User login
Incorrect About Telemetry Status
Cardiac telemetry is overused in hospitals and continues to be a source of healthcare waste.1-4 Its overuse is considered a leading issue in quality initiatives, as highlighted by its presence in the top 5 recommendations by the Society of Hospital Medicine to the Choosing Wisely Campaign.5 There have been multiple published studies on efforts to curb telemetry overuse, including educational campaigns, hard-wiring guidelines into the electronic health record (EHR), and discontinuation protocols.6-9
Less studied, however, are the causes of telemetry overuse. While lack of knowledge of guidelines may contribute to inappropriate initial ordering of telemetry,1,4 physicians may forget to discontinue it when the original indication is no longer present, ie, a form of “clinical inertia.” The authors aimed to study how often inpatient clinicians were aware (or unaware) of the telemetry status of their patients.
METHODS
The authors conducted a cross-sectional observational study at 2 academic medical centers within the same healthcare system (University of California, Los Angeles [UCLA] Health System) over a 10-week period, from December 12, 2014 to February 18, 2015. The survey included senior resident physicians (in years 2 or 3 of training), attending physicians on teaching services (“teaching attendings”), and attending physicians on nonteaching services (“direct-care attendings”) caring for hospitalized patients on general internal medicine (nonintensive care) units. First-year residents (“interns”) were not surveyed because their presence at interdisciplinary rounds, where surveying took place, was not mandatory. At both hospitals, telemetry is initiated by placing a “Continuous Cardiac Monitoring” order in the EHR, and is terminated by selecting “Discontinue” on that same order. Telemetry status of patients was determined through a daily review of the EHR at UCLA Ronald Reagan Hospital, where presence of telemetry was defined as an active order for telemetry as of 7 AM. At UCLA Santa Monica Hospital, telemetry status was determined by daily review of the morning telemetry technician logs, which reflected telemetry status as of 7 AM.
Once-weekly, prior to afternoon interdisciplinary rounds, members of the study team would give physicians a print-out of their patient list and ask them to mark whether or not their patients were on telemetry as of that morning. They were allowed to reference their own printed patient list, but were not allowed to reference the EHR. Since interdisciplinary rounds occurred in the afternoon, it was assumed that all clinicians had seen and examined their patients. The authors did not mandate that physicians respond to the survey, and we did not collect information on individual physician characteristics other than training status.
The primary outcome of interest was correct assessment of telemetry status. The authors first presented descriptive statistics for patient, provider, and telemetry status, and used χ2 tests and McNemar’s test to compare the type of physician (resident, teaching attending, or direct-care attending) with the binary outcome (correct or incorrect assessment). STATA/SE, 13.1 (StataCorp), was used for all statistical analysis, and P values < 0.05 were considered statistically significant. The study was submitted to the UCLA Office of Human Research Protection Program and exempted from Institutional Review Board review.
RESULTS
A total of 1,379 physician-assessments on 962 patients were obtained during the study period. During this time, 53.1% (511/962) of patients were on telemetry. Overall, physicians were incorrect in 26.5% (365/1379) of their assessments of telemetry status (Table). Of the 745 assessments of a patient on telemetry, clinicians erroneously reported that they were not 27.9% of the time (n = 208). Of the 634 assessments of a patient not on telemetry, clinicians erroneously reported that patients were on it 24.8% of the time (n = 157).
Assessments by direct-care attendings were more accurate than those done by teaching attendings (80.9% vs. 72.4%, P < 0.05) and resident physicians (80.9% vs. 71.8%, P < 0.05). There was no statistically significant difference in accuracy of resident physician assessments when compared to teaching attending assessments (71.8% vs. 72.4%, P = 0.81).
DISCUSSION
In this study, clinicians often inaccurately recalled the telemetry status of their hospitalized patients. These findings have implications for both patient safety as well as telemetry overuse, as ignorance of telemetry status may limit its discontinuation.
The authors also found that assessments done by direct-care attendings were more accurate than those done by teaching attendings. This discrepancy is likely related to different roles in patient care: teaching attendings provide supervisory roles, while direct-care attendings routinely review orders and perform detailed exams on their patients. Similarly, resident physician assessments were found to be less accurate than direct-care attending assessments, which may reflect less clinical experience as well as their supervisory role.
In light of these findings, interventions to reduce telemetry overuse should include efforts to increase real-time telemetry awareness as well as reduce inappropriate use, and should target all levels of training. Using research on urinary catheter removal10 as a model, strategies to increase telemetry awareness could include daily verbal or written reminders of telemetry status, requests to assess daily need, high visibility signs in charts or in patient rooms, or electronic reminders that telemetry is in place. Furthermore, efforts to promote and operationalize medical mindfulness, in which providers are trained to be aware of indications, timely removal, and the presence of monitoring devices could be incorporated into broader telemetry stewardship and high-value care efforts.11
There are limitations to this study. The authors did not collect information on the number of unique individual physicians represented by the study, and, thus, clinicians may have been surveyed multiple times throughout the study, potentially influencing their attention to the telemetry status of their patients. In addition, this study was conducted within a single healthcare system, limiting its generalizability.
In conclusion, the authors found that physicians were often incorrect when assessing the telemetry status of their patients. Interventions to help raise awareness of a patient’s telemetry status may help reduce telemetry overuse.
Disclosure: Nothing to report.
1. Henriques-Forsythe MN, Ivonye CC, Jamched U, Kamuguisha LKK, Olejeme KA, Onwuanyi AE. Is telemetry overused? Is it as helpful as thought? Cleve Clin J Med. 2009;76:368-372. PubMed
2. Kanwar M, Fares R, Minnick S, Rosman HS, Saravolatz L. Inpatient cardiac telemetry monitoring: are we overdoing it. JCOM. 2008;15(1):16-20.
3. Chong-Yik R, Bennett A, Milani R, Morin D. Telemetry overuse and its economic implications. J Am Coll Cardiol.2016;67(13_S):1993.
4. Najafi N, Auerbach A. Use and outcomes of telemetry monitoring on a medicine service. Arch Intern Med. 2012;172:1349-1350. PubMed
5. Bulger J, Nickel W, Messler J, et al. Choosing wisely in adult hospital medicine: five opportunities for improved healthcare value. J Hosp Med. 2013;8:486-492. PubMed
6. Leighton H, Kianfar H, Serynek S, Kerwin T. Effect of an electronic ordering system on adherence to the American College of Cardiology/American Heart Association guidelines for cardiac monitoring. Crit Pathw Cardiol. 2013;12:6-8. PubMed
7. Lee JC, Lamb P, Rand E, Ryan C, Rubal BJ. Optimizing telemetry utilization in an academic medical center. JCOM. 2008;15(9).
8. Boggan JC, Navar-Boggan AM, Patel V, Schulteis RD, Simel DL. Reductions in telemetry order duration do not reduce telemetry utilization. J Hosp Med. 2014;9:795-796. PubMed
9. Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering overuse of cardiac telemetry in non-intensive care unit settings by hardwiring the use of American Heart Association guidelines. JAMA Intern Med. 2014;174:1852-1854. PubMed
10. Meddings J, Krein SL, Fakih MG, Olmsted RN, Saint S. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infections: brief update review. In: Making Health Care Safer II: An Updated Critical Analysis of the Evidence for Patient Safety Practices. (Evidence Reports/Technology Assessments, No. 211.) Chapter 9. Rockville (MD): Agency for Healthcare Research and Quality (US); 2013. Available from: http://www.ncbi.nlm.nih.gov/books/NBK133354/. May 15, 2016. PubMed
11. Kiyoshi-Teo H, Krein SL, Saint S. Applying mindful evidence-based practice at the bedside: using catheter-associated urinary tract infection as a model. Infect Control Hosp Epidemiol. 2013;34:1099-1001. PubMed
Cardiac telemetry is overused in hospitals and continues to be a source of healthcare waste.1-4 Its overuse is considered a leading issue in quality initiatives, as highlighted by its presence in the top 5 recommendations by the Society of Hospital Medicine to the Choosing Wisely Campaign.5 There have been multiple published studies on efforts to curb telemetry overuse, including educational campaigns, hard-wiring guidelines into the electronic health record (EHR), and discontinuation protocols.6-9
Less studied, however, are the causes of telemetry overuse. While lack of knowledge of guidelines may contribute to inappropriate initial ordering of telemetry,1,4 physicians may forget to discontinue it when the original indication is no longer present, ie, a form of “clinical inertia.” The authors aimed to study how often inpatient clinicians were aware (or unaware) of the telemetry status of their patients.
METHODS
The authors conducted a cross-sectional observational study at 2 academic medical centers within the same healthcare system (University of California, Los Angeles [UCLA] Health System) over a 10-week period, from December 12, 2014 to February 18, 2015. The survey included senior resident physicians (in years 2 or 3 of training), attending physicians on teaching services (“teaching attendings”), and attending physicians on nonteaching services (“direct-care attendings”) caring for hospitalized patients on general internal medicine (nonintensive care) units. First-year residents (“interns”) were not surveyed because their presence at interdisciplinary rounds, where surveying took place, was not mandatory. At both hospitals, telemetry is initiated by placing a “Continuous Cardiac Monitoring” order in the EHR, and is terminated by selecting “Discontinue” on that same order. Telemetry status of patients was determined through a daily review of the EHR at UCLA Ronald Reagan Hospital, where presence of telemetry was defined as an active order for telemetry as of 7 AM. At UCLA Santa Monica Hospital, telemetry status was determined by daily review of the morning telemetry technician logs, which reflected telemetry status as of 7 AM.
Once-weekly, prior to afternoon interdisciplinary rounds, members of the study team would give physicians a print-out of their patient list and ask them to mark whether or not their patients were on telemetry as of that morning. They were allowed to reference their own printed patient list, but were not allowed to reference the EHR. Since interdisciplinary rounds occurred in the afternoon, it was assumed that all clinicians had seen and examined their patients. The authors did not mandate that physicians respond to the survey, and we did not collect information on individual physician characteristics other than training status.
The primary outcome of interest was correct assessment of telemetry status. The authors first presented descriptive statistics for patient, provider, and telemetry status, and used χ2 tests and McNemar’s test to compare the type of physician (resident, teaching attending, or direct-care attending) with the binary outcome (correct or incorrect assessment). STATA/SE, 13.1 (StataCorp), was used for all statistical analysis, and P values < 0.05 were considered statistically significant. The study was submitted to the UCLA Office of Human Research Protection Program and exempted from Institutional Review Board review.
RESULTS
A total of 1,379 physician-assessments on 962 patients were obtained during the study period. During this time, 53.1% (511/962) of patients were on telemetry. Overall, physicians were incorrect in 26.5% (365/1379) of their assessments of telemetry status (Table). Of the 745 assessments of a patient on telemetry, clinicians erroneously reported that they were not 27.9% of the time (n = 208). Of the 634 assessments of a patient not on telemetry, clinicians erroneously reported that patients were on it 24.8% of the time (n = 157).
Assessments by direct-care attendings were more accurate than those done by teaching attendings (80.9% vs. 72.4%, P < 0.05) and resident physicians (80.9% vs. 71.8%, P < 0.05). There was no statistically significant difference in accuracy of resident physician assessments when compared to teaching attending assessments (71.8% vs. 72.4%, P = 0.81).
DISCUSSION
In this study, clinicians often inaccurately recalled the telemetry status of their hospitalized patients. These findings have implications for both patient safety as well as telemetry overuse, as ignorance of telemetry status may limit its discontinuation.
The authors also found that assessments done by direct-care attendings were more accurate than those done by teaching attendings. This discrepancy is likely related to different roles in patient care: teaching attendings provide supervisory roles, while direct-care attendings routinely review orders and perform detailed exams on their patients. Similarly, resident physician assessments were found to be less accurate than direct-care attending assessments, which may reflect less clinical experience as well as their supervisory role.
In light of these findings, interventions to reduce telemetry overuse should include efforts to increase real-time telemetry awareness as well as reduce inappropriate use, and should target all levels of training. Using research on urinary catheter removal10 as a model, strategies to increase telemetry awareness could include daily verbal or written reminders of telemetry status, requests to assess daily need, high visibility signs in charts or in patient rooms, or electronic reminders that telemetry is in place. Furthermore, efforts to promote and operationalize medical mindfulness, in which providers are trained to be aware of indications, timely removal, and the presence of monitoring devices could be incorporated into broader telemetry stewardship and high-value care efforts.11
There are limitations to this study. The authors did not collect information on the number of unique individual physicians represented by the study, and, thus, clinicians may have been surveyed multiple times throughout the study, potentially influencing their attention to the telemetry status of their patients. In addition, this study was conducted within a single healthcare system, limiting its generalizability.
In conclusion, the authors found that physicians were often incorrect when assessing the telemetry status of their patients. Interventions to help raise awareness of a patient’s telemetry status may help reduce telemetry overuse.
Disclosure: Nothing to report.
Cardiac telemetry is overused in hospitals and continues to be a source of healthcare waste.1-4 Its overuse is considered a leading issue in quality initiatives, as highlighted by its presence in the top 5 recommendations by the Society of Hospital Medicine to the Choosing Wisely Campaign.5 There have been multiple published studies on efforts to curb telemetry overuse, including educational campaigns, hard-wiring guidelines into the electronic health record (EHR), and discontinuation protocols.6-9
Less studied, however, are the causes of telemetry overuse. While lack of knowledge of guidelines may contribute to inappropriate initial ordering of telemetry,1,4 physicians may forget to discontinue it when the original indication is no longer present, ie, a form of “clinical inertia.” The authors aimed to study how often inpatient clinicians were aware (or unaware) of the telemetry status of their patients.
METHODS
The authors conducted a cross-sectional observational study at 2 academic medical centers within the same healthcare system (University of California, Los Angeles [UCLA] Health System) over a 10-week period, from December 12, 2014 to February 18, 2015. The survey included senior resident physicians (in years 2 or 3 of training), attending physicians on teaching services (“teaching attendings”), and attending physicians on nonteaching services (“direct-care attendings”) caring for hospitalized patients on general internal medicine (nonintensive care) units. First-year residents (“interns”) were not surveyed because their presence at interdisciplinary rounds, where surveying took place, was not mandatory. At both hospitals, telemetry is initiated by placing a “Continuous Cardiac Monitoring” order in the EHR, and is terminated by selecting “Discontinue” on that same order. Telemetry status of patients was determined through a daily review of the EHR at UCLA Ronald Reagan Hospital, where presence of telemetry was defined as an active order for telemetry as of 7 AM. At UCLA Santa Monica Hospital, telemetry status was determined by daily review of the morning telemetry technician logs, which reflected telemetry status as of 7 AM.
Once-weekly, prior to afternoon interdisciplinary rounds, members of the study team would give physicians a print-out of their patient list and ask them to mark whether or not their patients were on telemetry as of that morning. They were allowed to reference their own printed patient list, but were not allowed to reference the EHR. Since interdisciplinary rounds occurred in the afternoon, it was assumed that all clinicians had seen and examined their patients. The authors did not mandate that physicians respond to the survey, and we did not collect information on individual physician characteristics other than training status.
The primary outcome of interest was correct assessment of telemetry status. The authors first presented descriptive statistics for patient, provider, and telemetry status, and used χ2 tests and McNemar’s test to compare the type of physician (resident, teaching attending, or direct-care attending) with the binary outcome (correct or incorrect assessment). STATA/SE, 13.1 (StataCorp), was used for all statistical analysis, and P values < 0.05 were considered statistically significant. The study was submitted to the UCLA Office of Human Research Protection Program and exempted from Institutional Review Board review.
RESULTS
A total of 1,379 physician-assessments on 962 patients were obtained during the study period. During this time, 53.1% (511/962) of patients were on telemetry. Overall, physicians were incorrect in 26.5% (365/1379) of their assessments of telemetry status (Table). Of the 745 assessments of a patient on telemetry, clinicians erroneously reported that they were not 27.9% of the time (n = 208). Of the 634 assessments of a patient not on telemetry, clinicians erroneously reported that patients were on it 24.8% of the time (n = 157).
Assessments by direct-care attendings were more accurate than those done by teaching attendings (80.9% vs. 72.4%, P < 0.05) and resident physicians (80.9% vs. 71.8%, P < 0.05). There was no statistically significant difference in accuracy of resident physician assessments when compared to teaching attending assessments (71.8% vs. 72.4%, P = 0.81).
DISCUSSION
In this study, clinicians often inaccurately recalled the telemetry status of their hospitalized patients. These findings have implications for both patient safety as well as telemetry overuse, as ignorance of telemetry status may limit its discontinuation.
The authors also found that assessments done by direct-care attendings were more accurate than those done by teaching attendings. This discrepancy is likely related to different roles in patient care: teaching attendings provide supervisory roles, while direct-care attendings routinely review orders and perform detailed exams on their patients. Similarly, resident physician assessments were found to be less accurate than direct-care attending assessments, which may reflect less clinical experience as well as their supervisory role.
In light of these findings, interventions to reduce telemetry overuse should include efforts to increase real-time telemetry awareness as well as reduce inappropriate use, and should target all levels of training. Using research on urinary catheter removal10 as a model, strategies to increase telemetry awareness could include daily verbal or written reminders of telemetry status, requests to assess daily need, high visibility signs in charts or in patient rooms, or electronic reminders that telemetry is in place. Furthermore, efforts to promote and operationalize medical mindfulness, in which providers are trained to be aware of indications, timely removal, and the presence of monitoring devices could be incorporated into broader telemetry stewardship and high-value care efforts.11
There are limitations to this study. The authors did not collect information on the number of unique individual physicians represented by the study, and, thus, clinicians may have been surveyed multiple times throughout the study, potentially influencing their attention to the telemetry status of their patients. In addition, this study was conducted within a single healthcare system, limiting its generalizability.
In conclusion, the authors found that physicians were often incorrect when assessing the telemetry status of their patients. Interventions to help raise awareness of a patient’s telemetry status may help reduce telemetry overuse.
Disclosure: Nothing to report.
1. Henriques-Forsythe MN, Ivonye CC, Jamched U, Kamuguisha LKK, Olejeme KA, Onwuanyi AE. Is telemetry overused? Is it as helpful as thought? Cleve Clin J Med. 2009;76:368-372. PubMed
2. Kanwar M, Fares R, Minnick S, Rosman HS, Saravolatz L. Inpatient cardiac telemetry monitoring: are we overdoing it. JCOM. 2008;15(1):16-20.
3. Chong-Yik R, Bennett A, Milani R, Morin D. Telemetry overuse and its economic implications. J Am Coll Cardiol.2016;67(13_S):1993.
4. Najafi N, Auerbach A. Use and outcomes of telemetry monitoring on a medicine service. Arch Intern Med. 2012;172:1349-1350. PubMed
5. Bulger J, Nickel W, Messler J, et al. Choosing wisely in adult hospital medicine: five opportunities for improved healthcare value. J Hosp Med. 2013;8:486-492. PubMed
6. Leighton H, Kianfar H, Serynek S, Kerwin T. Effect of an electronic ordering system on adherence to the American College of Cardiology/American Heart Association guidelines for cardiac monitoring. Crit Pathw Cardiol. 2013;12:6-8. PubMed
7. Lee JC, Lamb P, Rand E, Ryan C, Rubal BJ. Optimizing telemetry utilization in an academic medical center. JCOM. 2008;15(9).
8. Boggan JC, Navar-Boggan AM, Patel V, Schulteis RD, Simel DL. Reductions in telemetry order duration do not reduce telemetry utilization. J Hosp Med. 2014;9:795-796. PubMed
9. Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering overuse of cardiac telemetry in non-intensive care unit settings by hardwiring the use of American Heart Association guidelines. JAMA Intern Med. 2014;174:1852-1854. PubMed
10. Meddings J, Krein SL, Fakih MG, Olmsted RN, Saint S. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infections: brief update review. In: Making Health Care Safer II: An Updated Critical Analysis of the Evidence for Patient Safety Practices. (Evidence Reports/Technology Assessments, No. 211.) Chapter 9. Rockville (MD): Agency for Healthcare Research and Quality (US); 2013. Available from: http://www.ncbi.nlm.nih.gov/books/NBK133354/. May 15, 2016. PubMed
11. Kiyoshi-Teo H, Krein SL, Saint S. Applying mindful evidence-based practice at the bedside: using catheter-associated urinary tract infection as a model. Infect Control Hosp Epidemiol. 2013;34:1099-1001. PubMed
1. Henriques-Forsythe MN, Ivonye CC, Jamched U, Kamuguisha LKK, Olejeme KA, Onwuanyi AE. Is telemetry overused? Is it as helpful as thought? Cleve Clin J Med. 2009;76:368-372. PubMed
2. Kanwar M, Fares R, Minnick S, Rosman HS, Saravolatz L. Inpatient cardiac telemetry monitoring: are we overdoing it. JCOM. 2008;15(1):16-20.
3. Chong-Yik R, Bennett A, Milani R, Morin D. Telemetry overuse and its economic implications. J Am Coll Cardiol.2016;67(13_S):1993.
4. Najafi N, Auerbach A. Use and outcomes of telemetry monitoring on a medicine service. Arch Intern Med. 2012;172:1349-1350. PubMed
5. Bulger J, Nickel W, Messler J, et al. Choosing wisely in adult hospital medicine: five opportunities for improved healthcare value. J Hosp Med. 2013;8:486-492. PubMed
6. Leighton H, Kianfar H, Serynek S, Kerwin T. Effect of an electronic ordering system on adherence to the American College of Cardiology/American Heart Association guidelines for cardiac monitoring. Crit Pathw Cardiol. 2013;12:6-8. PubMed
7. Lee JC, Lamb P, Rand E, Ryan C, Rubal BJ. Optimizing telemetry utilization in an academic medical center. JCOM. 2008;15(9).
8. Boggan JC, Navar-Boggan AM, Patel V, Schulteis RD, Simel DL. Reductions in telemetry order duration do not reduce telemetry utilization. J Hosp Med. 2014;9:795-796. PubMed
9. Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering overuse of cardiac telemetry in non-intensive care unit settings by hardwiring the use of American Heart Association guidelines. JAMA Intern Med. 2014;174:1852-1854. PubMed
10. Meddings J, Krein SL, Fakih MG, Olmsted RN, Saint S. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infections: brief update review. In: Making Health Care Safer II: An Updated Critical Analysis of the Evidence for Patient Safety Practices. (Evidence Reports/Technology Assessments, No. 211.) Chapter 9. Rockville (MD): Agency for Healthcare Research and Quality (US); 2013. Available from: http://www.ncbi.nlm.nih.gov/books/NBK133354/. May 15, 2016. PubMed
11. Kiyoshi-Teo H, Krein SL, Saint S. Applying mindful evidence-based practice at the bedside: using catheter-associated urinary tract infection as a model. Infect Control Hosp Epidemiol. 2013;34:1099-1001. PubMed
© 2017 Society of Hospital Medicine
Depression in pediatric bipolar disorder
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Hip Arthroscopy
Editor’s Note: AJO is fortunate to have Shane Nho, one of the nation’s leading hip arthroscopists, as our Deputy Editor-in-Chief. He has compiled an outstanding update for all orthopedic surgeons who see hip patients. It’s my pleasure to turn this issue over to him. On a side note, we’ve added a new feature for our speed readers. From now on, all articles published in AJO will feature a “Take-Home Points” text box. These points represent the most important items that the authors wish to convey from their article. Please enjoy this month’s issue and keep the feedback coming. We are striving to continuously improve AJO and make it your go-to journal for practical information that you can apply directly to your practice.
—Bryan T. Hanypsiak, MD
Hip arthroscopy has been evolving over the past 2 decades as our techniques have been refined and our clinical outcomes have been reported. We have reached a point in our field to look back at the progress that has been made while also providing our readers with the most up-to-date information on diagnosis, imaging studies, and decision making for appropriate treatment.
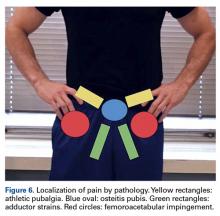
Trofa and colleagues provide an excellent overview on intra- and extra-articular pathology of the hip and pelvis in their article, “Mastering the Physical Examination of the Athlete’s Hip”. The authors review common injuries in the athlete and provide physical examination tests to differentiate between adductor strain, athletic pubalgia, osteitis pubis, and femoroacetabular impingement (FAI). Also in this issue, Lewis and colleagues provide a comprehensive review of imaging studies in the “Imaging for Nonarthritic Hip Pathology”. The authors review the most common radiographic measurements to detect FAI as well as describe the role of computed tomography and magnetic resonance imaging.
The mastery of hip arthroscopy for the treatment of FAI has a steep learning curve and the techniques have evolved along with our understanding of the importance of the labrum and capsule. We are fortunate to have an article provided by one of the pioneers in the field, Dr. Marc J. Philippon, describing his role in advancing the field in the article “Treatment of FAI: Labrum, Cartilage, Osseous Deformity, and Capsule”. Kollmorgen and Mather provide the most up-to-date techniques for labrum repair and reconstruction. Friel and colleagues report on capsular repair and plication using the T-capsulotomy and the extensile interportal capsulotomy.
We also have the opportunity to read about a number of clinical studies describing the experiences of multi-center studies and epidemiologic studies on large volumes of data. The ANCHOR group provides a summary of the experiences of some of the most renowned hip surgeons in North America as the treatment of FAI evolved from an open approach to an all-arthroscopic approach. The MASH group is a large multi-center group of hip arthroscopists in the United States who describe their current indications for surgical treatment of FAI.
