User login
Acute Dyspnea: Try Physiologic Approach in Differential Diagnosis
DENVER – If you presume that a patient who comes to the emergency department with acute dyspnea primarily has a pulmonary cause, you’ll almost always be right. Those few other cases, though, take a bit of detective work.
In the approximately 5% of cases in which dyspnea is not easily referable to the lungs, the culprit may be a cardiac problem (usually in a very young child) or, rarely, other problems – hemoglobinopathies, diseases that cause metabolic acidosis, or neurologic disorders, Dr. Jeffrey Sankoff said at the annual meeting of the American College of Emergency Physicians.
Take a physiologic approach that can guide you through the differential diagnosis, he suggested. "As somebody who trained in critical care, everything boils down to physiology," said Dr. Sankoff of the University of Colorado, Denver, and director of quality and patient safety at Denver Health Medical Center.
To begin, think of diseases that cause hypoxemia, hypercapnia, or metabolic acidosis, which lead to dyspnea.
Hypoxemia
The most common cause of hypoxemia is ventilation-perfusion (V-Q) mismatch, in which blood flows in the lungs but areas are not getting oxygen. Diffusion abnormalities, in which oxygen gets into alveoli but oxygen transit to the bloodstream is impaired, also cause hypoxemia. These occur in primary pulmonary disease.
But extrapulmonary disease processes create four causes of hypoxemia: a shunt, low mixed venous oxygen saturation (MVO2), decreased fraction of inspired oxygen (FiO2), and alveolar hypoventilation.
A V-Q mismatch at its most extreme is a shunt, in which blood bypasses the lungs altogether, he said. Disease processes that cause blood to go directly from the right to the left side of circulation result in hypoxemia. A shunt is almost always intracardiac, rarely intrapulmonary.
In children, shunts are seen at characteristic times for the development of cyanotic congenital heart disease, most commonly patent ductus arteriosus in an infant.
Look for a shunt by its hallmark – oxygen saturation will not improve when you give the patient oxygen. "This is the test for any young child under the age of 6 weeks who comes to the emergency department hypoxemic," Dr. Sankoff said.
Adults with shunts will have a murmur as well as dyspnea. "Adults don’t develop shunts de novo. This is going to be happening as part of some acute process," he said. The chest x-rays in adults with shunts often are normal.
The second cause of hypoxia – low MVO2 – occurs mainly when blood flows too slowly through the capillary bed, allowing excess oxygen extraction, and blood returns to the heart in a deoxygenated state. When you see this, focus on right ventricular impairment to identify the etiology. Left ventricular impairment will show up on x-ray as pulmonary edema. A right-sided infarction or cor pulmonale from pulmonary embolism will impair right ventricular function. Cardiac tamponade from infectious, inflammatory, or neoplastic processes also can cause low MVO2 and dyspnea, though nobody really understands why, he added.
The third cause of hypoxia– decreased FiO– usually is a problem relegated to people at high altitudes or industrial workers in enclosed spaces, where hypoxemia (low partial pressure of oxygen in blood) causes hypoxia (low oxygen levels in tissues). But Dr. Sankoff uses this category to remind himself to look for diseases that are not associated with lower FiO2 and hypoxemia but still are associated with hypoxia – primarily hemoglobinopathies.
"If a patient has 100% oxygen saturation yet is hypoxic, they have a problem with hemoglobin," Dr. Sankoff said. It may be a severe or acute garden-variety anemia causing the dyspnea, or occasionally a hereditary hemoglobinopathy such as thalassemia or sickle cell disease. To diagnose these, have a high index of suspicion. You’ll see no patient improvement on oxygen therapy, and some diseases create a characteristic appearance of the blood.
Alveolar hypoventilation may be the most insidious cause of hypoxemia, and dyspnea and may be a flag for impending respiratory compromise if the patient has peripheral weakness. The most common acquired causes of peripheral neuromuscular weakness are Guillain-Barre syndrome, amyotrophic lateral sclerosis, and Colorado tick paralysis.
Make the diagnosis in context with other findings, he said. Expect an abnormal motor exam. Check the negative inspiratory force; if it isn’t at least –20 cm H2O, it’s abnormal and the patient likely will need respiratory support.
Hypercapnia
Diseases that cause hypercapnia can cause dyspnea. Three things cause carbon dioxide levels in the blood to rise: increased metabolic rate (which tends to be seen in the ICU, not in the emergency department), decreased minute ventilation, and increased pulmonary dead space. All can be diagnosed by checking arterial blood gases.
Metabolic Acidosis
Acidosis, usually due to high levels of lactate, stimulates respiratory drive to try and balance pH. Sepsis is the most important cause of acidosis. When sepsis is developing, dyspnea frequently is a subtle sign. Have a high index of suspicion for sepsis, and be wary of a normal oxygen saturation level in a patient with dyspnea, he said. Other causes of metabolic acidosis that lead to dyspnea include diabetic or alcoholic ketoacidosis.
Putting this physiologic approach to dyspnea into context, consider three scenarios, Dr. Sankoff suggested. A patient with dyspnea who responds to oxygen therapy and has an abnormal chest x-ray has a primary pulmonary problem. A patient who responds to oxygen but has a normal chest x-ray may have sepsis, another cause of acidosis, or alveolar hypoventilation; their response to oxygen may be transient. They will respond to oxygen but continue to be tachypneic.
The third scenario – normal x-ray, but the patient does not respond to oxygen therapy – raises a broad differential diagnosis including sepsis, other causes of acidosis, hypercapnia, cardiac causes, and hemoglobinopathies. Narrow the differential by recalling the history and physical findings and getting arterial blood gas tests.
Only after everything else has been excluded should you consider anxiety or pain as the cause of dyspnea, he said.
Dr. Sankoff reported having no financial disclosures.
DENVER – If you presume that a patient who comes to the emergency department with acute dyspnea primarily has a pulmonary cause, you’ll almost always be right. Those few other cases, though, take a bit of detective work.
In the approximately 5% of cases in which dyspnea is not easily referable to the lungs, the culprit may be a cardiac problem (usually in a very young child) or, rarely, other problems – hemoglobinopathies, diseases that cause metabolic acidosis, or neurologic disorders, Dr. Jeffrey Sankoff said at the annual meeting of the American College of Emergency Physicians.
Take a physiologic approach that can guide you through the differential diagnosis, he suggested. "As somebody who trained in critical care, everything boils down to physiology," said Dr. Sankoff of the University of Colorado, Denver, and director of quality and patient safety at Denver Health Medical Center.
To begin, think of diseases that cause hypoxemia, hypercapnia, or metabolic acidosis, which lead to dyspnea.
Hypoxemia
The most common cause of hypoxemia is ventilation-perfusion (V-Q) mismatch, in which blood flows in the lungs but areas are not getting oxygen. Diffusion abnormalities, in which oxygen gets into alveoli but oxygen transit to the bloodstream is impaired, also cause hypoxemia. These occur in primary pulmonary disease.
But extrapulmonary disease processes create four causes of hypoxemia: a shunt, low mixed venous oxygen saturation (MVO2), decreased fraction of inspired oxygen (FiO2), and alveolar hypoventilation.
A V-Q mismatch at its most extreme is a shunt, in which blood bypasses the lungs altogether, he said. Disease processes that cause blood to go directly from the right to the left side of circulation result in hypoxemia. A shunt is almost always intracardiac, rarely intrapulmonary.
In children, shunts are seen at characteristic times for the development of cyanotic congenital heart disease, most commonly patent ductus arteriosus in an infant.
Look for a shunt by its hallmark – oxygen saturation will not improve when you give the patient oxygen. "This is the test for any young child under the age of 6 weeks who comes to the emergency department hypoxemic," Dr. Sankoff said.
Adults with shunts will have a murmur as well as dyspnea. "Adults don’t develop shunts de novo. This is going to be happening as part of some acute process," he said. The chest x-rays in adults with shunts often are normal.
The second cause of hypoxia – low MVO2 – occurs mainly when blood flows too slowly through the capillary bed, allowing excess oxygen extraction, and blood returns to the heart in a deoxygenated state. When you see this, focus on right ventricular impairment to identify the etiology. Left ventricular impairment will show up on x-ray as pulmonary edema. A right-sided infarction or cor pulmonale from pulmonary embolism will impair right ventricular function. Cardiac tamponade from infectious, inflammatory, or neoplastic processes also can cause low MVO2 and dyspnea, though nobody really understands why, he added.
The third cause of hypoxia– decreased FiO– usually is a problem relegated to people at high altitudes or industrial workers in enclosed spaces, where hypoxemia (low partial pressure of oxygen in blood) causes hypoxia (low oxygen levels in tissues). But Dr. Sankoff uses this category to remind himself to look for diseases that are not associated with lower FiO2 and hypoxemia but still are associated with hypoxia – primarily hemoglobinopathies.
"If a patient has 100% oxygen saturation yet is hypoxic, they have a problem with hemoglobin," Dr. Sankoff said. It may be a severe or acute garden-variety anemia causing the dyspnea, or occasionally a hereditary hemoglobinopathy such as thalassemia or sickle cell disease. To diagnose these, have a high index of suspicion. You’ll see no patient improvement on oxygen therapy, and some diseases create a characteristic appearance of the blood.
Alveolar hypoventilation may be the most insidious cause of hypoxemia, and dyspnea and may be a flag for impending respiratory compromise if the patient has peripheral weakness. The most common acquired causes of peripheral neuromuscular weakness are Guillain-Barre syndrome, amyotrophic lateral sclerosis, and Colorado tick paralysis.
Make the diagnosis in context with other findings, he said. Expect an abnormal motor exam. Check the negative inspiratory force; if it isn’t at least –20 cm H2O, it’s abnormal and the patient likely will need respiratory support.
Hypercapnia
Diseases that cause hypercapnia can cause dyspnea. Three things cause carbon dioxide levels in the blood to rise: increased metabolic rate (which tends to be seen in the ICU, not in the emergency department), decreased minute ventilation, and increased pulmonary dead space. All can be diagnosed by checking arterial blood gases.
Metabolic Acidosis
Acidosis, usually due to high levels of lactate, stimulates respiratory drive to try and balance pH. Sepsis is the most important cause of acidosis. When sepsis is developing, dyspnea frequently is a subtle sign. Have a high index of suspicion for sepsis, and be wary of a normal oxygen saturation level in a patient with dyspnea, he said. Other causes of metabolic acidosis that lead to dyspnea include diabetic or alcoholic ketoacidosis.
Putting this physiologic approach to dyspnea into context, consider three scenarios, Dr. Sankoff suggested. A patient with dyspnea who responds to oxygen therapy and has an abnormal chest x-ray has a primary pulmonary problem. A patient who responds to oxygen but has a normal chest x-ray may have sepsis, another cause of acidosis, or alveolar hypoventilation; their response to oxygen may be transient. They will respond to oxygen but continue to be tachypneic.
The third scenario – normal x-ray, but the patient does not respond to oxygen therapy – raises a broad differential diagnosis including sepsis, other causes of acidosis, hypercapnia, cardiac causes, and hemoglobinopathies. Narrow the differential by recalling the history and physical findings and getting arterial blood gas tests.
Only after everything else has been excluded should you consider anxiety or pain as the cause of dyspnea, he said.
Dr. Sankoff reported having no financial disclosures.
DENVER – If you presume that a patient who comes to the emergency department with acute dyspnea primarily has a pulmonary cause, you’ll almost always be right. Those few other cases, though, take a bit of detective work.
In the approximately 5% of cases in which dyspnea is not easily referable to the lungs, the culprit may be a cardiac problem (usually in a very young child) or, rarely, other problems – hemoglobinopathies, diseases that cause metabolic acidosis, or neurologic disorders, Dr. Jeffrey Sankoff said at the annual meeting of the American College of Emergency Physicians.
Take a physiologic approach that can guide you through the differential diagnosis, he suggested. "As somebody who trained in critical care, everything boils down to physiology," said Dr. Sankoff of the University of Colorado, Denver, and director of quality and patient safety at Denver Health Medical Center.
To begin, think of diseases that cause hypoxemia, hypercapnia, or metabolic acidosis, which lead to dyspnea.
Hypoxemia
The most common cause of hypoxemia is ventilation-perfusion (V-Q) mismatch, in which blood flows in the lungs but areas are not getting oxygen. Diffusion abnormalities, in which oxygen gets into alveoli but oxygen transit to the bloodstream is impaired, also cause hypoxemia. These occur in primary pulmonary disease.
But extrapulmonary disease processes create four causes of hypoxemia: a shunt, low mixed venous oxygen saturation (MVO2), decreased fraction of inspired oxygen (FiO2), and alveolar hypoventilation.
A V-Q mismatch at its most extreme is a shunt, in which blood bypasses the lungs altogether, he said. Disease processes that cause blood to go directly from the right to the left side of circulation result in hypoxemia. A shunt is almost always intracardiac, rarely intrapulmonary.
In children, shunts are seen at characteristic times for the development of cyanotic congenital heart disease, most commonly patent ductus arteriosus in an infant.
Look for a shunt by its hallmark – oxygen saturation will not improve when you give the patient oxygen. "This is the test for any young child under the age of 6 weeks who comes to the emergency department hypoxemic," Dr. Sankoff said.
Adults with shunts will have a murmur as well as dyspnea. "Adults don’t develop shunts de novo. This is going to be happening as part of some acute process," he said. The chest x-rays in adults with shunts often are normal.
The second cause of hypoxia – low MVO2 – occurs mainly when blood flows too slowly through the capillary bed, allowing excess oxygen extraction, and blood returns to the heart in a deoxygenated state. When you see this, focus on right ventricular impairment to identify the etiology. Left ventricular impairment will show up on x-ray as pulmonary edema. A right-sided infarction or cor pulmonale from pulmonary embolism will impair right ventricular function. Cardiac tamponade from infectious, inflammatory, or neoplastic processes also can cause low MVO2 and dyspnea, though nobody really understands why, he added.
The third cause of hypoxia– decreased FiO– usually is a problem relegated to people at high altitudes or industrial workers in enclosed spaces, where hypoxemia (low partial pressure of oxygen in blood) causes hypoxia (low oxygen levels in tissues). But Dr. Sankoff uses this category to remind himself to look for diseases that are not associated with lower FiO2 and hypoxemia but still are associated with hypoxia – primarily hemoglobinopathies.
"If a patient has 100% oxygen saturation yet is hypoxic, they have a problem with hemoglobin," Dr. Sankoff said. It may be a severe or acute garden-variety anemia causing the dyspnea, or occasionally a hereditary hemoglobinopathy such as thalassemia or sickle cell disease. To diagnose these, have a high index of suspicion. You’ll see no patient improvement on oxygen therapy, and some diseases create a characteristic appearance of the blood.
Alveolar hypoventilation may be the most insidious cause of hypoxemia, and dyspnea and may be a flag for impending respiratory compromise if the patient has peripheral weakness. The most common acquired causes of peripheral neuromuscular weakness are Guillain-Barre syndrome, amyotrophic lateral sclerosis, and Colorado tick paralysis.
Make the diagnosis in context with other findings, he said. Expect an abnormal motor exam. Check the negative inspiratory force; if it isn’t at least –20 cm H2O, it’s abnormal and the patient likely will need respiratory support.
Hypercapnia
Diseases that cause hypercapnia can cause dyspnea. Three things cause carbon dioxide levels in the blood to rise: increased metabolic rate (which tends to be seen in the ICU, not in the emergency department), decreased minute ventilation, and increased pulmonary dead space. All can be diagnosed by checking arterial blood gases.
Metabolic Acidosis
Acidosis, usually due to high levels of lactate, stimulates respiratory drive to try and balance pH. Sepsis is the most important cause of acidosis. When sepsis is developing, dyspnea frequently is a subtle sign. Have a high index of suspicion for sepsis, and be wary of a normal oxygen saturation level in a patient with dyspnea, he said. Other causes of metabolic acidosis that lead to dyspnea include diabetic or alcoholic ketoacidosis.
Putting this physiologic approach to dyspnea into context, consider three scenarios, Dr. Sankoff suggested. A patient with dyspnea who responds to oxygen therapy and has an abnormal chest x-ray has a primary pulmonary problem. A patient who responds to oxygen but has a normal chest x-ray may have sepsis, another cause of acidosis, or alveolar hypoventilation; their response to oxygen may be transient. They will respond to oxygen but continue to be tachypneic.
The third scenario – normal x-ray, but the patient does not respond to oxygen therapy – raises a broad differential diagnosis including sepsis, other causes of acidosis, hypercapnia, cardiac causes, and hemoglobinopathies. Narrow the differential by recalling the history and physical findings and getting arterial blood gas tests.
Only after everything else has been excluded should you consider anxiety or pain as the cause of dyspnea, he said.
Dr. Sankoff reported having no financial disclosures.
EXPERT ANALYSIS AT THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF EMERGENCY PHYSICIANS
Earlier End-of-Life Talks Deter Aggressive Care of Terminal Cancer Patients
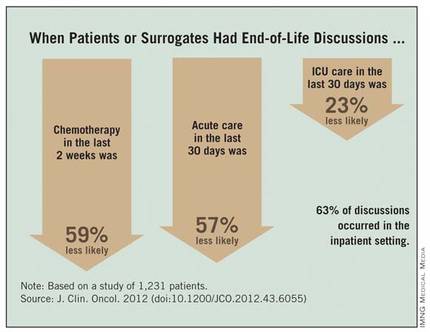
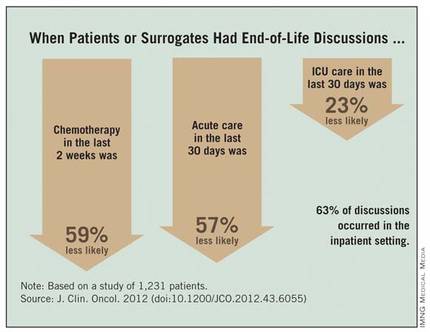
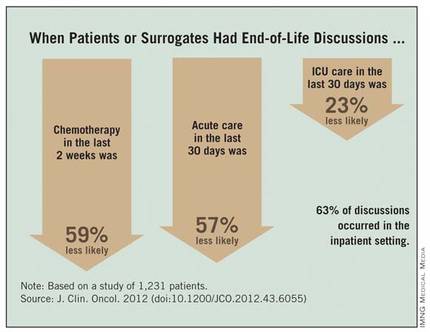
Patients with stage IV lung or colorectal cancer who had end-of-life discussions with caregivers before the last 30 days of life were significantly less likely to receive aggressive care in their final days and more likely to get hospice care and to enter hospice earlier, a study of 1,231 patients found.
Nearly half received some kind of aggressive care in their last 30 days (47%), including chemotherapy in the last 14 days (16%), ICU care in the last 30 days (6%), and/or acute hospital-based care in the last 30 days of life (40%), Dr. Jennifer W. Mack and her associates reported.
Multiple current guidelines recommend starting end-of-life care planning for patients with incurable cancer early in the course of the disease while patients are relatively stable, not when they are acutely deteriorating.
Many physicians in the study postponed the discussion until the final month of life, and many patients didn’t remember or didn’t recognize the end-of-life discussions. Discussions that were documented in charts were not associated with less-aggressive care or greater hospice use, if patients or their surrogates said no end-of-life discussions took place.
Eighty-eight percent of patients in the current study had end-of-life discussions. Twenty-three percent of the discussion were reported by patients or their surrogates in interviews but not documented in records, 17% were documented in medical records but not reported by patients or surrogates, and 48% were both reported and documented.
Among the 794 patients with end-of-life discussions documented in medical records, 39% took place in the last 30 days of life, 63% happened in the inpatient setting, and 40% included an oncologist. Fifty-eight percent of patients entered hospice care, which started in the last 7 days of life for 15% of them, reported Dr. Mack, a pediatric oncologist at the Dana-Farber Cancer Institute and Harvard Medical School, Boston.
The study was published online Nov. 13, 2012 by the Journal of Clinical Oncology (doi:10.1200/JCO.2012.43.6055).
Chemotherapy in the last 2 weeks of life was 59% less likely, acute care in the last 30 days was 57% less likely, and ICU care in the last 30 days was 23% less likely when patients or surrogates reported having end-of-life discussions.
Patients Followed 15 Months After Diagnosis
Patients whose first end-of-life discussion happened while they were hospitalized were more than twice as likely to get any kind of aggressive care at the end of life and three times more likely to get acute care or ICU care in the last 30 days and to have hospice care start within the last week before death.
Having a medical oncologist present at the first end-of-life discussion increased the odds of having chemotherapy in the last 2 weeks of life by 48%, decreased the odds of ICU care in the last 30 days by 56%, increased the likelihood of hospice care by 43%, and doubled the chance of hospice care starting in the last 7 days of life. All of these odds ratios were significant after controlling for other factors.
Data came from a larger cohort of 2,155 patients with stage IV lung or colorectal cancer receiving care in HMOs or Veterans Affairs medical centers in five states. All were followed for 15 months after diagnosis in the Cancer Care Outcomes Research and Surveillance Consortium.
An earlier analysis by the same investigators showed that 87% of the 1,470 patients who died and 41% of the 685 still alive by the end of follow-up had end-of-life care discussions, but oncologists documented end-of-life discussions with only 27% of their patients, suggesting that most discussions were with non-oncologists. Among those who died, documented discussions took place a median of 33 days before death (Ann. Intern. Med. 2012;156:204-10).
"Our previous study on this database found that most physicians do have end-of-life discussions before death, but most occur near the end of life," Dr. Mack said in an interview.
