, but company officials declined to comment.
‘A Good Thing for Patients’
Dr. Roy Beveridge, chief medical officer for the US Oncology Network, supported by McKesson Specialty Health, said in an interview that he’s confident that Sanofi made the price reduction in a way that will benefit patients and payers eventually. And he applauded the company’s unprecedented move to slash the price.
"It’s a good thing for patients," Dr. Beveridge said. "It’s a good thing for the system."
At the 1,000-plus physician US Oncology Network, oncologists consider efficacy, toxicity, and price when making determinations about which drugs are placed on its Level I Pathways. If something is more effective, it’s the first choice on the treatment pathway, Dr. Beveridge said. But if treatments are comparable in terms of efficacy and toxicity, then cost is a major consideration.
"We, as oncologists, recognize that increases of 15% per year are just not sustainable," he said.
With Sanofi’s decision to drop the price, Dr. Beveridge said he thinks more companies will be under pressure not to debut drugs with sky-high prices if they don’t offer significant new benefits.
"For those companies that have true innovative products and have something which is completely different and better, you’ll still see cost pressure going up," he said. "But for those that have results that are more comparable to other treatments, there’s going to be huge price pressure to be equal or lower than others."
Zaltrap Compared with Avastin
In October, Dr. Saltz, along with two other physicians at Memorial Sloan-Kettering, penned the op-ed in the New York Times saying that they had decided not to give Zaltrap to their patients because the drug did not provide greater efficacy than Genentech’s bevacizumab (Avastin), which sells for about $5,000 a month or less than half the cost of Zaltrap.
It was a relatively easy decision to make, said Dr. Saltz, who has been a paid consultant for Genentech and an unpaid consultant to Sanofi this year. They found no evidence that Zaltrap offered any benefit over Avastin, which they could get for about half the price. But Dr. Saltz said there needs to be more discussion in the United States about what to do in those more complicated cases where drugs offer fractionally more benefit at substantially increased prices.
There’s been a sense in the country that everything in health care is so important that it’s wrong to discuss costs, Dr. Saltz said, but that attitude has to change.
"We can’t afford that," he said. "It’s a fantasy and it’s untrue. We can’t just say that because we’re talking about health care, money is no object."
The drugmaker Sanofi is cutting the price of its new colorectal cancer drug Zaltrap in half after physicians balked at the $11,000-a-month price tag.
Sanofi has not released official documentation detailing the specifics of the change, but in recent conversations with oncology experts, company officials laid out a plan to offer a 50% discount to anyone who purchases ziv-aflibercept (Zaltrap) from them on the wholesale market.
The move follows a New York Times op-ed column in which Dr. Leonard B. Saltz, chief of the gastrointestinal oncology service at Memorial Sloan-Kettering Cancer Center (MSKCC) in New York, and two colleagues announced that they would not use Zaltrap because of its high price. He said in an interview that there are some lingering questions about the newly announced price reduction.
Discount vs. Price Reduction
For instance, he expressed concern that the 50% discount given to physicians and hospitals may not translate into a reduction in either Medicare reimbursement or copayments for patients, both of which are tied to the wholesale acquisition cost (WAC) of the drug.
Another problem with offering a discount without changing the official price of the drug is that this could inadvertently create a financial inducement for providers to choose that drug, Dr. Saltz said. If the providers are getting a 50% discount but are still being reimbursed at the full price, they would make a significant profit for using Zaltrap.
Dr. Saltz said he and his colleagues at Memorial Sloan-Kettering raised these issues with Sanofi officials but didn’t get an immediate response.
The Oncology Report contacted Sanofi about the Zaltrap price reduction, but company officials declined to comment.
‘A Good Thing for Patients’
Dr. Roy Beveridge, chief medical officer for the US Oncology Network, supported by McKesson Specialty Health, said in an interview that he’s confident that Sanofi made the price reduction in a way that will benefit patients and payers eventually. And he applauded the company’s unprecedented move to slash the price.
"It’s a good thing for patients," Dr. Beveridge said. "It’s a good thing for the system."
At the 1,000-plus physician US Oncology Network, oncologists consider efficacy, toxicity, and price when making determinations about which drugs are placed on its Level I Pathways. If something is more effective, it’s the first choice on the treatment pathway, Dr. Beveridge said. But if treatments are comparable in terms of efficacy and toxicity, then cost is a major consideration.
"We, as oncologists, recognize that increases of 15% per year are just not sustainable," he said.
With Sanofi’s decision to drop the price, Dr. Beveridge said he thinks more companies will be under pressure not to debut drugs with sky-high prices if they don’t offer significant new benefits.
"For those companies that have true innovative products and have something which is completely different and better, you’ll still see cost pressure going up," he said. "But for those that have results that are more comparable to other treatments, there’s going to be huge price pressure to be equal or lower than others."
Zaltrap Compared with Avastin
In October, Dr. Saltz, along with two other physicians at Memorial Sloan-Kettering, penned the op-ed in the New York Times saying that they had decided not to give Zaltrap to their patients because the drug did not provide greater efficacy than Genentech’s bevacizumab (Avastin), which sells for about $5,000 a month or less than half the cost of Zaltrap.
It was a relatively easy decision to make, said Dr. Saltz, who has been a paid consultant for Genentech and an unpaid consultant to Sanofi this year. They found no evidence that Zaltrap offered any benefit over Avastin, which they could get for about half the price. But Dr. Saltz said there needs to be more discussion in the United States about what to do in those more complicated cases where drugs offer fractionally more benefit at substantially increased prices.
There’s been a sense in the country that everything in health care is so important that it’s wrong to discuss costs, Dr. Saltz said, but that attitude has to change.
"We can’t afford that," he said. "It’s a fantasy and it’s untrue. We can’t just say that because we’re talking about health care, money is no object."