User login
Stroke: Secondary prevention of ischemic events
Patients who suffer a stroke rarely have just one vascular risk factor. Therefore, the approach to secondary stroke prevention must be multifactorial. In fact, it has been estimated that 80% of recurrent strokes could be prevented through the application of a comprehensive, multifactorial approach that includes lifestyle modification and optimal medical management.1 Such an achievement would save millions of people from disability and functional decline, as well as millions of dollars in related medical costs.
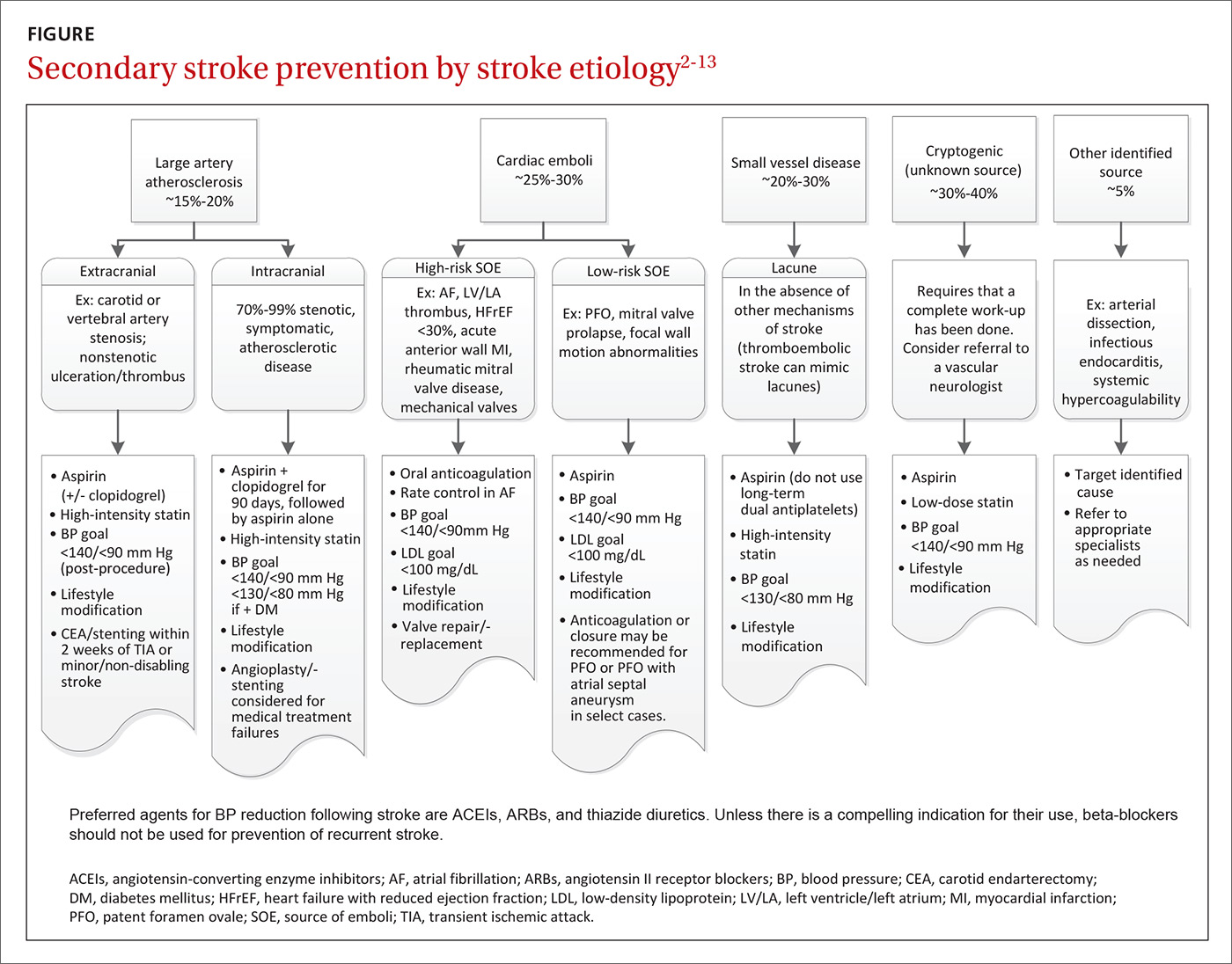
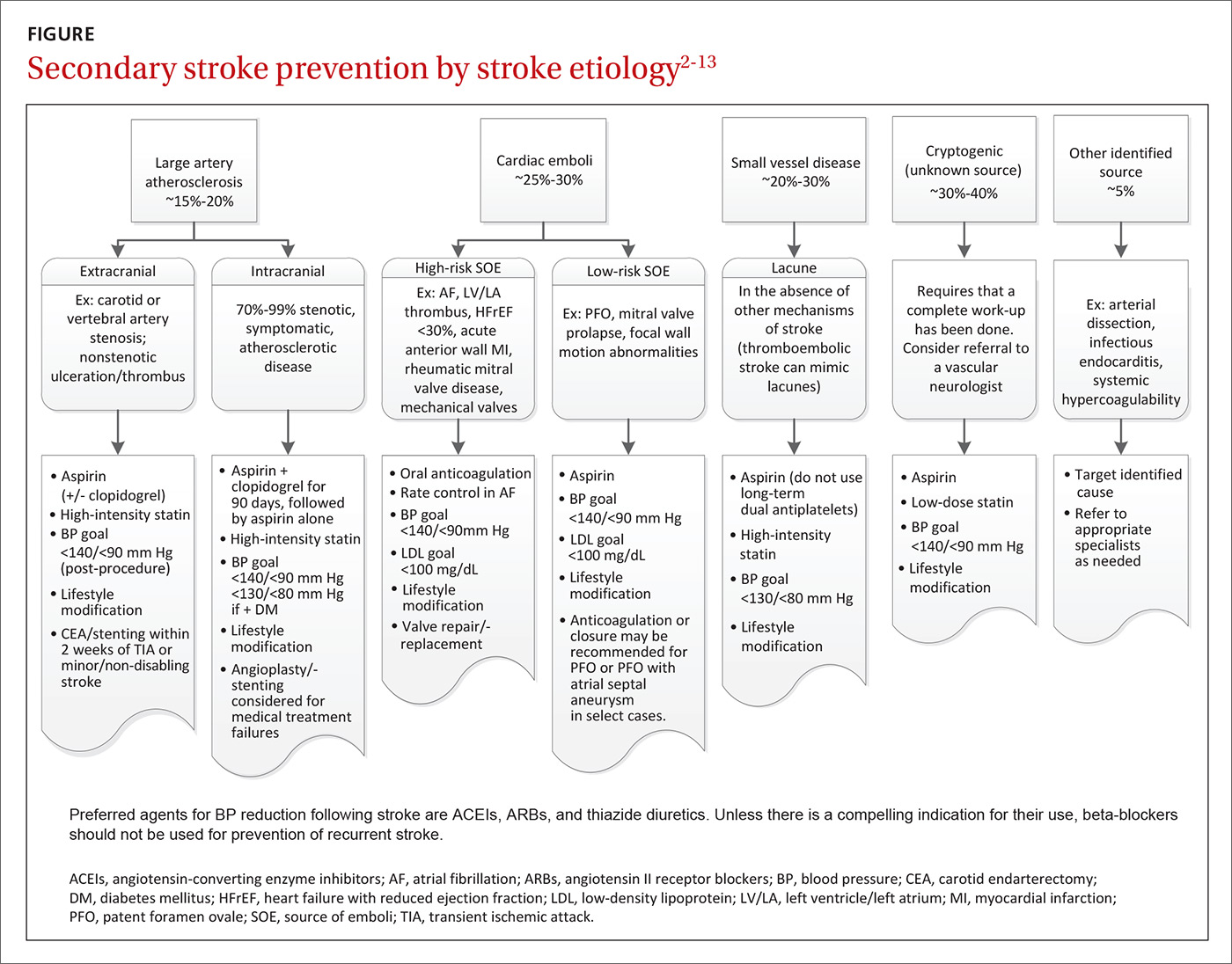
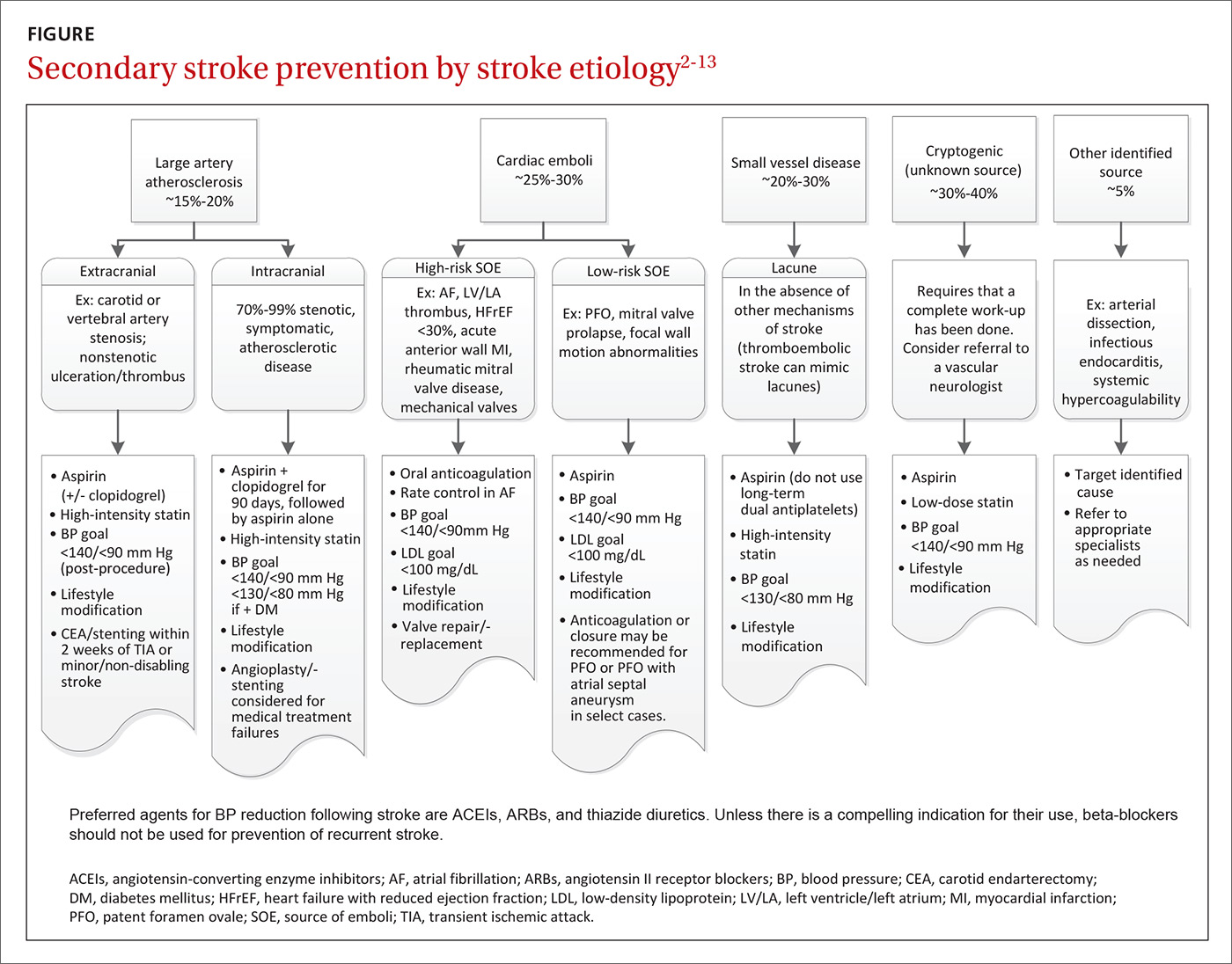
The initial approach to patients with stroke is focused on stabilization and a rapid work-up to identify the most likely etiology. Common causes of stroke include large artery atherosclerosis, cardiac emboli, and small vessel disease; less common causes include dissection, aortic emboli, and non-atherosclerotic vascular disease. If a complete diagnostic work-up is unrevealing, the stroke is said to be cryptogenic. Determining the correct etiology of a stroke is paramount to preventing secondary stroke (FIGURE2-13).
Effective secondary prevention strategies designed to prevent a stroke or transient ischemic attack (TIA) in a patient with a known history of either event include lifestyle modifications, medications, and when appropriate, mechanical interventions. As a primary care physician (PCP), you are uniquely positioned to spearhead the prevention of secondary strokes: Not only are you at the forefront of prevention and the use of techniques such as motivational interviewing, but you also have longstanding relationships with many of your patients. In fact, the success of many interventions is improved by the informed, enduring, and trusting nature of relationships between patients and their PCPs.
In the first part of this 2-part series, we focused on subacute stroke management and outlined the recommended work-up for subacute stroke/TIA (see “Stroke: A road map to subacute management,” 2017;66:366-374). In this part, we focus on secondary prevention. The more common modifiable conditions encountered in primary care are discussed here, while many of the more rare etiologies (hypercoagulable states, sickle cell disease, and vasculitis) are outside the scope of this article.
Lifestyle interventions: Target tobacco use, obesity, alcohol intake
Lifestyle modifications can have a positive impact on many of America’s most prevalent diseases, and stroke is no exception.14 Many of the disease states identified as risk factors for stroke (type 2 diabetes, hypertension, dyslipidemia) are exacerbated by tobacco use, obesity, and excessive alcohol intake.
Does your patient smoke? Up to 25% of all strokes are directly attributable to cigarette smoking.15 Smoking raises an individual’s risk for stroke in a dose-dependent fashion.15,16 One study demonstrated that, compared to never-smokers, women ages 15 to 49 years who smoked a half-pack per day had an odds ratio for ischemic stroke of 2.2; those who smoked 2 packs per day had an odds ratio of 9.1.17 After cessation, stroke risk generally returns to baseline within 5 years.16 Thus, smoking cessation is among the most significant steps a patient can take to reduce the risk of both primary and secondary stroke.
Is your patient overweight? While obesity in and of itself is a risk factor for stroke, a focus on nutrition and physical activity as mechanisms for weight loss is far superior to focusing on either element alone. Physical activity—consisting of at least 40 minutes of moderate intensity aerobic exercise 3 to 4 times per week—and a diet that emphasizes fruits and vegetables, whole grains, and healthy fats, have both independently demonstrated benefits in secondary stroke prevention and are important parts of American College of Cardiology (ACC)/American Heart Association (AHA) guidelines.2,3
The Mediterranean Diet, which emphasizes consumption of fruits and vegetables, legumes, tree nuts, olive oil, and lean protein, has long been associated with cardiovascular benefit.18 One prospective, randomized, single-blinded trial involving approximately 600 patients that looked at secondary prevention of coronary heart disease found that following the diet significantly reduced mortality compared with a usual prudent post-infarct diet (number needed to treat [NNT]=30 over 4 years).19
Is alcohol consumption an issue? Chronic heavy alcohol intake contributes to the development of hemorrhagic and ischemic stroke through multiple mechanisms, including alcohol-induced hypertension, alcoholic cardiomyopathy, and atrial fibrillation (AF). Light or moderate alcohol consumption has a paradoxical mild protective effect on ischemic stroke, thought to possibly be mediated by an increase in high-density lipoprotein (HDL) level and mild antiplatelet effect.3
AHA/American Stroke Association (ASA) guidelines indicate that no more than one standard drink per day for women and 2 drinks per day for men is reasonable.3 Counsel patients who drink in excess of this about the benefits of decreasing alcohol intake or abstaining altogether.
Choosing medications to manage BP, cholesterol, and clotting
Optimize blood pressure control. Blood pressure (BP) plays a critical role in both the management and prevention of stroke and is considered to be the most important modifiable risk factor in both primary and secondary stroke prevention.20 In the first 24 to 48 hours following a cerebral ischemic event that is not eligible for thrombolysis, permissive hypertension (treating BP only if it exceeds 220/120 mm Hg unless there is a concurrent medical illness that requires you do so) is appropriate, as hypotension or rapid fluctuations in BP can be harmful.21
This flexibility does not continue into the subacute phase of management (at a minimum, after the initial 48 hours) or into secondary prevention. Initiation and titration of oral agents to gradually achieve a BP <140/90 mm Hg or a reduction of 10/5 mm Hg for patients already within optimal range are the most widely recognized goals.3,20 Patients with stroke secondary to small vessel disease may benefit from an even lower goal of <130/<80 mm Hg.11 Encourage patients to monitor their BP at home for added accuracy and consistency.22
Pharmacologic BP management is appropriate for patients who are consistently above optimal range despite attempting recommended lifestyle modifications. The data are relatively consistent with respect to the effects of different drug classes after a stroke: beta-blockers have no effect on any outcome; thiazide diuretics significantly reduce stroke and total vascular events; angiotensin-converting enzyme (ACE) inhibitors significantly reduce myocardial infarction (MI); and the combination of an ACE inhibitor and thiazide diuretic reduces stroke, MI, and combined vascular events.4
This has led many stroke specialists to recommend the combination of an ACE inhibitor or angiotensin II receptor blocker (ARB) and a thiazide diuretic as a first-line approach to secondary stroke prevention rather than a beta-blocker (assuming there is no additional indication for a beta-blocker). Similarly, there is ample evidence to show that the magnitude of BP reduction is proportional to the reduction in recurrent vascular events.3
Make use of statin therapy—regardless of LDL. The SPARCL (Stroke Prevention by Aggressive Reduction in Cholesterol Levels) trial5 explored the potential role of statin medication for secondary stroke prevention. Researchers randomly assigned almost 5000 participants who’d had a stroke or TIA one to 6 months before study entry (but had no known history of coronary artery disease) to placebo or a high-intensity statin (80 mg/d atorvastatin). The statin group demonstrated a 4.9-year absolute risk reduction in fatal or nonfatal recurrent stroke of 1.9% (NNT=53).
Given these findings and those from other studies, the AHA and ASA recommend treating patients with stroke or TIA presumed to be of atherosclerotic origin with high-intensity statin therapy, regardless of low-density lipoprotein (LDL) level.3 Of note, statins are not indicated for the secondary prevention of hemorrhagic stroke.
Select antiplatelet therapy based on ischemic stroke subtype. Investigators are still trying to determine the optimal antiplatelet for secondary stroke prevention; it is likely that the ideal choice depends largely on the etiology of the stroke. Trials that did not select patients based on subtype of ischemic stroke have not shown a long-term benefit from dual antiplatelet therapy (clopidogrel and aspirin),23,24 and one double-blind, multicenter trial involving more than 3000 patients with recent stroke secondary to small vessel disease demonstrated harm from such therapy in terms of a significantly increased risk of bleeding and death.6
However, a 2011 study compared aggressive medical management (aspirin 325 mg/d plus clopidogrel 75 mg/d for 90 days) alone to aggressive medical management plus percutaneous transluminal angioplasty and stenting (PTAS). The study involved almost 500 patients who'd had a recent TIA or stroke attributed to intracranial atherosclerotic stenosis. The authors found that the 30-day rate of stroke or death was 14.7% in the PTAS group vs 5.8% in the medical management group.25
Similarly, a randomized double-blind, placebo-controlled trial published in 2013 involving over 5000 patients in China found that short-term use of dual antiplatelets (clopidogrel and aspirin for the first 21 days after an ischemic event, followed by aspirin monotherapy for 90 days) had an absolute risk reduction of 3.5% without increasing the risk of major bleeding in patients with high-risk TIA or minor stroke.26
All stroke patients who do not have an indication for oral anticoagulation should be placed on long-term daily aspirin (75-325 mg); research has shown that lower doses are as effective as higher doses but with a lower risk of adverse gastrointestinal effects, including bleeding.3,20 Aspirin 81 mg/d is a common effective dose.
For patients who cannot tolerate aspirin due to allergy, clopidogrel 75 mg/d is a reasonable alternative. Long-term studies of aspirin vs clopidogrel7 and clopidogrel vs extended-release dipyridamole8 showed no difference in secondary stroke prevention. The International Stroke Trial27 and Chinese Acute Stroke Trial28 both indicate that aspirin should be started as soon as possible after the onset of an acute stroke.
This special population should probably get antiplatelets, too. One recent study explored the use of an antiplatelet vs anticoagulation therapy for stroke patients with carotid artery dissection. The CADISS (Cervical Artery Dissection in Stroke Study) trial29 randomized 250 patients with extracranial carotid and vertebral artery dissection with onset of symptoms within the previous 7 days to either antiplatelet or anticoagulation therapy and found no difference in the primary outcomes of recurrent stroke or death. The study also demonstrated a low risk of recurrent stroke in this population, which was 2% at 3-month follow-up.
Most patients with cervical artery dissection, therefore, are now treated with antiplatelet therapy. That said, situations may still arise in which anticoagulation can be considered, and consultation with a neurologist for guidance on choice of therapy is recommended.
Is an anticoagulant in order? Which agent, when
The most common cause of cardioembolic stroke is AF, which accounts for at least 15% of ischemic strokes, a number that rises in those over the age of 80.20,30,31 A meta-analysis of more than 28,000 patients with non-valvular AF demonstrated that warfarin reduced the risk of stroke by 64%.32
The rate of intracerebral hemorrhages during oral anticoagulation ranges from 0.3% to 0.6% per year.33 The risk of bleeding complications can be mitigated by keeping international normalized ratios ≤3.0, maintaining good BP control, and avoiding concurrent use of antiplatelets in the absence of a clear indication for them.33
Several risk assessment scores, such as the HAS-BLED,34 can help with estimating the risk of hemorrhagic complications, although these scores have their limitations.35,36 Even in an older population (mean age 83 years) with a high risk for falls, warfarin provided a net benefit in a composite endpoint of out-of-hospital death or hospitalization for stroke, MI, or hemorrhage in a retrospective study of over 1200 Medicare beneficiaries.37
AF is not the only cause of cardioembolic stroke to consider. Additional high-risk factors warranting anticoagulation include rheumatic mitral valve disease, the presence of mechanical aortic or mitral valves, known mural thrombus, and acute anterior ST segment elevation myocardial infarctions (STEMIs) with resulting anterior apical dyskinesis/akinesis and concurrent ischemic stroke/TIA.3 (The specific management of each of these situations is beyond the scope of this paper.)
The choice of anticoagulation agent is based on multiple factors, including cost, risk of non-reversible bleeding, drug interactions, renal function, and patient preference. Approved options currently include warfarin/vitamin K antagonist therapy, apixaban, rivaroxaban, dabigatran and edoxaban.3 Choice of therapy will continue to evolve as reversal agents, such as idarucizumab, are developed. Idarucizumab, a reversal agent for dabigatran, received approval from the US Food and Drug Administration in October 2015.38
When to start anticoagulation. There are limited data regarding the optimal timing of initiation of anticoagulation following a stroke; however, a recent multicenter prospective study supported the common practice of initiating anticoagulation therapy within 4 to 14 days of the event.39 Individual patient factors must be taken into consideration, including the size of the stroke (the larger the stroke, the higher the risk for hemorrhagic transformation), BP control, any additional risk factors for bleeding, and the estimated risk of early recurrent stroke.
Bridging patients onto anticoagulation with unfractionated or low-molecular-weight heparin in the setting of acute stroke is not recommended.40 Results from randomized controlled trials involving unfractionated heparin, heparinoids, and low-molecular-weight heparin have not reported any benefit to these agents over aspirin at preventing early stroke recurrence.27,41,42
For immobile or hospitalized patients. Subcutaneous heparin for the prevention of deep vein thrombosis (DVT) during immobility and hospitalization is recommended.43 Patients who cannot tolerate anticoagulation should be maintained on low-dose antiplatelet therapy. Experts do not recommend dual treatment with aspirin and anticoagulation in most cases. However, recent coronary artery stent placement does require temporary dual treatment, with duration dependent on the type of stent placed.
A role for glycemic control? Still to be determined
The specific role of diabetic management in secondary stroke prevention remains unclear. The 2008 ACCORD trial,44 a randomized study involving over 10,000 patients with a median glycated hemoglobin level of 8.1%, investigated intensive hyperglycemic control (targeting a glycated hemoglobin level <6.0% vs <7.9%) as a means of decreasing cardiovascular risk. However, the trial ended 17 months early because of an increase in all-cause mortality in the intensive treatment arm compared with the standard management group. The same trial was also unable to demonstrate a decrease in stroke risk with a decrease in A1c.44
More recently, the IRIS (Insulin Resistance Intervention after Stroke) trial45 (2016) found a 2.8% absolute risk reduction in stroke or MI among participants who had a stroke or TIA in the previous 6 months who were treated with pioglitazone vs placebo over 4.8 years (NNT=36). Participants were required to have insulin resistance, but were excluded if they had diabetes. The authors did, however, report a notable increase in the risk of bone fractures requiring surgery or hospitalization in the pioglitazone arm (5.1% vs 3.2%; number needed to harm [NNH]=53).
The impact this single study should have on standard secondary prevention is not yet clear. The authors concluded, “It seems reasonable to consider individual treatment preference and risk of drug-related adverse events in addition to potential benefits when making patient-specific decisions regarding therapy.”45
Determining whether mechanical interventions are needed
Almost all conditions leading to stroke warrant active medical management, but a few benefit from procedural intervention, as well.
Extracranial carotid atherosclerosis. Carotid endarterectomy or carotid artery stenting is recommended as secondary prevention for patients with a history of stroke or TIA who have ipsilateral high-grade extracranial carotid stenosis of 70% to 99% and, in some cases, 50% to 69%.3,9,20 In patients with mild non-disabling stroke, the optimal timing for these procedures is within 2 weeks of the ischemic event. A delay of 6 weeks is generally preferred for moderate or larger strokes to allow for some healing of the injured brain.
The choice of procedure is based on risk profile, with the most important factor being age. For patients >70 years, endarterectomy is preferred because stenting is associated with an increased risk of stroke.3,9,10 Experts do not recommend either procedure for patients who have had a severe disabling stroke. Generally speaking, these procedures have higher rates of success when they are performed in centers that perform a higher number of these procedures.10
Vertebrobasilar atherosclerosis. Due to generally good compensatory blood flow of the contralateral vertebral artery in the setting of vertebral artery stenosis, and an unacceptably high complication rate of angioplasty and stenting in the basilar artery, medical management is typically the first-line approach. If a patient has recurrent symptoms in the setting of optimal medical management and a focal lesion that is amenable to an endovascular intervention (most commonly a vertebral artery origin high-grade stenosis), angioplasty and stenting may be considered.10
Intracranial atherosclerosis. Similarly, medical management is the preferred strategy for intracranial atherosclerosis. Angioplasty and/or stenting are reserved for complex cases or recurrence despite adherence to secondary stroke prevention measures. Ideally, these patients should be managed with long-term aspirin 81 mg/d, adjunctive clopidogrel 75 mg/d for 90 days post stroke, a high-intensity statin, BP optimization, and any relevant lifestyle interventions.13
Patent foramen ovale. Research to date has not shown that closure of a patent foramen ovale (PFO) is superior to medical therapy for secondary stroke prevention in patients <60 years with cryptogenic stroke.12,46,47 The decision to anticoagulate these patients should be based on the presence or absence of a DVT and not on a PFO alone. In patients with an identified DVT and a contraindication to oral anticoagulation, inferior vena cava filter placement should be considered. For patients with ongoing prothrombotic risk thought to increase the chances of future paradoxical embolism, closure of the PFO may be considered.
CORRESPONDENCE
Stephen A. Martin, MD, EdM, Barre Family Health Center, 151 Worcester Road, Barre, MA 01005; [email protected].
1. Hackam DG, Spence JD. Combining multiple approaches for the secondary prevention of vascular events after stroke: a quantitative modeling study. Stroke. 2007;38:1881-1885.
2. Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S76-S99.
3. Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2160-2236.
4. Rashid P, Leonardi-Bee J, Bath P. Blood pressure reduction and secondary prevention of stroke and other vascular events: a systematic review. Stroke. 2003;34:2741-2748.
5. Amarenco P, Bogousslavsky J, Callahan A, et al, for the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355:549-559.
6. Benavente OR, Hart RG, McClure LA, et al, for the SPS3 Investigators. Effects of clopidogrel added to aspirin in patients with recent lacunar stroke. N Engl J Med. 2012;367:817-825.
7. CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee. Lancet. 1996;348:1329-1339.
8. Sacco RL, Diener HC, Yusuf S, et al. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med. 2008;359:1238-1251.
9. Diethrich EB, N’diaye M, Reid DB. The Carotid Revascularization Endarterectomy versus Stenting Trial (CREST): implications for clinical practice. In: Henry M, Diethrich EB, Polydorou A, eds. The Carotid and Supra-Aortic Trunks: Diagnosis, Angioplasty and Stenting. 2nd ed. Oxford, UK: Wiley-Blackwell; 2011.
10. Brott TG, Halperin JL, Abbara S, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. Circulation. 2011;124:489-532.
11. SPS3 Study Group. Blood pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet. 2013;382:507-515.
12. Carroll JD, Saver JL, Thaler DE, et al. Closure of patent foramen ovale versus medical therapy after cryptogenic stroke. N Engl J Med. 2013;368:1092-1100.
13. Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365:993-1003.
14. Romero JR, Morris J, Pikula A. Stroke prevention: modifying risk factors. Ther Adv Cardiovasc Dis. 2008;2:287-303.
15. Hankey GJ. Smoking and risk of stroke. J Cardiovasc Risk. 1999;6:207-211.
16. Shah RS, Cole JW. Smoking and stroke: the more you smoke the more you stroke. Expert Rev Cardiovasc Ther. 2010;8:917-932.
17. Bhat VM, Cole JW, Sorkin JD, et al. Dose-response relationship between cigarette smoking and risk of ischemic stroke in young women. Stroke. 2008;39:2439-2443.
18. Lakkur S, Judd SE. Diet and stroke: recent evidence supporting a Mediterranean-style diet and food in the primary prevention of stroke. Stroke. 2015;46:2007-2011.
19. de Lorgeril M, Salen P, Martin JL, et al. Mediterranean dietary pattern in a randomized trial: prolonged survival and possible reduced cancer rate. Arch Intern Med. 1998;158:1181-1187.
20. Davis SM, Donnan GA. Clinical practice. Secondary prevention after ischemic stroke or transient ischemic attack. N Engl J Med. 2012;366:1914-1922.
21. Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870-947.
22. Magid DJ, Green BB. Home blood pressure monitoring: take it to the bank. JAMA. 2013;310:40-41.
23. Diener H-C, Bogousslavsky J, Brass LM, et al. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. Lancet (London, England). 2004;364:331-337.
24. Bhatt DL, Fox KAA, Hacke W, et al. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med. 2006;354:1706-1717.
25. Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365:993-1003.
26. Wang Y, Wang Y, Zhao X, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013;369:11-19.
27. The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke. International Stroke Trial Collaborative Group. Lancet. 1997;349:1569-1581.
28. CAST: randomised placebo-controlled trial of early aspirin use in 20,000 patients with acute ischaemic stroke. CAST (Chinese Acute Stroke Trial) Collaborative Group. Lancet. 1997;349:1641-1649.
29. CADISS trial investigators, Markus HS, Hayter E, et al. Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): a randomised trial. Lancet Neurol. 2015;14:361-367.
30. Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. EAFT (European Atrial Fibrillation Trial) Study Group. Lancet. 1993;342:1255-1262.
31. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983-988.
32. Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Int Med. 2007;146:857-867.
33. Hart RG, Tonarelli SB, Pearce LA. Avoiding central nervous system bleeding during antithrombotic therapy. Recent data and ideas. Stroke. 2005;36:1588-1593.
34. Pisters R, Lane DA, Nieuwlaat R, et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: The Euro Heart Survey. Chest. 2010;138:1093-1100.
35. Quinn GR, Singer DE, Chang Y, et al. How well do stroke risk scores predict hemorrhage in patients with atrial fibrillation? Am J Cardiol. 2016;118:697-699.
36. Gorman EW, Perkel D, Dennis D, et al. Validation of the HAS-BLED tool in atrial fibrillation patients receiving rivaroxaban. J Atr Fibrillation. 2016;9:1461.
37. Gage BF, Birman-Deych E, Kerzner R, et al. Incidence of intracranial hemorrhage in patients with atrial fibrillation who are prone to fall. Am J Med. 2005;118:612-617.
38. US Food and Drug Administration. FDA approves Praxbind, the first reversal agent for the anticoagulant Pradaxa. October 16, 2015. Available at: https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm467300.htm. Accessed May 26, 2017.
39. Paciaroni M, Agnelli G, Falocci N, et al. Early recurrence and cerebral bleeding in patients with acute ischemic stroke and atrial fibrillation: effect of anticoagulation and its timing: the RAF Study. Stroke. 2015;46:2175-2182.
40. Sandercock PA, Counsell C, Kane EJ. Anticoagulants for acute ischaemic stroke. Cochrane Database Syst Rev. 2015;3:CD000024.
41. Bath PM, Lindenstrom E, Boysen G, et al. Tinzaparin in acute ischaemic stroke (TAIST): a randomised aspirin-controlled trial. Lancet. 2001;358:702-710.
42. Berge E, Abdelnoor M, Nakstad PH, et al. Low molecular-weight heparin versus aspirin in patients with acute ischaemic stroke and atrial fibrillation: a double-blind randomised study. HAEST Study Group. Heparin in Acute Embolic Stroke Trial. Lancet. 2000;355:1205-1210.
43. Sherman DG, Albers GW, Bladin C, et al. The efficacy and safety of enoxaparin versus unfractionated heparin for the prevention of venous thromboembolism after acute ischaemic stroke (PREVAIL Study): an open-label randomised comparison. Lancet. 2007;369:1347-1355.
44. Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545-2559.
45. Kernan WN, Viscoli CM, Furie KL, et al. Pioglitazone after ischemic stroke or transient ischemic attack. N Engl J Med. 2016;374:1321-1331.
46. Meier B, Kalesan B, Mattle HP, et al. Percutaneous closure of patent foramen ovale in cryptogenic embolism. N Engl J Med. 2013;368:1083-1091.
47. Furlan AJ, Reisman M, Massaro J, et al. Closure or medical therapy for cryptogenic stroke with patent foramen ovale. N Engl J Med. 2012;366:991-999.
Patients who suffer a stroke rarely have just one vascular risk factor. Therefore, the approach to secondary stroke prevention must be multifactorial. In fact, it has been estimated that 80% of recurrent strokes could be prevented through the application of a comprehensive, multifactorial approach that includes lifestyle modification and optimal medical management.1 Such an achievement would save millions of people from disability and functional decline, as well as millions of dollars in related medical costs.
The initial approach to patients with stroke is focused on stabilization and a rapid work-up to identify the most likely etiology. Common causes of stroke include large artery atherosclerosis, cardiac emboli, and small vessel disease; less common causes include dissection, aortic emboli, and non-atherosclerotic vascular disease. If a complete diagnostic work-up is unrevealing, the stroke is said to be cryptogenic. Determining the correct etiology of a stroke is paramount to preventing secondary stroke (FIGURE2-13).
Effective secondary prevention strategies designed to prevent a stroke or transient ischemic attack (TIA) in a patient with a known history of either event include lifestyle modifications, medications, and when appropriate, mechanical interventions. As a primary care physician (PCP), you are uniquely positioned to spearhead the prevention of secondary strokes: Not only are you at the forefront of prevention and the use of techniques such as motivational interviewing, but you also have longstanding relationships with many of your patients. In fact, the success of many interventions is improved by the informed, enduring, and trusting nature of relationships between patients and their PCPs.
In the first part of this 2-part series, we focused on subacute stroke management and outlined the recommended work-up for subacute stroke/TIA (see “Stroke: A road map to subacute management,” 2017;66:366-374). In this part, we focus on secondary prevention. The more common modifiable conditions encountered in primary care are discussed here, while many of the more rare etiologies (hypercoagulable states, sickle cell disease, and vasculitis) are outside the scope of this article.
Lifestyle interventions: Target tobacco use, obesity, alcohol intake
Lifestyle modifications can have a positive impact on many of America’s most prevalent diseases, and stroke is no exception.14 Many of the disease states identified as risk factors for stroke (type 2 diabetes, hypertension, dyslipidemia) are exacerbated by tobacco use, obesity, and excessive alcohol intake.
Does your patient smoke? Up to 25% of all strokes are directly attributable to cigarette smoking.15 Smoking raises an individual’s risk for stroke in a dose-dependent fashion.15,16 One study demonstrated that, compared to never-smokers, women ages 15 to 49 years who smoked a half-pack per day had an odds ratio for ischemic stroke of 2.2; those who smoked 2 packs per day had an odds ratio of 9.1.17 After cessation, stroke risk generally returns to baseline within 5 years.16 Thus, smoking cessation is among the most significant steps a patient can take to reduce the risk of both primary and secondary stroke.
Is your patient overweight? While obesity in and of itself is a risk factor for stroke, a focus on nutrition and physical activity as mechanisms for weight loss is far superior to focusing on either element alone. Physical activity—consisting of at least 40 minutes of moderate intensity aerobic exercise 3 to 4 times per week—and a diet that emphasizes fruits and vegetables, whole grains, and healthy fats, have both independently demonstrated benefits in secondary stroke prevention and are important parts of American College of Cardiology (ACC)/American Heart Association (AHA) guidelines.2,3
The Mediterranean Diet, which emphasizes consumption of fruits and vegetables, legumes, tree nuts, olive oil, and lean protein, has long been associated with cardiovascular benefit.18 One prospective, randomized, single-blinded trial involving approximately 600 patients that looked at secondary prevention of coronary heart disease found that following the diet significantly reduced mortality compared with a usual prudent post-infarct diet (number needed to treat [NNT]=30 over 4 years).19
Is alcohol consumption an issue? Chronic heavy alcohol intake contributes to the development of hemorrhagic and ischemic stroke through multiple mechanisms, including alcohol-induced hypertension, alcoholic cardiomyopathy, and atrial fibrillation (AF). Light or moderate alcohol consumption has a paradoxical mild protective effect on ischemic stroke, thought to possibly be mediated by an increase in high-density lipoprotein (HDL) level and mild antiplatelet effect.3
AHA/American Stroke Association (ASA) guidelines indicate that no more than one standard drink per day for women and 2 drinks per day for men is reasonable.3 Counsel patients who drink in excess of this about the benefits of decreasing alcohol intake or abstaining altogether.
Choosing medications to manage BP, cholesterol, and clotting
Optimize blood pressure control. Blood pressure (BP) plays a critical role in both the management and prevention of stroke and is considered to be the most important modifiable risk factor in both primary and secondary stroke prevention.20 In the first 24 to 48 hours following a cerebral ischemic event that is not eligible for thrombolysis, permissive hypertension (treating BP only if it exceeds 220/120 mm Hg unless there is a concurrent medical illness that requires you do so) is appropriate, as hypotension or rapid fluctuations in BP can be harmful.21
This flexibility does not continue into the subacute phase of management (at a minimum, after the initial 48 hours) or into secondary prevention. Initiation and titration of oral agents to gradually achieve a BP <140/90 mm Hg or a reduction of 10/5 mm Hg for patients already within optimal range are the most widely recognized goals.3,20 Patients with stroke secondary to small vessel disease may benefit from an even lower goal of <130/<80 mm Hg.11 Encourage patients to monitor their BP at home for added accuracy and consistency.22
Pharmacologic BP management is appropriate for patients who are consistently above optimal range despite attempting recommended lifestyle modifications. The data are relatively consistent with respect to the effects of different drug classes after a stroke: beta-blockers have no effect on any outcome; thiazide diuretics significantly reduce stroke and total vascular events; angiotensin-converting enzyme (ACE) inhibitors significantly reduce myocardial infarction (MI); and the combination of an ACE inhibitor and thiazide diuretic reduces stroke, MI, and combined vascular events.4
This has led many stroke specialists to recommend the combination of an ACE inhibitor or angiotensin II receptor blocker (ARB) and a thiazide diuretic as a first-line approach to secondary stroke prevention rather than a beta-blocker (assuming there is no additional indication for a beta-blocker). Similarly, there is ample evidence to show that the magnitude of BP reduction is proportional to the reduction in recurrent vascular events.3
Make use of statin therapy—regardless of LDL. The SPARCL (Stroke Prevention by Aggressive Reduction in Cholesterol Levels) trial5 explored the potential role of statin medication for secondary stroke prevention. Researchers randomly assigned almost 5000 participants who’d had a stroke or TIA one to 6 months before study entry (but had no known history of coronary artery disease) to placebo or a high-intensity statin (80 mg/d atorvastatin). The statin group demonstrated a 4.9-year absolute risk reduction in fatal or nonfatal recurrent stroke of 1.9% (NNT=53).
Given these findings and those from other studies, the AHA and ASA recommend treating patients with stroke or TIA presumed to be of atherosclerotic origin with high-intensity statin therapy, regardless of low-density lipoprotein (LDL) level.3 Of note, statins are not indicated for the secondary prevention of hemorrhagic stroke.