The current study analyzed data for 1,231 of the patients who died but who lived at least 1 month after diagnosis, in order to assess whether the timing of discussions influenced end-of-life care. "Besides the fact that that seems like logical practice, there really wasn’t a clear evidence base that that affects care," she said.
Patients were significantly less likely to say they’d had an end-of-life discussion if they were unmarried, black or non-white Hispanic, or not in an HMO.
Start Talks Closer to Diagnosis
When discussions don’t begin until the last 30 days of life, the end-of-life period usually is already underway, the investigators noted. Physicians should consider moving end-of-life care discussions closer to diagnosis, they suggested, while patients are relatively well and have time to plan for what’s ahead.
"It’s something that any physician can do," but some previous studies report that physicians are reluctant to start end-of-life discussions early because these are emotionally difficult conversations, they worry about taking away hope, and they are concerned about the psychological impact on patients – though there is no clear evidence that it does have psychological consequences for patients, Dr. Mack said.
"It’s a compassionate instinct," she said. "Being in the room with a family when I deliver this kind of news, that emotional impact is right in front of me. I believe there are bigger consequences" from not discussing end-of-life care, such as perpetuating false hopes and asking people to make decisions about what’s ahead without a clear picture of the situation, she added.
The conversation should take place more than once because patient preferences may change over time and patients need time to process the information and their thoughts about it, Dr. Mack said.
Ask Patients What They Hear
Further work is needed on why some documented end-of-life discussions were not reported by patients/surrogates. "Every physician can relate to this, that sometimes we have conversations but they’re not heard or understood by patients," she said. "It reminds me that I need to ask patients what they’re taking away from these conversations and use that to guide me going forward."
That finding echoes two recent large, population-based studies that found many patients with terminal cancer mistakenly think that palliative chemotherapy or radiation will cure their disease.
Some previous studies suggest that patients dying of cancer increasingly are receiving aggressive care at the end of life and that this trend may be modifiable. Cross-sectional studies that assessed one point in time between diagnosis and death have shown that many patients don’t have end-of-life discussions, but these studies probably missed discussions closer to death, Dr. Mack noted.
Other studies have reported an association between having end-of-life discussions and reduced intensity in care. The current study was longitudinal and is one of the first to look at the effects of the timing of these discussions and other factors.
Most patients who realize that they are dying do not want aggressive care, previous studies have shown. Other studies report that less-aggressive end-of-life care is easier on family members and less expensive.
Guidelines from the National Comprehensive Cancer Network, the National Consensus Project for Quality Palliative Care, the American Society of Clinical Oncology, and the American College of Physicians and American Society of Internal Medicine recommend beginning end-of-life discussions early for patients with incurable cancer.
When investigators conducted secondary analyses that excluded patients from Veterans Affairs sites or excluded interviews with patient surrogates, the findings were similar to results of the main analysis.
In the current analysis, 82% of patients had lung cancer, and the rest had colorectal cancer.
Future research on this topic could take many paths, Dr. Mack suggested, including implementing routine early discussions and seeing whether that alters the intensity of final care. Much more could be learned about the quality of discussions between physicians and patients. The current study had no data on discussions led by nurses or social workers or that took place among family members without a medical provider present.
"We’re also interested in looking at a longer trajectory of end-of-life decision making" for patients with incurable cancer – from diagnosis to death, she said.
Dr. Mack and her associates reported having no financial disclosures.
This is an important study that documents the fact that early discussions about end-of-life care for patients with stage IV cancer are associated with decreased intensity of care at the end of life, and that the timing of the initiation of these discussions is very important and should happen earlier than it does much of the time.
This is not the first study to show that this communication is associated with decreased intensity of care (JAMA 2008;300:1665-73). However, this is an important study because it is the first to document that early discussions are important (prior to the last 30 days of life).

|
|
Moving end-of-life discussions closer to diagnosis definitely is realistic and the way this should occur. However, it is not an "either-or" situation. Early discussions don’t mean that later discussions aren’t necessary and important. Early discussions set the frame and make it easier to have later discussions if/when patients get worse.
There is a need for physicians to improve communication to make sure patients or their surrogates understand end-of-life discussions. Our challenge now is to find successful ways to teach these communication skills to physicians and help physicians implement these discussions in clinical practice. It is not useful to tell physicians to have these discussions if they haven’t been trained to do it well, and we don’t create systems that make it practical and feasible.
When the Obama administration tried to implement a policy of paying physicians to conduct advance care planning on an annual basis through Medicare, Sarah Palin and others used the "death panel" scare tactics to defeat this important effort. We need to change the public discussion to be more aware of the importance of early and regular discussions about advance care planning.
We also need research to figure out how best to implement "earlier discussions" in clinical practice and to identify the long-term consequences of such a practice.
Dr. J. Randall Curtis is director of the University of Washington Palliative Care Center of Excellence and head of Pulmonary and Critical Care Medicine at Harborview Medical Center, Seattle. He provided these comments in an interview. Dr. Curtis reported having no financial disclosures.
This is an important study that documents the fact that early discussions about end-of-life care for patients with stage IV cancer are associated with decreased intensity of care at the end of life, and that the timing of the initiation of these discussions is very important and should happen earlier than it does much of the time.
This is not the first study to show that this communication is associated with decreased intensity of care (JAMA 2008;300:1665-73). However, this is an important study because it is the first to document that early discussions are important (prior to the last 30 days of life).

|
|
Moving end-of-life discussions closer to diagnosis definitely is realistic and the way this should occur. However, it is not an "either-or" situation. Early discussions don’t mean that later discussions aren’t necessary and important. Early discussions set the frame and make it easier to have later discussions if/when patients get worse.
There is a need for physicians to improve communication to make sure patients or their surrogates understand end-of-life discussions. Our challenge now is to find successful ways to teach these communication skills to physicians and help physicians implement these discussions in clinical practice. It is not useful to tell physicians to have these discussions if they haven’t been trained to do it well, and we don’t create systems that make it practical and feasible.
When the Obama administration tried to implement a policy of paying physicians to conduct advance care planning on an annual basis through Medicare, Sarah Palin and others used the "death panel" scare tactics to defeat this important effort. We need to change the public discussion to be more aware of the importance of early and regular discussions about advance care planning.
We also need research to figure out how best to implement "earlier discussions" in clinical practice and to identify the long-term consequences of such a practice.
Dr. J. Randall Curtis is director of the University of Washington Palliative Care Center of Excellence and head of Pulmonary and Critical Care Medicine at Harborview Medical Center, Seattle. He provided these comments in an interview. Dr. Curtis reported having no financial disclosures.
This is an important study that documents the fact that early discussions about end-of-life care for patients with stage IV cancer are associated with decreased intensity of care at the end of life, and that the timing of the initiation of these discussions is very important and should happen earlier than it does much of the time.
This is not the first study to show that this communication is associated with decreased intensity of care (JAMA 2008;300:1665-73). However, this is an important study because it is the first to document that early discussions are important (prior to the last 30 days of life).

|
|
Moving end-of-life discussions closer to diagnosis definitely is realistic and the way this should occur. However, it is not an "either-or" situation. Early discussions don’t mean that later discussions aren’t necessary and important. Early discussions set the frame and make it easier to have later discussions if/when patients get worse.
There is a need for physicians to improve communication to make sure patients or their surrogates understand end-of-life discussions. Our challenge now is to find successful ways to teach these communication skills to physicians and help physicians implement these discussions in clinical practice. It is not useful to tell physicians to have these discussions if they haven’t been trained to do it well, and we don’t create systems that make it practical and feasible.
When the Obama administration tried to implement a policy of paying physicians to conduct advance care planning on an annual basis through Medicare, Sarah Palin and others used the "death panel" scare tactics to defeat this important effort. We need to change the public discussion to be more aware of the importance of early and regular discussions about advance care planning.
We also need research to figure out how best to implement "earlier discussions" in clinical practice and to identify the long-term consequences of such a practice.
Dr. J. Randall Curtis is director of the University of Washington Palliative Care Center of Excellence and head of Pulmonary and Critical Care Medicine at Harborview Medical Center, Seattle. He provided these comments in an interview. Dr. Curtis reported having no financial disclosures.
Patients with stage IV lung or colorectal cancer who had end-of-life discussions with caregivers before the last 30 days of life were significantly less likely to receive aggressive care in their final days and more likely to get hospice care and to enter hospice earlier, a study of 1,231 patients found.
Nearly half received some kind of aggressive care in their last 30 days (47%), including chemotherapy in the last 14 days (16%), ICU care in the last 30 days (6%), and/or acute hospital-based care in the last 30 days of life (40%), Dr. Jennifer W. Mack and her associates reported.
Multiple current guidelines recommend starting end-of-life care planning for patients with incurable cancer early in the course of the disease while patients are relatively stable, not when they are acutely deteriorating.
Many physicians in the study postponed the discussion until the final month of life, and many patients didn’t remember or didn’t recognize the end-of-life discussions. Discussions that were documented in charts were not associated with less-aggressive care or greater hospice use, if patients or their surrogates said no end-of-life discussions took place.
Eighty-eight percent of patients in the current study had end-of-life discussions. Twenty-three percent of the discussion were reported by patients or their surrogates in interviews but not documented in records, 17% were documented in medical records but not reported by patients or surrogates, and 48% were both reported and documented.
Among the 794 patients with end-of-life discussions documented in medical records, 39% took place in the last 30 days of life, 63% happened in the inpatient setting, and 40% included an oncologist. Fifty-eight percent of patients entered hospice care, which started in the last 7 days of life for 15% of them, reported Dr. Mack, a pediatric oncologist at the Dana-Farber Cancer Institute and Harvard Medical School, Boston.
The study was published online Nov. 13, 2012 by the Journal of Clinical Oncology (doi:10.1200/JCO.2012.43.6055).
Chemotherapy in the last 2 weeks of life was 59% less likely, acute care in the last 30 days was 57% less likely, and ICU care in the last 30 days was 23% less likely when patients or surrogates reported having end-of-life discussions.
Patients Followed 15 Months After Diagnosis
Patients whose first end-of-life discussion happened while they were hospitalized were more than twice as likely to get any kind of aggressive care at the end of life and three times more likely to get acute care or ICU care in the last 30 days and to have hospice care start within the last week before death.
Having a medical oncologist present at the first end-of-life discussion increased the odds of having chemotherapy in the last 2 weeks of life by 48%, decreased the odds of ICU care in the last 30 days by 56%, increased the likelihood of hospice care by 43%, and doubled the chance of hospice care starting in the last 7 days of life. All of these odds ratios were significant after controlling for other factors.
Data came from a larger cohort of 2,155 patients with stage IV lung or colorectal cancer receiving care in HMOs or Veterans Affairs medical centers in five states. All were followed for 15 months after diagnosis in the Cancer Care Outcomes Research and Surveillance Consortium.
An earlier analysis by the same investigators showed that 87% of the 1,470 patients who died and 41% of the 685 still alive by the end of follow-up had end-of-life care discussions, but oncologists documented end-of-life discussions with only 27% of their patients, suggesting that most discussions were with non-oncologists. Among those who died, documented discussions took place a median of 33 days before death (Ann. Intern. Med. 2012;156:204-10).
"Our previous study on this database found that most physicians do have end-of-life discussions before death, but most occur near the end of life," Dr. Mack said in an interview.
The current study analyzed data for 1,231 of the patients who died but who lived at least 1 month after diagnosis, in order to assess whether the timing of discussions influenced end-of-life care. "Besides the fact that that seems like logical practice, there really wasn’t a clear evidence base that that affects care," she said.
Patients were significantly less likely to say they’d had an end-of-life discussion if they were unmarried, black or non-white Hispanic, or not in an HMO.
Start Talks Closer to Diagnosis
When discussions don’t begin until the last 30 days of life, the end-of-life period usually is already underway, the investigators noted. Physicians should consider moving end-of-life care discussions closer to diagnosis, they suggested, while patients are relatively well and have time to plan for what’s ahead.
"It’s something that any physician can do," but some previous studies report that physicians are reluctant to start end-of-life discussions early because these are emotionally difficult conversations, they worry about taking away hope, and they are concerned about the psychological impact on patients – though there is no clear evidence that it does have psychological consequences for patients, Dr. Mack said.
"It’s a compassionate instinct," she said. "Being in the room with a family when I deliver this kind of news, that emotional impact is right in front of me. I believe there are bigger consequences" from not discussing end-of-life care, such as perpetuating false hopes and asking people to make decisions about what’s ahead without a clear picture of the situation, she added.
The conversation should take place more than once because patient preferences may change over time and patients need time to process the information and their thoughts about it, Dr. Mack said.
Ask Patients What They Hear
Further work is needed on why some documented end-of-life discussions were not reported by patients/surrogates. "Every physician can relate to this, that sometimes we have conversations but they’re not heard or understood by patients," she said. "It reminds me that I need to ask patients what they’re taking away from these conversations and use that to guide me going forward."
That finding echoes two recent large, population-based studies that found many patients with terminal cancer mistakenly think that palliative chemotherapy or radiation will cure their disease.
Some previous studies suggest that patients dying of cancer increasingly are receiving aggressive care at the end of life and that this trend may be modifiable. Cross-sectional studies that assessed one point in time between diagnosis and death have shown that many patients don’t have end-of-life discussions, but these studies probably missed discussions closer to death, Dr. Mack noted.
Other studies have reported an association between having end-of-life discussions and reduced intensity in care. The current study was longitudinal and is one of the first to look at the effects of the timing of these discussions and other factors.
Most patients who realize that they are dying do not want aggressive care, previous studies have shown. Other studies report that less-aggressive end-of-life care is easier on family members and less expensive.
Guidelines from the National Comprehensive Cancer Network, the National Consensus Project for Quality Palliative Care, the American Society of Clinical Oncology, and the American College of Physicians and American Society of Internal Medicine recommend beginning end-of-life discussions early for patients with incurable cancer.
When investigators conducted secondary analyses that excluded patients from Veterans Affairs sites or excluded interviews with patient surrogates, the findings were similar to results of the main analysis.
In the current analysis, 82% of patients had lung cancer, and the rest had colorectal cancer.
Future research on this topic could take many paths, Dr. Mack suggested, including implementing routine early discussions and seeing whether that alters the intensity of final care. Much more could be learned about the quality of discussions between physicians and patients. The current study had no data on discussions led by nurses or social workers or that took place among family members without a medical provider present.
"We’re also interested in looking at a longer trajectory of end-of-life decision making" for patients with incurable cancer – from diagnosis to death, she said.
Dr. Mack and her associates reported having no financial disclosures.
Patients with stage IV lung or colorectal cancer who had end-of-life discussions with caregivers before the last 30 days of life were significantly less likely to receive aggressive care in their final days and more likely to get hospice care and to enter hospice earlier, a study of 1,231 patients found.
Nearly half received some kind of aggressive care in their last 30 days (47%), including chemotherapy in the last 14 days (16%), ICU care in the last 30 days (6%), and/or acute hospital-based care in the last 30 days of life (40%), Dr. Jennifer W. Mack and her associates reported.
Multiple current guidelines recommend starting end-of-life care planning for patients with incurable cancer early in the course of the disease while patients are relatively stable, not when they are acutely deteriorating.
Many physicians in the study postponed the discussion until the final month of life, and many patients didn’t remember or didn’t recognize the end-of-life discussions. Discussions that were documented in charts were not associated with less-aggressive care or greater hospice use, if patients or their surrogates said no end-of-life discussions took place.
Eighty-eight percent of patients in the current study had end-of-life discussions. Twenty-three percent of the discussion were reported by patients or their surrogates in interviews but not documented in records, 17% were documented in medical records but not reported by patients or surrogates, and 48% were both reported and documented.
Among the 794 patients with end-of-life discussions documented in medical records, 39% took place in the last 30 days of life, 63% happened in the inpatient setting, and 40% included an oncologist. Fifty-eight percent of patients entered hospice care, which started in the last 7 days of life for 15% of them, reported Dr. Mack, a pediatric oncologist at the Dana-Farber Cancer Institute and Harvard Medical School, Boston.
The study was published online Nov. 13, 2012 by the Journal of Clinical Oncology (doi:10.1200/JCO.2012.43.6055).
Chemotherapy in the last 2 weeks of life was 59% less likely, acute care in the last 30 days was 57% less likely, and ICU care in the last 30 days was 23% less likely when patients or surrogates reported having end-of-life discussions.
Patients Followed 15 Months After Diagnosis
Patients whose first end-of-life discussion happened while they were hospitalized were more than twice as likely to get any kind of aggressive care at the end of life and three times more likely to get acute care or ICU care in the last 30 days and to have hospice care start within the last week before death.
Having a medical oncologist present at the first end-of-life discussion increased the odds of having chemotherapy in the last 2 weeks of life by 48%, decreased the odds of ICU care in the last 30 days by 56%, increased the likelihood of hospice care by 43%, and doubled the chance of hospice care starting in the last 7 days of life. All of these odds ratios were significant after controlling for other factors.
Data came from a larger cohort of 2,155 patients with stage IV lung or colorectal cancer receiving care in HMOs or Veterans Affairs medical centers in five states. All were followed for 15 months after diagnosis in the Cancer Care Outcomes Research and Surveillance Consortium.
An earlier analysis by the same investigators showed that 87% of the 1,470 patients who died and 41% of the 685 still alive by the end of follow-up had end-of-life care discussions, but oncologists documented end-of-life discussions with only 27% of their patients, suggesting that most discussions were with non-oncologists. Among those who died, documented discussions took place a median of 33 days before death (Ann. Intern. Med. 2012;156:204-10).
"Our previous study on this database found that most physicians do have end-of-life discussions before death, but most occur near the end of life," Dr. Mack said in an interview.
The current study analyzed data for 1,231 of the patients who died but who lived at least 1 month after diagnosis, in order to assess whether the timing of discussions influenced end-of-life care. "Besides the fact that that seems like logical practice, there really wasn’t a clear evidence base that that affects care," she said.
Patients were significantly less likely to say they’d had an end-of-life discussion if they were unmarried, black or non-white Hispanic, or not in an HMO.
Start Talks Closer to Diagnosis
When discussions don’t begin until the last 30 days of life, the end-of-life period usually is already underway, the investigators noted. Physicians should consider moving end-of-life care discussions closer to diagnosis, they suggested, while patients are relatively well and have time to plan for what’s ahead.
"It’s something that any physician can do," but some previous studies report that physicians are reluctant to start end-of-life discussions early because these are emotionally difficult conversations, they worry about taking away hope, and they are concerned about the psychological impact on patients – though there is no clear evidence that it does have psychological consequences for patients, Dr. Mack said.
"It’s a compassionate instinct," she said. "Being in the room with a family when I deliver this kind of news, that emotional impact is right in front of me. I believe there are bigger consequences" from not discussing end-of-life care, such as perpetuating false hopes and asking people to make decisions about what’s ahead without a clear picture of the situation, she added.
The conversation should take place more than once because patient preferences may change over time and patients need time to process the information and their thoughts about it, Dr. Mack said.
Ask Patients What They Hear
Further work is needed on why some documented end-of-life discussions were not reported by patients/surrogates. "Every physician can relate to this, that sometimes we have conversations but they’re not heard or understood by patients," she said. "It reminds me that I need to ask patients what they’re taking away from these conversations and use that to guide me going forward."
That finding echoes two recent large, population-based studies that found many patients with terminal cancer mistakenly think that palliative chemotherapy or radiation will cure their disease.
Some previous studies suggest that patients dying of cancer increasingly are receiving aggressive care at the end of life and that this trend may be modifiable. Cross-sectional studies that assessed one point in time between diagnosis and death have shown that many patients don’t have end-of-life discussions, but these studies probably missed discussions closer to death, Dr. Mack noted.
Other studies have reported an association between having end-of-life discussions and reduced intensity in care. The current study was longitudinal and is one of the first to look at the effects of the timing of these discussions and other factors.
Most patients who realize that they are dying do not want aggressive care, previous studies have shown. Other studies report that less-aggressive end-of-life care is easier on family members and less expensive.
Guidelines from the National Comprehensive Cancer Network, the National Consensus Project for Quality Palliative Care, the American Society of Clinical Oncology, and the American College of Physicians and American Society of Internal Medicine recommend beginning end-of-life discussions early for patients with incurable cancer.
When investigators conducted secondary analyses that excluded patients from Veterans Affairs sites or excluded interviews with patient surrogates, the findings were similar to results of the main analysis.
In the current analysis, 82% of patients had lung cancer, and the rest had colorectal cancer.
Future research on this topic could take many paths, Dr. Mack suggested, including implementing routine early discussions and seeing whether that alters the intensity of final care. Much more could be learned about the quality of discussions between physicians and patients. The current study had no data on discussions led by nurses or social workers or that took place among family members without a medical provider present.
"We’re also interested in looking at a longer trajectory of end-of-life decision making" for patients with incurable cancer – from diagnosis to death, she said.
Dr. Mack and her associates reported having no financial disclosures.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Major Finding: Chemotherapy in the last 2 weeks of life was 59% less likely, acute care in the last 30 days was 57% less likely, and ICU care in the last 30 days was 23% less likely when patients or their surrogates reported having end-of-life discussions.
Data Source: This was a longitudinal study of 1,231 patients with stage IV lung or colorectal cancer at HMOs or Veterans Affairs sites in five states.
Disclosures: Dr. Mack and her associates reported having no financial disclosures.
