User login
Don’t forget liver disease often has mental health component
PHILADELPHIA – To help ensure the best outcomes in patients with a range of liver pathologies, be alert for signs of neurologic and psychiatric abnormalities caused by hepatic encephalopathy, according to an expert.
“The patient doesn’t have to have cirrhosis or liver disease, but can just have portosystemic shunting with absolutely no liver disease, and still have hepatic encephalopathy,” Dr. Jasmohan S. Bajaj said at the meeting held by Global Academy for Medical Education and Rutgers, the State University of New Jersey.
Hepatic encephalopathy is believed to be due to dysbiosis caused by an altered bile acid profile, leading to an impaired intestinal barrier, which allows high levels of ammonia to circulate through the bloodstream, contributing to systemic inflammation and brain dysfunction, according to Dr. Bajaj, an associate professor of medicine at Virginia Commonwealth University and McGuire VA Medical Center, Richmond, Va.
“Ultimately, all the manifestations that we see are because of neuronal dysfunction, which is why the patient is depressed, anxious, sleepy, and has tremors,” Dr. Bajaj said.
Guidelines issued by the American Association for the Study of Liver Diseases stratify hepatic encephalopathy into four grades, the first being the difficult-to-detect subclinical form that is present in up at as many as 60% of patients with hepatic pathologies.
Because covert hepatic encephalopathy will likely progress to a more overt form, adversely impacting a patient’s quality of life and other outcomes, Dr. Bajaj emphasized the importance of testing for it.
One means of detection is to evaluate a patient’s response time using a modified version of the psychiatric Stroop test that measures cognitive dysfunction. Another is to consider collaborative care with a psychologist who can test for and diagnose cognitive impairment. Patients who select at least four items in the Sickness Impact Profile are “80% likely” to have covert hepatic encephalopathy, according to Dr. Bajaj.
Overt manifestations of hepatic encephalopathy include obvious signs of altered mental status, usually reported by the caregiver. Clinicians should consider as part of their differential diagnosis for overt hepatic encephalopathy whether the patient is diabetic, intoxicated, suffering an electrolyte disorder, or is experiencing intracranial bleeding or stroke, and should consider precipitating factors such as an infection, gastrointestinal bleeding, or an overdose of diuretics.
Avoid treatment decisions based on blood ammonia status superseding a patient’s mental status because “there are many people who are completely alert who have high ammonia levels,” Dr. Bajaj said. “When the patient presents at the emergency [department] with confusion but has a completely normal ammonia level, that is the only time ammonia levels are useful.”
Treating hepatic encephalopathy is possible by reducing the nitrogenous load in the gut with lactulose, rifaximin, probiotics, or laxatives, according to Dr. Bajaj, who noted that most overt hepatic encephalopathy patients will require inpatient evaluation, and that in cases with recurrent precipitating factors, patients should be considered for liver transplant suitability.
Dr. Bajaj said he receives grant support from Grifols, Norgine, and Salix.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
PHILADELPHIA – To help ensure the best outcomes in patients with a range of liver pathologies, be alert for signs of neurologic and psychiatric abnormalities caused by hepatic encephalopathy, according to an expert.
“The patient doesn’t have to have cirrhosis or liver disease, but can just have portosystemic shunting with absolutely no liver disease, and still have hepatic encephalopathy,” Dr. Jasmohan S. Bajaj said at the meeting held by Global Academy for Medical Education and Rutgers, the State University of New Jersey.
Hepatic encephalopathy is believed to be due to dysbiosis caused by an altered bile acid profile, leading to an impaired intestinal barrier, which allows high levels of ammonia to circulate through the bloodstream, contributing to systemic inflammation and brain dysfunction, according to Dr. Bajaj, an associate professor of medicine at Virginia Commonwealth University and McGuire VA Medical Center, Richmond, Va.
“Ultimately, all the manifestations that we see are because of neuronal dysfunction, which is why the patient is depressed, anxious, sleepy, and has tremors,” Dr. Bajaj said.
Guidelines issued by the American Association for the Study of Liver Diseases stratify hepatic encephalopathy into four grades, the first being the difficult-to-detect subclinical form that is present in up at as many as 60% of patients with hepatic pathologies.
Because covert hepatic encephalopathy will likely progress to a more overt form, adversely impacting a patient’s quality of life and other outcomes, Dr. Bajaj emphasized the importance of testing for it.
One means of detection is to evaluate a patient’s response time using a modified version of the psychiatric Stroop test that measures cognitive dysfunction. Another is to consider collaborative care with a psychologist who can test for and diagnose cognitive impairment. Patients who select at least four items in the Sickness Impact Profile are “80% likely” to have covert hepatic encephalopathy, according to Dr. Bajaj.
Overt manifestations of hepatic encephalopathy include obvious signs of altered mental status, usually reported by the caregiver. Clinicians should consider as part of their differential diagnosis for overt hepatic encephalopathy whether the patient is diabetic, intoxicated, suffering an electrolyte disorder, or is experiencing intracranial bleeding or stroke, and should consider precipitating factors such as an infection, gastrointestinal bleeding, or an overdose of diuretics.
Avoid treatment decisions based on blood ammonia status superseding a patient’s mental status because “there are many people who are completely alert who have high ammonia levels,” Dr. Bajaj said. “When the patient presents at the emergency [department] with confusion but has a completely normal ammonia level, that is the only time ammonia levels are useful.”
Treating hepatic encephalopathy is possible by reducing the nitrogenous load in the gut with lactulose, rifaximin, probiotics, or laxatives, according to Dr. Bajaj, who noted that most overt hepatic encephalopathy patients will require inpatient evaluation, and that in cases with recurrent precipitating factors, patients should be considered for liver transplant suitability.
Dr. Bajaj said he receives grant support from Grifols, Norgine, and Salix.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
PHILADELPHIA – To help ensure the best outcomes in patients with a range of liver pathologies, be alert for signs of neurologic and psychiatric abnormalities caused by hepatic encephalopathy, according to an expert.
“The patient doesn’t have to have cirrhosis or liver disease, but can just have portosystemic shunting with absolutely no liver disease, and still have hepatic encephalopathy,” Dr. Jasmohan S. Bajaj said at the meeting held by Global Academy for Medical Education and Rutgers, the State University of New Jersey.
Hepatic encephalopathy is believed to be due to dysbiosis caused by an altered bile acid profile, leading to an impaired intestinal barrier, which allows high levels of ammonia to circulate through the bloodstream, contributing to systemic inflammation and brain dysfunction, according to Dr. Bajaj, an associate professor of medicine at Virginia Commonwealth University and McGuire VA Medical Center, Richmond, Va.
“Ultimately, all the manifestations that we see are because of neuronal dysfunction, which is why the patient is depressed, anxious, sleepy, and has tremors,” Dr. Bajaj said.
Guidelines issued by the American Association for the Study of Liver Diseases stratify hepatic encephalopathy into four grades, the first being the difficult-to-detect subclinical form that is present in up at as many as 60% of patients with hepatic pathologies.
Because covert hepatic encephalopathy will likely progress to a more overt form, adversely impacting a patient’s quality of life and other outcomes, Dr. Bajaj emphasized the importance of testing for it.
One means of detection is to evaluate a patient’s response time using a modified version of the psychiatric Stroop test that measures cognitive dysfunction. Another is to consider collaborative care with a psychologist who can test for and diagnose cognitive impairment. Patients who select at least four items in the Sickness Impact Profile are “80% likely” to have covert hepatic encephalopathy, according to Dr. Bajaj.
Overt manifestations of hepatic encephalopathy include obvious signs of altered mental status, usually reported by the caregiver. Clinicians should consider as part of their differential diagnosis for overt hepatic encephalopathy whether the patient is diabetic, intoxicated, suffering an electrolyte disorder, or is experiencing intracranial bleeding or stroke, and should consider precipitating factors such as an infection, gastrointestinal bleeding, or an overdose of diuretics.
Avoid treatment decisions based on blood ammonia status superseding a patient’s mental status because “there are many people who are completely alert who have high ammonia levels,” Dr. Bajaj said. “When the patient presents at the emergency [department] with confusion but has a completely normal ammonia level, that is the only time ammonia levels are useful.”
Treating hepatic encephalopathy is possible by reducing the nitrogenous load in the gut with lactulose, rifaximin, probiotics, or laxatives, according to Dr. Bajaj, who noted that most overt hepatic encephalopathy patients will require inpatient evaluation, and that in cases with recurrent precipitating factors, patients should be considered for liver transplant suitability.
Dr. Bajaj said he receives grant support from Grifols, Norgine, and Salix.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
AT DIGESTIVE DISEASES: NEW ADVANCES
VIDEO: Stenting to improve quality of life in esophageal cancer
PHILADELPHIA – An esophageal stent can improve quality of life for patients with advanced esophageal cancer, according to Dr. Sushil Ahlawat, director of endoscopy at Rutgers University, New Brunswick, N.J.
“An esophageal stent can be an important modality for palliating patients’ dysphagia, [which] can happen because the tumor is obstructing the esophagus,” says Dr. Ahlawat in this video. He also discusses how this minimally invasive procedure can support those undergoing chemoradiation therapy or surgery for esophageal cancer.
The video was recorded at this year’s meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy for Medical Education and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
PHILADELPHIA – An esophageal stent can improve quality of life for patients with advanced esophageal cancer, according to Dr. Sushil Ahlawat, director of endoscopy at Rutgers University, New Brunswick, N.J.
“An esophageal stent can be an important modality for palliating patients’ dysphagia, [which] can happen because the tumor is obstructing the esophagus,” says Dr. Ahlawat in this video. He also discusses how this minimally invasive procedure can support those undergoing chemoradiation therapy or surgery for esophageal cancer.
