User login
Fractures of the clavicle, which account for 2.6% of all fractures, are displaced in 70% of cases and are mid-diaphyseal in 80% of cases.1-3 Historically, both displaced and nondisplaced fractures were treated nonoperatively with excellent outcomes reported in the majority of patients.1-3 Traditionally, the indications for surgical fixation of a clavicular fracture include open fractures, which occur infrequently, accounting for only 3.2% of clavicle fractures.4 Other indications include floating shoulder girdle or scapulothoracic dissociation, neurovascular injury, and skin “tenting” by the fracture fragments.3,5 Recently, both meta-analyses and randomized clinical trials have reported reduced malunion rates and improved patient outcomes with open reduction and internal fixation (ORIF).6-9 Consequently, operative fixation could be considered in patients with 100% displacement or greater than 1.5 cm shortening.6-9 Open reduction and internal fixation of the clavicle has been demonstrated to have excellent outcomes in pediatric populations as well.10
The clavicle is subcutaneous for much of its length and, thus, displaced clavicular fractures often result in a visible deformity with a stretch of the soft-tissue envelope over the fracture. While this has been suggested as an operative indication, several recent sources indicate that this concern may only be theoretical. According to the fourth edition of Skeletal Trauma, “It is often stated that open reduction and internal fixation should be considered if the skin is threatened by pressure from a prominent clavicle fracture fragment; however, it is extremely rare of the skin to be perforated from within.”5 The most recent Journal of Bone and Joint Surgery Current Concepts Review on the subject stated that “open fractures or soft-tissue tenting sufficient to produce skin necrosis is uncommon.”3 To the best of our knowledge, there is no reported case of a displaced midshaft clavicle fracture with secondary skin necrosis and conversion into an open fracture, validating the conclusion that this complication may be only theoretical. Given that surgical fixation carries a risk of complications including wound complications, infection, nonunion, malunion, and damage to the nearby neurovascular structures and pleural apices,11 some surgeons may be uncertain how to proceed in cases at risk for disturbance of the soft tissues.
We report 2 adolescent cases of displaced, comminuted clavicle fractures in which the skin was initially intact. Both were managed nonoperatively and both secondarily presented with open lesions at the fracture site requiring urgent irrigation and débridement (I&D) and ORIF. The patients and their guardians provided written informed consent for print and electronic publication of these case reports.
Case Reports
Case 1
A 15-year-old boy with no significant medical or surgical history flipped over the handlebars of his bicycle the day prior to presentation and sustained a clavicle fracture on his left nondominant upper extremity. This was an isolated injury. On examination, his skin was intact with an area of tender mild osseous protuberance at the midclavicle with associated surrounding edema. He was neurovascularly intact. Radiographs showed a displaced fracture of the midshaft of the clavicle with 20% shortening with a vertically angulated piece of comminution (Figure 1A). After a discussion of the treatment options with the family, the decision was made to pursue nonoperative treatment with sling immobilization as needed and restriction from gym and sports.
Two and a half weeks later, the patient presented at follow-up with significant reduction but persistence of his pain and a new complaint of drainage from the area of the fracture. On examination, he was found to have a puncture wound of the skin with exposed clavicle protruding through the wound with a 1-cm circumferential area of erythema without purulence present or expressible. The patient denied reinjury and endorsed compliance with sling immobilization. He was taken for urgent I&D and ORIF. After excision of the eschar surrounding the open lesion and full I&D of the soft tissues, the protruding spike was partially excised and the fracture site was débrided. The fracture was reduced and fixated with a lag screw and neutralization plate technique using an anatomically contoured locking clavicle plate (Synthes). Vancomycin powder was sprinkled into the wound at the completion of the procedure to reduce the chance of infection.12
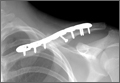
Postoperatively, the patient was prescribed oral clindamycin but was subsequently switched to oral cephalexin because of mild signs of an allergic reaction, for a total course of antibiotics of 1 week. The patient was immobilized in a sling for comfort for the first 9 weeks postoperatively until radiographic union occurred. The patient’s wound healed uneventfully and with acceptable cosmesis. He was released to full activities at 10 weeks postoperatively. At final follow-up 6 months after surgery, the patient had returned to all of his regular activities without pain, and with full range of motion and no demonstrable deficits with radiographic union (Figure 1B).
