User login
Thrombosis precautions in IBD not met in two-thirds of high-risk cases
HOLLYWOOD, FLA. – The relative risk of thromboembolic events is greater in inpatient inflammatory bowel disease patients than in the general population, but prophylactic treatment is still not standard, according to a speaker at a conference on inflammatory bowel diseases.
"It’s a relatively rare problem, only about 1 to 1.5 percent," said Dr. Athos Bousvaros, of Boston Children’s Hospital. "So, why worry about it so much? Because it really is a major source of morbidity in the IBD population. It usually happens in the sick patients, the ones at risk for strokes; and it usually happens at the worst time, when you’re thinking about colectomy."
However, Dr. Bousvaros said only about a third of IBD patients at risk for a thromboembolic event are given prophylactic treatment in the inpatient setting, especially in severe colitis, and it is generally recommended.
Although pharmacologic prophylaxis is included in the American College of Gastroenterology guidelines, Dr. Bousvaros cited a recent study that found only 35% of gastroenterologists in the United States actually do so (J. Clin. Gastroenterol. 2013;47:e1-e6).
"In the inpatient setting, especially in severe colitis, [prophylaxis] is generally recommended," Dr. Bousvaros said. "It is included in the AGA [American Gastroenterological Association] physician performance measure set." In the outpatient setting, data do not support it, he said.
Relative risk high
While the absolute risk is low, the relative risk of a venous thromboembolic event is six times greater in IBD, particularly in patients aged 20 years or less, said Dr. Bousvaros, citing a cohort study that used Danish administrative data (Gut 2011;60:937-43). "It’s mainly patients with flares, and mainly those with colitis, either Crohn’s or severe ulcerative colitis," Dr. Bousvaros said.
In a prospective study of about 2,800 IBD patients (mean age, 42 years) recruited over 2.5 years, matched with non-IBD controls, and followed for several years, about 4% developed de novo venous thromboembolism (Gastroenterol. 2010;139:779-787.e1). Dr. Bousvaros emphasized that IBD was an independent risk factor for VTE recurrence in the study. "They were typically treated with long-standing prophylaxis. And if any anticoagulation was involved, the risk of recurrence was high," he said at the meeting, which was sponsored by the Crohn’s & Colitis Foundation of America.
High-risk criteria
Overall, the relative risk for VTE was found by a just-published meta-analysis of more than 200,000 IBD patients to be 2.4 for deep vein thrombosis, 2.5 for pulmonary embolism, 1.3 for ischemic heart disease, and 3.4 for mesenteric ischemia (J. Crohns Colitis 2013 Oct 29 [doi: 10.1016/j.crohns.2013.09.021]). Dr. Bousvaros said the investigators did not find an increased risk for arterial thromboembolic events in IBD, but that VTEs "were highly significant in this population."
Patients with IBD should be considered high risk for VTE if they are being treated in hospital for severe colitis and have a personal or family history of thrombosis, have known thrombophilia, have been taking oral contraceptives, have a history of smoking, are obese, or have had a PICC line.
"Any of those makes you a particularly high-risk patient," Dr. Bousvaros said.
Dr. Bousvaros disclosed he has consulting relationships with Cubist, Dyax, and Millennium.
HOLLYWOOD, FLA. – The relative risk of thromboembolic events is greater in inpatient inflammatory bowel disease patients than in the general population, but prophylactic treatment is still not standard, according to a speaker at a conference on inflammatory bowel diseases.
"It’s a relatively rare problem, only about 1 to 1.5 percent," said Dr. Athos Bousvaros, of Boston Children’s Hospital. "So, why worry about it so much? Because it really is a major source of morbidity in the IBD population. It usually happens in the sick patients, the ones at risk for strokes; and it usually happens at the worst time, when you’re thinking about colectomy."
However, Dr. Bousvaros said only about a third of IBD patients at risk for a thromboembolic event are given prophylactic treatment in the inpatient setting, especially in severe colitis, and it is generally recommended.
Although pharmacologic prophylaxis is included in the American College of Gastroenterology guidelines, Dr. Bousvaros cited a recent study that found only 35% of gastroenterologists in the United States actually do so (J. Clin. Gastroenterol. 2013;47:e1-e6).
"In the inpatient setting, especially in severe colitis, [prophylaxis] is generally recommended," Dr. Bousvaros said. "It is included in the AGA [American Gastroenterological Association] physician performance measure set." In the outpatient setting, data do not support it, he said.
Relative risk high
While the absolute risk is low, the relative risk of a venous thromboembolic event is six times greater in IBD, particularly in patients aged 20 years or less, said Dr. Bousvaros, citing a cohort study that used Danish administrative data (Gut 2011;60:937-43). "It’s mainly patients with flares, and mainly those with colitis, either Crohn’s or severe ulcerative colitis," Dr. Bousvaros said.
In a prospective study of about 2,800 IBD patients (mean age, 42 years) recruited over 2.5 years, matched with non-IBD controls, and followed for several years, about 4% developed de novo venous thromboembolism (Gastroenterol. 2010;139:779-787.e1). Dr. Bousvaros emphasized that IBD was an independent risk factor for VTE recurrence in the study. "They were typically treated with long-standing prophylaxis. And if any anticoagulation was involved, the risk of recurrence was high," he said at the meeting, which was sponsored by the Crohn’s & Colitis Foundation of America.
High-risk criteria
Overall, the relative risk for VTE was found by a just-published meta-analysis of more than 200,000 IBD patients to be 2.4 for deep vein thrombosis, 2.5 for pulmonary embolism, 1.3 for ischemic heart disease, and 3.4 for mesenteric ischemia (J. Crohns Colitis 2013 Oct 29 [doi: 10.1016/j.crohns.2013.09.021]). Dr. Bousvaros said the investigators did not find an increased risk for arterial thromboembolic events in IBD, but that VTEs "were highly significant in this population."
Patients with IBD should be considered high risk for VTE if they are being treated in hospital for severe colitis and have a personal or family history of thrombosis, have known thrombophilia, have been taking oral contraceptives, have a history of smoking, are obese, or have had a PICC line.
"Any of those makes you a particularly high-risk patient," Dr. Bousvaros said.
Dr. Bousvaros disclosed he has consulting relationships with Cubist, Dyax, and Millennium.
HOLLYWOOD, FLA. – The relative risk of thromboembolic events is greater in inpatient inflammatory bowel disease patients than in the general population, but prophylactic treatment is still not standard, according to a speaker at a conference on inflammatory bowel diseases.
"It’s a relatively rare problem, only about 1 to 1.5 percent," said Dr. Athos Bousvaros, of Boston Children’s Hospital. "So, why worry about it so much? Because it really is a major source of morbidity in the IBD population. It usually happens in the sick patients, the ones at risk for strokes; and it usually happens at the worst time, when you’re thinking about colectomy."
However, Dr. Bousvaros said only about a third of IBD patients at risk for a thromboembolic event are given prophylactic treatment in the inpatient setting, especially in severe colitis, and it is generally recommended.
Although pharmacologic prophylaxis is included in the American College of Gastroenterology guidelines, Dr. Bousvaros cited a recent study that found only 35% of gastroenterologists in the United States actually do so (J. Clin. Gastroenterol. 2013;47:e1-e6).
"In the inpatient setting, especially in severe colitis, [prophylaxis] is generally recommended," Dr. Bousvaros said. "It is included in the AGA [American Gastroenterological Association] physician performance measure set." In the outpatient setting, data do not support it, he said.
Relative risk high
While the absolute risk is low, the relative risk of a venous thromboembolic event is six times greater in IBD, particularly in patients aged 20 years or less, said Dr. Bousvaros, citing a cohort study that used Danish administrative data (Gut 2011;60:937-43). "It’s mainly patients with flares, and mainly those with colitis, either Crohn’s or severe ulcerative colitis," Dr. Bousvaros said.
In a prospective study of about 2,800 IBD patients (mean age, 42 years) recruited over 2.5 years, matched with non-IBD controls, and followed for several years, about 4% developed de novo venous thromboembolism (Gastroenterol. 2010;139:779-787.e1). Dr. Bousvaros emphasized that IBD was an independent risk factor for VTE recurrence in the study. "They were typically treated with long-standing prophylaxis. And if any anticoagulation was involved, the risk of recurrence was high," he said at the meeting, which was sponsored by the Crohn’s & Colitis Foundation of America.
High-risk criteria
Overall, the relative risk for VTE was found by a just-published meta-analysis of more than 200,000 IBD patients to be 2.4 for deep vein thrombosis, 2.5 for pulmonary embolism, 1.3 for ischemic heart disease, and 3.4 for mesenteric ischemia (J. Crohns Colitis 2013 Oct 29 [doi: 10.1016/j.crohns.2013.09.021]). Dr. Bousvaros said the investigators did not find an increased risk for arterial thromboembolic events in IBD, but that VTEs "were highly significant in this population."
Patients with IBD should be considered high risk for VTE if they are being treated in hospital for severe colitis and have a personal or family history of thrombosis, have known thrombophilia, have been taking oral contraceptives, have a history of smoking, are obese, or have had a PICC line.
"Any of those makes you a particularly high-risk patient," Dr. Bousvaros said.
Dr. Bousvaros disclosed he has consulting relationships with Cubist, Dyax, and Millennium.
EXPERT ANALYSIS FROM 2013 ADVANCES IN IBD
Psychoeducation, compliance contracts curb postsurgery alcohol abuse
ATLANTA – Pre–bariatric surgery psychoeducation and compliance contracts are two ways to help lower the risk of patient alcohol abuse after surgery.
"Surgery itself changes a patient’s susceptibility to alcohol," said Leslie Heinberg, Ph.D., director of behavioral services for the Bariatric and Metabolic Institute at Cleveland Clinic. "There’s going to be increased sensitivity to alcohol and decreased tolerance," Dr. Heinberg said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Programs that screen and triage bariatric surgery candidates, as well as inform them of how alcohol will affect them post surgery, can help manage their risk, according to Dr. Heinberg.
"I tell patients: ‘You’re going to get drunk very easily, very quickly, and it’s going to last a very long time.’ "
Dr. Heinberg cited a case cross-over trial that showed how at 6 months post gastric bypass surgery, patients had higher postoperative peak blood alcohol content levels after drinking one 5-ounce glass of red wine, and took longer to recover than they did before surgery.
"Patients that have one glass of red wine before surgery, they’re about at .02 [blood alcohol content], and they’re legally fine," she said. "Six months after surgery, they’re legally drunk." (J. Am. Coll. Surg. 2011;212:209-14).
The physical experience of drinking alcohol changes post surgery, too. "Postop, people are more likely to report that they feel dizzy and lightheaded and have double vision," said Dr. Heinberg, also professor of medicine in the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
‘Addiction transfer’
Reasons for the increased susceptibility in this patient population include the change in ratio between body weight and alcohol concentration, as well as the physiologic change inherent to gastric bypass where a pouch is placed in the jejunum. "There is a bolus of alcohol that hits and hits very quickly," said Dr. Heinberg.
Another reason is that in weight-loss surgery, one of the body’s primary sources of antialcohol dehydrogenase, the stomach, has been reduced in volume, she said.
Dr. Heinberg also said new data suggest "addiction transfer," thought to be the result of the body’s shared neural pathways for compulsive eating and substance abuse, might lead to either relapse in patients with histories of alcohol abuse or new-onset alcoholism in those who may not have abused alcohol, but who were compulsive eaters (Arch. Gen. Psychiatry. 2011;68:808-16).
Risk predictors
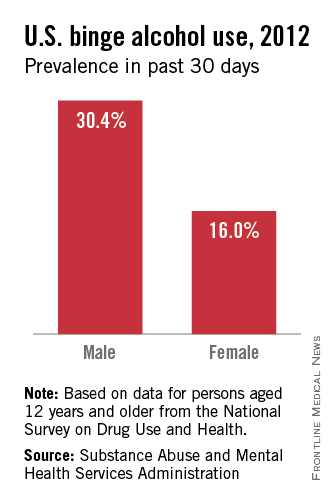
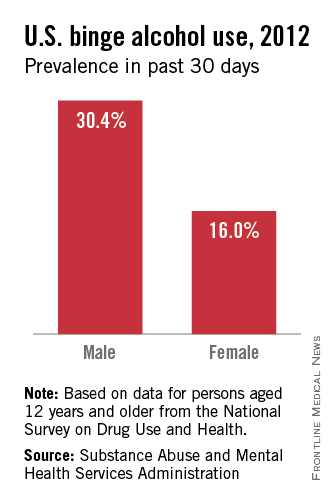
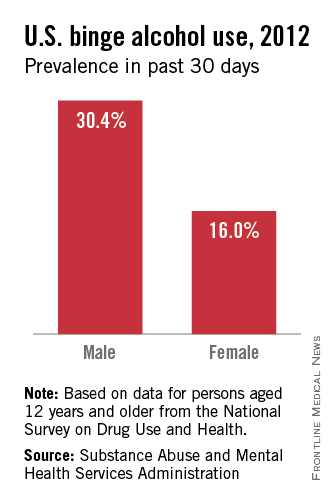
Dr. Heinberg cited a longitudinal study showing that predictors of risk included being male; presurgery use of tobacco, alcohol, and recreational drugs; having weak social support networks; and having gastric bypass surgery rather than other surgical weight loss procedures (JAMA 2012;307:2516-25).
The "good news," said Dr. Heinberg, is that contrary to her own hypothesis, a study of 400 patients with a history of substance abuse, controlled for presurgical body mass index, surgery type, gender, and race showed that people with a history of substance abuse had lost more weight 2 years after surgery (Surg. Obes. Relat. Dis. 2012 8:357-63).
"I think people who achieve abstinence have figured out how to completely change their lifestyle," said Dr. Heinberg. "Maybe those skills that helped them quit drinking are helping them post surgery."
Improved compliance
In an online questionnaire, 84% of 318 bariatric surgery patients surveyed admitted they continued to drink after their surgery, said Dr. Heinberg. "I think it’s important to screen each and every patient for all kinds of alcohol problems."
To help ensure compliance, she suggested clinics use free screening tools and guidelines available from the National Institute on Alcohol Abuse and Alcoholism. She described various levels of psychoeducation in use at her clinic, depending upon how severe the risk per the screening.
Participants deemed by her clinic to be at greater risk are given substance risk reduction education, which includes pre- and posttests. This helps avoid patients’ claims that they were unaware of the risks of alcohol after the surgery, said Dr. Heinberg. "We just pull out the test and say, ‘You got a 100%."
In some cases, she suggested that asking a patient who is a compliance risk concern to sign a contract agreeing not to drink after the surgery might help "get around risk management."
Dr. Heinberg concluded that this is a "vulnerable" patient population that may not be aware of the risks posed by alcohol post surgery. "Most programs need to think about putting this in their informed consent and providing more psychoeducation prior to surgery, sometimes even behavioral contracts," she said.
ATLANTA – Pre–bariatric surgery psychoeducation and compliance contracts are two ways to help lower the risk of patient alcohol abuse after surgery.
"Surgery itself changes a patient’s susceptibility to alcohol," said Leslie Heinberg, Ph.D., director of behavioral services for the Bariatric and Metabolic Institute at Cleveland Clinic. "There’s going to be increased sensitivity to alcohol and decreased tolerance," Dr. Heinberg said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Programs that screen and triage bariatric surgery candidates, as well as inform them of how alcohol will affect them post surgery, can help manage their risk, according to Dr. Heinberg.
