User login
Acne is a common and distressing condition that typically presents in adolescents and young adults and has been associated with not only medical but also emotional and aesthetic consequences. Acne treatments that offer faster improvement are the coveted goal. Although clinical studies support the use of combination therapy with topical retinoids and antibiotics, the overuse of antibiotics raises caution for bacterial resistance.1 Therefore, adjunctive treatments such as chemical peels, light therapy, and laser treatments can hasten the response to traditional acne treatments and in some cases may potentially decrease use of both oral and topical antibiotics.
Light therapy, particularly with visible light, may improve acne outcomes. Pneumatic broadband light (PBBL) is a light treatment in the broadband range (400–1200 nm) combined with a vacuum. The suction created by the vacuum has several effects on acne lesions, such as creating a mechanical lysis of thin-walled pustules and dislodging pore impaction. The blue light with a wavelength of 410 nm targets endogenous porphyrins in Propionibacterium acnes and elicits singlet oxygen production, resulting in bacterial destruction.2,3 Studies showed that PBBL alone was effective in most patients with mild to moderate acne and caused minimal side effects.2-4
We sought to determine if PBBL combined with a topical retinoid can accelerate and prolong acne improvement. We evaluated the efficacy, safety, and tolerability of PBBL plus adapalene gel 0.3% versus adapalene gel 0.3% monotherapy in patients with mild to moderate acne.
METHODSPatient Population
Patients with mild to moderate acne were eligible for the study if they were 18 years or older at screening, in good health, had stopped oral isotretinoin for at least 1 year prior to treatment initiation, and were not taking oral or topical antibiotics or using any topical retinoid derivatives for at least 1 month prior to treatment initiation. Inclusion criteria included at least 10 acne lesions on the face. Patients were excluded if they had a history of receiving PBBL treatment; had a history of scarring, hypopigmentation, or hyperpigmentation from laser or light treatments; and/or were pregnant or refused use of contraception during the study period.
Study Design
This single-blind, randomized, split-face study was approved by the institutional review board of the University of Pennsylvania (Philadelphia, Pennsylvania). All participants provided informed consent before entering the study. Each participant was randomly assigned to receive PBBL on one side of the face for 6 consecutive weeks and apply adapalene gel 0.3% to both sides of the face nightly for 10 weeks. Pneumatic broadband light treatment was performed using the following settings: starting power 2 (approximately 4–6 J/cm2) and vacuum setting 3 (negative pressure, approximately 3 lb/in2). The power setting was increased to a maximum of 6 (12–14 J/cm2) at subsequent visits depending on tolerability of the participants.
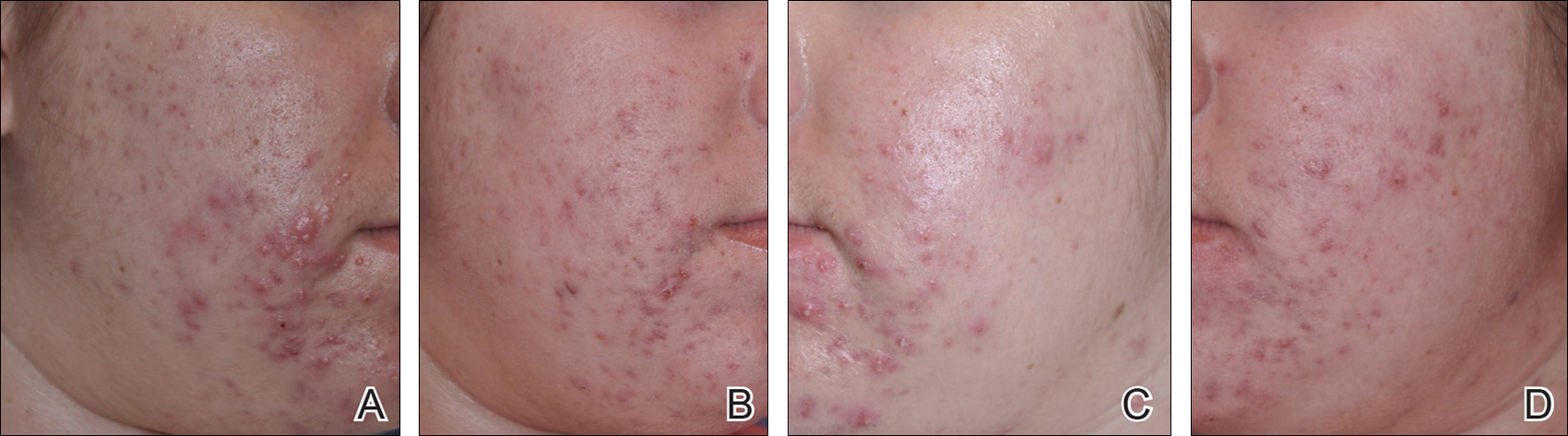
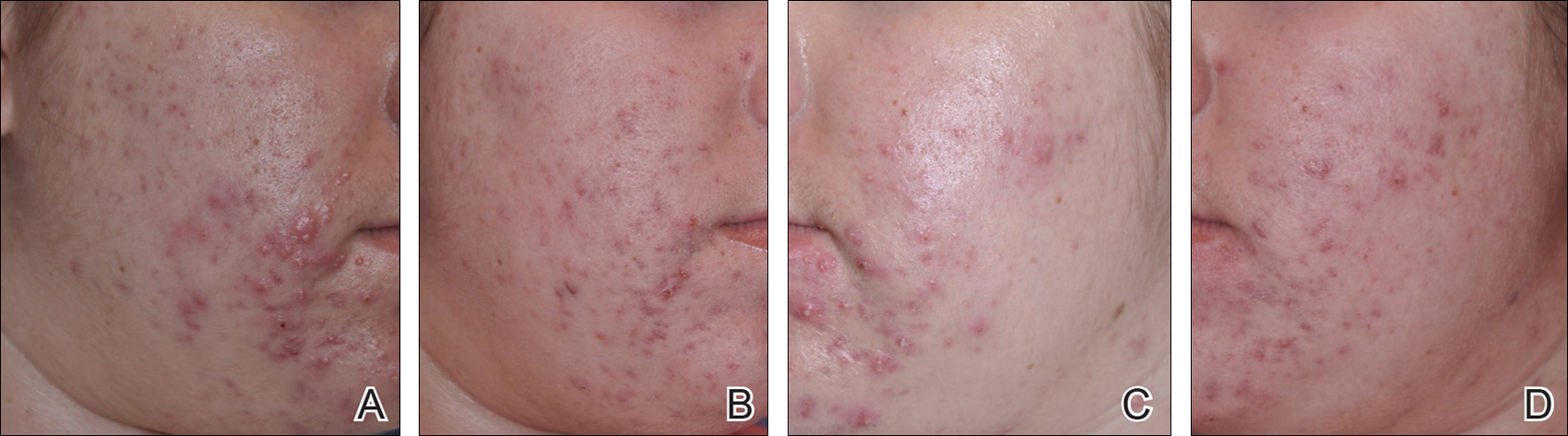
All participants visited the clinic weekly for 6 weeks and also returned for follow-up at week 10 (4 weeks following last PBBL treatment). At each visit, the participants completed satisfaction questionnaires and were assessed by a dermatologist evaluator using several parameters including the modified Global Acne Grading Score (mGAGS), clinical photography, participant self-assessment, physician assessment, and Wong Baker FACES Pain Rating Scale (WBPRS). The physician evaluator was blinded to the side of the face receiving PBBL treatment. Clinical photographs were taken to compare the clinical outcome at each visit versus baseline.
Efficacy Evaluation
Acne Counts
The blinded evaluator counted acne lesions and assessed the mGAGS at each visit prior to administration of the PBBL treatment. Acne lesions were counted separately as noninflammatory (comedones) and inflammatory (papules, pustules, nodules) on the forehead, cheeks, nose, and chin.
Modified Global Acne Grading Score
The modified Global Acne Grading Score was modified from the Global Acne Grading Scale (GAGS) that has previously been used to evaluate acne severity.5 The original GAGS used the type and location of the acne lesions. The GAGS considers 6 locations on the face, chest, and upper back, with a grading factor for each location (forehead=2; cheeks=2; nose=1; chin=1). Another grading factor represented the lesion type (0=no lesion; 1=comedone; 2=papule; 3=pustule; 4=nodule). The local score was calculated by multiplying the location grading factor by the lesion type grading factor. The total score was the sum of the individual local scores for the 4 locations.