Case 2
An 11-year-old boy with no significant medical or surgical history fell onto his right dominant upper extremity while doing a jump on his dirt bike 1 week prior to presentation, sustaining a clavicle fracture. This was an isolated injury. He was seen and evaluated by an outside orthopedist who noted that the soft-tissue envelope was intact and the patient was neurovascularly intact. Radiographs showed a displaced fracture of the midshaft of the clavicle with 15% shortening and with a vertically angulated piece of comminution (Figure 1C). Nonoperative treatment with a figure-of-8 brace was recommended. The patient’s discomfort completely resolved.
One week later, when he presented to the outside orthopedist for follow-up, the development of a wound overlying the fracture site was noted, and the patient was started on oral trimethoprim/sulfamethoxazole and referred to our office for treatment (Figure 1D). The patient denied reinjury and endorsed compliance with brace immobilization. On examination, the patient was afebrile and was noted to have a puncture wound at the fracture site with a protruding spike of bone and surrounding erythema but without present or expressible discharge (Figure 2). The patient was taken urgently for I&D and ORIF, using a similar technique to case 1, except that no lag screw was employed.
Postoperatively, the patient did well with no complications; he was prescribed oral cephalexin for 1 week. The patient was immobilized in a sling for the first 5 weeks after surgery until radiographic union had occurred, after which the sling was discontinued. The patient’s wound healed uneventfully and with acceptable cosmesis. The patient was released from activity restrictions at 6 weeks postoperatively. At final follow-up 5 weeks after surgery, the patient had full painless range of motion, no tenderness at the fracture site, no signs of infection on examination, and radiographic union (Figure 1D).
Discussion
Optimal treatment of displaced clavicle fractures is controversial. While nonoperative treatment has been recommended,1-3 especially in skeletally immature populations with a capacity for remodeling,7-9 2 recent randomized clinical trials have demonstrated improved patient outcomes with ORIF.6,8,9 Traditionally, ORIF was recommended with tenting of the skin because of concern for an impending open fracture. However, recent review materials have implied that this complication may only be theoretical.3,5 Indeed, in 2 randomized trials, sufficient displacement to cause concern for impending violation of the skin envelope was not listed as an exclusion criteria.8,9 We report 2 cases of displaced comminuted clavicle fractures that were initially managed nonoperatively but developed open lesions at the fracture site. This complication, while rare, is possible, and surgeons must consider it as a possibility when assessing patients with displaced clavicle fractures. To the best of the authors’ knowledge, no guidelines exist to direct antibiotic choice and duration in secondarily open fractures.
These 2 cases have several features in common that may serve as risk factors for impending violation of the skin envelope. Both fractures had a vertically angulated segmental piece of comminution with a sharp spike. This feature has been identified as a potential risk factor for subsequent development of an open fracture in a case report of fragment excision without reduction or fixation to allow rapid return to play in a professional jockey.13 Both patients in these cases presented with high-velocity mechanisms of injury and significant displacement, both of which may serve as risk factors. In the only similar case the authors could identify, Strauss and colleagues14 described a distal clavicle fracture with significant displacement and with secondary ulceration of the skin complicated by infection presenting with purulent discharge, cultured positive for methicillin-sensitive Staphylococcus aureus, requiring management with an external fixator and 6 weeks of intravenous antibiotics. Because both cases presented here occurred in healthy adolescent patients who were taken urgently for I&D and ORIF as soon as the wound was discovered, deep infection was avoided in these cases. Finally, in 1 case, a figure-of-8 brace was employed, which may also have placed pressure on the skin overlying the fracture and may have predisposed this patient to this complication.
Conclusion
In displaced midshaft clavicle fractures, tenting of the skin sufficient to cause subsequent violation of the soft-tissue envelope is possible and is more than a theoretical risk. At-risk patients, ie, those with a vertically angulated sharp fragment of comminution, should be counseled appropriately and observed closely or considered for primary ORIF.
1. Neer CS 2nd. Nonunion of the clavicle. J Am Med Assoc. 1960;172:1006-1011.
2. Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. 1998;80(3):476-484.
3. Khan LA, Bradnock TJ, Scott C, Robinson CM. Fractures of the clavicle. J Bone Joint Surg Am. 2009;91(2):447-460.
4. Gottschalk HP, Dumont G, Khanani S, Browne RH, Starr AJ. Open clavicle fractures: patterns of trauma and associated injuries. J Orthop Trauma. 2012;26(2):107-109.