Pediatric Psychiatry Services Infiltrate Primary Care
SAN FRANCISCO – After more than 2 decades as a primary care pediatrician, Dr. Teresa M. Hargrave was so frustrated by the lack of psychiatric services for her patients that she retrained as a child and adolescent psychiatrist. Now, she’s part of a New York state program that spreads her psychiatric skills to more patients than she imagined could be possible.
"If this program had been in place when I was a pediatrician, I would never have had to switch," said Dr. Hargrave of the State University of New York (SUNY) in Syracuse.
Today, New York primary care physicians can call 855-227-7272 toll free on weekdays for an immediate consultation with a master’s level therapist in the Child and Adolescent Psychiatry for Primary Care program (CAP PC). If a patient seems to need psychotropic medication, the therapist connects the pediatrician with a psychiatrist on the program’s team, such as Dr. Hargrave, who helps the primary care physician manage treatment through phone consultations and, if needed, in-person assessments.
Dozens of similar efforts – in a variety of formats – have sprung up across the country. They’re all trying to address a fundamental mismatch: There are only 7,400 practicing child and adolescent psychiatrists in the United States but more than 15 million young people in those age groups who need psychiatric care, according to data analyses from the American Academy of Child and Adolescent Psychiatry.
The National Network of Child Psychiatry Access Programs acts as a hub for these programs in 24 states, with programs in 4 more states set to take their first calls soon.
These model programs are making great inroads in getting care to the estimated 15%-25% of children seen in primary care offices who have behavioral health disorders, but reimbursement problems create a roadblock that must be overcome in the years ahead for the programs to be fully effective, several experts said in interviews at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
New York Program
New York’s CAP PC program modeled itself after one of the first state-wide programs, the Massachusetts Child Psychiatry Access Project, with some key changes. The CAP PC program covers 95% of the New York state population but uses the same toll-free number everywhere, compared with multiple different phone numbers being used in different regions in Massachusetts. New York’s program also added an educational component for primary care physicians – a free 15-hour "Mini-Fellowship" weekend program followed by a dozen 1-hour biweekly case-based conference calls.
Primary care physicians seem to love the help, Dr. David Kaye said at a poster presentation at the meeting. In its 2 years of operation, the CAP PC program has registered 829 primary care physicians (80% pediatricians, 20% family physicians), 292 of whom took the training sessions. The program handled 1,016 intake and follow-up calls, provided 993 consultations with a psychiatrist, conducted 94 face-to-face evaluations, and referred 305 patients to other services, reported Dr. Kaye, professor of psychiatry and director of child and adolescent psychiatry training at SUNY in Buffalo, N.Y.
Among 325 primary care physicians surveyed 2 weeks after contact with the CAP PC program, 94% said the consultations were very or extremely helpful, and 99% said they would recommend the program to other primary care physicians.
The program has greatly increased the number of children accessing psychiatric services compared with a previous pilot program in central New York that provided immediate telephone referrals and psychiatric consultation within 24 hours of a request, Dr. Hargrave said in a separate poster presentation at the meeting.
The CAP PC program improved upon the pilot by offering psychiatric consultation within 2 hours of a request, occasional in-person consultations, the education program, and a centralized computer database that allows the therapists and psychiatrists on different shifts to access patient records quickly, she said.
Compared with data from 2 years of the pilot program, data from the CAP PC program in the central New York area showed an increase in the number of children served from 6 to 14 per month (a 133% gain), an increase in the number of clinicians involved from 77 to 116 per month (a 51% gain), and an increase in the proportion of patients managed within the primary care office because of a decrease in the rate of referrals to more expensive specialists from 39% to 22%, Dr. Hargrave reported.
"The amount of morbidity that primary care physicians are coping with is amazing," especially in rural areas, she said.
Texas Model
A different model in Texas significantly decreased psychiatric symptoms and improved quality of life in children and adolescents participating in the program, Dr. Steven R. Pliszka reported in another poster presentation.
The Services Uniting Pediatrics and Psychiatry Outreaching to Texas (SUPPORT) program, funded by the Department of State Health Services, placed master’s level licensed therapists into primary care pediatric practices in six regions across the state. These therapists tried to see patients the same day that pediatricians referred them, and typically saw each patient for one to six sessions of practical, problem-focused therapies. A consulting child and adolescent psychiatrist helped determine which patients might need psychotropic medication and advised pediatricians on drug choice, dosing, and monitoring.
The SUPPORT program enrolled 145 pediatricians and 14,582 children covered by Medicaid. The outcomes evaluation involved a subset of 4,047 patients who were assessed at baseline, 3 month, and 6 months using the Child Behavior Checklist (CBCL) and the Pediatric Quality of Life Inventory (PedsQL).
In both younger (1.5-5 years of age) and older children (5-18 years), scores significantly decreased on the internalizing, externalizing, and total scales of the CBCL as well as on the individual symptom scales. Scores on the PedsQL improved significantly in each of four age groups (2-4 years, 5-7 years, 8-12 years, and 13-18 years), said Dr. Pliszka, professor and chair of child and adolescent psychiatry at the University of Texas at San Antonio.
Mean total scores on the CBCL, for example, decreased from approximately 63 to about 53 at 6 months. Mean PedsQL scores at baseline ranged approximately from 68 to 71 at baseline (depending on the age group) and increased to a range of about 77-81.
Data on diagnoses and prescriptions tracked by the program suggest that the pediatricians prescribed appropriate medications to the 2,207 patients who received at least one psychotropic medication (15% of all patients), Dr. Pliszka said.
"So, kids with ADHD got treated with a stimulant, kids with depression got an antidepressant, [and] kids with bipolar disorder got combinations of different medications. We also did not have any really bad outcomes. There were no suicides, no serious adverse drug effects. It shows that the model is a way to treat even fairly serious mental illnesses in the primary care setting," he said.
Dr. Pliszka and his associates next plan to compare outcomes for patients managed through SUPPORT and usual care (referral by primary care physicians to mental health clinics in the community).
Reimbursement Issues
Government and academic funds support these programs for now, but better funding mechanisms for collaborative care are needed for long-term sustainability, each of the physicians interviewed said.
New York’s CAP PC is a collaboration among five academic centers that is funded by a grant from the State Office of Mental Health. The SUPPORT program received Medicaid support in Texas.
While there probably are enough master’s level therapists to expand SUPPORT beyond the Medicaid population, "what’s lacking is that it’s difficult for both the pediatrician and the master’s level person to get reimbursed for that type of activity because they use completely different codes," Dr. Pliszka said. "Projects of this type would make the argument for modifying the reimbursement system to allow more integrated care."
Part of CAP PC’s education program helps New York primary care physicians get comfortable with coding for their mental health work, but there are gaps in that approach, Dr. Kaye said. "In some of our regions, docs can be paid reasonably for what they’re doing, but in lots of places, they can’t put in a code for ADHD or depression and get reimbursed" because insurers say they’re not credentialed mental health providers.
"There’s got to be a way on the payment side that Medicaid and/or the insurers figure out how to pay primary care docs to do this work, and to pay them fairly," he said. "I think this is going to be a huge part of the future of primary care. The numbers are that mental health problems are the most common chronic condition that kids get."
Even for the psychiatrists involved, the current model is not sustainable, he added. The New York grant pays each of the five academic centers for a 10-hour day of consultation each week, which is far less than the actual hours contributed.
"We’re all university based. We believe in the project, so we’ve been able to sustain that. Can we do that for 20 years? I don’t know," Dr. Kaye said.
"The major drawback is that it takes time, and insurance does not reimburse for that time. To really get such a system as this off the ground or well integrated" will require reimbursement for the time spent by all the health care providers involved, Dr. Hargrave said.
She said she hopes that in the future, all children and primary care clinicians will have access to mental health care, advice and support, "and that the clinicians – whether primary care or psychiatric – could be paid adequately for the work that we do."
Dr. Pliszka reported financial associations with Shire Pharmaceuticals and Ortho-McNeil-Janssen Pharmaceuticals. Dr. Kaye and Dr. Hargrave received research support from the New York State Office of Mental Health. Some of their coinvestigators reported financial associations with the Resource for Advancing Children’s Health Institute, American Psychiatric Publishing, Marriott Foundation, Shire Pharmaceuticals, and Ortho-McNeil-Janssen.
SAN FRANCISCO – After more than 2 decades as a primary care pediatrician, Dr. Teresa M. Hargrave was so frustrated by the lack of psychiatric services for her patients that she retrained as a child and adolescent psychiatrist. Now, she’s part of a New York state program that spreads her psychiatric skills to more patients than she imagined could be possible.
"If this program had been in place when I was a pediatrician, I would never have had to switch," said Dr. Hargrave of the State University of New York (SUNY) in Syracuse.
Today, New York primary care physicians can call 855-227-7272 toll free on weekdays for an immediate consultation with a master’s level therapist in the Child and Adolescent Psychiatry for Primary Care program (CAP PC). If a patient seems to need psychotropic medication, the therapist connects the pediatrician with a psychiatrist on the program’s team, such as Dr. Hargrave, who helps the primary care physician manage treatment through phone consultations and, if needed, in-person assessments.
Dozens of similar efforts – in a variety of formats – have sprung up across the country. They’re all trying to address a fundamental mismatch: There are only 7,400 practicing child and adolescent psychiatrists in the United States but more than 15 million young people in those age groups who need psychiatric care, according to data analyses from the American Academy of Child and Adolescent Psychiatry.
The National Network of Child Psychiatry Access Programs acts as a hub for these programs in 24 states, with programs in 4 more states set to take their first calls soon.
These model programs are making great inroads in getting care to the estimated 15%-25% of children seen in primary care offices who have behavioral health disorders, but reimbursement problems create a roadblock that must be overcome in the years ahead for the programs to be fully effective, several experts said in interviews at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
New York Program
New York’s CAP PC program modeled itself after one of the first state-wide programs, the Massachusetts Child Psychiatry Access Project, with some key changes. The CAP PC program covers 95% of the New York state population but uses the same toll-free number everywhere, compared with multiple different phone numbers being used in different regions in Massachusetts. New York’s program also added an educational component for primary care physicians – a free 15-hour "Mini-Fellowship" weekend program followed by a dozen 1-hour biweekly case-based conference calls.
Primary care physicians seem to love the help, Dr. David Kaye said at a poster presentation at the meeting. In its 2 years of operation, the CAP PC program has registered 829 primary care physicians (80% pediatricians, 20% family physicians), 292 of whom took the training sessions. The program handled 1,016 intake and follow-up calls, provided 993 consultations with a psychiatrist, conducted 94 face-to-face evaluations, and referred 305 patients to other services, reported Dr. Kaye, professor of psychiatry and director of child and adolescent psychiatry training at SUNY in Buffalo, N.Y.
Among 325 primary care physicians surveyed 2 weeks after contact with the CAP PC program, 94% said the consultations were very or extremely helpful, and 99% said they would recommend the program to other primary care physicians.
The program has greatly increased the number of children accessing psychiatric services compared with a previous pilot program in central New York that provided immediate telephone referrals and psychiatric consultation within 24 hours of a request, Dr. Hargrave said in a separate poster presentation at the meeting.
The CAP PC program improved upon the pilot by offering psychiatric consultation within 2 hours of a request, occasional in-person consultations, the education program, and a centralized computer database that allows the therapists and psychiatrists on different shifts to access patient records quickly, she said.
Compared with data from 2 years of the pilot program, data from the CAP PC program in the central New York area showed an increase in the number of children served from 6 to 14 per month (a 133% gain), an increase in the number of clinicians involved from 77 to 116 per month (a 51% gain), and an increase in the proportion of patients managed within the primary care office because of a decrease in the rate of referrals to more expensive specialists from 39% to 22%, Dr. Hargrave reported.
"The amount of morbidity that primary care physicians are coping with is amazing," especially in rural areas, she said.
Texas Model
A different model in Texas significantly decreased psychiatric symptoms and improved quality of life in children and adolescents participating in the program, Dr. Steven R. Pliszka reported in another poster presentation.
The Services Uniting Pediatrics and Psychiatry Outreaching to Texas (SUPPORT) program, funded by the Department of State Health Services, placed master’s level licensed therapists into primary care pediatric practices in six regions across the state. These therapists tried to see patients the same day that pediatricians referred them, and typically saw each patient for one to six sessions of practical, problem-focused therapies. A consulting child and adolescent psychiatrist helped determine which patients might need psychotropic medication and advised pediatricians on drug choice, dosing, and monitoring.
The SUPPORT program enrolled 145 pediatricians and 14,582 children covered by Medicaid. The outcomes evaluation involved a subset of 4,047 patients who were assessed at baseline, 3 month, and 6 months using the Child Behavior Checklist (CBCL) and the Pediatric Quality of Life Inventory (PedsQL).
In both younger (1.5-5 years of age) and older children (5-18 years), scores significantly decreased on the internalizing, externalizing, and total scales of the CBCL as well as on the individual symptom scales. Scores on the PedsQL improved significantly in each of four age groups (2-4 years, 5-7 years, 8-12 years, and 13-18 years), said Dr. Pliszka, professor and chair of child and adolescent psychiatry at the University of Texas at San Antonio.
Mean total scores on the CBCL, for example, decreased from approximately 63 to about 53 at 6 months. Mean PedsQL scores at baseline ranged approximately from 68 to 71 at baseline (depending on the age group) and increased to a range of about 77-81.
Data on diagnoses and prescriptions tracked by the program suggest that the pediatricians prescribed appropriate medications to the 2,207 patients who received at least one psychotropic medication (15% of all patients), Dr. Pliszka said.
"So, kids with ADHD got treated with a stimulant, kids with depression got an antidepressant, [and] kids with bipolar disorder got combinations of different medications. We also did not have any really bad outcomes. There were no suicides, no serious adverse drug effects. It shows that the model is a way to treat even fairly serious mental illnesses in the primary care setting," he said.
Dr. Pliszka and his associates next plan to compare outcomes for patients managed through SUPPORT and usual care (referral by primary care physicians to mental health clinics in the community).
Reimbursement Issues
Government and academic funds support these programs for now, but better funding mechanisms for collaborative care are needed for long-term sustainability, each of the physicians interviewed said.
New York’s CAP PC is a collaboration among five academic centers that is funded by a grant from the State Office of Mental Health. The SUPPORT program received Medicaid support in Texas.
While there probably are enough master’s level therapists to expand SUPPORT beyond the Medicaid population, "what’s lacking is that it’s difficult for both the pediatrician and the master’s level person to get reimbursed for that type of activity because they use completely different codes," Dr. Pliszka said. "Projects of this type would make the argument for modifying the reimbursement system to allow more integrated care."
Part of CAP PC’s education program helps New York primary care physicians get comfortable with coding for their mental health work, but there are gaps in that approach, Dr. Kaye said. "In some of our regions, docs can be paid reasonably for what they’re doing, but in lots of places, they can’t put in a code for ADHD or depression and get reimbursed" because insurers say they’re not credentialed mental health providers.
"There’s got to be a way on the payment side that Medicaid and/or the insurers figure out how to pay primary care docs to do this work, and to pay them fairly," he said. "I think this is going to be a huge part of the future of primary care. The numbers are that mental health problems are the most common chronic condition that kids get."
Even for the psychiatrists involved, the current model is not sustainable, he added. The New York grant pays each of the five academic centers for a 10-hour day of consultation each week, which is far less than the actual hours contributed.
"We’re all university based. We believe in the project, so we’ve been able to sustain that. Can we do that for 20 years? I don’t know," Dr. Kaye said.
"The major drawback is that it takes time, and insurance does not reimburse for that time. To really get such a system as this off the ground or well integrated" will require reimbursement for the time spent by all the health care providers involved, Dr. Hargrave said.
She said she hopes that in the future, all children and primary care clinicians will have access to mental health care, advice and support, "and that the clinicians – whether primary care or psychiatric – could be paid adequately for the work that we do."
Dr. Pliszka reported financial associations with Shire Pharmaceuticals and Ortho-McNeil-Janssen Pharmaceuticals. Dr. Kaye and Dr. Hargrave received research support from the New York State Office of Mental Health. Some of their coinvestigators reported financial associations with the Resource for Advancing Children’s Health Institute, American Psychiatric Publishing, Marriott Foundation, Shire Pharmaceuticals, and Ortho-McNeil-Janssen.
SAN FRANCISCO – After more than 2 decades as a primary care pediatrician, Dr. Teresa M. Hargrave was so frustrated by the lack of psychiatric services for her patients that she retrained as a child and adolescent psychiatrist. Now, she’s part of a New York state program that spreads her psychiatric skills to more patients than she imagined could be possible.
"If this program had been in place when I was a pediatrician, I would never have had to switch," said Dr. Hargrave of the State University of New York (SUNY) in Syracuse.
Today, New York primary care physicians can call 855-227-7272 toll free on weekdays for an immediate consultation with a master’s level therapist in the Child and Adolescent Psychiatry for Primary Care program (CAP PC). If a patient seems to need psychotropic medication, the therapist connects the pediatrician with a psychiatrist on the program’s team, such as Dr. Hargrave, who helps the primary care physician manage treatment through phone consultations and, if needed, in-person assessments.
Dozens of similar efforts – in a variety of formats – have sprung up across the country. They’re all trying to address a fundamental mismatch: There are only 7,400 practicing child and adolescent psychiatrists in the United States but more than 15 million young people in those age groups who need psychiatric care, according to data analyses from the American Academy of Child and Adolescent Psychiatry.
The National Network of Child Psychiatry Access Programs acts as a hub for these programs in 24 states, with programs in 4 more states set to take their first calls soon.
These model programs are making great inroads in getting care to the estimated 15%-25% of children seen in primary care offices who have behavioral health disorders, but reimbursement problems create a roadblock that must be overcome in the years ahead for the programs to be fully effective, several experts said in interviews at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
New York Program
New York’s CAP PC program modeled itself after one of the first state-wide programs, the Massachusetts Child Psychiatry Access Project, with some key changes. The CAP PC program covers 95% of the New York state population but uses the same toll-free number everywhere, compared with multiple different phone numbers being used in different regions in Massachusetts. New York’s program also added an educational component for primary care physicians – a free 15-hour "Mini-Fellowship" weekend program followed by a dozen 1-hour biweekly case-based conference calls.
Primary care physicians seem to love the help, Dr. David Kaye said at a poster presentation at the meeting. In its 2 years of operation, the CAP PC program has registered 829 primary care physicians (80% pediatricians, 20% family physicians), 292 of whom took the training sessions. The program handled 1,016 intake and follow-up calls, provided 993 consultations with a psychiatrist, conducted 94 face-to-face evaluations, and referred 305 patients to other services, reported Dr. Kaye, professor of psychiatry and director of child and adolescent psychiatry training at SUNY in Buffalo, N.Y.
Among 325 primary care physicians surveyed 2 weeks after contact with the CAP PC program, 94% said the consultations were very or extremely helpful, and 99% said they would recommend the program to other primary care physicians.
The program has greatly increased the number of children accessing psychiatric services compared with a previous pilot program in central New York that provided immediate telephone referrals and psychiatric consultation within 24 hours of a request, Dr. Hargrave said in a separate poster presentation at the meeting.
The CAP PC program improved upon the pilot by offering psychiatric consultation within 2 hours of a request, occasional in-person consultations, the education program, and a centralized computer database that allows the therapists and psychiatrists on different shifts to access patient records quickly, she said.
Compared with data from 2 years of the pilot program, data from the CAP PC program in the central New York area showed an increase in the number of children served from 6 to 14 per month (a 133% gain), an increase in the number of clinicians involved from 77 to 116 per month (a 51% gain), and an increase in the proportion of patients managed within the primary care office because of a decrease in the rate of referrals to more expensive specialists from 39% to 22%, Dr. Hargrave reported.
"The amount of morbidity that primary care physicians are coping with is amazing," especially in rural areas, she said.
Texas Model
A different model in Texas significantly decreased psychiatric symptoms and improved quality of life in children and adolescents participating in the program, Dr. Steven R. Pliszka reported in another poster presentation.
The Services Uniting Pediatrics and Psychiatry Outreaching to Texas (SUPPORT) program, funded by the Department of State Health Services, placed master’s level licensed therapists into primary care pediatric practices in six regions across the state. These therapists tried to see patients the same day that pediatricians referred them, and typically saw each patient for one to six sessions of practical, problem-focused therapies. A consulting child and adolescent psychiatrist helped determine which patients might need psychotropic medication and advised pediatricians on drug choice, dosing, and monitoring.
The SUPPORT program enrolled 145 pediatricians and 14,582 children covered by Medicaid. The outcomes evaluation involved a subset of 4,047 patients who were assessed at baseline, 3 month, and 6 months using the Child Behavior Checklist (CBCL) and the Pediatric Quality of Life Inventory (PedsQL).
In both younger (1.5-5 years of age) and older children (5-18 years), scores significantly decreased on the internalizing, externalizing, and total scales of the CBCL as well as on the individual symptom scales. Scores on the PedsQL improved significantly in each of four age groups (2-4 years, 5-7 years, 8-12 years, and 13-18 years), said Dr. Pliszka, professor and chair of child and adolescent psychiatry at the University of Texas at San Antonio.
Mean total scores on the CBCL, for example, decreased from approximately 63 to about 53 at 6 months. Mean PedsQL scores at baseline ranged approximately from 68 to 71 at baseline (depending on the age group) and increased to a range of about 77-81.
Data on diagnoses and prescriptions tracked by the program suggest that the pediatricians prescribed appropriate medications to the 2,207 patients who received at least one psychotropic medication (15% of all patients), Dr. Pliszka said.