Given that the number of acne lesions is important, we modified the GAGS by adding a grading factor that represented the number of lesions to improve the accuracy of the test (1=0–10 lesions; 2=11–20 lesions; 3=21–30 lesions; 4=≥31 lesions). The local score of mGAGS was calculated by multiplying the grading factors for location, lesion type, and number of lesions. Each local score was then added to yield a total score. The mGAGS may be useful and more accurate to determine the severity of acne (0=none; 1–44=mild; 45–80=moderate; 81–132=severe; 133–176=very severe).
Participant Self-assessment
Participants assessed their acne lesions using an 11-point rating scale (–5=100% worsening; –4=76%–99% worsening; –3=51%–75% worsening; –2=26%–50% worsening; –1=1%–25% worsening; 0=no improvement; 1=1%–25% improvement; 2=26%–50% improvement; 3=51%–75% improvement; 4=76%–99% improvement; 5=100% acne clear) to compare their acne at each treatment visit and week 10 follow-up with a baseline photograph.
Physician Assessment
The blinded evaluator assessed acne lesions on the face using the same 11-point rating scale that was used for participant self-assessment. For each participant, assessments were made at each treatment visit and week 10 follow-up by comparing baseline photographs.
Safety Evaluation
The WBPRS score, a standardized 6-point scale (0=no pain; 1=hurts a little bit; 2=hurts a little bit more; 3=hurts even more; 4=hurts whole lot; 5=hurt worst),6 was used to evaluate pain toleration during PBBL treatments and was recorded along with adverse events throughout the study.
Statistical Analysis
Based on data from 2 prior studies,3,7 we expected that the favorable clinical outcome of adapalene gel 0.3% and PBBL therapy would be 23% and 78%, respectively. If the adjunctive therapy with PBBL was beneficial, the favorable outcome would be higher than 78%. To be able to detect this difference, the sample size of 11 patients was needed when 5% type I error and 20% type II error were accepted.
