User login
Welcome to Current Psychiatry, a leading source of information, online and in print, for practitioners of psychiatry and its related subspecialties, including addiction psychiatry, child and adolescent psychiatry, and geriatric psychiatry. This Web site contains evidence-based reviews of the prevention, diagnosis, and treatment of mental illness and psychological disorders; case reports; updates on psychopharmacology; news about the specialty of psychiatry; pearls for practice; and other topics of interest and use to this audience.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-current-psychiatry')]
div[contains(@class, 'pane-pub-home-current-psychiatry')]
div[contains(@class, 'pane-pub-topic-current-psychiatry')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
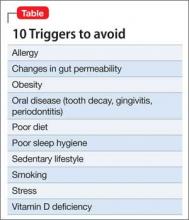
10 Triggers of inflammation to be avoided, to reduce the risk of depression
Neuroinflammation is well-established as an underlying mechanism in depression, as well as in other neuropsychiatric disorders, including schizophrenia, multiple sclerosis, stroke, Parkinson’s disease, and sleep disorders.1 There is a dearth of prevention strategies for neuropsychiatric disorders but, given emerging scientific knowledge about immune dysregulation and the associated rise in inflammatory markers during the course of depression,2,3 it is logical to postulate that avoiding triggers of neuroinflammation might be a useful tactic to prevent depression or, perhaps, to minimize its severity.
Challenge your patients to avoid triggers of depression
What is known about what instigates the rise of inflammatory markers in the body and the brain? Actually, quite a substantial body of knowledge exists on the subject.4 Consider the 10 risk factors for depression that I enumerate here (Table), and advise patients to avoid them.
Sedentary lifestyle. Physical inactivity during childhood is associated with depression in adulthood. This is worrisome because video games seem ever more popular among children these days—more popular and prevalent than playing outdoors. Use this knowledge about the preventive benefit of exercise for long-range prevention in young patients.
Adults with a sedentary lifestyle usually have increased adiposity, which increases the risk of depression. Regular exercise has been shown to down-regulate systemic inflammation.
Smoking. Hundreds of toxic and inflammatory components in tobacco smoke (tars, metals, free radicals) can induce inflammation across the body and brain tissue, which explains not only depression but serious pulmonary and cerebrovascular diseases seen in smokers. People with depression are more likely to smoke than the general population, possibly because nicotine has a mild mood-elevating effect. Yet smoking might make depression worse by exacerbating inflammation, thus negating any mood-elevating effect of nicotine.
Poor diet. It is well known that the Western diet (processed meats, refined sugars, saturated fats) can increase the body’s level of inflammatory markers. The Mediterranean diet, on the other hand, which comprises fruits, vegetables, fish, legumes, and foods rich in omega-3 fatty acids (fish, nuts, leafy green vegetables), is anti-inflammatory. Furthermore, lycopene-containing foods (tomatoes, papaya, red cabbage, watermelon, carrots, asparagus) are rich in antioxidants and thus reduce inflammation.
The possible epigenetic effects of diet are an interesting phenomenon. Offspring of rats who were fed a diet rich in saturated fats have elevated levels of inflammatory markers, even when they had been fed a normal diet, suggesting a transgenerational effect. What parents eat before they conceive might doom their child’s health— regardless of what they feed them.
Tooth decay, gingivitis, periodontitis. Oral inflammation afflicts a large percentage of the population. These conditions can lead to systemic inflammation with elevated levels of C-reactive protein (CRP) and interleukins, which are conducive to depression.
Poor sleep hygiene. Sleep disorders, such as insomnia and insufficient sleep (which is epidemic in the United States), are risk factors for mood disorders. Sleep deprivation disrupts immune function and triggers the cascade of elevated cytokines, CRP, and tumor necrosis factor (TNF)-α. Just as depression is associated with impaired neurogenesis, so is chronic lack of sleep, suggesting a convergence of neurobiologic mechanisms.
Vitamin D deficiency. A link between vitamin D deficiency, now common in the United States, and depression and immune function has been recognized. Vitamin D has anti-inflammatory effects and can reduce oxidative stress, which culminates in inflammation. Vitamin D supplementation has been shown to alleviate neuro-immune disorders, such as multiple sclerosis.
Obesity. Obese people are >50% more likely to develop depression than non-obese people. Technically, obesity is a pro-inflammatory state, and inflammatory biomarkers, such as cytokines, are abundant in fat cells, especially abdominal (visceral or peri-omental) adiposity. When an obese person loses weight, levels of inflammatory markers (interleukin-6, TNF-α, leptin) decrease. We know that abdominal obesity is associated with neuroinflammation and early dementia.
Allergy involves inflammation triggered by the cascade of events consequent to the body’s fight against antigens, and the well-known hyper-sensitivity reaction, causing edema, coughing, sneezing, and itching. It is well-established that the incidence of atopy and allergy is high among people with depression.
Changes in gut permeability. Intestinal inflammatory diseases, such as ulcerative colitis, are recognized as pathways to depression. The mechanism is believed to be the immune response to lipopolysaccharides by commensal bacteria that live by the trillions in the gut. The result? Abnormal gut permeability, bacterial translocation, and depressed mood, possibly because serotonin is more abundant in the gut than in the CNS.
Stress. Arguably, the most common pathway to depression is stressful events of daily life. Stress-induced systemic inflammation hastens cardiovascular disease and leads to neuro-inflammation and neuropsychiatric disorders as well.
Especially malignant is the severe stress of childhood trauma (physical and sexual abuse, parental discord and death), which stimulates pro-inflammatory cytokines and detrimental neurobiological sensitization that lead to psychopathology, including depression and psychosis in adulthood. Childhood trauma has been reported to shorten life by 7 to 15 years.
Posttraumatic stress disorder is the best known clinical model of stress-induced depression and anxiety. The disorder is associated with a significant increase in pro-inflammatory cytokines and loss of brain tissue.
2-fold challenge: Reduce severity of disease, reduce risk before disease
We psychiatrists almost always see patients after they’ve developed depression and other psychiatric disorders in which neuroinflammation is already present. In addition to pharmacotherapy and psychotherapy (both reduce inflammation), educating patients about adopting a healthy lifestyle—not smoking, exercising, eating wisely, avoiding weight gain, getting enough sleep, maintaining good oral hygiene, and managing stress—might reduce psychiatric relapse and prolong their life.
We also should be challenged by the fact that the pathways to inflammation, including the 10 I’ve described here, are common among the population at large. Let’s increase our efforts to preemptively reduce the risk of brain disorders by encouraging parents and their children to adopt a healthy lifestyle and maintain wellness—and thus avoid falling victim to depression.
1. Baune BT. Inflammation and neurodegenerative disorders: is there still hope for therapeutic intervention? Curr Opin Psychiatry. 2015;28(2):148-154.
2. Leonard B, Maes M. Mechanistic explanations how cell-mediated immune activation, inflammation and oxidative and nitrosative stress pathways and their sequels and concomitants play a role in the pathophysiology of unipolar depression. Neurosc Biobehav Rev. 2012;36(2):764-785.
3. Bakunina N, Pariante CM, Zunszain PA. Immune mechanisms linked to depression via oxidative stress and neuroprogression [published online January 10, 2015]. Immunology. 2015. doi: 10.1111/imm.12443.
4. Berk M, Williams LJ, Jacka FN, et al. So depression is an inflammatory disease, but where does the inflammation come from? BMC Med. 2013;11:200.
Neuroinflammation is well-established as an underlying mechanism in depression, as well as in other neuropsychiatric disorders, including schizophrenia, multiple sclerosis, stroke, Parkinson’s disease, and sleep disorders.1 There is a dearth of prevention strategies for neuropsychiatric disorders but, given emerging scientific knowledge about immune dysregulation and the associated rise in inflammatory markers during the course of depression,2,3 it is logical to postulate that avoiding triggers of neuroinflammation might be a useful tactic to prevent depression or, perhaps, to minimize its severity.
Challenge your patients to avoid triggers of depression
What is known about what instigates the rise of inflammatory markers in the body and the brain? Actually, quite a substantial body of knowledge exists on the subject.4 Consider the 10 risk factors for depression that I enumerate here (Table), and advise patients to avoid them.
Sedentary lifestyle. Physical inactivity during childhood is associated with depression in adulthood. This is worrisome because video games seem ever more popular among children these days—more popular and prevalent than playing outdoors. Use this knowledge about the preventive benefit of exercise for long-range prevention in young patients.
Adults with a sedentary lifestyle usually have increased adiposity, which increases the risk of depression. Regular exercise has been shown to down-regulate systemic inflammation.
Smoking. Hundreds of toxic and inflammatory components in tobacco smoke (tars, metals, free radicals) can induce inflammation across the body and brain tissue, which explains not only depression but serious pulmonary and cerebrovascular diseases seen in smokers. People with depression are more likely to smoke than the general population, possibly because nicotine has a mild mood-elevating effect. Yet smoking might make depression worse by exacerbating inflammation, thus negating any mood-elevating effect of nicotine.
Poor diet. It is well known that the Western diet (processed meats, refined sugars, saturated fats) can increase the body’s level of inflammatory markers. The Mediterranean diet, on the other hand, which comprises fruits, vegetables, fish, legumes, and foods rich in omega-3 fatty acids (fish, nuts, leafy green vegetables), is anti-inflammatory. Furthermore, lycopene-containing foods (tomatoes, papaya, red cabbage, watermelon, carrots, asparagus) are rich in antioxidants and thus reduce inflammation.
The possible epigenetic effects of diet are an interesting phenomenon. Offspring of rats who were fed a diet rich in saturated fats have elevated levels of inflammatory markers, even when they had been fed a normal diet, suggesting a transgenerational effect. What parents eat before they conceive might doom their child’s health— regardless of what they feed them.
Tooth decay, gingivitis, periodontitis. Oral inflammation afflicts a large percentage of the population. These conditions can lead to systemic inflammation with elevated levels of C-reactive protein (CRP) and interleukins, which are conducive to depression.
Poor sleep hygiene. Sleep disorders, such as insomnia and insufficient sleep (which is epidemic in the United States), are risk factors for mood disorders. Sleep deprivation disrupts immune function and triggers the cascade of elevated cytokines, CRP, and tumor necrosis factor (TNF)-α. Just as depression is associated with impaired neurogenesis, so is chronic lack of sleep, suggesting a convergence of neurobiologic mechanisms.
Vitamin D deficiency. A link between vitamin D deficiency, now common in the United States, and depression and immune function has been recognized. Vitamin D has anti-inflammatory effects and can reduce oxidative stress, which culminates in inflammation. Vitamin D supplementation has been shown to alleviate neuro-immune disorders, such as multiple sclerosis.
Obesity. Obese people are >50% more likely to develop depression than non-obese people. Technically, obesity is a pro-inflammatory state, and inflammatory biomarkers, such as cytokines, are abundant in fat cells, especially abdominal (visceral or peri-omental) adiposity. When an obese person loses weight, levels of inflammatory markers (interleukin-6, TNF-α, leptin) decrease. We know that abdominal obesity is associated with neuroinflammation and early dementia.
Allergy involves inflammation triggered by the cascade of events consequent to the body’s fight against antigens, and the well-known hyper-sensitivity reaction, causing edema, coughing, sneezing, and itching. It is well-established that the incidence of atopy and allergy is high among people with depression.
Changes in gut permeability. Intestinal inflammatory diseases, such as ulcerative colitis, are recognized as pathways to depression. The mechanism is believed to be the immune response to lipopolysaccharides by commensal bacteria that live by the trillions in the gut. The result? Abnormal gut permeability, bacterial translocation, and depressed mood, possibly because serotonin is more abundant in the gut than in the CNS.
Stress. Arguably, the most common pathway to depression is stressful events of daily life. Stress-induced systemic inflammation hastens cardiovascular disease and leads to neuro-inflammation and neuropsychiatric disorders as well.
Especially malignant is the severe stress of childhood trauma (physical and sexual abuse, parental discord and death), which stimulates pro-inflammatory cytokines and detrimental neurobiological sensitization that lead to psychopathology, including depression and psychosis in adulthood. Childhood trauma has been reported to shorten life by 7 to 15 years.
Posttraumatic stress disorder is the best known clinical model of stress-induced depression and anxiety. The disorder is associated with a significant increase in pro-inflammatory cytokines and loss of brain tissue.
2-fold challenge: Reduce severity of disease, reduce risk before disease
We psychiatrists almost always see patients after they’ve developed depression and other psychiatric disorders in which neuroinflammation is already present. In addition to pharmacotherapy and psychotherapy (both reduce inflammation), educating patients about adopting a healthy lifestyle—not smoking, exercising, eating wisely, avoiding weight gain, getting enough sleep, maintaining good oral hygiene, and managing stress—might reduce psychiatric relapse and prolong their life.
We also should be challenged by the fact that the pathways to inflammation, including the 10 I’ve described here, are common among the population at large. Let’s increase our efforts to preemptively reduce the risk of brain disorders by encouraging parents and their children to adopt a healthy lifestyle and maintain wellness—and thus avoid falling victim to depression.
Neuroinflammation is well-established as an underlying mechanism in depression, as well as in other neuropsychiatric disorders, including schizophrenia, multiple sclerosis, stroke, Parkinson’s disease, and sleep disorders.1 There is a dearth of prevention strategies for neuropsychiatric disorders but, given emerging scientific knowledge about immune dysregulation and the associated rise in inflammatory markers during the course of depression,2,3 it is logical to postulate that avoiding triggers of neuroinflammation might be a useful tactic to prevent depression or, perhaps, to minimize its severity.
Challenge your patients to avoid triggers of depression
What is known about what instigates the rise of inflammatory markers in the body and the brain? Actually, quite a substantial body of knowledge exists on the subject.4 Consider the 10 risk factors for depression that I enumerate here (Table), and advise patients to avoid them.
Sedentary lifestyle. Physical inactivity during childhood is associated with depression in adulthood. This is worrisome because video games seem ever more popular among children these days—more popular and prevalent than playing outdoors. Use this knowledge about the preventive benefit of exercise for long-range prevention in young patients.
Adults with a sedentary lifestyle usually have increased adiposity, which increases the risk of depression. Regular exercise has been shown to down-regulate systemic inflammation.
Smoking. Hundreds of toxic and inflammatory components in tobacco smoke (tars, metals, free radicals) can induce inflammation across the body and brain tissue, which explains not only depression but serious pulmonary and cerebrovascular diseases seen in smokers. People with depression are more likely to smoke than the general population, possibly because nicotine has a mild mood-elevating effect. Yet smoking might make depression worse by exacerbating inflammation, thus negating any mood-elevating effect of nicotine.
Poor diet. It is well known that the Western diet (processed meats, refined sugars, saturated fats) can increase the body’s level of inflammatory markers. The Mediterranean diet, on the other hand, which comprises fruits, vegetables, fish, legumes, and foods rich in omega-3 fatty acids (fish, nuts, leafy green vegetables), is anti-inflammatory. Furthermore, lycopene-containing foods (tomatoes, papaya, red cabbage, watermelon, carrots, asparagus) are rich in antioxidants and thus reduce inflammation.
The possible epigenetic effects of diet are an interesting phenomenon. Offspring of rats who were fed a diet rich in saturated fats have elevated levels of inflammatory markers, even when they had been fed a normal diet, suggesting a transgenerational effect. What parents eat before they conceive might doom their child’s health— regardless of what they feed them.
Tooth decay, gingivitis, periodontitis. Oral inflammation afflicts a large percentage of the population. These conditions can lead to systemic inflammation with elevated levels of C-reactive protein (CRP) and interleukins, which are conducive to depression.
Poor sleep hygiene. Sleep disorders, such as insomnia and insufficient sleep (which is epidemic in the United States), are risk factors for mood disorders. Sleep deprivation disrupts immune function and triggers the cascade of elevated cytokines, CRP, and tumor necrosis factor (TNF)-α. Just as depression is associated with impaired neurogenesis, so is chronic lack of sleep, suggesting a convergence of neurobiologic mechanisms.
Vitamin D deficiency. A link between vitamin D deficiency, now common in the United States, and depression and immune function has been recognized. Vitamin D has anti-inflammatory effects and can reduce oxidative stress, which culminates in inflammation. Vitamin D supplementation has been shown to alleviate neuro-immune disorders, such as multiple sclerosis.
Obesity. Obese people are >50% more likely to develop depression than non-obese people. Technically, obesity is a pro-inflammatory state, and inflammatory biomarkers, such as cytokines, are abundant in fat cells, especially abdominal (visceral or peri-omental) adiposity. When an obese person loses weight, levels of inflammatory markers (interleukin-6, TNF-α, leptin) decrease. We know that abdominal obesity is associated with neuroinflammation and early dementia.
Allergy involves inflammation triggered by the cascade of events consequent to the body’s fight against antigens, and the well-known hyper-sensitivity reaction, causing edema, coughing, sneezing, and itching. It is well-established that the incidence of atopy and allergy is high among people with depression.
Changes in gut permeability. Intestinal inflammatory diseases, such as ulcerative colitis, are recognized as pathways to depression. The mechanism is believed to be the immune response to lipopolysaccharides by commensal bacteria that live by the trillions in the gut. The result? Abnormal gut permeability, bacterial translocation, and depressed mood, possibly because serotonin is more abundant in the gut than in the CNS.
Stress. Arguably, the most common pathway to depression is stressful events of daily life. Stress-induced systemic inflammation hastens cardiovascular disease and leads to neuro-inflammation and neuropsychiatric disorders as well.
Especially malignant is the severe stress of childhood trauma (physical and sexual abuse, parental discord and death), which stimulates pro-inflammatory cytokines and detrimental neurobiological sensitization that lead to psychopathology, including depression and psychosis in adulthood. Childhood trauma has been reported to shorten life by 7 to 15 years.
Posttraumatic stress disorder is the best known clinical model of stress-induced depression and anxiety. The disorder is associated with a significant increase in pro-inflammatory cytokines and loss of brain tissue.
2-fold challenge: Reduce severity of disease, reduce risk before disease
We psychiatrists almost always see patients after they’ve developed depression and other psychiatric disorders in which neuroinflammation is already present. In addition to pharmacotherapy and psychotherapy (both reduce inflammation), educating patients about adopting a healthy lifestyle—not smoking, exercising, eating wisely, avoiding weight gain, getting enough sleep, maintaining good oral hygiene, and managing stress—might reduce psychiatric relapse and prolong their life.
We also should be challenged by the fact that the pathways to inflammation, including the 10 I’ve described here, are common among the population at large. Let’s increase our efforts to preemptively reduce the risk of brain disorders by encouraging parents and their children to adopt a healthy lifestyle and maintain wellness—and thus avoid falling victim to depression.
1. Baune BT. Inflammation and neurodegenerative disorders: is there still hope for therapeutic intervention? Curr Opin Psychiatry. 2015;28(2):148-154.
2. Leonard B, Maes M. Mechanistic explanations how cell-mediated immune activation, inflammation and oxidative and nitrosative stress pathways and their sequels and concomitants play a role in the pathophysiology of unipolar depression. Neurosc Biobehav Rev. 2012;36(2):764-785.
3. Bakunina N, Pariante CM, Zunszain PA. Immune mechanisms linked to depression via oxidative stress and neuroprogression [published online January 10, 2015]. Immunology. 2015. doi: 10.1111/imm.12443.
4. Berk M, Williams LJ, Jacka FN, et al. So depression is an inflammatory disease, but where does the inflammation come from? BMC Med. 2013;11:200.
1. Baune BT. Inflammation and neurodegenerative disorders: is there still hope for therapeutic intervention? Curr Opin Psychiatry. 2015;28(2):148-154.
2. Leonard B, Maes M. Mechanistic explanations how cell-mediated immune activation, inflammation and oxidative and nitrosative stress pathways and their sequels and concomitants play a role in the pathophysiology of unipolar depression. Neurosc Biobehav Rev. 2012;36(2):764-785.
3. Bakunina N, Pariante CM, Zunszain PA. Immune mechanisms linked to depression via oxidative stress and neuroprogression [published online January 10, 2015]. Immunology. 2015. doi: 10.1111/imm.12443.
4. Berk M, Williams LJ, Jacka FN, et al. So depression is an inflammatory disease, but where does the inflammation come from? BMC Med. 2013;11:200.
Sedating antidepressants for insomnia
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Glutamatergic therapies
6 Strategies to address risk factors for school violence
School shootings engender the deepest of public concern. They violate strongly held cross-culture beliefs about the sanctity of childhood and the obligation to protect children from harm.
Prevention and intervention approaches to school shootings have emerged (1) in the literature, from case studies, and (2) from discourse among experts.1 Approaches include:
• bolstering security at schools
• reducing the facilities’ vulnerability to intrusion
• increasing the capacity to respond at the moment of threat
• transforming the school climate
• increasing attachment and bonding.1,2
Psychiatrists often are consulted by school districts to provide expertise for the latter 2 approaches. Using the following strategies, you can help address risk factors for school violence.
Strengthen school attachment. Develop curricular and extracurricular programs for students that create, and contribute to, a sense of belonging. This, in turn, decreases alienation and reduces hostility. Unaddressed hostility can lead to depression, anger, and, subsequently, violence.
Reduce social aggression. Social aggression, such as teasing, taunting, humiliating, and bullying, is an important predictor of developmental outcomes in victims and perpetrators.3 Social aggression has been linked to peer victimization and low school attachment. Implement social skills programs, such as Making Choices, which have yielded positive effects on social aggression in elementary school students.4
Break codes of silence. This can involve encouraging schools to:
• develop an anonymous mechanism of voicing concerns
• take diligent action based on students’ concerns
• treat disclosures discreetly.
Establish resources for troubled and rejected students. Develop routine emergency modes of communication, such as a protocol for high-priority referral to mental health resources. These could reduce the likelihood of students acting out against the school.