On AmJOrthopedics.com, Matsuda and colleagues describe the outcomes of borderline dysplasia patients compared to normal controls across multiple centers. Anthony and colleagues report on the complication rates using the National Surgical Quality Improvement Program database.
I believe that our Hip Arthroscopy issue will not disappoint you. It is a comprehensive review of the state-of-the-art in hip arthroscopy from physical examination to current surgical techniques to clinical outcomes from large databases for the treatment of FAI. After reviewing this issue, you will be equipped with the most up-to-date information on the treatment of nonarthritic hip disease.
Am J Orthop. 2017;46(1):8. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
Editor’s Note: AJO is fortunate to have Shane Nho, one of the nation’s leading hip arthroscopists, as our Deputy Editor-in-Chief. He has compiled an outstanding update for all orthopedic surgeons who see hip patients. It’s my pleasure to turn this issue over to him. On a side note, we’ve added a new feature for our speed readers. From now on, all articles published in AJO will feature a “Take-Home Points” text box. These points represent the most important items that the authors wish to convey from their article. Please enjoy this month’s issue and keep the feedback coming. We are striving to continuously improve AJO and make it your go-to journal for practical information that you can apply directly to your practice.
—Bryan T. Hanypsiak, MD
Hip arthroscopy has been evolving over the past 2 decades as our techniques have been refined and our clinical outcomes have been reported. We have reached a point in our field to look back at the progress that has been made while also providing our readers with the most up-to-date information on diagnosis, imaging studies, and decision making for appropriate treatment.
Trofa and colleagues provide an excellent overview on intra- and extra-articular pathology of the hip and pelvis in their article, “Mastering the Physical Examination of the Athlete’s Hip”. The authors review common injuries in the athlete and provide physical examination tests to differentiate between adductor strain, athletic pubalgia, osteitis pubis, and femoroacetabular impingement (FAI). Also in this issue, Lewis and colleagues provide a comprehensive review of imaging studies in the “Imaging for Nonarthritic Hip Pathology”. The authors review the most common radiographic measurements to detect FAI as well as describe the role of computed tomography and magnetic resonance imaging.
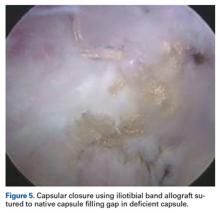
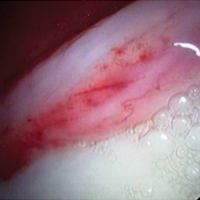
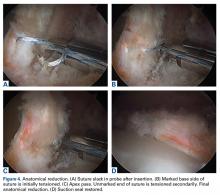
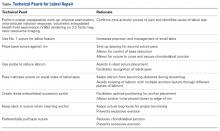
The mastery of hip arthroscopy for the treatment of FAI has a steep learning curve and the techniques have evolved along with our understanding of the importance of the labrum and capsule. We are fortunate to have an article provided by one of the pioneers in the field, Dr. Marc J. Philippon, describing his role in advancing the field in the article “Treatment of FAI: Labrum, Cartilage, Osseous Deformity, and Capsule”. Kollmorgen and Mather provide the most up-to-date techniques for labrum repair and reconstruction. Friel and colleagues report on capsular repair and plication using the T-capsulotomy and the extensile interportal capsulotomy.
We also have the opportunity to read about a number of clinical studies describing the experiences of multi-center studies and epidemiologic studies on large volumes of data. The ANCHOR group provides a summary of the experiences of some of the most renowned hip surgeons in North America as the treatment of FAI evolved from an open approach to an all-arthroscopic approach. The MASH group is a large multi-center group of hip arthroscopists in the United States who describe their current indications for surgical treatment of FAI.
On AmJOrthopedics.com, Matsuda and colleagues describe the outcomes of borderline dysplasia patients compared to normal controls across multiple centers. Anthony and colleagues report on the complication rates using the National Surgical Quality Improvement Program database.
I believe that our Hip Arthroscopy issue will not disappoint you. It is a comprehensive review of the state-of-the-art in hip arthroscopy from physical examination to current surgical techniques to clinical outcomes from large databases for the treatment of FAI. After reviewing this issue, you will be equipped with the most up-to-date information on the treatment of nonarthritic hip disease.
Am J Orthop. 2017;46(1):8. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
Editor’s Note: AJO is fortunate to have Shane Nho, one of the nation’s leading hip arthroscopists, as our Deputy Editor-in-Chief. He has compiled an outstanding update for all orthopedic surgeons who see hip patients. It’s my pleasure to turn this issue over to him. On a side note, we’ve added a new feature for our speed readers. From now on, all articles published in AJO will feature a “Take-Home Points” text box. These points represent the most important items that the authors wish to convey from their article. Please enjoy this month’s issue and keep the feedback coming. We are striving to continuously improve AJO and make it your go-to journal for practical information that you can apply directly to your practice.
—Bryan T. Hanypsiak, MD
Hip arthroscopy has been evolving over the past 2 decades as our techniques have been refined and our clinical outcomes have been reported. We have reached a point in our field to look back at the progress that has been made while also providing our readers with the most up-to-date information on diagnosis, imaging studies, and decision making for appropriate treatment.
Trofa and colleagues provide an excellent overview on intra- and extra-articular pathology of the hip and pelvis in their article, “Mastering the Physical Examination of the Athlete’s Hip”. The authors review common injuries in the athlete and provide physical examination tests to differentiate between adductor strain, athletic pubalgia, osteitis pubis, and femoroacetabular impingement (FAI). Also in this issue, Lewis and colleagues provide a comprehensive review of imaging studies in the “Imaging for Nonarthritic Hip Pathology”. The authors review the most common radiographic measurements to detect FAI as well as describe the role of computed tomography and magnetic resonance imaging.
The mastery of hip arthroscopy for the treatment of FAI has a steep learning curve and the techniques have evolved along with our understanding of the importance of the labrum and capsule. We are fortunate to have an article provided by one of the pioneers in the field, Dr. Marc J. Philippon, describing his role in advancing the field in the article “Treatment of FAI: Labrum, Cartilage, Osseous Deformity, and Capsule”. Kollmorgen and Mather provide the most up-to-date techniques for labrum repair and reconstruction. Friel and colleagues report on capsular repair and plication using the T-capsulotomy and the extensile interportal capsulotomy.
We also have the opportunity to read about a number of clinical studies describing the experiences of multi-center studies and epidemiologic studies on large volumes of data. The ANCHOR group provides a summary of the experiences of some of the most renowned hip surgeons in North America as the treatment of FAI evolved from an open approach to an all-arthroscopic approach. The MASH group is a large multi-center group of hip arthroscopists in the United States who describe their current indications for surgical treatment of FAI.
On AmJOrthopedics.com, Matsuda and colleagues describe the outcomes of borderline dysplasia patients compared to normal controls across multiple centers. Anthony and colleagues report on the complication rates using the National Surgical Quality Improvement Program database.
I believe that our Hip Arthroscopy issue will not disappoint you. It is a comprehensive review of the state-of-the-art in hip arthroscopy from physical examination to current surgical techniques to clinical outcomes from large databases for the treatment of FAI. After reviewing this issue, you will be equipped with the most up-to-date information on the treatment of nonarthritic hip disease.
Am J Orthop. 2017;46(1):8. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
Mastering the Physical Examination of the Athlete’s Hip
Take-Home Points
- Perform a comprehensive examination to determine intra-articular pathology as well as potential extra-articular sources of hip and pelvic pain.
- Adductor strains can be prevented with adequate rehabilitation focused on correcting predisposing factors (ie, adductor weakness or tightness, limited range of motion, and core imbalance).
- Athletic pubalgia is diagnosed when tenderness can be elicited over the pubic tubercle.
- Osteitis pubis is diagnosed with pain over the pubic symphysis.
- FAI and labral injury classically present with a C-sign but can also present with lateral hip pain, buttock pain, low back pain, anterior thigh pain, and knee pain.
Hip and groin pain is a common finding among athletes of all ages and activity levels. Such pain most often occurs among athletes in sports such as football, hockey, rugby, soccer, and ballet, which demand frequent cutting, pivoting, and acceleration.1-4 Previously, pain about the hip and groin was attributed to muscular strains and soft-tissue contusions, but improvements in physical examination skills, imaging modalities, and disease-specific treatment options have led to increased recognition of hip injuries as a significant source of disability in the athletic population.5,6 These injuries make up 6% or more of all sports injuries, and the rate is increasing.7-9
In this review, we describe precise methods for evaluating the athlete’s hip or groin with an emphasis on recognizing the most common extra-articular and intra-articular pathologies, including adductor strains, athletic pubalgia, osteitis pubis, and femoroacetabular impingement (FAI) with labral tears.
Hip Pathoanatomy
The first step in determining the etiology of pain is to establish if there is true pathology of the hip joint and surrounding structures, or if the pain is referred from another source.
Patient History
The physical examination is guided by the patient’s history. Important patient-specific factors to be ascertained include age, sport(s) played, competition level, seasonal timing, and effect of the injury on performance. Regarding presenting symptoms, attention should be given to pain location, timing (acute vs chronic), onset, nature (clicking, catching, instability), and precipitating factors. Acute-onset pain with muscle contraction or stretching, possibly accompanied by an audible pop, is likely musculotendinous in origin. Insidious-onset dull aching pain that worsens with activity more commonly involves intra-articular processes. Most classically, this pain occurs deep in the groin and is demonstrated by the C sign: The patient cups a hand with its fingers pointing toward the anterior groin at the level of the greater trochanter (Figure 1).11
A comprehensive hip evaluation can be performed with the patient in the standing, seated, supine, lateral, and prone positions, as previously described (Table 2).6,12,13
Extra-Articular Hip Pathologies
Adductor Strains
The adductor muscle group includes the adductor magnus, adductor brevis, gracilis, obturator externus, pectineus, and adductor longus, which is the most commonly strained. Adductor strains are the most common cause of groin pain in athletes, and usually occur in sports that require forceful eccentric contraction of the adductors.14 Among professional soccer players, adductor strains represent almost one fourth of all muscle injuries and result in lost playing time averaging 2 weeks and an 18% reinjury rate.15 These injuries are particularly detrimental to performance because the adductor muscles help stabilize the pelvis during closed-chain activities.3 Diagnosis and adequate rehabilitation focused on correcting predisposing factors (eg, adductor weakness or tightness, loss of hip range of motion, core imbalance) are paramount in reinjury prevention.16,17
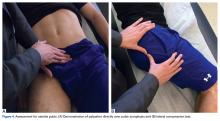
On presentation, athletes complain of aching groin or medial thigh pain. The examiner should assess for swelling or ecchymosis. There typically is tenderness to palpation at or near the origin on the pubic bones, with pain exacerbated with resisted adduction and passive stretch into abduction during examination. Palpation of adductors requires proper exposure and is most easily performed with the patient supine and the lower extremity in a figure-of-4 position (Figure 2A).
Athletic Pubalgia
Athletic pubalgia, also known as sports hernia or core muscle injury, is an injury to the soft tissues of the lower abdominal or posterior inguinal wall. Although not fully understood, the condition is considered the result of repetitive trunk hyperextension and thigh hyperabduction resulting in shearing at the pubic symphysis where there is a muscle imbalance between the strong proximal thigh muscles and weaker abdominals. This condition is more common in men and typically is insidious in onset with a prolonged course recalcitrant to nonoperative treatment.18 In studies of chronic groin pain in athletes, the rate of athletic pubalgia as the primary etiology ranges from 39% to 85%.9,19,20
Patients typically complain of increasing pain in the lower abdominal and proximal adductors during activity. Symptoms include unilateral or bilateral lower abdominal pain, which can radiate toward the perineum, rectus muscle, and proximal adductors during sport but usually abates with rest.18 Athletes endorse they are not capable of playing at their full athletic potential. Symptoms are initiated with sudden forceful movements, as in sit-ups, sprints, and valsalva maneuvers like coughs and sneezes. Valsalva maneuvers worsen pain in about 10% of patients.21-23On physical examination with the patient supine, tenderness can be elicited over the pubic tubercle, abdominal obliques, and/or rectus abdominis insertion (Figure 3A). Athletes may also have tenderness at the adductor longus tendon origin at or near the pubic symphysis, which may make the diagnosis difficult to distinguish from an adductor strain.
Osteitis Pubis
Osteitis pubis is a painful overuse injury that results in noninfectious inflammation of the pubic symphysis from increased motion at this normally stable immobile joint.3 As with athletic pubalgia, the exact mechanism is unclear, but likely it is similar to the repetitive stress placed on the pubic symphysis by unequal forces of the abdominal and adductor muscles.24 The disease can result in bony erosions and cartilage breakdown with irregularity of the pubic symphysis.
Athletes may complain of anterior and medial groin pain that can radiate to the lower abdominal muscles, perineum, inguinal region, and medial thigh. Walking, pelvic motion, adductor stretching, abdominal muscle exercises, and standing up can exacerbate pain.24 Some cases involve impaired internal or external rotation of the hip, sacroiliac joint dysfunction, or adductor and abductor muscle weakness.25The distinguishing feature of osteitis pubis is pain over the pubic symphysis with direct palpation (Figure 4A). Examination maneuvers that place stress on the pubic symphysis can aid in diagnosis.26
Intra-Articular Hip Pathology: Femoroacetabular Impingement
In athletes, FAI is a leading cause of intra-articular pathology, which can lead to labral tears.28,29 FAI lesions include cam-type impingement from an aspherical femoral head and pincer impingement from acetabular overcoverage, both of which limit internal rotation and cause acetabular rim abutment, which damages the labrum.
Athletes present with activity-related groin or hip pain that is exacerbated by hip flexion and internal rotation, with possible mechanical symptoms from labral tearing.30 However, the pain distribution varies. In a study by Clohisy and colleagues,31 of patients with symptomatic FAI that required surgical intervention, 88% had groin pain, 67% had lateral hip pain, 35% had anterior thigh pain, 29% had buttock pain, 27% had knee pain, and 23% had low back pain.
Careful attention should be given to range of motion in FAI patients, as they can usually flex their hip to 90° to 110°, and in this position there is limited internal rotation and asymmetric external rotation relative to the contralateral leg.32 The anterior impingement test is one of the most reliable tests for FAI (Figure 5A).32 With the patient supine, the hip is dynamically flexed to 90°, adducted, and internally rotated. A positive test elicits deep anterior groin pain that generally replicates the patient’s symptoms.29
Conclusion
Careful, directed history taking and physical examination are essential in narrowing the diagnostic possibilities before initiating a workup for the common intra-articular and extra-articular causes of hip and groin pain in athletes.
Am J Orthop. 2017;46(1):10-16. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Boyd KT, Peirce NS, Batt ME. Common hip injuries in sport. Sports Med. 1997;24(4):273-288.
2. Duthon VB, Charbonnier C, Kolo FC, et al. Correlation of clinical and magnetic resonance imaging findings in hips of elite female ballet dancers. Arthroscopy. 2013;29(3):411-419.
3. Prather H, Cheng A. Diagnosis and treatment of hip girdle pain in the athlete. PM R. 2016;8(3 suppl):S45-S60.
4. Larson CM. Sports hernia/athletic pubalgia: evaluation and management. Sports Health. 2014;6(2):139-144.
5. Bizzini M, Notzli HP, Maffiuletti NA. Femoroacetabular impingement in professional ice hockey players: a case series of 5 athletes after open surgical decompression of the hip. Am J Sports Med. 2007;35(11):1955-1959.
6. Lynch TS, Terry MA, Bedi A, Kelly BT. Hip arthroscopic surgery: patient evaluation, current indications, and outcomes. Am J Sports Med. 2013;41(5):1174-1189.
7. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29(4):521-533.
8. Fon LJ, Spence RA. Sportsman’s hernia. Br J Surg. 2000;87(5):545-552.
9. Kluin J, den Hoed PT, van Linschoten R, IJzerman JC, van Steensel CJ. Endoscopic evaluation and treatment of groin pain in the athlete. Am J Sports Med. 2004;32(4):944-949.
10. Ward D, Parvizi J. Management of hip pain in young adults. Orthop Clin North Am. 2016;47(3):485-496.
11. Byrd JW. Hip arthroscopy. J Am Acad Orthop Surg. 2006;14(7):433-444.
12. Martin HD, Palmer IJ. History and physical examination of the hip: the basics. Curr Rev Musculoskelet Med. 2013;6(3):219-225.
13. Shindle MK, Voos JE, Nho SJ, Heyworth BE, Kelly BT. Arthroscopic management of labral tears in the hip. J Bone Joint Surg Am. 2008;90(suppl 4):2-19.
14. Morelli V, Smith V. Groin injuries in athletes. Am Fam Physician. 2001;64(8):1405-1414.
15. Ekstrand J, Hagglund M, Walden M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226-1232.
16. Ekstrand J, Gillquist J. The avoidability of soccer injuries. Int J Sports Med. 1983;4(2):124-128.
17. Tyler TF, Nicholas SJ, Campbell RJ, McHugh MP. The association of hip strength and flexibility with the incidence of adductor muscle strains in professional ice hockey players. Am J Sports Med. 2001;29(2):124-128.
18. Farber AJ, Wilckens JH. Sports hernia: diagnosis and therapeutic approach. J Am Acad Orthop Surg. 2007;15(8):507-514.
19. De Paulis F, Cacchio A, Michelini O, Damiani A, Saggini R. Sports injuries in the pelvis and hip: diagnostic imaging. Eur J Radiol. 1998;27(suppl 1):S49-S59.
20. Lovell G. The diagnosis of chronic groin pain in athletes: a review of 189 cases. Aust J Sci Med Sport. 1995;27(suppl 1):76-79.
21. Strosberg DS, Ellis TJ, Renton DB. The role of femoroacetabular impingement in core muscle injury/athletic pubalgia: diagnosis and management. Front Surg. 2016;3:6.
22. Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BR. Management of severe lower abdominal or inguinal pain in high-performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med. 2000;28(1):2-8.
23. Ahumada LA, Ashruf S, Espinosa-de-los-Monteros A, et al. Athletic pubalgia: definition and surgical treatment. Ann Plast Surg. 2005;55(4):393-396.
24. Angoules AG. Osteitis pubis in elite athletes: diagnostic and therapeutic approach. World J Orthop. 2015;6(9):672-679.
25. Hiti CJ, Stevens KJ, Jamati MK, Garza D, Matheson GO. Athletic osteitis pubis. Sports Med. 2011;41(5):361-376.
26. Mehin R, Meek R, O’Brien P, Blachut P. Surgery for osteitis pubis. Can J Surg. 2006;49(3):170-176.
27. Grace JN, Sim FH, Shives TC, Coventry MB. Wedge resection of the symphysis pubis for the treatment of osteitis pubis. J Bone Joint Surg Am. 1989;71(3):358-364.
28. Amanatullah DF, Antkowiak T, Pillay K, et al. Femoroacetabular impingement: current concepts in diagnosis and treatment. Orthopedics. 2015;38(3):185-199.
29. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112-120.
30. Redmond JM, Gupta A, Hammarstedt JE, Stake CE, Dunne KF, Domb BG. Labral injury: radiographic predictors at the time of hip arthroscopy. Arthroscopy. 2015;31(1):51-56.
31. Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467(3):638-644.
32. Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73(3):423-429.
33. Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006;25(2):299-308.
34. McCarthy JC, Lee JA. Hip arthroscopy: indications, outcomes, and complications. Instr Course Lect. 2006;55:301-308.
Take-Home Points
- Perform a comprehensive examination to determine intra-articular pathology as well as potential extra-articular sources of hip and pelvic pain.
- Adductor strains can be prevented with adequate rehabilitation focused on correcting predisposing factors (ie, adductor weakness or tightness, limited range of motion, and core imbalance).
- Athletic pubalgia is diagnosed when tenderness can be elicited over the pubic tubercle.
- Osteitis pubis is diagnosed with pain over the pubic symphysis.
- FAI and labral injury classically present with a C-sign but can also present with lateral hip pain, buttock pain, low back pain, anterior thigh pain, and knee pain.
Hip and groin pain is a common finding among athletes of all ages and activity levels. Such pain most often occurs among athletes in sports such as football, hockey, rugby, soccer, and ballet, which demand frequent cutting, pivoting, and acceleration.1-4 Previously, pain about the hip and groin was attributed to muscular strains and soft-tissue contusions, but improvements in physical examination skills, imaging modalities, and disease-specific treatment options have led to increased recognition of hip injuries as a significant source of disability in the athletic population.5,6 These injuries make up 6% or more of all sports injuries, and the rate is increasing.7-9
In this review, we describe precise methods for evaluating the athlete’s hip or groin with an emphasis on recognizing the most common extra-articular and intra-articular pathologies, including adductor strains, athletic pubalgia, osteitis pubis, and femoroacetabular impingement (FAI) with labral tears.
Hip Pathoanatomy
The first step in determining the etiology of pain is to establish if there is true pathology of the hip joint and surrounding structures, or if the pain is referred from another source.
Patient History
The physical examination is guided by the patient’s history. Important patient-specific factors to be ascertained include age, sport(s) played, competition level, seasonal timing, and effect of the injury on performance. Regarding presenting symptoms, attention should be given to pain location, timing (acute vs chronic), onset, nature (clicking, catching, instability), and precipitating factors. Acute-onset pain with muscle contraction or stretching, possibly accompanied by an audible pop, is likely musculotendinous in origin. Insidious-onset dull aching pain that worsens with activity more commonly involves intra-articular processes. Most classically, this pain occurs deep in the groin and is demonstrated by the C sign: The patient cups a hand with its fingers pointing toward the anterior groin at the level of the greater trochanter (Figure 1).11
A comprehensive hip evaluation can be performed with the patient in the standing, seated, supine, lateral, and prone positions, as previously described (Table 2).6,12,13
Extra-Articular Hip Pathologies
Adductor Strains
The adductor muscle group includes the adductor magnus, adductor brevis, gracilis, obturator externus, pectineus, and adductor longus, which is the most commonly strained. Adductor strains are the most common cause of groin pain in athletes, and usually occur in sports that require forceful eccentric contraction of the adductors.14 Among professional soccer players, adductor strains represent almost one fourth of all muscle injuries and result in lost playing time averaging 2 weeks and an 18% reinjury rate.15 These injuries are particularly detrimental to performance because the adductor muscles help stabilize the pelvis during closed-chain activities.3 Diagnosis and adequate rehabilitation focused on correcting predisposing factors (eg, adductor weakness or tightness, loss of hip range of motion, core imbalance) are paramount in reinjury prevention.16,17
On presentation, athletes complain of aching groin or medial thigh pain. The examiner should assess for swelling or ecchymosis. There typically is tenderness to palpation at or near the origin on the pubic bones, with pain exacerbated with resisted adduction and passive stretch into abduction during examination. Palpation of adductors requires proper exposure and is most easily performed with the patient supine and the lower extremity in a figure-of-4 position (Figure 2A).
Athletic Pubalgia
Athletic pubalgia, also known as sports hernia or core muscle injury, is an injury to the soft tissues of the lower abdominal or posterior inguinal wall. Although not fully understood, the condition is considered the result of repetitive trunk hyperextension and thigh hyperabduction resulting in shearing at the pubic symphysis where there is a muscle imbalance between the strong proximal thigh muscles and weaker abdominals. This condition is more common in men and typically is insidious in onset with a prolonged course recalcitrant to nonoperative treatment.18 In studies of chronic groin pain in athletes, the rate of athletic pubalgia as the primary etiology ranges from 39% to 85%.9,19,20
Patients typically complain of increasing pain in the lower abdominal and proximal adductors during activity. Symptoms include unilateral or bilateral lower abdominal pain, which can radiate toward the perineum, rectus muscle, and proximal adductors during sport but usually abates with rest.18 Athletes endorse they are not capable of playing at their full athletic potential. Symptoms are initiated with sudden forceful movements, as in sit-ups, sprints, and valsalva maneuvers like coughs and sneezes. Valsalva maneuvers worsen pain in about 10% of patients.21-23On physical examination with the patient supine, tenderness can be elicited over the pubic tubercle, abdominal obliques, and/or rectus abdominis insertion (Figure 3A). Athletes may also have tenderness at the adductor longus tendon origin at or near the pubic symphysis, which may make the diagnosis difficult to distinguish from an adductor strain.
Osteitis Pubis
Osteitis pubis is a painful overuse injury that results in noninfectious inflammation of the pubic symphysis from increased motion at this normally stable immobile joint.3 As with athletic pubalgia, the exact mechanism is unclear, but likely it is similar to the repetitive stress placed on the pubic symphysis by unequal forces of the abdominal and adductor muscles.24 The disease can result in bony erosions and cartilage breakdown with irregularity of the pubic symphysis.
Athletes may complain of anterior and medial groin pain that can radiate to the lower abdominal muscles, perineum, inguinal region, and medial thigh. Walking, pelvic motion, adductor stretching, abdominal muscle exercises, and standing up can exacerbate pain.24 Some cases involve impaired internal or external rotation of the hip, sacroiliac joint dysfunction, or adductor and abductor muscle weakness.25The distinguishing feature of osteitis pubis is pain over the pubic symphysis with direct palpation (Figure 4A). Examination maneuvers that place stress on the pubic symphysis can aid in diagnosis.26
Intra-Articular Hip Pathology: Femoroacetabular Impingement
In athletes, FAI is a leading cause of intra-articular pathology, which can lead to labral tears.28,29 FAI lesions include cam-type impingement from an aspherical femoral head and pincer impingement from acetabular overcoverage, both of which limit internal rotation and cause acetabular rim abutment, which damages the labrum.
