User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Aged black garlic supplement may help lower BP
After 6 weeks, consumption of ABG with a high concentration of s-allyl-L-cystine (SAC) was associated with a nearly 6-mm Hg reduction in DBP in men. Other cardiovascular disease (CVD) risk factors were not significantly affected.
“The observed reduction in DBP by ABG extract was similar to the effects of dietary approaches, including the effects of the Dietary Approaches to Stop Hypertension(DASH) diet on BP,” say Rosa M. Valls, PhD, Universitat Rovira i Virgili, Reus, Spain, and colleagues.
“The potential beneficial effects of ABG may contribute to obtaining an optimal DBP” but were “better observed in men and in nonoptimal DBP populations,” they write in the study, published in Nutrients.
Pure SAC and aged garlics have shown healthy effects on multiple targets in in vitro and in vivo tests. However, previous studies in humans have not focused on ABG but rather on other types of aged garlic in patients with some type of CVD risk factor and suffered from methodologic or design weaknesses, the authors note.
To address this gap, Dr. Valls and colleagues randomly assigned 67 individuals with moderate hypercholesterolemia (defined as LDL levels of at least 115 mg/dL) to receive one ABG tablet (250 mg ABG extract/1.25 mg SAC) or placebo daily for 6 weeks. Following a 3-week washout, the groups were reversed and the new intervention continued for another 6 weeks.
Participants received dietary recommendations regarding CVD risk factors and had their dietary habits assessed through a 3-day food record at baseline and after 6 weeks during both treatments.
Individuals receiving lipid-lowering treatment or antihypertensives were excluded, as were those with a body mass index of 35 kg/m2 or higher, those with a fasting blood glucose of at least 126 mg/dL, or active smokers.
There were no differences in baseline characteristics between the two groups. The mean systolic and diastolic pressures at baseline were 124/75 mm Hg in the ABG group and 121/74 mm Hg in the placebo group. Their mean age was 53 years.
Adherence with the protocol was “high” at 96.5% in both groups, and no adverse effects were reported.
Reduced risk of death from stroke, ischemic heart disease
Although no significant differences between ABG and placebo were observed at 3 weeks, the decline in DBP after consumption of the ABG extract became significant at 6 weeks (mean change, –3.7 mm Hg vs. –0.10 mm Hg; P = .007).
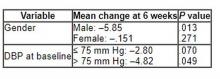
When stratified by sex and categories of DBP, the mean change in DBP after 6 weeks of ABG consumption was particularly prominent in men and in those with a baseline DBP of at least 75 mm Hg.
The 6-week change in systolic blood pressure with ABG and placebo was 1.32 mm Hg and 2.84 mm Hg, respectively (P = .694).
At week 6, total cholesterol levels showed a “quadratic decreasing trend” after ABG treatment (P = .047), but no other significant differences between groups were observed for lipid profile, apolipoproteins, or other outcomes of interest, including serum insulin, waist circumference, and body mass index.
The authors note that although systolic BP elevation “has a greater effect on outcomes, both systolic and diastolic hypertension independently influence the risk of adverse cardiovascular events, regardless of the definition of hypertension” and that the risk of death from ischemic heart disease and stroke doubles with every 10 mm Hg increase in DBP in people between the ages of 40 and 89 years.
“Thus, reducing DBP by 5 mm Hg results in a 40% lower risk of death from stroke and a 30% lower risk of death from ischemic heart disease or other vascular death,” they state.
Small study
Commenting for this news organization, Linda Van Horn, PhD, RDN, professor and chief of the department of preventive medicine’s nutrition division, Northwestern University, Chicago, said that for many years, garlic has been “reported to be an adjunct to the benefits of a healthy eating pattern, with inconclusive results.”
She noted that ABG is “literally aged for many months to years, and the resulting concentrate is found higher in many organosulfur compounds and phytochemicals that suggest enhanced response.”
Dr. Van Horn, a member of the American Heart Association’s Nutrition Committee, who was not involved with the study, continued: “The data suggest that ABG that is much more highly concentrated than fresh or processed garlic might be helpful in lowering BP in certain subgroups, in this case men with higher BP.”
However, she cautioned, “these results are limited in a small study, and ... potential other issues, such as sodium, potassium, or other nutrients known to be associated with blood pressure, were not reported, thereby raising questions about the exclusivity of the ABG over other accompanying dietary factors.”
The study was funded by the Center for the Development of Industrial Technology of the Spanish Ministry of Science and Innovation. Two authors are employees of Pharmactive Biotech Products, SL (Madrid), which manufactured the ABG product, but neither played a role in any result or conclusion. The other authors and Dr. Van Horn report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
After 6 weeks, consumption of ABG with a high concentration of s-allyl-L-cystine (SAC) was associated with a nearly 6-mm Hg reduction in DBP in men. Other cardiovascular disease (CVD) risk factors were not significantly affected.
“The observed reduction in DBP by ABG extract was similar to the effects of dietary approaches, including the effects of the Dietary Approaches to Stop Hypertension(DASH) diet on BP,” say Rosa M. Valls, PhD, Universitat Rovira i Virgili, Reus, Spain, and colleagues.
“The potential beneficial effects of ABG may contribute to obtaining an optimal DBP” but were “better observed in men and in nonoptimal DBP populations,” they write in the study, published in Nutrients.
Pure SAC and aged garlics have shown healthy effects on multiple targets in in vitro and in vivo tests. However, previous studies in humans have not focused on ABG but rather on other types of aged garlic in patients with some type of CVD risk factor and suffered from methodologic or design weaknesses, the authors note.
To address this gap, Dr. Valls and colleagues randomly assigned 67 individuals with moderate hypercholesterolemia (defined as LDL levels of at least 115 mg/dL) to receive one ABG tablet (250 mg ABG extract/1.25 mg SAC) or placebo daily for 6 weeks. Following a 3-week washout, the groups were reversed and the new intervention continued for another 6 weeks.
Participants received dietary recommendations regarding CVD risk factors and had their dietary habits assessed through a 3-day food record at baseline and after 6 weeks during both treatments.
Individuals receiving lipid-lowering treatment or antihypertensives were excluded, as were those with a body mass index of 35 kg/m2 or higher, those with a fasting blood glucose of at least 126 mg/dL, or active smokers.
There were no differences in baseline characteristics between the two groups. The mean systolic and diastolic pressures at baseline were 124/75 mm Hg in the ABG group and 121/74 mm Hg in the placebo group. Their mean age was 53 years.
Adherence with the protocol was “high” at 96.5% in both groups, and no adverse effects were reported.
Reduced risk of death from stroke, ischemic heart disease
Although no significant differences between ABG and placebo were observed at 3 weeks, the decline in DBP after consumption of the ABG extract became significant at 6 weeks (mean change, –3.7 mm Hg vs. –0.10 mm Hg; P = .007).
When stratified by sex and categories of DBP, the mean change in DBP after 6 weeks of ABG consumption was particularly prominent in men and in those with a baseline DBP of at least 75 mm Hg.
The 6-week change in systolic blood pressure with ABG and placebo was 1.32 mm Hg and 2.84 mm Hg, respectively (P = .694).
At week 6, total cholesterol levels showed a “quadratic decreasing trend” after ABG treatment (P = .047), but no other significant differences between groups were observed for lipid profile, apolipoproteins, or other outcomes of interest, including serum insulin, waist circumference, and body mass index.
The authors note that although systolic BP elevation “has a greater effect on outcomes, both systolic and diastolic hypertension independently influence the risk of adverse cardiovascular events, regardless of the definition of hypertension” and that the risk of death from ischemic heart disease and stroke doubles with every 10 mm Hg increase in DBP in people between the ages of 40 and 89 years.
“Thus, reducing DBP by 5 mm Hg results in a 40% lower risk of death from stroke and a 30% lower risk of death from ischemic heart disease or other vascular death,” they state.
Small study
Commenting for this news organization, Linda Van Horn, PhD, RDN, professor and chief of the department of preventive medicine’s nutrition division, Northwestern University, Chicago, said that for many years, garlic has been “reported to be an adjunct to the benefits of a healthy eating pattern, with inconclusive results.”
She noted that ABG is “literally aged for many months to years, and the resulting concentrate is found higher in many organosulfur compounds and phytochemicals that suggest enhanced response.”
Dr. Van Horn, a member of the American Heart Association’s Nutrition Committee, who was not involved with the study, continued: “The data suggest that ABG that is much more highly concentrated than fresh or processed garlic might be helpful in lowering BP in certain subgroups, in this case men with higher BP.”
However, she cautioned, “these results are limited in a small study, and ... potential other issues, such as sodium, potassium, or other nutrients known to be associated with blood pressure, were not reported, thereby raising questions about the exclusivity of the ABG over other accompanying dietary factors.”
The study was funded by the Center for the Development of Industrial Technology of the Spanish Ministry of Science and Innovation. Two authors are employees of Pharmactive Biotech Products, SL (Madrid), which manufactured the ABG product, but neither played a role in any result or conclusion. The other authors and Dr. Van Horn report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
After 6 weeks, consumption of ABG with a high concentration of s-allyl-L-cystine (SAC) was associated with a nearly 6-mm Hg reduction in DBP in men. Other cardiovascular disease (CVD) risk factors were not significantly affected.
“The observed reduction in DBP by ABG extract was similar to the effects of dietary approaches, including the effects of the Dietary Approaches to Stop Hypertension(DASH) diet on BP,” say Rosa M. Valls, PhD, Universitat Rovira i Virgili, Reus, Spain, and colleagues.
“The potential beneficial effects of ABG may contribute to obtaining an optimal DBP” but were “better observed in men and in nonoptimal DBP populations,” they write in the study, published in Nutrients.
Pure SAC and aged garlics have shown healthy effects on multiple targets in in vitro and in vivo tests. However, previous studies in humans have not focused on ABG but rather on other types of aged garlic in patients with some type of CVD risk factor and suffered from methodologic or design weaknesses, the authors note.
To address this gap, Dr. Valls and colleagues randomly assigned 67 individuals with moderate hypercholesterolemia (defined as LDL levels of at least 115 mg/dL) to receive one ABG tablet (250 mg ABG extract/1.25 mg SAC) or placebo daily for 6 weeks. Following a 3-week washout, the groups were reversed and the new intervention continued for another 6 weeks.
Participants received dietary recommendations regarding CVD risk factors and had their dietary habits assessed through a 3-day food record at baseline and after 6 weeks during both treatments.
Individuals receiving lipid-lowering treatment or antihypertensives were excluded, as were those with a body mass index of 35 kg/m2 or higher, those with a fasting blood glucose of at least 126 mg/dL, or active smokers.
There were no differences in baseline characteristics between the two groups. The mean systolic and diastolic pressures at baseline were 124/75 mm Hg in the ABG group and 121/74 mm Hg in the placebo group. Their mean age was 53 years.
Adherence with the protocol was “high” at 96.5% in both groups, and no adverse effects were reported.
Reduced risk of death from stroke, ischemic heart disease
Although no significant differences between ABG and placebo were observed at 3 weeks, the decline in DBP after consumption of the ABG extract became significant at 6 weeks (mean change, –3.7 mm Hg vs. –0.10 mm Hg; P = .007).
When stratified by sex and categories of DBP, the mean change in DBP after 6 weeks of ABG consumption was particularly prominent in men and in those with a baseline DBP of at least 75 mm Hg.
The 6-week change in systolic blood pressure with ABG and placebo was 1.32 mm Hg and 2.84 mm Hg, respectively (P = .694).
At week 6, total cholesterol levels showed a “quadratic decreasing trend” after ABG treatment (P = .047), but no other significant differences between groups were observed for lipid profile, apolipoproteins, or other outcomes of interest, including serum insulin, waist circumference, and body mass index.
The authors note that although systolic BP elevation “has a greater effect on outcomes, both systolic and diastolic hypertension independently influence the risk of adverse cardiovascular events, regardless of the definition of hypertension” and that the risk of death from ischemic heart disease and stroke doubles with every 10 mm Hg increase in DBP in people between the ages of 40 and 89 years.
“Thus, reducing DBP by 5 mm Hg results in a 40% lower risk of death from stroke and a 30% lower risk of death from ischemic heart disease or other vascular death,” they state.
Small study
Commenting for this news organization, Linda Van Horn, PhD, RDN, professor and chief of the department of preventive medicine’s nutrition division, Northwestern University, Chicago, said that for many years, garlic has been “reported to be an adjunct to the benefits of a healthy eating pattern, with inconclusive results.”
She noted that ABG is “literally aged for many months to years, and the resulting concentrate is found higher in many organosulfur compounds and phytochemicals that suggest enhanced response.”
Dr. Van Horn, a member of the American Heart Association’s Nutrition Committee, who was not involved with the study, continued: “The data suggest that ABG that is much more highly concentrated than fresh or processed garlic might be helpful in lowering BP in certain subgroups, in this case men with higher BP.”
However, she cautioned, “these results are limited in a small study, and ... potential other issues, such as sodium, potassium, or other nutrients known to be associated with blood pressure, were not reported, thereby raising questions about the exclusivity of the ABG over other accompanying dietary factors.”
The study was funded by the Center for the Development of Industrial Technology of the Spanish Ministry of Science and Innovation. Two authors are employees of Pharmactive Biotech Products, SL (Madrid), which manufactured the ABG product, but neither played a role in any result or conclusion. The other authors and Dr. Van Horn report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NUTRIENTS
New York NPs join half of states with full practice authority
according to leading national nurse organizations.
New York joins 24 other states, the District of Columbia, and two U.S. territories that have adopted FPA legislation, as reported by the American Association of Nurse Practitioners (AANP). Like other states, New York has been under an emergency order during the pandemic that allowed NPs to practice to their full authority because of staffing shortages. That order was extended multiple times and was expected to expire this month, AANP reports.
“This has been in the making for nurse practitioners in New York since 2014, trying to get full practice authority,” Michelle Jones, RN, MSN, ANP-C, director at large for the New York State Nurses Association, said in an interview.
NPs who were allowed to practice independently during the pandemic campaigned for that provision to become permanent once the emergency order expired, she said. Ms. Jones explained that the FPA law expands the scope of practice and “removes unnecessary barriers,” namely an agreement with doctors to oversee NPs’ actions.
FPA gives NPs the authority to evaluate patients; diagnose, order, and interpret diagnostic tests; and initiate and manage treatments – including prescribing medications – without oversight by a doctor or state medical board, according to AANP.
Before the pandemic, New York NPs had “reduced” practice authority with those who had more than 3,600 hours of experience required to maintain a collaborative practice agreement with doctors and those with less experience maintaining a written agreement. The change gives full practice authority to those with more than 3,600 hours of experience, Stephen A. Ferrara, DNP, FNP-BC, AANP regional director, said in an interview.
Ferrara, who practices in New York, said the state is the largest to change to FPA. He said the state and others that have moved to FPA have determined that there “has been no lapse in quality care” during the emergency order period and that the regulatory barriers kept NPs from providing access to care.
Jones said that the law also will allow NPs to open private practices and serve underserved patients in areas that lack access to health care. “This is a step to improve access to health care and health equity of the New York population.”
It’s been a while since another state passed FPA legislation, Massachusetts in January 2021 and Delaware in August 2021, according to AANP.
Earlier this month, AANP released new data showing a 9% increase in NPs licensed to practice in the United States, rising from 325,000 in May 2021 to 355,000.
The New York legislation “will help New York attract and retain nurse practitioners and provide New Yorkers better access to quality care,” AANP President April Kapu, DNP, APRN, said in a statement.
A version of this article first appeared on Medscape.com.
according to leading national nurse organizations.
New York joins 24 other states, the District of Columbia, and two U.S. territories that have adopted FPA legislation, as reported by the American Association of Nurse Practitioners (AANP). Like other states, New York has been under an emergency order during the pandemic that allowed NPs to practice to their full authority because of staffing shortages. That order was extended multiple times and was expected to expire this month, AANP reports.
“This has been in the making for nurse practitioners in New York since 2014, trying to get full practice authority,” Michelle Jones, RN, MSN, ANP-C, director at large for the New York State Nurses Association, said in an interview.
NPs who were allowed to practice independently during the pandemic campaigned for that provision to become permanent once the emergency order expired, she said. Ms. Jones explained that the FPA law expands the scope of practice and “removes unnecessary barriers,” namely an agreement with doctors to oversee NPs’ actions.