Recommend that security be enhanced. Establishing the position of school resource officer might increase confidence and decrease feelings of vulnerability among teachers, students, and parents. This can increase the perception of school security, potentially helps school attachment, and promotes breaking down codes of silence.5
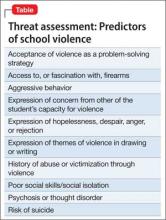
Increase communication within the school, and between the school and law enforcement agencies. Effective communication can help identify the location of an attacker and disrupt a developing event. Create an alert system to notify students, faculty, and parents with an automated text message or phone call during an emergency. Increased accessibility of the students by the school alert system might be a quicker way to reach the school community. Work with security agencies to develop a protocol for communicating and assessing threat potential. Also, develop guidelines to outline referral and assessing procedures for students whose writings may present indication for possible attack or whose class behavior may be alienating or intimidating to either faculty or other students. Behavior that can lead to school violence is outlined in the Table.
You also can educate school administrators about the following:
• School violence has been significantly associated with mental health problems, such as depression and inability to form age appropriate social connections,6 which in combination with extreme social rejection and specific personality-related issues (eg, antisocial personality disorder) can culminate in violent outbreaks.7 Work closely with school nurses and counselors to identify and treat vulnerable students.
• In most multiple-victim incidents, more than 1 person had information about the attack before it occurred that was not communicated to an authority figure. Educate school officials about being sensitive to warnings or threats about possible attack, and help develop ways get counseling for potential attackers.2
• Zero-tolerance policies are ineffective at preventing school shootings, mostly because of literal interpretation and inconsistent implementation of such policies.8 Help circumvent a more stringent zero-tolerance policy with adequate availability of mental health care for students who are identified as being at risk of perpetrating an attack.
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Culley MR, Conkling M, Emshoff J, et al. Environmental and contextual influences on school violence and its prevention. J Prim Prev. 2006;27(3):217-227.
2. Wike TL, Fraser MW. School shooting: making sense of the senseless. Aggress Violent Behav. 2009;14(3):162-169.
3. Rudatsikira E, Singh P, Job J, et al. Variables associated with weapon-carrying among young adolescents in southern California. J Adolesc Health. 2007;40(5):470-473.
4. Fraser MW, Galinsky MJ, Smokowski PR, et al. Social information-processing skills training to promote social competence and prevent aggressive behavior in the third grades. J Consult Clin Psychol. 2005;73(6):1045-1055.
5. Finn P. School resource officer programs. Finding the funding, reaping the benefits. FBI Law Enforcement Bulletin. 2006;75(8):1-13.
6. Ferguson C, Coulson M, Barnett J. Psychological profiles of school shooters: positive directions and one big wrong turn. J Police Crisis Negot. 2011;11:1-17.
7. Leary MR, Kowalski RM, Smith L, et al. Teasing, rejection and violence: case studies of the school shootings. Aggressive Behavior. 2003;29(3):202-214.
8. American Psychological Association Zero Tolerance Task Force. Are zero tolerance policies effective in the schools?: an evidentiary review and recommendation. Am Psychol. 2008;63(9):852-862.
School shootings engender the deepest of public concern. They violate strongly held cross-culture beliefs about the sanctity of childhood and the obligation to protect children from harm.
Prevention and intervention approaches to school shootings have emerged (1) in the literature, from case studies, and (2) from discourse among experts.1 Approaches include:
• bolstering security at schools
• reducing the facilities’ vulnerability to intrusion
• increasing the capacity to respond at the moment of threat
• transforming the school climate
• increasing attachment and bonding.1,2
Psychiatrists often are consulted by school districts to provide expertise for the latter 2 approaches. Using the following strategies, you can help address risk factors for school violence.
Strengthen school attachment. Develop curricular and extracurricular programs for students that create, and contribute to, a sense of belonging. This, in turn, decreases alienation and reduces hostility. Unaddressed hostility can lead to depression, anger, and, subsequently, violence.
Reduce social aggression. Social aggression, such as teasing, taunting, humiliating, and bullying, is an important predictor of developmental outcomes in victims and perpetrators.3 Social aggression has been linked to peer victimization and low school attachment. Implement social skills programs, such as Making Choices, which have yielded positive effects on social aggression in elementary school students.4
Break codes of silence. This can involve encouraging schools to:
• develop an anonymous mechanism of voicing concerns
• take diligent action based on students’ concerns
• treat disclosures discreetly.
Establish resources for troubled and rejected students. Develop routine emergency modes of communication, such as a protocol for high-priority referral to mental health resources. These could reduce the likelihood of students acting out against the school.
Recommend that security be enhanced. Establishing the position of school resource officer might increase confidence and decrease feelings of vulnerability among teachers, students, and parents. This can increase the perception of school security, potentially helps school attachment, and promotes breaking down codes of silence.5
Increase communication within the school, and between the school and law enforcement agencies. Effective communication can help identify the location of an attacker and disrupt a developing event. Create an alert system to notify students, faculty, and parents with an automated text message or phone call during an emergency. Increased accessibility of the students by the school alert system might be a quicker way to reach the school community. Work with security agencies to develop a protocol for communicating and assessing threat potential. Also, develop guidelines to outline referral and assessing procedures for students whose writings may present indication for possible attack or whose class behavior may be alienating or intimidating to either faculty or other students. Behavior that can lead to school violence is outlined in the Table.
You also can educate school administrators about the following:
• School violence has been significantly associated with mental health problems, such as depression and inability to form age appropriate social connections,6 which in combination with extreme social rejection and specific personality-related issues (eg, antisocial personality disorder) can culminate in violent outbreaks.7 Work closely with school nurses and counselors to identify and treat vulnerable students.
• In most multiple-victim incidents, more than 1 person had information about the attack before it occurred that was not communicated to an authority figure. Educate school officials about being sensitive to warnings or threats about possible attack, and help develop ways get counseling for potential attackers.2
• Zero-tolerance policies are ineffective at preventing school shootings, mostly because of literal interpretation and inconsistent implementation of such policies.8 Help circumvent a more stringent zero-tolerance policy with adequate availability of mental health care for students who are identified as being at risk of perpetrating an attack.
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
School shootings engender the deepest of public concern. They violate strongly held cross-culture beliefs about the sanctity of childhood and the obligation to protect children from harm.
Prevention and intervention approaches to school shootings have emerged (1) in the literature, from case studies, and (2) from discourse among experts.1 Approaches include:
• bolstering security at schools
• reducing the facilities’ vulnerability to intrusion
• increasing the capacity to respond at the moment of threat
• transforming the school climate
• increasing attachment and bonding.1,2
Psychiatrists often are consulted by school districts to provide expertise for the latter 2 approaches. Using the following strategies, you can help address risk factors for school violence.
Strengthen school attachment. Develop curricular and extracurricular programs for students that create, and contribute to, a sense of belonging. This, in turn, decreases alienation and reduces hostility. Unaddressed hostility can lead to depression, anger, and, subsequently, violence.
Reduce social aggression. Social aggression, such as teasing, taunting, humiliating, and bullying, is an important predictor of developmental outcomes in victims and perpetrators.3 Social aggression has been linked to peer victimization and low school attachment. Implement social skills programs, such as Making Choices, which have yielded positive effects on social aggression in elementary school students.4
Break codes of silence. This can involve encouraging schools to:
• develop an anonymous mechanism of voicing concerns
• take diligent action based on students’ concerns
• treat disclosures discreetly.
Establish resources for troubled and rejected students. Develop routine emergency modes of communication, such as a protocol for high-priority referral to mental health resources. These could reduce the likelihood of students acting out against the school.
Recommend that security be enhanced. Establishing the position of school resource officer might increase confidence and decrease feelings of vulnerability among teachers, students, and parents. This can increase the perception of school security, potentially helps school attachment, and promotes breaking down codes of silence.5
Increase communication within the school, and between the school and law enforcement agencies. Effective communication can help identify the location of an attacker and disrupt a developing event. Create an alert system to notify students, faculty, and parents with an automated text message or phone call during an emergency. Increased accessibility of the students by the school alert system might be a quicker way to reach the school community. Work with security agencies to develop a protocol for communicating and assessing threat potential. Also, develop guidelines to outline referral and assessing procedures for students whose writings may present indication for possible attack or whose class behavior may be alienating or intimidating to either faculty or other students. Behavior that can lead to school violence is outlined in the Table.
You also can educate school administrators about the following:
• School violence has been significantly associated with mental health problems, such as depression and inability to form age appropriate social connections,6 which in combination with extreme social rejection and specific personality-related issues (eg, antisocial personality disorder) can culminate in violent outbreaks.7 Work closely with school nurses and counselors to identify and treat vulnerable students.
• In most multiple-victim incidents, more than 1 person had information about the attack before it occurred that was not communicated to an authority figure. Educate school officials about being sensitive to warnings or threats about possible attack, and help develop ways get counseling for potential attackers.2
• Zero-tolerance policies are ineffective at preventing school shootings, mostly because of literal interpretation and inconsistent implementation of such policies.8 Help circumvent a more stringent zero-tolerance policy with adequate availability of mental health care for students who are identified as being at risk of perpetrating an attack.
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Culley MR, Conkling M, Emshoff J, et al. Environmental and contextual influences on school violence and its prevention. J Prim Prev. 2006;27(3):217-227.
2. Wike TL, Fraser MW. School shooting: making sense of the senseless. Aggress Violent Behav. 2009;14(3):162-169.
3. Rudatsikira E, Singh P, Job J, et al. Variables associated with weapon-carrying among young adolescents in southern California. J Adolesc Health. 2007;40(5):470-473.
4. Fraser MW, Galinsky MJ, Smokowski PR, et al. Social information-processing skills training to promote social competence and prevent aggressive behavior in the third grades. J Consult Clin Psychol. 2005;73(6):1045-1055.
5. Finn P. School resource officer programs. Finding the funding, reaping the benefits. FBI Law Enforcement Bulletin. 2006;75(8):1-13.
6. Ferguson C, Coulson M, Barnett J. Psychological profiles of school shooters: positive directions and one big wrong turn. J Police Crisis Negot. 2011;11:1-17.
7. Leary MR, Kowalski RM, Smith L, et al. Teasing, rejection and violence: case studies of the school shootings. Aggressive Behavior. 2003;29(3):202-214.
8. American Psychological Association Zero Tolerance Task Force. Are zero tolerance policies effective in the schools?: an evidentiary review and recommendation. Am Psychol. 2008;63(9):852-862.
1. Culley MR, Conkling M, Emshoff J, et al. Environmental and contextual influences on school violence and its prevention. J Prim Prev. 2006;27(3):217-227.
2. Wike TL, Fraser MW. School shooting: making sense of the senseless. Aggress Violent Behav. 2009;14(3):162-169.
3. Rudatsikira E, Singh P, Job J, et al. Variables associated with weapon-carrying among young adolescents in southern California. J Adolesc Health. 2007;40(5):470-473.
4. Fraser MW, Galinsky MJ, Smokowski PR, et al. Social information-processing skills training to promote social competence and prevent aggressive behavior in the third grades. J Consult Clin Psychol. 2005;73(6):1045-1055.
5. Finn P. School resource officer programs. Finding the funding, reaping the benefits. FBI Law Enforcement Bulletin. 2006;75(8):1-13.
6. Ferguson C, Coulson M, Barnett J. Psychological profiles of school shooters: positive directions and one big wrong turn. J Police Crisis Negot. 2011;11:1-17.
7. Leary MR, Kowalski RM, Smith L, et al. Teasing, rejection and violence: case studies of the school shootings. Aggressive Behavior. 2003;29(3):202-214.
8. American Psychological Association Zero Tolerance Task Force. Are zero tolerance policies effective in the schools?: an evidentiary review and recommendation. Am Psychol. 2008;63(9):852-862.
‘No SAD Me’: A memory device for treating bipolar depression with an antidepressant
Depression is the first affective episode in >50% of patients with bipolar disorder, and is associated with considerable morbidity and mortality.
The mean duration of a bipolar depressive episode is considerably longer than a manic episode; >20% of bipolar depressive episodes run a chronic course.1 Evidence suggests that depressive episodes and symptoms are equal to, or more disabling than, corresponding levels of manic or hypomanic symptoms.2
Debate over appropriate therapy
Using antidepressants to treat bipolar depression remains controversial. Much of the debate surrounds concern that antidepressants have the potential to switch a patient to mania/hypomania or to destabilize mood over the longitudinal course of illness.2
Several guidelines for informing the use of antidepressants in bipolar depression have been published, including the International Society for Bipolar Disorders task force report on antidepressant use in bipolar disorders3 and the guideline of the World Federation of Societies of Biological Psychiatry.4 To summarize the most recent consensus on treating bipolar depression, we devised the mnemonic No SAD Me:
No n-antidepressant treatments should be considered as monotherapy before antidepressants are used. Consider lithium, lamotrigine, olanzapine, quetiapine, or lurasidone first for bipolar depression.3
S afe-to-use adjunctive antidepressants can be considered if the patient relapses to a depressive episode after antidepressant therapy is stopped. Consider using a selective serotonin reuptake inhibitor (SSRI) and bupropion (1) for an acute bipolar I or II depressive episode when the patient has a history of a positive response to an antidepressant and (2) as maintenance treatment with SSRIs and bupropion as adjunctive therapy.2,3
A void antidepressants as monotherapy. If using an antidepressant to treat bipolar I disorder, prescribe a mood-stabilizer concomitantly, even though the evidence for antidepressant-associated mood-switching is mixed and the ability of mood stabilizers to prevent such responses to antidepressant treatment is unproven.
D o not use tricyclic antidepressants (TCAs) or venlafaxine. Evidence does not show 1 type of antidepressant is more or less effective or dangerous than another. Nevertheless, TCAs and venlafaxine appear to carry a particularly high risk of inducing pathologically elevated states of mood and behavior.3
M onitor closely. Bipolar disorder patients who are being started on an antidepressant should be closely monitored for signs of hypomania or mania and increased psychomotor agitation. Discontinue the antidepressant if such signs are observed or emerge.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Sidor MM, MacQueen GM. An update on antidepressant use in bipolar depression. Curr Psychiatry Rep. 2012;14(6):696-704.
2. Pacchiarotti I, Mazzarini L, Colom F, et al. Treatment-resistant bipolar depression: towards a new definition. Acta Psychiatr Scand. 2009;120(6):429-440.
3. Pacchiarotti I, Bond DJ, Baldessarini RJ, et al. The International Society for Bipolar Disorders (ISBD) task force report on antidepressant use in bipolar disorders. Am J Psychiatry. 2013; 170(11):1249-1262.
4. Grunze H, Vieta E, Goodwin GM, et al; WFSBP Task Force On Treatment Guidelines For Bipolar Disorders. The World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the Biological Treatment of Bipolar Disorders: Update 2010 on the treatment of acute bipolar depression. World J Biol Psychiatry. 2010;11:81-109.
Depression is the first affective episode in >50% of patients with bipolar disorder, and is associated with considerable morbidity and mortality.
The mean duration of a bipolar depressive episode is considerably longer than a manic episode; >20% of bipolar depressive episodes run a chronic course.1 Evidence suggests that depressive episodes and symptoms are equal to, or more disabling than, corresponding levels of manic or hypomanic symptoms.2
Debate over appropriate therapy
Using antidepressants to treat bipolar depression remains controversial. Much of the debate surrounds concern that antidepressants have the potential to switch a patient to mania/hypomania or to destabilize mood over the longitudinal course of illness.2
Several guidelines for informing the use of antidepressants in bipolar depression have been published, including the International Society for Bipolar Disorders task force report on antidepressant use in bipolar disorders3 and the guideline of the World Federation of Societies of Biological Psychiatry.4 To summarize the most recent consensus on treating bipolar depression, we devised the mnemonic No SAD Me:
No n-antidepressant treatments should be considered as monotherapy before antidepressants are used. Consider lithium, lamotrigine, olanzapine, quetiapine, or lurasidone first for bipolar depression.3
S afe-to-use adjunctive antidepressants can be considered if the patient relapses to a depressive episode after antidepressant therapy is stopped. Consider using a selective serotonin reuptake inhibitor (SSRI) and bupropion (1) for an acute bipolar I or II depressive episode when the patient has a history of a positive response to an antidepressant and (2) as maintenance treatment with SSRIs and bupropion as adjunctive therapy.2,3
A void antidepressants as monotherapy. If using an antidepressant to treat bipolar I disorder, prescribe a mood-stabilizer concomitantly, even though the evidence for antidepressant-associated mood-switching is mixed and the ability of mood stabilizers to prevent such responses to antidepressant treatment is unproven.
D o not use tricyclic antidepressants (TCAs) or venlafaxine. Evidence does not show 1 type of antidepressant is more or less effective or dangerous than another. Nevertheless, TCAs and venlafaxine appear to carry a particularly high risk of inducing pathologically elevated states of mood and behavior.3
M onitor closely. Bipolar disorder patients who are being started on an antidepressant should be closely monitored for signs of hypomania or mania and increased psychomotor agitation. Discontinue the antidepressant if such signs are observed or emerge.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Depression is the first affective episode in >50% of patients with bipolar disorder, and is associated with considerable morbidity and mortality.
The mean duration of a bipolar depressive episode is considerably longer than a manic episode; >20% of bipolar depressive episodes run a chronic course.1 Evidence suggests that depressive episodes and symptoms are equal to, or more disabling than, corresponding levels of manic or hypomanic symptoms.2
Debate over appropriate therapy
Using antidepressants to treat bipolar depression remains controversial. Much of the debate surrounds concern that antidepressants have the potential to switch a patient to mania/hypomania or to destabilize mood over the longitudinal course of illness.2
Several guidelines for informing the use of antidepressants in bipolar depression have been published, including the International Society for Bipolar Disorders task force report on antidepressant use in bipolar disorders3 and the guideline of the World Federation of Societies of Biological Psychiatry.4 To summarize the most recent consensus on treating bipolar depression, we devised the mnemonic No SAD Me:
No n-antidepressant treatments should be considered as monotherapy before antidepressants are used. Consider lithium, lamotrigine, olanzapine, quetiapine, or lurasidone first for bipolar depression.3
S afe-to-use adjunctive antidepressants can be considered if the patient relapses to a depressive episode after antidepressant therapy is stopped. Consider using a selective serotonin reuptake inhibitor (SSRI) and bupropion (1) for an acute bipolar I or II depressive episode when the patient has a history of a positive response to an antidepressant and (2) as maintenance treatment with SSRIs and bupropion as adjunctive therapy.2,3
A void antidepressants as monotherapy. If using an antidepressant to treat bipolar I disorder, prescribe a mood-stabilizer concomitantly, even though the evidence for antidepressant-associated mood-switching is mixed and the ability of mood stabilizers to prevent such responses to antidepressant treatment is unproven.
D o not use tricyclic antidepressants (TCAs) or venlafaxine. Evidence does not show 1 type of antidepressant is more or less effective or dangerous than another. Nevertheless, TCAs and venlafaxine appear to carry a particularly high risk of inducing pathologically elevated states of mood and behavior.3
M onitor closely. Bipolar disorder patients who are being started on an antidepressant should be closely monitored for signs of hypomania or mania and increased psychomotor agitation. Discontinue the antidepressant if such signs are observed or emerge.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Sidor MM, MacQueen GM. An update on antidepressant use in bipolar depression. Curr Psychiatry Rep. 2012;14(6):696-704.
2. Pacchiarotti I, Mazzarini L, Colom F, et al. Treatment-resistant bipolar depression: towards a new definition. Acta Psychiatr Scand. 2009;120(6):429-440.
3. Pacchiarotti I, Bond DJ, Baldessarini RJ, et al. The International Society for Bipolar Disorders (ISBD) task force report on antidepressant use in bipolar disorders. Am J Psychiatry. 2013; 170(11):1249-1262.
4. Grunze H, Vieta E, Goodwin GM, et al; WFSBP Task Force On Treatment Guidelines For Bipolar Disorders. The World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the Biological Treatment of Bipolar Disorders: Update 2010 on the treatment of acute bipolar depression. World J Biol Psychiatry. 2010;11:81-109.
1. Sidor MM, MacQueen GM. An update on antidepressant use in bipolar depression. Curr Psychiatry Rep. 2012;14(6):696-704.
2. Pacchiarotti I, Mazzarini L, Colom F, et al. Treatment-resistant bipolar depression: towards a new definition. Acta Psychiatr Scand. 2009;120(6):429-440.
3. Pacchiarotti I, Bond DJ, Baldessarini RJ, et al. The International Society for Bipolar Disorders (ISBD) task force report on antidepressant use in bipolar disorders. Am J Psychiatry. 2013; 170(11):1249-1262.
4. Grunze H, Vieta E, Goodwin GM, et al; WFSBP Task Force On Treatment Guidelines For Bipolar Disorders. The World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the Biological Treatment of Bipolar Disorders: Update 2010 on the treatment of acute bipolar depression. World J Biol Psychiatry. 2010;11:81-109.
Can social media help mental health practitioners prevent suicides?
Suicide is the tenth leading cause of death among Americans and the third leading cause among those age 15 to 24.1 As many as 36% of suicide victims leave a suicide note.2 Researchers have analyzed such notes with the aim of identifying specific content and patterns that might aid in creating more effective strategies for preventing suicide.3-5
One study found that the presence of a suicide note is an indicator of serious intent; that is, when the initial attempt fails, those who had left a suicide note were found to be at increased risk of subsequent completed suicide.4 Researchers also found that 75% of suicide notes contained the theme “apology/shame,” suggesting that many suicide victims might have welcomed an alternative to suicide to solve their personal predicament. Tragically, however, most suicide notes are not discovered until suicide has been attempted or completed.4
That’s where social media comes in. As platforms for self-expression, social networking sites such as Facebook, Twitter, and Tumblr are sources of real-time information that could aid in suicide prevention.6 With that in mind, we:
• present 2 cases in which a patient announced her suicidal ideation on Facebook
• consider the opportunities that social media present for early intervention
• propose high-tech monitoring methods for high-risk patients.
CASE 1 Major depressive disorder (MDD) and nonadherence
Ms. S, age 24, has a 4-year history of MDD and treatment nonadherence. She had no history of suicide attempt or inpatient treatment, but she had briefly engaged in psychotherapy before discontinuing visits. Physically healthy and employed as a security officer, Ms. S recently broke up with her boyfriend who had abused her physically—and against whom she had an order of protection.
