User login
Ready or not? Most ICUs not as prepared for disaster as they think
CHICAGO – When Superstorm Sandy was done barreling across New York City and the surrounding coast 14 months ago, flooding streets and knocking out power to millions, Dr. Laura Evans, director of the medical intensive care unit at Bellevue Hospital along the East River in Manhattan, emerged weary and wiser.
At one point, the ICU faced the real possibility of having just a handful of working power outlets to serve dozens of patients, and the number of crucial decisions to be made rose along with the water level. "Prior to the storm, disaster preparedness was not a core interest of mine, and it’s something I hope never to repeat," Dr. Evans told attendees at the annual meeting of the American College of Chest Physicians.
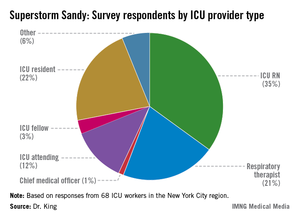
In a recent survey, ICU practitioners who endured havoc caused by Sandy in the New York City region reported having had little to no training in emergency evacuation care. "When I look at these data, I think there is a mismatch in terms of our self-perception of readiness compared to what patients actually require in an evacuation. It’s in stark contrast to the checklist we use every single day to put in a central venous catheter," said Dr. Mary Alice King, who presented her research as a copanelist with Dr. Evans. Dr. King is medical director of the pediatric trauma ICU at Harborview Medical Center in Seattle.
Contingency for loss of power
The nation’s oldest public hospital, Bellevue is adjacent to New York’s tidal East River. The river’s high tide the evening of Oct. 29, 2012, coincided with the arrival of the storm’s surge, and within minutes the hospital’s basement was inundated with 10 million gallons of seawater. And then the main power went out, taking with it the use of 32 elevators, the entire voice-over-Internet-protocol phone system, and the electronic medical records system, Dr. Evans said. The flood also knocked out the hospital’s ability to connect to its Internet servers. "We had very impaired means of communication," Dr. Evans said.
Survey data presented by Dr. King underscored that loss of power affects ICU functions in virtually all ways. The number one tool Dr. King’s survey respondents said they’d depended on most during their disaster response was their flashlights (24%); meanwhile, the top two items the respondents said they wished they’d had on hand were reliable phones, since, as at Bellevue, many of their phones were powered by voice-over-Internet protocols which, for most, went down with power outages; and backup electricity sources such as generators.
Leadership plan
Of the 68 survey respondents, 34% of whom were in evacuation leadership roles, Dr. King said only 23% admitted to having felt ill prepared to manage the pressure and details necessary to safely evacuate their patients. "As nonemergency department hospital providers, we receive little to no training on how to evacuate patients," said Dr. King.
In Bellevue’s case, Dr. Evans said that there was a leadership contingency already in place because of the hospital’s having been prepared the year before, when Hurricane Irene muscled its way up the Northeast’s Atlantic coast, also causing flooding and wind damage, though on a far smaller scare. "We had an ad hoc committee," said Dr. Evans. "Although we didn’t know exactly who would be on it because we didn’t know who would be there during the storm, we knew we would have medical, nursing, and ethical leaders to make resource allocation decisions." Most important about the leadership committee’s makeup, she said, was that ultimately, "none of us were directly involved in patient care, so none of us had the responsibility for being advocates. We wanted the attending physicians to be able to advocate for their patients."
The committee discerned that if backup generators failed, the ICU would have only six power outlets to depend on for its almost 60 patients. "The question was, whom would they be allocated for out of the 56 patients?
"Our responsibility was to make the wisest decisions about allocating a scarce resource," Dr. Evans said.
Practice the plan
Dry runs matter. "Forty-seven percent of survey respondents said that patient triage criteria were determined at the time of [the storm]," and a third of those surveyed said they weren’t aware of any triage criteria, Dr. King said.
And once plans are made, "it’s important to drill them," emphasized Dr. King’s copresenter Dr. Colin Grissom, associate medical director of the shock trauma ICU at Intermountain Medical Center, Murray, Utah. Superstorm Sandy, for all its havoc, came with some notice – the weather forecast. However, he pointed out that typically disasters happen without warning: "More than half of all hospital evacuations occur as a result of an internal event such as a fire or an intruder."
Also important to consider, said Dr. King, is that neonatal and pediatric ICUs have different evacuation needs from adult ones. "Regions should consider stockpiling neonatal transport ventilators and circuits," she said. "They should also consider designating pediatric disaster receiving hospitals, similar to burn disaster receiving hospitals."
Ethical considerations
At Bellevue, Dr. Evans said the hospital’s leadership planned patient triage according to influenza pandemic guidelines issued by the provincial government of Ontario, Canada, and the New York State Taskforce on Life and the Law guidelines for ventilator allocation during a public health disaster.
"We knew that if the disaster went very badly, we would be met with much criticism," said Dr. Evans, who joked that she was up nights worried about seeing her name skewered in local headlines: "I kept wondering, ‘What rhymes with Evans?’ "
Using the two sets of guidelines, both heavily oriented toward allocating ventilators, said Dr. Evans, "we did what we thought was ethical and fair. We made the best decisions we could."
The Ontario guidelines, she said, are predicated on Sequential Organ Failure Assessment (SOFA) scores. Just as the ad hoc committee determined that of the 56 patients in the census, there were "far more folks in the red (highest priority) and yellow (immediate priority) group than we had power outlets," the group received word that the protective housing around the generator fuel pumps had failed, and total loss of power was anticipated in 2 hours.
The committee reconfigured and, among other contingencies, began assigning coverage of two providers each to the bedside of every ventilated patient, and preparing nurses to count drops per minute of continuous medication.
The ‘bucket brigade’
Although the intensivists who’d participated in Superstorm Sandy evacuations said they felt most frustrated by the lack of communication during the event, 57% said that teamwork had been essential to the success of the evacuations.
"We work as teams in our units. That is something I think we bring as a real strength to ICU evacuations," said Dr. King.
And so it was at Bellevue.
"Due to the heroics of a lot of staff and volunteers, we did not have to execute this plan," said Dr. Evans. Instead, the "Bellevue bucket brigade," using 5-gallon jugs, formed a relay team stretching from the ground floor outside where the fuel tanks were, up to the 13th, where the backup generators were located. "The fuel tank up on the 13th floor was only accessible by stepladder, so someone had to climb up there and pour the fuel through a funnel," said Dr. Evans. "But because of this, we never lost backup power, and we successfully evacuated our hospital without complications to our patients."
Individualized plan key to success
While leadership and communication were essential, said Dr. Evans, she concluded that thinking through how existing guidelines can help was also key, but did not go far enough. "Unfortunately, no document can provide for all contingencies. Complete reliance on any [guidelines] is not good. You have to think about how you would individualize things to your own facility."
The survey was sponsored by the ACCP and conducted by Dr. King as part of her role on the ACCP’s mass critical care task force evacuation panel, which will issue a consensus on the topic sometime in early 2014.
Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Ten keys to ICU evacuation plan
When not under immediate threat
1) Create transport and other agreements with other facilities in region, including triage criteria.
2) Detail ICU evacuation plan, including vertical evacuation plan; simulate so all parties are familiar with their role, including those involved in patient transport.
3) Designate critical care leadership.
During imminent threat
4) Request assistance from regional facilities and appropriate agencies.
5) Ensure power and transportation resources are operable and in place.
6) Prioritize patients for evacuation.
During evacuation
7) Triage patients.
8) Include all patient information with patient.
9) Transport patients.
10) Track patients and all equipment.
Source: Dr. Colin Grissom
*This story has been updated 11/26/13
Dr. W. Michael Alberts, FCCP, comments: To paraphrase an old saying about insurance, "disaster preparedness is not needed until it is." Those health care facilities that have a clear documented plan and have drilled on the specifics are very pleased that they devoted time and effort when disaster strikes. While – knock on wood – the Moffitt Cancer Center here in Tampa has not needed our "Disaster Management Plan" (or as we in Florida say "Hurricane Management Plan") this year, it is only a matter of time and we’ll be ready when the need arises.
We urge you to review your plan before you need it.
Dr. W. Michael Alberts is chief medical officer, Moffitt Cancer Center, and professor of oncology and medicine at the University of South Florida, Tampa.
Dr. W. Michael Alberts, FCCP, comments: To paraphrase an old saying about insurance, "disaster preparedness is not needed until it is." Those health care facilities that have a clear documented plan and have drilled on the specifics are very pleased that they devoted time and effort when disaster strikes. While – knock on wood – the Moffitt Cancer Center here in Tampa has not needed our "Disaster Management Plan" (or as we in Florida say "Hurricane Management Plan") this year, it is only a matter of time and we’ll be ready when the need arises.
We urge you to review your plan before you need it.
Dr. W. Michael Alberts is chief medical officer, Moffitt Cancer Center, and professor of oncology and medicine at the University of South Florida, Tampa.
Dr. W. Michael Alberts, FCCP, comments: To paraphrase an old saying about insurance, "disaster preparedness is not needed until it is." Those health care facilities that have a clear documented plan and have drilled on the specifics are very pleased that they devoted time and effort when disaster strikes. While – knock on wood – the Moffitt Cancer Center here in Tampa has not needed our "Disaster Management Plan" (or as we in Florida say "Hurricane Management Plan") this year, it is only a matter of time and we’ll be ready when the need arises.
We urge you to review your plan before you need it.
Dr. W. Michael Alberts is chief medical officer, Moffitt Cancer Center, and professor of oncology and medicine at the University of South Florida, Tampa.
CHICAGO – When Superstorm Sandy was done barreling across New York City and the surrounding coast 14 months ago, flooding streets and knocking out power to millions, Dr. Laura Evans, director of the medical intensive care unit at Bellevue Hospital along the East River in Manhattan, emerged weary and wiser.
At one point, the ICU faced the real possibility of having just a handful of working power outlets to serve dozens of patients, and the number of crucial decisions to be made rose along with the water level. "Prior to the storm, disaster preparedness was not a core interest of mine, and it’s something I hope never to repeat," Dr. Evans told attendees at the annual meeting of the American College of Chest Physicians.
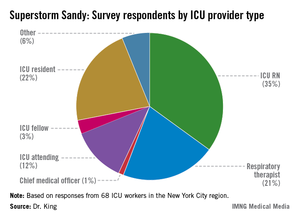
In a recent survey, ICU practitioners who endured havoc caused by Sandy in the New York City region reported having had little to no training in emergency evacuation care. "When I look at these data, I think there is a mismatch in terms of our self-perception of readiness compared to what patients actually require in an evacuation. It’s in stark contrast to the checklist we use every single day to put in a central venous catheter," said Dr. Mary Alice King, who presented her research as a copanelist with Dr. Evans. Dr. King is medical director of the pediatric trauma ICU at Harborview Medical Center in Seattle.
Contingency for loss of power
The nation’s oldest public hospital, Bellevue is adjacent to New York’s tidal East River. The river’s high tide the evening of Oct. 29, 2012, coincided with the arrival of the storm’s surge, and within minutes the hospital’s basement was inundated with 10 million gallons of seawater. And then the main power went out, taking with it the use of 32 elevators, the entire voice-over-Internet-protocol phone system, and the electronic medical records system, Dr. Evans said. The flood also knocked out the hospital’s ability to connect to its Internet servers. "We had very impaired means of communication," Dr. Evans said.
Survey data presented by Dr. King underscored that loss of power affects ICU functions in virtually all ways. The number one tool Dr. King’s survey respondents said they’d depended on most during their disaster response was their flashlights (24%); meanwhile, the top two items the respondents said they wished they’d had on hand were reliable phones, since, as at Bellevue, many of their phones were powered by voice-over-Internet protocols which, for most, went down with power outages; and backup electricity sources such as generators.
Leadership plan
Of the 68 survey respondents, 34% of whom were in evacuation leadership roles, Dr. King said only 23% admitted to having felt ill prepared to manage the pressure and details necessary to safely evacuate their patients. "As nonemergency department hospital providers, we receive little to no training on how to evacuate patients," said Dr. King.
In Bellevue’s case, Dr. Evans said that there was a leadership contingency already in place because of the hospital’s having been prepared the year before, when Hurricane Irene muscled its way up the Northeast’s Atlantic coast, also causing flooding and wind damage, though on a far smaller scare. "We had an ad hoc committee," said Dr. Evans. "Although we didn’t know exactly who would be on it because we didn’t know who would be there during the storm, we knew we would have medical, nursing, and ethical leaders to make resource allocation decisions." Most important about the leadership committee’s makeup, she said, was that ultimately, "none of us were directly involved in patient care, so none of us had the responsibility for being advocates. We wanted the attending physicians to be able to advocate for their patients."
The committee discerned that if backup generators failed, the ICU would have only six power outlets to depend on for its almost 60 patients. "The question was, whom would they be allocated for out of the 56 patients?
"Our responsibility was to make the wisest decisions about allocating a scarce resource," Dr. Evans said.
Practice the plan
Dry runs matter. "Forty-seven percent of survey respondents said that patient triage criteria were determined at the time of [the storm]," and a third of those surveyed said they weren’t aware of any triage criteria, Dr. King said.
And once plans are made, "it’s important to drill them," emphasized Dr. King’s copresenter Dr. Colin Grissom, associate medical director of the shock trauma ICU at Intermountain Medical Center, Murray, Utah. Superstorm Sandy, for all its havoc, came with some notice – the weather forecast. However, he pointed out that typically disasters happen without warning: "More than half of all hospital evacuations occur as a result of an internal event such as a fire or an intruder."
Also important to consider, said Dr. King, is that neonatal and pediatric ICUs have different evacuation needs from adult ones. "Regions should consider stockpiling neonatal transport ventilators and circuits," she said. "They should also consider designating pediatric disaster receiving hospitals, similar to burn disaster receiving hospitals."
Ethical considerations
At Bellevue, Dr. Evans said the hospital’s leadership planned patient triage according to influenza pandemic guidelines issued by the provincial government of Ontario, Canada, and the New York State Taskforce on Life and the Law guidelines for ventilator allocation during a public health disaster.
"We knew that if the disaster went very badly, we would be met with much criticism," said Dr. Evans, who joked that she was up nights worried about seeing her name skewered in local headlines: "I kept wondering, ‘What rhymes with Evans?’ "
Using the two sets of guidelines, both heavily oriented toward allocating ventilators, said Dr. Evans, "we did what we thought was ethical and fair. We made the best decisions we could."
The Ontario guidelines, she said, are predicated on Sequential Organ Failure Assessment (SOFA) scores. Just as the ad hoc committee determined that of the 56 patients in the census, there were "far more folks in the red (highest priority) and yellow (immediate priority) group than we had power outlets," the group received word that the protective housing around the generator fuel pumps had failed, and total loss of power was anticipated in 2 hours.
The committee reconfigured and, among other contingencies, began assigning coverage of two providers each to the bedside of every ventilated patient, and preparing nurses to count drops per minute of continuous medication.
The ‘bucket brigade’
Although the intensivists who’d participated in Superstorm Sandy evacuations said they felt most frustrated by the lack of communication during the event, 57% said that teamwork had been essential to the success of the evacuations.
"We work as teams in our units. That is something I think we bring as a real strength to ICU evacuations," said Dr. King.
And so it was at Bellevue.
"Due to the heroics of a lot of staff and volunteers, we did not have to execute this plan," said Dr. Evans. Instead, the "Bellevue bucket brigade," using 5-gallon jugs, formed a relay team stretching from the ground floor outside where the fuel tanks were, up to the 13th, where the backup generators were located. "The fuel tank up on the 13th floor was only accessible by stepladder, so someone had to climb up there and pour the fuel through a funnel," said Dr. Evans. "But because of this, we never lost backup power, and we successfully evacuated our hospital without complications to our patients."
Individualized plan key to success
While leadership and communication were essential, said Dr. Evans, she concluded that thinking through how existing guidelines can help was also key, but did not go far enough. "Unfortunately, no document can provide for all contingencies. Complete reliance on any [guidelines] is not good. You have to think about how you would individualize things to your own facility."
The survey was sponsored by the ACCP and conducted by Dr. King as part of her role on the ACCP’s mass critical care task force evacuation panel, which will issue a consensus on the topic sometime in early 2014.
Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Ten keys to ICU evacuation plan
When not under immediate threat
1) Create transport and other agreements with other facilities in region, including triage criteria.
2) Detail ICU evacuation plan, including vertical evacuation plan; simulate so all parties are familiar with their role, including those involved in patient transport.
3) Designate critical care leadership.
During imminent threat
4) Request assistance from regional facilities and appropriate agencies.
5) Ensure power and transportation resources are operable and in place.
6) Prioritize patients for evacuation.
During evacuation
7) Triage patients.
8) Include all patient information with patient.
9) Transport patients.
10) Track patients and all equipment.
Source: Dr. Colin Grissom
*This story has been updated 11/26/13
CHICAGO – When Superstorm Sandy was done barreling across New York City and the surrounding coast 14 months ago, flooding streets and knocking out power to millions, Dr. Laura Evans, director of the medical intensive care unit at Bellevue Hospital along the East River in Manhattan, emerged weary and wiser.
At one point, the ICU faced the real possibility of having just a handful of working power outlets to serve dozens of patients, and the number of crucial decisions to be made rose along with the water level. "Prior to the storm, disaster preparedness was not a core interest of mine, and it’s something I hope never to repeat," Dr. Evans told attendees at the annual meeting of the American College of Chest Physicians.
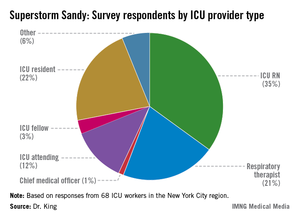
In a recent survey, ICU practitioners who endured havoc caused by Sandy in the New York City region reported having had little to no training in emergency evacuation care. "When I look at these data, I think there is a mismatch in terms of our self-perception of readiness compared to what patients actually require in an evacuation. It’s in stark contrast to the checklist we use every single day to put in a central venous catheter," said Dr. Mary Alice King, who presented her research as a copanelist with Dr. Evans. Dr. King is medical director of the pediatric trauma ICU at Harborview Medical Center in Seattle.
Contingency for loss of power
The nation’s oldest public hospital, Bellevue is adjacent to New York’s tidal East River. The river’s high tide the evening of Oct. 29, 2012, coincided with the arrival of the storm’s surge, and within minutes the hospital’s basement was inundated with 10 million gallons of seawater. And then the main power went out, taking with it the use of 32 elevators, the entire voice-over-Internet-protocol phone system, and the electronic medical records system, Dr. Evans said. The flood also knocked out the hospital’s ability to connect to its Internet servers. "We had very impaired means of communication," Dr. Evans said.