The video was recorded at this year’s meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy for Medical Education and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
PHILADELPHIA – An esophageal stent can improve quality of life for patients with advanced esophageal cancer, according to Dr. Sushil Ahlawat, director of endoscopy at Rutgers University, New Brunswick, N.J.
“An esophageal stent can be an important modality for palliating patients’ dysphagia, [which] can happen because the tumor is obstructing the esophagus,” says Dr. Ahlawat in this video. He also discusses how this minimally invasive procedure can support those undergoing chemoradiation therapy or surgery for esophageal cancer.
The video was recorded at this year’s meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy for Medical Education and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM DIGESTIVE DISEASES: NEW ADVANCES
VIDEO: How to recognize and treat nonalcoholic fatty liver disease
PHILADELPHIA – Nonalcoholic fatty liver disease is on the rise worldwide, but many clinicians are unaware of how to recognize this potentially fatal condition, in part because it can be difficult to separate from common comorbidities such as obesity and diabetes.
In an interview at the Digestive Diseases: New Advances 2016 meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey, Dr. Zobair M. Younossi, chairman of the department of medicine at Inova Fairfax (Va.) Hospital, discussed what clinicians should know in order to screen for and treat this disease.
Dr. Younossi said he is a consultant to Conatus Pharmaceuticals, Enterome Bioscience, and Gilead, and on the advisory boards of Janssen, Salix Pharmaceuticals, and Vertex Pharmaceuticals.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
PHILADELPHIA – Nonalcoholic fatty liver disease is on the rise worldwide, but many clinicians are unaware of how to recognize this potentially fatal condition, in part because it can be difficult to separate from common comorbidities such as obesity and diabetes.
In an interview at the Digestive Diseases: New Advances 2016 meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey, Dr. Zobair M. Younossi, chairman of the department of medicine at Inova Fairfax (Va.) Hospital, discussed what clinicians should know in order to screen for and treat this disease.
Dr. Younossi said he is a consultant to Conatus Pharmaceuticals, Enterome Bioscience, and Gilead, and on the advisory boards of Janssen, Salix Pharmaceuticals, and Vertex Pharmaceuticals.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
PHILADELPHIA – Nonalcoholic fatty liver disease is on the rise worldwide, but many clinicians are unaware of how to recognize this potentially fatal condition, in part because it can be difficult to separate from common comorbidities such as obesity and diabetes.
In an interview at the Digestive Diseases: New Advances 2016 meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey, Dr. Zobair M. Younossi, chairman of the department of medicine at Inova Fairfax (Va.) Hospital, discussed what clinicians should know in order to screen for and treat this disease.
Dr. Younossi said he is a consultant to Conatus Pharmaceuticals, Enterome Bioscience, and Gilead, and on the advisory boards of Janssen, Salix Pharmaceuticals, and Vertex Pharmaceuticals.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
AT DIGESTIVE DISEASES: NEW ADVANCES 2016
VIDEO: Myths and truths of gluten-free diets
PHILADELPHIA – Do you have patients with undiagnosed celiac disease or legitimate gluten sensitivity, or are they self-diagnosing with the need to steer clear of gluten, only to find themselves in danger of nutritional deficiencies and other health concerns?
Of the roughly 1% of Americans who have celiac disease, only about 17% ever receive a diagnosis, leaving the remainder at risk for serious health complications, according to Dr. Peter H.R. Green, director of the Celiac Disease Center at Columbia University, New York.
Meanwhile, many people choose to go gluten free, which Dr. Green calls the most popular “fad” diet in the country. Aside from this trend being more expensive, and often inconvenient, it’s also a health risk. “It’s ironic that so many people who should be on a gluten-free diet aren’t, and those who are don’t need to be, and might even be harming their health,” he said in an interview.
In this video, Dr. Green discusses how to determine whether patients have celiac disease or another diagnosis, and how to counsel those who do have the disease and those who don’t.
The video was recorded at this year’s Digestive Diseases: New Advances, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
PHILADELPHIA – Do you have patients with undiagnosed celiac disease or legitimate gluten sensitivity, or are they self-diagnosing with the need to steer clear of gluten, only to find themselves in danger of nutritional deficiencies and other health concerns?
Of the roughly 1% of Americans who have celiac disease, only about 17% ever receive a diagnosis, leaving the remainder at risk for serious health complications, according to Dr. Peter H.R. Green, director of the Celiac Disease Center at Columbia University, New York.
Meanwhile, many people choose to go gluten free, which Dr. Green calls the most popular “fad” diet in the country. Aside from this trend being more expensive, and often inconvenient, it’s also a health risk. “It’s ironic that so many people who should be on a gluten-free diet aren’t, and those who are don’t need to be, and might even be harming their health,” he said in an interview.
In this video, Dr. Green discusses how to determine whether patients have celiac disease or another diagnosis, and how to counsel those who do have the disease and those who don’t.
The video was recorded at this year’s Digestive Diseases: New Advances, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
PHILADELPHIA – Do you have patients with undiagnosed celiac disease or legitimate gluten sensitivity, or are they self-diagnosing with the need to steer clear of gluten, only to find themselves in danger of nutritional deficiencies and other health concerns?
Of the roughly 1% of Americans who have celiac disease, only about 17% ever receive a diagnosis, leaving the remainder at risk for serious health complications, according to Dr. Peter H.R. Green, director of the Celiac Disease Center at Columbia University, New York.
Meanwhile, many people choose to go gluten free, which Dr. Green calls the most popular “fad” diet in the country. Aside from this trend being more expensive, and often inconvenient, it’s also a health risk. “It’s ironic that so many people who should be on a gluten-free diet aren’t, and those who are don’t need to be, and might even be harming their health,” he said in an interview.
In this video, Dr. Green discusses how to determine whether patients have celiac disease or another diagnosis, and how to counsel those who do have the disease and those who don’t.
The video was recorded at this year’s Digestive Diseases: New Advances, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM DIGESTIVE DISEASES: NEW ADVANCES
VIDEO: Management of difficult-to-treat IBD cases
PHILADELPHIA – The lack of evidence-based management strategies for the treatment of difficult inflammatory bowel disease cases, such as with Crohn’s disease, can lead to confusion for some clinicians.
Dr. Mark T. Osterman, assistant professor of medicine at the University of Pennsylvania, Philadelphia, discusses when to use antibiotics in Crohn’s disease and when to consider antibiotics in combination with draining fistulae. He also discusses available pharmacotherapies, and the value of bowel rest.
“The best treatment of all for difficult inflammatory bowel disease is aggressive and early, so that the condition doesn’t go from bad to worse,” Dr. Osterman said.
The video was recorded at this year’s meeting of Digestive Diseases: New Advances, a meeting held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
PHILADELPHIA – The lack of evidence-based management strategies for the treatment of difficult inflammatory bowel disease cases, such as with Crohn’s disease, can lead to confusion for some clinicians.
Dr. Mark T. Osterman, assistant professor of medicine at the University of Pennsylvania, Philadelphia, discusses when to use antibiotics in Crohn’s disease and when to consider antibiotics in combination with draining fistulae. He also discusses available pharmacotherapies, and the value of bowel rest.
“The best treatment of all for difficult inflammatory bowel disease is aggressive and early, so that the condition doesn’t go from bad to worse,” Dr. Osterman said.
The video was recorded at this year’s meeting of Digestive Diseases: New Advances, a meeting held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
PHILADELPHIA – The lack of evidence-based management strategies for the treatment of difficult inflammatory bowel disease cases, such as with Crohn’s disease, can lead to confusion for some clinicians.
Dr. Mark T. Osterman, assistant professor of medicine at the University of Pennsylvania, Philadelphia, discusses when to use antibiotics in Crohn’s disease and when to consider antibiotics in combination with draining fistulae. He also discusses available pharmacotherapies, and the value of bowel rest.
“The best treatment of all for difficult inflammatory bowel disease is aggressive and early, so that the condition doesn’t go from bad to worse,” Dr. Osterman said.
The video was recorded at this year’s meeting of Digestive Diseases: New Advances, a meeting held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM DIGESTIVE DISEASES: NEW ADVANCES
Pediatric mental illness dx, drug prescribing vary widely
A lack of psychiatrists only partially accounted for substantial variations in rates of mental illness diagnosis and prescriptions for psychotropic medications in practices nationwide, a study has shown.
Although a lack of available specialty care was associated with significantly higher odds of a diagnosis or prescription, the colocation of mental health professionals or percentage of children in foster care treated in a practice did not fully explain the differences.
Among 294,748 children aged 4-18 years, seen one or more times in 43 primary care practices nationwide, 15% received a mental health diagnosis between Jan. 1, 2009, and June 30, 2014. Psychotropic medications were prescribed to 14%, reported lead researcher Stephanie L. Mayne of the center for pediatric clinical effectiveness at the the Children’s Hospital of Philadelphia (Pediatrics. 2016 doi: 10.1542/peds.2015-2974).
The most common diagnosis was attention-deficit/hyperactivity disorder at a rate of between 1% and 16%. Differences in other diagnoses “were smaller, but still meaningful” at ranges of 1%-8% for anxiety, 0%-5% for depression, 0.2%-3% for autism, 0%-3% for conduct disorder, and 0%-2% for oppositional-defiant disorder. Bipolar disorder was “uncommon” at less than 1%, Ms. Mayne and her associates reported.
The rate of children receiving any psychotropic medication was between 4% and 26%, while the proportion of patients receiving two or more medication classes ranged between 1% and 12%. Prescription rates for specific medication classes also varied at between 4% and 18% for stimulants, 1% and 12% for antidepressants, 0.1% and 8% for alpha-agonists, and 0.1% and 5% for second-generation antipsychotics.