"So, kids with ADHD got treated with a stimulant, kids with depression got an antidepressant, [and] kids with bipolar disorder got combinations of different medications. We also did not have any really bad outcomes. There were no suicides, no serious adverse drug effects. It shows that the model is a way to treat even fairly serious mental illnesses in the primary care setting," he said.
Dr. Pliszka and his associates next plan to compare outcomes for patients managed through SUPPORT and usual care (referral by primary care physicians to mental health clinics in the community).
Reimbursement Issues
Government and academic funds support these programs for now, but better funding mechanisms for collaborative care are needed for long-term sustainability, each of the physicians interviewed said.
New York’s CAP PC is a collaboration among five academic centers that is funded by a grant from the State Office of Mental Health. The SUPPORT program received Medicaid support in Texas.
While there probably are enough master’s level therapists to expand SUPPORT beyond the Medicaid population, "what’s lacking is that it’s difficult for both the pediatrician and the master’s level person to get reimbursed for that type of activity because they use completely different codes," Dr. Pliszka said. "Projects of this type would make the argument for modifying the reimbursement system to allow more integrated care."
Part of CAP PC’s education program helps New York primary care physicians get comfortable with coding for their mental health work, but there are gaps in that approach, Dr. Kaye said. "In some of our regions, docs can be paid reasonably for what they’re doing, but in lots of places, they can’t put in a code for ADHD or depression and get reimbursed" because insurers say they’re not credentialed mental health providers.
"There’s got to be a way on the payment side that Medicaid and/or the insurers figure out how to pay primary care docs to do this work, and to pay them fairly," he said. "I think this is going to be a huge part of the future of primary care. The numbers are that mental health problems are the most common chronic condition that kids get."
Even for the psychiatrists involved, the current model is not sustainable, he added. The New York grant pays each of the five academic centers for a 10-hour day of consultation each week, which is far less than the actual hours contributed.
"We’re all university based. We believe in the project, so we’ve been able to sustain that. Can we do that for 20 years? I don’t know," Dr. Kaye said.
"The major drawback is that it takes time, and insurance does not reimburse for that time. To really get such a system as this off the ground or well integrated" will require reimbursement for the time spent by all the health care providers involved, Dr. Hargrave said.
She said she hopes that in the future, all children and primary care clinicians will have access to mental health care, advice and support, "and that the clinicians – whether primary care or psychiatric – could be paid adequately for the work that we do."
Dr. Pliszka reported financial associations with Shire Pharmaceuticals and Ortho-McNeil-Janssen Pharmaceuticals. Dr. Kaye and Dr. Hargrave received research support from the New York State Office of Mental Health. Some of their coinvestigators reported financial associations with the Resource for Advancing Children’s Health Institute, American Psychiatric Publishing, Marriott Foundation, Shire Pharmaceuticals, and Ortho-McNeil-Janssen.
AT THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF CHILD AND ADOLESCENT PSYCHIATRY
Major Finding: Ninety-four percent of 325 New York primary care physicians who were surveyed rated the CAP PC program as very or extremely helpful. The program increased the number of children served by 133% in one region. The SUPPORT program significantly decreased psychiatric symptoms and improved quality of life scores in Texas children and adolescents.
Data Source: Data are from New York and Texas programs aimed at giving primary care physicians greater access to pediatric and adolescent psychiatric services.
Disclosures: Dr. Pliszka reported financial associations with Shire Pharmaceuticals and Ortho-McNeil-Janssen Pharmaceuticals. Dr. Kaye and Dr. Hargrave received research support from the New York State Office of Mental Health. Some of their coinvestigators reported financial associations with the Resource for Advancing Children’s Health Institute, American Psychiatric Publishing, Marriott Foundation, Shire Pharmaceuticals, and Ortho-McNeil-Janssen.
Recent Evidence Challenges Four Inpatient Management Habits
Why did you order that test? Dr. Leonard S. Feldman wants you to turn off the autopilot and consider the evidence from the medical literature on the following four practices:
• Is the best target hematocrit for a cardiac patient 30% (or a hemoglobin level of 10 g/dL)?
• Should nasogastric lavage be routine in patients with suspected GI bleeds?
• Is it helpful to measure the fractional excretion of sodium or fractional excretion of urea nitrogen when evaluating acute kidney injury?
• Are daily chest x-rays a good idea in patients on mechanical ventilation in an ICU or step-down unit?
"Many of us do all of these things regularly on a reflexive basis," said Dr. Feldman, director of the general medicine comprehensive consult service at Johns Hopkins University, Baltimore.
Yet recent studies challenge the value of these approaches:
Transfusions
Three studies influenced the AABB (formerly the American Association of Blood Banks) to publish a clinical practice guideline this year recommending a restrictive strategy when considering blood transfusions in hospitalized patients with preexisting cardiovascular disease. The AABB says not to transfuse if the hemoglobin level is above 7-8 g/dL and to consider transfusing patients who are symptomatic or who have a hemoglobin level of less than 8 g/dL, the AABB says (Ann. Intern. Med. 2012;157:49-58).
One recent study randomized 502 patients undergoing coronary artery bypass grafting (CABG) or valve replacement who were on cardiac bypass support to either a liberal strategy aiming to maintain a hematocrit of at or above 30% from the start of surgery until discharge from the ICU or a restrictive strategy that aimed to keep the hematocrit at or above 24%.
Both groups were able to meet these goals. The two groups did not differ significantly, however, in a composite end point of 30-day all-cause mortality and severe morbidity occurring during hospitalization (JAMA 2011;304:1559-67).
There was a trend toward higher risk of death with the restrictive strategy, with a hazard ratio of 1.28, but the ratio ranged from 0.6 to 2.7, so the risk was not statistically significant. Analysis of a slew of secondary outcomes also found no significant differences between groups.
Another study randomized 2,016 patients aged 50 years or older who either had a history of cardiovascular disease or cardiac risk factors and who had a hemoglobin level below 10 g/dL after surgery for hip fracture. The liberal strategy triggered transfusion in all patients with a hemoglobin below 10 g/dL. The restrictive strategy transfused only if the patient showed symptoms of anemia or at the physician’s discretion in patients with a hemoglobin level less than 8 g/dL.
Patients received a lot more blood under the liberal strategy compared with the restrictive strategy – 1,866 vs. 652 units of blood, respectively – but the groups did not differ significantly in death rates or the ability to walk across a room without human assistance at 30 and 60 days after surgery (N. Engl. J. Med. 2011;365:2453-62). Sixty days after surgery, 35% of patients in each group had died or were unable to walk across a room unaided.
"This is a trial that you should be showing all of your orthopedists," Dr. Feldman said. "When the orthopedist says that we need to give a patient blood so the patient will be able to do better in rehab" after hip surgery, point to the data showing that this isn’t necessarily true, he suggested.
An earlier trial of 838 critically ill patients who had hemoglobin levels below 9 g/dL within 72 hours of admission to the ICU found 30-day mortality rates of 19% in those randomized to a restrictive transfusion strategy and 23% in patients randomized to a liberal transfusion strategy, a difference that was not statistically significant (N. Engl. J. Med. 1999;340:409-17).
The liberal strategy transfused when hemoglobin levels fell below 10 g/dL and maintained the hemoglobin at 10-12 g/dL. The restrictive strategy waited until hemoglobin levels fell below 7 g/dL before transfusing and maintained hemoglobin at 7-9 g/dL.
"So, we have three different studies here that really seem to indicate that for transfusion of those patients who are at highest risk – cardiac patients – it did not seem to make a difference in their outcomes, particularly in mortality, if you were restrictive or liberal" in setting thresholds for transfusion, Dr. Feldman said. "This is not the same, though, for patients who are having an acute coronary syndrome. We don’t have any good data for them," and the AABB doesn’t recommend for or against liberal or restrictive transfusion thresholds, he added.
The evidence behind the AABB recommendation is only of moderate quality because there are only the three studies. Although the literature generally favors a restrictive versus a liberal approach, there’s no robust evidence for any particular transfusion threshold, said Dr. Daniel S. VanderEnde, a hospitalist and member of the joint transfusion committee at Emory University, Atlanta.
Pointing to the limited amount of research, the AABB itself calls the recommendation’s quality of evidence "very low" and the strength of the recommendation "uncertain."
"Subpar" evidence is one reason that Dr. VanderEnde’s institution leaves transfusion decisions to individual clinicians, he said in an interview. One ICU may transfuse at a hemoglobin threshold "in the mid-7s, and another ICU will have a transfusion threshold in the mid-8s."
Emory is starting a computer order entry protocol requiring physicians to tell why they’re transfusing blood, compared with no previous oversight. "It doesn’t stop them from transfusing for any reason. It is just trying to collect data, in the hopes that maybe they will be more restrictive in their use rather than liberal," he said.
Anecdotally, transfusion practices do seem to be shifting, at least among newly-trained physicians, Dr. VanderEnde added. Five years ago when he would ask medical students about transfusion thresholds, many hewed to "the old 10/30 rule," but far fewer do so today, he said. "The younger orthopedists tend to not transfuse as much as the older orthopedists."
Nasogastric Lavage
Few procedures performed in emergency departments are more painful for patients than nasogastric intubation, and there’s a study to prove that (Ann. Emerg. Med. 1999;33:652-8).
"Patients think nasogastric lavage and nasogastric intubation really stink, so we need to have a good reason to do it," Dr. Feldman said.
And, like all invasive procedures, there are risks involved, Dr. Chad T. Whelan said in an interview. There are only modestly convincing data suggesting that nasogastric lavage can provide some prognostic or "localizing" information (such as differentiating upper vs. lower bleed). "Therefore, the risk/benefit ratio of routinely performing them for all patients has shifted with our increasing understanding of their risks and benefits," said Dr. Whelan, a hospitalist at the University of Chicago.
International consensus recommendations on the management of patients with nonvariceal upper GI bleeding suggest that physicians consider placing a nasogastric tube in selected patients because the findings may have prognostic value – not very helpful advice in decision making, Dr. Feldman said. (Ann. Intern. Med. 2010;152:101-13).
The rationale until now has been that patients with bloody aspirate on nasogastric lavage are significantly more likely to have high-risk GI lesions on endoscopy, compared with patients with clear or bilious aspirates on lavage. But does knowing this improve outcomes?
One review of the literature on how to determine if a patient has a severe upper GI bleed confirmed that a bloody aspirate on nasogastric lavage increases the likelihood of an upper GI bleed but there’s only a mildly increased likelihood of a severe bleed, "and the negative likelihood ratio is not unimpressive," Dr. Feldman said (JAMA 2012;307:1072-19).
Results of a separate propensity-matched retrospective analysis of data on 632 patients admitted with GI bleeding are "as good as we’re going to get on this topic," he said. The study found that getting or not getting nasogastric lavage did not change 30-day mortality, mean length of stay, transfusion requirements, or emergency surgery rates (Gastrointest. Endosc. 2011;74:971-80).
The only things that nasogastric lavage did change were an increase in the rate of patients undergoing endoscopy, a shorter interval to endoscopy, and a shorter length of stay among patients who had endoscopy.
That suggests that there was an individual-provider confounder that the study could not measure. Perhaps emergency physicians or gastroenterologists who order nasogastric lavage are simply more aggressive, Dr. Feldman said. "This is information that you might want to take to your emergency department," he said.
In a joint editorial accompanying the study, an emergency physician and an endoscopist concluded that the practice of nasogastric lavage in patients with acute upper GI bleeding is "antiquated."
Dr. Whelan said the role of nasogastric lavage "is in transition rather than antiquated." As upper GI bleeding epidemiology evolves and endoscopic interventions improve, "the widespread use of nasogastric lavage as a universal piece of the upper GI bleed protocol should decrease. Whether nasogastric lavage ultimately becomes a completely unnecessary procedure remains to be seen," he said.
Physicians at his institution no longer routinely perform nasogastric lavage when evaluating suspected upper GI bleeding, but "it has not completely disappeared from practice, either," he said. That’s less a factor of "aggressive" physicians and more a result of how practice changes and environmental factors, Dr. Whelan added. "Not all emergency rooms have access to full-service endoscopy on site, so emergency room physicians may have a different set of risk/benefit tradeoffs to consider."
Acute Kidney Injury
Can the fractional excretion of sodium (FENa) or fractional excretion of urea nitrogen (FEUN) help narrow the differential diagnosis in acute kidney disease? Widespread use of these measures began after a 17-person study in 1976 suggested that patients with prerenal azotemia had a FENa of less than 1 and patients with acute tubular necrosis had a FENa greater than 3 (JAMA 1976;236:579-81).
The FENa is not perfect, because many intrinsic kidney disorders can cause low FENa and the FENa can be elevated when diuretic use contributes to prerenal states, so a few studies looked at adding the FEUN to the diagnostic tools. Their results were contradictory.
One study of 102 patients in the ICU found that incorporating FEUN was 85% sensitive and 92% specific in detecting prerenal injury, but the study excluded patients with acute glomerulonephritis and obstructive nephropathy, "so you have to make sure that you exclude those patients if you’re going to use FEUN," Dr. Feldman said (Kidney Int. 2002;62:2223-9).
In a separate study of 99 patients, however, the FENa and FEUN were much less impressive in patients with or without diuretics. In patients on diuretics, FEUN had a sensitivity for distinguishing transient from persistent acute kidney injury of 79% and a specificity of 33%, and in patients not on diuretics the sensitivity was 48% and the specificity was 75% (Am. J. Kidney Dis. 2007;50:568-73).
A recent analysis reviewed the literature to provide some guidance for clinicians, but the end result is confusing, Dr. Feldman said. Under best-case scenarios, these two measures would be likely to make a difference in diagnosing the cause of acute kidney injury, but under worst-case scenarios, "they really stink," he said (Cleve. Clin. J. Med. 2012;79:121-6).
The authors cautioned that a single index calculated at a specific time often is insufficient to properly characterize the pathogenesis of acute kidney injury. "In the end, probably FENa and FEUN really don’t help you very much to decide" the reason behind acute kidney injury, Dr. Feldman said.
Chest X-Rays
Routine chest x-rays in mechanically ventilated patients in ICUs provide, well, too many unneeded x-rays, recent data show.
A crossover study that randomized 21 French ICUs to either routine daily chest x-rays for these patients or x-rays on demand found that the on-demand strategy reduced the number of x-rays by 32% without affecting the number of days on ventilation, length of ICU stay, or mortality. With the daily x-ray strategy, 424 patients got 4,607 x-rays, compared with 3,148 x-rays in 425 patients under the on-demand strategy (Lancet 2009;374:1687-93).
Patients had their ventilators changed more often under the on-demand strategy, probably as clinicians were troubleshooting potential problems, but the number of interventions did not differ significantly by x-ray strategy, Dr. Feldman noted.
A meta-analysis this year of eight trials including 7,078 adult ICU patients concluded that routine daily x-rays can be eliminated without increasing adverse outcomes (Radiology 2012;255:386-95).
Dr. Feldman suggested specific goals for these four scenarios, which he presented at the annual meeting of the Society of Hospitalist Medicine.
"Do not reflexively transfuse cardiac patients to hematocrits of 30%. Do not do routine daily chest x-rays. Do not reflexively NG [nasogastric] lavage our patients. And spend more time doing a really great history and physical and thinking about why your patient has acute renal failure than trying to use indices that don’t actually help us very much," he said.
He added a personal goal: "If I can make the residents at Johns Hopkins change, that will be a real feat, because they love to order tests on everybody."
Dr. Feldman, Dr. Whelan, and Dr. VanderEnde reported having no financial disclosures.
Why did you order that test? Dr. Leonard S. Feldman wants you to turn off the autopilot and consider the evidence from the medical literature on the following four practices:
• Is the best target hematocrit for a cardiac patient 30% (or a hemoglobin level of 10 g/dL)?
• Should nasogastric lavage be routine in patients with suspected GI bleeds?
• Is it helpful to measure the fractional excretion of sodium or fractional excretion of urea nitrogen when evaluating acute kidney injury?
• Are daily chest x-rays a good idea in patients on mechanical ventilation in an ICU or step-down unit?
"Many of us do all of these things regularly on a reflexive basis," said Dr. Feldman, director of the general medicine comprehensive consult service at Johns Hopkins University, Baltimore.
Yet recent studies challenge the value of these approaches:
Transfusions
Three studies influenced the AABB (formerly the American Association of Blood Banks) to publish a clinical practice guideline this year recommending a restrictive strategy when considering blood transfusions in hospitalized patients with preexisting cardiovascular disease. The AABB says not to transfuse if the hemoglobin level is above 7-8 g/dL and to consider transfusing patients who are symptomatic or who have a hemoglobin level of less than 8 g/dL, the AABB says (Ann. Intern. Med. 2012;157:49-58).
One recent study randomized 502 patients undergoing coronary artery bypass grafting (CABG) or valve replacement who were on cardiac bypass support to either a liberal strategy aiming to maintain a hematocrit of at or above 30% from the start of surgery until discharge from the ICU or a restrictive strategy that aimed to keep the hematocrit at or above 24%.
Both groups were able to meet these goals. The two groups did not differ significantly, however, in a composite end point of 30-day all-cause mortality and severe morbidity occurring during hospitalization (JAMA 2011;304:1559-67).
There was a trend toward higher risk of death with the restrictive strategy, with a hazard ratio of 1.28, but the ratio ranged from 0.6 to 2.7, so the risk was not statistically significant. Analysis of a slew of secondary outcomes also found no significant differences between groups.
Another study randomized 2,016 patients aged 50 years or older who either had a history of cardiovascular disease or cardiac risk factors and who had a hemoglobin level below 10 g/dL after surgery for hip fracture. The liberal strategy triggered transfusion in all patients with a hemoglobin below 10 g/dL. The restrictive strategy transfused only if the patient showed symptoms of anemia or at the physician’s discretion in patients with a hemoglobin level less than 8 g/dL.
Patients received a lot more blood under the liberal strategy compared with the restrictive strategy – 1,866 vs. 652 units of blood, respectively – but the groups did not differ significantly in death rates or the ability to walk across a room without human assistance at 30 and 60 days after surgery (N. Engl. J. Med. 2011;365:2453-62). Sixty days after surgery, 35% of patients in each group had died or were unable to walk across a room unaided.
"This is a trial that you should be showing all of your orthopedists," Dr. Feldman said. "When the orthopedist says that we need to give a patient blood so the patient will be able to do better in rehab" after hip surgery, point to the data showing that this isn’t necessarily true, he suggested.
An earlier trial of 838 critically ill patients who had hemoglobin levels below 9 g/dL within 72 hours of admission to the ICU found 30-day mortality rates of 19% in those randomized to a restrictive transfusion strategy and 23% in patients randomized to a liberal transfusion strategy, a difference that was not statistically significant (N. Engl. J. Med. 1999;340:409-17).
The liberal strategy transfused when hemoglobin levels fell below 10 g/dL and maintained the hemoglobin at 10-12 g/dL. The restrictive strategy waited until hemoglobin levels fell below 7 g/dL before transfusing and maintained hemoglobin at 7-9 g/dL.
"So, we have three different studies here that really seem to indicate that for transfusion of those patients who are at highest risk – cardiac patients – it did not seem to make a difference in their outcomes, particularly in mortality, if you were restrictive or liberal" in setting thresholds for transfusion, Dr. Feldman said. "This is not the same, though, for patients who are having an acute coronary syndrome. We don’t have any good data for them," and the AABB doesn’t recommend for or against liberal or restrictive transfusion thresholds, he added.
The evidence behind the AABB recommendation is only of moderate quality because there are only the three studies. Although the literature generally favors a restrictive versus a liberal approach, there’s no robust evidence for any particular transfusion threshold, said Dr. Daniel S. VanderEnde, a hospitalist and member of the joint transfusion committee at Emory University, Atlanta.
Pointing to the limited amount of research, the AABB itself calls the recommendation’s quality of evidence "very low" and the strength of the recommendation "uncertain."
"Subpar" evidence is one reason that Dr. VanderEnde’s institution leaves transfusion decisions to individual clinicians, he said in an interview. One ICU may transfuse at a hemoglobin threshold "in the mid-7s, and another ICU will have a transfusion threshold in the mid-8s."
Emory is starting a computer order entry protocol requiring physicians to tell why they’re transfusing blood, compared with no previous oversight. "It doesn’t stop them from transfusing for any reason. It is just trying to collect data, in the hopes that maybe they will be more restrictive in their use rather than liberal," he said.
Anecdotally, transfusion practices do seem to be shifting, at least among newly-trained physicians, Dr. VanderEnde added. Five years ago when he would ask medical students about transfusion thresholds, many hewed to "the old 10/30 rule," but far fewer do so today, he said. "The younger orthopedists tend to not transfuse as much as the older orthopedists."
Nasogastric Lavage
Few procedures performed in emergency departments are more painful for patients than nasogastric intubation, and there’s a study to prove that (Ann. Emerg. Med. 1999;33:652-8).
"Patients think nasogastric lavage and nasogastric intubation really stink, so we need to have a good reason to do it," Dr. Feldman said.
And, like all invasive procedures, there are risks involved, Dr. Chad T. Whelan said in an interview. There are only modestly convincing data suggesting that nasogastric lavage can provide some prognostic or "localizing" information (such as differentiating upper vs. lower bleed). "Therefore, the risk/benefit ratio of routinely performing them for all patients has shifted with our increasing understanding of their risks and benefits," said Dr. Whelan, a hospitalist at the University of Chicago.