On the day in question, Ms. S posted several status updates on Facebook expressing hopelessness, which, over the course of the day, escalated to expression of frank suicidal ideation:
• “I am ugly, no man would ever want to live with me.”
• “I have made no effect on the world and I’m just a waste of space.”
• “It’s sad that I want to die but such is life. We all die one day.”
• “I’m going to kill myself. It was nice knowing you world. Goodbye everyone.”
CASE 2 Substance abuse and previous suicide attempt
Ms. B, age 21, had a remote (approximately age 16) history of a suicide attempt and was actively abusing 3,4-methylenedioxymethamphetamine (MDMA [“Ecstasy,” “Molly”]) and Cannabis. She was not receiving outpatient care. One afternoon, Ms. B walked into the emergency department (ED) and said she had just taken 17 ibuprofen pills with the intent of killing herself.
On initial evaluation, Ms. B was irritable and uncooperative, denying all psychiatric symptoms and refusing to divulge details of her recent behavior. Her mother, who had not accompanied her daughter to the ED, reported that Ms. B had engaged in excessive risk-taking—speeding, driving while intoxicated, having multiple sex partners—for the past 5 years, resulting in several arrests for minor offenses, and she had been depressed and was sleeping and eating poorly in the 2 weeks leading up to the suicide attempt.
Two days ago, her mother added, Ms. B had posted disturbing notes on Facebook: ”Life is useless,” she declared in one post; “I’d be better off dead,” in another.
Suicidal content online
Worldwide, Facebook has 1.35 billion active users each month.7 Thus far, a limited number of posts indicating suicidal intent have been reported in the lay press,8 but evidence suggests that the use of social media for this purpose is an emerging trend.9
A search of the literature yielded only 3 case reports.8,10,11 In one case, a delayed response to a suicide note resulted in a failure to prevent the suicide.8 In another, a clinician’s discovery of a patient’s explicitly suicidal Facebook post led to what the team leader described as a more meaningful therapeutic relationship.10 The clinician’s discovery might have been pivotal in preventing the patient from committing suicide.
The authors of these case reports explored the idea of using Facebook for suicide prevention, raising a number of practical and ethical issues. Among them are the potential for immediate intervention by other Facebook users and the extent to which suicidal posts on social media sites induce copycat suicides.8
Issues associated with clinicians’ use of social media to follow or monitor patients include the ethical concepts of beneficence and nonmaleficence, privacy and confidentiality, clinical judgment, and informed consent,8,10 including potential benefit and harm and the difference between actual and perceived privacy violations. Bennett et al11 recommend developing guidelines for the use of social media to enhance medical care and provide appropriate protections to both patients and providers.
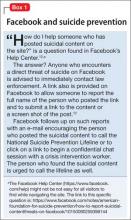
Reporting suicidal content. Although the primary purpose of Facebook is to give users the opportunity to share life events and thoughts with friends and family, the company does address the question of suicidal content in its Help Center (Box 1).12 As our 2 cases illustrate, however, intervention can be significantly delayed.
CASE 1 CONTINUED Call to 911
Fortunately for Ms. S, a friend who read her Facebook posts called 911; even then, however, 16 hours passed between the initial postings and the patient’s arrival at the ED. When emergency medical services brought Ms. S to the Comprehensive Psychiatry Emergency Program, she acknowledged suicidal ideation without an active plan. Other symptoms included depressed mood, a sense of hopelessness, feelings of worthlessness lasting >2 months, low self-esteem, dissatisfaction with body image, and a recent verbal altercation with a friend.
Ms. S was admitted to the inpatient unit for further observation and stabilization.
CASE 2 CONTINUED No one answered her calls
Ms. B, who did not arrive at the ED until 2 days after her suicidal posts, corroborated the history given by her mother. She also reported that she had attempted to reach out to her friends for support, but no one had answered her phone calls. She felt hurt because of this, Ms. B said, and impulsively ingested the pills.
Ms. B said she regretted the suicide attempt. Nevertheless, in light of her recent attempt and persistent distress, she was admitted to the inpatient unit for observation and stabilization.
Can artificial intelligence help?
There is no effective means of tracking high-risk patients after their first contact with the mental health system, despite the fact that (1) those who attempt suicide are at high risk of subsequent suicide attempts3 and (2) we have the potential to prevent future attempts based on self-expressed online cues. We propose machine learning algorithms—a branch of artificial intelligence—to capture and process suicide notes on Facebook in real time.
Machine learning can be broadly defined as computational methods using experience to improve performance or make accurate predictions. In this context, “experience” refers to past information, typically in the form of electronic data collected and analyzed to design accurate and efficient predictive algorithms. Machine learning, which incorporates fundamental concepts in computer science, as well as statistics, probability, and optimization, already has been established in a variety of applications, such as detecting e-mail spam, natural language processing, and computational biology.13
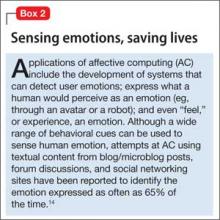
Affective computing, known as emotion-oriented computing, is a branch of artificial intelligence that involves the design of systems and devices that can recognize, interpret, and process human moods and emotions (Box 2).14
Prediction models, developed by Poulin et al15 to estimate the risk of suicide (based on keywords and multiword phrases from unstructured clinical notes from a national sample of U.S. Veterans Administration medical records), resulted in an inference accuracy of ≥65%. Pestian et al16 created and annotated a collection of suicide notes—a vital resource for scientists to use for machine learning and data mining. Machine learning algorithms based on such notes and clinical data might be used to capture alarming social media posts by high-risk patients and activate crisis management, with potentially life-saving results.
But limitations remain
It is not easy to identify or analyze people’s emotions based on social media posts; emotions can be implicit, based on specific events or situations. To distinguish among different emotions purely on the basis of keywords is to deal in great subtlety. Framing algorithms to include multiple parameters—the duration of suicidal content and the number of suicidal posts, for example—would help mitigate the risk of false alarms.
Another problem is that not all Facebook profiles are public. In fact, only 28% of users share all or most of their posts with anyone other than their friends.17 This limitation could be addressed by urging patients identified as being at high risk of suicide during an initial clinical encounter with a mental health provider to “friend” a generic Web page created by the hospital or clinic to protect patients’ privacy.
As Levahot et al10 wrote in their report of the patient whose clinician discovered a patient’s explicitly suicidal Facebook post, the incident “did not hinder the therapeutic alliance.” Instead, the team leader said, the discovery deepened the therapeutic relationship and helped the patient “better understand his mental illness and need for increased support.”
Bottom Line
Machine learning algorithms offer the possibility of analyzing status updates from patients who express suicidal ideation on social media and alerting clinicians to the need for early intervention. There are steps clinicians can take now, however, to take advantage of Facebook, in particular, to monitor and potentially prevent suicide attempts by those at high risk.
Related Resource
• Ahuja AK, Biesaga K, Sudak DM, et al. Suicide on Facebook. J Psychiatr Pract. 2014;20(2):141-146.
Acknowledgement
Zafar Sharif MD, Associate Clinical Professor of Psychiatry, Columbia University College of Physicians and Surgeons, and Director of Psychiatry, Harlem Hospital Center, New York, New York, and Michael Yogman MD, Assistant Clinical Professor of Pediatrics, Harvard Medical School, Boston Children’s Hospital, Boston, Massachusetts, provided insight into the topic and useful feedback on the manuscript of this article.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) 2010. http://www.cdc.gov/injury/wisqars/index.html. Updated July 7, 2014. Accessed January 19, 2015.
2. Shioiri T, Nishimura A, Akazawa K, et al. Incidence of note-leaving remains constant despite increasing suicide rates. Psychiatr Clin Neurosci. 2005;59(2):226-228.
3. Barr W, Leitner M, Thomas J. Self-harm or attempted suicide? Do suicide notes help us decide the level of intent in those who survive? Accid Emerg Nurs. 2007;15(3):122-127.
4. Foster T. Suicide note themes and suicide prevention. Int J Psychiatry Med. 2003;33(4):323-331.
5. Bhatia MS, Verma SK, Murty OP. Suicide notes: psychological and clinical profile. Int J Psychiatry Med. 2006;36(2):163-170.
6. Jashinsky J, Burton SH, Hanson CL, et al. Tracking suicide risk factors through Twitter in the US. Crisis. 2014;35(1):51-59.
7. Facebook news room. Company info. http://newsroom. fb.com/company-info. Accessed January 7, 2015.
8. Ruder TD, Hatch GM, Ampanozi G, et al. Suicide announcement on Facebook. Crisis. 2011;32(5):280-282.
9. Luxton DD, June JD, Fairall JM. Social media and suicide: a public health perspective. Am J Public Health. 2012;102(suppl 2):S195-S200.
10. Lehavot K, Ben-Zeev D, Neville RE. Ethical considerations and social media: a case of suicidal postings on Facebook. Journal of Dual Diagnosis. 2012;8(4):341-346.
11. Bennett A, Pourmand A, Shokoohi H, et al. Impacts of social networking sites on patient care in the emergency department. Telemed J E Health. 2014;20(1):94-96.
12. How to report suicidal content/threats on Facebook. h t tps ://www. facebook.com/notes/amer ican-foundation-for-suicide-prevention/how-to-report-suicidal-contentthreats-on-facebook/10150090259398144. Published February 15, 2011. Accessed January 22, 2015.
13. Mohri M, Rostamizadeh A, Talwalker A. Foundations of machine learning (adaptive computation and machine learning series). Cambridge, MA: MIT Press; 2012:14.
14. Blázquez Gil G, Berlanga de Jesús A, Molina Lopéz JM. Combining machine learning techniques and natural language processing to infer emotions using Spanish Twitter corpus. Communications in Computer and Information Science. 2013;365:149-157.
15. Poulin C, Shiner B, Thompson P, et al. Predicting the risk of suicide by analyzing the text of clinical notes. PLoS One. 2014;9(1):e85733.
16. Pestian JP, Matykiewicz P, Linn-Gust M. What’s in a note: construction of a suicide note corpus. Biomed Inform Insights. 2012;5:1-6.
17. ConsumerReports.org. Facebook & your privacy. http:// www.consumerreports.org/cro/magazine/2012/06/ facebook-your-privacy/index.html. Published June 2012. Accessed January 22, 2015
Suicide is the tenth leading cause of death among Americans and the third leading cause among those age 15 to 24.1 As many as 36% of suicide victims leave a suicide note.2 Researchers have analyzed such notes with the aim of identifying specific content and patterns that might aid in creating more effective strategies for preventing suicide.3-5
One study found that the presence of a suicide note is an indicator of serious intent; that is, when the initial attempt fails, those who had left a suicide note were found to be at increased risk of subsequent completed suicide.4 Researchers also found that 75% of suicide notes contained the theme “apology/shame,” suggesting that many suicide victims might have welcomed an alternative to suicide to solve their personal predicament. Tragically, however, most suicide notes are not discovered until suicide has been attempted or completed.4
That’s where social media comes in. As platforms for self-expression, social networking sites such as Facebook, Twitter, and Tumblr are sources of real-time information that could aid in suicide prevention.6 With that in mind, we:
• present 2 cases in which a patient announced her suicidal ideation on Facebook
• consider the opportunities that social media present for early intervention
• propose high-tech monitoring methods for high-risk patients.
CASE 1 Major depressive disorder (MDD) and nonadherence
Ms. S, age 24, has a 4-year history of MDD and treatment nonadherence. She had no history of suicide attempt or inpatient treatment, but she had briefly engaged in psychotherapy before discontinuing visits. Physically healthy and employed as a security officer, Ms. S recently broke up with her boyfriend who had abused her physically—and against whom she had an order of protection.
On the day in question, Ms. S posted several status updates on Facebook expressing hopelessness, which, over the course of the day, escalated to expression of frank suicidal ideation:
• “I am ugly, no man would ever want to live with me.”
• “I have made no effect on the world and I’m just a waste of space.”
• “It’s sad that I want to die but such is life. We all die one day.”
• “I’m going to kill myself. It was nice knowing you world. Goodbye everyone.”
CASE 2 Substance abuse and previous suicide attempt
Ms. B, age 21, had a remote (approximately age 16) history of a suicide attempt and was actively abusing 3,4-methylenedioxymethamphetamine (MDMA [“Ecstasy,” “Molly”]) and Cannabis. She was not receiving outpatient care. One afternoon, Ms. B walked into the emergency department (ED) and said she had just taken 17 ibuprofen pills with the intent of killing herself.
On initial evaluation, Ms. B was irritable and uncooperative, denying all psychiatric symptoms and refusing to divulge details of her recent behavior. Her mother, who had not accompanied her daughter to the ED, reported that Ms. B had engaged in excessive risk-taking—speeding, driving while intoxicated, having multiple sex partners—for the past 5 years, resulting in several arrests for minor offenses, and she had been depressed and was sleeping and eating poorly in the 2 weeks leading up to the suicide attempt.
Two days ago, her mother added, Ms. B had posted disturbing notes on Facebook: ”Life is useless,” she declared in one post; “I’d be better off dead,” in another.
Suicidal content online
Worldwide, Facebook has 1.35 billion active users each month.7 Thus far, a limited number of posts indicating suicidal intent have been reported in the lay press,8 but evidence suggests that the use of social media for this purpose is an emerging trend.9
A search of the literature yielded only 3 case reports.8,10,11 In one case, a delayed response to a suicide note resulted in a failure to prevent the suicide.8 In another, a clinician’s discovery of a patient’s explicitly suicidal Facebook post led to what the team leader described as a more meaningful therapeutic relationship.10 The clinician’s discovery might have been pivotal in preventing the patient from committing suicide.
The authors of these case reports explored the idea of using Facebook for suicide prevention, raising a number of practical and ethical issues. Among them are the potential for immediate intervention by other Facebook users and the extent to which suicidal posts on social media sites induce copycat suicides.8
Issues associated with clinicians’ use of social media to follow or monitor patients include the ethical concepts of beneficence and nonmaleficence, privacy and confidentiality, clinical judgment, and informed consent,8,10 including potential benefit and harm and the difference between actual and perceived privacy violations. Bennett et al11 recommend developing guidelines for the use of social media to enhance medical care and provide appropriate protections to both patients and providers.
Reporting suicidal content. Although the primary purpose of Facebook is to give users the opportunity to share life events and thoughts with friends and family, the company does address the question of suicidal content in its Help Center (Box 1).12 As our 2 cases illustrate, however, intervention can be significantly delayed.
CASE 1 CONTINUED Call to 911
Fortunately for Ms. S, a friend who read her Facebook posts called 911; even then, however, 16 hours passed between the initial postings and the patient’s arrival at the ED. When emergency medical services brought Ms. S to the Comprehensive Psychiatry Emergency Program, she acknowledged suicidal ideation without an active plan. Other symptoms included depressed mood, a sense of hopelessness, feelings of worthlessness lasting >2 months, low self-esteem, dissatisfaction with body image, and a recent verbal altercation with a friend.
Ms. S was admitted to the inpatient unit for further observation and stabilization.
CASE 2 CONTINUED No one answered her calls
Ms. B, who did not arrive at the ED until 2 days after her suicidal posts, corroborated the history given by her mother. She also reported that she had attempted to reach out to her friends for support, but no one had answered her phone calls. She felt hurt because of this, Ms. B said, and impulsively ingested the pills.
Ms. B said she regretted the suicide attempt. Nevertheless, in light of her recent attempt and persistent distress, she was admitted to the inpatient unit for observation and stabilization.
Can artificial intelligence help?
There is no effective means of tracking high-risk patients after their first contact with the mental health system, despite the fact that (1) those who attempt suicide are at high risk of subsequent suicide attempts3 and (2) we have the potential to prevent future attempts based on self-expressed online cues. We propose machine learning algorithms—a branch of artificial intelligence—to capture and process suicide notes on Facebook in real time.
Machine learning can be broadly defined as computational methods using experience to improve performance or make accurate predictions. In this context, “experience” refers to past information, typically in the form of electronic data collected and analyzed to design accurate and efficient predictive algorithms. Machine learning, which incorporates fundamental concepts in computer science, as well as statistics, probability, and optimization, already has been established in a variety of applications, such as detecting e-mail spam, natural language processing, and computational biology.13
Affective computing, known as emotion-oriented computing, is a branch of artificial intelligence that involves the design of systems and devices that can recognize, interpret, and process human moods and emotions (Box 2).14
Prediction models, developed by Poulin et al15 to estimate the risk of suicide (based on keywords and multiword phrases from unstructured clinical notes from a national sample of U.S. Veterans Administration medical records), resulted in an inference accuracy of ≥65%. Pestian et al16 created and annotated a collection of suicide notes—a vital resource for scientists to use for machine learning and data mining. Machine learning algorithms based on such notes and clinical data might be used to capture alarming social media posts by high-risk patients and activate crisis management, with potentially life-saving results.
But limitations remain
It is not easy to identify or analyze people’s emotions based on social media posts; emotions can be implicit, based on specific events or situations. To distinguish among different emotions purely on the basis of keywords is to deal in great subtlety. Framing algorithms to include multiple parameters—the duration of suicidal content and the number of suicidal posts, for example—would help mitigate the risk of false alarms.
Another problem is that not all Facebook profiles are public. In fact, only 28% of users share all or most of their posts with anyone other than their friends.17 This limitation could be addressed by urging patients identified as being at high risk of suicide during an initial clinical encounter with a mental health provider to “friend” a generic Web page created by the hospital or clinic to protect patients’ privacy.
As Levahot et al10 wrote in their report of the patient whose clinician discovered a patient’s explicitly suicidal Facebook post, the incident “did not hinder the therapeutic alliance.” Instead, the team leader said, the discovery deepened the therapeutic relationship and helped the patient “better understand his mental illness and need for increased support.”
Bottom Line
Machine learning algorithms offer the possibility of analyzing status updates from patients who express suicidal ideation on social media and alerting clinicians to the need for early intervention. There are steps clinicians can take now, however, to take advantage of Facebook, in particular, to monitor and potentially prevent suicide attempts by those at high risk.
Related Resource
• Ahuja AK, Biesaga K, Sudak DM, et al. Suicide on Facebook. J Psychiatr Pract. 2014;20(2):141-146.
Acknowledgement
Zafar Sharif MD, Associate Clinical Professor of Psychiatry, Columbia University College of Physicians and Surgeons, and Director of Psychiatry, Harlem Hospital Center, New York, New York, and Michael Yogman MD, Assistant Clinical Professor of Pediatrics, Harvard Medical School, Boston Children’s Hospital, Boston, Massachusetts, provided insight into the topic and useful feedback on the manuscript of this article.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Suicide is the tenth leading cause of death among Americans and the third leading cause among those age 15 to 24.1 As many as 36% of suicide victims leave a suicide note.2 Researchers have analyzed such notes with the aim of identifying specific content and patterns that might aid in creating more effective strategies for preventing suicide.3-5
One study found that the presence of a suicide note is an indicator of serious intent; that is, when the initial attempt fails, those who had left a suicide note were found to be at increased risk of subsequent completed suicide.4 Researchers also found that 75% of suicide notes contained the theme “apology/shame,” suggesting that many suicide victims might have welcomed an alternative to suicide to solve their personal predicament. Tragically, however, most suicide notes are not discovered until suicide has been attempted or completed.4
That’s where social media comes in. As platforms for self-expression, social networking sites such as Facebook, Twitter, and Tumblr are sources of real-time information that could aid in suicide prevention.6 With that in mind, we:
• present 2 cases in which a patient announced her suicidal ideation on Facebook
• consider the opportunities that social media present for early intervention
• propose high-tech monitoring methods for high-risk patients.
CASE 1 Major depressive disorder (MDD) and nonadherence
Ms. S, age 24, has a 4-year history of MDD and treatment nonadherence. She had no history of suicide attempt or inpatient treatment, but she had briefly engaged in psychotherapy before discontinuing visits. Physically healthy and employed as a security officer, Ms. S recently broke up with her boyfriend who had abused her physically—and against whom she had an order of protection.
On the day in question, Ms. S posted several status updates on Facebook expressing hopelessness, which, over the course of the day, escalated to expression of frank suicidal ideation:
• “I am ugly, no man would ever want to live with me.”
• “I have made no effect on the world and I’m just a waste of space.”
• “It’s sad that I want to die but such is life. We all die one day.”
• “I’m going to kill myself. It was nice knowing you world. Goodbye everyone.”
CASE 2 Substance abuse and previous suicide attempt
Ms. B, age 21, had a remote (approximately age 16) history of a suicide attempt and was actively abusing 3,4-methylenedioxymethamphetamine (MDMA [“Ecstasy,” “Molly”]) and Cannabis. She was not receiving outpatient care. One afternoon, Ms. B walked into the emergency department (ED) and said she had just taken 17 ibuprofen pills with the intent of killing herself.
On initial evaluation, Ms. B was irritable and uncooperative, denying all psychiatric symptoms and refusing to divulge details of her recent behavior. Her mother, who had not accompanied her daughter to the ED, reported that Ms. B had engaged in excessive risk-taking—speeding, driving while intoxicated, having multiple sex partners—for the past 5 years, resulting in several arrests for minor offenses, and she had been depressed and was sleeping and eating poorly in the 2 weeks leading up to the suicide attempt.
Two days ago, her mother added, Ms. B had posted disturbing notes on Facebook: ”Life is useless,” she declared in one post; “I’d be better off dead,” in another.
Suicidal content online
Worldwide, Facebook has 1.35 billion active users each month.7 Thus far, a limited number of posts indicating suicidal intent have been reported in the lay press,8 but evidence suggests that the use of social media for this purpose is an emerging trend.9
A search of the literature yielded only 3 case reports.8,10,11 In one case, a delayed response to a suicide note resulted in a failure to prevent the suicide.8 In another, a clinician’s discovery of a patient’s explicitly suicidal Facebook post led to what the team leader described as a more meaningful therapeutic relationship.10 The clinician’s discovery might have been pivotal in preventing the patient from committing suicide.