Categorical variables were expressed as percentages, while continuous variables were expressed in terms of median (range). The clinical outcomes between both treatment groups were compared using the Wilcoxon signed rank test. A 2-tailed P value of ≤.05 was considered statistically significant. All statistical calculations were performed using STATA software version 10.0.
RESULTS
Baseline Characteristics
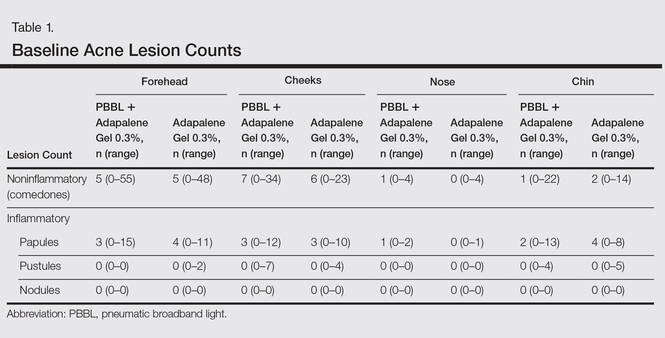
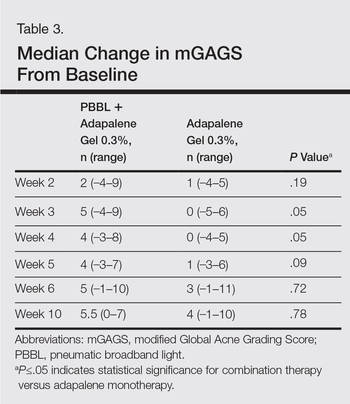
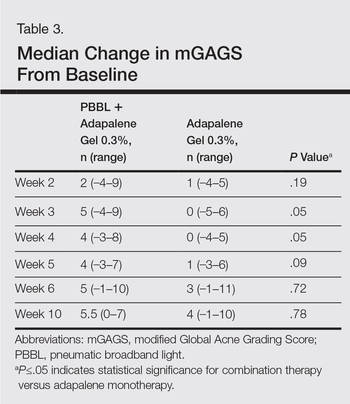
Four male and 7 female patients aged 18 to 35 years (median, 23 years) with mild to moderate acne were enrolled in the study. Of the 11 participants, 7 were white, 2 were black, 1 was Asian, and 1 was Latin American. Baseline characteristics of both sides of the face were comparable in all participants (Table 1). Eight participants (73%) completed the study. Two black participants withdrew from the study due to hyperpigmentation following PBBL treatment; 1 participant did not return for follow-up at week 10, as she was out of the country.
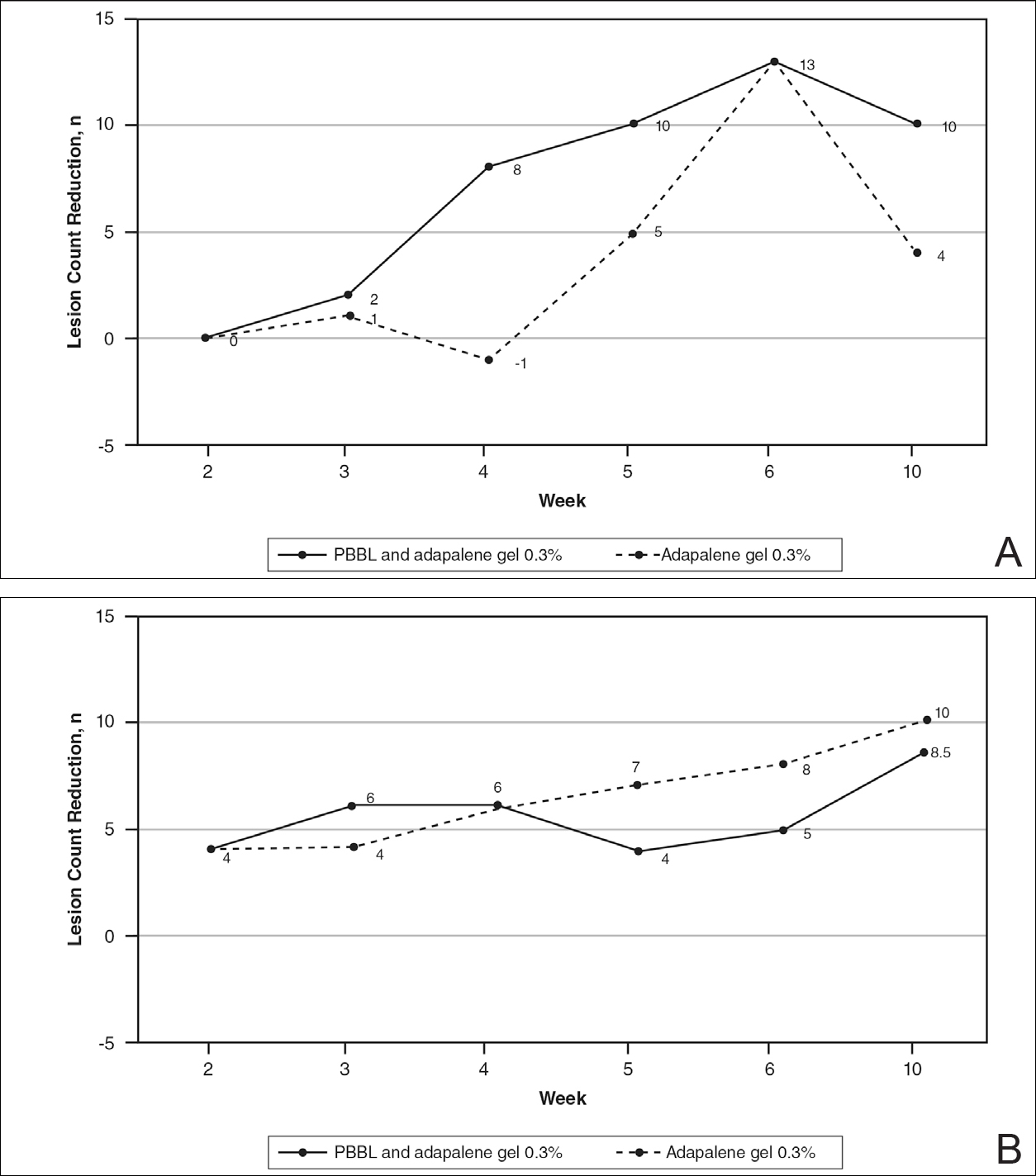
Lesion Counts
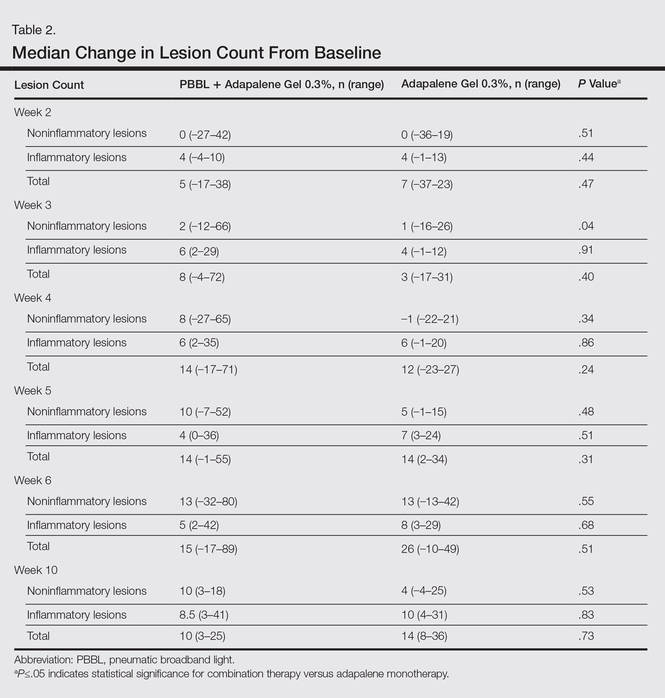
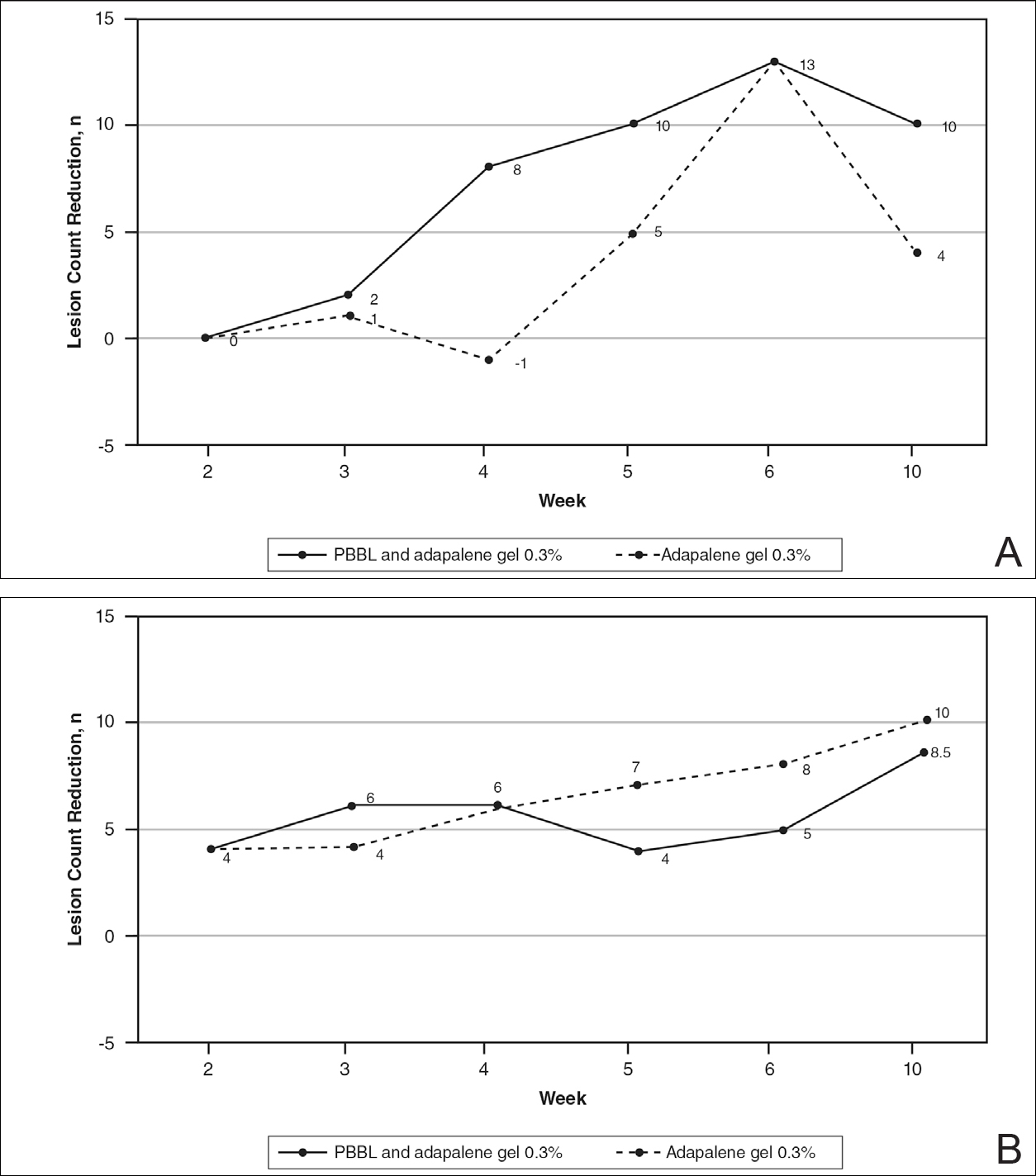
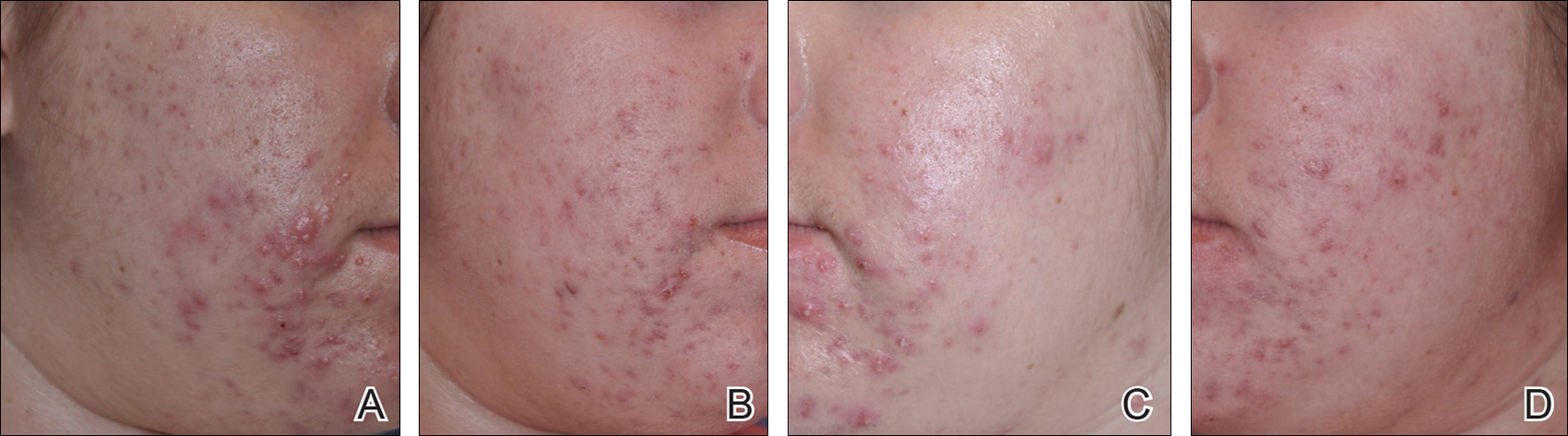
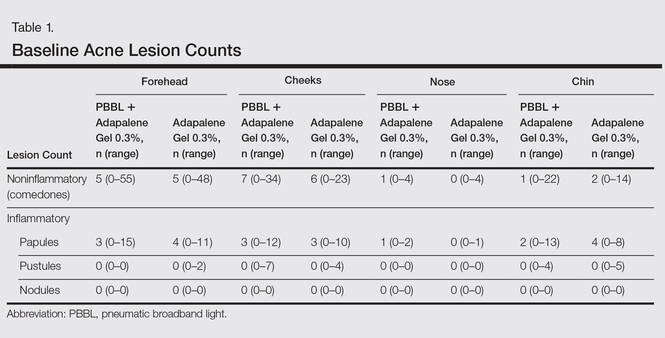
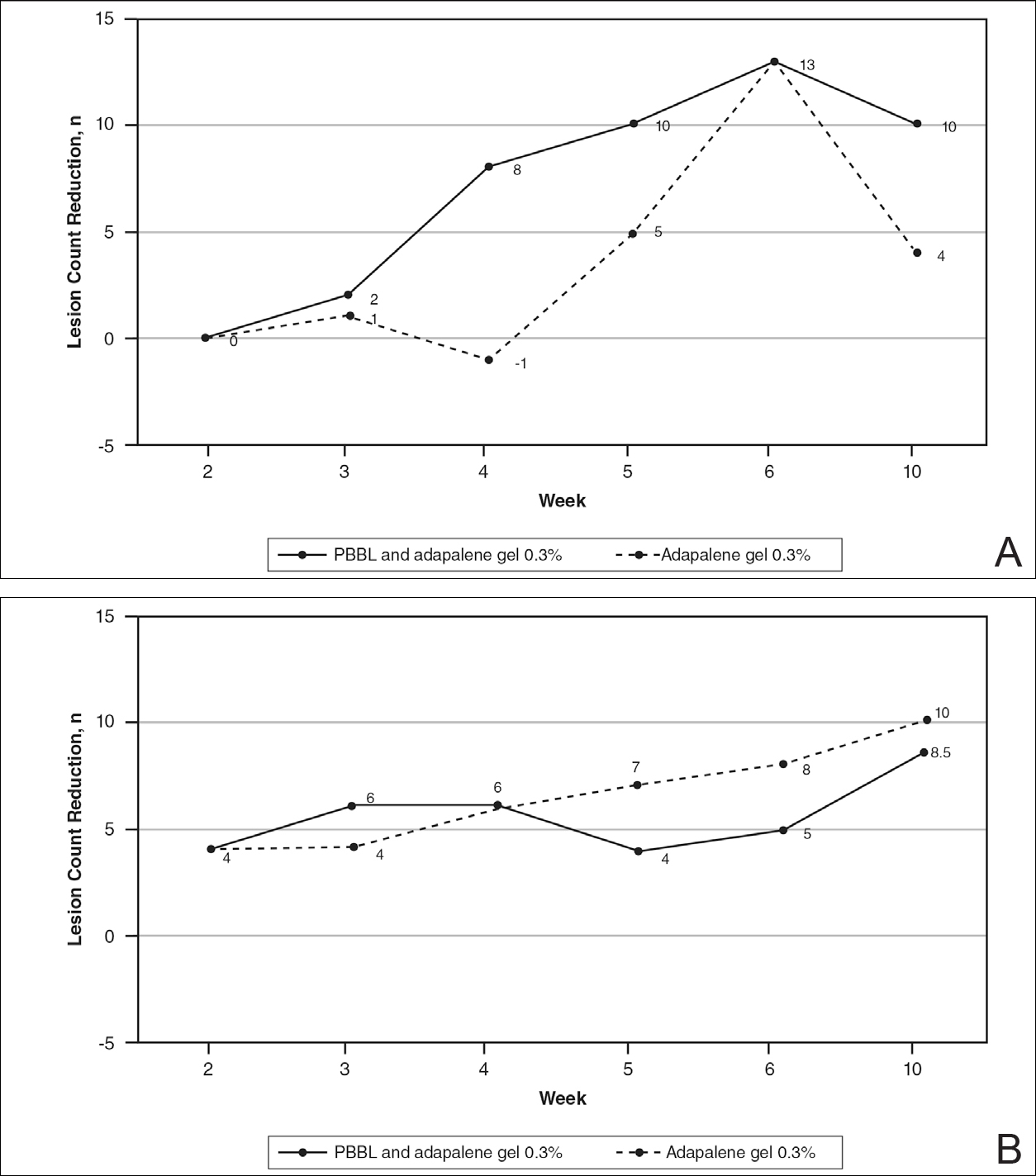
At week 3, reduction in noninflammatory lesions was significantly greater on the side receiving the combination therapy compared to the monotherapy side (P=.04)(Table 2). However, there was no significant difference between the combination therapy and the adapalene monotherapy sides in the reduction of noninflammatory and inflammatory lesions at week 4 (Figure 1). There was a remarkable improvement of the combination therapy and adapalene monotherapy sides in acne lesions, but there was no significant difference between the combination therapy and the adapalene monotherapy sides (Figure 2).