"I tell patients: ‘You’re going to get drunk very easily, very quickly, and it’s going to last a very long time.’ "
Dr. Heinberg cited a case cross-over trial that showed how at 6 months post gastric bypass surgery, patients had higher postoperative peak blood alcohol content levels after drinking one 5-ounce glass of red wine, and took longer to recover than they did before surgery.
"Patients that have one glass of red wine before surgery, they’re about at .02 [blood alcohol content], and they’re legally fine," she said. "Six months after surgery, they’re legally drunk." (J. Am. Coll. Surg. 2011;212:209-14).
The physical experience of drinking alcohol changes post surgery, too. "Postop, people are more likely to report that they feel dizzy and lightheaded and have double vision," said Dr. Heinberg, also professor of medicine in the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
‘Addiction transfer’
Reasons for the increased susceptibility in this patient population include the change in ratio between body weight and alcohol concentration, as well as the physiologic change inherent to gastric bypass where a pouch is placed in the jejunum. "There is a bolus of alcohol that hits and hits very quickly," said Dr. Heinberg.
Another reason is that in weight-loss surgery, one of the body’s primary sources of antialcohol dehydrogenase, the stomach, has been reduced in volume, she said.
Dr. Heinberg also said new data suggest "addiction transfer," thought to be the result of the body’s shared neural pathways for compulsive eating and substance abuse, might lead to either relapse in patients with histories of alcohol abuse or new-onset alcoholism in those who may not have abused alcohol, but who were compulsive eaters (Arch. Gen. Psychiatry. 2011;68:808-16).
Risk predictors
Dr. Heinberg cited a longitudinal study showing that predictors of risk included being male; presurgery use of tobacco, alcohol, and recreational drugs; having weak social support networks; and having gastric bypass surgery rather than other surgical weight loss procedures (JAMA 2012;307:2516-25).
The "good news," said Dr. Heinberg, is that contrary to her own hypothesis, a study of 400 patients with a history of substance abuse, controlled for presurgical body mass index, surgery type, gender, and race showed that people with a history of substance abuse had lost more weight 2 years after surgery (Surg. Obes. Relat. Dis. 2012 8:357-63).
"I think people who achieve abstinence have figured out how to completely change their lifestyle," said Dr. Heinberg. "Maybe those skills that helped them quit drinking are helping them post surgery."
Improved compliance
In an online questionnaire, 84% of 318 bariatric surgery patients surveyed admitted they continued to drink after their surgery, said Dr. Heinberg. "I think it’s important to screen each and every patient for all kinds of alcohol problems."
To help ensure compliance, she suggested clinics use free screening tools and guidelines available from the National Institute on Alcohol Abuse and Alcoholism. She described various levels of psychoeducation in use at her clinic, depending upon how severe the risk per the screening.
Participants deemed by her clinic to be at greater risk are given substance risk reduction education, which includes pre- and posttests. This helps avoid patients’ claims that they were unaware of the risks of alcohol after the surgery, said Dr. Heinberg. "We just pull out the test and say, ‘You got a 100%."
In some cases, she suggested that asking a patient who is a compliance risk concern to sign a contract agreeing not to drink after the surgery might help "get around risk management."
Dr. Heinberg concluded that this is a "vulnerable" patient population that may not be aware of the risks posed by alcohol post surgery. "Most programs need to think about putting this in their informed consent and providing more psychoeducation prior to surgery, sometimes even behavioral contracts," she said.
ATLANTA – Pre–bariatric surgery psychoeducation and compliance contracts are two ways to help lower the risk of patient alcohol abuse after surgery.
"Surgery itself changes a patient’s susceptibility to alcohol," said Leslie Heinberg, Ph.D., director of behavioral services for the Bariatric and Metabolic Institute at Cleveland Clinic. "There’s going to be increased sensitivity to alcohol and decreased tolerance," Dr. Heinberg said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Programs that screen and triage bariatric surgery candidates, as well as inform them of how alcohol will affect them post surgery, can help manage their risk, according to Dr. Heinberg.
"I tell patients: ‘You’re going to get drunk very easily, very quickly, and it’s going to last a very long time.’ "
Dr. Heinberg cited a case cross-over trial that showed how at 6 months post gastric bypass surgery, patients had higher postoperative peak blood alcohol content levels after drinking one 5-ounce glass of red wine, and took longer to recover than they did before surgery.
"Patients that have one glass of red wine before surgery, they’re about at .02 [blood alcohol content], and they’re legally fine," she said. "Six months after surgery, they’re legally drunk." (J. Am. Coll. Surg. 2011;212:209-14).
The physical experience of drinking alcohol changes post surgery, too. "Postop, people are more likely to report that they feel dizzy and lightheaded and have double vision," said Dr. Heinberg, also professor of medicine in the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
‘Addiction transfer’
Reasons for the increased susceptibility in this patient population include the change in ratio between body weight and alcohol concentration, as well as the physiologic change inherent to gastric bypass where a pouch is placed in the jejunum. "There is a bolus of alcohol that hits and hits very quickly," said Dr. Heinberg.
Another reason is that in weight-loss surgery, one of the body’s primary sources of antialcohol dehydrogenase, the stomach, has been reduced in volume, she said.
Dr. Heinberg also said new data suggest "addiction transfer," thought to be the result of the body’s shared neural pathways for compulsive eating and substance abuse, might lead to either relapse in patients with histories of alcohol abuse or new-onset alcoholism in those who may not have abused alcohol, but who were compulsive eaters (Arch. Gen. Psychiatry. 2011;68:808-16).
Risk predictors
Dr. Heinberg cited a longitudinal study showing that predictors of risk included being male; presurgery use of tobacco, alcohol, and recreational drugs; having weak social support networks; and having gastric bypass surgery rather than other surgical weight loss procedures (JAMA 2012;307:2516-25).
The "good news," said Dr. Heinberg, is that contrary to her own hypothesis, a study of 400 patients with a history of substance abuse, controlled for presurgical body mass index, surgery type, gender, and race showed that people with a history of substance abuse had lost more weight 2 years after surgery (Surg. Obes. Relat. Dis. 2012 8:357-63).
"I think people who achieve abstinence have figured out how to completely change their lifestyle," said Dr. Heinberg. "Maybe those skills that helped them quit drinking are helping them post surgery."
Improved compliance
In an online questionnaire, 84% of 318 bariatric surgery patients surveyed admitted they continued to drink after their surgery, said Dr. Heinberg. "I think it’s important to screen each and every patient for all kinds of alcohol problems."
To help ensure compliance, she suggested clinics use free screening tools and guidelines available from the National Institute on Alcohol Abuse and Alcoholism. She described various levels of psychoeducation in use at her clinic, depending upon how severe the risk per the screening.
Participants deemed by her clinic to be at greater risk are given substance risk reduction education, which includes pre- and posttests. This helps avoid patients’ claims that they were unaware of the risks of alcohol after the surgery, said Dr. Heinberg. "We just pull out the test and say, ‘You got a 100%."
In some cases, she suggested that asking a patient who is a compliance risk concern to sign a contract agreeing not to drink after the surgery might help "get around risk management."
Dr. Heinberg concluded that this is a "vulnerable" patient population that may not be aware of the risks posed by alcohol post surgery. "Most programs need to think about putting this in their informed consent and providing more psychoeducation prior to surgery, sometimes even behavioral contracts," she said.
EXPERT ANALYSIS FROM OBESITY WEEK
VTE rate not an accurate measure of hospital quality
Postoperative venous thromboembolism rates may not be an effective way of measuring hospital quality, according to Dr. Karl Y. Bilimoria and his colleagues.
The investigators calculated patient-level rates of venous thromboembolism as well as rates of imaging for VTE using data from the American Hospital Association and Medicare Compare from 2009 to 2010 from nearly 1 million patients discharged from 2,786 hospitals after a major surgery.
They sought to determine the association between hospital adherence to VTE reduction protocols (Surgical Care Improvement Project for VTE or SCIP-VTE-2) and risk-adjusted rates of VTE as measured by Patient Safety Indicator 12 (PSI-12) from the Agency for Healthcare Research and Quality. They also looked at how overall hospital quality scores correlated with VTE prophylaxis and risk-adjusted VTE scores.
They presented their findigns at the annual clinical congress of the American College of Surgeons and in JAMA [doi:10.1001/jama.2013.280048]).
Hospitals that adhered consistently to VTE reduction protocols paradoxically had higher PSI-12 scores, although not significantly so (P = .03). Hospitals with higher overall quality scores also adhered to VTE reduction protocols at a higher rate (93.3% in the lowest quartile vs. 95.5% in the highest) and had significantly higher risk-adjusted VTE event scores (P less than .001).
"Most important, hospital VTE rates were associated with the intensity of detecting VTE with imaging studies," the investigators said. Mean VTE diagnostic imaging rates ranged from 32/1,000 in the lowest quartile to 167/1,000 in the highest. Hospitals with the lowest imaging rates diagnosed 5.0 VTEs per 1,000 discharges, compared with hospitals with the highest imaging rates diagnosing 13.5 VTEs per 1,000 discharges.
In effect, PSI-12 scores the use of VTE imaging by hospitals instead of the quality of care provided, the investigators said. Further, surveillance bias impedes quality performance improvements; thus, decision making becomes more difficult for "patients seeking to identify a high-quality hospital."
In an accompanying editorial, Dr. Edwin H. Livingston, deputy editor of JAMA, noted that hypervigilance of VTEs might further worsen care in that "the very high compliance rate with VTE prophylaxis might result from many patients receiving treatments from which they are not likely to benefit. This is because current process measures were based on older guidelines that overestimated the benefits of VTE prophylaxis" (JAMA [doi:10.1001/jama.2013.280049]).
For that reason, Dr. Livingston recommended that public reporting of VTEs be "reconsidered or curtailed because few hospitals have sufficient numbers of patients to show statistically significant effects of prophylactic measures on VTE rates."
Measuring outcomes in general and safety events in particular is a complex proposition. This is particularly true when using patient safety indicators (PSIs) and hospital-acquired conditions as outcome metrics to compare performance across organizations.
In addition to the usual challenging nuances such as severity of illness adjustment, these indicators rely on accurate documentation and coding and as the Agency for Healthcare Research and Quality states: PSIs identify "potential in-hospital complications and adverse events following surgeries, procedures, and childbirth."
This is well meaning when an analytic team uses these metrics as part of a comprehensive quality and patient safety program to identify potential internal improvement opportunities. However, there are real limitations when using these metrics as outcomes that are tied to public reporting initiatives, payment incentives, and rankings.
The study in JAMA by Dr. Bilimoria and his colleagues highlights another limitation of some of these metrics – that of surveillance bias. Using PSI-12 (postoperative venous thromboembolism), risk-adjusted VTE rates were shown to correlate positively with intensity of imaging use (surveillance) and inversely with other measures of quality such as structure or process.
Thus, those with the highest VTE rates did everything right, but also looked for events more often.
This finding complicates the use of PSI-12 as an indicator to compare outcomes across health care systems. However, when used as an internal driver in the context of other local metrics of quality and safety, the original intent of PSI-12 as an indicator of potential hospital complications does not change.
This highlights the importance of health care systems in understanding the strengths and limitations of quality and safety metrics and in developing the analytic capabilities to turn data points into real opportunities to deliver better care, rather than going down the proverbial rabbit hole. Yet, regulatory agencies should also recognize that using imperfect metrics as a part of payment-reform initiatives needs to be done with extreme caution or there will be unintended consequences that do not lead to our collective goal of exceptional value in health care for our patients.
Dr. Robert Pendleton is chief medical quality officer for University of Utah Health Care, Salt Lake City.
Measuring outcomes in general and safety events in particular is a complex proposition. This is particularly true when using patient safety indicators (PSIs) and hospital-acquired conditions as outcome metrics to compare performance across organizations.
In addition to the usual challenging nuances such as severity of illness adjustment, these indicators rely on accurate documentation and coding and as the Agency for Healthcare Research and Quality states: PSIs identify "potential in-hospital complications and adverse events following surgeries, procedures, and childbirth."
This is well meaning when an analytic team uses these metrics as part of a comprehensive quality and patient safety program to identify potential internal improvement opportunities. However, there are real limitations when using these metrics as outcomes that are tied to public reporting initiatives, payment incentives, and rankings.
The study in JAMA by Dr. Bilimoria and his colleagues highlights another limitation of some of these metrics – that of surveillance bias. Using PSI-12 (postoperative venous thromboembolism), risk-adjusted VTE rates were shown to correlate positively with intensity of imaging use (surveillance) and inversely with other measures of quality such as structure or process.
Thus, those with the highest VTE rates did everything right, but also looked for events more often.
This finding complicates the use of PSI-12 as an indicator to compare outcomes across health care systems. However, when used as an internal driver in the context of other local metrics of quality and safety, the original intent of PSI-12 as an indicator of potential hospital complications does not change.
This highlights the importance of health care systems in understanding the strengths and limitations of quality and safety metrics and in developing the analytic capabilities to turn data points into real opportunities to deliver better care, rather than going down the proverbial rabbit hole. Yet, regulatory agencies should also recognize that using imperfect metrics as a part of payment-reform initiatives needs to be done with extreme caution or there will be unintended consequences that do not lead to our collective goal of exceptional value in health care for our patients.
Dr. Robert Pendleton is chief medical quality officer for University of Utah Health Care, Salt Lake City.
Measuring outcomes in general and safety events in particular is a complex proposition. This is particularly true when using patient safety indicators (PSIs) and hospital-acquired conditions as outcome metrics to compare performance across organizations.
In addition to the usual challenging nuances such as severity of illness adjustment, these indicators rely on accurate documentation and coding and as the Agency for Healthcare Research and Quality states: PSIs identify "potential in-hospital complications and adverse events following surgeries, procedures, and childbirth."
This is well meaning when an analytic team uses these metrics as part of a comprehensive quality and patient safety program to identify potential internal improvement opportunities. However, there are real limitations when using these metrics as outcomes that are tied to public reporting initiatives, payment incentives, and rankings.
The study in JAMA by Dr. Bilimoria and his colleagues highlights another limitation of some of these metrics – that of surveillance bias. Using PSI-12 (postoperative venous thromboembolism), risk-adjusted VTE rates were shown to correlate positively with intensity of imaging use (surveillance) and inversely with other measures of quality such as structure or process.
Thus, those with the highest VTE rates did everything right, but also looked for events more often.
This finding complicates the use of PSI-12 as an indicator to compare outcomes across health care systems. However, when used as an internal driver in the context of other local metrics of quality and safety, the original intent of PSI-12 as an indicator of potential hospital complications does not change.
This highlights the importance of health care systems in understanding the strengths and limitations of quality and safety metrics and in developing the analytic capabilities to turn data points into real opportunities to deliver better care, rather than going down the proverbial rabbit hole. Yet, regulatory agencies should also recognize that using imperfect metrics as a part of payment-reform initiatives needs to be done with extreme caution or there will be unintended consequences that do not lead to our collective goal of exceptional value in health care for our patients.
Dr. Robert Pendleton is chief medical quality officer for University of Utah Health Care, Salt Lake City.