5. Ring D, Jupiter JB. Injuries to the shoulder girdle. In: Browner BD, Jupiter JB, eds. Skeletal Trauma. 4th ed. New York, NY: Elsevier; 2009:1755–1778.
6. McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am. 2012;94(8):675-684.
7. Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD; Evidence-Based Orthopaedic Trauma Working Group. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005;19(7):504-507.
8. Robinson CM, Goudie EB, Murray IR, et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. J Bone Joint Surg Am. 2013;95(17):1576-1584.
9. Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89(1):1-10.
10. Mehlman CT, Yihua G, Bochang C, Zhigang W. Operative treatment of completely displaced clavicle shaft fractures in children. J Pediatr Orthop. 2009;29(8):851-855.
11. Gross CE, Chalmers PN, Ellman M, Fernandez JJ, Verma NN. Acute brachial plexopathy after clavicular open reduction and internal fixation. J Shoulder Elbow Surg. 2013;22(5):e6-e9.
12. Pahys JM, Pahys JR, Cho SK, et al. Methods to decrease postoperative infections following posterior cervical spine surgery. J Bone Joint Surg Am. 2013;95(6):549-554.
13. Mandalia V, Shivshanker V, Foy MA. Excision of a bony spike without fixation of the fractured clavicle in a jockey. Clin Orthop Relat Res. 2003;(409):275-277.
14. Strauss EJ, Kaplan KM, Paksima N, Bosco JA. Treatment of an open infected type IIB distal clavicle fracture: case report and review of the literature. Bull NYU Hosp Jt Dis. 2008;66(2):129-133.
Fractures of the clavicle, which account for 2.6% of all fractures, are displaced in 70% of cases and are mid-diaphyseal in 80% of cases.1-3 Historically, both displaced and nondisplaced fractures were treated nonoperatively with excellent outcomes reported in the majority of patients.1-3 Traditionally, the indications for surgical fixation of a clavicular fracture include open fractures, which occur infrequently, accounting for only 3.2% of clavicle fractures.4 Other indications include floating shoulder girdle or scapulothoracic dissociation, neurovascular injury, and skin “tenting” by the fracture fragments.3,5 Recently, both meta-analyses and randomized clinical trials have reported reduced malunion rates and improved patient outcomes with open reduction and internal fixation (ORIF).6-9 Consequently, operative fixation could be considered in patients with 100% displacement or greater than 1.5 cm shortening.6-9 Open reduction and internal fixation of the clavicle has been demonstrated to have excellent outcomes in pediatric populations as well.10
The clavicle is subcutaneous for much of its length and, thus, displaced clavicular fractures often result in a visible deformity with a stretch of the soft-tissue envelope over the fracture. While this has been suggested as an operative indication, several recent sources indicate that this concern may only be theoretical. According to the fourth edition of Skeletal Trauma, “It is often stated that open reduction and internal fixation should be considered if the skin is threatened by pressure from a prominent clavicle fracture fragment; however, it is extremely rare of the skin to be perforated from within.”5 The most recent Journal of Bone and Joint Surgery Current Concepts Review on the subject stated that “open fractures or soft-tissue tenting sufficient to produce skin necrosis is uncommon.”3 To the best of our knowledge, there is no reported case of a displaced midshaft clavicle fracture with secondary skin necrosis and conversion into an open fracture, validating the conclusion that this complication may be only theoretical. Given that surgical fixation carries a risk of complications including wound complications, infection, nonunion, malunion, and damage to the nearby neurovascular structures and pleural apices,11 some surgeons may be uncertain how to proceed in cases at risk for disturbance of the soft tissues.
We report 2 adolescent cases of displaced, comminuted clavicle fractures in which the skin was initially intact. Both were managed nonoperatively and both secondarily presented with open lesions at the fracture site requiring urgent irrigation and débridement (I&D) and ORIF. The patients and their guardians provided written informed consent for print and electronic publication of these case reports.
Case Reports
Case 1
A 15-year-old boy with no significant medical or surgical history flipped over the handlebars of his bicycle the day prior to presentation and sustained a clavicle fracture on his left nondominant upper extremity. This was an isolated injury. On examination, his skin was intact with an area of tender mild osseous protuberance at the midclavicle with associated surrounding edema. He was neurovascularly intact. Radiographs showed a displaced fracture of the midshaft of the clavicle with 20% shortening with a vertically angulated piece of comminution (Figure 1A). After a discussion of the treatment options with the family, the decision was made to pursue nonoperative treatment with sling immobilization as needed and restriction from gym and sports.