The authors of these case reports explored the idea of using Facebook for suicide prevention, raising a number of practical and ethical issues. Among them are the potential for immediate intervention by other Facebook users and the extent to which suicidal posts on social media sites induce copycat suicides.8
Issues associated with clinicians’ use of social media to follow or monitor patients include the ethical concepts of beneficence and nonmaleficence, privacy and confidentiality, clinical judgment, and informed consent,8,10 including potential benefit and harm and the difference between actual and perceived privacy violations. Bennett et al11 recommend developing guidelines for the use of social media to enhance medical care and provide appropriate protections to both patients and providers.
Reporting suicidal content. Although the primary purpose of Facebook is to give users the opportunity to share life events and thoughts with friends and family, the company does address the question of suicidal content in its Help Center (Box 1).12 As our 2 cases illustrate, however, intervention can be significantly delayed.
CASE 1 CONTINUED Call to 911
Fortunately for Ms. S, a friend who read her Facebook posts called 911; even then, however, 16 hours passed between the initial postings and the patient’s arrival at the ED. When emergency medical services brought Ms. S to the Comprehensive Psychiatry Emergency Program, she acknowledged suicidal ideation without an active plan. Other symptoms included depressed mood, a sense of hopelessness, feelings of worthlessness lasting >2 months, low self-esteem, dissatisfaction with body image, and a recent verbal altercation with a friend.
Ms. S was admitted to the inpatient unit for further observation and stabilization.
CASE 2 CONTINUED No one answered her calls
Ms. B, who did not arrive at the ED until 2 days after her suicidal posts, corroborated the history given by her mother. She also reported that she had attempted to reach out to her friends for support, but no one had answered her phone calls. She felt hurt because of this, Ms. B said, and impulsively ingested the pills.
Ms. B said she regretted the suicide attempt. Nevertheless, in light of her recent attempt and persistent distress, she was admitted to the inpatient unit for observation and stabilization.
Can artificial intelligence help?
There is no effective means of tracking high-risk patients after their first contact with the mental health system, despite the fact that (1) those who attempt suicide are at high risk of subsequent suicide attempts3 and (2) we have the potential to prevent future attempts based on self-expressed online cues. We propose machine learning algorithms—a branch of artificial intelligence—to capture and process suicide notes on Facebook in real time.
Machine learning can be broadly defined as computational methods using experience to improve performance or make accurate predictions. In this context, “experience” refers to past information, typically in the form of electronic data collected and analyzed to design accurate and efficient predictive algorithms. Machine learning, which incorporates fundamental concepts in computer science, as well as statistics, probability, and optimization, already has been established in a variety of applications, such as detecting e-mail spam, natural language processing, and computational biology.13
Affective computing, known as emotion-oriented computing, is a branch of artificial intelligence that involves the design of systems and devices that can recognize, interpret, and process human moods and emotions (Box 2).14
Prediction models, developed by Poulin et al15 to estimate the risk of suicide (based on keywords and multiword phrases from unstructured clinical notes from a national sample of U.S. Veterans Administration medical records), resulted in an inference accuracy of ≥65%. Pestian et al16 created and annotated a collection of suicide notes—a vital resource for scientists to use for machine learning and data mining. Machine learning algorithms based on such notes and clinical data might be used to capture alarming social media posts by high-risk patients and activate crisis management, with potentially life-saving results.
But limitations remain
It is not easy to identify or analyze people’s emotions based on social media posts; emotions can be implicit, based on specific events or situations. To distinguish among different emotions purely on the basis of keywords is to deal in great subtlety. Framing algorithms to include multiple parameters—the duration of suicidal content and the number of suicidal posts, for example—would help mitigate the risk of false alarms.
Another problem is that not all Facebook profiles are public. In fact, only 28% of users share all or most of their posts with anyone other than their friends.17 This limitation could be addressed by urging patients identified as being at high risk of suicide during an initial clinical encounter with a mental health provider to “friend” a generic Web page created by the hospital or clinic to protect patients’ privacy.
As Levahot et al10 wrote in their report of the patient whose clinician discovered a patient’s explicitly suicidal Facebook post, the incident “did not hinder the therapeutic alliance.” Instead, the team leader said, the discovery deepened the therapeutic relationship and helped the patient “better understand his mental illness and need for increased support.”
Bottom Line
Machine learning algorithms offer the possibility of analyzing status updates from patients who express suicidal ideation on social media and alerting clinicians to the need for early intervention. There are steps clinicians can take now, however, to take advantage of Facebook, in particular, to monitor and potentially prevent suicide attempts by those at high risk.
Related Resource
• Ahuja AK, Biesaga K, Sudak DM, et al. Suicide on Facebook. J Psychiatr Pract. 2014;20(2):141-146.
Acknowledgement
Zafar Sharif MD, Associate Clinical Professor of Psychiatry, Columbia University College of Physicians and Surgeons, and Director of Psychiatry, Harlem Hospital Center, New York, New York, and Michael Yogman MD, Assistant Clinical Professor of Pediatrics, Harvard Medical School, Boston Children’s Hospital, Boston, Massachusetts, provided insight into the topic and useful feedback on the manuscript of this article.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) 2010. http://www.cdc.gov/injury/wisqars/index.html. Updated July 7, 2014. Accessed January 19, 2015.
2. Shioiri T, Nishimura A, Akazawa K, et al. Incidence of note-leaving remains constant despite increasing suicide rates. Psychiatr Clin Neurosci. 2005;59(2):226-228.
3. Barr W, Leitner M, Thomas J. Self-harm or attempted suicide? Do suicide notes help us decide the level of intent in those who survive? Accid Emerg Nurs. 2007;15(3):122-127.
4. Foster T. Suicide note themes and suicide prevention. Int J Psychiatry Med. 2003;33(4):323-331.
5. Bhatia MS, Verma SK, Murty OP. Suicide notes: psychological and clinical profile. Int J Psychiatry Med. 2006;36(2):163-170.
6. Jashinsky J, Burton SH, Hanson CL, et al. Tracking suicide risk factors through Twitter in the US. Crisis. 2014;35(1):51-59.
7. Facebook news room. Company info. http://newsroom. fb.com/company-info. Accessed January 7, 2015.
8. Ruder TD, Hatch GM, Ampanozi G, et al. Suicide announcement on Facebook. Crisis. 2011;32(5):280-282.
9. Luxton DD, June JD, Fairall JM. Social media and suicide: a public health perspective. Am J Public Health. 2012;102(suppl 2):S195-S200.
10. Lehavot K, Ben-Zeev D, Neville RE. Ethical considerations and social media: a case of suicidal postings on Facebook. Journal of Dual Diagnosis. 2012;8(4):341-346.
11. Bennett A, Pourmand A, Shokoohi H, et al. Impacts of social networking sites on patient care in the emergency department. Telemed J E Health. 2014;20(1):94-96.
12. How to report suicidal content/threats on Facebook. h t tps ://www. facebook.com/notes/amer ican-foundation-for-suicide-prevention/how-to-report-suicidal-contentthreats-on-facebook/10150090259398144. Published February 15, 2011. Accessed January 22, 2015.
13. Mohri M, Rostamizadeh A, Talwalker A. Foundations of machine learning (adaptive computation and machine learning series). Cambridge, MA: MIT Press; 2012:14.
14. Blázquez Gil G, Berlanga de Jesús A, Molina Lopéz JM. Combining machine learning techniques and natural language processing to infer emotions using Spanish Twitter corpus. Communications in Computer and Information Science. 2013;365:149-157.
15. Poulin C, Shiner B, Thompson P, et al. Predicting the risk of suicide by analyzing the text of clinical notes. PLoS One. 2014;9(1):e85733.
16. Pestian JP, Matykiewicz P, Linn-Gust M. What’s in a note: construction of a suicide note corpus. Biomed Inform Insights. 2012;5:1-6.
17. ConsumerReports.org. Facebook & your privacy. http:// www.consumerreports.org/cro/magazine/2012/06/ facebook-your-privacy/index.html. Published June 2012. Accessed January 22, 2015
1. Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) 2010. http://www.cdc.gov/injury/wisqars/index.html. Updated July 7, 2014. Accessed January 19, 2015.
2. Shioiri T, Nishimura A, Akazawa K, et al. Incidence of note-leaving remains constant despite increasing suicide rates. Psychiatr Clin Neurosci. 2005;59(2):226-228.
3. Barr W, Leitner M, Thomas J. Self-harm or attempted suicide? Do suicide notes help us decide the level of intent in those who survive? Accid Emerg Nurs. 2007;15(3):122-127.
4. Foster T. Suicide note themes and suicide prevention. Int J Psychiatry Med. 2003;33(4):323-331.
5. Bhatia MS, Verma SK, Murty OP. Suicide notes: psychological and clinical profile. Int J Psychiatry Med. 2006;36(2):163-170.
6. Jashinsky J, Burton SH, Hanson CL, et al. Tracking suicide risk factors through Twitter in the US. Crisis. 2014;35(1):51-59.
7. Facebook news room. Company info. http://newsroom. fb.com/company-info. Accessed January 7, 2015.
8. Ruder TD, Hatch GM, Ampanozi G, et al. Suicide announcement on Facebook. Crisis. 2011;32(5):280-282.
9. Luxton DD, June JD, Fairall JM. Social media and suicide: a public health perspective. Am J Public Health. 2012;102(suppl 2):S195-S200.
10. Lehavot K, Ben-Zeev D, Neville RE. Ethical considerations and social media: a case of suicidal postings on Facebook. Journal of Dual Diagnosis. 2012;8(4):341-346.
11. Bennett A, Pourmand A, Shokoohi H, et al. Impacts of social networking sites on patient care in the emergency department. Telemed J E Health. 2014;20(1):94-96.
12. How to report suicidal content/threats on Facebook. h t tps ://www. facebook.com/notes/amer ican-foundation-for-suicide-prevention/how-to-report-suicidal-contentthreats-on-facebook/10150090259398144. Published February 15, 2011. Accessed January 22, 2015.
13. Mohri M, Rostamizadeh A, Talwalker A. Foundations of machine learning (adaptive computation and machine learning series). Cambridge, MA: MIT Press; 2012:14.
14. Blázquez Gil G, Berlanga de Jesús A, Molina Lopéz JM. Combining machine learning techniques and natural language processing to infer emotions using Spanish Twitter corpus. Communications in Computer and Information Science. 2013;365:149-157.
15. Poulin C, Shiner B, Thompson P, et al. Predicting the risk of suicide by analyzing the text of clinical notes. PLoS One. 2014;9(1):e85733.
16. Pestian JP, Matykiewicz P, Linn-Gust M. What’s in a note: construction of a suicide note corpus. Biomed Inform Insights. 2012;5:1-6.
17. ConsumerReports.org. Facebook & your privacy. http:// www.consumerreports.org/cro/magazine/2012/06/ facebook-your-privacy/index.html. Published June 2012. Accessed January 22, 2015
Prescriber’s guide to using 3 new antidepressants: Vilazodone, levomilnacipran, vortioxetine
With a prevalence >17%, depression is one of the most common mental disorders in the United States and the second leading cause of disability worldwide.1,2 For decades, primary care and mental health providers have used selective serotonin reuptake inhibitors (SSRIs) as first-line treatment for depression—yet the remission rate after the first trial of an antidepressant is <30%, and continues to decline after a first antidepressant failure.3
That is why clinicians continue to seek effective treatments for depression—ones that will provide quick and sustainable remission—and why scientists and pharmaceutical manufacturers have been competing to develop more effective antidepressant medications.
In the past 4 years, the FDA has approved 3 antidepressants—vilazodone, levomilnacipran, and vortioxetine—with the hope of increasing options for patients who suffer from major depression. These 3 antidepressants differ in their mechanisms of action from other available antidepressants, and all have been shown to have acceptable safety and tolerability profiles.
In this article, we review these novel antidepressants and present some clinical pearls for their use. We also present our observations that each agent appears to show particular advantage in a certain subpopulation of depressed patients who often do not respond, or who do not adequately respond, to other antidepressants.
Vilazodone
Vilazodone was approved by the FDA in 2011 (Table 1). The drug increases serotonin bioavailability in synapses through a strong dual action:
• blocking serotonin reuptake through the serotonin transporter
• partial agonism of the 5-HT1A presynaptic receptor.
Vilazodone also has a moderate effect on the 5-HT4 receptor and on dopamine and norepinephrine uptake inhibition.
The unique presynaptic 5-HT1A partial agonism of vilazodone is similar to that of buspirone, in which both drugs initially inhibit serotonin synthesis and neuronal firing.4 Researchers therefore expected that vilazodone would be more suitable for patients who have depression and a comorbid anxiety disorder; current FDA approval, however, is for depression only.
Adverse effects. The 5-HT4 receptor on which vilazodone acts is present in the gastrointestinal (GI) tract, and contributes to regulating symptoms in patients with irritable bowel syndrome (IBS)5; not surprisingly, the most frequent adverse effects of vilazodone are GI in nature (diarrhea, nausea, vomiting).
Headache is the most common non- GI side effect of vilazodone. Depressed patients who took vilazodone had no significant weight gain and did not report adverse sexual effects, compared with subjects given placebo.6
The following case—a patient with depression, significant anxiety, and IBS— exemplifies the type of patient for whom we find vilazodone most useful.
CASE Ms. A, age 19, is a college student with a history of major depressive disorder, social anxiety, and panic attacks for 2 years and IBS for 3 years. She was taking lubiprostone for IBS, with incomplete relief of GI symptoms. Because the family history included depression in Ms. A’s mother and sister, and both were doing well on escitalopram, we began a trial of that drug, 10 mg/d, that was quickly titrated to 20 mg/d.
Ms. A did not respond to 20 mg of escitalopram combined with psychotherapy.
We then started vilazodone, 10 mg/d after breakfast, for the first week, and reduced escitalopram to 10 mg/d. During Week 2, escitalopram was discontinued and vilazodone was increased to 20 mg/d. During Week 3, vilazodone was titrated to 40 mg/d.
Ms. A tolerated vilazodone well. Her depressive symptoms improved at the end of Week 2.
Unlike her experience with escitalopram, Ms. A’s anxiety symptoms—tenseness, racing thoughts, and panic attacks—all diminished when she switched to vilazodone. Notably, her IBS symptoms also were relieved, and she discontinued lubiprostone.
Ms. A’s depression remained in remission for 2 years, except for a brief period one summer, when she thought she “could do without any medication.” She tapered the vilazodone, week by week, to 10 mg/d, but her anxiety and bowel symptoms resurfaced to a degree that she resumed the 40-mg/d dosage.
Levomilnacipran
This drug is a 2013 addition to the small serotonin–norepinephrine reuptake inhibitor (SNRI) family of venlafaxine, desvenlafaxine, and duloxetine7 (Table 2). Levomilnacipran is the enantiomer of milnacipran, approved in Europe for depression but only for fibromyalgia pain and peripheral neuropathy in the United States.8 (Levomilnacipran is not FDA-approved for treating fibromyalgia pain.)
Levomilnacipran is unique because it is more of an NSRI, so to speak, than an SNRI: That is, the drug’s uptake inhibition of norepinephrine is more potent than its serotonin inhibition. Theoretically, levomilnacipran should help improve cognitive functions linked to the action of norepinephrine, such as concentration and motivation, and in turn, improve social function. The FDA also has approved levomilnacipran for treating functional impairment in depression.9
Adverse effects. The norepinephrine uptake inhibition of levomilnacipran might be responsible for observed increases in heart rate and blood pressure in some patients, and dose-dependent urinary hesitancy and erectile dysfunction in others. The drug has no significant effect on weight in depressed patients, compared with placebo.
Continue to: The benefits of levomilnacipran
The following case illustrates the benefits of levomilnacipran in a depressed patient who suffers from chronic pain and impaired social function.
CASE Mrs. C, age 44, was referred by her outpatient psychologist and her primary care provider for management of refractory depression. She did not respond to an SSRI, an SNRI, or augmentation with bupropion and aripiprazole.
Mrs. C was on disability leave from work because of depression and cervical spine pain that might have been related to repetitive movement as a telephone customer service representative. She complained of loss of motivation, fatigue, and high anxiety about returning to work because of the many unhappy customers she felt she had to soothe.
Levomilnacipran was started at 20 mg/d for 2 days, then titrated to 40 mg/d for 5 days, 80 mg/d for 1 week, and 120 mg/d thereafter. Her previous antidepressants, fluoxetine and bupropion, were discontinued while levomilnacipran was titrated.
Mrs. C continued to receive weekly psychotherapy and physical therapy and to take tizanidine, a muscle relaxant, and over-the-counter medications for pain. Her Patient Health Questionnaire (PHQ-9) score declined from 13 when levomilnacipran was started to 5 at the next visit, 6 weeks later.
Within 4 months of initiating levomilnacipran, Mrs. C returned to work with a series of cue cards to use when speaking with irate or unhappy customers. At that point, her cervical spine pain was barely noticeable and no longer interfered with function.
Vortioxetine
This agent has a novel multimodal mechanism of action (Table 3). It is an SSRI as well as a 5-HT1A full agonist and 5-HT3 receptor antagonist. Vortioxetine also has an inhibitory effect on 5-HT7 and 5-HT1D receptors and partial agonism of 5-HT1B receptors.
The downstream effect of this multimodal action is an increase in dopamine, norepinephrine, and acetylcholine activity in the prefrontal cortex.10 These downstream effects are thought to help restore some cognitive deficits associated with depression.11
Vortioxetine is the only antidepressant among the 3 discussed in this article that was studied over a long period to ensure that short-term benefits continue beyond the 6- to 8-week acute Phase-III studies. A high remission rate (61%) was observed in patients who were treated on an open-label basis with vortioxetine, 10 mg/d, then randomized to maintenance with vortioxetine or placebo.12
Older patients. Vortioxetine is unique among these 3 antidepressants in that it is the only one studied separately in geriatric patients: In an 8-week Phase-III trial, 452 geriatric patients age 64 to 88 were randomized to 5 mg/d of vortioxetine or placebo.13 Vortioxetine was significantly more effective than placebo at Week 6.
Vortioxetine also is the only antidepressant investigated for an effect on cognitive deficits: In a Phase-III double-blind, placebo-controlled study of 602 patients with major depressive disorder, using duloxetine as active reference, vortioxetine was found to have a significant effect on Digit Symbol Substitution Test scores, compared with placebo, independent of its antidepressant effect (ie, patients who did not show any antidepressant benefit still showed an improvement in attention, speed processing, memory, and executive function).14
We have found, therefore, that vortioxetine is helpful for depressed patients who have cognitive deficits, especially geriatric patients.
CASE Mrs. B, age 84, married, has a 4-year history of depression. She has taken several antidepressants with little consistent relief.
A brief psychiatric hospitalization 2 years ago temporarily reduced the severity of Mrs. B’s depression; gradually, she relapsed. She felt hopeless and resisted another psychiatric evaluation. Mrs. B’s family includes several clinicians, who wondered if she was developing cognitive deficits that were interfering with her recovery.
At initial evaluation, Mrs. B failed to recall 2 of 3 objects but performed the clock drawing test perfectly—qualifying her for a diagnosis of mild cognitive impairment in addition to major depression. Her PHQ-9 score at baseline was 22.
On the assumption that the severity of her depression was contributing to cognitive deficits, vortioxetine, 5 mg/d, was initiated for 2 weeks and then titrated to 10 mg/d.
At 4 weeks’ follow-up, Mrs. B passed the Mini-Cog test; her PHQ-9 score fell to 8. She has remained asymptomatic for 6 months at the 10-mg/d dosage; her lowest PHQ-9 score was 5.
Adverse effects. The most common adverse effects are mild or moderate GI in nature. Weight gain and adverse sexual effects were not significantly different among patients receiving vortioxetine than among patients given placebo.
A note about the safety of these agents
All 3 of these antidepressants carry the standard black-box warning about the elevated risk of suicide in patients taking an antidepressant. None of them are approved for patients age <18.
Continue to: Suicidal ideation was reported
Suicidal ideation was reported in 11.2% of patients taking vortioxetine, compared with 12.5% of those given placebo15; 24% of patients taking levomilnacipran reported suicidal ideation, compared with 22% of those who took placebo.16 In a long-term study of 599 patients taking vilazodone, 4 given placebo exhibited suicidal behavior, compared with 2 who took vilazodone.17
Drug-drug interactions are an important consideration when vilazodone, levomilnacipran, and vortioxetine are prescribed in combination with other medications. See the following discussion.
Vilazodone should be taken with food because it has 72% bioavailability after a meal.18 The drug is metabolized primarily by cytochrome P (CYP) 3A4 and CYP3A5; it does not affect CYP substrates or, it’s likely, produce significant changes to other medications metabolized by the CYP pathway.
Conversely, the dosage of vilazodone should be reduced to 20 mg/d if it is co- administered with a strong CYP3A4 inhibitor (eg, ketoconazole). The dosage should be increased as much as 2-fold when vilazodone is used concomitantly used with a strong CYP3A4 inducer (eg, carbamazepine) for >14 days. The maximum daily dosage should not exceed 80 mg/d.
Levomilnacipran. Unlike vilazodone and vortioxetine, levomilnacipran is affected by renal function.19 Concomitant medications, however, including those that influence CYP renal transporters (particularly CYP3A4, which metabolizes levomilnacipran), do not show an impact on the blood level of levomilnacipran.
No dosage adjustment is needed for patients who have mild renal impairment, but the maintenance dosage of levomilnacipran for patients who have moderate or severe renal impairment should not exceed 80 mg/d in 1 dose, and 60 mg/d in 1 dose, respectively.20
Vortioxetine. Seventy percent of a dose of vortioxetine is absorbed independent of food; the drug has a half-life of 66 hours. Vortioxetine is metabolized primarily by the CYP450 enzyme system, including 2D6, and, to a lesser extent, by CYP3A4, CYP3A5, CYP2C9, and CYP2C19.21
Vortioxetine has minimal effect on P450 substrates in in vitro studies, which was confirmed in 4 other in vivo studies.21-23 In studies of hormonal contraception, bupropion, and omeprazole, vortioxetine did not produce significant changes in the blood level of the other medications. The blood level of vortioxetine increased by 128% when taken with the CYP2D6 inhibitor bupropion,24 but the blood level did not markedly change with other inhibitors because the drug utilizes uses several CYP pathways. Use caution, therefore, when adding bupropion to vortioxetine because the combination elevates the risk of nausea, diarrhea, and headache.