Select antiplatelet therapy based on ischemic stroke subtype. Investigators are still trying to determine the optimal antiplatelet for secondary stroke prevention; it is likely that the ideal choice depends largely on the etiology of the stroke. Trials that did not select patients based on subtype of ischemic stroke have not shown a long-term benefit from dual antiplatelet therapy (clopidogrel and aspirin),23,24 and one double-blind, multicenter trial involving more than 3000 patients with recent stroke secondary to small vessel disease demonstrated harm from such therapy in terms of a significantly increased risk of bleeding and death.6
However, a 2011 study compared aggressive medical management (aspirin 325 mg/d plus clopidogrel 75 mg/d for 90 days) alone to aggressive medical management plus percutaneous transluminal angioplasty and stenting (PTAS). The study involved almost 500 patients who'd had a recent TIA or stroke attributed to intracranial atherosclerotic stenosis. The authors found that the 30-day rate of stroke or death was 14.7% in the PTAS group vs 5.8% in the medical management group.25
Similarly, a randomized double-blind, placebo-controlled trial published in 2013 involving over 5000 patients in China found that short-term use of dual antiplatelets (clopidogrel and aspirin for the first 21 days after an ischemic event, followed by aspirin monotherapy for 90 days) had an absolute risk reduction of 3.5% without increasing the risk of major bleeding in patients with high-risk TIA or minor stroke.26
All stroke patients who do not have an indication for oral anticoagulation should be placed on long-term daily aspirin (75-325 mg); research has shown that lower doses are as effective as higher doses but with a lower risk of adverse gastrointestinal effects, including bleeding.3,20 Aspirin 81 mg/d is a common effective dose.
For patients who cannot tolerate aspirin due to allergy, clopidogrel 75 mg/d is a reasonable alternative. Long-term studies of aspirin vs clopidogrel7 and clopidogrel vs extended-release dipyridamole8 showed no difference in secondary stroke prevention. The International Stroke Trial27 and Chinese Acute Stroke Trial28 both indicate that aspirin should be started as soon as possible after the onset of an acute stroke.
This special population should probably get antiplatelets, too. One recent study explored the use of an antiplatelet vs anticoagulation therapy for stroke patients with carotid artery dissection. The CADISS (Cervical Artery Dissection in Stroke Study) trial29 randomized 250 patients with extracranial carotid and vertebral artery dissection with onset of symptoms within the previous 7 days to either antiplatelet or anticoagulation therapy and found no difference in the primary outcomes of recurrent stroke or death. The study also demonstrated a low risk of recurrent stroke in this population, which was 2% at 3-month follow-up.
Most patients with cervical artery dissection, therefore, are now treated with antiplatelet therapy. That said, situations may still arise in which anticoagulation can be considered, and consultation with a neurologist for guidance on choice of therapy is recommended.
Is an anticoagulant in order? Which agent, when
The most common cause of cardioembolic stroke is AF, which accounts for at least 15% of ischemic strokes, a number that rises in those over the age of 80.20,30,31 A meta-analysis of more than 28,000 patients with non-valvular AF demonstrated that warfarin reduced the risk of stroke by 64%.32
The rate of intracerebral hemorrhages during oral anticoagulation ranges from 0.3% to 0.6% per year.33 The risk of bleeding complications can be mitigated by keeping international normalized ratios ≤3.0, maintaining good BP control, and avoiding concurrent use of antiplatelets in the absence of a clear indication for them.33
Several risk assessment scores, such as the HAS-BLED,34 can help with estimating the risk of hemorrhagic complications, although these scores have their limitations.35,36 Even in an older population (mean age 83 years) with a high risk for falls, warfarin provided a net benefit in a composite endpoint of out-of-hospital death or hospitalization for stroke, MI, or hemorrhage in a retrospective study of over 1200 Medicare beneficiaries.37
AF is not the only cause of cardioembolic stroke to consider. Additional high-risk factors warranting anticoagulation include rheumatic mitral valve disease, the presence of mechanical aortic or mitral valves, known mural thrombus, and acute anterior ST segment elevation myocardial infarctions (STEMIs) with resulting anterior apical dyskinesis/akinesis and concurrent ischemic stroke/TIA.3 (The specific management of each of these situations is beyond the scope of this paper.)
The choice of anticoagulation agent is based on multiple factors, including cost, risk of non-reversible bleeding, drug interactions, renal function, and patient preference. Approved options currently include warfarin/vitamin K antagonist therapy, apixaban, rivaroxaban, dabigatran and edoxaban.3 Choice of therapy will continue to evolve as reversal agents, such as idarucizumab, are developed. Idarucizumab, a reversal agent for dabigatran, received approval from the US Food and Drug Administration in October 2015.38
When to start anticoagulation. There are limited data regarding the optimal timing of initiation of anticoagulation following a stroke; however, a recent multicenter prospective study supported the common practice of initiating anticoagulation therapy within 4 to 14 days of the event.39 Individual patient factors must be taken into consideration, including the size of the stroke (the larger the stroke, the higher the risk for hemorrhagic transformation), BP control, any additional risk factors for bleeding, and the estimated risk of early recurrent stroke.
Bridging patients onto anticoagulation with unfractionated or low-molecular-weight heparin in the setting of acute stroke is not recommended.40 Results from randomized controlled trials involving unfractionated heparin, heparinoids, and low-molecular-weight heparin have not reported any benefit to these agents over aspirin at preventing early stroke recurrence.27,41,42
For immobile or hospitalized patients. Subcutaneous heparin for the prevention of deep vein thrombosis (DVT) during immobility and hospitalization is recommended.43 Patients who cannot tolerate anticoagulation should be maintained on low-dose antiplatelet therapy. Experts do not recommend dual treatment with aspirin and anticoagulation in most cases. However, recent coronary artery stent placement does require temporary dual treatment, with duration dependent on the type of stent placed.
A role for glycemic control? Still to be determined
The specific role of diabetic management in secondary stroke prevention remains unclear. The 2008 ACCORD trial,44 a randomized study involving over 10,000 patients with a median glycated hemoglobin level of 8.1%, investigated intensive hyperglycemic control (targeting a glycated hemoglobin level <6.0% vs <7.9%) as a means of decreasing cardiovascular risk. However, the trial ended 17 months early because of an increase in all-cause mortality in the intensive treatment arm compared with the standard management group. The same trial was also unable to demonstrate a decrease in stroke risk with a decrease in A1c.44
More recently, the IRIS (Insulin Resistance Intervention after Stroke) trial45 (2016) found a 2.8% absolute risk reduction in stroke or MI among participants who had a stroke or TIA in the previous 6 months who were treated with pioglitazone vs placebo over 4.8 years (NNT=36). Participants were required to have insulin resistance, but were excluded if they had diabetes. The authors did, however, report a notable increase in the risk of bone fractures requiring surgery or hospitalization in the pioglitazone arm (5.1% vs 3.2%; number needed to harm [NNH]=53).
The impact this single study should have on standard secondary prevention is not yet clear. The authors concluded, “It seems reasonable to consider individual treatment preference and risk of drug-related adverse events in addition to potential benefits when making patient-specific decisions regarding therapy.”45
Determining whether mechanical interventions are needed
Almost all conditions leading to stroke warrant active medical management, but a few benefit from procedural intervention, as well.
Extracranial carotid atherosclerosis. Carotid endarterectomy or carotid artery stenting is recommended as secondary prevention for patients with a history of stroke or TIA who have ipsilateral high-grade extracranial carotid stenosis of 70% to 99% and, in some cases, 50% to 69%.3,9,20 In patients with mild non-disabling stroke, the optimal timing for these procedures is within 2 weeks of the ischemic event. A delay of 6 weeks is generally preferred for moderate or larger strokes to allow for some healing of the injured brain.
The choice of procedure is based on risk profile, with the most important factor being age. For patients >70 years, endarterectomy is preferred because stenting is associated with an increased risk of stroke.3,9,10 Experts do not recommend either procedure for patients who have had a severe disabling stroke. Generally speaking, these procedures have higher rates of success when they are performed in centers that perform a higher number of these procedures.10
Vertebrobasilar atherosclerosis. Due to generally good compensatory blood flow of the contralateral vertebral artery in the setting of vertebral artery stenosis, and an unacceptably high complication rate of angioplasty and stenting in the basilar artery, medical management is typically the first-line approach. If a patient has recurrent symptoms in the setting of optimal medical management and a focal lesion that is amenable to an endovascular intervention (most commonly a vertebral artery origin high-grade stenosis), angioplasty and stenting may be considered.10
Intracranial atherosclerosis. Similarly, medical management is the preferred strategy for intracranial atherosclerosis. Angioplasty and/or stenting are reserved for complex cases or recurrence despite adherence to secondary stroke prevention measures. Ideally, these patients should be managed with long-term aspirin 81 mg/d, adjunctive clopidogrel 75 mg/d for 90 days post stroke, a high-intensity statin, BP optimization, and any relevant lifestyle interventions.13
Patent foramen ovale. Research to date has not shown that closure of a patent foramen ovale (PFO) is superior to medical therapy for secondary stroke prevention in patients <60 years with cryptogenic stroke.12,46,47 The decision to anticoagulate these patients should be based on the presence or absence of a DVT and not on a PFO alone. In patients with an identified DVT and a contraindication to oral anticoagulation, inferior vena cava filter placement should be considered. For patients with ongoing prothrombotic risk thought to increase the chances of future paradoxical embolism, closure of the PFO may be considered.
CORRESPONDENCE
Stephen A. Martin, MD, EdM, Barre Family Health Center, 151 Worcester Road, Barre, MA 01005; [email protected].
Patients who suffer a stroke rarely have just one vascular risk factor. Therefore, the approach to secondary stroke prevention must be multifactorial. In fact, it has been estimated that 80% of recurrent strokes could be prevented through the application of a comprehensive, multifactorial approach that includes lifestyle modification and optimal medical management.1 Such an achievement would save millions of people from disability and functional decline, as well as millions of dollars in related medical costs.
The initial approach to patients with stroke is focused on stabilization and a rapid work-up to identify the most likely etiology. Common causes of stroke include large artery atherosclerosis, cardiac emboli, and small vessel disease; less common causes include dissection, aortic emboli, and non-atherosclerotic vascular disease. If a complete diagnostic work-up is unrevealing, the stroke is said to be cryptogenic. Determining the correct etiology of a stroke is paramount to preventing secondary stroke (FIGURE2-13).
Effective secondary prevention strategies designed to prevent a stroke or transient ischemic attack (TIA) in a patient with a known history of either event include lifestyle modifications, medications, and when appropriate, mechanical interventions. As a primary care physician (PCP), you are uniquely positioned to spearhead the prevention of secondary strokes: Not only are you at the forefront of prevention and the use of techniques such as motivational interviewing, but you also have longstanding relationships with many of your patients. In fact, the success of many interventions is improved by the informed, enduring, and trusting nature of relationships between patients and their PCPs.
In the first part of this 2-part series, we focused on subacute stroke management and outlined the recommended work-up for subacute stroke/TIA (see “Stroke: A road map to subacute management,” 2017;66:366-374). In this part, we focus on secondary prevention. The more common modifiable conditions encountered in primary care are discussed here, while many of the more rare etiologies (hypercoagulable states, sickle cell disease, and vasculitis) are outside the scope of this article.
Lifestyle interventions: Target tobacco use, obesity, alcohol intake
Lifestyle modifications can have a positive impact on many of America’s most prevalent diseases, and stroke is no exception.14 Many of the disease states identified as risk factors for stroke (type 2 diabetes, hypertension, dyslipidemia) are exacerbated by tobacco use, obesity, and excessive alcohol intake.
Does your patient smoke? Up to 25% of all strokes are directly attributable to cigarette smoking.15 Smoking raises an individual’s risk for stroke in a dose-dependent fashion.15,16 One study demonstrated that, compared to never-smokers, women ages 15 to 49 years who smoked a half-pack per day had an odds ratio for ischemic stroke of 2.2; those who smoked 2 packs per day had an odds ratio of 9.1.17 After cessation, stroke risk generally returns to baseline within 5 years.16 Thus, smoking cessation is among the most significant steps a patient can take to reduce the risk of both primary and secondary stroke.
Is your patient overweight? While obesity in and of itself is a risk factor for stroke, a focus on nutrition and physical activity as mechanisms for weight loss is far superior to focusing on either element alone. Physical activity—consisting of at least 40 minutes of moderate intensity aerobic exercise 3 to 4 times per week—and a diet that emphasizes fruits and vegetables, whole grains, and healthy fats, have both independently demonstrated benefits in secondary stroke prevention and are important parts of American College of Cardiology (ACC)/American Heart Association (AHA) guidelines.2,3
The Mediterranean Diet, which emphasizes consumption of fruits and vegetables, legumes, tree nuts, olive oil, and lean protein, has long been associated with cardiovascular benefit.18 One prospective, randomized, single-blinded trial involving approximately 600 patients that looked at secondary prevention of coronary heart disease found that following the diet significantly reduced mortality compared with a usual prudent post-infarct diet (number needed to treat [NNT]=30 over 4 years).19
Is alcohol consumption an issue? Chronic heavy alcohol intake contributes to the development of hemorrhagic and ischemic stroke through multiple mechanisms, including alcohol-induced hypertension, alcoholic cardiomyopathy, and atrial fibrillation (AF). Light or moderate alcohol consumption has a paradoxical mild protective effect on ischemic stroke, thought to possibly be mediated by an increase in high-density lipoprotein (HDL) level and mild antiplatelet effect.3
AHA/American Stroke Association (ASA) guidelines indicate that no more than one standard drink per day for women and 2 drinks per day for men is reasonable.3 Counsel patients who drink in excess of this about the benefits of decreasing alcohol intake or abstaining altogether.
Choosing medications to manage BP, cholesterol, and clotting
Optimize blood pressure control. Blood pressure (BP) plays a critical role in both the management and prevention of stroke and is considered to be the most important modifiable risk factor in both primary and secondary stroke prevention.20 In the first 24 to 48 hours following a cerebral ischemic event that is not eligible for thrombolysis, permissive hypertension (treating BP only if it exceeds 220/120 mm Hg unless there is a concurrent medical illness that requires you do so) is appropriate, as hypotension or rapid fluctuations in BP can be harmful.21
This flexibility does not continue into the subacute phase of management (at a minimum, after the initial 48 hours) or into secondary prevention. Initiation and titration of oral agents to gradually achieve a BP <140/90 mm Hg or a reduction of 10/5 mm Hg for patients already within optimal range are the most widely recognized goals.3,20 Patients with stroke secondary to small vessel disease may benefit from an even lower goal of <130/<80 mm Hg.11 Encourage patients to monitor their BP at home for added accuracy and consistency.22
Pharmacologic BP management is appropriate for patients who are consistently above optimal range despite attempting recommended lifestyle modifications. The data are relatively consistent with respect to the effects of different drug classes after a stroke: beta-blockers have no effect on any outcome; thiazide diuretics significantly reduce stroke and total vascular events; angiotensin-converting enzyme (ACE) inhibitors significantly reduce myocardial infarction (MI); and the combination of an ACE inhibitor and thiazide diuretic reduces stroke, MI, and combined vascular events.4
This has led many stroke specialists to recommend the combination of an ACE inhibitor or angiotensin II receptor blocker (ARB) and a thiazide diuretic as a first-line approach to secondary stroke prevention rather than a beta-blocker (assuming there is no additional indication for a beta-blocker). Similarly, there is ample evidence to show that the magnitude of BP reduction is proportional to the reduction in recurrent vascular events.3
Make use of statin therapy—regardless of LDL. The SPARCL (Stroke Prevention by Aggressive Reduction in Cholesterol Levels) trial5 explored the potential role of statin medication for secondary stroke prevention. Researchers randomly assigned almost 5000 participants who’d had a stroke or TIA one to 6 months before study entry (but had no known history of coronary artery disease) to placebo or a high-intensity statin (80 mg/d atorvastatin). The statin group demonstrated a 4.9-year absolute risk reduction in fatal or nonfatal recurrent stroke of 1.9% (NNT=53).
Given these findings and those from other studies, the AHA and ASA recommend treating patients with stroke or TIA presumed to be of atherosclerotic origin with high-intensity statin therapy, regardless of low-density lipoprotein (LDL) level.3 Of note, statins are not indicated for the secondary prevention of hemorrhagic stroke.
Select antiplatelet therapy based on ischemic stroke subtype. Investigators are still trying to determine the optimal antiplatelet for secondary stroke prevention; it is likely that the ideal choice depends largely on the etiology of the stroke. Trials that did not select patients based on subtype of ischemic stroke have not shown a long-term benefit from dual antiplatelet therapy (clopidogrel and aspirin),23,24 and one double-blind, multicenter trial involving more than 3000 patients with recent stroke secondary to small vessel disease demonstrated harm from such therapy in terms of a significantly increased risk of bleeding and death.6
However, a 2011 study compared aggressive medical management (aspirin 325 mg/d plus clopidogrel 75 mg/d for 90 days) alone to aggressive medical management plus percutaneous transluminal angioplasty and stenting (PTAS). The study involved almost 500 patients who'd had a recent TIA or stroke attributed to intracranial atherosclerotic stenosis. The authors found that the 30-day rate of stroke or death was 14.7% in the PTAS group vs 5.8% in the medical management group.25
Similarly, a randomized double-blind, placebo-controlled trial published in 2013 involving over 5000 patients in China found that short-term use of dual antiplatelets (clopidogrel and aspirin for the first 21 days after an ischemic event, followed by aspirin monotherapy for 90 days) had an absolute risk reduction of 3.5% without increasing the risk of major bleeding in patients with high-risk TIA or minor stroke.26
All stroke patients who do not have an indication for oral anticoagulation should be placed on long-term daily aspirin (75-325 mg); research has shown that lower doses are as effective as higher doses but with a lower risk of adverse gastrointestinal effects, including bleeding.3,20 Aspirin 81 mg/d is a common effective dose.
For patients who cannot tolerate aspirin due to allergy, clopidogrel 75 mg/d is a reasonable alternative. Long-term studies of aspirin vs clopidogrel7 and clopidogrel vs extended-release dipyridamole8 showed no difference in secondary stroke prevention. The International Stroke Trial27 and Chinese Acute Stroke Trial28 both indicate that aspirin should be started as soon as possible after the onset of an acute stroke.
This special population should probably get antiplatelets, too. One recent study explored the use of an antiplatelet vs anticoagulation therapy for stroke patients with carotid artery dissection. The CADISS (Cervical Artery Dissection in Stroke Study) trial29 randomized 250 patients with extracranial carotid and vertebral artery dissection with onset of symptoms within the previous 7 days to either antiplatelet or anticoagulation therapy and found no difference in the primary outcomes of recurrent stroke or death. The study also demonstrated a low risk of recurrent stroke in this population, which was 2% at 3-month follow-up.
Most patients with cervical artery dissection, therefore, are now treated with antiplatelet therapy. That said, situations may still arise in which anticoagulation can be considered, and consultation with a neurologist for guidance on choice of therapy is recommended.
Is an anticoagulant in order? Which agent, when
The most common cause of cardioembolic stroke is AF, which accounts for at least 15% of ischemic strokes, a number that rises in those over the age of 80.20,30,31 A meta-analysis of more than 28,000 patients with non-valvular AF demonstrated that warfarin reduced the risk of stroke by 64%.32
The rate of intracerebral hemorrhages during oral anticoagulation ranges from 0.3% to 0.6% per year.33 The risk of bleeding complications can be mitigated by keeping international normalized ratios ≤3.0, maintaining good BP control, and avoiding concurrent use of antiplatelets in the absence of a clear indication for them.33
Several risk assessment scores, such as the HAS-BLED,34 can help with estimating the risk of hemorrhagic complications, although these scores have their limitations.35,36 Even in an older population (mean age 83 years) with a high risk for falls, warfarin provided a net benefit in a composite endpoint of out-of-hospital death or hospitalization for stroke, MI, or hemorrhage in a retrospective study of over 1200 Medicare beneficiaries.37
AF is not the only cause of cardioembolic stroke to consider. Additional high-risk factors warranting anticoagulation include rheumatic mitral valve disease, the presence of mechanical aortic or mitral valves, known mural thrombus, and acute anterior ST segment elevation myocardial infarctions (STEMIs) with resulting anterior apical dyskinesis/akinesis and concurrent ischemic stroke/TIA.3 (The specific management of each of these situations is beyond the scope of this paper.)
The choice of anticoagulation agent is based on multiple factors, including cost, risk of non-reversible bleeding, drug interactions, renal function, and patient preference. Approved options currently include warfarin/vitamin K antagonist therapy, apixaban, rivaroxaban, dabigatran and edoxaban.3 Choice of therapy will continue to evolve as reversal agents, such as idarucizumab, are developed. Idarucizumab, a reversal agent for dabigatran, received approval from the US Food and Drug Administration in October 2015.38
When to start anticoagulation. There are limited data regarding the optimal timing of initiation of anticoagulation following a stroke; however, a recent multicenter prospective study supported the common practice of initiating anticoagulation therapy within 4 to 14 days of the event.39 Individual patient factors must be taken into consideration, including the size of the stroke (the larger the stroke, the higher the risk for hemorrhagic transformation), BP control, any additional risk factors for bleeding, and the estimated risk of early recurrent stroke.
Bridging patients onto anticoagulation with unfractionated or low-molecular-weight heparin in the setting of acute stroke is not recommended.40 Results from randomized controlled trials involving unfractionated heparin, heparinoids, and low-molecular-weight heparin have not reported any benefit to these agents over aspirin at preventing early stroke recurrence.27,41,42
For immobile or hospitalized patients. Subcutaneous heparin for the prevention of deep vein thrombosis (DVT) during immobility and hospitalization is recommended.43 Patients who cannot tolerate anticoagulation should be maintained on low-dose antiplatelet therapy. Experts do not recommend dual treatment with aspirin and anticoagulation in most cases. However, recent coronary artery stent placement does require temporary dual treatment, with duration dependent on the type of stent placed.
A role for glycemic control? Still to be determined
The specific role of diabetic management in secondary stroke prevention remains unclear. The 2008 ACCORD trial,44 a randomized study involving over 10,000 patients with a median glycated hemoglobin level of 8.1%, investigated intensive hyperglycemic control (targeting a glycated hemoglobin level <6.0% vs <7.9%) as a means of decreasing cardiovascular risk. However, the trial ended 17 months early because of an increase in all-cause mortality in the intensive treatment arm compared with the standard management group. The same trial was also unable to demonstrate a decrease in stroke risk with a decrease in A1c.44
More recently, the IRIS (Insulin Resistance Intervention after Stroke) trial45 (2016) found a 2.8% absolute risk reduction in stroke or MI among participants who had a stroke or TIA in the previous 6 months who were treated with pioglitazone vs placebo over 4.8 years (NNT=36). Participants were required to have insulin resistance, but were excluded if they had diabetes. The authors did, however, report a notable increase in the risk of bone fractures requiring surgery or hospitalization in the pioglitazone arm (5.1% vs 3.2%; number needed to harm [NNH]=53).
The impact this single study should have on standard secondary prevention is not yet clear. The authors concluded, “It seems reasonable to consider individual treatment preference and risk of drug-related adverse events in addition to potential benefits when making patient-specific decisions regarding therapy.”45
Determining whether mechanical interventions are needed
Almost all conditions leading to stroke warrant active medical management, but a few benefit from procedural intervention, as well.
Extracranial carotid atherosclerosis. Carotid endarterectomy or carotid artery stenting is recommended as secondary prevention for patients with a history of stroke or TIA who have ipsilateral high-grade extracranial carotid stenosis of 70% to 99% and, in some cases, 50% to 69%.3,9,20 In patients with mild non-disabling stroke, the optimal timing for these procedures is within 2 weeks of the ischemic event. A delay of 6 weeks is generally preferred for moderate or larger strokes to allow for some healing of the injured brain.
The choice of procedure is based on risk profile, with the most important factor being age. For patients >70 years, endarterectomy is preferred because stenting is associated with an increased risk of stroke.3,9,10 Experts do not recommend either procedure for patients who have had a severe disabling stroke. Generally speaking, these procedures have higher rates of success when they are performed in centers that perform a higher number of these procedures.10
Vertebrobasilar atherosclerosis. Due to generally good compensatory blood flow of the contralateral vertebral artery in the setting of vertebral artery stenosis, and an unacceptably high complication rate of angioplasty and stenting in the basilar artery, medical management is typically the first-line approach. If a patient has recurrent symptoms in the setting of optimal medical management and a focal lesion that is amenable to an endovascular intervention (most commonly a vertebral artery origin high-grade stenosis), angioplasty and stenting may be considered.10
Intracranial atherosclerosis. Similarly, medical management is the preferred strategy for intracranial atherosclerosis. Angioplasty and/or stenting are reserved for complex cases or recurrence despite adherence to secondary stroke prevention measures. Ideally, these patients should be managed with long-term aspirin 81 mg/d, adjunctive clopidogrel 75 mg/d for 90 days post stroke, a high-intensity statin, BP optimization, and any relevant lifestyle interventions.13
Patent foramen ovale. Research to date has not shown that closure of a patent foramen ovale (PFO) is superior to medical therapy for secondary stroke prevention in patients <60 years with cryptogenic stroke.12,46,47 The decision to anticoagulate these patients should be based on the presence or absence of a DVT and not on a PFO alone. In patients with an identified DVT and a contraindication to oral anticoagulation, inferior vena cava filter placement should be considered. For patients with ongoing prothrombotic risk thought to increase the chances of future paradoxical embolism, closure of the PFO may be considered.
CORRESPONDENCE
Stephen A. Martin, MD, EdM, Barre Family Health Center, 151 Worcester Road, Barre, MA 01005; [email protected].
1. Hackam DG, Spence JD. Combining multiple approaches for the secondary prevention of vascular events after stroke: a quantitative modeling study. Stroke. 2007;38:1881-1885.
2. Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S76-S99.
3. Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2160-2236.
4. Rashid P, Leonardi-Bee J, Bath P. Blood pressure reduction and secondary prevention of stroke and other vascular events: a systematic review. Stroke. 2003;34:2741-2748.
5. Amarenco P, Bogousslavsky J, Callahan A, et al, for the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355:549-559.
6. Benavente OR, Hart RG, McClure LA, et al, for the SPS3 Investigators. Effects of clopidogrel added to aspirin in patients with recent lacunar stroke. N Engl J Med. 2012;367:817-825.
7. CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee. Lancet. 1996;348:1329-1339.
8. Sacco RL, Diener HC, Yusuf S, et al. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med. 2008;359:1238-1251.
9. Diethrich EB, N’diaye M, Reid DB. The Carotid Revascularization Endarterectomy versus Stenting Trial (CREST): implications for clinical practice. In: Henry M, Diethrich EB, Polydorou A, eds. The Carotid and Supra-Aortic Trunks: Diagnosis, Angioplasty and Stenting. 2nd ed. Oxford, UK: Wiley-Blackwell; 2011.
10. Brott TG, Halperin JL, Abbara S, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. Circulation. 2011;124:489-532.
11. SPS3 Study Group. Blood pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet. 2013;382:507-515.
12. Carroll JD, Saver JL, Thaler DE, et al. Closure of patent foramen ovale versus medical therapy after cryptogenic stroke. N Engl J Med. 2013;368:1092-1100.
13. Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365:993-1003.
14. Romero JR, Morris J, Pikula A. Stroke prevention: modifying risk factors. Ther Adv Cardiovasc Dis. 2008;2:287-303.
15. Hankey GJ. Smoking and risk of stroke. J Cardiovasc Risk. 1999;6:207-211.
16. Shah RS, Cole JW. Smoking and stroke: the more you smoke the more you stroke. Expert Rev Cardiovasc Ther. 2010;8:917-932.
17. Bhat VM, Cole JW, Sorkin JD, et al. Dose-response relationship between cigarette smoking and risk of ischemic stroke in young women. Stroke. 2008;39:2439-2443.
18. Lakkur S, Judd SE. Diet and stroke: recent evidence supporting a Mediterranean-style diet and food in the primary prevention of stroke. Stroke. 2015;46:2007-2011.
19. de Lorgeril M, Salen P, Martin JL, et al. Mediterranean dietary pattern in a randomized trial: prolonged survival and possible reduced cancer rate. Arch Intern Med. 1998;158:1181-1187.
20. Davis SM, Donnan GA. Clinical practice. Secondary prevention after ischemic stroke or transient ischemic attack. N Engl J Med. 2012;366:1914-1922.
21. Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870-947.
22. Magid DJ, Green BB. Home blood pressure monitoring: take it to the bank. JAMA. 2013;310:40-41.
23. Diener H-C, Bogousslavsky J, Brass LM, et al. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. Lancet (London, England). 2004;364:331-337.
24. Bhatt DL, Fox KAA, Hacke W, et al. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med. 2006;354:1706-1717.
25. Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365:993-1003.
26. Wang Y, Wang Y, Zhao X, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013;369:11-19.
27. The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke. International Stroke Trial Collaborative Group. Lancet. 1997;349:1569-1581.
28. CAST: randomised placebo-controlled trial of early aspirin use in 20,000 patients with acute ischaemic stroke. CAST (Chinese Acute Stroke Trial) Collaborative Group. Lancet. 1997;349:1641-1649.
29. CADISS trial investigators, Markus HS, Hayter E, et al. Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): a randomised trial. Lancet Neurol. 2015;14:361-367.
30. Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. EAFT (European Atrial Fibrillation Trial) Study Group. Lancet. 1993;342:1255-1262.
31. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983-988.
32. Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Int Med. 2007;146:857-867.
33. Hart RG, Tonarelli SB, Pearce LA. Avoiding central nervous system bleeding during antithrombotic therapy. Recent data and ideas. Stroke. 2005;36:1588-1593.
34. Pisters R, Lane DA, Nieuwlaat R, et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: The Euro Heart Survey. Chest. 2010;138:1093-1100.
35. Quinn GR, Singer DE, Chang Y, et al. How well do stroke risk scores predict hemorrhage in patients with atrial fibrillation? Am J Cardiol. 2016;118:697-699.
36. Gorman EW, Perkel D, Dennis D, et al. Validation of the HAS-BLED tool in atrial fibrillation patients receiving rivaroxaban. J Atr Fibrillation. 2016;9:1461.
37. Gage BF, Birman-Deych E, Kerzner R, et al. Incidence of intracranial hemorrhage in patients with atrial fibrillation who are prone to fall. Am J Med. 2005;118:612-617.
38. US Food and Drug Administration. FDA approves Praxbind, the first reversal agent for the anticoagulant Pradaxa. October 16, 2015. Available at: https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm467300.htm. Accessed May 26, 2017.
39. Paciaroni M, Agnelli G, Falocci N, et al. Early recurrence and cerebral bleeding in patients with acute ischemic stroke and atrial fibrillation: effect of anticoagulation and its timing: the RAF Study. Stroke. 2015;46:2175-2182.
40. Sandercock PA, Counsell C, Kane EJ. Anticoagulants for acute ischaemic stroke. Cochrane Database Syst Rev. 2015;3:CD000024.
41. Bath PM, Lindenstrom E, Boysen G, et al. Tinzaparin in acute ischaemic stroke (TAIST): a randomised aspirin-controlled trial. Lancet. 2001;358:702-710.
42. Berge E, Abdelnoor M, Nakstad PH, et al. Low molecular-weight heparin versus aspirin in patients with acute ischaemic stroke and atrial fibrillation: a double-blind randomised study. HAEST Study Group. Heparin in Acute Embolic Stroke Trial. Lancet. 2000;355:1205-1210.
43. Sherman DG, Albers GW, Bladin C, et al. The efficacy and safety of enoxaparin versus unfractionated heparin for the prevention of venous thromboembolism after acute ischaemic stroke (PREVAIL Study): an open-label randomised comparison. Lancet. 2007;369:1347-1355.
44. Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545-2559.
45. Kernan WN, Viscoli CM, Furie KL, et al. Pioglitazone after ischemic stroke or transient ischemic attack. N Engl J Med. 2016;374:1321-1331.
46. Meier B, Kalesan B, Mattle HP, et al. Percutaneous closure of patent foramen ovale in cryptogenic embolism. N Engl J Med. 2013;368:1083-1091.
47. Furlan AJ, Reisman M, Massaro J, et al. Closure or medical therapy for cryptogenic stroke with patent foramen ovale. N Engl J Med. 2012;366:991-999.
1. Hackam DG, Spence JD. Combining multiple approaches for the secondary prevention of vascular events after stroke: a quantitative modeling study. Stroke. 2007;38:1881-1885.
2. Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S76-S99.
3. Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2160-2236.
4. Rashid P, Leonardi-Bee J, Bath P. Blood pressure reduction and secondary prevention of stroke and other vascular events: a systematic review. Stroke. 2003;34:2741-2748.
5. Amarenco P, Bogousslavsky J, Callahan A, et al, for the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355:549-559.
6. Benavente OR, Hart RG, McClure LA, et al, for the SPS3 Investigators. Effects of clopidogrel added to aspirin in patients with recent lacunar stroke. N Engl J Med. 2012;367:817-825.
7. CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee. Lancet. 1996;348:1329-1339.
8. Sacco RL, Diener HC, Yusuf S, et al. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med. 2008;359:1238-1251.
9. Diethrich EB, N’diaye M, Reid DB. The Carotid Revascularization Endarterectomy versus Stenting Trial (CREST): implications for clinical practice. In: Henry M, Diethrich EB, Polydorou A, eds. The Carotid and Supra-Aortic Trunks: Diagnosis, Angioplasty and Stenting. 2nd ed. Oxford, UK: Wiley-Blackwell; 2011.
10. Brott TG, Halperin JL, Abbara S, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. Circulation. 2011;124:489-532.
11. SPS3 Study Group. Blood pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet. 2013;382:507-515.
12. Carroll JD, Saver JL, Thaler DE, et al. Closure of patent foramen ovale versus medical therapy after cryptogenic stroke. N Engl J Med. 2013;368:1092-1100.
13. Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365:993-1003.
14. Romero JR, Morris J, Pikula A. Stroke prevention: modifying risk factors. Ther Adv Cardiovasc Dis. 2008;2:287-303.
15. Hankey GJ. Smoking and risk of stroke. J Cardiovasc Risk. 1999;6:207-211.
16. Shah RS, Cole JW. Smoking and stroke: the more you smoke the more you stroke. Expert Rev Cardiovasc Ther. 2010;8:917-932.
17. Bhat VM, Cole JW, Sorkin JD, et al. Dose-response relationship between cigarette smoking and risk of ischemic stroke in young women. Stroke. 2008;39:2439-2443.
18. Lakkur S, Judd SE. Diet and stroke: recent evidence supporting a Mediterranean-style diet and food in the primary prevention of stroke. Stroke. 2015;46:2007-2011.
19. de Lorgeril M, Salen P, Martin JL, et al. Mediterranean dietary pattern in a randomized trial: prolonged survival and possible reduced cancer rate. Arch Intern Med. 1998;158:1181-1187.
20. Davis SM, Donnan GA. Clinical practice. Secondary prevention after ischemic stroke or transient ischemic attack. N Engl J Med. 2012;366:1914-1922.
21. Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870-947.
22. Magid DJ, Green BB. Home blood pressure monitoring: take it to the bank. JAMA. 2013;310:40-41.
23. Diener H-C, Bogousslavsky J, Brass LM, et al. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. Lancet (London, England). 2004;364:331-337.
24. Bhatt DL, Fox KAA, Hacke W, et al. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med. 2006;354:1706-1717.
25. Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365:993-1003.
26. Wang Y, Wang Y, Zhao X, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013;369:11-19.
27. The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke. International Stroke Trial Collaborative Group. Lancet. 1997;349:1569-1581.
28. CAST: randomised placebo-controlled trial of early aspirin use in 20,000 patients with acute ischaemic stroke. CAST (Chinese Acute Stroke Trial) Collaborative Group. Lancet. 1997;349:1641-1649.
29. CADISS trial investigators, Markus HS, Hayter E, et al. Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): a randomised trial. Lancet Neurol. 2015;14:361-367.
30. Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. EAFT (European Atrial Fibrillation Trial) Study Group. Lancet. 1993;342:1255-1262.
31. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983-988.
32. Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Int Med. 2007;146:857-867.
33. Hart RG, Tonarelli SB, Pearce LA. Avoiding central nervous system bleeding during antithrombotic therapy. Recent data and ideas. Stroke. 2005;36:1588-1593.
34. Pisters R, Lane DA, Nieuwlaat R, et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: The Euro Heart Survey. Chest. 2010;138:1093-1100.
35. Quinn GR, Singer DE, Chang Y, et al. How well do stroke risk scores predict hemorrhage in patients with atrial fibrillation? Am J Cardiol. 2016;118:697-699.
36. Gorman EW, Perkel D, Dennis D, et al. Validation of the HAS-BLED tool in atrial fibrillation patients receiving rivaroxaban. J Atr Fibrillation. 2016;9:1461.
37. Gage BF, Birman-Deych E, Kerzner R, et al. Incidence of intracranial hemorrhage in patients with atrial fibrillation who are prone to fall. Am J Med. 2005;118:612-617.
38. US Food and Drug Administration. FDA approves Praxbind, the first reversal agent for the anticoagulant Pradaxa. October 16, 2015. Available at: https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm467300.htm. Accessed May 26, 2017.
39. Paciaroni M, Agnelli G, Falocci N, et al. Early recurrence and cerebral bleeding in patients with acute ischemic stroke and atrial fibrillation: effect of anticoagulation and its timing: the RAF Study. Stroke. 2015;46:2175-2182.
40. Sandercock PA, Counsell C, Kane EJ. Anticoagulants for acute ischaemic stroke. Cochrane Database Syst Rev. 2015;3:CD000024.
41. Bath PM, Lindenstrom E, Boysen G, et al. Tinzaparin in acute ischaemic stroke (TAIST): a randomised aspirin-controlled trial. Lancet. 2001;358:702-710.
42. Berge E, Abdelnoor M, Nakstad PH, et al. Low molecular-weight heparin versus aspirin in patients with acute ischaemic stroke and atrial fibrillation: a double-blind randomised study. HAEST Study Group. Heparin in Acute Embolic Stroke Trial. Lancet. 2000;355:1205-1210.
43. Sherman DG, Albers GW, Bladin C, et al. The efficacy and safety of enoxaparin versus unfractionated heparin for the prevention of venous thromboembolism after acute ischaemic stroke (PREVAIL Study): an open-label randomised comparison. Lancet. 2007;369:1347-1355.
44. Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545-2559.
45. Kernan WN, Viscoli CM, Furie KL, et al. Pioglitazone after ischemic stroke or transient ischemic attack. N Engl J Med. 2016;374:1321-1331.
46. Meier B, Kalesan B, Mattle HP, et al. Percutaneous closure of patent foramen ovale in cryptogenic embolism. N Engl J Med. 2013;368:1083-1091.
47. Furlan AJ, Reisman M, Massaro J, et al. Closure or medical therapy for cryptogenic stroke with patent foramen ovale. N Engl J Med. 2012;366:991-999.
From The Journal of Family Practice | 2017;66(7):420-422,424-427.
PRACTICE RECOMMENDATIONS
› Encourage lifestyle modifications, including smoking cessation, alcohol moderation, appropriate diet, and exercise to reduce the risk of recurrent stroke. A
› Optimize blood pressure control using an angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker and a thiazide diuretic. A
› Only use beta-blockers if there is another indication for them. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Stroke: A road map for subacute management
CASE › A 68-year-old woman with hypertension and hyperlipidemia comes into your office for evaluation of a 30-minute episode of sudden-onset right-hand weakness and difficulty speaking that occurred 4 days earlier. The patient, who is also a smoker, has come in at the insistence of her daughter. On examination, her blood pressure (BP) is 145/88 mm Hg and her heart rate is 76 beats/minute and regular. She appears well and her language function is normal. The rest of her examination is normal. How would you proceed?
Stroke—the death of nerve cells due to a lack of blood supply from either infarction or hemorrhage—strikes nearly 800,000 people in the United States every year.1,2 Of these events, 130,000 are fatal, making stroke the fifth leading cause of death.3 Effective, early evaluation and cause-specific treatment are crucial parts of stroke care.
Research has helped to clarify the critical role primary care physicians play in recognizing, triaging, and managing stroke and transient ischemic attacks (TIA). This article reviews what we know about the different ways that a stroke and a TIA can present, the appropriate diagnostic work-up for patients presenting with symptoms of either event, and management strategies for subacute care (24 hours to up to 14 days after a stroke has occurred).4,5 Unless otherwise specified, this review will focus on ischemic stroke because 87% of strokes are attributable to ischemia.1
A follow-up to this article on secondary stroke prevention will appear in the journal next month.
Look to onset more than type of symptoms for clues
Stroke presents as a sudden onset of neurologic deficits (language, motor, sensory, cerebellar, or brainstem functions) (TABLE 14). Because presenting symptoms can vary widely, sudden onset, rather than particular symptoms, should raise a red flag for potential stroke.