Modified Global Acne Grading Score
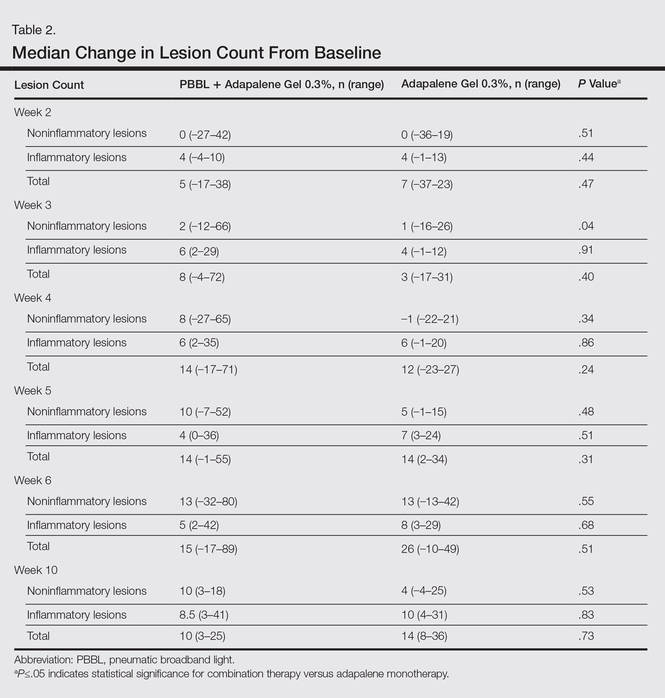
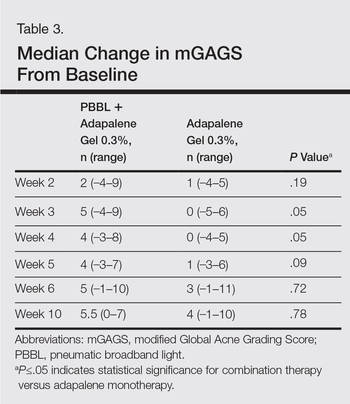
At weeks 3 and 4, the improvement of mGAGS was significantly greater on the side treated with the combination therapy (P=.05). However, this significant difference was not sustained (Table 3).
Participant Self-assessment and Physician Assessment
The rate of acne improvement according to participant self-assessment was slightly higher on the side receiving the combination therapy compared to the monotherapy side at week 2 (26%–50% vs 1%–25%) and week 6 (76%–99% vs 51%–75%). However, there was no statistically significant difference. For the physician assessment, there was no significant difference between the monotherapy and combination therapy sides.
Safety
The median WBPRS score was 1 (hurts a little bit) throughout all PBBL treatment visits. The maximum score was highest at week 1 (4=hurts whole lot) and subsequently decreased to 2 (hurts a little bit more) at week 6.
After the PBBL treatment, all participants experienced transient erythema in the treatment area. All participants noted their skin had become drier than usual from adapalene, except 1 participant (11%) who reported very dry skin on areas where adapalene gel 0.3% had been applied. However, the dryness was tolerable and relief was reported following application of a moisturizer. No participants withdrew from the study due to skin dryness.
Both black participants experienced hyperpigmentation caused by PBBL (1 on the treatment sites, the other on the test spot) and withdrew from the study. The hyperpigmentation resolved over time following application of a topical bleaching cream. One patient experienced purpura following PBBL treatment at week 4, which was associated with an increase in PBBL power. No other side effects (eg, scaling, stinging, burning, vesicle formation, blistering, crusting, scarring) were observed.