With each agent, specific benefit
Vilazodone, levomilnacipran, and vortioxetine each add distinct benefit to the clinician’s toolbox of treatments for major depressive disorder. Although all antidepressants to some extent alleviate anxiety and pain and reverse cognitive decline associated with depression, our experience suggests using vilazodone for anxious depressed patients; levomilnacipran for depressed patients who experience pain; and vortioxetine for depressed patients who suffer cognitive decline and for geriatric patients.
Bottom Line
The FDA has approved 3 antidepressants in the past 4 years: vilazodone, levomilnacipran, and vortioxetine. The hope is that these agents will bolster treatment options for major depression—perhaps especially so, as we have seen, in the anxious depressed (vilazodone), the depressed in pain (levomilnacipran), and the depressed with cognitive decline, or geriatric patients (vortioxetine).
Related Resources
• Kalia R, Mittal M, Preskorn S. Vilazodone for major depressive disorder. Current Psychiatry. 2011;10(4):84-86,88.
• Lincoln J, Wehler C. Vortioxetine for major depressive disorder. Current Psychiatry. 2014;13(2):67-70.
• Macaluso M, Kazanchi H, Malhotra V. Levomilnacipran for the treatment of major depressive disorder. Current Psychiatry. 2013;12(12):50-52,54,55.
• McIntyre RS, Lophaven S, Olsen CK. A randomized, double-blind, placebo-controlled study of vortioxetine on cognitive function in depressed adults. Int J Neuropsychopharmacol. 2014;17(10):1557-1567.
• Thase ME, Chen D, Edwards J, et al. Efficacy of vilazodone on anxiety symptoms in patients with major depressive disorder. Int Clin Psychopharmacol. 2014;29(6):351-356.
Drug Brand Names
Aripiprazole • Abilify Levomilnacipran • Fetzima
Bupropion • Wellbutrin, Zyban Lubiprostone • Amitiza
Buspirone • BuSpar Milnacipran • Savella
Carbamazepine • Tegretol, Equetro Omeprazole • Prilosec
Desvenlafaxine • Pristiq Tizanidine • Zanaflex
Duloxetine • Cymbalta Venlafaxine • Effexor
Escitalopram • Lexapro Vilazodone • Viibryd
Fluoxetine • Prozac Vortioxetine • Brintellix
Ketoconazole • Nizoral
1. Andrade L, Caraveo-Anduaga JJ, Berglund P, et al. The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. Int J Methods Psychiatr Res. 2003;12(1):3-21.
2. Ferrari AJ, Charlson FJ, Norman RE, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10(11):e1001547.
3. Warden D, Rush AJ, Trivedi MH, et al. The STAR*D Project results: a comprehensive review of findings. Curr Psychiatry Rep. 2007;9(6):449-459.
4. Khan A. Vilazodone, a novel dual-acting serotonergic antidepressant for managing major depression. Expert Opin Investig Drugs. 2009;18(11):1753-1764.
5. Khan A, Sambunaris A, Edwards J, et al. Vilazodone in the treatment of major depressive disorder: efficacy across symptoms and severity of depression. Int Clin Psychopharmacol. 2014;29(2):86-92.
6. Robinson DS, Kajdasz DK, Gallipoli S, et al. A 1-year, open-label study assessing the safety and tolerability of vilazodone in patients with major depressive disorder. J Clin Psychopharmacol. 2011;31(5):643-646.
7. Saraceni MM, Venci JV, Gandhi MA. Levomilnacipran (Fetzima): a new serotonin-norepinephrine reuptake inhibitor for the treatment of major depressive disorder. J Pharm Pract. 2013;27(4):389-395.
8. Deardorff WJ, Grossberg GT. A review of the clinical efficacy, safety and tolerability of the antidepressants vilazodone, levomilnacipran and vortioxetine. Expert Opin Pharmacother. 2014;15(17):2525-2542.
9. Citrome L. Levomilnacipran for major depressive disorder: a systematic review of the efficacy and safety profile for this newly approved antidepressant—what is the number needed to treat, number needed to harm and likelihood to be helped or harmed? Int J Clin Pract. 2013;67(11):1089-1104.
10. Mørk A, Pehrson A, Brennum LT, et al. Pharmacological effects of Lu AA21004: a novel multimodal compound for the treatment of major depressive disorder. J Pharmacol Exp Ther. 2012;340(3):666-675.
11. Pehrson AL, Leiser SC, Gulinello M, et al. Treatment of cognitive dysfunction in major depressive disorder-a review of the preclinical evidence for efficacy of selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors and the multimodal-acting antidepressant vortioxetine [published online August 5, 2014]. Eur J Pharmacol. doi: 10.1016/j.ejphar.2014.07.044.
12. Baldwin DS, Hansen T, Florea I. Vortioxetine (Lu AA21004) in the long-term open-label treatment of major depressive disorder. Curr Med Res Opin. 2012;28(10):1717-1724.
13. Katona C, Hansen T, Olsen CK. A randomized, double-blind, placebo-controlled, duloxetine-referenced, fixed-dose study comparing the efficacy and safety of Lu AA21004 in elderly patients with major depressive disorder. Int Clin Psychopharmacol. 2012;27(4):215-523.
14. Raskin J, Wiltse CG, Siegal A, et al. Efficacy of duloxetine on cognition, depression, and pain in elderly patients with major depressive disorder: an 8-week, double-blind, placebo-controlled trial. Am J Psychiatry. 2007;164(6): 900-909.
15. Boulenger JP, Loft H, Olsen CK. Efficacy and safety of vortioxetine (Lu AA21004), 15 and 20 mg/day: a randomized, double-blind, placebo-controlled, duloxetine-referenced study in the acute treatment of adult patients with major depressive disorder. Int Clin Psychopharmacol. 2014;29(3):138-149.
16. Mago R, Forero G, Greenberg WM, et al. Safety and tolerability of levomilnacipran ER in major depressive disorder: results from an open-label, 48-week extension study. Clin Drug Investig. 2013;33(10):761-771.
17. Khan A, Sambunaris A, Edwards J, et al. Vilazodone in the treatment of major depressive disorder: efficacy across symptoms and severity of depression. Int Clin Psychopharmacol. 2014;29(2):86-92.
18. Boinpally R, Gad N, Gupta S, et al. Influence of CYP3A4 induction/inhibition on the pharmacokinetics of vilazodone in healthy subjects. Clin Ther. 2014; 36(11):1638-1649.
19. Chen L, Boinpally R, Greenberg WM, et al. Effect of hepatic impairment on the pharmacokinetics of levomilnacipran following a single oral dose of a levomilnacipran extended-release capsule in human participants. Clin Drug Investig. 2014;34(5):351-359.
20. Asnis GM, Bose A, Gommoll CP, et al. Efficacy and safety of levomilnacipran sustained release 40 mg, 80 mg, or 120 mg in major depressive disorder: a phase 3, randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2013;74(3):242-248.
21. Hvenegaard MG, Bang-Andersen B, Pedersen H, et al. Identification of the cytochrome P450 and other enzymes involved in the in vitro oxidative metabolism of a novel antidepressant, Lu AA21004. Drug Metab Dispos. 2012; 40(7):1357-1365.
22. Chen G, Lee R, Højer AM, et al. Pharmacokinetic drug interactions involving vortioxetine (Lu AA21004), a multimodal antidepressant. Clin Drug Investig. 2013; 33(10):727-736.
23. Areberg J, Søgaard B, Højer AM. The clinical pharmacokinetics of Lu AA21004 and its major metabolite in healthy young volunteers. Basic Clin Pharmacol Toxicol. 2012;111(3):198-205.
24. Areberg J, Petersen KB, Chen G, et al. Population pharmacokinetic meta-analysis of vortioxetine in healthy individuals. Basic Clin Pharmacol Toxicol. 2014;115(6):552-559.
With a prevalence >17%, depression is one of the most common mental disorders in the United States and the second leading cause of disability worldwide.1,2 For decades, primary care and mental health providers have used selective serotonin reuptake inhibitors (SSRIs) as first-line treatment for depression—yet the remission rate after the first trial of an antidepressant is <30%, and continues to decline after a first antidepressant failure.3
That is why clinicians continue to seek effective treatments for depression—ones that will provide quick and sustainable remission—and why scientists and pharmaceutical manufacturers have been competing to develop more effective antidepressant medications.
In the past 4 years, the FDA has approved 3 antidepressants—vilazodone, levomilnacipran, and vortioxetine—with the hope of increasing options for patients who suffer from major depression. These 3 antidepressants differ in their mechanisms of action from other available antidepressants, and all have been shown to have acceptable safety and tolerability profiles.
In this article, we review these novel antidepressants and present some clinical pearls for their use. We also present our observations that each agent appears to show particular advantage in a certain subpopulation of depressed patients who often do not respond, or who do not adequately respond, to other antidepressants.
Vilazodone
Vilazodone was approved by the FDA in 2011 (Table 1). The drug increases serotonin bioavailability in synapses through a strong dual action:
• blocking serotonin reuptake through the serotonin transporter
• partial agonism of the 5-HT1A presynaptic receptor.
Vilazodone also has a moderate effect on the 5-HT4 receptor and on dopamine and norepinephrine uptake inhibition.
The unique presynaptic 5-HT1A partial agonism of vilazodone is similar to that of buspirone, in which both drugs initially inhibit serotonin synthesis and neuronal firing.4 Researchers therefore expected that vilazodone would be more suitable for patients who have depression and a comorbid anxiety disorder; current FDA approval, however, is for depression only.
Adverse effects. The 5-HT4 receptor on which vilazodone acts is present in the gastrointestinal (GI) tract, and contributes to regulating symptoms in patients with irritable bowel syndrome (IBS)5; not surprisingly, the most frequent adverse effects of vilazodone are GI in nature (diarrhea, nausea, vomiting).
Headache is the most common non- GI side effect of vilazodone. Depressed patients who took vilazodone had no significant weight gain and did not report adverse sexual effects, compared with subjects given placebo.6
The following case—a patient with depression, significant anxiety, and IBS— exemplifies the type of patient for whom we find vilazodone most useful.
CASE Ms. A, age 19, is a college student with a history of major depressive disorder, social anxiety, and panic attacks for 2 years and IBS for 3 years. She was taking lubiprostone for IBS, with incomplete relief of GI symptoms. Because the family history included depression in Ms. A’s mother and sister, and both were doing well on escitalopram, we began a trial of that drug, 10 mg/d, that was quickly titrated to 20 mg/d.
Ms. A did not respond to 20 mg of escitalopram combined with psychotherapy.
We then started vilazodone, 10 mg/d after breakfast, for the first week, and reduced escitalopram to 10 mg/d. During Week 2, escitalopram was discontinued and vilazodone was increased to 20 mg/d. During Week 3, vilazodone was titrated to 40 mg/d.
Ms. A tolerated vilazodone well. Her depressive symptoms improved at the end of Week 2.
Unlike her experience with escitalopram, Ms. A’s anxiety symptoms—tenseness, racing thoughts, and panic attacks—all diminished when she switched to vilazodone. Notably, her IBS symptoms also were relieved, and she discontinued lubiprostone.
Ms. A’s depression remained in remission for 2 years, except for a brief period one summer, when she thought she “could do without any medication.” She tapered the vilazodone, week by week, to 10 mg/d, but her anxiety and bowel symptoms resurfaced to a degree that she resumed the 40-mg/d dosage.
Levomilnacipran
This drug is a 2013 addition to the small serotonin–norepinephrine reuptake inhibitor (SNRI) family of venlafaxine, desvenlafaxine, and duloxetine7 (Table 2). Levomilnacipran is the enantiomer of milnacipran, approved in Europe for depression but only for fibromyalgia pain and peripheral neuropathy in the United States.8 (Levomilnacipran is not FDA-approved for treating fibromyalgia pain.)
Levomilnacipran is unique because it is more of an NSRI, so to speak, than an SNRI: That is, the drug’s uptake inhibition of norepinephrine is more potent than its serotonin inhibition. Theoretically, levomilnacipran should help improve cognitive functions linked to the action of norepinephrine, such as concentration and motivation, and in turn, improve social function. The FDA also has approved levomilnacipran for treating functional impairment in depression.9
Adverse effects. The norepinephrine uptake inhibition of levomilnacipran might be responsible for observed increases in heart rate and blood pressure in some patients, and dose-dependent urinary hesitancy and erectile dysfunction in others. The drug has no significant effect on weight in depressed patients, compared with placebo.
Continue to: The benefits of levomilnacipran
The following case illustrates the benefits of levomilnacipran in a depressed patient who suffers from chronic pain and impaired social function.
CASE Mrs. C, age 44, was referred by her outpatient psychologist and her primary care provider for management of refractory depression. She did not respond to an SSRI, an SNRI, or augmentation with bupropion and aripiprazole.
Mrs. C was on disability leave from work because of depression and cervical spine pain that might have been related to repetitive movement as a telephone customer service representative. She complained of loss of motivation, fatigue, and high anxiety about returning to work because of the many unhappy customers she felt she had to soothe.
Levomilnacipran was started at 20 mg/d for 2 days, then titrated to 40 mg/d for 5 days, 80 mg/d for 1 week, and 120 mg/d thereafter. Her previous antidepressants, fluoxetine and bupropion, were discontinued while levomilnacipran was titrated.
Mrs. C continued to receive weekly psychotherapy and physical therapy and to take tizanidine, a muscle relaxant, and over-the-counter medications for pain. Her Patient Health Questionnaire (PHQ-9) score declined from 13 when levomilnacipran was started to 5 at the next visit, 6 weeks later.
Within 4 months of initiating levomilnacipran, Mrs. C returned to work with a series of cue cards to use when speaking with irate or unhappy customers. At that point, her cervical spine pain was barely noticeable and no longer interfered with function.
Vortioxetine
This agent has a novel multimodal mechanism of action (Table 3). It is an SSRI as well as a 5-HT1A full agonist and 5-HT3 receptor antagonist. Vortioxetine also has an inhibitory effect on 5-HT7 and 5-HT1D receptors and partial agonism of 5-HT1B receptors.
The downstream effect of this multimodal action is an increase in dopamine, norepinephrine, and acetylcholine activity in the prefrontal cortex.10 These downstream effects are thought to help restore some cognitive deficits associated with depression.11
Vortioxetine is the only antidepressant among the 3 discussed in this article that was studied over a long period to ensure that short-term benefits continue beyond the 6- to 8-week acute Phase-III studies. A high remission rate (61%) was observed in patients who were treated on an open-label basis with vortioxetine, 10 mg/d, then randomized to maintenance with vortioxetine or placebo.12
Older patients. Vortioxetine is unique among these 3 antidepressants in that it is the only one studied separately in geriatric patients: In an 8-week Phase-III trial, 452 geriatric patients age 64 to 88 were randomized to 5 mg/d of vortioxetine or placebo.13 Vortioxetine was significantly more effective than placebo at Week 6.
Vortioxetine also is the only antidepressant investigated for an effect on cognitive deficits: In a Phase-III double-blind, placebo-controlled study of 602 patients with major depressive disorder, using duloxetine as active reference, vortioxetine was found to have a significant effect on Digit Symbol Substitution Test scores, compared with placebo, independent of its antidepressant effect (ie, patients who did not show any antidepressant benefit still showed an improvement in attention, speed processing, memory, and executive function).14
We have found, therefore, that vortioxetine is helpful for depressed patients who have cognitive deficits, especially geriatric patients.
CASE Mrs. B, age 84, married, has a 4-year history of depression. She has taken several antidepressants with little consistent relief.
A brief psychiatric hospitalization 2 years ago temporarily reduced the severity of Mrs. B’s depression; gradually, she relapsed. She felt hopeless and resisted another psychiatric evaluation. Mrs. B’s family includes several clinicians, who wondered if she was developing cognitive deficits that were interfering with her recovery.
At initial evaluation, Mrs. B failed to recall 2 of 3 objects but performed the clock drawing test perfectly—qualifying her for a diagnosis of mild cognitive impairment in addition to major depression. Her PHQ-9 score at baseline was 22.
On the assumption that the severity of her depression was contributing to cognitive deficits, vortioxetine, 5 mg/d, was initiated for 2 weeks and then titrated to 10 mg/d.
At 4 weeks’ follow-up, Mrs. B passed the Mini-Cog test; her PHQ-9 score fell to 8. She has remained asymptomatic for 6 months at the 10-mg/d dosage; her lowest PHQ-9 score was 5.
Adverse effects. The most common adverse effects are mild or moderate GI in nature. Weight gain and adverse sexual effects were not significantly different among patients receiving vortioxetine than among patients given placebo.
A note about the safety of these agents
All 3 of these antidepressants carry the standard black-box warning about the elevated risk of suicide in patients taking an antidepressant. None of them are approved for patients age <18.
Continue to: Suicidal ideation was reported
Suicidal ideation was reported in 11.2% of patients taking vortioxetine, compared with 12.5% of those given placebo15; 24% of patients taking levomilnacipran reported suicidal ideation, compared with 22% of those who took placebo.16 In a long-term study of 599 patients taking vilazodone, 4 given placebo exhibited suicidal behavior, compared with 2 who took vilazodone.17
Drug-drug interactions are an important consideration when vilazodone, levomilnacipran, and vortioxetine are prescribed in combination with other medications. See the following discussion.
Vilazodone should be taken with food because it has 72% bioavailability after a meal.18 The drug is metabolized primarily by cytochrome P (CYP) 3A4 and CYP3A5; it does not affect CYP substrates or, it’s likely, produce significant changes to other medications metabolized by the CYP pathway.
Conversely, the dosage of vilazodone should be reduced to 20 mg/d if it is co- administered with a strong CYP3A4 inhibitor (eg, ketoconazole). The dosage should be increased as much as 2-fold when vilazodone is used concomitantly used with a strong CYP3A4 inducer (eg, carbamazepine) for >14 days. The maximum daily dosage should not exceed 80 mg/d.
Levomilnacipran. Unlike vilazodone and vortioxetine, levomilnacipran is affected by renal function.19 Concomitant medications, however, including those that influence CYP renal transporters (particularly CYP3A4, which metabolizes levomilnacipran), do not show an impact on the blood level of levomilnacipran.
No dosage adjustment is needed for patients who have mild renal impairment, but the maintenance dosage of levomilnacipran for patients who have moderate or severe renal impairment should not exceed 80 mg/d in 1 dose, and 60 mg/d in 1 dose, respectively.20
Vortioxetine. Seventy percent of a dose of vortioxetine is absorbed independent of food; the drug has a half-life of 66 hours. Vortioxetine is metabolized primarily by the CYP450 enzyme system, including 2D6, and, to a lesser extent, by CYP3A4, CYP3A5, CYP2C9, and CYP2C19.21
Vortioxetine has minimal effect on P450 substrates in in vitro studies, which was confirmed in 4 other in vivo studies.21-23 In studies of hormonal contraception, bupropion, and omeprazole, vortioxetine did not produce significant changes in the blood level of the other medications. The blood level of vortioxetine increased by 128% when taken with the CYP2D6 inhibitor bupropion,24 but the blood level did not markedly change with other inhibitors because the drug utilizes uses several CYP pathways. Use caution, therefore, when adding bupropion to vortioxetine because the combination elevates the risk of nausea, diarrhea, and headache.
With each agent, specific benefit
Vilazodone, levomilnacipran, and vortioxetine each add distinct benefit to the clinician’s toolbox of treatments for major depressive disorder. Although all antidepressants to some extent alleviate anxiety and pain and reverse cognitive decline associated with depression, our experience suggests using vilazodone for anxious depressed patients; levomilnacipran for depressed patients who experience pain; and vortioxetine for depressed patients who suffer cognitive decline and for geriatric patients.
Bottom Line
The FDA has approved 3 antidepressants in the past 4 years: vilazodone, levomilnacipran, and vortioxetine. The hope is that these agents will bolster treatment options for major depression—perhaps especially so, as we have seen, in the anxious depressed (vilazodone), the depressed in pain (levomilnacipran), and the depressed with cognitive decline, or geriatric patients (vortioxetine).
Related Resources
• Kalia R, Mittal M, Preskorn S. Vilazodone for major depressive disorder. Current Psychiatry. 2011;10(4):84-86,88.
• Lincoln J, Wehler C. Vortioxetine for major depressive disorder. Current Psychiatry. 2014;13(2):67-70.
• Macaluso M, Kazanchi H, Malhotra V. Levomilnacipran for the treatment of major depressive disorder. Current Psychiatry. 2013;12(12):50-52,54,55.
• McIntyre RS, Lophaven S, Olsen CK. A randomized, double-blind, placebo-controlled study of vortioxetine on cognitive function in depressed adults. Int J Neuropsychopharmacol. 2014;17(10):1557-1567.
• Thase ME, Chen D, Edwards J, et al. Efficacy of vilazodone on anxiety symptoms in patients with major depressive disorder. Int Clin Psychopharmacol. 2014;29(6):351-356.
Drug Brand Names
Aripiprazole • Abilify Levomilnacipran • Fetzima
Bupropion • Wellbutrin, Zyban Lubiprostone • Amitiza
Buspirone • BuSpar Milnacipran • Savella
Carbamazepine • Tegretol, Equetro Omeprazole • Prilosec
Desvenlafaxine • Pristiq Tizanidine • Zanaflex
Duloxetine • Cymbalta Venlafaxine • Effexor
Escitalopram • Lexapro Vilazodone • Viibryd
Fluoxetine • Prozac Vortioxetine • Brintellix
Ketoconazole • Nizoral
With a prevalence >17%, depression is one of the most common mental disorders in the United States and the second leading cause of disability worldwide.1,2 For decades, primary care and mental health providers have used selective serotonin reuptake inhibitors (SSRIs) as first-line treatment for depression—yet the remission rate after the first trial of an antidepressant is <30%, and continues to decline after a first antidepressant failure.3
That is why clinicians continue to seek effective treatments for depression—ones that will provide quick and sustainable remission—and why scientists and pharmaceutical manufacturers have been competing to develop more effective antidepressant medications.