Survey data presented by Dr. King underscored that loss of power affects ICU functions in virtually all ways. The number one tool Dr. King’s survey respondents said they’d depended on most during their disaster response was their flashlights (24%); meanwhile, the top two items the respondents said they wished they’d had on hand were reliable phones, since, as at Bellevue, many of their phones were powered by voice-over-Internet protocols which, for most, went down with power outages; and backup electricity sources such as generators.
Leadership plan
Of the 68 survey respondents, 34% of whom were in evacuation leadership roles, Dr. King said only 23% admitted to having felt ill prepared to manage the pressure and details necessary to safely evacuate their patients. "As nonemergency department hospital providers, we receive little to no training on how to evacuate patients," said Dr. King.
In Bellevue’s case, Dr. Evans said that there was a leadership contingency already in place because of the hospital’s having been prepared the year before, when Hurricane Irene muscled its way up the Northeast’s Atlantic coast, also causing flooding and wind damage, though on a far smaller scare. "We had an ad hoc committee," said Dr. Evans. "Although we didn’t know exactly who would be on it because we didn’t know who would be there during the storm, we knew we would have medical, nursing, and ethical leaders to make resource allocation decisions." Most important about the leadership committee’s makeup, she said, was that ultimately, "none of us were directly involved in patient care, so none of us had the responsibility for being advocates. We wanted the attending physicians to be able to advocate for their patients."
The committee discerned that if backup generators failed, the ICU would have only six power outlets to depend on for its almost 60 patients. "The question was, whom would they be allocated for out of the 56 patients?
"Our responsibility was to make the wisest decisions about allocating a scarce resource," Dr. Evans said.
Practice the plan
Dry runs matter. "Forty-seven percent of survey respondents said that patient triage criteria were determined at the time of [the storm]," and a third of those surveyed said they weren’t aware of any triage criteria, Dr. King said.
And once plans are made, "it’s important to drill them," emphasized Dr. King’s copresenter Dr. Colin Grissom, associate medical director of the shock trauma ICU at Intermountain Medical Center, Murray, Utah. Superstorm Sandy, for all its havoc, came with some notice – the weather forecast. However, he pointed out that typically disasters happen without warning: "More than half of all hospital evacuations occur as a result of an internal event such as a fire or an intruder."
Also important to consider, said Dr. King, is that neonatal and pediatric ICUs have different evacuation needs from adult ones. "Regions should consider stockpiling neonatal transport ventilators and circuits," she said. "They should also consider designating pediatric disaster receiving hospitals, similar to burn disaster receiving hospitals."
Ethical considerations
At Bellevue, Dr. Evans said the hospital’s leadership planned patient triage according to influenza pandemic guidelines issued by the provincial government of Ontario, Canada, and the New York State Taskforce on Life and the Law guidelines for ventilator allocation during a public health disaster.
"We knew that if the disaster went very badly, we would be met with much criticism," said Dr. Evans, who joked that she was up nights worried about seeing her name skewered in local headlines: "I kept wondering, ‘What rhymes with Evans?’ "
Using the two sets of guidelines, both heavily oriented toward allocating ventilators, said Dr. Evans, "we did what we thought was ethical and fair. We made the best decisions we could."
The Ontario guidelines, she said, are predicated on Sequential Organ Failure Assessment (SOFA) scores. Just as the ad hoc committee determined that of the 56 patients in the census, there were "far more folks in the red (highest priority) and yellow (immediate priority) group than we had power outlets," the group received word that the protective housing around the generator fuel pumps had failed, and total loss of power was anticipated in 2 hours.
The committee reconfigured and, among other contingencies, began assigning coverage of two providers each to the bedside of every ventilated patient, and preparing nurses to count drops per minute of continuous medication.
The ‘bucket brigade’
Although the intensivists who’d participated in Superstorm Sandy evacuations said they felt most frustrated by the lack of communication during the event, 57% said that teamwork had been essential to the success of the evacuations.
"We work as teams in our units. That is something I think we bring as a real strength to ICU evacuations," said Dr. King.
And so it was at Bellevue.
"Due to the heroics of a lot of staff and volunteers, we did not have to execute this plan," said Dr. Evans. Instead, the "Bellevue bucket brigade," using 5-gallon jugs, formed a relay team stretching from the ground floor outside where the fuel tanks were, up to the 13th, where the backup generators were located. "The fuel tank up on the 13th floor was only accessible by stepladder, so someone had to climb up there and pour the fuel through a funnel," said Dr. Evans. "But because of this, we never lost backup power, and we successfully evacuated our hospital without complications to our patients."
Individualized plan key to success
While leadership and communication were essential, said Dr. Evans, she concluded that thinking through how existing guidelines can help was also key, but did not go far enough. "Unfortunately, no document can provide for all contingencies. Complete reliance on any [guidelines] is not good. You have to think about how you would individualize things to your own facility."
The survey was sponsored by the ACCP and conducted by Dr. King as part of her role on the ACCP’s mass critical care task force evacuation panel, which will issue a consensus on the topic sometime in early 2014.
Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Ten keys to ICU evacuation plan
When not under immediate threat
1) Create transport and other agreements with other facilities in region, including triage criteria.
2) Detail ICU evacuation plan, including vertical evacuation plan; simulate so all parties are familiar with their role, including those involved in patient transport.
3) Designate critical care leadership.
During imminent threat
4) Request assistance from regional facilities and appropriate agencies.
5) Ensure power and transportation resources are operable and in place.
6) Prioritize patients for evacuation.
During evacuation
7) Triage patients.
8) Include all patient information with patient.
9) Transport patients.
10) Track patients and all equipment.
Source: Dr. Colin Grissom
*This story has been updated 11/26/13
EXPERT ANALYSIS FROM CHEST 2013
Major finding: Although 78% of ICU staff had never performed a vertical ICU evacuation drill, only 23% admitted to feeling "inadequately trained" during Superstorm Sandy evacuations.
Data source: Survey of 68 ICU workers in the New York City region, all of whom worked through Superstorm Sandy.
Disclosures: Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Electrocautery incision of lymph nodes improved biopsy yield
Endobronchial ultrasound–guided biopsies made after an electrocautery incision to the lymph node improved biopsy yields from 39% to 71% in 38 nodes, according to a small study presented at the annual meeting of the American College of Chest Physicians meeting.
"Because it is not always possible to pass biopsy forceps through defects in the lymph node – the literature indicates a failure rate of between 10% and 29% – we developed a novel technique," said presenter Dr. Kyle Bramley of Yale University, New Haven, Conn.
The technique employs EBUS, and involves passing an electrocautery knife activated at 40 W through the working channel of the scope in order to make an incision in the bronchial wall and enlarge the defect in the lymph node. This facilitates passage of the forceps into the node so that a larger biopsy sample can be obtained.
To test their technique, Dr. Bramley and his colleagues designed a prospective observational cohort study at a single tertiary academic medical center. Twenty patients (mean age, 68 years), including 11 women, who were undergoing EBUS were enrolled. An associated lung mass was present in 14 (70%) of the participants; 6 (30%) had isolated lymphadenopathy. One patient had prior lymphoma, and two others had prior lung cancer.
The researchers evaluated 68 nodes in all; 19 patients had nodes greater than 9 mm. Cautery was only used when initial attempts failed to biopsy nodes 9 mm or larger using EBUS-guided miniforceps of 1.2 mm.
The average node size biopsied using EBUS-transbronchial needle aspiration (EBUS-TBNA) was 5.7 mm. The average forceps-biopsied node was 15.8 mm.
In all, 23 nodes were biopsied successfully on the first pass using EBUS-TBNA only. The biopsies yielded diagnostic material such as lymphocytes, malignancy, or granulomas in 15 of these nodes.
Of the 15 nodes that required cautery, 12 yielded diagnostic material, and 3 had no diagnostic material.
The overall yield increased from 39% (15 out of 38) without cautery to 71% (27 out of 38) when cautery was used.
Notably, four patients had clinically relevant discrepancies between their cytologies and histopathologies. "In all four, TBNA provided a definitive diagnosis," said Dr. Bramley. "The forceps provided fibroconnective tissue or necrotic debris."
These results did not negate the efficacy of the cautery technique, according to Dr. Bramley. "We think we had a forceps issue ... the 1.2 mm are flexible, but they were unable to push all the way through a tough lymph node capsule."
Dr. Bramley also said that other factors, including the operator learning curve, the smaller size of the nodes the investigators attempted to biopsy, and the "nonideal" population they were studying, contributed to these results.
He and his colleagues have since adjusted the procedure to make cauterization routine and to include a 1.9-mm transbronchial biopsy forceps needle, "which, incidentally, is a lot less expensive than the larger forceps we’d been using," he said.
Although more study is needed, Dr. Bramley said he and his team believed that this technique would be appropriate for future use in isolated mediastinal lymphadenopathy, especially with a low suspicion of non–small cell lung carcinoma; evaluation of lymphoma; and clinical trials requiring core biopsy.
Dr. Bramley had no relevant disclosures.
Dr. Frank Podbielski, FCCP, comments: The authors have again proven that a larger pathology specimen obtained at the time of biopsy significantly improves diagnostic accuracy, especially in the setting of mediastinal nodes that are difficult to access and thus require an electrocautery incision through the airway in concert with EBUS guidance.
Dr. Francis J. Podbielski leads the Lung Cancer Program at Jordan Hospital in Plymouth, Mass.
Dr. Frank Podbielski, FCCP, comments: The authors have again proven that a larger pathology specimen obtained at the time of biopsy significantly improves diagnostic accuracy, especially in the setting of mediastinal nodes that are difficult to access and thus require an electrocautery incision through the airway in concert with EBUS guidance.
Dr. Francis J. Podbielski leads the Lung Cancer Program at Jordan Hospital in Plymouth, Mass.
Dr. Frank Podbielski, FCCP, comments: The authors have again proven that a larger pathology specimen obtained at the time of biopsy significantly improves diagnostic accuracy, especially in the setting of mediastinal nodes that are difficult to access and thus require an electrocautery incision through the airway in concert with EBUS guidance.
Dr. Francis J. Podbielski leads the Lung Cancer Program at Jordan Hospital in Plymouth, Mass.
Endobronchial ultrasound–guided biopsies made after an electrocautery incision to the lymph node improved biopsy yields from 39% to 71% in 38 nodes, according to a small study presented at the annual meeting of the American College of Chest Physicians meeting.
"Because it is not always possible to pass biopsy forceps through defects in the lymph node – the literature indicates a failure rate of between 10% and 29% – we developed a novel technique," said presenter Dr. Kyle Bramley of Yale University, New Haven, Conn.
The technique employs EBUS, and involves passing an electrocautery knife activated at 40 W through the working channel of the scope in order to make an incision in the bronchial wall and enlarge the defect in the lymph node. This facilitates passage of the forceps into the node so that a larger biopsy sample can be obtained.
To test their technique, Dr. Bramley and his colleagues designed a prospective observational cohort study at a single tertiary academic medical center. Twenty patients (mean age, 68 years), including 11 women, who were undergoing EBUS were enrolled. An associated lung mass was present in 14 (70%) of the participants; 6 (30%) had isolated lymphadenopathy. One patient had prior lymphoma, and two others had prior lung cancer.
The researchers evaluated 68 nodes in all; 19 patients had nodes greater than 9 mm. Cautery was only used when initial attempts failed to biopsy nodes 9 mm or larger using EBUS-guided miniforceps of 1.2 mm.
The average node size biopsied using EBUS-transbronchial needle aspiration (EBUS-TBNA) was 5.7 mm. The average forceps-biopsied node was 15.8 mm.
In all, 23 nodes were biopsied successfully on the first pass using EBUS-TBNA only. The biopsies yielded diagnostic material such as lymphocytes, malignancy, or granulomas in 15 of these nodes.
Of the 15 nodes that required cautery, 12 yielded diagnostic material, and 3 had no diagnostic material.
The overall yield increased from 39% (15 out of 38) without cautery to 71% (27 out of 38) when cautery was used.
Notably, four patients had clinically relevant discrepancies between their cytologies and histopathologies. "In all four, TBNA provided a definitive diagnosis," said Dr. Bramley. "The forceps provided fibroconnective tissue or necrotic debris."
These results did not negate the efficacy of the cautery technique, according to Dr. Bramley. "We think we had a forceps issue ... the 1.2 mm are flexible, but they were unable to push all the way through a tough lymph node capsule."
Dr. Bramley also said that other factors, including the operator learning curve, the smaller size of the nodes the investigators attempted to biopsy, and the "nonideal" population they were studying, contributed to these results.
He and his colleagues have since adjusted the procedure to make cauterization routine and to include a 1.9-mm transbronchial biopsy forceps needle, "which, incidentally, is a lot less expensive than the larger forceps we’d been using," he said.
Although more study is needed, Dr. Bramley said he and his team believed that this technique would be appropriate for future use in isolated mediastinal lymphadenopathy, especially with a low suspicion of non–small cell lung carcinoma; evaluation of lymphoma; and clinical trials requiring core biopsy.
Dr. Bramley had no relevant disclosures.
Endobronchial ultrasound–guided biopsies made after an electrocautery incision to the lymph node improved biopsy yields from 39% to 71% in 38 nodes, according to a small study presented at the annual meeting of the American College of Chest Physicians meeting.
"Because it is not always possible to pass biopsy forceps through defects in the lymph node – the literature indicates a failure rate of between 10% and 29% – we developed a novel technique," said presenter Dr. Kyle Bramley of Yale University, New Haven, Conn.
The technique employs EBUS, and involves passing an electrocautery knife activated at 40 W through the working channel of the scope in order to make an incision in the bronchial wall and enlarge the defect in the lymph node. This facilitates passage of the forceps into the node so that a larger biopsy sample can be obtained.
To test their technique, Dr. Bramley and his colleagues designed a prospective observational cohort study at a single tertiary academic medical center. Twenty patients (mean age, 68 years), including 11 women, who were undergoing EBUS were enrolled. An associated lung mass was present in 14 (70%) of the participants; 6 (30%) had isolated lymphadenopathy. One patient had prior lymphoma, and two others had prior lung cancer.
The researchers evaluated 68 nodes in all; 19 patients had nodes greater than 9 mm. Cautery was only used when initial attempts failed to biopsy nodes 9 mm or larger using EBUS-guided miniforceps of 1.2 mm.
The average node size biopsied using EBUS-transbronchial needle aspiration (EBUS-TBNA) was 5.7 mm. The average forceps-biopsied node was 15.8 mm.
In all, 23 nodes were biopsied successfully on the first pass using EBUS-TBNA only. The biopsies yielded diagnostic material such as lymphocytes, malignancy, or granulomas in 15 of these nodes.
Of the 15 nodes that required cautery, 12 yielded diagnostic material, and 3 had no diagnostic material.
The overall yield increased from 39% (15 out of 38) without cautery to 71% (27 out of 38) when cautery was used.
Notably, four patients had clinically relevant discrepancies between their cytologies and histopathologies. "In all four, TBNA provided a definitive diagnosis," said Dr. Bramley. "The forceps provided fibroconnective tissue or necrotic debris."
These results did not negate the efficacy of the cautery technique, according to Dr. Bramley. "We think we had a forceps issue ... the 1.2 mm are flexible, but they were unable to push all the way through a tough lymph node capsule."
Dr. Bramley also said that other factors, including the operator learning curve, the smaller size of the nodes the investigators attempted to biopsy, and the "nonideal" population they were studying, contributed to these results.
He and his colleagues have since adjusted the procedure to make cauterization routine and to include a 1.9-mm transbronchial biopsy forceps needle, "which, incidentally, is a lot less expensive than the larger forceps we’d been using," he said.
Although more study is needed, Dr. Bramley said he and his team believed that this technique would be appropriate for future use in isolated mediastinal lymphadenopathy, especially with a low suspicion of non–small cell lung carcinoma; evaluation of lymphoma; and clinical trials requiring core biopsy.
Dr. Bramley had no relevant disclosures.
Major finding: EBUS-guided lymph node biopsies made after electrocautery incision improved biopsy yields from 39% to 71% in 38 lymph nodes.
Data source: Prospective observational cohort study of 20 patients at a single tertiary academic medical center.
Disclosures: Dr. Bramley had no relevant disclosures.
Embracing change is the only option in ACA era
CHICAGO – The Affordable Care Act may still be stumbling into place, but it’s here to stay, bringing with it changes especially acute for private physicians.
That’s the consensus of a panel of experts who presented their perspective on the impact of "Obamacare" at this year’s annual meeting of the American College of Chest Physicians.
"Younger physicians are more supportive of the ACA than older physicians," said to Dr. Akram Khan of Oregon Health & Science University, Portland, referencing a survey that found 80% of physicians between 25 and 39 years were optimistic about the future of health care in America. "Older physicians have adapted to the fee-for-service system we currently are in, and so are more ambivalent about the effects of the ACA than [the younger generation] than younger physicians who have not adapted to the system yet."
Private practitioners pay more
Regardless of the number of years in practice, Dr. Edward J. Diamond told the audience that even though he had tried to "dig my head in the sand and tried not to think about this, but unfortunately we are compelled to address it."
The president of large, multisite pulmonary practice in suburban Chicago, Dr. Diamond listed some of the pressing concerns he said should be on the minds of all private physicians, who are almost always employers as well.
The first concern he noted was abiding by the ACA mandate that employee premiums do not exceed 9.5% of the employee’s gross income, and that employer-sponsored plans share at least 60% of the total cost.
Because the cost of private insurance is tied to that of public exchange enrollment and are therefore fluid, Dr. Diamond said this equates with "an enormous administrative burden. We as employers are now going to have to monitor the marketplace of health plans because we’re going to have to compare what we’re offering our employees to what they can get in an insurance exchange."
Further complicating coverage, he said, would be the need to tier coverage to accommodate the variances in office and medical staff salaries vis-à-vis the ACA’s definition of affordability.
Drag on system "real"
Dr. Mark Levine, chief medical officer for the Denver office of the Centers for Medicare and Medicaid Services, said that despite the multitudinous problems with the official ACA website, healthcare.gov, "It really does make comparisons of health plans much easier." He added that only "qualified health plans are listed, which means that they are of known benefit structure and quality."