Athletes present with activity-related groin or hip pain that is exacerbated by hip flexion and internal rotation, with possible mechanical symptoms from labral tearing.30 However, the pain distribution varies. In a study by Clohisy and colleagues,31 of patients with symptomatic FAI that required surgical intervention, 88% had groin pain, 67% had lateral hip pain, 35% had anterior thigh pain, 29% had buttock pain, 27% had knee pain, and 23% had low back pain.
Careful attention should be given to range of motion in FAI patients, as they can usually flex their hip to 90° to 110°, and in this position there is limited internal rotation and asymmetric external rotation relative to the contralateral leg.32 The anterior impingement test is one of the most reliable tests for FAI (Figure 5A).32 With the patient supine, the hip is dynamically flexed to 90°, adducted, and internally rotated. A positive test elicits deep anterior groin pain that generally replicates the patient’s symptoms.29
Conclusion
Careful, directed history taking and physical examination are essential in narrowing the diagnostic possibilities before initiating a workup for the common intra-articular and extra-articular causes of hip and groin pain in athletes.
Am J Orthop. 2017;46(1):10-16. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
Take-Home Points
- Perform a comprehensive examination to determine intra-articular pathology as well as potential extra-articular sources of hip and pelvic pain.
- Adductor strains can be prevented with adequate rehabilitation focused on correcting predisposing factors (ie, adductor weakness or tightness, limited range of motion, and core imbalance).
- Athletic pubalgia is diagnosed when tenderness can be elicited over the pubic tubercle.
- Osteitis pubis is diagnosed with pain over the pubic symphysis.
- FAI and labral injury classically present with a C-sign but can also present with lateral hip pain, buttock pain, low back pain, anterior thigh pain, and knee pain.
Hip and groin pain is a common finding among athletes of all ages and activity levels. Such pain most often occurs among athletes in sports such as football, hockey, rugby, soccer, and ballet, which demand frequent cutting, pivoting, and acceleration.1-4 Previously, pain about the hip and groin was attributed to muscular strains and soft-tissue contusions, but improvements in physical examination skills, imaging modalities, and disease-specific treatment options have led to increased recognition of hip injuries as a significant source of disability in the athletic population.5,6 These injuries make up 6% or more of all sports injuries, and the rate is increasing.7-9
In this review, we describe precise methods for evaluating the athlete’s hip or groin with an emphasis on recognizing the most common extra-articular and intra-articular pathologies, including adductor strains, athletic pubalgia, osteitis pubis, and femoroacetabular impingement (FAI) with labral tears.
Hip Pathoanatomy
The first step in determining the etiology of pain is to establish if there is true pathology of the hip joint and surrounding structures, or if the pain is referred from another source.
Patient History
The physical examination is guided by the patient’s history. Important patient-specific factors to be ascertained include age, sport(s) played, competition level, seasonal timing, and effect of the injury on performance. Regarding presenting symptoms, attention should be given to pain location, timing (acute vs chronic), onset, nature (clicking, catching, instability), and precipitating factors. Acute-onset pain with muscle contraction or stretching, possibly accompanied by an audible pop, is likely musculotendinous in origin. Insidious-onset dull aching pain that worsens with activity more commonly involves intra-articular processes. Most classically, this pain occurs deep in the groin and is demonstrated by the C sign: The patient cups a hand with its fingers pointing toward the anterior groin at the level of the greater trochanter (Figure 1).11
A comprehensive hip evaluation can be performed with the patient in the standing, seated, supine, lateral, and prone positions, as previously described (Table 2).6,12,13
Extra-Articular Hip Pathologies
Adductor Strains
The adductor muscle group includes the adductor magnus, adductor brevis, gracilis, obturator externus, pectineus, and adductor longus, which is the most commonly strained. Adductor strains are the most common cause of groin pain in athletes, and usually occur in sports that require forceful eccentric contraction of the adductors.14 Among professional soccer players, adductor strains represent almost one fourth of all muscle injuries and result in lost playing time averaging 2 weeks and an 18% reinjury rate.15 These injuries are particularly detrimental to performance because the adductor muscles help stabilize the pelvis during closed-chain activities.3 Diagnosis and adequate rehabilitation focused on correcting predisposing factors (eg, adductor weakness or tightness, loss of hip range of motion, core imbalance) are paramount in reinjury prevention.16,17
On presentation, athletes complain of aching groin or medial thigh pain. The examiner should assess for swelling or ecchymosis. There typically is tenderness to palpation at or near the origin on the pubic bones, with pain exacerbated with resisted adduction and passive stretch into abduction during examination. Palpation of adductors requires proper exposure and is most easily performed with the patient supine and the lower extremity in a figure-of-4 position (Figure 2A).
Athletic Pubalgia
Athletic pubalgia, also known as sports hernia or core muscle injury, is an injury to the soft tissues of the lower abdominal or posterior inguinal wall. Although not fully understood, the condition is considered the result of repetitive trunk hyperextension and thigh hyperabduction resulting in shearing at the pubic symphysis where there is a muscle imbalance between the strong proximal thigh muscles and weaker abdominals. This condition is more common in men and typically is insidious in onset with a prolonged course recalcitrant to nonoperative treatment.18 In studies of chronic groin pain in athletes, the rate of athletic pubalgia as the primary etiology ranges from 39% to 85%.9,19,20
Patients typically complain of increasing pain in the lower abdominal and proximal adductors during activity. Symptoms include unilateral or bilateral lower abdominal pain, which can radiate toward the perineum, rectus muscle, and proximal adductors during sport but usually abates with rest.18 Athletes endorse they are not capable of playing at their full athletic potential. Symptoms are initiated with sudden forceful movements, as in sit-ups, sprints, and valsalva maneuvers like coughs and sneezes. Valsalva maneuvers worsen pain in about 10% of patients.21-23On physical examination with the patient supine, tenderness can be elicited over the pubic tubercle, abdominal obliques, and/or rectus abdominis insertion (Figure 3A). Athletes may also have tenderness at the adductor longus tendon origin at or near the pubic symphysis, which may make the diagnosis difficult to distinguish from an adductor strain.
Osteitis Pubis
Osteitis pubis is a painful overuse injury that results in noninfectious inflammation of the pubic symphysis from increased motion at this normally stable immobile joint.3 As with athletic pubalgia, the exact mechanism is unclear, but likely it is similar to the repetitive stress placed on the pubic symphysis by unequal forces of the abdominal and adductor muscles.24 The disease can result in bony erosions and cartilage breakdown with irregularity of the pubic symphysis.
Athletes may complain of anterior and medial groin pain that can radiate to the lower abdominal muscles, perineum, inguinal region, and medial thigh. Walking, pelvic motion, adductor stretching, abdominal muscle exercises, and standing up can exacerbate pain.24 Some cases involve impaired internal or external rotation of the hip, sacroiliac joint dysfunction, or adductor and abductor muscle weakness.25The distinguishing feature of osteitis pubis is pain over the pubic symphysis with direct palpation (Figure 4A). Examination maneuvers that place stress on the pubic symphysis can aid in diagnosis.26
Intra-Articular Hip Pathology: Femoroacetabular Impingement
In athletes, FAI is a leading cause of intra-articular pathology, which can lead to labral tears.28,29 FAI lesions include cam-type impingement from an aspherical femoral head and pincer impingement from acetabular overcoverage, both of which limit internal rotation and cause acetabular rim abutment, which damages the labrum.
Athletes present with activity-related groin or hip pain that is exacerbated by hip flexion and internal rotation, with possible mechanical symptoms from labral tearing.30 However, the pain distribution varies. In a study by Clohisy and colleagues,31 of patients with symptomatic FAI that required surgical intervention, 88% had groin pain, 67% had lateral hip pain, 35% had anterior thigh pain, 29% had buttock pain, 27% had knee pain, and 23% had low back pain.
Careful attention should be given to range of motion in FAI patients, as they can usually flex their hip to 90° to 110°, and in this position there is limited internal rotation and asymmetric external rotation relative to the contralateral leg.32 The anterior impingement test is one of the most reliable tests for FAI (Figure 5A).32 With the patient supine, the hip is dynamically flexed to 90°, adducted, and internally rotated. A positive test elicits deep anterior groin pain that generally replicates the patient’s symptoms.29
Conclusion
Careful, directed history taking and physical examination are essential in narrowing the diagnostic possibilities before initiating a workup for the common intra-articular and extra-articular causes of hip and groin pain in athletes.
Am J Orthop. 2017;46(1):10-16. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Boyd KT, Peirce NS, Batt ME. Common hip injuries in sport. Sports Med. 1997;24(4):273-288.
2. Duthon VB, Charbonnier C, Kolo FC, et al. Correlation of clinical and magnetic resonance imaging findings in hips of elite female ballet dancers. Arthroscopy. 2013;29(3):411-419.
3. Prather H, Cheng A. Diagnosis and treatment of hip girdle pain in the athlete. PM R. 2016;8(3 suppl):S45-S60.
4. Larson CM. Sports hernia/athletic pubalgia: evaluation and management. Sports Health. 2014;6(2):139-144.
5. Bizzini M, Notzli HP, Maffiuletti NA. Femoroacetabular impingement in professional ice hockey players: a case series of 5 athletes after open surgical decompression of the hip. Am J Sports Med. 2007;35(11):1955-1959.
6. Lynch TS, Terry MA, Bedi A, Kelly BT. Hip arthroscopic surgery: patient evaluation, current indications, and outcomes. Am J Sports Med. 2013;41(5):1174-1189.
7. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29(4):521-533.
8. Fon LJ, Spence RA. Sportsman’s hernia. Br J Surg. 2000;87(5):545-552.
9. Kluin J, den Hoed PT, van Linschoten R, IJzerman JC, van Steensel CJ. Endoscopic evaluation and treatment of groin pain in the athlete. Am J Sports Med. 2004;32(4):944-949.
10. Ward D, Parvizi J. Management of hip pain in young adults. Orthop Clin North Am. 2016;47(3):485-496.
11. Byrd JW. Hip arthroscopy. J Am Acad Orthop Surg. 2006;14(7):433-444.
12. Martin HD, Palmer IJ. History and physical examination of the hip: the basics. Curr Rev Musculoskelet Med. 2013;6(3):219-225.
13. Shindle MK, Voos JE, Nho SJ, Heyworth BE, Kelly BT. Arthroscopic management of labral tears in the hip. J Bone Joint Surg Am. 2008;90(suppl 4):2-19.
14. Morelli V, Smith V. Groin injuries in athletes. Am Fam Physician. 2001;64(8):1405-1414.
15. Ekstrand J, Hagglund M, Walden M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226-1232.
16. Ekstrand J, Gillquist J. The avoidability of soccer injuries. Int J Sports Med. 1983;4(2):124-128.
17. Tyler TF, Nicholas SJ, Campbell RJ, McHugh MP. The association of hip strength and flexibility with the incidence of adductor muscle strains in professional ice hockey players. Am J Sports Med. 2001;29(2):124-128.
18. Farber AJ, Wilckens JH. Sports hernia: diagnosis and therapeutic approach. J Am Acad Orthop Surg. 2007;15(8):507-514.
19. De Paulis F, Cacchio A, Michelini O, Damiani A, Saggini R. Sports injuries in the pelvis and hip: diagnostic imaging. Eur J Radiol. 1998;27(suppl 1):S49-S59.
20. Lovell G. The diagnosis of chronic groin pain in athletes: a review of 189 cases. Aust J Sci Med Sport. 1995;27(suppl 1):76-79.
21. Strosberg DS, Ellis TJ, Renton DB. The role of femoroacetabular impingement in core muscle injury/athletic pubalgia: diagnosis and management. Front Surg. 2016;3:6.
22. Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BR. Management of severe lower abdominal or inguinal pain in high-performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med. 2000;28(1):2-8.
23. Ahumada LA, Ashruf S, Espinosa-de-los-Monteros A, et al. Athletic pubalgia: definition and surgical treatment. Ann Plast Surg. 2005;55(4):393-396.
24. Angoules AG. Osteitis pubis in elite athletes: diagnostic and therapeutic approach. World J Orthop. 2015;6(9):672-679.
25. Hiti CJ, Stevens KJ, Jamati MK, Garza D, Matheson GO. Athletic osteitis pubis. Sports Med. 2011;41(5):361-376.
26. Mehin R, Meek R, O’Brien P, Blachut P. Surgery for osteitis pubis. Can J Surg. 2006;49(3):170-176.
27. Grace JN, Sim FH, Shives TC, Coventry MB. Wedge resection of the symphysis pubis for the treatment of osteitis pubis. J Bone Joint Surg Am. 1989;71(3):358-364.
28. Amanatullah DF, Antkowiak T, Pillay K, et al. Femoroacetabular impingement: current concepts in diagnosis and treatment. Orthopedics. 2015;38(3):185-199.
29. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112-120.
30. Redmond JM, Gupta A, Hammarstedt JE, Stake CE, Dunne KF, Domb BG. Labral injury: radiographic predictors at the time of hip arthroscopy. Arthroscopy. 2015;31(1):51-56.
31. Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467(3):638-644.
32. Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73(3):423-429.
33. Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006;25(2):299-308.
34. McCarthy JC, Lee JA. Hip arthroscopy: indications, outcomes, and complications. Instr Course Lect. 2006;55:301-308.
1. Boyd KT, Peirce NS, Batt ME. Common hip injuries in sport. Sports Med. 1997;24(4):273-288.
2. Duthon VB, Charbonnier C, Kolo FC, et al. Correlation of clinical and magnetic resonance imaging findings in hips of elite female ballet dancers. Arthroscopy. 2013;29(3):411-419.
3. Prather H, Cheng A. Diagnosis and treatment of hip girdle pain in the athlete. PM R. 2016;8(3 suppl):S45-S60.
4. Larson CM. Sports hernia/athletic pubalgia: evaluation and management. Sports Health. 2014;6(2):139-144.
5. Bizzini M, Notzli HP, Maffiuletti NA. Femoroacetabular impingement in professional ice hockey players: a case series of 5 athletes after open surgical decompression of the hip. Am J Sports Med. 2007;35(11):1955-1959.
6. Lynch TS, Terry MA, Bedi A, Kelly BT. Hip arthroscopic surgery: patient evaluation, current indications, and outcomes. Am J Sports Med. 2013;41(5):1174-1189.
7. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29(4):521-533.
8. Fon LJ, Spence RA. Sportsman’s hernia. Br J Surg. 2000;87(5):545-552.
9. Kluin J, den Hoed PT, van Linschoten R, IJzerman JC, van Steensel CJ. Endoscopic evaluation and treatment of groin pain in the athlete. Am J Sports Med. 2004;32(4):944-949.
10. Ward D, Parvizi J. Management of hip pain in young adults. Orthop Clin North Am. 2016;47(3):485-496.
11. Byrd JW. Hip arthroscopy. J Am Acad Orthop Surg. 2006;14(7):433-444.
12. Martin HD, Palmer IJ. History and physical examination of the hip: the basics. Curr Rev Musculoskelet Med. 2013;6(3):219-225.
13. Shindle MK, Voos JE, Nho SJ, Heyworth BE, Kelly BT. Arthroscopic management of labral tears in the hip. J Bone Joint Surg Am. 2008;90(suppl 4):2-19.
14. Morelli V, Smith V. Groin injuries in athletes. Am Fam Physician. 2001;64(8):1405-1414.
15. Ekstrand J, Hagglund M, Walden M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226-1232.
16. Ekstrand J, Gillquist J. The avoidability of soccer injuries. Int J Sports Med. 1983;4(2):124-128.
17. Tyler TF, Nicholas SJ, Campbell RJ, McHugh MP. The association of hip strength and flexibility with the incidence of adductor muscle strains in professional ice hockey players. Am J Sports Med. 2001;29(2):124-128.
18. Farber AJ, Wilckens JH. Sports hernia: diagnosis and therapeutic approach. J Am Acad Orthop Surg. 2007;15(8):507-514.
19. De Paulis F, Cacchio A, Michelini O, Damiani A, Saggini R. Sports injuries in the pelvis and hip: diagnostic imaging. Eur J Radiol. 1998;27(suppl 1):S49-S59.
20. Lovell G. The diagnosis of chronic groin pain in athletes: a review of 189 cases. Aust J Sci Med Sport. 1995;27(suppl 1):76-79.
21. Strosberg DS, Ellis TJ, Renton DB. The role of femoroacetabular impingement in core muscle injury/athletic pubalgia: diagnosis and management. Front Surg. 2016;3:6.
22. Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BR. Management of severe lower abdominal or inguinal pain in high-performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med. 2000;28(1):2-8.
23. Ahumada LA, Ashruf S, Espinosa-de-los-Monteros A, et al. Athletic pubalgia: definition and surgical treatment. Ann Plast Surg. 2005;55(4):393-396.
24. Angoules AG. Osteitis pubis in elite athletes: diagnostic and therapeutic approach. World J Orthop. 2015;6(9):672-679.
25. Hiti CJ, Stevens KJ, Jamati MK, Garza D, Matheson GO. Athletic osteitis pubis. Sports Med. 2011;41(5):361-376.
26. Mehin R, Meek R, O’Brien P, Blachut P. Surgery for osteitis pubis. Can J Surg. 2006;49(3):170-176.
27. Grace JN, Sim FH, Shives TC, Coventry MB. Wedge resection of the symphysis pubis for the treatment of osteitis pubis. J Bone Joint Surg Am. 1989;71(3):358-364.
28. Amanatullah DF, Antkowiak T, Pillay K, et al. Femoroacetabular impingement: current concepts in diagnosis and treatment. Orthopedics. 2015;38(3):185-199.
29. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112-120.
30. Redmond JM, Gupta A, Hammarstedt JE, Stake CE, Dunne KF, Domb BG. Labral injury: radiographic predictors at the time of hip arthroscopy. Arthroscopy. 2015;31(1):51-56.
31. Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467(3):638-644.
32. Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73(3):423-429.
33. Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006;25(2):299-308.
34. McCarthy JC, Lee JA. Hip arthroscopy: indications, outcomes, and complications. Instr Course Lect. 2006;55:301-308.
Treatment of Femoroacetabular Impingement: Labrum, Cartilage, Osseous Deformity, and Capsule
Take-Home Points
- Repair the labrum when tissue quality is good.
- Avoid overcorrection of acetabulum by measuring center edge angle.
- Cam resection should be comprehensive and restore a smooth head-neck offset to restore the suction seal.
- Chondral débridement for Outerbridge grade 0-3 and microfracture for grade 4.
- Routine capsular closure to prevent postoperative instability.
The surgical approach of femoroacetabular impingement (FAI) pathology should cover the entire hip joint. Both bony and cartilaginous tissue pathology should be adequately addressed. However, treating soft-tissue abnormalities (acetabular labrum and joint capsule) is also crucial. Overall, any surgical intervention should focus on restoring the hip labrum seal mechanism to ensure successful clinical outcomes. This restoration, combined with the use of biological therapies and rehabilitation, will produce the maximum benefit for the patient.
Management of Acetabular Labrum
The final decision regarding how to surgically approach the acetabular labrum is made during the operation. We focus restoring the labrum seal mechanism, which is crucial for proper function and health of the hip joint.1 The intra-articular hydrostatic pressure loss caused by labral deficiency results in abnormal load distribution and joint microinstability, which have detrimental effects on cartilage and periarticular tissues. A biomechanical study highlighted the role of the hip labrum in maintaining intra-articular fluid pressurization and showed that labral reconstruction restores intra-articular fluid pressure to levels similar to those of the intact state.1
In cases in which the remaining labral tissue is adequate and of good quality (reparable), the labral repair technique is preferred.2 After diagnostic arthroscopy, the labral tear is identified, and a 4.5-mm burr is used to correct (rim-trim) any osseous deformity of the acetabulum to create a “new rim” for labrum reattachment. Suture anchors are placed on the rim about 2 mm to 3 mm below the cartilage surface. Considering the rim angle3 is helpful in avoiding acetabular cartilage damage. Labral sutures can be looped around or pierced through the labrum to secure it to the acetabulum. No difference in clinical outcomes was found between the 2 suture types,4 though biomechanically piercing sutures help restore the labrum seal better.1 When the labrum is deficient and longitudinal fibers remain but are insufficient for seal restoration, the repair can be augmented with adjacent iliotibial band (ITB) tissue. This technique is similar to labral reconstruction but involves placing a graft on top of the remaining labral tissue, and suture around both the native tissue and the graft. The additional tissue gives the labrum the volume it needs to recreate the seal.
The labral reconstruction technique is indicated when the remaining labrum is irreparable, absent, or severely hypotrophic or deficient, or when an irreparable complex tear or poor-quality tissue is present. Different types of grafts can be used to reconstruct the labrum. ITB, semitendinosus, gracilis, and anterior tibialis grafts and the human acetabular labrum exhibit similar cyclic elongation behavior in response to simulated physiologic forces, though there is variability in both elongation and geometry for all graft types.5 We prefer the ITB autograft technique.6 The graft should be about 30% to 40% longer than the labral defect as measured with arthroscopic probe. With the leg in traction, the graft is inserted through the mid-anterior portal, and a suture anchor is used to secure it against the acetabulum medially.
With proper patient selection, these techniques have excellent clinical outcomes.4,7 Severe osteoarthritis (joint space <2 mm) is a contraindication for these procedures.8
Osseous Deformity
On approaching the bony structures of the hip joint, the surgeon should examine the acetabular rim (pincer lesion), the femoral head and neck shape (cam lesion), and the anterior inferior iliac spine (AIIS). Preoperative imaging and physical examination are important for identifying severe bone deformities that can complicate the procedure.9
The acetabular rim can be directly viewed after labrum detachment, but usually complete detachment is not necessary. Pincer deformity causes focal or global overcoverage of the femoral head. Rim trimming is performed with a 4.5-mm round curved burr. Resection is usually performed to the end of rim chondrosis (about 3-5 mm). Using a simple formula, you can calculate how the lateral center edge will be reduced by the amount of rim resected, maintaining a safe margin.2 A new acetabular “bed” is created where the to-be-attached labral tissue will contribute to the suction seal mechanism of the joint.2Cam lesion correction is challenging, and the amount of bone that should be resected is a matter of disagreement. We perform cam osteochondroplasty2 with a 5.5-mm round burr inserted through the anterolateral portal while the hip is positioned in 45° of flexion, neutral rotation, and adduction/abduction. This position allows an osteoplasty from 6 to 10 o’clock on the head–neck junction. Osteoplasty performed between 10 and 12 o’clock requires hip extension and slight traction. The proximal limit of osteochondroplasty is about 15 mm from the labral edge, while distally the resection stops beneath the zona orbicularis. The lateral epiphyseal vessels and the Weitbrecht ligament constitute the lateral and medial borders, respectively.
The surgeon should create a smooth head–neck offset that prevents elevation of the labrum during flexion and achieves a nearly perfect anatomical relationship between the femoral head and the acetabular labrum, restoring the hip joint seal (Figure 2).
A hypertrophic AIIS can impinge the femur (extra-articular subspinal impingement). Patients present with limited range of motion (especially hip flexion), pain in the AIIS area, and, in some cases, a history of avulsion injury.11 Seeing a bruised labrum (Figure 3) during surgery is common with this pathology.
Treatment of Cartilage Lesions
The indications and contraindications for hip arthroscopy in patients with cartilage lesions are important. Our study’s 5-year outcomes of treating FAI with hip arthroscopy in patients with preserved joint space (>2 mm) were promising, though 86% of patients with limited joint space (≤2 mm) converted to total hip arthroplasty.8 We regard patients with severe osteoarthritis as not being candidates for hip arthroscopy.
As 3 Tesla magnetic resonance imaging has low positive predictive value in identifying severe cartilage damage,13 the cartilage should be examined during surgery to further define the diagnosis. Nearly half of the hip arthroscopy patients in our study had at least 1 Outerbridge grade 3 or 4 cartilage lesion.14 Compared with the femoral head, acetabular cartilage was damaged 3 times more often. More than 90% of acetabular cartilage lesions were in the anterosuperior region.
Grades 0 and 1 cartilage lesions are usually left untreated; no intervention is necessary. Grades 2 and 3 cartilage lesions are reduced by partial débridement and/or thermal shrinkage. With the improved joint microenvironment arising from simple correction of the underlying hip bony abnormalities, these lesions should not produce further symptoms.
Grade 4 hip cartilage defects are challenging. We prefer microfracture for grade 4 lesions (Figure 4).
A ring curette is used to prepare the defect, and perpendicular borders are created to hold the clot in place. Deep débridement removes the calcified layer while maintaining the integrity of the subchondral plate.15 As a recent study found microfracture performed with small-diameter awls improved cartilage repair more effectively than microfracture with large-diameter awls,16 we prefer making small-diameter holes when establishing the maximum number of holes possible. As it is important to make a perpendicular hole, not a scratch, we use an XL Microfracture Pick (Smith & Nephew) 90° curve, which is suitable for creating a vertical entry point. The 60° curved awl is then used to further deepen the hole. Creation and stability of the marrow clot are ensured by shutting down the infusion pump device and verifying that blood and marrow elements are released from the microfractures.