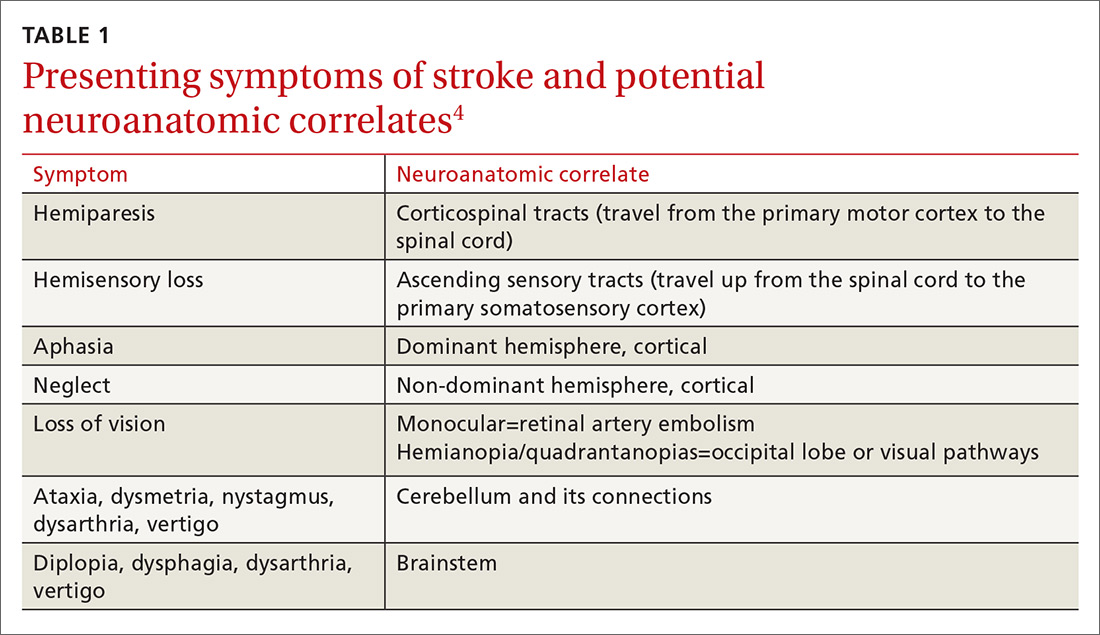
The differential diagnosis includes: seizure, complex migraine, medication effect (eg, slurred speech or confusion after taking a central nervous system [CNS] depressant), toxin exposure, electrolyte abnormalities (especially hypoglycemia), concussion/trauma, infection of the CNS, peripheral vertigo, demyelination, intracranial mass, Bell’s palsy, and psychogenic disorders. The history and physical, along with laboratory findings and brain imaging (detailed later in this article), will guide the FP toward (or away from) these various etiologies.
Optimal triage is a subject of ongoing interest and research
If stroke or TIA remains a possibility after an initial assessment, it’s time to stratify patients by risk.
One of the most widely accepted tools is the ABCD2 score (see TABLE 26). Clinicians can employ the ABCD2 risk stratification tool when trying to determine whether it is reasonable to pursue an expedited work-up (ie, <1 day) in the outpatient setting or recommend that the patient be evaluated in an emergency department (ED). The 90-day stroke rate following a TIA ranges from 3% with an ABCD2 score of 0 to 3 to 18% with a score of 6 or 7. A score of 0 to 3 is considered relatively low risk; in the absence of other compelling factors, rapid outpatient evaluation is appropriate. For patients with an ABCD2 score ≥4, referral to the ED or direct admission to the hospital is advised.
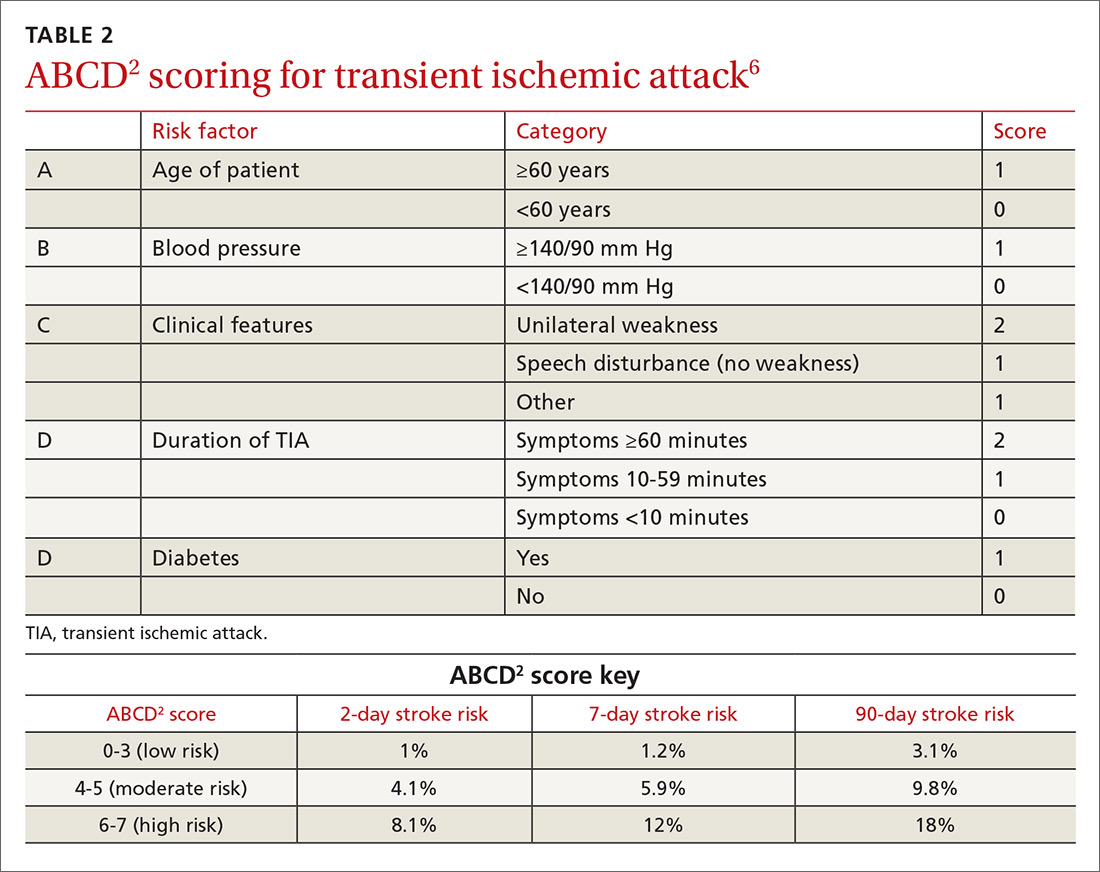
The validity of the ABCD2 score for risk stratification has been studied extensively with conflicting results.7-10 As with any assessment tool, it should be used as a guide, and should not supplant a full assessment of the patient or the judgment of the examining physician. In making the decision regarding inpatient or outpatient evaluation, it’s also important to consider available resources, access to specialists, and patient preference.
In a 2016 population-based study, the 30-day recurrent stroke/TIA rate for patients hospitalized for TIA was 3% compared with 10.7% for those discharged from the ED with referral to a stroke clinic and 10.6% for those discharged from the ED without a referral to a stroke clinic.11 These data suggest that only patients for whom you have a low clinical suspicion of stroke/TIA should be worked up as outpatients, and that hospital admission is advised in moderate- and high-risk cases. The findings also highlight the critical role that primary care physicians can play in triaging and managing these patients for secondary prevention.
CASE › This patient’s recent history of sudden-onset right-sided weakness and expressive language dysfunction is suspicious for left hemispheric ischemia. She has several risk factors for stroke, and her ABCD2 score is 5 (hypertension, age ≥60 years, unilateral weakness, and duration 10-59 min), which places her at moderate risk. Thus, the recommendation would be to have her go directly to an ED for rapid evaluation.
The diagnostic work-up
Even when a patient is sent to the ED, the FP plays a critical role in his or her continuing care. FPs will often coordinate with inpatient care and manage transition of care to the outpatient setting. (And in many communities, the ED or hospital physicians may themselves be family practitioners.)
In terms of care, not even an aspirin should be administered in a case like this because the patient has not yet had any neuroimaging, and differentiation of ischemic from hemorrhagic stroke cannot be made on clinical grounds alone. Once an ischemic stroke is confirmed, determining the etiology is critical given the significant management differences between the different types of stroke (atherosclerotic, cardioembolic, lacunar, or other).
Which imaging method, and when?
While a computerized tomography (CT) scan is the preferred initial imaging strategy for acute stroke to discern the ischemic type from the hemorrhagic, MRI is preferred for the evaluation of acute ischemic stroke because the method has a higher sensitivity for infarction and a greater ability to identify findings (such as demyelination) that would suggest an alternative diagnosis.
In addition to evaluating the brain parenchyma, physicians must also assess the cerebral vasculature. CT angiography (CTA) or MR angiography (MRA) of the head and neck are preferred over carotid ultrasound because they are capable of evaluating the entire cerebrovascular system12,13 and can be instrumental in identifying potential causes of stroke, as well as guiding therapeutic decisions. Carotid ultrasound is a reasonable alternative for patients presenting with symptoms indicative of anterior circulation involvement when CTA and MRA are unavailable or contraindicated, but it will not identify intracranial vascular disease, proximal common carotid disease, or vertebrobasilar disease.
Getting to the cause of suspected stroke: Labs and other diagnostic tests
A routine work-up includes BP checks, routine labs (complete blood count, complete metabolic panel, coagulation profile, and troponin), an electrocardiogram (EKG), a transthoracic echocardiogram (TTE) with bubble study if possible, and a minimum of 24 to 48 hours of cardiac rhythm monitoring. Cardiac rhythm monitoring should be extended in the setting of clinical concern for unidentified paroxysmal atrial fibrillation, such as an embolism without a proximal vascular source, multiple embolic infarcts in different vascular territories, a dilated left atrium, or other risk factors for atrial fibrillation that include smoking, systolic hypertension, diabetes, and heart failure (see TABLE 312,13,17,18).14-16 This standard diagnostic work-up will identify the cause of stroke in 70% to 80% of patients.19
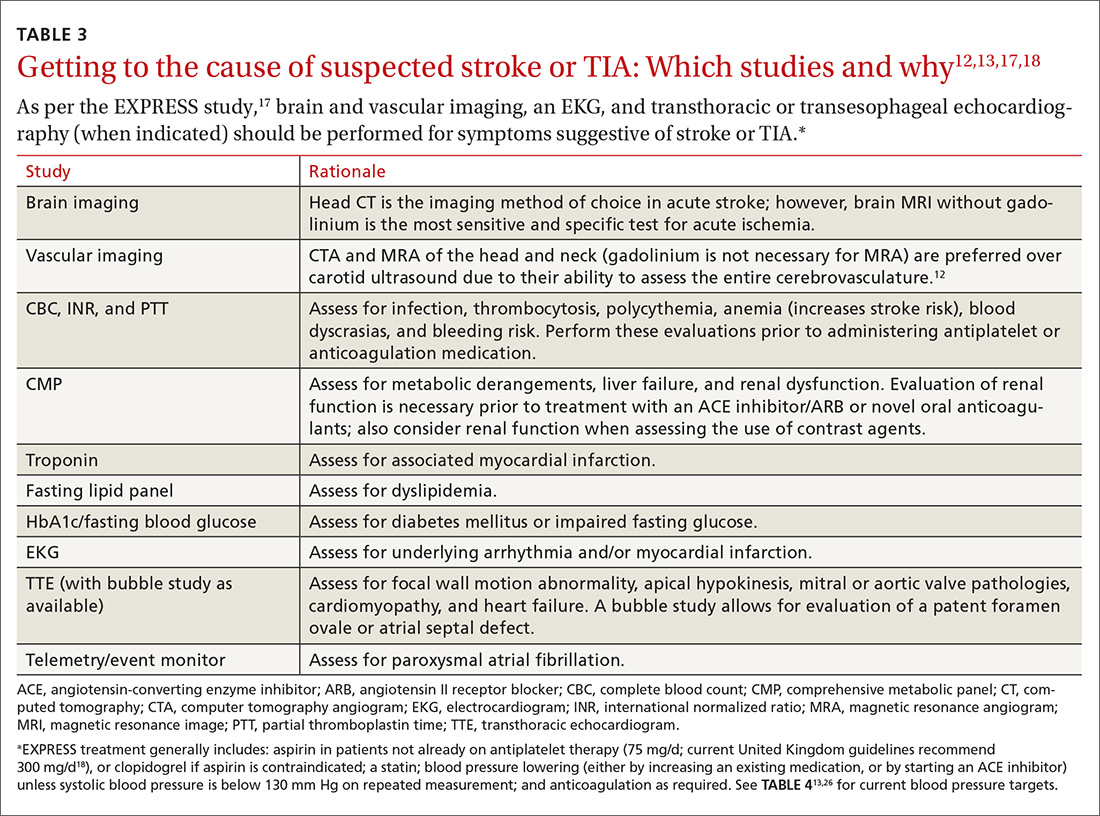
Additional investigations to consider if the etiology is not yet elucidated include a transesophageal echocardiogram (TEE), cerebral angiography, a coagulopathy evaluation, a lumbar puncture, and a vasculitis work-up. If available, consultation with a neurologist is appropriate for any patient who has had a stroke or TIA. Patients with unclear etiologies or for whom there are questions concerning strategies for preventing secondary stroke should be referred to Neurology and preferably a stroke specialist.
Timing matters, even when symptoms have resolved (ie, TIA).11,20 The EXPRESS trial17 (the Early use of eXisting PREventive Strategies for Stroke) looked at the effect of urgent assessment and treatment (≤1 day) of patients presenting with a TIA or minor stroke on the risk of recurrent stroke within 90 days. The diagnostic work-up included brain and vascular imaging together with an EKG. This intensive approach led to an absolute risk reduction of 8.2% (from 10.3% to 2.1%) in the risk of recurrent stroke at 90 days (number needed to treat [NNT]=12).17
Expedited work-up and treatment was also recently evaluated in a non-trial, real-world setting and was associated with reducing recurrent stroke by more than half the rate reported in older studies.20 Overall, the data suggest that evaluation within 24 hours confers substantial benefit, and that this evaluation can happen in an outpatient setting.21-23
Acute management: Use of tPA
Once imaging rules out intracranial hemorrhage, patients should be treated with tissue plasminogen activator (tPA) or an endovascular intervention as per guidelines.24 For patients with ischemic stroke ineligible for tPA or endovascular treatments, the initial focus is to determine the etiology of the symptoms so that the best strategies for prevention of secondary stroke may be employed.
Aspirin should be provided within 24 to 48 hours to all patients after intracranial hemorrhage is ruled out. Aspirin should be delayed for 24 hours in those given thrombolytics. The initial recommended dose of aspirin is 325 mg with continued low-dose (81 mg) aspirin daily.13 The addition of clopidogrel to aspirin within 24 hours of an event and continued for 21 days, followed by aspirin alone, was shown to be beneficial in a Chinese population with high-risk TIA (ABCD2 score ≥4) or minor stroke (National Institutes of Health Stroke Scale [NIHSS] ≤3).25 Anticoagulation with heparin, warfarin, or a novel oral anticoagulant is generally not indicated in the acute setting due to the risk of hemorrhagic transformation.
Acute BP management depends upon the type of stroke (ischemic or hemorrhagic), eligibility for thrombolytics, timing of presentation, and possible comorbidities such as myocardial infarction or aortic dissection (see TABLE 413,26). In the absence of contraindications, high-intensity statins should be initiated in all patients able to take oral medications.
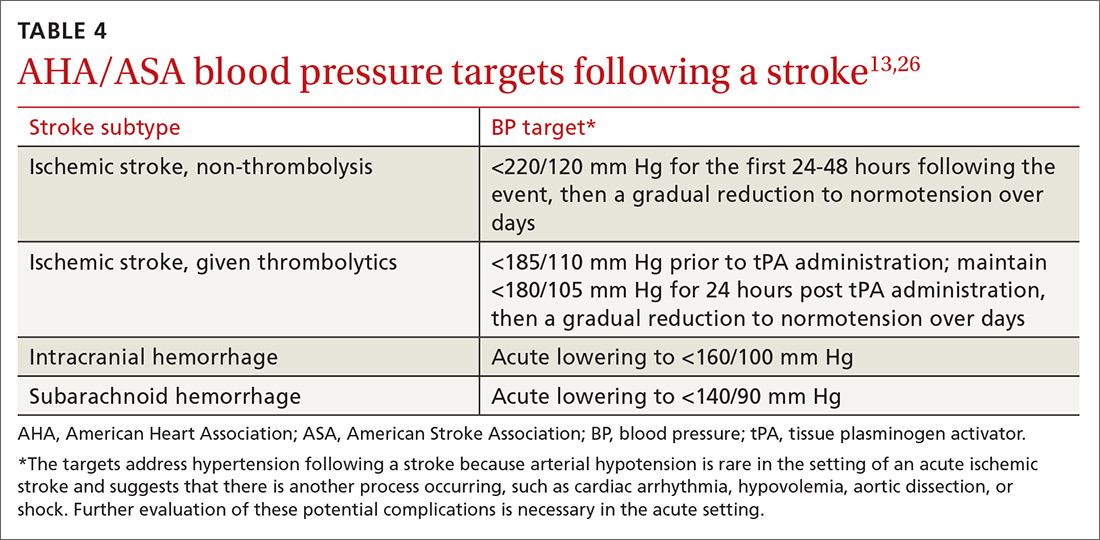
CASE › You appropriately referred your patient to the local ED. A head CT with head and neck CTA was performed. While the head CT did not show any abnormalities, the CTA demonstrated high-grade left internal carotid artery stenosis. The patient was given an initial dose of aspirin 325 mg and a high-intensity statin and admitted for further management. An MRI revealed a small shower of emboli in the left hemisphere, confirming the diagnosis of stroke over TIA. Labs were marginally remarkable with a low-density lipoprotein level of 115 mg/dL and an HbA1c of 6.2. Telemetry monitoring did not reveal any arrhythmias, and TTE was normal. BP remained in the high-normal to low-hypertensive range.
A Vascular Surgery consultation was obtained and the patient underwent a left carotid endarterectomy the following day. She did well without surgical complications. Her BP medications were adjusted; a combination of an angiotensin-converting enzyme inhibitor and a thiazide diuretic achieved a goal BP <140/90 mm Hg.
Permissive hypertension was not indicated due to her presentation >48 hours beyond the acute event. Low-dose aspirin and a high-intensity statin were continued, for secondary stroke prevention in the setting of atherosclerotic disease. She received smoking cessation counseling, which will continue.
CORRESPONDENCE
Stephen A. Martin, MD, EdM, Barre Family Health Center, 151 Worcester Road, Barre, MA 01005; [email protected].
1. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135:e146-e603.
2. Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:2064-2089.
3. Kochanek KD, Murphy SL, Xu J, et al. Mortality in the United States, 2013. NCHS Data Brief. 2014:1-8. Available at: https://www.cdc.gov/nchs/data/databriefs/db178.pdf. Accessed June 5, 2016.
4. Flossmann E, Redgrave JN, Briley D, et al. Reliability of clinical diagnosis of the symptomatic vascular territory in patients with recent transient ischemic attack or minor stroke. Stroke. 2008;39:2457-2460.
5. Josephson SA, Sidney S, Pham TN, et al. Higher ABCD2 score predicts patients most likely to have true transient ischemic attack. Stroke. 2008;39:3096-3098. Available at: http://www.ncbi.nlm.nih.gov/pubmed/18688003. Accessed June 5, 2016.
6. Hankey GJ. The ABCD, California, and unified ABCD2 risk scores predicted stroke within 2, 7, and 90 days after TIA. Evid Based Med. 2007;12:88.
7. Sheehan OC, Kyne L, Kelly LA, et al. Population-based study of ABCD2 score, carotid stenosis, and atrial fibrillation for early stroke prediction after transient ischemic attack: the North Dublin TIA study. Stroke. 2010;41:844-850.
8. Rothwell PM, Giles MF, Flossmann E, et al. A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet. 2005; 366:29-36.
9. Tsivgoulis G, Spengos K, Manta P, et al. Validation of the ABCD score in identifying individuals at high early risk of stroke after a transient ischemic attack: a hospital-based case series study. Stroke. 2006;37:2892-2897.
10. Kiyohara T, Kamouchi M, Kumai Y, et al. ABCD3 and ABCD3-I scores are superior to ABCD2 score in the prediction of short- and long-term risks of stroke after transient ischemic attack. Stroke. 2014;45:418-425.
11. Sacco RL, Rundek T. The value of urgent specialized care for TIA and minor stroke. N Engl J Med. 2016;374:1577-1579.
12. Demchuk AM, Menon BK, Goyal M. Comparing vessel imaging: noncontrast computed tomography/computed tomographic angiography should be the new minimum standard in acute disabling stroke. Stroke. 2016;47:273-281.
13. Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870-947.
14. Gladstone DJ, Spring M, Dorian P, et al. Atrial fibrillation in patients with cryptogenic stroke. N Engl J Med. 2014;370:2467-2477.
15. Sanna T, Diener HC, Passman RS, et al. Cryptogenic stroke and underlying atrial fibrillation. N Engl J Med. 2014;370:2478-2486.
16. Christophersen IE, Yin X, Larson MG, et al. A comparison of the CHARGE-AF and the CHA2DS2-VASc risk scores for prediction of atrial fibrillation ni the Framingham Heart Study. Am Heart J. 2016;178:45-54.
17. Rothwell PM, Giles MF, Chandratheva A, et al. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet. 2007;370:1432-1442.
18. National Institute for Health and Care Excellence. Stroke and transient ischaemic attack in over 16s: diagnosis and initial management. Available at: https://www.nice.org.uk/guidance/cg68. Published 2008. Accessed February 5, 2017.
19. Hart RG, Diener HC, Coutts SB, et al. Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol. 2014;13:429-438.
20. Amarenco P, Lavallée PC, Labreuche J, et al. One-year risk of stroke after transient ischemic attack or minor stroke. N Engl J Med. 2016;374:1533-1542.
21. Joshi JK, Ouyang B, Prabhakaran S. Should TIA patients be hospitalized or referred to a same-day clinic? A decision analysis. Neurology. 2011;77:2082-2088.
22. Mijalski C, Silver B. TIA management: should TIA patients be admitted? should TIA patients get combination antiplatelet therapy? The Neurohospitalist. 2015;5:151-160.
23. Silver B, Adeoye O. Management of patients with transient ischemic attack in the emergency department. Neurology. 2016;86:1568-1569.
24. Demaerschalk BM, Kleindorfer DO, Adeoye OM, et al. Scientific rationale for the inclusion and exclusion criteria for intravenous alteplase in acute ischemic stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47:581-641.
25. Wang Y, Wang Y, Zhao X, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013;369:11-19.
26. Hemphill JC, Greenberg SM, Anderson CS, et al. Guidelines for the management of spontaneous intracerebral hemorrhage. Stroke. 2015;46:2032-2060.
CASE › A 68-year-old woman with hypertension and hyperlipidemia comes into your office for evaluation of a 30-minute episode of sudden-onset right-hand weakness and difficulty speaking that occurred 4 days earlier. The patient, who is also a smoker, has come in at the insistence of her daughter. On examination, her blood pressure (BP) is 145/88 mm Hg and her heart rate is 76 beats/minute and regular. She appears well and her language function is normal. The rest of her examination is normal. How would you proceed?
Stroke—the death of nerve cells due to a lack of blood supply from either infarction or hemorrhage—strikes nearly 800,000 people in the United States every year.1,2 Of these events, 130,000 are fatal, making stroke the fifth leading cause of death.3 Effective, early evaluation and cause-specific treatment are crucial parts of stroke care.
Research has helped to clarify the critical role primary care physicians play in recognizing, triaging, and managing stroke and transient ischemic attacks (TIA). This article reviews what we know about the different ways that a stroke and a TIA can present, the appropriate diagnostic work-up for patients presenting with symptoms of either event, and management strategies for subacute care (24 hours to up to 14 days after a stroke has occurred).4,5 Unless otherwise specified, this review will focus on ischemic stroke because 87% of strokes are attributable to ischemia.1
A follow-up to this article on secondary stroke prevention will appear in the journal next month.
Look to onset more than type of symptoms for clues
Stroke presents as a sudden onset of neurologic deficits (language, motor, sensory, cerebellar, or brainstem functions) (TABLE 14). Because presenting symptoms can vary widely, sudden onset, rather than particular symptoms, should raise a red flag for potential stroke.
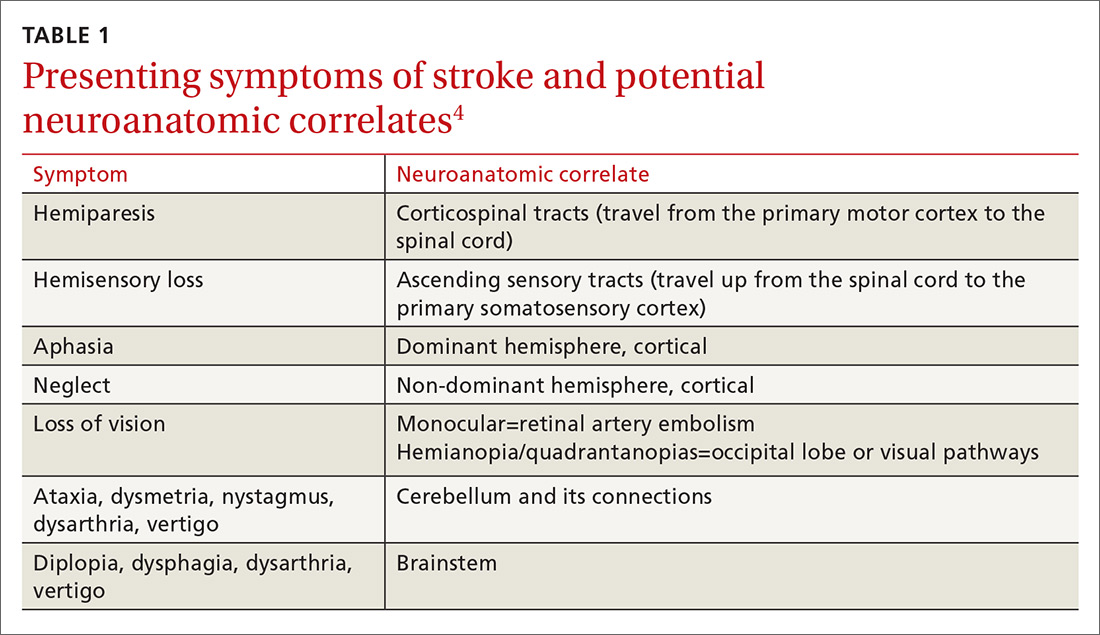
The differential diagnosis includes: seizure, complex migraine, medication effect (eg, slurred speech or confusion after taking a central nervous system [CNS] depressant), toxin exposure, electrolyte abnormalities (especially hypoglycemia), concussion/trauma, infection of the CNS, peripheral vertigo, demyelination, intracranial mass, Bell’s palsy, and psychogenic disorders. The history and physical, along with laboratory findings and brain imaging (detailed later in this article), will guide the FP toward (or away from) these various etiologies.
Optimal triage is a subject of ongoing interest and research
If stroke or TIA remains a possibility after an initial assessment, it’s time to stratify patients by risk.
One of the most widely accepted tools is the ABCD2 score (see TABLE 26). Clinicians can employ the ABCD2 risk stratification tool when trying to determine whether it is reasonable to pursue an expedited work-up (ie, <1 day) in the outpatient setting or recommend that the patient be evaluated in an emergency department (ED). The 90-day stroke rate following a TIA ranges from 3% with an ABCD2 score of 0 to 3 to 18% with a score of 6 or 7. A score of 0 to 3 is considered relatively low risk; in the absence of other compelling factors, rapid outpatient evaluation is appropriate. For patients with an ABCD2 score ≥4, referral to the ED or direct admission to the hospital is advised.
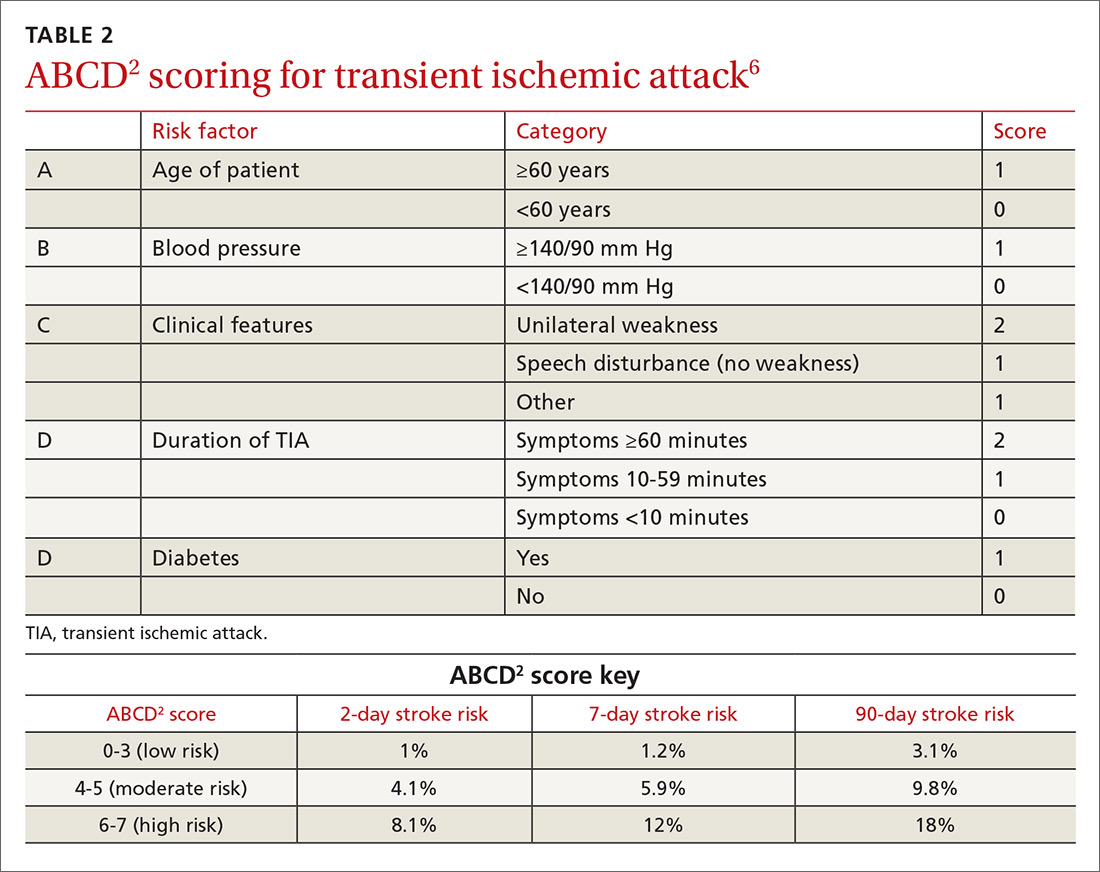
The validity of the ABCD2 score for risk stratification has been studied extensively with conflicting results.7-10 As with any assessment tool, it should be used as a guide, and should not supplant a full assessment of the patient or the judgment of the examining physician. In making the decision regarding inpatient or outpatient evaluation, it’s also important to consider available resources, access to specialists, and patient preference.
In a 2016 population-based study, the 30-day recurrent stroke/TIA rate for patients hospitalized for TIA was 3% compared with 10.7% for those discharged from the ED with referral to a stroke clinic and 10.6% for those discharged from the ED without a referral to a stroke clinic.11 These data suggest that only patients for whom you have a low clinical suspicion of stroke/TIA should be worked up as outpatients, and that hospital admission is advised in moderate- and high-risk cases. The findings also highlight the critical role that primary care physicians can play in triaging and managing these patients for secondary prevention.
CASE › This patient’s recent history of sudden-onset right-sided weakness and expressive language dysfunction is suspicious for left hemispheric ischemia. She has several risk factors for stroke, and her ABCD2 score is 5 (hypertension, age ≥60 years, unilateral weakness, and duration 10-59 min), which places her at moderate risk. Thus, the recommendation would be to have her go directly to an ED for rapid evaluation.
The diagnostic work-up
Even when a patient is sent to the ED, the FP plays a critical role in his or her continuing care. FPs will often coordinate with inpatient care and manage transition of care to the outpatient setting. (And in many communities, the ED or hospital physicians may themselves be family practitioners.)
In terms of care, not even an aspirin should be administered in a case like this because the patient has not yet had any neuroimaging, and differentiation of ischemic from hemorrhagic stroke cannot be made on clinical grounds alone. Once an ischemic stroke is confirmed, determining the etiology is critical given the significant management differences between the different types of stroke (atherosclerotic, cardioembolic, lacunar, or other).
Which imaging method, and when?
While a computerized tomography (CT) scan is the preferred initial imaging strategy for acute stroke to discern the ischemic type from the hemorrhagic, MRI is preferred for the evaluation of acute ischemic stroke because the method has a higher sensitivity for infarction and a greater ability to identify findings (such as demyelination) that would suggest an alternative diagnosis.
In addition to evaluating the brain parenchyma, physicians must also assess the cerebral vasculature. CT angiography (CTA) or MR angiography (MRA) of the head and neck are preferred over carotid ultrasound because they are capable of evaluating the entire cerebrovascular system12,13 and can be instrumental in identifying potential causes of stroke, as well as guiding therapeutic decisions. Carotid ultrasound is a reasonable alternative for patients presenting with symptoms indicative of anterior circulation involvement when CTA and MRA are unavailable or contraindicated, but it will not identify intracranial vascular disease, proximal common carotid disease, or vertebrobasilar disease.
Getting to the cause of suspected stroke: Labs and other diagnostic tests
A routine work-up includes BP checks, routine labs (complete blood count, complete metabolic panel, coagulation profile, and troponin), an electrocardiogram (EKG), a transthoracic echocardiogram (TTE) with bubble study if possible, and a minimum of 24 to 48 hours of cardiac rhythm monitoring. Cardiac rhythm monitoring should be extended in the setting of clinical concern for unidentified paroxysmal atrial fibrillation, such as an embolism without a proximal vascular source, multiple embolic infarcts in different vascular territories, a dilated left atrium, or other risk factors for atrial fibrillation that include smoking, systolic hypertension, diabetes, and heart failure (see TABLE 312,13,17,18).14-16 This standard diagnostic work-up will identify the cause of stroke in 70% to 80% of patients.19
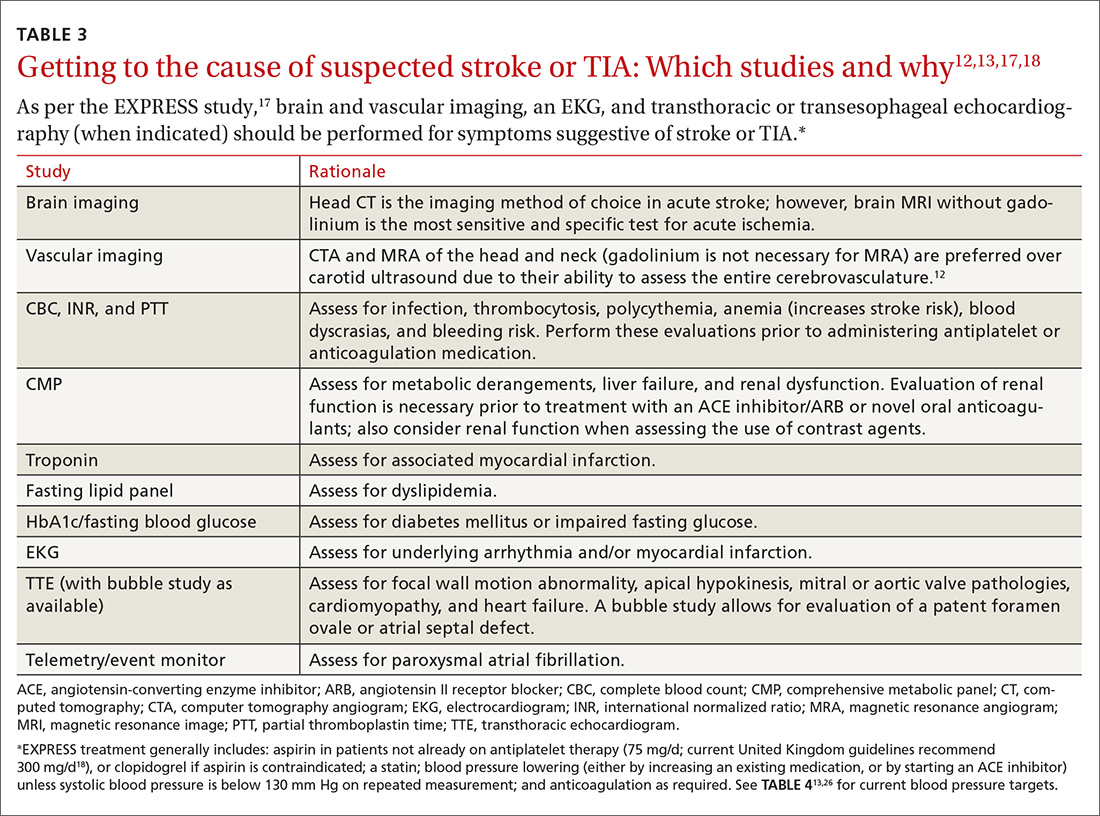
Additional investigations to consider if the etiology is not yet elucidated include a transesophageal echocardiogram (TEE), cerebral angiography, a coagulopathy evaluation, a lumbar puncture, and a vasculitis work-up. If available, consultation with a neurologist is appropriate for any patient who has had a stroke or TIA. Patients with unclear etiologies or for whom there are questions concerning strategies for preventing secondary stroke should be referred to Neurology and preferably a stroke specialist.
Timing matters, even when symptoms have resolved (ie, TIA).11,20 The EXPRESS trial17 (the Early use of eXisting PREventive Strategies for Stroke) looked at the effect of urgent assessment and treatment (≤1 day) of patients presenting with a TIA or minor stroke on the risk of recurrent stroke within 90 days. The diagnostic work-up included brain and vascular imaging together with an EKG. This intensive approach led to an absolute risk reduction of 8.2% (from 10.3% to 2.1%) in the risk of recurrent stroke at 90 days (number needed to treat [NNT]=12).17
Expedited work-up and treatment was also recently evaluated in a non-trial, real-world setting and was associated with reducing recurrent stroke by more than half the rate reported in older studies.20 Overall, the data suggest that evaluation within 24 hours confers substantial benefit, and that this evaluation can happen in an outpatient setting.21-23
Acute management: Use of tPA
Once imaging rules out intracranial hemorrhage, patients should be treated with tissue plasminogen activator (tPA) or an endovascular intervention as per guidelines.24 For patients with ischemic stroke ineligible for tPA or endovascular treatments, the initial focus is to determine the etiology of the symptoms so that the best strategies for prevention of secondary stroke may be employed.
Aspirin should be provided within 24 to 48 hours to all patients after intracranial hemorrhage is ruled out. Aspirin should be delayed for 24 hours in those given thrombolytics. The initial recommended dose of aspirin is 325 mg with continued low-dose (81 mg) aspirin daily.13 The addition of clopidogrel to aspirin within 24 hours of an event and continued for 21 days, followed by aspirin alone, was shown to be beneficial in a Chinese population with high-risk TIA (ABCD2 score ≥4) or minor stroke (National Institutes of Health Stroke Scale [NIHSS] ≤3).25 Anticoagulation with heparin, warfarin, or a novel oral anticoagulant is generally not indicated in the acute setting due to the risk of hemorrhagic transformation.
Acute BP management depends upon the type of stroke (ischemic or hemorrhagic), eligibility for thrombolytics, timing of presentation, and possible comorbidities such as myocardial infarction or aortic dissection (see TABLE 413,26). In the absence of contraindications, high-intensity statins should be initiated in all patients able to take oral medications.
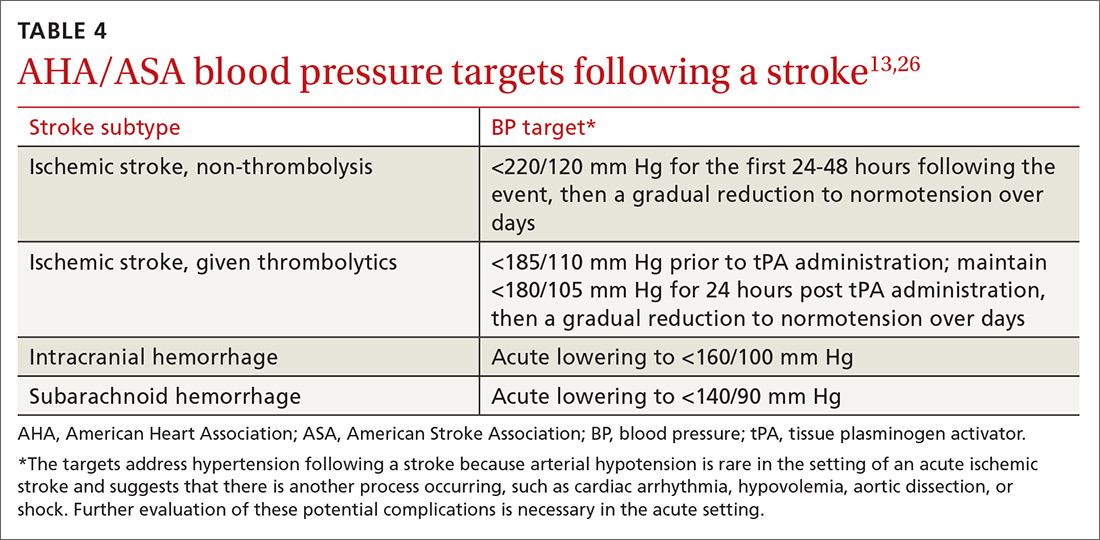
CASE › You appropriately referred your patient to the local ED. A head CT with head and neck CTA was performed. While the head CT did not show any abnormalities, the CTA demonstrated high-grade left internal carotid artery stenosis. The patient was given an initial dose of aspirin 325 mg and a high-intensity statin and admitted for further management. An MRI revealed a small shower of emboli in the left hemisphere, confirming the diagnosis of stroke over TIA. Labs were marginally remarkable with a low-density lipoprotein level of 115 mg/dL and an HbA1c of 6.2. Telemetry monitoring did not reveal any arrhythmias, and TTE was normal. BP remained in the high-normal to low-hypertensive range.