International consensus recommendations on the management of patients with nonvariceal upper GI bleeding suggest that physicians consider placing a nasogastric tube in selected patients because the findings may have prognostic value – not very helpful advice in decision making, Dr. Feldman said. (Ann. Intern. Med. 2010;152:101-13).
The rationale until now has been that patients with bloody aspirate on nasogastric lavage are significantly more likely to have high-risk GI lesions on endoscopy, compared with patients with clear or bilious aspirates on lavage. But does knowing this improve outcomes?
One review of the literature on how to determine if a patient has a severe upper GI bleed confirmed that a bloody aspirate on nasogastric lavage increases the likelihood of an upper GI bleed but there’s only a mildly increased likelihood of a severe bleed, "and the negative likelihood ratio is not unimpressive," Dr. Feldman said (JAMA 2012;307:1072-19).
Results of a separate propensity-matched retrospective analysis of data on 632 patients admitted with GI bleeding are "as good as we’re going to get on this topic," he said. The study found that getting or not getting nasogastric lavage did not change 30-day mortality, mean length of stay, transfusion requirements, or emergency surgery rates (Gastrointest. Endosc. 2011;74:971-80).
The only things that nasogastric lavage did change were an increase in the rate of patients undergoing endoscopy, a shorter interval to endoscopy, and a shorter length of stay among patients who had endoscopy.
That suggests that there was an individual-provider confounder that the study could not measure. Perhaps emergency physicians or gastroenterologists who order nasogastric lavage are simply more aggressive, Dr. Feldman said. "This is information that you might want to take to your emergency department," he said.
In a joint editorial accompanying the study, an emergency physician and an endoscopist concluded that the practice of nasogastric lavage in patients with acute upper GI bleeding is "antiquated."
Dr. Whelan said the role of nasogastric lavage "is in transition rather than antiquated." As upper GI bleeding epidemiology evolves and endoscopic interventions improve, "the widespread use of nasogastric lavage as a universal piece of the upper GI bleed protocol should decrease. Whether nasogastric lavage ultimately becomes a completely unnecessary procedure remains to be seen," he said.
Physicians at his institution no longer routinely perform nasogastric lavage when evaluating suspected upper GI bleeding, but "it has not completely disappeared from practice, either," he said. That’s less a factor of "aggressive" physicians and more a result of how practice changes and environmental factors, Dr. Whelan added. "Not all emergency rooms have access to full-service endoscopy on site, so emergency room physicians may have a different set of risk/benefit tradeoffs to consider."
Acute Kidney Injury
Can the fractional excretion of sodium (FENa) or fractional excretion of urea nitrogen (FEUN) help narrow the differential diagnosis in acute kidney disease? Widespread use of these measures began after a 17-person study in 1976 suggested that patients with prerenal azotemia had a FENa of less than 1 and patients with acute tubular necrosis had a FENa greater than 3 (JAMA 1976;236:579-81).
The FENa is not perfect, because many intrinsic kidney disorders can cause low FENa and the FENa can be elevated when diuretic use contributes to prerenal states, so a few studies looked at adding the FEUN to the diagnostic tools. Their results were contradictory.
One study of 102 patients in the ICU found that incorporating FEUN was 85% sensitive and 92% specific in detecting prerenal injury, but the study excluded patients with acute glomerulonephritis and obstructive nephropathy, "so you have to make sure that you exclude those patients if you’re going to use FEUN," Dr. Feldman said (Kidney Int. 2002;62:2223-9).
In a separate study of 99 patients, however, the FENa and FEUN were much less impressive in patients with or without diuretics. In patients on diuretics, FEUN had a sensitivity for distinguishing transient from persistent acute kidney injury of 79% and a specificity of 33%, and in patients not on diuretics the sensitivity was 48% and the specificity was 75% (Am. J. Kidney Dis. 2007;50:568-73).
A recent analysis reviewed the literature to provide some guidance for clinicians, but the end result is confusing, Dr. Feldman said. Under best-case scenarios, these two measures would be likely to make a difference in diagnosing the cause of acute kidney injury, but under worst-case scenarios, "they really stink," he said (Cleve. Clin. J. Med. 2012;79:121-6).
The authors cautioned that a single index calculated at a specific time often is insufficient to properly characterize the pathogenesis of acute kidney injury. "In the end, probably FENa and FEUN really don’t help you very much to decide" the reason behind acute kidney injury, Dr. Feldman said.
Chest X-Rays
Routine chest x-rays in mechanically ventilated patients in ICUs provide, well, too many unneeded x-rays, recent data show.
A crossover study that randomized 21 French ICUs to either routine daily chest x-rays for these patients or x-rays on demand found that the on-demand strategy reduced the number of x-rays by 32% without affecting the number of days on ventilation, length of ICU stay, or mortality. With the daily x-ray strategy, 424 patients got 4,607 x-rays, compared with 3,148 x-rays in 425 patients under the on-demand strategy (Lancet 2009;374:1687-93).
Patients had their ventilators changed more often under the on-demand strategy, probably as clinicians were troubleshooting potential problems, but the number of interventions did not differ significantly by x-ray strategy, Dr. Feldman noted.
A meta-analysis this year of eight trials including 7,078 adult ICU patients concluded that routine daily x-rays can be eliminated without increasing adverse outcomes (Radiology 2012;255:386-95).
Dr. Feldman suggested specific goals for these four scenarios, which he presented at the annual meeting of the Society of Hospitalist Medicine.
"Do not reflexively transfuse cardiac patients to hematocrits of 30%. Do not do routine daily chest x-rays. Do not reflexively NG [nasogastric] lavage our patients. And spend more time doing a really great history and physical and thinking about why your patient has acute renal failure than trying to use indices that don’t actually help us very much," he said.
He added a personal goal: "If I can make the residents at Johns Hopkins change, that will be a real feat, because they love to order tests on everybody."
Dr. Feldman, Dr. Whelan, and Dr. VanderEnde reported having no financial disclosures.
Why did you order that test? Dr. Leonard S. Feldman wants you to turn off the autopilot and consider the evidence from the medical literature on the following four practices:
• Is the best target hematocrit for a cardiac patient 30% (or a hemoglobin level of 10 g/dL)?
• Should nasogastric lavage be routine in patients with suspected GI bleeds?
• Is it helpful to measure the fractional excretion of sodium or fractional excretion of urea nitrogen when evaluating acute kidney injury?
• Are daily chest x-rays a good idea in patients on mechanical ventilation in an ICU or step-down unit?
"Many of us do all of these things regularly on a reflexive basis," said Dr. Feldman, director of the general medicine comprehensive consult service at Johns Hopkins University, Baltimore.
Yet recent studies challenge the value of these approaches:
Transfusions
Three studies influenced the AABB (formerly the American Association of Blood Banks) to publish a clinical practice guideline this year recommending a restrictive strategy when considering blood transfusions in hospitalized patients with preexisting cardiovascular disease. The AABB says not to transfuse if the hemoglobin level is above 7-8 g/dL and to consider transfusing patients who are symptomatic or who have a hemoglobin level of less than 8 g/dL, the AABB says (Ann. Intern. Med. 2012;157:49-58).
One recent study randomized 502 patients undergoing coronary artery bypass grafting (CABG) or valve replacement who were on cardiac bypass support to either a liberal strategy aiming to maintain a hematocrit of at or above 30% from the start of surgery until discharge from the ICU or a restrictive strategy that aimed to keep the hematocrit at or above 24%.
Both groups were able to meet these goals. The two groups did not differ significantly, however, in a composite end point of 30-day all-cause mortality and severe morbidity occurring during hospitalization (JAMA 2011;304:1559-67).
There was a trend toward higher risk of death with the restrictive strategy, with a hazard ratio of 1.28, but the ratio ranged from 0.6 to 2.7, so the risk was not statistically significant. Analysis of a slew of secondary outcomes also found no significant differences between groups.
Another study randomized 2,016 patients aged 50 years or older who either had a history of cardiovascular disease or cardiac risk factors and who had a hemoglobin level below 10 g/dL after surgery for hip fracture. The liberal strategy triggered transfusion in all patients with a hemoglobin below 10 g/dL. The restrictive strategy transfused only if the patient showed symptoms of anemia or at the physician’s discretion in patients with a hemoglobin level less than 8 g/dL.
Patients received a lot more blood under the liberal strategy compared with the restrictive strategy – 1,866 vs. 652 units of blood, respectively – but the groups did not differ significantly in death rates or the ability to walk across a room without human assistance at 30 and 60 days after surgery (N. Engl. J. Med. 2011;365:2453-62). Sixty days after surgery, 35% of patients in each group had died or were unable to walk across a room unaided.
"This is a trial that you should be showing all of your orthopedists," Dr. Feldman said. "When the orthopedist says that we need to give a patient blood so the patient will be able to do better in rehab" after hip surgery, point to the data showing that this isn’t necessarily true, he suggested.
An earlier trial of 838 critically ill patients who had hemoglobin levels below 9 g/dL within 72 hours of admission to the ICU found 30-day mortality rates of 19% in those randomized to a restrictive transfusion strategy and 23% in patients randomized to a liberal transfusion strategy, a difference that was not statistically significant (N. Engl. J. Med. 1999;340:409-17).
The liberal strategy transfused when hemoglobin levels fell below 10 g/dL and maintained the hemoglobin at 10-12 g/dL. The restrictive strategy waited until hemoglobin levels fell below 7 g/dL before transfusing and maintained hemoglobin at 7-9 g/dL.
"So, we have three different studies here that really seem to indicate that for transfusion of those patients who are at highest risk – cardiac patients – it did not seem to make a difference in their outcomes, particularly in mortality, if you were restrictive or liberal" in setting thresholds for transfusion, Dr. Feldman said. "This is not the same, though, for patients who are having an acute coronary syndrome. We don’t have any good data for them," and the AABB doesn’t recommend for or against liberal or restrictive transfusion thresholds, he added.
The evidence behind the AABB recommendation is only of moderate quality because there are only the three studies. Although the literature generally favors a restrictive versus a liberal approach, there’s no robust evidence for any particular transfusion threshold, said Dr. Daniel S. VanderEnde, a hospitalist and member of the joint transfusion committee at Emory University, Atlanta.
Pointing to the limited amount of research, the AABB itself calls the recommendation’s quality of evidence "very low" and the strength of the recommendation "uncertain."
"Subpar" evidence is one reason that Dr. VanderEnde’s institution leaves transfusion decisions to individual clinicians, he said in an interview. One ICU may transfuse at a hemoglobin threshold "in the mid-7s, and another ICU will have a transfusion threshold in the mid-8s."
Emory is starting a computer order entry protocol requiring physicians to tell why they’re transfusing blood, compared with no previous oversight. "It doesn’t stop them from transfusing for any reason. It is just trying to collect data, in the hopes that maybe they will be more restrictive in their use rather than liberal," he said.
Anecdotally, transfusion practices do seem to be shifting, at least among newly-trained physicians, Dr. VanderEnde added. Five years ago when he would ask medical students about transfusion thresholds, many hewed to "the old 10/30 rule," but far fewer do so today, he said. "The younger orthopedists tend to not transfuse as much as the older orthopedists."
Nasogastric Lavage
Few procedures performed in emergency departments are more painful for patients than nasogastric intubation, and there’s a study to prove that (Ann. Emerg. Med. 1999;33:652-8).
"Patients think nasogastric lavage and nasogastric intubation really stink, so we need to have a good reason to do it," Dr. Feldman said.
And, like all invasive procedures, there are risks involved, Dr. Chad T. Whelan said in an interview. There are only modestly convincing data suggesting that nasogastric lavage can provide some prognostic or "localizing" information (such as differentiating upper vs. lower bleed). "Therefore, the risk/benefit ratio of routinely performing them for all patients has shifted with our increasing understanding of their risks and benefits," said Dr. Whelan, a hospitalist at the University of Chicago.
International consensus recommendations on the management of patients with nonvariceal upper GI bleeding suggest that physicians consider placing a nasogastric tube in selected patients because the findings may have prognostic value – not very helpful advice in decision making, Dr. Feldman said. (Ann. Intern. Med. 2010;152:101-13).
The rationale until now has been that patients with bloody aspirate on nasogastric lavage are significantly more likely to have high-risk GI lesions on endoscopy, compared with patients with clear or bilious aspirates on lavage. But does knowing this improve outcomes?
One review of the literature on how to determine if a patient has a severe upper GI bleed confirmed that a bloody aspirate on nasogastric lavage increases the likelihood of an upper GI bleed but there’s only a mildly increased likelihood of a severe bleed, "and the negative likelihood ratio is not unimpressive," Dr. Feldman said (JAMA 2012;307:1072-19).
Results of a separate propensity-matched retrospective analysis of data on 632 patients admitted with GI bleeding are "as good as we’re going to get on this topic," he said. The study found that getting or not getting nasogastric lavage did not change 30-day mortality, mean length of stay, transfusion requirements, or emergency surgery rates (Gastrointest. Endosc. 2011;74:971-80).
The only things that nasogastric lavage did change were an increase in the rate of patients undergoing endoscopy, a shorter interval to endoscopy, and a shorter length of stay among patients who had endoscopy.
That suggests that there was an individual-provider confounder that the study could not measure. Perhaps emergency physicians or gastroenterologists who order nasogastric lavage are simply more aggressive, Dr. Feldman said. "This is information that you might want to take to your emergency department," he said.
In a joint editorial accompanying the study, an emergency physician and an endoscopist concluded that the practice of nasogastric lavage in patients with acute upper GI bleeding is "antiquated."
Dr. Whelan said the role of nasogastric lavage "is in transition rather than antiquated." As upper GI bleeding epidemiology evolves and endoscopic interventions improve, "the widespread use of nasogastric lavage as a universal piece of the upper GI bleed protocol should decrease. Whether nasogastric lavage ultimately becomes a completely unnecessary procedure remains to be seen," he said.
Physicians at his institution no longer routinely perform nasogastric lavage when evaluating suspected upper GI bleeding, but "it has not completely disappeared from practice, either," he said. That’s less a factor of "aggressive" physicians and more a result of how practice changes and environmental factors, Dr. Whelan added. "Not all emergency rooms have access to full-service endoscopy on site, so emergency room physicians may have a different set of risk/benefit tradeoffs to consider."
Acute Kidney Injury
Can the fractional excretion of sodium (FENa) or fractional excretion of urea nitrogen (FEUN) help narrow the differential diagnosis in acute kidney disease? Widespread use of these measures began after a 17-person study in 1976 suggested that patients with prerenal azotemia had a FENa of less than 1 and patients with acute tubular necrosis had a FENa greater than 3 (JAMA 1976;236:579-81).
The FENa is not perfect, because many intrinsic kidney disorders can cause low FENa and the FENa can be elevated when diuretic use contributes to prerenal states, so a few studies looked at adding the FEUN to the diagnostic tools. Their results were contradictory.
One study of 102 patients in the ICU found that incorporating FEUN was 85% sensitive and 92% specific in detecting prerenal injury, but the study excluded patients with acute glomerulonephritis and obstructive nephropathy, "so you have to make sure that you exclude those patients if you’re going to use FEUN," Dr. Feldman said (Kidney Int. 2002;62:2223-9).
In a separate study of 99 patients, however, the FENa and FEUN were much less impressive in patients with or without diuretics. In patients on diuretics, FEUN had a sensitivity for distinguishing transient from persistent acute kidney injury of 79% and a specificity of 33%, and in patients not on diuretics the sensitivity was 48% and the specificity was 75% (Am. J. Kidney Dis. 2007;50:568-73).
A recent analysis reviewed the literature to provide some guidance for clinicians, but the end result is confusing, Dr. Feldman said. Under best-case scenarios, these two measures would be likely to make a difference in diagnosing the cause of acute kidney injury, but under worst-case scenarios, "they really stink," he said (Cleve. Clin. J. Med. 2012;79:121-6).
The authors cautioned that a single index calculated at a specific time often is insufficient to properly characterize the pathogenesis of acute kidney injury. "In the end, probably FENa and FEUN really don’t help you very much to decide" the reason behind acute kidney injury, Dr. Feldman said.
Chest X-Rays
Routine chest x-rays in mechanically ventilated patients in ICUs provide, well, too many unneeded x-rays, recent data show.
A crossover study that randomized 21 French ICUs to either routine daily chest x-rays for these patients or x-rays on demand found that the on-demand strategy reduced the number of x-rays by 32% without affecting the number of days on ventilation, length of ICU stay, or mortality. With the daily x-ray strategy, 424 patients got 4,607 x-rays, compared with 3,148 x-rays in 425 patients under the on-demand strategy (Lancet 2009;374:1687-93).
Patients had their ventilators changed more often under the on-demand strategy, probably as clinicians were troubleshooting potential problems, but the number of interventions did not differ significantly by x-ray strategy, Dr. Feldman noted.
A meta-analysis this year of eight trials including 7,078 adult ICU patients concluded that routine daily x-rays can be eliminated without increasing adverse outcomes (Radiology 2012;255:386-95).
Dr. Feldman suggested specific goals for these four scenarios, which he presented at the annual meeting of the Society of Hospitalist Medicine.
"Do not reflexively transfuse cardiac patients to hematocrits of 30%. Do not do routine daily chest x-rays. Do not reflexively NG [nasogastric] lavage our patients. And spend more time doing a really great history and physical and thinking about why your patient has acute renal failure than trying to use indices that don’t actually help us very much," he said.
He added a personal goal: "If I can make the residents at Johns Hopkins change, that will be a real feat, because they love to order tests on everybody."
Dr. Feldman, Dr. Whelan, and Dr. VanderEnde reported having no financial disclosures.
Don't Overreach for Subthreshold Pediatric Bipolar Disorder
SAN FRANCISCO – When youths get referred for help with symptoms that don’t quite meet diagnostic criteria for bipolar illness, there’s a 50-50 chance they’ll progress to a diagnosis of bipolar disorder I or II within 7 years. The odds are a coin toss.
The risk logically might be even lower in general clinical settings than in this defined group. That’s why Dr. David A. Axelson and his associates advocate using conservative criteria for diagnosing "bipolar not otherwise specified" (BP-NOS) in general clinics.
Dr. Axelson won the American Academy of Child and Adolescent Psychiatry’s Klingenstein Third Generation Foundation Award for his longitudinal research on 140 children and adolescents who met an operationalized diagnosis of BP-NOS. At a median follow-up of 5 years, 45% had converted to bipolar disorder I or II (BP I/II) within a mean of 58 weeks after intake (J. Am. Acad. Child. Adolesc. Psychiatry 2011;50:1001-16.e3).
New data from the ongoing study show that 50% progressed to BP I/II at a median follow-up of 7 years, he said at the academy’s annual meeting. Symptoms for most of the youths in the COBY (Course and Outcome of Bipolar Youth) study far exceeded the minimum BP-NOS criteria at baseline.
Very few factors predicted whether patients would convert to BP I/II or not, and even those were not strong predictors, said Dr. Axelson, medical director of Child and Adolescent Bipolar Services Outpatient Program at the University of Pittsburgh’s Western Psychiatric Institute and Clinic.
Many children and adolescents present to clinics with manic symptomatology that does not meet diagnostic criteria for BP I/II in the DSM-IV. Clinicians walk a tightrope between intervening as early as possible for best treatment results and mislabeling (and then mistreating) some youths who don’t have bipolar illness.
The criteria for BP-NOS in the DSM-IV are vague and nonspecific, Dr. Axelson said. Based on his and other studies of "subthreshold" bipolar symptoms in children and adolescents, Dr. Axelson proposed that criteria for diagnosing BP-NOS in general clinical settings include:
• Use of full DSM symptom criteria for a hypomanic or manic episode.
Almost all of the children and adolescents in his COBY study met medical criteria for symptoms, he noted.
• Having hypomanic symptoms for most of the day.
"Similar to what we think about for major depression," Dr. Axelson said. "This most-of-the-day specifier will be in DSM 5 for manic or hypomanic episodes."
• At least one episode of 2-day duration.
• At least four recurrent episodes.
Almost all the children and adolescents with BP-NOS in the COBY study already had recurrent episodes.
These criteria are "probably the best balance between sensitivity and specificity, understanding the fact that this is going to miss some kids in the early phase of illness," he said.
The COBY study enrolled 153 youths seen at three academic medical centers, 140 of whom had at least one follow-up visit. The main reasons the diagnosis was BP-NOS instead of BP I/II were because the duration of manic or hypomanic episodes was too short (only 1-3 days in 86% of patients); the youth had hypomania with no major depressive episode (11%); or the youth did not have the required number of symptoms for BP I/II (3%).
The investigators tracked at least 17 factors that they hypothesized might help predict which youths would progress to BP I/II. "Much to my surprise, very little of this actually predicted future onset," Dr. Axelson said. The main predictor was a family history of mania or hypomania and, "the effect size isn’t huge."
At intake, the 63 patients who later converted to BP I/II were significantly more likely to have a family history of mania or hypomania (64%) or depression (90%), compared with the 77 patients who did not convert to BP I/II (40% and 78%), respectively.
A total of 58% of youths with a family history of mania or hypomania converted to BP I/II by a median 5-year follow-up, compared with 36% of youths without this family history. The newest data suggest that by 8 years, two-thirds of youths with a family history of mania or hypomania convert to BP I/II, compared with just under half of youths without this family history, he reported.
"One thing that’s interesting is the progression rate keeps going up in both groups if you follow them longer," Dr. Axelson said. "These kids continue to go forward in converting to bipolar illness."