FPA gives NPs the authority to evaluate patients; diagnose, order, and interpret diagnostic tests; and initiate and manage treatments – including prescribing medications – without oversight by a doctor or state medical board, according to AANP.
Before the pandemic, New York NPs had “reduced” practice authority with those who had more than 3,600 hours of experience required to maintain a collaborative practice agreement with doctors and those with less experience maintaining a written agreement. The change gives full practice authority to those with more than 3,600 hours of experience, Stephen A. Ferrara, DNP, FNP-BC, AANP regional director, said in an interview.
Ferrara, who practices in New York, said the state is the largest to change to FPA. He said the state and others that have moved to FPA have determined that there “has been no lapse in quality care” during the emergency order period and that the regulatory barriers kept NPs from providing access to care.
Jones said that the law also will allow NPs to open private practices and serve underserved patients in areas that lack access to health care. “This is a step to improve access to health care and health equity of the New York population.”
It’s been a while since another state passed FPA legislation, Massachusetts in January 2021 and Delaware in August 2021, according to AANP.
Earlier this month, AANP released new data showing a 9% increase in NPs licensed to practice in the United States, rising from 325,000 in May 2021 to 355,000.
The New York legislation “will help New York attract and retain nurse practitioners and provide New Yorkers better access to quality care,” AANP President April Kapu, DNP, APRN, said in a statement.
A version of this article first appeared on Medscape.com.
according to leading national nurse organizations.
New York joins 24 other states, the District of Columbia, and two U.S. territories that have adopted FPA legislation, as reported by the American Association of Nurse Practitioners (AANP). Like other states, New York has been under an emergency order during the pandemic that allowed NPs to practice to their full authority because of staffing shortages. That order was extended multiple times and was expected to expire this month, AANP reports.
“This has been in the making for nurse practitioners in New York since 2014, trying to get full practice authority,” Michelle Jones, RN, MSN, ANP-C, director at large for the New York State Nurses Association, said in an interview.
NPs who were allowed to practice independently during the pandemic campaigned for that provision to become permanent once the emergency order expired, she said. Ms. Jones explained that the FPA law expands the scope of practice and “removes unnecessary barriers,” namely an agreement with doctors to oversee NPs’ actions.
FPA gives NPs the authority to evaluate patients; diagnose, order, and interpret diagnostic tests; and initiate and manage treatments – including prescribing medications – without oversight by a doctor or state medical board, according to AANP.
Before the pandemic, New York NPs had “reduced” practice authority with those who had more than 3,600 hours of experience required to maintain a collaborative practice agreement with doctors and those with less experience maintaining a written agreement. The change gives full practice authority to those with more than 3,600 hours of experience, Stephen A. Ferrara, DNP, FNP-BC, AANP regional director, said in an interview.
Ferrara, who practices in New York, said the state is the largest to change to FPA. He said the state and others that have moved to FPA have determined that there “has been no lapse in quality care” during the emergency order period and that the regulatory barriers kept NPs from providing access to care.
Jones said that the law also will allow NPs to open private practices and serve underserved patients in areas that lack access to health care. “This is a step to improve access to health care and health equity of the New York population.”
It’s been a while since another state passed FPA legislation, Massachusetts in January 2021 and Delaware in August 2021, according to AANP.
Earlier this month, AANP released new data showing a 9% increase in NPs licensed to practice in the United States, rising from 325,000 in May 2021 to 355,000.
The New York legislation “will help New York attract and retain nurse practitioners and provide New Yorkers better access to quality care,” AANP President April Kapu, DNP, APRN, said in a statement.
A version of this article first appeared on Medscape.com.
More medical schools build training in transgender care
Klay Noto wants to be the kind of doctor he never had when he began to question his gender identity.
A second-year student at Tulane University in New Orleans, he wants to listen compassionately to patients’ concerns and recognize the hurt when they question who they are. He will be the kind of doctor who knows that a breast exam can be traumatizing if someone has been breast binding or that instructing a patient to take everything off and put on a gown can be triggering for someone with gender dysphoria.
Being in the room for hard conversations is part of why he pursued med school. “There aren’t many LGBT people in medicine and as I started to understand all the dynamics that go into it, I started to see that I could do it and I could be that different kind of doctor,” he told this news organization.
Mr. Noto, who transitioned after college, wants to see more transgender people like himself teaching gender medicine, and for all medical students to be trained in what it means to be transgender and how to give compassionate and comprehensive care to all patients.
Gains have been made in providing curriculum in transgender care that trains medical students in such concepts as how to approach gender identity with sensitivity and how to manage hormone therapy and surgery for transitioning patients who request that, according to those interviewed for this story.
But they agree there’s a long way to go to having widespread medical school integration of the health care needs of about 1.4 million transgender people in the United States.
According to the Association of American Medical Colleges (AAMC) Curriculum Inventory data collected from 131 U.S. medical schools, more than 65% offered some form of transgender-related education in 2018, and more than 80% of those provided such curriculum in required courses.
Lack of transgender, nonbinary faculty
Jason Klein, MD, is a pediatric endocrinologist and medical director of the Transgender Youth Health Program at New York (N.Y.) University.
He said in an interview that the number of programs nationally that have gender medicine as a structured part of their curriculum has increased over the last 5-10 years, but that education is not standardized from program to program.
The program at NYU includes lecture-style learning, case presentations, real-world conversations with people in the community, group discussions, and patient care, Dr. Klein said. There are formal lectures as part of adolescent medicine where students learn the differences between gender and sexual identity, and education on medical treatment of transgender and nonbinary adolescents, starting with puberty blockers and moving into affirming hormones.
Doctors also learn to know their limits and decide when to refer patients to a specialist.
“The focus is really about empathic and supportive care,” said Dr. Klein, assistant professor in the department of pediatrics at Hassenfeld Children’s Hospital at NYU Langone Health. “It’s about communication and understanding and the language we use and how to deliver affirming care in a health care setting in general.”
Imagine the potential stressors, he said, of a transgender person entering a typical health care setting. The electronic health record may only have room for the legal name of a person and not the name a person may currently be using. The intake form typically asks patients to check either male or female. The bathrooms give the same two choices.
“Every physician should know how to speak with, treat, emote with, and empathize with care for the trans and nonbinary individual,” Dr. Klein said.
Dr. Klein noted there is a glaring shortage of trans and nonbinary physicians to lead efforts to expand education on integrating the medical, psychological, and psychosocial care that patients will receive.
Currently, gender medicine is not included on board exams for adolescent medicine or endocrinology, he said.
“Adding formal training in gender medicine to board exams would really help solidify the importance of this arena of medicine,” he noted.
First AAMC standards
In 2014, the AAMC released the first standards to guide curricula across medical school and residency to support training doctors to be competent in caring for transgender patients.
The standards include recommending that all doctors be able to communicate with patients related to their gender identity and understand how to deliver high-quality care to transgender and gender-diverse patients within their specialty, Kristen L. Eckstrand, MD, a coauthor of the guidelines, told this news organization.
“Many medical schools have developed their own curricula to meet these standards,” said Dr. Eckstrand, medical director for LGBTQIA+ Health at the University of Pittsburgh Medical Center.
Norma Poll-Hunter, PhD, AAMC’s senior director for workforce diversity, noted that the organization recently released its diversity, equity, and inclusion competencies that guide the medical education of students, residents, and faculty.
Dr. Poll-Hunter told this news organization that AAMC partners with the Building the Next Generation of Academic Physicians LGBT Health Workforce Conference “to support safe spaces for scholarly efforts and mentorship to advance this area of work.”
Team approach at Rutgers
Among the medical schools that incorporate comprehensive transgender care into the curriculum is Rutgers University’s Robert Wood Johnson Medical School in New Brunswick, N.J.
Gloria Bachmann, MD, is professor of obstetrics and gynecology at the school and medical director of its partner, the PROUD Gender Center of New Jersey. PROUD stands for “Promoting Respect, Outreach, Understanding, and Dignity,” and the center provides comprehensive care for transgender and nonbinary patients in one location.
Dr. Bachmann said Rutgers takes a team approach with both instructors and learners teaching medical students about transgender care. The teachers are not only professors in traditional classroom lectures, but patient navigators and nurses at the PROUD center, established as part of the medical school in 2020. Students learn from the navigators, for instance, how to help patients through the spectrum of inpatient and outpatient care.
“All of our learners do get to care for individuals who identify as transgender,” said Dr. Bachmann.
Among the improvements in educating students on transgender care over the years, she said, is the emphasis on social determinants of health. In the transgender population, initial questions may include whether the person is able to access care through insurance as laws vary widely on what care and procedures are covered.
As another example, Dr. Bachmann cites: “If they are seen on an emergency basis and are sent home with medication and follow-up, can they afford it?”
Another consideration is whether there is a home to which they can return.
“Many individuals who are transgender may not have a home. Their family may not be accepting of them. Therefore, it’s the social determinants of health as well as their transgender identity that have to be put into the equation of best care,” she said.
Giving back to the trans community
Mr. Noto doesn’t know whether he will specialize in gender medicine, but he is committed to serving the transgender community in whatever physician path he chooses.
He said he realizes he is fortunate to have strong family support and good insurance and that he can afford fees, such as the copay to see transgender care specialists. Many in the community do not have those resources and are likely to get care “only if they have to.”
At Tulane, training in transgender care starts during orientation week and continues on different levels, with different options, throughout medical school and residency, he added.
Mr. Noto said he would like to see more mandatory learning such as a “queer-centered exam, where you have to give an organ inventory and you have to ask patients if it’s OK to talk about X, Y, and Z.” He’d also like more opportunities for clinical interaction with transgender patients, such as queer-centered rotations.
When physicians aren’t well trained in transgender care, you have patients educating the doctors, which, Mr. Noto said, should not be acceptable.
“People come to you on their worst day. And to not be informed about them in my mind is negligent. In what other population can you choose not to learn about someone just because you don’t want to?” he said.
A version of this article first appeared on Medscape.com.
Klay Noto wants to be the kind of doctor he never had when he began to question his gender identity.
A second-year student at Tulane University in New Orleans, he wants to listen compassionately to patients’ concerns and recognize the hurt when they question who they are. He will be the kind of doctor who knows that a breast exam can be traumatizing if someone has been breast binding or that instructing a patient to take everything off and put on a gown can be triggering for someone with gender dysphoria.
Being in the room for hard conversations is part of why he pursued med school. “There aren’t many LGBT people in medicine and as I started to understand all the dynamics that go into it, I started to see that I could do it and I could be that different kind of doctor,” he told this news organization.
Mr. Noto, who transitioned after college, wants to see more transgender people like himself teaching gender medicine, and for all medical students to be trained in what it means to be transgender and how to give compassionate and comprehensive care to all patients.
Gains have been made in providing curriculum in transgender care that trains medical students in such concepts as how to approach gender identity with sensitivity and how to manage hormone therapy and surgery for transitioning patients who request that, according to those interviewed for this story.
But they agree there’s a long way to go to having widespread medical school integration of the health care needs of about 1.4 million transgender people in the United States.
According to the Association of American Medical Colleges (AAMC) Curriculum Inventory data collected from 131 U.S. medical schools, more than 65% offered some form of transgender-related education in 2018, and more than 80% of those provided such curriculum in required courses.
Lack of transgender, nonbinary faculty
Jason Klein, MD, is a pediatric endocrinologist and medical director of the Transgender Youth Health Program at New York (N.Y.) University.
He said in an interview that the number of programs nationally that have gender medicine as a structured part of their curriculum has increased over the last 5-10 years, but that education is not standardized from program to program.
The program at NYU includes lecture-style learning, case presentations, real-world conversations with people in the community, group discussions, and patient care, Dr. Klein said. There are formal lectures as part of adolescent medicine where students learn the differences between gender and sexual identity, and education on medical treatment of transgender and nonbinary adolescents, starting with puberty blockers and moving into affirming hormones.
Doctors also learn to know their limits and decide when to refer patients to a specialist.
“The focus is really about empathic and supportive care,” said Dr. Klein, assistant professor in the department of pediatrics at Hassenfeld Children’s Hospital at NYU Langone Health. “It’s about communication and understanding and the language we use and how to deliver affirming care in a health care setting in general.”
Imagine the potential stressors, he said, of a transgender person entering a typical health care setting. The electronic health record may only have room for the legal name of a person and not the name a person may currently be using. The intake form typically asks patients to check either male or female. The bathrooms give the same two choices.
“Every physician should know how to speak with, treat, emote with, and empathize with care for the trans and nonbinary individual,” Dr. Klein said.
Dr. Klein noted there is a glaring shortage of trans and nonbinary physicians to lead efforts to expand education on integrating the medical, psychological, and psychosocial care that patients will receive.
Currently, gender medicine is not included on board exams for adolescent medicine or endocrinology, he said.
“Adding formal training in gender medicine to board exams would really help solidify the importance of this arena of medicine,” he noted.
First AAMC standards
In 2014, the AAMC released the first standards to guide curricula across medical school and residency to support training doctors to be competent in caring for transgender patients.
The standards include recommending that all doctors be able to communicate with patients related to their gender identity and understand how to deliver high-quality care to transgender and gender-diverse patients within their specialty, Kristen L. Eckstrand, MD, a coauthor of the guidelines, told this news organization.
“Many medical schools have developed their own curricula to meet these standards,” said Dr. Eckstrand, medical director for LGBTQIA+ Health at the University of Pittsburgh Medical Center.
Norma Poll-Hunter, PhD, AAMC’s senior director for workforce diversity, noted that the organization recently released its diversity, equity, and inclusion competencies that guide the medical education of students, residents, and faculty.
Dr. Poll-Hunter told this news organization that AAMC partners with the Building the Next Generation of Academic Physicians LGBT Health Workforce Conference “to support safe spaces for scholarly efforts and mentorship to advance this area of work.”
Team approach at Rutgers
Among the medical schools that incorporate comprehensive transgender care into the curriculum is Rutgers University’s Robert Wood Johnson Medical School in New Brunswick, N.J.
Gloria Bachmann, MD, is professor of obstetrics and gynecology at the school and medical director of its partner, the PROUD Gender Center of New Jersey. PROUD stands for “Promoting Respect, Outreach, Understanding, and Dignity,” and the center provides comprehensive care for transgender and nonbinary patients in one location.
Dr. Bachmann said Rutgers takes a team approach with both instructors and learners teaching medical students about transgender care. The teachers are not only professors in traditional classroom lectures, but patient navigators and nurses at the PROUD center, established as part of the medical school in 2020. Students learn from the navigators, for instance, how to help patients through the spectrum of inpatient and outpatient care.
“All of our learners do get to care for individuals who identify as transgender,” said Dr. Bachmann.
Among the improvements in educating students on transgender care over the years, she said, is the emphasis on social determinants of health. In the transgender population, initial questions may include whether the person is able to access care through insurance as laws vary widely on what care and procedures are covered.
As another example, Dr. Bachmann cites: “If they are seen on an emergency basis and are sent home with medication and follow-up, can they afford it?”
Another consideration is whether there is a home to which they can return.
“Many individuals who are transgender may not have a home. Their family may not be accepting of them. Therefore, it’s the social determinants of health as well as their transgender identity that have to be put into the equation of best care,” she said.
Giving back to the trans community
Mr. Noto doesn’t know whether he will specialize in gender medicine, but he is committed to serving the transgender community in whatever physician path he chooses.
He said he realizes he is fortunate to have strong family support and good insurance and that he can afford fees, such as the copay to see transgender care specialists. Many in the community do not have those resources and are likely to get care “only if they have to.”
At Tulane, training in transgender care starts during orientation week and continues on different levels, with different options, throughout medical school and residency, he added.
Mr. Noto said he would like to see more mandatory learning such as a “queer-centered exam, where you have to give an organ inventory and you have to ask patients if it’s OK to talk about X, Y, and Z.” He’d also like more opportunities for clinical interaction with transgender patients, such as queer-centered rotations.
When physicians aren’t well trained in transgender care, you have patients educating the doctors, which, Mr. Noto said, should not be acceptable.
“People come to you on their worst day. And to not be informed about them in my mind is negligent. In what other population can you choose not to learn about someone just because you don’t want to?” he said.
A version of this article first appeared on Medscape.com.
Klay Noto wants to be the kind of doctor he never had when he began to question his gender identity.
A second-year student at Tulane University in New Orleans, he wants to listen compassionately to patients’ concerns and recognize the hurt when they question who they are. He will be the kind of doctor who knows that a breast exam can be traumatizing if someone has been breast binding or that instructing a patient to take everything off and put on a gown can be triggering for someone with gender dysphoria.