A Vascular Surgery consultation was obtained and the patient underwent a left carotid endarterectomy the following day. She did well without surgical complications. Her BP medications were adjusted; a combination of an angiotensin-converting enzyme inhibitor and a thiazide diuretic achieved a goal BP <140/90 mm Hg.
Permissive hypertension was not indicated due to her presentation >48 hours beyond the acute event. Low-dose aspirin and a high-intensity statin were continued, for secondary stroke prevention in the setting of atherosclerotic disease. She received smoking cessation counseling, which will continue.
CORRESPONDENCE
Stephen A. Martin, MD, EdM, Barre Family Health Center, 151 Worcester Road, Barre, MA 01005; [email protected].
CASE › A 68-year-old woman with hypertension and hyperlipidemia comes into your office for evaluation of a 30-minute episode of sudden-onset right-hand weakness and difficulty speaking that occurred 4 days earlier. The patient, who is also a smoker, has come in at the insistence of her daughter. On examination, her blood pressure (BP) is 145/88 mm Hg and her heart rate is 76 beats/minute and regular. She appears well and her language function is normal. The rest of her examination is normal. How would you proceed?
Stroke—the death of nerve cells due to a lack of blood supply from either infarction or hemorrhage—strikes nearly 800,000 people in the United States every year.1,2 Of these events, 130,000 are fatal, making stroke the fifth leading cause of death.3 Effective, early evaluation and cause-specific treatment are crucial parts of stroke care.
Research has helped to clarify the critical role primary care physicians play in recognizing, triaging, and managing stroke and transient ischemic attacks (TIA). This article reviews what we know about the different ways that a stroke and a TIA can present, the appropriate diagnostic work-up for patients presenting with symptoms of either event, and management strategies for subacute care (24 hours to up to 14 days after a stroke has occurred).4,5 Unless otherwise specified, this review will focus on ischemic stroke because 87% of strokes are attributable to ischemia.1
A follow-up to this article on secondary stroke prevention will appear in the journal next month.
Look to onset more than type of symptoms for clues
Stroke presents as a sudden onset of neurologic deficits (language, motor, sensory, cerebellar, or brainstem functions) (TABLE 14). Because presenting symptoms can vary widely, sudden onset, rather than particular symptoms, should raise a red flag for potential stroke.
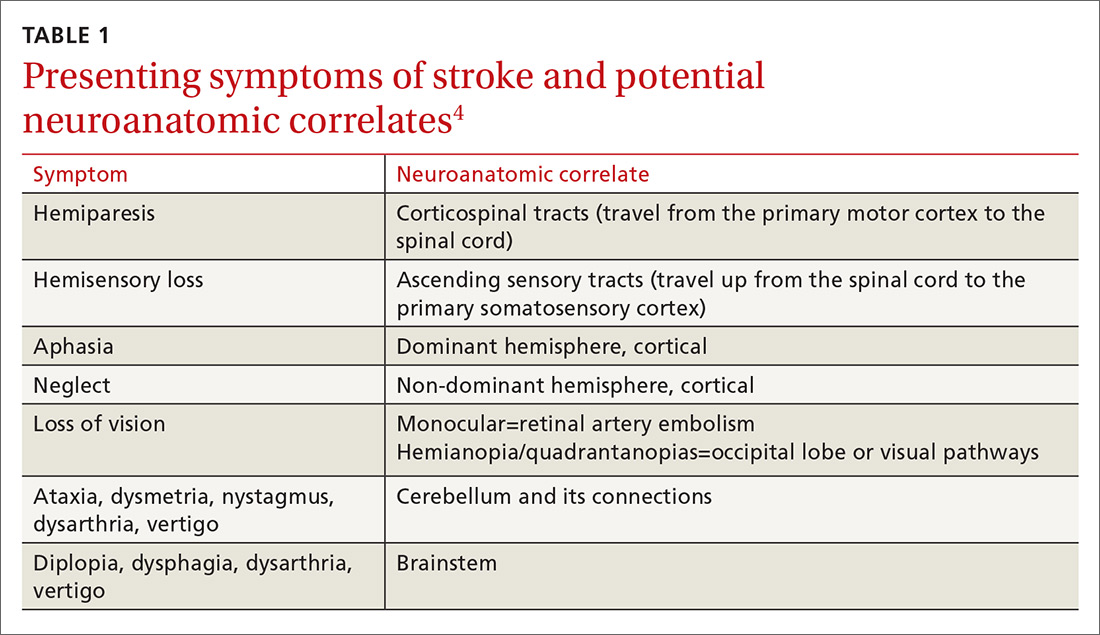
The differential diagnosis includes: seizure, complex migraine, medication effect (eg, slurred speech or confusion after taking a central nervous system [CNS] depressant), toxin exposure, electrolyte abnormalities (especially hypoglycemia), concussion/trauma, infection of the CNS, peripheral vertigo, demyelination, intracranial mass, Bell’s palsy, and psychogenic disorders. The history and physical, along with laboratory findings and brain imaging (detailed later in this article), will guide the FP toward (or away from) these various etiologies.
Optimal triage is a subject of ongoing interest and research
If stroke or TIA remains a possibility after an initial assessment, it’s time to stratify patients by risk.
One of the most widely accepted tools is the ABCD2 score (see TABLE 26). Clinicians can employ the ABCD2 risk stratification tool when trying to determine whether it is reasonable to pursue an expedited work-up (ie, <1 day) in the outpatient setting or recommend that the patient be evaluated in an emergency department (ED). The 90-day stroke rate following a TIA ranges from 3% with an ABCD2 score of 0 to 3 to 18% with a score of 6 or 7. A score of 0 to 3 is considered relatively low risk; in the absence of other compelling factors, rapid outpatient evaluation is appropriate. For patients with an ABCD2 score ≥4, referral to the ED or direct admission to the hospital is advised.
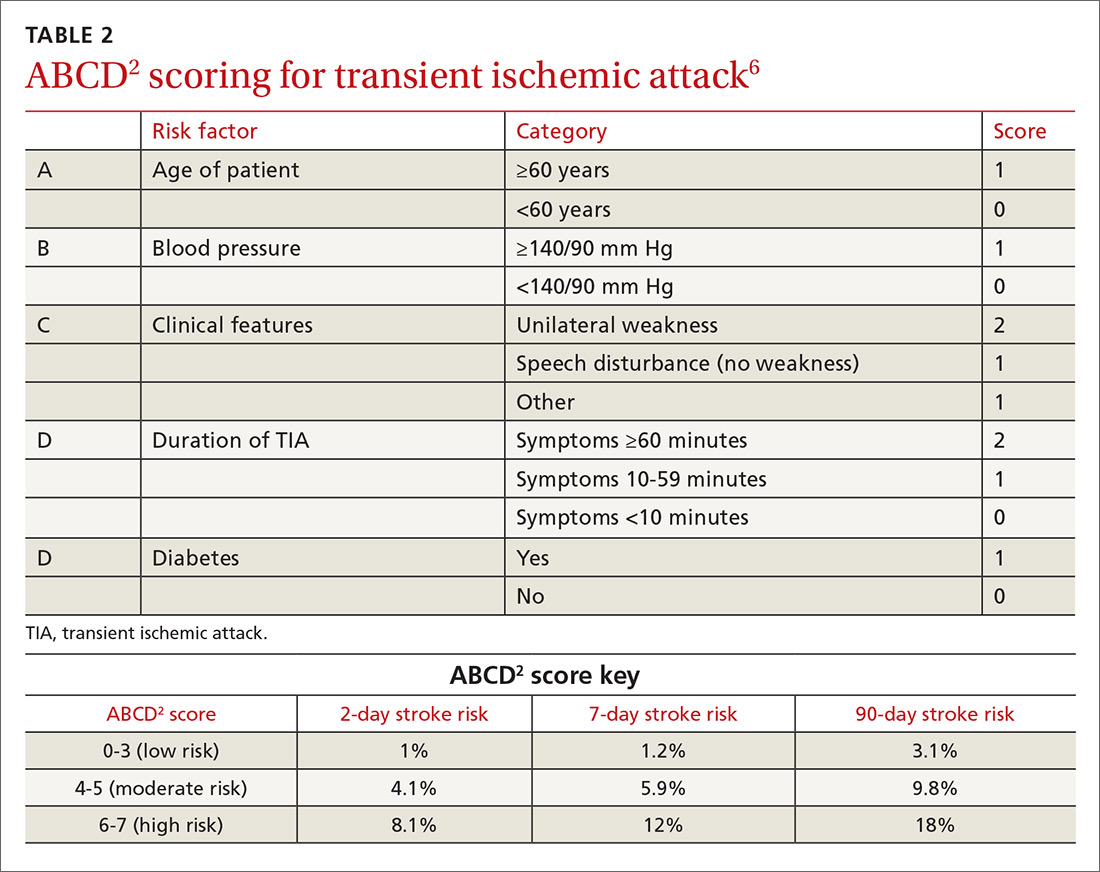
The validity of the ABCD2 score for risk stratification has been studied extensively with conflicting results.7-10 As with any assessment tool, it should be used as a guide, and should not supplant a full assessment of the patient or the judgment of the examining physician. In making the decision regarding inpatient or outpatient evaluation, it’s also important to consider available resources, access to specialists, and patient preference.
In a 2016 population-based study, the 30-day recurrent stroke/TIA rate for patients hospitalized for TIA was 3% compared with 10.7% for those discharged from the ED with referral to a stroke clinic and 10.6% for those discharged from the ED without a referral to a stroke clinic.11 These data suggest that only patients for whom you have a low clinical suspicion of stroke/TIA should be worked up as outpatients, and that hospital admission is advised in moderate- and high-risk cases. The findings also highlight the critical role that primary care physicians can play in triaging and managing these patients for secondary prevention.
CASE › This patient’s recent history of sudden-onset right-sided weakness and expressive language dysfunction is suspicious for left hemispheric ischemia. She has several risk factors for stroke, and her ABCD2 score is 5 (hypertension, age ≥60 years, unilateral weakness, and duration 10-59 min), which places her at moderate risk. Thus, the recommendation would be to have her go directly to an ED for rapid evaluation.
The diagnostic work-up
Even when a patient is sent to the ED, the FP plays a critical role in his or her continuing care. FPs will often coordinate with inpatient care and manage transition of care to the outpatient setting. (And in many communities, the ED or hospital physicians may themselves be family practitioners.)
In terms of care, not even an aspirin should be administered in a case like this because the patient has not yet had any neuroimaging, and differentiation of ischemic from hemorrhagic stroke cannot be made on clinical grounds alone. Once an ischemic stroke is confirmed, determining the etiology is critical given the significant management differences between the different types of stroke (atherosclerotic, cardioembolic, lacunar, or other).
Which imaging method, and when?
While a computerized tomography (CT) scan is the preferred initial imaging strategy for acute stroke to discern the ischemic type from the hemorrhagic, MRI is preferred for the evaluation of acute ischemic stroke because the method has a higher sensitivity for infarction and a greater ability to identify findings (such as demyelination) that would suggest an alternative diagnosis.
In addition to evaluating the brain parenchyma, physicians must also assess the cerebral vasculature. CT angiography (CTA) or MR angiography (MRA) of the head and neck are preferred over carotid ultrasound because they are capable of evaluating the entire cerebrovascular system12,13 and can be instrumental in identifying potential causes of stroke, as well as guiding therapeutic decisions. Carotid ultrasound is a reasonable alternative for patients presenting with symptoms indicative of anterior circulation involvement when CTA and MRA are unavailable or contraindicated, but it will not identify intracranial vascular disease, proximal common carotid disease, or vertebrobasilar disease.
Getting to the cause of suspected stroke: Labs and other diagnostic tests
A routine work-up includes BP checks, routine labs (complete blood count, complete metabolic panel, coagulation profile, and troponin), an electrocardiogram (EKG), a transthoracic echocardiogram (TTE) with bubble study if possible, and a minimum of 24 to 48 hours of cardiac rhythm monitoring. Cardiac rhythm monitoring should be extended in the setting of clinical concern for unidentified paroxysmal atrial fibrillation, such as an embolism without a proximal vascular source, multiple embolic infarcts in different vascular territories, a dilated left atrium, or other risk factors for atrial fibrillation that include smoking, systolic hypertension, diabetes, and heart failure (see TABLE 312,13,17,18).14-16 This standard diagnostic work-up will identify the cause of stroke in 70% to 80% of patients.19
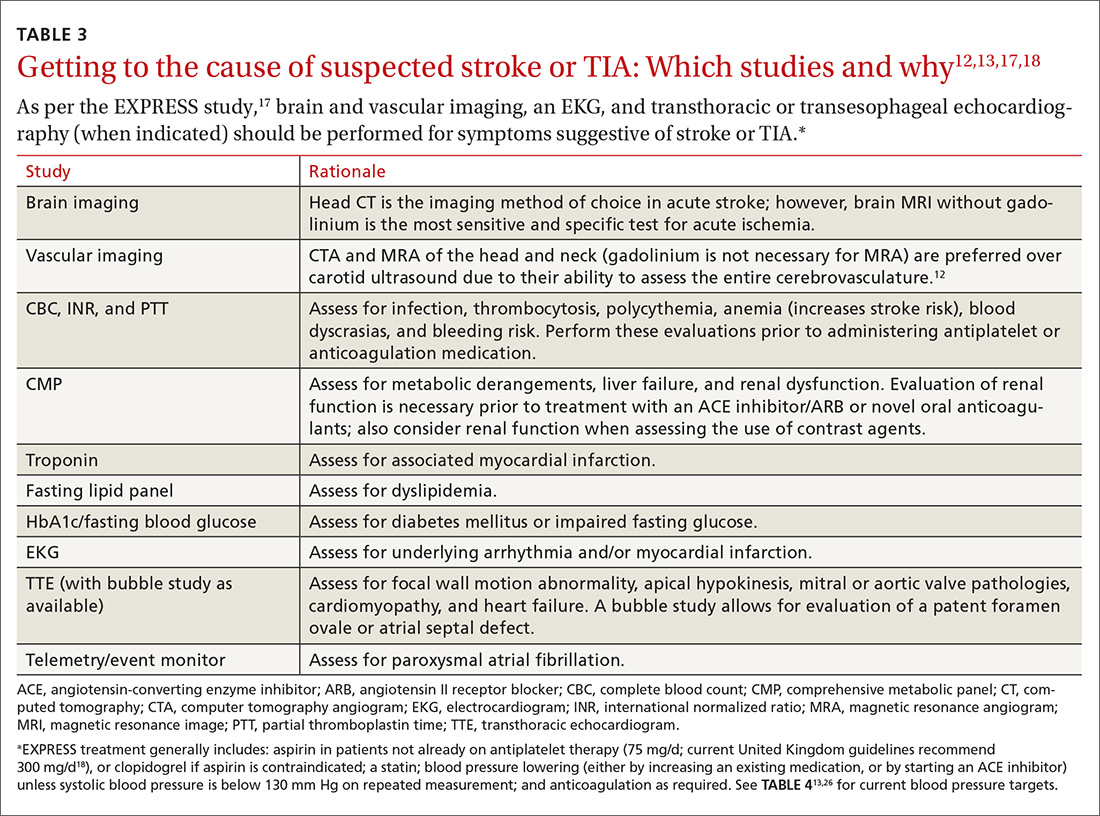
Additional investigations to consider if the etiology is not yet elucidated include a transesophageal echocardiogram (TEE), cerebral angiography, a coagulopathy evaluation, a lumbar puncture, and a vasculitis work-up. If available, consultation with a neurologist is appropriate for any patient who has had a stroke or TIA. Patients with unclear etiologies or for whom there are questions concerning strategies for preventing secondary stroke should be referred to Neurology and preferably a stroke specialist.
Timing matters, even when symptoms have resolved (ie, TIA).11,20 The EXPRESS trial17 (the Early use of eXisting PREventive Strategies for Stroke) looked at the effect of urgent assessment and treatment (≤1 day) of patients presenting with a TIA or minor stroke on the risk of recurrent stroke within 90 days. The diagnostic work-up included brain and vascular imaging together with an EKG. This intensive approach led to an absolute risk reduction of 8.2% (from 10.3% to 2.1%) in the risk of recurrent stroke at 90 days (number needed to treat [NNT]=12).17
Expedited work-up and treatment was also recently evaluated in a non-trial, real-world setting and was associated with reducing recurrent stroke by more than half the rate reported in older studies.20 Overall, the data suggest that evaluation within 24 hours confers substantial benefit, and that this evaluation can happen in an outpatient setting.21-23
Acute management: Use of tPA
Once imaging rules out intracranial hemorrhage, patients should be treated with tissue plasminogen activator (tPA) or an endovascular intervention as per guidelines.24 For patients with ischemic stroke ineligible for tPA or endovascular treatments, the initial focus is to determine the etiology of the symptoms so that the best strategies for prevention of secondary stroke may be employed.
Aspirin should be provided within 24 to 48 hours to all patients after intracranial hemorrhage is ruled out. Aspirin should be delayed for 24 hours in those given thrombolytics. The initial recommended dose of aspirin is 325 mg with continued low-dose (81 mg) aspirin daily.13 The addition of clopidogrel to aspirin within 24 hours of an event and continued for 21 days, followed by aspirin alone, was shown to be beneficial in a Chinese population with high-risk TIA (ABCD2 score ≥4) or minor stroke (National Institutes of Health Stroke Scale [NIHSS] ≤3).25 Anticoagulation with heparin, warfarin, or a novel oral anticoagulant is generally not indicated in the acute setting due to the risk of hemorrhagic transformation.
Acute BP management depends upon the type of stroke (ischemic or hemorrhagic), eligibility for thrombolytics, timing of presentation, and possible comorbidities such as myocardial infarction or aortic dissection (see TABLE 413,26). In the absence of contraindications, high-intensity statins should be initiated in all patients able to take oral medications.
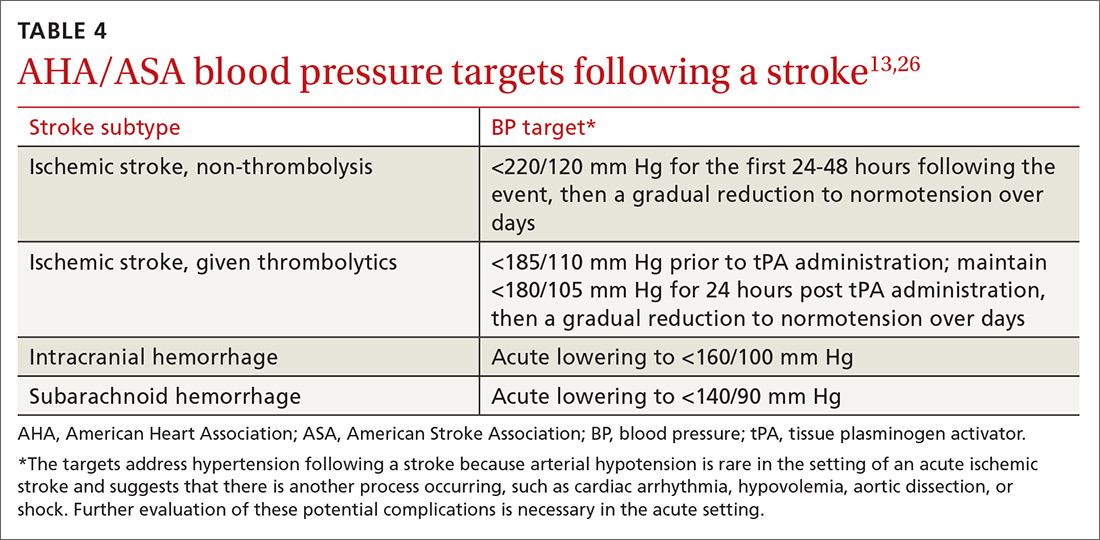
CASE › You appropriately referred your patient to the local ED. A head CT with head and neck CTA was performed. While the head CT did not show any abnormalities, the CTA demonstrated high-grade left internal carotid artery stenosis. The patient was given an initial dose of aspirin 325 mg and a high-intensity statin and admitted for further management. An MRI revealed a small shower of emboli in the left hemisphere, confirming the diagnosis of stroke over TIA. Labs were marginally remarkable with a low-density lipoprotein level of 115 mg/dL and an HbA1c of 6.2. Telemetry monitoring did not reveal any arrhythmias, and TTE was normal. BP remained in the high-normal to low-hypertensive range.
A Vascular Surgery consultation was obtained and the patient underwent a left carotid endarterectomy the following day. She did well without surgical complications. Her BP medications were adjusted; a combination of an angiotensin-converting enzyme inhibitor and a thiazide diuretic achieved a goal BP <140/90 mm Hg.
Permissive hypertension was not indicated due to her presentation >48 hours beyond the acute event. Low-dose aspirin and a high-intensity statin were continued, for secondary stroke prevention in the setting of atherosclerotic disease. She received smoking cessation counseling, which will continue.
CORRESPONDENCE
Stephen A. Martin, MD, EdM, Barre Family Health Center, 151 Worcester Road, Barre, MA 01005; [email protected].
1. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135:e146-e603.
2. Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:2064-2089.
3. Kochanek KD, Murphy SL, Xu J, et al. Mortality in the United States, 2013. NCHS Data Brief. 2014:1-8. Available at: https://www.cdc.gov/nchs/data/databriefs/db178.pdf. Accessed June 5, 2016.
4. Flossmann E, Redgrave JN, Briley D, et al. Reliability of clinical diagnosis of the symptomatic vascular territory in patients with recent transient ischemic attack or minor stroke. Stroke. 2008;39:2457-2460.
5. Josephson SA, Sidney S, Pham TN, et al. Higher ABCD2 score predicts patients most likely to have true transient ischemic attack. Stroke. 2008;39:3096-3098. Available at: http://www.ncbi.nlm.nih.gov/pubmed/18688003. Accessed June 5, 2016.
6. Hankey GJ. The ABCD, California, and unified ABCD2 risk scores predicted stroke within 2, 7, and 90 days after TIA. Evid Based Med. 2007;12:88.
7. Sheehan OC, Kyne L, Kelly LA, et al. Population-based study of ABCD2 score, carotid stenosis, and atrial fibrillation for early stroke prediction after transient ischemic attack: the North Dublin TIA study. Stroke. 2010;41:844-850.
8. Rothwell PM, Giles MF, Flossmann E, et al. A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet. 2005; 366:29-36.
9. Tsivgoulis G, Spengos K, Manta P, et al. Validation of the ABCD score in identifying individuals at high early risk of stroke after a transient ischemic attack: a hospital-based case series study. Stroke. 2006;37:2892-2897.
10. Kiyohara T, Kamouchi M, Kumai Y, et al. ABCD3 and ABCD3-I scores are superior to ABCD2 score in the prediction of short- and long-term risks of stroke after transient ischemic attack. Stroke. 2014;45:418-425.
11. Sacco RL, Rundek T. The value of urgent specialized care for TIA and minor stroke. N Engl J Med. 2016;374:1577-1579.
12. Demchuk AM, Menon BK, Goyal M. Comparing vessel imaging: noncontrast computed tomography/computed tomographic angiography should be the new minimum standard in acute disabling stroke. Stroke. 2016;47:273-281.
13. Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870-947.
14. Gladstone DJ, Spring M, Dorian P, et al. Atrial fibrillation in patients with cryptogenic stroke. N Engl J Med. 2014;370:2467-2477.
15. Sanna T, Diener HC, Passman RS, et al. Cryptogenic stroke and underlying atrial fibrillation. N Engl J Med. 2014;370:2478-2486.
16. Christophersen IE, Yin X, Larson MG, et al. A comparison of the CHARGE-AF and the CHA2DS2-VASc risk scores for prediction of atrial fibrillation ni the Framingham Heart Study. Am Heart J. 2016;178:45-54.
17. Rothwell PM, Giles MF, Chandratheva A, et al. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet. 2007;370:1432-1442.
18. National Institute for Health and Care Excellence. Stroke and transient ischaemic attack in over 16s: diagnosis and initial management. Available at: https://www.nice.org.uk/guidance/cg68. Published 2008. Accessed February 5, 2017.
19. Hart RG, Diener HC, Coutts SB, et al. Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol. 2014;13:429-438.
20. Amarenco P, Lavallée PC, Labreuche J, et al. One-year risk of stroke after transient ischemic attack or minor stroke. N Engl J Med. 2016;374:1533-1542.
21. Joshi JK, Ouyang B, Prabhakaran S. Should TIA patients be hospitalized or referred to a same-day clinic? A decision analysis. Neurology. 2011;77:2082-2088.
22. Mijalski C, Silver B. TIA management: should TIA patients be admitted? should TIA patients get combination antiplatelet therapy? The Neurohospitalist. 2015;5:151-160.
23. Silver B, Adeoye O. Management of patients with transient ischemic attack in the emergency department. Neurology. 2016;86:1568-1569.
24. Demaerschalk BM, Kleindorfer DO, Adeoye OM, et al. Scientific rationale for the inclusion and exclusion criteria for intravenous alteplase in acute ischemic stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47:581-641.
25. Wang Y, Wang Y, Zhao X, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013;369:11-19.
26. Hemphill JC, Greenberg SM, Anderson CS, et al. Guidelines for the management of spontaneous intracerebral hemorrhage. Stroke. 2015;46:2032-2060.
1. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135:e146-e603.
2. Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:2064-2089.
3. Kochanek KD, Murphy SL, Xu J, et al. Mortality in the United States, 2013. NCHS Data Brief. 2014:1-8. Available at: https://www.cdc.gov/nchs/data/databriefs/db178.pdf. Accessed June 5, 2016.
4. Flossmann E, Redgrave JN, Briley D, et al. Reliability of clinical diagnosis of the symptomatic vascular territory in patients with recent transient ischemic attack or minor stroke. Stroke. 2008;39:2457-2460.
5. Josephson SA, Sidney S, Pham TN, et al. Higher ABCD2 score predicts patients most likely to have true transient ischemic attack. Stroke. 2008;39:3096-3098. Available at: http://www.ncbi.nlm.nih.gov/pubmed/18688003. Accessed June 5, 2016.
6. Hankey GJ. The ABCD, California, and unified ABCD2 risk scores predicted stroke within 2, 7, and 90 days after TIA. Evid Based Med. 2007;12:88.
7. Sheehan OC, Kyne L, Kelly LA, et al. Population-based study of ABCD2 score, carotid stenosis, and atrial fibrillation for early stroke prediction after transient ischemic attack: the North Dublin TIA study. Stroke. 2010;41:844-850.
8. Rothwell PM, Giles MF, Flossmann E, et al. A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet. 2005; 366:29-36.
9. Tsivgoulis G, Spengos K, Manta P, et al. Validation of the ABCD score in identifying individuals at high early risk of stroke after a transient ischemic attack: a hospital-based case series study. Stroke. 2006;37:2892-2897.
10. Kiyohara T, Kamouchi M, Kumai Y, et al. ABCD3 and ABCD3-I scores are superior to ABCD2 score in the prediction of short- and long-term risks of stroke after transient ischemic attack. Stroke. 2014;45:418-425.
11. Sacco RL, Rundek T. The value of urgent specialized care for TIA and minor stroke. N Engl J Med. 2016;374:1577-1579.
12. Demchuk AM, Menon BK, Goyal M. Comparing vessel imaging: noncontrast computed tomography/computed tomographic angiography should be the new minimum standard in acute disabling stroke. Stroke. 2016;47:273-281.
13. Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870-947.
14. Gladstone DJ, Spring M, Dorian P, et al. Atrial fibrillation in patients with cryptogenic stroke. N Engl J Med. 2014;370:2467-2477.
15. Sanna T, Diener HC, Passman RS, et al. Cryptogenic stroke and underlying atrial fibrillation. N Engl J Med. 2014;370:2478-2486.
16. Christophersen IE, Yin X, Larson MG, et al. A comparison of the CHARGE-AF and the CHA2DS2-VASc risk scores for prediction of atrial fibrillation ni the Framingham Heart Study. Am Heart J. 2016;178:45-54.
17. Rothwell PM, Giles MF, Chandratheva A, et al. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet. 2007;370:1432-1442.
18. National Institute for Health and Care Excellence. Stroke and transient ischaemic attack in over 16s: diagnosis and initial management. Available at: https://www.nice.org.uk/guidance/cg68. Published 2008. Accessed February 5, 2017.
19. Hart RG, Diener HC, Coutts SB, et al. Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol. 2014;13:429-438.
20. Amarenco P, Lavallée PC, Labreuche J, et al. One-year risk of stroke after transient ischemic attack or minor stroke. N Engl J Med. 2016;374:1533-1542.
21. Joshi JK, Ouyang B, Prabhakaran S. Should TIA patients be hospitalized or referred to a same-day clinic? A decision analysis. Neurology. 2011;77:2082-2088.
22. Mijalski C, Silver B. TIA management: should TIA patients be admitted? should TIA patients get combination antiplatelet therapy? The Neurohospitalist. 2015;5:151-160.
23. Silver B, Adeoye O. Management of patients with transient ischemic attack in the emergency department. Neurology. 2016;86:1568-1569.
24. Demaerschalk BM, Kleindorfer DO, Adeoye OM, et al. Scientific rationale for the inclusion and exclusion criteria for intravenous alteplase in acute ischemic stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47:581-641.
25. Wang Y, Wang Y, Zhao X, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013;369:11-19.
26. Hemphill JC, Greenberg SM, Anderson CS, et al. Guidelines for the management of spontaneous intracerebral hemorrhage. Stroke. 2015;46:2032-2060.
PRACTICE RECOMMENDATIONS
› Perform an urgent work-up on patients presenting with symptoms of a transient ischemic attack or stroke. A
› Employ the ABCD2 risk stratification tool when determining whether it is reasonable to pursue an expedited work-up in the outpatient setting or recommend that a patient be evaluated in an emergency department. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Staying afloat in a sea of information: Point-of-care resources
It is friday afternoon on a sunny July day. The last patient of the day, Ms. Connecticut, is an active hiker who has had Lyme disease previously. She found a tick on her ankle yesterday. She successfully removed the tick but has not brought the tick with her to the appointment. She had been hiking several times over the last week and is not certain when the tick bite occurred. Her question for you centers on the role of antibiotic prophylaxis and Lyme disease prevention.
TECHNOLOGY: PROBLEM AND SOLUTION
Physicians need to keep up with an ever-increasing stream of information—new guidelines, new medications, and updates in medical literature.1 They have to do this while seeing more patients with more chronic problems in less time and while meeting reporting requirements for meaningful use or quality measures for accountable care organizations.
Though some of these challenges are due to technology, one solution is to use technology to our advantage. While researching information in textbooks won’t drain a phone battery, carrying a textbook around is not feasible, and many textbooks (including their electronic versions) contain information that is outdated before they go to print or that is quickly outdated thereafter.2 Further, even online textbooks are currently more dense than the online resources that we review here.
Different types of resources can help task-saturated healthcare providers stay aware of new information while delivering evidence-based care. These tools—online textbooks, decision guides embedded within electronic health record systems, or even a Google search—are termed “point-of-care” resources when used at the time of patient care for decision-making in the moment.
Not all of these resources are of high quality, with reliable factual information. Researchers estimate that up to 70% of clinicians may use Wikipedia to research medical questions, and a comparison of 10 Wikipedia articles vs peer-reviewed sources on the 10 most costly diseases found that 9 of the 10 Wikipedia articles had errors.3,4
In an earlier article,5 we advocated a proactive approach to managing information, highlighting ways to scan for new information and to develop habits of extracting useful information that can then be stored and easily recovered. To complement this strategy and weed out erroneous information, physicians need reliable sources of unbiased information to efficiently answer clinical questions at the point of care.1,6
Here, to help busy clinicians choose which point-of-care resources to use, we review several of the most popular ones, examining their ease of use, key elements, strengths, and weaknesses.
WHAT MAKES A RESOURCE GOOD?
Key features that make point-of-care tools effective include:
Ease of use, with standard formats, a summary for each topic, or both
Links to original articles and concise, capsular summaries and syntheses of the data
Continuing medical education (CME) credit. Tip: when searching, add “CME” to the search string on the browser to access resources that provide this.
Institutional and individual accounts. For clinicians who work for large organizations, point-of-care products may be paid for already, or reimbursement may be available for your subscription. If unsure, ask your director of information technology or library services.
Freedom from advertisements. Many Internet sources have advertisements that either run alongside the information you want to see or, more annoyingly, pop up and require an action to move forward. There is also continuing concern about the effect of industry support on content.7 While not all of the resources that we use regularly and that we review here are ad-free, avoiding programs with high ad content helps limit the possibility of bias and the time it takes to access information. Although advertisements do bring up a risk of bias, resources with a low-level ad content can limit bias while providing free or low-cost access.
Evidence, not expert opinion. Many resources have an “about” page that explains their philosophy and the source of their information. It is vital to be sure that point-of-care databases are providing facts based on evidence.8 This page also typically addresses how authors and editors are selected and whether expert opinion is used when randomized trials are lacking.
Ease of access. Many tools can be accessed not only on computers but also through apps for smartphones and tablets. Some electronic medical records have clinical decision tools embedded in them, with varying capabilities.
Disclosure of conflict of interest. As conflicts of interest can shade recommendations, information sources should clearly disclose financial relationships that could be perceived as conflicts of interest—for example, authors writing about medications sold by companies with whom they have a financial relationship.
NO SINGLE RESOURCE DOES EVERYTHING
There are many types of tools for finding evidence-based medical information. Different tools serve different purposes. Table 1 lists “toolbox essentials” for clinicians needing to answer clinical questions during patient care.
For example, when a question about the need for a bone mineral density measurement comes up, it is useful to be able to quickly compare guidelines from different professional societies on the National Guideline Clearing House. For another example, if a patient brings in a medication in an unlabeled bottle, a pill identifier app can tell you what it is. Clinicians who can use these resources appropriately will be at an advantage in being able to use information to provide better care to their patients.
To date, no point-of-care summary source has been shown to be superior in all categories, and use may be driven by ease of navigation, clinician preference, clinical question, or past success.9,10
Reviewed below are several applications that can be used as point-of-care resources (Table 2).
CLINICAL EVIDENCE
Clinical Evidence provides systematic reviews on medical topics. Founded in 1999 by the British Medical Journal, it is available in print as the Clinical Evidence Handbook and in online desktop and smartphone formats.
More than any other source we reviewed, Clinical Evidence addresses not only the evidence that exists, but also the data that do not exist to guide decisions. Compared with 9 other point-of-care resources, Clinical Evidence was found to have the highest quality of evidence.11
Strengths of Clinical Evidence
- Uncommonly transparent in terms of source of evidence or disclosing when there is a lack of evidence.
- Clearly lists the strength and relevance of the evidence.
- Personalization. Users can add notes to articles, save personal searches, and bookmark pages for easy access later.
- Navigability. Users can easily access systematic reviews, key points, retracted papers, or guidelines.
- Intuitive organization, with information categorized as research, education, news, or campaigns.
- New content daily: podcasts, articles, videos.
Weaknesses of Clinical Evidence
- Limited topics (eg, Lyme disease was not available)
- The limited content is a challenge when needing quick information at the point of care and may cause most clinicians to use another source unless looking for comparisons of interventions.
- Cost. Subscribing to the service “on demand,” ie, to look up a single specific topic, costs $36 for 48 hours of access; monthly access or a “season ticket” allows 30 days of viewing of all content for $53. At over $600/year, this is one of the most costly of the sources we reviewed.
- Marketing of Clinical Evidence to academic institutions that support the service for faculty may limit its appeal to other clinicians.
DYNAMED
Dynamed, a clinical reference created by a group of physicians, was previously owned by the American College of Physicians and known as Smart Medicine; it is now owned by EBSCO.12 Reviewers investigate the literature for a given topic and create pithy summaries for busy clinicians. A top feature in Dynamed is its links to full articles cited for best practices or evidence-based guidelines. The company describes their content as free of expert opinion, while being unbiased and evidence-based.
Dynamed uses a 7-step algorithm for searched topics that identifies articles, assesses clinical relevance, evaluates validity of outcomes, compiles the evidence from multiple articles, and then updates the final recommendations daily.
Dynamed Plus, the new upgraded version, updates searched topics several times a day. Dynamed may be the most frequently updated point-of-care resource, with the least risk of conflict of interest, but it offers limited topics drawn from evidence-based findings.11,13–15
With the rapid doubling of the medical literature, frequent updates allow clinicians to be most current with practice guidelines. This potentially affects quality of care for antibiotic use, vaccination, health promotion, and screening as well as newly approved medications.
Strengths of Dynamed
- Large collection of topics, critically appraised, written for primary care physicians, presented in bulleted format
- The most frequently updated database11,14,15
- Can integrate with major electronic health records (eg, Epic, Allscripts, NextGen, Cerner)
- Has an area devoted to new information that changes current practice
- Chosen topic grouped with related topics in the differential diagnosis after the initial search
- Easy-to-read outline for quick access to information such as billing, diagnosis, and references
- Medical calculators
- No advertisements
- Helpful embedded tools
- Icons to print or email the article
- An icon to create a “perma-link” to topics, searches, and browse categories
- Graded evidence with a link to the grading model used
- Links to primary articles
- Patient information handouts
- Alerts for updated information
- CME credit
- Special consideration and features for medical education
- The upgraded version Dynamed Plus contains Micromedex for a medication database, expanded graphics, semantic search, concise overview for each topic, and expanded content.
Weaknesses of Dynamed
- Although the topic list is large, it is only about one-third the size of UpToDate.
- A subscription for a physician costs $395 a year. Residents can sign up for about $150, and students for just under $100.
- CME is obtainable but cumbersome; one submits the CME credits through Tufts Healthcare, which requires a second sign-on to access and track.
- Drug and nondrug treatments for diseases cannot be separated.
- Useful calculators include decision trees for clinical decision-making, but there is no way to search them—one must waste time scrolling through the topics and specialties looking for desired information.
- Major shortcoming: there is no medication reference tool unless you upgrade to Dynamed Plus.
- The expanded graphics of Dynamed Plus are difficult to view on mobile applications within the articles (they are brought up more reliably when searching just for the image).
- The use of strict evidence-based methodology without expert opinion is a strength, but limits the collection of topics without randomized controlled trials, for which turning to expert opinion may be the only option.
EVIDENCE ESSENTIALS
Evidence Essentials is a point-of-care resource from Wiley that offers a variety of content types. The website lists 13,000 medical topics; however, they are not all summary reviews as discussed in the other products above. Subject matter is reviewed 3 times a year. Comprehensive reviews number just under 800 individual topics, with the remaining content consisting of Cochrane reviews, calculators, decision support tools, POEMs (Patient-Oriented Evidence that Matters), evidence-based medical guidelines, and dermatology images (1,000).
Evidence Essentials provides some unique content including a quick evaluation and management (E/M) code-finder and calculators not only for the typical medical equations, but also for history and physical examination likelihood ratios and pretest probabilities, which are practical and an excellent teaching aid. It also offers CME along with POEMs, e-mail alerts, and a listing of upcoming topics.
Strengths of Evidence Essentials
- Relatively inexpensive at $85 a year.
- High-functioning filter system to choose to search one or multiple databases.
- Related results are listed for aid in differential diagnosis, similar to Dynamed.
- Authors, editors, and date of last review are highly visible. As in UpToDate, relevant medical calculators appear on the page.
- The likelihood and odds ratio calculators are a huge plus for clinical decision-making and putting guidelines into practice.
- “Overall bottom line” highlights key points
- Grading of evidence per topic.
- Bulleted and tabbed information for quick access.
- Tabs for information on background, prevention, diagnosis, treatment, references, guidelines, and special populations.
Weaknesses of Evidence Essentials
- Limited number of topics with comprehensive reviews.
- While you can click on any drug name and link to a choice of two drug databases, this is not included in the subscription and requires a second account.
- The resources tabs had some broken links. In our clinical example, the tab contained several videos at the top that were not related, followed by a map and tables that were relevant to Lyme disease.
- Likewise, some of the guideline references were disappointing. For example, the guideline link for Lyme disease is for the US Department of Labor Occupational Safety and Health Administration rather than a professional society.
- For the provider wanting a narrative, this is more of a bare-bones text.
FIRST CONSULT
First Consult is Elsevier’s point-of-care clinical decision product contained within ClinicalKey.
Unlike UpToDate and Dynamed, in which authors and editors read original articles and summarize or synthesize information for the learner, First Consult is a “smart” search engine that will research a question, together with associated terms and key words. Filters such as full-text availability, journal articles, and patient education can be applied.
You may need to read about your topic in a textbook first, and then, if you are looking for treatment information, find an original article through First Consult. It is available in mobile and desktop formats, and the point-of-care product, First Consult, has an app that can be downloaded and used for free for the first 60 days.
Importantly, the First Consult portion of ClinicalKey with the summary topics was rated by Shurtz and Foster13 as least current of the products we are discussing in this article. On the other hand, it was the only product that had an embedded program to assist the user in making presentations by allowing drag and drop of images and automatic citing of sources. Kim et al report that First Consult is one of the resources providers prefer.9
Strengths of First Consult
- Lengthy free trial
- Ability to access original articles from a list vs lengthy narrative
- Access to journals and books published by Elsevier
- Powerful search engine that applies associated terms automatically
- Patient education is available in different languages and font size with the ability to add instructions and even a local branding
- Can integrate with electronic health record
- Can filter results by guideline, patient education, topic overviews
- Presentation assistance.
Weaknesses of First Consult
- Time-intensive. A provider needing quick advice on treatment for a medical condition has to guess if an article or textbook will have the most up-to-date and digestible information, whereas this has already been summarized in other products. For the busy clinician, this may be prohibitive.