Regarding the ACA’s direct effect on patient care, Dr. Diamond said that while practices that can accommodate a larger patient load will benefit, quality likely will suffer in practices that are already operating at capacity.
"You’ll be seeing patients that are more complex because they were uninsured in the past and have multiple medical problems," he said, adding that this will take more time and will be reimbursed at lower rates than was done previously.
Dr. Levine concurred, "There will be a drag on the system at first" because of the surge in patients with complex medical needs left untreated by their previously uninsured status.
"Perhaps everybody else needs to chip in to account for that and for the kind of cost shifting we have seen and these phantom pricing mechanisms that have been so common in American health care," said Dr. Levine. "The lack of coverage to a needy population is only going to exacerbate the systemic concerns."
Regardless of burdens shouldered, plenty of Americans will remain needy, according to Dr. Jonathan Pak, also of the Oregon Health & Science University.
"The goal is to get everyone insured, but we will be nowhere close to that 10 years into the future," he said, citing data released by the Congressional Budget Office earlier this year, indicating that in the year 2022, 31 million will remain uninsured. "Make no mistake, this is not a universal health care plan."
Impact on critical care
The ACA might actually benefit the bottom lines of hospitalists and intensivists, said Dr. Diamond. "In the critical care arena, you’re going to have an improved payer mix, you’re going to have the same number of patients, and you have a business model [in which] you don’t have clerical staff," he said.
Dr. Pak had a different view. Already shrinking numbers of critical care resources such as beds and critical care staff likely will be further stressed under the ACA, forcing up per-bed costs and exacerbating shortages of intensivists. "I think, despite many improvements, it won’t be very long before we have to face structural health reform all over again."
Still, Dr. Pak said there are some reasons to feel hopeful. "The ACA will relieve the suffering of millions and will potentially reduce the number of people who end up in the ICU because of better primary care," he said, among other benefits such as the ACA’s increased funding for critical care research.
"Think aggressively"
"It’s serious. You’ve got to cut costs," said Dr. Diamond, who said it was a good time to be a nurse practitioner or a physician assistant, as they are more in demand than are high-salary specialists.
Having appropriate software to improve efficiencies is also essential to the new world of ACA, said Dr. Diamond. "What is coming is clinical integration," he said, referring to ACA mandates on collecting patient and financial data. "You’re also going to be measured on a daily basis on clinical protocols, so you need to be thinking about this very aggressively. How will you have the IT to support what you’ve got to do?"
Included in this overhaul, said Dr. Diamond, must be an attitude change toward working with other providers, including local hospitals and pharmacies, in order to decrease the variation of practice and adhere to evidence-based medicine protocols and national guidelines.
Dr. Levine defended the ACA saying that the current system is "unsustainable" and that for the first time, portions of the ACA such as value-based purchasing, "which holds groups of people responsible" would help the CMS implement its 5-year plan for Americans to have "Better care, better health, and lower costs."
"The past is past," said Dr. Diamond. "You have to embrace change."
CHICAGO – The Affordable Care Act may still be stumbling into place, but it’s here to stay, bringing with it changes especially acute for private physicians.
That’s the consensus of a panel of experts who presented their perspective on the impact of "Obamacare" at this year’s annual meeting of the American College of Chest Physicians.
"Younger physicians are more supportive of the ACA than older physicians," said to Dr. Akram Khan of Oregon Health & Science University, Portland, referencing a survey that found 80% of physicians between 25 and 39 years were optimistic about the future of health care in America. "Older physicians have adapted to the fee-for-service system we currently are in, and so are more ambivalent about the effects of the ACA than [the younger generation] than younger physicians who have not adapted to the system yet."
Private practitioners pay more
Regardless of the number of years in practice, Dr. Edward J. Diamond told the audience that even though he had tried to "dig my head in the sand and tried not to think about this, but unfortunately we are compelled to address it."
The president of large, multisite pulmonary practice in suburban Chicago, Dr. Diamond listed some of the pressing concerns he said should be on the minds of all private physicians, who are almost always employers as well.
The first concern he noted was abiding by the ACA mandate that employee premiums do not exceed 9.5% of the employee’s gross income, and that employer-sponsored plans share at least 60% of the total cost.
Because the cost of private insurance is tied to that of public exchange enrollment and are therefore fluid, Dr. Diamond said this equates with "an enormous administrative burden. We as employers are now going to have to monitor the marketplace of health plans because we’re going to have to compare what we’re offering our employees to what they can get in an insurance exchange."
Further complicating coverage, he said, would be the need to tier coverage to accommodate the variances in office and medical staff salaries vis-à-vis the ACA’s definition of affordability.
Drag on system "real"
Dr. Mark Levine, chief medical officer for the Denver office of the Centers for Medicare and Medicaid Services, said that despite the multitudinous problems with the official ACA website, healthcare.gov, "It really does make comparisons of health plans much easier." He added that only "qualified health plans are listed, which means that they are of known benefit structure and quality."
Regarding the ACA’s direct effect on patient care, Dr. Diamond said that while practices that can accommodate a larger patient load will benefit, quality likely will suffer in practices that are already operating at capacity.
"You’ll be seeing patients that are more complex because they were uninsured in the past and have multiple medical problems," he said, adding that this will take more time and will be reimbursed at lower rates than was done previously.
Dr. Levine concurred, "There will be a drag on the system at first" because of the surge in patients with complex medical needs left untreated by their previously uninsured status.
"Perhaps everybody else needs to chip in to account for that and for the kind of cost shifting we have seen and these phantom pricing mechanisms that have been so common in American health care," said Dr. Levine. "The lack of coverage to a needy population is only going to exacerbate the systemic concerns."
Regardless of burdens shouldered, plenty of Americans will remain needy, according to Dr. Jonathan Pak, also of the Oregon Health & Science University.
"The goal is to get everyone insured, but we will be nowhere close to that 10 years into the future," he said, citing data released by the Congressional Budget Office earlier this year, indicating that in the year 2022, 31 million will remain uninsured. "Make no mistake, this is not a universal health care plan."
Impact on critical care
The ACA might actually benefit the bottom lines of hospitalists and intensivists, said Dr. Diamond. "In the critical care arena, you’re going to have an improved payer mix, you’re going to have the same number of patients, and you have a business model [in which] you don’t have clerical staff," he said.
Dr. Pak had a different view. Already shrinking numbers of critical care resources such as beds and critical care staff likely will be further stressed under the ACA, forcing up per-bed costs and exacerbating shortages of intensivists. "I think, despite many improvements, it won’t be very long before we have to face structural health reform all over again."
Still, Dr. Pak said there are some reasons to feel hopeful. "The ACA will relieve the suffering of millions and will potentially reduce the number of people who end up in the ICU because of better primary care," he said, among other benefits such as the ACA’s increased funding for critical care research.
"Think aggressively"
"It’s serious. You’ve got to cut costs," said Dr. Diamond, who said it was a good time to be a nurse practitioner or a physician assistant, as they are more in demand than are high-salary specialists.
Having appropriate software to improve efficiencies is also essential to the new world of ACA, said Dr. Diamond. "What is coming is clinical integration," he said, referring to ACA mandates on collecting patient and financial data. "You’re also going to be measured on a daily basis on clinical protocols, so you need to be thinking about this very aggressively. How will you have the IT to support what you’ve got to do?"
Included in this overhaul, said Dr. Diamond, must be an attitude change toward working with other providers, including local hospitals and pharmacies, in order to decrease the variation of practice and adhere to evidence-based medicine protocols and national guidelines.
Dr. Levine defended the ACA saying that the current system is "unsustainable" and that for the first time, portions of the ACA such as value-based purchasing, "which holds groups of people responsible" would help the CMS implement its 5-year plan for Americans to have "Better care, better health, and lower costs."
"The past is past," said Dr. Diamond. "You have to embrace change."
CHICAGO – The Affordable Care Act may still be stumbling into place, but it’s here to stay, bringing with it changes especially acute for private physicians.
That’s the consensus of a panel of experts who presented their perspective on the impact of "Obamacare" at this year’s annual meeting of the American College of Chest Physicians.
"Younger physicians are more supportive of the ACA than older physicians," said to Dr. Akram Khan of Oregon Health & Science University, Portland, referencing a survey that found 80% of physicians between 25 and 39 years were optimistic about the future of health care in America. "Older physicians have adapted to the fee-for-service system we currently are in, and so are more ambivalent about the effects of the ACA than [the younger generation] than younger physicians who have not adapted to the system yet."
Private practitioners pay more
Regardless of the number of years in practice, Dr. Edward J. Diamond told the audience that even though he had tried to "dig my head in the sand and tried not to think about this, but unfortunately we are compelled to address it."
The president of large, multisite pulmonary practice in suburban Chicago, Dr. Diamond listed some of the pressing concerns he said should be on the minds of all private physicians, who are almost always employers as well.
The first concern he noted was abiding by the ACA mandate that employee premiums do not exceed 9.5% of the employee’s gross income, and that employer-sponsored plans share at least 60% of the total cost.
Because the cost of private insurance is tied to that of public exchange enrollment and are therefore fluid, Dr. Diamond said this equates with "an enormous administrative burden. We as employers are now going to have to monitor the marketplace of health plans because we’re going to have to compare what we’re offering our employees to what they can get in an insurance exchange."
Further complicating coverage, he said, would be the need to tier coverage to accommodate the variances in office and medical staff salaries vis-à-vis the ACA’s definition of affordability.
Drag on system "real"
Dr. Mark Levine, chief medical officer for the Denver office of the Centers for Medicare and Medicaid Services, said that despite the multitudinous problems with the official ACA website, healthcare.gov, "It really does make comparisons of health plans much easier." He added that only "qualified health plans are listed, which means that they are of known benefit structure and quality."
Regarding the ACA’s direct effect on patient care, Dr. Diamond said that while practices that can accommodate a larger patient load will benefit, quality likely will suffer in practices that are already operating at capacity.
"You’ll be seeing patients that are more complex because they were uninsured in the past and have multiple medical problems," he said, adding that this will take more time and will be reimbursed at lower rates than was done previously.
Dr. Levine concurred, "There will be a drag on the system at first" because of the surge in patients with complex medical needs left untreated by their previously uninsured status.
"Perhaps everybody else needs to chip in to account for that and for the kind of cost shifting we have seen and these phantom pricing mechanisms that have been so common in American health care," said Dr. Levine. "The lack of coverage to a needy population is only going to exacerbate the systemic concerns."
Regardless of burdens shouldered, plenty of Americans will remain needy, according to Dr. Jonathan Pak, also of the Oregon Health & Science University.
"The goal is to get everyone insured, but we will be nowhere close to that 10 years into the future," he said, citing data released by the Congressional Budget Office earlier this year, indicating that in the year 2022, 31 million will remain uninsured. "Make no mistake, this is not a universal health care plan."
Impact on critical care
The ACA might actually benefit the bottom lines of hospitalists and intensivists, said Dr. Diamond. "In the critical care arena, you’re going to have an improved payer mix, you’re going to have the same number of patients, and you have a business model [in which] you don’t have clerical staff," he said.
Dr. Pak had a different view. Already shrinking numbers of critical care resources such as beds and critical care staff likely will be further stressed under the ACA, forcing up per-bed costs and exacerbating shortages of intensivists. "I think, despite many improvements, it won’t be very long before we have to face structural health reform all over again."
Still, Dr. Pak said there are some reasons to feel hopeful. "The ACA will relieve the suffering of millions and will potentially reduce the number of people who end up in the ICU because of better primary care," he said, among other benefits such as the ACA’s increased funding for critical care research.
"Think aggressively"
"It’s serious. You’ve got to cut costs," said Dr. Diamond, who said it was a good time to be a nurse practitioner or a physician assistant, as they are more in demand than are high-salary specialists.
Having appropriate software to improve efficiencies is also essential to the new world of ACA, said Dr. Diamond. "What is coming is clinical integration," he said, referring to ACA mandates on collecting patient and financial data. "You’re also going to be measured on a daily basis on clinical protocols, so you need to be thinking about this very aggressively. How will you have the IT to support what you’ve got to do?"
Included in this overhaul, said Dr. Diamond, must be an attitude change toward working with other providers, including local hospitals and pharmacies, in order to decrease the variation of practice and adhere to evidence-based medicine protocols and national guidelines.
Dr. Levine defended the ACA saying that the current system is "unsustainable" and that for the first time, portions of the ACA such as value-based purchasing, "which holds groups of people responsible" would help the CMS implement its 5-year plan for Americans to have "Better care, better health, and lower costs."
"The past is past," said Dr. Diamond. "You have to embrace change."
EXPERT ANALYSIS FROM CHEST 2013
Major finding: Private physicians may be unprepared for how drastically the ACA will change their practice.
Data source: Expert analysis from CHEST 2013
Disclosures: Dr. Kahn, Dr. Levine, Dr. Pak, and Dr. Diamond had no relevant disclosures.
Under ACA, practices risk tripping over antitrust regulations
CHICAGO – Probably the last thing on the minds of office-based physicians is whether they are running afoul of antitrust regulations.
However, according to Dr. Edward J. Diamond, a pulmonary specialist, a faculty member of the American College of Chest Physicians, and president of Suburban Lung Associates – a large network of pulmonary care offices near Chicago – physicians can add that to their list of concerns about the Affordable Care Act.
The danger zone, according to Dr. Diamond, is what’s known as "clinical integration": pooling patient and protocol data for the purpose of meeting the ACA’s data-driven call on providers to improve care and lower costs. This can be achieved for less when physicians in private practice band together, but it’s not as simple as a handshake, said Dr. Diamond.
The U.S. Department of Justice specifically defines clinical integration as a "network implementing an active and ongoing program to evaluate and modify practice patterns ... and create a high degree of interdependence and cooperation among the physicians to control costs and ensure quality..."
"You have to really adhere to this definition to avoid antitrust issues," said Dr. Diamond, who made his remarks at the annual meeting of the American College of Chest Physicians.
"The Statements of Antitrust Enforcement Policy in Health Care, issued jointly by the Federal Trade Commission and Department of Justice in 1996, carve out certain safety zones for physician network joint ventures," said Christopher Gordon, a specialist in health care antitrust law at Squire Sanders LLP in Washington.
Mr. Gordon said that the DOJ and the FTC "will typically not challenge an exclusive physician network joint venture where the participants share substantial financial risk and constitute 20% or less of the physicians in each specialty practicing in the relevant geographic market. Where the network is nonexclusive, that number rises to 30% or less."
If they are too large, or if they don’t keep to these predetermined percentages of competing physicians by specialty, groups of competing health care providers cooperating to make their ACA mandates could be in danger.
"Networks that fall outside these safety zones – either because they include a higher percentage of physicians or do not involve financial risk sharing – do not necessarily raise antitrust concerns, but instead will have their conduct reviewed under what is known as the "rule of reason" to determine whether, on balance, the conduct is anticompetitive or not," said Mr. Gordon.
"You have to be very careful you don’t end up accused of illegal collective bargaining," said Dr. Diamond. "There is a disconnect between what the Department of Justice and what the ACA are asking."
If not a disconnect, at least a proscribed field of play.
According to Mr. Gordon, providers have latitude in how they cooperate when it comes to developing clinical protocols and best practices, so long as that cooperation does not include pricing agreements among multiple, independent clinics. "Such conduct would arguably constitute a per se violation of the antitrust laws regardless of how small or big the clinics are," he said.
Although the justice department and the FTC are primarily focused on conduct that impacts commercial health insurance markets, fee schedules and reimbursements that are part of any Medicare Advantage plan are considered part of the marketplace, because these plans are offered by private insurers contracting with the federal government, Mr. Gordon said. Medicare proper, meanwhile, is unaffected by antitrust concerns because "its pricing is set by the government, so there is little or no risk that provider misconduct could impact those prices," he noted.
Whatever happens, said Dr. Diamond, to survive in the era of the ACA, providers who will thrive with clinical integration are those who can develop areas of expertise such as excellent electronic health record systems, which make them attractive partners to other clinics and health care facilities. "Be a friendly competitor," he said, Above all else, he added: "Embrace change."
Dr. Diamond reported having no disclosures.

|
| Dr. Burt Lesnick |
Dr. Burt Lesnick, FCCP, comments: Practices can come together via financial integration or clinical integration, each with its own sets of guidelines to avoid antitrust issues. Financial integration requires some degree of risk sharing. Clinical integration does not require risk sharing but has stringent requirements from the Department of Justice.The ACCP's former treasurer, Dr. Diamond, outlines these in this article.

|
| Dr. Burt Lesnick |
Dr. Burt Lesnick, FCCP, comments: Practices can come together via financial integration or clinical integration, each with its own sets of guidelines to avoid antitrust issues. Financial integration requires some degree of risk sharing. Clinical integration does not require risk sharing but has stringent requirements from the Department of Justice.The ACCP's former treasurer, Dr. Diamond, outlines these in this article.

|
| Dr. Burt Lesnick |
Dr. Burt Lesnick, FCCP, comments: Practices can come together via financial integration or clinical integration, each with its own sets of guidelines to avoid antitrust issues. Financial integration requires some degree of risk sharing. Clinical integration does not require risk sharing but has stringent requirements from the Department of Justice.The ACCP's former treasurer, Dr. Diamond, outlines these in this article.
CHICAGO – Probably the last thing on the minds of office-based physicians is whether they are running afoul of antitrust regulations.
However, according to Dr. Edward J. Diamond, a pulmonary specialist, a faculty member of the American College of Chest Physicians, and president of Suburban Lung Associates – a large network of pulmonary care offices near Chicago – physicians can add that to their list of concerns about the Affordable Care Act.
The danger zone, according to Dr. Diamond, is what’s known as "clinical integration": pooling patient and protocol data for the purpose of meeting the ACA’s data-driven call on providers to improve care and lower costs. This can be achieved for less when physicians in private practice band together, but it’s not as simple as a handshake, said Dr. Diamond.
The U.S. Department of Justice specifically defines clinical integration as a "network implementing an active and ongoing program to evaluate and modify practice patterns ... and create a high degree of interdependence and cooperation among the physicians to control costs and ensure quality..."
"You have to really adhere to this definition to avoid antitrust issues," said Dr. Diamond, who made his remarks at the annual meeting of the American College of Chest Physicians.