Being in the room for hard conversations is part of why he pursued med school. “There aren’t many LGBT people in medicine and as I started to understand all the dynamics that go into it, I started to see that I could do it and I could be that different kind of doctor,” he told this news organization.
Mr. Noto, who transitioned after college, wants to see more transgender people like himself teaching gender medicine, and for all medical students to be trained in what it means to be transgender and how to give compassionate and comprehensive care to all patients.
Gains have been made in providing curriculum in transgender care that trains medical students in such concepts as how to approach gender identity with sensitivity and how to manage hormone therapy and surgery for transitioning patients who request that, according to those interviewed for this story.
But they agree there’s a long way to go to having widespread medical school integration of the health care needs of about 1.4 million transgender people in the United States.
According to the Association of American Medical Colleges (AAMC) Curriculum Inventory data collected from 131 U.S. medical schools, more than 65% offered some form of transgender-related education in 2018, and more than 80% of those provided such curriculum in required courses.
Lack of transgender, nonbinary faculty
Jason Klein, MD, is a pediatric endocrinologist and medical director of the Transgender Youth Health Program at New York (N.Y.) University.
He said in an interview that the number of programs nationally that have gender medicine as a structured part of their curriculum has increased over the last 5-10 years, but that education is not standardized from program to program.
The program at NYU includes lecture-style learning, case presentations, real-world conversations with people in the community, group discussions, and patient care, Dr. Klein said. There are formal lectures as part of adolescent medicine where students learn the differences between gender and sexual identity, and education on medical treatment of transgender and nonbinary adolescents, starting with puberty blockers and moving into affirming hormones.
Doctors also learn to know their limits and decide when to refer patients to a specialist.
“The focus is really about empathic and supportive care,” said Dr. Klein, assistant professor in the department of pediatrics at Hassenfeld Children’s Hospital at NYU Langone Health. “It’s about communication and understanding and the language we use and how to deliver affirming care in a health care setting in general.”
Imagine the potential stressors, he said, of a transgender person entering a typical health care setting. The electronic health record may only have room for the legal name of a person and not the name a person may currently be using. The intake form typically asks patients to check either male or female. The bathrooms give the same two choices.
“Every physician should know how to speak with, treat, emote with, and empathize with care for the trans and nonbinary individual,” Dr. Klein said.
Dr. Klein noted there is a glaring shortage of trans and nonbinary physicians to lead efforts to expand education on integrating the medical, psychological, and psychosocial care that patients will receive.
Currently, gender medicine is not included on board exams for adolescent medicine or endocrinology, he said.
“Adding formal training in gender medicine to board exams would really help solidify the importance of this arena of medicine,” he noted.
First AAMC standards
In 2014, the AAMC released the first standards to guide curricula across medical school and residency to support training doctors to be competent in caring for transgender patients.
The standards include recommending that all doctors be able to communicate with patients related to their gender identity and understand how to deliver high-quality care to transgender and gender-diverse patients within their specialty, Kristen L. Eckstrand, MD, a coauthor of the guidelines, told this news organization.
“Many medical schools have developed their own curricula to meet these standards,” said Dr. Eckstrand, medical director for LGBTQIA+ Health at the University of Pittsburgh Medical Center.
Norma Poll-Hunter, PhD, AAMC’s senior director for workforce diversity, noted that the organization recently released its diversity, equity, and inclusion competencies that guide the medical education of students, residents, and faculty.
Dr. Poll-Hunter told this news organization that AAMC partners with the Building the Next Generation of Academic Physicians LGBT Health Workforce Conference “to support safe spaces for scholarly efforts and mentorship to advance this area of work.”
Team approach at Rutgers
Among the medical schools that incorporate comprehensive transgender care into the curriculum is Rutgers University’s Robert Wood Johnson Medical School in New Brunswick, N.J.
Gloria Bachmann, MD, is professor of obstetrics and gynecology at the school and medical director of its partner, the PROUD Gender Center of New Jersey. PROUD stands for “Promoting Respect, Outreach, Understanding, and Dignity,” and the center provides comprehensive care for transgender and nonbinary patients in one location.
Dr. Bachmann said Rutgers takes a team approach with both instructors and learners teaching medical students about transgender care. The teachers are not only professors in traditional classroom lectures, but patient navigators and nurses at the PROUD center, established as part of the medical school in 2020. Students learn from the navigators, for instance, how to help patients through the spectrum of inpatient and outpatient care.
“All of our learners do get to care for individuals who identify as transgender,” said Dr. Bachmann.
Among the improvements in educating students on transgender care over the years, she said, is the emphasis on social determinants of health. In the transgender population, initial questions may include whether the person is able to access care through insurance as laws vary widely on what care and procedures are covered.
As another example, Dr. Bachmann cites: “If they are seen on an emergency basis and are sent home with medication and follow-up, can they afford it?”
Another consideration is whether there is a home to which they can return.
“Many individuals who are transgender may not have a home. Their family may not be accepting of them. Therefore, it’s the social determinants of health as well as their transgender identity that have to be put into the equation of best care,” she said.
Giving back to the trans community
Mr. Noto doesn’t know whether he will specialize in gender medicine, but he is committed to serving the transgender community in whatever physician path he chooses.
He said he realizes he is fortunate to have strong family support and good insurance and that he can afford fees, such as the copay to see transgender care specialists. Many in the community do not have those resources and are likely to get care “only if they have to.”
At Tulane, training in transgender care starts during orientation week and continues on different levels, with different options, throughout medical school and residency, he added.
Mr. Noto said he would like to see more mandatory learning such as a “queer-centered exam, where you have to give an organ inventory and you have to ask patients if it’s OK to talk about X, Y, and Z.” He’d also like more opportunities for clinical interaction with transgender patients, such as queer-centered rotations.
When physicians aren’t well trained in transgender care, you have patients educating the doctors, which, Mr. Noto said, should not be acceptable.
“People come to you on their worst day. And to not be informed about them in my mind is negligent. In what other population can you choose not to learn about someone just because you don’t want to?” he said.
A version of this article first appeared on Medscape.com.
The best statins to lower non-HDL cholesterol in diabetes?
A network meta-analysis of 42 clinical trials concludes that rosuvastatin, simvastatin, and atorvastatin are the statins most effective at lowering non-high-density-lipoprotein cholesterol (non-HDL-C) in people with diabetes and at risk for cardiovascular disease.
The analysis focused on the efficacy of statin treatment on reducing non-HDL-C, as opposed to reducing low-density-lipoprotein cholesterol (LDL-C), which has traditionally been used as a surrogate to determine cardiovascular disease risk from hypercholesterolemia.
“The National Cholesterol Education Program in the United States recommends that LDL-C values should be used to estimate the risk of cardiovascular disease related to lipoproteins,” lead author Alexander Hodkinson, MD, senior National Institute for Health Research fellow, University of Manchester, England, told this news organization.
“But we believe that non-high-density-lipoprotein cholesterol is more strongly associated with the risk of cardiovascular disease, because non-HDL-C combines all the bad types of cholesterol, which LDL-C misses, so it could be a better tool than LDL-C for assessing CVD risk and effects of treatment. We already knew which of the statins reduce LDL-C, but we wanted to know which ones reduced non-HDL-C; hence the reason for our study,” Dr. Hodkinson said.
The findings were published online in BMJ.
In April 2021, the National Institute for Health and Care Excellence (NICE) in the United Kingdom updated guidelines for adults with diabetes to recommend that non-HDL-C should replace LDL-C as the primary target for reducing the risk for cardiovascular disease with lipid-lowering treatment.
Currently, NICE is alone in its recommendation. Other international guidelines do not have a non-HDL-C target and use LDL-C reduction instead. These include guidelines from the European Society of Cardiology (ESC), the American College of Cardiology (ACC), the American Heart Association (AHA), and the National Lipid Association.
Non–HDL-C is simple to calculate and can easily be done by clinicians by subtracting HDL-C from the total cholesterol level, he added.
This analysis compared the effectiveness of different statins at different intensities in reducing levels of non-HDL-C in 42 randomized controlled trials that included 20,193 adults with diabetes.
Compared with placebo, rosuvastatin, given at moderate- and high-intensity doses, and simvastatin and atorvastatin at high-intensity doses, were the best at lowering levels of non-HDL-C over an average treatment period of 12 weeks.
High-intensity rosuvastatin led to a 2.31 mmol/L reduction in non-HDL-C (95% credible interval, –3.39 to –1.21). Moderate-intensity rosuvastatin led to a 2.27 mmol/L reduction in non-HDL-C (95% credible interval, –3.00 to –1.49).
High-intensity simvastatin led to a 2.26 mmol/L reduction in non-HDL-C (95% credible interval, –2.99 to –1.51).
High-intensity atorvastatin led to a 2.20 mmol/L reduction in non-HDL-C (95% credible interval, –2.69 to –1.70).
Atorvastatin and simvastatin at any intensity and pravastatin at low intensity were also effective in reducing levels of non-HDL-C, the researchers noted.
In 4,670 patients who were at great risk for a major cardiovascular event, atorvastatin at high intensity showed the largest reduction in levels of non-HDL-C (1.98 mmol/L; 95% credible interval, –4.16 to 0.26).
In addition, high-intensity simvastatin and rosuvastatin were the most effective in reducing LDL-C.
High-intensity simvastatin led to a 1.93 mmol/L reduction in LDL-C (95% credible interval, –2.63 to –1.21), and high-intensity rosuvastatin led to a 1.76 mmol/L reduction in LDL-C (95% credible interval, –2.37 to –1.15).
In four studies, significant reductions in nonfatal myocardial infarction were shown for atorvastatin at moderate intensity, compared with placebo (relative risk, 0.57; 95% confidence interval, 0.43-.76). No significant differences were seen for discontinuations, nonfatal stroke, or cardiovascular death.
“We hope our findings will help guide clinicians on statin selection itself, and what types of doses they should be giving patients. These results support using NICE’s new policy guidelines on cholesterol monitoring, using this non-HDL-C measure, which contains all the bad types of cholesterol for patients with diabetes,” Dr. Hodkinson said.
“This study further emphasizes what we have known about the benefit of statin therapy in patients with type 2 diabetes,” Prakash Deedwania, MD, professor of medicine, University of California, San Francisco, told this news organization.
Dr. Deedwania and others have published data on patients with diabetes that showed that treatment with high-intensity atorvastatin was associated with significant reductions in major adverse cardiovascular events.
“Here they use non-HDL cholesterol as a target. The NICE guidelines are the only guidelines looking at non-HDL cholesterol; however, all guidelines suggest an LDL to be less than 70 in all people with diabetes, and for those with recent acute coronary syndromes, the latest evidence suggests the LDL should actually be less than 50,” said Dr. Deedwania, spokesperson for the AHA and ACC.
As far as which measure to use, he believes both are useful. “It’s six of one and half a dozen of the other, in my opinion. The societies have not recommended non-HDL cholesterol and it’s easier to stay with what is readily available for clinicians, and using LDL cholesterol is still okay. The results of this analysis are confirmatory, in that looking at non-HDL cholesterol gives results very similar to what these statins have shown for their effect on LDL cholesterol,” he said.
Non-HDL cholesterol a better marker?
For Robert Rosenson, MD, director of metabolism and lipids at Mount Sinai Health System and professor of medicine and cardiology at the Icahn School of Medicine at Mount Sinai, New York, non-HDL cholesterol is becoming an important marker of risk for several reasons.
“The focus on LDL cholesterol has been due to the causal relationship of LDL with atherosclerotic cardiovascular disease, but in the last few decades, non-HDL has emerged because more people are overweight, have insulin resistance, and have diabetes,” Dr. Rosenson told this news organization. “In those situations, the LDL cholesterol underrepresents the risk of the LDL particles. With insulin resistance, the particles become more triglycerides and less cholesterol, so on a per-particle basis, you need to get more LDL particles to get to a certain LDL cholesterol concentration.”
Non-HDL cholesterol testing does not require fasting, another advantage of using it to monitor cholesterol, he added.
What is often forgotten is that moderate- to high-intensity statins have very good triglyceride-lowering effects, Dr. Rosenson said.
“This article highlights that, by using higher doses, you get more triglyceride-lowering. Hopefully, this will get practitioners to recognize that non-HDL cholesterol is a better predictor of risk in people with diabetes,” he said.
The study was funded by the National Institute for Health Research. Dr. Hodkinson, Dr. Rosenson, and Dr. Deedwania report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A network meta-analysis of 42 clinical trials concludes that rosuvastatin, simvastatin, and atorvastatin are the statins most effective at lowering non-high-density-lipoprotein cholesterol (non-HDL-C) in people with diabetes and at risk for cardiovascular disease.
The analysis focused on the efficacy of statin treatment on reducing non-HDL-C, as opposed to reducing low-density-lipoprotein cholesterol (LDL-C), which has traditionally been used as a surrogate to determine cardiovascular disease risk from hypercholesterolemia.
“The National Cholesterol Education Program in the United States recommends that LDL-C values should be used to estimate the risk of cardiovascular disease related to lipoproteins,” lead author Alexander Hodkinson, MD, senior National Institute for Health Research fellow, University of Manchester, England, told this news organization.
“But we believe that non-high-density-lipoprotein cholesterol is more strongly associated with the risk of cardiovascular disease, because non-HDL-C combines all the bad types of cholesterol, which LDL-C misses, so it could be a better tool than LDL-C for assessing CVD risk and effects of treatment. We already knew which of the statins reduce LDL-C, but we wanted to know which ones reduced non-HDL-C; hence the reason for our study,” Dr. Hodkinson said.
The findings were published online in BMJ.
In April 2021, the National Institute for Health and Care Excellence (NICE) in the United Kingdom updated guidelines for adults with diabetes to recommend that non-HDL-C should replace LDL-C as the primary target for reducing the risk for cardiovascular disease with lipid-lowering treatment.
Currently, NICE is alone in its recommendation. Other international guidelines do not have a non-HDL-C target and use LDL-C reduction instead. These include guidelines from the European Society of Cardiology (ESC), the American College of Cardiology (ACC), the American Heart Association (AHA), and the National Lipid Association.
Non–HDL-C is simple to calculate and can easily be done by clinicians by subtracting HDL-C from the total cholesterol level, he added.
This analysis compared the effectiveness of different statins at different intensities in reducing levels of non-HDL-C in 42 randomized controlled trials that included 20,193 adults with diabetes.
Compared with placebo, rosuvastatin, given at moderate- and high-intensity doses, and simvastatin and atorvastatin at high-intensity doses, were the best at lowering levels of non-HDL-C over an average treatment period of 12 weeks.
High-intensity rosuvastatin led to a 2.31 mmol/L reduction in non-HDL-C (95% credible interval, –3.39 to –1.21). Moderate-intensity rosuvastatin led to a 2.27 mmol/L reduction in non-HDL-C (95% credible interval, –3.00 to –1.49).
High-intensity simvastatin led to a 2.26 mmol/L reduction in non-HDL-C (95% credible interval, –2.99 to –1.51).
High-intensity atorvastatin led to a 2.20 mmol/L reduction in non-HDL-C (95% credible interval, –2.69 to –1.70).
Atorvastatin and simvastatin at any intensity and pravastatin at low intensity were also effective in reducing levels of non-HDL-C, the researchers noted.
In 4,670 patients who were at great risk for a major cardiovascular event, atorvastatin at high intensity showed the largest reduction in levels of non-HDL-C (1.98 mmol/L; 95% credible interval, –4.16 to 0.26).
In addition, high-intensity simvastatin and rosuvastatin were the most effective in reducing LDL-C.
High-intensity simvastatin led to a 1.93 mmol/L reduction in LDL-C (95% credible interval, –2.63 to –1.21), and high-intensity rosuvastatin led to a 1.76 mmol/L reduction in LDL-C (95% credible interval, –2.37 to –1.15).
In four studies, significant reductions in nonfatal myocardial infarction were shown for atorvastatin at moderate intensity, compared with placebo (relative risk, 0.57; 95% confidence interval, 0.43-.76). No significant differences were seen for discontinuations, nonfatal stroke, or cardiovascular death.
“We hope our findings will help guide clinicians on statin selection itself, and what types of doses they should be giving patients. These results support using NICE’s new policy guidelines on cholesterol monitoring, using this non-HDL-C measure, which contains all the bad types of cholesterol for patients with diabetes,” Dr. Hodkinson said.