Two and a half weeks later, the patient presented at follow-up with significant reduction but persistence of his pain and a new complaint of drainage from the area of the fracture. On examination, he was found to have a puncture wound of the skin with exposed clavicle protruding through the wound with a 1-cm circumferential area of erythema without purulence present or expressible. The patient denied reinjury and endorsed compliance with sling immobilization. He was taken for urgent I&D and ORIF. After excision of the eschar surrounding the open lesion and full I&D of the soft tissues, the protruding spike was partially excised and the fracture site was débrided. The fracture was reduced and fixated with a lag screw and neutralization plate technique using an anatomically contoured locking clavicle plate (Synthes). Vancomycin powder was sprinkled into the wound at the completion of the procedure to reduce the chance of infection.12
Postoperatively, the patient was prescribed oral clindamycin but was subsequently switched to oral cephalexin because of mild signs of an allergic reaction, for a total course of antibiotics of 1 week. The patient was immobilized in a sling for comfort for the first 9 weeks postoperatively until radiographic union occurred. The patient’s wound healed uneventfully and with acceptable cosmesis. He was released to full activities at 10 weeks postoperatively. At final follow-up 6 months after surgery, the patient had returned to all of his regular activities without pain, and with full range of motion and no demonstrable deficits with radiographic union (Figure 1B).
Case 2
An 11-year-old boy with no significant medical or surgical history fell onto his right dominant upper extremity while doing a jump on his dirt bike 1 week prior to presentation, sustaining a clavicle fracture. This was an isolated injury. He was seen and evaluated by an outside orthopedist who noted that the soft-tissue envelope was intact and the patient was neurovascularly intact. Radiographs showed a displaced fracture of the midshaft of the clavicle with 15% shortening and with a vertically angulated piece of comminution (Figure 1C). Nonoperative treatment with a figure-of-8 brace was recommended. The patient’s discomfort completely resolved.
One week later, when he presented to the outside orthopedist for follow-up, the development of a wound overlying the fracture site was noted, and the patient was started on oral trimethoprim/sulfamethoxazole and referred to our office for treatment (Figure 1D). The patient denied reinjury and endorsed compliance with brace immobilization. On examination, the patient was afebrile and was noted to have a puncture wound at the fracture site with a protruding spike of bone and surrounding erythema but without present or expressible discharge (Figure 2). The patient was taken urgently for I&D and ORIF, using a similar technique to case 1, except that no lag screw was employed.
Postoperatively, the patient did well with no complications; he was prescribed oral cephalexin for 1 week. The patient was immobilized in a sling for the first 5 weeks after surgery until radiographic union had occurred, after which the sling was discontinued. The patient’s wound healed uneventfully and with acceptable cosmesis. The patient was released from activity restrictions at 6 weeks postoperatively. At final follow-up 5 weeks after surgery, the patient had full painless range of motion, no tenderness at the fracture site, no signs of infection on examination, and radiographic union (Figure 1D).
Discussion
Optimal treatment of displaced clavicle fractures is controversial. While nonoperative treatment has been recommended,1-3 especially in skeletally immature populations with a capacity for remodeling,7-9 2 recent randomized clinical trials have demonstrated improved patient outcomes with ORIF.6,8,9 Traditionally, ORIF was recommended with tenting of the skin because of concern for an impending open fracture. However, recent review materials have implied that this complication may only be theoretical.3,5 Indeed, in 2 randomized trials, sufficient displacement to cause concern for impending violation of the skin envelope was not listed as an exclusion criteria.8,9 We report 2 cases of displaced comminuted clavicle fractures that were initially managed nonoperatively but developed open lesions at the fracture site. This complication, while rare, is possible, and surgeons must consider it as a possibility when assessing patients with displaced clavicle fractures. To the best of the authors’ knowledge, no guidelines exist to direct antibiotic choice and duration in secondarily open fractures.