“Primary care providers’ level of agreement with current guidelines, perceived self-efficacy in diagnosing or treating particular conditions, training, relationships with schools, and reimbursement from insurers might affect prescribing practices,” Ms. Mayne and her associates wrote.
“Even with colocation, barriers such as financial differences in reimbursement for medical and mental health services, difficulties with information sharing, differing expertise, and limited hours may impede integration,” they commented.
Dr. Alexander G. Fiks is an investigator for Pfizer; the other researchers said they had no relevant financial disclosures. This study was funded by the National Institutes of Health and the National Institute of Child Health and Human Development under the Best Pharmaceuticals for Children Act.
On Twitter @whitneymcknight
The integration of mental health services into primary care is an important strategy for increasing access. Future studies that investigate variations in mental health care seen in the primary care setting can help us better understand the quality of this care and consistency with published guidelines.

|
Dr. Lee Savio Beers |
Increased education and support for primary care physicians is essential, as they are at the front lines of providing care to children with mental and behavioral health concerns. However, working together with specialty mental health providers is also important, as they are important partners in the early identification, diagnosis, and treatment of mental disorders.
Education and consultation models such as Child Psychiatry Access Programs can significantly improve a primary care physician’s capacity to care for children with mental health concerns in the medical home, and arrange for appropriate specialty mental health treatment when indicated.
Dr. Lee Savio Beers is the medical director for municipal and regional affairs for the Child Health Advocacy Institute at Children’s National Medical Center, the director of the Washington, D.C., Mental Health Access in Pediatrics (DC MAP) program, and an assistant professor of pediatrics at George Washington University, all in Washington. She had no relevant financial disclosures.
The integration of mental health services into primary care is an important strategy for increasing access. Future studies that investigate variations in mental health care seen in the primary care setting can help us better understand the quality of this care and consistency with published guidelines.

|
Dr. Lee Savio Beers |
Increased education and support for primary care physicians is essential, as they are at the front lines of providing care to children with mental and behavioral health concerns. However, working together with specialty mental health providers is also important, as they are important partners in the early identification, diagnosis, and treatment of mental disorders.
Education and consultation models such as Child Psychiatry Access Programs can significantly improve a primary care physician’s capacity to care for children with mental health concerns in the medical home, and arrange for appropriate specialty mental health treatment when indicated.
Dr. Lee Savio Beers is the medical director for municipal and regional affairs for the Child Health Advocacy Institute at Children’s National Medical Center, the director of the Washington, D.C., Mental Health Access in Pediatrics (DC MAP) program, and an assistant professor of pediatrics at George Washington University, all in Washington. She had no relevant financial disclosures.
The integration of mental health services into primary care is an important strategy for increasing access. Future studies that investigate variations in mental health care seen in the primary care setting can help us better understand the quality of this care and consistency with published guidelines.

|
Dr. Lee Savio Beers |
Increased education and support for primary care physicians is essential, as they are at the front lines of providing care to children with mental and behavioral health concerns. However, working together with specialty mental health providers is also important, as they are important partners in the early identification, diagnosis, and treatment of mental disorders.
Education and consultation models such as Child Psychiatry Access Programs can significantly improve a primary care physician’s capacity to care for children with mental health concerns in the medical home, and arrange for appropriate specialty mental health treatment when indicated.
Dr. Lee Savio Beers is the medical director for municipal and regional affairs for the Child Health Advocacy Institute at Children’s National Medical Center, the director of the Washington, D.C., Mental Health Access in Pediatrics (DC MAP) program, and an assistant professor of pediatrics at George Washington University, all in Washington. She had no relevant financial disclosures.
A lack of psychiatrists only partially accounted for substantial variations in rates of mental illness diagnosis and prescriptions for psychotropic medications in practices nationwide, a study has shown.
Although a lack of available specialty care was associated with significantly higher odds of a diagnosis or prescription, the colocation of mental health professionals or percentage of children in foster care treated in a practice did not fully explain the differences.
Among 294,748 children aged 4-18 years, seen one or more times in 43 primary care practices nationwide, 15% received a mental health diagnosis between Jan. 1, 2009, and June 30, 2014. Psychotropic medications were prescribed to 14%, reported lead researcher Stephanie L. Mayne of the center for pediatric clinical effectiveness at the the Children’s Hospital of Philadelphia (Pediatrics. 2016 doi: 10.1542/peds.2015-2974).
The most common diagnosis was attention-deficit/hyperactivity disorder at a rate of between 1% and 16%. Differences in other diagnoses “were smaller, but still meaningful” at ranges of 1%-8% for anxiety, 0%-5% for depression, 0.2%-3% for autism, 0%-3% for conduct disorder, and 0%-2% for oppositional-defiant disorder. Bipolar disorder was “uncommon” at less than 1%, Ms. Mayne and her associates reported.
The rate of children receiving any psychotropic medication was between 4% and 26%, while the proportion of patients receiving two or more medication classes ranged between 1% and 12%. Prescription rates for specific medication classes also varied at between 4% and 18% for stimulants, 1% and 12% for antidepressants, 0.1% and 8% for alpha-agonists, and 0.1% and 5% for second-generation antipsychotics.
“Primary care providers’ level of agreement with current guidelines, perceived self-efficacy in diagnosing or treating particular conditions, training, relationships with schools, and reimbursement from insurers might affect prescribing practices,” Ms. Mayne and her associates wrote.
“Even with colocation, barriers such as financial differences in reimbursement for medical and mental health services, difficulties with information sharing, differing expertise, and limited hours may impede integration,” they commented.
Dr. Alexander G. Fiks is an investigator for Pfizer; the other researchers said they had no relevant financial disclosures. This study was funded by the National Institutes of Health and the National Institute of Child Health and Human Development under the Best Pharmaceuticals for Children Act.
On Twitter @whitneymcknight
A lack of psychiatrists only partially accounted for substantial variations in rates of mental illness diagnosis and prescriptions for psychotropic medications in practices nationwide, a study has shown.
Although a lack of available specialty care was associated with significantly higher odds of a diagnosis or prescription, the colocation of mental health professionals or percentage of children in foster care treated in a practice did not fully explain the differences.
Among 294,748 children aged 4-18 years, seen one or more times in 43 primary care practices nationwide, 15% received a mental health diagnosis between Jan. 1, 2009, and June 30, 2014. Psychotropic medications were prescribed to 14%, reported lead researcher Stephanie L. Mayne of the center for pediatric clinical effectiveness at the the Children’s Hospital of Philadelphia (Pediatrics. 2016 doi: 10.1542/peds.2015-2974).
The most common diagnosis was attention-deficit/hyperactivity disorder at a rate of between 1% and 16%. Differences in other diagnoses “were smaller, but still meaningful” at ranges of 1%-8% for anxiety, 0%-5% for depression, 0.2%-3% for autism, 0%-3% for conduct disorder, and 0%-2% for oppositional-defiant disorder. Bipolar disorder was “uncommon” at less than 1%, Ms. Mayne and her associates reported.
The rate of children receiving any psychotropic medication was between 4% and 26%, while the proportion of patients receiving two or more medication classes ranged between 1% and 12%. Prescription rates for specific medication classes also varied at between 4% and 18% for stimulants, 1% and 12% for antidepressants, 0.1% and 8% for alpha-agonists, and 0.1% and 5% for second-generation antipsychotics.
“Primary care providers’ level of agreement with current guidelines, perceived self-efficacy in diagnosing or treating particular conditions, training, relationships with schools, and reimbursement from insurers might affect prescribing practices,” Ms. Mayne and her associates wrote.
“Even with colocation, barriers such as financial differences in reimbursement for medical and mental health services, difficulties with information sharing, differing expertise, and limited hours may impede integration,” they commented.
Dr. Alexander G. Fiks is an investigator for Pfizer; the other researchers said they had no relevant financial disclosures. This study was funded by the National Institutes of Health and the National Institute of Child Health and Human Development under the Best Pharmaceuticals for Children Act.
On Twitter @whitneymcknight
FROM PEDIATRICS
Key clinical point: A lack of psychiatrists only partially accounted for substantial variations in rates of mental illness diagnosis and prescriptions for psychotropic medications given in practices nationwide, a study has shown.
Major finding: Nationwide, 15% of pediatric patients received a mental health diagnosis, and 14% were prescribed psychotropic medications in primary care, regardless of colocated mental health services.
Data source: A retrospective study of electronic health records for 294,748 patients aged 4-18 years.
Disclosures: Dr. Alexander G. Fiks is an investigator for Pfizer; the other researchers said they had no relevant financial disclosures. This study was funded by the National Institutes of Health and the National Institute of Child Health and Human Development under the Best Pharmaceuticals for Children Act.
Medicare may expand preventive prediabetes coverage
Expanded Medicare coverage of preventive services for type 2 diabetes may mean providers will need to add staff or connect with community resources as early as next year.
Results from the pilot National Diabetes Prevention Program were persuasive enough for the independent Office of the Actuary in the Centers for Medicare & Medicaid Services to certify that the expansion would result in reduced net spending and better patient outcomes.
It’s the first preventive model to be developed in the CMS Innovation Center, which itself was created as part of the Affordable Care Act.
“This program has been shown to reduce health care costs and help prevent diabetes, and is one that Medicare, employers, and private insurers can use to help 86 million Americans live healthier,” Department of Health & Human Services Secretary Sylvia M. Burwell said in a statement issued on the ACA’s sixth anniversary. “The Affordable Care Act gave Medicare the tools to support this groundbreaking effort and to expand this program more broadly.”
The Centers for Disease Control and Prevention estimates that as many as one in three adult Americans has prediabetes, which with weight loss and exercise can be prevented from progressing to type 2 diabetes.