Postoperative venous thromboembolism rates may not be an effective way of measuring hospital quality, according to Dr. Karl Y. Bilimoria and his colleagues.
The investigators calculated patient-level rates of venous thromboembolism as well as rates of imaging for VTE using data from the American Hospital Association and Medicare Compare from 2009 to 2010 from nearly 1 million patients discharged from 2,786 hospitals after a major surgery.
They sought to determine the association between hospital adherence to VTE reduction protocols (Surgical Care Improvement Project for VTE or SCIP-VTE-2) and risk-adjusted rates of VTE as measured by Patient Safety Indicator 12 (PSI-12) from the Agency for Healthcare Research and Quality. They also looked at how overall hospital quality scores correlated with VTE prophylaxis and risk-adjusted VTE scores.
They presented their findigns at the annual clinical congress of the American College of Surgeons and in JAMA [doi:10.1001/jama.2013.280048]).
Hospitals that adhered consistently to VTE reduction protocols paradoxically had higher PSI-12 scores, although not significantly so (P = .03). Hospitals with higher overall quality scores also adhered to VTE reduction protocols at a higher rate (93.3% in the lowest quartile vs. 95.5% in the highest) and had significantly higher risk-adjusted VTE event scores (P less than .001).
"Most important, hospital VTE rates were associated with the intensity of detecting VTE with imaging studies," the investigators said. Mean VTE diagnostic imaging rates ranged from 32/1,000 in the lowest quartile to 167/1,000 in the highest. Hospitals with the lowest imaging rates diagnosed 5.0 VTEs per 1,000 discharges, compared with hospitals with the highest imaging rates diagnosing 13.5 VTEs per 1,000 discharges.
In effect, PSI-12 scores the use of VTE imaging by hospitals instead of the quality of care provided, the investigators said. Further, surveillance bias impedes quality performance improvements; thus, decision making becomes more difficult for "patients seeking to identify a high-quality hospital."
In an accompanying editorial, Dr. Edwin H. Livingston, deputy editor of JAMA, noted that hypervigilance of VTEs might further worsen care in that "the very high compliance rate with VTE prophylaxis might result from many patients receiving treatments from which they are not likely to benefit. This is because current process measures were based on older guidelines that overestimated the benefits of VTE prophylaxis" (JAMA [doi:10.1001/jama.2013.280049]).
For that reason, Dr. Livingston recommended that public reporting of VTEs be "reconsidered or curtailed because few hospitals have sufficient numbers of patients to show statistically significant effects of prophylactic measures on VTE rates."
Postoperative venous thromboembolism rates may not be an effective way of measuring hospital quality, according to Dr. Karl Y. Bilimoria and his colleagues.
The investigators calculated patient-level rates of venous thromboembolism as well as rates of imaging for VTE using data from the American Hospital Association and Medicare Compare from 2009 to 2010 from nearly 1 million patients discharged from 2,786 hospitals after a major surgery.
They sought to determine the association between hospital adherence to VTE reduction protocols (Surgical Care Improvement Project for VTE or SCIP-VTE-2) and risk-adjusted rates of VTE as measured by Patient Safety Indicator 12 (PSI-12) from the Agency for Healthcare Research and Quality. They also looked at how overall hospital quality scores correlated with VTE prophylaxis and risk-adjusted VTE scores.
They presented their findigns at the annual clinical congress of the American College of Surgeons and in JAMA [doi:10.1001/jama.2013.280048]).
Hospitals that adhered consistently to VTE reduction protocols paradoxically had higher PSI-12 scores, although not significantly so (P = .03). Hospitals with higher overall quality scores also adhered to VTE reduction protocols at a higher rate (93.3% in the lowest quartile vs. 95.5% in the highest) and had significantly higher risk-adjusted VTE event scores (P less than .001).
"Most important, hospital VTE rates were associated with the intensity of detecting VTE with imaging studies," the investigators said. Mean VTE diagnostic imaging rates ranged from 32/1,000 in the lowest quartile to 167/1,000 in the highest. Hospitals with the lowest imaging rates diagnosed 5.0 VTEs per 1,000 discharges, compared with hospitals with the highest imaging rates diagnosing 13.5 VTEs per 1,000 discharges.
In effect, PSI-12 scores the use of VTE imaging by hospitals instead of the quality of care provided, the investigators said. Further, surveillance bias impedes quality performance improvements; thus, decision making becomes more difficult for "patients seeking to identify a high-quality hospital."
In an accompanying editorial, Dr. Edwin H. Livingston, deputy editor of JAMA, noted that hypervigilance of VTEs might further worsen care in that "the very high compliance rate with VTE prophylaxis might result from many patients receiving treatments from which they are not likely to benefit. This is because current process measures were based on older guidelines that overestimated the benefits of VTE prophylaxis" (JAMA [doi:10.1001/jama.2013.280049]).
For that reason, Dr. Livingston recommended that public reporting of VTEs be "reconsidered or curtailed because few hospitals have sufficient numbers of patients to show statistically significant effects of prophylactic measures on VTE rates."
Major finding: Hospitals that adhered consistently to VTE reduction protocols had higher rates of VTE, although not significantly so (P = .03).
Data source: Study of hospital risk-adjusted VTE prophylaxis adherence rates to postoperative VTE event rates in 2,786 hospitals.
Disclosures: The study was funded by the AHRQ and Northwestern University. Dr. Bilimoria has received honoraria from hospitals, professional societies, and continuing medical education companies for presentation on quality improvement.
Diet drinks’ link to cardiometabolic disease elusive
ATLANTA – Diet drinks might be protective rather than causative in cardiometabolic diseases such as obesity and type 2 diabetes, but definitive data are lacking.
"I would say that based on the scientific evidence to date, it might be a good idea to switch to artificially sweetened beverages, but I don’t see the evidence to either promote or avoid them," said Mark Pereira, Ph.D., of the School of Public Health at the University of Minnesota, Minneapolis.
There are data linking sugar-sweetened beverages to metabolic disorders. Findings from a recent, small, but "pretty provocative" randomized pilot study point to a relationship between sugar-sweetened beverages’ strong effect on visceral fat, particularly in the intra-abdominal cavity, he said. Diet drinks were not found in the study to have a positive association with this kind of adiposity (Am. J. Clin. Nutr. 2012;95:283-9).
The significance of this is that visceral adipose tissue in the gut "is consistent with a higher cardiometabolic risk profile," he said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The study supports findings from the National Heart, Blood, and Lung Institute’s prospective Coronary Artery Risk Development in Young Adults (CARDIA) study of 3,000 individuals. Imaging done across the cohort at year 25 of the study showed a weak association between artificially sweetened beverages and the volume of fat in the visceral cavity, but a "really, really strong" association with sugar-sweetened beverages and visceral cavity adipose tissue, said Dr. Pereira.
"If you look at the true drivers of metabolic risk, the visceral fat, it’s not there with the artificially sweetened drinks, it’s only there with the sugar-sweetened ones," he said.
Although both diet and sugar-sweetened drinks have positive associations with incident diabetes and other metabolic disturbances, the relationship between "diet drinks and cardiometabolic risk may be an anomaly of reverse causality," Dr. Pereira said.
While findings from the CARDIA study show an association between waist circumference and consumption of diet drinks, there was not an association with blood sugar, lipids, or blood pressure. "So, the question is, ‘Why isn’t [diet drink consumption] driving the risk factors?" asked Dr. Pereira.
The reason may be that consumers of high amounts of diet drinks "are more likely to be overweight and obese, and are more likely to be at high risk for chronic disease so they choose beverages with low calories to try to lower their risk," he suggested.
However, the extent of reverse causality in this patient population, said Dr. Pereira, is still unknown: "There could be an increased risk [of cardiometabolic disease] with a higher intake of artificially sweetened drinks, but you could also say it is protective."
The lack of certainty, according to Dr. Pereira, is due to a drought of data from well designed studies.
"I argue with some of my colleagues who believe that we can learn just as much or more on this from observational prospective epidemiological studies," he said, adding, "I am kind of steadfast that this is a topic that should be clearly addressed in terms of mechanisms and causality through better randomized controlled trials."
Dr. Pereira reported he has received support from the Robert Wood Johnson Foundation.
ATLANTA – Diet drinks might be protective rather than causative in cardiometabolic diseases such as obesity and type 2 diabetes, but definitive data are lacking.
"I would say that based on the scientific evidence to date, it might be a good idea to switch to artificially sweetened beverages, but I don’t see the evidence to either promote or avoid them," said Mark Pereira, Ph.D., of the School of Public Health at the University of Minnesota, Minneapolis.
There are data linking sugar-sweetened beverages to metabolic disorders. Findings from a recent, small, but "pretty provocative" randomized pilot study point to a relationship between sugar-sweetened beverages’ strong effect on visceral fat, particularly in the intra-abdominal cavity, he said. Diet drinks were not found in the study to have a positive association with this kind of adiposity (Am. J. Clin. Nutr. 2012;95:283-9).
The significance of this is that visceral adipose tissue in the gut "is consistent with a higher cardiometabolic risk profile," he said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The study supports findings from the National Heart, Blood, and Lung Institute’s prospective Coronary Artery Risk Development in Young Adults (CARDIA) study of 3,000 individuals. Imaging done across the cohort at year 25 of the study showed a weak association between artificially sweetened beverages and the volume of fat in the visceral cavity, but a "really, really strong" association with sugar-sweetened beverages and visceral cavity adipose tissue, said Dr. Pereira.
"If you look at the true drivers of metabolic risk, the visceral fat, it’s not there with the artificially sweetened drinks, it’s only there with the sugar-sweetened ones," he said.
Although both diet and sugar-sweetened drinks have positive associations with incident diabetes and other metabolic disturbances, the relationship between "diet drinks and cardiometabolic risk may be an anomaly of reverse causality," Dr. Pereira said.
While findings from the CARDIA study show an association between waist circumference and consumption of diet drinks, there was not an association with blood sugar, lipids, or blood pressure. "So, the question is, ‘Why isn’t [diet drink consumption] driving the risk factors?" asked Dr. Pereira.
The reason may be that consumers of high amounts of diet drinks "are more likely to be overweight and obese, and are more likely to be at high risk for chronic disease so they choose beverages with low calories to try to lower their risk," he suggested.
However, the extent of reverse causality in this patient population, said Dr. Pereira, is still unknown: "There could be an increased risk [of cardiometabolic disease] with a higher intake of artificially sweetened drinks, but you could also say it is protective."
The lack of certainty, according to Dr. Pereira, is due to a drought of data from well designed studies.
"I argue with some of my colleagues who believe that we can learn just as much or more on this from observational prospective epidemiological studies," he said, adding, "I am kind of steadfast that this is a topic that should be clearly addressed in terms of mechanisms and causality through better randomized controlled trials."
Dr. Pereira reported he has received support from the Robert Wood Johnson Foundation.
ATLANTA – Diet drinks might be protective rather than causative in cardiometabolic diseases such as obesity and type 2 diabetes, but definitive data are lacking.
"I would say that based on the scientific evidence to date, it might be a good idea to switch to artificially sweetened beverages, but I don’t see the evidence to either promote or avoid them," said Mark Pereira, Ph.D., of the School of Public Health at the University of Minnesota, Minneapolis.
There are data linking sugar-sweetened beverages to metabolic disorders. Findings from a recent, small, but "pretty provocative" randomized pilot study point to a relationship between sugar-sweetened beverages’ strong effect on visceral fat, particularly in the intra-abdominal cavity, he said. Diet drinks were not found in the study to have a positive association with this kind of adiposity (Am. J. Clin. Nutr. 2012;95:283-9).
The significance of this is that visceral adipose tissue in the gut "is consistent with a higher cardiometabolic risk profile," he said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The study supports findings from the National Heart, Blood, and Lung Institute’s prospective Coronary Artery Risk Development in Young Adults (CARDIA) study of 3,000 individuals. Imaging done across the cohort at year 25 of the study showed a weak association between artificially sweetened beverages and the volume of fat in the visceral cavity, but a "really, really strong" association with sugar-sweetened beverages and visceral cavity adipose tissue, said Dr. Pereira.
"If you look at the true drivers of metabolic risk, the visceral fat, it’s not there with the artificially sweetened drinks, it’s only there with the sugar-sweetened ones," he said.
Although both diet and sugar-sweetened drinks have positive associations with incident diabetes and other metabolic disturbances, the relationship between "diet drinks and cardiometabolic risk may be an anomaly of reverse causality," Dr. Pereira said.
While findings from the CARDIA study show an association between waist circumference and consumption of diet drinks, there was not an association with blood sugar, lipids, or blood pressure. "So, the question is, ‘Why isn’t [diet drink consumption] driving the risk factors?" asked Dr. Pereira.
The reason may be that consumers of high amounts of diet drinks "are more likely to be overweight and obese, and are more likely to be at high risk for chronic disease so they choose beverages with low calories to try to lower their risk," he suggested.
However, the extent of reverse causality in this patient population, said Dr. Pereira, is still unknown: "There could be an increased risk [of cardiometabolic disease] with a higher intake of artificially sweetened drinks, but you could also say it is protective."
The lack of certainty, according to Dr. Pereira, is due to a drought of data from well designed studies.
"I argue with some of my colleagues who believe that we can learn just as much or more on this from observational prospective epidemiological studies," he said, adding, "I am kind of steadfast that this is a topic that should be clearly addressed in terms of mechanisms and causality through better randomized controlled trials."
Dr. Pereira reported he has received support from the Robert Wood Johnson Foundation.
EXPERT ANALYSIS FROM OBESITY WEEK
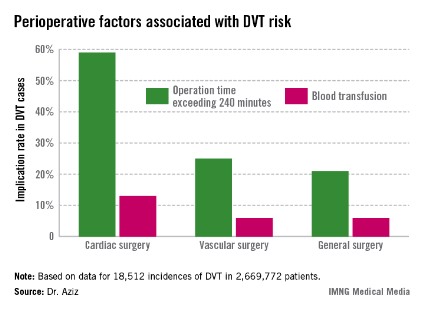
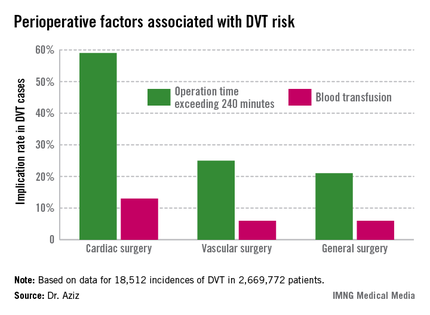
DVT risk higher in cardiac and vascular surgery patients
WASHINGTON – Cardiac and vascular surgery patients are at higher risk for deep vein thrombosis than are general surgery patients, according to data presented at the annual clinical congress of the American College of Surgeons.
In a retrospective analysis of 2,669,772 patients with a median age of 64 years, 43% of whom were males, in the ACS-National Surgery Quality Improvement Program (NSQIP) during 2005-2009, Dr. Faisal Aziz of Penn State Hershey (Pa.) Heart and Vascular Institute and his colleagues sought to determine the actual rate of deep vein thrombosis (DVT) during revascularization procedures, compared with general surgery. They also investigated the relationship between the type of operation and the DVT incidence rate.