- Search results are limited to Elsevier products, and major journals such as the New England Journal of Medicine are not available.
- Inconsistent platform functionality. The app version was somewhat “sticky” to use, as pages did not always load efficiently, and the menu bar navigation is not ideal.
- Expensive, especially given cheaper alternatives. For example, subscribing to the specialty of internal medicine or family medicine costs $499 and provides access to 8 journals and 11 books. Extended access costs $998 and offers full-text access to 23 books and 45 journals. The complete service has a total of 400 journals, 700 books, and 2,500 procedural videos.
MEDSCAPE
Medscape, owned by parent company WebMD, has long been a popular resource. The most recent versions are available for both for Android and iOS mobile platforms. The desktop and mobile apps claim to be designed for point-of-care use, and can be downloaded at no cost after registering as a Medscape user.
Medscape has some interesting features, including a handy pill identifier tool that is new to Medscape and perfect for the “I take one blue pill for my cholesterol” moments. The drug information tools and other features work well offline.
Medscape contains a well-presented drug database and interaction checker, as well as a growing collection of evidence-based articles and videos with links to references in Medline. From the point-of-care standpoint, Medscape also offers a number of decision-making algorithms and a continuously updated medical literature and health-related newsfeed. It contains in-app medical calculators, searchable directories for providers, hospitals, and pharmacies, and CME that can be earned on the website or from the application.
The main Medscape website contains pop-up advertisements, but the mobile app has fewer. Among the occasional frustrations, updates are relatively infrequent, the content is slow to load, and the phone app can be cumbersome. Of note, in one review,11 Medscape was found to have the lowest quality of evidence.
Strengths of Medscape
- Free with registration
- Medical calculator
- Drug interaction checker
- Pill identifier
- Evidence-based information covering about 4,000 conditions with links to references in Medline
- Ability to e-mail articles for sharing or future reference
- CME
- Unique database of hospitals, providers, and pharmacies to aid in referrals or locating other healthcare professionals
- Algorithms for decision-making
- Images and videos for procedural review and learning
- Option for downloading certain databases for offline use
- Medical news helps you keep up with what patients are watching and reading.
Weaknesses of Medscape
- Advertisements (many of them pop-up)
- The content is updated less frequently than other products listed in this article
- The smartphone app can run slowly
- Quality of reviews may be a concern.
UpToDate
UpToDate (Wolters Kluwer) is used widely by medical students, residents, and fellows as well as practicing providers. It contains narrative reviews of topics written by respected experts directed at both clinicians and clinical staff. In hopes of appealing to many markets, it offers different subscription types so you can customize your choices with add-on features (UpToDate Desktop and UpToDate MobileComplete allow downloading of all content to be accessed offline), different service packages (1-, 2-, and 3-year subscriptions), and the traditional base product that provides online access.
Of the products we reviewed, UpToDate has the largest selection of medical topics, approaching 10,000.14 In some studies,10,15 it also had the fastest retrieval time for searches. It uses evidence-based graded recommendations that are updated regularly.
Some have lamented that there is too much information per topic.9 In response to early reviews, Wolters Kluwer has made significant changes in the platform and greatly improved the search engine. UpToDate has expanded to include CME and patient information, trying to become that Holy Grail of websites—a one-stop experience. For the lucky few, UpToDate integrates into some electronic health records and provides a relatively seamless experience at the point of care.
Strengths of UpToDate
- One-stop shopping for information, resources, and CME
- Patient information is easy to read and accessible from the same screen
- The largest repository of medical subject matter
- Ability to cull out only pediatric or adult topics
- Searching available within a medical topic
- Tabs for quick access
- The What’s New feature allows access to practice-changing medical updates
- Medical calculators
- Drug interactions
- CME is is tracked in the system, allowing for CME credit information for hospital privileges and board certification
- Flexibility of access: can use online or download content to mobile/desktop device (the online version is easy to use, although robust wireless reception is needed; offices with slow Internet benefit from the offline feature)
- Electronic health record integration is possible with the most popular systems, such as Epic, eClinicalWorks, NextGen, and Allscripts
- Patient education and medication interaction features embedded in the electronic health record; produced in collaboration with Lexicomp
- Integrated drug database
- Alerts for updates
- References have links to full-text articles
- The date of last update is easily found for verifying information accuracy
- May be provided free for clinicians who are a part of a university or large health system.
Weaknesses of UpToDate
- Articles can be lengthy, which is both a strength and a weakness. Searches can retrieve too much information.9 High volume of text can frustrate the user trying to find bulleted, easy-to-read facts. However, for the person looking for a narrative summary, the content is organized as narrative paragraphs with appropriate headers in the left margin, and the search function is robust and powerful.
- Each topic has a “Summary of Recommendations,” but answers here often require linking back to the main text.
- Patient information is sometimes at a high literacy level.
- Costs more than Dynamed. A 1-year subscription is $499 for a physician, but you have the option of paying $53 for a 30-day recurring subscription. Residents, fellows, and students can pay $199 for 1 year or $19 for a 30-day recurring subscription.
- The requirement to download means that users need to keep their version updated on all of their computers—in each of their examination rooms, for example.
- Concerns about conflict of interest arise because authors and editors may maintain financial relationships with companies that produce medications discussed in the articles they have written.
BUILDING YOUR OWN PERSONAL ONLINE REPOSITORY
Our previous article5 reviewed how to store information using tools such as Evernote and Diigo that allow information viewed on a web page to be exported to any online repository. This can be done using extensions for a web browser or by sending the information to a custom e-mail account for these services.
For information that a provider knows he or she will need repeatedly, storage in one system is actually the easiest method. Such a system can then incorporate key information from the summary tools we have reviewed here. The ideal “electronic filing cabinet” should have several features such as a the capability to label articles by topic, to separate or sort as you see fit, and a search function to find information quickly—making it a personalized and effective point-of-care resource.
STAYING AFLOAT
Clinicians make many decisions every day. In fact, the release of How Doctors Think (both publications) has led to increased research into how clinical decisions and diagnoses are formed.16,17
With the medical literature expected to double every 73 days by 2020,18 there is an ever-widening ocean of information to sift through. With this onslaught, clinicians can no longer remain fully current. Instead, refining skills in accessing, sorting, and interpreting accurate scientific evidence efficiently is crucial to time spent actually caring for patients and coordinating their care.
Guidelines, algorithms, and comprehensive databases can aid clinicians in all aspects of care, from generating more complete differential diagnoses to managing disease-specific treatment. Individuals can first think about and list the qualities of a tool that are most important to them (eg, breadth of topics, frequency of updates, integration within their electronic health record, and cost) before focusing on a few applications or websites that meet those goals. With practice, point-of-care knowledge can become part of the everyday visit.
Effective integration into electronic health records will require design input from front-line clinicians. Otherwise, systems are prone to add too much “support” and overly rely on orthodox metrics and guidelines, resulting in alarm fatigue and frustration rather than facilitation.19–23
OUR CONCLUSIONS
Comprehensive point-of-care resources can play a significant role in helping busy clinicians provide best evidence-based care to their patients. Embedded clinical decision guides within an electronic health record are ideal, but low topic coverage has limited the usefulness of these systems.24 Here are our conclusions:
Medscape, ePocrates, and Wikipedia are probably the most popular free resources. Dynamed has offered free subscriptions to Wikipedia’s top health editors with the hopes of correcting factual errors. Medscape has excellent features but is supported by sponsored content, which raises a concern about bias and potential time-consuming distractions.
Dynamed and UpToDate have both been reported to answer more questions than other sources.12
UpToDate has the largest repository, with each topic curated by an expert or experts in that subject. This content can be dense and difficult to scan quickly at the point of care, but this is balanced by the ability to search within a medical topic, which has given it the fastest retrieval time.15 It does, however, allow authors and editors to maintain financial relationships with companies that produce medications discussed in the article.22
Dynamed has the advantage in frequency of updates, clearest conflict-of-interest policy, and the least amount of conflict of interest. Its topic list is not as extensive as UpToDate’s due to the limitation of using only evidence-based medicine without expert opinion.
First Consult has high user satisfaction, but as a point-of-care resource it can be time-consuming to find the best source for the clinical question at hand, and its expanded access is costly.9
ART AND SCIENCE
Point-of-care resources do not solve all the complicated problems of patient care, and no single resource is ideal for all situations. A busy clinician has limited time to process the evolving literature to practice the best evidence-based medicine. Effective information access, quality of care provided, and the marginal time cost required create a complex calculus. Clinical decision-making remains an art and a science,25 but these technologies help define a new era in its pursuit.
Ultimately, a clinician’s choice needs to correlate with a provider’s resources and style. This article has detailed several options available on the market today. This is a quickly evolving area of products and services. Longer term, users might consider a tool’s preferred key features when evaluating any current or future resource in order to choose the right ones for their practice.
CASE REVISITED
Before we leave for the weekend, we need a plan for Ms. Connecticut. To find appropriate recommendations for our patient, we search several of our point-of-care resources: UpToDate and Dynamed. Both resources have correct information according to the Infectious Disease Society of America (IDSA) guidelines.
UpToDate has a monograph of approximately 2,000 words on Lyme disease, which is lengthy but adds to clinical-decision making skills for a learner thinking through the decision. This service also has a patient handout highlighting the recommendations. The topic was last updated in 2016, but states that it is current with literature through January 2017.
Dynamed has bulleted information that is quicker to digest, but essentially highlights the IDSA recommendations without the thought process behind them. It too, has patient resources with links to a variety of handouts from professional organizations such as the US Centers for Disease Control and Prevention. They last updated the topic January 31, 2017.
When searching for the topic on both sites, a clinician can see the breadth of information in each program. However, this is also a detractor. Searching for Lyme disease prophylaxis on Dynamed brought up related data (that doxycycline is not FDA-approved for prophylaxis), but not the primary information. Likewise, the search under UpToDate first brought us to the patient information. Both articles have helpful tables and links to associated topics.
My partner chose the UpToDate article, in part to review the topic with a medical student. However, I used Dynamed for its quick bulleted information, as I was on call that evening and needed to return to the hospital. We both came to the same conclusion, and Ms. Connecticut chose no prophylaxis even though her home is in an endemic area. She has done well.
- Worster A, Haynes RB. How do I find a point-of-care answer to my clinical question? CJEM 2012; 14:31–35.
- Jeffery R, Navarro T, Lokker C, Haynes RB, Wilczynski NL, Farjou G. How current are leading evidence-based medical textbooks? An analytic survey of four online textbooks. J Med Internet Res 2012; 14:e175.
- ClinicalKey. Errors found in nine out of ten Wikipedia health entries. www.clinicalkey.com/info/blog/errors-in-wikipedia-health/. Accessed February 9, 2017.
- Hasty RT, Garbalosa RC, Barbato VA, et al. Wikipedia vs peer-reviewed medical literature for information about the 10 most costly medical conditions. J Am Osteopath Assoc 2014; 114:368–373.
- Mehta NB, Martin SA, Maypole J, Andrews R. Information management for clinicians. Cleve Clin J Med 2016; 83:589–595.
- Cook DA, Sorensen KJ, Hersh W, Berger RA, Wilkinson JM. Features of effective medical knowledge resources to support point of care learning: a focus group study. PLoS One 2013; 8:e80318.
- Steinbrook R. Future directions in industry funding of continuing medical education. Arch Intern Med 2011; 171:257–258.
- Isaacs D, Fitzgerald D. Seven alternatives to evidence based medicine. BMJ 1999; 319:1618.
- Kim S, Noveck H, Galt J, Hogshire L, Willett L, O’Rourke K. Searching for answers to clinical questions using Google versus evidence-based summary resources: a randomized controlled crossover study. Acad Med 2014; 89:940–943.
- Ahmadi SF, Faghankhani M, Javanbakht A, et al. A comparison of answer retrieval through four evidence-based textbooks (ACP PIER, Essential Evidence Plus, First Consult, and UpToDate): a randomized controlled trial. Med Teach 2011; 33:724–730.
- Prorok JC, Iserman EC, Wilczynski NL, Haynes RB. The quality, breadth, and timeliness of content updating vary substantially for 10 online medical texts: an analytic survey. J Clin Epidemiol 2012; 65:1289–1295.
- Prorok JC, Iserman EC, Wilczynski NL, Haynes RB. The quality, breadth, and timeliness of content updating vary substantially for 10 online medical texts: an analytic survey. J Clin Epidemiol 2012; 65:1289–1295.
- Shurtz S, Foster MJ. Developing and using a rubric for evaluating evidence-based medicine point-of-care tools. J Med Libr Assoc 2011; 99:247–254.
- Ketterman E, Besaw M. An evaluation of citation counts, search results, and frequency of updates in Dynamed and UpToDate. J Electron Res in Med Libr 2010; 7:273–280.
- Amber KT, Dhiman G, Goodman KW. Conflict of interest in online point-of-care clinical support websites. J Med Ethics 2014; 40:578–580.
- Montgomery K. How Doctors Think: Clinical Judgment and the Practice of Medicine. New York, NY: Oxford University Press; 2005.
- Groopman J. How Doctors Think. Boston, MA: Houghton Mifflin; 2008.
- Densen P. Challenges and opportunities facing medical education. Trans Am Clin Climatol Assoc 2010; 122:48–58.
- Kesselheim AS, Cresswell K, Phansalkar S, Bates DW, Sheikh A. Clinical decision support systems could be modified to reduce ‘alert fatigue’ while still minimizing the risk of litigation. Health Aff (Millwood) 2011; 30:2310–2317.
- Russ AL, Zillich AJ, McManus MS, Doebbeling BN, Saleem JJ. Prescribers’ interactions with medication alerts at the point of prescribing: a multi-method, in situ investigation of the human-computer interaction. Int J Med Inform 2012; 81:232–243.
- Fraccaro P, Arguello Castelerio M, Ainsworth J, Buchan I. Adoption of clinical decision support in multimorbidity: a systematic review. JMIR Med Informatics 2015; 3:e4.
- McLeod W, Eidus R, Stewart EE. Clinical decision support: using technology to identify patients’ unmet needs. Fam Pract Manag 2012; 19:22–28.
- Colla CH. Swimming against the current—what might work to reduce low-value care? N Engl J Med 2014; 371:1280–1283.
- Cook DA, Sorensen KJ, Nishimura RA, Ommen SR, Lloyd FJ. A comprehensive information technology system to support physician learning at the point of care. Acad Med 2015; 90:33–39.
- Woolever DR. The art and science of clinical decision making. Fam Pract Manag 2008; 15:31–36.
It is friday afternoon on a sunny July day. The last patient of the day, Ms. Connecticut, is an active hiker who has had Lyme disease previously. She found a tick on her ankle yesterday. She successfully removed the tick but has not brought the tick with her to the appointment. She had been hiking several times over the last week and is not certain when the tick bite occurred. Her question for you centers on the role of antibiotic prophylaxis and Lyme disease prevention.
TECHNOLOGY: PROBLEM AND SOLUTION
Physicians need to keep up with an ever-increasing stream of information—new guidelines, new medications, and updates in medical literature.1 They have to do this while seeing more patients with more chronic problems in less time and while meeting reporting requirements for meaningful use or quality measures for accountable care organizations.
Though some of these challenges are due to technology, one solution is to use technology to our advantage. While researching information in textbooks won’t drain a phone battery, carrying a textbook around is not feasible, and many textbooks (including their electronic versions) contain information that is outdated before they go to print or that is quickly outdated thereafter.2 Further, even online textbooks are currently more dense than the online resources that we review here.
Different types of resources can help task-saturated healthcare providers stay aware of new information while delivering evidence-based care. These tools—online textbooks, decision guides embedded within electronic health record systems, or even a Google search—are termed “point-of-care” resources when used at the time of patient care for decision-making in the moment.
Not all of these resources are of high quality, with reliable factual information. Researchers estimate that up to 70% of clinicians may use Wikipedia to research medical questions, and a comparison of 10 Wikipedia articles vs peer-reviewed sources on the 10 most costly diseases found that 9 of the 10 Wikipedia articles had errors.3,4
In an earlier article,5 we advocated a proactive approach to managing information, highlighting ways to scan for new information and to develop habits of extracting useful information that can then be stored and easily recovered. To complement this strategy and weed out erroneous information, physicians need reliable sources of unbiased information to efficiently answer clinical questions at the point of care.1,6
Here, to help busy clinicians choose which point-of-care resources to use, we review several of the most popular ones, examining their ease of use, key elements, strengths, and weaknesses.
WHAT MAKES A RESOURCE GOOD?
Key features that make point-of-care tools effective include:
Ease of use, with standard formats, a summary for each topic, or both
Links to original articles and concise, capsular summaries and syntheses of the data
Continuing medical education (CME) credit. Tip: when searching, add “CME” to the search string on the browser to access resources that provide this.
Institutional and individual accounts. For clinicians who work for large organizations, point-of-care products may be paid for already, or reimbursement may be available for your subscription. If unsure, ask your director of information technology or library services.
Freedom from advertisements. Many Internet sources have advertisements that either run alongside the information you want to see or, more annoyingly, pop up and require an action to move forward. There is also continuing concern about the effect of industry support on content.7 While not all of the resources that we use regularly and that we review here are ad-free, avoiding programs with high ad content helps limit the possibility of bias and the time it takes to access information. Although advertisements do bring up a risk of bias, resources with a low-level ad content can limit bias while providing free or low-cost access.
Evidence, not expert opinion. Many resources have an “about” page that explains their philosophy and the source of their information. It is vital to be sure that point-of-care databases are providing facts based on evidence.8 This page also typically addresses how authors and editors are selected and whether expert opinion is used when randomized trials are lacking.
Ease of access. Many tools can be accessed not only on computers but also through apps for smartphones and tablets. Some electronic medical records have clinical decision tools embedded in them, with varying capabilities.
Disclosure of conflict of interest. As conflicts of interest can shade recommendations, information sources should clearly disclose financial relationships that could be perceived as conflicts of interest—for example, authors writing about medications sold by companies with whom they have a financial relationship.
NO SINGLE RESOURCE DOES EVERYTHING
There are many types of tools for finding evidence-based medical information. Different tools serve different purposes. Table 1 lists “toolbox essentials” for clinicians needing to answer clinical questions during patient care.
For example, when a question about the need for a bone mineral density measurement comes up, it is useful to be able to quickly compare guidelines from different professional societies on the National Guideline Clearing House. For another example, if a patient brings in a medication in an unlabeled bottle, a pill identifier app can tell you what it is. Clinicians who can use these resources appropriately will be at an advantage in being able to use information to provide better care to their patients.
To date, no point-of-care summary source has been shown to be superior in all categories, and use may be driven by ease of navigation, clinician preference, clinical question, or past success.9,10
Reviewed below are several applications that can be used as point-of-care resources (Table 2).
CLINICAL EVIDENCE
Clinical Evidence provides systematic reviews on medical topics. Founded in 1999 by the British Medical Journal, it is available in print as the Clinical Evidence Handbook and in online desktop and smartphone formats.
More than any other source we reviewed, Clinical Evidence addresses not only the evidence that exists, but also the data that do not exist to guide decisions. Compared with 9 other point-of-care resources, Clinical Evidence was found to have the highest quality of evidence.11
Strengths of Clinical Evidence
- Uncommonly transparent in terms of source of evidence or disclosing when there is a lack of evidence.
- Clearly lists the strength and relevance of the evidence.
- Personalization. Users can add notes to articles, save personal searches, and bookmark pages for easy access later.
- Navigability. Users can easily access systematic reviews, key points, retracted papers, or guidelines.
- Intuitive organization, with information categorized as research, education, news, or campaigns.
- New content daily: podcasts, articles, videos.
Weaknesses of Clinical Evidence
- Limited topics (eg, Lyme disease was not available)
- The limited content is a challenge when needing quick information at the point of care and may cause most clinicians to use another source unless looking for comparisons of interventions.
- Cost. Subscribing to the service “on demand,” ie, to look up a single specific topic, costs $36 for 48 hours of access; monthly access or a “season ticket” allows 30 days of viewing of all content for $53. At over $600/year, this is one of the most costly of the sources we reviewed.
- Marketing of Clinical Evidence to academic institutions that support the service for faculty may limit its appeal to other clinicians.
DYNAMED
Dynamed, a clinical reference created by a group of physicians, was previously owned by the American College of Physicians and known as Smart Medicine; it is now owned by EBSCO.12 Reviewers investigate the literature for a given topic and create pithy summaries for busy clinicians. A top feature in Dynamed is its links to full articles cited for best practices or evidence-based guidelines. The company describes their content as free of expert opinion, while being unbiased and evidence-based.
Dynamed uses a 7-step algorithm for searched topics that identifies articles, assesses clinical relevance, evaluates validity of outcomes, compiles the evidence from multiple articles, and then updates the final recommendations daily.
Dynamed Plus, the new upgraded version, updates searched topics several times a day. Dynamed may be the most frequently updated point-of-care resource, with the least risk of conflict of interest, but it offers limited topics drawn from evidence-based findings.11,13–15
With the rapid doubling of the medical literature, frequent updates allow clinicians to be most current with practice guidelines. This potentially affects quality of care for antibiotic use, vaccination, health promotion, and screening as well as newly approved medications.
Strengths of Dynamed
- Large collection of topics, critically appraised, written for primary care physicians, presented in bulleted format
- The most frequently updated database11,14,15
- Can integrate with major electronic health records (eg, Epic, Allscripts, NextGen, Cerner)
- Has an area devoted to new information that changes current practice
- Chosen topic grouped with related topics in the differential diagnosis after the initial search
- Easy-to-read outline for quick access to information such as billing, diagnosis, and references
- Medical calculators
- No advertisements
- Helpful embedded tools
- Icons to print or email the article
- An icon to create a “perma-link” to topics, searches, and browse categories
- Graded evidence with a link to the grading model used
- Links to primary articles
- Patient information handouts
- Alerts for updated information
- CME credit
- Special consideration and features for medical education
- The upgraded version Dynamed Plus contains Micromedex for a medication database, expanded graphics, semantic search, concise overview for each topic, and expanded content.
Weaknesses of Dynamed
- Although the topic list is large, it is only about one-third the size of UpToDate.
- A subscription for a physician costs $395 a year. Residents can sign up for about $150, and students for just under $100.
- CME is obtainable but cumbersome; one submits the CME credits through Tufts Healthcare, which requires a second sign-on to access and track.
- Drug and nondrug treatments for diseases cannot be separated.
- Useful calculators include decision trees for clinical decision-making, but there is no way to search them—one must waste time scrolling through the topics and specialties looking for desired information.
- Major shortcoming: there is no medication reference tool unless you upgrade to Dynamed Plus.
- The expanded graphics of Dynamed Plus are difficult to view on mobile applications within the articles (they are brought up more reliably when searching just for the image).
- The use of strict evidence-based methodology without expert opinion is a strength, but limits the collection of topics without randomized controlled trials, for which turning to expert opinion may be the only option.
EVIDENCE ESSENTIALS
Evidence Essentials is a point-of-care resource from Wiley that offers a variety of content types. The website lists 13,000 medical topics; however, they are not all summary reviews as discussed in the other products above. Subject matter is reviewed 3 times a year. Comprehensive reviews number just under 800 individual topics, with the remaining content consisting of Cochrane reviews, calculators, decision support tools, POEMs (Patient-Oriented Evidence that Matters), evidence-based medical guidelines, and dermatology images (1,000).
Evidence Essentials provides some unique content including a quick evaluation and management (E/M) code-finder and calculators not only for the typical medical equations, but also for history and physical examination likelihood ratios and pretest probabilities, which are practical and an excellent teaching aid. It also offers CME along with POEMs, e-mail alerts, and a listing of upcoming topics.
Strengths of Evidence Essentials
- Relatively inexpensive at $85 a year.
- High-functioning filter system to choose to search one or multiple databases.
- Related results are listed for aid in differential diagnosis, similar to Dynamed.
- Authors, editors, and date of last review are highly visible. As in UpToDate, relevant medical calculators appear on the page.
- The likelihood and odds ratio calculators are a huge plus for clinical decision-making and putting guidelines into practice.
- “Overall bottom line” highlights key points
- Grading of evidence per topic.
- Bulleted and tabbed information for quick access.
- Tabs for information on background, prevention, diagnosis, treatment, references, guidelines, and special populations.
Weaknesses of Evidence Essentials
- Limited number of topics with comprehensive reviews.
- While you can click on any drug name and link to a choice of two drug databases, this is not included in the subscription and requires a second account.
- The resources tabs had some broken links. In our clinical example, the tab contained several videos at the top that were not related, followed by a map and tables that were relevant to Lyme disease.
- Likewise, some of the guideline references were disappointing. For example, the guideline link for Lyme disease is for the US Department of Labor Occupational Safety and Health Administration rather than a professional society.
- For the provider wanting a narrative, this is more of a bare-bones text.
FIRST CONSULT
First Consult is Elsevier’s point-of-care clinical decision product contained within ClinicalKey.
Unlike UpToDate and Dynamed, in which authors and editors read original articles and summarize or synthesize information for the learner, First Consult is a “smart” search engine that will research a question, together with associated terms and key words. Filters such as full-text availability, journal articles, and patient education can be applied.
You may need to read about your topic in a textbook first, and then, if you are looking for treatment information, find an original article through First Consult. It is available in mobile and desktop formats, and the point-of-care product, First Consult, has an app that can be downloaded and used for free for the first 60 days.
Importantly, the First Consult portion of ClinicalKey with the summary topics was rated by Shurtz and Foster13 as least current of the products we are discussing in this article. On the other hand, it was the only product that had an embedded program to assist the user in making presentations by allowing drag and drop of images and automatic citing of sources. Kim et al report that First Consult is one of the resources providers prefer.9
Strengths of First Consult
- Lengthy free trial
- Ability to access original articles from a list vs lengthy narrative
- Access to journals and books published by Elsevier
- Powerful search engine that applies associated terms automatically
- Patient education is available in different languages and font size with the ability to add instructions and even a local branding
- Can integrate with electronic health record
- Can filter results by guideline, patient education, topic overviews
- Presentation assistance.
Weaknesses of First Consult
- Time-intensive. A provider needing quick advice on treatment for a medical condition has to guess if an article or textbook will have the most up-to-date and digestible information, whereas this has already been summarized in other products. For the busy clinician, this may be prohibitive.
- Search results are limited to Elsevier products, and major journals such as the New England Journal of Medicine are not available.
- Inconsistent platform functionality. The app version was somewhat “sticky” to use, as pages did not always load efficiently, and the menu bar navigation is not ideal.
- Expensive, especially given cheaper alternatives. For example, subscribing to the specialty of internal medicine or family medicine costs $499 and provides access to 8 journals and 11 books. Extended access costs $998 and offers full-text access to 23 books and 45 journals. The complete service has a total of 400 journals, 700 books, and 2,500 procedural videos.
MEDSCAPE
Medscape, owned by parent company WebMD, has long been a popular resource. The most recent versions are available for both for Android and iOS mobile platforms. The desktop and mobile apps claim to be designed for point-of-care use, and can be downloaded at no cost after registering as a Medscape user.
Medscape has some interesting features, including a handy pill identifier tool that is new to Medscape and perfect for the “I take one blue pill for my cholesterol” moments. The drug information tools and other features work well offline.
Medscape contains a well-presented drug database and interaction checker, as well as a growing collection of evidence-based articles and videos with links to references in Medline. From the point-of-care standpoint, Medscape also offers a number of decision-making algorithms and a continuously updated medical literature and health-related newsfeed. It contains in-app medical calculators, searchable directories for providers, hospitals, and pharmacies, and CME that can be earned on the website or from the application.
The main Medscape website contains pop-up advertisements, but the mobile app has fewer. Among the occasional frustrations, updates are relatively infrequent, the content is slow to load, and the phone app can be cumbersome. Of note, in one review,11 Medscape was found to have the lowest quality of evidence.
Strengths of Medscape
- Free with registration
- Medical calculator
- Drug interaction checker
- Pill identifier
- Evidence-based information covering about 4,000 conditions with links to references in Medline
- Ability to e-mail articles for sharing or future reference
- CME
- Unique database of hospitals, providers, and pharmacies to aid in referrals or locating other healthcare professionals
- Algorithms for decision-making
- Images and videos for procedural review and learning
- Option for downloading certain databases for offline use
- Medical news helps you keep up with what patients are watching and reading.
Weaknesses of Medscape
- Advertisements (many of them pop-up)
- The content is updated less frequently than other products listed in this article
- The smartphone app can run slowly
- Quality of reviews may be a concern.
UpToDate
UpToDate (Wolters Kluwer) is used widely by medical students, residents, and fellows as well as practicing providers. It contains narrative reviews of topics written by respected experts directed at both clinicians and clinical staff. In hopes of appealing to many markets, it offers different subscription types so you can customize your choices with add-on features (UpToDate Desktop and UpToDate MobileComplete allow downloading of all content to be accessed offline), different service packages (1-, 2-, and 3-year subscriptions), and the traditional base product that provides online access.
Of the products we reviewed, UpToDate has the largest selection of medical topics, approaching 10,000.14 In some studies,10,15 it also had the fastest retrieval time for searches. It uses evidence-based graded recommendations that are updated regularly.
Some have lamented that there is too much information per topic.9 In response to early reviews, Wolters Kluwer has made significant changes in the platform and greatly improved the search engine. UpToDate has expanded to include CME and patient information, trying to become that Holy Grail of websites—a one-stop experience. For the lucky few, UpToDate integrates into some electronic health records and provides a relatively seamless experience at the point of care.
Strengths of UpToDate
- One-stop shopping for information, resources, and CME
- Patient information is easy to read and accessible from the same screen
- The largest repository of medical subject matter
- Ability to cull out only pediatric or adult topics
- Searching available within a medical topic
- Tabs for quick access
- The What’s New feature allows access to practice-changing medical updates
- Medical calculators
- Drug interactions
- CME is is tracked in the system, allowing for CME credit information for hospital privileges and board certification
- Flexibility of access: can use online or download content to mobile/desktop device (the online version is easy to use, although robust wireless reception is needed; offices with slow Internet benefit from the offline feature)
- Electronic health record integration is possible with the most popular systems, such as Epic, eClinicalWorks, NextGen, and Allscripts
- Patient education and medication interaction features embedded in the electronic health record; produced in collaboration with Lexicomp
- Integrated drug database
- Alerts for updates
- References have links to full-text articles
- The date of last update is easily found for verifying information accuracy
- May be provided free for clinicians who are a part of a university or large health system.
Weaknesses of UpToDate
- Articles can be lengthy, which is both a strength and a weakness. Searches can retrieve too much information.9 High volume of text can frustrate the user trying to find bulleted, easy-to-read facts. However, for the person looking for a narrative summary, the content is organized as narrative paragraphs with appropriate headers in the left margin, and the search function is robust and powerful.
- Each topic has a “Summary of Recommendations,” but answers here often require linking back to the main text.
- Patient information is sometimes at a high literacy level.
- Costs more than Dynamed. A 1-year subscription is $499 for a physician, but you have the option of paying $53 for a 30-day recurring subscription. Residents, fellows, and students can pay $199 for 1 year or $19 for a 30-day recurring subscription.
- The requirement to download means that users need to keep their version updated on all of their computers—in each of their examination rooms, for example.
- Concerns about conflict of interest arise because authors and editors may maintain financial relationships with companies that produce medications discussed in the articles they have written.
BUILDING YOUR OWN PERSONAL ONLINE REPOSITORY
Our previous article5 reviewed how to store information using tools such as Evernote and Diigo that allow information viewed on a web page to be exported to any online repository. This can be done using extensions for a web browser or by sending the information to a custom e-mail account for these services.
For information that a provider knows he or she will need repeatedly, storage in one system is actually the easiest method. Such a system can then incorporate key information from the summary tools we have reviewed here. The ideal “electronic filing cabinet” should have several features such as a the capability to label articles by topic, to separate or sort as you see fit, and a search function to find information quickly—making it a personalized and effective point-of-care resource.
STAYING AFLOAT
Clinicians make many decisions every day. In fact, the release of How Doctors Think (both publications) has led to increased research into how clinical decisions and diagnoses are formed.16,17
With the medical literature expected to double every 73 days by 2020,18 there is an ever-widening ocean of information to sift through. With this onslaught, clinicians can no longer remain fully current. Instead, refining skills in accessing, sorting, and interpreting accurate scientific evidence efficiently is crucial to time spent actually caring for patients and coordinating their care.
Guidelines, algorithms, and comprehensive databases can aid clinicians in all aspects of care, from generating more complete differential diagnoses to managing disease-specific treatment. Individuals can first think about and list the qualities of a tool that are most important to them (eg, breadth of topics, frequency of updates, integration within their electronic health record, and cost) before focusing on a few applications or websites that meet those goals. With practice, point-of-care knowledge can become part of the everyday visit.
Effective integration into electronic health records will require design input from front-line clinicians. Otherwise, systems are prone to add too much “support” and overly rely on orthodox metrics and guidelines, resulting in alarm fatigue and frustration rather than facilitation.19–23
OUR CONCLUSIONS
Comprehensive point-of-care resources can play a significant role in helping busy clinicians provide best evidence-based care to their patients. Embedded clinical decision guides within an electronic health record are ideal, but low topic coverage has limited the usefulness of these systems.24 Here are our conclusions:
Medscape, ePocrates, and Wikipedia are probably the most popular free resources. Dynamed has offered free subscriptions to Wikipedia’s top health editors with the hopes of correcting factual errors. Medscape has excellent features but is supported by sponsored content, which raises a concern about bias and potential time-consuming distractions.
Dynamed and UpToDate have both been reported to answer more questions than other sources.12
UpToDate has the largest repository, with each topic curated by an expert or experts in that subject. This content can be dense and difficult to scan quickly at the point of care, but this is balanced by the ability to search within a medical topic, which has given it the fastest retrieval time.15 It does, however, allow authors and editors to maintain financial relationships with companies that produce medications discussed in the article.22
Dynamed has the advantage in frequency of updates, clearest conflict-of-interest policy, and the least amount of conflict of interest. Its topic list is not as extensive as UpToDate’s due to the limitation of using only evidence-based medicine without expert opinion.
First Consult has high user satisfaction, but as a point-of-care resource it can be time-consuming to find the best source for the clinical question at hand, and its expanded access is costly.9
ART AND SCIENCE
Point-of-care resources do not solve all the complicated problems of patient care, and no single resource is ideal for all situations. A busy clinician has limited time to process the evolving literature to practice the best evidence-based medicine. Effective information access, quality of care provided, and the marginal time cost required create a complex calculus. Clinical decision-making remains an art and a science,25 but these technologies help define a new era in its pursuit.
Ultimately, a clinician’s choice needs to correlate with a provider’s resources and style. This article has detailed several options available on the market today. This is a quickly evolving area of products and services. Longer term, users might consider a tool’s preferred key features when evaluating any current or future resource in order to choose the right ones for their practice.
CASE REVISITED
Before we leave for the weekend, we need a plan for Ms. Connecticut. To find appropriate recommendations for our patient, we search several of our point-of-care resources: UpToDate and Dynamed. Both resources have correct information according to the Infectious Disease Society of America (IDSA) guidelines.
UpToDate has a monograph of approximately 2,000 words on Lyme disease, which is lengthy but adds to clinical-decision making skills for a learner thinking through the decision. This service also has a patient handout highlighting the recommendations. The topic was last updated in 2016, but states that it is current with literature through January 2017.
Dynamed has bulleted information that is quicker to digest, but essentially highlights the IDSA recommendations without the thought process behind them. It too, has patient resources with links to a variety of handouts from professional organizations such as the US Centers for Disease Control and Prevention. They last updated the topic January 31, 2017.
When searching for the topic on both sites, a clinician can see the breadth of information in each program. However, this is also a detractor. Searching for Lyme disease prophylaxis on Dynamed brought up related data (that doxycycline is not FDA-approved for prophylaxis), but not the primary information. Likewise, the search under UpToDate first brought us to the patient information. Both articles have helpful tables and links to associated topics.
My partner chose the UpToDate article, in part to review the topic with a medical student. However, I used Dynamed for its quick bulleted information, as I was on call that evening and needed to return to the hospital. We both came to the same conclusion, and Ms. Connecticut chose no prophylaxis even though her home is in an endemic area. She has done well.
It is friday afternoon on a sunny July day. The last patient of the day, Ms. Connecticut, is an active hiker who has had Lyme disease previously. She found a tick on her ankle yesterday. She successfully removed the tick but has not brought the tick with her to the appointment. She had been hiking several times over the last week and is not certain when the tick bite occurred. Her question for you centers on the role of antibiotic prophylaxis and Lyme disease prevention.
TECHNOLOGY: PROBLEM AND SOLUTION
Physicians need to keep up with an ever-increasing stream of information—new guidelines, new medications, and updates in medical literature.1 They have to do this while seeing more patients with more chronic problems in less time and while meeting reporting requirements for meaningful use or quality measures for accountable care organizations.
Though some of these challenges are due to technology, one solution is to use technology to our advantage. While researching information in textbooks won’t drain a phone battery, carrying a textbook around is not feasible, and many textbooks (including their electronic versions) contain information that is outdated before they go to print or that is quickly outdated thereafter.2 Further, even online textbooks are currently more dense than the online resources that we review here.
Different types of resources can help task-saturated healthcare providers stay aware of new information while delivering evidence-based care. These tools—online textbooks, decision guides embedded within electronic health record systems, or even a Google search—are termed “point-of-care” resources when used at the time of patient care for decision-making in the moment.
Not all of these resources are of high quality, with reliable factual information. Researchers estimate that up to 70% of clinicians may use Wikipedia to research medical questions, and a comparison of 10 Wikipedia articles vs peer-reviewed sources on the 10 most costly diseases found that 9 of the 10 Wikipedia articles had errors.3,4
In an earlier article,5 we advocated a proactive approach to managing information, highlighting ways to scan for new information and to develop habits of extracting useful information that can then be stored and easily recovered. To complement this strategy and weed out erroneous information, physicians need reliable sources of unbiased information to efficiently answer clinical questions at the point of care.1,6
Here, to help busy clinicians choose which point-of-care resources to use, we review several of the most popular ones, examining their ease of use, key elements, strengths, and weaknesses.
WHAT MAKES A RESOURCE GOOD?
Key features that make point-of-care tools effective include:
Ease of use, with standard formats, a summary for each topic, or both
Links to original articles and concise, capsular summaries and syntheses of the data
Continuing medical education (CME) credit. Tip: when searching, add “CME” to the search string on the browser to access resources that provide this.
Institutional and individual accounts. For clinicians who work for large organizations, point-of-care products may be paid for already, or reimbursement may be available for your subscription. If unsure, ask your director of information technology or library services.
Freedom from advertisements. Many Internet sources have advertisements that either run alongside the information you want to see or, more annoyingly, pop up and require an action to move forward. There is also continuing concern about the effect of industry support on content.7 While not all of the resources that we use regularly and that we review here are ad-free, avoiding programs with high ad content helps limit the possibility of bias and the time it takes to access information. Although advertisements do bring up a risk of bias, resources with a low-level ad content can limit bias while providing free or low-cost access.
Evidence, not expert opinion. Many resources have an “about” page that explains their philosophy and the source of their information. It is vital to be sure that point-of-care databases are providing facts based on evidence.8 This page also typically addresses how authors and editors are selected and whether expert opinion is used when randomized trials are lacking.
Ease of access. Many tools can be accessed not only on computers but also through apps for smartphones and tablets. Some electronic medical records have clinical decision tools embedded in them, with varying capabilities.
Disclosure of conflict of interest. As conflicts of interest can shade recommendations, information sources should clearly disclose financial relationships that could be perceived as conflicts of interest—for example, authors writing about medications sold by companies with whom they have a financial relationship.
NO SINGLE RESOURCE DOES EVERYTHING
There are many types of tools for finding evidence-based medical information. Different tools serve different purposes. Table 1 lists “toolbox essentials” for clinicians needing to answer clinical questions during patient care.
For example, when a question about the need for a bone mineral density measurement comes up, it is useful to be able to quickly compare guidelines from different professional societies on the National Guideline Clearing House. For another example, if a patient brings in a medication in an unlabeled bottle, a pill identifier app can tell you what it is. Clinicians who can use these resources appropriately will be at an advantage in being able to use information to provide better care to their patients.
To date, no point-of-care summary source has been shown to be superior in all categories, and use may be driven by ease of navigation, clinician preference, clinical question, or past success.9,10
Reviewed below are several applications that can be used as point-of-care resources (Table 2).
CLINICAL EVIDENCE
Clinical Evidence provides systematic reviews on medical topics. Founded in 1999 by the British Medical Journal, it is available in print as the Clinical Evidence Handbook and in online desktop and smartphone formats.
More than any other source we reviewed, Clinical Evidence addresses not only the evidence that exists, but also the data that do not exist to guide decisions. Compared with 9 other point-of-care resources, Clinical Evidence was found to have the highest quality of evidence.11
Strengths of Clinical Evidence
- Uncommonly transparent in terms of source of evidence or disclosing when there is a lack of evidence.
- Clearly lists the strength and relevance of the evidence.
- Personalization. Users can add notes to articles, save personal searches, and bookmark pages for easy access later.
- Navigability. Users can easily access systematic reviews, key points, retracted papers, or guidelines.
- Intuitive organization, with information categorized as research, education, news, or campaigns.
- New content daily: podcasts, articles, videos.
Weaknesses of Clinical Evidence
- Limited topics (eg, Lyme disease was not available)
- The limited content is a challenge when needing quick information at the point of care and may cause most clinicians to use another source unless looking for comparisons of interventions.