According to the CMS, the evidence-based diabetes prevention program resulted in savings of $2,650 per enrollee over 15 months, compared with costs associated with nonprogram beneficiaries – enough to cover the cost of the program. Program participants also were shown to lose about 5% of their body weight.
But who will deliver these preventive services and how they will be paid for are still questions to be answered.
“While the government supports expansion of the diabetes prevention program, it must now go through a period of rule making and public comment beginning this summer,” American Medical Association President-Elect Andrew W. Gurman said in an interview.
The AMA supports the expansion, having already helped to develop and pilot a similar community-based prevention program nationally in partnership with the YMCA. Based on that experience, the AMA has created a resource base for physicians and other providers to screen, test, and refer patients for their prediabetes, available online.
“This is an important step in advancing more enlightened health policy and recognizing the important role of prevention in stemming the tide of chronic disease in our country,” Dr. Gurman said.
The joint pilot AMA-YMCA diabetes prevention program relied mainly upon trained lifestyle coaches rather than physicians for service delivery.
When introduced this summer, the proposed 2017 Medicare Physician Fee Schedule will likely have more on the prediabetes program expansion, according to CMS officials.
The American College of Physicians suggests members consider adopting the patient-centered medical home model of care, which emphasizes team-based care and helping patients gain access to lifestyle change programs.
That is particularly helpful in anticipation of the 2019 merit-based reimbursement schedules featured in the Medicare Access and CHIP Reauthorization Act (MACRA), according to Shari Erickson, the ACP’s vice president for governmental affairs and medical practice. Such an approach is already gaining traction nationally and is used across the country by a number of payers, both public and private, she added.
“The ACP also has been seeking the development of a code bundle for diabetic care management to emphasize better care coordination, communication, and integration of the care team aimed at a better overall outcome and cost of care for the Medicare beneficiary,” Ms. Erickson said in an interview.
Leveraging the ACA for better diabetes care
Endocrinologists are calling for more integrated approaches to diabetes care and prevention.
A trifecta of concerns – cost saving, improved patient outcomes, and potential workforce shortages – are cited in a white paper published online outlining ways the health care system can leverage the Affordable Care Act to create multidisciplinary modes of diabetes care.
“Coordinated care is necessary to ensure the best possible outcomes for people with diabetes. An effective team-based approach must provide comprehensive, continuous, and timely care without duplicating any tests or services,” Dr. Alvin C. Powers, the report’s lead author and an endocrinologist at Vanderbilt University, Nashville, Tenn., said in a statement released by the Endocrine Society on the ACA’s sixth anniversary.
Currently, more than 29 million Americans have diabetes, according to the society. Without public health interventions, that number is expected to roughly double over the next 5 years, at an estimated cost to the U.S. health care system of $512 billion.
Passage of the ACA has helped increase the number of insured people able to receive a clinical diabetes diagnosis, creating the need for a broader and deeper range of diabetes-related services, according to the society.
People with diabetes often require care from a range of specialists, such as nephrologists, podiatrists, and ophthalmologists, as well as endocrinologists and primary care physicians who are skilled in managing diabetes.
The society supports programs such as the one announced by HHS Secretary Burwell, along with evidence-based community and employer-sponsored care, and incentives to providers to integrate diabetes care in practice.
The society is also calling for additional federally funded research, faster medication approvals from the Food and Drug Administration, and incorporation of the drugs into CMS beneficiary packages.
On Twitter @whitneymcknight
Expanded Medicare coverage of preventive services for type 2 diabetes may mean providers will need to add staff or connect with community resources as early as next year.
Results from the pilot National Diabetes Prevention Program were persuasive enough for the independent Office of the Actuary in the Centers for Medicare & Medicaid Services to certify that the expansion would result in reduced net spending and better patient outcomes.
It’s the first preventive model to be developed in the CMS Innovation Center, which itself was created as part of the Affordable Care Act.
“This program has been shown to reduce health care costs and help prevent diabetes, and is one that Medicare, employers, and private insurers can use to help 86 million Americans live healthier,” Department of Health & Human Services Secretary Sylvia M. Burwell said in a statement issued on the ACA’s sixth anniversary. “The Affordable Care Act gave Medicare the tools to support this groundbreaking effort and to expand this program more broadly.”
The Centers for Disease Control and Prevention estimates that as many as one in three adult Americans has prediabetes, which with weight loss and exercise can be prevented from progressing to type 2 diabetes.
According to the CMS, the evidence-based diabetes prevention program resulted in savings of $2,650 per enrollee over 15 months, compared with costs associated with nonprogram beneficiaries – enough to cover the cost of the program. Program participants also were shown to lose about 5% of their body weight.
But who will deliver these preventive services and how they will be paid for are still questions to be answered.
“While the government supports expansion of the diabetes prevention program, it must now go through a period of rule making and public comment beginning this summer,” American Medical Association President-Elect Andrew W. Gurman said in an interview.
The AMA supports the expansion, having already helped to develop and pilot a similar community-based prevention program nationally in partnership with the YMCA. Based on that experience, the AMA has created a resource base for physicians and other providers to screen, test, and refer patients for their prediabetes, available online.
“This is an important step in advancing more enlightened health policy and recognizing the important role of prevention in stemming the tide of chronic disease in our country,” Dr. Gurman said.
The joint pilot AMA-YMCA diabetes prevention program relied mainly upon trained lifestyle coaches rather than physicians for service delivery.
When introduced this summer, the proposed 2017 Medicare Physician Fee Schedule will likely have more on the prediabetes program expansion, according to CMS officials.
The American College of Physicians suggests members consider adopting the patient-centered medical home model of care, which emphasizes team-based care and helping patients gain access to lifestyle change programs.
That is particularly helpful in anticipation of the 2019 merit-based reimbursement schedules featured in the Medicare Access and CHIP Reauthorization Act (MACRA), according to Shari Erickson, the ACP’s vice president for governmental affairs and medical practice. Such an approach is already gaining traction nationally and is used across the country by a number of payers, both public and private, she added.
“The ACP also has been seeking the development of a code bundle for diabetic care management to emphasize better care coordination, communication, and integration of the care team aimed at a better overall outcome and cost of care for the Medicare beneficiary,” Ms. Erickson said in an interview.
Leveraging the ACA for better diabetes care
Endocrinologists are calling for more integrated approaches to diabetes care and prevention.
A trifecta of concerns – cost saving, improved patient outcomes, and potential workforce shortages – are cited in a white paper published online outlining ways the health care system can leverage the Affordable Care Act to create multidisciplinary modes of diabetes care.
“Coordinated care is necessary to ensure the best possible outcomes for people with diabetes. An effective team-based approach must provide comprehensive, continuous, and timely care without duplicating any tests or services,” Dr. Alvin C. Powers, the report’s lead author and an endocrinologist at Vanderbilt University, Nashville, Tenn., said in a statement released by the Endocrine Society on the ACA’s sixth anniversary.
Currently, more than 29 million Americans have diabetes, according to the society. Without public health interventions, that number is expected to roughly double over the next 5 years, at an estimated cost to the U.S. health care system of $512 billion.
Passage of the ACA has helped increase the number of insured people able to receive a clinical diabetes diagnosis, creating the need for a broader and deeper range of diabetes-related services, according to the society.
People with diabetes often require care from a range of specialists, such as nephrologists, podiatrists, and ophthalmologists, as well as endocrinologists and primary care physicians who are skilled in managing diabetes.
The society supports programs such as the one announced by HHS Secretary Burwell, along with evidence-based community and employer-sponsored care, and incentives to providers to integrate diabetes care in practice.
The society is also calling for additional federally funded research, faster medication approvals from the Food and Drug Administration, and incorporation of the drugs into CMS beneficiary packages.
On Twitter @whitneymcknight
Expanded Medicare coverage of preventive services for type 2 diabetes may mean providers will need to add staff or connect with community resources as early as next year.
Results from the pilot National Diabetes Prevention Program were persuasive enough for the independent Office of the Actuary in the Centers for Medicare & Medicaid Services to certify that the expansion would result in reduced net spending and better patient outcomes.
It’s the first preventive model to be developed in the CMS Innovation Center, which itself was created as part of the Affordable Care Act.
“This program has been shown to reduce health care costs and help prevent diabetes, and is one that Medicare, employers, and private insurers can use to help 86 million Americans live healthier,” Department of Health & Human Services Secretary Sylvia M. Burwell said in a statement issued on the ACA’s sixth anniversary. “The Affordable Care Act gave Medicare the tools to support this groundbreaking effort and to expand this program more broadly.”
The Centers for Disease Control and Prevention estimates that as many as one in three adult Americans has prediabetes, which with weight loss and exercise can be prevented from progressing to type 2 diabetes.
According to the CMS, the evidence-based diabetes prevention program resulted in savings of $2,650 per enrollee over 15 months, compared with costs associated with nonprogram beneficiaries – enough to cover the cost of the program. Program participants also were shown to lose about 5% of their body weight.
But who will deliver these preventive services and how they will be paid for are still questions to be answered.
“While the government supports expansion of the diabetes prevention program, it must now go through a period of rule making and public comment beginning this summer,” American Medical Association President-Elect Andrew W. Gurman said in an interview.
The AMA supports the expansion, having already helped to develop and pilot a similar community-based prevention program nationally in partnership with the YMCA. Based on that experience, the AMA has created a resource base for physicians and other providers to screen, test, and refer patients for their prediabetes, available online.
“This is an important step in advancing more enlightened health policy and recognizing the important role of prevention in stemming the tide of chronic disease in our country,” Dr. Gurman said.
The joint pilot AMA-YMCA diabetes prevention program relied mainly upon trained lifestyle coaches rather than physicians for service delivery.
When introduced this summer, the proposed 2017 Medicare Physician Fee Schedule will likely have more on the prediabetes program expansion, according to CMS officials.