The Agency for Healthcare Research and Quality considers the incidence rate of DVT a patient safety indicator. Dr. Aziz cited data indicating that one in four patients who develop DVT postoperatively before discharge has an additional venous thromboembolic event–related event in the subsequent 21 months requiring hospitalization, at a cost of approximately $15,000, or roughly 21% higher than the original DVT event (J. Manag. Care. Pharm. 2007;13:475-86).
The researchers sorted patients according to DVT risk factors such as age, gender, body mass index over 40 kg/m2, and whether the surgery was acute. They then assessed intraoperative factors such as total time to completion and its American Society of Anesthesiology score. They then considered the postoperative factors associated with DVT, such as blood transfusions, return to the operating room, deep wound infection, cardiac arrest, and mortality.
Dr. Aziz and his team determined that there were 18,512 incidences of DVT, equaling 0.69% of all patients studied. Of those, 0.66% occurred during general surgery, 2.08% occurred during cardiac surgery, and 1% occurred during vascular surgery.
"The implications of our study are that, contrary to popular belief, the incidence of postoperative DVT is actually higher after cardiac surgery and vascular surgery procedures," he said.
The cardiac surgery procedures associated with the highest DVT incidence rate were tricuspid valve replacement (8%), thoracic endovascular aortic repair (5%), thoracic aortic graft replacement (4%), and pericardial window (4%).
In a comparison of cardiac procedures, tricuspid valve replacement vs. aortic valve replacement had a risk ratio of 3.5 (P < .001). In tricuspid valve replacement vs. coronary artery bypass, the former had a risk ratio of 11.24 (P < .001).
Vascular surgeries with the highest DVT incidence rates were peripheral bypass (1%), amputation (trans-metatarsal, 0.75%; below knee, 1%; above the knee, 1%), and ruptured aortic aneurysms (3.5%), Dr. Aziz reported.
Intra-and postoperative factors associated with DVT risk included operation times exceeding 240 minutes and previous DVT. Compared with 21% of general surgery patients, operation time was implicated in 59% of cardiac surgery patients (relative risk, 2.72; P < .001) and 25% of vascular surgery patients (RR, 1.14; P <.001). Blood transfusions affected 13% of cardiac surgery patients (RR, 2.3; P < .001), 6% of vascular surgery patients (RR, 1.3; P < .001), and 6% of general surgery patients.
Compared with 24% for general surgery patients, returning to the operating room was implicated in 27% of cardiac patients (RR, 1.4; P = .27) and 32% of vascular surgery patients (RR, 1.3; P < .001).
"Procedures and perioperative factors associated with high risk of postoperative DVT should be identified, and adequate DVT prophylaxis should be ensured for these patients," he concluded.
Dr. Aziz and his associates had no disclosures.
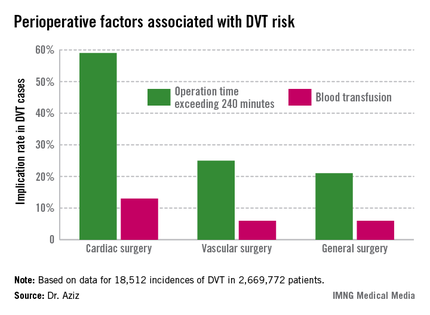
WASHINGTON – Cardiac and vascular surgery patients are at higher risk for deep vein thrombosis than are general surgery patients, according to data presented at the annual clinical congress of the American College of Surgeons.
In a retrospective analysis of 2,669,772 patients with a median age of 64 years, 43% of whom were males, in the ACS-National Surgery Quality Improvement Program (NSQIP) during 2005-2009, Dr. Faisal Aziz of Penn State Hershey (Pa.) Heart and Vascular Institute and his colleagues sought to determine the actual rate of deep vein thrombosis (DVT) during revascularization procedures, compared with general surgery. They also investigated the relationship between the type of operation and the DVT incidence rate.
The Agency for Healthcare Research and Quality considers the incidence rate of DVT a patient safety indicator. Dr. Aziz cited data indicating that one in four patients who develop DVT postoperatively before discharge has an additional venous thromboembolic event–related event in the subsequent 21 months requiring hospitalization, at a cost of approximately $15,000, or roughly 21% higher than the original DVT event (J. Manag. Care. Pharm. 2007;13:475-86).
The researchers sorted patients according to DVT risk factors such as age, gender, body mass index over 40 kg/m2, and whether the surgery was acute. They then assessed intraoperative factors such as total time to completion and its American Society of Anesthesiology score. They then considered the postoperative factors associated with DVT, such as blood transfusions, return to the operating room, deep wound infection, cardiac arrest, and mortality.
Dr. Aziz and his team determined that there were 18,512 incidences of DVT, equaling 0.69% of all patients studied. Of those, 0.66% occurred during general surgery, 2.08% occurred during cardiac surgery, and 1% occurred during vascular surgery.
"The implications of our study are that, contrary to popular belief, the incidence of postoperative DVT is actually higher after cardiac surgery and vascular surgery procedures," he said.
The cardiac surgery procedures associated with the highest DVT incidence rate were tricuspid valve replacement (8%), thoracic endovascular aortic repair (5%), thoracic aortic graft replacement (4%), and pericardial window (4%).
In a comparison of cardiac procedures, tricuspid valve replacement vs. aortic valve replacement had a risk ratio of 3.5 (P < .001). In tricuspid valve replacement vs. coronary artery bypass, the former had a risk ratio of 11.24 (P < .001).
Vascular surgeries with the highest DVT incidence rates were peripheral bypass (1%), amputation (trans-metatarsal, 0.75%; below knee, 1%; above the knee, 1%), and ruptured aortic aneurysms (3.5%), Dr. Aziz reported.
Intra-and postoperative factors associated with DVT risk included operation times exceeding 240 minutes and previous DVT. Compared with 21% of general surgery patients, operation time was implicated in 59% of cardiac surgery patients (relative risk, 2.72; P < .001) and 25% of vascular surgery patients (RR, 1.14; P <.001). Blood transfusions affected 13% of cardiac surgery patients (RR, 2.3; P < .001), 6% of vascular surgery patients (RR, 1.3; P < .001), and 6% of general surgery patients.
Compared with 24% for general surgery patients, returning to the operating room was implicated in 27% of cardiac patients (RR, 1.4; P = .27) and 32% of vascular surgery patients (RR, 1.3; P < .001).
"Procedures and perioperative factors associated with high risk of postoperative DVT should be identified, and adequate DVT prophylaxis should be ensured for these patients," he concluded.
Dr. Aziz and his associates had no disclosures.
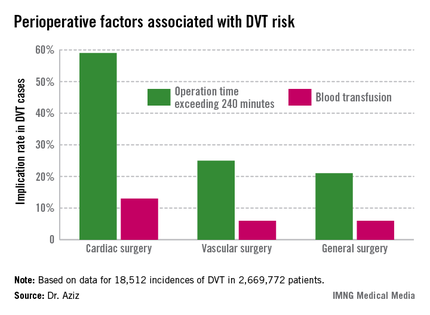
WASHINGTON – Cardiac and vascular surgery patients are at higher risk for deep vein thrombosis than are general surgery patients, according to data presented at the annual clinical congress of the American College of Surgeons.
In a retrospective analysis of 2,669,772 patients with a median age of 64 years, 43% of whom were males, in the ACS-National Surgery Quality Improvement Program (NSQIP) during 2005-2009, Dr. Faisal Aziz of Penn State Hershey (Pa.) Heart and Vascular Institute and his colleagues sought to determine the actual rate of deep vein thrombosis (DVT) during revascularization procedures, compared with general surgery. They also investigated the relationship between the type of operation and the DVT incidence rate.
The Agency for Healthcare Research and Quality considers the incidence rate of DVT a patient safety indicator. Dr. Aziz cited data indicating that one in four patients who develop DVT postoperatively before discharge has an additional venous thromboembolic event–related event in the subsequent 21 months requiring hospitalization, at a cost of approximately $15,000, or roughly 21% higher than the original DVT event (J. Manag. Care. Pharm. 2007;13:475-86).
The researchers sorted patients according to DVT risk factors such as age, gender, body mass index over 40 kg/m2, and whether the surgery was acute. They then assessed intraoperative factors such as total time to completion and its American Society of Anesthesiology score. They then considered the postoperative factors associated with DVT, such as blood transfusions, return to the operating room, deep wound infection, cardiac arrest, and mortality.
Dr. Aziz and his team determined that there were 18,512 incidences of DVT, equaling 0.69% of all patients studied. Of those, 0.66% occurred during general surgery, 2.08% occurred during cardiac surgery, and 1% occurred during vascular surgery.
"The implications of our study are that, contrary to popular belief, the incidence of postoperative DVT is actually higher after cardiac surgery and vascular surgery procedures," he said.
The cardiac surgery procedures associated with the highest DVT incidence rate were tricuspid valve replacement (8%), thoracic endovascular aortic repair (5%), thoracic aortic graft replacement (4%), and pericardial window (4%).
In a comparison of cardiac procedures, tricuspid valve replacement vs. aortic valve replacement had a risk ratio of 3.5 (P < .001). In tricuspid valve replacement vs. coronary artery bypass, the former had a risk ratio of 11.24 (P < .001).
Vascular surgeries with the highest DVT incidence rates were peripheral bypass (1%), amputation (trans-metatarsal, 0.75%; below knee, 1%; above the knee, 1%), and ruptured aortic aneurysms (3.5%), Dr. Aziz reported.
Intra-and postoperative factors associated with DVT risk included operation times exceeding 240 minutes and previous DVT. Compared with 21% of general surgery patients, operation time was implicated in 59% of cardiac surgery patients (relative risk, 2.72; P < .001) and 25% of vascular surgery patients (RR, 1.14; P <.001). Blood transfusions affected 13% of cardiac surgery patients (RR, 2.3; P < .001), 6% of vascular surgery patients (RR, 1.3; P < .001), and 6% of general surgery patients.
Compared with 24% for general surgery patients, returning to the operating room was implicated in 27% of cardiac patients (RR, 1.4; P = .27) and 32% of vascular surgery patients (RR, 1.3; P < .001).
"Procedures and perioperative factors associated with high risk of postoperative DVT should be identified, and adequate DVT prophylaxis should be ensured for these patients," he concluded.
Dr. Aziz and his associates had no disclosures.
AT THE ACS CLINICAL CONGRESS
Major finding: Of the 2,669,772 patients studied, 18,512 (0.69%) had DVTs during surgery. The rate was 0.66% for general surgery, 2.08% for cardiac surgery, and 1% for vascular surgery.
Data source: Retrospective analysis of NSQIP 2005-2009 database analyzed according to surgical specialty.
Disclosures: Dr. Aziz and his associates had no disclosures.
Cognitive impairment at baseline linked to poorer bariatric surgery outcomes
ATLANTA – Higher baseline levels of cognitive impairment are associated with poorer weight loss outcomes after bariatric surgery.
"People with problems of memory, problem solving, or attention prior to surgery show reduced ability to lose weight," said John Gunstad, Ph.D., at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
In a prospective study of 109 bariatric surgery patients enrolled in the LABS (Longitudinal Assessment of Bariatric Surgery) study and 41 obese matched controls who’d not had surgery, Dr. Gunstad, who is professor and chairman of neuroscience at Kent (Ohio) State University, and his colleagues assessed all participants’ cognitive function at baseline, at 12 weeks, and at 12, 24, and 36 months.
They found that 25% of all surgical patients had baseline cognitive impairment. "These were individuals who were at least 1.5 standard deviations below normal-weight persons in at least one cognitive domain," said Dr. Gunstad. "If these individuals came to my clinic, I would have to diagnose them with some kind of cognitive disorder."
Expanding the criteria to 1 standard deviation meant that 40% of participants had subtle impairment. "Patients who are coming in for bariatric surgery are between 5 and 8 times more likely to have cognitive impairment than their normal-weight counterparts. That’s a remarkable number," said Dr. Gunstad.
At 12 weeks, surgery patients who’d lost an average of 48 pounds showed gains in cognitive functioning. Overall, the study showed initial, rapid cognitive improvement, and then either continued or sustained improvement 3 years out.
"We went from a quarter of patients being clinically impaired prior to surgery," said Dr. Gunstad. "At 3 years after surgery, that number was down to 4%."
However, in a related study, Dr. Gunstad and his colleagues found that greater levels of cognitive impairment correlated to less weight loss at all follow-up points (Surg. Obes. Relat. Dis. 2013;9:765-70).
Dr. Gunstad said this was likely due to patient adherence issues after the tumult of bariatric surgery. "You have to eat in a different way. You have to think in a different way. You have to restructure every moment of your life," said Dr. Gunstad. "If you have problems with memory, problem solving, or organizing, it will be much more difficult to make and persist with those changes."
The clinical implication, said Dr. Gunstad, is that better screening of bariatric surgery candidates might be helpful. "If we know the cognitive status of our patients, it’s likely we will know what the outcomes will be," he said.
The drawback, he said, is that even though most third-party payers will cover the costs of evaluations, if a physician has a large practice of hundreds of patients, then the number of referrals might be overwhelming to the system, which might not have enough neuropsychologists to perform the tests.
Self-reporting might also be an issue because of the phenomenon of the "worried well" – the patients who overreport their problems – or because the patients with cognitive impairment won’t necessarily recognize the symptoms they need to report, said Dr. Gunstad.
By next year, said Dr. Gunstad, he hoped he and his colleagues will have finalized a better screening tool for clinicians who treat bariatric surgery patients.
Dr. Gunstad did not report any financial disclosures.
ATLANTA – Higher baseline levels of cognitive impairment are associated with poorer weight loss outcomes after bariatric surgery.
"People with problems of memory, problem solving, or attention prior to surgery show reduced ability to lose weight," said John Gunstad, Ph.D., at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
In a prospective study of 109 bariatric surgery patients enrolled in the LABS (Longitudinal Assessment of Bariatric Surgery) study and 41 obese matched controls who’d not had surgery, Dr. Gunstad, who is professor and chairman of neuroscience at Kent (Ohio) State University, and his colleagues assessed all participants’ cognitive function at baseline, at 12 weeks, and at 12, 24, and 36 months.
They found that 25% of all surgical patients had baseline cognitive impairment. "These were individuals who were at least 1.5 standard deviations below normal-weight persons in at least one cognitive domain," said Dr. Gunstad. "If these individuals came to my clinic, I would have to diagnose them with some kind of cognitive disorder."
Expanding the criteria to 1 standard deviation meant that 40% of participants had subtle impairment. "Patients who are coming in for bariatric surgery are between 5 and 8 times more likely to have cognitive impairment than their normal-weight counterparts. That’s a remarkable number," said Dr. Gunstad.
At 12 weeks, surgery patients who’d lost an average of 48 pounds showed gains in cognitive functioning. Overall, the study showed initial, rapid cognitive improvement, and then either continued or sustained improvement 3 years out.
"We went from a quarter of patients being clinically impaired prior to surgery," said Dr. Gunstad. "At 3 years after surgery, that number was down to 4%."
However, in a related study, Dr. Gunstad and his colleagues found that greater levels of cognitive impairment correlated to less weight loss at all follow-up points (Surg. Obes. Relat. Dis. 2013;9:765-70).
Dr. Gunstad said this was likely due to patient adherence issues after the tumult of bariatric surgery. "You have to eat in a different way. You have to think in a different way. You have to restructure every moment of your life," said Dr. Gunstad. "If you have problems with memory, problem solving, or organizing, it will be much more difficult to make and persist with those changes."