Capsule Management
The increase in hip arthroscopies performed worldwide has generated interest in proper capsular management and development of iatrogenic microinstability.17 Hip capsulotomy is routinely performed for adequate visualization of the intra-articular compartment. Standard anterosuperior interportal capsulotomy for hip arthroscopic surgery (12 to 3 o’clock) sacrifices the integrity of the iliofemoral ligament (ligament of Bigelow),18 which provides rotational stability. Failure to restore the anatomical and biomechanical properties of the iliofemoral ligament after arthroscopic surgery increases the likelihood of postoperative microinstability or gross instability,19 which can lead to persistent pain and/or sense of an unstable joint, in addition to accelerated cartilage wear.
Capsulotomies are useful in obtaining adequate intraoperative exposure of the central and peripheral compartments. In the past, little attention was given to capsular closure on completion of the procedure. However, concern about postoperative instability from capsular laxity or deficiency made the introduction of capsular repair techniques necessary. Although deciding between capsular closure and plication remains debatable, we routinely perform capsular closure with a Quebec City slider knot.20 Mindful management of the capsule throughout the procedure is important in avoiding irreversible capsular damage, which would complicate capsular closure. Mindful management involves leaving a proximal leaflet of at least 1 cm during the capsulotomy, avoiding capsular thinning during shaver use, and using a cannula to prevent soft-tissue bridging.
Recent evidence suggests that capsule repair restores near native hip joint stability.17 In addition to capsular shift or capsulorrhaphy, 2 to 6 sutures have been used for capsular closure or plication after an interportal or T capsulotomy. Chahla and colleagues21 reported that 2- and 3-suture constructs produced comparable biomechanical failure torques when external rotation forces were applied to conventional hip capsulotomy on cadavers. Three-suture constructs were significantly stronger than 1-suture constructs, but there was no significant difference between 2- and 3-suture constructs. All constructs failed at about 36° of external rotation. Therefore, restricted external rotation is recommended for 3 weeks after surgery.
In one study, 35% of revision hip arthroscopy patients had undiagnosed hip instability from iatrogenic injury,22 which can lead to labral and chondral injury.17 Capsular reconstruction is recommended in cases of symptomatic capsular deficiency; capsular deficiency caused by adhesion removal; and pain and range-of-motion limitation caused by capsular adhesions. However, indications need to be further established. We have performed capsular reconstruction with ITB allograft23 (Figure 5).
Biologics
At the end of the procedure, we use platelet-rich plasma and/or bone marrow aspirate injections (individualized to the patient) to potentiate the biological healing of the tissues. Further research is planned to determine how to prepare these biological products to provide the best mix of biological factors for improved healing. Antifibrotic factors are useful in preventing adhesions, and angiotensin II receptor blockers are effective, but clinical studies are needed to establish their use.
Rehabilitation
Immediately after surgery, a postoperative hip brace and antirotational boots are applied to the patient to protect the operative site and reduce pain. The actual postoperative protocol is based on the procedure and individualized to the patient. During microfractures, the patient is kept 20 pounds touch-toe weight-bearing for 4 to 8 weeks. The capsular closure is brace-protected by limiting abduction to 0° to 45° and hip flexion to 0° to 90° while external rotation and extension are prohibited (first 3 weeks). Immediate mobilization with passive rotational movement is crucial in preventing adhesions. Stationary bike exercise and use of a continuous passive motion machine are helpful. Progressive functional and sport-specific rehabilitation help the patient return to full activity, though the decision to return to full activity is based on several factors, both objective (functional tests) and subjective (physician–patient co-decisions).
Conclusion
Although hip arthroscopic techniques have expanded significantly in recent years, our treatment approach is based on restoring the normal anatomy of the hip joint—combining the procedures with biological therapies and a postoperative rehabilitation program that is individualized to the patient’s special needs.
Am J Orthop. 2017;46(1):23-27. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Philippon MJ, Nepple JJ, Campbell KJ, et al. The hip fluid seal—part I: the effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):722-729.
2. Philippon MJ, Faucet SC, Briggs KK. Arthroscopic hip labral repair. Arthrosc Tech. 2013;2(2):e73-e76.
3. Lertwanich P, Ejnisman L, Torry MR, Giphart JE, Philippon MJ. Defining a safety margin for labral suture anchor insertion using the acetabular rim angle. Am J Sports Med. 2011;39(suppl):111S-116S.
4. Sawyer GA, Briggs KK, Dornan GJ, Ommen ND, Philippon MJ. Clinical outcomes after arthroscopic hip labral repair using looped versus pierced suture techniques. Am J Sports Med. 2015;43(7):1683-1688.
5. Ferro FP, Philippon MJ, Rasmussen MT, Smith SD, LaPrade RF, Wijdicks CA. Tensile properties of the human acetabular labrum and hip labral reconstruction grafts. Am J Sports Med. 2015;43(5):1222-1227.
6. Philippon MJ, Briggs KK, Boykin RE. Results of arthroscopic labral reconstruction of the hip in elite athletes: response. Am J Sports Med. 2014;42(10):NP48.
7. Geyer MR, Philippon MJ, Fagrelius TS, Briggs KK. Acetabular labral reconstruction with an iliotibial band autograft: outcome and survivorship analysis at minimum 3-year follow-up. Am J Sports Med. 2013;41(8):1750-1756.
8. Skendzel JG, Philippon MJ, Briggs KK, Goljan P. The effect of joint space on midterm outcomes after arthroscopic hip surgery for femoroacetabular impingement. Am J Sports Med. 2014;42(5):1127-1133.
9. Yeung M, Kowalczuk M, Simunovic N, Ayeni OR. Hip arthroscopy in the setting of hip dysplasia: a systematic review. Bone Joint Res. 2016;5(6):225-231.
10. Locks R, Chahla J, Mitchell JJ, Soares E, Philippon MJ. Dynamic hip examination for assesment of impingement during hip arthroscopy. Arthroscopy Tech. 2016 Nov 28. http://dx.doi.org/10.1016/j.eats.2016.08.011
11. Nabhan DC, Moreau WJ, McNamara SC, Briggs KK, Philippon MJ. Subspine hip impingement: an unusual cause of hip pain in an elite weightlifter. Curr Sports Med Rep. 2016;15(5):315-319.
12. Philippon MJ, Michalski MP, Campbell KJ, et al. An anatomical study of the acetabulum with clinical applications to hip arthroscopy. J Bone Joint Surg Am. 2014;96(20):1673-1682.
13. Ho CP, Ommen ND, Bhatia S, et al. Predictive value of 3-T magnetic resonance imaging in diagnosing grade 3 and 4 chondral lesions in the hip. Arthroscopy. 2016;32(9):1808-1813.
14. Bhatia S, Nowak DD, Briggs KK, Patterson DC, Philippon MJ. Outerbridge grade IV cartilage lesions in the hip identified at arthroscopy. Arthroscopy. 2016;32(5):814-819.
15. Frisbie DD, Morisset S, Ho CP, Rodkey WG, Steadman JR, McIlwraith CW. Effects of calcified cartilage on healing of chondral defects treated with microfracture in horses. Am J Sports Med. 2006;34(11):1824-1831.
16. Orth P, Duffner J, Zurakowski D, Cucchiarini M, Madry H. Small-diameter awls improve articular cartilage repair after microfracture treatment in a translational animal model. Am J Sports Med. 2016;44(1):209-219.
17. Domb BG, Philippon MJ, Giordano BD. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: relation to atraumatic instability. Arthroscopy. 2013;29(1):162-173.
18. Asopa V, Singh PJ. The intracapsular atraumatic arthroscopic technique for closure of the hip capsule. Arthrosc Tech. 2014;3(2):e245-e247.
19. Frank RM, Lee S, Bush-Joseph CA, Kelly BT, Salata MJ, Nho SJ. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42(11):2634-2642.
20. Menge TJ, Chahla J, Soares E, Mitchell JJ, Philippon MJ. The Quebec City slider: a technique for capsular closure and plication in hip arthroscopy. Arthrosc Tech. 2016;5(5):e971-e974.
21. Chahla J, Mikula JD, Schon JM, et al. Hip capsular closure: a biomechanical analysis of failure torque. Am J Sports Med. doi:10.1177/0363546516666353.
22. Philippon MJ, Schenker ML, Briggs KK, Kuppersmith DA, Maxwell RB, Stubbs AJ. Revision hip arthroscopy. Am J Sports Med. 2007;35(11):1918-1921.
23. Trindade CA, Sawyer GA, Fukui K, Briggs KK, Philippon MJ. Arthroscopic capsule reconstruction in the hip using iliotibial band allograft. Arthrosc Tech. 2015;4(1):e71-e74.
Take-Home Points
- Repair the labrum when tissue quality is good.
- Avoid overcorrection of acetabulum by measuring center edge angle.
- Cam resection should be comprehensive and restore a smooth head-neck offset to restore the suction seal.
- Chondral débridement for Outerbridge grade 0-3 and microfracture for grade 4.
- Routine capsular closure to prevent postoperative instability.
The surgical approach of femoroacetabular impingement (FAI) pathology should cover the entire hip joint. Both bony and cartilaginous tissue pathology should be adequately addressed. However, treating soft-tissue abnormalities (acetabular labrum and joint capsule) is also crucial. Overall, any surgical intervention should focus on restoring the hip labrum seal mechanism to ensure successful clinical outcomes. This restoration, combined with the use of biological therapies and rehabilitation, will produce the maximum benefit for the patient.
Management of Acetabular Labrum
The final decision regarding how to surgically approach the acetabular labrum is made during the operation. We focus restoring the labrum seal mechanism, which is crucial for proper function and health of the hip joint.1 The intra-articular hydrostatic pressure loss caused by labral deficiency results in abnormal load distribution and joint microinstability, which have detrimental effects on cartilage and periarticular tissues. A biomechanical study highlighted the role of the hip labrum in maintaining intra-articular fluid pressurization and showed that labral reconstruction restores intra-articular fluid pressure to levels similar to those of the intact state.1
In cases in which the remaining labral tissue is adequate and of good quality (reparable), the labral repair technique is preferred.2 After diagnostic arthroscopy, the labral tear is identified, and a 4.5-mm burr is used to correct (rim-trim) any osseous deformity of the acetabulum to create a “new rim” for labrum reattachment. Suture anchors are placed on the rim about 2 mm to 3 mm below the cartilage surface. Considering the rim angle3 is helpful in avoiding acetabular cartilage damage. Labral sutures can be looped around or pierced through the labrum to secure it to the acetabulum. No difference in clinical outcomes was found between the 2 suture types,4 though biomechanically piercing sutures help restore the labrum seal better.1 When the labrum is deficient and longitudinal fibers remain but are insufficient for seal restoration, the repair can be augmented with adjacent iliotibial band (ITB) tissue. This technique is similar to labral reconstruction but involves placing a graft on top of the remaining labral tissue, and suture around both the native tissue and the graft. The additional tissue gives the labrum the volume it needs to recreate the seal.
The labral reconstruction technique is indicated when the remaining labrum is irreparable, absent, or severely hypotrophic or deficient, or when an irreparable complex tear or poor-quality tissue is present. Different types of grafts can be used to reconstruct the labrum. ITB, semitendinosus, gracilis, and anterior tibialis grafts and the human acetabular labrum exhibit similar cyclic elongation behavior in response to simulated physiologic forces, though there is variability in both elongation and geometry for all graft types.5 We prefer the ITB autograft technique.6 The graft should be about 30% to 40% longer than the labral defect as measured with arthroscopic probe. With the leg in traction, the graft is inserted through the mid-anterior portal, and a suture anchor is used to secure it against the acetabulum medially.
With proper patient selection, these techniques have excellent clinical outcomes.4,7 Severe osteoarthritis (joint space <2 mm) is a contraindication for these procedures.8
Osseous Deformity
On approaching the bony structures of the hip joint, the surgeon should examine the acetabular rim (pincer lesion), the femoral head and neck shape (cam lesion), and the anterior inferior iliac spine (AIIS). Preoperative imaging and physical examination are important for identifying severe bone deformities that can complicate the procedure.9
The acetabular rim can be directly viewed after labrum detachment, but usually complete detachment is not necessary. Pincer deformity causes focal or global overcoverage of the femoral head. Rim trimming is performed with a 4.5-mm round curved burr. Resection is usually performed to the end of rim chondrosis (about 3-5 mm). Using a simple formula, you can calculate how the lateral center edge will be reduced by the amount of rim resected, maintaining a safe margin.2 A new acetabular “bed” is created where the to-be-attached labral tissue will contribute to the suction seal mechanism of the joint.2Cam lesion correction is challenging, and the amount of bone that should be resected is a matter of disagreement. We perform cam osteochondroplasty2 with a 5.5-mm round burr inserted through the anterolateral portal while the hip is positioned in 45° of flexion, neutral rotation, and adduction/abduction. This position allows an osteoplasty from 6 to 10 o’clock on the head–neck junction. Osteoplasty performed between 10 and 12 o’clock requires hip extension and slight traction. The proximal limit of osteochondroplasty is about 15 mm from the labral edge, while distally the resection stops beneath the zona orbicularis. The lateral epiphyseal vessels and the Weitbrecht ligament constitute the lateral and medial borders, respectively.
The surgeon should create a smooth head–neck offset that prevents elevation of the labrum during flexion and achieves a nearly perfect anatomical relationship between the femoral head and the acetabular labrum, restoring the hip joint seal (Figure 2).
A hypertrophic AIIS can impinge the femur (extra-articular subspinal impingement). Patients present with limited range of motion (especially hip flexion), pain in the AIIS area, and, in some cases, a history of avulsion injury.11 Seeing a bruised labrum (Figure 3) during surgery is common with this pathology.
Treatment of Cartilage Lesions
The indications and contraindications for hip arthroscopy in patients with cartilage lesions are important. Our study’s 5-year outcomes of treating FAI with hip arthroscopy in patients with preserved joint space (>2 mm) were promising, though 86% of patients with limited joint space (≤2 mm) converted to total hip arthroplasty.8 We regard patients with severe osteoarthritis as not being candidates for hip arthroscopy.
As 3 Tesla magnetic resonance imaging has low positive predictive value in identifying severe cartilage damage,13 the cartilage should be examined during surgery to further define the diagnosis. Nearly half of the hip arthroscopy patients in our study had at least 1 Outerbridge grade 3 or 4 cartilage lesion.14 Compared with the femoral head, acetabular cartilage was damaged 3 times more often. More than 90% of acetabular cartilage lesions were in the anterosuperior region.
Grades 0 and 1 cartilage lesions are usually left untreated; no intervention is necessary. Grades 2 and 3 cartilage lesions are reduced by partial débridement and/or thermal shrinkage. With the improved joint microenvironment arising from simple correction of the underlying hip bony abnormalities, these lesions should not produce further symptoms.
Grade 4 hip cartilage defects are challenging. We prefer microfracture for grade 4 lesions (Figure 4).
A ring curette is used to prepare the defect, and perpendicular borders are created to hold the clot in place. Deep débridement removes the calcified layer while maintaining the integrity of the subchondral plate.15 As a recent study found microfracture performed with small-diameter awls improved cartilage repair more effectively than microfracture with large-diameter awls,16 we prefer making small-diameter holes when establishing the maximum number of holes possible. As it is important to make a perpendicular hole, not a scratch, we use an XL Microfracture Pick (Smith & Nephew) 90° curve, which is suitable for creating a vertical entry point. The 60° curved awl is then used to further deepen the hole. Creation and stability of the marrow clot are ensured by shutting down the infusion pump device and verifying that blood and marrow elements are released from the microfractures.
Capsule Management
The increase in hip arthroscopies performed worldwide has generated interest in proper capsular management and development of iatrogenic microinstability.17 Hip capsulotomy is routinely performed for adequate visualization of the intra-articular compartment. Standard anterosuperior interportal capsulotomy for hip arthroscopic surgery (12 to 3 o’clock) sacrifices the integrity of the iliofemoral ligament (ligament of Bigelow),18 which provides rotational stability. Failure to restore the anatomical and biomechanical properties of the iliofemoral ligament after arthroscopic surgery increases the likelihood of postoperative microinstability or gross instability,19 which can lead to persistent pain and/or sense of an unstable joint, in addition to accelerated cartilage wear.
Capsulotomies are useful in obtaining adequate intraoperative exposure of the central and peripheral compartments. In the past, little attention was given to capsular closure on completion of the procedure. However, concern about postoperative instability from capsular laxity or deficiency made the introduction of capsular repair techniques necessary. Although deciding between capsular closure and plication remains debatable, we routinely perform capsular closure with a Quebec City slider knot.20 Mindful management of the capsule throughout the procedure is important in avoiding irreversible capsular damage, which would complicate capsular closure. Mindful management involves leaving a proximal leaflet of at least 1 cm during the capsulotomy, avoiding capsular thinning during shaver use, and using a cannula to prevent soft-tissue bridging.
Recent evidence suggests that capsule repair restores near native hip joint stability.17 In addition to capsular shift or capsulorrhaphy, 2 to 6 sutures have been used for capsular closure or plication after an interportal or T capsulotomy. Chahla and colleagues21 reported that 2- and 3-suture constructs produced comparable biomechanical failure torques when external rotation forces were applied to conventional hip capsulotomy on cadavers. Three-suture constructs were significantly stronger than 1-suture constructs, but there was no significant difference between 2- and 3-suture constructs. All constructs failed at about 36° of external rotation. Therefore, restricted external rotation is recommended for 3 weeks after surgery.
In one study, 35% of revision hip arthroscopy patients had undiagnosed hip instability from iatrogenic injury,22 which can lead to labral and chondral injury.17 Capsular reconstruction is recommended in cases of symptomatic capsular deficiency; capsular deficiency caused by adhesion removal; and pain and range-of-motion limitation caused by capsular adhesions. However, indications need to be further established. We have performed capsular reconstruction with ITB allograft23 (Figure 5).
Biologics
At the end of the procedure, we use platelet-rich plasma and/or bone marrow aspirate injections (individualized to the patient) to potentiate the biological healing of the tissues. Further research is planned to determine how to prepare these biological products to provide the best mix of biological factors for improved healing. Antifibrotic factors are useful in preventing adhesions, and angiotensin II receptor blockers are effective, but clinical studies are needed to establish their use.
Rehabilitation
Immediately after surgery, a postoperative hip brace and antirotational boots are applied to the patient to protect the operative site and reduce pain. The actual postoperative protocol is based on the procedure and individualized to the patient. During microfractures, the patient is kept 20 pounds touch-toe weight-bearing for 4 to 8 weeks. The capsular closure is brace-protected by limiting abduction to 0° to 45° and hip flexion to 0° to 90° while external rotation and extension are prohibited (first 3 weeks). Immediate mobilization with passive rotational movement is crucial in preventing adhesions. Stationary bike exercise and use of a continuous passive motion machine are helpful. Progressive functional and sport-specific rehabilitation help the patient return to full activity, though the decision to return to full activity is based on several factors, both objective (functional tests) and subjective (physician–patient co-decisions).
Conclusion
Although hip arthroscopic techniques have expanded significantly in recent years, our treatment approach is based on restoring the normal anatomy of the hip joint—combining the procedures with biological therapies and a postoperative rehabilitation program that is individualized to the patient’s special needs.
Am J Orthop. 2017;46(1):23-27. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
Take-Home Points
- Repair the labrum when tissue quality is good.
- Avoid overcorrection of acetabulum by measuring center edge angle.
- Cam resection should be comprehensive and restore a smooth head-neck offset to restore the suction seal.
- Chondral débridement for Outerbridge grade 0-3 and microfracture for grade 4.
- Routine capsular closure to prevent postoperative instability.
The surgical approach of femoroacetabular impingement (FAI) pathology should cover the entire hip joint. Both bony and cartilaginous tissue pathology should be adequately addressed. However, treating soft-tissue abnormalities (acetabular labrum and joint capsule) is also crucial. Overall, any surgical intervention should focus on restoring the hip labrum seal mechanism to ensure successful clinical outcomes. This restoration, combined with the use of biological therapies and rehabilitation, will produce the maximum benefit for the patient.
Management of Acetabular Labrum
The final decision regarding how to surgically approach the acetabular labrum is made during the operation. We focus restoring the labrum seal mechanism, which is crucial for proper function and health of the hip joint.1 The intra-articular hydrostatic pressure loss caused by labral deficiency results in abnormal load distribution and joint microinstability, which have detrimental effects on cartilage and periarticular tissues. A biomechanical study highlighted the role of the hip labrum in maintaining intra-articular fluid pressurization and showed that labral reconstruction restores intra-articular fluid pressure to levels similar to those of the intact state.1
In cases in which the remaining labral tissue is adequate and of good quality (reparable), the labral repair technique is preferred.2 After diagnostic arthroscopy, the labral tear is identified, and a 4.5-mm burr is used to correct (rim-trim) any osseous deformity of the acetabulum to create a “new rim” for labrum reattachment. Suture anchors are placed on the rim about 2 mm to 3 mm below the cartilage surface. Considering the rim angle3 is helpful in avoiding acetabular cartilage damage. Labral sutures can be looped around or pierced through the labrum to secure it to the acetabulum. No difference in clinical outcomes was found between the 2 suture types,4 though biomechanically piercing sutures help restore the labrum seal better.1 When the labrum is deficient and longitudinal fibers remain but are insufficient for seal restoration, the repair can be augmented with adjacent iliotibial band (ITB) tissue. This technique is similar to labral reconstruction but involves placing a graft on top of the remaining labral tissue, and suture around both the native tissue and the graft. The additional tissue gives the labrum the volume it needs to recreate the seal.
The labral reconstruction technique is indicated when the remaining labrum is irreparable, absent, or severely hypotrophic or deficient, or when an irreparable complex tear or poor-quality tissue is present. Different types of grafts can be used to reconstruct the labrum. ITB, semitendinosus, gracilis, and anterior tibialis grafts and the human acetabular labrum exhibit similar cyclic elongation behavior in response to simulated physiologic forces, though there is variability in both elongation and geometry for all graft types.5 We prefer the ITB autograft technique.6 The graft should be about 30% to 40% longer than the labral defect as measured with arthroscopic probe. With the leg in traction, the graft is inserted through the mid-anterior portal, and a suture anchor is used to secure it against the acetabulum medially.
With proper patient selection, these techniques have excellent clinical outcomes.4,7 Severe osteoarthritis (joint space <2 mm) is a contraindication for these procedures.8
Osseous Deformity
On approaching the bony structures of the hip joint, the surgeon should examine the acetabular rim (pincer lesion), the femoral head and neck shape (cam lesion), and the anterior inferior iliac spine (AIIS). Preoperative imaging and physical examination are important for identifying severe bone deformities that can complicate the procedure.9
The acetabular rim can be directly viewed after labrum detachment, but usually complete detachment is not necessary. Pincer deformity causes focal or global overcoverage of the femoral head. Rim trimming is performed with a 4.5-mm round curved burr. Resection is usually performed to the end of rim chondrosis (about 3-5 mm). Using a simple formula, you can calculate how the lateral center edge will be reduced by the amount of rim resected, maintaining a safe margin.2 A new acetabular “bed” is created where the to-be-attached labral tissue will contribute to the suction seal mechanism of the joint.2Cam lesion correction is challenging, and the amount of bone that should be resected is a matter of disagreement. We perform cam osteochondroplasty2 with a 5.5-mm round burr inserted through the anterolateral portal while the hip is positioned in 45° of flexion, neutral rotation, and adduction/abduction. This position allows an osteoplasty from 6 to 10 o’clock on the head–neck junction. Osteoplasty performed between 10 and 12 o’clock requires hip extension and slight traction. The proximal limit of osteochondroplasty is about 15 mm from the labral edge, while distally the resection stops beneath the zona orbicularis. The lateral epiphyseal vessels and the Weitbrecht ligament constitute the lateral and medial borders, respectively.
The surgeon should create a smooth head–neck offset that prevents elevation of the labrum during flexion and achieves a nearly perfect anatomical relationship between the femoral head and the acetabular labrum, restoring the hip joint seal (Figure 2).
A hypertrophic AIIS can impinge the femur (extra-articular subspinal impingement). Patients present with limited range of motion (especially hip flexion), pain in the AIIS area, and, in some cases, a history of avulsion injury.11 Seeing a bruised labrum (Figure 3) during surgery is common with this pathology.
Treatment of Cartilage Lesions
The indications and contraindications for hip arthroscopy in patients with cartilage lesions are important. Our study’s 5-year outcomes of treating FAI with hip arthroscopy in patients with preserved joint space (>2 mm) were promising, though 86% of patients with limited joint space (≤2 mm) converted to total hip arthroplasty.8 We regard patients with severe osteoarthritis as not being candidates for hip arthroscopy.
As 3 Tesla magnetic resonance imaging has low positive predictive value in identifying severe cartilage damage,13 the cartilage should be examined during surgery to further define the diagnosis. Nearly half of the hip arthroscopy patients in our study had at least 1 Outerbridge grade 3 or 4 cartilage lesion.14 Compared with the femoral head, acetabular cartilage was damaged 3 times more often. More than 90% of acetabular cartilage lesions were in the anterosuperior region.
Grades 0 and 1 cartilage lesions are usually left untreated; no intervention is necessary. Grades 2 and 3 cartilage lesions are reduced by partial débridement and/or thermal shrinkage. With the improved joint microenvironment arising from simple correction of the underlying hip bony abnormalities, these lesions should not produce further symptoms.
Grade 4 hip cartilage defects are challenging. We prefer microfracture for grade 4 lesions (Figure 4).