- Cost. Subscribing to the service “on demand,” ie, to look up a single specific topic, costs $36 for 48 hours of access; monthly access or a “season ticket” allows 30 days of viewing of all content for $53. At over $600/year, this is one of the most costly of the sources we reviewed.
- Marketing of Clinical Evidence to academic institutions that support the service for faculty may limit its appeal to other clinicians.
DYNAMED
Dynamed, a clinical reference created by a group of physicians, was previously owned by the American College of Physicians and known as Smart Medicine; it is now owned by EBSCO.12 Reviewers investigate the literature for a given topic and create pithy summaries for busy clinicians. A top feature in Dynamed is its links to full articles cited for best practices or evidence-based guidelines. The company describes their content as free of expert opinion, while being unbiased and evidence-based.
Dynamed uses a 7-step algorithm for searched topics that identifies articles, assesses clinical relevance, evaluates validity of outcomes, compiles the evidence from multiple articles, and then updates the final recommendations daily.
Dynamed Plus, the new upgraded version, updates searched topics several times a day. Dynamed may be the most frequently updated point-of-care resource, with the least risk of conflict of interest, but it offers limited topics drawn from evidence-based findings.11,13–15
With the rapid doubling of the medical literature, frequent updates allow clinicians to be most current with practice guidelines. This potentially affects quality of care for antibiotic use, vaccination, health promotion, and screening as well as newly approved medications.
Strengths of Dynamed
- Large collection of topics, critically appraised, written for primary care physicians, presented in bulleted format
- The most frequently updated database11,14,15
- Can integrate with major electronic health records (eg, Epic, Allscripts, NextGen, Cerner)
- Has an area devoted to new information that changes current practice
- Chosen topic grouped with related topics in the differential diagnosis after the initial search
- Easy-to-read outline for quick access to information such as billing, diagnosis, and references
- Medical calculators
- No advertisements
- Helpful embedded tools
- Icons to print or email the article
- An icon to create a “perma-link” to topics, searches, and browse categories
- Graded evidence with a link to the grading model used
- Links to primary articles
- Patient information handouts
- Alerts for updated information
- CME credit
- Special consideration and features for medical education
- The upgraded version Dynamed Plus contains Micromedex for a medication database, expanded graphics, semantic search, concise overview for each topic, and expanded content.
Weaknesses of Dynamed
- Although the topic list is large, it is only about one-third the size of UpToDate.
- A subscription for a physician costs $395 a year. Residents can sign up for about $150, and students for just under $100.
- CME is obtainable but cumbersome; one submits the CME credits through Tufts Healthcare, which requires a second sign-on to access and track.
- Drug and nondrug treatments for diseases cannot be separated.
- Useful calculators include decision trees for clinical decision-making, but there is no way to search them—one must waste time scrolling through the topics and specialties looking for desired information.
- Major shortcoming: there is no medication reference tool unless you upgrade to Dynamed Plus.
- The expanded graphics of Dynamed Plus are difficult to view on mobile applications within the articles (they are brought up more reliably when searching just for the image).
- The use of strict evidence-based methodology without expert opinion is a strength, but limits the collection of topics without randomized controlled trials, for which turning to expert opinion may be the only option.
EVIDENCE ESSENTIALS
Evidence Essentials is a point-of-care resource from Wiley that offers a variety of content types. The website lists 13,000 medical topics; however, they are not all summary reviews as discussed in the other products above. Subject matter is reviewed 3 times a year. Comprehensive reviews number just under 800 individual topics, with the remaining content consisting of Cochrane reviews, calculators, decision support tools, POEMs (Patient-Oriented Evidence that Matters), evidence-based medical guidelines, and dermatology images (1,000).
Evidence Essentials provides some unique content including a quick evaluation and management (E/M) code-finder and calculators not only for the typical medical equations, but also for history and physical examination likelihood ratios and pretest probabilities, which are practical and an excellent teaching aid. It also offers CME along with POEMs, e-mail alerts, and a listing of upcoming topics.
Strengths of Evidence Essentials
- Relatively inexpensive at $85 a year.
- High-functioning filter system to choose to search one or multiple databases.
- Related results are listed for aid in differential diagnosis, similar to Dynamed.
- Authors, editors, and date of last review are highly visible. As in UpToDate, relevant medical calculators appear on the page.
- The likelihood and odds ratio calculators are a huge plus for clinical decision-making and putting guidelines into practice.
- “Overall bottom line” highlights key points
- Grading of evidence per topic.
- Bulleted and tabbed information for quick access.
- Tabs for information on background, prevention, diagnosis, treatment, references, guidelines, and special populations.
Weaknesses of Evidence Essentials
- Limited number of topics with comprehensive reviews.
- While you can click on any drug name and link to a choice of two drug databases, this is not included in the subscription and requires a second account.
- The resources tabs had some broken links. In our clinical example, the tab contained several videos at the top that were not related, followed by a map and tables that were relevant to Lyme disease.
- Likewise, some of the guideline references were disappointing. For example, the guideline link for Lyme disease is for the US Department of Labor Occupational Safety and Health Administration rather than a professional society.
- For the provider wanting a narrative, this is more of a bare-bones text.
FIRST CONSULT
First Consult is Elsevier’s point-of-care clinical decision product contained within ClinicalKey.
Unlike UpToDate and Dynamed, in which authors and editors read original articles and summarize or synthesize information for the learner, First Consult is a “smart” search engine that will research a question, together with associated terms and key words. Filters such as full-text availability, journal articles, and patient education can be applied.
You may need to read about your topic in a textbook first, and then, if you are looking for treatment information, find an original article through First Consult. It is available in mobile and desktop formats, and the point-of-care product, First Consult, has an app that can be downloaded and used for free for the first 60 days.
Importantly, the First Consult portion of ClinicalKey with the summary topics was rated by Shurtz and Foster13 as least current of the products we are discussing in this article. On the other hand, it was the only product that had an embedded program to assist the user in making presentations by allowing drag and drop of images and automatic citing of sources. Kim et al report that First Consult is one of the resources providers prefer.9
Strengths of First Consult
- Lengthy free trial
- Ability to access original articles from a list vs lengthy narrative
- Access to journals and books published by Elsevier
- Powerful search engine that applies associated terms automatically
- Patient education is available in different languages and font size with the ability to add instructions and even a local branding
- Can integrate with electronic health record
- Can filter results by guideline, patient education, topic overviews
- Presentation assistance.
Weaknesses of First Consult
- Time-intensive. A provider needing quick advice on treatment for a medical condition has to guess if an article or textbook will have the most up-to-date and digestible information, whereas this has already been summarized in other products. For the busy clinician, this may be prohibitive.
- Search results are limited to Elsevier products, and major journals such as the New England Journal of Medicine are not available.
- Inconsistent platform functionality. The app version was somewhat “sticky” to use, as pages did not always load efficiently, and the menu bar navigation is not ideal.
- Expensive, especially given cheaper alternatives. For example, subscribing to the specialty of internal medicine or family medicine costs $499 and provides access to 8 journals and 11 books. Extended access costs $998 and offers full-text access to 23 books and 45 journals. The complete service has a total of 400 journals, 700 books, and 2,500 procedural videos.
MEDSCAPE
Medscape, owned by parent company WebMD, has long been a popular resource. The most recent versions are available for both for Android and iOS mobile platforms. The desktop and mobile apps claim to be designed for point-of-care use, and can be downloaded at no cost after registering as a Medscape user.
Medscape has some interesting features, including a handy pill identifier tool that is new to Medscape and perfect for the “I take one blue pill for my cholesterol” moments. The drug information tools and other features work well offline.
Medscape contains a well-presented drug database and interaction checker, as well as a growing collection of evidence-based articles and videos with links to references in Medline. From the point-of-care standpoint, Medscape also offers a number of decision-making algorithms and a continuously updated medical literature and health-related newsfeed. It contains in-app medical calculators, searchable directories for providers, hospitals, and pharmacies, and CME that can be earned on the website or from the application.
The main Medscape website contains pop-up advertisements, but the mobile app has fewer. Among the occasional frustrations, updates are relatively infrequent, the content is slow to load, and the phone app can be cumbersome. Of note, in one review,11 Medscape was found to have the lowest quality of evidence.
Strengths of Medscape
- Free with registration
- Medical calculator
- Drug interaction checker
- Pill identifier
- Evidence-based information covering about 4,000 conditions with links to references in Medline
- Ability to e-mail articles for sharing or future reference
- CME
- Unique database of hospitals, providers, and pharmacies to aid in referrals or locating other healthcare professionals
- Algorithms for decision-making
- Images and videos for procedural review and learning
- Option for downloading certain databases for offline use
- Medical news helps you keep up with what patients are watching and reading.
Weaknesses of Medscape
- Advertisements (many of them pop-up)
- The content is updated less frequently than other products listed in this article
- The smartphone app can run slowly
- Quality of reviews may be a concern.
UpToDate
UpToDate (Wolters Kluwer) is used widely by medical students, residents, and fellows as well as practicing providers. It contains narrative reviews of topics written by respected experts directed at both clinicians and clinical staff. In hopes of appealing to many markets, it offers different subscription types so you can customize your choices with add-on features (UpToDate Desktop and UpToDate MobileComplete allow downloading of all content to be accessed offline), different service packages (1-, 2-, and 3-year subscriptions), and the traditional base product that provides online access.
Of the products we reviewed, UpToDate has the largest selection of medical topics, approaching 10,000.14 In some studies,10,15 it also had the fastest retrieval time for searches. It uses evidence-based graded recommendations that are updated regularly.
Some have lamented that there is too much information per topic.9 In response to early reviews, Wolters Kluwer has made significant changes in the platform and greatly improved the search engine. UpToDate has expanded to include CME and patient information, trying to become that Holy Grail of websites—a one-stop experience. For the lucky few, UpToDate integrates into some electronic health records and provides a relatively seamless experience at the point of care.
Strengths of UpToDate
- One-stop shopping for information, resources, and CME
- Patient information is easy to read and accessible from the same screen
- The largest repository of medical subject matter
- Ability to cull out only pediatric or adult topics
- Searching available within a medical topic
- Tabs for quick access
- The What’s New feature allows access to practice-changing medical updates
- Medical calculators
- Drug interactions
- CME is is tracked in the system, allowing for CME credit information for hospital privileges and board certification
- Flexibility of access: can use online or download content to mobile/desktop device (the online version is easy to use, although robust wireless reception is needed; offices with slow Internet benefit from the offline feature)
- Electronic health record integration is possible with the most popular systems, such as Epic, eClinicalWorks, NextGen, and Allscripts
- Patient education and medication interaction features embedded in the electronic health record; produced in collaboration with Lexicomp
- Integrated drug database
- Alerts for updates
- References have links to full-text articles
- The date of last update is easily found for verifying information accuracy
- May be provided free for clinicians who are a part of a university or large health system.
Weaknesses of UpToDate
- Articles can be lengthy, which is both a strength and a weakness. Searches can retrieve too much information.9 High volume of text can frustrate the user trying to find bulleted, easy-to-read facts. However, for the person looking for a narrative summary, the content is organized as narrative paragraphs with appropriate headers in the left margin, and the search function is robust and powerful.
- Each topic has a “Summary of Recommendations,” but answers here often require linking back to the main text.
- Patient information is sometimes at a high literacy level.
- Costs more than Dynamed. A 1-year subscription is $499 for a physician, but you have the option of paying $53 for a 30-day recurring subscription. Residents, fellows, and students can pay $199 for 1 year or $19 for a 30-day recurring subscription.
- The requirement to download means that users need to keep their version updated on all of their computers—in each of their examination rooms, for example.
- Concerns about conflict of interest arise because authors and editors may maintain financial relationships with companies that produce medications discussed in the articles they have written.
BUILDING YOUR OWN PERSONAL ONLINE REPOSITORY
Our previous article5 reviewed how to store information using tools such as Evernote and Diigo that allow information viewed on a web page to be exported to any online repository. This can be done using extensions for a web browser or by sending the information to a custom e-mail account for these services.
For information that a provider knows he or she will need repeatedly, storage in one system is actually the easiest method. Such a system can then incorporate key information from the summary tools we have reviewed here. The ideal “electronic filing cabinet” should have several features such as a the capability to label articles by topic, to separate or sort as you see fit, and a search function to find information quickly—making it a personalized and effective point-of-care resource.
STAYING AFLOAT
Clinicians make many decisions every day. In fact, the release of How Doctors Think (both publications) has led to increased research into how clinical decisions and diagnoses are formed.16,17
With the medical literature expected to double every 73 days by 2020,18 there is an ever-widening ocean of information to sift through. With this onslaught, clinicians can no longer remain fully current. Instead, refining skills in accessing, sorting, and interpreting accurate scientific evidence efficiently is crucial to time spent actually caring for patients and coordinating their care.
Guidelines, algorithms, and comprehensive databases can aid clinicians in all aspects of care, from generating more complete differential diagnoses to managing disease-specific treatment. Individuals can first think about and list the qualities of a tool that are most important to them (eg, breadth of topics, frequency of updates, integration within their electronic health record, and cost) before focusing on a few applications or websites that meet those goals. With practice, point-of-care knowledge can become part of the everyday visit.
Effective integration into electronic health records will require design input from front-line clinicians. Otherwise, systems are prone to add too much “support” and overly rely on orthodox metrics and guidelines, resulting in alarm fatigue and frustration rather than facilitation.19–23
OUR CONCLUSIONS
Comprehensive point-of-care resources can play a significant role in helping busy clinicians provide best evidence-based care to their patients. Embedded clinical decision guides within an electronic health record are ideal, but low topic coverage has limited the usefulness of these systems.24 Here are our conclusions:
Medscape, ePocrates, and Wikipedia are probably the most popular free resources. Dynamed has offered free subscriptions to Wikipedia’s top health editors with the hopes of correcting factual errors. Medscape has excellent features but is supported by sponsored content, which raises a concern about bias and potential time-consuming distractions.
Dynamed and UpToDate have both been reported to answer more questions than other sources.12
UpToDate has the largest repository, with each topic curated by an expert or experts in that subject. This content can be dense and difficult to scan quickly at the point of care, but this is balanced by the ability to search within a medical topic, which has given it the fastest retrieval time.15 It does, however, allow authors and editors to maintain financial relationships with companies that produce medications discussed in the article.22
Dynamed has the advantage in frequency of updates, clearest conflict-of-interest policy, and the least amount of conflict of interest. Its topic list is not as extensive as UpToDate’s due to the limitation of using only evidence-based medicine without expert opinion.
First Consult has high user satisfaction, but as a point-of-care resource it can be time-consuming to find the best source for the clinical question at hand, and its expanded access is costly.9
ART AND SCIENCE
Point-of-care resources do not solve all the complicated problems of patient care, and no single resource is ideal for all situations. A busy clinician has limited time to process the evolving literature to practice the best evidence-based medicine. Effective information access, quality of care provided, and the marginal time cost required create a complex calculus. Clinical decision-making remains an art and a science,25 but these technologies help define a new era in its pursuit.
Ultimately, a clinician’s choice needs to correlate with a provider’s resources and style. This article has detailed several options available on the market today. This is a quickly evolving area of products and services. Longer term, users might consider a tool’s preferred key features when evaluating any current or future resource in order to choose the right ones for their practice.
CASE REVISITED
Before we leave for the weekend, we need a plan for Ms. Connecticut. To find appropriate recommendations for our patient, we search several of our point-of-care resources: UpToDate and Dynamed. Both resources have correct information according to the Infectious Disease Society of America (IDSA) guidelines.
UpToDate has a monograph of approximately 2,000 words on Lyme disease, which is lengthy but adds to clinical-decision making skills for a learner thinking through the decision. This service also has a patient handout highlighting the recommendations. The topic was last updated in 2016, but states that it is current with literature through January 2017.
Dynamed has bulleted information that is quicker to digest, but essentially highlights the IDSA recommendations without the thought process behind them. It too, has patient resources with links to a variety of handouts from professional organizations such as the US Centers for Disease Control and Prevention. They last updated the topic January 31, 2017.
When searching for the topic on both sites, a clinician can see the breadth of information in each program. However, this is also a detractor. Searching for Lyme disease prophylaxis on Dynamed brought up related data (that doxycycline is not FDA-approved for prophylaxis), but not the primary information. Likewise, the search under UpToDate first brought us to the patient information. Both articles have helpful tables and links to associated topics.
My partner chose the UpToDate article, in part to review the topic with a medical student. However, I used Dynamed for its quick bulleted information, as I was on call that evening and needed to return to the hospital. We both came to the same conclusion, and Ms. Connecticut chose no prophylaxis even though her home is in an endemic area. She has done well.
- Worster A, Haynes RB. How do I find a point-of-care answer to my clinical question? CJEM 2012; 14:31–35.
- Jeffery R, Navarro T, Lokker C, Haynes RB, Wilczynski NL, Farjou G. How current are leading evidence-based medical textbooks? An analytic survey of four online textbooks. J Med Internet Res 2012; 14:e175.
- ClinicalKey. Errors found in nine out of ten Wikipedia health entries. www.clinicalkey.com/info/blog/errors-in-wikipedia-health/. Accessed February 9, 2017.
- Hasty RT, Garbalosa RC, Barbato VA, et al. Wikipedia vs peer-reviewed medical literature for information about the 10 most costly medical conditions. J Am Osteopath Assoc 2014; 114:368–373.
- Mehta NB, Martin SA, Maypole J, Andrews R. Information management for clinicians. Cleve Clin J Med 2016; 83:589–595.
- Cook DA, Sorensen KJ, Hersh W, Berger RA, Wilkinson JM. Features of effective medical knowledge resources to support point of care learning: a focus group study. PLoS One 2013; 8:e80318.
- Steinbrook R. Future directions in industry funding of continuing medical education. Arch Intern Med 2011; 171:257–258.
- Isaacs D, Fitzgerald D. Seven alternatives to evidence based medicine. BMJ 1999; 319:1618.
- Kim S, Noveck H, Galt J, Hogshire L, Willett L, O’Rourke K. Searching for answers to clinical questions using Google versus evidence-based summary resources: a randomized controlled crossover study. Acad Med 2014; 89:940–943.
- Ahmadi SF, Faghankhani M, Javanbakht A, et al. A comparison of answer retrieval through four evidence-based textbooks (ACP PIER, Essential Evidence Plus, First Consult, and UpToDate): a randomized controlled trial. Med Teach 2011; 33:724–730.
- Prorok JC, Iserman EC, Wilczynski NL, Haynes RB. The quality, breadth, and timeliness of content updating vary substantially for 10 online medical texts: an analytic survey. J Clin Epidemiol 2012; 65:1289–1295.
- Prorok JC, Iserman EC, Wilczynski NL, Haynes RB. The quality, breadth, and timeliness of content updating vary substantially for 10 online medical texts: an analytic survey. J Clin Epidemiol 2012; 65:1289–1295.
- Shurtz S, Foster MJ. Developing and using a rubric for evaluating evidence-based medicine point-of-care tools. J Med Libr Assoc 2011; 99:247–254.
- Ketterman E, Besaw M. An evaluation of citation counts, search results, and frequency of updates in Dynamed and UpToDate. J Electron Res in Med Libr 2010; 7:273–280.
- Amber KT, Dhiman G, Goodman KW. Conflict of interest in online point-of-care clinical support websites. J Med Ethics 2014; 40:578–580.
- Montgomery K. How Doctors Think: Clinical Judgment and the Practice of Medicine. New York, NY: Oxford University Press; 2005.
- Groopman J. How Doctors Think. Boston, MA: Houghton Mifflin; 2008.
- Densen P. Challenges and opportunities facing medical education. Trans Am Clin Climatol Assoc 2010; 122:48–58.
- Kesselheim AS, Cresswell K, Phansalkar S, Bates DW, Sheikh A. Clinical decision support systems could be modified to reduce ‘alert fatigue’ while still minimizing the risk of litigation. Health Aff (Millwood) 2011; 30:2310–2317.
- Russ AL, Zillich AJ, McManus MS, Doebbeling BN, Saleem JJ. Prescribers’ interactions with medication alerts at the point of prescribing: a multi-method, in situ investigation of the human-computer interaction. Int J Med Inform 2012; 81:232–243.
- Fraccaro P, Arguello Castelerio M, Ainsworth J, Buchan I. Adoption of clinical decision support in multimorbidity: a systematic review. JMIR Med Informatics 2015; 3:e4.
- McLeod W, Eidus R, Stewart EE. Clinical decision support: using technology to identify patients’ unmet needs. Fam Pract Manag 2012; 19:22–28.
- Colla CH. Swimming against the current—what might work to reduce low-value care? N Engl J Med 2014; 371:1280–1283.
- Cook DA, Sorensen KJ, Nishimura RA, Ommen SR, Lloyd FJ. A comprehensive information technology system to support physician learning at the point of care. Acad Med 2015; 90:33–39.
- Woolever DR. The art and science of clinical decision making. Fam Pract Manag 2008; 15:31–36.
- Worster A, Haynes RB. How do I find a point-of-care answer to my clinical question? CJEM 2012; 14:31–35.
- Jeffery R, Navarro T, Lokker C, Haynes RB, Wilczynski NL, Farjou G. How current are leading evidence-based medical textbooks? An analytic survey of four online textbooks. J Med Internet Res 2012; 14:e175.
- ClinicalKey. Errors found in nine out of ten Wikipedia health entries. www.clinicalkey.com/info/blog/errors-in-wikipedia-health/. Accessed February 9, 2017.
- Hasty RT, Garbalosa RC, Barbato VA, et al. Wikipedia vs peer-reviewed medical literature for information about the 10 most costly medical conditions. J Am Osteopath Assoc 2014; 114:368–373.
- Mehta NB, Martin SA, Maypole J, Andrews R. Information management for clinicians. Cleve Clin J Med 2016; 83:589–595.
- Cook DA, Sorensen KJ, Hersh W, Berger RA, Wilkinson JM. Features of effective medical knowledge resources to support point of care learning: a focus group study. PLoS One 2013; 8:e80318.
- Steinbrook R. Future directions in industry funding of continuing medical education. Arch Intern Med 2011; 171:257–258.
- Isaacs D, Fitzgerald D. Seven alternatives to evidence based medicine. BMJ 1999; 319:1618.
- Kim S, Noveck H, Galt J, Hogshire L, Willett L, O’Rourke K. Searching for answers to clinical questions using Google versus evidence-based summary resources: a randomized controlled crossover study. Acad Med 2014; 89:940–943.
- Ahmadi SF, Faghankhani M, Javanbakht A, et al. A comparison of answer retrieval through four evidence-based textbooks (ACP PIER, Essential Evidence Plus, First Consult, and UpToDate): a randomized controlled trial. Med Teach 2011; 33:724–730.
- Prorok JC, Iserman EC, Wilczynski NL, Haynes RB. The quality, breadth, and timeliness of content updating vary substantially for 10 online medical texts: an analytic survey. J Clin Epidemiol 2012; 65:1289–1295.
- Prorok JC, Iserman EC, Wilczynski NL, Haynes RB. The quality, breadth, and timeliness of content updating vary substantially for 10 online medical texts: an analytic survey. J Clin Epidemiol 2012; 65:1289–1295.
- Shurtz S, Foster MJ. Developing and using a rubric for evaluating evidence-based medicine point-of-care tools. J Med Libr Assoc 2011; 99:247–254.
- Ketterman E, Besaw M. An evaluation of citation counts, search results, and frequency of updates in Dynamed and UpToDate. J Electron Res in Med Libr 2010; 7:273–280.
- Amber KT, Dhiman G, Goodman KW. Conflict of interest in online point-of-care clinical support websites. J Med Ethics 2014; 40:578–580.
- Montgomery K. How Doctors Think: Clinical Judgment and the Practice of Medicine. New York, NY: Oxford University Press; 2005.
- Groopman J. How Doctors Think. Boston, MA: Houghton Mifflin; 2008.
- Densen P. Challenges and opportunities facing medical education. Trans Am Clin Climatol Assoc 2010; 122:48–58.
- Kesselheim AS, Cresswell K, Phansalkar S, Bates DW, Sheikh A. Clinical decision support systems could be modified to reduce ‘alert fatigue’ while still minimizing the risk of litigation. Health Aff (Millwood) 2011; 30:2310–2317.
- Russ AL, Zillich AJ, McManus MS, Doebbeling BN, Saleem JJ. Prescribers’ interactions with medication alerts at the point of prescribing: a multi-method, in situ investigation of the human-computer interaction. Int J Med Inform 2012; 81:232–243.
- Fraccaro P, Arguello Castelerio M, Ainsworth J, Buchan I. Adoption of clinical decision support in multimorbidity: a systematic review. JMIR Med Informatics 2015; 3:e4.
- McLeod W, Eidus R, Stewart EE. Clinical decision support: using technology to identify patients’ unmet needs. Fam Pract Manag 2012; 19:22–28.
- Colla CH. Swimming against the current—what might work to reduce low-value care? N Engl J Med 2014; 371:1280–1283.
- Cook DA, Sorensen KJ, Nishimura RA, Ommen SR, Lloyd FJ. A comprehensive information technology system to support physician learning at the point of care. Acad Med 2015; 90:33–39.
- Woolever DR. The art and science of clinical decision making. Fam Pract Manag 2008; 15:31–36.
KEY POINTS
- Today, it seems impossible to keep up with all the information we need, but we can refine our skills in accessing, sorting, and interpreting accurate scientific evidence.
- The resources reviewed in this article require paid subscriptions except for Medscape, which is supported by advertising.
- Each of the resources has strengths and weaknesses. For example, UpToDate offers the most topics, but its articles tend to be too long to be practical to read at the point of care.
- Physicians should familiarize themselves with these resources and use the ones that best suit their needs.
Information management for clinicians
Accessing, absorbing, organizing, storing, and retrieving potentially useful medical information is a challenge. Physicians used to try meet this challenge with personal libraries of journal articles in their file cabinet. Today, that is inadequate to combat the deluge of digital information. In 2013, the Institute of Medicine acknowledged this problem, stating, “The ever-increasing volume of evidence makes it difficult for clinicians to maintain a working knowledge of new clinical information.”1
The sheer volume of data has meant that, rather than try to maintain a regular diet of professional reading (proactive scanning2), many of us now seek information only when we need answers to specific clinical questions (reactive searching). This approach promotes lifelong problem-based learning but assumes that we are consciously aware of this need and are aware of the need to search for new information.
We need to constantly scan for new evidence in our area of practice to avoid becoming falsely assured of our knowledge. We also need to be able to find information we have seen before we need to use it. The following are examples of how using this approach could dramatically empower a busy clinician.
On a recent clinic day, a colleague pokes his head into your office and asks, “Have you heard anything about niacin in the news? I have a patient who is asking me if we should discontinue it.” You respond: “Yes, there was something that just came out. I am not sure where I read it or heard about it. Give me a couple of seconds and I can find it.” True to your word, a few seconds later you find and share the latest article on the HPS2-THRIVE trial and a commentary on the results.
Later, your first patient of the day asks you, “When we switched to dabigatran, you mentioned that, unlike warfarin, there was no specific reversal agent. I heard that there is one now?” Instead of being taken aback, you nod your head. “Yes, I saw that recent article showing that the medication rapidly and completely reverses the effect of dabigatran in the majority of patients. While I hope we don’t need it, this is good news, particularly as there did not seem to be any major adverse events.”
Sounds too good to be true? Can this really be you? In this article, we outline an information management strategy (Figure 1) and tools to help busy clinicians stay up to date with new medical evidence in their areas of interest or expertise. In addition, we provide a strategy for leveraging technology to easily retrieve previously viewed information. A future article will specifically show how to best access information at the point of patient care.
THE NEED TO MANAGE INFORMATION
Physicians are expected to practice evidence-based medicine. When faced with a clinical question, we should search for evidence using focused queries of primary and secondary sources such as PubMed or the Cochrane Library. This is an important skill and is appropriate when we take time to look for an evidence-based answer to a specific question. In many cases, it is appropriate to continue with a current practice until newer information has been reviewed and validated.
Unfortunately, indexing and adding new recommendations to these information sources takes time. We may also be unaware that new information is available and may continue to practice as usual until faced with a situation like those outlined above or until we attend a continuing medical education activity, often quite by chance.
Today we can proactively update ourselves in a manner tailored to our own interests and focus and retrieve important information easily when we need it.
A STRATEGY FOR INFORMATION MANAGEMENT
In general, we come across new information in one of three ways:
- Proactive scanning of personalized sources of information—as discussed above, a habit of regular scanning is critical to information management
- Reactive searching for information to answer clinical problems or when doing research
- Incidentally—an e-mail from a colleague, information shared on a social network or encountered while surfing the Internet.
In each case, we may find information that is potentially useful, something we may need to find again in the future. But unless we use this information often, we will not remember the details or may even forget we had seen it. Thus, we need a strategy to store this information so we can retrieve it easily at any time with any device; neuroscientists call this the “externalization” of memory.3 Ideally, even if we forget that we ever saw this information or where we stored it, a search would retrieve the location and details of this formerly viewed information.
In the following sections, we outline steps and tools of a strategy for managing clinical information relevant to your practice.
STEP 1: SETTING UP INFORMATION FEEDS
The first step in this information management strategy is to become aware of relevant new information in your area of practice or research. To do this, you proactively set up feeds of information from reliable and authentic sources. These feeds can be browsed on any computer or smart mobile device.
There are several possibilities for creating these feeds. One option is to subscribe to the table of contents (TOC) of relevant journals via e-mail.
A more versatile and full-featured option is a research site summary (RSS) feed-reader. RSS is a standard for publishing summaries (feeds) of frequently updated content on the World Wide Web, such as journal TOCs and items from medical journal news sites (Table 1 shows what this looks like on screen), as well as aggregators like the American College of Physicians Journal Club. You can subscribe to these using feed-reader software from Feedly (www.feedly.com) or Inoreader (www.inoreader.com), which can be used with any browser on a desktop or laptop. They are also available as apps for mobile devices such as smartphones and tablets. The feed-reader periodically checks for new content and automatically downloads it to the device. Thus, you do not need to check multiple websites for updates or have e-mail inboxes fill with content; the content is delivered to your device for perusal at your convenience. (See online supplement “Information Management for Clinicians” for step-by-step instructions on creating a free Inoreader account and subscribing to feeds.)

RSS feed-readers have several advantages over e-mailed TOCs:
- RSS feeds create a centralized searchable repository of all subscribed information.
- The software keeps track of what you have read and displays only unread items; after a journal TOC e-mail is opened, the entire TOC is marked as having been read.
- You can organize news items into folders by tagging key words.
- Most journals and medical news sites like Medscape and the health section of the New York Times provide RSS feeds at no cost.
- An unlimited number of feed items, or articles, are stored in the cloud and do not affect e-mail storage capacity.
- The feed is automatically updated multiple times a day instead of once a week or once a month.
- In addition, one can create RSS feeds on PubMed for custom searches. Thus, a physician can get automatic regular updates of new articles indexed in MEDLINE in their area of interest.
Users can thus build their own personalized magazine of constantly updated information for access and can search from any web-enabled device. (Note: It is advisable to turn off notifications generated by these apps on mobile devices to reduce distraction.)
STEP 2: BOOKMARKING EVIDENCE
When you find something useful or interesting, bookmarks help you find the information again quickly when you need it. But while the browsers Firefox, Chrome, Internet Explorer, and Safari allow bookmarking, they have significant limitations. Bookmarks may be available only on the device they were created on, and because people use more than one device to go online, they may not remember which device they used to bookmark or view the web page.
Browser bookmarks generally store the address (URL) of the web page and a label that you create, but they do not do much else. Sharing bookmarks with others is also difficult or impossible.
Social bookmarking
Social bookmarking lets you create bookmarks you can share across other devices and with other people. Diigo (www.diigo.com) and Delicious (www.delicious.com) are two social bookmarking services that let you integrate with all popular browsers through a button or toolbar. They allow you to save displayed web pages with labels, descriptions, and tags.
Diigo offers two additional features. It allows web pages to be annotated with highlights and notes. And during a Google search, relevant results from the Diigo library are simultaneously displayed.
If you forget you bookmarked something and saved it in your Diigo library, when you search for the information again on Google, Diigo will automatically display any results from your Diigo library next to the Google search results. This is very helpful as it is much easier to review information you have already read, marked up, and saved than it is to start over.
Bookmarks and annotations are stored in the cloud and can be accessed by any device. (See “Information Management for Clinicians” to learn how to sign up for a free Diigo account, and how to use it.)
STEP 3: STORING YOUR INFORMATION
You may want the option to store full-text information in your personal library. This information was once stored in file cabinets and, more recently, on hard drives and USB flash drives. But information stored with these methods is not available or searchable on multiple devices from any location.
Cloud storage
Cloud storage services meet the need for access to stored information at any time and with any device. Options include Dropbox (www.dropbox.com), Box (www.box.com), Google Drive (drive.google.com), OneDrive (onedrive.live.com), and Evernote (www.evernote.com). Each provides different amounts of free storage and has apps available for most platforms and devices. They provide search tools and the ability to share articles or “folders” with other users. The information on these online drives is “synced” between all devices so that the most up-to-date version is always available to the user regardless of location and device.
Evernote offers multiple folders called notebooks to store and segregate data. The open notebook shown in Figure 2 is named “reference articles.” It has the HPS2-Thrive article from the New England Journal of Medicine (N Engl J Med) tagged with the terms “niacin” and “lipid” to facilitate retrieval. The article was saved from that journal’s website using an Evernote browser extension that allows entire web pages or selections to be saved to Evernote with a single click. Evernote also has a powerful search feature that can find text in images or in PDF documents. In addition, it allows easy sharing of a note or an entire notebook. Once a note or notebook is shared, all parties can add to it. In The Evernote app also allows tablet and smartphone access to the shareable content.
The other services listed here have similar feature sets. Dropbox is perhaps the easiest to adopt, but it offers the least amount of free storage. If you use Microsoft Office software, OneDrive lets you edit documents online, and an Office 365 subscription includes 1 terabyte of storage. Google Drive is probably the best solution for online collaboration, such as coauthoring a paper. Box is one of the few online storage solutions that complies with the Health Insurance Portability and Accountability privacy rules.
PUTTING IT ALL INTO PRACTICE
Once you have become familiar with Inoreader and Diigo (see Information Management for Clinicians for step-by-step instructions), the following scenario shows how to adapt them into an efficient workflow.
Dr. Smith has a smartphone, a tablet, a laptop at home, and a desktop at work. She signs onto Google Chrome as her preferred browser on all devices. This seamlessly loads her Diigo extension when she is using a laptop or desktop. She has set her RSS feeds for her preferred journal TOCs and medical news sites to be downloaded to Inoreader. (For details on how to add a medical journals feed bundle and a medical news feed bundle, visit Information Management for Clinicians.)
Instead of reading paper journals, Dr. Smith browses her customized up-to-date “magazine” on Inoreader. When she comes across a relevant article, she marks it as “favorite.” If she has more time, she visits the web page, reviews the information, and saves it to her Diigo library with annotations if appropriate.
When searching for information on the web, she uses Google—without having to remember if she bookmarked information related to the search term. The Diigo extension in her browser automatically searches and displays information from her Diigo library next to her Google search results, and she can instantly see her notes from the last time she read the article.
Relating this workflow to the example of the dabigatran story above, Dr. Smith sees an article about dabigatran reversal while viewing her N Engl J Med medical news feed on her feed-reader. She marks it as a favorite and tags it with the key terms “cardiology” and “vascular” (Figure 3).
Dr. Smith later returns to look at her favorite feed items and visits the article on the N Engl J Med website. She annotates the article and saves it to her Diigo library (Figure 4).
Since this information is highly relevant to her practice, she also visits the N Engl J Med website to read the full article and the accompanying editorial (Figure 5). She annotates these and also saves them to her Diigo library.
Later, if she searches Google for dabigatran (using her default Google Chrome browser with Diigo extension), she will see the usual Google search results and twinned Diigo bookmarks (Figure 6).
If she clicks on one of the links, the browser will load the web page with all the annotations that she made when she first visited.
CONCLUSION
The strategies and tools we describe here let you create a personalized and constantly updated medical news “magazine,” accessible from any of your web-enabled devices. They can transform the Internet into a searchable notebook of personally selected, annotated information, helping you to more easily stay up to date with advances in your field of practice, and to more easily manage the modern information overload.
- Institute of Medicine (IOM). Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: National Academies Press; 2013. www.nap.edu/openbook.php?record_id=13444&page=R1. Accessed May 17, 2016.
- Slotnick HB. Physicians’ learning strategies. Chest 2000; 118(suppl 2):18S–23S.
- Levitin DJ. The Organized Mind: Thinking Straight in the Age of Information Overload. New York, NY: Dutton; 2014:528.
Accessing, absorbing, organizing, storing, and retrieving potentially useful medical information is a challenge. Physicians used to try meet this challenge with personal libraries of journal articles in their file cabinet. Today, that is inadequate to combat the deluge of digital information. In 2013, the Institute of Medicine acknowledged this problem, stating, “The ever-increasing volume of evidence makes it difficult for clinicians to maintain a working knowledge of new clinical information.”1
The sheer volume of data has meant that, rather than try to maintain a regular diet of professional reading (proactive scanning2), many of us now seek information only when we need answers to specific clinical questions (reactive searching). This approach promotes lifelong problem-based learning but assumes that we are consciously aware of this need and are aware of the need to search for new information.
We need to constantly scan for new evidence in our area of practice to avoid becoming falsely assured of our knowledge. We also need to be able to find information we have seen before we need to use it. The following are examples of how using this approach could dramatically empower a busy clinician.
On a recent clinic day, a colleague pokes his head into your office and asks, “Have you heard anything about niacin in the news? I have a patient who is asking me if we should discontinue it.” You respond: “Yes, there was something that just came out. I am not sure where I read it or heard about it. Give me a couple of seconds and I can find it.” True to your word, a few seconds later you find and share the latest article on the HPS2-THRIVE trial and a commentary on the results.
Later, your first patient of the day asks you, “When we switched to dabigatran, you mentioned that, unlike warfarin, there was no specific reversal agent. I heard that there is one now?” Instead of being taken aback, you nod your head. “Yes, I saw that recent article showing that the medication rapidly and completely reverses the effect of dabigatran in the majority of patients. While I hope we don’t need it, this is good news, particularly as there did not seem to be any major adverse events.”
Sounds too good to be true? Can this really be you? In this article, we outline an information management strategy (Figure 1) and tools to help busy clinicians stay up to date with new medical evidence in their areas of interest or expertise. In addition, we provide a strategy for leveraging technology to easily retrieve previously viewed information. A future article will specifically show how to best access information at the point of patient care.
THE NEED TO MANAGE INFORMATION
Physicians are expected to practice evidence-based medicine. When faced with a clinical question, we should search for evidence using focused queries of primary and secondary sources such as PubMed or the Cochrane Library. This is an important skill and is appropriate when we take time to look for an evidence-based answer to a specific question. In many cases, it is appropriate to continue with a current practice until newer information has been reviewed and validated.
Unfortunately, indexing and adding new recommendations to these information sources takes time. We may also be unaware that new information is available and may continue to practice as usual until faced with a situation like those outlined above or until we attend a continuing medical education activity, often quite by chance.
Today we can proactively update ourselves in a manner tailored to our own interests and focus and retrieve important information easily when we need it.
A STRATEGY FOR INFORMATION MANAGEMENT
In general, we come across new information in one of three ways:
- Proactive scanning of personalized sources of information—as discussed above, a habit of regular scanning is critical to information management
- Reactive searching for information to answer clinical problems or when doing research
- Incidentally—an e-mail from a colleague, information shared on a social network or encountered while surfing the Internet.
In each case, we may find information that is potentially useful, something we may need to find again in the future. But unless we use this information often, we will not remember the details or may even forget we had seen it. Thus, we need a strategy to store this information so we can retrieve it easily at any time with any device; neuroscientists call this the “externalization” of memory.3 Ideally, even if we forget that we ever saw this information or where we stored it, a search would retrieve the location and details of this formerly viewed information.
In the following sections, we outline steps and tools of a strategy for managing clinical information relevant to your practice.
STEP 1: SETTING UP INFORMATION FEEDS
The first step in this information management strategy is to become aware of relevant new information in your area of practice or research. To do this, you proactively set up feeds of information from reliable and authentic sources. These feeds can be browsed on any computer or smart mobile device.
There are several possibilities for creating these feeds. One option is to subscribe to the table of contents (TOC) of relevant journals via e-mail.
A more versatile and full-featured option is a research site summary (RSS) feed-reader. RSS is a standard for publishing summaries (feeds) of frequently updated content on the World Wide Web, such as journal TOCs and items from medical journal news sites (Table 1 shows what this looks like on screen), as well as aggregators like the American College of Physicians Journal Club. You can subscribe to these using feed-reader software from Feedly (www.feedly.com) or Inoreader (www.inoreader.com), which can be used with any browser on a desktop or laptop. They are also available as apps for mobile devices such as smartphones and tablets. The feed-reader periodically checks for new content and automatically downloads it to the device. Thus, you do not need to check multiple websites for updates or have e-mail inboxes fill with content; the content is delivered to your device for perusal at your convenience. (See online supplement “Information Management for Clinicians” for step-by-step instructions on creating a free Inoreader account and subscribing to feeds.)

RSS feed-readers have several advantages over e-mailed TOCs:
- RSS feeds create a centralized searchable repository of all subscribed information.
- The software keeps track of what you have read and displays only unread items; after a journal TOC e-mail is opened, the entire TOC is marked as having been read.