These 2 cases have several features in common that may serve as risk factors for impending violation of the skin envelope. Both fractures had a vertically angulated segmental piece of comminution with a sharp spike. This feature has been identified as a potential risk factor for subsequent development of an open fracture in a case report of fragment excision without reduction or fixation to allow rapid return to play in a professional jockey.13 Both patients in these cases presented with high-velocity mechanisms of injury and significant displacement, both of which may serve as risk factors. In the only similar case the authors could identify, Strauss and colleagues14 described a distal clavicle fracture with significant displacement and with secondary ulceration of the skin complicated by infection presenting with purulent discharge, cultured positive for methicillin-sensitive Staphylococcus aureus, requiring management with an external fixator and 6 weeks of intravenous antibiotics. Because both cases presented here occurred in healthy adolescent patients who were taken urgently for I&D and ORIF as soon as the wound was discovered, deep infection was avoided in these cases. Finally, in 1 case, a figure-of-8 brace was employed, which may also have placed pressure on the skin overlying the fracture and may have predisposed this patient to this complication.
Conclusion
In displaced midshaft clavicle fractures, tenting of the skin sufficient to cause subsequent violation of the soft-tissue envelope is possible and is more than a theoretical risk. At-risk patients, ie, those with a vertically angulated sharp fragment of comminution, should be counseled appropriately and observed closely or considered for primary ORIF.
Fractures of the clavicle, which account for 2.6% of all fractures, are displaced in 70% of cases and are mid-diaphyseal in 80% of cases.1-3 Historically, both displaced and nondisplaced fractures were treated nonoperatively with excellent outcomes reported in the majority of patients.1-3 Traditionally, the indications for surgical fixation of a clavicular fracture include open fractures, which occur infrequently, accounting for only 3.2% of clavicle fractures.4 Other indications include floating shoulder girdle or scapulothoracic dissociation, neurovascular injury, and skin “tenting” by the fracture fragments.3,5 Recently, both meta-analyses and randomized clinical trials have reported reduced malunion rates and improved patient outcomes with open reduction and internal fixation (ORIF).6-9 Consequently, operative fixation could be considered in patients with 100% displacement or greater than 1.5 cm shortening.6-9 Open reduction and internal fixation of the clavicle has been demonstrated to have excellent outcomes in pediatric populations as well.10
The clavicle is subcutaneous for much of its length and, thus, displaced clavicular fractures often result in a visible deformity with a stretch of the soft-tissue envelope over the fracture. While this has been suggested as an operative indication, several recent sources indicate that this concern may only be theoretical. According to the fourth edition of Skeletal Trauma, “It is often stated that open reduction and internal fixation should be considered if the skin is threatened by pressure from a prominent clavicle fracture fragment; however, it is extremely rare of the skin to be perforated from within.”5 The most recent Journal of Bone and Joint Surgery Current Concepts Review on the subject stated that “open fractures or soft-tissue tenting sufficient to produce skin necrosis is uncommon.”3 To the best of our knowledge, there is no reported case of a displaced midshaft clavicle fracture with secondary skin necrosis and conversion into an open fracture, validating the conclusion that this complication may be only theoretical. Given that surgical fixation carries a risk of complications including wound complications, infection, nonunion, malunion, and damage to the nearby neurovascular structures and pleural apices,11 some surgeons may be uncertain how to proceed in cases at risk for disturbance of the soft tissues.
We report 2 adolescent cases of displaced, comminuted clavicle fractures in which the skin was initially intact. Both were managed nonoperatively and both secondarily presented with open lesions at the fracture site requiring urgent irrigation and débridement (I&D) and ORIF. The patients and their guardians provided written informed consent for print and electronic publication of these case reports.
Case Reports
Case 1
A 15-year-old boy with no significant medical or surgical history flipped over the handlebars of his bicycle the day prior to presentation and sustained a clavicle fracture on his left nondominant upper extremity. This was an isolated injury. On examination, his skin was intact with an area of tender mild osseous protuberance at the midclavicle with associated surrounding edema. He was neurovascularly intact. Radiographs showed a displaced fracture of the midshaft of the clavicle with 20% shortening with a vertically angulated piece of comminution (Figure 1A). After a discussion of the treatment options with the family, the decision was made to pursue nonoperative treatment with sling immobilization as needed and restriction from gym and sports.