A ring curette is used to prepare the defect, and perpendicular borders are created to hold the clot in place. Deep débridement removes the calcified layer while maintaining the integrity of the subchondral plate.15 As a recent study found microfracture performed with small-diameter awls improved cartilage repair more effectively than microfracture with large-diameter awls,16 we prefer making small-diameter holes when establishing the maximum number of holes possible. As it is important to make a perpendicular hole, not a scratch, we use an XL Microfracture Pick (Smith & Nephew) 90° curve, which is suitable for creating a vertical entry point. The 60° curved awl is then used to further deepen the hole. Creation and stability of the marrow clot are ensured by shutting down the infusion pump device and verifying that blood and marrow elements are released from the microfractures.
Capsule Management
The increase in hip arthroscopies performed worldwide has generated interest in proper capsular management and development of iatrogenic microinstability.17 Hip capsulotomy is routinely performed for adequate visualization of the intra-articular compartment. Standard anterosuperior interportal capsulotomy for hip arthroscopic surgery (12 to 3 o’clock) sacrifices the integrity of the iliofemoral ligament (ligament of Bigelow),18 which provides rotational stability. Failure to restore the anatomical and biomechanical properties of the iliofemoral ligament after arthroscopic surgery increases the likelihood of postoperative microinstability or gross instability,19 which can lead to persistent pain and/or sense of an unstable joint, in addition to accelerated cartilage wear.
Capsulotomies are useful in obtaining adequate intraoperative exposure of the central and peripheral compartments. In the past, little attention was given to capsular closure on completion of the procedure. However, concern about postoperative instability from capsular laxity or deficiency made the introduction of capsular repair techniques necessary. Although deciding between capsular closure and plication remains debatable, we routinely perform capsular closure with a Quebec City slider knot.20 Mindful management of the capsule throughout the procedure is important in avoiding irreversible capsular damage, which would complicate capsular closure. Mindful management involves leaving a proximal leaflet of at least 1 cm during the capsulotomy, avoiding capsular thinning during shaver use, and using a cannula to prevent soft-tissue bridging.
Recent evidence suggests that capsule repair restores near native hip joint stability.17 In addition to capsular shift or capsulorrhaphy, 2 to 6 sutures have been used for capsular closure or plication after an interportal or T capsulotomy. Chahla and colleagues21 reported that 2- and 3-suture constructs produced comparable biomechanical failure torques when external rotation forces were applied to conventional hip capsulotomy on cadavers. Three-suture constructs were significantly stronger than 1-suture constructs, but there was no significant difference between 2- and 3-suture constructs. All constructs failed at about 36° of external rotation. Therefore, restricted external rotation is recommended for 3 weeks after surgery.
In one study, 35% of revision hip arthroscopy patients had undiagnosed hip instability from iatrogenic injury,22 which can lead to labral and chondral injury.17 Capsular reconstruction is recommended in cases of symptomatic capsular deficiency; capsular deficiency caused by adhesion removal; and pain and range-of-motion limitation caused by capsular adhesions. However, indications need to be further established. We have performed capsular reconstruction with ITB allograft23 (Figure 5).
Biologics
At the end of the procedure, we use platelet-rich plasma and/or bone marrow aspirate injections (individualized to the patient) to potentiate the biological healing of the tissues. Further research is planned to determine how to prepare these biological products to provide the best mix of biological factors for improved healing. Antifibrotic factors are useful in preventing adhesions, and angiotensin II receptor blockers are effective, but clinical studies are needed to establish their use.
Rehabilitation
Immediately after surgery, a postoperative hip brace and antirotational boots are applied to the patient to protect the operative site and reduce pain. The actual postoperative protocol is based on the procedure and individualized to the patient. During microfractures, the patient is kept 20 pounds touch-toe weight-bearing for 4 to 8 weeks. The capsular closure is brace-protected by limiting abduction to 0° to 45° and hip flexion to 0° to 90° while external rotation and extension are prohibited (first 3 weeks). Immediate mobilization with passive rotational movement is crucial in preventing adhesions. Stationary bike exercise and use of a continuous passive motion machine are helpful. Progressive functional and sport-specific rehabilitation help the patient return to full activity, though the decision to return to full activity is based on several factors, both objective (functional tests) and subjective (physician–patient co-decisions).
Conclusion
Although hip arthroscopic techniques have expanded significantly in recent years, our treatment approach is based on restoring the normal anatomy of the hip joint—combining the procedures with biological therapies and a postoperative rehabilitation program that is individualized to the patient’s special needs.
Am J Orthop. 2017;46(1):23-27. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Philippon MJ, Nepple JJ, Campbell KJ, et al. The hip fluid seal—part I: the effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):722-729.
2. Philippon MJ, Faucet SC, Briggs KK. Arthroscopic hip labral repair. Arthrosc Tech. 2013;2(2):e73-e76.
3. Lertwanich P, Ejnisman L, Torry MR, Giphart JE, Philippon MJ. Defining a safety margin for labral suture anchor insertion using the acetabular rim angle. Am J Sports Med. 2011;39(suppl):111S-116S.
4. Sawyer GA, Briggs KK, Dornan GJ, Ommen ND, Philippon MJ. Clinical outcomes after arthroscopic hip labral repair using looped versus pierced suture techniques. Am J Sports Med. 2015;43(7):1683-1688.
5. Ferro FP, Philippon MJ, Rasmussen MT, Smith SD, LaPrade RF, Wijdicks CA. Tensile properties of the human acetabular labrum and hip labral reconstruction grafts. Am J Sports Med. 2015;43(5):1222-1227.
6. Philippon MJ, Briggs KK, Boykin RE. Results of arthroscopic labral reconstruction of the hip in elite athletes: response. Am J Sports Med. 2014;42(10):NP48.
7. Geyer MR, Philippon MJ, Fagrelius TS, Briggs KK. Acetabular labral reconstruction with an iliotibial band autograft: outcome and survivorship analysis at minimum 3-year follow-up. Am J Sports Med. 2013;41(8):1750-1756.
8. Skendzel JG, Philippon MJ, Briggs KK, Goljan P. The effect of joint space on midterm outcomes after arthroscopic hip surgery for femoroacetabular impingement. Am J Sports Med. 2014;42(5):1127-1133.
9. Yeung M, Kowalczuk M, Simunovic N, Ayeni OR. Hip arthroscopy in the setting of hip dysplasia: a systematic review. Bone Joint Res. 2016;5(6):225-231.
10. Locks R, Chahla J, Mitchell JJ, Soares E, Philippon MJ. Dynamic hip examination for assesment of impingement during hip arthroscopy. Arthroscopy Tech. 2016 Nov 28. http://dx.doi.org/10.1016/j.eats.2016.08.011
11. Nabhan DC, Moreau WJ, McNamara SC, Briggs KK, Philippon MJ. Subspine hip impingement: an unusual cause of hip pain in an elite weightlifter. Curr Sports Med Rep. 2016;15(5):315-319.
12. Philippon MJ, Michalski MP, Campbell KJ, et al. An anatomical study of the acetabulum with clinical applications to hip arthroscopy. J Bone Joint Surg Am. 2014;96(20):1673-1682.
13. Ho CP, Ommen ND, Bhatia S, et al. Predictive value of 3-T magnetic resonance imaging in diagnosing grade 3 and 4 chondral lesions in the hip. Arthroscopy. 2016;32(9):1808-1813.
14. Bhatia S, Nowak DD, Briggs KK, Patterson DC, Philippon MJ. Outerbridge grade IV cartilage lesions in the hip identified at arthroscopy. Arthroscopy. 2016;32(5):814-819.
15. Frisbie DD, Morisset S, Ho CP, Rodkey WG, Steadman JR, McIlwraith CW. Effects of calcified cartilage on healing of chondral defects treated with microfracture in horses. Am J Sports Med. 2006;34(11):1824-1831.
16. Orth P, Duffner J, Zurakowski D, Cucchiarini M, Madry H. Small-diameter awls improve articular cartilage repair after microfracture treatment in a translational animal model. Am J Sports Med. 2016;44(1):209-219.
17. Domb BG, Philippon MJ, Giordano BD. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: relation to atraumatic instability. Arthroscopy. 2013;29(1):162-173.
18. Asopa V, Singh PJ. The intracapsular atraumatic arthroscopic technique for closure of the hip capsule. Arthrosc Tech. 2014;3(2):e245-e247.
19. Frank RM, Lee S, Bush-Joseph CA, Kelly BT, Salata MJ, Nho SJ. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42(11):2634-2642.
20. Menge TJ, Chahla J, Soares E, Mitchell JJ, Philippon MJ. The Quebec City slider: a technique for capsular closure and plication in hip arthroscopy. Arthrosc Tech. 2016;5(5):e971-e974.
21. Chahla J, Mikula JD, Schon JM, et al. Hip capsular closure: a biomechanical analysis of failure torque. Am J Sports Med. doi:10.1177/0363546516666353.
22. Philippon MJ, Schenker ML, Briggs KK, Kuppersmith DA, Maxwell RB, Stubbs AJ. Revision hip arthroscopy. Am J Sports Med. 2007;35(11):1918-1921.
23. Trindade CA, Sawyer GA, Fukui K, Briggs KK, Philippon MJ. Arthroscopic capsule reconstruction in the hip using iliotibial band allograft. Arthrosc Tech. 2015;4(1):e71-e74.
1. Philippon MJ, Nepple JJ, Campbell KJ, et al. The hip fluid seal—part I: the effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):722-729.
2. Philippon MJ, Faucet SC, Briggs KK. Arthroscopic hip labral repair. Arthrosc Tech. 2013;2(2):e73-e76.
3. Lertwanich P, Ejnisman L, Torry MR, Giphart JE, Philippon MJ. Defining a safety margin for labral suture anchor insertion using the acetabular rim angle. Am J Sports Med. 2011;39(suppl):111S-116S.
4. Sawyer GA, Briggs KK, Dornan GJ, Ommen ND, Philippon MJ. Clinical outcomes after arthroscopic hip labral repair using looped versus pierced suture techniques. Am J Sports Med. 2015;43(7):1683-1688.
5. Ferro FP, Philippon MJ, Rasmussen MT, Smith SD, LaPrade RF, Wijdicks CA. Tensile properties of the human acetabular labrum and hip labral reconstruction grafts. Am J Sports Med. 2015;43(5):1222-1227.
6. Philippon MJ, Briggs KK, Boykin RE. Results of arthroscopic labral reconstruction of the hip in elite athletes: response. Am J Sports Med. 2014;42(10):NP48.
7. Geyer MR, Philippon MJ, Fagrelius TS, Briggs KK. Acetabular labral reconstruction with an iliotibial band autograft: outcome and survivorship analysis at minimum 3-year follow-up. Am J Sports Med. 2013;41(8):1750-1756.
8. Skendzel JG, Philippon MJ, Briggs KK, Goljan P. The effect of joint space on midterm outcomes after arthroscopic hip surgery for femoroacetabular impingement. Am J Sports Med. 2014;42(5):1127-1133.
9. Yeung M, Kowalczuk M, Simunovic N, Ayeni OR. Hip arthroscopy in the setting of hip dysplasia: a systematic review. Bone Joint Res. 2016;5(6):225-231.
10. Locks R, Chahla J, Mitchell JJ, Soares E, Philippon MJ. Dynamic hip examination for assesment of impingement during hip arthroscopy. Arthroscopy Tech. 2016 Nov 28. http://dx.doi.org/10.1016/j.eats.2016.08.011
11. Nabhan DC, Moreau WJ, McNamara SC, Briggs KK, Philippon MJ. Subspine hip impingement: an unusual cause of hip pain in an elite weightlifter. Curr Sports Med Rep. 2016;15(5):315-319.
12. Philippon MJ, Michalski MP, Campbell KJ, et al. An anatomical study of the acetabulum with clinical applications to hip arthroscopy. J Bone Joint Surg Am. 2014;96(20):1673-1682.
13. Ho CP, Ommen ND, Bhatia S, et al. Predictive value of 3-T magnetic resonance imaging in diagnosing grade 3 and 4 chondral lesions in the hip. Arthroscopy. 2016;32(9):1808-1813.
14. Bhatia S, Nowak DD, Briggs KK, Patterson DC, Philippon MJ. Outerbridge grade IV cartilage lesions in the hip identified at arthroscopy. Arthroscopy. 2016;32(5):814-819.
15. Frisbie DD, Morisset S, Ho CP, Rodkey WG, Steadman JR, McIlwraith CW. Effects of calcified cartilage on healing of chondral defects treated with microfracture in horses. Am J Sports Med. 2006;34(11):1824-1831.
16. Orth P, Duffner J, Zurakowski D, Cucchiarini M, Madry H. Small-diameter awls improve articular cartilage repair after microfracture treatment in a translational animal model. Am J Sports Med. 2016;44(1):209-219.
17. Domb BG, Philippon MJ, Giordano BD. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: relation to atraumatic instability. Arthroscopy. 2013;29(1):162-173.
18. Asopa V, Singh PJ. The intracapsular atraumatic arthroscopic technique for closure of the hip capsule. Arthrosc Tech. 2014;3(2):e245-e247.
19. Frank RM, Lee S, Bush-Joseph CA, Kelly BT, Salata MJ, Nho SJ. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42(11):2634-2642.
20. Menge TJ, Chahla J, Soares E, Mitchell JJ, Philippon MJ. The Quebec City slider: a technique for capsular closure and plication in hip arthroscopy. Arthrosc Tech. 2016;5(5):e971-e974.
21. Chahla J, Mikula JD, Schon JM, et al. Hip capsular closure: a biomechanical analysis of failure torque. Am J Sports Med. doi:10.1177/0363546516666353.
22. Philippon MJ, Schenker ML, Briggs KK, Kuppersmith DA, Maxwell RB, Stubbs AJ. Revision hip arthroscopy. Am J Sports Med. 2007;35(11):1918-1921.
23. Trindade CA, Sawyer GA, Fukui K, Briggs KK, Philippon MJ. Arthroscopic capsule reconstruction in the hip using iliotibial band allograft. Arthrosc Tech. 2015;4(1):e71-e74.
Current Concepts in Labral Repair and Refixation: Anatomical Approach to Labral Management
Take-Home Points
- Labral preservation is recommended when possible to ensure restoration of suction seal, stability, and contact pressure of the hip joint.
- Over 95% of labral tears can be addressed with primary repair.
- Consider using an accessory portal (ie, DALA) to allow for more anatomic placement of suture anchor.
- Mattress stitch when labrum >3 mm and looped stitch when labrum <3 mm.
- 10Control labral repair to avoid excessive inversion or eversion.
Arthroscopic labral repair and refixation have garnered much attention over the past several years. Restoration of suction seal and native labral function has been an evolving focus for achieving excellent results in hip preservation surgery.1-6 Given the superior results of labral repair, including level I evidence, repair or refixation should be pursued whenever possible.7 Authors have reported using several labral management techniques: débridement, labralization, looped suture fixation, base stitch fixation, inversion-eversion, and reconstruction.7-13 The optimal technique is yet to be determined. When possible, steps should be taken to repair the labrum to an anatomical position. Absolute indications for labral repair are a confirmed intra-articular diagnosis with symptomatic pain, joint space >2 mm with or without femoroacetabular impingement (FAI), labral tear or instability, and failed conservative management.9,11,12,14,15 More important, the surgeon must have a clear etiology of the pathologic cause of the tear and be aware of the limitations of the procedure. Labral repair is relatively contraindicated in end-stage arthritis and has failed when used alone in undiagnosed dysplasia or hip instability.16 In this article, we discuss indications for labral repair; describe Dr. Mather’s preoperative planning, labral repair technique, and postoperative care; and review published outcomes and future trends in labral repair.
Indications
At our institution, anatomical labral repair is the preferred procedure for most primary and revision hip arthroscopy procedures. We aim to restore the suction seal, re-create the contact of the labrum and the femoral head to facilitate proprioception, and restore normal stability of the labrum. Indications for primary repair are labrum width >3 mm, no more than 2 repairs, and ability to hold a suture. Our indications for reconstruction or débridement are stage 3 irreparable labral tear, calcified/cystic labrum, and multiple failed labral repairs or reconstructions. The decision to perform labral débridement or reconstruction is made on a case-by-case basis but is primarily influenced by the stability of the hip joint and the activity goals of the patient. If preoperative presentation and intraoperative examination suggest labral instability as a major component of the pathology, or if the patient wants to return to high-demand activity, we more strongly favor reconstruction over débridement. In our experience, with the technique described in this article, more than 95% of all primary labral tears can be addressed with repair.
Preoperative Planning
The goals in hip preservation surgery are to identify and address the underlying cause of the labral tear, whether it be FAI syndrome, trauma, labral instability, or all 3, and to re-create the anatomy and biomechanics of the acetabular labrum. For repair, we prefer an inversion-eversion technique with independent control of the labrum. Our initial work-up includes a thorough history and physical examination with baseline patient-reported outcome scores. Standard erect anteroposterior pelvis, Dunn lateral, and false-profile radiographs are obtained. Standard measurements of lateral center edge angle, anterior center edge angle, Tönnis angle, Tönnis grade, lateral joint space, and head extrusion indices are evaluated. Selective in-office ultrasound-guided injections are used to confirm an intra-articular source of pain. At our institution, noncontrast 3.0 Tesla magnetic resonance imaging (MRI) with volumetric interpolated breath-hold examination (VIBE) sequencing and 3-dimensional rendering is obtained for evaluation of labral and FAI morphology.17 All advanced imaging is performed without arthrogram or radiation exposure (Figures 1A-1C).
With use of the radiographs and the MRI scans, we engage the patient in an informed discussion about the labral tear, FAI, and concomitant pathology. We discuss expected outcomes of conservative or operative management given the patient’s expected functional activities, and inform the patient that primary repair is indicated for many others in similar situations. The potential for possible labral reconstruction is discussed if the patient had prior intra-articular hip surgery, has a large calcified labrum or a cystic labrum, is an athlete with failed prior surgery, or is younger than 40 years.
Labral Repair Technique
The patient is taken to the surgical suite, and a general anesthetic is administered. A peripheral nerve block is not routinely used. The patient’s feet are padded, and boots for the traction table are applied. The patient is carefully placed on a Hana table in modified supine position. Balanced traction is used to achieve proper joint distraction. The C-arm is used to verify proper distraction, assess hip stability, and achieve standard anterolateral (AL) portal placement. A midanterior portal (MAP) is created and an interportal capsulotomy is performed. Capsular suspension is performed with the InJector II Capsule Restoration System (Stryker Sports Medicine) and typically 4 or 5 high-strength No. 2 sutures (Zipline; Stryker Sports Medicine).19 Diagnostic arthroscopy is performed to identify the tear type, measure the labral width, determine the impingement area, and identify the intra-articular pathology. After the intra-articular pathology is addressed, a radiofrequency Ambient HIPVAC 50 Coblation Wand (Smith & Nephew) is used to expose the acetabular rim and subspine as indicated. Acetabuloplasty or subspine decompression is performed, and then a primary repair or refixation of the labrum is performed. We do not routinely detach the labrum for acetabular rim trimming. A crucial step here is to expose a bleeding surface to which the labrum can be repaired. If the rim is sclerotic, or the rim cannot be removed because of underlying low acetabular coverage, we prefer to obtain the bleeding surface with a microdrilling device (Stryker) that is routinely used for acetabular microfracture.
Labrum quality is used to determine which repair method to use. A hypertrophic labrum is debulked. The acetabular rim is seldom resected >3 mm, but, when it is, the newly exposed cartilage is removed. We have found that >3 mm of residual cartilage prevents refixation of the labrum directly to the bone and may interfere with anatomical positioning. When a labrum is <3 mm in width or will not hold a base technique, repair stability is the priority, and a looped method is used. A knotless anchor with No. 1 permanent suture designed for hip labral repair (CinchLock; Stryker) is our first-line anchor choice. A distal anterolateral accessory (DALA) portal is created with an outside-in technique, and anchors are drilled through this portal into zones 2 to 4 (Figures 2A-2E).
A 2.4-mm drill guide is advanced through the DALA portal and placed in the appropriate position for drilling. We aim for 1 mm to 2 mm from the chondrolabral junction. Next, the probe is placed intra-articular and medial to the anchor insertion site, and the anchor is loaded and then inserted around the probe (Figures 3A-3E).
The hip is then reduced. If indicated, a T-capsulotomy is performed for femoral osteochondroplasty.
Postoperative Care
Patients are placed in a postoperative hip brace and use a continuous passive motion machine 6 hours a day for 2 weeks, and an ice machine. They maintain 30 lb of foot-flat weight-bearing for 3 weeks, and begin a standard labral repair protocol on postoperative days 3 to 7.
Discussion
Hip labral preservation has evolved over the past 10 years, and current options for labral management include excision, débridement, labralization, repair, and reconstruction.1-13 Labral excision was studied by Miozzari and colleagues,8 who postulated on the basis of animal models that the labrum may regenerate. In their series of 9 patients treated with surgical hip dislocation and labral excision at average 4-year follow-up, repeat magnetic resonance angiography revealed no regeneration of tissue—modified Harris Hip Score was 83. The hip scores were less than those of patients treated with the same procedure with repair, and the authors concluded that defining labral débridement versus excision in the literature, and treating patients with primary repair or reconstruction techniques, may lead to better results. Their study used a small sample and was limited to an open procedure. Arthroscopic labral débridement in isolation was also a poor option for treatment of a labral tear. In a 2-year follow-up of 59 isolated labral débridement procedures, Krych and colleagues9 found 47% combined poor results.
There is level I evidence of the importance of labral repair. In 2013, Krych and colleagues7 conducted a randomized control trial of 38 female patients who underwent hip arthroscopy for FAI. At time of surgery, patients were randomly assigned to either débridement or repair. At 1-year follow-up, activities of daily living and Sports specific Hip Outcome Scores were statistically significantly superior in the repair group. On a subjective scale, 94% vs 78% of patients reported normal or near normal hips in the repair versus débridement groups respectively. Ayeni and colleagues20 performed a systematic review of 6 studies in an attempt to develop labral management recommendations. Five of the studies (N = 490 patients total) had improved results with labral repair over reconstruction. Although the studies had a low level of evidence, they found a trend toward improved results with labral repair. These studies highlight the importance of labral preservation and proper FAI management.
Techniques for labrum repair have advanced as well—from a looped suture technique to a base stitch and knotless independent tensioning.11-13 Restoration of the hip labrum function as a suction seal, fluid circulator and anatomic capsular repair is paramount to excellent results and stresses the importance of performing an anatomic labral repair.1-6 Knotless anchor repair is not novel and has been previously described. Fry and Domb12 reported on a knotless labral repair technique that uses push-lock devices (Arthrex) that do not allow for independent tensioning. Inversion-eversion was introduced to the literature by Moreira and colleagues,13 who described an independent tensioning technique that uses speed-lock anchors (Smith & Nephew). Our technique differs in that it involves a DALA portal; labral reduction and tensioning with a probe assist to ensure the second pass of the base stitch is at the apex of the labrum; and use of No. 1 instead of No. 2 suture. Although seemingly subtle, these differences allow for proper anchor placement nearer the rim, additional support in achieving precise suture placement, and less disruption of small labra. These differences are particularly relevant for smaller labra.
Evaluating repair techniques on the basis of high-evidence literature is challenging. In a matched-cohort study of 220 patients, Jackson and colleagues21 compared 2 techniques: looped and base stitch. At 2-year follow-up, patients in both groups showed improvement, and there was no statistically significant difference in patient-reported outcome measures between the groups. Sawyer and colleagues22 studied the outcomes of 326 consecutive patients who underwent looped, pierced, or combined labral repair at an average 32-month follow-up. The groups’ revision rates were comparable, each group improved in postoperative patient-reported outcomes, and the pierced group had significantly higher preoperative scores on the Western Ontario and McMaster Universities Osteoarthritis Index. These studies described a base or pierce repair that did not differ from a looped repair, though the techniques did not allow for independent tensioning to re-create an anatomical inversion-eversion repair and may have altered the reported outcomes.
Our current technique uses independent tensioning of the repair to allow control of labrum inversion-eversion to give an anatomical repair with restoration of the suction seal. Preoperative planning, addressing the FAI appropriately, proper suture-passing technique, controlling the labrum in inversion-eversion fashion, and anatomical labral repair are the elements of Dr. Mather’s preferred method for preserving the native labrum and allowing it to assume its native function.
Future Directions
As our understanding of FAI and labral function evolves, labral preservation surgery continues to advance. With surgeons continually developing new techniques and following up on previous techniques, the ability to preserve the native hip with lasting procedures evolves as well. Proper identification of the underlying cause of the labral tear and proper anatomical repair are paramount to the success of FAI surgery.
Am J Orthop. 2017;46(1):42-48. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Philippon MJ, Nepple JJ, Campbell KJ, et al. The hip fluid seal—part I: the effect of an acetabular labral tear, repair, resection and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):722-729.
2. Nepple JJ, Philippon MJ, Campbell KJ, et al. The hip fluid seal—part II: the effect of an acetabular labral tear, repair, resection and reconstruction on hip stability to distraction. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):730-736.
3. Dwyer MK, Jones HL, Hogan MG, Field RE, McCarthy JC, Noble PC. The acetabular labrum regulates fluid circulation of the hip joint during functional activities. Am J Sports Med. 2014;42(4):812-819.
4. Greaves LL, Gilbart MK, Yung AC, Kozlowski, Wilson DR. Effect of acetabular labral tears, repair and resection on hip cartilage strain: a 7T MR study. J Biomech. 2010;43(5):858-863.