The clinical implication, said Dr. Gunstad, is that better screening of bariatric surgery candidates might be helpful. "If we know the cognitive status of our patients, it’s likely we will know what the outcomes will be," he said.
The drawback, he said, is that even though most third-party payers will cover the costs of evaluations, if a physician has a large practice of hundreds of patients, then the number of referrals might be overwhelming to the system, which might not have enough neuropsychologists to perform the tests.
Self-reporting might also be an issue because of the phenomenon of the "worried well" – the patients who overreport their problems – or because the patients with cognitive impairment won’t necessarily recognize the symptoms they need to report, said Dr. Gunstad.
By next year, said Dr. Gunstad, he hoped he and his colleagues will have finalized a better screening tool for clinicians who treat bariatric surgery patients.
Dr. Gunstad did not report any financial disclosures.
ATLANTA – Higher baseline levels of cognitive impairment are associated with poorer weight loss outcomes after bariatric surgery.
"People with problems of memory, problem solving, or attention prior to surgery show reduced ability to lose weight," said John Gunstad, Ph.D., at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
In a prospective study of 109 bariatric surgery patients enrolled in the LABS (Longitudinal Assessment of Bariatric Surgery) study and 41 obese matched controls who’d not had surgery, Dr. Gunstad, who is professor and chairman of neuroscience at Kent (Ohio) State University, and his colleagues assessed all participants’ cognitive function at baseline, at 12 weeks, and at 12, 24, and 36 months.
They found that 25% of all surgical patients had baseline cognitive impairment. "These were individuals who were at least 1.5 standard deviations below normal-weight persons in at least one cognitive domain," said Dr. Gunstad. "If these individuals came to my clinic, I would have to diagnose them with some kind of cognitive disorder."
Expanding the criteria to 1 standard deviation meant that 40% of participants had subtle impairment. "Patients who are coming in for bariatric surgery are between 5 and 8 times more likely to have cognitive impairment than their normal-weight counterparts. That’s a remarkable number," said Dr. Gunstad.
At 12 weeks, surgery patients who’d lost an average of 48 pounds showed gains in cognitive functioning. Overall, the study showed initial, rapid cognitive improvement, and then either continued or sustained improvement 3 years out.
"We went from a quarter of patients being clinically impaired prior to surgery," said Dr. Gunstad. "At 3 years after surgery, that number was down to 4%."
However, in a related study, Dr. Gunstad and his colleagues found that greater levels of cognitive impairment correlated to less weight loss at all follow-up points (Surg. Obes. Relat. Dis. 2013;9:765-70).
Dr. Gunstad said this was likely due to patient adherence issues after the tumult of bariatric surgery. "You have to eat in a different way. You have to think in a different way. You have to restructure every moment of your life," said Dr. Gunstad. "If you have problems with memory, problem solving, or organizing, it will be much more difficult to make and persist with those changes."
The clinical implication, said Dr. Gunstad, is that better screening of bariatric surgery candidates might be helpful. "If we know the cognitive status of our patients, it’s likely we will know what the outcomes will be," he said.
The drawback, he said, is that even though most third-party payers will cover the costs of evaluations, if a physician has a large practice of hundreds of patients, then the number of referrals might be overwhelming to the system, which might not have enough neuropsychologists to perform the tests.
Self-reporting might also be an issue because of the phenomenon of the "worried well" – the patients who overreport their problems – or because the patients with cognitive impairment won’t necessarily recognize the symptoms they need to report, said Dr. Gunstad.
By next year, said Dr. Gunstad, he hoped he and his colleagues will have finalized a better screening tool for clinicians who treat bariatric surgery patients.
Dr. Gunstad did not report any financial disclosures.
AT OBESITY WEEK
Vegetarian, Vegan Diets for Weight Loss?
Earn 0.25 hours AMA PRA Category 1 credit: Read this article, and click the link at the end to take the post-test.
ATLANTA – Vegetarian and vegan diets that did not emphasize counting calories led to more weight loss over 8 weeks and at 6 months than did diets that included meat, according to data presented at Obesity Week.
"We’re not trying to get people to lose weight just so they can look attractive," said Gabrielle Turner-McGrievy, Ph.D., in an interview. "We’re hoping they will choose a healthy body weight to prevent diabetes and cancer."
The results are from the first randomized study to directly compare the effect of vegan, vegetarian, and omnivorous diets, without caloric restrictions, on body weight, said Dr. Turner-McGrievy, of the department of health promotion, education, and behavior at the Arnold School of Public Health at the University of South Carolina in Columbia.
In the New DIETs (New Dietary Interventions to Enhance the Treatments for Weight Loss) study, 63 adults (73% female, 79% white) with a mean age of 49 years and a mean body mass index of 35 kg/m2 were randomly assigned to one of five diets: vegan, vegetarian, pesco-vegetarian, semi-vegetarian, and omnivorous*. All five dietary approaches emphasized low-fat, low-glycemic-index foods but did not require caloric restriction. All participants attended weekly meetings to learn more about the type of diet they had been assigned. All diets stressed consumption of foods that were as unprocessed as possible. Participants who screened positive for eating disorder–like behavior were not included in the study.
An intent-to-treat analysis showed that at 8 weeks, the groups that followed a plant-based diet had lost an average of 8-10 pounds, while those consuming some meat lost an average of 5 pounds.
At 6 months, the vegans had lost about 7% of their body weight, the semi-vegetarian group had lost about 4% of their body weight, the pesco-vegetarian group had lost about 3%, and the omnivorous group had lost about 3%, Dr. Turner-McGrievy reported.
"All groups lost a significant amount of weight without having to count calories, but it was greatest in the vegan group," she said. Compliance in the vegan group at 8 weeks averaged about half; at 6 months, it had dropped to 30%.
"Our message here is that adherence may not be completely necessary," she said. "We shifted people so far down the dietary spectrum that even if they added a little cheese or meat here or there, they still weren’t going back to where they were before."
The exact reason for the greater weight loss in the plant-based diet groups was not clear, said Dr. Turner-McGrievy, but she and her colleagues theorized that changes in macronutrient content, which were found to be significantly different across groups (P < .05), may be a factor. "When we looked at the nutritive changes of these five different diets, we saw a much greater decrease of saturated fat among the vegan diet group," she said. "Vegetarians and vegans also decreased their cholesterol more than the other groups."
When Dr. Turner-McGrievy was asked whether any groups consumed more food, on average, than other groups, she said her team had not determined if there were different levels of hunger between the groups. Study participants were enthusiastic about the "freedom" they had from calorie counting: "On calorie-restricted diets, if at the end of the day you’ve reached your calorie allotment, but you’re still hungry, then you go to bed hungry," she said.
Despite the limited sample size and duration of the NEW DIETs study, Dr. Turner-McGrievy said one of the study’s implications is that when it comes to treating obesity and its attendant comorbidities, there can be a focus on nutrition. "It moves this area of science forward and shows there is another approach that can be used instead of calorie restriction," she said. People with obesity could also be placed on a "stepwise" system, where they start out eating slightly less meat, and eventually move to a more plant-based diet, she noted.
Obesity Week was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Turner-McGrievy did not have any relevant disclosures.
*Correction, 12/11/2013: An earlier version of this article misstated one of the diets included in the New DIETs study.
To earn 0.25 hours AMA PRA Category 1 credit after reading this article, take the post-test here.
Earn 0.25 hours AMA PRA Category 1 credit: Read this article, and click the link at the end to take the post-test.
ATLANTA – Vegetarian and vegan diets that did not emphasize counting calories led to more weight loss over 8 weeks and at 6 months than did diets that included meat, according to data presented at Obesity Week.
"We’re not trying to get people to lose weight just so they can look attractive," said Gabrielle Turner-McGrievy, Ph.D., in an interview. "We’re hoping they will choose a healthy body weight to prevent diabetes and cancer."
The results are from the first randomized study to directly compare the effect of vegan, vegetarian, and omnivorous diets, without caloric restrictions, on body weight, said Dr. Turner-McGrievy, of the department of health promotion, education, and behavior at the Arnold School of Public Health at the University of South Carolina in Columbia.
In the New DIETs (New Dietary Interventions to Enhance the Treatments for Weight Loss) study, 63 adults (73% female, 79% white) with a mean age of 49 years and a mean body mass index of 35 kg/m2 were randomly assigned to one of five diets: vegan, vegetarian, pesco-vegetarian, semi-vegetarian, and omnivorous*. All five dietary approaches emphasized low-fat, low-glycemic-index foods but did not require caloric restriction. All participants attended weekly meetings to learn more about the type of diet they had been assigned. All diets stressed consumption of foods that were as unprocessed as possible. Participants who screened positive for eating disorder–like behavior were not included in the study.
An intent-to-treat analysis showed that at 8 weeks, the groups that followed a plant-based diet had lost an average of 8-10 pounds, while those consuming some meat lost an average of 5 pounds.
At 6 months, the vegans had lost about 7% of their body weight, the semi-vegetarian group had lost about 4% of their body weight, the pesco-vegetarian group had lost about 3%, and the omnivorous group had lost about 3%, Dr. Turner-McGrievy reported.
"All groups lost a significant amount of weight without having to count calories, but it was greatest in the vegan group," she said. Compliance in the vegan group at 8 weeks averaged about half; at 6 months, it had dropped to 30%.
"Our message here is that adherence may not be completely necessary," she said. "We shifted people so far down the dietary spectrum that even if they added a little cheese or meat here or there, they still weren’t going back to where they were before."
The exact reason for the greater weight loss in the plant-based diet groups was not clear, said Dr. Turner-McGrievy, but she and her colleagues theorized that changes in macronutrient content, which were found to be significantly different across groups (P < .05), may be a factor. "When we looked at the nutritive changes of these five different diets, we saw a much greater decrease of saturated fat among the vegan diet group," she said. "Vegetarians and vegans also decreased their cholesterol more than the other groups."
When Dr. Turner-McGrievy was asked whether any groups consumed more food, on average, than other groups, she said her team had not determined if there were different levels of hunger between the groups. Study participants were enthusiastic about the "freedom" they had from calorie counting: "On calorie-restricted diets, if at the end of the day you’ve reached your calorie allotment, but you’re still hungry, then you go to bed hungry," she said.
Despite the limited sample size and duration of the NEW DIETs study, Dr. Turner-McGrievy said one of the study’s implications is that when it comes to treating obesity and its attendant comorbidities, there can be a focus on nutrition. "It moves this area of science forward and shows there is another approach that can be used instead of calorie restriction," she said. People with obesity could also be placed on a "stepwise" system, where they start out eating slightly less meat, and eventually move to a more plant-based diet, she noted.
Obesity Week was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Turner-McGrievy did not have any relevant disclosures.
*Correction, 12/11/2013: An earlier version of this article misstated one of the diets included in the New DIETs study.
To earn 0.25 hours AMA PRA Category 1 credit after reading this article, take the post-test here.
Earn 0.25 hours AMA PRA Category 1 credit: Read this article, and click the link at the end to take the post-test.
ATLANTA – Vegetarian and vegan diets that did not emphasize counting calories led to more weight loss over 8 weeks and at 6 months than did diets that included meat, according to data presented at Obesity Week.
"We’re not trying to get people to lose weight just so they can look attractive," said Gabrielle Turner-McGrievy, Ph.D., in an interview. "We’re hoping they will choose a healthy body weight to prevent diabetes and cancer."
The results are from the first randomized study to directly compare the effect of vegan, vegetarian, and omnivorous diets, without caloric restrictions, on body weight, said Dr. Turner-McGrievy, of the department of health promotion, education, and behavior at the Arnold School of Public Health at the University of South Carolina in Columbia.
In the New DIETs (New Dietary Interventions to Enhance the Treatments for Weight Loss) study, 63 adults (73% female, 79% white) with a mean age of 49 years and a mean body mass index of 35 kg/m2 were randomly assigned to one of five diets: vegan, vegetarian, pesco-vegetarian, semi-vegetarian, and omnivorous*. All five dietary approaches emphasized low-fat, low-glycemic-index foods but did not require caloric restriction. All participants attended weekly meetings to learn more about the type of diet they had been assigned. All diets stressed consumption of foods that were as unprocessed as possible. Participants who screened positive for eating disorder–like behavior were not included in the study.
An intent-to-treat analysis showed that at 8 weeks, the groups that followed a plant-based diet had lost an average of 8-10 pounds, while those consuming some meat lost an average of 5 pounds.
At 6 months, the vegans had lost about 7% of their body weight, the semi-vegetarian group had lost about 4% of their body weight, the pesco-vegetarian group had lost about 3%, and the omnivorous group had lost about 3%, Dr. Turner-McGrievy reported.
"All groups lost a significant amount of weight without having to count calories, but it was greatest in the vegan group," she said. Compliance in the vegan group at 8 weeks averaged about half; at 6 months, it had dropped to 30%.
"Our message here is that adherence may not be completely necessary," she said. "We shifted people so far down the dietary spectrum that even if they added a little cheese or meat here or there, they still weren’t going back to where they were before."
The exact reason for the greater weight loss in the plant-based diet groups was not clear, said Dr. Turner-McGrievy, but she and her colleagues theorized that changes in macronutrient content, which were found to be significantly different across groups (P < .05), may be a factor. "When we looked at the nutritive changes of these five different diets, we saw a much greater decrease of saturated fat among the vegan diet group," she said. "Vegetarians and vegans also decreased their cholesterol more than the other groups."
When Dr. Turner-McGrievy was asked whether any groups consumed more food, on average, than other groups, she said her team had not determined if there were different levels of hunger between the groups. Study participants were enthusiastic about the "freedom" they had from calorie counting: "On calorie-restricted diets, if at the end of the day you’ve reached your calorie allotment, but you’re still hungry, then you go to bed hungry," she said.
Despite the limited sample size and duration of the NEW DIETs study, Dr. Turner-McGrievy said one of the study’s implications is that when it comes to treating obesity and its attendant comorbidities, there can be a focus on nutrition. "It moves this area of science forward and shows there is another approach that can be used instead of calorie restriction," she said. People with obesity could also be placed on a "stepwise" system, where they start out eating slightly less meat, and eventually move to a more plant-based diet, she noted.
Obesity Week was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Turner-McGrievy did not have any relevant disclosures.
*Correction, 12/11/2013: An earlier version of this article misstated one of the diets included in the New DIETs study.
To earn 0.25 hours AMA PRA Category 1 credit after reading this article, take the post-test here.
AT OBESITY WEEK
Obese and overweight adults lost significant weight on vegetarian, vegan diets
ATLANTA – Vegetarian and vegan diets that did not emphasize counting calories led to more weight loss over 8 weeks and at 6 months than did diets that included meat, according to data presented at Obesity Week.
"We’re not trying to get people to lose weight just so they can look attractive," said Gabrielle Turner-McGrievy, Ph.D., in an interview. "We’re hoping they will choose a healthy body weight to prevent diabetes and cancer."
The results are from the first randomized study to directly compare the effect of vegan, vegetarian, and omnivorous diets, without caloric restrictions, on body weight, said Dr. Turner-McGrievy, of the department of health promotion, education, and behavior at the Arnold School of Public Health at the University of South Carolina in Columbia.