Two and a half weeks later, the patient presented at follow-up with significant reduction but persistence of his pain and a new complaint of drainage from the area of the fracture. On examination, he was found to have a puncture wound of the skin with exposed clavicle protruding through the wound with a 1-cm circumferential area of erythema without purulence present or expressible. The patient denied reinjury and endorsed compliance with sling immobilization. He was taken for urgent I&D and ORIF. After excision of the eschar surrounding the open lesion and full I&D of the soft tissues, the protruding spike was partially excised and the fracture site was débrided. The fracture was reduced and fixated with a lag screw and neutralization plate technique using an anatomically contoured locking clavicle plate (Synthes). Vancomycin powder was sprinkled into the wound at the completion of the procedure to reduce the chance of infection.12
Postoperatively, the patient was prescribed oral clindamycin but was subsequently switched to oral cephalexin because of mild signs of an allergic reaction, for a total course of antibiotics of 1 week. The patient was immobilized in a sling for comfort for the first 9 weeks postoperatively until radiographic union occurred. The patient’s wound healed uneventfully and with acceptable cosmesis. He was released to full activities at 10 weeks postoperatively. At final follow-up 6 months after surgery, the patient had returned to all of his regular activities without pain, and with full range of motion and no demonstrable deficits with radiographic union (Figure 1B).
Case 2
An 11-year-old boy with no significant medical or surgical history fell onto his right dominant upper extremity while doing a jump on his dirt bike 1 week prior to presentation, sustaining a clavicle fracture. This was an isolated injury. He was seen and evaluated by an outside orthopedist who noted that the soft-tissue envelope was intact and the patient was neurovascularly intact. Radiographs showed a displaced fracture of the midshaft of the clavicle with 15% shortening and with a vertically angulated piece of comminution (Figure 1C). Nonoperative treatment with a figure-of-8 brace was recommended. The patient’s discomfort completely resolved.
One week later, when he presented to the outside orthopedist for follow-up, the development of a wound overlying the fracture site was noted, and the patient was started on oral trimethoprim/sulfamethoxazole and referred to our office for treatment (Figure 1D). The patient denied reinjury and endorsed compliance with brace immobilization. On examination, the patient was afebrile and was noted to have a puncture wound at the fracture site with a protruding spike of bone and surrounding erythema but without present or expressible discharge (Figure 2). The patient was taken urgently for I&D and ORIF, using a similar technique to case 1, except that no lag screw was employed.
Postoperatively, the patient did well with no complications; he was prescribed oral cephalexin for 1 week. The patient was immobilized in a sling for the first 5 weeks after surgery until radiographic union had occurred, after which the sling was discontinued. The patient’s wound healed uneventfully and with acceptable cosmesis. The patient was released from activity restrictions at 6 weeks postoperatively. At final follow-up 5 weeks after surgery, the patient had full painless range of motion, no tenderness at the fracture site, no signs of infection on examination, and radiographic union (Figure 1D).
Discussion
Optimal treatment of displaced clavicle fractures is controversial. While nonoperative treatment has been recommended,1-3 especially in skeletally immature populations with a capacity for remodeling,7-9 2 recent randomized clinical trials have demonstrated improved patient outcomes with ORIF.6,8,9 Traditionally, ORIF was recommended with tenting of the skin because of concern for an impending open fracture. However, recent review materials have implied that this complication may only be theoretical.3,5 Indeed, in 2 randomized trials, sufficient displacement to cause concern for impending violation of the skin envelope was not listed as an exclusion criteria.8,9 We report 2 cases of displaced comminuted clavicle fractures that were initially managed nonoperatively but developed open lesions at the fracture site. This complication, while rare, is possible, and surgeons must consider it as a possibility when assessing patients with displaced clavicle fractures. To the best of the authors’ knowledge, no guidelines exist to direct antibiotic choice and duration in secondarily open fractures.
These 2 cases have several features in common that may serve as risk factors for impending violation of the skin envelope. Both fractures had a vertically angulated segmental piece of comminution with a sharp spike. This feature has been identified as a potential risk factor for subsequent development of an open fracture in a case report of fragment excision without reduction or fixation to allow rapid return to play in a professional jockey.13 Both patients in these cases presented with high-velocity mechanisms of injury and significant displacement, both of which may serve as risk factors. In the only similar case the authors could identify, Strauss and colleagues14 described a distal clavicle fracture with significant displacement and with secondary ulceration of the skin complicated by infection presenting with purulent discharge, cultured positive for methicillin-sensitive Staphylococcus aureus, requiring management with an external fixator and 6 weeks of intravenous antibiotics. Because both cases presented here occurred in healthy adolescent patients who were taken urgently for I&D and ORIF as soon as the wound was discovered, deep infection was avoided in these cases. Finally, in 1 case, a figure-of-8 brace was employed, which may also have placed pressure on the skin overlying the fracture and may have predisposed this patient to this complication.