5. Freehill MT, Safran MR. The labrum of the hip: diagnosis and rationale for surgical correction. Clin Sports Med. 2011;30(2):293-315.
6. Myers CA, Register BC, Lertwanich P, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39(suppl):85S-91S.
7. Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy. 2013;29(1):46-53.
8. Miozzari HH, Celia M, Clark JM, Werlen S, Naal FD, Nötzli HP. No regeneration of the human acetabular labrum after excision to bone. Clin Orthop Relat Res. 2015;473(4):1349-1357.
9. Krych AJ, Kuzma SA, Kovachevich R, Hudgens JL, Stuart MJ, Levy BA. Modest mid-term outcomes after isolated arthroscopic debridement of acetabular labral tears. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):763-767.
10. Matsuda DK. Arthroscopic labralization of the hip: an alternative to labral reconstruction. Arthrosc Tech. 2014;3(1):e131-e133.
11. Philippon MJ, Faucet SC, Briggs KK. Arthroscopic hip labral repair. Arthrosc Tech. 2013;2(2):e73-e76.
12. Fry D, Domb B. Labral base refixation in the hip: rationale and technique for an anatomic approach to labral repair. Arthroscopy. 2010;26(9 suppl):S81-S89.
13. Moreira B, Pascual-Garrido C, Chadayamurri V, Mei-Dan O. Eversion-inversion labral repair and reconstruction technique for optimal suction seal. Arthrosc Tech. 2015;4(6):e697-e700.
14. Mook WR, Briggs KK, Philippon MJ. Evidence and approach for management of labral deficiency: the role for labral reconstruction. Sports Med Arthrosc. 2015;23(4):205-212.
15. Gupta A, Suarez-Ahedo C, Redmond JM, et al. Best practices during hip arthroscopy: aggregate recommendations of high-volume surgeons. Arthroscopy. 2015;31(9):1722-1727.
16. Yeung M, Kowalczuk M, Simunovic N, Ayeni OR. Hip arthroscopy in the setting of hip dysplasia: a systematic review. Bone Joint Res. 2016;5(6):225-231.
17. Hash TW. Magnetic resonance imaging of the hip. In: Nho SJ, Leunig M, Larson CM, Bedi A, Kelly BT, eds. Hip Arthroscopy and Hip Joint Preservation Surgery, Vol. 1. New York, NY: Springer; 2015:65-113.
18. Sutter R, Zubler V, Hoffmann A, et al. Hip MRI: how useful is intraarticular contrast material for evaluating surgically proven lesions of the labrum and articular cartilage? AJR Am J Roentgenol. 2014;202(1):160-169.
19. Federer AE, Karas V, Nho S, Coleman SH, Mather RC 3rd. Capsular suspension technique for hip arthroscopy. Arthrosc Tech. 2015;4(4):e317-e322.
20. Ayeni OR, Adamich J, Farrokhyar F, et al. Surgical management of labral tears during femoroacetabular impingement surgery: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):756-762.
21. Jackson TJ, Hammarstedt JE, Vemula SP, Domb BG. Acetabular labral base repair versus circumferential suture repair: a matched-paired comparison of clinical outcomes. Arthroscopy. 2015;31(9):1716-1721.
22. Sawyer GA, Briggs KK, Dornan GJ, Ommen ND, Philippon MJ. Clinical outcomes after arthroscopic hip labral repair using looped versus pierced suture techniques. Am J Sports Med. 2015;43(7):1683-1688.
Take-Home Points
- Labral preservation is recommended when possible to ensure restoration of suction seal, stability, and contact pressure of the hip joint.
- Over 95% of labral tears can be addressed with primary repair.
- Consider using an accessory portal (ie, DALA) to allow for more anatomic placement of suture anchor.
- Mattress stitch when labrum >3 mm and looped stitch when labrum <3 mm.
- 10Control labral repair to avoid excessive inversion or eversion.
Arthroscopic labral repair and refixation have garnered much attention over the past several years. Restoration of suction seal and native labral function has been an evolving focus for achieving excellent results in hip preservation surgery.1-6 Given the superior results of labral repair, including level I evidence, repair or refixation should be pursued whenever possible.7 Authors have reported using several labral management techniques: débridement, labralization, looped suture fixation, base stitch fixation, inversion-eversion, and reconstruction.7-13 The optimal technique is yet to be determined. When possible, steps should be taken to repair the labrum to an anatomical position. Absolute indications for labral repair are a confirmed intra-articular diagnosis with symptomatic pain, joint space >2 mm with or without femoroacetabular impingement (FAI), labral tear or instability, and failed conservative management.9,11,12,14,15 More important, the surgeon must have a clear etiology of the pathologic cause of the tear and be aware of the limitations of the procedure. Labral repair is relatively contraindicated in end-stage arthritis and has failed when used alone in undiagnosed dysplasia or hip instability.16 In this article, we discuss indications for labral repair; describe Dr. Mather’s preoperative planning, labral repair technique, and postoperative care; and review published outcomes and future trends in labral repair.
Indications
At our institution, anatomical labral repair is the preferred procedure for most primary and revision hip arthroscopy procedures. We aim to restore the suction seal, re-create the contact of the labrum and the femoral head to facilitate proprioception, and restore normal stability of the labrum. Indications for primary repair are labrum width >3 mm, no more than 2 repairs, and ability to hold a suture. Our indications for reconstruction or débridement are stage 3 irreparable labral tear, calcified/cystic labrum, and multiple failed labral repairs or reconstructions. The decision to perform labral débridement or reconstruction is made on a case-by-case basis but is primarily influenced by the stability of the hip joint and the activity goals of the patient. If preoperative presentation and intraoperative examination suggest labral instability as a major component of the pathology, or if the patient wants to return to high-demand activity, we more strongly favor reconstruction over débridement. In our experience, with the technique described in this article, more than 95% of all primary labral tears can be addressed with repair.
Preoperative Planning
The goals in hip preservation surgery are to identify and address the underlying cause of the labral tear, whether it be FAI syndrome, trauma, labral instability, or all 3, and to re-create the anatomy and biomechanics of the acetabular labrum. For repair, we prefer an inversion-eversion technique with independent control of the labrum. Our initial work-up includes a thorough history and physical examination with baseline patient-reported outcome scores. Standard erect anteroposterior pelvis, Dunn lateral, and false-profile radiographs are obtained. Standard measurements of lateral center edge angle, anterior center edge angle, Tönnis angle, Tönnis grade, lateral joint space, and head extrusion indices are evaluated. Selective in-office ultrasound-guided injections are used to confirm an intra-articular source of pain. At our institution, noncontrast 3.0 Tesla magnetic resonance imaging (MRI) with volumetric interpolated breath-hold examination (VIBE) sequencing and 3-dimensional rendering is obtained for evaluation of labral and FAI morphology.17 All advanced imaging is performed without arthrogram or radiation exposure (Figures 1A-1C).
With use of the radiographs and the MRI scans, we engage the patient in an informed discussion about the labral tear, FAI, and concomitant pathology. We discuss expected outcomes of conservative or operative management given the patient’s expected functional activities, and inform the patient that primary repair is indicated for many others in similar situations. The potential for possible labral reconstruction is discussed if the patient had prior intra-articular hip surgery, has a large calcified labrum or a cystic labrum, is an athlete with failed prior surgery, or is younger than 40 years.
Labral Repair Technique
The patient is taken to the surgical suite, and a general anesthetic is administered. A peripheral nerve block is not routinely used. The patient’s feet are padded, and boots for the traction table are applied. The patient is carefully placed on a Hana table in modified supine position. Balanced traction is used to achieve proper joint distraction. The C-arm is used to verify proper distraction, assess hip stability, and achieve standard anterolateral (AL) portal placement. A midanterior portal (MAP) is created and an interportal capsulotomy is performed. Capsular suspension is performed with the InJector II Capsule Restoration System (Stryker Sports Medicine) and typically 4 or 5 high-strength No. 2 sutures (Zipline; Stryker Sports Medicine).19 Diagnostic arthroscopy is performed to identify the tear type, measure the labral width, determine the impingement area, and identify the intra-articular pathology. After the intra-articular pathology is addressed, a radiofrequency Ambient HIPVAC 50 Coblation Wand (Smith & Nephew) is used to expose the acetabular rim and subspine as indicated. Acetabuloplasty or subspine decompression is performed, and then a primary repair or refixation of the labrum is performed. We do not routinely detach the labrum for acetabular rim trimming. A crucial step here is to expose a bleeding surface to which the labrum can be repaired. If the rim is sclerotic, or the rim cannot be removed because of underlying low acetabular coverage, we prefer to obtain the bleeding surface with a microdrilling device (Stryker) that is routinely used for acetabular microfracture.
Labrum quality is used to determine which repair method to use. A hypertrophic labrum is debulked. The acetabular rim is seldom resected >3 mm, but, when it is, the newly exposed cartilage is removed. We have found that >3 mm of residual cartilage prevents refixation of the labrum directly to the bone and may interfere with anatomical positioning. When a labrum is <3 mm in width or will not hold a base technique, repair stability is the priority, and a looped method is used. A knotless anchor with No. 1 permanent suture designed for hip labral repair (CinchLock; Stryker) is our first-line anchor choice. A distal anterolateral accessory (DALA) portal is created with an outside-in technique, and anchors are drilled through this portal into zones 2 to 4 (Figures 2A-2E).
A 2.4-mm drill guide is advanced through the DALA portal and placed in the appropriate position for drilling. We aim for 1 mm to 2 mm from the chondrolabral junction. Next, the probe is placed intra-articular and medial to the anchor insertion site, and the anchor is loaded and then inserted around the probe (Figures 3A-3E).
The hip is then reduced. If indicated, a T-capsulotomy is performed for femoral osteochondroplasty.
Postoperative Care
Patients are placed in a postoperative hip brace and use a continuous passive motion machine 6 hours a day for 2 weeks, and an ice machine. They maintain 30 lb of foot-flat weight-bearing for 3 weeks, and begin a standard labral repair protocol on postoperative days 3 to 7.
Discussion
Hip labral preservation has evolved over the past 10 years, and current options for labral management include excision, débridement, labralization, repair, and reconstruction.1-13 Labral excision was studied by Miozzari and colleagues,8 who postulated on the basis of animal models that the labrum may regenerate. In their series of 9 patients treated with surgical hip dislocation and labral excision at average 4-year follow-up, repeat magnetic resonance angiography revealed no regeneration of tissue—modified Harris Hip Score was 83. The hip scores were less than those of patients treated with the same procedure with repair, and the authors concluded that defining labral débridement versus excision in the literature, and treating patients with primary repair or reconstruction techniques, may lead to better results. Their study used a small sample and was limited to an open procedure. Arthroscopic labral débridement in isolation was also a poor option for treatment of a labral tear. In a 2-year follow-up of 59 isolated labral débridement procedures, Krych and colleagues9 found 47% combined poor results.
There is level I evidence of the importance of labral repair. In 2013, Krych and colleagues7 conducted a randomized control trial of 38 female patients who underwent hip arthroscopy for FAI. At time of surgery, patients were randomly assigned to either débridement or repair. At 1-year follow-up, activities of daily living and Sports specific Hip Outcome Scores were statistically significantly superior in the repair group. On a subjective scale, 94% vs 78% of patients reported normal or near normal hips in the repair versus débridement groups respectively. Ayeni and colleagues20 performed a systematic review of 6 studies in an attempt to develop labral management recommendations. Five of the studies (N = 490 patients total) had improved results with labral repair over reconstruction. Although the studies had a low level of evidence, they found a trend toward improved results with labral repair. These studies highlight the importance of labral preservation and proper FAI management.
Techniques for labrum repair have advanced as well—from a looped suture technique to a base stitch and knotless independent tensioning.11-13 Restoration of the hip labrum function as a suction seal, fluid circulator and anatomic capsular repair is paramount to excellent results and stresses the importance of performing an anatomic labral repair.1-6 Knotless anchor repair is not novel and has been previously described. Fry and Domb12 reported on a knotless labral repair technique that uses push-lock devices (Arthrex) that do not allow for independent tensioning. Inversion-eversion was introduced to the literature by Moreira and colleagues,13 who described an independent tensioning technique that uses speed-lock anchors (Smith & Nephew). Our technique differs in that it involves a DALA portal; labral reduction and tensioning with a probe assist to ensure the second pass of the base stitch is at the apex of the labrum; and use of No. 1 instead of No. 2 suture. Although seemingly subtle, these differences allow for proper anchor placement nearer the rim, additional support in achieving precise suture placement, and less disruption of small labra. These differences are particularly relevant for smaller labra.
Evaluating repair techniques on the basis of high-evidence literature is challenging. In a matched-cohort study of 220 patients, Jackson and colleagues21 compared 2 techniques: looped and base stitch. At 2-year follow-up, patients in both groups showed improvement, and there was no statistically significant difference in patient-reported outcome measures between the groups. Sawyer and colleagues22 studied the outcomes of 326 consecutive patients who underwent looped, pierced, or combined labral repair at an average 32-month follow-up. The groups’ revision rates were comparable, each group improved in postoperative patient-reported outcomes, and the pierced group had significantly higher preoperative scores on the Western Ontario and McMaster Universities Osteoarthritis Index. These studies described a base or pierce repair that did not differ from a looped repair, though the techniques did not allow for independent tensioning to re-create an anatomical inversion-eversion repair and may have altered the reported outcomes.
Our current technique uses independent tensioning of the repair to allow control of labrum inversion-eversion to give an anatomical repair with restoration of the suction seal. Preoperative planning, addressing the FAI appropriately, proper suture-passing technique, controlling the labrum in inversion-eversion fashion, and anatomical labral repair are the elements of Dr. Mather’s preferred method for preserving the native labrum and allowing it to assume its native function.
Future Directions
As our understanding of FAI and labral function evolves, labral preservation surgery continues to advance. With surgeons continually developing new techniques and following up on previous techniques, the ability to preserve the native hip with lasting procedures evolves as well. Proper identification of the underlying cause of the labral tear and proper anatomical repair are paramount to the success of FAI surgery.
Am J Orthop. 2017;46(1):42-48. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
Take-Home Points
- Labral preservation is recommended when possible to ensure restoration of suction seal, stability, and contact pressure of the hip joint.
- Over 95% of labral tears can be addressed with primary repair.
- Consider using an accessory portal (ie, DALA) to allow for more anatomic placement of suture anchor.
- Mattress stitch when labrum >3 mm and looped stitch when labrum <3 mm.
- 10Control labral repair to avoid excessive inversion or eversion.
Arthroscopic labral repair and refixation have garnered much attention over the past several years. Restoration of suction seal and native labral function has been an evolving focus for achieving excellent results in hip preservation surgery.1-6 Given the superior results of labral repair, including level I evidence, repair or refixation should be pursued whenever possible.7 Authors have reported using several labral management techniques: débridement, labralization, looped suture fixation, base stitch fixation, inversion-eversion, and reconstruction.7-13 The optimal technique is yet to be determined. When possible, steps should be taken to repair the labrum to an anatomical position. Absolute indications for labral repair are a confirmed intra-articular diagnosis with symptomatic pain, joint space >2 mm with or without femoroacetabular impingement (FAI), labral tear or instability, and failed conservative management.9,11,12,14,15 More important, the surgeon must have a clear etiology of the pathologic cause of the tear and be aware of the limitations of the procedure. Labral repair is relatively contraindicated in end-stage arthritis and has failed when used alone in undiagnosed dysplasia or hip instability.16 In this article, we discuss indications for labral repair; describe Dr. Mather’s preoperative planning, labral repair technique, and postoperative care; and review published outcomes and future trends in labral repair.
Indications
At our institution, anatomical labral repair is the preferred procedure for most primary and revision hip arthroscopy procedures. We aim to restore the suction seal, re-create the contact of the labrum and the femoral head to facilitate proprioception, and restore normal stability of the labrum. Indications for primary repair are labrum width >3 mm, no more than 2 repairs, and ability to hold a suture. Our indications for reconstruction or débridement are stage 3 irreparable labral tear, calcified/cystic labrum, and multiple failed labral repairs or reconstructions. The decision to perform labral débridement or reconstruction is made on a case-by-case basis but is primarily influenced by the stability of the hip joint and the activity goals of the patient. If preoperative presentation and intraoperative examination suggest labral instability as a major component of the pathology, or if the patient wants to return to high-demand activity, we more strongly favor reconstruction over débridement. In our experience, with the technique described in this article, more than 95% of all primary labral tears can be addressed with repair.
Preoperative Planning
The goals in hip preservation surgery are to identify and address the underlying cause of the labral tear, whether it be FAI syndrome, trauma, labral instability, or all 3, and to re-create the anatomy and biomechanics of the acetabular labrum. For repair, we prefer an inversion-eversion technique with independent control of the labrum. Our initial work-up includes a thorough history and physical examination with baseline patient-reported outcome scores. Standard erect anteroposterior pelvis, Dunn lateral, and false-profile radiographs are obtained. Standard measurements of lateral center edge angle, anterior center edge angle, Tönnis angle, Tönnis grade, lateral joint space, and head extrusion indices are evaluated. Selective in-office ultrasound-guided injections are used to confirm an intra-articular source of pain. At our institution, noncontrast 3.0 Tesla magnetic resonance imaging (MRI) with volumetric interpolated breath-hold examination (VIBE) sequencing and 3-dimensional rendering is obtained for evaluation of labral and FAI morphology.17 All advanced imaging is performed without arthrogram or radiation exposure (Figures 1A-1C).
With use of the radiographs and the MRI scans, we engage the patient in an informed discussion about the labral tear, FAI, and concomitant pathology. We discuss expected outcomes of conservative or operative management given the patient’s expected functional activities, and inform the patient that primary repair is indicated for many others in similar situations. The potential for possible labral reconstruction is discussed if the patient had prior intra-articular hip surgery, has a large calcified labrum or a cystic labrum, is an athlete with failed prior surgery, or is younger than 40 years.
Labral Repair Technique
The patient is taken to the surgical suite, and a general anesthetic is administered. A peripheral nerve block is not routinely used. The patient’s feet are padded, and boots for the traction table are applied. The patient is carefully placed on a Hana table in modified supine position. Balanced traction is used to achieve proper joint distraction. The C-arm is used to verify proper distraction, assess hip stability, and achieve standard anterolateral (AL) portal placement. A midanterior portal (MAP) is created and an interportal capsulotomy is performed. Capsular suspension is performed with the InJector II Capsule Restoration System (Stryker Sports Medicine) and typically 4 or 5 high-strength No. 2 sutures (Zipline; Stryker Sports Medicine).19 Diagnostic arthroscopy is performed to identify the tear type, measure the labral width, determine the impingement area, and identify the intra-articular pathology. After the intra-articular pathology is addressed, a radiofrequency Ambient HIPVAC 50 Coblation Wand (Smith & Nephew) is used to expose the acetabular rim and subspine as indicated. Acetabuloplasty or subspine decompression is performed, and then a primary repair or refixation of the labrum is performed. We do not routinely detach the labrum for acetabular rim trimming. A crucial step here is to expose a bleeding surface to which the labrum can be repaired. If the rim is sclerotic, or the rim cannot be removed because of underlying low acetabular coverage, we prefer to obtain the bleeding surface with a microdrilling device (Stryker) that is routinely used for acetabular microfracture.
Labrum quality is used to determine which repair method to use. A hypertrophic labrum is debulked. The acetabular rim is seldom resected >3 mm, but, when it is, the newly exposed cartilage is removed. We have found that >3 mm of residual cartilage prevents refixation of the labrum directly to the bone and may interfere with anatomical positioning. When a labrum is <3 mm in width or will not hold a base technique, repair stability is the priority, and a looped method is used. A knotless anchor with No. 1 permanent suture designed for hip labral repair (CinchLock; Stryker) is our first-line anchor choice. A distal anterolateral accessory (DALA) portal is created with an outside-in technique, and anchors are drilled through this portal into zones 2 to 4 (Figures 2A-2E).
A 2.4-mm drill guide is advanced through the DALA portal and placed in the appropriate position for drilling. We aim for 1 mm to 2 mm from the chondrolabral junction. Next, the probe is placed intra-articular and medial to the anchor insertion site, and the anchor is loaded and then inserted around the probe (Figures 3A-3E).
The hip is then reduced. If indicated, a T-capsulotomy is performed for femoral osteochondroplasty.
Postoperative Care
Patients are placed in a postoperative hip brace and use a continuous passive motion machine 6 hours a day for 2 weeks, and an ice machine. They maintain 30 lb of foot-flat weight-bearing for 3 weeks, and begin a standard labral repair protocol on postoperative days 3 to 7.
Discussion
Hip labral preservation has evolved over the past 10 years, and current options for labral management include excision, débridement, labralization, repair, and reconstruction.1-13 Labral excision was studied by Miozzari and colleagues,8 who postulated on the basis of animal models that the labrum may regenerate. In their series of 9 patients treated with surgical hip dislocation and labral excision at average 4-year follow-up, repeat magnetic resonance angiography revealed no regeneration of tissue—modified Harris Hip Score was 83. The hip scores were less than those of patients treated with the same procedure with repair, and the authors concluded that defining labral débridement versus excision in the literature, and treating patients with primary repair or reconstruction techniques, may lead to better results. Their study used a small sample and was limited to an open procedure. Arthroscopic labral débridement in isolation was also a poor option for treatment of a labral tear. In a 2-year follow-up of 59 isolated labral débridement procedures, Krych and colleagues9 found 47% combined poor results.
There is level I evidence of the importance of labral repair. In 2013, Krych and colleagues7 conducted a randomized control trial of 38 female patients who underwent hip arthroscopy for FAI. At time of surgery, patients were randomly assigned to either débridement or repair. At 1-year follow-up, activities of daily living and Sports specific Hip Outcome Scores were statistically significantly superior in the repair group. On a subjective scale, 94% vs 78% of patients reported normal or near normal hips in the repair versus débridement groups respectively. Ayeni and colleagues20 performed a systematic review of 6 studies in an attempt to develop labral management recommendations. Five of the studies (N = 490 patients total) had improved results with labral repair over reconstruction. Although the studies had a low level of evidence, they found a trend toward improved results with labral repair. These studies highlight the importance of labral preservation and proper FAI management.
Techniques for labrum repair have advanced as well—from a looped suture technique to a base stitch and knotless independent tensioning.11-13 Restoration of the hip labrum function as a suction seal, fluid circulator and anatomic capsular repair is paramount to excellent results and stresses the importance of performing an anatomic labral repair.1-6 Knotless anchor repair is not novel and has been previously described. Fry and Domb12 reported on a knotless labral repair technique that uses push-lock devices (Arthrex) that do not allow for independent tensioning. Inversion-eversion was introduced to the literature by Moreira and colleagues,13 who described an independent tensioning technique that uses speed-lock anchors (Smith & Nephew). Our technique differs in that it involves a DALA portal; labral reduction and tensioning with a probe assist to ensure the second pass of the base stitch is at the apex of the labrum; and use of No. 1 instead of No. 2 suture. Although seemingly subtle, these differences allow for proper anchor placement nearer the rim, additional support in achieving precise suture placement, and less disruption of small labra. These differences are particularly relevant for smaller labra.
Evaluating repair techniques on the basis of high-evidence literature is challenging. In a matched-cohort study of 220 patients, Jackson and colleagues21 compared 2 techniques: looped and base stitch. At 2-year follow-up, patients in both groups showed improvement, and there was no statistically significant difference in patient-reported outcome measures between the groups. Sawyer and colleagues22 studied the outcomes of 326 consecutive patients who underwent looped, pierced, or combined labral repair at an average 32-month follow-up. The groups’ revision rates were comparable, each group improved in postoperative patient-reported outcomes, and the pierced group had significantly higher preoperative scores on the Western Ontario and McMaster Universities Osteoarthritis Index. These studies described a base or pierce repair that did not differ from a looped repair, though the techniques did not allow for independent tensioning to re-create an anatomical inversion-eversion repair and may have altered the reported outcomes.
Our current technique uses independent tensioning of the repair to allow control of labrum inversion-eversion to give an anatomical repair with restoration of the suction seal. Preoperative planning, addressing the FAI appropriately, proper suture-passing technique, controlling the labrum in inversion-eversion fashion, and anatomical labral repair are the elements of Dr. Mather’s preferred method for preserving the native labrum and allowing it to assume its native function.
Future Directions
As our understanding of FAI and labral function evolves, labral preservation surgery continues to advance. With surgeons continually developing new techniques and following up on previous techniques, the ability to preserve the native hip with lasting procedures evolves as well. Proper identification of the underlying cause of the labral tear and proper anatomical repair are paramount to the success of FAI surgery.
Am J Orthop. 2017;46(1):42-48. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
1. Philippon MJ, Nepple JJ, Campbell KJ, et al. The hip fluid seal—part I: the effect of an acetabular labral tear, repair, resection and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):722-729.
2. Nepple JJ, Philippon MJ, Campbell KJ, et al. The hip fluid seal—part II: the effect of an acetabular labral tear, repair, resection and reconstruction on hip stability to distraction. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):730-736.
3. Dwyer MK, Jones HL, Hogan MG, Field RE, McCarthy JC, Noble PC. The acetabular labrum regulates fluid circulation of the hip joint during functional activities. Am J Sports Med. 2014;42(4):812-819.
4. Greaves LL, Gilbart MK, Yung AC, Kozlowski, Wilson DR. Effect of acetabular labral tears, repair and resection on hip cartilage strain: a 7T MR study. J Biomech. 2010;43(5):858-863.