“This study further emphasizes what we have known about the benefit of statin therapy in patients with type 2 diabetes,” Prakash Deedwania, MD, professor of medicine, University of California, San Francisco, told this news organization.
Dr. Deedwania and others have published data on patients with diabetes that showed that treatment with high-intensity atorvastatin was associated with significant reductions in major adverse cardiovascular events.
“Here they use non-HDL cholesterol as a target. The NICE guidelines are the only guidelines looking at non-HDL cholesterol; however, all guidelines suggest an LDL to be less than 70 in all people with diabetes, and for those with recent acute coronary syndromes, the latest evidence suggests the LDL should actually be less than 50,” said Dr. Deedwania, spokesperson for the AHA and ACC.
As far as which measure to use, he believes both are useful. “It’s six of one and half a dozen of the other, in my opinion. The societies have not recommended non-HDL cholesterol and it’s easier to stay with what is readily available for clinicians, and using LDL cholesterol is still okay. The results of this analysis are confirmatory, in that looking at non-HDL cholesterol gives results very similar to what these statins have shown for their effect on LDL cholesterol,” he said.
Non-HDL cholesterol a better marker?
For Robert Rosenson, MD, director of metabolism and lipids at Mount Sinai Health System and professor of medicine and cardiology at the Icahn School of Medicine at Mount Sinai, New York, non-HDL cholesterol is becoming an important marker of risk for several reasons.
“The focus on LDL cholesterol has been due to the causal relationship of LDL with atherosclerotic cardiovascular disease, but in the last few decades, non-HDL has emerged because more people are overweight, have insulin resistance, and have diabetes,” Dr. Rosenson told this news organization. “In those situations, the LDL cholesterol underrepresents the risk of the LDL particles. With insulin resistance, the particles become more triglycerides and less cholesterol, so on a per-particle basis, you need to get more LDL particles to get to a certain LDL cholesterol concentration.”
Non-HDL cholesterol testing does not require fasting, another advantage of using it to monitor cholesterol, he added.
What is often forgotten is that moderate- to high-intensity statins have very good triglyceride-lowering effects, Dr. Rosenson said.
“This article highlights that, by using higher doses, you get more triglyceride-lowering. Hopefully, this will get practitioners to recognize that non-HDL cholesterol is a better predictor of risk in people with diabetes,” he said.
The study was funded by the National Institute for Health Research. Dr. Hodkinson, Dr. Rosenson, and Dr. Deedwania report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A network meta-analysis of 42 clinical trials concludes that rosuvastatin, simvastatin, and atorvastatin are the statins most effective at lowering non-high-density-lipoprotein cholesterol (non-HDL-C) in people with diabetes and at risk for cardiovascular disease.
The analysis focused on the efficacy of statin treatment on reducing non-HDL-C, as opposed to reducing low-density-lipoprotein cholesterol (LDL-C), which has traditionally been used as a surrogate to determine cardiovascular disease risk from hypercholesterolemia.
“The National Cholesterol Education Program in the United States recommends that LDL-C values should be used to estimate the risk of cardiovascular disease related to lipoproteins,” lead author Alexander Hodkinson, MD, senior National Institute for Health Research fellow, University of Manchester, England, told this news organization.
“But we believe that non-high-density-lipoprotein cholesterol is more strongly associated with the risk of cardiovascular disease, because non-HDL-C combines all the bad types of cholesterol, which LDL-C misses, so it could be a better tool than LDL-C for assessing CVD risk and effects of treatment. We already knew which of the statins reduce LDL-C, but we wanted to know which ones reduced non-HDL-C; hence the reason for our study,” Dr. Hodkinson said.
The findings were published online in BMJ.
In April 2021, the National Institute for Health and Care Excellence (NICE) in the United Kingdom updated guidelines for adults with diabetes to recommend that non-HDL-C should replace LDL-C as the primary target for reducing the risk for cardiovascular disease with lipid-lowering treatment.
Currently, NICE is alone in its recommendation. Other international guidelines do not have a non-HDL-C target and use LDL-C reduction instead. These include guidelines from the European Society of Cardiology (ESC), the American College of Cardiology (ACC), the American Heart Association (AHA), and the National Lipid Association.
Non–HDL-C is simple to calculate and can easily be done by clinicians by subtracting HDL-C from the total cholesterol level, he added.
This analysis compared the effectiveness of different statins at different intensities in reducing levels of non-HDL-C in 42 randomized controlled trials that included 20,193 adults with diabetes.
Compared with placebo, rosuvastatin, given at moderate- and high-intensity doses, and simvastatin and atorvastatin at high-intensity doses, were the best at lowering levels of non-HDL-C over an average treatment period of 12 weeks.
High-intensity rosuvastatin led to a 2.31 mmol/L reduction in non-HDL-C (95% credible interval, –3.39 to –1.21). Moderate-intensity rosuvastatin led to a 2.27 mmol/L reduction in non-HDL-C (95% credible interval, –3.00 to –1.49).
High-intensity simvastatin led to a 2.26 mmol/L reduction in non-HDL-C (95% credible interval, –2.99 to –1.51).
High-intensity atorvastatin led to a 2.20 mmol/L reduction in non-HDL-C (95% credible interval, –2.69 to –1.70).
Atorvastatin and simvastatin at any intensity and pravastatin at low intensity were also effective in reducing levels of non-HDL-C, the researchers noted.
In 4,670 patients who were at great risk for a major cardiovascular event, atorvastatin at high intensity showed the largest reduction in levels of non-HDL-C (1.98 mmol/L; 95% credible interval, –4.16 to 0.26).
In addition, high-intensity simvastatin and rosuvastatin were the most effective in reducing LDL-C.
High-intensity simvastatin led to a 1.93 mmol/L reduction in LDL-C (95% credible interval, –2.63 to –1.21), and high-intensity rosuvastatin led to a 1.76 mmol/L reduction in LDL-C (95% credible interval, –2.37 to –1.15).
In four studies, significant reductions in nonfatal myocardial infarction were shown for atorvastatin at moderate intensity, compared with placebo (relative risk, 0.57; 95% confidence interval, 0.43-.76). No significant differences were seen for discontinuations, nonfatal stroke, or cardiovascular death.
“We hope our findings will help guide clinicians on statin selection itself, and what types of doses they should be giving patients. These results support using NICE’s new policy guidelines on cholesterol monitoring, using this non-HDL-C measure, which contains all the bad types of cholesterol for patients with diabetes,” Dr. Hodkinson said.
“This study further emphasizes what we have known about the benefit of statin therapy in patients with type 2 diabetes,” Prakash Deedwania, MD, professor of medicine, University of California, San Francisco, told this news organization.
Dr. Deedwania and others have published data on patients with diabetes that showed that treatment with high-intensity atorvastatin was associated with significant reductions in major adverse cardiovascular events.
“Here they use non-HDL cholesterol as a target. The NICE guidelines are the only guidelines looking at non-HDL cholesterol; however, all guidelines suggest an LDL to be less than 70 in all people with diabetes, and for those with recent acute coronary syndromes, the latest evidence suggests the LDL should actually be less than 50,” said Dr. Deedwania, spokesperson for the AHA and ACC.
As far as which measure to use, he believes both are useful. “It’s six of one and half a dozen of the other, in my opinion. The societies have not recommended non-HDL cholesterol and it’s easier to stay with what is readily available for clinicians, and using LDL cholesterol is still okay. The results of this analysis are confirmatory, in that looking at non-HDL cholesterol gives results very similar to what these statins have shown for their effect on LDL cholesterol,” he said.
Non-HDL cholesterol a better marker?
For Robert Rosenson, MD, director of metabolism and lipids at Mount Sinai Health System and professor of medicine and cardiology at the Icahn School of Medicine at Mount Sinai, New York, non-HDL cholesterol is becoming an important marker of risk for several reasons.
“The focus on LDL cholesterol has been due to the causal relationship of LDL with atherosclerotic cardiovascular disease, but in the last few decades, non-HDL has emerged because more people are overweight, have insulin resistance, and have diabetes,” Dr. Rosenson told this news organization. “In those situations, the LDL cholesterol underrepresents the risk of the LDL particles. With insulin resistance, the particles become more triglycerides and less cholesterol, so on a per-particle basis, you need to get more LDL particles to get to a certain LDL cholesterol concentration.”
Non-HDL cholesterol testing does not require fasting, another advantage of using it to monitor cholesterol, he added.
What is often forgotten is that moderate- to high-intensity statins have very good triglyceride-lowering effects, Dr. Rosenson said.
“This article highlights that, by using higher doses, you get more triglyceride-lowering. Hopefully, this will get practitioners to recognize that non-HDL cholesterol is a better predictor of risk in people with diabetes,” he said.
The study was funded by the National Institute for Health Research. Dr. Hodkinson, Dr. Rosenson, and Dr. Deedwania report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
U.S. life expectancy dropped by 2 years in 2020: Study
according to a new study.
The study, published in medRxiv, said U.S. life expectancy went from 78.86 years in 2019 to 76.99 years in 2020, during the thick of the global COVID-19 pandemic. Though vaccines were widely available in 2021, the U.S. life expectancy was expected to keep going down, to 76.60 years.
In “peer countries” – Austria, Belgium, Denmark, England and Wales, Finland, France, Germany, Israel, Italy, the Netherlands, New Zealand, Northern Ireland, Norway, Portugal, Scotland, South Korea, Spain, Sweden, and Switzerland – life expectancy went down only 0.57 years from 2019 to 2020 and increased by 0.28 years in 2021, the study said. The peer countries now have a life expectancy that’s 5 years longer than in the United States.
“The fact the U.S. lost so many more lives than other high-income countries speaks not only to how we managed the pandemic, but also to more deeply rooted problems that predated the pandemic,” said Steven H. Woolf, MD, one of the study authors and a professor of family medicine and population health at Virginia Commonwealth University, Richmond, according to Reuters.
“U.S. life expectancy has been falling behind other countries since the 1980s, and the gap has widened over time, especially in the last decade.”
Lack of universal health care, income and educational inequality, and less-healthy physical and social environments helped lead to the decline in American life expectancy, according to Dr. Woolf.
The life expectancy drop from 2019 to 2020 hit Black and Hispanic people hardest, according to the study. But the drop from 2020 to 2021 affected White people the most, with average life expectancy among them going down about a third of a year.
Researchers looked at death data from the National Center for Health Statistics, the Human Mortality Database, and overseas statistical agencies. Life expectancy for 2021 was estimated “using a previously validated modeling method,” the study said.
A version of this article first appeared on WebMD.com.
according to a new study.
The study, published in medRxiv, said U.S. life expectancy went from 78.86 years in 2019 to 76.99 years in 2020, during the thick of the global COVID-19 pandemic. Though vaccines were widely available in 2021, the U.S. life expectancy was expected to keep going down, to 76.60 years.
In “peer countries” – Austria, Belgium, Denmark, England and Wales, Finland, France, Germany, Israel, Italy, the Netherlands, New Zealand, Northern Ireland, Norway, Portugal, Scotland, South Korea, Spain, Sweden, and Switzerland – life expectancy went down only 0.57 years from 2019 to 2020 and increased by 0.28 years in 2021, the study said. The peer countries now have a life expectancy that’s 5 years longer than in the United States.
“The fact the U.S. lost so many more lives than other high-income countries speaks not only to how we managed the pandemic, but also to more deeply rooted problems that predated the pandemic,” said Steven H. Woolf, MD, one of the study authors and a professor of family medicine and population health at Virginia Commonwealth University, Richmond, according to Reuters.
“U.S. life expectancy has been falling behind other countries since the 1980s, and the gap has widened over time, especially in the last decade.”
Lack of universal health care, income and educational inequality, and less-healthy physical and social environments helped lead to the decline in American life expectancy, according to Dr. Woolf.
The life expectancy drop from 2019 to 2020 hit Black and Hispanic people hardest, according to the study. But the drop from 2020 to 2021 affected White people the most, with average life expectancy among them going down about a third of a year.
Researchers looked at death data from the National Center for Health Statistics, the Human Mortality Database, and overseas statistical agencies. Life expectancy for 2021 was estimated “using a previously validated modeling method,” the study said.
A version of this article first appeared on WebMD.com.
according to a new study.
The study, published in medRxiv, said U.S. life expectancy went from 78.86 years in 2019 to 76.99 years in 2020, during the thick of the global COVID-19 pandemic. Though vaccines were widely available in 2021, the U.S. life expectancy was expected to keep going down, to 76.60 years.
In “peer countries” – Austria, Belgium, Denmark, England and Wales, Finland, France, Germany, Israel, Italy, the Netherlands, New Zealand, Northern Ireland, Norway, Portugal, Scotland, South Korea, Spain, Sweden, and Switzerland – life expectancy went down only 0.57 years from 2019 to 2020 and increased by 0.28 years in 2021, the study said. The peer countries now have a life expectancy that’s 5 years longer than in the United States.
“The fact the U.S. lost so many more lives than other high-income countries speaks not only to how we managed the pandemic, but also to more deeply rooted problems that predated the pandemic,” said Steven H. Woolf, MD, one of the study authors and a professor of family medicine and population health at Virginia Commonwealth University, Richmond, according to Reuters.
“U.S. life expectancy has been falling behind other countries since the 1980s, and the gap has widened over time, especially in the last decade.”
Lack of universal health care, income and educational inequality, and less-healthy physical and social environments helped lead to the decline in American life expectancy, according to Dr. Woolf.
The life expectancy drop from 2019 to 2020 hit Black and Hispanic people hardest, according to the study. But the drop from 2020 to 2021 affected White people the most, with average life expectancy among them going down about a third of a year.
Researchers looked at death data from the National Center for Health Statistics, the Human Mortality Database, and overseas statistical agencies. Life expectancy for 2021 was estimated “using a previously validated modeling method,” the study said.
A version of this article first appeared on WebMD.com.
FROM MEDRXIV
Aspirin exposure fails to reduce cardiovascular event risk
The benefits of aspirin use for the primary prevention of atherosclerotic cardiovascular disease (ASCVD) have been questioned in light of data showing neutral outcomes in low-risk patients and concerns about increased bleeding risk and mortality in healthy older adults, wrote Rita Del Pinto, MD, of University of L’Aquila (Italy) and colleagues in JAMA Network Open.
In the study, Dr. Del Pinto and colleagues conducted a post hoc analysis of data from more than 2,500 participants in SPRINT (Systolic Blood Pressure Intervention Trial), a multicenter, randomized trial conducted from 2010 to 2013.
The goal of SPRINT was to compare intensive and standard blood pressure–lowering strategies for hypertension patients. The primary outcome of the current study was risk of a first cardiovascular event, which included adjudicated myocardial infarction, non–myocardial infarction acute coronary syndrome, stroke, acute heart failure, and CVD death.“There has been considerable improvement in the management of cardiovascular risk factors since the first reports on aspirin use for cardiovascular prevention,” Dr. Del Pinto said in an interview.
“As for hypertension, not only have more effective antihypertensive medications become available, but also evidence has recently emerged in support of a downwards redefinition of blood pressure targets during treatment,” she said. “In this context, in an era when great attention is paid to the personalization of treatment, no specific studies had addressed the association of aspirin use as a primary prevention strategy in a cohort of relatively old, high-risk individuals with treated systolic blood pressure steadily below the recommended target,” she added.
The researchers assessed whether aspirin use in addition to standard blood pressure management (a target of less than 140 mm Hg) decreased risk and improved survival.
The study population included 2,664 adult patients; 29.3% were women, and 24.5% were aged 75 years and older. Half of the patients (1,332) received aspirin and 1,332 did not.
In a multivariate analysis, 42 cardiovascular events occurred in the aspirin group, compared with 20 events in those not exposed to aspirin (hazard ratio, 2.30). The findings were consistent in subgroup analyses of younger individuals, current and former smokers, and patients on statins.
An additional subgroup analysis of individuals randomized to standard care or intensive care in the SPRINT study showed no significant difference in primary outcome rates between individuals who received aspirin and those who did not. The rates for aspirin use vs. non–aspirin use were 5.85% vs. 3.60% in the standard treatment group and 4.66% vs. 2.56% in the intensive treatment group.
The study findings were limited by several factors, including the post hoc design, short follow-up period, and lack of data on the initiation of aspirin and bleeding events, the researchers wrote. However, the results suggest that modern management of hypertension may have redefined the potential benefits of aspirin in patients with hypertension, they concluded.