"The Statements of Antitrust Enforcement Policy in Health Care, issued jointly by the Federal Trade Commission and Department of Justice in 1996, carve out certain safety zones for physician network joint ventures," said Christopher Gordon, a specialist in health care antitrust law at Squire Sanders LLP in Washington.
Mr. Gordon said that the DOJ and the FTC "will typically not challenge an exclusive physician network joint venture where the participants share substantial financial risk and constitute 20% or less of the physicians in each specialty practicing in the relevant geographic market. Where the network is nonexclusive, that number rises to 30% or less."
If they are too large, or if they don’t keep to these predetermined percentages of competing physicians by specialty, groups of competing health care providers cooperating to make their ACA mandates could be in danger.
"Networks that fall outside these safety zones – either because they include a higher percentage of physicians or do not involve financial risk sharing – do not necessarily raise antitrust concerns, but instead will have their conduct reviewed under what is known as the "rule of reason" to determine whether, on balance, the conduct is anticompetitive or not," said Mr. Gordon.
"You have to be very careful you don’t end up accused of illegal collective bargaining," said Dr. Diamond. "There is a disconnect between what the Department of Justice and what the ACA are asking."
If not a disconnect, at least a proscribed field of play.
According to Mr. Gordon, providers have latitude in how they cooperate when it comes to developing clinical protocols and best practices, so long as that cooperation does not include pricing agreements among multiple, independent clinics. "Such conduct would arguably constitute a per se violation of the antitrust laws regardless of how small or big the clinics are," he said.
Although the justice department and the FTC are primarily focused on conduct that impacts commercial health insurance markets, fee schedules and reimbursements that are part of any Medicare Advantage plan are considered part of the marketplace, because these plans are offered by private insurers contracting with the federal government, Mr. Gordon said. Medicare proper, meanwhile, is unaffected by antitrust concerns because "its pricing is set by the government, so there is little or no risk that provider misconduct could impact those prices," he noted.
Whatever happens, said Dr. Diamond, to survive in the era of the ACA, providers who will thrive with clinical integration are those who can develop areas of expertise such as excellent electronic health record systems, which make them attractive partners to other clinics and health care facilities. "Be a friendly competitor," he said, Above all else, he added: "Embrace change."
Dr. Diamond reported having no disclosures.
CHICAGO – Probably the last thing on the minds of office-based physicians is whether they are running afoul of antitrust regulations.
However, according to Dr. Edward J. Diamond, a pulmonary specialist, a faculty member of the American College of Chest Physicians, and president of Suburban Lung Associates – a large network of pulmonary care offices near Chicago – physicians can add that to their list of concerns about the Affordable Care Act.
The danger zone, according to Dr. Diamond, is what’s known as "clinical integration": pooling patient and protocol data for the purpose of meeting the ACA’s data-driven call on providers to improve care and lower costs. This can be achieved for less when physicians in private practice band together, but it’s not as simple as a handshake, said Dr. Diamond.
The U.S. Department of Justice specifically defines clinical integration as a "network implementing an active and ongoing program to evaluate and modify practice patterns ... and create a high degree of interdependence and cooperation among the physicians to control costs and ensure quality..."
"You have to really adhere to this definition to avoid antitrust issues," said Dr. Diamond, who made his remarks at the annual meeting of the American College of Chest Physicians.
"The Statements of Antitrust Enforcement Policy in Health Care, issued jointly by the Federal Trade Commission and Department of Justice in 1996, carve out certain safety zones for physician network joint ventures," said Christopher Gordon, a specialist in health care antitrust law at Squire Sanders LLP in Washington.
Mr. Gordon said that the DOJ and the FTC "will typically not challenge an exclusive physician network joint venture where the participants share substantial financial risk and constitute 20% or less of the physicians in each specialty practicing in the relevant geographic market. Where the network is nonexclusive, that number rises to 30% or less."
If they are too large, or if they don’t keep to these predetermined percentages of competing physicians by specialty, groups of competing health care providers cooperating to make their ACA mandates could be in danger.
"Networks that fall outside these safety zones – either because they include a higher percentage of physicians or do not involve financial risk sharing – do not necessarily raise antitrust concerns, but instead will have their conduct reviewed under what is known as the "rule of reason" to determine whether, on balance, the conduct is anticompetitive or not," said Mr. Gordon.
"You have to be very careful you don’t end up accused of illegal collective bargaining," said Dr. Diamond. "There is a disconnect between what the Department of Justice and what the ACA are asking."
If not a disconnect, at least a proscribed field of play.
According to Mr. Gordon, providers have latitude in how they cooperate when it comes to developing clinical protocols and best practices, so long as that cooperation does not include pricing agreements among multiple, independent clinics. "Such conduct would arguably constitute a per se violation of the antitrust laws regardless of how small or big the clinics are," he said.
Although the justice department and the FTC are primarily focused on conduct that impacts commercial health insurance markets, fee schedules and reimbursements that are part of any Medicare Advantage plan are considered part of the marketplace, because these plans are offered by private insurers contracting with the federal government, Mr. Gordon said. Medicare proper, meanwhile, is unaffected by antitrust concerns because "its pricing is set by the government, so there is little or no risk that provider misconduct could impact those prices," he noted.
Whatever happens, said Dr. Diamond, to survive in the era of the ACA, providers who will thrive with clinical integration are those who can develop areas of expertise such as excellent electronic health record systems, which make them attractive partners to other clinics and health care facilities. "Be a friendly competitor," he said, Above all else, he added: "Embrace change."
Dr. Diamond reported having no disclosures.
EXPERT ANALYSIS FROM CHEST 2013
Clinical phenotypes in COPD lead to better diagnosis, more targeted treatments
CHICAGO – Accurate phenotyping, in the ascendant over the last decade, equates with more effectively targeted treatments for chronic obstructive pulmonary disease, according to a proponent of personalized pulmonary medicine.
"We know that COPD is not the same, but right now we are treating these patients as though one size fits all," Dr. Nicola A. Hanania of the Baylor College of Medicine, Houston, said in a packed session on COPD at the annual meeting of the American College of Chest Physicians.
Because phenotypes describe differences in individuals, they should have relevance to clinically meaningful outcomes. "In COPD, that relates to symptoms, exacerbation, disease progression, response to therapy, and survival," he said.
Potential phenotypes that have been identified according to clinical, physiologic, and radiologic criteria include chronic bronchitis, asthma/COPD overlap, frequent exacerbator, radiologic CT, and persistent systemic inflammation.
Chronic bronchitis
Chronic bronchitis tends to occur more in younger people who smoke. It also is characterized by more wheezing and thicker airway walls. Data presented by Dr. Hanania also showed that this phenotype has more frequent acute exacerbations (Chest 2011;140:1107-8).
In one study, 290 subjects deemed chronically bronchitic – chronic cough and phlegm lasting 3 months of every year for 2 consecutive years – were compared with 771 subjects who were not chronically bronchitic. Investigators found that patients in the first group had more frequent exacerbations per patient: 1.21-1.62 vs. 0.63-1.12 (P < .027). The first group also reported more severe exacerbations: 26.6% vs. 20% (P < .024) (Chest 2011;140:626-33).
Asthma/COPD overlap
"This is a phenotype that deserves more attention. We all have patients where we scratch our head, ‘Is this asthma, or is this COPD?’ " said Dr. Hanania. "We don’t really know because these patients are notoriously excluded from both asthma and COPD studies." He cited estimates suggesting that 13%-20% of COPD patients overlap with asthma (Arch. Bronconeumol. 2012;48:331-7).
Proposed diagnostic criteria for the overlap syndrome phenotype may include two major criteria: marked response to bronchodilators (>15% and >400 mL in forced expiratory volume in 1 second [FEV1]), history of asthma if patient is younger than 40 years, and sputum eosinophilia. Overlap also can be diagnosed by one major criterion and two of the following: response to bronchodilation at least two separate times (>12% and >200 mL in FEV1), history of atopy, and increased total serum IgE. At this time, he said, these criteria are based on expert opinion and on data, "but the clinical implications, once we do the homework, is that these patients deserve to be on antibiotics and corticosteroids early on."
Frequent exacerbator
Defined in the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines as two or more exacerbations per year, the frequent exacerbator phenotype was explained in the ECLIPSE study (Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints), Dr. Hanania said, which showed that, although exacerbations become more frequent and more severe as COPD progresses, the rate at which they occur appears to reflect an independent susceptibility phenotype (N. Engl. J. Med. 2010; 363:1128-38).
Frequent exacerbators have higher-stage COPD, more severe obstruction, and more hospitalizations, Dr. Hanania noted.
In addition, the ECLIPSE investigators found that, in 2,138 patients, frequent exacerbator types had an odds ratio of 5.72 of having had an exacerbation in the previous year
Although there other risk factors implicating this phenotype, "the most important question to ask the patient is whether they have had an exacerbation in the previous year," he said. Chronic cough is another factor.
The clinical benefit to identifying the frequent exacerbator, according to Dr. Hanania, is that this group has a greater range of comorbidities, including more inflammation, heightened viral susceptibility, and increased cardiovascular risk, among other susceptibilities.
Using CT for phenotyping
Noting that radiologic phenotyping in COPD is more advanced than in asthma at this time, Dr. Hanania said that quantitative and visual assessment of CT radiographs is "promising" and has helped identify COPD subphenotypes such as emphysema because of accurate assessment of lung inflation, wall thickness, and other factors.
Identifying patients with bronchiectasis, pulmonary arterial enlargement, and acute exacerbations in COPD is also possible with CT radiography, making it possible to predict the different outcomes in each situation. "The clinical implication is that these patients tend to have more frequent exacerbation, worse lung function, and infection," he said, noting that nascent research using imaging to determine biomarkers in functional small airways disease also is occurring.
Systemic inflammation
In the ECLIPSE study, 2,164 COPD patients had an odds ratio of 2.23 for being a current smoker and had higher levels of inflammation, as determined using biomarkers such as C-reactive protein, compared with 337 smokers without COPD and 245 nonsmokers. At the 3-year follow-up, this group with persistently higher inflammation also was classified as having significantly higher all-cause mortality than the group with less inflammation (13% vs. 2%); exacerbation rates in this group were also persistently higher (1.5 vs. 0.9) (PLoS ONE 2012;7:e37483).
Therapeutic implications
Coupling these phenotypes with molecular descriptions of mechanisms and their underlying pathologies can lead to accurate, personalized treatment of COPD. "Phenotypes without clear implications for prognosis and treatment are of little clinical use," Dr. Hanania said, noting that longitudinal studies to validate these phenotypes are necessary.
"Research can help identify mechanisms and courses in different phenotypes, including gender differences," he concluded. "Examining therapeutic responses to different phenotypes can lead to future interventions."
Dr. Hanania disclosed several relationships with a variety of pharmaceutical and medical manufacturers, including Genentech, GlaxoSmithKline* and Astra Zeneca.
Beyond GOLD: A tale of two COPD guidelines
Both address severity and comorbidity, but only one COPD guideline takes into account the latest research on phenotyping in chronic obstructive pulmonary disease.
"The GOLD guidelines do not include clinical phenotypes," said Dr. Joan Soriano, a presenter at the meeting. "But the Spanish ones do."
In fact, there is really only one area where the two documents overlap, said Dr. Soriano: how they define COPD, and even that is not the same. "They both mention the fundamental aspect, which is airflow limitation, and also that the mechanism involved is inflammation," he said. The GOLD definition, however, recognizes the importance of comorbidities, which the Spanish guidelines address the role of tobacco and symptomology.
GOLD (Global Initiative for Chronic Obstructive Lung Disease) is an organization of health care professionals from around the world. "I am not a member of GOLD," Dr. Soriano told the packed session.
The Spanish guidelines are issued by SEPAR, the Spanish Society for Pneumology and Thoracic Surgery. Dr. Soriano is the director of epidemiology and clinical research at the International Center of Advanced Respiratory Medicine (CIMERA) in Palma, Spain.
How the two approach diagnosis also differs. The Spanish guidelines begin with the general COPD diagnosis, then move to the characterization and phenotype, then move to the severity of the disease. They are more specific about age (over 35 years), and have lower limit of normal (LLN) values for persons aged over 70 years and less than 50 years. The GOLD guidelines do not address LLN.
To characterize the disease specifically, the Spanish guidelines address the existence of phenotypes, according to Dr. Soriano, beginning with determining the frequency of exacerbation the patient has per year, and then classifying them eventually into four types: mixed, chronic bronchitis, emphysema, and exacerbator. The GOLD guidelines do not mention phenotypes.
When it comes to the multidimensional assessment of COPD, "the GOLD guidelines lump the mild with the severe spirometry. This is very hard for me to understand," he said. Other classification divergence includes that the Spanish guidelines consider the BODE index.
Treatment in the two guidelines begins similarly, but vectors off from there. "Basically, we are looking at the same trials, so the initial treatments should be short-acting bronchodilators," Dr. Soriano said, but because phenotyping allows for more targeted treatment, the Spanish guidelines offer more detailed treatment options.
In a paper coauthored by Dr. Soriano earlier this year, specific treatment per phenotype included phosphodiesterase-4 inhibitors only for those with chronic bronchitis, inhaled corticosteroids for overlap COPD-asthma, and bronchodilators for infrequent exacerbators (Eur. Respir. J. 2013;41:1252-6).
In the end, the guidelines might not follow the same trajectory, but each has value, he said. "Whatever guidelines you choose, don’t go back and forth. Pick one and use them."
Dr. Soriano reported relationships with Novartis Spain, AstraZeneca, Pfizer, and several other pharmaceutical and medical manufacturers.
*CORRECTION, 2/20/2014: An earlier version of this story misstated the name of GlaxoSmithKline.
CHICAGO – Accurate phenotyping, in the ascendant over the last decade, equates with more effectively targeted treatments for chronic obstructive pulmonary disease, according to a proponent of personalized pulmonary medicine.
"We know that COPD is not the same, but right now we are treating these patients as though one size fits all," Dr. Nicola A. Hanania of the Baylor College of Medicine, Houston, said in a packed session on COPD at the annual meeting of the American College of Chest Physicians.
Because phenotypes describe differences in individuals, they should have relevance to clinically meaningful outcomes. "In COPD, that relates to symptoms, exacerbation, disease progression, response to therapy, and survival," he said.
Potential phenotypes that have been identified according to clinical, physiologic, and radiologic criteria include chronic bronchitis, asthma/COPD overlap, frequent exacerbator, radiologic CT, and persistent systemic inflammation.
Chronic bronchitis
Chronic bronchitis tends to occur more in younger people who smoke. It also is characterized by more wheezing and thicker airway walls. Data presented by Dr. Hanania also showed that this phenotype has more frequent acute exacerbations (Chest 2011;140:1107-8).
In one study, 290 subjects deemed chronically bronchitic – chronic cough and phlegm lasting 3 months of every year for 2 consecutive years – were compared with 771 subjects who were not chronically bronchitic. Investigators found that patients in the first group had more frequent exacerbations per patient: 1.21-1.62 vs. 0.63-1.12 (P < .027). The first group also reported more severe exacerbations: 26.6% vs. 20% (P < .024) (Chest 2011;140:626-33).
Asthma/COPD overlap
"This is a phenotype that deserves more attention. We all have patients where we scratch our head, ‘Is this asthma, or is this COPD?’ " said Dr. Hanania. "We don’t really know because these patients are notoriously excluded from both asthma and COPD studies." He cited estimates suggesting that 13%-20% of COPD patients overlap with asthma (Arch. Bronconeumol. 2012;48:331-7).
Proposed diagnostic criteria for the overlap syndrome phenotype may include two major criteria: marked response to bronchodilators (>15% and >400 mL in forced expiratory volume in 1 second [FEV1]), history of asthma if patient is younger than 40 years, and sputum eosinophilia. Overlap also can be diagnosed by one major criterion and two of the following: response to bronchodilation at least two separate times (>12% and >200 mL in FEV1), history of atopy, and increased total serum IgE. At this time, he said, these criteria are based on expert opinion and on data, "but the clinical implications, once we do the homework, is that these patients deserve to be on antibiotics and corticosteroids early on."
Frequent exacerbator
Defined in the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines as two or more exacerbations per year, the frequent exacerbator phenotype was explained in the ECLIPSE study (Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints), Dr. Hanania said, which showed that, although exacerbations become more frequent and more severe as COPD progresses, the rate at which they occur appears to reflect an independent susceptibility phenotype (N. Engl. J. Med. 2010; 363:1128-38).
Frequent exacerbators have higher-stage COPD, more severe obstruction, and more hospitalizations, Dr. Hanania noted.
In addition, the ECLIPSE investigators found that, in 2,138 patients, frequent exacerbator types had an odds ratio of 5.72 of having had an exacerbation in the previous year
Although there other risk factors implicating this phenotype, "the most important question to ask the patient is whether they have had an exacerbation in the previous year," he said. Chronic cough is another factor.
The clinical benefit to identifying the frequent exacerbator, according to Dr. Hanania, is that this group has a greater range of comorbidities, including more inflammation, heightened viral susceptibility, and increased cardiovascular risk, among other susceptibilities.
Using CT for phenotyping
Noting that radiologic phenotyping in COPD is more advanced than in asthma at this time, Dr. Hanania said that quantitative and visual assessment of CT radiographs is "promising" and has helped identify COPD subphenotypes such as emphysema because of accurate assessment of lung inflation, wall thickness, and other factors.
Identifying patients with bronchiectasis, pulmonary arterial enlargement, and acute exacerbations in COPD is also possible with CT radiography, making it possible to predict the different outcomes in each situation. "The clinical implication is that these patients tend to have more frequent exacerbation, worse lung function, and infection," he said, noting that nascent research using imaging to determine biomarkers in functional small airways disease also is occurring.
Systemic inflammation
In the ECLIPSE study, 2,164 COPD patients had an odds ratio of 2.23 for being a current smoker and had higher levels of inflammation, as determined using biomarkers such as C-reactive protein, compared with 337 smokers without COPD and 245 nonsmokers. At the 3-year follow-up, this group with persistently higher inflammation also was classified as having significantly higher all-cause mortality than the group with less inflammation (13% vs. 2%); exacerbation rates in this group were also persistently higher (1.5 vs. 0.9) (PLoS ONE 2012;7:e37483).
Therapeutic implications
Coupling these phenotypes with molecular descriptions of mechanisms and their underlying pathologies can lead to accurate, personalized treatment of COPD. "Phenotypes without clear implications for prognosis and treatment are of little clinical use," Dr. Hanania said, noting that longitudinal studies to validate these phenotypes are necessary.