In the New DIETs (New Dietary Interventions to Enhance the Treatments for Weight Loss) study, 63 adults (73% female, 79% white) with a mean age of 49 years and a mean body mass index of 35 kg/m2 were randomly assigned to one of five diets: vegan, vegetarian, pesco-vegetarian, semi-vegetarian, and omnivorous*. All five dietary approaches emphasized low-fat, low-glycemic-index foods but did not require caloric restriction. All participants attended weekly meetings to learn more about the type of diet they had been assigned. All diets stressed consumption of foods that were as unprocessed as possible. Participants who screened positive for eating disorder–like behavior were not included in the study.
An intent-to-treat analysis showed that at 8 weeks, the groups that followed a plant-based diet had lost an average of 8-10 pounds, while those consuming some meat lost an average of 5 pounds.
At 6 months, the vegans had lost about 7% of their body weight, the semi-vegetarian group had lost about 4% of their body weight, the pesco-vegetarian group had lost about 3%, and the omnivorous group had lost about 3%, Dr. Turner-McGrievy reported.
"All groups lost a significant amount of weight without having to count calories, but it was greatest in the vegan group," she said. Compliance in the vegan group at 8 weeks averaged about half; at 6 months, it had dropped to 30%.
"Our message here is that adherence may not be completely necessary," she said. "We shifted people so far down the dietary spectrum that even if they added a little cheese or meat here or there, they still weren’t going back to where they were before."
The exact reason for the greater weight loss in the plant-based diet groups was not clear, said Dr. Turner-McGrievy, but she and her colleagues theorized that changes in macronutrient content, which were found to be significantly different across groups (P < .05), may be a factor. "When we looked at the nutritive changes of these five different diets, we saw a much greater decrease of saturated fat among the vegan diet group," she said. "Vegetarians and vegans also decreased their cholesterol more than the other groups."
When Dr. Turner-McGrievy was asked whether any groups consumed more food, on average, than other groups, she said her team had not determined if there were different levels of hunger between the groups. Study participants were enthusiastic about the "freedom" they had from calorie counting: "On calorie-restricted diets, if at the end of the day you’ve reached your calorie allotment, but you’re still hungry, then you go to bed hungry," she said.
Despite the limited sample size and duration of the NEW DIETs study, Dr. Turner-McGrievy said one of the study’s implications is that when it comes to treating obesity and its attendant comorbidities, there can be a focus on nutrition. "It moves this area of science forward and shows there is another approach that can be used instead of calorie restriction," she said. People with obesity could also be placed on a "stepwise" system, where they start out eating slightly less meat, and eventually move to a more plant-based diet, she noted.
Obesity Week was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Turner-McGrievy did not have any relevant disclosures.
*Correction, 12/11/2013: An earlier version of this article misstated one of the diets included in the New DIETs study.
ATLANTA – Vegetarian and vegan diets that did not emphasize counting calories led to more weight loss over 8 weeks and at 6 months than did diets that included meat, according to data presented at Obesity Week.
"We’re not trying to get people to lose weight just so they can look attractive," said Gabrielle Turner-McGrievy, Ph.D., in an interview. "We’re hoping they will choose a healthy body weight to prevent diabetes and cancer."
The results are from the first randomized study to directly compare the effect of vegan, vegetarian, and omnivorous diets, without caloric restrictions, on body weight, said Dr. Turner-McGrievy, of the department of health promotion, education, and behavior at the Arnold School of Public Health at the University of South Carolina in Columbia.
In the New DIETs (New Dietary Interventions to Enhance the Treatments for Weight Loss) study, 63 adults (73% female, 79% white) with a mean age of 49 years and a mean body mass index of 35 kg/m2 were randomly assigned to one of five diets: vegan, vegetarian, pesco-vegetarian, semi-vegetarian, and omnivorous*. All five dietary approaches emphasized low-fat, low-glycemic-index foods but did not require caloric restriction. All participants attended weekly meetings to learn more about the type of diet they had been assigned. All diets stressed consumption of foods that were as unprocessed as possible. Participants who screened positive for eating disorder–like behavior were not included in the study.
An intent-to-treat analysis showed that at 8 weeks, the groups that followed a plant-based diet had lost an average of 8-10 pounds, while those consuming some meat lost an average of 5 pounds.
At 6 months, the vegans had lost about 7% of their body weight, the semi-vegetarian group had lost about 4% of their body weight, the pesco-vegetarian group had lost about 3%, and the omnivorous group had lost about 3%, Dr. Turner-McGrievy reported.
"All groups lost a significant amount of weight without having to count calories, but it was greatest in the vegan group," she said. Compliance in the vegan group at 8 weeks averaged about half; at 6 months, it had dropped to 30%.
"Our message here is that adherence may not be completely necessary," she said. "We shifted people so far down the dietary spectrum that even if they added a little cheese or meat here or there, they still weren’t going back to where they were before."
The exact reason for the greater weight loss in the plant-based diet groups was not clear, said Dr. Turner-McGrievy, but she and her colleagues theorized that changes in macronutrient content, which were found to be significantly different across groups (P < .05), may be a factor. "When we looked at the nutritive changes of these five different diets, we saw a much greater decrease of saturated fat among the vegan diet group," she said. "Vegetarians and vegans also decreased their cholesterol more than the other groups."
When Dr. Turner-McGrievy was asked whether any groups consumed more food, on average, than other groups, she said her team had not determined if there were different levels of hunger between the groups. Study participants were enthusiastic about the "freedom" they had from calorie counting: "On calorie-restricted diets, if at the end of the day you’ve reached your calorie allotment, but you’re still hungry, then you go to bed hungry," she said.
Despite the limited sample size and duration of the NEW DIETs study, Dr. Turner-McGrievy said one of the study’s implications is that when it comes to treating obesity and its attendant comorbidities, there can be a focus on nutrition. "It moves this area of science forward and shows there is another approach that can be used instead of calorie restriction," she said. People with obesity could also be placed on a "stepwise" system, where they start out eating slightly less meat, and eventually move to a more plant-based diet, she noted.
Obesity Week was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Turner-McGrievy did not have any relevant disclosures.
*Correction, 12/11/2013: An earlier version of this article misstated one of the diets included in the New DIETs study.
ATLANTA – Vegetarian and vegan diets that did not emphasize counting calories led to more weight loss over 8 weeks and at 6 months than did diets that included meat, according to data presented at Obesity Week.
"We’re not trying to get people to lose weight just so they can look attractive," said Gabrielle Turner-McGrievy, Ph.D., in an interview. "We’re hoping they will choose a healthy body weight to prevent diabetes and cancer."
The results are from the first randomized study to directly compare the effect of vegan, vegetarian, and omnivorous diets, without caloric restrictions, on body weight, said Dr. Turner-McGrievy, of the department of health promotion, education, and behavior at the Arnold School of Public Health at the University of South Carolina in Columbia.
In the New DIETs (New Dietary Interventions to Enhance the Treatments for Weight Loss) study, 63 adults (73% female, 79% white) with a mean age of 49 years and a mean body mass index of 35 kg/m2 were randomly assigned to one of five diets: vegan, vegetarian, pesco-vegetarian, semi-vegetarian, and omnivorous*. All five dietary approaches emphasized low-fat, low-glycemic-index foods but did not require caloric restriction. All participants attended weekly meetings to learn more about the type of diet they had been assigned. All diets stressed consumption of foods that were as unprocessed as possible. Participants who screened positive for eating disorder–like behavior were not included in the study.
An intent-to-treat analysis showed that at 8 weeks, the groups that followed a plant-based diet had lost an average of 8-10 pounds, while those consuming some meat lost an average of 5 pounds.
At 6 months, the vegans had lost about 7% of their body weight, the semi-vegetarian group had lost about 4% of their body weight, the pesco-vegetarian group had lost about 3%, and the omnivorous group had lost about 3%, Dr. Turner-McGrievy reported.
"All groups lost a significant amount of weight without having to count calories, but it was greatest in the vegan group," she said. Compliance in the vegan group at 8 weeks averaged about half; at 6 months, it had dropped to 30%.
"Our message here is that adherence may not be completely necessary," she said. "We shifted people so far down the dietary spectrum that even if they added a little cheese or meat here or there, they still weren’t going back to where they were before."
The exact reason for the greater weight loss in the plant-based diet groups was not clear, said Dr. Turner-McGrievy, but she and her colleagues theorized that changes in macronutrient content, which were found to be significantly different across groups (P < .05), may be a factor. "When we looked at the nutritive changes of these five different diets, we saw a much greater decrease of saturated fat among the vegan diet group," she said. "Vegetarians and vegans also decreased their cholesterol more than the other groups."
When Dr. Turner-McGrievy was asked whether any groups consumed more food, on average, than other groups, she said her team had not determined if there were different levels of hunger between the groups. Study participants were enthusiastic about the "freedom" they had from calorie counting: "On calorie-restricted diets, if at the end of the day you’ve reached your calorie allotment, but you’re still hungry, then you go to bed hungry," she said.
Despite the limited sample size and duration of the NEW DIETs study, Dr. Turner-McGrievy said one of the study’s implications is that when it comes to treating obesity and its attendant comorbidities, there can be a focus on nutrition. "It moves this area of science forward and shows there is another approach that can be used instead of calorie restriction," she said. People with obesity could also be placed on a "stepwise" system, where they start out eating slightly less meat, and eventually move to a more plant-based diet, she noted.
Obesity Week was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Turner-McGrievy did not have any relevant disclosures.
*Correction, 12/11/2013: An earlier version of this article misstated one of the diets included in the New DIETs study.
AT OBESITY WEEK
Major finding: Plant-based diets, without calorie restriction, led to nearly twice as much weight loss as diets that included meat in 63 obese and overweight adults.
Data source: Randomized controlled pilot study conducted over 8 weeks and followed up at 6 months.
Disclosures: Dr. Turner-McGrievy did not have any relevant disclosures.
Gastric bypass associated with reversal of aging process
ATLANTA – Gastric bypass was associated with the lengthening of telomeres, an indication that surgical weight loss may reverse aging in obese patients.
The most significant changes in telomere length occurred in patients with biomarkers indicative of higher levels of preoperative inflammation and cholesterol, according to findings presented by bariatric surgeon John Morton at this year’s Obesity Week.
"Telomeres are unique markers for aging and are linked to chronic diseases and things like smoking and depression," Dr. Morton said in an interview. "There are a lot of things that can potentially affect telomeres, but there aren’t a lot of things that can affect them in a positive sense."
Dr. Morton and his colleagues at Stanford (Calif.) University measured the baseline telomere length, weight, C-reactive protein (CRP) levels, cholesterol levels, and fasting insulin levels in 51 gastric bypass surgery patients (77% female, average age 49 years). The group’s mean body mass index was 44 kg/m2. The measurements were taken again at 3, 6, and 12 months. Telomere length was determined using quantitative polymerase chain reaction testing.
In all patients, excess body weight loss at 12 months averaged 71%; CRP levels, indicative of inflammation, dropped an average of more than 60%. Fasting insulin levels decreased from 24 uIU/mL at baseline to 6 uIU/mL when measured 1 year after surgery. These results were consistent with those of previous studies, but this study was the first to correlate such changes with the body’s biomarkers for aging, telomeres, Dr. Morton said.
Unexpected results
Telomere length did not change significantly across the cohort, but when analyzed according to CRP and LDL levels, significant changes in telomere length were found in patients whose levels of both were higher at baseline (P = .0387 and P = .005). In those whose baseline CRP was high, there also was a significant positive correlation between telomere lengthening and weight loss (P = .0498) and increases in HDL cholesterol level (P = .0176).
The results were somewhat unexpected. "The thing that surprised me the most was that if there were going to be changes, then they should be across the board," said Dr. Morton. "But where it really made a difference was in those who had [high levels of markers of] inflammation. It was a pretty specific result in a pretty specific population."
At least one other longitudinal study has shown the impact of nonsurgical intervention, namely a change in diet, on the length of telomeres (PLoS One 2013;8:e62781[doi:10.1371/journal.pone.0062781]), but Dr. Morton said the study, which emphasized eating less red meat and more fish, fresh vegetables, and olive oil did not demonstrate results that were notably different from his findings.
"One thing that study’s diet, the Mediterranean Diet, is known to do is to raise HDL," said Dr. Morton. "In our study we also saw a correlation between telomere lengthening and increases in HDL. That’s really hard to do. There aren’t a lot of medicines that can really affect the ‘good’ cholesterol."
‘Unique ability’ of gastric bypass
The study did not examine the relationship between telomeres and other kinds of surgical interventions for weight loss, but Dr. Morton said future studies on bariatric procedures such as the sleeve gastrectomy need to be conducted before they can be equated with bypass.
"Gastric bypass has a unique affect on inflammation that is independent of the other operations," said Dr. Morton, referring to data he presented earlier this year at the American College of Surgeons annual meeting, discussing the relationship between bypass and diabetes. "We have shown that C-reactive protein decreases more with gastric bypass than with other operations."
That of all the surgical interventions, gastric bypass has the greatest impact on diabetes, independent of weight loss, points to future research on inflammation, said Dr. Morton. "People are starting to think that type 2 diabetes is not just a burned-out pancreas, but that a lot of inflammation is involved."
Calling bariatric surgery a "platform for investigation" that can help [us] understand the connection between inflammation and the processes of disease in the general population, not just those with obesity, Dr. Morton said, "I think the future will elucidate some of those processes, and will come up with different interventions such as drugs."
Dr. Morton said he did not have any relevant financial disclosures.
ATLANTA – Gastric bypass was associated with the lengthening of telomeres, an indication that surgical weight loss may reverse aging in obese patients.
The most significant changes in telomere length occurred in patients with biomarkers indicative of higher levels of preoperative inflammation and cholesterol, according to findings presented by bariatric surgeon John Morton at this year’s Obesity Week.
"Telomeres are unique markers for aging and are linked to chronic diseases and things like smoking and depression," Dr. Morton said in an interview. "There are a lot of things that can potentially affect telomeres, but there aren’t a lot of things that can affect them in a positive sense."
Dr. Morton and his colleagues at Stanford (Calif.) University measured the baseline telomere length, weight, C-reactive protein (CRP) levels, cholesterol levels, and fasting insulin levels in 51 gastric bypass surgery patients (77% female, average age 49 years). The group’s mean body mass index was 44 kg/m2. The measurements were taken again at 3, 6, and 12 months. Telomere length was determined using quantitative polymerase chain reaction testing.
In all patients, excess body weight loss at 12 months averaged 71%; CRP levels, indicative of inflammation, dropped an average of more than 60%. Fasting insulin levels decreased from 24 uIU/mL at baseline to 6 uIU/mL when measured 1 year after surgery. These results were consistent with those of previous studies, but this study was the first to correlate such changes with the body’s biomarkers for aging, telomeres, Dr. Morton said.
Unexpected results
Telomere length did not change significantly across the cohort, but when analyzed according to CRP and LDL levels, significant changes in telomere length were found in patients whose levels of both were higher at baseline (P = .0387 and P = .005). In those whose baseline CRP was high, there also was a significant positive correlation between telomere lengthening and weight loss (P = .0498) and increases in HDL cholesterol level (P = .0176).
The results were somewhat unexpected. "The thing that surprised me the most was that if there were going to be changes, then they should be across the board," said Dr. Morton. "But where it really made a difference was in those who had [high levels of markers of] inflammation. It was a pretty specific result in a pretty specific population."