A multivariate analysis found that a family history of mania or hypomania tripled the risk for progression to BP I/II. So did white race, which "we can’t really explain," he said. Any lifetime history of psychiatric hospitalization multiplied the risk for progression 2.5 times. Higher scores on the Young Mania Rating Scale in the past month increased the risk of progression by 3%, which was statistically significant.
Any lifetime history of psychotic symptoms, however, was significantly and negatively associated with progression to BP I/II, "something we still don’t fully understand," Dr. Axelson said. Patients with a history of psychotic symptoms were 71% less likely to convert to BP I/II.
Having a family history of mania or hypomania is "a useful predictor, because more kids with family history did convert, however it’s not so strong that you can say it’s definitive," he said. "Lots of kids who had a family history didn’t progress, and a full third of the kids who didn’t have a family history progressed."
Dr. Axelson reported having no financial disclosures.
SAN FRANCISCO – When youths get referred for help with symptoms that don’t quite meet diagnostic criteria for bipolar illness, there’s a 50-50 chance they’ll progress to a diagnosis of bipolar disorder I or II within 7 years. The odds are a coin toss.
The risk logically might be even lower in general clinical settings than in this defined group. That’s why Dr. David A. Axelson and his associates advocate using conservative criteria for diagnosing "bipolar not otherwise specified" (BP-NOS) in general clinics.
Dr. Axelson won the American Academy of Child and Adolescent Psychiatry’s Klingenstein Third Generation Foundation Award for his longitudinal research on 140 children and adolescents who met an operationalized diagnosis of BP-NOS. At a median follow-up of 5 years, 45% had converted to bipolar disorder I or II (BP I/II) within a mean of 58 weeks after intake (J. Am. Acad. Child. Adolesc. Psychiatry 2011;50:1001-16.e3).
New data from the ongoing study show that 50% progressed to BP I/II at a median follow-up of 7 years, he said at the academy’s annual meeting. Symptoms for most of the youths in the COBY (Course and Outcome of Bipolar Youth) study far exceeded the minimum BP-NOS criteria at baseline.
Very few factors predicted whether patients would convert to BP I/II or not, and even those were not strong predictors, said Dr. Axelson, medical director of Child and Adolescent Bipolar Services Outpatient Program at the University of Pittsburgh’s Western Psychiatric Institute and Clinic.
Many children and adolescents present to clinics with manic symptomatology that does not meet diagnostic criteria for BP I/II in the DSM-IV. Clinicians walk a tightrope between intervening as early as possible for best treatment results and mislabeling (and then mistreating) some youths who don’t have bipolar illness.
The criteria for BP-NOS in the DSM-IV are vague and nonspecific, Dr. Axelson said. Based on his and other studies of "subthreshold" bipolar symptoms in children and adolescents, Dr. Axelson proposed that criteria for diagnosing BP-NOS in general clinical settings include:
• Use of full DSM symptom criteria for a hypomanic or manic episode.
Almost all of the children and adolescents in his COBY study met medical criteria for symptoms, he noted.
• Having hypomanic symptoms for most of the day.
"Similar to what we think about for major depression," Dr. Axelson said. "This most-of-the-day specifier will be in DSM 5 for manic or hypomanic episodes."
• At least one episode of 2-day duration.
• At least four recurrent episodes.
Almost all the children and adolescents with BP-NOS in the COBY study already had recurrent episodes.
These criteria are "probably the best balance between sensitivity and specificity, understanding the fact that this is going to miss some kids in the early phase of illness," he said.
The COBY study enrolled 153 youths seen at three academic medical centers, 140 of whom had at least one follow-up visit. The main reasons the diagnosis was BP-NOS instead of BP I/II were because the duration of manic or hypomanic episodes was too short (only 1-3 days in 86% of patients); the youth had hypomania with no major depressive episode (11%); or the youth did not have the required number of symptoms for BP I/II (3%).
The investigators tracked at least 17 factors that they hypothesized might help predict which youths would progress to BP I/II. "Much to my surprise, very little of this actually predicted future onset," Dr. Axelson said. The main predictor was a family history of mania or hypomania and, "the effect size isn’t huge."
At intake, the 63 patients who later converted to BP I/II were significantly more likely to have a family history of mania or hypomania (64%) or depression (90%), compared with the 77 patients who did not convert to BP I/II (40% and 78%), respectively.
A total of 58% of youths with a family history of mania or hypomania converted to BP I/II by a median 5-year follow-up, compared with 36% of youths without this family history. The newest data suggest that by 8 years, two-thirds of youths with a family history of mania or hypomania convert to BP I/II, compared with just under half of youths without this family history, he reported.
"One thing that’s interesting is the progression rate keeps going up in both groups if you follow them longer," Dr. Axelson said. "These kids continue to go forward in converting to bipolar illness."
A multivariate analysis found that a family history of mania or hypomania tripled the risk for progression to BP I/II. So did white race, which "we can’t really explain," he said. Any lifetime history of psychiatric hospitalization multiplied the risk for progression 2.5 times. Higher scores on the Young Mania Rating Scale in the past month increased the risk of progression by 3%, which was statistically significant.
Any lifetime history of psychotic symptoms, however, was significantly and negatively associated with progression to BP I/II, "something we still don’t fully understand," Dr. Axelson said. Patients with a history of psychotic symptoms were 71% less likely to convert to BP I/II.
Having a family history of mania or hypomania is "a useful predictor, because more kids with family history did convert, however it’s not so strong that you can say it’s definitive," he said. "Lots of kids who had a family history didn’t progress, and a full third of the kids who didn’t have a family history progressed."
Dr. Axelson reported having no financial disclosures.
SAN FRANCISCO – When youths get referred for help with symptoms that don’t quite meet diagnostic criteria for bipolar illness, there’s a 50-50 chance they’ll progress to a diagnosis of bipolar disorder I or II within 7 years. The odds are a coin toss.
The risk logically might be even lower in general clinical settings than in this defined group. That’s why Dr. David A. Axelson and his associates advocate using conservative criteria for diagnosing "bipolar not otherwise specified" (BP-NOS) in general clinics.
Dr. Axelson won the American Academy of Child and Adolescent Psychiatry’s Klingenstein Third Generation Foundation Award for his longitudinal research on 140 children and adolescents who met an operationalized diagnosis of BP-NOS. At a median follow-up of 5 years, 45% had converted to bipolar disorder I or II (BP I/II) within a mean of 58 weeks after intake (J. Am. Acad. Child. Adolesc. Psychiatry 2011;50:1001-16.e3).
New data from the ongoing study show that 50% progressed to BP I/II at a median follow-up of 7 years, he said at the academy’s annual meeting. Symptoms for most of the youths in the COBY (Course and Outcome of Bipolar Youth) study far exceeded the minimum BP-NOS criteria at baseline.
Very few factors predicted whether patients would convert to BP I/II or not, and even those were not strong predictors, said Dr. Axelson, medical director of Child and Adolescent Bipolar Services Outpatient Program at the University of Pittsburgh’s Western Psychiatric Institute and Clinic.
Many children and adolescents present to clinics with manic symptomatology that does not meet diagnostic criteria for BP I/II in the DSM-IV. Clinicians walk a tightrope between intervening as early as possible for best treatment results and mislabeling (and then mistreating) some youths who don’t have bipolar illness.
The criteria for BP-NOS in the DSM-IV are vague and nonspecific, Dr. Axelson said. Based on his and other studies of "subthreshold" bipolar symptoms in children and adolescents, Dr. Axelson proposed that criteria for diagnosing BP-NOS in general clinical settings include:
• Use of full DSM symptom criteria for a hypomanic or manic episode.
Almost all of the children and adolescents in his COBY study met medical criteria for symptoms, he noted.
• Having hypomanic symptoms for most of the day.
"Similar to what we think about for major depression," Dr. Axelson said. "This most-of-the-day specifier will be in DSM 5 for manic or hypomanic episodes."
• At least one episode of 2-day duration.
• At least four recurrent episodes.
Almost all the children and adolescents with BP-NOS in the COBY study already had recurrent episodes.
These criteria are "probably the best balance between sensitivity and specificity, understanding the fact that this is going to miss some kids in the early phase of illness," he said.
The COBY study enrolled 153 youths seen at three academic medical centers, 140 of whom had at least one follow-up visit. The main reasons the diagnosis was BP-NOS instead of BP I/II were because the duration of manic or hypomanic episodes was too short (only 1-3 days in 86% of patients); the youth had hypomania with no major depressive episode (11%); or the youth did not have the required number of symptoms for BP I/II (3%).
The investigators tracked at least 17 factors that they hypothesized might help predict which youths would progress to BP I/II. "Much to my surprise, very little of this actually predicted future onset," Dr. Axelson said. The main predictor was a family history of mania or hypomania and, "the effect size isn’t huge."
At intake, the 63 patients who later converted to BP I/II were significantly more likely to have a family history of mania or hypomania (64%) or depression (90%), compared with the 77 patients who did not convert to BP I/II (40% and 78%), respectively.
A total of 58% of youths with a family history of mania or hypomania converted to BP I/II by a median 5-year follow-up, compared with 36% of youths without this family history. The newest data suggest that by 8 years, two-thirds of youths with a family history of mania or hypomania convert to BP I/II, compared with just under half of youths without this family history, he reported.
"One thing that’s interesting is the progression rate keeps going up in both groups if you follow them longer," Dr. Axelson said. "These kids continue to go forward in converting to bipolar illness."
A multivariate analysis found that a family history of mania or hypomania tripled the risk for progression to BP I/II. So did white race, which "we can’t really explain," he said. Any lifetime history of psychiatric hospitalization multiplied the risk for progression 2.5 times. Higher scores on the Young Mania Rating Scale in the past month increased the risk of progression by 3%, which was statistically significant.
Any lifetime history of psychotic symptoms, however, was significantly and negatively associated with progression to BP I/II, "something we still don’t fully understand," Dr. Axelson said. Patients with a history of psychotic symptoms were 71% less likely to convert to BP I/II.
Having a family history of mania or hypomania is "a useful predictor, because more kids with family history did convert, however it’s not so strong that you can say it’s definitive," he said. "Lots of kids who had a family history didn’t progress, and a full third of the kids who didn’t have a family history progressed."
Dr. Axelson reported having no financial disclosures.
AT THE ANNUAL MEETING OF THE AMERICAN ACADEMY OF CHILD AND ADOLESCENT PSYCHIATRY
Major Finding: Half of youths referred for BP-NOS progressed to a diagnosis of bipolar disorder I or II within a mean of 7 years.
Data Source: Ongoing longitudinal study of 140 children and adolescents referred for symptoms that don’t quite meet diagnostic criteria for BP I/II.
Disclosures: Dr. Axelson reported having no financial disclosures.
Acetaminophen: Effect on Drinkers' ALT Levels Appears Safe
SAN DIEGO – Giving acetaminophen to patients who reported consuming ethanol did not adversely affect markers of liver damage in a meta-analysis of randomized, controlled trials.
"One of the questions we often get asked is the role of acetaminophen in patients with liver disease," according to Dr. Kennon J. Heard, who is an emergency medicine physician at the University of Colorado and director of the Medical Toxicology Fellowship at the Rocky Mountain Poison and Drug Center, Denver.
The findings of the meta-analysis suggest that "acetaminophen is safe in alcoholics," Dr. Heard said at the annual meeting of the Society of Hospital Medicine.
The meta-analysis included five trials involving 901 subjects (including patients who reported drinking ethanol) who were randomized to receive acetaminophen or placebo.
Dr. Heard and his associates looked at daily ALT measurements out to a mean of 4 days, a time period for which most of the studies had data.
They also looked for any evidence of liver injury or dysfunction, hepatotoxicity, or death.
The alanine aminotransferase (ALT) levels changed by a mean of 0.04 IU/L after starting acetaminophen or placebo, "less than a tenth of a point in ALT," reported Dr. Heard.
"Essentially, in this group of patients who consume alcohol, if you give them acetaminophen for 4 days, you don’t see any change in their ALT," according to Dr. Heard.
The study is to be published in the journal Pharmacotherapy.
When acetaminophen consumption continued beyond 4 days, ALT levels increased in most patients who consumed alcohol but also increased in 60% of nondrinkers.
"The changes in the alcoholics look exactly like the changes in the nonalcoholics," he said.
The median increase in ALT was between 10-20 IU/L.
Among patients who drink alcohol, the highest ALT level in the acetaminophen group was 312 IU/L, "which is pretty impressive until you see that in the placebo group, somebody went up 288" IU/L, he said.
The biggest increase in ALT was in a healthy nondrinking patient on acetaminophen, whose ALT increased by 638 IU/L.
Most importantly, none of the 551 people who received acetaminophen in those trials developed an increase in International Normalized Ratio, bilirubin level, or symptomatic liver injury, Dr. Heard and his associates found.
Dr. Heard said that he and his associates are now in the process of finishing a separate study that appears to confirm that these are asymptomatic, self-limiting elevations in ALT that will go away even if people stay on acetaminophen.
Such information is valuable, he said. "It is worth knowing that if you have someone who has an ALT elevation while taking acetaminophen, it may be the cause, and it is reasonable to stop the acetaminophen and see if their ALT elevations go away rather than do an extensive work-up for hepatitis," Dr. Heard said.
SAN DIEGO – Giving acetaminophen to patients who reported consuming ethanol did not adversely affect markers of liver damage in a meta-analysis of randomized, controlled trials.
"One of the questions we often get asked is the role of acetaminophen in patients with liver disease," according to Dr. Kennon J. Heard, who is an emergency medicine physician at the University of Colorado and director of the Medical Toxicology Fellowship at the Rocky Mountain Poison and Drug Center, Denver.
The findings of the meta-analysis suggest that "acetaminophen is safe in alcoholics," Dr. Heard said at the annual meeting of the Society of Hospital Medicine.
The meta-analysis included five trials involving 901 subjects (including patients who reported drinking ethanol) who were randomized to receive acetaminophen or placebo.
Dr. Heard and his associates looked at daily ALT measurements out to a mean of 4 days, a time period for which most of the studies had data.
They also looked for any evidence of liver injury or dysfunction, hepatotoxicity, or death.
The alanine aminotransferase (ALT) levels changed by a mean of 0.04 IU/L after starting acetaminophen or placebo, "less than a tenth of a point in ALT," reported Dr. Heard.
"Essentially, in this group of patients who consume alcohol, if you give them acetaminophen for 4 days, you don’t see any change in their ALT," according to Dr. Heard.
The study is to be published in the journal Pharmacotherapy.
When acetaminophen consumption continued beyond 4 days, ALT levels increased in most patients who consumed alcohol but also increased in 60% of nondrinkers.
"The changes in the alcoholics look exactly like the changes in the nonalcoholics," he said.
The median increase in ALT was between 10-20 IU/L.
Among patients who drink alcohol, the highest ALT level in the acetaminophen group was 312 IU/L, "which is pretty impressive until you see that in the placebo group, somebody went up 288" IU/L, he said.
The biggest increase in ALT was in a healthy nondrinking patient on acetaminophen, whose ALT increased by 638 IU/L.
Most importantly, none of the 551 people who received acetaminophen in those trials developed an increase in International Normalized Ratio, bilirubin level, or symptomatic liver injury, Dr. Heard and his associates found.
Dr. Heard said that he and his associates are now in the process of finishing a separate study that appears to confirm that these are asymptomatic, self-limiting elevations in ALT that will go away even if people stay on acetaminophen.
Such information is valuable, he said. "It is worth knowing that if you have someone who has an ALT elevation while taking acetaminophen, it may be the cause, and it is reasonable to stop the acetaminophen and see if their ALT elevations go away rather than do an extensive work-up for hepatitis," Dr. Heard said.
SAN DIEGO – Giving acetaminophen to patients who reported consuming ethanol did not adversely affect markers of liver damage in a meta-analysis of randomized, controlled trials.
"One of the questions we often get asked is the role of acetaminophen in patients with liver disease," according to Dr. Kennon J. Heard, who is an emergency medicine physician at the University of Colorado and director of the Medical Toxicology Fellowship at the Rocky Mountain Poison and Drug Center, Denver.
The findings of the meta-analysis suggest that "acetaminophen is safe in alcoholics," Dr. Heard said at the annual meeting of the Society of Hospital Medicine.
The meta-analysis included five trials involving 901 subjects (including patients who reported drinking ethanol) who were randomized to receive acetaminophen or placebo.
Dr. Heard and his associates looked at daily ALT measurements out to a mean of 4 days, a time period for which most of the studies had data.
They also looked for any evidence of liver injury or dysfunction, hepatotoxicity, or death.
The alanine aminotransferase (ALT) levels changed by a mean of 0.04 IU/L after starting acetaminophen or placebo, "less than a tenth of a point in ALT," reported Dr. Heard.
"Essentially, in this group of patients who consume alcohol, if you give them acetaminophen for 4 days, you don’t see any change in their ALT," according to Dr. Heard.
The study is to be published in the journal Pharmacotherapy.
When acetaminophen consumption continued beyond 4 days, ALT levels increased in most patients who consumed alcohol but also increased in 60% of nondrinkers.
"The changes in the alcoholics look exactly like the changes in the nonalcoholics," he said.
The median increase in ALT was between 10-20 IU/L.
Among patients who drink alcohol, the highest ALT level in the acetaminophen group was 312 IU/L, "which is pretty impressive until you see that in the placebo group, somebody went up 288" IU/L, he said.
The biggest increase in ALT was in a healthy nondrinking patient on acetaminophen, whose ALT increased by 638 IU/L.
Most importantly, none of the 551 people who received acetaminophen in those trials developed an increase in International Normalized Ratio, bilirubin level, or symptomatic liver injury, Dr. Heard and his associates found.
Dr. Heard said that he and his associates are now in the process of finishing a separate study that appears to confirm that these are asymptomatic, self-limiting elevations in ALT that will go away even if people stay on acetaminophen.
Such information is valuable, he said. "It is worth knowing that if you have someone who has an ALT elevation while taking acetaminophen, it may be the cause, and it is reasonable to stop the acetaminophen and see if their ALT elevations go away rather than do an extensive work-up for hepatitis," Dr. Heard said.
Major Finding: ALT levels changed by a median of 0.04 IU/L in alcohol drinkers and nondrinkers after taking acetaminophen for 4 days, with no significant difference between subjects on acetaminophen or placebo.
Data Source: The meta-analysis of five randomized, controlled trials included 901 subjects.
Disclosures: Dr. Heard has been a consultant or received research grants from Cadence Pharmaceuticals, McNeil Consumer Healthcare, and Cumberland Pharmaceuticals.
Stewardship Team Caught Drug Errors in Hospitalized HIV Patients
SAN FRANCISCO – Medication reviews by an antimicrobial stewardship team often led inpatient physicians to adjust antiretroviral regimens or opportunistic infection drugs in hospitalized patients with HIV, according to a recent study at the University of Michigan, Ann Arbor.
The team, consisting of two physicians and three pharmacists specializing in infectious diseases, assessed medications for 69 HIV-infected patients during 114 hospitalizations from March to December 2011.
"Errors were present both at the time of admission and throughout hospitalization," Jerod L. Nagel, Pharm.D., said in a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Some previous studies have suggested that prescribing errors can be reduced if clinical pharmacists review antiretroviral medications when a patient is admitted, but this may be the first study to integrate daily assessments of antiretroviral therapy and opportunistic infection prophylaxis into the work of a hospital antimicrobial stewardship team, said Dr. Nagel.
Hospitalizations averaged 4 days in duration. The antimicrobial stewardship team identified errors in antiretroviral therapy or opportunistic infection prophylaxis at a mean of 2 days after admission (range, 1-5 days after admission), and made recommendations to the inpatient physician in charge of the patient. All inpatient physicians accepted all of the team’s recommendations reported Dr. Nagel of the University of Michigan, Ann Arbor, and his associates.
As the management of HIV disease has shifted to a chronic-disease model that mainly utilizes outpatient care, hospital providers may be less knowledgeable about the complexities of antiretroviral regimens. The risk of medication errors also is influenced by drug-drug interactions and the need to adjust antiretroviral therapy for acute organ dysfunction that may go undetected throughout hospitalization, he said at the meeting, which was sponsored by the American Society for Microbiology.
Patients in the study ranged in age from 14 to 82 years. They were admitted through the Medicine service in 63% of cases, Surgery in 16%, Hematology/Oncology in 15%, and Pediatrics in 2%; and the rest were admitted through other services.
The antimicrobial stewardship team incorporated into its work flow daily evaluations of the appropriateness of antiretroviral therapy and the dosage regimen (including renal and hepatic adjustments), the appropriateness of regimens and dosages for prophylaxis against opportunistic infections, and clinically significant drug-drug interactions. They evaluated only patients who were on antiretroviral therapy, and so could not assess potential errors in which antiretroviral therapy was omitted completely.
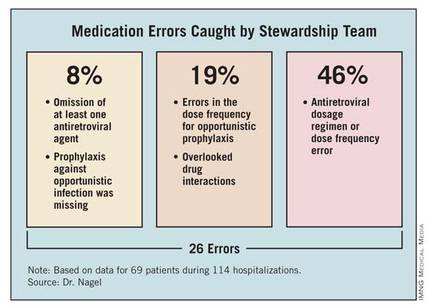
The team identified a total of 26 errors. Of these, 2 involved the omission of at least one antiretroviral agent (8%). Twelve errors involved the antiretroviral dosage regimen incorrectly adjusted for renal impairment or a dose frequency error independent of organ dysfunction (46%). Prophylaxis against opportunistic infection was missing in two patients (8%). The team identified errors in the dose frequency for opportunistic prophylaxis in five patients (19%). Five patients (19%) had clinically significant drug-drug interactions that were not being addressed, involving atazanavir and ranitidine, darunavir and vincristine, or phenytoin and lopinavir/ritonavir.