Findings confirm value of preventive care
“The study was conducted as a post-hoc analysis on an experimental cohort, which must be considered when interpreting the results,” Dr. Del Pinto said.
Despite the limitations, the study findings affirm that effective treatment of major cardiovascular risk factors, such as hypertension, with proven drugs is “a mainstay of the primary prevention of ASCVD,” she emphasized.
As for additional research, “Testing our findings in a dedicated setting with sufficiently long follow-up, where aspirin dose and indication, as well as any possible bleeding event, are reported could expand the clinical meaning of our observations,” said Dr. Del Pinto. “Also, the clinical impact of aspirin, even in combination with novel cardiovascular drugs such as direct oral anticoagulants, in populations exposed to combinations of risk factors, deserves further investigation.”
Data support shared decision-making
“While recent evidence has not shown a benefit of aspirin in the primary prevention of ASCVD in several populations, the subpopulation of patients with hypertension as an ASCVD risk factor is also of interest to the clinician,” Suman Pal, MD, of the University of New Mexico, Albuquerque, said in an interview. “The lack of benefit of aspirin in this study, despite its limitations, was surprising, and I would be eager to see how the role of aspirin in ASCVD prevention would continue to evolve in conjunction with improvement in other therapies for modification of risk factors.”
“The decision to continue aspirin in this subgroup of patients should warrant a discussion with patients and a reexamination of risks and benefits until further data are available,” Dr. Pal emphasized.
Larger studies with long-term follow-ups would be required to further clarify the role of aspirin in primary prevention of ASCVD in patients with hypertension without diabetes or chronic kidney disease, he added.
Data were supplied courtesy of BioLINCC. The study received no outside funding. The researchers and Dr. Pal had no financial conflicts to disclose.
The benefits of aspirin use for the primary prevention of atherosclerotic cardiovascular disease (ASCVD) have been questioned in light of data showing neutral outcomes in low-risk patients and concerns about increased bleeding risk and mortality in healthy older adults, wrote Rita Del Pinto, MD, of University of L’Aquila (Italy) and colleagues in JAMA Network Open.
In the study, Dr. Del Pinto and colleagues conducted a post hoc analysis of data from more than 2,500 participants in SPRINT (Systolic Blood Pressure Intervention Trial), a multicenter, randomized trial conducted from 2010 to 2013.
The goal of SPRINT was to compare intensive and standard blood pressure–lowering strategies for hypertension patients. The primary outcome of the current study was risk of a first cardiovascular event, which included adjudicated myocardial infarction, non–myocardial infarction acute coronary syndrome, stroke, acute heart failure, and CVD death.“There has been considerable improvement in the management of cardiovascular risk factors since the first reports on aspirin use for cardiovascular prevention,” Dr. Del Pinto said in an interview.
“As for hypertension, not only have more effective antihypertensive medications become available, but also evidence has recently emerged in support of a downwards redefinition of blood pressure targets during treatment,” she said. “In this context, in an era when great attention is paid to the personalization of treatment, no specific studies had addressed the association of aspirin use as a primary prevention strategy in a cohort of relatively old, high-risk individuals with treated systolic blood pressure steadily below the recommended target,” she added.
The researchers assessed whether aspirin use in addition to standard blood pressure management (a target of less than 140 mm Hg) decreased risk and improved survival.
The study population included 2,664 adult patients; 29.3% were women, and 24.5% were aged 75 years and older. Half of the patients (1,332) received aspirin and 1,332 did not.
In a multivariate analysis, 42 cardiovascular events occurred in the aspirin group, compared with 20 events in those not exposed to aspirin (hazard ratio, 2.30). The findings were consistent in subgroup analyses of younger individuals, current and former smokers, and patients on statins.
An additional subgroup analysis of individuals randomized to standard care or intensive care in the SPRINT study showed no significant difference in primary outcome rates between individuals who received aspirin and those who did not. The rates for aspirin use vs. non–aspirin use were 5.85% vs. 3.60% in the standard treatment group and 4.66% vs. 2.56% in the intensive treatment group.
The study findings were limited by several factors, including the post hoc design, short follow-up period, and lack of data on the initiation of aspirin and bleeding events, the researchers wrote. However, the results suggest that modern management of hypertension may have redefined the potential benefits of aspirin in patients with hypertension, they concluded.
Findings confirm value of preventive care
“The study was conducted as a post-hoc analysis on an experimental cohort, which must be considered when interpreting the results,” Dr. Del Pinto said.
Despite the limitations, the study findings affirm that effective treatment of major cardiovascular risk factors, such as hypertension, with proven drugs is “a mainstay of the primary prevention of ASCVD,” she emphasized.
As for additional research, “Testing our findings in a dedicated setting with sufficiently long follow-up, where aspirin dose and indication, as well as any possible bleeding event, are reported could expand the clinical meaning of our observations,” said Dr. Del Pinto. “Also, the clinical impact of aspirin, even in combination with novel cardiovascular drugs such as direct oral anticoagulants, in populations exposed to combinations of risk factors, deserves further investigation.”
Data support shared decision-making
“While recent evidence has not shown a benefit of aspirin in the primary prevention of ASCVD in several populations, the subpopulation of patients with hypertension as an ASCVD risk factor is also of interest to the clinician,” Suman Pal, MD, of the University of New Mexico, Albuquerque, said in an interview. “The lack of benefit of aspirin in this study, despite its limitations, was surprising, and I would be eager to see how the role of aspirin in ASCVD prevention would continue to evolve in conjunction with improvement in other therapies for modification of risk factors.”
“The decision to continue aspirin in this subgroup of patients should warrant a discussion with patients and a reexamination of risks and benefits until further data are available,” Dr. Pal emphasized.
Larger studies with long-term follow-ups would be required to further clarify the role of aspirin in primary prevention of ASCVD in patients with hypertension without diabetes or chronic kidney disease, he added.
Data were supplied courtesy of BioLINCC. The study received no outside funding. The researchers and Dr. Pal had no financial conflicts to disclose.
The benefits of aspirin use for the primary prevention of atherosclerotic cardiovascular disease (ASCVD) have been questioned in light of data showing neutral outcomes in low-risk patients and concerns about increased bleeding risk and mortality in healthy older adults, wrote Rita Del Pinto, MD, of University of L’Aquila (Italy) and colleagues in JAMA Network Open.
In the study, Dr. Del Pinto and colleagues conducted a post hoc analysis of data from more than 2,500 participants in SPRINT (Systolic Blood Pressure Intervention Trial), a multicenter, randomized trial conducted from 2010 to 2013.
The goal of SPRINT was to compare intensive and standard blood pressure–lowering strategies for hypertension patients. The primary outcome of the current study was risk of a first cardiovascular event, which included adjudicated myocardial infarction, non–myocardial infarction acute coronary syndrome, stroke, acute heart failure, and CVD death.“There has been considerable improvement in the management of cardiovascular risk factors since the first reports on aspirin use for cardiovascular prevention,” Dr. Del Pinto said in an interview.
“As for hypertension, not only have more effective antihypertensive medications become available, but also evidence has recently emerged in support of a downwards redefinition of blood pressure targets during treatment,” she said. “In this context, in an era when great attention is paid to the personalization of treatment, no specific studies had addressed the association of aspirin use as a primary prevention strategy in a cohort of relatively old, high-risk individuals with treated systolic blood pressure steadily below the recommended target,” she added.
The researchers assessed whether aspirin use in addition to standard blood pressure management (a target of less than 140 mm Hg) decreased risk and improved survival.
The study population included 2,664 adult patients; 29.3% were women, and 24.5% were aged 75 years and older. Half of the patients (1,332) received aspirin and 1,332 did not.
In a multivariate analysis, 42 cardiovascular events occurred in the aspirin group, compared with 20 events in those not exposed to aspirin (hazard ratio, 2.30). The findings were consistent in subgroup analyses of younger individuals, current and former smokers, and patients on statins.
An additional subgroup analysis of individuals randomized to standard care or intensive care in the SPRINT study showed no significant difference in primary outcome rates between individuals who received aspirin and those who did not. The rates for aspirin use vs. non–aspirin use were 5.85% vs. 3.60% in the standard treatment group and 4.66% vs. 2.56% in the intensive treatment group.
The study findings were limited by several factors, including the post hoc design, short follow-up period, and lack of data on the initiation of aspirin and bleeding events, the researchers wrote. However, the results suggest that modern management of hypertension may have redefined the potential benefits of aspirin in patients with hypertension, they concluded.
Findings confirm value of preventive care
“The study was conducted as a post-hoc analysis on an experimental cohort, which must be considered when interpreting the results,” Dr. Del Pinto said.
Despite the limitations, the study findings affirm that effective treatment of major cardiovascular risk factors, such as hypertension, with proven drugs is “a mainstay of the primary prevention of ASCVD,” she emphasized.
As for additional research, “Testing our findings in a dedicated setting with sufficiently long follow-up, where aspirin dose and indication, as well as any possible bleeding event, are reported could expand the clinical meaning of our observations,” said Dr. Del Pinto. “Also, the clinical impact of aspirin, even in combination with novel cardiovascular drugs such as direct oral anticoagulants, in populations exposed to combinations of risk factors, deserves further investigation.”
Data support shared decision-making
“While recent evidence has not shown a benefit of aspirin in the primary prevention of ASCVD in several populations, the subpopulation of patients with hypertension as an ASCVD risk factor is also of interest to the clinician,” Suman Pal, MD, of the University of New Mexico, Albuquerque, said in an interview. “The lack of benefit of aspirin in this study, despite its limitations, was surprising, and I would be eager to see how the role of aspirin in ASCVD prevention would continue to evolve in conjunction with improvement in other therapies for modification of risk factors.”
“The decision to continue aspirin in this subgroup of patients should warrant a discussion with patients and a reexamination of risks and benefits until further data are available,” Dr. Pal emphasized.
Larger studies with long-term follow-ups would be required to further clarify the role of aspirin in primary prevention of ASCVD in patients with hypertension without diabetes or chronic kidney disease, he added.
Data were supplied courtesy of BioLINCC. The study received no outside funding. The researchers and Dr. Pal had no financial conflicts to disclose.
FROM JAMA NETWORK OPEN
University of Washington, Harvard ranked top medical schools for second year
It may seem like déjà vu, as not much has changed regarding the rankings of top U.S. medical schools over the past 2 years.
The University of Washington, Seattle retained its ranking from the U.S. News & World Report as the top medical school for primary care for 2023. Also repeating its 2022 standing as the top medical school for research is Harvard University.
In the primary care ranking, the top 10 schools after the University of Washington were the University of California, San Francisco; the University of Minnesota; Oregon Health and Science University; the University of North Carolina at Chapel Hill; the University of Colorado; the University of Nebraska Medical Center; the University of California, Davis; and Harvard. Three schools tied for the no. 10 slot: the University of Kansas Medical Center, the University of Massachusetts Chan Medical Center, and the University of Pittsburgh.
The top five schools with the most graduates practicing in primary care specialties are Des Moines University, Iowa (50.6%); the University of Pikeville (Ky.) (46.8%); Western University of Health Sciences, Pomona, California (46%); William Carey University College of Osteopathic Medicine, Hattiesburg, Mississippi (44.7%); and A.T. Still University of Health Sciences, Kirksville, Missouri (44.3%).
Best for research
When it comes to schools ranking the highest for research, the Grossman School of Medicine at New York University takes the no. 2 spot after Harvard. Three schools were tied for the no. 3 spot: Columbia University, Johns Hopkins University, and the University of California, San Francisco; and two schools for no. 6: Duke University and the Perelman School of Medicine at the University of Pennsylvania, Philadelphia. No. 8 goes to Stanford University, followed by the University of Washington. Rounding out the top 10 is Yale University.
Specialty ranks
The top-ranked schools in eight specialties are as follows:
- Anesthesiology: Harvard
- Family medicine: the University of Washington
- Internal medicine: Johns Hopkins
- Obstetrics/gynecology: Harvard
- Pediatrics: the University of Pennsylvania (Perelman)
- Psychiatry: Harvard
- Radiology: Johns Hopkins
- Surgery: Harvard
Most diverse student body
If you’re looking for a school with significant minority representation, Howard University, Washington, D.C., ranked highest (76.8%), followed by the Wertheim College of Medicine at Florida International University, Miami (43.2%). The University of California, Davis (40%), Sacramento, California, and the University of Vermont (Larner), Burlington (14.1%), tied for third.
Three southern schools take top honors for the most graduates practicing in underserved areas, starting with the University of South Carolina (70.9%), followed by the University of Mississippi (66.2%), and East Tennessee State University (Quillen), Johnson City, Tennessee (65.8%).
The colleges with the most graduates practicing in rural areas are William Carey University College of Osteopathic Medicine (28%), the University of Pikesville (25.6%), and the University of Mississippi (22.1%).
College debt
The medical school where graduates have the most debt is Nova Southeastern University Patel College of Osteopathic Medicine, Fort Lauderdale, Florida. Graduates incurred an average debt of $309,206. Western University of Health Sciences graduates racked up $276,840 in debt, followed by graduates of West Virginia School of Osteopathic Medicine, owing $268,416.
Ranking criteria
Each year, U.S. News ranks hundreds of U.S. colleges and universities. Medical schools fall under the rankings for best graduate schools.
U.S. News surveyed 192 medical and osteopathic schools accredited in 2021 by the Liaison Committee on Medical Education or the American Osteopathic Association. Among the schools surveyed in fall 2021 and early 2022, 130 schools responded. Of those, 124 were included in both the research and primary care rankings.
The criteria for ranking include faculty resources, academic achievements of entering students, and qualitative assessments by schools and residency directors.
A version of this article first appeared on Medscape.com.
It may seem like déjà vu, as not much has changed regarding the rankings of top U.S. medical schools over the past 2 years.
The University of Washington, Seattle retained its ranking from the U.S. News & World Report as the top medical school for primary care for 2023. Also repeating its 2022 standing as the top medical school for research is Harvard University.
In the primary care ranking, the top 10 schools after the University of Washington were the University of California, San Francisco; the University of Minnesota; Oregon Health and Science University; the University of North Carolina at Chapel Hill; the University of Colorado; the University of Nebraska Medical Center; the University of California, Davis; and Harvard. Three schools tied for the no. 10 slot: the University of Kansas Medical Center, the University of Massachusetts Chan Medical Center, and the University of Pittsburgh.
The top five schools with the most graduates practicing in primary care specialties are Des Moines University, Iowa (50.6%); the University of Pikeville (Ky.) (46.8%); Western University of Health Sciences, Pomona, California (46%); William Carey University College of Osteopathic Medicine, Hattiesburg, Mississippi (44.7%); and A.T. Still University of Health Sciences, Kirksville, Missouri (44.3%).
Best for research
When it comes to schools ranking the highest for research, the Grossman School of Medicine at New York University takes the no. 2 spot after Harvard. Three schools were tied for the no. 3 spot: Columbia University, Johns Hopkins University, and the University of California, San Francisco; and two schools for no. 6: Duke University and the Perelman School of Medicine at the University of Pennsylvania, Philadelphia. No. 8 goes to Stanford University, followed by the University of Washington. Rounding out the top 10 is Yale University.
Specialty ranks
The top-ranked schools in eight specialties are as follows:
- Anesthesiology: Harvard
- Family medicine: the University of Washington
- Internal medicine: Johns Hopkins
- Obstetrics/gynecology: Harvard
- Pediatrics: the University of Pennsylvania (Perelman)
- Psychiatry: Harvard
- Radiology: Johns Hopkins
- Surgery: Harvard
Most diverse student body
If you’re looking for a school with significant minority representation, Howard University, Washington, D.C., ranked highest (76.8%), followed by the Wertheim College of Medicine at Florida International University, Miami (43.2%). The University of California, Davis (40%), Sacramento, California, and the University of Vermont (Larner), Burlington (14.1%), tied for third.
Three southern schools take top honors for the most graduates practicing in underserved areas, starting with the University of South Carolina (70.9%), followed by the University of Mississippi (66.2%), and East Tennessee State University (Quillen), Johnson City, Tennessee (65.8%).
The colleges with the most graduates practicing in rural areas are William Carey University College of Osteopathic Medicine (28%), the University of Pikesville (25.6%), and the University of Mississippi (22.1%).