COMMENT
This 10-week study demonstrated that PBBL initially improved the appearance of acne in the first month of treatment, as determined by the significantly greater reduction in mGAGS for the combination side versus the adapalene monotherapy side. Differences in the reduction of acne lesions were not significant between the 2 treatments, except for noninflammatory lesion reduction at week 3. Analysis of physician assessment with photographs revealed acne improvement from baseline in the first month but no additional effects with the PBBL treatment at the end of study. Similarly, participant assessment indicated an improvement by week 2 with the combination therapy compared to adapalene monotherapy in their assessment of acne lesion reductions from baseline. By the end of the study, there was no significant difference between monotherapy and combination therapy.
These findings illustrate that combination therapy with PBBL plus adapalene improved the appearance of acne lesions within the first month of treatment, but there were no further signs of improvement at weeks 5 and 6. These results are consistent with at least 2 other studies that demonstrated acne reduction within the first 3 weeks of PBBL treatment.2,4 The current study was completed as planned with 6 weeks of combination therapy and patients continued adapalene application until the last follow-up visit in week 10. The length of the combination treatment was enough to determine that extension of treatment would not be necessary to gain any further benefits in this study. Because of the small sample size, we would not be able to detect any significant differences, as the difference between the combination therapy and the adapalene monotherapy was less than 55%. Therefore, a future study with a larger sample size is needed to draw a better conclusion.
Pneumatic broadband light has shown impressive results in acne treatment. However, some side effects need to be considered. Minimal adverse events have been reported such as erythema, dryness, peeling, burning, and itching.2-4 In this study, we found that all patients experienced transient erythema during and after PBBL treatment, but this effect disappeared in minutes. Purpura can occur if a higher power of PBBL is performed (6 or greater). Black patients experienced hyperpigmentation that can occur in darker skin types, as reported when light therapy is performed despite using the correct skin type tips.8 Therefore, care must be used in darker skin types, and we advocate a skin test in this population prior to general use.
Our study showed that PBBL can be safely combined with adapalene gel 0.3% and is well tolerated in the treatment of mild to moderate facial acne vulgaris for patients with Fitzpatrick skin types I to III. The combination of PBBL and adapalene reduces acne severity, as shown by the reduction in mGAGS during the first month of treatment. Patients noted faster improvement in their acne lesions with this combination. Although this study was limited by a relatively small sample size, this information may be useful in getting patients to be compliant overall, as they appeared to see results sooner, giving other therapies time to initiate their effect. It appears that 4 consecutive weekly treatments are enough to see that effect. Additionally, this combination therapy provides results without having to resort to oral antibiotics, as many patients today are concerned about creating future antibiotic resistance.
Conclusion
Adapalene gel 0.3% can be safely combined with PBBL for treatment of mild to moderate acne. Although the benefits of this combination therapy can be seen after 4 consecutive weekly treatments, the beneficial effect is not sustained.
Acknowledgment
The authors would like to thank Joyce Okawa, RN (Philadelphia, Pennsylvania), for her assistance in the submission to the University of Pennsylvania institutional review board.
- Thiboutot D, Gollnick H, Bettoli V, et al. New insights into the management of acne: an update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol. 2009;60(5 suppl):S1-S50.
- Gold MH, Biron J. Efficacy of a novel combination of pneumatic energy and broadband light for the treatment of acne. J Drugs Dermatol. 2008;7:639-642.
- Shamban AT, Enokibori M, Narurkar V, et al. Photopneumatic technology for the treatment of acne vulgaris. J Drugs Dermatol. 2008;7:139-145.
- Wanitphakdeedecha R, Tanzi EL, Alster TS. Photopneumatic therapy for the treatment of acne. J Drugs Dermatol. 2009;8:239-241.
- Doshi A, Zaheer A, Stiller MJ. A comparison of current acne grading systems and proposal of a novel system. Int J Dermatol. 1997;36:416-418.
- Wong DL, Baker CM. Pain in children: comparison of assessment scales. Pediatr Nurs. 1988;14:9-17.
- Thiboutot D, Pariser DM, Egan N, et al. Adapalene gel 0.3% for the treatment of acne vulgaris: a multicenter, randomized, double-blind, controlled, phase III trial. J Am Acad Dermatol. 2006;54:242-250.
- Yeung CK, Shek SY, Bjerring P, et al. A comparative study of intense pulsed light alone and its combination with photodynamic therapy for the treatment of facial acne in Asian skin. Lasers Surg Med. 2007;39:1-6.
Acne is a common and distressing condition that typically presents in adolescents and young adults and has been associated with not only medical but also emotional and aesthetic consequences. Acne treatments that offer faster improvement are the coveted goal. Although clinical studies support the use of combination therapy with topical retinoids and antibiotics, the overuse of antibiotics raises caution for bacterial resistance.1 Therefore, adjunctive treatments such as chemical peels, light therapy, and laser treatments can hasten the response to traditional acne treatments and in some cases may potentially decrease use of both oral and topical antibiotics.
Light therapy, particularly with visible light, may improve acne outcomes. Pneumatic broadband light (PBBL) is a light treatment in the broadband range (400–1200 nm) combined with a vacuum. The suction created by the vacuum has several effects on acne lesions, such as creating a mechanical lysis of thin-walled pustules and dislodging pore impaction. The blue light with a wavelength of 410 nm targets endogenous porphyrins in Propionibacterium acnes and elicits singlet oxygen production, resulting in bacterial destruction.2,3 Studies showed that PBBL alone was effective in most patients with mild to moderate acne and caused minimal side effects.2-4
We sought to determine if PBBL combined with a topical retinoid can accelerate and prolong acne improvement. We evaluated the efficacy, safety, and tolerability of PBBL plus adapalene gel 0.3% versus adapalene gel 0.3% monotherapy in patients with mild to moderate acne.
METHODSPatient Population
Patients with mild to moderate acne were eligible for the study if they were 18 years or older at screening, in good health, had stopped oral isotretinoin for at least 1 year prior to treatment initiation, and were not taking oral or topical antibiotics or using any topical retinoid derivatives for at least 1 month prior to treatment initiation. Inclusion criteria included at least 10 acne lesions on the face. Patients were excluded if they had a history of receiving PBBL treatment; had a history of scarring, hypopigmentation, or hyperpigmentation from laser or light treatments; and/or were pregnant or refused use of contraception during the study period.
Study Design
This single-blind, randomized, split-face study was approved by the institutional review board of the University of Pennsylvania (Philadelphia, Pennsylvania). All participants provided informed consent before entering the study. Each participant was randomly assigned to receive PBBL on one side of the face for 6 consecutive weeks and apply adapalene gel 0.3% to both sides of the face nightly for 10 weeks. Pneumatic broadband light treatment was performed using the following settings: starting power 2 (approximately 4–6 J/cm2) and vacuum setting 3 (negative pressure, approximately 3 lb/in2). The power setting was increased to a maximum of 6 (12–14 J/cm2) at subsequent visits depending on tolerability of the participants.
All participants visited the clinic weekly for 6 weeks and also returned for follow-up at week 10 (4 weeks following last PBBL treatment). At each visit, the participants completed satisfaction questionnaires and were assessed by a dermatologist evaluator using several parameters including the modified Global Acne Grading Score (mGAGS), clinical photography, participant self-assessment, physician assessment, and Wong Baker FACES Pain Rating Scale (WBPRS). The physician evaluator was blinded to the side of the face receiving PBBL treatment. Clinical photographs were taken to compare the clinical outcome at each visit versus baseline.
Efficacy Evaluation
Acne Counts
The blinded evaluator counted acne lesions and assessed the mGAGS at each visit prior to administration of the PBBL treatment. Acne lesions were counted separately as noninflammatory (comedones) and inflammatory (papules, pustules, nodules) on the forehead, cheeks, nose, and chin.
Modified Global Acne Grading Score
The modified Global Acne Grading Score was modified from the Global Acne Grading Scale (GAGS) that has previously been used to evaluate acne severity.5 The original GAGS used the type and location of the acne lesions. The GAGS considers 6 locations on the face, chest, and upper back, with a grading factor for each location (forehead=2; cheeks=2; nose=1; chin=1). Another grading factor represented the lesion type (0=no lesion; 1=comedone; 2=papule; 3=pustule; 4=nodule). The local score was calculated by multiplying the location grading factor by the lesion type grading factor. The total score was the sum of the individual local scores for the 4 locations.