Enlisting an antimicrobial stewardship team to help manage hospitalized patients with HIV, who are at "a considerable risk of medication errors," might help detect the errors, shorten the duration of their effects, and improve patient care, Dr. Nagel suggested. Computerized systems to reconcile medications and assist clinical decision-making might help prevent these errors, he added.
A tradition of collaboration supports the stewardship team’s work. "We are fortunate to have an excellent working relationship between our hospitalists and clinical pharmacy staff," Dr. Nagel said. "So, implementing an initiative to improve the management of HIV patients by our antibiotic stewardship group wasn’t a major change of culture at our institution. Overall, I think physicians appreciate pharmacy input and don’t view it as ‘correcting’ errors."
The study did not include a historical control group for comparison or analyze clinical and virological outcomes associated with the team’s involvement, but the investigators may pursue these, as well as a cost analysis, in future studies, Dr. Nagel said in an interview.
In general, hospital antimicrobial stewardship teams have started to expand their roles beyond limited functions such as making sure a patient is on the right drug. "We’re trying to focus on a high-risk group and see if we can improve some outcomes," he said.
Dr. Nagel reported having no financial disclosures.
Having the antimicrobial stewardship team on hand to work with hospitalists at the University of Michigan, Ann Arbor, is valuable on several levels, said Dr. Jeffrey Rohde, assistant professor in the Hospital Medicine Program at the University of Michigan.
"In general, collaboration with other clinical professionals in the hospital not only contributes additional support to the increasingly difficult endeavor to care for complicated, acutely ill hospitalized patients, but it also helps to expand a sense of professional satisfaction to us hospitalists as we are able to be part of a like-minded team that is striving for a common goal, to provide the ideal inpatient care experience.
"Hence, this sort of collaboration with clinical pharmacy is very valuable to me as well as other hospitalists, as it is a natural extension of the multidisciplinary care that we provide to our patients every day."
The stewardship team’s presence also opens the door to more precise and accurate prescribing and better dialogue, Dr. Rohde said. "Optimizing medication regimens during an acute hospital stay can be challenging, especially for the wide variety of medications that are prescribed for patients with HIV. The vastly expanding list of new ART [antiretroviral therapy] medications provides both wonderful opportunities to optimize and personalize therapy, but this also presents a significant challenge to general medicine internists to accurately and effectively maintain and adjust these regimens.
"Having infectious disease pharmacy specialists also evaluating regimens and providing timely feedback and suggestions provides opportunities for better patient care. Furthermore, direct face-to-face communication allows for a discussion about different therapeutic options and a consensus to be reached, as opposed to the often unidirectional communication that is all too frequently done via paging."
Personal interaction has trumped technology in contributing to the initiative’s success, observed Dr. Rohde. "We have a strong and long-standing relationship with clinical pharmacy who round with the hospitalists daily, which serves as a wonderful foundation for such initiatives. Given the quality of the recommendations we receive from the clinical pharmacists and the antibiotic stewardship team, it is no surprise that all of their interventions were accepted and implemented. Some medication alerts have been built into our EMR [electronic medical record] and CPOE [computerized physician order entry] systems; however, these alerts all too often simply result in alert fatigue and are oftentimes only cursively evaluated.
"Having a discussion about how clinically important certain medication interactions and adjustments are is certainly more rewarding, informative, and beneficial than simply clicking on a pop-up box that is automatically generated," Dr. Rohde said.
"This pilot initiative is a great example arguing for the implementation of expanded medication reconciliation services for specialized patient populations with complex medication regimens."
Having the antimicrobial stewardship team on hand to work with hospitalists at the University of Michigan, Ann Arbor, is valuable on several levels, said Dr. Jeffrey Rohde, assistant professor in the Hospital Medicine Program at the University of Michigan.
"In general, collaboration with other clinical professionals in the hospital not only contributes additional support to the increasingly difficult endeavor to care for complicated, acutely ill hospitalized patients, but it also helps to expand a sense of professional satisfaction to us hospitalists as we are able to be part of a like-minded team that is striving for a common goal, to provide the ideal inpatient care experience.
"Hence, this sort of collaboration with clinical pharmacy is very valuable to me as well as other hospitalists, as it is a natural extension of the multidisciplinary care that we provide to our patients every day."
The stewardship team’s presence also opens the door to more precise and accurate prescribing and better dialogue, Dr. Rohde said. "Optimizing medication regimens during an acute hospital stay can be challenging, especially for the wide variety of medications that are prescribed for patients with HIV. The vastly expanding list of new ART [antiretroviral therapy] medications provides both wonderful opportunities to optimize and personalize therapy, but this also presents a significant challenge to general medicine internists to accurately and effectively maintain and adjust these regimens.
"Having infectious disease pharmacy specialists also evaluating regimens and providing timely feedback and suggestions provides opportunities for better patient care. Furthermore, direct face-to-face communication allows for a discussion about different therapeutic options and a consensus to be reached, as opposed to the often unidirectional communication that is all too frequently done via paging."
Personal interaction has trumped technology in contributing to the initiative’s success, observed Dr. Rohde. "We have a strong and long-standing relationship with clinical pharmacy who round with the hospitalists daily, which serves as a wonderful foundation for such initiatives. Given the quality of the recommendations we receive from the clinical pharmacists and the antibiotic stewardship team, it is no surprise that all of their interventions were accepted and implemented. Some medication alerts have been built into our EMR [electronic medical record] and CPOE [computerized physician order entry] systems; however, these alerts all too often simply result in alert fatigue and are oftentimes only cursively evaluated.
"Having a discussion about how clinically important certain medication interactions and adjustments are is certainly more rewarding, informative, and beneficial than simply clicking on a pop-up box that is automatically generated," Dr. Rohde said.
"This pilot initiative is a great example arguing for the implementation of expanded medication reconciliation services for specialized patient populations with complex medication regimens."
Having the antimicrobial stewardship team on hand to work with hospitalists at the University of Michigan, Ann Arbor, is valuable on several levels, said Dr. Jeffrey Rohde, assistant professor in the Hospital Medicine Program at the University of Michigan.
"In general, collaboration with other clinical professionals in the hospital not only contributes additional support to the increasingly difficult endeavor to care for complicated, acutely ill hospitalized patients, but it also helps to expand a sense of professional satisfaction to us hospitalists as we are able to be part of a like-minded team that is striving for a common goal, to provide the ideal inpatient care experience.
"Hence, this sort of collaboration with clinical pharmacy is very valuable to me as well as other hospitalists, as it is a natural extension of the multidisciplinary care that we provide to our patients every day."
The stewardship team’s presence also opens the door to more precise and accurate prescribing and better dialogue, Dr. Rohde said. "Optimizing medication regimens during an acute hospital stay can be challenging, especially for the wide variety of medications that are prescribed for patients with HIV. The vastly expanding list of new ART [antiretroviral therapy] medications provides both wonderful opportunities to optimize and personalize therapy, but this also presents a significant challenge to general medicine internists to accurately and effectively maintain and adjust these regimens.
"Having infectious disease pharmacy specialists also evaluating regimens and providing timely feedback and suggestions provides opportunities for better patient care. Furthermore, direct face-to-face communication allows for a discussion about different therapeutic options and a consensus to be reached, as opposed to the often unidirectional communication that is all too frequently done via paging."
Personal interaction has trumped technology in contributing to the initiative’s success, observed Dr. Rohde. "We have a strong and long-standing relationship with clinical pharmacy who round with the hospitalists daily, which serves as a wonderful foundation for such initiatives. Given the quality of the recommendations we receive from the clinical pharmacists and the antibiotic stewardship team, it is no surprise that all of their interventions were accepted and implemented. Some medication alerts have been built into our EMR [electronic medical record] and CPOE [computerized physician order entry] systems; however, these alerts all too often simply result in alert fatigue and are oftentimes only cursively evaluated.
"Having a discussion about how clinically important certain medication interactions and adjustments are is certainly more rewarding, informative, and beneficial than simply clicking on a pop-up box that is automatically generated," Dr. Rohde said.
"This pilot initiative is a great example arguing for the implementation of expanded medication reconciliation services for specialized patient populations with complex medication regimens."
SAN FRANCISCO – Medication reviews by an antimicrobial stewardship team often led inpatient physicians to adjust antiretroviral regimens or opportunistic infection drugs in hospitalized patients with HIV, according to a recent study at the University of Michigan, Ann Arbor.
The team, consisting of two physicians and three pharmacists specializing in infectious diseases, assessed medications for 69 HIV-infected patients during 114 hospitalizations from March to December 2011.
"Errors were present both at the time of admission and throughout hospitalization," Jerod L. Nagel, Pharm.D., said in a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Some previous studies have suggested that prescribing errors can be reduced if clinical pharmacists review antiretroviral medications when a patient is admitted, but this may be the first study to integrate daily assessments of antiretroviral therapy and opportunistic infection prophylaxis into the work of a hospital antimicrobial stewardship team, said Dr. Nagel.
Hospitalizations averaged 4 days in duration. The antimicrobial stewardship team identified errors in antiretroviral therapy or opportunistic infection prophylaxis at a mean of 2 days after admission (range, 1-5 days after admission), and made recommendations to the inpatient physician in charge of the patient. All inpatient physicians accepted all of the team’s recommendations reported Dr. Nagel of the University of Michigan, Ann Arbor, and his associates.
As the management of HIV disease has shifted to a chronic-disease model that mainly utilizes outpatient care, hospital providers may be less knowledgeable about the complexities of antiretroviral regimens. The risk of medication errors also is influenced by drug-drug interactions and the need to adjust antiretroviral therapy for acute organ dysfunction that may go undetected throughout hospitalization, he said at the meeting, which was sponsored by the American Society for Microbiology.
Patients in the study ranged in age from 14 to 82 years. They were admitted through the Medicine service in 63% of cases, Surgery in 16%, Hematology/Oncology in 15%, and Pediatrics in 2%; and the rest were admitted through other services.
The antimicrobial stewardship team incorporated into its work flow daily evaluations of the appropriateness of antiretroviral therapy and the dosage regimen (including renal and hepatic adjustments), the appropriateness of regimens and dosages for prophylaxis against opportunistic infections, and clinically significant drug-drug interactions. They evaluated only patients who were on antiretroviral therapy, and so could not assess potential errors in which antiretroviral therapy was omitted completely.
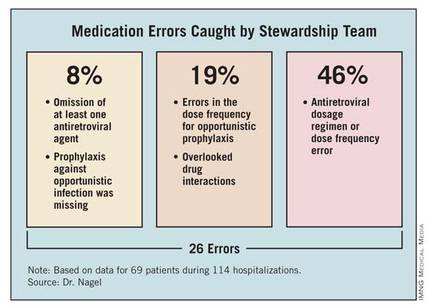
The team identified a total of 26 errors. Of these, 2 involved the omission of at least one antiretroviral agent (8%). Twelve errors involved the antiretroviral dosage regimen incorrectly adjusted for renal impairment or a dose frequency error independent of organ dysfunction (46%). Prophylaxis against opportunistic infection was missing in two patients (8%). The team identified errors in the dose frequency for opportunistic prophylaxis in five patients (19%). Five patients (19%) had clinically significant drug-drug interactions that were not being addressed, involving atazanavir and ranitidine, darunavir and vincristine, or phenytoin and lopinavir/ritonavir.
Enlisting an antimicrobial stewardship team to help manage hospitalized patients with HIV, who are at "a considerable risk of medication errors," might help detect the errors, shorten the duration of their effects, and improve patient care, Dr. Nagel suggested. Computerized systems to reconcile medications and assist clinical decision-making might help prevent these errors, he added.
A tradition of collaboration supports the stewardship team’s work. "We are fortunate to have an excellent working relationship between our hospitalists and clinical pharmacy staff," Dr. Nagel said. "So, implementing an initiative to improve the management of HIV patients by our antibiotic stewardship group wasn’t a major change of culture at our institution. Overall, I think physicians appreciate pharmacy input and don’t view it as ‘correcting’ errors."
The study did not include a historical control group for comparison or analyze clinical and virological outcomes associated with the team’s involvement, but the investigators may pursue these, as well as a cost analysis, in future studies, Dr. Nagel said in an interview.
In general, hospital antimicrobial stewardship teams have started to expand their roles beyond limited functions such as making sure a patient is on the right drug. "We’re trying to focus on a high-risk group and see if we can improve some outcomes," he said.
Dr. Nagel reported having no financial disclosures.
SAN FRANCISCO – Medication reviews by an antimicrobial stewardship team often led inpatient physicians to adjust antiretroviral regimens or opportunistic infection drugs in hospitalized patients with HIV, according to a recent study at the University of Michigan, Ann Arbor.
The team, consisting of two physicians and three pharmacists specializing in infectious diseases, assessed medications for 69 HIV-infected patients during 114 hospitalizations from March to December 2011.
"Errors were present both at the time of admission and throughout hospitalization," Jerod L. Nagel, Pharm.D., said in a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Some previous studies have suggested that prescribing errors can be reduced if clinical pharmacists review antiretroviral medications when a patient is admitted, but this may be the first study to integrate daily assessments of antiretroviral therapy and opportunistic infection prophylaxis into the work of a hospital antimicrobial stewardship team, said Dr. Nagel.
Hospitalizations averaged 4 days in duration. The antimicrobial stewardship team identified errors in antiretroviral therapy or opportunistic infection prophylaxis at a mean of 2 days after admission (range, 1-5 days after admission), and made recommendations to the inpatient physician in charge of the patient. All inpatient physicians accepted all of the team’s recommendations reported Dr. Nagel of the University of Michigan, Ann Arbor, and his associates.
As the management of HIV disease has shifted to a chronic-disease model that mainly utilizes outpatient care, hospital providers may be less knowledgeable about the complexities of antiretroviral regimens. The risk of medication errors also is influenced by drug-drug interactions and the need to adjust antiretroviral therapy for acute organ dysfunction that may go undetected throughout hospitalization, he said at the meeting, which was sponsored by the American Society for Microbiology.
Patients in the study ranged in age from 14 to 82 years. They were admitted through the Medicine service in 63% of cases, Surgery in 16%, Hematology/Oncology in 15%, and Pediatrics in 2%; and the rest were admitted through other services.
The antimicrobial stewardship team incorporated into its work flow daily evaluations of the appropriateness of antiretroviral therapy and the dosage regimen (including renal and hepatic adjustments), the appropriateness of regimens and dosages for prophylaxis against opportunistic infections, and clinically significant drug-drug interactions. They evaluated only patients who were on antiretroviral therapy, and so could not assess potential errors in which antiretroviral therapy was omitted completely.
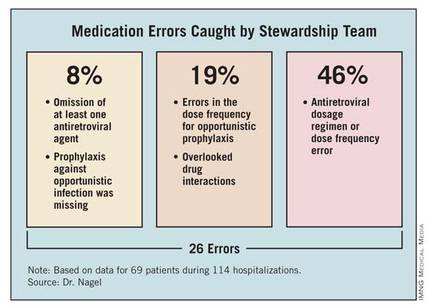
The team identified a total of 26 errors. Of these, 2 involved the omission of at least one antiretroviral agent (8%). Twelve errors involved the antiretroviral dosage regimen incorrectly adjusted for renal impairment or a dose frequency error independent of organ dysfunction (46%). Prophylaxis against opportunistic infection was missing in two patients (8%). The team identified errors in the dose frequency for opportunistic prophylaxis in five patients (19%). Five patients (19%) had clinically significant drug-drug interactions that were not being addressed, involving atazanavir and ranitidine, darunavir and vincristine, or phenytoin and lopinavir/ritonavir.
Enlisting an antimicrobial stewardship team to help manage hospitalized patients with HIV, who are at "a considerable risk of medication errors," might help detect the errors, shorten the duration of their effects, and improve patient care, Dr. Nagel suggested. Computerized systems to reconcile medications and assist clinical decision-making might help prevent these errors, he added.
A tradition of collaboration supports the stewardship team’s work. "We are fortunate to have an excellent working relationship between our hospitalists and clinical pharmacy staff," Dr. Nagel said. "So, implementing an initiative to improve the management of HIV patients by our antibiotic stewardship group wasn’t a major change of culture at our institution. Overall, I think physicians appreciate pharmacy input and don’t view it as ‘correcting’ errors."
The study did not include a historical control group for comparison or analyze clinical and virological outcomes associated with the team’s involvement, but the investigators may pursue these, as well as a cost analysis, in future studies, Dr. Nagel said in an interview.
In general, hospital antimicrobial stewardship teams have started to expand their roles beyond limited functions such as making sure a patient is on the right drug. "We’re trying to focus on a high-risk group and see if we can improve some outcomes," he said.
Dr. Nagel reported having no financial disclosures.
AT THE ANNUAL INTERSCIENCE CONFERENCE ON ANTIMICROBIAL AGENTS AND CHEMOTHERAPY
Major Finding: An antimicrobial stewardship team identified 26 errors associated with HIV-associated medications in 69 hospitalized patients with HIV over a 9-month period.
Data Source: This was a prospective study using a team for daily evaluation of drug regimens in HIV-infected patients at one institution from March to December 2011.
Disclosures: Dr. Nagel reported having no financial disclosures.
UV Light Beat Bleach for C. difficile Decontamination
SAN FRANCISCO – The M.D. Anderson Cancer Center is abandoning bleach for cleaning hospital rooms exposed to Clostridium difficile in favor of a new machine that kills the organism using ultraviolet light.
The machine reduced C. difficile counts as much as, or more than, bleach cleaning in a preliminary prospective trial in 30 hospital rooms previously occupied by patients infected with C. difficile. The machine is a bit more expensive than bleach at a cost of approximately $82,000 (or $3,000-$4,000 per month to lease), but it avoids damage to materials and the toxic environment for workers caused by the use of bleach or other corrosive chemicals, Dr. Shashank S. Ghantoji said in an interview at a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Bleach treatment reduced the average number of colony-forming units of C. difficile from 2.39 before cleaning to 0.71, a 70% reduction in the contamination level. Treatment with the Pulsed Xenon UV machine (PX-UV) reduced the average number of colony-forming units from 22.97 to 1.10, a 95% reduction.
The postcleaning contamination levels were not statistically different between the bleach and PX-UV rooms, Dr. Ghantoji and his associates found. However, PX-UV decontamination is faster than using bleach, Dr. Ghantoji said. "It takes at least 45 minutes to clean a room with bleach, and it’s not good for the patients or the health care professionals," plus admissions staff usually are clamoring for the room to be ready as soon as possible, he said. Cleaning a room using the PX-UV method takes perhaps 15 minutes.
The PX-UV machine has been available for some time, but its adoption depends on how proactive hospital infection control teams are, he added. He said he is aware of at least two medical centers beyond M.D. Anderson that are also using the machine.
In the study, 298 samples were taken before and after cleaning from high-touch surfaces – the bathroom handrail, the bed control panel, the bed rail, the top of the bedside table, and the IV pole control panel or other equipment control panel – and analyzed for C. difficile endospores. Fifteen rooms were cleaned by the conventional method using a 1:10 solution of sodium hypochlorite (bleach), and 15 underwent a visual, nonbleach cleaning of surfaces followed by 15 minutes of treatment with the PX-UV.
With the PX-UV method, housekeeping workers clean the bathroom and place the remote-operated PX-UV in the bathroom with the door shut while they finish cleaning the rest of the room. Then the machine is placed on each side of the bed for 4 minutes of operation with workers gone. Sensors stop the machine if any movement is detected.
It works by emitting ultraviolet C light, which kills C. difficile. And here’s a bonus – it also kills vancomycin-resistant enterococci and methicillin-resistant Staphylococcus aureus, Dr. Ghantoji of M.D. Anderson, Houston, said at the meeting, sponsored by the American Society for Microbiology.
"The PX-UV method may be a promising alternative to the current standard of decontamination, bleach," he said. Future studies should look at whether the PX-UV method decreases not just endospore counts but transmission of C. difficile, he added.
C. difficile causes more than 300,000 health care–associated infections each year in the United States, incurring $2,500-$3,500 in costs per infection aside from any surgical costs, he estimated. Current guidelines recommend that rooms previously occupied by patients infected with C. difficile be cleaned with a disinfectant registered with the Environmental Protection Agency as effective against the organism.
Xenex Healthcare Services, which markets the PX-UV machine, funded the study, and two of the investigators are employees of the company. Dr. Ghantoji reported having no other relevant financial disclosures.
SAN FRANCISCO – The M.D. Anderson Cancer Center is abandoning bleach for cleaning hospital rooms exposed to Clostridium difficile in favor of a new machine that kills the organism using ultraviolet light.
The machine reduced C. difficile counts as much as, or more than, bleach cleaning in a preliminary prospective trial in 30 hospital rooms previously occupied by patients infected with C. difficile. The machine is a bit more expensive than bleach at a cost of approximately $82,000 (or $3,000-$4,000 per month to lease), but it avoids damage to materials and the toxic environment for workers caused by the use of bleach or other corrosive chemicals, Dr. Shashank S. Ghantoji said in an interview at a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Bleach treatment reduced the average number of colony-forming units of C. difficile from 2.39 before cleaning to 0.71, a 70% reduction in the contamination level. Treatment with the Pulsed Xenon UV machine (PX-UV) reduced the average number of colony-forming units from 22.97 to 1.10, a 95% reduction.