At least one other longitudinal study has shown the impact of nonsurgical intervention, namely a change in diet, on the length of telomeres (PLoS One 2013;8:e62781[doi:10.1371/journal.pone.0062781]), but Dr. Morton said the study, which emphasized eating less red meat and more fish, fresh vegetables, and olive oil did not demonstrate results that were notably different from his findings.
"One thing that study’s diet, the Mediterranean Diet, is known to do is to raise HDL," said Dr. Morton. "In our study we also saw a correlation between telomere lengthening and increases in HDL. That’s really hard to do. There aren’t a lot of medicines that can really affect the ‘good’ cholesterol."
‘Unique ability’ of gastric bypass
The study did not examine the relationship between telomeres and other kinds of surgical interventions for weight loss, but Dr. Morton said future studies on bariatric procedures such as the sleeve gastrectomy need to be conducted before they can be equated with bypass.
"Gastric bypass has a unique affect on inflammation that is independent of the other operations," said Dr. Morton, referring to data he presented earlier this year at the American College of Surgeons annual meeting, discussing the relationship between bypass and diabetes. "We have shown that C-reactive protein decreases more with gastric bypass than with other operations."
That of all the surgical interventions, gastric bypass has the greatest impact on diabetes, independent of weight loss, points to future research on inflammation, said Dr. Morton. "People are starting to think that type 2 diabetes is not just a burned-out pancreas, but that a lot of inflammation is involved."
Calling bariatric surgery a "platform for investigation" that can help [us] understand the connection between inflammation and the processes of disease in the general population, not just those with obesity, Dr. Morton said, "I think the future will elucidate some of those processes, and will come up with different interventions such as drugs."
Dr. Morton said he did not have any relevant financial disclosures.
ATLANTA – Gastric bypass was associated with the lengthening of telomeres, an indication that surgical weight loss may reverse aging in obese patients.
The most significant changes in telomere length occurred in patients with biomarkers indicative of higher levels of preoperative inflammation and cholesterol, according to findings presented by bariatric surgeon John Morton at this year’s Obesity Week.
"Telomeres are unique markers for aging and are linked to chronic diseases and things like smoking and depression," Dr. Morton said in an interview. "There are a lot of things that can potentially affect telomeres, but there aren’t a lot of things that can affect them in a positive sense."
Dr. Morton and his colleagues at Stanford (Calif.) University measured the baseline telomere length, weight, C-reactive protein (CRP) levels, cholesterol levels, and fasting insulin levels in 51 gastric bypass surgery patients (77% female, average age 49 years). The group’s mean body mass index was 44 kg/m2. The measurements were taken again at 3, 6, and 12 months. Telomere length was determined using quantitative polymerase chain reaction testing.
In all patients, excess body weight loss at 12 months averaged 71%; CRP levels, indicative of inflammation, dropped an average of more than 60%. Fasting insulin levels decreased from 24 uIU/mL at baseline to 6 uIU/mL when measured 1 year after surgery. These results were consistent with those of previous studies, but this study was the first to correlate such changes with the body’s biomarkers for aging, telomeres, Dr. Morton said.
Unexpected results
Telomere length did not change significantly across the cohort, but when analyzed according to CRP and LDL levels, significant changes in telomere length were found in patients whose levels of both were higher at baseline (P = .0387 and P = .005). In those whose baseline CRP was high, there also was a significant positive correlation between telomere lengthening and weight loss (P = .0498) and increases in HDL cholesterol level (P = .0176).
The results were somewhat unexpected. "The thing that surprised me the most was that if there were going to be changes, then they should be across the board," said Dr. Morton. "But where it really made a difference was in those who had [high levels of markers of] inflammation. It was a pretty specific result in a pretty specific population."
At least one other longitudinal study has shown the impact of nonsurgical intervention, namely a change in diet, on the length of telomeres (PLoS One 2013;8:e62781[doi:10.1371/journal.pone.0062781]), but Dr. Morton said the study, which emphasized eating less red meat and more fish, fresh vegetables, and olive oil did not demonstrate results that were notably different from his findings.
"One thing that study’s diet, the Mediterranean Diet, is known to do is to raise HDL," said Dr. Morton. "In our study we also saw a correlation between telomere lengthening and increases in HDL. That’s really hard to do. There aren’t a lot of medicines that can really affect the ‘good’ cholesterol."
‘Unique ability’ of gastric bypass
The study did not examine the relationship between telomeres and other kinds of surgical interventions for weight loss, but Dr. Morton said future studies on bariatric procedures such as the sleeve gastrectomy need to be conducted before they can be equated with bypass.
"Gastric bypass has a unique affect on inflammation that is independent of the other operations," said Dr. Morton, referring to data he presented earlier this year at the American College of Surgeons annual meeting, discussing the relationship between bypass and diabetes. "We have shown that C-reactive protein decreases more with gastric bypass than with other operations."
That of all the surgical interventions, gastric bypass has the greatest impact on diabetes, independent of weight loss, points to future research on inflammation, said Dr. Morton. "People are starting to think that type 2 diabetes is not just a burned-out pancreas, but that a lot of inflammation is involved."
Calling bariatric surgery a "platform for investigation" that can help [us] understand the connection between inflammation and the processes of disease in the general population, not just those with obesity, Dr. Morton said, "I think the future will elucidate some of those processes, and will come up with different interventions such as drugs."
Dr. Morton said he did not have any relevant financial disclosures.
AT OBESITY WEEK
Major finding: Significant increases in telomere length were observed after gastric bypass in individuals with high baseline CRP or LDL cholesterol levels (P = .0387 and P = .005, respectively); weight loss and increased levels of HDL cholesterol were positively correlated with telomere length in patients with high baseline CRP (P = .0498 and P = .0176).
Data source: A prospective study of 51 gastric bypass patients (77% female) whose telomere lengths, LDL, and CRP levels were measured at baseline and at 3,6, and 12 months.
Disclosures: Dr. Morton said he did not have any relevant financial disclosures.
Ready or not? Most ICUs not as prepared for disaster as they think
CHICAGO – When Superstorm Sandy was done barreling across New York City and the surrounding coast 14 months ago, flooding streets and knocking out power to millions, Dr. Laura Evans, director of the medical intensive care unit at Bellevue Hospital along the East River in Manhattan, emerged weary and wiser.
At one point, the ICU faced the real possibility of having just a handful of working power outlets to serve dozens of patients, and the number of crucial decisions to be made rose along with the water level. "Prior to the storm, disaster preparedness was not a core interest of mine, and it’s something I hope never to repeat," Dr. Evans told attendees at the annual meeting of the American College of Chest Physicians.
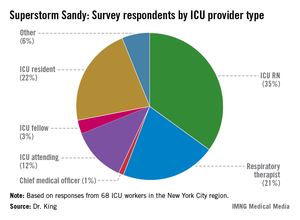
In a recent survey, ICU practitioners who endured havoc caused by Sandy in the New York City region reported having had little to no training in emergency evacuation care. "When I look at these data, I think there is a mismatch in terms of our self-perception of readiness compared to what patients actually require in an evacuation. It’s in stark contrast to the checklist we use every single day to put in a central venous catheter," said Dr. Mary Alice King, who presented her research as a copanelist with Dr. Evans. Dr. King is medical director of the pediatric trauma ICU at Harborview Medical Center in Seattle.
Contingency for loss of power
The nation’s oldest public hospital, Bellevue is adjacent to New York’s tidal East River. The river’s high tide the evening of Oct. 29, 2012, coincided with the arrival of the storm’s surge, and within minutes the hospital’s basement was inundated with 10 million gallons of seawater. And then the main power went out, taking with it the use of 32 elevators, the entire voice-over-Internet-protocol phone system, and the electronic medical records system, Dr. Evans said. The flood also knocked out the hospital’s ability to connect to its Internet servers. "We had very impaired means of communication," Dr. Evans said.
Survey data presented by Dr. King underscored that loss of power affects ICU functions in virtually all ways. The number one tool Dr. King’s survey respondents said they’d depended on most during their disaster response was their flashlights (24%); meanwhile, the top two items the respondents said they wished they’d had on hand were reliable phones, since, as at Bellevue, many of their phones were powered by voice-over-Internet protocols which, for most, went down with power outages; and backup electricity sources such as generators.
Leadership plan
Of the 68 survey respondents, 34% of whom were in evacuation leadership roles, Dr. King said only 23% admitted to having felt ill prepared to manage the pressure and details necessary to safely evacuate their patients. "As nonemergency department hospital providers, we receive little to no training on how to evacuate patients," said Dr. King.
In Bellevue’s case, Dr. Evans said that there was a leadership contingency already in place because of the hospital’s having been prepared the year before, when Hurricane Irene muscled its way up the Northeast’s Atlantic coast, also causing flooding and wind damage, though on a far smaller scare. "We had an ad hoc committee," said Dr. Evans. "Although we didn’t know exactly who would be on it because we didn’t know who would be there during the storm, we knew we would have medical, nursing, and ethical leaders to make resource allocation decisions." Most important about the leadership committee’s makeup, she said, was that ultimately, "none of us were directly involved in patient care, so none of us had the responsibility for being advocates. We wanted the attending physicians to be able to advocate for their patients."
The committee discerned that if backup generators failed, the ICU would have only six power outlets to depend on for its almost 60 patients. "The question was, whom would they be allocated for out of the 56 patients?
"Our responsibility was to make the wisest decisions about allocating a scarce resource," Dr. Evans said.
Practice the plan
Dry runs matter. "Forty-seven percent of survey respondents said that patient triage criteria were determined at the time of [the storm]," and a third of those surveyed said they weren’t aware of any triage criteria, Dr. King said.
And once plans are made, "it’s important to drill them," emphasized Dr. King’s copresenter Dr. Colin Grissom, associate medical director of the shock trauma ICU at Intermountain Medical Center, Murray, Utah. Superstorm Sandy, for all its havoc, came with some notice – the weather forecast. However, he pointed out that typically disasters happen without warning: "More than half of all hospital evacuations occur as a result of an internal event such as a fire or an intruder."
Also important to consider, said Dr. King, is that neonatal and pediatric ICUs have different evacuation needs from adult ones. "Regions should consider stockpiling neonatal transport ventilators and circuits," she said. "They should also consider designating pediatric disaster receiving hospitals, similar to burn disaster receiving hospitals."
Ethical considerations
At Bellevue, Dr. Evans said the hospital’s leadership planned patient triage according to influenza pandemic guidelines issued by the provincial government of Ontario, Canada, and the New York State Taskforce on Life and the Law guidelines for ventilator allocation during a public health disaster.
"We knew that if the disaster went very badly, we would be met with much criticism," said Dr. Evans, who joked that she was up nights worried about seeing her name skewered in local headlines: "I kept wondering, ‘What rhymes with Evans?’ "
Using the two sets of guidelines, both heavily oriented toward allocating ventilators, said Dr. Evans, "we did what we thought was ethical and fair. We made the best decisions we could."
The Ontario guidelines, she said, are predicated on Sequential Organ Failure Assessment (SOFA) scores. Just as the ad hoc committee determined that of the 56 patients in the census, there were "far more folks in the red (highest priority) and yellow (immediate priority) group than we had power outlets," the group received word that the protective housing around the generator fuel pumps had failed, and total loss of power was anticipated in 2 hours.
The committee reconfigured and, among other contingencies, began assigning coverage of two providers each to the bedside of every ventilated patient, and preparing nurses to count drops per minute of continuous medication.
The ‘bucket brigade’
Although the intensivists who’d participated in Superstorm Sandy evacuations said they felt most frustrated by the lack of communication during the event, 57% said that teamwork had been essential to the success of the evacuations.
"We work as teams in our units. That is something I think we bring as a real strength to ICU evacuations," said Dr. King.
And so it was at Bellevue.
"Due to the heroics of a lot of staff and volunteers, we did not have to execute this plan," said Dr. Evans. Instead, the "Bellevue bucket brigade," using 5-gallon jugs, formed a relay team stretching from the ground floor outside where the fuel tanks were, up to the 13th, where the backup generators were located. "The fuel tank up on the 13th floor was only accessible by stepladder, so someone had to climb up there and pour the fuel through a funnel," said Dr. Evans. "But because of this, we never lost backup power, and we successfully evacuated our hospital without complications to our patients."
Individualized plan key to success
While leadership and communication were essential, said Dr. Evans, she concluded that thinking through how existing guidelines can help was also key, but did not go far enough. "Unfortunately, no document can provide for all contingencies. Complete reliance on any [guidelines] is not good. You have to think about how you would individualize things to your own facility."
The survey was sponsored by the ACCP and conducted by Dr. King as part of her role on the ACCP’s mass critical care task force evacuation panel, which will issue a consensus on the topic sometime in early 2014.
Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Ten keys to ICU evacuation plan
When not under immediate threat
1) Create transport and other agreements with other facilities in region, including triage criteria.
2) Detail ICU evacuation plan, including vertical evacuation plan; simulate so all parties are familiar with their role, including those involved in patient transport.
3) Designate critical care leadership.
During imminent threat
4) Request assistance from regional facilities and appropriate agencies.
5) Ensure power and transportation resources are operable and in place.
6) Prioritize patients for evacuation.
During evacuation
7) Triage patients.
8) Include all patient information with patient.
9) Transport patients.
10) Track patients and all equipment.
Source: Dr. Colin Grissom
*This story has been updated 11/26/13
Dr. W. Michael Alberts, FCCP, comments: To paraphrase an old saying about insurance, "disaster preparedness is not needed until it is." Those health care facilities that have a clear documented plan and have drilled on the specifics are very pleased that they devoted time and effort when disaster strikes. While – knock on wood – the Moffitt Cancer Center here in Tampa has not needed our "Disaster Management Plan" (or as we in Florida say "Hurricane Management Plan") this year, it is only a matter of time and we’ll be ready when the need arises.
We urge you to review your plan before you need it.
Dr. W. Michael Alberts is chief medical officer, Moffitt Cancer Center, and professor of oncology and medicine at the University of South Florida, Tampa.
Dr. W. Michael Alberts, FCCP, comments: To paraphrase an old saying about insurance, "disaster preparedness is not needed until it is." Those health care facilities that have a clear documented plan and have drilled on the specifics are very pleased that they devoted time and effort when disaster strikes. While – knock on wood – the Moffitt Cancer Center here in Tampa has not needed our "Disaster Management Plan" (or as we in Florida say "Hurricane Management Plan") this year, it is only a matter of time and we’ll be ready when the need arises.
We urge you to review your plan before you need it.
Dr. W. Michael Alberts is chief medical officer, Moffitt Cancer Center, and professor of oncology and medicine at the University of South Florida, Tampa.
Dr. W. Michael Alberts, FCCP, comments: To paraphrase an old saying about insurance, "disaster preparedness is not needed until it is." Those health care facilities that have a clear documented plan and have drilled on the specifics are very pleased that they devoted time and effort when disaster strikes. While – knock on wood – the Moffitt Cancer Center here in Tampa has not needed our "Disaster Management Plan" (or as we in Florida say "Hurricane Management Plan") this year, it is only a matter of time and we’ll be ready when the need arises.
We urge you to review your plan before you need it.
Dr. W. Michael Alberts is chief medical officer, Moffitt Cancer Center, and professor of oncology and medicine at the University of South Florida, Tampa.