"Research can help identify mechanisms and courses in different phenotypes, including gender differences," he concluded. "Examining therapeutic responses to different phenotypes can lead to future interventions."
Dr. Hanania disclosed several relationships with a variety of pharmaceutical and medical manufacturers, including Genentech, GlaxoSmithKline* and Astra Zeneca.
Beyond GOLD: A tale of two COPD guidelines
Both address severity and comorbidity, but only one COPD guideline takes into account the latest research on phenotyping in chronic obstructive pulmonary disease.
"The GOLD guidelines do not include clinical phenotypes," said Dr. Joan Soriano, a presenter at the meeting. "But the Spanish ones do."
In fact, there is really only one area where the two documents overlap, said Dr. Soriano: how they define COPD, and even that is not the same. "They both mention the fundamental aspect, which is airflow limitation, and also that the mechanism involved is inflammation," he said. The GOLD definition, however, recognizes the importance of comorbidities, which the Spanish guidelines address the role of tobacco and symptomology.
GOLD (Global Initiative for Chronic Obstructive Lung Disease) is an organization of health care professionals from around the world. "I am not a member of GOLD," Dr. Soriano told the packed session.
The Spanish guidelines are issued by SEPAR, the Spanish Society for Pneumology and Thoracic Surgery. Dr. Soriano is the director of epidemiology and clinical research at the International Center of Advanced Respiratory Medicine (CIMERA) in Palma, Spain.
How the two approach diagnosis also differs. The Spanish guidelines begin with the general COPD diagnosis, then move to the characterization and phenotype, then move to the severity of the disease. They are more specific about age (over 35 years), and have lower limit of normal (LLN) values for persons aged over 70 years and less than 50 years. The GOLD guidelines do not address LLN.
To characterize the disease specifically, the Spanish guidelines address the existence of phenotypes, according to Dr. Soriano, beginning with determining the frequency of exacerbation the patient has per year, and then classifying them eventually into four types: mixed, chronic bronchitis, emphysema, and exacerbator. The GOLD guidelines do not mention phenotypes.
When it comes to the multidimensional assessment of COPD, "the GOLD guidelines lump the mild with the severe spirometry. This is very hard for me to understand," he said. Other classification divergence includes that the Spanish guidelines consider the BODE index.
Treatment in the two guidelines begins similarly, but vectors off from there. "Basically, we are looking at the same trials, so the initial treatments should be short-acting bronchodilators," Dr. Soriano said, but because phenotyping allows for more targeted treatment, the Spanish guidelines offer more detailed treatment options.
In a paper coauthored by Dr. Soriano earlier this year, specific treatment per phenotype included phosphodiesterase-4 inhibitors only for those with chronic bronchitis, inhaled corticosteroids for overlap COPD-asthma, and bronchodilators for infrequent exacerbators (Eur. Respir. J. 2013;41:1252-6).
In the end, the guidelines might not follow the same trajectory, but each has value, he said. "Whatever guidelines you choose, don’t go back and forth. Pick one and use them."
Dr. Soriano reported relationships with Novartis Spain, AstraZeneca, Pfizer, and several other pharmaceutical and medical manufacturers.
*CORRECTION, 2/20/2014: An earlier version of this story misstated the name of GlaxoSmithKline.
CHICAGO – Accurate phenotyping, in the ascendant over the last decade, equates with more effectively targeted treatments for chronic obstructive pulmonary disease, according to a proponent of personalized pulmonary medicine.
"We know that COPD is not the same, but right now we are treating these patients as though one size fits all," Dr. Nicola A. Hanania of the Baylor College of Medicine, Houston, said in a packed session on COPD at the annual meeting of the American College of Chest Physicians.
Because phenotypes describe differences in individuals, they should have relevance to clinically meaningful outcomes. "In COPD, that relates to symptoms, exacerbation, disease progression, response to therapy, and survival," he said.
Potential phenotypes that have been identified according to clinical, physiologic, and radiologic criteria include chronic bronchitis, asthma/COPD overlap, frequent exacerbator, radiologic CT, and persistent systemic inflammation.
Chronic bronchitis
Chronic bronchitis tends to occur more in younger people who smoke. It also is characterized by more wheezing and thicker airway walls. Data presented by Dr. Hanania also showed that this phenotype has more frequent acute exacerbations (Chest 2011;140:1107-8).
In one study, 290 subjects deemed chronically bronchitic – chronic cough and phlegm lasting 3 months of every year for 2 consecutive years – were compared with 771 subjects who were not chronically bronchitic. Investigators found that patients in the first group had more frequent exacerbations per patient: 1.21-1.62 vs. 0.63-1.12 (P < .027). The first group also reported more severe exacerbations: 26.6% vs. 20% (P < .024) (Chest 2011;140:626-33).
Asthma/COPD overlap
"This is a phenotype that deserves more attention. We all have patients where we scratch our head, ‘Is this asthma, or is this COPD?’ " said Dr. Hanania. "We don’t really know because these patients are notoriously excluded from both asthma and COPD studies." He cited estimates suggesting that 13%-20% of COPD patients overlap with asthma (Arch. Bronconeumol. 2012;48:331-7).
Proposed diagnostic criteria for the overlap syndrome phenotype may include two major criteria: marked response to bronchodilators (>15% and >400 mL in forced expiratory volume in 1 second [FEV1]), history of asthma if patient is younger than 40 years, and sputum eosinophilia. Overlap also can be diagnosed by one major criterion and two of the following: response to bronchodilation at least two separate times (>12% and >200 mL in FEV1), history of atopy, and increased total serum IgE. At this time, he said, these criteria are based on expert opinion and on data, "but the clinical implications, once we do the homework, is that these patients deserve to be on antibiotics and corticosteroids early on."
Frequent exacerbator
Defined in the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines as two or more exacerbations per year, the frequent exacerbator phenotype was explained in the ECLIPSE study (Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints), Dr. Hanania said, which showed that, although exacerbations become more frequent and more severe as COPD progresses, the rate at which they occur appears to reflect an independent susceptibility phenotype (N. Engl. J. Med. 2010; 363:1128-38).
Frequent exacerbators have higher-stage COPD, more severe obstruction, and more hospitalizations, Dr. Hanania noted.
In addition, the ECLIPSE investigators found that, in 2,138 patients, frequent exacerbator types had an odds ratio of 5.72 of having had an exacerbation in the previous year
Although there other risk factors implicating this phenotype, "the most important question to ask the patient is whether they have had an exacerbation in the previous year," he said. Chronic cough is another factor.
The clinical benefit to identifying the frequent exacerbator, according to Dr. Hanania, is that this group has a greater range of comorbidities, including more inflammation, heightened viral susceptibility, and increased cardiovascular risk, among other susceptibilities.
Using CT for phenotyping
Noting that radiologic phenotyping in COPD is more advanced than in asthma at this time, Dr. Hanania said that quantitative and visual assessment of CT radiographs is "promising" and has helped identify COPD subphenotypes such as emphysema because of accurate assessment of lung inflation, wall thickness, and other factors.
Identifying patients with bronchiectasis, pulmonary arterial enlargement, and acute exacerbations in COPD is also possible with CT radiography, making it possible to predict the different outcomes in each situation. "The clinical implication is that these patients tend to have more frequent exacerbation, worse lung function, and infection," he said, noting that nascent research using imaging to determine biomarkers in functional small airways disease also is occurring.
Systemic inflammation
In the ECLIPSE study, 2,164 COPD patients had an odds ratio of 2.23 for being a current smoker and had higher levels of inflammation, as determined using biomarkers such as C-reactive protein, compared with 337 smokers without COPD and 245 nonsmokers. At the 3-year follow-up, this group with persistently higher inflammation also was classified as having significantly higher all-cause mortality than the group with less inflammation (13% vs. 2%); exacerbation rates in this group were also persistently higher (1.5 vs. 0.9) (PLoS ONE 2012;7:e37483).
Therapeutic implications
Coupling these phenotypes with molecular descriptions of mechanisms and their underlying pathologies can lead to accurate, personalized treatment of COPD. "Phenotypes without clear implications for prognosis and treatment are of little clinical use," Dr. Hanania said, noting that longitudinal studies to validate these phenotypes are necessary.
"Research can help identify mechanisms and courses in different phenotypes, including gender differences," he concluded. "Examining therapeutic responses to different phenotypes can lead to future interventions."
Dr. Hanania disclosed several relationships with a variety of pharmaceutical and medical manufacturers, including Genentech, GlaxoSmithKline* and Astra Zeneca.
Beyond GOLD: A tale of two COPD guidelines
Both address severity and comorbidity, but only one COPD guideline takes into account the latest research on phenotyping in chronic obstructive pulmonary disease.
"The GOLD guidelines do not include clinical phenotypes," said Dr. Joan Soriano, a presenter at the meeting. "But the Spanish ones do."
In fact, there is really only one area where the two documents overlap, said Dr. Soriano: how they define COPD, and even that is not the same. "They both mention the fundamental aspect, which is airflow limitation, and also that the mechanism involved is inflammation," he said. The GOLD definition, however, recognizes the importance of comorbidities, which the Spanish guidelines address the role of tobacco and symptomology.
GOLD (Global Initiative for Chronic Obstructive Lung Disease) is an organization of health care professionals from around the world. "I am not a member of GOLD," Dr. Soriano told the packed session.
The Spanish guidelines are issued by SEPAR, the Spanish Society for Pneumology and Thoracic Surgery. Dr. Soriano is the director of epidemiology and clinical research at the International Center of Advanced Respiratory Medicine (CIMERA) in Palma, Spain.
How the two approach diagnosis also differs. The Spanish guidelines begin with the general COPD diagnosis, then move to the characterization and phenotype, then move to the severity of the disease. They are more specific about age (over 35 years), and have lower limit of normal (LLN) values for persons aged over 70 years and less than 50 years. The GOLD guidelines do not address LLN.
To characterize the disease specifically, the Spanish guidelines address the existence of phenotypes, according to Dr. Soriano, beginning with determining the frequency of exacerbation the patient has per year, and then classifying them eventually into four types: mixed, chronic bronchitis, emphysema, and exacerbator. The GOLD guidelines do not mention phenotypes.
When it comes to the multidimensional assessment of COPD, "the GOLD guidelines lump the mild with the severe spirometry. This is very hard for me to understand," he said. Other classification divergence includes that the Spanish guidelines consider the BODE index.
Treatment in the two guidelines begins similarly, but vectors off from there. "Basically, we are looking at the same trials, so the initial treatments should be short-acting bronchodilators," Dr. Soriano said, but because phenotyping allows for more targeted treatment, the Spanish guidelines offer more detailed treatment options.
In a paper coauthored by Dr. Soriano earlier this year, specific treatment per phenotype included phosphodiesterase-4 inhibitors only for those with chronic bronchitis, inhaled corticosteroids for overlap COPD-asthma, and bronchodilators for infrequent exacerbators (Eur. Respir. J. 2013;41:1252-6).
In the end, the guidelines might not follow the same trajectory, but each has value, he said. "Whatever guidelines you choose, don’t go back and forth. Pick one and use them."
Dr. Soriano reported relationships with Novartis Spain, AstraZeneca, Pfizer, and several other pharmaceutical and medical manufacturers.
*CORRECTION, 2/20/2014: An earlier version of this story misstated the name of GlaxoSmithKline.
EXPERT ANALYSIS FROM CHEST 2013
Off-label use of opioids can provide relief in refractory dyspnea
CHICAGO – Low doses of opioids titrated based on patient ratings of breathing difficulty are effective in managing refractory dyspnea, according to Dr. Donald Mahler.
Because refractory dyspnea is a neuromechanical dissociation, treating more than the pulmonary system can be beneficial, Dr. Mahler said at the annual meeting of the American College of Chest Physicians. "We have targets for the lungs to relieve dyspnea, but we may also have potential targets in the central nervous system that may also provide benefit."
Referring to published data from two randomized controlled studies about the effect of naloxone on blocking opioid signals in patients with COPD who reported breathlessness and perceived "unpleasantness" of dyspnea after exercise, Dr. Mahler said that endogenous opioids modulate the perception of dyspnea; exogenous opioids could therefore do the same (Eur. Respir. J. 2009;33:771-7 and COPD 2011;8:160-6).
Opioid receptors in the limbic system have 100 times greater binding density in the bronchioles and alveolar walls. "That may play a role when thinking about a nebulized approach," said Dr. Mahler of Dartmouth-Hitchcock Medical Center, Lebanon, N.H. The number of side effects, including constipation, was lower with this approach, he added.
Because opioids are known to decrease respiratory drive, there is a "presumable" effect on corollary discharge, which can lead to less perception of breathlessness, according to Dr. Mahler. Narcotics’ dulling effect on the perception of pain and anxiety might also contribute. "Maybe by relieving symptoms, there’s less anxiety as a result," said Dr. Mahler.
He addressed concerns over the "double effect" whereby opioids used to lessen symptoms might actually hasten death in a patient with refractory dyspnea, saying the studies "don’t really support that." Dr. Mahler cited data indicating that higher doses of benzodiazepines used in withdrawal of life-sustaining treatment were not associated with a decreased time from withdrawal of life support to death (CHEST 2004;126:286-93).
As for respiratory depression, Dr. Mahler said he had reviewed 11 studies and found only one report of any change in oxygen saturation after opioid administration.
In deciding whether a patient should be given opioid therapy, Dr. Mahler said physicians should be sure that standard therapies are inadequate and that the risk/benefit ratio favors trial treatment. Establishing treatment goals and confirming that the patient and/or the patient’s family are on board with a trial of opioid treatment is key, he added.
To determine titration, physicians should ask the patients to rate their breathing difficulty. "This is a critical part of the assessment," said Dr. Mahler, noting that the level of breathlessness determines the dose and duration of action.
If dyspnea is episodic, he said, "it doesn’t make sense to administer a long-acting opioid" and so an immediate-release or short-acting form should be considered. If it’s constant, sustained release may be effective, he said.
Dr. Mahler, who said his presentation was related to the off-label use of morphine only, said that the important thing is to "titrate the opioid to achieve the lower effective dose based on the patient’s rating of the dyspnea." Adding an anxiolytic could also be considered, he said. "It’s pretty straightforward that you should discontinue the opioid if there is an unsatisfactory response or if there is an adverse effect."
Dr. Mahler disclosed ties with numerous pharmaceutical manufacturers and other medical organizations, including GlaxoSmithKline, Novartis, and Sunovion.
CHICAGO – Low doses of opioids titrated based on patient ratings of breathing difficulty are effective in managing refractory dyspnea, according to Dr. Donald Mahler.
Because refractory dyspnea is a neuromechanical dissociation, treating more than the pulmonary system can be beneficial, Dr. Mahler said at the annual meeting of the American College of Chest Physicians. "We have targets for the lungs to relieve dyspnea, but we may also have potential targets in the central nervous system that may also provide benefit."
Referring to published data from two randomized controlled studies about the effect of naloxone on blocking opioid signals in patients with COPD who reported breathlessness and perceived "unpleasantness" of dyspnea after exercise, Dr. Mahler said that endogenous opioids modulate the perception of dyspnea; exogenous opioids could therefore do the same (Eur. Respir. J. 2009;33:771-7 and COPD 2011;8:160-6).
Opioid receptors in the limbic system have 100 times greater binding density in the bronchioles and alveolar walls. "That may play a role when thinking about a nebulized approach," said Dr. Mahler of Dartmouth-Hitchcock Medical Center, Lebanon, N.H. The number of side effects, including constipation, was lower with this approach, he added.
Because opioids are known to decrease respiratory drive, there is a "presumable" effect on corollary discharge, which can lead to less perception of breathlessness, according to Dr. Mahler. Narcotics’ dulling effect on the perception of pain and anxiety might also contribute. "Maybe by relieving symptoms, there’s less anxiety as a result," said Dr. Mahler.
He addressed concerns over the "double effect" whereby opioids used to lessen symptoms might actually hasten death in a patient with refractory dyspnea, saying the studies "don’t really support that." Dr. Mahler cited data indicating that higher doses of benzodiazepines used in withdrawal of life-sustaining treatment were not associated with a decreased time from withdrawal of life support to death (CHEST 2004;126:286-93).
As for respiratory depression, Dr. Mahler said he had reviewed 11 studies and found only one report of any change in oxygen saturation after opioid administration.
In deciding whether a patient should be given opioid therapy, Dr. Mahler said physicians should be sure that standard therapies are inadequate and that the risk/benefit ratio favors trial treatment. Establishing treatment goals and confirming that the patient and/or the patient’s family are on board with a trial of opioid treatment is key, he added.
To determine titration, physicians should ask the patients to rate their breathing difficulty. "This is a critical part of the assessment," said Dr. Mahler, noting that the level of breathlessness determines the dose and duration of action.
If dyspnea is episodic, he said, "it doesn’t make sense to administer a long-acting opioid" and so an immediate-release or short-acting form should be considered. If it’s constant, sustained release may be effective, he said.
Dr. Mahler, who said his presentation was related to the off-label use of morphine only, said that the important thing is to "titrate the opioid to achieve the lower effective dose based on the patient’s rating of the dyspnea." Adding an anxiolytic could also be considered, he said. "It’s pretty straightforward that you should discontinue the opioid if there is an unsatisfactory response or if there is an adverse effect."
Dr. Mahler disclosed ties with numerous pharmaceutical manufacturers and other medical organizations, including GlaxoSmithKline, Novartis, and Sunovion.
CHICAGO – Low doses of opioids titrated based on patient ratings of breathing difficulty are effective in managing refractory dyspnea, according to Dr. Donald Mahler.
Because refractory dyspnea is a neuromechanical dissociation, treating more than the pulmonary system can be beneficial, Dr. Mahler said at the annual meeting of the American College of Chest Physicians. "We have targets for the lungs to relieve dyspnea, but we may also have potential targets in the central nervous system that may also provide benefit."
Referring to published data from two randomized controlled studies about the effect of naloxone on blocking opioid signals in patients with COPD who reported breathlessness and perceived "unpleasantness" of dyspnea after exercise, Dr. Mahler said that endogenous opioids modulate the perception of dyspnea; exogenous opioids could therefore do the same (Eur. Respir. J. 2009;33:771-7 and COPD 2011;8:160-6).