In the past 4 years, the FDA has approved 3 antidepressants—vilazodone, levomilnacipran, and vortioxetine—with the hope of increasing options for patients who suffer from major depression. These 3 antidepressants differ in their mechanisms of action from other available antidepressants, and all have been shown to have acceptable safety and tolerability profiles.
In this article, we review these novel antidepressants and present some clinical pearls for their use. We also present our observations that each agent appears to show particular advantage in a certain subpopulation of depressed patients who often do not respond, or who do not adequately respond, to other antidepressants.
Vilazodone
Vilazodone was approved by the FDA in 2011 (Table 1). The drug increases serotonin bioavailability in synapses through a strong dual action:
• blocking serotonin reuptake through the serotonin transporter
• partial agonism of the 5-HT1A presynaptic receptor.
Vilazodone also has a moderate effect on the 5-HT4 receptor and on dopamine and norepinephrine uptake inhibition.
The unique presynaptic 5-HT1A partial agonism of vilazodone is similar to that of buspirone, in which both drugs initially inhibit serotonin synthesis and neuronal firing.4 Researchers therefore expected that vilazodone would be more suitable for patients who have depression and a comorbid anxiety disorder; current FDA approval, however, is for depression only.
Adverse effects. The 5-HT4 receptor on which vilazodone acts is present in the gastrointestinal (GI) tract, and contributes to regulating symptoms in patients with irritable bowel syndrome (IBS)5; not surprisingly, the most frequent adverse effects of vilazodone are GI in nature (diarrhea, nausea, vomiting).
Headache is the most common non- GI side effect of vilazodone. Depressed patients who took vilazodone had no significant weight gain and did not report adverse sexual effects, compared with subjects given placebo.6
The following case—a patient with depression, significant anxiety, and IBS— exemplifies the type of patient for whom we find vilazodone most useful.
CASE Ms. A, age 19, is a college student with a history of major depressive disorder, social anxiety, and panic attacks for 2 years and IBS for 3 years. She was taking lubiprostone for IBS, with incomplete relief of GI symptoms. Because the family history included depression in Ms. A’s mother and sister, and both were doing well on escitalopram, we began a trial of that drug, 10 mg/d, that was quickly titrated to 20 mg/d.
Ms. A did not respond to 20 mg of escitalopram combined with psychotherapy.
We then started vilazodone, 10 mg/d after breakfast, for the first week, and reduced escitalopram to 10 mg/d. During Week 2, escitalopram was discontinued and vilazodone was increased to 20 mg/d. During Week 3, vilazodone was titrated to 40 mg/d.
Ms. A tolerated vilazodone well. Her depressive symptoms improved at the end of Week 2.
Unlike her experience with escitalopram, Ms. A’s anxiety symptoms—tenseness, racing thoughts, and panic attacks—all diminished when she switched to vilazodone. Notably, her IBS symptoms also were relieved, and she discontinued lubiprostone.
Ms. A’s depression remained in remission for 2 years, except for a brief period one summer, when she thought she “could do without any medication.” She tapered the vilazodone, week by week, to 10 mg/d, but her anxiety and bowel symptoms resurfaced to a degree that she resumed the 40-mg/d dosage.
Levomilnacipran
This drug is a 2013 addition to the small serotonin–norepinephrine reuptake inhibitor (SNRI) family of venlafaxine, desvenlafaxine, and duloxetine7 (Table 2). Levomilnacipran is the enantiomer of milnacipran, approved in Europe for depression but only for fibromyalgia pain and peripheral neuropathy in the United States.8 (Levomilnacipran is not FDA-approved for treating fibromyalgia pain.)
Levomilnacipran is unique because it is more of an NSRI, so to speak, than an SNRI: That is, the drug’s uptake inhibition of norepinephrine is more potent than its serotonin inhibition. Theoretically, levomilnacipran should help improve cognitive functions linked to the action of norepinephrine, such as concentration and motivation, and in turn, improve social function. The FDA also has approved levomilnacipran for treating functional impairment in depression.9
Adverse effects. The norepinephrine uptake inhibition of levomilnacipran might be responsible for observed increases in heart rate and blood pressure in some patients, and dose-dependent urinary hesitancy and erectile dysfunction in others. The drug has no significant effect on weight in depressed patients, compared with placebo.
Continue to: The benefits of levomilnacipran
The following case illustrates the benefits of levomilnacipran in a depressed patient who suffers from chronic pain and impaired social function.
CASE Mrs. C, age 44, was referred by her outpatient psychologist and her primary care provider for management of refractory depression. She did not respond to an SSRI, an SNRI, or augmentation with bupropion and aripiprazole.
Mrs. C was on disability leave from work because of depression and cervical spine pain that might have been related to repetitive movement as a telephone customer service representative. She complained of loss of motivation, fatigue, and high anxiety about returning to work because of the many unhappy customers she felt she had to soothe.
Levomilnacipran was started at 20 mg/d for 2 days, then titrated to 40 mg/d for 5 days, 80 mg/d for 1 week, and 120 mg/d thereafter. Her previous antidepressants, fluoxetine and bupropion, were discontinued while levomilnacipran was titrated.
Mrs. C continued to receive weekly psychotherapy and physical therapy and to take tizanidine, a muscle relaxant, and over-the-counter medications for pain. Her Patient Health Questionnaire (PHQ-9) score declined from 13 when levomilnacipran was started to 5 at the next visit, 6 weeks later.
Within 4 months of initiating levomilnacipran, Mrs. C returned to work with a series of cue cards to use when speaking with irate or unhappy customers. At that point, her cervical spine pain was barely noticeable and no longer interfered with function.
Vortioxetine
This agent has a novel multimodal mechanism of action (Table 3). It is an SSRI as well as a 5-HT1A full agonist and 5-HT3 receptor antagonist. Vortioxetine also has an inhibitory effect on 5-HT7 and 5-HT1D receptors and partial agonism of 5-HT1B receptors.
The downstream effect of this multimodal action is an increase in dopamine, norepinephrine, and acetylcholine activity in the prefrontal cortex.10 These downstream effects are thought to help restore some cognitive deficits associated with depression.11
Vortioxetine is the only antidepressant among the 3 discussed in this article that was studied over a long period to ensure that short-term benefits continue beyond the 6- to 8-week acute Phase-III studies. A high remission rate (61%) was observed in patients who were treated on an open-label basis with vortioxetine, 10 mg/d, then randomized to maintenance with vortioxetine or placebo.12
Older patients. Vortioxetine is unique among these 3 antidepressants in that it is the only one studied separately in geriatric patients: In an 8-week Phase-III trial, 452 geriatric patients age 64 to 88 were randomized to 5 mg/d of vortioxetine or placebo.13 Vortioxetine was significantly more effective than placebo at Week 6.
Vortioxetine also is the only antidepressant investigated for an effect on cognitive deficits: In a Phase-III double-blind, placebo-controlled study of 602 patients with major depressive disorder, using duloxetine as active reference, vortioxetine was found to have a significant effect on Digit Symbol Substitution Test scores, compared with placebo, independent of its antidepressant effect (ie, patients who did not show any antidepressant benefit still showed an improvement in attention, speed processing, memory, and executive function).14
We have found, therefore, that vortioxetine is helpful for depressed patients who have cognitive deficits, especially geriatric patients.
CASE Mrs. B, age 84, married, has a 4-year history of depression. She has taken several antidepressants with little consistent relief.
A brief psychiatric hospitalization 2 years ago temporarily reduced the severity of Mrs. B’s depression; gradually, she relapsed. She felt hopeless and resisted another psychiatric evaluation. Mrs. B’s family includes several clinicians, who wondered if she was developing cognitive deficits that were interfering with her recovery.
At initial evaluation, Mrs. B failed to recall 2 of 3 objects but performed the clock drawing test perfectly—qualifying her for a diagnosis of mild cognitive impairment in addition to major depression. Her PHQ-9 score at baseline was 22.
On the assumption that the severity of her depression was contributing to cognitive deficits, vortioxetine, 5 mg/d, was initiated for 2 weeks and then titrated to 10 mg/d.
At 4 weeks’ follow-up, Mrs. B passed the Mini-Cog test; her PHQ-9 score fell to 8. She has remained asymptomatic for 6 months at the 10-mg/d dosage; her lowest PHQ-9 score was 5.
Adverse effects. The most common adverse effects are mild or moderate GI in nature. Weight gain and adverse sexual effects were not significantly different among patients receiving vortioxetine than among patients given placebo.
A note about the safety of these agents
All 3 of these antidepressants carry the standard black-box warning about the elevated risk of suicide in patients taking an antidepressant. None of them are approved for patients age <18.
Continue to: Suicidal ideation was reported
Suicidal ideation was reported in 11.2% of patients taking vortioxetine, compared with 12.5% of those given placebo15; 24% of patients taking levomilnacipran reported suicidal ideation, compared with 22% of those who took placebo.16 In a long-term study of 599 patients taking vilazodone, 4 given placebo exhibited suicidal behavior, compared with 2 who took vilazodone.17
Drug-drug interactions are an important consideration when vilazodone, levomilnacipran, and vortioxetine are prescribed in combination with other medications. See the following discussion.
Vilazodone should be taken with food because it has 72% bioavailability after a meal.18 The drug is metabolized primarily by cytochrome P (CYP) 3A4 and CYP3A5; it does not affect CYP substrates or, it’s likely, produce significant changes to other medications metabolized by the CYP pathway.
Conversely, the dosage of vilazodone should be reduced to 20 mg/d if it is co- administered with a strong CYP3A4 inhibitor (eg, ketoconazole). The dosage should be increased as much as 2-fold when vilazodone is used concomitantly used with a strong CYP3A4 inducer (eg, carbamazepine) for >14 days. The maximum daily dosage should not exceed 80 mg/d.
Levomilnacipran. Unlike vilazodone and vortioxetine, levomilnacipran is affected by renal function.19 Concomitant medications, however, including those that influence CYP renal transporters (particularly CYP3A4, which metabolizes levomilnacipran), do not show an impact on the blood level of levomilnacipran.
No dosage adjustment is needed for patients who have mild renal impairment, but the maintenance dosage of levomilnacipran for patients who have moderate or severe renal impairment should not exceed 80 mg/d in 1 dose, and 60 mg/d in 1 dose, respectively.20
Vortioxetine. Seventy percent of a dose of vortioxetine is absorbed independent of food; the drug has a half-life of 66 hours. Vortioxetine is metabolized primarily by the CYP450 enzyme system, including 2D6, and, to a lesser extent, by CYP3A4, CYP3A5, CYP2C9, and CYP2C19.21
Vortioxetine has minimal effect on P450 substrates in in vitro studies, which was confirmed in 4 other in vivo studies.21-23 In studies of hormonal contraception, bupropion, and omeprazole, vortioxetine did not produce significant changes in the blood level of the other medications. The blood level of vortioxetine increased by 128% when taken with the CYP2D6 inhibitor bupropion,24 but the blood level did not markedly change with other inhibitors because the drug utilizes uses several CYP pathways. Use caution, therefore, when adding bupropion to vortioxetine because the combination elevates the risk of nausea, diarrhea, and headache.
With each agent, specific benefit
Vilazodone, levomilnacipran, and vortioxetine each add distinct benefit to the clinician’s toolbox of treatments for major depressive disorder. Although all antidepressants to some extent alleviate anxiety and pain and reverse cognitive decline associated with depression, our experience suggests using vilazodone for anxious depressed patients; levomilnacipran for depressed patients who experience pain; and vortioxetine for depressed patients who suffer cognitive decline and for geriatric patients.
Bottom Line
The FDA has approved 3 antidepressants in the past 4 years: vilazodone, levomilnacipran, and vortioxetine. The hope is that these agents will bolster treatment options for major depression—perhaps especially so, as we have seen, in the anxious depressed (vilazodone), the depressed in pain (levomilnacipran), and the depressed with cognitive decline, or geriatric patients (vortioxetine).
Related Resources
• Kalia R, Mittal M, Preskorn S. Vilazodone for major depressive disorder. Current Psychiatry. 2011;10(4):84-86,88.
• Lincoln J, Wehler C. Vortioxetine for major depressive disorder. Current Psychiatry. 2014;13(2):67-70.
• Macaluso M, Kazanchi H, Malhotra V. Levomilnacipran for the treatment of major depressive disorder. Current Psychiatry. 2013;12(12):50-52,54,55.
• McIntyre RS, Lophaven S, Olsen CK. A randomized, double-blind, placebo-controlled study of vortioxetine on cognitive function in depressed adults. Int J Neuropsychopharmacol. 2014;17(10):1557-1567.
• Thase ME, Chen D, Edwards J, et al. Efficacy of vilazodone on anxiety symptoms in patients with major depressive disorder. Int Clin Psychopharmacol. 2014;29(6):351-356.
Drug Brand Names
Aripiprazole • Abilify Levomilnacipran • Fetzima
Bupropion • Wellbutrin, Zyban Lubiprostone • Amitiza
Buspirone • BuSpar Milnacipran • Savella
Carbamazepine • Tegretol, Equetro Omeprazole • Prilosec
Desvenlafaxine • Pristiq Tizanidine • Zanaflex
Duloxetine • Cymbalta Venlafaxine • Effexor
Escitalopram • Lexapro Vilazodone • Viibryd
Fluoxetine • Prozac Vortioxetine • Brintellix
Ketoconazole • Nizoral
1. Andrade L, Caraveo-Anduaga JJ, Berglund P, et al. The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. Int J Methods Psychiatr Res. 2003;12(1):3-21.
2. Ferrari AJ, Charlson FJ, Norman RE, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10(11):e1001547.
3. Warden D, Rush AJ, Trivedi MH, et al. The STAR*D Project results: a comprehensive review of findings. Curr Psychiatry Rep. 2007;9(6):449-459.
4. Khan A. Vilazodone, a novel dual-acting serotonergic antidepressant for managing major depression. Expert Opin Investig Drugs. 2009;18(11):1753-1764.
5. Khan A, Sambunaris A, Edwards J, et al. Vilazodone in the treatment of major depressive disorder: efficacy across symptoms and severity of depression. Int Clin Psychopharmacol. 2014;29(2):86-92.
6. Robinson DS, Kajdasz DK, Gallipoli S, et al. A 1-year, open-label study assessing the safety and tolerability of vilazodone in patients with major depressive disorder. J Clin Psychopharmacol. 2011;31(5):643-646.
7. Saraceni MM, Venci JV, Gandhi MA. Levomilnacipran (Fetzima): a new serotonin-norepinephrine reuptake inhibitor for the treatment of major depressive disorder. J Pharm Pract. 2013;27(4):389-395.
8. Deardorff WJ, Grossberg GT. A review of the clinical efficacy, safety and tolerability of the antidepressants vilazodone, levomilnacipran and vortioxetine. Expert Opin Pharmacother. 2014;15(17):2525-2542.
9. Citrome L. Levomilnacipran for major depressive disorder: a systematic review of the efficacy and safety profile for this newly approved antidepressant—what is the number needed to treat, number needed to harm and likelihood to be helped or harmed? Int J Clin Pract. 2013;67(11):1089-1104.
10. Mørk A, Pehrson A, Brennum LT, et al. Pharmacological effects of Lu AA21004: a novel multimodal compound for the treatment of major depressive disorder. J Pharmacol Exp Ther. 2012;340(3):666-675.
11. Pehrson AL, Leiser SC, Gulinello M, et al. Treatment of cognitive dysfunction in major depressive disorder-a review of the preclinical evidence for efficacy of selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors and the multimodal-acting antidepressant vortioxetine [published online August 5, 2014]. Eur J Pharmacol. doi: 10.1016/j.ejphar.2014.07.044.
12. Baldwin DS, Hansen T, Florea I. Vortioxetine (Lu AA21004) in the long-term open-label treatment of major depressive disorder. Curr Med Res Opin. 2012;28(10):1717-1724.
13. Katona C, Hansen T, Olsen CK. A randomized, double-blind, placebo-controlled, duloxetine-referenced, fixed-dose study comparing the efficacy and safety of Lu AA21004 in elderly patients with major depressive disorder. Int Clin Psychopharmacol. 2012;27(4):215-523.
14. Raskin J, Wiltse CG, Siegal A, et al. Efficacy of duloxetine on cognition, depression, and pain in elderly patients with major depressive disorder: an 8-week, double-blind, placebo-controlled trial. Am J Psychiatry. 2007;164(6): 900-909.
15. Boulenger JP, Loft H, Olsen CK. Efficacy and safety of vortioxetine (Lu AA21004), 15 and 20 mg/day: a randomized, double-blind, placebo-controlled, duloxetine-referenced study in the acute treatment of adult patients with major depressive disorder. Int Clin Psychopharmacol. 2014;29(3):138-149.
16. Mago R, Forero G, Greenberg WM, et al. Safety and tolerability of levomilnacipran ER in major depressive disorder: results from an open-label, 48-week extension study. Clin Drug Investig. 2013;33(10):761-771.
17. Khan A, Sambunaris A, Edwards J, et al. Vilazodone in the treatment of major depressive disorder: efficacy across symptoms and severity of depression. Int Clin Psychopharmacol. 2014;29(2):86-92.
18. Boinpally R, Gad N, Gupta S, et al. Influence of CYP3A4 induction/inhibition on the pharmacokinetics of vilazodone in healthy subjects. Clin Ther. 2014; 36(11):1638-1649.
19. Chen L, Boinpally R, Greenberg WM, et al. Effect of hepatic impairment on the pharmacokinetics of levomilnacipran following a single oral dose of a levomilnacipran extended-release capsule in human participants. Clin Drug Investig. 2014;34(5):351-359.
20. Asnis GM, Bose A, Gommoll CP, et al. Efficacy and safety of levomilnacipran sustained release 40 mg, 80 mg, or 120 mg in major depressive disorder: a phase 3, randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2013;74(3):242-248.
21. Hvenegaard MG, Bang-Andersen B, Pedersen H, et al. Identification of the cytochrome P450 and other enzymes involved in the in vitro oxidative metabolism of a novel antidepressant, Lu AA21004. Drug Metab Dispos. 2012; 40(7):1357-1365.
22. Chen G, Lee R, Højer AM, et al. Pharmacokinetic drug interactions involving vortioxetine (Lu AA21004), a multimodal antidepressant. Clin Drug Investig. 2013; 33(10):727-736.
23. Areberg J, Søgaard B, Højer AM. The clinical pharmacokinetics of Lu AA21004 and its major metabolite in healthy young volunteers. Basic Clin Pharmacol Toxicol. 2012;111(3):198-205.
24. Areberg J, Petersen KB, Chen G, et al. Population pharmacokinetic meta-analysis of vortioxetine in healthy individuals. Basic Clin Pharmacol Toxicol. 2014;115(6):552-559.
1. Andrade L, Caraveo-Anduaga JJ, Berglund P, et al. The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. Int J Methods Psychiatr Res. 2003;12(1):3-21.
2. Ferrari AJ, Charlson FJ, Norman RE, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10(11):e1001547.
3. Warden D, Rush AJ, Trivedi MH, et al. The STAR*D Project results: a comprehensive review of findings. Curr Psychiatry Rep. 2007;9(6):449-459.
4. Khan A. Vilazodone, a novel dual-acting serotonergic antidepressant for managing major depression. Expert Opin Investig Drugs. 2009;18(11):1753-1764.
5. Khan A, Sambunaris A, Edwards J, et al. Vilazodone in the treatment of major depressive disorder: efficacy across symptoms and severity of depression. Int Clin Psychopharmacol. 2014;29(2):86-92.
6. Robinson DS, Kajdasz DK, Gallipoli S, et al. A 1-year, open-label study assessing the safety and tolerability of vilazodone in patients with major depressive disorder. J Clin Psychopharmacol. 2011;31(5):643-646.
7. Saraceni MM, Venci JV, Gandhi MA. Levomilnacipran (Fetzima): a new serotonin-norepinephrine reuptake inhibitor for the treatment of major depressive disorder. J Pharm Pract. 2013;27(4):389-395.
8. Deardorff WJ, Grossberg GT. A review of the clinical efficacy, safety and tolerability of the antidepressants vilazodone, levomilnacipran and vortioxetine. Expert Opin Pharmacother. 2014;15(17):2525-2542.
9. Citrome L. Levomilnacipran for major depressive disorder: a systematic review of the efficacy and safety profile for this newly approved antidepressant—what is the number needed to treat, number needed to harm and likelihood to be helped or harmed? Int J Clin Pract. 2013;67(11):1089-1104.
10. Mørk A, Pehrson A, Brennum LT, et al. Pharmacological effects of Lu AA21004: a novel multimodal compound for the treatment of major depressive disorder. J Pharmacol Exp Ther. 2012;340(3):666-675.
11. Pehrson AL, Leiser SC, Gulinello M, et al. Treatment of cognitive dysfunction in major depressive disorder-a review of the preclinical evidence for efficacy of selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors and the multimodal-acting antidepressant vortioxetine [published online August 5, 2014]. Eur J Pharmacol. doi: 10.1016/j.ejphar.2014.07.044.
12. Baldwin DS, Hansen T, Florea I. Vortioxetine (Lu AA21004) in the long-term open-label treatment of major depressive disorder. Curr Med Res Opin. 2012;28(10):1717-1724.
13. Katona C, Hansen T, Olsen CK. A randomized, double-blind, placebo-controlled, duloxetine-referenced, fixed-dose study comparing the efficacy and safety of Lu AA21004 in elderly patients with major depressive disorder. Int Clin Psychopharmacol. 2012;27(4):215-523.