The American College of Physicians suggests members consider adopting the patient-centered medical home model of care, which emphasizes team-based care and helping patients gain access to lifestyle change programs.
That is particularly helpful in anticipation of the 2019 merit-based reimbursement schedules featured in the Medicare Access and CHIP Reauthorization Act (MACRA), according to Shari Erickson, the ACP’s vice president for governmental affairs and medical practice. Such an approach is already gaining traction nationally and is used across the country by a number of payers, both public and private, she added.
“The ACP also has been seeking the development of a code bundle for diabetic care management to emphasize better care coordination, communication, and integration of the care team aimed at a better overall outcome and cost of care for the Medicare beneficiary,” Ms. Erickson said in an interview.
Leveraging the ACA for better diabetes care
Endocrinologists are calling for more integrated approaches to diabetes care and prevention.
A trifecta of concerns – cost saving, improved patient outcomes, and potential workforce shortages – are cited in a white paper published online outlining ways the health care system can leverage the Affordable Care Act to create multidisciplinary modes of diabetes care.
“Coordinated care is necessary to ensure the best possible outcomes for people with diabetes. An effective team-based approach must provide comprehensive, continuous, and timely care without duplicating any tests or services,” Dr. Alvin C. Powers, the report’s lead author and an endocrinologist at Vanderbilt University, Nashville, Tenn., said in a statement released by the Endocrine Society on the ACA’s sixth anniversary.
Currently, more than 29 million Americans have diabetes, according to the society. Without public health interventions, that number is expected to roughly double over the next 5 years, at an estimated cost to the U.S. health care system of $512 billion.
Passage of the ACA has helped increase the number of insured people able to receive a clinical diabetes diagnosis, creating the need for a broader and deeper range of diabetes-related services, according to the society.
People with diabetes often require care from a range of specialists, such as nephrologists, podiatrists, and ophthalmologists, as well as endocrinologists and primary care physicians who are skilled in managing diabetes.
The society supports programs such as the one announced by HHS Secretary Burwell, along with evidence-based community and employer-sponsored care, and incentives to providers to integrate diabetes care in practice.
The society is also calling for additional federally funded research, faster medication approvals from the Food and Drug Administration, and incorporation of the drugs into CMS beneficiary packages.
On Twitter @whitneymcknight
IBD: Chronic, not ‘crisis’ care
BOSTON – Inflammatory bowel disease (IBD) has gone from being a condition largely managed on a crisis basis to one in which the goal is to prevent acute exacerbations and preserve a low level of disease activity over its chronic course.
While this model saves costs and creates better patient outcomes overall, it requires specialists to approach care differently, including leveraging an ever-widening array of clinical innovations.
“The chronic disease management model requires regular monitoring and advanced technologies to better characterize the disease activity and response to therapy,” said Dr. David Rubin, section chief of gastroenterology, hepatology, and nutrition at the University of Chicago. In addition to keeping chronic disease from drifting away from stability, Dr. Rubin said, “Effective monitoring should allow proactive management decisions and ongoing control and changing disease natural history.”
The challenge has been to identify tools useful in monitoring patients with IBD to ensure that disease is under control, according to a panel of speakers addressing this topic at the 2016 AGA Tech Summit, which is sponsored by the AGA Center for GI Innovation and Technology. The relationship of inflammation in the bowel to symptoms is notoriously poor, including both a high degree of disease activity in those with relatively few symptoms and a low degree of inflammation in those seeking care because of a poor quality of life.
“We need better and less invasive ways to monitor disease control as well as better predictors of risk of exacerbations,” Dr. Rubin said. Although a variety of biomarkers are already used to evaluate IBD, such as C-reactive protein and fecal calprotectin levels, none is fully reliable as an isolated measure, according to Dr. Rubin. Ongoing studies are pursuing biomarkers measured in the urine, from the breath, and by genetic analysis, but the key to each is demonstrating that changing management on the basis of the information they provide results in better long-term outcomes.
Currently, endoscopy is the most reliable tool for evaluating disease activity and guiding therapeutic decisions, according to Dr. Edward V. Loftus, professor of medicine at the Mayo Clinic, Rochester, Minn., and a session copanelist with Dr. Rubin. Although several scoring systems are employed to reduce subjectivity in endoscopic evaluation of disease activity, Dr. Loftus suggested that no scoring system eliminates interobserver variability.
At least for clinical trials, employing central reading of endoscopic studies has been one approach to reduce interobserver variability and to “drive down placebo rates” that are typically substantial in drug trial studies. Not least important among endoscopic measures is the confirmation of mucosal healing.
“Mucosal healing is a binary concept. It is either complete or it is not,” explained Dr. Loftus, citing several studies suggesting that the risk of disease relapse is lower when mucosal healing is achieved. Endoscopy is currently the only reliable method of establishing mucosal healing. However, he said that precise measurement of disease activity “takes a little bit of training,” a problem that represents “an unmet need” for more efficient disease evaluation.
“One could envision somebody designing software built into the scope that will automatically score the degree of IBD severity.” Dr. Loftus said. “These tools have already resulted in a change in the types of clinical trial endpoints used, and one could argue that they are more objective now.”
The need for better tools for prognosis will only increase as treatments for IBD continue to expand, according to Dr. Gary R. Lichtenstein, professor of medicine at the University of Pennsylvania, Philadelphia. He emphasized that there is wide variability in response even to the most effective treatments. Tools useful for quickly evaluating when a therapy is or is not working would be extremely useful for switching patients to an alternative drug.
These alternative drugs include an expanding array of mechanisms of action with more reaching late stages of clinical testing, according to Dr. Lichtenstein, who reviewed the mechanism of integrin inhibitors, small-molecule therapies targeting the JAK pathway, and cytokine inhibitors. There are also strategies being pursued that involve manipulating the microbiome to control IBD.
“The therapies we have currently are totally inadequate,” said Dr. Lichtenstein, underscoring the excitement about clinical activity observed with drugs that offer novel mechanisms of action.
The activity in this field is being closely monitored by the AGA’s Center for Diagnostics and Therapeutics (CDT), which is chaired by Dr. Colin. W. Howden, gastroenterology chief at the University of Tennessee Health Science Center, Memphis. Although the interests of the CDT, which met last summer with the U.S. Food and Drug Administration to discuss issues of mutual interest in GI therapeutics, is not limited to IBD, this set of diseases was a focus in its first stand-alone conference held in October 2015. According to Dr. Howden, the discussion at that meeting provided the framework for the program at the 2016 AGA Tech Summit.
On Twitter @whitneymcknight
BOSTON – Inflammatory bowel disease (IBD) has gone from being a condition largely managed on a crisis basis to one in which the goal is to prevent acute exacerbations and preserve a low level of disease activity over its chronic course.
While this model saves costs and creates better patient outcomes overall, it requires specialists to approach care differently, including leveraging an ever-widening array of clinical innovations.
“The chronic disease management model requires regular monitoring and advanced technologies to better characterize the disease activity and response to therapy,” said Dr. David Rubin, section chief of gastroenterology, hepatology, and nutrition at the University of Chicago. In addition to keeping chronic disease from drifting away from stability, Dr. Rubin said, “Effective monitoring should allow proactive management decisions and ongoing control and changing disease natural history.”
The challenge has been to identify tools useful in monitoring patients with IBD to ensure that disease is under control, according to a panel of speakers addressing this topic at the 2016 AGA Tech Summit, which is sponsored by the AGA Center for GI Innovation and Technology. The relationship of inflammation in the bowel to symptoms is notoriously poor, including both a high degree of disease activity in those with relatively few symptoms and a low degree of inflammation in those seeking care because of a poor quality of life.
“We need better and less invasive ways to monitor disease control as well as better predictors of risk of exacerbations,” Dr. Rubin said. Although a variety of biomarkers are already used to evaluate IBD, such as C-reactive protein and fecal calprotectin levels, none is fully reliable as an isolated measure, according to Dr. Rubin. Ongoing studies are pursuing biomarkers measured in the urine, from the breath, and by genetic analysis, but the key to each is demonstrating that changing management on the basis of the information they provide results in better long-term outcomes.
Currently, endoscopy is the most reliable tool for evaluating disease activity and guiding therapeutic decisions, according to Dr. Edward V. Loftus, professor of medicine at the Mayo Clinic, Rochester, Minn., and a session copanelist with Dr. Rubin. Although several scoring systems are employed to reduce subjectivity in endoscopic evaluation of disease activity, Dr. Loftus suggested that no scoring system eliminates interobserver variability.
At least for clinical trials, employing central reading of endoscopic studies has been one approach to reduce interobserver variability and to “drive down placebo rates” that are typically substantial in drug trial studies. Not least important among endoscopic measures is the confirmation of mucosal healing.
“Mucosal healing is a binary concept. It is either complete or it is not,” explained Dr. Loftus, citing several studies suggesting that the risk of disease relapse is lower when mucosal healing is achieved. Endoscopy is currently the only reliable method of establishing mucosal healing. However, he said that precise measurement of disease activity “takes a little bit of training,” a problem that represents “an unmet need” for more efficient disease evaluation.
“One could envision somebody designing software built into the scope that will automatically score the degree of IBD severity.” Dr. Loftus said. “These tools have already resulted in a change in the types of clinical trial endpoints used, and one could argue that they are more objective now.”
The need for better tools for prognosis will only increase as treatments for IBD continue to expand, according to Dr. Gary R. Lichtenstein, professor of medicine at the University of Pennsylvania, Philadelphia. He emphasized that there is wide variability in response even to the most effective treatments. Tools useful for quickly evaluating when a therapy is or is not working would be extremely useful for switching patients to an alternative drug.