Opioid receptors in the limbic system have 100 times greater binding density in the bronchioles and alveolar walls. "That may play a role when thinking about a nebulized approach," said Dr. Mahler of Dartmouth-Hitchcock Medical Center, Lebanon, N.H. The number of side effects, including constipation, was lower with this approach, he added.
Because opioids are known to decrease respiratory drive, there is a "presumable" effect on corollary discharge, which can lead to less perception of breathlessness, according to Dr. Mahler. Narcotics’ dulling effect on the perception of pain and anxiety might also contribute. "Maybe by relieving symptoms, there’s less anxiety as a result," said Dr. Mahler.
He addressed concerns over the "double effect" whereby opioids used to lessen symptoms might actually hasten death in a patient with refractory dyspnea, saying the studies "don’t really support that." Dr. Mahler cited data indicating that higher doses of benzodiazepines used in withdrawal of life-sustaining treatment were not associated with a decreased time from withdrawal of life support to death (CHEST 2004;126:286-93).
As for respiratory depression, Dr. Mahler said he had reviewed 11 studies and found only one report of any change in oxygen saturation after opioid administration.
In deciding whether a patient should be given opioid therapy, Dr. Mahler said physicians should be sure that standard therapies are inadequate and that the risk/benefit ratio favors trial treatment. Establishing treatment goals and confirming that the patient and/or the patient’s family are on board with a trial of opioid treatment is key, he added.
To determine titration, physicians should ask the patients to rate their breathing difficulty. "This is a critical part of the assessment," said Dr. Mahler, noting that the level of breathlessness determines the dose and duration of action.
If dyspnea is episodic, he said, "it doesn’t make sense to administer a long-acting opioid" and so an immediate-release or short-acting form should be considered. If it’s constant, sustained release may be effective, he said.
Dr. Mahler, who said his presentation was related to the off-label use of morphine only, said that the important thing is to "titrate the opioid to achieve the lower effective dose based on the patient’s rating of the dyspnea." Adding an anxiolytic could also be considered, he said. "It’s pretty straightforward that you should discontinue the opioid if there is an unsatisfactory response or if there is an adverse effect."
Dr. Mahler disclosed ties with numerous pharmaceutical manufacturers and other medical organizations, including GlaxoSmithKline, Novartis, and Sunovion.
EXPERT ANALYSIS FROM CHEST 2013
Discharge protocols cut 30-day bariatric surgery readmissions
ATLANTA – The addition of a comprehensive discharge protocol checklist and follow-up contact for bariatric surgery patients resulted in slightly longer hospital lengths of stay but significant reductions in readmissions.
"I feel the small amount of extra length of stay really supports the 46% overall decrease in readmissions. That’s pretty good," Sharon A. Krzyzanowski, RN, said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
To determine if the addition of discharge protocols had helped their bariatric surgery facility reduce the rate of 30-day readmissions, Ms. Krzyzanowski and her colleagues at the Celebration Health Florida Hospital in Orlando retrospectively analyzed patient data both pre- and post-implementation.
They compared the data of 224 Roux-en-Y gastric bypass (RYGB) patients before implementation of the protocols to 242 post-protocol RYGB patients; 125 pre-protocol laparoscopic gastric sleeve (LGS) patients to 178 post-protocol patients; and 100 gastric band patients admitted before the center had the protocols in place, vs. 50 such patients after the protocols.
Discharge protocols stipulated that patients must not be in extreme pain and were able to tolerate their pain medication; that they were not nauseous and were able to tolerate their nausea medication; and that they were able to comfortably drink a minimum of 30 ounces on the day of discharge. Respiratory values also had to be at "status quo," said Ms. Krzyzanowski. If patients did not meet any of those protocols, they were not discharged that day.
The second portion of the protocol that the researchers examined was post-discharge patient follow-up, either by phone or by e-mail. Under the protocol, a nurse contacted patients to discuss mental status, medications, postoperative regime, and any other questions the patients might have.
Patient readmissions were sorted according to reasons of technical concern, such as organ injury or leak; physical issues, such as an infection or a thromboembolic event; or general malaise, such as dehydration or benign abdominal pain.
The investigators determined that readmission rates in RYGB patients declined by 38.3%; 34.7% in LGS patients; and 100% in gastric banding patients.
The hospital length of stay in the RYGB group went from a pre-protocol average of 2.12 days to 2.50 days post protocol; in the LGS group, the average length of stay went from 1.93 to 2.10 average days.
The investigators found there was an overall reduction in readmissions of 46%. Readmissions associated with malaise were reduced from 6.5% to 2.9%; those associated with physical concerns were reduced from 2.9% to 2.1%, said Ms. Krzyzanowski. Technical readmissions did not change significantly.
During the question-and-answer portion of the presentation, Ms. Krzyzanowski said in response to a query about reimbursements for keeping patients an extra day, "As long as it’s documented why the patient is staying, insurance will review that and they will be fine. We have not had anybody denied for a third day."
Ms. Krzyzanowski, Dr. Kim, and Dr. Buffington reported no relevant disclosures.
ATLANTA – The addition of a comprehensive discharge protocol checklist and follow-up contact for bariatric surgery patients resulted in slightly longer hospital lengths of stay but significant reductions in readmissions.
"I feel the small amount of extra length of stay really supports the 46% overall decrease in readmissions. That’s pretty good," Sharon A. Krzyzanowski, RN, said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
To determine if the addition of discharge protocols had helped their bariatric surgery facility reduce the rate of 30-day readmissions, Ms. Krzyzanowski and her colleagues at the Celebration Health Florida Hospital in Orlando retrospectively analyzed patient data both pre- and post-implementation.
They compared the data of 224 Roux-en-Y gastric bypass (RYGB) patients before implementation of the protocols to 242 post-protocol RYGB patients; 125 pre-protocol laparoscopic gastric sleeve (LGS) patients to 178 post-protocol patients; and 100 gastric band patients admitted before the center had the protocols in place, vs. 50 such patients after the protocols.
Discharge protocols stipulated that patients must not be in extreme pain and were able to tolerate their pain medication; that they were not nauseous and were able to tolerate their nausea medication; and that they were able to comfortably drink a minimum of 30 ounces on the day of discharge. Respiratory values also had to be at "status quo," said Ms. Krzyzanowski. If patients did not meet any of those protocols, they were not discharged that day.
The second portion of the protocol that the researchers examined was post-discharge patient follow-up, either by phone or by e-mail. Under the protocol, a nurse contacted patients to discuss mental status, medications, postoperative regime, and any other questions the patients might have.
Patient readmissions were sorted according to reasons of technical concern, such as organ injury or leak; physical issues, such as an infection or a thromboembolic event; or general malaise, such as dehydration or benign abdominal pain.
The investigators determined that readmission rates in RYGB patients declined by 38.3%; 34.7% in LGS patients; and 100% in gastric banding patients.
The hospital length of stay in the RYGB group went from a pre-protocol average of 2.12 days to 2.50 days post protocol; in the LGS group, the average length of stay went from 1.93 to 2.10 average days.
The investigators found there was an overall reduction in readmissions of 46%. Readmissions associated with malaise were reduced from 6.5% to 2.9%; those associated with physical concerns were reduced from 2.9% to 2.1%, said Ms. Krzyzanowski. Technical readmissions did not change significantly.
During the question-and-answer portion of the presentation, Ms. Krzyzanowski said in response to a query about reimbursements for keeping patients an extra day, "As long as it’s documented why the patient is staying, insurance will review that and they will be fine. We have not had anybody denied for a third day."
Ms. Krzyzanowski, Dr. Kim, and Dr. Buffington reported no relevant disclosures.
ATLANTA – The addition of a comprehensive discharge protocol checklist and follow-up contact for bariatric surgery patients resulted in slightly longer hospital lengths of stay but significant reductions in readmissions.
"I feel the small amount of extra length of stay really supports the 46% overall decrease in readmissions. That’s pretty good," Sharon A. Krzyzanowski, RN, said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
To determine if the addition of discharge protocols had helped their bariatric surgery facility reduce the rate of 30-day readmissions, Ms. Krzyzanowski and her colleagues at the Celebration Health Florida Hospital in Orlando retrospectively analyzed patient data both pre- and post-implementation.
They compared the data of 224 Roux-en-Y gastric bypass (RYGB) patients before implementation of the protocols to 242 post-protocol RYGB patients; 125 pre-protocol laparoscopic gastric sleeve (LGS) patients to 178 post-protocol patients; and 100 gastric band patients admitted before the center had the protocols in place, vs. 50 such patients after the protocols.
Discharge protocols stipulated that patients must not be in extreme pain and were able to tolerate their pain medication; that they were not nauseous and were able to tolerate their nausea medication; and that they were able to comfortably drink a minimum of 30 ounces on the day of discharge. Respiratory values also had to be at "status quo," said Ms. Krzyzanowski. If patients did not meet any of those protocols, they were not discharged that day.
The second portion of the protocol that the researchers examined was post-discharge patient follow-up, either by phone or by e-mail. Under the protocol, a nurse contacted patients to discuss mental status, medications, postoperative regime, and any other questions the patients might have.
Patient readmissions were sorted according to reasons of technical concern, such as organ injury or leak; physical issues, such as an infection or a thromboembolic event; or general malaise, such as dehydration or benign abdominal pain.
The investigators determined that readmission rates in RYGB patients declined by 38.3%; 34.7% in LGS patients; and 100% in gastric banding patients.
The hospital length of stay in the RYGB group went from a pre-protocol average of 2.12 days to 2.50 days post protocol; in the LGS group, the average length of stay went from 1.93 to 2.10 average days.
The investigators found there was an overall reduction in readmissions of 46%. Readmissions associated with malaise were reduced from 6.5% to 2.9%; those associated with physical concerns were reduced from 2.9% to 2.1%, said Ms. Krzyzanowski. Technical readmissions did not change significantly.
During the question-and-answer portion of the presentation, Ms. Krzyzanowski said in response to a query about reimbursements for keeping patients an extra day, "As long as it’s documented why the patient is staying, insurance will review that and they will be fine. We have not had anybody denied for a third day."
Ms. Krzyzanowski, Dr. Kim, and Dr. Buffington reported no relevant disclosures.
AT OBESITY WEEK
Major finding: 30-day readmissions after bariatric surgery fell 46% after implementation of discharge protocols.
Data source: Review of single surgery site patient data pre- and post-protocol implementation.
Disclosures: Ms. Krzyzanowski, Dr. Kim, and Dr. Buffington reported no relevant disclosures.
Battle brews over screening for asymptomatic kidney disease
Adults who don’t show symptoms of, or have risk factors for, early chronic kidney disease should not be screened for it, according to new guidelines from the American College of Physicians.
But the ACP’s recommendation prompted the American Society of Nephrology to counter with its own strong recommendation in favor of kidney disease screening regardless of a patient’s risk factors.
"There is no evidence that obtaining a ‘baseline creatinine’ level, or screening for renal dysfunction in asymptomatic individuals with no risk factors for kidney disease, improves outcomes for patients," said ACP President Molly Cooke in an interview.
The clinical practice guidelines are the first issued by the ACP for the screening, monitoring, and treatment of stage 1-3 chronic kidney disease in adults. Major risk factors for CKD in adults include diabetes, hypertension, and cardiovascular disease.
The ACP published the guidelines online in Annals of Internal Medicine 2013 Oct. 22 [doi:10.7326/0003-4819-159-12-201312170-00726]).
The college’s Clinical Guidelines Committee used Medline and Cochrane databases to systematically review all relevant data published between 1985 and November 2011. Outcomes assessed for the guidelines included all-cause mortality, cardiovascular events and disease, composite renal and vascular outcomes, end-stage renal disease, quality of life, physical function, and activities of daily living.
The investigators determined that there was not enough evidence to evaluate the benefits and harms of screening for early CKD, and so they recommended that clinicians not perform it.
The ACP specifically recommended against proteinuria testing in adults with or without diabetes and who are currently taking angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs). That recommendation was a “reminder to physicians not to do tests that will not change patient management,” Dr. Cooke said. ACE inhibitors or ARBs are already the treatment for microalbuminuria, a form of low-grade proteinuria. “There is no evidence that monitoring proteinuria to assess the effects of pharmacological hypertension management produces better outcomes,” she added.
ASN: No screen? No way!
The ACP’s recommendations spurred an immediate rebuke from the American Society of Nephrology.
“Early detection is the key to preventing patients from progressing to relying on dialysis to stay alive,” Dr. Tod Ibrahim, the ASN’s executive director, said in a statement. “ASN and its nearly 15,000 members – all of whom are experts in kidney disease – are disappointed by ACP’s irresponsible recommendation.”
The lack of evidence on the benefits and harms of early CKD screening is precisely why physicians should test for early-stage CKD, according to ASN President Bruce Molitoris.
“One of the problems with CKD is we don’t have effective mechanisms to detect it early,” he said in an interview. “What we do have is screening for proteinuria, which is a very simple, extremely inexpensive test that can give great insight.”
As for proteinuria testing in adults taking ACE inhibitors or ARBs, there might be a more nuanced benefit, Dr. Molitoris explained. “It’s a little bit more incentive to increase compliance in a patient who is taking a medication for hypertension if you tell them they’re getting progressive kidney disease if they don’t control their blood pressure,” he said. “Not all patients with hypertension are started out on those first-line drugs,” he added.
The ACP endorses treating patients who have hypertension or stage 1-3 CKD with ACE inhibitors or ARBs, as well as giving patients with early CKD appropriate statin therapy to manage elevated levels of low-density lipoprotein. However, the college calls additional screening and treatment largely superfluous.
“For doctors who have been using a thiazide diuretic or a beta-blocker as their initial antihypertensive of choice, this guideline should change their practice,” said Dr. Cooke. However, because many practice “report cards” call for an annual urine microalbumin test in diabetic patients, many physicians perform the test on patients who are already on an ACE inhibitor or an ARB, she said.
“This guideline should prompt them to respond ‘test not indicated’ when it is requested,” Dr. Cooke said.
The ACP found no significant differences in outcomes between ACE inhibitors and ARBs, although it did note that the risk of adverse effects (cough, hyperkalemia, hypotension, and dialysis) significantly increased in combined ACE inhibitor and ARB therapy.
Meanwhile, the National Kidney Foundation recommends that anyone with diabetes, hypertension, cardiovascular disease, age over 60, or a family history of kidney failure have a blood test to estimate their glomerular filtration rate (GFR) and a urine test for proteinuria.
“The ACP guidelines looked at the clinical outcomes of CKD very differently than our guidelines did,” cautioned Sean Roach, spokesperson for the NKF, in an e-mail. The ACP put “CKD stages 1-3 together when they have markedly different risks of adverse outcomes, and [didn’t take] into account all of the patient safety issues that arise due to ignorance of a patient’s level of kidney function.
“We acknowledge that there have been no randomized trials of CKD screening,” Mr. Roach noted, “but our recommendations are based on extensive analysis of observational trials, clinical trials of diabetes and antihypertensive drugs, and clinical experience.”
Critics question CKD criteria
A recent U.S. Preventive Services Task Force (USPSTF) report took a position similar to the ACP’s, stating there is currently insufficient evidence to recommend general population-based screening. That report noted that although early screening could affect outcomes for people already diagnosed with conditions such as diabetes or hypertension, no evidence existed to show the benefits of early treatment in people without these risk factors.
The ASN swiftly responded. "We sent [the USPSTF] a letter asking them to reconsider," said Dr. Molitoris. "That was within the last 6 months. They came back with a ‘high recommendation’ for collecting more data to analyze the cost effectiveness of screening."
In 2002, the NFK-sponsored Kidney Disease: Improving Global Outcomes (KDIGO) released landmark guidelines on CKD. In a 2012 guidelines update, KDIGO kept the criteria it established in 2002 for CKD, including diagnostic thresholds of a GFR less than 60 mL/min per 1.73 m2 and an albumin/creatinine ratio (ACR) of at least 30 mg/g. And it maintained its five-stage CKD classification system.
But it expanded the existing five-stage classification system to include two subcategories of grade 3 GFR categories – G3a, with a GFR of 45-59; and G3b, with a GFR of 30-44 – and three additional categories of albuminuria (Ann. Intern. Med. 2013;158:825-30).
Those CKD criteria raised eyebrows not just at the ACP, but also with some evidence-based medicine scholars. In an analysis published online earlier this year in BMJ, Dr. Roy Moynihan of the Centre for Research in Evidence-Based Practice, Robina, Australia, cited data that the GFR value used by KDIGO to determine early CKD falls within the normal range for men over age 60 and women over age 50.
By "labeling so many people at low risk of symptoms as having chronic kidney disease, the new definition axiomatically produces overdiagnosis," Dr. Moynihan and his colleagues cautioned (BMJ 2013;347:f4298).
Prior to the 2002 publication of the KDIGO criteria for CKD, according to Dr. Moynihan, the incidence rate for CKD in U.S. adults was estimated to be around 1.7%. After 2002, using the KDIGO criteria, it rose to 1 in 8 adults, or about 14% of the adult population.
"The controversial aspect around that is, at what point as your GFR decreases does it become abnormal?" cautioned Dr. Molitoris. "If you have a reduced GFR, and proteinuria, we know that’s abnormal. That’s why the screening for proteinuria is so important. If you just have a reduced GFR to a certain extent, it may be a normal aging process. That’s the European perspective, and I think they have a point there."
‘Different worldview’
While the ACP guidelines for CKD refer to the KDIGO criteria as their counterpoint, Dr. Cooke said she did not know what motivated KDIGO to expand the criteria. She suggested it might be the "different worldview" phenomenon that often occurs between subspecialists and generalists.
"It’s tempting to say, ‘Let’s just test everybody’s creatinine,’ " Dr. Cooke noted. "But it’s just like with prostate cancer screening: Once you start to factor in all the costs – and not just the money – of testing on that broad of a scale, it doesn’t [add up]."
But Dr. Molitoris countered that CKD screening is more akin to testing for cardiovascular disease.
"One could make the comparison to checking for cholesterol, only that’s invasive – that’s drawing blood," he said. "This is just taking urine, and yet, how many people do we screen for cholesterol? There is no risk in doing the proteinuria test. You collect the urine, put a stick into it, and read it. If it’s positive, then you will follow up with a more sophisticated chemical test." He also noted that false positives in proteinuria tests are rare.
The ACP guidelines offer physicians what it calls "high-value care advice": Skip early CKD screening, because in the absence of evidence that screening improves clinical outcomes, "testing will add costs, owing to both the screening test and additional follow-up tests (including those resulting from false-positive findings), increased medical visits, and costs of keeping or obtaining health insurance."