14. Raskin J, Wiltse CG, Siegal A, et al. Efficacy of duloxetine on cognition, depression, and pain in elderly patients with major depressive disorder: an 8-week, double-blind, placebo-controlled trial. Am J Psychiatry. 2007;164(6): 900-909.
15. Boulenger JP, Loft H, Olsen CK. Efficacy and safety of vortioxetine (Lu AA21004), 15 and 20 mg/day: a randomized, double-blind, placebo-controlled, duloxetine-referenced study in the acute treatment of adult patients with major depressive disorder. Int Clin Psychopharmacol. 2014;29(3):138-149.
16. Mago R, Forero G, Greenberg WM, et al. Safety and tolerability of levomilnacipran ER in major depressive disorder: results from an open-label, 48-week extension study. Clin Drug Investig. 2013;33(10):761-771.
17. Khan A, Sambunaris A, Edwards J, et al. Vilazodone in the treatment of major depressive disorder: efficacy across symptoms and severity of depression. Int Clin Psychopharmacol. 2014;29(2):86-92.
18. Boinpally R, Gad N, Gupta S, et al. Influence of CYP3A4 induction/inhibition on the pharmacokinetics of vilazodone in healthy subjects. Clin Ther. 2014; 36(11):1638-1649.
19. Chen L, Boinpally R, Greenberg WM, et al. Effect of hepatic impairment on the pharmacokinetics of levomilnacipran following a single oral dose of a levomilnacipran extended-release capsule in human participants. Clin Drug Investig. 2014;34(5):351-359.
20. Asnis GM, Bose A, Gommoll CP, et al. Efficacy and safety of levomilnacipran sustained release 40 mg, 80 mg, or 120 mg in major depressive disorder: a phase 3, randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2013;74(3):242-248.
21. Hvenegaard MG, Bang-Andersen B, Pedersen H, et al. Identification of the cytochrome P450 and other enzymes involved in the in vitro oxidative metabolism of a novel antidepressant, Lu AA21004. Drug Metab Dispos. 2012; 40(7):1357-1365.
22. Chen G, Lee R, Højer AM, et al. Pharmacokinetic drug interactions involving vortioxetine (Lu AA21004), a multimodal antidepressant. Clin Drug Investig. 2013; 33(10):727-736.
23. Areberg J, Søgaard B, Højer AM. The clinical pharmacokinetics of Lu AA21004 and its major metabolite in healthy young volunteers. Basic Clin Pharmacol Toxicol. 2012;111(3):198-205.
24. Areberg J, Petersen KB, Chen G, et al. Population pharmacokinetic meta-analysis of vortioxetine in healthy individuals. Basic Clin Pharmacol Toxicol. 2014;115(6):552-559.
Delusional and aggressive, while playing the lottery
CASE Delusional and aggressive
Mr. P, age 78, of Filipino heritage, is brought to the psychiatric hospital because he has been verbally aggressive toward his wife for several weeks. He has no history of a psychiatric diagnosis or inpatient psychiatric hospitalization, and no history of taking any psychotropic medications.
According to his wife, Mr. P has been ruminating about his father, who died in World War II, saying that “the Japanese never gave his body back” to him. Also, his wife describes 3 weeks of physically aggressive behavior, such as throwing punches; the last episode was 2 days before admission.
Mr. P is not bathing, eating, taking his medications, and attending to his activities of daily living. He sleeps for only 1 to 2 hours a night; is irritable and easily distractible; and experiences flight of ideas. Mr. P has been buying lottery tickets, telling his daughter that he will become a millionaire and then buy a house in the Philippines.
Mr. P reports depressed mood, but no other depressive symptoms are present. He reports no suicidal or homicidal ideations, auditory or visual hallucinations, or anxiety symptoms. He has no history of substance abuse.
What diagnosis would you give Mr. P?
a) late-onset bipolar disorder
b) Alzheimer’s disease
c) major depressive disorder
d) frontotemporal dementia
The authors’ observations
Bipolar disorder in later life is a complex and confounding neuropsychiatric syndrome with diagnostic and therapeutic challenges. The disorder can affect people of all ages and is not uncommon among geriatric patients, with a 1-year prevalence in United States of 0.4%.1 In one study, 10% of new bipolar disorder cases were found to occur after age 50.2 As the American population grows older, the number of bipolar disorder cases among seniors is expected to increase.3
It was once thought that symptoms of bipolar disorder disappear with age; newer research has disproved this theory, and proposes that untreated bipolar disorder worsens over time.4 Persons who are given the diagnosis later in life could have had bipolar disorder for decades, but symptoms became more noticeable and problematic with age.5
Common symptoms in geriatric patients can differ from what we might expect in younger patients: agitation, hyperactivity, irritability, confusion, and psychosis.6 When the disorder presents in patients age >60, it can be severe, with significant changes in cognitive function, including difficulties with memory, perception, judgment, and problem-solving.7,8
HISTORY Medical comorbidities
Mr. P emigrated from the Philippines 20 years ago, is married, and lives with his wife. He has 3 brothers; his parents were divorced, and his mother remarried. Mr. P completed high school.
Mr. P has an extensive medical history: diabetes mellitus, hypertension, dyslipidemia, and recent double coronary artery bypass grafting. He is taking several medications: sitagliptin, 25 mg/d; pantoprazole, 5 mg/d; metformin, 1,000 mg/d; rivaroxaban, 20 mg/d; amiodarone, 200 mg/d; metoprolol, 12.5 mg/d; olmesartan medoxomil, 40 mg/d; aspirin, 81 mg/d; simvastatin, 10 mg/d; eszopiclone, 3 mg at bedtime; and amlodipine, 5 mg at bedtime.
Mr. P was following up with his primary care physician for his medical conditions and was adherent with treatment until 1 week before he was admitted to our facility.
The authors’ observations
Always rule out medical causes in a case of new-onset mania, which is particularly important in geriatric patients. Older patients with new-onset mania are more than twice as likely to have a comorbid neurologic disorder.9 Neurologic causes of late-onset mania include:
• stroke
• tumor
• epilepsy
• Huntington’s disease and other movement disorders
• multiple sclerosis and other white-matter diseases
• head trauma
• infection (such as neurosyphilis)
• Creutzfeldt-Jakob disease
• frontotemporal dementia.10
Mr. P’s presentation of psychomotor agitation, impaired functioning, decreased need for sleep, increased energy, hyperverbal speech, and complex paranoid delusions meets DSM-5 criteria for bipolar disorder, manic phase. In addition, older manic patients frequently present with confusion, disorientation, and distractibility. Younger patients with mania often present with euphoric moods and grandiosity; in contrast, geriatric patients are more likely to show a mixture of depressed affect and manic symptoms (pressured speech and a decreased need for sleep).11-15
We considered an emerging neurodegenerative process, because dementia can present early with disinhibition, lability, and other behavioral disturbances, including classic manic syndromes.16 Although we could not fully rule out a neurodegenerative process in the initial phase of treatment, Mr. P’s longitudinal course demonstrated no change in baseline cognitive function and no evidence of subsequent decline, making dementia unlikely.17
Patients with frontotemporal dementia are more likely to present initially to a psychiatrist than to a neurologist.18
Frontotemporal dementia is a progressive neurodegenerative disease that affects the frontal and temporal cortices; it is a common cause of dementia in patients age <65.19 Frontotemporal dementia is characterized by insidious behavioral and personality changes; often, the initial presentation lacks any clear neurologic signs or symptoms. Key features include apathy, disinhibition, loss of sympathy and empathy, repetitive motor behaviors, and overeating.20
Mr. P’s symptoms stabilized with divalproex sprinkles and risperidone. There was no evidence of decline in memory, social interaction, or behavior.
EVALUATION Paranoia
On mental status exam, Mr. P has an appropriate appearance; he is clean and shaven, with good eye contact. Muscular tone and gait are within normal limits. Level of activity is increased; he exhibits psychomotor agitation. Speech is rapid, over-productive, and loud; thought process shows flight of ideas, and thought associations are circumstantial.
Mr. P has paranoid delusions about the staff trying to hurt him. His judgment is poor, evidenced by an inability to take care of himself. Insight is minimal, as seen by noncompliance with treatment. Mr. P is oriented only to person and place. His mood is anxious; affect is labile.
Complete blood count, comprehensive metabolic profile, blood alcohol level, urine analysis, urine toxicology, electrocardiogram, and CT scan of the head are within normal limits.
Mr. P is given a diagnosis of mood disorder due to general medical condition, psychotic disorder due to general medical condition. The team rules out acute delirium, bipolar I disorder, and neurodegenerative disorders such as frontotemporal dementia.
Mr. P is maintained on pre-admission medications for his medical conditions. A mood stabilizer, divalproex sprinkles, 250 mg/d, is added.
Once on the unit, Mr. P is re-evaluated. Divalproex is increased to 500 mg/d; risperidone, 0.5 mg/d, is added to address paranoia. Mr. P also receives group and individual psychotherapy. He does not participate in neuropsychological testing, and no single-photon emission CT analysis is done. Mr. P remains in the hospital for 2 weeks. After a family meeting, his daughter says she feels comfortable taking Mr. P home. He follows up in the outpatient clinic and is doing well.
The authors’ observations
Treating geriatric patients with bipolar disorder requires attention to several factors (Table). Older patients might tolerate or metabolize medications differently than younger adults, and therefore may need a different dosage. Older patients are more likely to have comorbid medical conditions and to be taking medications for those ailments. Treatment is much more complicated for this age group because physicians need to account for possible drug-drug interactions.21
A number of medications can be helpful in treating older patients who have bipolar disorder.11 Ongoing research compares lithium with anticonvulsants in older bipolar disorder patients to determine which drug has the greatest benefit with the lowest risk of side effects.
Psychotherapy can be a valuable addition to pharmacotherapy in older adults. Some psychotherapy programs are specifically geared to older bipolar disorder patients.22,23
Use of divalproex sodium in older patients
First, perform baseline laboratory tests: complete blood count, liver function, and electrocardiogram. Initiate divalproex sodium, 250 mg at bedtime, increasing the dosage every 3 to 5 days by 250 mg, with a target dose of 500 to 2,000 mg/d (divided into 2 or 3 doses). Monitor serum levels; levels of 29 to 100 μg/mL are effective and well tolerated. Common side effects include excess sedation, ataxia, tremor, nausea, and, rarely, hepatotoxicity, leukopenia, and thrombocytopenia.24
Use of lithium in geriatric patients
First, perform baseline laboratory tests: electrolytes, creatinine, blood urea nitrogen, urine, thyroid stimulating hormone, and electrocardiogram. Starting dosage is 300 mg at bedtime (150 mg for frail cachectic patients). Monitor serum levels 12 hours after last dose, adjusting dosage every 5 days until a target serum level of 0.5 to 0.8 mEq/L is reached. Common dosages for geriatric patients are 300 to 600 mg/d, which often can be given as a single bedtime dose. Cautions: When using lithium with a thiazide diuretic or nonsteroidal anti-inflammatory drug, watch for dehydration, vomiting, and diarrhea, which will elevate the serum lithium level. Side effects include ataxia, tremor, urinary frequency, thirst, nausea, diarrhea, hypothyroidism, and exacerbation of psoriasis. Once stabilized, monitor the serum lithium level, thyroid-stimulating hormone, and kidney function every 3 to 6 months.24
Bottom Line
In geriatric patients, bipolar disorder can present with agitation, irritability, confusion, and psychosis, rather than euphoric mood and grandiosity. When you suspect bipolar disorder in an older patient, first rule out medical causes of symptoms. When selecting treatment, consider comorbid medical conditions and possible drug-drug interactions.
Related Resources
• Sajatovic M, Forester BP, Gildengers A, et al. Aging changes and medical complexity in late-life bipolar disorder: emerging research findings that may help advance care. Neuropsychiatry (London). 2013;3(6):621-633.
• Dols A, Rhebergen D, Beekman A, et al. Psychiatric and medical comorbidities: results from a bipolar elderly cohort study. Am J Geriatr Psychiatry. 2014;22(11):1066-1074.
Drug Brand Names
Amiodarone • Cordarone Olanzapine • Zyprexa
Amlodipine • Norvasc Olmesartan medoxomil • Benicar
Divalproex sodium • Depakote Pantoprazole • Protonix
Eszopiclone • Lunesta Risperidone • Risperdal
Lithium • Eskalith, Lithobid Rivaroxaban • Xarelto
Lorazepam • Ativan Simvastatin • Zocor
Metformin • Glucophage Sitagliptin • Januvia
Metoprolol • Lopressor
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Weissman MM, Leaf PJ, Tischler GL, et al. Affective disorders in five United States communities. Psychol Med. 1988;18(1):141-153.
2. Yassa R, Nair NP, Iskandar H. Late-onset bipolar disorder. Psychiatr Clin North Am. 1988;11(1):117-131.
3. Verdoux H, Bourgeois M. Secondary mania caused by cerebral organic pathology [in French]. Ann Med Psychol (Paris). 1995;153(3):161-168.
4. Fadden G, Bebbington P, Kuipers L. The burden of care: the impact of functional psychiatric illness in the patient’s family. Br J Psychiatry. 1987;150:285-292.
5. Yassa R, Nair V, Nastase C, et al. Prevalence of bipolar disorder in a psychogeriatric population. J Affect Disord. 1988;14(3):197-201.
6. Robinson RG, Boston JD, Starkstein SE, et al. Comparison of mania with depression following brain injury: casual factors. Am J Psychiatry. 1988;145(2):172-178.
7. Starkstein SE, Boston JD, Robinson RG. Mechanisms of mania after brain injury: 12 case reports and review of the literature. J Nerv Ment Dis. 1988;176(2):87-100.
8. Herrmann N, Bremner KE, Naranjo CA. Pharmacotherapy of late life mood disorders. Clin Neurosci. 1997;4(1):41-47.
9. Tohen M, Shulman KI, Satlin A. First-episode mania in late life. Am J Psychiatry. 1994;151(1):130-132.
10. Mendez MF. Mania in neurologic disorders. Curr Psychiatry Rep. 2000;2(5):440-445.
11. Eagles JM, Whalley LJ. Aging and affective disorders: the age at first onset of affective disorders in Scotland, 1969- 1978. Br J Psychiatry. 1985;147:180-187.
12. Snowdon J. A retrospective case-note study of bipolar disorder in old age. Br J Psychiatry. 1991;158:485-490.
13. Winokur G. The Iowa 500: heterogeneity and course in manic-depressive illness (bipolar). Compr Psychiatry. 1975;16(2):125-131.
14. Shulman K, Post F. Bipolar affective disorder in old age. Br J Psychiatry. 1980;136:26-32.
15. Young RC, Falk JR. Age, manic psychopathology, and treatment response. Int J Geriatr Psychiatry. 1989;4(2):73-78.
16. Almeida OP. Bipolar disorder with late onset: an organic variety of mood disorder [in Portuguese]? Rev Bras Psiquiatr. 2004;26(suppl 3):27-30.
17. Carlino AR, Stinnett JL, Kim DR. New onset of bipolar disorder in late life. Psychosomatics. 2013;54(1):94-97.
18. Woolley JD, Wilson MR, Hung E, et al. Frontotemporal dementia and mania. Am J Psychiatry. 2007;164(12):1811-1816.
19. Ratnavalli E, Brayne C, Dawson K, et al. The prevalence of frontotemporal dementia. Neurology. 2002;58(11):1615-1621.
20. Gregory CA, Hodges JR. Clinical features of frontal lobe dementia in comparison to Alzheimer’s disease. J Neural Transm Suppl. 1996;47:103-123.
21. Broadhead J, Jacoby R. Mania in old age: a first prospective study. Int J Geriatr Psychiatry. 1990;5(4):215-222.
22. Dhingra U, Rabins PV. Mania in the elderly: a 5-7 year follow-up. J Am Geriatr Soc. 1991;39(6):581-583.
23. Shulman KI. Neurologic comorbidity and mania in old age. Clin Neurosci. 1997;4(1):37-40.
24. Shulman KI, Herrmann N. Bipolar disorder in old age. Can Fam Physician. 1999;45:1229-1237.
CASE Delusional and aggressive
Mr. P, age 78, of Filipino heritage, is brought to the psychiatric hospital because he has been verbally aggressive toward his wife for several weeks. He has no history of a psychiatric diagnosis or inpatient psychiatric hospitalization, and no history of taking any psychotropic medications.
According to his wife, Mr. P has been ruminating about his father, who died in World War II, saying that “the Japanese never gave his body back” to him. Also, his wife describes 3 weeks of physically aggressive behavior, such as throwing punches; the last episode was 2 days before admission.
Mr. P is not bathing, eating, taking his medications, and attending to his activities of daily living. He sleeps for only 1 to 2 hours a night; is irritable and easily distractible; and experiences flight of ideas. Mr. P has been buying lottery tickets, telling his daughter that he will become a millionaire and then buy a house in the Philippines.
Mr. P reports depressed mood, but no other depressive symptoms are present. He reports no suicidal or homicidal ideations, auditory or visual hallucinations, or anxiety symptoms. He has no history of substance abuse.
What diagnosis would you give Mr. P?
a) late-onset bipolar disorder
b) Alzheimer’s disease
c) major depressive disorder
d) frontotemporal dementia
The authors’ observations
Bipolar disorder in later life is a complex and confounding neuropsychiatric syndrome with diagnostic and therapeutic challenges. The disorder can affect people of all ages and is not uncommon among geriatric patients, with a 1-year prevalence in United States of 0.4%.1 In one study, 10% of new bipolar disorder cases were found to occur after age 50.2 As the American population grows older, the number of bipolar disorder cases among seniors is expected to increase.3
It was once thought that symptoms of bipolar disorder disappear with age; newer research has disproved this theory, and proposes that untreated bipolar disorder worsens over time.4 Persons who are given the diagnosis later in life could have had bipolar disorder for decades, but symptoms became more noticeable and problematic with age.5
Common symptoms in geriatric patients can differ from what we might expect in younger patients: agitation, hyperactivity, irritability, confusion, and psychosis.6 When the disorder presents in patients age >60, it can be severe, with significant changes in cognitive function, including difficulties with memory, perception, judgment, and problem-solving.7,8
HISTORY Medical comorbidities
Mr. P emigrated from the Philippines 20 years ago, is married, and lives with his wife. He has 3 brothers; his parents were divorced, and his mother remarried. Mr. P completed high school.
Mr. P has an extensive medical history: diabetes mellitus, hypertension, dyslipidemia, and recent double coronary artery bypass grafting. He is taking several medications: sitagliptin, 25 mg/d; pantoprazole, 5 mg/d; metformin, 1,000 mg/d; rivaroxaban, 20 mg/d; amiodarone, 200 mg/d; metoprolol, 12.5 mg/d; olmesartan medoxomil, 40 mg/d; aspirin, 81 mg/d; simvastatin, 10 mg/d; eszopiclone, 3 mg at bedtime; and amlodipine, 5 mg at bedtime.
Mr. P was following up with his primary care physician for his medical conditions and was adherent with treatment until 1 week before he was admitted to our facility.
The authors’ observations
Always rule out medical causes in a case of new-onset mania, which is particularly important in geriatric patients. Older patients with new-onset mania are more than twice as likely to have a comorbid neurologic disorder.9 Neurologic causes of late-onset mania include:
• stroke
• tumor
• epilepsy
• Huntington’s disease and other movement disorders
• multiple sclerosis and other white-matter diseases
• head trauma
• infection (such as neurosyphilis)
• Creutzfeldt-Jakob disease
• frontotemporal dementia.10
Mr. P’s presentation of psychomotor agitation, impaired functioning, decreased need for sleep, increased energy, hyperverbal speech, and complex paranoid delusions meets DSM-5 criteria for bipolar disorder, manic phase. In addition, older manic patients frequently present with confusion, disorientation, and distractibility. Younger patients with mania often present with euphoric moods and grandiosity; in contrast, geriatric patients are more likely to show a mixture of depressed affect and manic symptoms (pressured speech and a decreased need for sleep).11-15
We considered an emerging neurodegenerative process, because dementia can present early with disinhibition, lability, and other behavioral disturbances, including classic manic syndromes.16 Although we could not fully rule out a neurodegenerative process in the initial phase of treatment, Mr. P’s longitudinal course demonstrated no change in baseline cognitive function and no evidence of subsequent decline, making dementia unlikely.17
Patients with frontotemporal dementia are more likely to present initially to a psychiatrist than to a neurologist.18
Frontotemporal dementia is a progressive neurodegenerative disease that affects the frontal and temporal cortices; it is a common cause of dementia in patients age <65.19 Frontotemporal dementia is characterized by insidious behavioral and personality changes; often, the initial presentation lacks any clear neurologic signs or symptoms. Key features include apathy, disinhibition, loss of sympathy and empathy, repetitive motor behaviors, and overeating.20
Mr. P’s symptoms stabilized with divalproex sprinkles and risperidone. There was no evidence of decline in memory, social interaction, or behavior.
EVALUATION Paranoia
On mental status exam, Mr. P has an appropriate appearance; he is clean and shaven, with good eye contact. Muscular tone and gait are within normal limits. Level of activity is increased; he exhibits psychomotor agitation. Speech is rapid, over-productive, and loud; thought process shows flight of ideas, and thought associations are circumstantial.
Mr. P has paranoid delusions about the staff trying to hurt him. His judgment is poor, evidenced by an inability to take care of himself. Insight is minimal, as seen by noncompliance with treatment. Mr. P is oriented only to person and place. His mood is anxious; affect is labile.
Complete blood count, comprehensive metabolic profile, blood alcohol level, urine analysis, urine toxicology, electrocardiogram, and CT scan of the head are within normal limits.
Mr. P is given a diagnosis of mood disorder due to general medical condition, psychotic disorder due to general medical condition. The team rules out acute delirium, bipolar I disorder, and neurodegenerative disorders such as frontotemporal dementia.
Mr. P is maintained on pre-admission medications for his medical conditions. A mood stabilizer, divalproex sprinkles, 250 mg/d, is added.