Given that the number of acne lesions is important, we modified the GAGS by adding a grading factor that represented the number of lesions to improve the accuracy of the test (1=0–10 lesions; 2=11–20 lesions; 3=21–30 lesions; 4=≥31 lesions). The local score of mGAGS was calculated by multiplying the grading factors for location, lesion type, and number of lesions. Each local score was then added to yield a total score. The mGAGS may be useful and more accurate to determine the severity of acne (0=none; 1–44=mild; 45–80=moderate; 81–132=severe; 133–176=very severe).
Participant Self-assessment
Participants assessed their acne lesions using an 11-point rating scale (–5=100% worsening; –4=76%–99% worsening; –3=51%–75% worsening; –2=26%–50% worsening; –1=1%–25% worsening; 0=no improvement; 1=1%–25% improvement; 2=26%–50% improvement; 3=51%–75% improvement; 4=76%–99% improvement; 5=100% acne clear) to compare their acne at each treatment visit and week 10 follow-up with a baseline photograph.
Physician Assessment
The blinded evaluator assessed acne lesions on the face using the same 11-point rating scale that was used for participant self-assessment. For each participant, assessments were made at each treatment visit and week 10 follow-up by comparing baseline photographs.
Safety Evaluation
The WBPRS score, a standardized 6-point scale (0=no pain; 1=hurts a little bit; 2=hurts a little bit more; 3=hurts even more; 4=hurts whole lot; 5=hurt worst),6 was used to evaluate pain toleration during PBBL treatments and was recorded along with adverse events throughout the study.
Statistical Analysis
Based on data from 2 prior studies,3,7 we expected that the favorable clinical outcome of adapalene gel 0.3% and PBBL therapy would be 23% and 78%, respectively. If the adjunctive therapy with PBBL was beneficial, the favorable outcome would be higher than 78%. To be able to detect this difference, the sample size of 11 patients was needed when 5% type I error and 20% type II error were accepted.
Categorical variables were expressed as percentages, while continuous variables were expressed in terms of median (range). The clinical outcomes between both treatment groups were compared using the Wilcoxon signed rank test. A 2-tailed P value of ≤.05 was considered statistically significant. All statistical calculations were performed using STATA software version 10.0.
RESULTS
Baseline Characteristics
Four male and 7 female patients aged 18 to 35 years (median, 23 years) with mild to moderate acne were enrolled in the study. Of the 11 participants, 7 were white, 2 were black, 1 was Asian, and 1 was Latin American. Baseline characteristics of both sides of the face were comparable in all participants (Table 1). Eight participants (73%) completed the study. Two black participants withdrew from the study due to hyperpigmentation following PBBL treatment; 1 participant did not return for follow-up at week 10, as she was out of the country.
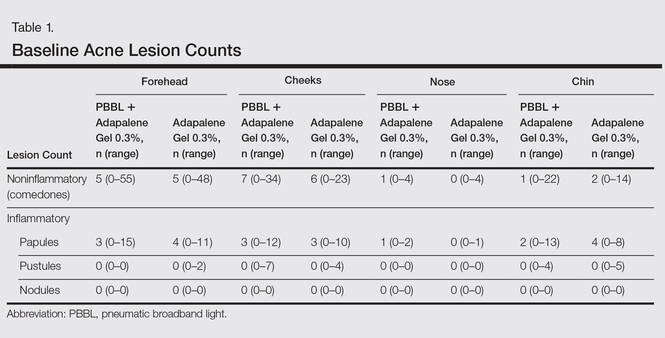
Lesion Counts
At week 3, reduction in noninflammatory lesions was significantly greater on the side receiving the combination therapy compared to the monotherapy side (P=.04)(Table 2). However, there was no significant difference between the combination therapy and the adapalene monotherapy sides in the reduction of noninflammatory and inflammatory lesions at week 4 (Figure 1). There was a remarkable improvement of the combination therapy and adapalene monotherapy sides in acne lesions, but there was no significant difference between the combination therapy and the adapalene monotherapy sides (Figure 2).
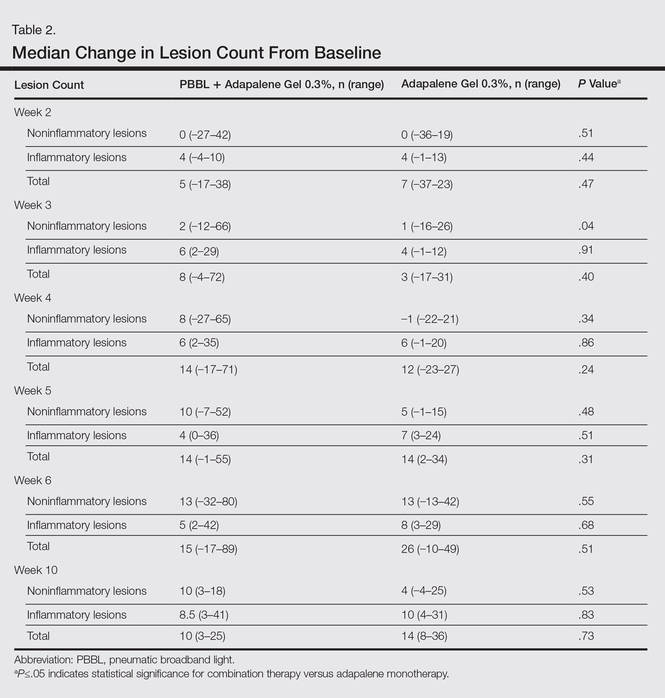
Modified Global Acne Grading Score
At weeks 3 and 4, the improvement of mGAGS was significantly greater on the side treated with the combination therapy (P=.05). However, this significant difference was not sustained (Table 3).
Participant Self-assessment and Physician Assessment
The rate of acne improvement according to participant self-assessment was slightly higher on the side receiving the combination therapy compared to the monotherapy side at week 2 (26%–50% vs 1%–25%) and week 6 (76%–99% vs 51%–75%). However, there was no statistically significant difference. For the physician assessment, there was no significant difference between the monotherapy and combination therapy sides.
Safety
The median WBPRS score was 1 (hurts a little bit) throughout all PBBL treatment visits. The maximum score was highest at week 1 (4=hurts whole lot) and subsequently decreased to 2 (hurts a little bit more) at week 6.
After the PBBL treatment, all participants experienced transient erythema in the treatment area. All participants noted their skin had become drier than usual from adapalene, except 1 participant (11%) who reported very dry skin on areas where adapalene gel 0.3% had been applied. However, the dryness was tolerable and relief was reported following application of a moisturizer. No participants withdrew from the study due to skin dryness.
Both black participants experienced hyperpigmentation caused by PBBL (1 on the treatment sites, the other on the test spot) and withdrew from the study. The hyperpigmentation resolved over time following application of a topical bleaching cream. One patient experienced purpura following PBBL treatment at week 4, which was associated with an increase in PBBL power. No other side effects (eg, scaling, stinging, burning, vesicle formation, blistering, crusting, scarring) were observed.
COMMENT
This 10-week study demonstrated that PBBL initially improved the appearance of acne in the first month of treatment, as determined by the significantly greater reduction in mGAGS for the combination side versus the adapalene monotherapy side. Differences in the reduction of acne lesions were not significant between the 2 treatments, except for noninflammatory lesion reduction at week 3. Analysis of physician assessment with photographs revealed acne improvement from baseline in the first month but no additional effects with the PBBL treatment at the end of study. Similarly, participant assessment indicated an improvement by week 2 with the combination therapy compared to adapalene monotherapy in their assessment of acne lesion reductions from baseline. By the end of the study, there was no significant difference between monotherapy and combination therapy.
These findings illustrate that combination therapy with PBBL plus adapalene improved the appearance of acne lesions within the first month of treatment, but there were no further signs of improvement at weeks 5 and 6. These results are consistent with at least 2 other studies that demonstrated acne reduction within the first 3 weeks of PBBL treatment.2,4 The current study was completed as planned with 6 weeks of combination therapy and patients continued adapalene application until the last follow-up visit in week 10. The length of the combination treatment was enough to determine that extension of treatment would not be necessary to gain any further benefits in this study. Because of the small sample size, we would not be able to detect any significant differences, as the difference between the combination therapy and the adapalene monotherapy was less than 55%. Therefore, a future study with a larger sample size is needed to draw a better conclusion.