Dr. Molitoris disagreed, citing "the aggressive and silent nature" of kidney disease in all its stages.
"You have to think of the cost analysis as how many screenings you can do for the cost of one patient who goes on to need dialysis. That costs between $80,000 and $90,000 a year to maintain for every year [a patient is] on it," Dr. Molitoris explained. "You can do a lot of screening on that."
Dr. Cooke said the ACP was calling for a "middle ground" to bring the discussion back to what is best for the patient, not the practitioner.
"We are saying that unless the patient has a reason for you to be concerned, other than the fact that they are a human being, there is no reason to screen for CKD every year," she explained. "There is no evidence that diagnosing the average person on the street as stage 1 or 2 [CKD] does them any good if they don’t have any risk factors."
The American College of Physicians funded the guidelines. The guidelines’ authors had no relevant disclosures.
Adults who don’t show symptoms of, or have risk factors for, early chronic kidney disease should not be screened for it, according to new guidelines from the American College of Physicians.
But the ACP’s recommendation prompted the American Society of Nephrology to counter with its own strong recommendation in favor of kidney disease screening regardless of a patient’s risk factors.
"There is no evidence that obtaining a ‘baseline creatinine’ level, or screening for renal dysfunction in asymptomatic individuals with no risk factors for kidney disease, improves outcomes for patients," said ACP President Molly Cooke in an interview.
The clinical practice guidelines are the first issued by the ACP for the screening, monitoring, and treatment of stage 1-3 chronic kidney disease in adults. Major risk factors for CKD in adults include diabetes, hypertension, and cardiovascular disease.
The ACP published the guidelines online in Annals of Internal Medicine 2013 Oct. 22 [doi:10.7326/0003-4819-159-12-201312170-00726]).
The college’s Clinical Guidelines Committee used Medline and Cochrane databases to systematically review all relevant data published between 1985 and November 2011. Outcomes assessed for the guidelines included all-cause mortality, cardiovascular events and disease, composite renal and vascular outcomes, end-stage renal disease, quality of life, physical function, and activities of daily living.
The investigators determined that there was not enough evidence to evaluate the benefits and harms of screening for early CKD, and so they recommended that clinicians not perform it.
The ACP specifically recommended against proteinuria testing in adults with or without diabetes and who are currently taking angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs). That recommendation was a “reminder to physicians not to do tests that will not change patient management,” Dr. Cooke said. ACE inhibitors or ARBs are already the treatment for microalbuminuria, a form of low-grade proteinuria. “There is no evidence that monitoring proteinuria to assess the effects of pharmacological hypertension management produces better outcomes,” she added.
ASN: No screen? No way!
The ACP’s recommendations spurred an immediate rebuke from the American Society of Nephrology.
“Early detection is the key to preventing patients from progressing to relying on dialysis to stay alive,” Dr. Tod Ibrahim, the ASN’s executive director, said in a statement. “ASN and its nearly 15,000 members – all of whom are experts in kidney disease – are disappointed by ACP’s irresponsible recommendation.”
The lack of evidence on the benefits and harms of early CKD screening is precisely why physicians should test for early-stage CKD, according to ASN President Bruce Molitoris.
“One of the problems with CKD is we don’t have effective mechanisms to detect it early,” he said in an interview. “What we do have is screening for proteinuria, which is a very simple, extremely inexpensive test that can give great insight.”
As for proteinuria testing in adults taking ACE inhibitors or ARBs, there might be a more nuanced benefit, Dr. Molitoris explained. “It’s a little bit more incentive to increase compliance in a patient who is taking a medication for hypertension if you tell them they’re getting progressive kidney disease if they don’t control their blood pressure,” he said. “Not all patients with hypertension are started out on those first-line drugs,” he added.
The ACP endorses treating patients who have hypertension or stage 1-3 CKD with ACE inhibitors or ARBs, as well as giving patients with early CKD appropriate statin therapy to manage elevated levels of low-density lipoprotein. However, the college calls additional screening and treatment largely superfluous.
“For doctors who have been using a thiazide diuretic or a beta-blocker as their initial antihypertensive of choice, this guideline should change their practice,” said Dr. Cooke. However, because many practice “report cards” call for an annual urine microalbumin test in diabetic patients, many physicians perform the test on patients who are already on an ACE inhibitor or an ARB, she said.
“This guideline should prompt them to respond ‘test not indicated’ when it is requested,” Dr. Cooke said.
The ACP found no significant differences in outcomes between ACE inhibitors and ARBs, although it did note that the risk of adverse effects (cough, hyperkalemia, hypotension, and dialysis) significantly increased in combined ACE inhibitor and ARB therapy.
Meanwhile, the National Kidney Foundation recommends that anyone with diabetes, hypertension, cardiovascular disease, age over 60, or a family history of kidney failure have a blood test to estimate their glomerular filtration rate (GFR) and a urine test for proteinuria.
“The ACP guidelines looked at the clinical outcomes of CKD very differently than our guidelines did,” cautioned Sean Roach, spokesperson for the NKF, in an e-mail. The ACP put “CKD stages 1-3 together when they have markedly different risks of adverse outcomes, and [didn’t take] into account all of the patient safety issues that arise due to ignorance of a patient’s level of kidney function.
“We acknowledge that there have been no randomized trials of CKD screening,” Mr. Roach noted, “but our recommendations are based on extensive analysis of observational trials, clinical trials of diabetes and antihypertensive drugs, and clinical experience.”
Critics question CKD criteria
A recent U.S. Preventive Services Task Force (USPSTF) report took a position similar to the ACP’s, stating there is currently insufficient evidence to recommend general population-based screening. That report noted that although early screening could affect outcomes for people already diagnosed with conditions such as diabetes or hypertension, no evidence existed to show the benefits of early treatment in people without these risk factors.
The ASN swiftly responded. "We sent [the USPSTF] a letter asking them to reconsider," said Dr. Molitoris. "That was within the last 6 months. They came back with a ‘high recommendation’ for collecting more data to analyze the cost effectiveness of screening."
In 2002, the NFK-sponsored Kidney Disease: Improving Global Outcomes (KDIGO) released landmark guidelines on CKD. In a 2012 guidelines update, KDIGO kept the criteria it established in 2002 for CKD, including diagnostic thresholds of a GFR less than 60 mL/min per 1.73 m2 and an albumin/creatinine ratio (ACR) of at least 30 mg/g. And it maintained its five-stage CKD classification system.
But it expanded the existing five-stage classification system to include two subcategories of grade 3 GFR categories – G3a, with a GFR of 45-59; and G3b, with a GFR of 30-44 – and three additional categories of albuminuria (Ann. Intern. Med. 2013;158:825-30).
Those CKD criteria raised eyebrows not just at the ACP, but also with some evidence-based medicine scholars. In an analysis published online earlier this year in BMJ, Dr. Roy Moynihan of the Centre for Research in Evidence-Based Practice, Robina, Australia, cited data that the GFR value used by KDIGO to determine early CKD falls within the normal range for men over age 60 and women over age 50.
By "labeling so many people at low risk of symptoms as having chronic kidney disease, the new definition axiomatically produces overdiagnosis," Dr. Moynihan and his colleagues cautioned (BMJ 2013;347:f4298).
Prior to the 2002 publication of the KDIGO criteria for CKD, according to Dr. Moynihan, the incidence rate for CKD in U.S. adults was estimated to be around 1.7%. After 2002, using the KDIGO criteria, it rose to 1 in 8 adults, or about 14% of the adult population.
"The controversial aspect around that is, at what point as your GFR decreases does it become abnormal?" cautioned Dr. Molitoris. "If you have a reduced GFR, and proteinuria, we know that’s abnormal. That’s why the screening for proteinuria is so important. If you just have a reduced GFR to a certain extent, it may be a normal aging process. That’s the European perspective, and I think they have a point there."
‘Different worldview’
While the ACP guidelines for CKD refer to the KDIGO criteria as their counterpoint, Dr. Cooke said she did not know what motivated KDIGO to expand the criteria. She suggested it might be the "different worldview" phenomenon that often occurs between subspecialists and generalists.
"It’s tempting to say, ‘Let’s just test everybody’s creatinine,’ " Dr. Cooke noted. "But it’s just like with prostate cancer screening: Once you start to factor in all the costs – and not just the money – of testing on that broad of a scale, it doesn’t [add up]."
But Dr. Molitoris countered that CKD screening is more akin to testing for cardiovascular disease.
"One could make the comparison to checking for cholesterol, only that’s invasive – that’s drawing blood," he said. "This is just taking urine, and yet, how many people do we screen for cholesterol? There is no risk in doing the proteinuria test. You collect the urine, put a stick into it, and read it. If it’s positive, then you will follow up with a more sophisticated chemical test." He also noted that false positives in proteinuria tests are rare.
The ACP guidelines offer physicians what it calls "high-value care advice": Skip early CKD screening, because in the absence of evidence that screening improves clinical outcomes, "testing will add costs, owing to both the screening test and additional follow-up tests (including those resulting from false-positive findings), increased medical visits, and costs of keeping or obtaining health insurance."
Dr. Molitoris disagreed, citing "the aggressive and silent nature" of kidney disease in all its stages.
"You have to think of the cost analysis as how many screenings you can do for the cost of one patient who goes on to need dialysis. That costs between $80,000 and $90,000 a year to maintain for every year [a patient is] on it," Dr. Molitoris explained. "You can do a lot of screening on that."
Dr. Cooke said the ACP was calling for a "middle ground" to bring the discussion back to what is best for the patient, not the practitioner.
"We are saying that unless the patient has a reason for you to be concerned, other than the fact that they are a human being, there is no reason to screen for CKD every year," she explained. "There is no evidence that diagnosing the average person on the street as stage 1 or 2 [CKD] does them any good if they don’t have any risk factors."
The American College of Physicians funded the guidelines. The guidelines’ authors had no relevant disclosures.
Adults who don’t show symptoms of, or have risk factors for, early chronic kidney disease should not be screened for it, according to new guidelines from the American College of Physicians.
But the ACP’s recommendation prompted the American Society of Nephrology to counter with its own strong recommendation in favor of kidney disease screening regardless of a patient’s risk factors.
"There is no evidence that obtaining a ‘baseline creatinine’ level, or screening for renal dysfunction in asymptomatic individuals with no risk factors for kidney disease, improves outcomes for patients," said ACP President Molly Cooke in an interview.
The clinical practice guidelines are the first issued by the ACP for the screening, monitoring, and treatment of stage 1-3 chronic kidney disease in adults. Major risk factors for CKD in adults include diabetes, hypertension, and cardiovascular disease.
The ACP published the guidelines online in Annals of Internal Medicine 2013 Oct. 22 [doi:10.7326/0003-4819-159-12-201312170-00726]).
The college’s Clinical Guidelines Committee used Medline and Cochrane databases to systematically review all relevant data published between 1985 and November 2011. Outcomes assessed for the guidelines included all-cause mortality, cardiovascular events and disease, composite renal and vascular outcomes, end-stage renal disease, quality of life, physical function, and activities of daily living.
The investigators determined that there was not enough evidence to evaluate the benefits and harms of screening for early CKD, and so they recommended that clinicians not perform it.
The ACP specifically recommended against proteinuria testing in adults with or without diabetes and who are currently taking angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs). That recommendation was a “reminder to physicians not to do tests that will not change patient management,” Dr. Cooke said. ACE inhibitors or ARBs are already the treatment for microalbuminuria, a form of low-grade proteinuria. “There is no evidence that monitoring proteinuria to assess the effects of pharmacological hypertension management produces better outcomes,” she added.
ASN: No screen? No way!
The ACP’s recommendations spurred an immediate rebuke from the American Society of Nephrology.
“Early detection is the key to preventing patients from progressing to relying on dialysis to stay alive,” Dr. Tod Ibrahim, the ASN’s executive director, said in a statement. “ASN and its nearly 15,000 members – all of whom are experts in kidney disease – are disappointed by ACP’s irresponsible recommendation.”
The lack of evidence on the benefits and harms of early CKD screening is precisely why physicians should test for early-stage CKD, according to ASN President Bruce Molitoris.
“One of the problems with CKD is we don’t have effective mechanisms to detect it early,” he said in an interview. “What we do have is screening for proteinuria, which is a very simple, extremely inexpensive test that can give great insight.”
As for proteinuria testing in adults taking ACE inhibitors or ARBs, there might be a more nuanced benefit, Dr. Molitoris explained. “It’s a little bit more incentive to increase compliance in a patient who is taking a medication for hypertension if you tell them they’re getting progressive kidney disease if they don’t control their blood pressure,” he said. “Not all patients with hypertension are started out on those first-line drugs,” he added.
The ACP endorses treating patients who have hypertension or stage 1-3 CKD with ACE inhibitors or ARBs, as well as giving patients with early CKD appropriate statin therapy to manage elevated levels of low-density lipoprotein. However, the college calls additional screening and treatment largely superfluous.
“For doctors who have been using a thiazide diuretic or a beta-blocker as their initial antihypertensive of choice, this guideline should change their practice,” said Dr. Cooke. However, because many practice “report cards” call for an annual urine microalbumin test in diabetic patients, many physicians perform the test on patients who are already on an ACE inhibitor or an ARB, she said.
“This guideline should prompt them to respond ‘test not indicated’ when it is requested,” Dr. Cooke said.
The ACP found no significant differences in outcomes between ACE inhibitors and ARBs, although it did note that the risk of adverse effects (cough, hyperkalemia, hypotension, and dialysis) significantly increased in combined ACE inhibitor and ARB therapy.
Meanwhile, the National Kidney Foundation recommends that anyone with diabetes, hypertension, cardiovascular disease, age over 60, or a family history of kidney failure have a blood test to estimate their glomerular filtration rate (GFR) and a urine test for proteinuria.
“The ACP guidelines looked at the clinical outcomes of CKD very differently than our guidelines did,” cautioned Sean Roach, spokesperson for the NKF, in an e-mail. The ACP put “CKD stages 1-3 together when they have markedly different risks of adverse outcomes, and [didn’t take] into account all of the patient safety issues that arise due to ignorance of a patient’s level of kidney function.
“We acknowledge that there have been no randomized trials of CKD screening,” Mr. Roach noted, “but our recommendations are based on extensive analysis of observational trials, clinical trials of diabetes and antihypertensive drugs, and clinical experience.”
Critics question CKD criteria
A recent U.S. Preventive Services Task Force (USPSTF) report took a position similar to the ACP’s, stating there is currently insufficient evidence to recommend general population-based screening. That report noted that although early screening could affect outcomes for people already diagnosed with conditions such as diabetes or hypertension, no evidence existed to show the benefits of early treatment in people without these risk factors.
The ASN swiftly responded. "We sent [the USPSTF] a letter asking them to reconsider," said Dr. Molitoris. "That was within the last 6 months. They came back with a ‘high recommendation’ for collecting more data to analyze the cost effectiveness of screening."
In 2002, the NFK-sponsored Kidney Disease: Improving Global Outcomes (KDIGO) released landmark guidelines on CKD. In a 2012 guidelines update, KDIGO kept the criteria it established in 2002 for CKD, including diagnostic thresholds of a GFR less than 60 mL/min per 1.73 m2 and an albumin/creatinine ratio (ACR) of at least 30 mg/g. And it maintained its five-stage CKD classification system.
But it expanded the existing five-stage classification system to include two subcategories of grade 3 GFR categories – G3a, with a GFR of 45-59; and G3b, with a GFR of 30-44 – and three additional categories of albuminuria (Ann. Intern. Med. 2013;158:825-30).
Those CKD criteria raised eyebrows not just at the ACP, but also with some evidence-based medicine scholars. In an analysis published online earlier this year in BMJ, Dr. Roy Moynihan of the Centre for Research in Evidence-Based Practice, Robina, Australia, cited data that the GFR value used by KDIGO to determine early CKD falls within the normal range for men over age 60 and women over age 50.
By "labeling so many people at low risk of symptoms as having chronic kidney disease, the new definition axiomatically produces overdiagnosis," Dr. Moynihan and his colleagues cautioned (BMJ 2013;347:f4298).
Prior to the 2002 publication of the KDIGO criteria for CKD, according to Dr. Moynihan, the incidence rate for CKD in U.S. adults was estimated to be around 1.7%. After 2002, using the KDIGO criteria, it rose to 1 in 8 adults, or about 14% of the adult population.
"The controversial aspect around that is, at what point as your GFR decreases does it become abnormal?" cautioned Dr. Molitoris. "If you have a reduced GFR, and proteinuria, we know that’s abnormal. That’s why the screening for proteinuria is so important. If you just have a reduced GFR to a certain extent, it may be a normal aging process. That’s the European perspective, and I think they have a point there."
‘Different worldview’
While the ACP guidelines for CKD refer to the KDIGO criteria as their counterpoint, Dr. Cooke said she did not know what motivated KDIGO to expand the criteria. She suggested it might be the "different worldview" phenomenon that often occurs between subspecialists and generalists.
"It’s tempting to say, ‘Let’s just test everybody’s creatinine,’ " Dr. Cooke noted. "But it’s just like with prostate cancer screening: Once you start to factor in all the costs – and not just the money – of testing on that broad of a scale, it doesn’t [add up]."
But Dr. Molitoris countered that CKD screening is more akin to testing for cardiovascular disease.
"One could make the comparison to checking for cholesterol, only that’s invasive – that’s drawing blood," he said. "This is just taking urine, and yet, how many people do we screen for cholesterol? There is no risk in doing the proteinuria test. You collect the urine, put a stick into it, and read it. If it’s positive, then you will follow up with a more sophisticated chemical test." He also noted that false positives in proteinuria tests are rare.
The ACP guidelines offer physicians what it calls "high-value care advice": Skip early CKD screening, because in the absence of evidence that screening improves clinical outcomes, "testing will add costs, owing to both the screening test and additional follow-up tests (including those resulting from false-positive findings), increased medical visits, and costs of keeping or obtaining health insurance."
Dr. Molitoris disagreed, citing "the aggressive and silent nature" of kidney disease in all its stages.
"You have to think of the cost analysis as how many screenings you can do for the cost of one patient who goes on to need dialysis. That costs between $80,000 and $90,000 a year to maintain for every year [a patient is] on it," Dr. Molitoris explained. "You can do a lot of screening on that."