Conclusion
In displaced midshaft clavicle fractures, tenting of the skin sufficient to cause subsequent violation of the soft-tissue envelope is possible and is more than a theoretical risk. At-risk patients, ie, those with a vertically angulated sharp fragment of comminution, should be counseled appropriately and observed closely or considered for primary ORIF.
1. Neer CS 2nd. Nonunion of the clavicle. J Am Med Assoc. 1960;172:1006-1011.
2. Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. 1998;80(3):476-484.
3. Khan LA, Bradnock TJ, Scott C, Robinson CM. Fractures of the clavicle. J Bone Joint Surg Am. 2009;91(2):447-460.
4. Gottschalk HP, Dumont G, Khanani S, Browne RH, Starr AJ. Open clavicle fractures: patterns of trauma and associated injuries. J Orthop Trauma. 2012;26(2):107-109.
5. Ring D, Jupiter JB. Injuries to the shoulder girdle. In: Browner BD, Jupiter JB, eds. Skeletal Trauma. 4th ed. New York, NY: Elsevier; 2009:1755–1778.
6. McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am. 2012;94(8):675-684.
7. Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD; Evidence-Based Orthopaedic Trauma Working Group. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005;19(7):504-507.
8. Robinson CM, Goudie EB, Murray IR, et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. J Bone Joint Surg Am. 2013;95(17):1576-1584.
9. Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89(1):1-10.
10. Mehlman CT, Yihua G, Bochang C, Zhigang W. Operative treatment of completely displaced clavicle shaft fractures in children. J Pediatr Orthop. 2009;29(8):851-855.
11. Gross CE, Chalmers PN, Ellman M, Fernandez JJ, Verma NN. Acute brachial plexopathy after clavicular open reduction and internal fixation. J Shoulder Elbow Surg. 2013;22(5):e6-e9.
12. Pahys JM, Pahys JR, Cho SK, et al. Methods to decrease postoperative infections following posterior cervical spine surgery. J Bone Joint Surg Am. 2013;95(6):549-554.
13. Mandalia V, Shivshanker V, Foy MA. Excision of a bony spike without fixation of the fractured clavicle in a jockey. Clin Orthop Relat Res. 2003;(409):275-277.
14. Strauss EJ, Kaplan KM, Paksima N, Bosco JA. Treatment of an open infected type IIB distal clavicle fracture: case report and review of the literature. Bull NYU Hosp Jt Dis. 2008;66(2):129-133.
1. Neer CS 2nd. Nonunion of the clavicle. J Am Med Assoc. 1960;172:1006-1011.
2. Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. 1998;80(3):476-484.
3. Khan LA, Bradnock TJ, Scott C, Robinson CM. Fractures of the clavicle. J Bone Joint Surg Am. 2009;91(2):447-460.
4. Gottschalk HP, Dumont G, Khanani S, Browne RH, Starr AJ. Open clavicle fractures: patterns of trauma and associated injuries. J Orthop Trauma. 2012;26(2):107-109.
5. Ring D, Jupiter JB. Injuries to the shoulder girdle. In: Browner BD, Jupiter JB, eds. Skeletal Trauma. 4th ed. New York, NY: Elsevier; 2009:1755–1778.
6. McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am. 2012;94(8):675-684.
7. Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD; Evidence-Based Orthopaedic Trauma Working Group. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005;19(7):504-507.
8. Robinson CM, Goudie EB, Murray IR, et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. J Bone Joint Surg Am. 2013;95(17):1576-1584.
9. Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89(1):1-10.
10. Mehlman CT, Yihua G, Bochang C, Zhigang W. Operative treatment of completely displaced clavicle shaft fractures in children. J Pediatr Orthop. 2009;29(8):851-855.
11. Gross CE, Chalmers PN, Ellman M, Fernandez JJ, Verma NN. Acute brachial plexopathy after clavicular open reduction and internal fixation. J Shoulder Elbow Surg. 2013;22(5):e6-e9.
12. Pahys JM, Pahys JR, Cho SK, et al. Methods to decrease postoperative infections following posterior cervical spine surgery. J Bone Joint Surg Am. 2013;95(6):549-554.
13. Mandalia V, Shivshanker V, Foy MA. Excision of a bony spike without fixation of the fractured clavicle in a jockey. Clin Orthop Relat Res. 2003;(409):275-277.
14. Strauss EJ, Kaplan KM, Paksima N, Bosco JA. Treatment of an open infected type IIB distal clavicle fracture: case report and review of the literature. Bull NYU Hosp Jt Dis. 2008;66(2):129-133.