These alternative drugs include an expanding array of mechanisms of action with more reaching late stages of clinical testing, according to Dr. Lichtenstein, who reviewed the mechanism of integrin inhibitors, small-molecule therapies targeting the JAK pathway, and cytokine inhibitors. There are also strategies being pursued that involve manipulating the microbiome to control IBD.
“The therapies we have currently are totally inadequate,” said Dr. Lichtenstein, underscoring the excitement about clinical activity observed with drugs that offer novel mechanisms of action.
The activity in this field is being closely monitored by the AGA’s Center for Diagnostics and Therapeutics (CDT), which is chaired by Dr. Colin. W. Howden, gastroenterology chief at the University of Tennessee Health Science Center, Memphis. Although the interests of the CDT, which met last summer with the U.S. Food and Drug Administration to discuss issues of mutual interest in GI therapeutics, is not limited to IBD, this set of diseases was a focus in its first stand-alone conference held in October 2015. According to Dr. Howden, the discussion at that meeting provided the framework for the program at the 2016 AGA Tech Summit.
On Twitter @whitneymcknight
BOSTON – Inflammatory bowel disease (IBD) has gone from being a condition largely managed on a crisis basis to one in which the goal is to prevent acute exacerbations and preserve a low level of disease activity over its chronic course.
While this model saves costs and creates better patient outcomes overall, it requires specialists to approach care differently, including leveraging an ever-widening array of clinical innovations.
“The chronic disease management model requires regular monitoring and advanced technologies to better characterize the disease activity and response to therapy,” said Dr. David Rubin, section chief of gastroenterology, hepatology, and nutrition at the University of Chicago. In addition to keeping chronic disease from drifting away from stability, Dr. Rubin said, “Effective monitoring should allow proactive management decisions and ongoing control and changing disease natural history.”
The challenge has been to identify tools useful in monitoring patients with IBD to ensure that disease is under control, according to a panel of speakers addressing this topic at the 2016 AGA Tech Summit, which is sponsored by the AGA Center for GI Innovation and Technology. The relationship of inflammation in the bowel to symptoms is notoriously poor, including both a high degree of disease activity in those with relatively few symptoms and a low degree of inflammation in those seeking care because of a poor quality of life.
“We need better and less invasive ways to monitor disease control as well as better predictors of risk of exacerbations,” Dr. Rubin said. Although a variety of biomarkers are already used to evaluate IBD, such as C-reactive protein and fecal calprotectin levels, none is fully reliable as an isolated measure, according to Dr. Rubin. Ongoing studies are pursuing biomarkers measured in the urine, from the breath, and by genetic analysis, but the key to each is demonstrating that changing management on the basis of the information they provide results in better long-term outcomes.
Currently, endoscopy is the most reliable tool for evaluating disease activity and guiding therapeutic decisions, according to Dr. Edward V. Loftus, professor of medicine at the Mayo Clinic, Rochester, Minn., and a session copanelist with Dr. Rubin. Although several scoring systems are employed to reduce subjectivity in endoscopic evaluation of disease activity, Dr. Loftus suggested that no scoring system eliminates interobserver variability.
At least for clinical trials, employing central reading of endoscopic studies has been one approach to reduce interobserver variability and to “drive down placebo rates” that are typically substantial in drug trial studies. Not least important among endoscopic measures is the confirmation of mucosal healing.
“Mucosal healing is a binary concept. It is either complete or it is not,” explained Dr. Loftus, citing several studies suggesting that the risk of disease relapse is lower when mucosal healing is achieved. Endoscopy is currently the only reliable method of establishing mucosal healing. However, he said that precise measurement of disease activity “takes a little bit of training,” a problem that represents “an unmet need” for more efficient disease evaluation.
“One could envision somebody designing software built into the scope that will automatically score the degree of IBD severity.” Dr. Loftus said. “These tools have already resulted in a change in the types of clinical trial endpoints used, and one could argue that they are more objective now.”
The need for better tools for prognosis will only increase as treatments for IBD continue to expand, according to Dr. Gary R. Lichtenstein, professor of medicine at the University of Pennsylvania, Philadelphia. He emphasized that there is wide variability in response even to the most effective treatments. Tools useful for quickly evaluating when a therapy is or is not working would be extremely useful for switching patients to an alternative drug.
These alternative drugs include an expanding array of mechanisms of action with more reaching late stages of clinical testing, according to Dr. Lichtenstein, who reviewed the mechanism of integrin inhibitors, small-molecule therapies targeting the JAK pathway, and cytokine inhibitors. There are also strategies being pursued that involve manipulating the microbiome to control IBD.
“The therapies we have currently are totally inadequate,” said Dr. Lichtenstein, underscoring the excitement about clinical activity observed with drugs that offer novel mechanisms of action.
The activity in this field is being closely monitored by the AGA’s Center for Diagnostics and Therapeutics (CDT), which is chaired by Dr. Colin. W. Howden, gastroenterology chief at the University of Tennessee Health Science Center, Memphis. Although the interests of the CDT, which met last summer with the U.S. Food and Drug Administration to discuss issues of mutual interest in GI therapeutics, is not limited to IBD, this set of diseases was a focus in its first stand-alone conference held in October 2015. According to Dr. Howden, the discussion at that meeting provided the framework for the program at the 2016 AGA Tech Summit.
On Twitter @whitneymcknight
AT THE 2016 AGA TECH SUMMIT
Chaplains play important part of integrated palliative care
WASHINGTON – Hospital chaplains are key partners in meeting the needs of palliative care patients and, as such, have much to offer psychiatry, according to an expert.
“I think we should work with chaplains,” Dr. Laura B. Dunn, professor of psychiatry and behavioral sciences at Stanford (Calif.) University, said in an interview at the annual meeting of the American Association for Geriatric Psychiatry. “It’s very helpful to know what they do, and for them to know what we do in terms of diagnosing and using a biopsychosocial model.”
Dr. Dunn said the relegation of chaplaincy and spiritual care in medicine has been unfortunate. After all, the level of a patient’s spiritual health is an inherent aspect of quality of life in palliative care, particularly for those over age 60 who often want help reconciling with loved ones, data collected by Dr. Dunn show. Viewing those patients in terms of their core needs rather than seeking a psychiatric diagnosis can make them more satisfied with their overall palliative care experience, she said.
How is spiritual health measured? There are few models and even fewer empirical studies, but Dr. Dunn said in addition learning how to deliver pastoral care, professional chaplains are trained to assess, intervene, and observe outcomes in spiritual health.
To begin with, spirituality is defined not in terms of “religiosity” but more as following an ethical path, similar to the idea of the Golden Rule or the ethic of reciprocity: Love your neighbor as yourself, in other words. The spiritual maturity to follow such a path requires the ability to love oneself that is balanced with a connection to others, and God, “if your belief includes God,” said Dr. Dunn, who pointed out that chaplaincy programs for atheists also exist.
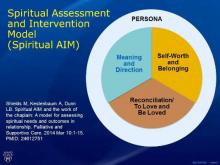
By observing a person’s behavior and conversing with him or her, paying close attention to the person’s attributions of blame, if any, and expressions of chief concerns, a chaplain will assess where on the continuum that person is in three key components of spiritual health: the need for meaning and direction, a sense of self-worth and belonging, and an ability to love and be loved. This latter component often is facilitated through seeking reconciliation when relationships are broken.
In the face of crisis, such as with terminal illness, one of those needs typically supersedes the others. This is what is known as the person’s “core spiritual need,” said Dr. Dunn, who also serves director of the university’s Geriatric Psychiatry Fellowship Training Program, and has extensive research and clinical experience evaluating and managing older adults with mood, anxiety, and cognitive disorders. As part of her research, she and her colleagues have developed a schematic called the Spiritual AIM (Spiritual Assessment and Intervention Model), which depicts those three concerns in relation to one another (Palliat Support Care. 2015 Feb;13:75-89).
Chaplains also are trained to rely on their own feelings about people, similar to the way in which psychiatrists use countertransference. “It is not intrapersonal; it is interpersonal,” Dr. Dunn said. “Healing happens in relationship, and the focus is on that relationship.”
Chaplains undergo standardized clinical pastoral training programs predicated on a combination of theological reflection and psychological theory, plus critique from professional peers and students.
“Their model is very similar to what we [geriatric psychiatrists] do when we assess a patient,” Dr. Dunn said. “We might be more structured trying to ferret out a diagnosis, but we’re assessing all the time.”
Depending on which aspect of spiritual health is most lacking, the chaplain will choose the role of either a “guide” to help with balancing the need for meaning and direction, a “valuer” to help restore feelings of worth and belonging, or a “truth-teller” who will explore with the patient ways he or she might have contributed to broken relationships, and actions the patient might take in order to heal them. This is all done within the context of an interdisciplinary team, Dr. Dunn said.
She and a team of researchers, including a chaplain, conducted a study of 31 advanced-stage adult cancer patients in an outpatient palliative care service, that measured self-reported changes in their spiritual, psychological, and physical symptoms both before and after Spiritual AIM sessions with a chaplain.
The need for balancing one of the three key components of spiritual health was determined by the chaplain to be fairly equal across the cohort, although just more than half of patients younger than 60 years of age struggled more with self-worth and belonging (P = .030). Those over 60 years were equally concerned with either reconciliation or meaning and direction (P less than .05). Two-thirds of the cohort were women, although a relationship between gender and spiritual assessment needs was not determined. Two-thirds also identified themselves as Christian, just over one-third were Jewish, and the rest identified as either Buddhist or nondenominational.