Dr. Cooke said the ACP was calling for a "middle ground" to bring the discussion back to what is best for the patient, not the practitioner.
"We are saying that unless the patient has a reason for you to be concerned, other than the fact that they are a human being, there is no reason to screen for CKD every year," she explained. "There is no evidence that diagnosing the average person on the street as stage 1 or 2 [CKD] does them any good if they don’t have any risk factors."
The American College of Physicians funded the guidelines. The guidelines’ authors had no relevant disclosures.
FROM ANNALS OF INTERNAL MEDICINE
Major finding: New guidelines from the American College of Physicians warn that the risks outweigh the benefits of screening asymptomatic adults with no risk factors for stage 1-3 chronic kidney disease.
Data source: Systematic evidence review of relevant studies in the 1985-2011 Medline and Cochrane databases.
Disclosures: The American College of Physicians funded the guidelines. The guidelines’ authors had no relevant disclosures.
Reimbursement shortfall stymies pediatric obesity care
ATLANTA – The thought of bariatric surgery for obese pediatric patients makes Dr. Sarah Barlow, lead author of recommendations on the prevention, assessment, and treatment of obesity, uncomfortable.
"I have a little bit of a love/hate relationship with bariatric surgery," said Dr. Barlow. For some young people, the procedure can be life altering, "but there is a big jump [from] a behavior-based intervention to bariatric surgery," she said at the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Her reservation hinges upon the question that runs specialtywide for physicians who treat obesity: Just who "owns" the disease?
"Is this a health care problem that needs to be taken care of by doctors, or is this a community problem, and this is all about prevention?" was Dr. Barlow’s rhetorical question. "There are a lot of barriers. There are a lot of players, but not really any reimbursement," she said.
In the case of bariatric surgery for children, Dr. Barlow said she wonders whether obese youngsters are sometimes pushed into having medical treatments in order to skirt reimbursement issues, or because it’s just one more item to tick off for guideline-laden office practitioners who have limited time with patients but an ever-increasing list of precautionary pearls they are meant to dispense?
"The hate part of my relationship is that the bariatric results are so wonderful that I feel people aren’t putting resources into intensive [nonsurgical] treatments," said Dr. Barlow. "I think it’s an option that should be on the table, but I think that medication and behavioral interventions and other tertiary care type interventions should be considered," she noted, adding that bariatric surgery is certainly not the answer to severe obesity in a 10-year-old.
Dr. Barlow is the lead author of the oft-cited Expert Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity, published by the American Academy of Pediatrics in 2007, and jointly sponsored by the American Medical Association, the U.S. Health Resources and Service Administration, and the Centers for Disease Control and Prevention. The recommendations emphasize behavior modifications with techniques such as motivational interviewing and culturally oriented nutritional counseling.
However, while pediatricians are willing to talk to patients about eating habits and exercise, said Dr. Barlow, the discussion is "very superficial. It gets lost in the ultralong list of anticipatory guidance that has to get done in a very short time frame."
As for reimbursements, it is unclear whether the Affordable Care Act will help or hurt pediatricians faced with an obesity epidemic in their patients, but it may help, said Dr. Barlow of Baylor College of Medicine, Houston. The legislation emphasizes research, improved access to primary care, and community-oriented health care initiatives as ways that awareness may be raised, she noted.
As for the ACA’s impact on reimbursements, she said, "I believe the ACA says anything that the U.S. Preventative Services Task Force promotes should be covered." The group’s 2010 report said there is little evidence of impact from moderate to intensive behavior-based treatments, she added.
"The conclusion from that is that those kinds of programs should not be covered," said Dr. Barlow. "The question the task force was addressing was whether it was worth it [for pediatricians] to take the time to calculate [body mass index]. They want screening tests that are sensitive and once you have the answer, you can do something with."
When asked if the underlying problem will be identified any time soon, such as through genetics, food addiction, food environment, or lifestyle, Dr. Barlow said, "everyone wants to treat it as being black or white, using a very medical approach. But we just don’t know."
ATLANTA – The thought of bariatric surgery for obese pediatric patients makes Dr. Sarah Barlow, lead author of recommendations on the prevention, assessment, and treatment of obesity, uncomfortable.
"I have a little bit of a love/hate relationship with bariatric surgery," said Dr. Barlow. For some young people, the procedure can be life altering, "but there is a big jump [from] a behavior-based intervention to bariatric surgery," she said at the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Her reservation hinges upon the question that runs specialtywide for physicians who treat obesity: Just who "owns" the disease?
"Is this a health care problem that needs to be taken care of by doctors, or is this a community problem, and this is all about prevention?" was Dr. Barlow’s rhetorical question. "There are a lot of barriers. There are a lot of players, but not really any reimbursement," she said.
In the case of bariatric surgery for children, Dr. Barlow said she wonders whether obese youngsters are sometimes pushed into having medical treatments in order to skirt reimbursement issues, or because it’s just one more item to tick off for guideline-laden office practitioners who have limited time with patients but an ever-increasing list of precautionary pearls they are meant to dispense?
"The hate part of my relationship is that the bariatric results are so wonderful that I feel people aren’t putting resources into intensive [nonsurgical] treatments," said Dr. Barlow. "I think it’s an option that should be on the table, but I think that medication and behavioral interventions and other tertiary care type interventions should be considered," she noted, adding that bariatric surgery is certainly not the answer to severe obesity in a 10-year-old.
Dr. Barlow is the lead author of the oft-cited Expert Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity, published by the American Academy of Pediatrics in 2007, and jointly sponsored by the American Medical Association, the U.S. Health Resources and Service Administration, and the Centers for Disease Control and Prevention. The recommendations emphasize behavior modifications with techniques such as motivational interviewing and culturally oriented nutritional counseling.
However, while pediatricians are willing to talk to patients about eating habits and exercise, said Dr. Barlow, the discussion is "very superficial. It gets lost in the ultralong list of anticipatory guidance that has to get done in a very short time frame."
As for reimbursements, it is unclear whether the Affordable Care Act will help or hurt pediatricians faced with an obesity epidemic in their patients, but it may help, said Dr. Barlow of Baylor College of Medicine, Houston. The legislation emphasizes research, improved access to primary care, and community-oriented health care initiatives as ways that awareness may be raised, she noted.
As for the ACA’s impact on reimbursements, she said, "I believe the ACA says anything that the U.S. Preventative Services Task Force promotes should be covered." The group’s 2010 report said there is little evidence of impact from moderate to intensive behavior-based treatments, she added.
"The conclusion from that is that those kinds of programs should not be covered," said Dr. Barlow. "The question the task force was addressing was whether it was worth it [for pediatricians] to take the time to calculate [body mass index]. They want screening tests that are sensitive and once you have the answer, you can do something with."
When asked if the underlying problem will be identified any time soon, such as through genetics, food addiction, food environment, or lifestyle, Dr. Barlow said, "everyone wants to treat it as being black or white, using a very medical approach. But we just don’t know."
ATLANTA – The thought of bariatric surgery for obese pediatric patients makes Dr. Sarah Barlow, lead author of recommendations on the prevention, assessment, and treatment of obesity, uncomfortable.
"I have a little bit of a love/hate relationship with bariatric surgery," said Dr. Barlow. For some young people, the procedure can be life altering, "but there is a big jump [from] a behavior-based intervention to bariatric surgery," she said at the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Her reservation hinges upon the question that runs specialtywide for physicians who treat obesity: Just who "owns" the disease?
"Is this a health care problem that needs to be taken care of by doctors, or is this a community problem, and this is all about prevention?" was Dr. Barlow’s rhetorical question. "There are a lot of barriers. There are a lot of players, but not really any reimbursement," she said.
In the case of bariatric surgery for children, Dr. Barlow said she wonders whether obese youngsters are sometimes pushed into having medical treatments in order to skirt reimbursement issues, or because it’s just one more item to tick off for guideline-laden office practitioners who have limited time with patients but an ever-increasing list of precautionary pearls they are meant to dispense?
"The hate part of my relationship is that the bariatric results are so wonderful that I feel people aren’t putting resources into intensive [nonsurgical] treatments," said Dr. Barlow. "I think it’s an option that should be on the table, but I think that medication and behavioral interventions and other tertiary care type interventions should be considered," she noted, adding that bariatric surgery is certainly not the answer to severe obesity in a 10-year-old.
Dr. Barlow is the lead author of the oft-cited Expert Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity, published by the American Academy of Pediatrics in 2007, and jointly sponsored by the American Medical Association, the U.S. Health Resources and Service Administration, and the Centers for Disease Control and Prevention. The recommendations emphasize behavior modifications with techniques such as motivational interviewing and culturally oriented nutritional counseling.
However, while pediatricians are willing to talk to patients about eating habits and exercise, said Dr. Barlow, the discussion is "very superficial. It gets lost in the ultralong list of anticipatory guidance that has to get done in a very short time frame."
As for reimbursements, it is unclear whether the Affordable Care Act will help or hurt pediatricians faced with an obesity epidemic in their patients, but it may help, said Dr. Barlow of Baylor College of Medicine, Houston. The legislation emphasizes research, improved access to primary care, and community-oriented health care initiatives as ways that awareness may be raised, she noted.
As for the ACA’s impact on reimbursements, she said, "I believe the ACA says anything that the U.S. Preventative Services Task Force promotes should be covered." The group’s 2010 report said there is little evidence of impact from moderate to intensive behavior-based treatments, she added.
"The conclusion from that is that those kinds of programs should not be covered," said Dr. Barlow. "The question the task force was addressing was whether it was worth it [for pediatricians] to take the time to calculate [body mass index]. They want screening tests that are sensitive and once you have the answer, you can do something with."
When asked if the underlying problem will be identified any time soon, such as through genetics, food addiction, food environment, or lifestyle, Dr. Barlow said, "everyone wants to treat it as being black or white, using a very medical approach. But we just don’t know."
EXPERT ANALYSIS FROM OBESITY WEEK
Gastric bypass associated with greatest improvement in cardiac risk factors
WASHINGTON – One year out from surgery, gastric bypass, gastric sleeve, and gastric banding all showed considerable reductions in cardiac risk factors, but gastric bypass showed the greatest risk reduction of all three, as well as greater improvement in body mass index, according to a study presented at this year’s annual clinical congress of the American College of Surgeons.
Baseline and 1-year postoperative data were collected on 1,398 consecutive bariatric surgery patients by Christopher S. Crowe and his colleagues at Stanford (Calif.) University. The investigators sought to evaluate each type of surgery’s effect on biochemical cardiovascular risk factors. The follow-up rate at 12 months was 77%.
The values measured were hemoglobin A1c, fasting insulin, high-density lipoprotein (HDL), low-density lipoprotein (LDL), total cholesterol, triglycerides, high-sensitivity C-reactive protein (CRP), homocysteine, and lipoprotein (a).
Across the three groups, bypass patients tended to be younger by 1-2 years (mean age of this group was 44.3 years), and they had a higher baseline body mass index on average.
Excess weight loss after 1 year averaged 75% in the bypass patients, 55% in the patients with a sleeve, and 40% in those with a band.
When analyzing laboratory values for each group, the investigators found that fasting insulin levels were notably improved in all three groups; but at an improvement rate of 67.0%, the bypass patients had more than double the improvement of the gastric-band patients, while the gastric-sleeve patients showed a 63.7% improvement rate.
The CRP levels also improved dramatically in the bypass patients (67.1%), especially when compared with the band (21.2%) and sleeve (26.3%) groups. In addition, the ratio between triglycerides and HDL, a strong predictor of cardiovascular events, was differentially most improved in the bypass patients (38.5%), although improvement was also seen in both band (20.6%) and sleeve (35.2%) groups.
The investigators also sought to correlate each bariatric procedure’s resultant weight loss to improvement in specific cardiac risk factors. Only bypass was found to have a correlate between weight loss and total cholesterol and LDL reduction.
The triglyceride/HDL ratio improved with weight loss in both the bypass and band surgical groups. However, patients over age 50 and with a BMI greater than 50 kg/m2 had the least improvement in this ratio.
Reduction in CRP level was not found to be related to weight loss for any of the procedures, although CRP did improve substantially after all three operations, primarily in bypass patients. In response to a question from an audience member, Mr. Crowe, a medical student, said this was probably because of changes in patient lifestyle, diet, and medications, as well as smoking cessation, postoperatively.
"When someone comes in for a bariatric procedure, they’re not just receiving the surgery, they are changing a lot about their life," said Mr. Crowe. "Those changes could, in effect, decrease the CRP levels after surgery, without it being weight loss–dependent."
Mr. Crowe reported no relevant disclosures. His coinvestigators reported serving as consultants to Ethicon and Covidien.
WASHINGTON – One year out from surgery, gastric bypass, gastric sleeve, and gastric banding all showed considerable reductions in cardiac risk factors, but gastric bypass showed the greatest risk reduction of all three, as well as greater improvement in body mass index, according to a study presented at this year’s annual clinical congress of the American College of Surgeons.
Baseline and 1-year postoperative data were collected on 1,398 consecutive bariatric surgery patients by Christopher S. Crowe and his colleagues at Stanford (Calif.) University. The investigators sought to evaluate each type of surgery’s effect on biochemical cardiovascular risk factors. The follow-up rate at 12 months was 77%.
The values measured were hemoglobin A1c, fasting insulin, high-density lipoprotein (HDL), low-density lipoprotein (LDL), total cholesterol, triglycerides, high-sensitivity C-reactive protein (CRP), homocysteine, and lipoprotein (a).
Across the three groups, bypass patients tended to be younger by 1-2 years (mean age of this group was 44.3 years), and they had a higher baseline body mass index on average.
Excess weight loss after 1 year averaged 75% in the bypass patients, 55% in the patients with a sleeve, and 40% in those with a band.
When analyzing laboratory values for each group, the investigators found that fasting insulin levels were notably improved in all three groups; but at an improvement rate of 67.0%, the bypass patients had more than double the improvement of the gastric-band patients, while the gastric-sleeve patients showed a 63.7% improvement rate.
The CRP levels also improved dramatically in the bypass patients (67.1%), especially when compared with the band (21.2%) and sleeve (26.3%) groups. In addition, the ratio between triglycerides and HDL, a strong predictor of cardiovascular events, was differentially most improved in the bypass patients (38.5%), although improvement was also seen in both band (20.6%) and sleeve (35.2%) groups.
The investigators also sought to correlate each bariatric procedure’s resultant weight loss to improvement in specific cardiac risk factors. Only bypass was found to have a correlate between weight loss and total cholesterol and LDL reduction.
The triglyceride/HDL ratio improved with weight loss in both the bypass and band surgical groups. However, patients over age 50 and with a BMI greater than 50 kg/m2 had the least improvement in this ratio.
Reduction in CRP level was not found to be related to weight loss for any of the procedures, although CRP did improve substantially after all three operations, primarily in bypass patients. In response to a question from an audience member, Mr. Crowe, a medical student, said this was probably because of changes in patient lifestyle, diet, and medications, as well as smoking cessation, postoperatively.
"When someone comes in for a bariatric procedure, they’re not just receiving the surgery, they are changing a lot about their life," said Mr. Crowe. "Those changes could, in effect, decrease the CRP levels after surgery, without it being weight loss–dependent."
Mr. Crowe reported no relevant disclosures. His coinvestigators reported serving as consultants to Ethicon and Covidien.
WASHINGTON – One year out from surgery, gastric bypass, gastric sleeve, and gastric banding all showed considerable reductions in cardiac risk factors, but gastric bypass showed the greatest risk reduction of all three, as well as greater improvement in body mass index, according to a study presented at this year’s annual clinical congress of the American College of Surgeons.
Baseline and 1-year postoperative data were collected on 1,398 consecutive bariatric surgery patients by Christopher S. Crowe and his colleagues at Stanford (Calif.) University. The investigators sought to evaluate each type of surgery’s effect on biochemical cardiovascular risk factors. The follow-up rate at 12 months was 77%.
The values measured were hemoglobin A1c, fasting insulin, high-density lipoprotein (HDL), low-density lipoprotein (LDL), total cholesterol, triglycerides, high-sensitivity C-reactive protein (CRP), homocysteine, and lipoprotein (a).
Across the three groups, bypass patients tended to be younger by 1-2 years (mean age of this group was 44.3 years), and they had a higher baseline body mass index on average.
Excess weight loss after 1 year averaged 75% in the bypass patients, 55% in the patients with a sleeve, and 40% in those with a band.
When analyzing laboratory values for each group, the investigators found that fasting insulin levels were notably improved in all three groups; but at an improvement rate of 67.0%, the bypass patients had more than double the improvement of the gastric-band patients, while the gastric-sleeve patients showed a 63.7% improvement rate.
The CRP levels also improved dramatically in the bypass patients (67.1%), especially when compared with the band (21.2%) and sleeve (26.3%) groups. In addition, the ratio between triglycerides and HDL, a strong predictor of cardiovascular events, was differentially most improved in the bypass patients (38.5%), although improvement was also seen in both band (20.6%) and sleeve (35.2%) groups.
The investigators also sought to correlate each bariatric procedure’s resultant weight loss to improvement in specific cardiac risk factors. Only bypass was found to have a correlate between weight loss and total cholesterol and LDL reduction.
The triglyceride/HDL ratio improved with weight loss in both the bypass and band surgical groups. However, patients over age 50 and with a BMI greater than 50 kg/m2 had the least improvement in this ratio.
Reduction in CRP level was not found to be related to weight loss for any of the procedures, although CRP did improve substantially after all three operations, primarily in bypass patients. In response to a question from an audience member, Mr. Crowe, a medical student, said this was probably because of changes in patient lifestyle, diet, and medications, as well as smoking cessation, postoperatively.
"When someone comes in for a bariatric procedure, they’re not just receiving the surgery, they are changing a lot about their life," said Mr. Crowe. "Those changes could, in effect, decrease the CRP levels after surgery, without it being weight loss–dependent."
Mr. Crowe reported no relevant disclosures. His coinvestigators reported serving as consultants to Ethicon and Covidien.
AT THE ACS CLINICAL CONGRESS
Major finding: Gastric bypass showed greater improvement in all cardiovascular risk factors 1 year postoperatively.
Data source: Prospective analysis of 1,398 consecutive bariatric procedures (gastric bypass, sleeve gastrectomy, gastric banding) at baseline and 1 year postoperatively.
Disclosures: Mr. Crowe reported no relevant disclosures. His coinvestigators reported serving as consultants to Ethicon and Covidien.