- You can organize news items into folders by tagging key words.
- Most journals and medical news sites like Medscape and the health section of the New York Times provide RSS feeds at no cost.
- An unlimited number of feed items, or articles, are stored in the cloud and do not affect e-mail storage capacity.
- The feed is automatically updated multiple times a day instead of once a week or once a month.
- In addition, one can create RSS feeds on PubMed for custom searches. Thus, a physician can get automatic regular updates of new articles indexed in MEDLINE in their area of interest.
Users can thus build their own personalized magazine of constantly updated information for access and can search from any web-enabled device. (Note: It is advisable to turn off notifications generated by these apps on mobile devices to reduce distraction.)
STEP 2: BOOKMARKING EVIDENCE
When you find something useful or interesting, bookmarks help you find the information again quickly when you need it. But while the browsers Firefox, Chrome, Internet Explorer, and Safari allow bookmarking, they have significant limitations. Bookmarks may be available only on the device they were created on, and because people use more than one device to go online, they may not remember which device they used to bookmark or view the web page.
Browser bookmarks generally store the address (URL) of the web page and a label that you create, but they do not do much else. Sharing bookmarks with others is also difficult or impossible.
Social bookmarking
Social bookmarking lets you create bookmarks you can share across other devices and with other people. Diigo (www.diigo.com) and Delicious (www.delicious.com) are two social bookmarking services that let you integrate with all popular browsers through a button or toolbar. They allow you to save displayed web pages with labels, descriptions, and tags.
Diigo offers two additional features. It allows web pages to be annotated with highlights and notes. And during a Google search, relevant results from the Diigo library are simultaneously displayed.
If you forget you bookmarked something and saved it in your Diigo library, when you search for the information again on Google, Diigo will automatically display any results from your Diigo library next to the Google search results. This is very helpful as it is much easier to review information you have already read, marked up, and saved than it is to start over.
Bookmarks and annotations are stored in the cloud and can be accessed by any device. (See “Information Management for Clinicians” to learn how to sign up for a free Diigo account, and how to use it.)
STEP 3: STORING YOUR INFORMATION
You may want the option to store full-text information in your personal library. This information was once stored in file cabinets and, more recently, on hard drives and USB flash drives. But information stored with these methods is not available or searchable on multiple devices from any location.
Cloud storage
Cloud storage services meet the need for access to stored information at any time and with any device. Options include Dropbox (www.dropbox.com), Box (www.box.com), Google Drive (drive.google.com), OneDrive (onedrive.live.com), and Evernote (www.evernote.com). Each provides different amounts of free storage and has apps available for most platforms and devices. They provide search tools and the ability to share articles or “folders” with other users. The information on these online drives is “synced” between all devices so that the most up-to-date version is always available to the user regardless of location and device.
Evernote offers multiple folders called notebooks to store and segregate data. The open notebook shown in Figure 2 is named “reference articles.” It has the HPS2-Thrive article from the New England Journal of Medicine (N Engl J Med) tagged with the terms “niacin” and “lipid” to facilitate retrieval. The article was saved from that journal’s website using an Evernote browser extension that allows entire web pages or selections to be saved to Evernote with a single click. Evernote also has a powerful search feature that can find text in images or in PDF documents. In addition, it allows easy sharing of a note or an entire notebook. Once a note or notebook is shared, all parties can add to it. In The Evernote app also allows tablet and smartphone access to the shareable content.
The other services listed here have similar feature sets. Dropbox is perhaps the easiest to adopt, but it offers the least amount of free storage. If you use Microsoft Office software, OneDrive lets you edit documents online, and an Office 365 subscription includes 1 terabyte of storage. Google Drive is probably the best solution for online collaboration, such as coauthoring a paper. Box is one of the few online storage solutions that complies with the Health Insurance Portability and Accountability privacy rules.
PUTTING IT ALL INTO PRACTICE
Once you have become familiar with Inoreader and Diigo (see Information Management for Clinicians for step-by-step instructions), the following scenario shows how to adapt them into an efficient workflow.
Dr. Smith has a smartphone, a tablet, a laptop at home, and a desktop at work. She signs onto Google Chrome as her preferred browser on all devices. This seamlessly loads her Diigo extension when she is using a laptop or desktop. She has set her RSS feeds for her preferred journal TOCs and medical news sites to be downloaded to Inoreader. (For details on how to add a medical journals feed bundle and a medical news feed bundle, visit Information Management for Clinicians.)
Instead of reading paper journals, Dr. Smith browses her customized up-to-date “magazine” on Inoreader. When she comes across a relevant article, she marks it as “favorite.” If she has more time, she visits the web page, reviews the information, and saves it to her Diigo library with annotations if appropriate.
When searching for information on the web, she uses Google—without having to remember if she bookmarked information related to the search term. The Diigo extension in her browser automatically searches and displays information from her Diigo library next to her Google search results, and she can instantly see her notes from the last time she read the article.
Relating this workflow to the example of the dabigatran story above, Dr. Smith sees an article about dabigatran reversal while viewing her N Engl J Med medical news feed on her feed-reader. She marks it as a favorite and tags it with the key terms “cardiology” and “vascular” (Figure 3).
Dr. Smith later returns to look at her favorite feed items and visits the article on the N Engl J Med website. She annotates the article and saves it to her Diigo library (Figure 4).
Since this information is highly relevant to her practice, she also visits the N Engl J Med website to read the full article and the accompanying editorial (Figure 5). She annotates these and also saves them to her Diigo library.
Later, if she searches Google for dabigatran (using her default Google Chrome browser with Diigo extension), she will see the usual Google search results and twinned Diigo bookmarks (Figure 6).
If she clicks on one of the links, the browser will load the web page with all the annotations that she made when she first visited.
CONCLUSION
The strategies and tools we describe here let you create a personalized and constantly updated medical news “magazine,” accessible from any of your web-enabled devices. They can transform the Internet into a searchable notebook of personally selected, annotated information, helping you to more easily stay up to date with advances in your field of practice, and to more easily manage the modern information overload.
Accessing, absorbing, organizing, storing, and retrieving potentially useful medical information is a challenge. Physicians used to try meet this challenge with personal libraries of journal articles in their file cabinet. Today, that is inadequate to combat the deluge of digital information. In 2013, the Institute of Medicine acknowledged this problem, stating, “The ever-increasing volume of evidence makes it difficult for clinicians to maintain a working knowledge of new clinical information.”1
The sheer volume of data has meant that, rather than try to maintain a regular diet of professional reading (proactive scanning2), many of us now seek information only when we need answers to specific clinical questions (reactive searching). This approach promotes lifelong problem-based learning but assumes that we are consciously aware of this need and are aware of the need to search for new information.
We need to constantly scan for new evidence in our area of practice to avoid becoming falsely assured of our knowledge. We also need to be able to find information we have seen before we need to use it. The following are examples of how using this approach could dramatically empower a busy clinician.
On a recent clinic day, a colleague pokes his head into your office and asks, “Have you heard anything about niacin in the news? I have a patient who is asking me if we should discontinue it.” You respond: “Yes, there was something that just came out. I am not sure where I read it or heard about it. Give me a couple of seconds and I can find it.” True to your word, a few seconds later you find and share the latest article on the HPS2-THRIVE trial and a commentary on the results.
Later, your first patient of the day asks you, “When we switched to dabigatran, you mentioned that, unlike warfarin, there was no specific reversal agent. I heard that there is one now?” Instead of being taken aback, you nod your head. “Yes, I saw that recent article showing that the medication rapidly and completely reverses the effect of dabigatran in the majority of patients. While I hope we don’t need it, this is good news, particularly as there did not seem to be any major adverse events.”
Sounds too good to be true? Can this really be you? In this article, we outline an information management strategy (Figure 1) and tools to help busy clinicians stay up to date with new medical evidence in their areas of interest or expertise. In addition, we provide a strategy for leveraging technology to easily retrieve previously viewed information. A future article will specifically show how to best access information at the point of patient care.
THE NEED TO MANAGE INFORMATION
Physicians are expected to practice evidence-based medicine. When faced with a clinical question, we should search for evidence using focused queries of primary and secondary sources such as PubMed or the Cochrane Library. This is an important skill and is appropriate when we take time to look for an evidence-based answer to a specific question. In many cases, it is appropriate to continue with a current practice until newer information has been reviewed and validated.
Unfortunately, indexing and adding new recommendations to these information sources takes time. We may also be unaware that new information is available and may continue to practice as usual until faced with a situation like those outlined above or until we attend a continuing medical education activity, often quite by chance.
Today we can proactively update ourselves in a manner tailored to our own interests and focus and retrieve important information easily when we need it.
A STRATEGY FOR INFORMATION MANAGEMENT
In general, we come across new information in one of three ways:
- Proactive scanning of personalized sources of information—as discussed above, a habit of regular scanning is critical to information management
- Reactive searching for information to answer clinical problems or when doing research
- Incidentally—an e-mail from a colleague, information shared on a social network or encountered while surfing the Internet.
In each case, we may find information that is potentially useful, something we may need to find again in the future. But unless we use this information often, we will not remember the details or may even forget we had seen it. Thus, we need a strategy to store this information so we can retrieve it easily at any time with any device; neuroscientists call this the “externalization” of memory.3 Ideally, even if we forget that we ever saw this information or where we stored it, a search would retrieve the location and details of this formerly viewed information.
In the following sections, we outline steps and tools of a strategy for managing clinical information relevant to your practice.
STEP 1: SETTING UP INFORMATION FEEDS
The first step in this information management strategy is to become aware of relevant new information in your area of practice or research. To do this, you proactively set up feeds of information from reliable and authentic sources. These feeds can be browsed on any computer or smart mobile device.
There are several possibilities for creating these feeds. One option is to subscribe to the table of contents (TOC) of relevant journals via e-mail.
A more versatile and full-featured option is a research site summary (RSS) feed-reader. RSS is a standard for publishing summaries (feeds) of frequently updated content on the World Wide Web, such as journal TOCs and items from medical journal news sites (Table 1 shows what this looks like on screen), as well as aggregators like the American College of Physicians Journal Club. You can subscribe to these using feed-reader software from Feedly (www.feedly.com) or Inoreader (www.inoreader.com), which can be used with any browser on a desktop or laptop. They are also available as apps for mobile devices such as smartphones and tablets. The feed-reader periodically checks for new content and automatically downloads it to the device. Thus, you do not need to check multiple websites for updates or have e-mail inboxes fill with content; the content is delivered to your device for perusal at your convenience. (See online supplement “Information Management for Clinicians” for step-by-step instructions on creating a free Inoreader account and subscribing to feeds.)

RSS feed-readers have several advantages over e-mailed TOCs:
- RSS feeds create a centralized searchable repository of all subscribed information.
- The software keeps track of what you have read and displays only unread items; after a journal TOC e-mail is opened, the entire TOC is marked as having been read.
- You can organize news items into folders by tagging key words.
- Most journals and medical news sites like Medscape and the health section of the New York Times provide RSS feeds at no cost.
- An unlimited number of feed items, or articles, are stored in the cloud and do not affect e-mail storage capacity.
- The feed is automatically updated multiple times a day instead of once a week or once a month.
- In addition, one can create RSS feeds on PubMed for custom searches. Thus, a physician can get automatic regular updates of new articles indexed in MEDLINE in their area of interest.
Users can thus build their own personalized magazine of constantly updated information for access and can search from any web-enabled device. (Note: It is advisable to turn off notifications generated by these apps on mobile devices to reduce distraction.)
STEP 2: BOOKMARKING EVIDENCE
When you find something useful or interesting, bookmarks help you find the information again quickly when you need it. But while the browsers Firefox, Chrome, Internet Explorer, and Safari allow bookmarking, they have significant limitations. Bookmarks may be available only on the device they were created on, and because people use more than one device to go online, they may not remember which device they used to bookmark or view the web page.
Browser bookmarks generally store the address (URL) of the web page and a label that you create, but they do not do much else. Sharing bookmarks with others is also difficult or impossible.
Social bookmarking
Social bookmarking lets you create bookmarks you can share across other devices and with other people. Diigo (www.diigo.com) and Delicious (www.delicious.com) are two social bookmarking services that let you integrate with all popular browsers through a button or toolbar. They allow you to save displayed web pages with labels, descriptions, and tags.
Diigo offers two additional features. It allows web pages to be annotated with highlights and notes. And during a Google search, relevant results from the Diigo library are simultaneously displayed.
If you forget you bookmarked something and saved it in your Diigo library, when you search for the information again on Google, Diigo will automatically display any results from your Diigo library next to the Google search results. This is very helpful as it is much easier to review information you have already read, marked up, and saved than it is to start over.
Bookmarks and annotations are stored in the cloud and can be accessed by any device. (See “Information Management for Clinicians” to learn how to sign up for a free Diigo account, and how to use it.)
STEP 3: STORING YOUR INFORMATION
You may want the option to store full-text information in your personal library. This information was once stored in file cabinets and, more recently, on hard drives and USB flash drives. But information stored with these methods is not available or searchable on multiple devices from any location.
Cloud storage
Cloud storage services meet the need for access to stored information at any time and with any device. Options include Dropbox (www.dropbox.com), Box (www.box.com), Google Drive (drive.google.com), OneDrive (onedrive.live.com), and Evernote (www.evernote.com). Each provides different amounts of free storage and has apps available for most platforms and devices. They provide search tools and the ability to share articles or “folders” with other users. The information on these online drives is “synced” between all devices so that the most up-to-date version is always available to the user regardless of location and device.
Evernote offers multiple folders called notebooks to store and segregate data. The open notebook shown in Figure 2 is named “reference articles.” It has the HPS2-Thrive article from the New England Journal of Medicine (N Engl J Med) tagged with the terms “niacin” and “lipid” to facilitate retrieval. The article was saved from that journal’s website using an Evernote browser extension that allows entire web pages or selections to be saved to Evernote with a single click. Evernote also has a powerful search feature that can find text in images or in PDF documents. In addition, it allows easy sharing of a note or an entire notebook. Once a note or notebook is shared, all parties can add to it. In The Evernote app also allows tablet and smartphone access to the shareable content.
The other services listed here have similar feature sets. Dropbox is perhaps the easiest to adopt, but it offers the least amount of free storage. If you use Microsoft Office software, OneDrive lets you edit documents online, and an Office 365 subscription includes 1 terabyte of storage. Google Drive is probably the best solution for online collaboration, such as coauthoring a paper. Box is one of the few online storage solutions that complies with the Health Insurance Portability and Accountability privacy rules.
PUTTING IT ALL INTO PRACTICE
Once you have become familiar with Inoreader and Diigo (see Information Management for Clinicians for step-by-step instructions), the following scenario shows how to adapt them into an efficient workflow.
Dr. Smith has a smartphone, a tablet, a laptop at home, and a desktop at work. She signs onto Google Chrome as her preferred browser on all devices. This seamlessly loads her Diigo extension when she is using a laptop or desktop. She has set her RSS feeds for her preferred journal TOCs and medical news sites to be downloaded to Inoreader. (For details on how to add a medical journals feed bundle and a medical news feed bundle, visit Information Management for Clinicians.)
Instead of reading paper journals, Dr. Smith browses her customized up-to-date “magazine” on Inoreader. When she comes across a relevant article, she marks it as “favorite.” If she has more time, she visits the web page, reviews the information, and saves it to her Diigo library with annotations if appropriate.
When searching for information on the web, she uses Google—without having to remember if she bookmarked information related to the search term. The Diigo extension in her browser automatically searches and displays information from her Diigo library next to her Google search results, and she can instantly see her notes from the last time she read the article.
Relating this workflow to the example of the dabigatran story above, Dr. Smith sees an article about dabigatran reversal while viewing her N Engl J Med medical news feed on her feed-reader. She marks it as a favorite and tags it with the key terms “cardiology” and “vascular” (Figure 3).
Dr. Smith later returns to look at her favorite feed items and visits the article on the N Engl J Med website. She annotates the article and saves it to her Diigo library (Figure 4).
Since this information is highly relevant to her practice, she also visits the N Engl J Med website to read the full article and the accompanying editorial (Figure 5). She annotates these and also saves them to her Diigo library.
Later, if she searches Google for dabigatran (using her default Google Chrome browser with Diigo extension), she will see the usual Google search results and twinned Diigo bookmarks (Figure 6).
If she clicks on one of the links, the browser will load the web page with all the annotations that she made when she first visited.
CONCLUSION
The strategies and tools we describe here let you create a personalized and constantly updated medical news “magazine,” accessible from any of your web-enabled devices. They can transform the Internet into a searchable notebook of personally selected, annotated information, helping you to more easily stay up to date with advances in your field of practice, and to more easily manage the modern information overload.
- Institute of Medicine (IOM). Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: National Academies Press; 2013. www.nap.edu/openbook.php?record_id=13444&page=R1. Accessed May 17, 2016.
- Slotnick HB. Physicians’ learning strategies. Chest 2000; 118(suppl 2):18S–23S.
- Levitin DJ. The Organized Mind: Thinking Straight in the Age of Information Overload. New York, NY: Dutton; 2014:528.
- Institute of Medicine (IOM). Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: National Academies Press; 2013. www.nap.edu/openbook.php?record_id=13444&page=R1. Accessed May 17, 2016.
- Slotnick HB. Physicians’ learning strategies. Chest 2000; 118(suppl 2):18S–23S.
- Levitin DJ. The Organized Mind: Thinking Straight in the Age of Information Overload. New York, NY: Dutton; 2014:528.
KEY POINTS
- The first step in information management is to become aware of relevant new information in your area of practice and set up feeds of information from reliable and authentic sources. These feeds should be accessible from any computer or mobile device and scanned regularly.
- Useful information you come across in various digital streams needs to be bookmarked for future search and retrieval. Social bookmarking lets you create bookmarks you can share across other devices and with other people and retrieve with an Internet search.
- Cloud storage services have apps for most platforms and devices, providing search tools and the ability to share articles or “folders” with other users. The information is “synced” between all devices so that the most up-to-date version is always available, regardless of location and device.
Derm emergencies— detecting early signs of trouble
• Consider starting a course of systemic corticosteroids for a patient with erythroderma, fever, and multiorgan involvement when you strongly suspect a drug reaction is the cause—and have ruled out infection. C
• Suspect Stevens– Johnson syndrome/toxic epidermal necrolysis (SJS/TEN) in a patient with widespread and rapidly progressive desquamation, fever, hypotension, and end-organ involvement. C
• In assessing the severity of skin pain, consider the location; involvement of the eyes, perineum, and hands are associated with greater morbidity. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
The usual approach to dermatologic conditions—honed pattern recognition, a deliberate differential diagnosis, and empiric treatment with longer follow-up—runs counter to the response that dermatologic red flags require. Because patients with signs and symptoms associated with dermatologic emergencies have the potential for rapid clinical deterioration, urgent action is paramount.
With this in mind, we’ve focused on 4 red flags—erythroderma, desquamation, skin pain, and petechiae/purpura—as a starting point, rather than presenting a list of dermatologic emergencies and discussing each diagnosis in turn. The text, tables, and images on the pages that follow will increase your awareness of dermatologic presentations that require an immediate response and help you differentiate between signs and symptoms of serious skin disorders and benign findings that might be described as red flag mimics (TABLE 1).
TABLE 1
Conditions that mimic dermatologic emergencies
| Red skin | |
| Diagnosis | Key discriminating features |
| Allergic contact dermatitis | Itchy, rather than painful |
| Red man syndrome | History of vancomycin infusion |
| Stasis dermatitis | Stasis dermatitis location (lower extremities), pruritus |
| Sunburn | History, sun-exposed areas |
| Desquamation | |
| Diagnosis | Key discriminating features |
| Bullous impetigo | Localized; no systemic manifestations |
| Postinfectious desquamation | Subungual location common; occurs during convalescent phase of illness |
| Petechiae and purpura | |
| Diagnosis | Key discriminating features |
| Local trauma | History and location |
| Pigmented purpuric dermatosis | History and healthy appearance |
| Viral exanthema | Healthy appearance |
Erythroderma: Red skin that’s life-threatening
From an etymological perspective, “erythroderma” simply means red skin. Clinically, however, it is defined as extensive erythema, typically covering ≥90% of the skin surface (FIGURE 1). True erythroderma can be life-threatening and must always be considered a dermatologic emergency.1,2
Diligent monitoring of the speed of progression and the presence of fever, systemic symptoms, and multiorgan dysfunction is essential. In a case review of 56 children who presented to an emergency department with fever and erythroderma, 45% progressed to shock.3 Some common causes of erythroderma are psoriasis; contact, atopic, and seborrheic dermatitis; pityriasis rubra pilaris; cutaneous T-cell lymphoma; drug reaction; and toxic shock syndrome (TSS).4
Is it a drug reaction? Erythroderma, fever, and evidence of multiorgan involvement in a patient taking any medication—not just a new one—prompts consideration of a drug reaction. Antiepileptics, dapsone, and sulfonamides are the most frequent offenders.5
DRESS syndrome (drug reaction with eosinophilia and systemic symptoms) is characterized by fever, lymphadenopathy, elevated liver enzymes, and leukocytosis with eosinophilia, as well as erythroderma. The rash may be urticarial or morbilliform in appearance; petechiae, purpura, and blisters may be present, as well.
Because fever, leukocytosis, and transaminitis are also suggestive of an infectious etiology, DRESS syndrome is frequently overlooked. As a result, its true incidence is unknown. Estimates range from about one in 1000 to one in 10,000 drug exposures.6
In addition to discontinuing the medication, treatment for DRESS calls for systemic corticosteroids—which may actually be harmful when infection, rather than a drug reaction, is the cause. Thus, it is necessary to maintain a high index of suspicion and to thoroughly review the medication history of
any patient who presents with erythroderma and systemic symptoms.
When to suspect toxic shock syndrome. Consider TSS in any patient with erythroderma and hypotension, as well as laboratory evidence of end-organ involvement (including transaminitis, elevated creatinine, anemia, thrombocytopenia, and elevated creatinine kinase). Diagnostic criteria are detailed in FIGURE 2.7 Group A Streptococcus and Staphylococcus aureus are the classic infectious causes, but other bacteria have been implicated, as well. In most cases, the responsible bacterium is not known initially.
Because the toxins produced by these streptococcal and staphylococcal strains act as superantigens that fuel the immune response and worsen the shock, patients with a presumptive diagnosis of TSS should begin empiric treatment with an antimicrobial agent that inhibits toxin synthesis, such as clindamycin, immediately.8,9
FIGURE 1
Erythema covering the chest and arms
This patient was given a diagnosis of erythrodermic psoriasis.
FIGURE 2
Diagnostic criteria for toxic shock syndrome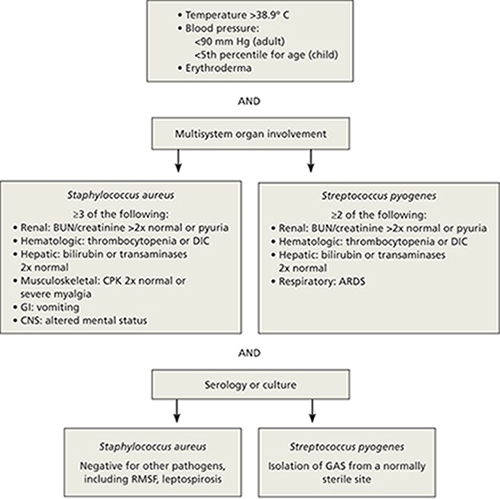
ARDS, acute respiratory distress syndrome; BUN, blood urea nitrogen; CNS, central nervous system; CPK, creatinine phosphokinase; DIC, disseminated intravascular coagulation; GAS, group A Streptococcus; GI, gastrointestinal; RMSF, Rocky Mountain spotted fever.
Adapted from: Pickering LK, et al, eds. Red Book: 2009 Report of the Committee on Infectious Diseases. 2009.7
Desquamation/blistering: Act quickly when it’s widespread
Although desquamation can be seen in benign skin conditions, widespread desquamation with or without bullae requires careful evaluation and a rapid response. Separation, either at the dermal-epidermal junction or intraepidermally, raises the specter of 2 emergent conditions: the Stevens–Johnson syndrome/toxic epidermal necrolysis (SJS/TEN) spectrum and staphylococcal scalded skin syndrome (SSSS). Mucosal involvement is another red flag, if the patient appears ill and the desquamation is progressing rapidly. Conjunctival involvement, in particular, is associated with greater morbidity, and a consult with an ophthalmologist is prude
Rapid progression is a hallmark of SJS/TEN. Desquamation that’s widespread and rapidly progressive in a patient with fever, hypotension, and end-organ involvement is suggestive of SJS/TEN (FIGURE 3). Medications, including allopurinol, antimicrobials, and antiepileptics, are frequent culprits.10,11
Nonsteroidal anti-inflammatory drugs (NSAIDs) have also been linked to SJS/TEN.10 Given their widespread use (1-2 per million users per week), however, the likelihood of NSAIDs leading to SJS/TEN is exceedingly low.12
Signs and symptoms of SJS/TEN may include target lesions with dusky centers, erythroderma, or significant pain without any visible skin abnormality, typically accompanied by fever and malaise. Widespread sloughing of the skin may be seen within several hours.11
Admission to an intensive care unit—preferably a burn unit—is suggested for aggressive fluid resuscitation and management of shock and end-organ dysfunction. Intravenous immunoglobulin G (IVIG) and steroids are often used, although there is little consensus as to the most effective treatment.13 Mortality from TEN approaches 50%.13
SSSS can present at any age. Newborns often present with SSSS during their first week of life: Widespread erythema is quickly followed by fragile blisters, which may have already ruptured by the time the infant receives medical attention. Mucosal surfaces are not typically involved. Nikolsky’s sign (separation of the upper epidermis with gentle pressure) is a classic finding.
Infants with SSSS are frequently irritable, suggesting that the skin may be painful. Cultures from unruptured bullae will be negative as the blisters represent a cutaneous reaction to an infection, rather than a skin infection, but blood, urine, and nasopharynx cultures may be positive. Systemic treatment with nafcillin or oxacillin should be initiated, and supportive skin care provided.14,15 Clindamycin or vancomycin should be used in parts of the country in which methicillin-resistant Staphylococcus aureus is prevalent. In very young infants, the outcome of SSSS is generally favorable. Not so with adults.
Because mature kidneys have a greater ability to excrete exfoliative toxins, SSSS primarily affects adults with significant comorbidities—and has a much poorer prognosis.16 You may also see chronic autoimmune bullous diseases, such as bullous pemphigoid and pemphigus vulgaris, with widespread desquamation and blistering, in the adult population. Untreated, the secondary infection and electrolyte disturbances from fluid loss associated with pemphigus vulgaris can be fatal.
Desquamation is a late finding in Kawasaki disease. Desquamation is often cited as a potential skin finding in children with Kawasaki disease (KD) (FIGURE 4), but usually not until the convalescent stage.17 (Desquamation may also appear during the recovery period of several other infections, including scarlet fever and TSS.) IVIG can prevent coronary aneurysm, the major complication of KD, but only if it is administered during the acute phase of the illness. Therefore, early diagnosis of KD (TABLE 2)18—before desquamation occurs—is critical.19
FIGURE 3
Desquamation, full-thickness epidermal necrosis on the upper back
Erythroderma and widespread denudation on the upper back of a patient who was given a diagnosis of toxic epidermal necrolysis.
FIGURE 4
Desquamation on a young patient
Desquamation associated with Kawasaki disease (shown on the hand of a child) usually occurs during the convalescent stage.
TABLE 2
Diagnostic criteria for Kawasaki disease
| Fever for ≥5 days, and 4 out of 5 criteria (required): |
|---|
|
| Supporting findings: |
|
| CRP, C-reactive protein; ESR, erythrocyte sedimentation rate. Source: Kawasaki Disease Research Committee. Pediatr Int. 2005.18 |
Skin pain is always a red flag
Widespread skin pain should always be taken seriously, as it is rarely associated with minor dermatoses.20 Infectious cellulitis is the most likely diagnosis of a painful erythematous skin lesion. Patients with cellulitis do not usually have erythroderma, as the affected area tends to be very localized.
Cellulitis may be over- or undertreated. Once cellulitis has been diagnosed, the next thing to consider is severity. A recent retrospective study found that misclassification of skin and soft-tissue infections may result in both significant overtreatment of mild soft-tissue infections and dangerous undertreatment of severe infections, with consequent morbidity.21
Location is a key consideration, as cellulitis in certain locations—including the eye, perineum, and hand—carries an increased risk of morbidity. Orbital cellulitis—which may be characterized by proptosis, ophthalmoplegia, and pain with extraocular movements—most often results from initial sinusitis, and can lead to vision loss, intracranial infection, and significant invasive disease. Prompt antimicrobial therapy and urgent ophthalmologic consultation are essential, as operative drainage may be required.22,23
When the perineum is involved, a careful exam must be performed to determine the limits of the affected area. Although Fournier’s gangrene is uncommon, it is a life-threatening infection. In one small retrospective study, more than half of the patients presented with a perianal abscess.24
Similarly, the hand is vulnerable to significant infection, particularly if it is inoculated with bacteria from human mouth flora (the well-described “fight bite”). In a review of 100 cases of human fight bites, 18 patients ultimately required amputation.25
Early necrotizing fasciitis is often missed. Clinicians generally expect painful lesions to also have erythema, swelling, and increased warmth—the cardinal signs of inflammation. As a result, early necrotizing fasciitis, which initially presents with pain out of proportion to other dermatologic findings, may be overlooked. In fact, pain can precede significant skin findings by 24 to 48 hours; prior to that, only mild erythema or swelling (with minimal pain, in some cases) may be evident.26,27
The general pattern, however, is for a site with exquisite tenderness to evolve into a smooth, swollen area, then to develop dusky plaques and late-stage full thickness necrosis with hemorrhagic bullae.26 At that point, necrosis can render the skin insensate. Case reviews have found necrotizing fasciitis to be protean, with only 3 findings—erythema, edema, and tenderness beyond the expected lesion borders—present in most patients.27 Assiduous attention to skin pain in the presence of any other skin manifestation is the key to early diagnosis and rapid treatment.
Petechiae/purpura may be severe or benign
Petechiae are flat, pinpoint, nonblanching spots caused by intradermal hemorrhage associated with a wide variety of conditions, ranging from benign (local trauma) to severe (eg, disseminated intravascular coagulation [DIC] and sepsis). Similarly, purpura—larger lesions that may be palpable—can accompany less severe diseases, such as Henoch-Schönlein purpura (HSP), or life-threatening conditions like sepsis and DIC (FIGURE 5). Here, as in many other dermatologic conditions, the key differentiating features are location (local vs diffuse), speed of progression, and signs and symptoms of systemic illness.
FIGURE 5
Signs of a life-threatening condition
Hemorrhagic bullae with surrounding erythema on the lateral thigh of a patient with purpura fulminans from bacterial sepsis.
Localized petechiae are common with direct trauma, as well as barotrauma associated with coughing, vomiting, or even asphyxiation. Location is an important clue. Periorbital petechiae and petechiae on the chest above the nipple line suggest that the lesions were caused by the force of the barotrauma, rather than systemic disease.28 A careful history and physical exam are needed to rule out serious underlying conditions, such as pneumonia, dehydration, and abdominal obstruction.
Petechiae out of proportion to the force applied may be an indication of an underlying bleeding diathesis, including thrombocytopenia, coagulation defects, and some fulminant infections. Idiopathic thrombocytopenic purpura (ITP) and HSP may present with more widespread petechiae/purpura, but without fever or systemic symptoms. ITP can develop spontaneously, after a viral infection or after a child’s inoculation with the measles-mumps-rubella vaccine.29 ITP typically presents as easy bruising and petechiae out of proportion to the condition that caused it. These patients, as a rule, will have a healthy appearance.
Treatment (with steroids, IVIG, or anti-D immunoglobulin) is generally not required for children with ITP unless they have bleeding that is mucosal or substantial, as spontaneous remission is expected. Adults, who are more likely to develop chronic ITP, may benefit from treatment.30
HSP occurs most commonly in children, who may have palpable purpura, typically in the lower extremities, as well as arthritis or arthralgia, abdominal pain, and renal involvement that can progress from microscopic hematuria or proteinuria to renal insufficiency.31 Typically, children whose disease is in the acute phase do not appear to be sick, with an important exception: Those who develop hemorrhage and edema in the bowel wall, resulting in intussusception, have significant abdominal pain and are more likely to need surgical reduction.32
Diffuse petechiae in the absence of any trauma, accompanied by significant signs of systemic illness, may be an indication of fulminant infection, including meningococcemia, DIC, and Rocky Mountain spotted fever (RMSF). (Fever and diffuse petechiae can also be seen in viral exanthema, but patients usually look well and the rash often has both blanching and petechial components.33)
When a returning traveler presents with a rash and systemic symptoms, it is important to take a thorough history and to consider infections endemic to the area visited. RMSF may initially be localized to the wrists and progress to widespread petechiae over hours to days. Because the cutaneous findings may not be as fulminant—and up to 10% of patients with RMSF have no rash at all34—attention to the noncutaneous features is important. Fever, headache, neurologic symptoms, joint complaints, and abdominal pain (or only a few of these manifestations) in the context of potential tick bite exposure should prompt consideration of RMSF.35
Keep in mind, too, that in cases of fulminant infections such as meningococcemia and DIC, the hallmark purpura fulminans may not be present initially.36 Although the initial cutaneous findings may be subtle, however, such patients will appear quite ill, and their condition will deteriorate rapidly. Because prompt antibiotic therapy can save life and limb, a high index of suspicion should be maintained for any patient who presents with a rash in the setting of fever and hypotension or other evidence of shock.
1. Botella-Estrada R, Sanmartin O, Oliver V, et al. Erythroderma. A clinicopathological study of 56 cases. Arch Dermatol. 1994;130:1503-1507.
2. King LE, Jr, Dufresne RG, Jr, Lovett GL, et al. Erythroderma: review of 82 cases. South Med J. 1986;79:1210-1215.
3. Byer RL, Bachur RG. Clinical deterioration among patients with fever and erythroderma. Pediatrics. 2006;118:2450-2460.
4. Yuan XY, Guo JY, Dang YP, et al. Erythroderma: a clinical-etiological study of 82 cases. Eur J Dermatol. 2010;20:373-377.
5. Walsh SA, Creamer D. Drug reaction with eosinophilia and systemic symptoms (DRESS): a clinical update and review of current thinking. Clin Exp Dermatol. 2010;36:6-11.
6. Cacoub P, Musette P, Descamps V, et al. The DRESS syndrome: a literature review. Am J Med. 2011;124:588-597.
7. Pickering LK, Baker CJ, Kimberlin DW, et al. eds Red Book: 2009 Report of the Committee on Infectious Diseases. 28th ed. Elk Grove Village, Ill: American Academy of Pediatrics; 2009.
8. Silversides JA, Lappin E, Ferguson AJ. Staphylococcal toxic shock syndrome: mechanisms and management. Curr Infect Dis Rep. 2011;12:392-400.
9. Lappin E, Ferguson AJ. Gram-positive toxic shock syndromes. Lancet Infect Dis. 2009;9:281-290.
10. Sanmarkan AD, Sori T, Thappa DM, et al. Retrospective analysis of Stevens-Johnson syndrome and toxic epidermal necrolysis over a period of 10 years. Indian J Dermatol. 2011;56:25-29.
11. Fritsch PO, Sidoroff A. Drug-induced Stevens-Johnson syndrome/toxic epidermal necrolysis. Am J Clin Dermatol. 2000;1:349-360.
12. Ward KE, Archambault R, Mersfelder TL. Severe adverse skin reactions to nonsteroidal antiinflammatory drugs: a review of the literature. Am J Health Syst Pharm. 2010;67:206-213.
13. Worswick S, Cotliar J. Stevens-Johnson syndrome and toxic epidermal necrolysis: a review of treatment options. Dermatol Ther. 2011;24:207-218.
14. Patel GK, Finlay AY. Staphylococcal scalded skin syndrome: diagnosis and management. Am J Clin Dermatol. 2003;4:165-175.
15. Berk DR, Bayliss SJ. MRSA, staphylococcal scalded skin syndrome, and other cutaneous bacterial emergencies. Pediatr Ann. 2010;39:627-633.
16. Dobson CM, King CM. Adult staphylococcal scalded skin syndrome: histological pitfalls and new diagnostic perspectives. Br J Dermatol. 2003;148:1068-1069.
17. Wang S, Best BM, Burns JC. Periungual desquamation in patients with Kawasaki disease. Pediatr Infect Dis J. 2009;28:538-539.
18. Kawasaki Disease Research Committee. Revision of diagnostic guidelines for Kawasaki disease (the 5th rev ed). Pediatr Int. 2005;47:232-234.
19. Newburger JW, Takahashi M, Gerber MA, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation. 2004;110:2747-2771.
20. Lio PA. The many faces of cellulitis. Arch Dis Child Educ Pract Ed. 2009;94:50-54.
21. Koerner R, Johnson AP. Changes in the classification and management of skin and soft tissue infections. J Antimicrob Chemother. 2010;66:232-234.
22. Botting AM, McIntosh D, Mahadevan M. Paediatric pre- and post-septal periorbital infections are different diseases. A retrospective review of 262 cases. Int J Pediatr Otorhinolaryngol. 2008;72:377-383.
23. Liu IT, Kao SC, Wang AG, et al. Preseptal and orbital cellulitis: a 10-year review of hospitalized patients. J Chin Med Assoc. 2006;69:415-422.
24. Koukouras D, Kallidonis P, Panagoloulos C, et al. Fournier’s gangrene, a urologic and surgical emergency: presentation of a multi-institutional experience with 45 cases. Urol Int. 2011;86:167-172.
25. Mennen U, Howells CJ. Human fight-bite injuries of the hand. A study of 100 cases within 18 months. J Hand Surg Br. 1991;16:431-435.
26. Morgan MS. Diagnosis and management of necrotising fasciitis: a multiparametric approach. J Hosp Infect. 2010;75:249-257.
27. Sarani B, Strong M, Pascual J, et al. Necrotizing fasciitis: current concepts and review of the literature. J Am Coll Surg. 2009;208:279-288.
28. Baker RC, Seguin JH, Leslie N, Gilchrist MJ, Myers MG. Fever and petechiae in children. Pediatrics. 1989;84:1051-1055.
29. Mantadakis E, Farmaki E, Buchanan GR. Thrombocytopenic purpura after measles-mumps-rubella vaccination: a systematic review of the literature and guidance for management. J Pediatr. 2010;156:623-628.
30. Neunert C, Lim W, Crowther M, et al. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood. 2011;117:4190-4207.
31. Blanco R, Martinez-Taboada VM, Rodriguez-Valverde V, et al. Henoch-Schönlein purpura in adulthood and childhood: two different expressions of the same syndrome. Arthritis Rheum. 1997;40:859-864.
32. Choong CK, Beasley SW. Intra-abdominal manifestations of Henoch-Schönlein purpura. J Paediatr Child Health. 1998;34:405-409.
33. Klinkhammer MD, Colletti JE. Pediatric myth: fever and petechiae. CJEM. 2008;10:479-482.
34. Sexton DJ, Kaye KS. Rocky Mountain spotted fever. Med Clin North Am. 2002;86:351-360, vii-viii.
35. Elston DM. Tick bites and skin rashes. Curr Opin Infect Dis. 2010;23:132-138.
36. Milonovich LM. Meningococcemia: epidemiology, pathophysiology, and management. J Pediatr Health Care. 2007;21:75-80.
CORRESPONDENCE Stephen A. Martin, MD, EdM, Barre Family Health Center, 151 Worcester Road, Barre, MA 01005; [email protected]
• Consider starting a course of systemic corticosteroids for a patient with erythroderma, fever, and multiorgan involvement when you strongly suspect a drug reaction is the cause—and have ruled out infection. C
• Suspect Stevens– Johnson syndrome/toxic epidermal necrolysis (SJS/TEN) in a patient with widespread and rapidly progressive desquamation, fever, hypotension, and end-organ involvement. C
• In assessing the severity of skin pain, consider the location; involvement of the eyes, perineum, and hands are associated with greater morbidity. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
The usual approach to dermatologic conditions—honed pattern recognition, a deliberate differential diagnosis, and empiric treatment with longer follow-up—runs counter to the response that dermatologic red flags require. Because patients with signs and symptoms associated with dermatologic emergencies have the potential for rapid clinical deterioration, urgent action is paramount.
With this in mind, we’ve focused on 4 red flags—erythroderma, desquamation, skin pain, and petechiae/purpura—as a starting point, rather than presenting a list of dermatologic emergencies and discussing each diagnosis in turn. The text, tables, and images on the pages that follow will increase your awareness of dermatologic presentations that require an immediate response and help you differentiate between signs and symptoms of serious skin disorders and benign findings that might be described as red flag mimics (TABLE 1).