Using a variety of validated palliative care scales, such as the Edmonton Symptom Assessment Syndrome (ESAS) for physical complaints, the Center for Epidemiologic Studies Short Depression Scale, the Mini Mental Adjustment to Cancer scale (Mini-MAC), and the positive and negative RCOPE questionnaire for religious coping, among other scales, Dr. Dunn and her associates found that the change in baseline of overall spiritual health after intervention from the chaplain improved slightly in most measures. Mean baseline scores for the ESAS went from 25 to 24.4 post-intervention. The difference between baseline depression scores fell from 4.2 to 4.1.
Mini-MAC scores improved, particularly in “fighting spirit” and levels of fatalism (P = .084 and P = .036, respectively). In addition, maladaptive coping skills also improved (P = .018).The findings have helped Dr. Dunn in her work as a geriatric psychiatrist, especially when treating cancer patients, or in settings where there is not as much time for a full clinical assessment. “I think of patients in terms of their core needs and what I can do right now to help patients meet those needs.” Dr. Dunn cited, as an example, patients who feel like they don’t belong and are lonely. “If they’re in an assisted living home, can I get them to enter [the communal space]? That’s very different than thinking of them in terms only of depression.”
On Twitter @whitneymcknight
One reason chaplains are such a key part of the palliative care team is that they are seen by patients from a different perspective, Dr. Gurprit S. Lamba said. “Chaplains lend their ears, act as friends, and provide company to these patients,” Dr. Lamba said in an interview. “Discussing spiritual/religious matters helps these individuals cope better. Chaplains can provide more meaningful services with knowledge about different cultures, doctrines, and traditions, so that they can tailor their meetings accordingly.
“Studies have shown that psychiatrists are less religious and show less religious affiliation than their patients and than the population in general. As Dr. Dunn mentioned, chaplaincy programs for atheists also exist. Psychiatrists, with chaplains, can work with any individual to improve and optimize treatment. The critical part lies in assessment of patients’ religious views and spirituality along with their families’ opinions before offering meeting with chaplains.”
Dr. Lamba is a geriatric psychiatrist affiliated with BayRidge Hospital in Lynn, Mass.
One reason chaplains are such a key part of the palliative care team is that they are seen by patients from a different perspective, Dr. Gurprit S. Lamba said. “Chaplains lend their ears, act as friends, and provide company to these patients,” Dr. Lamba said in an interview. “Discussing spiritual/religious matters helps these individuals cope better. Chaplains can provide more meaningful services with knowledge about different cultures, doctrines, and traditions, so that they can tailor their meetings accordingly.
“Studies have shown that psychiatrists are less religious and show less religious affiliation than their patients and than the population in general. As Dr. Dunn mentioned, chaplaincy programs for atheists also exist. Psychiatrists, with chaplains, can work with any individual to improve and optimize treatment. The critical part lies in assessment of patients’ religious views and spirituality along with their families’ opinions before offering meeting with chaplains.”
Dr. Lamba is a geriatric psychiatrist affiliated with BayRidge Hospital in Lynn, Mass.
One reason chaplains are such a key part of the palliative care team is that they are seen by patients from a different perspective, Dr. Gurprit S. Lamba said. “Chaplains lend their ears, act as friends, and provide company to these patients,” Dr. Lamba said in an interview. “Discussing spiritual/religious matters helps these individuals cope better. Chaplains can provide more meaningful services with knowledge about different cultures, doctrines, and traditions, so that they can tailor their meetings accordingly.
“Studies have shown that psychiatrists are less religious and show less religious affiliation than their patients and than the population in general. As Dr. Dunn mentioned, chaplaincy programs for atheists also exist. Psychiatrists, with chaplains, can work with any individual to improve and optimize treatment. The critical part lies in assessment of patients’ religious views and spirituality along with their families’ opinions before offering meeting with chaplains.”
Dr. Lamba is a geriatric psychiatrist affiliated with BayRidge Hospital in Lynn, Mass.
WASHINGTON – Hospital chaplains are key partners in meeting the needs of palliative care patients and, as such, have much to offer psychiatry, according to an expert.
“I think we should work with chaplains,” Dr. Laura B. Dunn, professor of psychiatry and behavioral sciences at Stanford (Calif.) University, said in an interview at the annual meeting of the American Association for Geriatric Psychiatry. “It’s very helpful to know what they do, and for them to know what we do in terms of diagnosing and using a biopsychosocial model.”
Dr. Dunn said the relegation of chaplaincy and spiritual care in medicine has been unfortunate. After all, the level of a patient’s spiritual health is an inherent aspect of quality of life in palliative care, particularly for those over age 60 who often want help reconciling with loved ones, data collected by Dr. Dunn show. Viewing those patients in terms of their core needs rather than seeking a psychiatric diagnosis can make them more satisfied with their overall palliative care experience, she said.
How is spiritual health measured? There are few models and even fewer empirical studies, but Dr. Dunn said in addition learning how to deliver pastoral care, professional chaplains are trained to assess, intervene, and observe outcomes in spiritual health.
To begin with, spirituality is defined not in terms of “religiosity” but more as following an ethical path, similar to the idea of the Golden Rule or the ethic of reciprocity: Love your neighbor as yourself, in other words. The spiritual maturity to follow such a path requires the ability to love oneself that is balanced with a connection to others, and God, “if your belief includes God,” said Dr. Dunn, who pointed out that chaplaincy programs for atheists also exist.
By observing a person’s behavior and conversing with him or her, paying close attention to the person’s attributions of blame, if any, and expressions of chief concerns, a chaplain will assess where on the continuum that person is in three key components of spiritual health: the need for meaning and direction, a sense of self-worth and belonging, and an ability to love and be loved. This latter component often is facilitated through seeking reconciliation when relationships are broken.
In the face of crisis, such as with terminal illness, one of those needs typically supersedes the others. This is what is known as the person’s “core spiritual need,” said Dr. Dunn, who also serves director of the university’s Geriatric Psychiatry Fellowship Training Program, and has extensive research and clinical experience evaluating and managing older adults with mood, anxiety, and cognitive disorders. As part of her research, she and her colleagues have developed a schematic called the Spiritual AIM (Spiritual Assessment and Intervention Model), which depicts those three concerns in relation to one another (Palliat Support Care. 2015 Feb;13:75-89).
Chaplains also are trained to rely on their own feelings about people, similar to the way in which psychiatrists use countertransference. “It is not intrapersonal; it is interpersonal,” Dr. Dunn said. “Healing happens in relationship, and the focus is on that relationship.”
Chaplains undergo standardized clinical pastoral training programs predicated on a combination of theological reflection and psychological theory, plus critique from professional peers and students.
“Their model is very similar to what we [geriatric psychiatrists] do when we assess a patient,” Dr. Dunn said. “We might be more structured trying to ferret out a diagnosis, but we’re assessing all the time.”
Depending on which aspect of spiritual health is most lacking, the chaplain will choose the role of either a “guide” to help with balancing the need for meaning and direction, a “valuer” to help restore feelings of worth and belonging, or a “truth-teller” who will explore with the patient ways he or she might have contributed to broken relationships, and actions the patient might take in order to heal them. This is all done within the context of an interdisciplinary team, Dr. Dunn said.
She and a team of researchers, including a chaplain, conducted a study of 31 advanced-stage adult cancer patients in an outpatient palliative care service, that measured self-reported changes in their spiritual, psychological, and physical symptoms both before and after Spiritual AIM sessions with a chaplain.
The need for balancing one of the three key components of spiritual health was determined by the chaplain to be fairly equal across the cohort, although just more than half of patients younger than 60 years of age struggled more with self-worth and belonging (P = .030). Those over 60 years were equally concerned with either reconciliation or meaning and direction (P less than .05). Two-thirds of the cohort were women, although a relationship between gender and spiritual assessment needs was not determined. Two-thirds also identified themselves as Christian, just over one-third were Jewish, and the rest identified as either Buddhist or nondenominational.
Using a variety of validated palliative care scales, such as the Edmonton Symptom Assessment Syndrome (ESAS) for physical complaints, the Center for Epidemiologic Studies Short Depression Scale, the Mini Mental Adjustment to Cancer scale (Mini-MAC), and the positive and negative RCOPE questionnaire for religious coping, among other scales, Dr. Dunn and her associates found that the change in baseline of overall spiritual health after intervention from the chaplain improved slightly in most measures. Mean baseline scores for the ESAS went from 25 to 24.4 post-intervention. The difference between baseline depression scores fell from 4.2 to 4.1.
Mini-MAC scores improved, particularly in “fighting spirit” and levels of fatalism (P = .084 and P = .036, respectively). In addition, maladaptive coping skills also improved (P = .018).The findings have helped Dr. Dunn in her work as a geriatric psychiatrist, especially when treating cancer patients, or in settings where there is not as much time for a full clinical assessment. “I think of patients in terms of their core needs and what I can do right now to help patients meet those needs.” Dr. Dunn cited, as an example, patients who feel like they don’t belong and are lonely. “If they’re in an assisted living home, can I get them to enter [the communal space]? That’s very different than thinking of them in terms only of depression.”
On Twitter @whitneymcknight
WASHINGTON – Hospital chaplains are key partners in meeting the needs of palliative care patients and, as such, have much to offer psychiatry, according to an expert.
“I think we should work with chaplains,” Dr. Laura B. Dunn, professor of psychiatry and behavioral sciences at Stanford (Calif.) University, said in an interview at the annual meeting of the American Association for Geriatric Psychiatry. “It’s very helpful to know what they do, and for them to know what we do in terms of diagnosing and using a biopsychosocial model.”
Dr. Dunn said the relegation of chaplaincy and spiritual care in medicine has been unfortunate. After all, the level of a patient’s spiritual health is an inherent aspect of quality of life in palliative care, particularly for those over age 60 who often want help reconciling with loved ones, data collected by Dr. Dunn show. Viewing those patients in terms of their core needs rather than seeking a psychiatric diagnosis can make them more satisfied with their overall palliative care experience, she said.