College debt
The medical school where graduates have the most debt is Nova Southeastern University Patel College of Osteopathic Medicine, Fort Lauderdale, Florida. Graduates incurred an average debt of $309,206. Western University of Health Sciences graduates racked up $276,840 in debt, followed by graduates of West Virginia School of Osteopathic Medicine, owing $268,416.
Ranking criteria
Each year, U.S. News ranks hundreds of U.S. colleges and universities. Medical schools fall under the rankings for best graduate schools.
U.S. News surveyed 192 medical and osteopathic schools accredited in 2021 by the Liaison Committee on Medical Education or the American Osteopathic Association. Among the schools surveyed in fall 2021 and early 2022, 130 schools responded. Of those, 124 were included in both the research and primary care rankings.
The criteria for ranking include faculty resources, academic achievements of entering students, and qualitative assessments by schools and residency directors.
A version of this article first appeared on Medscape.com.
It may seem like déjà vu, as not much has changed regarding the rankings of top U.S. medical schools over the past 2 years.
The University of Washington, Seattle retained its ranking from the U.S. News & World Report as the top medical school for primary care for 2023. Also repeating its 2022 standing as the top medical school for research is Harvard University.
In the primary care ranking, the top 10 schools after the University of Washington were the University of California, San Francisco; the University of Minnesota; Oregon Health and Science University; the University of North Carolina at Chapel Hill; the University of Colorado; the University of Nebraska Medical Center; the University of California, Davis; and Harvard. Three schools tied for the no. 10 slot: the University of Kansas Medical Center, the University of Massachusetts Chan Medical Center, and the University of Pittsburgh.
The top five schools with the most graduates practicing in primary care specialties are Des Moines University, Iowa (50.6%); the University of Pikeville (Ky.) (46.8%); Western University of Health Sciences, Pomona, California (46%); William Carey University College of Osteopathic Medicine, Hattiesburg, Mississippi (44.7%); and A.T. Still University of Health Sciences, Kirksville, Missouri (44.3%).
Best for research
When it comes to schools ranking the highest for research, the Grossman School of Medicine at New York University takes the no. 2 spot after Harvard. Three schools were tied for the no. 3 spot: Columbia University, Johns Hopkins University, and the University of California, San Francisco; and two schools for no. 6: Duke University and the Perelman School of Medicine at the University of Pennsylvania, Philadelphia. No. 8 goes to Stanford University, followed by the University of Washington. Rounding out the top 10 is Yale University.
Specialty ranks
The top-ranked schools in eight specialties are as follows:
- Anesthesiology: Harvard
- Family medicine: the University of Washington
- Internal medicine: Johns Hopkins
- Obstetrics/gynecology: Harvard
- Pediatrics: the University of Pennsylvania (Perelman)
- Psychiatry: Harvard
- Radiology: Johns Hopkins
- Surgery: Harvard
Most diverse student body
If you’re looking for a school with significant minority representation, Howard University, Washington, D.C., ranked highest (76.8%), followed by the Wertheim College of Medicine at Florida International University, Miami (43.2%). The University of California, Davis (40%), Sacramento, California, and the University of Vermont (Larner), Burlington (14.1%), tied for third.
Three southern schools take top honors for the most graduates practicing in underserved areas, starting with the University of South Carolina (70.9%), followed by the University of Mississippi (66.2%), and East Tennessee State University (Quillen), Johnson City, Tennessee (65.8%).
The colleges with the most graduates practicing in rural areas are William Carey University College of Osteopathic Medicine (28%), the University of Pikesville (25.6%), and the University of Mississippi (22.1%).
College debt
The medical school where graduates have the most debt is Nova Southeastern University Patel College of Osteopathic Medicine, Fort Lauderdale, Florida. Graduates incurred an average debt of $309,206. Western University of Health Sciences graduates racked up $276,840 in debt, followed by graduates of West Virginia School of Osteopathic Medicine, owing $268,416.
Ranking criteria
Each year, U.S. News ranks hundreds of U.S. colleges and universities. Medical schools fall under the rankings for best graduate schools.
U.S. News surveyed 192 medical and osteopathic schools accredited in 2021 by the Liaison Committee on Medical Education or the American Osteopathic Association. Among the schools surveyed in fall 2021 and early 2022, 130 schools responded. Of those, 124 were included in both the research and primary care rankings.
The criteria for ranking include faculty resources, academic achievements of entering students, and qualitative assessments by schools and residency directors.
A version of this article first appeared on Medscape.com.
Combo of SGLT2 inhibitor + GLP-1 RA boosts diabetes survival
WASHINGTON – Patients with type 2 diabetes and established atherosclerotic cardiovascular disease treated with both an sodium-glucose transporter 2 inhibitor and a glucagonlike peptide–1 receptor agonist had a significant 80% cut in their rate of all-cause death during 1-year follow-up, compared with matched patients treated with an agent from either class alone in an observational, retrospective study of more than 15,000 people in the U.S. Veterans Affairs health system.
For the study’s primary endpoint, the combined rate of all-cause death, nonfatal MI, or nonfatal stroke, combined treatment with both an agent from the sodium-glucose transporter 2 (SGLT2) inhibitor class and from the glucagonlike peptide–1 receptor agonist (GLP-1 RA) class linked with a significant, roughly 50% cut in events during 1-year follow-up, compared with patients treated with an agent from just one of these two classes, Persio D. Lopez, MD, reported at the annual scientific sessions of the American College of Cardiology.
This improvement in the combined endpoint outcome resulted entirely from reduced all-cause mortality. Dual treatment showed no significant association with the incidence of nonfatal MIs or strokes, compared with monotherapy, with rates that were nearly identical regardless of whether patients took one of the agents or both, said Dr. Lopez, a cardiologist at Mount Sinai Morningside and the James J. Peters VA Medical Center, both in New York.
Combining classes for hard-to-control diabetes
“We’re not sure what drives combined use” of agents from both drug classes in these types of patients, admitted Dr. Lopez during his talk. “Our hypothesis is that dual treatment is used in patients with harder-to-control diabetes.”
Salim S. Virani, MD, PhD, who practices in the VA system but was not involved with the study, agreed that this is the likely explanation for most instances of high-risk VA patients with diabetes who receive agents from both classes.
“I have a few patients” on both classes, usually “patients with higher starting A1c levels who need greater glycemic control,” said Dr. Virani, professor of medicine at Baylor College of Medicine and a cardiologist at the Michael E. DeBakey VA Medical Center, both in Houston.
U.S. use of either drug class, let alone both, in patients with type 2 diabetes is still struggling to gain traction in U.S. practice and remains limited to a minority of these patients, a prescribing pattern reflected in recent VA data. Analysis of more than half a million patients in the VA system with type 2 diabetes and atherosclerotic cardiovascular disease (ASCVD) who received treatment at any of 130 VA medical centers throughout 2020 showed that 11% had received an SGLT2 inhibitor, and 8% a GLP-1 RA.
The most frequently used antidiabetes drug classes in these patients were insulin in 36%, biguanides in 47%, and sulfonylureas in 22%.
These data also showed a striking level of variability among the 130 VA centers, with some of the sites prescribing either an SGLT2 inhibitor or a GLP-1 RA to as few as about 3% each of these patients, while other centers had a roughly 10-fold higher prescription rate for each of about 25%-30% of their patients with type 2 diabetes and ASCVD.
Despite the overall modest level of use of both classes in these types of patients as recently as 2020, no barriers exist at the VA to prescribing an agent from one or both classes “if you provide a good reason” for a patient to receive the drugs, Dr. Virani said in an interview. He also predicted that use of both classes in these patients, including combination treatment, will likely soon expand.
‘A lot of interest’ in combining an SGLT2 inhibitor and a GLP-1 RA
“There will be a lot of interest in combing the two classes. It makes intuitive sense [to treat with both classes] because most patients with diabetes need more than one drug” for glycemic control, he noted. “Why not use two classes that each reduce a patient’s risk” for adverse outcomes involving ASCVD, heart failure, and renal dysfunction, added Dr. Virani.
The study run by Dr. Lopez and his associates used data collected in the National VA Database and included 121,156 patients with both type 2 diabetes and established ASCVD. Using propensity-score matching the researchers compiled three subgroups that each included 5,277 matched patients. One subgroup had patients prescribed an SGLT2 inhibitor, a second subgroup included patients on a GLP-1 RA, and a third subgroup had patients on agents from both classes. Patient matching relied on age, sex, left ventricular ejection fraction, hemoglobin A1c level, systolic blood pressure, and the presence of coronary artery disease or peripheral artery disease.
Patients included in the analysis averaged about 67 years of age; 97% were men, their average body mass index was about 34 kg/m2, their average A1c was about 7.9%, their average estimated glomerular filtration rate was about 55-66 mL/min per 1.73 m2, and their average left ventricular ejection fraction was about 55%. The database provided a median follow-up of 902 days (about 2.5 years). The prespecified primary endpoint focused on events that occurred during the first year of follow-up, but the investigators also ran a 3-year follow-up analysis on a post hoc basis.
The most common SGLT2 inhibitor received by these patients was empagliflozin (Jardiance), used on virtually everyone who received an agent from this class. In contrast, the GLP-1 RA drugs that patients received split more widely. The most prescribed agent was liraglutide (Victoza), followed by semaglutide (Ozempic), and dulaglutide (Trulicity), with fewer than 5% receiving exenatide (Bydureon, Byetta).
Regarding other treatments, about 97% of all patients received a statin, about 94% were on a renin-angiotensin system inhibitor, about 90% were on metformin, and roughly 75% were on insulin, aspirin, and a beta-blocker, with smaller numbers on other types of agents.
For the study’s primary endpoint, the 1-year incidence of combined ASCVD events including all-cause death, patients on agents from both classes had a significant 46% reduced rate compared with those on an SGLT2 inhibitor only, and a significant 49% reduced rate, compared with those on a GLP-1 RA only. These between-group separations broadened slightly during 3-year follow-up. Dr. Lopez did not report results of a direct comparison between patients on just an SGLT2 inhibitor and those on just a GLP-1 RA.
For the endpoint of all-cause death, those on combined treatment had a 1-year rate that was 83% below the rate among patients on only an SGLT2 inhibitor, and 81% below the rate among patients who received a GLP-1 RA but not the other class.
Dr. Lopez cautioned that selection bias could have influenced the outcomes of patients who received both classes rather than one or the other, and he also highlighted that the analysis relied on administrative data rather than information gleaned from more detailed medical records or prospectively collected findings and was limited by only including a very small number of women.
“Our results need to be validated in prospective studies,” he declared.
Dr. Lopez and Dr. Virani had no commercial disclosures.
WASHINGTON – Patients with type 2 diabetes and established atherosclerotic cardiovascular disease treated with both an sodium-glucose transporter 2 inhibitor and a glucagonlike peptide–1 receptor agonist had a significant 80% cut in their rate of all-cause death during 1-year follow-up, compared with matched patients treated with an agent from either class alone in an observational, retrospective study of more than 15,000 people in the U.S. Veterans Affairs health system.
For the study’s primary endpoint, the combined rate of all-cause death, nonfatal MI, or nonfatal stroke, combined treatment with both an agent from the sodium-glucose transporter 2 (SGLT2) inhibitor class and from the glucagonlike peptide–1 receptor agonist (GLP-1 RA) class linked with a significant, roughly 50% cut in events during 1-year follow-up, compared with patients treated with an agent from just one of these two classes, Persio D. Lopez, MD, reported at the annual scientific sessions of the American College of Cardiology.
This improvement in the combined endpoint outcome resulted entirely from reduced all-cause mortality. Dual treatment showed no significant association with the incidence of nonfatal MIs or strokes, compared with monotherapy, with rates that were nearly identical regardless of whether patients took one of the agents or both, said Dr. Lopez, a cardiologist at Mount Sinai Morningside and the James J. Peters VA Medical Center, both in New York.
Combining classes for hard-to-control diabetes
“We’re not sure what drives combined use” of agents from both drug classes in these types of patients, admitted Dr. Lopez during his talk. “Our hypothesis is that dual treatment is used in patients with harder-to-control diabetes.”
Salim S. Virani, MD, PhD, who practices in the VA system but was not involved with the study, agreed that this is the likely explanation for most instances of high-risk VA patients with diabetes who receive agents from both classes.
“I have a few patients” on both classes, usually “patients with higher starting A1c levels who need greater glycemic control,” said Dr. Virani, professor of medicine at Baylor College of Medicine and a cardiologist at the Michael E. DeBakey VA Medical Center, both in Houston.
U.S. use of either drug class, let alone both, in patients with type 2 diabetes is still struggling to gain traction in U.S. practice and remains limited to a minority of these patients, a prescribing pattern reflected in recent VA data. Analysis of more than half a million patients in the VA system with type 2 diabetes and atherosclerotic cardiovascular disease (ASCVD) who received treatment at any of 130 VA medical centers throughout 2020 showed that 11% had received an SGLT2 inhibitor, and 8% a GLP-1 RA.
The most frequently used antidiabetes drug classes in these patients were insulin in 36%, biguanides in 47%, and sulfonylureas in 22%.
These data also showed a striking level of variability among the 130 VA centers, with some of the sites prescribing either an SGLT2 inhibitor or a GLP-1 RA to as few as about 3% each of these patients, while other centers had a roughly 10-fold higher prescription rate for each of about 25%-30% of their patients with type 2 diabetes and ASCVD.
Despite the overall modest level of use of both classes in these types of patients as recently as 2020, no barriers exist at the VA to prescribing an agent from one or both classes “if you provide a good reason” for a patient to receive the drugs, Dr. Virani said in an interview. He also predicted that use of both classes in these patients, including combination treatment, will likely soon expand.
‘A lot of interest’ in combining an SGLT2 inhibitor and a GLP-1 RA
“There will be a lot of interest in combing the two classes. It makes intuitive sense [to treat with both classes] because most patients with diabetes need more than one drug” for glycemic control, he noted. “Why not use two classes that each reduce a patient’s risk” for adverse outcomes involving ASCVD, heart failure, and renal dysfunction, added Dr. Virani.
The study run by Dr. Lopez and his associates used data collected in the National VA Database and included 121,156 patients with both type 2 diabetes and established ASCVD. Using propensity-score matching the researchers compiled three subgroups that each included 5,277 matched patients. One subgroup had patients prescribed an SGLT2 inhibitor, a second subgroup included patients on a GLP-1 RA, and a third subgroup had patients on agents from both classes. Patient matching relied on age, sex, left ventricular ejection fraction, hemoglobin A1c level, systolic blood pressure, and the presence of coronary artery disease or peripheral artery disease.
Patients included in the analysis averaged about 67 years of age; 97% were men, their average body mass index was about 34 kg/m2, their average A1c was about 7.9%, their average estimated glomerular filtration rate was about 55-66 mL/min per 1.73 m2, and their average left ventricular ejection fraction was about 55%. The database provided a median follow-up of 902 days (about 2.5 years). The prespecified primary endpoint focused on events that occurred during the first year of follow-up, but the investigators also ran a 3-year follow-up analysis on a post hoc basis.
The most common SGLT2 inhibitor received by these patients was empagliflozin (Jardiance), used on virtually everyone who received an agent from this class. In contrast, the GLP-1 RA drugs that patients received split more widely. The most prescribed agent was liraglutide (Victoza), followed by semaglutide (Ozempic), and dulaglutide (Trulicity), with fewer than 5% receiving exenatide (Bydureon, Byetta).
Regarding other treatments, about 97% of all patients received a statin, about 94% were on a renin-angiotensin system inhibitor, about 90% were on metformin, and roughly 75% were on insulin, aspirin, and a beta-blocker, with smaller numbers on other types of agents.
For the study’s primary endpoint, the 1-year incidence of combined ASCVD events including all-cause death, patients on agents from both classes had a significant 46% reduced rate compared with those on an SGLT2 inhibitor only, and a significant 49% reduced rate, compared with those on a GLP-1 RA only. These between-group separations broadened slightly during 3-year follow-up. Dr. Lopez did not report results of a direct comparison between patients on just an SGLT2 inhibitor and those on just a GLP-1 RA.
For the endpoint of all-cause death, those on combined treatment had a 1-year rate that was 83% below the rate among patients on only an SGLT2 inhibitor, and 81% below the rate among patients who received a GLP-1 RA but not the other class.
Dr. Lopez cautioned that selection bias could have influenced the outcomes of patients who received both classes rather than one or the other, and he also highlighted that the analysis relied on administrative data rather than information gleaned from more detailed medical records or prospectively collected findings and was limited by only including a very small number of women.