Pneumatic broadband light has shown impressive results in acne treatment. However, some side effects need to be considered. Minimal adverse events have been reported such as erythema, dryness, peeling, burning, and itching.2-4 In this study, we found that all patients experienced transient erythema during and after PBBL treatment, but this effect disappeared in minutes. Purpura can occur if a higher power of PBBL is performed (6 or greater). Black patients experienced hyperpigmentation that can occur in darker skin types, as reported when light therapy is performed despite using the correct skin type tips.8 Therefore, care must be used in darker skin types, and we advocate a skin test in this population prior to general use.
Our study showed that PBBL can be safely combined with adapalene gel 0.3% and is well tolerated in the treatment of mild to moderate facial acne vulgaris for patients with Fitzpatrick skin types I to III. The combination of PBBL and adapalene reduces acne severity, as shown by the reduction in mGAGS during the first month of treatment. Patients noted faster improvement in their acne lesions with this combination. Although this study was limited by a relatively small sample size, this information may be useful in getting patients to be compliant overall, as they appeared to see results sooner, giving other therapies time to initiate their effect. It appears that 4 consecutive weekly treatments are enough to see that effect. Additionally, this combination therapy provides results without having to resort to oral antibiotics, as many patients today are concerned about creating future antibiotic resistance.
Conclusion
Adapalene gel 0.3% can be safely combined with PBBL for treatment of mild to moderate acne. Although the benefits of this combination therapy can be seen after 4 consecutive weekly treatments, the beneficial effect is not sustained.
Acknowledgment
The authors would like to thank Joyce Okawa, RN (Philadelphia, Pennsylvania), for her assistance in the submission to the University of Pennsylvania institutional review board.
Acne is a common and distressing condition that typically presents in adolescents and young adults and has been associated with not only medical but also emotional and aesthetic consequences. Acne treatments that offer faster improvement are the coveted goal. Although clinical studies support the use of combination therapy with topical retinoids and antibiotics, the overuse of antibiotics raises caution for bacterial resistance.1 Therefore, adjunctive treatments such as chemical peels, light therapy, and laser treatments can hasten the response to traditional acne treatments and in some cases may potentially decrease use of both oral and topical antibiotics.
Light therapy, particularly with visible light, may improve acne outcomes. Pneumatic broadband light (PBBL) is a light treatment in the broadband range (400–1200 nm) combined with a vacuum. The suction created by the vacuum has several effects on acne lesions, such as creating a mechanical lysis of thin-walled pustules and dislodging pore impaction. The blue light with a wavelength of 410 nm targets endogenous porphyrins in Propionibacterium acnes and elicits singlet oxygen production, resulting in bacterial destruction.2,3 Studies showed that PBBL alone was effective in most patients with mild to moderate acne and caused minimal side effects.2-4
We sought to determine if PBBL combined with a topical retinoid can accelerate and prolong acne improvement. We evaluated the efficacy, safety, and tolerability of PBBL plus adapalene gel 0.3% versus adapalene gel 0.3% monotherapy in patients with mild to moderate acne.
METHODSPatient Population
Patients with mild to moderate acne were eligible for the study if they were 18 years or older at screening, in good health, had stopped oral isotretinoin for at least 1 year prior to treatment initiation, and were not taking oral or topical antibiotics or using any topical retinoid derivatives for at least 1 month prior to treatment initiation. Inclusion criteria included at least 10 acne lesions on the face. Patients were excluded if they had a history of receiving PBBL treatment; had a history of scarring, hypopigmentation, or hyperpigmentation from laser or light treatments; and/or were pregnant or refused use of contraception during the study period.
Study Design
This single-blind, randomized, split-face study was approved by the institutional review board of the University of Pennsylvania (Philadelphia, Pennsylvania). All participants provided informed consent before entering the study. Each participant was randomly assigned to receive PBBL on one side of the face for 6 consecutive weeks and apply adapalene gel 0.3% to both sides of the face nightly for 10 weeks. Pneumatic broadband light treatment was performed using the following settings: starting power 2 (approximately 4–6 J/cm2) and vacuum setting 3 (negative pressure, approximately 3 lb/in2). The power setting was increased to a maximum of 6 (12–14 J/cm2) at subsequent visits depending on tolerability of the participants.
All participants visited the clinic weekly for 6 weeks and also returned for follow-up at week 10 (4 weeks following last PBBL treatment). At each visit, the participants completed satisfaction questionnaires and were assessed by a dermatologist evaluator using several parameters including the modified Global Acne Grading Score (mGAGS), clinical photography, participant self-assessment, physician assessment, and Wong Baker FACES Pain Rating Scale (WBPRS). The physician evaluator was blinded to the side of the face receiving PBBL treatment. Clinical photographs were taken to compare the clinical outcome at each visit versus baseline.
Efficacy Evaluation
Acne Counts
The blinded evaluator counted acne lesions and assessed the mGAGS at each visit prior to administration of the PBBL treatment. Acne lesions were counted separately as noninflammatory (comedones) and inflammatory (papules, pustules, nodules) on the forehead, cheeks, nose, and chin.
Modified Global Acne Grading Score
The modified Global Acne Grading Score was modified from the Global Acne Grading Scale (GAGS) that has previously been used to evaluate acne severity.5 The original GAGS used the type and location of the acne lesions. The GAGS considers 6 locations on the face, chest, and upper back, with a grading factor for each location (forehead=2; cheeks=2; nose=1; chin=1). Another grading factor represented the lesion type (0=no lesion; 1=comedone; 2=papule; 3=pustule; 4=nodule). The local score was calculated by multiplying the location grading factor by the lesion type grading factor. The total score was the sum of the individual local scores for the 4 locations.
Given that the number of acne lesions is important, we modified the GAGS by adding a grading factor that represented the number of lesions to improve the accuracy of the test (1=0–10 lesions; 2=11–20 lesions; 3=21–30 lesions; 4=≥31 lesions). The local score of mGAGS was calculated by multiplying the grading factors for location, lesion type, and number of lesions. Each local score was then added to yield a total score. The mGAGS may be useful and more accurate to determine the severity of acne (0=none; 1–44=mild; 45–80=moderate; 81–132=severe; 133–176=very severe).
Participant Self-assessment
Participants assessed their acne lesions using an 11-point rating scale (–5=100% worsening; –4=76%–99% worsening; –3=51%–75% worsening; –2=26%–50% worsening; –1=1%–25% worsening; 0=no improvement; 1=1%–25% improvement; 2=26%–50% improvement; 3=51%–75% improvement; 4=76%–99% improvement; 5=100% acne clear) to compare their acne at each treatment visit and week 10 follow-up with a baseline photograph.
Physician Assessment
The blinded evaluator assessed acne lesions on the face using the same 11-point rating scale that was used for participant self-assessment. For each participant, assessments were made at each treatment visit and week 10 follow-up by comparing baseline photographs.
Safety Evaluation
The WBPRS score, a standardized 6-point scale (0=no pain; 1=hurts a little bit; 2=hurts a little bit more; 3=hurts even more; 4=hurts whole lot; 5=hurt worst),6 was used to evaluate pain toleration during PBBL treatments and was recorded along with adverse events throughout the study.
Statistical Analysis
Based on data from 2 prior studies,3,7 we expected that the favorable clinical outcome of adapalene gel 0.3% and PBBL therapy would be 23% and 78%, respectively. If the adjunctive therapy with PBBL was beneficial, the favorable outcome would be higher than 78%. To be able to detect this difference, the sample size of 11 patients was needed when 5% type I error and 20% type II error were accepted.
Categorical variables were expressed as percentages, while continuous variables were expressed in terms of median (range). The clinical outcomes between both treatment groups were compared using the Wilcoxon signed rank test. A 2-tailed P value of ≤.05 was considered statistically significant. All statistical calculations were performed using STATA software version 10.0.
RESULTS
Baseline Characteristics
Four male and 7 female patients aged 18 to 35 years (median, 23 years) with mild to moderate acne were enrolled in the study. Of the 11 participants, 7 were white, 2 were black, 1 was Asian, and 1 was Latin American. Baseline characteristics of both sides of the face were comparable in all participants (Table 1). Eight participants (73%) completed the study. Two black participants withdrew from the study due to hyperpigmentation following PBBL treatment; 1 participant did not return for follow-up at week 10, as she was out of the country.