5. Freehill MT, Safran MR. The labrum of the hip: diagnosis and rationale for surgical correction. Clin Sports Med. 2011;30(2):293-315.
6. Myers CA, Register BC, Lertwanich P, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39(suppl):85S-91S.
7. Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy. 2013;29(1):46-53.
8. Miozzari HH, Celia M, Clark JM, Werlen S, Naal FD, Nötzli HP. No regeneration of the human acetabular labrum after excision to bone. Clin Orthop Relat Res. 2015;473(4):1349-1357.
9. Krych AJ, Kuzma SA, Kovachevich R, Hudgens JL, Stuart MJ, Levy BA. Modest mid-term outcomes after isolated arthroscopic debridement of acetabular labral tears. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):763-767.
10. Matsuda DK. Arthroscopic labralization of the hip: an alternative to labral reconstruction. Arthrosc Tech. 2014;3(1):e131-e133.
11. Philippon MJ, Faucet SC, Briggs KK. Arthroscopic hip labral repair. Arthrosc Tech. 2013;2(2):e73-e76.
12. Fry D, Domb B. Labral base refixation in the hip: rationale and technique for an anatomic approach to labral repair. Arthroscopy. 2010;26(9 suppl):S81-S89.
13. Moreira B, Pascual-Garrido C, Chadayamurri V, Mei-Dan O. Eversion-inversion labral repair and reconstruction technique for optimal suction seal. Arthrosc Tech. 2015;4(6):e697-e700.
14. Mook WR, Briggs KK, Philippon MJ. Evidence and approach for management of labral deficiency: the role for labral reconstruction. Sports Med Arthrosc. 2015;23(4):205-212.
15. Gupta A, Suarez-Ahedo C, Redmond JM, et al. Best practices during hip arthroscopy: aggregate recommendations of high-volume surgeons. Arthroscopy. 2015;31(9):1722-1727.
16. Yeung M, Kowalczuk M, Simunovic N, Ayeni OR. Hip arthroscopy in the setting of hip dysplasia: a systematic review. Bone Joint Res. 2016;5(6):225-231.
17. Hash TW. Magnetic resonance imaging of the hip. In: Nho SJ, Leunig M, Larson CM, Bedi A, Kelly BT, eds. Hip Arthroscopy and Hip Joint Preservation Surgery, Vol. 1. New York, NY: Springer; 2015:65-113.
18. Sutter R, Zubler V, Hoffmann A, et al. Hip MRI: how useful is intraarticular contrast material for evaluating surgically proven lesions of the labrum and articular cartilage? AJR Am J Roentgenol. 2014;202(1):160-169.
19. Federer AE, Karas V, Nho S, Coleman SH, Mather RC 3rd. Capsular suspension technique for hip arthroscopy. Arthrosc Tech. 2015;4(4):e317-e322.
20. Ayeni OR, Adamich J, Farrokhyar F, et al. Surgical management of labral tears during femoroacetabular impingement surgery: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):756-762.
21. Jackson TJ, Hammarstedt JE, Vemula SP, Domb BG. Acetabular labral base repair versus circumferential suture repair: a matched-paired comparison of clinical outcomes. Arthroscopy. 2015;31(9):1716-1721.
22. Sawyer GA, Briggs KK, Dornan GJ, Ommen ND, Philippon MJ. Clinical outcomes after arthroscopic hip labral repair using looped versus pierced suture techniques. Am J Sports Med. 2015;43(7):1683-1688.
1. Philippon MJ, Nepple JJ, Campbell KJ, et al. The hip fluid seal—part I: the effect of an acetabular labral tear, repair, resection and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):722-729.
2. Nepple JJ, Philippon MJ, Campbell KJ, et al. The hip fluid seal—part II: the effect of an acetabular labral tear, repair, resection and reconstruction on hip stability to distraction. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):730-736.
3. Dwyer MK, Jones HL, Hogan MG, Field RE, McCarthy JC, Noble PC. The acetabular labrum regulates fluid circulation of the hip joint during functional activities. Am J Sports Med. 2014;42(4):812-819.
4. Greaves LL, Gilbart MK, Yung AC, Kozlowski, Wilson DR. Effect of acetabular labral tears, repair and resection on hip cartilage strain: a 7T MR study. J Biomech. 2010;43(5):858-863.
5. Freehill MT, Safran MR. The labrum of the hip: diagnosis and rationale for surgical correction. Clin Sports Med. 2011;30(2):293-315.
6. Myers CA, Register BC, Lertwanich P, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39(suppl):85S-91S.
7. Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy. 2013;29(1):46-53.
8. Miozzari HH, Celia M, Clark JM, Werlen S, Naal FD, Nötzli HP. No regeneration of the human acetabular labrum after excision to bone. Clin Orthop Relat Res. 2015;473(4):1349-1357.
9. Krych AJ, Kuzma SA, Kovachevich R, Hudgens JL, Stuart MJ, Levy BA. Modest mid-term outcomes after isolated arthroscopic debridement of acetabular labral tears. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):763-767.
10. Matsuda DK. Arthroscopic labralization of the hip: an alternative to labral reconstruction. Arthrosc Tech. 2014;3(1):e131-e133.
11. Philippon MJ, Faucet SC, Briggs KK. Arthroscopic hip labral repair. Arthrosc Tech. 2013;2(2):e73-e76.
12. Fry D, Domb B. Labral base refixation in the hip: rationale and technique for an anatomic approach to labral repair. Arthroscopy. 2010;26(9 suppl):S81-S89.
13. Moreira B, Pascual-Garrido C, Chadayamurri V, Mei-Dan O. Eversion-inversion labral repair and reconstruction technique for optimal suction seal. Arthrosc Tech. 2015;4(6):e697-e700.
14. Mook WR, Briggs KK, Philippon MJ. Evidence and approach for management of labral deficiency: the role for labral reconstruction. Sports Med Arthrosc. 2015;23(4):205-212.
15. Gupta A, Suarez-Ahedo C, Redmond JM, et al. Best practices during hip arthroscopy: aggregate recommendations of high-volume surgeons. Arthroscopy. 2015;31(9):1722-1727.
16. Yeung M, Kowalczuk M, Simunovic N, Ayeni OR. Hip arthroscopy in the setting of hip dysplasia: a systematic review. Bone Joint Res. 2016;5(6):225-231.
17. Hash TW. Magnetic resonance imaging of the hip. In: Nho SJ, Leunig M, Larson CM, Bedi A, Kelly BT, eds. Hip Arthroscopy and Hip Joint Preservation Surgery, Vol. 1. New York, NY: Springer; 2015:65-113.
18. Sutter R, Zubler V, Hoffmann A, et al. Hip MRI: how useful is intraarticular contrast material for evaluating surgically proven lesions of the labrum and articular cartilage? AJR Am J Roentgenol. 2014;202(1):160-169.
19. Federer AE, Karas V, Nho S, Coleman SH, Mather RC 3rd. Capsular suspension technique for hip arthroscopy. Arthrosc Tech. 2015;4(4):e317-e322.
20. Ayeni OR, Adamich J, Farrokhyar F, et al. Surgical management of labral tears during femoroacetabular impingement surgery: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):756-762.
21. Jackson TJ, Hammarstedt JE, Vemula SP, Domb BG. Acetabular labral base repair versus circumferential suture repair: a matched-paired comparison of clinical outcomes. Arthroscopy. 2015;31(9):1716-1721.
22. Sawyer GA, Briggs KK, Dornan GJ, Ommen ND, Philippon MJ. Clinical outcomes after arthroscopic hip labral repair using looped versus pierced suture techniques. Am J Sports Med. 2015;43(7):1683-1688.
Treating depression after TBI
REIGNITE the desire: Tackle burnout in psychiatry
Burnout among psychiatric clinicians can lead to reduced job satisfaction, poorer quality of patient care, and depression.1 Signs of burnout include a feeling of cynicism (eg, negative attitudes toward patients), overwhelming exhaustion (eg, feeling depleted), and a sense of ineffectiveness (eg, reduced productivity).1 Workplace variables and other factors that could perpetuate burnout among psychiatrists include, but are not limited to:
- too much work
- chronic staff shortages
- working with difficult patients
- inability to meet self-imposed demands
- a lack of meaningful relationships with colleagues and supervisors.1,2
The mnemonic REIGNITE provides strategies to reduce the risk of burnout.1,3
Recognize your limits. Although saying “no” may be difficult for mental health clinicians, saying “yes” too often can be detrimental. Techniques for setting limits without alienating colleagues include:
- declining tasks (“I appreciate you thinking of me to do that, but I can’t complete it right now”)
- delaying an answer (“Let me ponder what you are asking”)
- delegating tasks (“I could really use your help”)
- avoid taking on too much (“I thought that I could do that extra task, but I realize that taking on the additional assignment isn’t going to work out”).
Expand your portfolio. Developing a diverse work portfolio (eg, teaching part-time) could diminish stagnation. Adding regenerative activities (eg, outdoor activities) could be restorative.
Itemize your priorities. Ask yourself what is important to you. Is it work? If so, can work be modified so it continues to be rewarding without resulting in burnout? If it isn’t work, then what is? Money? Family? Evaluating what is important and pursuing those priorities could increase overall life satisfaction.
Go after your passions. What do you like to do aside from work? Do you paint or play a musical instrument? Pursuing hobbies and interests can revitalize your spirit.
Now. We as a profession are notorious for saying to ourselves, “I will get to it (being happy) someday.” We delay happiness until we catch up with work, save enough money, and so on. This approach is unrealistic. It is better to live in the present because there are a finite number of days to seize the day. Focus your energy in the moment.
Interact. Isolating oneself will lead to burnout. If you are in solo practice, connect with other providers or get involved in community activities. If you work with other providers, interact with them in a meaningful manner (eg, don’t complain but rather air your concerns, accept honest feedback, be open to suggestions, and seek assistance; it is acceptable to admit that you can’t do everything).
Take time off and take care of yourself. Although that seems intuitive, psychiatrists, as a group, don’t do a good job of it. Waiting until you are burned out to take a vacation is counterproductive because you will be too drained to enjoy it. Taking care of your physical and mental health is equally important.
Enjoyment in and at work. We make a difference in our patients’ lives throughthe emotional connections we develop with them. By viewing what we do as fulfilling a higher calling, we can learn to enjoy what we do rather than feeling burdened by it. Advocating for better recognition—whether financial, institutional, or social—can create opportunities for personal satisfaction.
1. Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15(2):103-111.
2. Bressi C, Porcellana M, Gambini O, et al. Burnout among psychiatrists in Milan: a multicenter survey. Psychiatr Serv. 2009;60(7):985-988.
3. Bohnert P, O’Connell A. How to avoid burnout
Burnout among psychiatric clinicians can lead to reduced job satisfaction, poorer quality of patient care, and depression.1 Signs of burnout include a feeling of cynicism (eg, negative attitudes toward patients), overwhelming exhaustion (eg, feeling depleted), and a sense of ineffectiveness (eg, reduced productivity).1 Workplace variables and other factors that could perpetuate burnout among psychiatrists include, but are not limited to:
- too much work
- chronic staff shortages
- working with difficult patients
- inability to meet self-imposed demands
- a lack of meaningful relationships with colleagues and supervisors.1,2
The mnemonic REIGNITE provides strategies to reduce the risk of burnout.1,3
Recognize your limits. Although saying “no” may be difficult for mental health clinicians, saying “yes” too often can be detrimental. Techniques for setting limits without alienating colleagues include:
- declining tasks (“I appreciate you thinking of me to do that, but I can’t complete it right now”)
- delaying an answer (“Let me ponder what you are asking”)
- delegating tasks (“I could really use your help”)
- avoid taking on too much (“I thought that I could do that extra task, but I realize that taking on the additional assignment isn’t going to work out”).
Expand your portfolio. Developing a diverse work portfolio (eg, teaching part-time) could diminish stagnation. Adding regenerative activities (eg, outdoor activities) could be restorative.
Itemize your priorities. Ask yourself what is important to you. Is it work? If so, can work be modified so it continues to be rewarding without resulting in burnout? If it isn’t work, then what is? Money? Family? Evaluating what is important and pursuing those priorities could increase overall life satisfaction.
Go after your passions. What do you like to do aside from work? Do you paint or play a musical instrument? Pursuing hobbies and interests can revitalize your spirit.
Now. We as a profession are notorious for saying to ourselves, “I will get to it (being happy) someday.” We delay happiness until we catch up with work, save enough money, and so on. This approach is unrealistic. It is better to live in the present because there are a finite number of days to seize the day. Focus your energy in the moment.
Interact. Isolating oneself will lead to burnout. If you are in solo practice, connect with other providers or get involved in community activities. If you work with other providers, interact with them in a meaningful manner (eg, don’t complain but rather air your concerns, accept honest feedback, be open to suggestions, and seek assistance; it is acceptable to admit that you can’t do everything).
Take time off and take care of yourself. Although that seems intuitive, psychiatrists, as a group, don’t do a good job of it. Waiting until you are burned out to take a vacation is counterproductive because you will be too drained to enjoy it. Taking care of your physical and mental health is equally important.
Enjoyment in and at work. We make a difference in our patients’ lives throughthe emotional connections we develop with them. By viewing what we do as fulfilling a higher calling, we can learn to enjoy what we do rather than feeling burdened by it. Advocating for better recognition—whether financial, institutional, or social—can create opportunities for personal satisfaction.
Burnout among psychiatric clinicians can lead to reduced job satisfaction, poorer quality of patient care, and depression.1 Signs of burnout include a feeling of cynicism (eg, negative attitudes toward patients), overwhelming exhaustion (eg, feeling depleted), and a sense of ineffectiveness (eg, reduced productivity).1 Workplace variables and other factors that could perpetuate burnout among psychiatrists include, but are not limited to:
- too much work
- chronic staff shortages
- working with difficult patients
- inability to meet self-imposed demands
- a lack of meaningful relationships with colleagues and supervisors.1,2
The mnemonic REIGNITE provides strategies to reduce the risk of burnout.1,3
Recognize your limits. Although saying “no” may be difficult for mental health clinicians, saying “yes” too often can be detrimental. Techniques for setting limits without alienating colleagues include:
- declining tasks (“I appreciate you thinking of me to do that, but I can’t complete it right now”)
- delaying an answer (“Let me ponder what you are asking”)
- delegating tasks (“I could really use your help”)
- avoid taking on too much (“I thought that I could do that extra task, but I realize that taking on the additional assignment isn’t going to work out”).
Expand your portfolio. Developing a diverse work portfolio (eg, teaching part-time) could diminish stagnation. Adding regenerative activities (eg, outdoor activities) could be restorative.
Itemize your priorities. Ask yourself what is important to you. Is it work? If so, can work be modified so it continues to be rewarding without resulting in burnout? If it isn’t work, then what is? Money? Family? Evaluating what is important and pursuing those priorities could increase overall life satisfaction.
Go after your passions. What do you like to do aside from work? Do you paint or play a musical instrument? Pursuing hobbies and interests can revitalize your spirit.
Now. We as a profession are notorious for saying to ourselves, “I will get to it (being happy) someday.” We delay happiness until we catch up with work, save enough money, and so on. This approach is unrealistic. It is better to live in the present because there are a finite number of days to seize the day. Focus your energy in the moment.
Interact. Isolating oneself will lead to burnout. If you are in solo practice, connect with other providers or get involved in community activities. If you work with other providers, interact with them in a meaningful manner (eg, don’t complain but rather air your concerns, accept honest feedback, be open to suggestions, and seek assistance; it is acceptable to admit that you can’t do everything).
Take time off and take care of yourself. Although that seems intuitive, psychiatrists, as a group, don’t do a good job of it. Waiting until you are burned out to take a vacation is counterproductive because you will be too drained to enjoy it. Taking care of your physical and mental health is equally important.
Enjoyment in and at work. We make a difference in our patients’ lives throughthe emotional connections we develop with them. By viewing what we do as fulfilling a higher calling, we can learn to enjoy what we do rather than feeling burdened by it. Advocating for better recognition—whether financial, institutional, or social—can create opportunities for personal satisfaction.
1. Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15(2):103-111.
2. Bressi C, Porcellana M, Gambini O, et al. Burnout among psychiatrists in Milan: a multicenter survey. Psychiatr Serv. 2009;60(7):985-988.
3. Bohnert P, O’Connell A. How to avoid burnout
1. Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15(2):103-111.
2. Bressi C, Porcellana M, Gambini O, et al. Burnout among psychiatrists in Milan: a multicenter survey. Psychiatr Serv. 2009;60(7):985-988.
3. Bohnert P, O’Connell A. How to avoid burnout
Maddening therapies: How hallucinogens morphed into novel treatments
Snake venom is deadly but is being used to treat some cancers,1 because it produces contortrostatin, a protein that “paralyzes” cancer cells and prevents them from migrating. Venoms from spiders are being investigated as a treatment to slow the progression of muscular dystrophy by preventing muscle cells from deteriorating. Venom from tarantulas can relieve chronic pain, and those from centipedes help rodents tolerate thermal, chemical, or acid pain. Scorpion venom can cause cancer cells to glow under a flashlight, enabling surgeons to locate and remove them. Anemones toxin could be used to treat autoimmune diseases, such as rheumatoid arthritis, multiple sclerosis, and lupus.
Vaccines are an excellent example of how deadly pathogens can be transformed into life-saving therapies. Billions of people have been protected from polio, smallpox, tetanus, diphtheria, measles, mumps, rubella, influenza, pneumococcus, hepatitis A and B, rabies, shingles, typhoid, meningitis, or cholera. Turning killers into saviors is one of the most remarkable miracles of medical research.2
The mind-boggling transformation of mind-altering drugs
In psychiatry, psychedelic drugs have been repurposed into useful therapies for mental illness. As recently as a decade ago, psychiatric practitioners—physicians and nurse practitioners—regarded hallucinogens as dangerous, “must-avoid” drugs of abuse that could trigger or exacerbate serious psychiatric disorders. Then, thanks to ongoing research, the psychedelic “caterpillars” transformed into therapeutic “butterflies,” and the despised drugs of abuse became welcome adjuncts for treating some stubborn psychopathologies. Such paradoxical developments are emblematic of how one can always find a silver lining.
Consider the following transformations of various psychedelics and hallucinogens—also called “entheogens”—into novel pharmacotherapies. Note that in most cases, the application of these mind-altering drugs into useful medications is still a work in progress.
LSD
Lysergic acid diethylamide (LSD) was used extensively for treating mood disorders in the pre-antidepressant era, before it was prohibited in the late 1960s. A review of 19 studies—many uncontrolled—concluded that approximately 80% of patients improved, according to the treating physicians.3 However, research on LSD was halted for several decades after it became illegal, and resumed in 2010. Neuropsychiatrists and neuroscience researchers are now employing advanced techniques, such as neuroimaging, molecular pharmacology, and connectomics, to study its therapeutic effects.4 LSD is not only being used for treatment-resistant depression but also anxiety, alcoholism, autism, and even schizophrenia. However, despite its potential uses for treating alcoholism and anxiety, enhancing creativity, or caring for terminally ill patients, using LSD requires expertise, caution, and adherence to ethical standards.5
In healthy individuals, the effects of LSD include visual hallucinations, audiovisual synesthesia, depersonalization and derealization, and a sense of well-being, happiness, closeness to others, and trust.
Biologic effects include increased heart rate and blood pressure, elevated temperature, dilated pupils, and increased serum cortisol, prolactin, oxytocin, and epinephrine. All effects subside within 3 days.6
Psilocybin
Psilocybin, a component of some mushrooms that is known for its use during rituals in some cultures, has been discovered to have antidepressant, anxiolytic, and anti-addictive effects.7 Recent controlled studies at Johns Hopkins University reported that a single dose of psilocybin can relieve anxiety or depression for up to 6 months, which, if replicated, could lead to a remarkable paradigm shift in treating mood and anxiety disorders, especially if patients do not respond to standard antidepressants.3 Other emerging uses of both psilocybin and LSD are in treating addictions8 where psychiatry is desperately looking for innovative new therapies.
Ecstasy
MDMA (3,4-methylenedioxymethamphetamine), also known as ecstasy, is widely regarded as a harmful party drug that produces euphoria, but not hallucinations. However, it has emerged as a useful treatment for posttraumatic stress disorder (PTSD). In one study of female sexual abuse victims, 80% of the patients who received MDMA with psychotherapy no longer met diagnostic criteria for PTSD after 2 months.9 Other studies showed no effects. Despite persistent skepticisms by many, the Multidisciplinary Association for Psychedelics Studies organization is investing millions of dollars into studying MDMA for PTSD in several countries.9,10 One hurdle is that it is difficult to conduct truly blind studies with psychedelic drugs because of their profound effects. MDMA releases cortisol, oxytocin—which are known to facilitate psychotherapy—and testosterone, but the debate about the risk–benefit ratio will continue.11 MDMA also is being studied for treating social anxiety in adults with autism.12
Ketamine
Ketamine is a weaker cousin of the potent psychotogenic phencyclidine (approximately one-fiftieth the potency) and is a well-known drug of abuse that causes dissociation and hallucinations. It is used as an anesthetic in veterinary medicine and in children undergoing surgical procedures. Until recently, its only use in psychiatry has been as an anesthetic during electroconvulsive therapy. However, over the past few years, IV ketamine has been in the spotlight as a breakthrough, rapid-onset antidepressant and anti-suicidal agent in several controlled studies.13 This drug is revolutionizing the management of treatment-resistant depression and suicidal ideation and generating new insights into the neurobiology of depression.
Cannabis
Last, but certainly not least, is marijuana, which is more widely used than all the other psychedelics combined, and is currently at the center of a national debate about its legalization. Although the director of the National Institute on Drug Abuse highlighted the many risk of marijuana,14 studies have pointed to the myriad medical uses of Cannabis.15,16 An editorial in Nature Medicine recently urged that regulators reconsider the tight constraints on marijuana research.17 Some of the medical applications of marijuana include:
- psychiatry (anxiety, PTSD)
- neurology (severe epilepsy, tremors in Parkinson’s disease, traumatic brain injury, pain of multiple sclerosis, muscle spasms, and progression of Alzheimer’s disease)
- oncology (nausea and pain of chemotherapy, reduction of metastasis)
- ophthalmology (decrease of intraocular pressure in glaucoma)
- autoimmune disorders (rheumatoid arthritis, Crohn’s disease, lupus).
However, as a schizophrenia researcher, I am wary about marijuana’s high risk of triggering psychosis in young adults with a family history of schizophrenia spectrum disorders.18
The above are examples of how psychiatry is finally recognizing the therapeutic value inherent in traditionally “evil” street drugs that we euphemistically refer to as “recreational drugs.” Even methamphetamine, the universally condemned and clearly harmful drug, was recently reported to be neuroprotective at low dosages!19 Could our field have suffered from a blind eye to the benefits of these hallucinogens and ignored the possibility that some persons with addiction who use these “recreational drugs” may have been self-medicating to alleviate their un-diagnosed psychiatric disorder? We need to reconceptualize the pejorative term “mind-altering drug” because of its implicitly negative connotation. After all, alteration may indicate a favorable, not just a deleterious, outcome.
1. Vyas VK, Brahmbhatt K, Bhatt H, et al. Therapeutic potential of snake venom in cancer therapy: current perspectives. Asian Pac J Trop Biomed. 2013;3(2):156-162.
2. Loehr J. The vaccine answer book: 200 essential answers to help you make the right decisions for your child. Naperville, IL: Sourcebooks Inc; 2009.
3. Rucker JJ, Jelen LA, Flynn S, et al. Psychedelics in the treatment of unipolar mood disorders: a systematic review. J Psychopharmacol. 2016;30(12):1220-1229.
4. Mucke HA. From psychiatry to flower power and back again: the amazing story of lysergic acid diethylamide [published online July 8, 2016]. Assay Drug Dev Technol. doi: 10.1089/adt.2016.747.
5. Das S, Barnwal P, Ramasamy A, et al. Lysergic acid diethylamide: a drug of ‘use’? Ther Advances Pychopharmacol. 2016;6(3):214-228.
6. Schmid Y, Enzler F, Gasser P, et al. Acute effects of lysergic acid diethylamide in healthy subjects. Biol Psychiatry. 2015;78(8):544-553.
7. Dos Santos RG, Osório FL, Crippa JA, et al. Antidepressive, anxiolytic, and antiaddictive effects of ayahuasca, psilocybin and lysergic acid diethylamide (LSD): a systematic review of clinical trials published in the last 25 years. Ther Adv Psychopharmacol. 2016;6(3):193-213.
8. Bogenschutz MP. Studying the effects of classic hallucinogens in the treatment of alcoholism: rationale, methodology, and current research with psilocybin. Curr Drug Abuse Rev. 2013;6(1):17-29.
9. Kupferschmidt K. Can ecstasy treat the agony of PTSD? Science. 2014;345:22-23.
10. Sessa B. MDMA and PTSD treatment: PTSD: from novel pathophysiology to innovative therapeutics [published online July 6, 2016]. Neurosci Lett. doi: 10.1016/j.neulet.2016.07.004.
11. Parrott AC. The potential dangers of using MDMA for psychotherapy. J Psychoactive Drugs. 2014;46(1):37-43.
12. Danforth AL, Struble CM, Yazar-Klosinski B, et al. MDMA-assisted therapy: a new treatment model for social anxiety in autistic adults. Prog Neuropsychopharmacol Biol Psychiatry. 2016;64:237-249.