“Our results need to be validated in prospective studies,” he declared.
Dr. Lopez and Dr. Virani had no commercial disclosures.
WASHINGTON – Patients with type 2 diabetes and established atherosclerotic cardiovascular disease treated with both an sodium-glucose transporter 2 inhibitor and a glucagonlike peptide–1 receptor agonist had a significant 80% cut in their rate of all-cause death during 1-year follow-up, compared with matched patients treated with an agent from either class alone in an observational, retrospective study of more than 15,000 people in the U.S. Veterans Affairs health system.
For the study’s primary endpoint, the combined rate of all-cause death, nonfatal MI, or nonfatal stroke, combined treatment with both an agent from the sodium-glucose transporter 2 (SGLT2) inhibitor class and from the glucagonlike peptide–1 receptor agonist (GLP-1 RA) class linked with a significant, roughly 50% cut in events during 1-year follow-up, compared with patients treated with an agent from just one of these two classes, Persio D. Lopez, MD, reported at the annual scientific sessions of the American College of Cardiology.
This improvement in the combined endpoint outcome resulted entirely from reduced all-cause mortality. Dual treatment showed no significant association with the incidence of nonfatal MIs or strokes, compared with monotherapy, with rates that were nearly identical regardless of whether patients took one of the agents or both, said Dr. Lopez, a cardiologist at Mount Sinai Morningside and the James J. Peters VA Medical Center, both in New York.
Combining classes for hard-to-control diabetes
“We’re not sure what drives combined use” of agents from both drug classes in these types of patients, admitted Dr. Lopez during his talk. “Our hypothesis is that dual treatment is used in patients with harder-to-control diabetes.”
Salim S. Virani, MD, PhD, who practices in the VA system but was not involved with the study, agreed that this is the likely explanation for most instances of high-risk VA patients with diabetes who receive agents from both classes.
“I have a few patients” on both classes, usually “patients with higher starting A1c levels who need greater glycemic control,” said Dr. Virani, professor of medicine at Baylor College of Medicine and a cardiologist at the Michael E. DeBakey VA Medical Center, both in Houston.
U.S. use of either drug class, let alone both, in patients with type 2 diabetes is still struggling to gain traction in U.S. practice and remains limited to a minority of these patients, a prescribing pattern reflected in recent VA data. Analysis of more than half a million patients in the VA system with type 2 diabetes and atherosclerotic cardiovascular disease (ASCVD) who received treatment at any of 130 VA medical centers throughout 2020 showed that 11% had received an SGLT2 inhibitor, and 8% a GLP-1 RA.
The most frequently used antidiabetes drug classes in these patients were insulin in 36%, biguanides in 47%, and sulfonylureas in 22%.
These data also showed a striking level of variability among the 130 VA centers, with some of the sites prescribing either an SGLT2 inhibitor or a GLP-1 RA to as few as about 3% each of these patients, while other centers had a roughly 10-fold higher prescription rate for each of about 25%-30% of their patients with type 2 diabetes and ASCVD.
Despite the overall modest level of use of both classes in these types of patients as recently as 2020, no barriers exist at the VA to prescribing an agent from one or both classes “if you provide a good reason” for a patient to receive the drugs, Dr. Virani said in an interview. He also predicted that use of both classes in these patients, including combination treatment, will likely soon expand.
‘A lot of interest’ in combining an SGLT2 inhibitor and a GLP-1 RA
“There will be a lot of interest in combing the two classes. It makes intuitive sense [to treat with both classes] because most patients with diabetes need more than one drug” for glycemic control, he noted. “Why not use two classes that each reduce a patient’s risk” for adverse outcomes involving ASCVD, heart failure, and renal dysfunction, added Dr. Virani.
The study run by Dr. Lopez and his associates used data collected in the National VA Database and included 121,156 patients with both type 2 diabetes and established ASCVD. Using propensity-score matching the researchers compiled three subgroups that each included 5,277 matched patients. One subgroup had patients prescribed an SGLT2 inhibitor, a second subgroup included patients on a GLP-1 RA, and a third subgroup had patients on agents from both classes. Patient matching relied on age, sex, left ventricular ejection fraction, hemoglobin A1c level, systolic blood pressure, and the presence of coronary artery disease or peripheral artery disease.
Patients included in the analysis averaged about 67 years of age; 97% were men, their average body mass index was about 34 kg/m2, their average A1c was about 7.9%, their average estimated glomerular filtration rate was about 55-66 mL/min per 1.73 m2, and their average left ventricular ejection fraction was about 55%. The database provided a median follow-up of 902 days (about 2.5 years). The prespecified primary endpoint focused on events that occurred during the first year of follow-up, but the investigators also ran a 3-year follow-up analysis on a post hoc basis.
The most common SGLT2 inhibitor received by these patients was empagliflozin (Jardiance), used on virtually everyone who received an agent from this class. In contrast, the GLP-1 RA drugs that patients received split more widely. The most prescribed agent was liraglutide (Victoza), followed by semaglutide (Ozempic), and dulaglutide (Trulicity), with fewer than 5% receiving exenatide (Bydureon, Byetta).
Regarding other treatments, about 97% of all patients received a statin, about 94% were on a renin-angiotensin system inhibitor, about 90% were on metformin, and roughly 75% were on insulin, aspirin, and a beta-blocker, with smaller numbers on other types of agents.
For the study’s primary endpoint, the 1-year incidence of combined ASCVD events including all-cause death, patients on agents from both classes had a significant 46% reduced rate compared with those on an SGLT2 inhibitor only, and a significant 49% reduced rate, compared with those on a GLP-1 RA only. These between-group separations broadened slightly during 3-year follow-up. Dr. Lopez did not report results of a direct comparison between patients on just an SGLT2 inhibitor and those on just a GLP-1 RA.
For the endpoint of all-cause death, those on combined treatment had a 1-year rate that was 83% below the rate among patients on only an SGLT2 inhibitor, and 81% below the rate among patients who received a GLP-1 RA but not the other class.
Dr. Lopez cautioned that selection bias could have influenced the outcomes of patients who received both classes rather than one or the other, and he also highlighted that the analysis relied on administrative data rather than information gleaned from more detailed medical records or prospectively collected findings and was limited by only including a very small number of women.
“Our results need to be validated in prospective studies,” he declared.
Dr. Lopez and Dr. Virani had no commercial disclosures.
AT ACC 2022
New smart device shows highly accurate AFib detection: mAFA II
Screening for heart rhythm disorders with a smartphone app and a wearable device had a high rate of correctly detecting atrial fibrillation (AFib) in a large new study.
The mAFA II study, conducted in a mass low-risk population in China, showed that more than 93% of possible AFib episodes detected by the smartphone app were confirmed to be AFib on further monitoring.
The study also used the app to screen for obstructive sleep apnea and found that sleep apnea was the most common risk factor associated with increased AFib susceptibility, and those identified as having the most severe sleep apnea were 1.5 times more likely to have AFib than those who did not have this condition.
This suggests that tools suitable for detecting both AFib and sleep apnea can work synergistically to further enhance health monitoring, said lead author, Yutao Guo, MD, professor of internal medicine at Chinese PLA General Hospital, Beijing.
Dr. Guo presented the mAFA II study at the American College of Cardiology (ACC) 2022 Scientific Session held in Washington, D.C., and online.
The trial, which involved more than 2.8 million participants, is the largest study to date to demonstrate how wearable consumer technologies can be used to screen for heart problems during everyday activities, Dr. Guo noted.
“Consumer-led screening with these technologies could increase early diagnosis of AFib and facilitate an integrated approach to fully implement clustered risk management to reduce AFib burden and its related complications,” she concluded.
Discussant of the study at the ACC session at which it was presented, Jodie Hurwitz, MD, Director of the Electrophysiology Lab at Medical City Hospital, Dallas, called this “a pretty impressive study. To get a 93.8% confirmation of AFib with these devices is great.”
But Dr. Hurwitz pointed out that the age of patients in the study was relatively young (average 37 years), and the group who really need to use such a device is much older than that.
“The take-home messages from this study are that AFib wearable detection algorithms have the ability to detect true AFib and that they might also be able to detect risk factors (such as sleep apnea) that predispose to AFib possibly even before AFib is present,” Dr. Hurwitz commented.
Moderator of the session, Edward Fry, MD, cardiologist at Ascension St. Vincent Heart Center, Indianapolis, and incoming president of the ACC, described the area of AFib screening with smart devices as “fascinating, especially with the perspective of the scalability of these types of studies.”
The mAFA II study tracked more than 2.8 million people who used a Huawei phone app together with Huawei and Honor smart devices incorporating photoplethysmography (PPG) technology, a light-based method to monitor blood flow and pulse. If an abnormal rhythm was detected, the wearer would be contacted by a clinician to set up an appointment for a clinical assessment.
Over the course of 4 years of the study, 12,244 (0.4%) of users received a notification of suspected AFib. Among 5,227 people who chose to follow up with a clinician, AFib was confirmed in 93.8% of patients using standard AFib diagnostic tools, including clinical evaluation, an electrocardiogram, and 24-hour Holter monitoring.
In this study, a subset of the individuals screened for AFib were also screened for signs of sleep apnea using the same PPG technology to detect physiological changes in parameters including oxygenation and respiratory rates. The app is also able to determine whether the individual is awake or asleep. Dr. Guo noted that the PPG algorithm for obstructive sleep apnea risk has been validated, compared with polysomnography or home sleep apnea tests.
Using measurements of apnea (signalled by a reduced respiratory rate) and hypopnea (when oxygenation would decrease), the apnea–hypopnea index (AHI) is calculated to determine the severity of the sleep apnea.
Of the 961,931 participants screened for sleep apnea, about 18,000 were notified they may have the condition.
Obstructive sleep apnea was the most reported common risk factor associated with increased AFib susceptibility, and those individuals with the highest risk sleep apnea (more than 80% monitoring measures with AHI greater than or equal to 30 during sleep) resulted in a 1.5-fold increase in prevalent AFib, Dr. Guo reported.
The mAFA II is the latest of several studies to show that AFib can be detected with various smartphone apps and wearable devices. Previous studies have included the Fitbit Heart Study and the Apple Heart Study.
Dr. Hurwitz told this news organization that the electrophysiologist community is enthusiastic about this new smart device technology.
“I sent my sister one so she could determine if she develops AFib: That’s a pretty good endorsement,” she commented, but added that there are still concerns about the rate of false-positive results.
Dr. Hurwitz said she suspected that there will probably be meaningful differences between the different apps and devices, but the algorithms are all proprietary, and the use of photoplethysmography seems to make a big difference.
She noted that the detection of sleep apnea in the current study was a novel approach. “This is important, as sleep apnea is felt to contribute to AFib, and treating it is felt to decrease the frequency of AFib. Perhaps if patients with sleep apnea were treated before they had documented AFib, the AFib burden could be reduced,” she said.
She added that further studies were needed to fine tune the algorithms and to try and identify other factors or heart rate variabilities that may predict future risk of AFib.
The study was funded by the National Natural Science Foundation of China. Dr. Guo reports no disclosures.
A version of this article first appeared on Medscape.com.
Screening for heart rhythm disorders with a smartphone app and a wearable device had a high rate of correctly detecting atrial fibrillation (AFib) in a large new study.
The mAFA II study, conducted in a mass low-risk population in China, showed that more than 93% of possible AFib episodes detected by the smartphone app were confirmed to be AFib on further monitoring.
The study also used the app to screen for obstructive sleep apnea and found that sleep apnea was the most common risk factor associated with increased AFib susceptibility, and those identified as having the most severe sleep apnea were 1.5 times more likely to have AFib than those who did not have this condition.
This suggests that tools suitable for detecting both AFib and sleep apnea can work synergistically to further enhance health monitoring, said lead author, Yutao Guo, MD, professor of internal medicine at Chinese PLA General Hospital, Beijing.
Dr. Guo presented the mAFA II study at the American College of Cardiology (ACC) 2022 Scientific Session held in Washington, D.C., and online.
The trial, which involved more than 2.8 million participants, is the largest study to date to demonstrate how wearable consumer technologies can be used to screen for heart problems during everyday activities, Dr. Guo noted.
“Consumer-led screening with these technologies could increase early diagnosis of AFib and facilitate an integrated approach to fully implement clustered risk management to reduce AFib burden and its related complications,” she concluded.
Discussant of the study at the ACC session at which it was presented, Jodie Hurwitz, MD, Director of the Electrophysiology Lab at Medical City Hospital, Dallas, called this “a pretty impressive study. To get a 93.8% confirmation of AFib with these devices is great.”
But Dr. Hurwitz pointed out that the age of patients in the study was relatively young (average 37 years), and the group who really need to use such a device is much older than that.
“The take-home messages from this study are that AFib wearable detection algorithms have the ability to detect true AFib and that they might also be able to detect risk factors (such as sleep apnea) that predispose to AFib possibly even before AFib is present,” Dr. Hurwitz commented.
Moderator of the session, Edward Fry, MD, cardiologist at Ascension St. Vincent Heart Center, Indianapolis, and incoming president of the ACC, described the area of AFib screening with smart devices as “fascinating, especially with the perspective of the scalability of these types of studies.”
The mAFA II study tracked more than 2.8 million people who used a Huawei phone app together with Huawei and Honor smart devices incorporating photoplethysmography (PPG) technology, a light-based method to monitor blood flow and pulse. If an abnormal rhythm was detected, the wearer would be contacted by a clinician to set up an appointment for a clinical assessment.
Over the course of 4 years of the study, 12,244 (0.4%) of users received a notification of suspected AFib. Among 5,227 people who chose to follow up with a clinician, AFib was confirmed in 93.8% of patients using standard AFib diagnostic tools, including clinical evaluation, an electrocardiogram, and 24-hour Holter monitoring.
In this study, a subset of the individuals screened for AFib were also screened for signs of sleep apnea using the same PPG technology to detect physiological changes in parameters including oxygenation and respiratory rates. The app is also able to determine whether the individual is awake or asleep. Dr. Guo noted that the PPG algorithm for obstructive sleep apnea risk has been validated, compared with polysomnography or home sleep apnea tests.
Using measurements of apnea (signalled by a reduced respiratory rate) and hypopnea (when oxygenation would decrease), the apnea–hypopnea index (AHI) is calculated to determine the severity of the sleep apnea.
Of the 961,931 participants screened for sleep apnea, about 18,000 were notified they may have the condition.
Obstructive sleep apnea was the most reported common risk factor associated with increased AFib susceptibility, and those individuals with the highest risk sleep apnea (more than 80% monitoring measures with AHI greater than or equal to 30 during sleep) resulted in a 1.5-fold increase in prevalent AFib, Dr. Guo reported.
The mAFA II is the latest of several studies to show that AFib can be detected with various smartphone apps and wearable devices. Previous studies have included the Fitbit Heart Study and the Apple Heart Study.
Dr. Hurwitz told this news organization that the electrophysiologist community is enthusiastic about this new smart device technology.
“I sent my sister one so she could determine if she develops AFib: That’s a pretty good endorsement,” she commented, but added that there are still concerns about the rate of false-positive results.
Dr. Hurwitz said she suspected that there will probably be meaningful differences between the different apps and devices, but the algorithms are all proprietary, and the use of photoplethysmography seems to make a big difference.
She noted that the detection of sleep apnea in the current study was a novel approach. “This is important, as sleep apnea is felt to contribute to AFib, and treating it is felt to decrease the frequency of AFib. Perhaps if patients with sleep apnea were treated before they had documented AFib, the AFib burden could be reduced,” she said.
She added that further studies were needed to fine tune the algorithms and to try and identify other factors or heart rate variabilities that may predict future risk of AFib.
The study was funded by the National Natural Science Foundation of China. Dr. Guo reports no disclosures.
A version of this article first appeared on Medscape.com.
Screening for heart rhythm disorders with a smartphone app and a wearable device had a high rate of correctly detecting atrial fibrillation (AFib) in a large new study.
The mAFA II study, conducted in a mass low-risk population in China, showed that more than 93% of possible AFib episodes detected by the smartphone app were confirmed to be AFib on further monitoring.
The study also used the app to screen for obstructive sleep apnea and found that sleep apnea was the most common risk factor associated with increased AFib susceptibility, and those identified as having the most severe sleep apnea were 1.5 times more likely to have AFib than those who did not have this condition.
This suggests that tools suitable for detecting both AFib and sleep apnea can work synergistically to further enhance health monitoring, said lead author, Yutao Guo, MD, professor of internal medicine at Chinese PLA General Hospital, Beijing.