The postcleaning contamination levels were not statistically different between the bleach and PX-UV rooms, Dr. Ghantoji and his associates found. However, PX-UV decontamination is faster than using bleach, Dr. Ghantoji said. "It takes at least 45 minutes to clean a room with bleach, and it’s not good for the patients or the health care professionals," plus admissions staff usually are clamoring for the room to be ready as soon as possible, he said. Cleaning a room using the PX-UV method takes perhaps 15 minutes.
The PX-UV machine has been available for some time, but its adoption depends on how proactive hospital infection control teams are, he added. He said he is aware of at least two medical centers beyond M.D. Anderson that are also using the machine.
In the study, 298 samples were taken before and after cleaning from high-touch surfaces – the bathroom handrail, the bed control panel, the bed rail, the top of the bedside table, and the IV pole control panel or other equipment control panel – and analyzed for C. difficile endospores. Fifteen rooms were cleaned by the conventional method using a 1:10 solution of sodium hypochlorite (bleach), and 15 underwent a visual, nonbleach cleaning of surfaces followed by 15 minutes of treatment with the PX-UV.
With the PX-UV method, housekeeping workers clean the bathroom and place the remote-operated PX-UV in the bathroom with the door shut while they finish cleaning the rest of the room. Then the machine is placed on each side of the bed for 4 minutes of operation with workers gone. Sensors stop the machine if any movement is detected.
It works by emitting ultraviolet C light, which kills C. difficile. And here’s a bonus – it also kills vancomycin-resistant enterococci and methicillin-resistant Staphylococcus aureus, Dr. Ghantoji of M.D. Anderson, Houston, said at the meeting, sponsored by the American Society for Microbiology.
"The PX-UV method may be a promising alternative to the current standard of decontamination, bleach," he said. Future studies should look at whether the PX-UV method decreases not just endospore counts but transmission of C. difficile, he added.
C. difficile causes more than 300,000 health care–associated infections each year in the United States, incurring $2,500-$3,500 in costs per infection aside from any surgical costs, he estimated. Current guidelines recommend that rooms previously occupied by patients infected with C. difficile be cleaned with a disinfectant registered with the Environmental Protection Agency as effective against the organism.
Xenex Healthcare Services, which markets the PX-UV machine, funded the study, and two of the investigators are employees of the company. Dr. Ghantoji reported having no other relevant financial disclosures.
SAN FRANCISCO – The M.D. Anderson Cancer Center is abandoning bleach for cleaning hospital rooms exposed to Clostridium difficile in favor of a new machine that kills the organism using ultraviolet light.
The machine reduced C. difficile counts as much as, or more than, bleach cleaning in a preliminary prospective trial in 30 hospital rooms previously occupied by patients infected with C. difficile. The machine is a bit more expensive than bleach at a cost of approximately $82,000 (or $3,000-$4,000 per month to lease), but it avoids damage to materials and the toxic environment for workers caused by the use of bleach or other corrosive chemicals, Dr. Shashank S. Ghantoji said in an interview at a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Bleach treatment reduced the average number of colony-forming units of C. difficile from 2.39 before cleaning to 0.71, a 70% reduction in the contamination level. Treatment with the Pulsed Xenon UV machine (PX-UV) reduced the average number of colony-forming units from 22.97 to 1.10, a 95% reduction.
The postcleaning contamination levels were not statistically different between the bleach and PX-UV rooms, Dr. Ghantoji and his associates found. However, PX-UV decontamination is faster than using bleach, Dr. Ghantoji said. "It takes at least 45 minutes to clean a room with bleach, and it’s not good for the patients or the health care professionals," plus admissions staff usually are clamoring for the room to be ready as soon as possible, he said. Cleaning a room using the PX-UV method takes perhaps 15 minutes.
The PX-UV machine has been available for some time, but its adoption depends on how proactive hospital infection control teams are, he added. He said he is aware of at least two medical centers beyond M.D. Anderson that are also using the machine.
In the study, 298 samples were taken before and after cleaning from high-touch surfaces – the bathroom handrail, the bed control panel, the bed rail, the top of the bedside table, and the IV pole control panel or other equipment control panel – and analyzed for C. difficile endospores. Fifteen rooms were cleaned by the conventional method using a 1:10 solution of sodium hypochlorite (bleach), and 15 underwent a visual, nonbleach cleaning of surfaces followed by 15 minutes of treatment with the PX-UV.
With the PX-UV method, housekeeping workers clean the bathroom and place the remote-operated PX-UV in the bathroom with the door shut while they finish cleaning the rest of the room. Then the machine is placed on each side of the bed for 4 minutes of operation with workers gone. Sensors stop the machine if any movement is detected.
It works by emitting ultraviolet C light, which kills C. difficile. And here’s a bonus – it also kills vancomycin-resistant enterococci and methicillin-resistant Staphylococcus aureus, Dr. Ghantoji of M.D. Anderson, Houston, said at the meeting, sponsored by the American Society for Microbiology.
"The PX-UV method may be a promising alternative to the current standard of decontamination, bleach," he said. Future studies should look at whether the PX-UV method decreases not just endospore counts but transmission of C. difficile, he added.
C. difficile causes more than 300,000 health care–associated infections each year in the United States, incurring $2,500-$3,500 in costs per infection aside from any surgical costs, he estimated. Current guidelines recommend that rooms previously occupied by patients infected with C. difficile be cleaned with a disinfectant registered with the Environmental Protection Agency as effective against the organism.
Xenex Healthcare Services, which markets the PX-UV machine, funded the study, and two of the investigators are employees of the company. Dr. Ghantoji reported having no other relevant financial disclosures.
Major Finding: Bleach killed 70% of C. difficile spores in hospital rooms compared with 95% decontamination using nonbleach cleaning plus UV light treatment. The difference between groups was not statistically significant.
Data Source: A prospective comparison was performed of the two cleaning methods in 30 rooms after discharge of patients infected with C. difficile.
Disclosures: Xenex Healthcare Services, which markets the PX-UV machine, funded the study, and two of the investigators are employees of the company. Dr. Ghantoji reported having no other relevant financial disclosures.
Promising C. difficile Antibiotic in Pipeline
SAN FRANCISCO – Those desperate for new treatments for Clostridium difficile infection may want to keep an eye on the experimental oral antibiotic cadazolid, which looked promising in an early-phase trial, according to Daniela Baldoni, Pharm.D.
Cadazolid is in the oxazolidinone class of antibiotics. Its mechanism of action consists mainly of bacterial protein-synthesis inhibition.
Cadazolid produced low systemic exposure with high concentrations at the desired site – the colon – and was well tolerated in 64 healthy men who received up to 3,000 mg b.i.d. for 10 days, she reported in a poster presentation at the conference. Dr. Baldoni is employed by Actelion Pharmaceuticals, the company that is developing cadazolid.
The study randomized nonsmoking men aged 45-60 years and a body mass index of 18-32 kg/m2 to single or multiple doses of cadazolid or placebo.
In the single-dose group, 30 fasting subjects received a single dose of 30, 100, 300, 1,000, or 3,000 mg cadazolid and 10 subjects received matching placebo. After a wash-out period of 8-15 days, the six subjects who had taken 300 mg received a second dose of 300 mg after eating instead of after fasting. In the multiple-dose group, 18 subjects took 300, 1,000, or 3,000 mg of cadazolid twice a day and 6 received matching placebo for 10 days.
Taking cadazolid with food appeared to increase the rate and extent of drug absorption by two- to fivefold. Blood samples showed low systemic exposure after single or multiple doses, with a minor, twofold increase in cadazolid in plasma after 10 days for all doses in the twice-a-day group, Dr. Baldoni reported at the meeting, sponsored by the American Society for Microbiology.
The dose or duration of treatment did not seem to affect the number of adverse events (none of which were serious). They occurred in 27%-39% of cadazolid-treated subjects and in 17%-40% taking placebo and were mostly headache or diarrhea.
All subjects completed the study except one man in the 100-mg single-dose subgroup who withdrew consent for reasons unrelated to adverse events.
SAN FRANCISCO – Those desperate for new treatments for Clostridium difficile infection may want to keep an eye on the experimental oral antibiotic cadazolid, which looked promising in an early-phase trial, according to Daniela Baldoni, Pharm.D.
Cadazolid is in the oxazolidinone class of antibiotics. Its mechanism of action consists mainly of bacterial protein-synthesis inhibition.
Cadazolid produced low systemic exposure with high concentrations at the desired site – the colon – and was well tolerated in 64 healthy men who received up to 3,000 mg b.i.d. for 10 days, she reported in a poster presentation at the conference. Dr. Baldoni is employed by Actelion Pharmaceuticals, the company that is developing cadazolid.
The study randomized nonsmoking men aged 45-60 years and a body mass index of 18-32 kg/m2 to single or multiple doses of cadazolid or placebo.
In the single-dose group, 30 fasting subjects received a single dose of 30, 100, 300, 1,000, or 3,000 mg cadazolid and 10 subjects received matching placebo. After a wash-out period of 8-15 days, the six subjects who had taken 300 mg received a second dose of 300 mg after eating instead of after fasting. In the multiple-dose group, 18 subjects took 300, 1,000, or 3,000 mg of cadazolid twice a day and 6 received matching placebo for 10 days.
Taking cadazolid with food appeared to increase the rate and extent of drug absorption by two- to fivefold. Blood samples showed low systemic exposure after single or multiple doses, with a minor, twofold increase in cadazolid in plasma after 10 days for all doses in the twice-a-day group, Dr. Baldoni reported at the meeting, sponsored by the American Society for Microbiology.
The dose or duration of treatment did not seem to affect the number of adverse events (none of which were serious). They occurred in 27%-39% of cadazolid-treated subjects and in 17%-40% taking placebo and were mostly headache or diarrhea.
All subjects completed the study except one man in the 100-mg single-dose subgroup who withdrew consent for reasons unrelated to adverse events.
SAN FRANCISCO – Those desperate for new treatments for Clostridium difficile infection may want to keep an eye on the experimental oral antibiotic cadazolid, which looked promising in an early-phase trial, according to Daniela Baldoni, Pharm.D.
Cadazolid is in the oxazolidinone class of antibiotics. Its mechanism of action consists mainly of bacterial protein-synthesis inhibition.
Cadazolid produced low systemic exposure with high concentrations at the desired site – the colon – and was well tolerated in 64 healthy men who received up to 3,000 mg b.i.d. for 10 days, she reported in a poster presentation at the conference. Dr. Baldoni is employed by Actelion Pharmaceuticals, the company that is developing cadazolid.
The study randomized nonsmoking men aged 45-60 years and a body mass index of 18-32 kg/m2 to single or multiple doses of cadazolid or placebo.
In the single-dose group, 30 fasting subjects received a single dose of 30, 100, 300, 1,000, or 3,000 mg cadazolid and 10 subjects received matching placebo. After a wash-out period of 8-15 days, the six subjects who had taken 300 mg received a second dose of 300 mg after eating instead of after fasting. In the multiple-dose group, 18 subjects took 300, 1,000, or 3,000 mg of cadazolid twice a day and 6 received matching placebo for 10 days.
Taking cadazolid with food appeared to increase the rate and extent of drug absorption by two- to fivefold. Blood samples showed low systemic exposure after single or multiple doses, with a minor, twofold increase in cadazolid in plasma after 10 days for all doses in the twice-a-day group, Dr. Baldoni reported at the meeting, sponsored by the American Society for Microbiology.
The dose or duration of treatment did not seem to affect the number of adverse events (none of which were serious). They occurred in 27%-39% of cadazolid-treated subjects and in 17%-40% taking placebo and were mostly headache or diarrhea.
All subjects completed the study except one man in the 100-mg single-dose subgroup who withdrew consent for reasons unrelated to adverse events.
Major Finding: The experimental antibiotic cadazolid concentrated in feces with low systemic exposure and few side effects after single doses or twice-a-day dosing for 10 days.
Data Source: Data are from a randomized, placebo-controlled study in 64 healthy, nonsmoking men.
Disclosures: Dr. Baldoni and most of her coinvestigators are employees of Actelion Pharmaceuticals, which funded the study.
Higher Dose for Severe C. difficile Speeds Response
SAN FRANCISCO – Two small studies suggest that treating severe Clostridium difficile infection with a higher initial dose of vancomycin may work better than the recommended dose of 125 mg every 6 hours.
The most recent study, presented in a poster at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy, surprised the investigators.
"Pharmacodynamically, the concentrations in stool of the standard dose of 125 mg are about 500-1,000 times greater than the MIC [minimum inhibitory concentration]," Yleana T. Garcia, Pharm.D., said in an interview. "So, we have enough concentration in the stool. We wanted to see that we have similar outcomes with patients who are treated with standard doses as with higher doses."
Instead, the retrospective review of 62 patients with severe diarrhea who received oral vancomycin for at least 3 days found that symptoms resolved significantly quicker in 19 patients who got 250 mg every 6 hours compared with 43 patients who got 125 mg every 6 hours, she and her associates reported.
Symptoms resolved by day 3 in nine patients (47%) on the high dose and six patients (15%) on the conventional dose, said Dr. Garcia, a palliative care fellow at the James J. Peters Veterans Affairs Medical Center, Bronx, N.Y.
There also were statistically nonsignificant trends toward a higher likelihood of clinical cure, shorter length of stay, and reduced risk of recurrence in patients with the higher dose. An increased death rate in the higher-dose group also was not statistically significant, and might be due to greater severity of illness at baseline in patients who got the higher dose of vancomycin, she said at the meeting, sponsored by the American Society for Microbiology.
The findings support those of a small prospective study that analyzed levels of vancomycin in feces collected from 15 patients with presumed or confirmed C. difficile infection. Drug concentrations were high in patients who got 250 or 500 mg q.i.d. but were inadequate in at least one patient on the first day of treatment with 125 mg q.i.d. (BMC Infect. Dis. 2010;10:363).<< http://www.biomedcentral.com/1471-2334/10/363 >>
"Higher doses like 250-500 mg may be warranted to reach adequate concentrations in the stool in the first 24-48 hours," Dr. Garcia said. "I’m not saying to use 250 for the whole treatment course, but there may be a role for a loading dose of 250 mg q6 for the first 24-48 hours, and then switching to 125 mg q6 for the remainder of the treatment course. We know that 125 does have adequate fecal concentration; it just may not be adequate on day 1."
The 2010 update to clinical practice guidelines for C. difficile infection in adults recommends treating severe C. difficile infection with oral vancomycin 125 mg every 6 hours or using 500 mg every 6 hours for patients with severe disease complicated by ileus, megacolon, or hypotension (Infect. Control Hosp. Epidemiol. 2010;31:431-55).
Severe C. difficile infection generally is defined as the presence of the organism plus leukocytosis with a white blood cell count of 15,000 cells/microL or greater, or a serum creatinine level at least 1.5 times baseline. The study reviewed records of patients who received vancomycin for these indications or hypotension, shock, ileus, megacolon, or evidence of colitis. The study excluded patients who were treated with any other medication besides metronidazole.
The study is continuing in order to increase the number of patients reviewed and the power of the findings.
Dr. Garcia reported having no financial disclosures.
SAN FRANCISCO – Two small studies suggest that treating severe Clostridium difficile infection with a higher initial dose of vancomycin may work better than the recommended dose of 125 mg every 6 hours.
The most recent study, presented in a poster at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy, surprised the investigators.
"Pharmacodynamically, the concentrations in stool of the standard dose of 125 mg are about 500-1,000 times greater than the MIC [minimum inhibitory concentration]," Yleana T. Garcia, Pharm.D., said in an interview. "So, we have enough concentration in the stool. We wanted to see that we have similar outcomes with patients who are treated with standard doses as with higher doses."
Instead, the retrospective review of 62 patients with severe diarrhea who received oral vancomycin for at least 3 days found that symptoms resolved significantly quicker in 19 patients who got 250 mg every 6 hours compared with 43 patients who got 125 mg every 6 hours, she and her associates reported.
Symptoms resolved by day 3 in nine patients (47%) on the high dose and six patients (15%) on the conventional dose, said Dr. Garcia, a palliative care fellow at the James J. Peters Veterans Affairs Medical Center, Bronx, N.Y.
There also were statistically nonsignificant trends toward a higher likelihood of clinical cure, shorter length of stay, and reduced risk of recurrence in patients with the higher dose. An increased death rate in the higher-dose group also was not statistically significant, and might be due to greater severity of illness at baseline in patients who got the higher dose of vancomycin, she said at the meeting, sponsored by the American Society for Microbiology.
The findings support those of a small prospective study that analyzed levels of vancomycin in feces collected from 15 patients with presumed or confirmed C. difficile infection. Drug concentrations were high in patients who got 250 or 500 mg q.i.d. but were inadequate in at least one patient on the first day of treatment with 125 mg q.i.d. (BMC Infect. Dis. 2010;10:363).<< http://www.biomedcentral.com/1471-2334/10/363 >>
"Higher doses like 250-500 mg may be warranted to reach adequate concentrations in the stool in the first 24-48 hours," Dr. Garcia said. "I’m not saying to use 250 for the whole treatment course, but there may be a role for a loading dose of 250 mg q6 for the first 24-48 hours, and then switching to 125 mg q6 for the remainder of the treatment course. We know that 125 does have adequate fecal concentration; it just may not be adequate on day 1."
The 2010 update to clinical practice guidelines for C. difficile infection in adults recommends treating severe C. difficile infection with oral vancomycin 125 mg every 6 hours or using 500 mg every 6 hours for patients with severe disease complicated by ileus, megacolon, or hypotension (Infect. Control Hosp. Epidemiol. 2010;31:431-55).
Severe C. difficile infection generally is defined as the presence of the organism plus leukocytosis with a white blood cell count of 15,000 cells/microL or greater, or a serum creatinine level at least 1.5 times baseline. The study reviewed records of patients who received vancomycin for these indications or hypotension, shock, ileus, megacolon, or evidence of colitis. The study excluded patients who were treated with any other medication besides metronidazole.
The study is continuing in order to increase the number of patients reviewed and the power of the findings.
Dr. Garcia reported having no financial disclosures.
SAN FRANCISCO – Two small studies suggest that treating severe Clostridium difficile infection with a higher initial dose of vancomycin may work better than the recommended dose of 125 mg every 6 hours.
The most recent study, presented in a poster at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy, surprised the investigators.
"Pharmacodynamically, the concentrations in stool of the standard dose of 125 mg are about 500-1,000 times greater than the MIC [minimum inhibitory concentration]," Yleana T. Garcia, Pharm.D., said in an interview. "So, we have enough concentration in the stool. We wanted to see that we have similar outcomes with patients who are treated with standard doses as with higher doses."
Instead, the retrospective review of 62 patients with severe diarrhea who received oral vancomycin for at least 3 days found that symptoms resolved significantly quicker in 19 patients who got 250 mg every 6 hours compared with 43 patients who got 125 mg every 6 hours, she and her associates reported.
Symptoms resolved by day 3 in nine patients (47%) on the high dose and six patients (15%) on the conventional dose, said Dr. Garcia, a palliative care fellow at the James J. Peters Veterans Affairs Medical Center, Bronx, N.Y.
There also were statistically nonsignificant trends toward a higher likelihood of clinical cure, shorter length of stay, and reduced risk of recurrence in patients with the higher dose. An increased death rate in the higher-dose group also was not statistically significant, and might be due to greater severity of illness at baseline in patients who got the higher dose of vancomycin, she said at the meeting, sponsored by the American Society for Microbiology.
The findings support those of a small prospective study that analyzed levels of vancomycin in feces collected from 15 patients with presumed or confirmed C. difficile infection. Drug concentrations were high in patients who got 250 or 500 mg q.i.d. but were inadequate in at least one patient on the first day of treatment with 125 mg q.i.d. (BMC Infect. Dis. 2010;10:363).<< http://www.biomedcentral.com/1471-2334/10/363 >>
"Higher doses like 250-500 mg may be warranted to reach adequate concentrations in the stool in the first 24-48 hours," Dr. Garcia said. "I’m not saying to use 250 for the whole treatment course, but there may be a role for a loading dose of 250 mg q6 for the first 24-48 hours, and then switching to 125 mg q6 for the remainder of the treatment course. We know that 125 does have adequate fecal concentration; it just may not be adequate on day 1."
The 2010 update to clinical practice guidelines for C. difficile infection in adults recommends treating severe C. difficile infection with oral vancomycin 125 mg every 6 hours or using 500 mg every 6 hours for patients with severe disease complicated by ileus, megacolon, or hypotension (Infect. Control Hosp. Epidemiol. 2010;31:431-55).
Severe C. difficile infection generally is defined as the presence of the organism plus leukocytosis with a white blood cell count of 15,000 cells/microL or greater, or a serum creatinine level at least 1.5 times baseline. The study reviewed records of patients who received vancomycin for these indications or hypotension, shock, ileus, megacolon, or evidence of colitis. The study excluded patients who were treated with any other medication besides metronidazole.
The study is continuing in order to increase the number of patients reviewed and the power of the findings.
Dr. Garcia reported having no financial disclosures.
Major Finding: Symptoms of severe C. difficile infection resolved by day 3 of oral vancomycin treatment in 9 of 19 patients treated with 250 mg every 6 hours (47%) compared with 6 of 43 patients on 125 mg every 6 hours (15%).
Data Source: Retrospective review of records on 62 adults at one institution treated for at least 3 days with oral vancomycin for severe C. difficile infection.
Disclosures: Dr. Garcia reported having no financial disclosures.