Lesion Counts
At week 3, reduction in noninflammatory lesions was significantly greater on the side receiving the combination therapy compared to the monotherapy side (P=.04)(Table 2). However, there was no significant difference between the combination therapy and the adapalene monotherapy sides in the reduction of noninflammatory and inflammatory lesions at week 4 (Figure 1). There was a remarkable improvement of the combination therapy and adapalene monotherapy sides in acne lesions, but there was no significant difference between the combination therapy and the adapalene monotherapy sides (Figure 2).
Modified Global Acne Grading Score
At weeks 3 and 4, the improvement of mGAGS was significantly greater on the side treated with the combination therapy (P=.05). However, this significant difference was not sustained (Table 3).
Participant Self-assessment and Physician Assessment
The rate of acne improvement according to participant self-assessment was slightly higher on the side receiving the combination therapy compared to the monotherapy side at week 2 (26%–50% vs 1%–25%) and week 6 (76%–99% vs 51%–75%). However, there was no statistically significant difference. For the physician assessment, there was no significant difference between the monotherapy and combination therapy sides.
Safety
The median WBPRS score was 1 (hurts a little bit) throughout all PBBL treatment visits. The maximum score was highest at week 1 (4=hurts whole lot) and subsequently decreased to 2 (hurts a little bit more) at week 6.
After the PBBL treatment, all participants experienced transient erythema in the treatment area. All participants noted their skin had become drier than usual from adapalene, except 1 participant (11%) who reported very dry skin on areas where adapalene gel 0.3% had been applied. However, the dryness was tolerable and relief was reported following application of a moisturizer. No participants withdrew from the study due to skin dryness.
Both black participants experienced hyperpigmentation caused by PBBL (1 on the treatment sites, the other on the test spot) and withdrew from the study. The hyperpigmentation resolved over time following application of a topical bleaching cream. One patient experienced purpura following PBBL treatment at week 4, which was associated with an increase in PBBL power. No other side effects (eg, scaling, stinging, burning, vesicle formation, blistering, crusting, scarring) were observed.
COMMENT
This 10-week study demonstrated that PBBL initially improved the appearance of acne in the first month of treatment, as determined by the significantly greater reduction in mGAGS for the combination side versus the adapalene monotherapy side. Differences in the reduction of acne lesions were not significant between the 2 treatments, except for noninflammatory lesion reduction at week 3. Analysis of physician assessment with photographs revealed acne improvement from baseline in the first month but no additional effects with the PBBL treatment at the end of study. Similarly, participant assessment indicated an improvement by week 2 with the combination therapy compared to adapalene monotherapy in their assessment of acne lesion reductions from baseline. By the end of the study, there was no significant difference between monotherapy and combination therapy.
These findings illustrate that combination therapy with PBBL plus adapalene improved the appearance of acne lesions within the first month of treatment, but there were no further signs of improvement at weeks 5 and 6. These results are consistent with at least 2 other studies that demonstrated acne reduction within the first 3 weeks of PBBL treatment.2,4 The current study was completed as planned with 6 weeks of combination therapy and patients continued adapalene application until the last follow-up visit in week 10. The length of the combination treatment was enough to determine that extension of treatment would not be necessary to gain any further benefits in this study. Because of the small sample size, we would not be able to detect any significant differences, as the difference between the combination therapy and the adapalene monotherapy was less than 55%. Therefore, a future study with a larger sample size is needed to draw a better conclusion.
Pneumatic broadband light has shown impressive results in acne treatment. However, some side effects need to be considered. Minimal adverse events have been reported such as erythema, dryness, peeling, burning, and itching.2-4 In this study, we found that all patients experienced transient erythema during and after PBBL treatment, but this effect disappeared in minutes. Purpura can occur if a higher power of PBBL is performed (6 or greater). Black patients experienced hyperpigmentation that can occur in darker skin types, as reported when light therapy is performed despite using the correct skin type tips.8 Therefore, care must be used in darker skin types, and we advocate a skin test in this population prior to general use.
Our study showed that PBBL can be safely combined with adapalene gel 0.3% and is well tolerated in the treatment of mild to moderate facial acne vulgaris for patients with Fitzpatrick skin types I to III. The combination of PBBL and adapalene reduces acne severity, as shown by the reduction in mGAGS during the first month of treatment. Patients noted faster improvement in their acne lesions with this combination. Although this study was limited by a relatively small sample size, this information may be useful in getting patients to be compliant overall, as they appeared to see results sooner, giving other therapies time to initiate their effect. It appears that 4 consecutive weekly treatments are enough to see that effect. Additionally, this combination therapy provides results without having to resort to oral antibiotics, as many patients today are concerned about creating future antibiotic resistance.
Conclusion
Adapalene gel 0.3% can be safely combined with PBBL for treatment of mild to moderate acne. Although the benefits of this combination therapy can be seen after 4 consecutive weekly treatments, the beneficial effect is not sustained.
Acknowledgment
The authors would like to thank Joyce Okawa, RN (Philadelphia, Pennsylvania), for her assistance in the submission to the University of Pennsylvania institutional review board.
- Thiboutot D, Gollnick H, Bettoli V, et al. New insights into the management of acne: an update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol. 2009;60(5 suppl):S1-S50.
- Gold MH, Biron J. Efficacy of a novel combination of pneumatic energy and broadband light for the treatment of acne. J Drugs Dermatol. 2008;7:639-642.
- Shamban AT, Enokibori M, Narurkar V, et al. Photopneumatic technology for the treatment of acne vulgaris. J Drugs Dermatol. 2008;7:139-145.
- Wanitphakdeedecha R, Tanzi EL, Alster TS. Photopneumatic therapy for the treatment of acne. J Drugs Dermatol. 2009;8:239-241.
- Doshi A, Zaheer A, Stiller MJ. A comparison of current acne grading systems and proposal of a novel system. Int J Dermatol. 1997;36:416-418.
- Wong DL, Baker CM. Pain in children: comparison of assessment scales. Pediatr Nurs. 1988;14:9-17.
- Thiboutot D, Pariser DM, Egan N, et al. Adapalene gel 0.3% for the treatment of acne vulgaris: a multicenter, randomized, double-blind, controlled, phase III trial. J Am Acad Dermatol. 2006;54:242-250.
- Yeung CK, Shek SY, Bjerring P, et al. A comparative study of intense pulsed light alone and its combination with photodynamic therapy for the treatment of facial acne in Asian skin. Lasers Surg Med. 2007;39:1-6.
- Thiboutot D, Gollnick H, Bettoli V, et al. New insights into the management of acne: an update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol. 2009;60(5 suppl):S1-S50.
- Gold MH, Biron J. Efficacy of a novel combination of pneumatic energy and broadband light for the treatment of acne. J Drugs Dermatol. 2008;7:639-642.
- Shamban AT, Enokibori M, Narurkar V, et al. Photopneumatic technology for the treatment of acne vulgaris. J Drugs Dermatol. 2008;7:139-145.
- Wanitphakdeedecha R, Tanzi EL, Alster TS. Photopneumatic therapy for the treatment of acne. J Drugs Dermatol. 2009;8:239-241.
- Doshi A, Zaheer A, Stiller MJ. A comparison of current acne grading systems and proposal of a novel system. Int J Dermatol. 1997;36:416-418.
- Wong DL, Baker CM. Pain in children: comparison of assessment scales. Pediatr Nurs. 1988;14:9-17.
- Thiboutot D, Pariser DM, Egan N, et al. Adapalene gel 0.3% for the treatment of acne vulgaris: a multicenter, randomized, double-blind, controlled, phase III trial. J Am Acad Dermatol. 2006;54:242-250.
- Yeung CK, Shek SY, Bjerring P, et al. A comparative study of intense pulsed light alone and its combination with photodynamic therapy for the treatment of facial acne in Asian skin. Lasers Surg Med. 2007;39:1-6.
Practice Points
- Compliance is achieved when patients can see improvements with their acne treatments quickly.
- Combination therapy achieves the goal of a quicker visual improvement of acneform pustules and papules with pneumatic broadband light while topical acne treatments have a chance to work, thus increasing compliance.