How is spiritual health measured? There are few models and even fewer empirical studies, but Dr. Dunn said in addition learning how to deliver pastoral care, professional chaplains are trained to assess, intervene, and observe outcomes in spiritual health.
To begin with, spirituality is defined not in terms of “religiosity” but more as following an ethical path, similar to the idea of the Golden Rule or the ethic of reciprocity: Love your neighbor as yourself, in other words. The spiritual maturity to follow such a path requires the ability to love oneself that is balanced with a connection to others, and God, “if your belief includes God,” said Dr. Dunn, who pointed out that chaplaincy programs for atheists also exist.
By observing a person’s behavior and conversing with him or her, paying close attention to the person’s attributions of blame, if any, and expressions of chief concerns, a chaplain will assess where on the continuum that person is in three key components of spiritual health: the need for meaning and direction, a sense of self-worth and belonging, and an ability to love and be loved. This latter component often is facilitated through seeking reconciliation when relationships are broken.
In the face of crisis, such as with terminal illness, one of those needs typically supersedes the others. This is what is known as the person’s “core spiritual need,” said Dr. Dunn, who also serves director of the university’s Geriatric Psychiatry Fellowship Training Program, and has extensive research and clinical experience evaluating and managing older adults with mood, anxiety, and cognitive disorders. As part of her research, she and her colleagues have developed a schematic called the Spiritual AIM (Spiritual Assessment and Intervention Model), which depicts those three concerns in relation to one another (Palliat Support Care. 2015 Feb;13:75-89).
Chaplains also are trained to rely on their own feelings about people, similar to the way in which psychiatrists use countertransference. “It is not intrapersonal; it is interpersonal,” Dr. Dunn said. “Healing happens in relationship, and the focus is on that relationship.”
Chaplains undergo standardized clinical pastoral training programs predicated on a combination of theological reflection and psychological theory, plus critique from professional peers and students.
“Their model is very similar to what we [geriatric psychiatrists] do when we assess a patient,” Dr. Dunn said. “We might be more structured trying to ferret out a diagnosis, but we’re assessing all the time.”
Depending on which aspect of spiritual health is most lacking, the chaplain will choose the role of either a “guide” to help with balancing the need for meaning and direction, a “valuer” to help restore feelings of worth and belonging, or a “truth-teller” who will explore with the patient ways he or she might have contributed to broken relationships, and actions the patient might take in order to heal them. This is all done within the context of an interdisciplinary team, Dr. Dunn said.
She and a team of researchers, including a chaplain, conducted a study of 31 advanced-stage adult cancer patients in an outpatient palliative care service, that measured self-reported changes in their spiritual, psychological, and physical symptoms both before and after Spiritual AIM sessions with a chaplain.
The need for balancing one of the three key components of spiritual health was determined by the chaplain to be fairly equal across the cohort, although just more than half of patients younger than 60 years of age struggled more with self-worth and belonging (P = .030). Those over 60 years were equally concerned with either reconciliation or meaning and direction (P less than .05). Two-thirds of the cohort were women, although a relationship between gender and spiritual assessment needs was not determined. Two-thirds also identified themselves as Christian, just over one-third were Jewish, and the rest identified as either Buddhist or nondenominational.
Using a variety of validated palliative care scales, such as the Edmonton Symptom Assessment Syndrome (ESAS) for physical complaints, the Center for Epidemiologic Studies Short Depression Scale, the Mini Mental Adjustment to Cancer scale (Mini-MAC), and the positive and negative RCOPE questionnaire for religious coping, among other scales, Dr. Dunn and her associates found that the change in baseline of overall spiritual health after intervention from the chaplain improved slightly in most measures. Mean baseline scores for the ESAS went from 25 to 24.4 post-intervention. The difference between baseline depression scores fell from 4.2 to 4.1.
Mini-MAC scores improved, particularly in “fighting spirit” and levels of fatalism (P = .084 and P = .036, respectively). In addition, maladaptive coping skills also improved (P = .018).The findings have helped Dr. Dunn in her work as a geriatric psychiatrist, especially when treating cancer patients, or in settings where there is not as much time for a full clinical assessment. “I think of patients in terms of their core needs and what I can do right now to help patients meet those needs.” Dr. Dunn cited, as an example, patients who feel like they don’t belong and are lonely. “If they’re in an assisted living home, can I get them to enter [the communal space]? That’s very different than thinking of them in terms only of depression.”
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM AAGP 2016
Higher levels of function before hip fracture tied to greater fears of falling at 1 year
WASHINGTON – Fear of falling at 12 weeks was associated with poorer functional recovery up to 1 year after hip fracture, particularly if the person had a high level of function before the fracture, a study has shown.
Inherent in this fear is a tendency of the patient to limit his activities, which in turn affects his sense of balance, visual attention, and gait. This leads to an increased risk of further falls, according to Emily Bower, a doctoral candidate who presented the findings at the annual meeting of the American Association for Geriatric Psychiatry.
The study included 241 hip fracture patients, three-quarters of whom were female, with an average age of 77 years. All of the patients lived in the community, nearly all were able to participate in basic activities of daily living, and three-quarters could walk without assistance.
Patients were assessed for their level of functionality at week 4, week 12, week 26, and week 52, as well as their fear of falling using the Falls Efficacy Scale International (FES-I).
The investigators found that by week 52, 48% of all patients had reached full recovery of functional status. At week 12, 53% of all patients had FES-I scores indicating a lower fear of falling.
“That means that almost half of our participants were reporting high fear of falling 3 months after hip fracture, which is a substantial number when you consider that in the general population, fear of falling is reported by about one in five older adults,” Ms. Bower, who is enrolled at the San Diego State University/University of California, San Diego, joint doctoral program in clinical psychology, said in an interview.
At 1-year after fracture, for each 1 point increase in FES-I scores, the odds of reaching full recovery were lowered by 12% (P = .003). Meanwhile, in patients with low baseline levels of functioning, there was “no effect of fear of falling,” according to Ms. Bower.
The upshot is that for patients with high levels of functional independence prior to injury, more intervention may be required to bring them back to their levels of activity before the fracture, according to Ms. Bower, who suggested multicomponent activities that combine psychological, physical, and environmental factors, such as tai chi.
On Twitter @whitneymcknight
WASHINGTON – Fear of falling at 12 weeks was associated with poorer functional recovery up to 1 year after hip fracture, particularly if the person had a high level of function before the fracture, a study has shown.
Inherent in this fear is a tendency of the patient to limit his activities, which in turn affects his sense of balance, visual attention, and gait. This leads to an increased risk of further falls, according to Emily Bower, a doctoral candidate who presented the findings at the annual meeting of the American Association for Geriatric Psychiatry.
The study included 241 hip fracture patients, three-quarters of whom were female, with an average age of 77 years. All of the patients lived in the community, nearly all were able to participate in basic activities of daily living, and three-quarters could walk without assistance.
Patients were assessed for their level of functionality at week 4, week 12, week 26, and week 52, as well as their fear of falling using the Falls Efficacy Scale International (FES-I).
The investigators found that by week 52, 48% of all patients had reached full recovery of functional status. At week 12, 53% of all patients had FES-I scores indicating a lower fear of falling.
“That means that almost half of our participants were reporting high fear of falling 3 months after hip fracture, which is a substantial number when you consider that in the general population, fear of falling is reported by about one in five older adults,” Ms. Bower, who is enrolled at the San Diego State University/University of California, San Diego, joint doctoral program in clinical psychology, said in an interview.
At 1-year after fracture, for each 1 point increase in FES-I scores, the odds of reaching full recovery were lowered by 12% (P = .003). Meanwhile, in patients with low baseline levels of functioning, there was “no effect of fear of falling,” according to Ms. Bower.
The upshot is that for patients with high levels of functional independence prior to injury, more intervention may be required to bring them back to their levels of activity before the fracture, according to Ms. Bower, who suggested multicomponent activities that combine psychological, physical, and environmental factors, such as tai chi.
On Twitter @whitneymcknight
WASHINGTON – Fear of falling at 12 weeks was associated with poorer functional recovery up to 1 year after hip fracture, particularly if the person had a high level of function before the fracture, a study has shown.
Inherent in this fear is a tendency of the patient to limit his activities, which in turn affects his sense of balance, visual attention, and gait. This leads to an increased risk of further falls, according to Emily Bower, a doctoral candidate who presented the findings at the annual meeting of the American Association for Geriatric Psychiatry.
The study included 241 hip fracture patients, three-quarters of whom were female, with an average age of 77 years. All of the patients lived in the community, nearly all were able to participate in basic activities of daily living, and three-quarters could walk without assistance.
Patients were assessed for their level of functionality at week 4, week 12, week 26, and week 52, as well as their fear of falling using the Falls Efficacy Scale International (FES-I).
The investigators found that by week 52, 48% of all patients had reached full recovery of functional status. At week 12, 53% of all patients had FES-I scores indicating a lower fear of falling.
“That means that almost half of our participants were reporting high fear of falling 3 months after hip fracture, which is a substantial number when you consider that in the general population, fear of falling is reported by about one in five older adults,” Ms. Bower, who is enrolled at the San Diego State University/University of California, San Diego, joint doctoral program in clinical psychology, said in an interview.
At 1-year after fracture, for each 1 point increase in FES-I scores, the odds of reaching full recovery were lowered by 12% (P = .003). Meanwhile, in patients with low baseline levels of functioning, there was “no effect of fear of falling,” according to Ms. Bower.
The upshot is that for patients with high levels of functional independence prior to injury, more intervention may be required to bring them back to their levels of activity before the fracture, according to Ms. Bower, who suggested multicomponent activities that combine psychological, physical, and environmental factors, such as tai chi.
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM AAGP 2016