13. Feifel D. Breaking sad: unleashing the breakthrough potential of ketamine’s rapid antidepressant effects [published online November 26, 2016]. Drug Dev Res. doi: 10.1002/ddr.21347.
14. Volkow ND, Baler RD, Compton WM, et al. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219-2227.
15. Murnion B. Medicinal cannabis. Aust Prescr. 2015;38(6):212-215.
16. Borgelt LM, Franson KL, Nussbaum AM, et al. The pharmacologic and clinical effects of medical cannabis. Pharmacotherapy. 2013;33(2):195-209.
17. Release the strains. Nat Med. 2015;21(9):963.
18. Moore TH, Zammit S, Lingford-Hughes A, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319-328.
19. Rau T, Ziemniak J, Poulsen D, et al. The neuroprotective potential of low-dose methamphetamine in preclinical models of stroke and traumatic brain injury. Prog Neuropsychopharmacol Biol Psychiatry. 2016;64:231-236.
Snake venom is deadly but is being used to treat some cancers,1 because it produces contortrostatin, a protein that “paralyzes” cancer cells and prevents them from migrating. Venoms from spiders are being investigated as a treatment to slow the progression of muscular dystrophy by preventing muscle cells from deteriorating. Venom from tarantulas can relieve chronic pain, and those from centipedes help rodents tolerate thermal, chemical, or acid pain. Scorpion venom can cause cancer cells to glow under a flashlight, enabling surgeons to locate and remove them. Anemones toxin could be used to treat autoimmune diseases, such as rheumatoid arthritis, multiple sclerosis, and lupus.
Vaccines are an excellent example of how deadly pathogens can be transformed into life-saving therapies. Billions of people have been protected from polio, smallpox, tetanus, diphtheria, measles, mumps, rubella, influenza, pneumococcus, hepatitis A and B, rabies, shingles, typhoid, meningitis, or cholera. Turning killers into saviors is one of the most remarkable miracles of medical research.2
The mind-boggling transformation of mind-altering drugs
In psychiatry, psychedelic drugs have been repurposed into useful therapies for mental illness. As recently as a decade ago, psychiatric practitioners—physicians and nurse practitioners—regarded hallucinogens as dangerous, “must-avoid” drugs of abuse that could trigger or exacerbate serious psychiatric disorders. Then, thanks to ongoing research, the psychedelic “caterpillars” transformed into therapeutic “butterflies,” and the despised drugs of abuse became welcome adjuncts for treating some stubborn psychopathologies. Such paradoxical developments are emblematic of how one can always find a silver lining.
Consider the following transformations of various psychedelics and hallucinogens—also called “entheogens”—into novel pharmacotherapies. Note that in most cases, the application of these mind-altering drugs into useful medications is still a work in progress.
LSD
Lysergic acid diethylamide (LSD) was used extensively for treating mood disorders in the pre-antidepressant era, before it was prohibited in the late 1960s. A review of 19 studies—many uncontrolled—concluded that approximately 80% of patients improved, according to the treating physicians.3 However, research on LSD was halted for several decades after it became illegal, and resumed in 2010. Neuropsychiatrists and neuroscience researchers are now employing advanced techniques, such as neuroimaging, molecular pharmacology, and connectomics, to study its therapeutic effects.4 LSD is not only being used for treatment-resistant depression but also anxiety, alcoholism, autism, and even schizophrenia. However, despite its potential uses for treating alcoholism and anxiety, enhancing creativity, or caring for terminally ill patients, using LSD requires expertise, caution, and adherence to ethical standards.5
In healthy individuals, the effects of LSD include visual hallucinations, audiovisual synesthesia, depersonalization and derealization, and a sense of well-being, happiness, closeness to others, and trust.
Biologic effects include increased heart rate and blood pressure, elevated temperature, dilated pupils, and increased serum cortisol, prolactin, oxytocin, and epinephrine. All effects subside within 3 days.6
Psilocybin
Psilocybin, a component of some mushrooms that is known for its use during rituals in some cultures, has been discovered to have antidepressant, anxiolytic, and anti-addictive effects.7 Recent controlled studies at Johns Hopkins University reported that a single dose of psilocybin can relieve anxiety or depression for up to 6 months, which, if replicated, could lead to a remarkable paradigm shift in treating mood and anxiety disorders, especially if patients do not respond to standard antidepressants.3 Other emerging uses of both psilocybin and LSD are in treating addictions8 where psychiatry is desperately looking for innovative new therapies.
Ecstasy
MDMA (3,4-methylenedioxymethamphetamine), also known as ecstasy, is widely regarded as a harmful party drug that produces euphoria, but not hallucinations. However, it has emerged as a useful treatment for posttraumatic stress disorder (PTSD). In one study of female sexual abuse victims, 80% of the patients who received MDMA with psychotherapy no longer met diagnostic criteria for PTSD after 2 months.9 Other studies showed no effects. Despite persistent skepticisms by many, the Multidisciplinary Association for Psychedelics Studies organization is investing millions of dollars into studying MDMA for PTSD in several countries.9,10 One hurdle is that it is difficult to conduct truly blind studies with psychedelic drugs because of their profound effects. MDMA releases cortisol, oxytocin—which are known to facilitate psychotherapy—and testosterone, but the debate about the risk–benefit ratio will continue.11 MDMA also is being studied for treating social anxiety in adults with autism.12
Ketamine
Ketamine is a weaker cousin of the potent psychotogenic phencyclidine (approximately one-fiftieth the potency) and is a well-known drug of abuse that causes dissociation and hallucinations. It is used as an anesthetic in veterinary medicine and in children undergoing surgical procedures. Until recently, its only use in psychiatry has been as an anesthetic during electroconvulsive therapy. However, over the past few years, IV ketamine has been in the spotlight as a breakthrough, rapid-onset antidepressant and anti-suicidal agent in several controlled studies.13 This drug is revolutionizing the management of treatment-resistant depression and suicidal ideation and generating new insights into the neurobiology of depression.
Cannabis
Last, but certainly not least, is marijuana, which is more widely used than all the other psychedelics combined, and is currently at the center of a national debate about its legalization. Although the director of the National Institute on Drug Abuse highlighted the many risk of marijuana,14 studies have pointed to the myriad medical uses of Cannabis.15,16 An editorial in Nature Medicine recently urged that regulators reconsider the tight constraints on marijuana research.17 Some of the medical applications of marijuana include:
- psychiatry (anxiety, PTSD)
- neurology (severe epilepsy, tremors in Parkinson’s disease, traumatic brain injury, pain of multiple sclerosis, muscle spasms, and progression of Alzheimer’s disease)
- oncology (nausea and pain of chemotherapy, reduction of metastasis)
- ophthalmology (decrease of intraocular pressure in glaucoma)
- autoimmune disorders (rheumatoid arthritis, Crohn’s disease, lupus).
However, as a schizophrenia researcher, I am wary about marijuana’s high risk of triggering psychosis in young adults with a family history of schizophrenia spectrum disorders.18
The above are examples of how psychiatry is finally recognizing the therapeutic value inherent in traditionally “evil” street drugs that we euphemistically refer to as “recreational drugs.” Even methamphetamine, the universally condemned and clearly harmful drug, was recently reported to be neuroprotective at low dosages!19 Could our field have suffered from a blind eye to the benefits of these hallucinogens and ignored the possibility that some persons with addiction who use these “recreational drugs” may have been self-medicating to alleviate their un-diagnosed psychiatric disorder? We need to reconceptualize the pejorative term “mind-altering drug” because of its implicitly negative connotation. After all, alteration may indicate a favorable, not just a deleterious, outcome.
Snake venom is deadly but is being used to treat some cancers,1 because it produces contortrostatin, a protein that “paralyzes” cancer cells and prevents them from migrating. Venoms from spiders are being investigated as a treatment to slow the progression of muscular dystrophy by preventing muscle cells from deteriorating. Venom from tarantulas can relieve chronic pain, and those from centipedes help rodents tolerate thermal, chemical, or acid pain. Scorpion venom can cause cancer cells to glow under a flashlight, enabling surgeons to locate and remove them. Anemones toxin could be used to treat autoimmune diseases, such as rheumatoid arthritis, multiple sclerosis, and lupus.
Vaccines are an excellent example of how deadly pathogens can be transformed into life-saving therapies. Billions of people have been protected from polio, smallpox, tetanus, diphtheria, measles, mumps, rubella, influenza, pneumococcus, hepatitis A and B, rabies, shingles, typhoid, meningitis, or cholera. Turning killers into saviors is one of the most remarkable miracles of medical research.2
The mind-boggling transformation of mind-altering drugs
In psychiatry, psychedelic drugs have been repurposed into useful therapies for mental illness. As recently as a decade ago, psychiatric practitioners—physicians and nurse practitioners—regarded hallucinogens as dangerous, “must-avoid” drugs of abuse that could trigger or exacerbate serious psychiatric disorders. Then, thanks to ongoing research, the psychedelic “caterpillars” transformed into therapeutic “butterflies,” and the despised drugs of abuse became welcome adjuncts for treating some stubborn psychopathologies. Such paradoxical developments are emblematic of how one can always find a silver lining.
Consider the following transformations of various psychedelics and hallucinogens—also called “entheogens”—into novel pharmacotherapies. Note that in most cases, the application of these mind-altering drugs into useful medications is still a work in progress.
LSD
Lysergic acid diethylamide (LSD) was used extensively for treating mood disorders in the pre-antidepressant era, before it was prohibited in the late 1960s. A review of 19 studies—many uncontrolled—concluded that approximately 80% of patients improved, according to the treating physicians.3 However, research on LSD was halted for several decades after it became illegal, and resumed in 2010. Neuropsychiatrists and neuroscience researchers are now employing advanced techniques, such as neuroimaging, molecular pharmacology, and connectomics, to study its therapeutic effects.4 LSD is not only being used for treatment-resistant depression but also anxiety, alcoholism, autism, and even schizophrenia. However, despite its potential uses for treating alcoholism and anxiety, enhancing creativity, or caring for terminally ill patients, using LSD requires expertise, caution, and adherence to ethical standards.5
In healthy individuals, the effects of LSD include visual hallucinations, audiovisual synesthesia, depersonalization and derealization, and a sense of well-being, happiness, closeness to others, and trust.
Biologic effects include increased heart rate and blood pressure, elevated temperature, dilated pupils, and increased serum cortisol, prolactin, oxytocin, and epinephrine. All effects subside within 3 days.6
Psilocybin
Psilocybin, a component of some mushrooms that is known for its use during rituals in some cultures, has been discovered to have antidepressant, anxiolytic, and anti-addictive effects.7 Recent controlled studies at Johns Hopkins University reported that a single dose of psilocybin can relieve anxiety or depression for up to 6 months, which, if replicated, could lead to a remarkable paradigm shift in treating mood and anxiety disorders, especially if patients do not respond to standard antidepressants.3 Other emerging uses of both psilocybin and LSD are in treating addictions8 where psychiatry is desperately looking for innovative new therapies.
Ecstasy
MDMA (3,4-methylenedioxymethamphetamine), also known as ecstasy, is widely regarded as a harmful party drug that produces euphoria, but not hallucinations. However, it has emerged as a useful treatment for posttraumatic stress disorder (PTSD). In one study of female sexual abuse victims, 80% of the patients who received MDMA with psychotherapy no longer met diagnostic criteria for PTSD after 2 months.9 Other studies showed no effects. Despite persistent skepticisms by many, the Multidisciplinary Association for Psychedelics Studies organization is investing millions of dollars into studying MDMA for PTSD in several countries.9,10 One hurdle is that it is difficult to conduct truly blind studies with psychedelic drugs because of their profound effects. MDMA releases cortisol, oxytocin—which are known to facilitate psychotherapy—and testosterone, but the debate about the risk–benefit ratio will continue.11 MDMA also is being studied for treating social anxiety in adults with autism.12
Ketamine
Ketamine is a weaker cousin of the potent psychotogenic phencyclidine (approximately one-fiftieth the potency) and is a well-known drug of abuse that causes dissociation and hallucinations. It is used as an anesthetic in veterinary medicine and in children undergoing surgical procedures. Until recently, its only use in psychiatry has been as an anesthetic during electroconvulsive therapy. However, over the past few years, IV ketamine has been in the spotlight as a breakthrough, rapid-onset antidepressant and anti-suicidal agent in several controlled studies.13 This drug is revolutionizing the management of treatment-resistant depression and suicidal ideation and generating new insights into the neurobiology of depression.
Cannabis
Last, but certainly not least, is marijuana, which is more widely used than all the other psychedelics combined, and is currently at the center of a national debate about its legalization. Although the director of the National Institute on Drug Abuse highlighted the many risk of marijuana,14 studies have pointed to the myriad medical uses of Cannabis.15,16 An editorial in Nature Medicine recently urged that regulators reconsider the tight constraints on marijuana research.17 Some of the medical applications of marijuana include:
- psychiatry (anxiety, PTSD)
- neurology (severe epilepsy, tremors in Parkinson’s disease, traumatic brain injury, pain of multiple sclerosis, muscle spasms, and progression of Alzheimer’s disease)
- oncology (nausea and pain of chemotherapy, reduction of metastasis)
- ophthalmology (decrease of intraocular pressure in glaucoma)
- autoimmune disorders (rheumatoid arthritis, Crohn’s disease, lupus).
However, as a schizophrenia researcher, I am wary about marijuana’s high risk of triggering psychosis in young adults with a family history of schizophrenia spectrum disorders.18
The above are examples of how psychiatry is finally recognizing the therapeutic value inherent in traditionally “evil” street drugs that we euphemistically refer to as “recreational drugs.” Even methamphetamine, the universally condemned and clearly harmful drug, was recently reported to be neuroprotective at low dosages!19 Could our field have suffered from a blind eye to the benefits of these hallucinogens and ignored the possibility that some persons with addiction who use these “recreational drugs” may have been self-medicating to alleviate their un-diagnosed psychiatric disorder? We need to reconceptualize the pejorative term “mind-altering drug” because of its implicitly negative connotation. After all, alteration may indicate a favorable, not just a deleterious, outcome.
1. Vyas VK, Brahmbhatt K, Bhatt H, et al. Therapeutic potential of snake venom in cancer therapy: current perspectives. Asian Pac J Trop Biomed. 2013;3(2):156-162.
2. Loehr J. The vaccine answer book: 200 essential answers to help you make the right decisions for your child. Naperville, IL: Sourcebooks Inc; 2009.
3. Rucker JJ, Jelen LA, Flynn S, et al. Psychedelics in the treatment of unipolar mood disorders: a systematic review. J Psychopharmacol. 2016;30(12):1220-1229.
4. Mucke HA. From psychiatry to flower power and back again: the amazing story of lysergic acid diethylamide [published online July 8, 2016]. Assay Drug Dev Technol. doi: 10.1089/adt.2016.747.
5. Das S, Barnwal P, Ramasamy A, et al. Lysergic acid diethylamide: a drug of ‘use’? Ther Advances Pychopharmacol. 2016;6(3):214-228.
6. Schmid Y, Enzler F, Gasser P, et al. Acute effects of lysergic acid diethylamide in healthy subjects. Biol Psychiatry. 2015;78(8):544-553.
7. Dos Santos RG, Osório FL, Crippa JA, et al. Antidepressive, anxiolytic, and antiaddictive effects of ayahuasca, psilocybin and lysergic acid diethylamide (LSD): a systematic review of clinical trials published in the last 25 years. Ther Adv Psychopharmacol. 2016;6(3):193-213.
8. Bogenschutz MP. Studying the effects of classic hallucinogens in the treatment of alcoholism: rationale, methodology, and current research with psilocybin. Curr Drug Abuse Rev. 2013;6(1):17-29.
9. Kupferschmidt K. Can ecstasy treat the agony of PTSD? Science. 2014;345:22-23.
10. Sessa B. MDMA and PTSD treatment: PTSD: from novel pathophysiology to innovative therapeutics [published online July 6, 2016]. Neurosci Lett. doi: 10.1016/j.neulet.2016.07.004.
11. Parrott AC. The potential dangers of using MDMA for psychotherapy. J Psychoactive Drugs. 2014;46(1):37-43.
12. Danforth AL, Struble CM, Yazar-Klosinski B, et al. MDMA-assisted therapy: a new treatment model for social anxiety in autistic adults. Prog Neuropsychopharmacol Biol Psychiatry. 2016;64:237-249.
13. Feifel D. Breaking sad: unleashing the breakthrough potential of ketamine’s rapid antidepressant effects [published online November 26, 2016]. Drug Dev Res. doi: 10.1002/ddr.21347.
14. Volkow ND, Baler RD, Compton WM, et al. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219-2227.
15. Murnion B. Medicinal cannabis. Aust Prescr. 2015;38(6):212-215.
16. Borgelt LM, Franson KL, Nussbaum AM, et al. The pharmacologic and clinical effects of medical cannabis. Pharmacotherapy. 2013;33(2):195-209.
17. Release the strains. Nat Med. 2015;21(9):963.
18. Moore TH, Zammit S, Lingford-Hughes A, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319-328.
19. Rau T, Ziemniak J, Poulsen D, et al. The neuroprotective potential of low-dose methamphetamine in preclinical models of stroke and traumatic brain injury. Prog Neuropsychopharmacol Biol Psychiatry. 2016;64:231-236.
1. Vyas VK, Brahmbhatt K, Bhatt H, et al. Therapeutic potential of snake venom in cancer therapy: current perspectives. Asian Pac J Trop Biomed. 2013;3(2):156-162.
2. Loehr J. The vaccine answer book: 200 essential answers to help you make the right decisions for your child. Naperville, IL: Sourcebooks Inc; 2009.
3. Rucker JJ, Jelen LA, Flynn S, et al. Psychedelics in the treatment of unipolar mood disorders: a systematic review. J Psychopharmacol. 2016;30(12):1220-1229.
4. Mucke HA. From psychiatry to flower power and back again: the amazing story of lysergic acid diethylamide [published online July 8, 2016]. Assay Drug Dev Technol. doi: 10.1089/adt.2016.747.
5. Das S, Barnwal P, Ramasamy A, et al. Lysergic acid diethylamide: a drug of ‘use’? Ther Advances Pychopharmacol. 2016;6(3):214-228.
6. Schmid Y, Enzler F, Gasser P, et al. Acute effects of lysergic acid diethylamide in healthy subjects. Biol Psychiatry. 2015;78(8):544-553.
7. Dos Santos RG, Osório FL, Crippa JA, et al. Antidepressive, anxiolytic, and antiaddictive effects of ayahuasca, psilocybin and lysergic acid diethylamide (LSD): a systematic review of clinical trials published in the last 25 years. Ther Adv Psychopharmacol. 2016;6(3):193-213.
8. Bogenschutz MP. Studying the effects of classic hallucinogens in the treatment of alcoholism: rationale, methodology, and current research with psilocybin. Curr Drug Abuse Rev. 2013;6(1):17-29.
9. Kupferschmidt K. Can ecstasy treat the agony of PTSD? Science. 2014;345:22-23.
10. Sessa B. MDMA and PTSD treatment: PTSD: from novel pathophysiology to innovative therapeutics [published online July 6, 2016]. Neurosci Lett. doi: 10.1016/j.neulet.2016.07.004.
11. Parrott AC. The potential dangers of using MDMA for psychotherapy. J Psychoactive Drugs. 2014;46(1):37-43.
12. Danforth AL, Struble CM, Yazar-Klosinski B, et al. MDMA-assisted therapy: a new treatment model for social anxiety in autistic adults. Prog Neuropsychopharmacol Biol Psychiatry. 2016;64:237-249.
13. Feifel D. Breaking sad: unleashing the breakthrough potential of ketamine’s rapid antidepressant effects [published online November 26, 2016]. Drug Dev Res. doi: 10.1002/ddr.21347.
14. Volkow ND, Baler RD, Compton WM, et al. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219-2227.
15. Murnion B. Medicinal cannabis. Aust Prescr. 2015;38(6):212-215.
16. Borgelt LM, Franson KL, Nussbaum AM, et al. The pharmacologic and clinical effects of medical cannabis. Pharmacotherapy. 2013;33(2):195-209.
17. Release the strains. Nat Med. 2015;21(9):963.
18. Moore TH, Zammit S, Lingford-Hughes A, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319-328.
19. Rau T, Ziemniak J, Poulsen D, et al. The neuroprotective potential of low-dose methamphetamine in preclinical models of stroke and traumatic brain injury. Prog Neuropsychopharmacol Biol Psychiatry. 2016;64:231-236.
Acute pancreatitis
Dear Colleagues,
Acute pancreatitis has long been one of the “bread and butter” conditions in gastroenterology and having up-to-date knowledge on its management will serve our community well. In this issue of The New Gastroenterologist, Abhishek Gulati and Georgios Papachristou (University of Pittsburgh) provide a comprehensive review of the latest advances in the treatment of acute pancreatitis and its complications, which has direct application to GI clinical practice.
Also included in this issue of The New Gastroenterologist is an article highlighting the importance of diversity in gastroenterology training by Sandra Quezada (University of Maryland) and an article on financial tips to ensure a secure retirement by an experienced contract and tax attorney. Additionally, Peter Liang (New York University), Tatyana Kushner (University of California at San Francisco), and Folasade May (University of California at Los Angeles), who are all members of the AGA Institute Trainee and Early Career Committee, provide an overview of the work that they have done to benefit the early career gastroenterology community and the opportunities that exist for getting involved in related AGA activities.
In prior issues of The New Gastroenterologist, we have typically featured a case from the “Clinical Challenges and Images in GI” section of Gastroenterology. However, in this issue we will instead feature a “Practical Teaching Case,” which is one of Gastroenterology’s newest features with a specific focus on the trainee and early-career gastroenterologist. These new cases are great didactic resources and I hope that they become a part of the regular reading of the early career GI community.
If you enjoy the articles in The New Gastroenterologist, have suggestions for future issues, or are interested in contributing to future issues, please let us know! You can contact me ([email protected]) or the Managing Editor of The New Gastroenterologist, Ryan Farrell ([email protected]).
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Bryson W. Katona is a instructor of medicine in the division of gasteroenterology at the University of Pennsylvania.
Dear Colleagues,
Acute pancreatitis has long been one of the “bread and butter” conditions in gastroenterology and having up-to-date knowledge on its management will serve our community well. In this issue of The New Gastroenterologist, Abhishek Gulati and Georgios Papachristou (University of Pittsburgh) provide a comprehensive review of the latest advances in the treatment of acute pancreatitis and its complications, which has direct application to GI clinical practice.
Also included in this issue of The New Gastroenterologist is an article highlighting the importance of diversity in gastroenterology training by Sandra Quezada (University of Maryland) and an article on financial tips to ensure a secure retirement by an experienced contract and tax attorney. Additionally, Peter Liang (New York University), Tatyana Kushner (University of California at San Francisco), and Folasade May (University of California at Los Angeles), who are all members of the AGA Institute Trainee and Early Career Committee, provide an overview of the work that they have done to benefit the early career gastroenterology community and the opportunities that exist for getting involved in related AGA activities.
In prior issues of The New Gastroenterologist, we have typically featured a case from the “Clinical Challenges and Images in GI” section of Gastroenterology. However, in this issue we will instead feature a “Practical Teaching Case,” which is one of Gastroenterology’s newest features with a specific focus on the trainee and early-career gastroenterologist. These new cases are great didactic resources and I hope that they become a part of the regular reading of the early career GI community.
If you enjoy the articles in The New Gastroenterologist, have suggestions for future issues, or are interested in contributing to future issues, please let us know! You can contact me ([email protected]) or the Managing Editor of The New Gastroenterologist, Ryan Farrell ([email protected]).
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Bryson W. Katona is a instructor of medicine in the division of gasteroenterology at the University of Pennsylvania.
Dear Colleagues,
Acute pancreatitis has long been one of the “bread and butter” conditions in gastroenterology and having up-to-date knowledge on its management will serve our community well. In this issue of The New Gastroenterologist, Abhishek Gulati and Georgios Papachristou (University of Pittsburgh) provide a comprehensive review of the latest advances in the treatment of acute pancreatitis and its complications, which has direct application to GI clinical practice.
Also included in this issue of The New Gastroenterologist is an article highlighting the importance of diversity in gastroenterology training by Sandra Quezada (University of Maryland) and an article on financial tips to ensure a secure retirement by an experienced contract and tax attorney. Additionally, Peter Liang (New York University), Tatyana Kushner (University of California at San Francisco), and Folasade May (University of California at Los Angeles), who are all members of the AGA Institute Trainee and Early Career Committee, provide an overview of the work that they have done to benefit the early career gastroenterology community and the opportunities that exist for getting involved in related AGA activities.
In prior issues of The New Gastroenterologist, we have typically featured a case from the “Clinical Challenges and Images in GI” section of Gastroenterology. However, in this issue we will instead feature a “Practical Teaching Case,” which is one of Gastroenterology’s newest features with a specific focus on the trainee and early-career gastroenterologist. These new cases are great didactic resources and I hope that they become a part of the regular reading of the early career GI community.
If you enjoy the articles in The New Gastroenterologist, have suggestions for future issues, or are interested in contributing to future issues, please let us know! You can contact me ([email protected]) or the Managing Editor of The New Gastroenterologist, Ryan Farrell ([email protected]).
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Bryson W. Katona is a instructor of medicine in the division of gasteroenterology at the University of Pennsylvania.