CHICAGO – When Superstorm Sandy was done barreling across New York City and the surrounding coast 14 months ago, flooding streets and knocking out power to millions, Dr. Laura Evans, director of the medical intensive care unit at Bellevue Hospital along the East River in Manhattan, emerged weary and wiser.
At one point, the ICU faced the real possibility of having just a handful of working power outlets to serve dozens of patients, and the number of crucial decisions to be made rose along with the water level. "Prior to the storm, disaster preparedness was not a core interest of mine, and it’s something I hope never to repeat," Dr. Evans told attendees at the annual meeting of the American College of Chest Physicians.
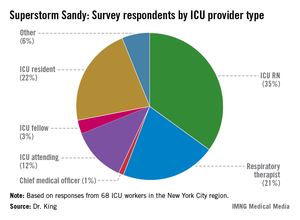
In a recent survey, ICU practitioners who endured havoc caused by Sandy in the New York City region reported having had little to no training in emergency evacuation care. "When I look at these data, I think there is a mismatch in terms of our self-perception of readiness compared to what patients actually require in an evacuation. It’s in stark contrast to the checklist we use every single day to put in a central venous catheter," said Dr. Mary Alice King, who presented her research as a copanelist with Dr. Evans. Dr. King is medical director of the pediatric trauma ICU at Harborview Medical Center in Seattle.
Contingency for loss of power
The nation’s oldest public hospital, Bellevue is adjacent to New York’s tidal East River. The river’s high tide the evening of Oct. 29, 2012, coincided with the arrival of the storm’s surge, and within minutes the hospital’s basement was inundated with 10 million gallons of seawater. And then the main power went out, taking with it the use of 32 elevators, the entire voice-over-Internet-protocol phone system, and the electronic medical records system, Dr. Evans said. The flood also knocked out the hospital’s ability to connect to its Internet servers. "We had very impaired means of communication," Dr. Evans said.
Survey data presented by Dr. King underscored that loss of power affects ICU functions in virtually all ways. The number one tool Dr. King’s survey respondents said they’d depended on most during their disaster response was their flashlights (24%); meanwhile, the top two items the respondents said they wished they’d had on hand were reliable phones, since, as at Bellevue, many of their phones were powered by voice-over-Internet protocols which, for most, went down with power outages; and backup electricity sources such as generators.
Leadership plan
Of the 68 survey respondents, 34% of whom were in evacuation leadership roles, Dr. King said only 23% admitted to having felt ill prepared to manage the pressure and details necessary to safely evacuate their patients. "As nonemergency department hospital providers, we receive little to no training on how to evacuate patients," said Dr. King.
In Bellevue’s case, Dr. Evans said that there was a leadership contingency already in place because of the hospital’s having been prepared the year before, when Hurricane Irene muscled its way up the Northeast’s Atlantic coast, also causing flooding and wind damage, though on a far smaller scare. "We had an ad hoc committee," said Dr. Evans. "Although we didn’t know exactly who would be on it because we didn’t know who would be there during the storm, we knew we would have medical, nursing, and ethical leaders to make resource allocation decisions." Most important about the leadership committee’s makeup, she said, was that ultimately, "none of us were directly involved in patient care, so none of us had the responsibility for being advocates. We wanted the attending physicians to be able to advocate for their patients."
The committee discerned that if backup generators failed, the ICU would have only six power outlets to depend on for its almost 60 patients. "The question was, whom would they be allocated for out of the 56 patients?
"Our responsibility was to make the wisest decisions about allocating a scarce resource," Dr. Evans said.
Practice the plan
Dry runs matter. "Forty-seven percent of survey respondents said that patient triage criteria were determined at the time of [the storm]," and a third of those surveyed said they weren’t aware of any triage criteria, Dr. King said.
And once plans are made, "it’s important to drill them," emphasized Dr. King’s copresenter Dr. Colin Grissom, associate medical director of the shock trauma ICU at Intermountain Medical Center, Murray, Utah. Superstorm Sandy, for all its havoc, came with some notice – the weather forecast. However, he pointed out that typically disasters happen without warning: "More than half of all hospital evacuations occur as a result of an internal event such as a fire or an intruder."
Also important to consider, said Dr. King, is that neonatal and pediatric ICUs have different evacuation needs from adult ones. "Regions should consider stockpiling neonatal transport ventilators and circuits," she said. "They should also consider designating pediatric disaster receiving hospitals, similar to burn disaster receiving hospitals."
Ethical considerations
At Bellevue, Dr. Evans said the hospital’s leadership planned patient triage according to influenza pandemic guidelines issued by the provincial government of Ontario, Canada, and the New York State Taskforce on Life and the Law guidelines for ventilator allocation during a public health disaster.
"We knew that if the disaster went very badly, we would be met with much criticism," said Dr. Evans, who joked that she was up nights worried about seeing her name skewered in local headlines: "I kept wondering, ‘What rhymes with Evans?’ "
Using the two sets of guidelines, both heavily oriented toward allocating ventilators, said Dr. Evans, "we did what we thought was ethical and fair. We made the best decisions we could."
The Ontario guidelines, she said, are predicated on Sequential Organ Failure Assessment (SOFA) scores. Just as the ad hoc committee determined that of the 56 patients in the census, there were "far more folks in the red (highest priority) and yellow (immediate priority) group than we had power outlets," the group received word that the protective housing around the generator fuel pumps had failed, and total loss of power was anticipated in 2 hours.
The committee reconfigured and, among other contingencies, began assigning coverage of two providers each to the bedside of every ventilated patient, and preparing nurses to count drops per minute of continuous medication.
The ‘bucket brigade’
Although the intensivists who’d participated in Superstorm Sandy evacuations said they felt most frustrated by the lack of communication during the event, 57% said that teamwork had been essential to the success of the evacuations.
"We work as teams in our units. That is something I think we bring as a real strength to ICU evacuations," said Dr. King.
And so it was at Bellevue.
"Due to the heroics of a lot of staff and volunteers, we did not have to execute this plan," said Dr. Evans. Instead, the "Bellevue bucket brigade," using 5-gallon jugs, formed a relay team stretching from the ground floor outside where the fuel tanks were, up to the 13th, where the backup generators were located. "The fuel tank up on the 13th floor was only accessible by stepladder, so someone had to climb up there and pour the fuel through a funnel," said Dr. Evans. "But because of this, we never lost backup power, and we successfully evacuated our hospital without complications to our patients."
Individualized plan key to success
While leadership and communication were essential, said Dr. Evans, she concluded that thinking through how existing guidelines can help was also key, but did not go far enough. "Unfortunately, no document can provide for all contingencies. Complete reliance on any [guidelines] is not good. You have to think about how you would individualize things to your own facility."
The survey was sponsored by the ACCP and conducted by Dr. King as part of her role on the ACCP’s mass critical care task force evacuation panel, which will issue a consensus on the topic sometime in early 2014.
Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Ten keys to ICU evacuation plan
When not under immediate threat
1) Create transport and other agreements with other facilities in region, including triage criteria.
2) Detail ICU evacuation plan, including vertical evacuation plan; simulate so all parties are familiar with their role, including those involved in patient transport.
3) Designate critical care leadership.
During imminent threat
4) Request assistance from regional facilities and appropriate agencies.
5) Ensure power and transportation resources are operable and in place.
6) Prioritize patients for evacuation.
During evacuation
7) Triage patients.
8) Include all patient information with patient.
9) Transport patients.
10) Track patients and all equipment.
Source: Dr. Colin Grissom
*This story has been updated 11/26/13
CHICAGO – When Superstorm Sandy was done barreling across New York City and the surrounding coast 14 months ago, flooding streets and knocking out power to millions, Dr. Laura Evans, director of the medical intensive care unit at Bellevue Hospital along the East River in Manhattan, emerged weary and wiser.
At one point, the ICU faced the real possibility of having just a handful of working power outlets to serve dozens of patients, and the number of crucial decisions to be made rose along with the water level. "Prior to the storm, disaster preparedness was not a core interest of mine, and it’s something I hope never to repeat," Dr. Evans told attendees at the annual meeting of the American College of Chest Physicians.
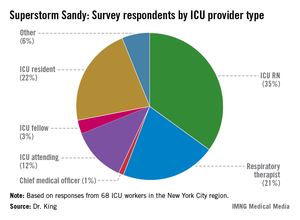
In a recent survey, ICU practitioners who endured havoc caused by Sandy in the New York City region reported having had little to no training in emergency evacuation care. "When I look at these data, I think there is a mismatch in terms of our self-perception of readiness compared to what patients actually require in an evacuation. It’s in stark contrast to the checklist we use every single day to put in a central venous catheter," said Dr. Mary Alice King, who presented her research as a copanelist with Dr. Evans. Dr. King is medical director of the pediatric trauma ICU at Harborview Medical Center in Seattle.
Contingency for loss of power
The nation’s oldest public hospital, Bellevue is adjacent to New York’s tidal East River. The river’s high tide the evening of Oct. 29, 2012, coincided with the arrival of the storm’s surge, and within minutes the hospital’s basement was inundated with 10 million gallons of seawater. And then the main power went out, taking with it the use of 32 elevators, the entire voice-over-Internet-protocol phone system, and the electronic medical records system, Dr. Evans said. The flood also knocked out the hospital’s ability to connect to its Internet servers. "We had very impaired means of communication," Dr. Evans said.
Survey data presented by Dr. King underscored that loss of power affects ICU functions in virtually all ways. The number one tool Dr. King’s survey respondents said they’d depended on most during their disaster response was their flashlights (24%); meanwhile, the top two items the respondents said they wished they’d had on hand were reliable phones, since, as at Bellevue, many of their phones were powered by voice-over-Internet protocols which, for most, went down with power outages; and backup electricity sources such as generators.
Leadership plan
Of the 68 survey respondents, 34% of whom were in evacuation leadership roles, Dr. King said only 23% admitted to having felt ill prepared to manage the pressure and details necessary to safely evacuate their patients. "As nonemergency department hospital providers, we receive little to no training on how to evacuate patients," said Dr. King.
In Bellevue’s case, Dr. Evans said that there was a leadership contingency already in place because of the hospital’s having been prepared the year before, when Hurricane Irene muscled its way up the Northeast’s Atlantic coast, also causing flooding and wind damage, though on a far smaller scare. "We had an ad hoc committee," said Dr. Evans. "Although we didn’t know exactly who would be on it because we didn’t know who would be there during the storm, we knew we would have medical, nursing, and ethical leaders to make resource allocation decisions." Most important about the leadership committee’s makeup, she said, was that ultimately, "none of us were directly involved in patient care, so none of us had the responsibility for being advocates. We wanted the attending physicians to be able to advocate for their patients."
The committee discerned that if backup generators failed, the ICU would have only six power outlets to depend on for its almost 60 patients. "The question was, whom would they be allocated for out of the 56 patients?
"Our responsibility was to make the wisest decisions about allocating a scarce resource," Dr. Evans said.
Practice the plan
Dry runs matter. "Forty-seven percent of survey respondents said that patient triage criteria were determined at the time of [the storm]," and a third of those surveyed said they weren’t aware of any triage criteria, Dr. King said.
And once plans are made, "it’s important to drill them," emphasized Dr. King’s copresenter Dr. Colin Grissom, associate medical director of the shock trauma ICU at Intermountain Medical Center, Murray, Utah. Superstorm Sandy, for all its havoc, came with some notice – the weather forecast. However, he pointed out that typically disasters happen without warning: "More than half of all hospital evacuations occur as a result of an internal event such as a fire or an intruder."
Also important to consider, said Dr. King, is that neonatal and pediatric ICUs have different evacuation needs from adult ones. "Regions should consider stockpiling neonatal transport ventilators and circuits," she said. "They should also consider designating pediatric disaster receiving hospitals, similar to burn disaster receiving hospitals."
Ethical considerations
At Bellevue, Dr. Evans said the hospital’s leadership planned patient triage according to influenza pandemic guidelines issued by the provincial government of Ontario, Canada, and the New York State Taskforce on Life and the Law guidelines for ventilator allocation during a public health disaster.
"We knew that if the disaster went very badly, we would be met with much criticism," said Dr. Evans, who joked that she was up nights worried about seeing her name skewered in local headlines: "I kept wondering, ‘What rhymes with Evans?’ "
Using the two sets of guidelines, both heavily oriented toward allocating ventilators, said Dr. Evans, "we did what we thought was ethical and fair. We made the best decisions we could."
The Ontario guidelines, she said, are predicated on Sequential Organ Failure Assessment (SOFA) scores. Just as the ad hoc committee determined that of the 56 patients in the census, there were "far more folks in the red (highest priority) and yellow (immediate priority) group than we had power outlets," the group received word that the protective housing around the generator fuel pumps had failed, and total loss of power was anticipated in 2 hours.
The committee reconfigured and, among other contingencies, began assigning coverage of two providers each to the bedside of every ventilated patient, and preparing nurses to count drops per minute of continuous medication.
The ‘bucket brigade’
Although the intensivists who’d participated in Superstorm Sandy evacuations said they felt most frustrated by the lack of communication during the event, 57% said that teamwork had been essential to the success of the evacuations.
"We work as teams in our units. That is something I think we bring as a real strength to ICU evacuations," said Dr. King.
And so it was at Bellevue.
"Due to the heroics of a lot of staff and volunteers, we did not have to execute this plan," said Dr. Evans. Instead, the "Bellevue bucket brigade," using 5-gallon jugs, formed a relay team stretching from the ground floor outside where the fuel tanks were, up to the 13th, where the backup generators were located. "The fuel tank up on the 13th floor was only accessible by stepladder, so someone had to climb up there and pour the fuel through a funnel," said Dr. Evans. "But because of this, we never lost backup power, and we successfully evacuated our hospital without complications to our patients."
Individualized plan key to success
While leadership and communication were essential, said Dr. Evans, she concluded that thinking through how existing guidelines can help was also key, but did not go far enough. "Unfortunately, no document can provide for all contingencies. Complete reliance on any [guidelines] is not good. You have to think about how you would individualize things to your own facility."
The survey was sponsored by the ACCP and conducted by Dr. King as part of her role on the ACCP’s mass critical care task force evacuation panel, which will issue a consensus on the topic sometime in early 2014.
Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.
Ten keys to ICU evacuation plan
When not under immediate threat
1) Create transport and other agreements with other facilities in region, including triage criteria.
2) Detail ICU evacuation plan, including vertical evacuation plan; simulate so all parties are familiar with their role, including those involved in patient transport.
3) Designate critical care leadership.
During imminent threat
4) Request assistance from regional facilities and appropriate agencies.
5) Ensure power and transportation resources are operable and in place.
6) Prioritize patients for evacuation.
During evacuation
7) Triage patients.
8) Include all patient information with patient.
9) Transport patients.
10) Track patients and all equipment.
Source: Dr. Colin Grissom
*This story has been updated 11/26/13
EXPERT ANALYSIS FROM CHEST 2013
Major finding: Although 78% of ICU staff had never performed a vertical ICU evacuation drill, only 23% admitted to feeling "inadequately trained" during Superstorm Sandy evacuations.
Data source: Survey of 68 ICU workers in the New York City region, all of whom worked through Superstorm Sandy.
Disclosures: Dr. Evans, Dr. King, and Dr. Grissom reported no relevant financial disclosures.