Dr. Guo presented the mAFA II study at the American College of Cardiology (ACC) 2022 Scientific Session held in Washington, D.C., and online.
The trial, which involved more than 2.8 million participants, is the largest study to date to demonstrate how wearable consumer technologies can be used to screen for heart problems during everyday activities, Dr. Guo noted.
“Consumer-led screening with these technologies could increase early diagnosis of AFib and facilitate an integrated approach to fully implement clustered risk management to reduce AFib burden and its related complications,” she concluded.
Discussant of the study at the ACC session at which it was presented, Jodie Hurwitz, MD, Director of the Electrophysiology Lab at Medical City Hospital, Dallas, called this “a pretty impressive study. To get a 93.8% confirmation of AFib with these devices is great.”
But Dr. Hurwitz pointed out that the age of patients in the study was relatively young (average 37 years), and the group who really need to use such a device is much older than that.
“The take-home messages from this study are that AFib wearable detection algorithms have the ability to detect true AFib and that they might also be able to detect risk factors (such as sleep apnea) that predispose to AFib possibly even before AFib is present,” Dr. Hurwitz commented.
Moderator of the session, Edward Fry, MD, cardiologist at Ascension St. Vincent Heart Center, Indianapolis, and incoming president of the ACC, described the area of AFib screening with smart devices as “fascinating, especially with the perspective of the scalability of these types of studies.”
The mAFA II study tracked more than 2.8 million people who used a Huawei phone app together with Huawei and Honor smart devices incorporating photoplethysmography (PPG) technology, a light-based method to monitor blood flow and pulse. If an abnormal rhythm was detected, the wearer would be contacted by a clinician to set up an appointment for a clinical assessment.
Over the course of 4 years of the study, 12,244 (0.4%) of users received a notification of suspected AFib. Among 5,227 people who chose to follow up with a clinician, AFib was confirmed in 93.8% of patients using standard AFib diagnostic tools, including clinical evaluation, an electrocardiogram, and 24-hour Holter monitoring.
In this study, a subset of the individuals screened for AFib were also screened for signs of sleep apnea using the same PPG technology to detect physiological changes in parameters including oxygenation and respiratory rates. The app is also able to determine whether the individual is awake or asleep. Dr. Guo noted that the PPG algorithm for obstructive sleep apnea risk has been validated, compared with polysomnography or home sleep apnea tests.
Using measurements of apnea (signalled by a reduced respiratory rate) and hypopnea (when oxygenation would decrease), the apnea–hypopnea index (AHI) is calculated to determine the severity of the sleep apnea.
Of the 961,931 participants screened for sleep apnea, about 18,000 were notified they may have the condition.
Obstructive sleep apnea was the most reported common risk factor associated with increased AFib susceptibility, and those individuals with the highest risk sleep apnea (more than 80% monitoring measures with AHI greater than or equal to 30 during sleep) resulted in a 1.5-fold increase in prevalent AFib, Dr. Guo reported.
The mAFA II is the latest of several studies to show that AFib can be detected with various smartphone apps and wearable devices. Previous studies have included the Fitbit Heart Study and the Apple Heart Study.
Dr. Hurwitz told this news organization that the electrophysiologist community is enthusiastic about this new smart device technology.
“I sent my sister one so she could determine if she develops AFib: That’s a pretty good endorsement,” she commented, but added that there are still concerns about the rate of false-positive results.
Dr. Hurwitz said she suspected that there will probably be meaningful differences between the different apps and devices, but the algorithms are all proprietary, and the use of photoplethysmography seems to make a big difference.
She noted that the detection of sleep apnea in the current study was a novel approach. “This is important, as sleep apnea is felt to contribute to AFib, and treating it is felt to decrease the frequency of AFib. Perhaps if patients with sleep apnea were treated before they had documented AFib, the AFib burden could be reduced,” she said.
She added that further studies were needed to fine tune the algorithms and to try and identify other factors or heart rate variabilities that may predict future risk of AFib.
The study was funded by the National Natural Science Foundation of China. Dr. Guo reports no disclosures.
A version of this article first appeared on Medscape.com.
Diagnosing PTSD: Heart rate variability may help
, according to a study published in Frontiers in Psychiatry.
It is estimated that between 8% and 15% of clinically recognized pregnancies and up to 30% of all pregnancies result in miscarriage – a loss that can be devastating for everyone. There are limited data on the strength of the association between perinatal loss and subsequent common mental health disorders, such as anxiety, depression, and PTSD. The prevalence of PTSD among this group is still unknown, and one of the factors that contribute to the absence of data is that diagnostic evaluation is subjective.
To address this issue, researchers from Anhembi Morumbi University (UAM) in São José dos Campos, Brazil, along with teams in the United States and United Arab Emirates (UAE), investigated biomarkers for the severity of PTSD. The hope is that the research will enable psychiatrists to assess women who experience pregnancy loss more objectively. Study author Ovidiu Constantin Baltatu, MD, PhD, a professor at Brazil’s UAM and the UAE’s Khalifa University, spoke to this news organization about the study.
Under the guidance of Dr. Baltatu, psychologist Cláudia de Faria Cardoso carried out the research as part of her studies in biomedical engineering at UAM. Fifty-three women were recruited; the average age of the cohort was 33 years. All participants had a history of at least one perinatal loss. Pregnancy loss intervals ranged from less than 40 days to more than 6 months.
Participants completed a clinical interview and a questionnaire; PTSD symptoms were assessed on the basis of criteria in the DSM-5. The instrument used for the assessment was the Brazilian version of the Post-traumatic Stress Disorder Checklist (PCL-5). In addition, to evaluate general autonomic dysfunction, patients completed the Composite Autonomic Symptom Score 31 (COMPASS-31) questionnaire.
HRV was assessed during a deep breathing test using an HRV scanner system with wireless electrocardiography that enabled real-time data analysis and visualization. The investigators examined the following HRV measures: standard deviation (SD) of normal R-R wave intervals (SDNN), square root of the mean of the sum of the squares of differences between adjacent normal R wave intervals, and the number of all R-R intervals in which the change in consecutive normal sinus intervals exceeds 50 ms divided by the total number of R-R intervals measured.
Of the 53 participants, 25 had been diagnosed with pregnancy loss–induced PTSD. The results indicated a significant association between PCL-5 scores and HRV indices. The SDNN index effectively distinguished between patients with PTSD and those without.
To Dr. Baltatu, HRV indices reflect dysfunction of the autonomic nervous system (ANS), one of the major neural pathways activated by stress.
Although the deep breathing test has been around for a long time, it’s not widely used in current clinical practice, he said. According to him, maximum and minimum heart rates during breathing at six cycles per minute can typically be used to calculate the inspiratory-to-expiratory ratio, thus providing an indication of ANS function. “Our group introduced the study of HRV during deep breathing test, which is a step forward,” he said.
The methodology used by the team was well received by the participants. “With the deep breathing test, the women were able to look at a screen and see real-time graphics displaying the stress that they were experiencing after having suffered trauma. This visualization of objective measures was perceived as an improved care,” said Dr. Baltatu.
In general, HRV provides a more objective means of diagnosing PTSD. “Normally, PTSD is assessed through a questionnaire and an interview with psychologists,” said Dr. Baltatu. The subjectivity of the assessment is one of the main factors associated with the underdiagnosis of this condition, he explained.
It is important to remember that other factors, such as a lack of awareness about the problem, also hinder the diagnosis of PTSD in this population, Dr. Baltatu added. Women who have had a miscarriage often don’t think that their symptoms may result from PTSD. This fact highlights why it is so important that hospitals have a clinical psychologist on staff. In addition, Dr. Baltatu pointed out that a woman who experiences a pregnancy loss usually has negative memories of the hospital and is therefore reluctant to reach out for professional help. “In our study, all psychological care and assessments took place outside of a hospital setting, which the participants seemed to appreciate,” he emphasized.
Dr. Baltatu and his team are conducting follow-up research. The preliminary results indicate that the biomarkers identified in the study are promising in the assessment of patients’ clinical progress. This finding may reflect the fact that the HRV indices have proven useful not only in diagnosing but also in monitoring women in treatment, because they are able to identify which patients are responding better to treatment.
A version of this article first appeared on Medscape.com.
, according to a study published in Frontiers in Psychiatry.
It is estimated that between 8% and 15% of clinically recognized pregnancies and up to 30% of all pregnancies result in miscarriage – a loss that can be devastating for everyone. There are limited data on the strength of the association between perinatal loss and subsequent common mental health disorders, such as anxiety, depression, and PTSD. The prevalence of PTSD among this group is still unknown, and one of the factors that contribute to the absence of data is that diagnostic evaluation is subjective.
To address this issue, researchers from Anhembi Morumbi University (UAM) in São José dos Campos, Brazil, along with teams in the United States and United Arab Emirates (UAE), investigated biomarkers for the severity of PTSD. The hope is that the research will enable psychiatrists to assess women who experience pregnancy loss more objectively. Study author Ovidiu Constantin Baltatu, MD, PhD, a professor at Brazil’s UAM and the UAE’s Khalifa University, spoke to this news organization about the study.
Under the guidance of Dr. Baltatu, psychologist Cláudia de Faria Cardoso carried out the research as part of her studies in biomedical engineering at UAM. Fifty-three women were recruited; the average age of the cohort was 33 years. All participants had a history of at least one perinatal loss. Pregnancy loss intervals ranged from less than 40 days to more than 6 months.
Participants completed a clinical interview and a questionnaire; PTSD symptoms were assessed on the basis of criteria in the DSM-5. The instrument used for the assessment was the Brazilian version of the Post-traumatic Stress Disorder Checklist (PCL-5). In addition, to evaluate general autonomic dysfunction, patients completed the Composite Autonomic Symptom Score 31 (COMPASS-31) questionnaire.
HRV was assessed during a deep breathing test using an HRV scanner system with wireless electrocardiography that enabled real-time data analysis and visualization. The investigators examined the following HRV measures: standard deviation (SD) of normal R-R wave intervals (SDNN), square root of the mean of the sum of the squares of differences between adjacent normal R wave intervals, and the number of all R-R intervals in which the change in consecutive normal sinus intervals exceeds 50 ms divided by the total number of R-R intervals measured.
Of the 53 participants, 25 had been diagnosed with pregnancy loss–induced PTSD. The results indicated a significant association between PCL-5 scores and HRV indices. The SDNN index effectively distinguished between patients with PTSD and those without.
To Dr. Baltatu, HRV indices reflect dysfunction of the autonomic nervous system (ANS), one of the major neural pathways activated by stress.
Although the deep breathing test has been around for a long time, it’s not widely used in current clinical practice, he said. According to him, maximum and minimum heart rates during breathing at six cycles per minute can typically be used to calculate the inspiratory-to-expiratory ratio, thus providing an indication of ANS function. “Our group introduced the study of HRV during deep breathing test, which is a step forward,” he said.
The methodology used by the team was well received by the participants. “With the deep breathing test, the women were able to look at a screen and see real-time graphics displaying the stress that they were experiencing after having suffered trauma. This visualization of objective measures was perceived as an improved care,” said Dr. Baltatu.
In general, HRV provides a more objective means of diagnosing PTSD. “Normally, PTSD is assessed through a questionnaire and an interview with psychologists,” said Dr. Baltatu. The subjectivity of the assessment is one of the main factors associated with the underdiagnosis of this condition, he explained.
It is important to remember that other factors, such as a lack of awareness about the problem, also hinder the diagnosis of PTSD in this population, Dr. Baltatu added. Women who have had a miscarriage often don’t think that their symptoms may result from PTSD. This fact highlights why it is so important that hospitals have a clinical psychologist on staff. In addition, Dr. Baltatu pointed out that a woman who experiences a pregnancy loss usually has negative memories of the hospital and is therefore reluctant to reach out for professional help. “In our study, all psychological care and assessments took place outside of a hospital setting, which the participants seemed to appreciate,” he emphasized.
Dr. Baltatu and his team are conducting follow-up research. The preliminary results indicate that the biomarkers identified in the study are promising in the assessment of patients’ clinical progress. This finding may reflect the fact that the HRV indices have proven useful not only in diagnosing but also in monitoring women in treatment, because they are able to identify which patients are responding better to treatment.
A version of this article first appeared on Medscape.com.
, according to a study published in Frontiers in Psychiatry.
It is estimated that between 8% and 15% of clinically recognized pregnancies and up to 30% of all pregnancies result in miscarriage – a loss that can be devastating for everyone. There are limited data on the strength of the association between perinatal loss and subsequent common mental health disorders, such as anxiety, depression, and PTSD. The prevalence of PTSD among this group is still unknown, and one of the factors that contribute to the absence of data is that diagnostic evaluation is subjective.
To address this issue, researchers from Anhembi Morumbi University (UAM) in São José dos Campos, Brazil, along with teams in the United States and United Arab Emirates (UAE), investigated biomarkers for the severity of PTSD. The hope is that the research will enable psychiatrists to assess women who experience pregnancy loss more objectively. Study author Ovidiu Constantin Baltatu, MD, PhD, a professor at Brazil’s UAM and the UAE’s Khalifa University, spoke to this news organization about the study.
Under the guidance of Dr. Baltatu, psychologist Cláudia de Faria Cardoso carried out the research as part of her studies in biomedical engineering at UAM. Fifty-three women were recruited; the average age of the cohort was 33 years. All participants had a history of at least one perinatal loss. Pregnancy loss intervals ranged from less than 40 days to more than 6 months.
Participants completed a clinical interview and a questionnaire; PTSD symptoms were assessed on the basis of criteria in the DSM-5. The instrument used for the assessment was the Brazilian version of the Post-traumatic Stress Disorder Checklist (PCL-5). In addition, to evaluate general autonomic dysfunction, patients completed the Composite Autonomic Symptom Score 31 (COMPASS-31) questionnaire.
HRV was assessed during a deep breathing test using an HRV scanner system with wireless electrocardiography that enabled real-time data analysis and visualization. The investigators examined the following HRV measures: standard deviation (SD) of normal R-R wave intervals (SDNN), square root of the mean of the sum of the squares of differences between adjacent normal R wave intervals, and the number of all R-R intervals in which the change in consecutive normal sinus intervals exceeds 50 ms divided by the total number of R-R intervals measured.
Of the 53 participants, 25 had been diagnosed with pregnancy loss–induced PTSD. The results indicated a significant association between PCL-5 scores and HRV indices. The SDNN index effectively distinguished between patients with PTSD and those without.
To Dr. Baltatu, HRV indices reflect dysfunction of the autonomic nervous system (ANS), one of the major neural pathways activated by stress.
Although the deep breathing test has been around for a long time, it’s not widely used in current clinical practice, he said. According to him, maximum and minimum heart rates during breathing at six cycles per minute can typically be used to calculate the inspiratory-to-expiratory ratio, thus providing an indication of ANS function. “Our group introduced the study of HRV during deep breathing test, which is a step forward,” he said.
The methodology used by the team was well received by the participants. “With the deep breathing test, the women were able to look at a screen and see real-time graphics displaying the stress that they were experiencing after having suffered trauma. This visualization of objective measures was perceived as an improved care,” said Dr. Baltatu.
In general, HRV provides a more objective means of diagnosing PTSD. “Normally, PTSD is assessed through a questionnaire and an interview with psychologists,” said Dr. Baltatu. The subjectivity of the assessment is one of the main factors associated with the underdiagnosis of this condition, he explained.
It is important to remember that other factors, such as a lack of awareness about the problem, also hinder the diagnosis of PTSD in this population, Dr. Baltatu added. Women who have had a miscarriage often don’t think that their symptoms may result from PTSD. This fact highlights why it is so important that hospitals have a clinical psychologist on staff. In addition, Dr. Baltatu pointed out that a woman who experiences a pregnancy loss usually has negative memories of the hospital and is therefore reluctant to reach out for professional help. “In our study, all psychological care and assessments took place outside of a hospital setting, which the participants seemed to appreciate,” he emphasized.
Dr. Baltatu and his team are conducting follow-up research. The preliminary results indicate that the biomarkers identified in the study are promising in the assessment of patients’ clinical progress. This finding may reflect the fact that the HRV indices have proven useful not only in diagnosing but also in monitoring women in treatment, because they are able to identify which patients are responding better to treatment.
A version of this article first appeared on Medscape.com.
FROM FRONTIERS IN PSYCHIATRY