TABLE 1
Conditions that mimic dermatologic emergencies
| Red skin | |
| Diagnosis | Key discriminating features |
| Allergic contact dermatitis | Itchy, rather than painful |
| Red man syndrome | History of vancomycin infusion |
| Stasis dermatitis | Stasis dermatitis location (lower extremities), pruritus |
| Sunburn | History, sun-exposed areas |
| Desquamation | |
| Diagnosis | Key discriminating features |
| Bullous impetigo | Localized; no systemic manifestations |
| Postinfectious desquamation | Subungual location common; occurs during convalescent phase of illness |
| Petechiae and purpura | |
| Diagnosis | Key discriminating features |
| Local trauma | History and location |
| Pigmented purpuric dermatosis | History and healthy appearance |
| Viral exanthema | Healthy appearance |
Erythroderma: Red skin that’s life-threatening
From an etymological perspective, “erythroderma” simply means red skin. Clinically, however, it is defined as extensive erythema, typically covering ≥90% of the skin surface (FIGURE 1). True erythroderma can be life-threatening and must always be considered a dermatologic emergency.1,2
Diligent monitoring of the speed of progression and the presence of fever, systemic symptoms, and multiorgan dysfunction is essential. In a case review of 56 children who presented to an emergency department with fever and erythroderma, 45% progressed to shock.3 Some common causes of erythroderma are psoriasis; contact, atopic, and seborrheic dermatitis; pityriasis rubra pilaris; cutaneous T-cell lymphoma; drug reaction; and toxic shock syndrome (TSS).4
Is it a drug reaction? Erythroderma, fever, and evidence of multiorgan involvement in a patient taking any medication—not just a new one—prompts consideration of a drug reaction. Antiepileptics, dapsone, and sulfonamides are the most frequent offenders.5
DRESS syndrome (drug reaction with eosinophilia and systemic symptoms) is characterized by fever, lymphadenopathy, elevated liver enzymes, and leukocytosis with eosinophilia, as well as erythroderma. The rash may be urticarial or morbilliform in appearance; petechiae, purpura, and blisters may be present, as well.
Because fever, leukocytosis, and transaminitis are also suggestive of an infectious etiology, DRESS syndrome is frequently overlooked. As a result, its true incidence is unknown. Estimates range from about one in 1000 to one in 10,000 drug exposures.6
In addition to discontinuing the medication, treatment for DRESS calls for systemic corticosteroids—which may actually be harmful when infection, rather than a drug reaction, is the cause. Thus, it is necessary to maintain a high index of suspicion and to thoroughly review the medication history of
any patient who presents with erythroderma and systemic symptoms.
When to suspect toxic shock syndrome. Consider TSS in any patient with erythroderma and hypotension, as well as laboratory evidence of end-organ involvement (including transaminitis, elevated creatinine, anemia, thrombocytopenia, and elevated creatinine kinase). Diagnostic criteria are detailed in FIGURE 2.7 Group A Streptococcus and Staphylococcus aureus are the classic infectious causes, but other bacteria have been implicated, as well. In most cases, the responsible bacterium is not known initially.
Because the toxins produced by these streptococcal and staphylococcal strains act as superantigens that fuel the immune response and worsen the shock, patients with a presumptive diagnosis of TSS should begin empiric treatment with an antimicrobial agent that inhibits toxin synthesis, such as clindamycin, immediately.8,9
FIGURE 1
Erythema covering the chest and arms
This patient was given a diagnosis of erythrodermic psoriasis.
FIGURE 2
Diagnostic criteria for toxic shock syndrome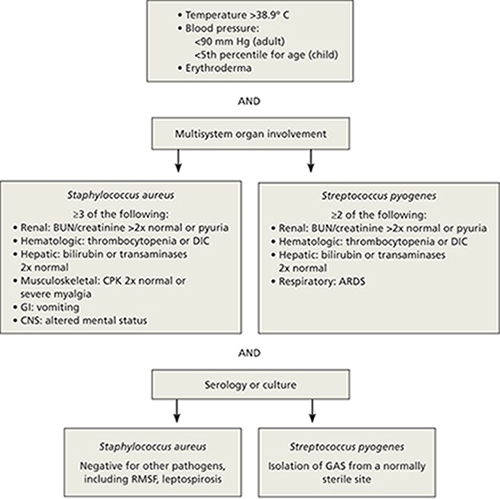
ARDS, acute respiratory distress syndrome; BUN, blood urea nitrogen; CNS, central nervous system; CPK, creatinine phosphokinase; DIC, disseminated intravascular coagulation; GAS, group A Streptococcus; GI, gastrointestinal; RMSF, Rocky Mountain spotted fever.
Adapted from: Pickering LK, et al, eds. Red Book: 2009 Report of the Committee on Infectious Diseases. 2009.7
Desquamation/blistering: Act quickly when it’s widespread
Although desquamation can be seen in benign skin conditions, widespread desquamation with or without bullae requires careful evaluation and a rapid response. Separation, either at the dermal-epidermal junction or intraepidermally, raises the specter of 2 emergent conditions: the Stevens–Johnson syndrome/toxic epidermal necrolysis (SJS/TEN) spectrum and staphylococcal scalded skin syndrome (SSSS). Mucosal involvement is another red flag, if the patient appears ill and the desquamation is progressing rapidly. Conjunctival involvement, in particular, is associated with greater morbidity, and a consult with an ophthalmologist is prude
Rapid progression is a hallmark of SJS/TEN. Desquamation that’s widespread and rapidly progressive in a patient with fever, hypotension, and end-organ involvement is suggestive of SJS/TEN (FIGURE 3). Medications, including allopurinol, antimicrobials, and antiepileptics, are frequent culprits.10,11
Nonsteroidal anti-inflammatory drugs (NSAIDs) have also been linked to SJS/TEN.10 Given their widespread use (1-2 per million users per week), however, the likelihood of NSAIDs leading to SJS/TEN is exceedingly low.12
Signs and symptoms of SJS/TEN may include target lesions with dusky centers, erythroderma, or significant pain without any visible skin abnormality, typically accompanied by fever and malaise. Widespread sloughing of the skin may be seen within several hours.11
Admission to an intensive care unit—preferably a burn unit—is suggested for aggressive fluid resuscitation and management of shock and end-organ dysfunction. Intravenous immunoglobulin G (IVIG) and steroids are often used, although there is little consensus as to the most effective treatment.13 Mortality from TEN approaches 50%.13
SSSS can present at any age. Newborns often present with SSSS during their first week of life: Widespread erythema is quickly followed by fragile blisters, which may have already ruptured by the time the infant receives medical attention. Mucosal surfaces are not typically involved. Nikolsky’s sign (separation of the upper epidermis with gentle pressure) is a classic finding.
Infants with SSSS are frequently irritable, suggesting that the skin may be painful. Cultures from unruptured bullae will be negative as the blisters represent a cutaneous reaction to an infection, rather than a skin infection, but blood, urine, and nasopharynx cultures may be positive. Systemic treatment with nafcillin or oxacillin should be initiated, and supportive skin care provided.14,15 Clindamycin or vancomycin should be used in parts of the country in which methicillin-resistant Staphylococcus aureus is prevalent. In very young infants, the outcome of SSSS is generally favorable. Not so with adults.
Because mature kidneys have a greater ability to excrete exfoliative toxins, SSSS primarily affects adults with significant comorbidities—and has a much poorer prognosis.16 You may also see chronic autoimmune bullous diseases, such as bullous pemphigoid and pemphigus vulgaris, with widespread desquamation and blistering, in the adult population. Untreated, the secondary infection and electrolyte disturbances from fluid loss associated with pemphigus vulgaris can be fatal.
Desquamation is a late finding in Kawasaki disease. Desquamation is often cited as a potential skin finding in children with Kawasaki disease (KD) (FIGURE 4), but usually not until the convalescent stage.17 (Desquamation may also appear during the recovery period of several other infections, including scarlet fever and TSS.) IVIG can prevent coronary aneurysm, the major complication of KD, but only if it is administered during the acute phase of the illness. Therefore, early diagnosis of KD (TABLE 2)18—before desquamation occurs—is critical.19
FIGURE 3
Desquamation, full-thickness epidermal necrosis on the upper back
Erythroderma and widespread denudation on the upper back of a patient who was given a diagnosis of toxic epidermal necrolysis.
FIGURE 4
Desquamation on a young patient
Desquamation associated with Kawasaki disease (shown on the hand of a child) usually occurs during the convalescent stage.
TABLE 2
Diagnostic criteria for Kawasaki disease
| Fever for ≥5 days, and 4 out of 5 criteria (required): |
|---|
|
| Supporting findings: |
|
| CRP, C-reactive protein; ESR, erythrocyte sedimentation rate. Source: Kawasaki Disease Research Committee. Pediatr Int. 2005.18 |
Skin pain is always a red flag
Widespread skin pain should always be taken seriously, as it is rarely associated with minor dermatoses.20 Infectious cellulitis is the most likely diagnosis of a painful erythematous skin lesion. Patients with cellulitis do not usually have erythroderma, as the affected area tends to be very localized.
Cellulitis may be over- or undertreated. Once cellulitis has been diagnosed, the next thing to consider is severity. A recent retrospective study found that misclassification of skin and soft-tissue infections may result in both significant overtreatment of mild soft-tissue infections and dangerous undertreatment of severe infections, with consequent morbidity.21
Location is a key consideration, as cellulitis in certain locations—including the eye, perineum, and hand—carries an increased risk of morbidity. Orbital cellulitis—which may be characterized by proptosis, ophthalmoplegia, and pain with extraocular movements—most often results from initial sinusitis, and can lead to vision loss, intracranial infection, and significant invasive disease. Prompt antimicrobial therapy and urgent ophthalmologic consultation are essential, as operative drainage may be required.22,23
When the perineum is involved, a careful exam must be performed to determine the limits of the affected area. Although Fournier’s gangrene is uncommon, it is a life-threatening infection. In one small retrospective study, more than half of the patients presented with a perianal abscess.24
Similarly, the hand is vulnerable to significant infection, particularly if it is inoculated with bacteria from human mouth flora (the well-described “fight bite”). In a review of 100 cases of human fight bites, 18 patients ultimately required amputation.25
Early necrotizing fasciitis is often missed. Clinicians generally expect painful lesions to also have erythema, swelling, and increased warmth—the cardinal signs of inflammation. As a result, early necrotizing fasciitis, which initially presents with pain out of proportion to other dermatologic findings, may be overlooked. In fact, pain can precede significant skin findings by 24 to 48 hours; prior to that, only mild erythema or swelling (with minimal pain, in some cases) may be evident.26,27
The general pattern, however, is for a site with exquisite tenderness to evolve into a smooth, swollen area, then to develop dusky plaques and late-stage full thickness necrosis with hemorrhagic bullae.26 At that point, necrosis can render the skin insensate. Case reviews have found necrotizing fasciitis to be protean, with only 3 findings—erythema, edema, and tenderness beyond the expected lesion borders—present in most patients.27 Assiduous attention to skin pain in the presence of any other skin manifestation is the key to early diagnosis and rapid treatment.
Petechiae/purpura may be severe or benign
Petechiae are flat, pinpoint, nonblanching spots caused by intradermal hemorrhage associated with a wide variety of conditions, ranging from benign (local trauma) to severe (eg, disseminated intravascular coagulation [DIC] and sepsis). Similarly, purpura—larger lesions that may be palpable—can accompany less severe diseases, such as Henoch-Schönlein purpura (HSP), or life-threatening conditions like sepsis and DIC (FIGURE 5). Here, as in many other dermatologic conditions, the key differentiating features are location (local vs diffuse), speed of progression, and signs and symptoms of systemic illness.
FIGURE 5
Signs of a life-threatening condition
Hemorrhagic bullae with surrounding erythema on the lateral thigh of a patient with purpura fulminans from bacterial sepsis.
Localized petechiae are common with direct trauma, as well as barotrauma associated with coughing, vomiting, or even asphyxiation. Location is an important clue. Periorbital petechiae and petechiae on the chest above the nipple line suggest that the lesions were caused by the force of the barotrauma, rather than systemic disease.28 A careful history and physical exam are needed to rule out serious underlying conditions, such as pneumonia, dehydration, and abdominal obstruction.
Petechiae out of proportion to the force applied may be an indication of an underlying bleeding diathesis, including thrombocytopenia, coagulation defects, and some fulminant infections. Idiopathic thrombocytopenic purpura (ITP) and HSP may present with more widespread petechiae/purpura, but without fever or systemic symptoms. ITP can develop spontaneously, after a viral infection or after a child’s inoculation with the measles-mumps-rubella vaccine.29 ITP typically presents as easy bruising and petechiae out of proportion to the condition that caused it. These patients, as a rule, will have a healthy appearance.
Treatment (with steroids, IVIG, or anti-D immunoglobulin) is generally not required for children with ITP unless they have bleeding that is mucosal or substantial, as spontaneous remission is expected. Adults, who are more likely to develop chronic ITP, may benefit from treatment.30
HSP occurs most commonly in children, who may have palpable purpura, typically in the lower extremities, as well as arthritis or arthralgia, abdominal pain, and renal involvement that can progress from microscopic hematuria or proteinuria to renal insufficiency.31 Typically, children whose disease is in the acute phase do not appear to be sick, with an important exception: Those who develop hemorrhage and edema in the bowel wall, resulting in intussusception, have significant abdominal pain and are more likely to need surgical reduction.32
Diffuse petechiae in the absence of any trauma, accompanied by significant signs of systemic illness, may be an indication of fulminant infection, including meningococcemia, DIC, and Rocky Mountain spotted fever (RMSF). (Fever and diffuse petechiae can also be seen in viral exanthema, but patients usually look well and the rash often has both blanching and petechial components.33)
When a returning traveler presents with a rash and systemic symptoms, it is important to take a thorough history and to consider infections endemic to the area visited. RMSF may initially be localized to the wrists and progress to widespread petechiae over hours to days. Because the cutaneous findings may not be as fulminant—and up to 10% of patients with RMSF have no rash at all34—attention to the noncutaneous features is important. Fever, headache, neurologic symptoms, joint complaints, and abdominal pain (or only a few of these manifestations) in the context of potential tick bite exposure should prompt consideration of RMSF.35
Keep in mind, too, that in cases of fulminant infections such as meningococcemia and DIC, the hallmark purpura fulminans may not be present initially.36 Although the initial cutaneous findings may be subtle, however, such patients will appear quite ill, and their condition will deteriorate rapidly. Because prompt antibiotic therapy can save life and limb, a high index of suspicion should be maintained for any patient who presents with a rash in the setting of fever and hypotension or other evidence of shock.
• Consider starting a course of systemic corticosteroids for a patient with erythroderma, fever, and multiorgan involvement when you strongly suspect a drug reaction is the cause—and have ruled out infection. C
• Suspect Stevens– Johnson syndrome/toxic epidermal necrolysis (SJS/TEN) in a patient with widespread and rapidly progressive desquamation, fever, hypotension, and end-organ involvement. C
• In assessing the severity of skin pain, consider the location; involvement of the eyes, perineum, and hands are associated with greater morbidity. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
The usual approach to dermatologic conditions—honed pattern recognition, a deliberate differential diagnosis, and empiric treatment with longer follow-up—runs counter to the response that dermatologic red flags require. Because patients with signs and symptoms associated with dermatologic emergencies have the potential for rapid clinical deterioration, urgent action is paramount.
With this in mind, we’ve focused on 4 red flags—erythroderma, desquamation, skin pain, and petechiae/purpura—as a starting point, rather than presenting a list of dermatologic emergencies and discussing each diagnosis in turn. The text, tables, and images on the pages that follow will increase your awareness of dermatologic presentations that require an immediate response and help you differentiate between signs and symptoms of serious skin disorders and benign findings that might be described as red flag mimics (TABLE 1).
TABLE 1
Conditions that mimic dermatologic emergencies
| Red skin | |
| Diagnosis | Key discriminating features |
| Allergic contact dermatitis | Itchy, rather than painful |
| Red man syndrome | History of vancomycin infusion |
| Stasis dermatitis | Stasis dermatitis location (lower extremities), pruritus |
| Sunburn | History, sun-exposed areas |
| Desquamation | |
| Diagnosis | Key discriminating features |
| Bullous impetigo | Localized; no systemic manifestations |
| Postinfectious desquamation | Subungual location common; occurs during convalescent phase of illness |
| Petechiae and purpura | |
| Diagnosis | Key discriminating features |
| Local trauma | History and location |
| Pigmented purpuric dermatosis | History and healthy appearance |
| Viral exanthema | Healthy appearance |
Erythroderma: Red skin that’s life-threatening
From an etymological perspective, “erythroderma” simply means red skin. Clinically, however, it is defined as extensive erythema, typically covering ≥90% of the skin surface (FIGURE 1). True erythroderma can be life-threatening and must always be considered a dermatologic emergency.1,2
Diligent monitoring of the speed of progression and the presence of fever, systemic symptoms, and multiorgan dysfunction is essential. In a case review of 56 children who presented to an emergency department with fever and erythroderma, 45% progressed to shock.3 Some common causes of erythroderma are psoriasis; contact, atopic, and seborrheic dermatitis; pityriasis rubra pilaris; cutaneous T-cell lymphoma; drug reaction; and toxic shock syndrome (TSS).4
Is it a drug reaction? Erythroderma, fever, and evidence of multiorgan involvement in a patient taking any medication—not just a new one—prompts consideration of a drug reaction. Antiepileptics, dapsone, and sulfonamides are the most frequent offenders.5
DRESS syndrome (drug reaction with eosinophilia and systemic symptoms) is characterized by fever, lymphadenopathy, elevated liver enzymes, and leukocytosis with eosinophilia, as well as erythroderma. The rash may be urticarial or morbilliform in appearance; petechiae, purpura, and blisters may be present, as well.
Because fever, leukocytosis, and transaminitis are also suggestive of an infectious etiology, DRESS syndrome is frequently overlooked. As a result, its true incidence is unknown. Estimates range from about one in 1000 to one in 10,000 drug exposures.6
In addition to discontinuing the medication, treatment for DRESS calls for systemic corticosteroids—which may actually be harmful when infection, rather than a drug reaction, is the cause. Thus, it is necessary to maintain a high index of suspicion and to thoroughly review the medication history of
any patient who presents with erythroderma and systemic symptoms.
When to suspect toxic shock syndrome. Consider TSS in any patient with erythroderma and hypotension, as well as laboratory evidence of end-organ involvement (including transaminitis, elevated creatinine, anemia, thrombocytopenia, and elevated creatinine kinase). Diagnostic criteria are detailed in FIGURE 2.7 Group A Streptococcus and Staphylococcus aureus are the classic infectious causes, but other bacteria have been implicated, as well. In most cases, the responsible bacterium is not known initially.
Because the toxins produced by these streptococcal and staphylococcal strains act as superantigens that fuel the immune response and worsen the shock, patients with a presumptive diagnosis of TSS should begin empiric treatment with an antimicrobial agent that inhibits toxin synthesis, such as clindamycin, immediately.8,9
FIGURE 1
Erythema covering the chest and arms
This patient was given a diagnosis of erythrodermic psoriasis.
FIGURE 2
Diagnostic criteria for toxic shock syndrome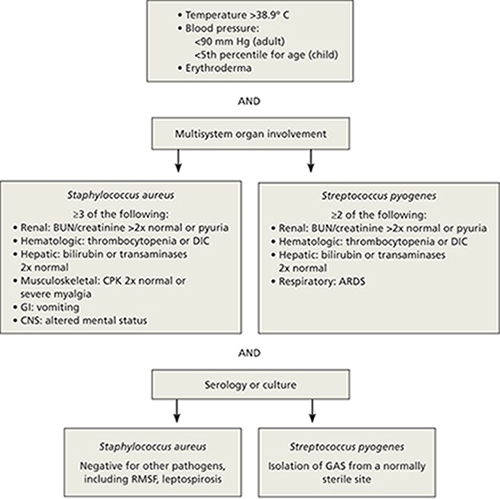
ARDS, acute respiratory distress syndrome; BUN, blood urea nitrogen; CNS, central nervous system; CPK, creatinine phosphokinase; DIC, disseminated intravascular coagulation; GAS, group A Streptococcus; GI, gastrointestinal; RMSF, Rocky Mountain spotted fever.
Adapted from: Pickering LK, et al, eds. Red Book: 2009 Report of the Committee on Infectious Diseases. 2009.7
Desquamation/blistering: Act quickly when it’s widespread
Although desquamation can be seen in benign skin conditions, widespread desquamation with or without bullae requires careful evaluation and a rapid response. Separation, either at the dermal-epidermal junction or intraepidermally, raises the specter of 2 emergent conditions: the Stevens–Johnson syndrome/toxic epidermal necrolysis (SJS/TEN) spectrum and staphylococcal scalded skin syndrome (SSSS). Mucosal involvement is another red flag, if the patient appears ill and the desquamation is progressing rapidly. Conjunctival involvement, in particular, is associated with greater morbidity, and a consult with an ophthalmologist is prude
Rapid progression is a hallmark of SJS/TEN. Desquamation that’s widespread and rapidly progressive in a patient with fever, hypotension, and end-organ involvement is suggestive of SJS/TEN (FIGURE 3). Medications, including allopurinol, antimicrobials, and antiepileptics, are frequent culprits.10,11
Nonsteroidal anti-inflammatory drugs (NSAIDs) have also been linked to SJS/TEN.10 Given their widespread use (1-2 per million users per week), however, the likelihood of NSAIDs leading to SJS/TEN is exceedingly low.12
Signs and symptoms of SJS/TEN may include target lesions with dusky centers, erythroderma, or significant pain without any visible skin abnormality, typically accompanied by fever and malaise. Widespread sloughing of the skin may be seen within several hours.11
Admission to an intensive care unit—preferably a burn unit—is suggested for aggressive fluid resuscitation and management of shock and end-organ dysfunction. Intravenous immunoglobulin G (IVIG) and steroids are often used, although there is little consensus as to the most effective treatment.13 Mortality from TEN approaches 50%.13
SSSS can present at any age. Newborns often present with SSSS during their first week of life: Widespread erythema is quickly followed by fragile blisters, which may have already ruptured by the time the infant receives medical attention. Mucosal surfaces are not typically involved. Nikolsky’s sign (separation of the upper epidermis with gentle pressure) is a classic finding.
Infants with SSSS are frequently irritable, suggesting that the skin may be painful. Cultures from unruptured bullae will be negative as the blisters represent a cutaneous reaction to an infection, rather than a skin infection, but blood, urine, and nasopharynx cultures may be positive. Systemic treatment with nafcillin or oxacillin should be initiated, and supportive skin care provided.14,15 Clindamycin or vancomycin should be used in parts of the country in which methicillin-resistant Staphylococcus aureus is prevalent. In very young infants, the outcome of SSSS is generally favorable. Not so with adults.
Because mature kidneys have a greater ability to excrete exfoliative toxins, SSSS primarily affects adults with significant comorbidities—and has a much poorer prognosis.16 You may also see chronic autoimmune bullous diseases, such as bullous pemphigoid and pemphigus vulgaris, with widespread desquamation and blistering, in the adult population. Untreated, the secondary infection and electrolyte disturbances from fluid loss associated with pemphigus vulgaris can be fatal.
Desquamation is a late finding in Kawasaki disease. Desquamation is often cited as a potential skin finding in children with Kawasaki disease (KD) (FIGURE 4), but usually not until the convalescent stage.17 (Desquamation may also appear during the recovery period of several other infections, including scarlet fever and TSS.) IVIG can prevent coronary aneurysm, the major complication of KD, but only if it is administered during the acute phase of the illness. Therefore, early diagnosis of KD (TABLE 2)18—before desquamation occurs—is critical.19
FIGURE 3
Desquamation, full-thickness epidermal necrosis on the upper back
Erythroderma and widespread denudation on the upper back of a patient who was given a diagnosis of toxic epidermal necrolysis.
FIGURE 4
Desquamation on a young patient
Desquamation associated with Kawasaki disease (shown on the hand of a child) usually occurs during the convalescent stage.
TABLE 2
Diagnostic criteria for Kawasaki disease
| Fever for ≥5 days, and 4 out of 5 criteria (required): |
|---|
|
| Supporting findings: |
|
| CRP, C-reactive protein; ESR, erythrocyte sedimentation rate. Source: Kawasaki Disease Research Committee. Pediatr Int. 2005.18 |
Skin pain is always a red flag
Widespread skin pain should always be taken seriously, as it is rarely associated with minor dermatoses.20 Infectious cellulitis is the most likely diagnosis of a painful erythematous skin lesion. Patients with cellulitis do not usually have erythroderma, as the affected area tends to be very localized.
Cellulitis may be over- or undertreated. Once cellulitis has been diagnosed, the next thing to consider is severity. A recent retrospective study found that misclassification of skin and soft-tissue infections may result in both significant overtreatment of mild soft-tissue infections and dangerous undertreatment of severe infections, with consequent morbidity.21
Location is a key consideration, as cellulitis in certain locations—including the eye, perineum, and hand—carries an increased risk of morbidity. Orbital cellulitis—which may be characterized by proptosis, ophthalmoplegia, and pain with extraocular movements—most often results from initial sinusitis, and can lead to vision loss, intracranial infection, and significant invasive disease. Prompt antimicrobial therapy and urgent ophthalmologic consultation are essential, as operative drainage may be required.22,23
When the perineum is involved, a careful exam must be performed to determine the limits of the affected area. Although Fournier’s gangrene is uncommon, it is a life-threatening infection. In one small retrospective study, more than half of the patients presented with a perianal abscess.24
Similarly, the hand is vulnerable to significant infection, particularly if it is inoculated with bacteria from human mouth flora (the well-described “fight bite”). In a review of 100 cases of human fight bites, 18 patients ultimately required amputation.25
Early necrotizing fasciitis is often missed. Clinicians generally expect painful lesions to also have erythema, swelling, and increased warmth—the cardinal signs of inflammation. As a result, early necrotizing fasciitis, which initially presents with pain out of proportion to other dermatologic findings, may be overlooked. In fact, pain can precede significant skin findings by 24 to 48 hours; prior to that, only mild erythema or swelling (with minimal pain, in some cases) may be evident.26,27
The general pattern, however, is for a site with exquisite tenderness to evolve into a smooth, swollen area, then to develop dusky plaques and late-stage full thickness necrosis with hemorrhagic bullae.26 At that point, necrosis can render the skin insensate. Case reviews have found necrotizing fasciitis to be protean, with only 3 findings—erythema, edema, and tenderness beyond the expected lesion borders—present in most patients.27 Assiduous attention to skin pain in the presence of any other skin manifestation is the key to early diagnosis and rapid treatment.
Petechiae/purpura may be severe or benign
Petechiae are flat, pinpoint, nonblanching spots caused by intradermal hemorrhage associated with a wide variety of conditions, ranging from benign (local trauma) to severe (eg, disseminated intravascular coagulation [DIC] and sepsis). Similarly, purpura—larger lesions that may be palpable—can accompany less severe diseases, such as Henoch-Schönlein purpura (HSP), or life-threatening conditions like sepsis and DIC (FIGURE 5). Here, as in many other dermatologic conditions, the key differentiating features are location (local vs diffuse), speed of progression, and signs and symptoms of systemic illness.
FIGURE 5
Signs of a life-threatening condition
Hemorrhagic bullae with surrounding erythema on the lateral thigh of a patient with purpura fulminans from bacterial sepsis.
Localized petechiae are common with direct trauma, as well as barotrauma associated with coughing, vomiting, or even asphyxiation. Location is an important clue. Periorbital petechiae and petechiae on the chest above the nipple line suggest that the lesions were caused by the force of the barotrauma, rather than systemic disease.28 A careful history and physical exam are needed to rule out serious underlying conditions, such as pneumonia, dehydration, and abdominal obstruction.
Petechiae out of proportion to the force applied may be an indication of an underlying bleeding diathesis, including thrombocytopenia, coagulation defects, and some fulminant infections. Idiopathic thrombocytopenic purpura (ITP) and HSP may present with more widespread petechiae/purpura, but without fever or systemic symptoms. ITP can develop spontaneously, after a viral infection or after a child’s inoculation with the measles-mumps-rubella vaccine.29 ITP typically presents as easy bruising and petechiae out of proportion to the condition that caused it. These patients, as a rule, will have a healthy appearance.
Treatment (with steroids, IVIG, or anti-D immunoglobulin) is generally not required for children with ITP unless they have bleeding that is mucosal or substantial, as spontaneous remission is expected. Adults, who are more likely to develop chronic ITP, may benefit from treatment.30
HSP occurs most commonly in children, who may have palpable purpura, typically in the lower extremities, as well as arthritis or arthralgia, abdominal pain, and renal involvement that can progress from microscopic hematuria or proteinuria to renal insufficiency.31 Typically, children whose disease is in the acute phase do not appear to be sick, with an important exception: Those who develop hemorrhage and edema in the bowel wall, resulting in intussusception, have significant abdominal pain and are more likely to need surgical reduction.32
Diffuse petechiae in the absence of any trauma, accompanied by significant signs of systemic illness, may be an indication of fulminant infection, including meningococcemia, DIC, and Rocky Mountain spotted fever (RMSF). (Fever and diffuse petechiae can also be seen in viral exanthema, but patients usually look well and the rash often has both blanching and petechial components.33)
When a returning traveler presents with a rash and systemic symptoms, it is important to take a thorough history and to consider infections endemic to the area visited. RMSF may initially be localized to the wrists and progress to widespread petechiae over hours to days. Because the cutaneous findings may not be as fulminant—and up to 10% of patients with RMSF have no rash at all34—attention to the noncutaneous features is important. Fever, headache, neurologic symptoms, joint complaints, and abdominal pain (or only a few of these manifestations) in the context of potential tick bite exposure should prompt consideration of RMSF.35
Keep in mind, too, that in cases of fulminant infections such as meningococcemia and DIC, the hallmark purpura fulminans may not be present initially.36 Although the initial cutaneous findings may be subtle, however, such patients will appear quite ill, and their condition will deteriorate rapidly. Because prompt antibiotic therapy can save life and limb, a high index of suspicion should be maintained for any patient who presents with a rash in the setting of fever and hypotension or other evidence of shock.
1. Botella-Estrada R, Sanmartin O, Oliver V, et al. Erythroderma. A clinicopathological study of 56 cases. Arch Dermatol. 1994;130:1503-1507.
2. King LE, Jr, Dufresne RG, Jr, Lovett GL, et al. Erythroderma: review of 82 cases. South Med J. 1986;79:1210-1215.
3. Byer RL, Bachur RG. Clinical deterioration among patients with fever and erythroderma. Pediatrics. 2006;118:2450-2460.
4. Yuan XY, Guo JY, Dang YP, et al. Erythroderma: a clinical-etiological study of 82 cases. Eur J Dermatol. 2010;20:373-377.
5. Walsh SA, Creamer D. Drug reaction with eosinophilia and systemic symptoms (DRESS): a clinical update and review of current thinking. Clin Exp Dermatol. 2010;36:6-11.
6. Cacoub P, Musette P, Descamps V, et al. The DRESS syndrome: a literature review. Am J Med. 2011;124:588-597.
7. Pickering LK, Baker CJ, Kimberlin DW, et al. eds Red Book: 2009 Report of the Committee on Infectious Diseases. 28th ed. Elk Grove Village, Ill: American Academy of Pediatrics; 2009.
8. Silversides JA, Lappin E, Ferguson AJ. Staphylococcal toxic shock syndrome: mechanisms and management. Curr Infect Dis Rep. 2011;12:392-400.
9. Lappin E, Ferguson AJ. Gram-positive toxic shock syndromes. Lancet Infect Dis. 2009;9:281-290.
10. Sanmarkan AD, Sori T, Thappa DM, et al. Retrospective analysis of Stevens-Johnson syndrome and toxic epidermal necrolysis over a period of 10 years. Indian J Dermatol. 2011;56:25-29.
11. Fritsch PO, Sidoroff A. Drug-induced Stevens-Johnson syndrome/toxic epidermal necrolysis. Am J Clin Dermatol. 2000;1:349-360.
12. Ward KE, Archambault R, Mersfelder TL. Severe adverse skin reactions to nonsteroidal antiinflammatory drugs: a review of the literature. Am J Health Syst Pharm. 2010;67:206-213.
13. Worswick S, Cotliar J. Stevens-Johnson syndrome and toxic epidermal necrolysis: a review of treatment options. Dermatol Ther. 2011;24:207-218.
14. Patel GK, Finlay AY. Staphylococcal scalded skin syndrome: diagnosis and management. Am J Clin Dermatol. 2003;4:165-175.
15. Berk DR, Bayliss SJ. MRSA, staphylococcal scalded skin syndrome, and other cutaneous bacterial emergencies. Pediatr Ann. 2010;39:627-633.
16. Dobson CM, King CM. Adult staphylococcal scalded skin syndrome: histological pitfalls and new diagnostic perspectives. Br J Dermatol. 2003;148:1068-1069.
17. Wang S, Best BM, Burns JC. Periungual desquamation in patients with Kawasaki disease. Pediatr Infect Dis J. 2009;28:538-539.
18. Kawasaki Disease Research Committee. Revision of diagnostic guidelines for Kawasaki disease (the 5th rev ed). Pediatr Int. 2005;47:232-234.
19. Newburger JW, Takahashi M, Gerber MA, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation. 2004;110:2747-2771.
20. Lio PA. The many faces of cellulitis. Arch Dis Child Educ Pract Ed. 2009;94:50-54.
21. Koerner R, Johnson AP. Changes in the classification and management of skin and soft tissue infections. J Antimicrob Chemother. 2010;66:232-234.
22. Botting AM, McIntosh D, Mahadevan M. Paediatric pre- and post-septal periorbital infections are different diseases. A retrospective review of 262 cases. Int J Pediatr Otorhinolaryngol. 2008;72:377-383.
23. Liu IT, Kao SC, Wang AG, et al. Preseptal and orbital cellulitis: a 10-year review of hospitalized patients. J Chin Med Assoc. 2006;69:415-422.
24. Koukouras D, Kallidonis P, Panagoloulos C, et al. Fournier’s gangrene, a urologic and surgical emergency: presentation of a multi-institutional experience with 45 cases. Urol Int. 2011;86:167-172.
25. Mennen U, Howells CJ. Human fight-bite injuries of the hand. A study of 100 cases within 18 months. J Hand Surg Br. 1991;16:431-435.
26. Morgan MS. Diagnosis and management of necrotising fasciitis: a multiparametric approach. J Hosp Infect. 2010;75:249-257.
27. Sarani B, Strong M, Pascual J, et al. Necrotizing fasciitis: current concepts and review of the literature. J Am Coll Surg. 2009;208:279-288.
28. Baker RC, Seguin JH, Leslie N, Gilchrist MJ, Myers MG. Fever and petechiae in children. Pediatrics. 1989;84:1051-1055.
29. Mantadakis E, Farmaki E, Buchanan GR. Thrombocytopenic purpura after measles-mumps-rubella vaccination: a systematic review of the literature and guidance for management. J Pediatr. 2010;156:623-628.
30. Neunert C, Lim W, Crowther M, et al. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood. 2011;117:4190-4207.
31. Blanco R, Martinez-Taboada VM, Rodriguez-Valverde V, et al. Henoch-Schönlein purpura in adulthood and childhood: two different expressions of the same syndrome. Arthritis Rheum. 1997;40:859-864.
32. Choong CK, Beasley SW. Intra-abdominal manifestations of Henoch-Schönlein purpura. J Paediatr Child Health. 1998;34:405-409.
33. Klinkhammer MD, Colletti JE. Pediatric myth: fever and petechiae. CJEM. 2008;10:479-482.
34. Sexton DJ, Kaye KS. Rocky Mountain spotted fever. Med Clin North Am. 2002;86:351-360, vii-viii.
35. Elston DM. Tick bites and skin rashes. Curr Opin Infect Dis. 2010;23:132-138.
36. Milonovich LM. Meningococcemia: epidemiology, pathophysiology, and management. J Pediatr Health Care. 2007;21:75-80.
CORRESPONDENCE Stephen A. Martin, MD, EdM, Barre Family Health Center, 151 Worcester Road, Barre, MA 01005; [email protected]
1. Botella-Estrada R, Sanmartin O, Oliver V, et al. Erythroderma. A clinicopathological study of 56 cases. Arch Dermatol. 1994;130:1503-1507.
2. King LE, Jr, Dufresne RG, Jr, Lovett GL, et al. Erythroderma: review of 82 cases. South Med J. 1986;79:1210-1215.
3. Byer RL, Bachur RG. Clinical deterioration among patients with fever and erythroderma. Pediatrics. 2006;118:2450-2460.
4. Yuan XY, Guo JY, Dang YP, et al. Erythroderma: a clinical-etiological study of 82 cases. Eur J Dermatol. 2010;20:373-377.
5. Walsh SA, Creamer D. Drug reaction with eosinophilia and systemic symptoms (DRESS): a clinical update and review of current thinking. Clin Exp Dermatol. 2010;36:6-11.
6. Cacoub P, Musette P, Descamps V, et al. The DRESS syndrome: a literature review. Am J Med. 2011;124:588-597.
7. Pickering LK, Baker CJ, Kimberlin DW, et al. eds Red Book: 2009 Report of the Committee on Infectious Diseases. 28th ed. Elk Grove Village, Ill: American Academy of Pediatrics; 2009.
8. Silversides JA, Lappin E, Ferguson AJ. Staphylococcal toxic shock syndrome: mechanisms and management. Curr Infect Dis Rep. 2011;12:392-400.
9. Lappin E, Ferguson AJ. Gram-positive toxic shock syndromes. Lancet Infect Dis. 2009;9:281-290.
10. Sanmarkan AD, Sori T, Thappa DM, et al. Retrospective analysis of Stevens-Johnson syndrome and toxic epidermal necrolysis over a period of 10 years. Indian J Dermatol. 2011;56:25-29.
11. Fritsch PO, Sidoroff A. Drug-induced Stevens-Johnson syndrome/toxic epidermal necrolysis. Am J Clin Dermatol. 2000;1:349-360.
12. Ward KE, Archambault R, Mersfelder TL. Severe adverse skin reactions to nonsteroidal antiinflammatory drugs: a review of the literature. Am J Health Syst Pharm. 2010;67:206-213.
13. Worswick S, Cotliar J. Stevens-Johnson syndrome and toxic epidermal necrolysis: a review of treatment options. Dermatol Ther. 2011;24:207-218.
14. Patel GK, Finlay AY. Staphylococcal scalded skin syndrome: diagnosis and management. Am J Clin Dermatol. 2003;4:165-175.
15. Berk DR, Bayliss SJ. MRSA, staphylococcal scalded skin syndrome, and other cutaneous bacterial emergencies. Pediatr Ann. 2010;39:627-633.
16. Dobson CM, King CM. Adult staphylococcal scalded skin syndrome: histological pitfalls and new diagnostic perspectives. Br J Dermatol. 2003;148:1068-1069.
17. Wang S, Best BM, Burns JC. Periungual desquamation in patients with Kawasaki disease. Pediatr Infect Dis J. 2009;28:538-539.
18. Kawasaki Disease Research Committee. Revision of diagnostic guidelines for Kawasaki disease (the 5th rev ed). Pediatr Int. 2005;47:232-234.
19. Newburger JW, Takahashi M, Gerber MA, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation. 2004;110:2747-2771.
20. Lio PA. The many faces of cellulitis. Arch Dis Child Educ Pract Ed. 2009;94:50-54.
21. Koerner R, Johnson AP. Changes in the classification and management of skin and soft tissue infections. J Antimicrob Chemother. 2010;66:232-234.
22. Botting AM, McIntosh D, Mahadevan M. Paediatric pre- and post-septal periorbital infections are different diseases. A retrospective review of 262 cases. Int J Pediatr Otorhinolaryngol. 2008;72:377-383.
23. Liu IT, Kao SC, Wang AG, et al. Preseptal and orbital cellulitis: a 10-year review of hospitalized patients. J Chin Med Assoc. 2006;69:415-422.
24. Koukouras D, Kallidonis P, Panagoloulos C, et al. Fournier’s gangrene, a urologic and surgical emergency: presentation of a multi-institutional experience with 45 cases. Urol Int. 2011;86:167-172.
25. Mennen U, Howells CJ. Human fight-bite injuries of the hand. A study of 100 cases within 18 months. J Hand Surg Br. 1991;16:431-435.
26. Morgan MS. Diagnosis and management of necrotising fasciitis: a multiparametric approach. J Hosp Infect. 2010;75:249-257.
27. Sarani B, Strong M, Pascual J, et al. Necrotizing fasciitis: current concepts and review of the literature. J Am Coll Surg. 2009;208:279-288.
28. Baker RC, Seguin JH, Leslie N, Gilchrist MJ, Myers MG. Fever and petechiae in children. Pediatrics. 1989;84:1051-1055.
29. Mantadakis E, Farmaki E, Buchanan GR. Thrombocytopenic purpura after measles-mumps-rubella vaccination: a systematic review of the literature and guidance for management. J Pediatr. 2010;156:623-628.
30. Neunert C, Lim W, Crowther M, et al. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood. 2011;117:4190-4207.
31. Blanco R, Martinez-Taboada VM, Rodriguez-Valverde V, et al. Henoch-Schönlein purpura in adulthood and childhood: two different expressions of the same syndrome. Arthritis Rheum. 1997;40:859-864.
32. Choong CK, Beasley SW. Intra-abdominal manifestations of Henoch-Schönlein purpura. J Paediatr Child Health. 1998;34:405-409.
33. Klinkhammer MD, Colletti JE. Pediatric myth: fever and petechiae. CJEM. 2008;10:479-482.
34. Sexton DJ, Kaye KS. Rocky Mountain spotted fever. Med Clin North Am. 2002;86:351-360, vii-viii.
35. Elston DM. Tick bites and skin rashes. Curr Opin Infect Dis. 2010;23:132-138.
36. Milonovich LM. Meningococcemia: epidemiology, pathophysiology, and management. J Pediatr Health Care. 2007;21:75-80.
CORRESPONDENCE Stephen A. Martin, MD, EdM, Barre Family Health Center, 151 Worcester Road, Barre, MA 01005; [email protected]