Once on the unit, Mr. P is re-evaluated. Divalproex is increased to 500 mg/d; risperidone, 0.5 mg/d, is added to address paranoia. Mr. P also receives group and individual psychotherapy. He does not participate in neuropsychological testing, and no single-photon emission CT analysis is done. Mr. P remains in the hospital for 2 weeks. After a family meeting, his daughter says she feels comfortable taking Mr. P home. He follows up in the outpatient clinic and is doing well.
The authors’ observations
Treating geriatric patients with bipolar disorder requires attention to several factors (Table). Older patients might tolerate or metabolize medications differently than younger adults, and therefore may need a different dosage. Older patients are more likely to have comorbid medical conditions and to be taking medications for those ailments. Treatment is much more complicated for this age group because physicians need to account for possible drug-drug interactions.21
A number of medications can be helpful in treating older patients who have bipolar disorder.11 Ongoing research compares lithium with anticonvulsants in older bipolar disorder patients to determine which drug has the greatest benefit with the lowest risk of side effects.
Psychotherapy can be a valuable addition to pharmacotherapy in older adults. Some psychotherapy programs are specifically geared to older bipolar disorder patients.22,23
Use of divalproex sodium in older patients
First, perform baseline laboratory tests: complete blood count, liver function, and electrocardiogram. Initiate divalproex sodium, 250 mg at bedtime, increasing the dosage every 3 to 5 days by 250 mg, with a target dose of 500 to 2,000 mg/d (divided into 2 or 3 doses). Monitor serum levels; levels of 29 to 100 μg/mL are effective and well tolerated. Common side effects include excess sedation, ataxia, tremor, nausea, and, rarely, hepatotoxicity, leukopenia, and thrombocytopenia.24
Use of lithium in geriatric patients
First, perform baseline laboratory tests: electrolytes, creatinine, blood urea nitrogen, urine, thyroid stimulating hormone, and electrocardiogram. Starting dosage is 300 mg at bedtime (150 mg for frail cachectic patients). Monitor serum levels 12 hours after last dose, adjusting dosage every 5 days until a target serum level of 0.5 to 0.8 mEq/L is reached. Common dosages for geriatric patients are 300 to 600 mg/d, which often can be given as a single bedtime dose. Cautions: When using lithium with a thiazide diuretic or nonsteroidal anti-inflammatory drug, watch for dehydration, vomiting, and diarrhea, which will elevate the serum lithium level. Side effects include ataxia, tremor, urinary frequency, thirst, nausea, diarrhea, hypothyroidism, and exacerbation of psoriasis. Once stabilized, monitor the serum lithium level, thyroid-stimulating hormone, and kidney function every 3 to 6 months.24
Bottom Line
In geriatric patients, bipolar disorder can present with agitation, irritability, confusion, and psychosis, rather than euphoric mood and grandiosity. When you suspect bipolar disorder in an older patient, first rule out medical causes of symptoms. When selecting treatment, consider comorbid medical conditions and possible drug-drug interactions.
Related Resources
• Sajatovic M, Forester BP, Gildengers A, et al. Aging changes and medical complexity in late-life bipolar disorder: emerging research findings that may help advance care. Neuropsychiatry (London). 2013;3(6):621-633.
• Dols A, Rhebergen D, Beekman A, et al. Psychiatric and medical comorbidities: results from a bipolar elderly cohort study. Am J Geriatr Psychiatry. 2014;22(11):1066-1074.
Drug Brand Names
Amiodarone • Cordarone Olanzapine • Zyprexa
Amlodipine • Norvasc Olmesartan medoxomil • Benicar
Divalproex sodium • Depakote Pantoprazole • Protonix
Eszopiclone • Lunesta Risperidone • Risperdal
Lithium • Eskalith, Lithobid Rivaroxaban • Xarelto
Lorazepam • Ativan Simvastatin • Zocor
Metformin • Glucophage Sitagliptin • Januvia
Metoprolol • Lopressor
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE Delusional and aggressive
Mr. P, age 78, of Filipino heritage, is brought to the psychiatric hospital because he has been verbally aggressive toward his wife for several weeks. He has no history of a psychiatric diagnosis or inpatient psychiatric hospitalization, and no history of taking any psychotropic medications.
According to his wife, Mr. P has been ruminating about his father, who died in World War II, saying that “the Japanese never gave his body back” to him. Also, his wife describes 3 weeks of physically aggressive behavior, such as throwing punches; the last episode was 2 days before admission.
Mr. P is not bathing, eating, taking his medications, and attending to his activities of daily living. He sleeps for only 1 to 2 hours a night; is irritable and easily distractible; and experiences flight of ideas. Mr. P has been buying lottery tickets, telling his daughter that he will become a millionaire and then buy a house in the Philippines.
Mr. P reports depressed mood, but no other depressive symptoms are present. He reports no suicidal or homicidal ideations, auditory or visual hallucinations, or anxiety symptoms. He has no history of substance abuse.
What diagnosis would you give Mr. P?
a) late-onset bipolar disorder
b) Alzheimer’s disease
c) major depressive disorder
d) frontotemporal dementia
The authors’ observations
Bipolar disorder in later life is a complex and confounding neuropsychiatric syndrome with diagnostic and therapeutic challenges. The disorder can affect people of all ages and is not uncommon among geriatric patients, with a 1-year prevalence in United States of 0.4%.1 In one study, 10% of new bipolar disorder cases were found to occur after age 50.2 As the American population grows older, the number of bipolar disorder cases among seniors is expected to increase.3
It was once thought that symptoms of bipolar disorder disappear with age; newer research has disproved this theory, and proposes that untreated bipolar disorder worsens over time.4 Persons who are given the diagnosis later in life could have had bipolar disorder for decades, but symptoms became more noticeable and problematic with age.5
Common symptoms in geriatric patients can differ from what we might expect in younger patients: agitation, hyperactivity, irritability, confusion, and psychosis.6 When the disorder presents in patients age >60, it can be severe, with significant changes in cognitive function, including difficulties with memory, perception, judgment, and problem-solving.7,8
HISTORY Medical comorbidities
Mr. P emigrated from the Philippines 20 years ago, is married, and lives with his wife. He has 3 brothers; his parents were divorced, and his mother remarried. Mr. P completed high school.
Mr. P has an extensive medical history: diabetes mellitus, hypertension, dyslipidemia, and recent double coronary artery bypass grafting. He is taking several medications: sitagliptin, 25 mg/d; pantoprazole, 5 mg/d; metformin, 1,000 mg/d; rivaroxaban, 20 mg/d; amiodarone, 200 mg/d; metoprolol, 12.5 mg/d; olmesartan medoxomil, 40 mg/d; aspirin, 81 mg/d; simvastatin, 10 mg/d; eszopiclone, 3 mg at bedtime; and amlodipine, 5 mg at bedtime.
Mr. P was following up with his primary care physician for his medical conditions and was adherent with treatment until 1 week before he was admitted to our facility.
The authors’ observations
Always rule out medical causes in a case of new-onset mania, which is particularly important in geriatric patients. Older patients with new-onset mania are more than twice as likely to have a comorbid neurologic disorder.9 Neurologic causes of late-onset mania include:
• stroke
• tumor
• epilepsy
• Huntington’s disease and other movement disorders
• multiple sclerosis and other white-matter diseases
• head trauma
• infection (such as neurosyphilis)
• Creutzfeldt-Jakob disease
• frontotemporal dementia.10
Mr. P’s presentation of psychomotor agitation, impaired functioning, decreased need for sleep, increased energy, hyperverbal speech, and complex paranoid delusions meets DSM-5 criteria for bipolar disorder, manic phase. In addition, older manic patients frequently present with confusion, disorientation, and distractibility. Younger patients with mania often present with euphoric moods and grandiosity; in contrast, geriatric patients are more likely to show a mixture of depressed affect and manic symptoms (pressured speech and a decreased need for sleep).11-15
We considered an emerging neurodegenerative process, because dementia can present early with disinhibition, lability, and other behavioral disturbances, including classic manic syndromes.16 Although we could not fully rule out a neurodegenerative process in the initial phase of treatment, Mr. P’s longitudinal course demonstrated no change in baseline cognitive function and no evidence of subsequent decline, making dementia unlikely.17
Patients with frontotemporal dementia are more likely to present initially to a psychiatrist than to a neurologist.18
Frontotemporal dementia is a progressive neurodegenerative disease that affects the frontal and temporal cortices; it is a common cause of dementia in patients age <65.19 Frontotemporal dementia is characterized by insidious behavioral and personality changes; often, the initial presentation lacks any clear neurologic signs or symptoms. Key features include apathy, disinhibition, loss of sympathy and empathy, repetitive motor behaviors, and overeating.20
Mr. P’s symptoms stabilized with divalproex sprinkles and risperidone. There was no evidence of decline in memory, social interaction, or behavior.
EVALUATION Paranoia
On mental status exam, Mr. P has an appropriate appearance; he is clean and shaven, with good eye contact. Muscular tone and gait are within normal limits. Level of activity is increased; he exhibits psychomotor agitation. Speech is rapid, over-productive, and loud; thought process shows flight of ideas, and thought associations are circumstantial.
Mr. P has paranoid delusions about the staff trying to hurt him. His judgment is poor, evidenced by an inability to take care of himself. Insight is minimal, as seen by noncompliance with treatment. Mr. P is oriented only to person and place. His mood is anxious; affect is labile.
Complete blood count, comprehensive metabolic profile, blood alcohol level, urine analysis, urine toxicology, electrocardiogram, and CT scan of the head are within normal limits.
Mr. P is given a diagnosis of mood disorder due to general medical condition, psychotic disorder due to general medical condition. The team rules out acute delirium, bipolar I disorder, and neurodegenerative disorders such as frontotemporal dementia.
Mr. P is maintained on pre-admission medications for his medical conditions. A mood stabilizer, divalproex sprinkles, 250 mg/d, is added.
Once on the unit, Mr. P is re-evaluated. Divalproex is increased to 500 mg/d; risperidone, 0.5 mg/d, is added to address paranoia. Mr. P also receives group and individual psychotherapy. He does not participate in neuropsychological testing, and no single-photon emission CT analysis is done. Mr. P remains in the hospital for 2 weeks. After a family meeting, his daughter says she feels comfortable taking Mr. P home. He follows up in the outpatient clinic and is doing well.
The authors’ observations
Treating geriatric patients with bipolar disorder requires attention to several factors (Table). Older patients might tolerate or metabolize medications differently than younger adults, and therefore may need a different dosage. Older patients are more likely to have comorbid medical conditions and to be taking medications for those ailments. Treatment is much more complicated for this age group because physicians need to account for possible drug-drug interactions.21
A number of medications can be helpful in treating older patients who have bipolar disorder.11 Ongoing research compares lithium with anticonvulsants in older bipolar disorder patients to determine which drug has the greatest benefit with the lowest risk of side effects.
Psychotherapy can be a valuable addition to pharmacotherapy in older adults. Some psychotherapy programs are specifically geared to older bipolar disorder patients.22,23
Use of divalproex sodium in older patients
First, perform baseline laboratory tests: complete blood count, liver function, and electrocardiogram. Initiate divalproex sodium, 250 mg at bedtime, increasing the dosage every 3 to 5 days by 250 mg, with a target dose of 500 to 2,000 mg/d (divided into 2 or 3 doses). Monitor serum levels; levels of 29 to 100 μg/mL are effective and well tolerated. Common side effects include excess sedation, ataxia, tremor, nausea, and, rarely, hepatotoxicity, leukopenia, and thrombocytopenia.24
Use of lithium in geriatric patients
First, perform baseline laboratory tests: electrolytes, creatinine, blood urea nitrogen, urine, thyroid stimulating hormone, and electrocardiogram. Starting dosage is 300 mg at bedtime (150 mg for frail cachectic patients). Monitor serum levels 12 hours after last dose, adjusting dosage every 5 days until a target serum level of 0.5 to 0.8 mEq/L is reached. Common dosages for geriatric patients are 300 to 600 mg/d, which often can be given as a single bedtime dose. Cautions: When using lithium with a thiazide diuretic or nonsteroidal anti-inflammatory drug, watch for dehydration, vomiting, and diarrhea, which will elevate the serum lithium level. Side effects include ataxia, tremor, urinary frequency, thirst, nausea, diarrhea, hypothyroidism, and exacerbation of psoriasis. Once stabilized, monitor the serum lithium level, thyroid-stimulating hormone, and kidney function every 3 to 6 months.24
Bottom Line
In geriatric patients, bipolar disorder can present with agitation, irritability, confusion, and psychosis, rather than euphoric mood and grandiosity. When you suspect bipolar disorder in an older patient, first rule out medical causes of symptoms. When selecting treatment, consider comorbid medical conditions and possible drug-drug interactions.
Related Resources
• Sajatovic M, Forester BP, Gildengers A, et al. Aging changes and medical complexity in late-life bipolar disorder: emerging research findings that may help advance care. Neuropsychiatry (London). 2013;3(6):621-633.
• Dols A, Rhebergen D, Beekman A, et al. Psychiatric and medical comorbidities: results from a bipolar elderly cohort study. Am J Geriatr Psychiatry. 2014;22(11):1066-1074.
Drug Brand Names
Amiodarone • Cordarone Olanzapine • Zyprexa
Amlodipine • Norvasc Olmesartan medoxomil • Benicar
Divalproex sodium • Depakote Pantoprazole • Protonix
Eszopiclone • Lunesta Risperidone • Risperdal
Lithium • Eskalith, Lithobid Rivaroxaban • Xarelto
Lorazepam • Ativan Simvastatin • Zocor
Metformin • Glucophage Sitagliptin • Januvia
Metoprolol • Lopressor
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Weissman MM, Leaf PJ, Tischler GL, et al. Affective disorders in five United States communities. Psychol Med. 1988;18(1):141-153.
2. Yassa R, Nair NP, Iskandar H. Late-onset bipolar disorder. Psychiatr Clin North Am. 1988;11(1):117-131.
3. Verdoux H, Bourgeois M. Secondary mania caused by cerebral organic pathology [in French]. Ann Med Psychol (Paris). 1995;153(3):161-168.
4. Fadden G, Bebbington P, Kuipers L. The burden of care: the impact of functional psychiatric illness in the patient’s family. Br J Psychiatry. 1987;150:285-292.
5. Yassa R, Nair V, Nastase C, et al. Prevalence of bipolar disorder in a psychogeriatric population. J Affect Disord. 1988;14(3):197-201.
6. Robinson RG, Boston JD, Starkstein SE, et al. Comparison of mania with depression following brain injury: casual factors. Am J Psychiatry. 1988;145(2):172-178.
7. Starkstein SE, Boston JD, Robinson RG. Mechanisms of mania after brain injury: 12 case reports and review of the literature. J Nerv Ment Dis. 1988;176(2):87-100.
8. Herrmann N, Bremner KE, Naranjo CA. Pharmacotherapy of late life mood disorders. Clin Neurosci. 1997;4(1):41-47.
9. Tohen M, Shulman KI, Satlin A. First-episode mania in late life. Am J Psychiatry. 1994;151(1):130-132.
10. Mendez MF. Mania in neurologic disorders. Curr Psychiatry Rep. 2000;2(5):440-445.
11. Eagles JM, Whalley LJ. Aging and affective disorders: the age at first onset of affective disorders in Scotland, 1969- 1978. Br J Psychiatry. 1985;147:180-187.
12. Snowdon J. A retrospective case-note study of bipolar disorder in old age. Br J Psychiatry. 1991;158:485-490.
13. Winokur G. The Iowa 500: heterogeneity and course in manic-depressive illness (bipolar). Compr Psychiatry. 1975;16(2):125-131.
14. Shulman K, Post F. Bipolar affective disorder in old age. Br J Psychiatry. 1980;136:26-32.
15. Young RC, Falk JR. Age, manic psychopathology, and treatment response. Int J Geriatr Psychiatry. 1989;4(2):73-78.
16. Almeida OP. Bipolar disorder with late onset: an organic variety of mood disorder [in Portuguese]? Rev Bras Psiquiatr. 2004;26(suppl 3):27-30.
17. Carlino AR, Stinnett JL, Kim DR. New onset of bipolar disorder in late life. Psychosomatics. 2013;54(1):94-97.
18. Woolley JD, Wilson MR, Hung E, et al. Frontotemporal dementia and mania. Am J Psychiatry. 2007;164(12):1811-1816.
19. Ratnavalli E, Brayne C, Dawson K, et al. The prevalence of frontotemporal dementia. Neurology. 2002;58(11):1615-1621.
20. Gregory CA, Hodges JR. Clinical features of frontal lobe dementia in comparison to Alzheimer’s disease. J Neural Transm Suppl. 1996;47:103-123.
21. Broadhead J, Jacoby R. Mania in old age: a first prospective study. Int J Geriatr Psychiatry. 1990;5(4):215-222.
22. Dhingra U, Rabins PV. Mania in the elderly: a 5-7 year follow-up. J Am Geriatr Soc. 1991;39(6):581-583.
23. Shulman KI. Neurologic comorbidity and mania in old age. Clin Neurosci. 1997;4(1):37-40.
24. Shulman KI, Herrmann N. Bipolar disorder in old age. Can Fam Physician. 1999;45:1229-1237.
1. Weissman MM, Leaf PJ, Tischler GL, et al. Affective disorders in five United States communities. Psychol Med. 1988;18(1):141-153.
2. Yassa R, Nair NP, Iskandar H. Late-onset bipolar disorder. Psychiatr Clin North Am. 1988;11(1):117-131.
3. Verdoux H, Bourgeois M. Secondary mania caused by cerebral organic pathology [in French]. Ann Med Psychol (Paris). 1995;153(3):161-168.
4. Fadden G, Bebbington P, Kuipers L. The burden of care: the impact of functional psychiatric illness in the patient’s family. Br J Psychiatry. 1987;150:285-292.
5. Yassa R, Nair V, Nastase C, et al. Prevalence of bipolar disorder in a psychogeriatric population. J Affect Disord. 1988;14(3):197-201.
6. Robinson RG, Boston JD, Starkstein SE, et al. Comparison of mania with depression following brain injury: casual factors. Am J Psychiatry. 1988;145(2):172-178.
7. Starkstein SE, Boston JD, Robinson RG. Mechanisms of mania after brain injury: 12 case reports and review of the literature. J Nerv Ment Dis. 1988;176(2):87-100.
8. Herrmann N, Bremner KE, Naranjo CA. Pharmacotherapy of late life mood disorders. Clin Neurosci. 1997;4(1):41-47.
9. Tohen M, Shulman KI, Satlin A. First-episode mania in late life. Am J Psychiatry. 1994;151(1):130-132.
10. Mendez MF. Mania in neurologic disorders. Curr Psychiatry Rep. 2000;2(5):440-445.
11. Eagles JM, Whalley LJ. Aging and affective disorders: the age at first onset of affective disorders in Scotland, 1969- 1978. Br J Psychiatry. 1985;147:180-187.
12. Snowdon J. A retrospective case-note study of bipolar disorder in old age. Br J Psychiatry. 1991;158:485-490.
13. Winokur G. The Iowa 500: heterogeneity and course in manic-depressive illness (bipolar). Compr Psychiatry. 1975;16(2):125-131.
14. Shulman K, Post F. Bipolar affective disorder in old age. Br J Psychiatry. 1980;136:26-32.
15. Young RC, Falk JR. Age, manic psychopathology, and treatment response. Int J Geriatr Psychiatry. 1989;4(2):73-78.
16. Almeida OP. Bipolar disorder with late onset: an organic variety of mood disorder [in Portuguese]? Rev Bras Psiquiatr. 2004;26(suppl 3):27-30.
17. Carlino AR, Stinnett JL, Kim DR. New onset of bipolar disorder in late life. Psychosomatics. 2013;54(1):94-97.
18. Woolley JD, Wilson MR, Hung E, et al. Frontotemporal dementia and mania. Am J Psychiatry. 2007;164(12):1811-1816.
19. Ratnavalli E, Brayne C, Dawson K, et al. The prevalence of frontotemporal dementia. Neurology. 2002;58(11):1615-1621.
20. Gregory CA, Hodges JR. Clinical features of frontal lobe dementia in comparison to Alzheimer’s disease. J Neural Transm Suppl. 1996;47:103-123.
21. Broadhead J, Jacoby R. Mania in old age: a first prospective study. Int J Geriatr Psychiatry. 1990;5(4):215-222.
22. Dhingra U, Rabins PV. Mania in the elderly: a 5-7 year follow-up. J Am Geriatr Soc. 1991;39(6):581-583.
23. Shulman KI. Neurologic comorbidity and mania in old age. Clin Neurosci. 1997;4(1):37-40.
24. Shulman KI, Herrmann N. Bipolar disorder in old age. Can Fam Physician. 1999;45:1229-1237.
Do glutamatergic drugs have a role in treating depression?
Mrs. S, age 46, has been struggling to manage depression for 7 years. She completed adequate trials of several selective serotonin reuptake inhibitors and bupropion. Currently, she is taking duloxetine, 60 mg/d, and aripiprazole, 5 mg/d.
At her most recent clinic visit, Mrs. S reports that she is doing “OK,” but that she still feels sad and disengaged most days of the week. She wants to know more about ketamine for treating depression after reading about it on the Internet and hearing it mentioned in a support group she attends. She asks if you think it would work for her, and gives you with a copy of an article about its use in patients with treatment-resistant depression. Mrs. S has no other health conditions and takes a daily vitamin D and calcium supplement.
The monoamine hypothesis of depression postulates that symptoms originate from underactivity of monoamines, such as serotonin, norepinephrine, and dopamine, in the brain. This hypothesis was formulated in the 1960s after researchers observed that monoamine oxidase inhibitors and tricyclic antidepressants relieved depressive symptoms; both were known to increase monoamine concentrations in the synaptic cleft.1
Regrettably, these medications do not adequately relieve depressive symptoms for many people. In fact, symptom remission occurs in only one-third of treated patients.2 This low remission rate reflects a lack of understanding of the pathophysiology of depression, and the need for drugs with unique mechanisms of action.
One of the newest drug targets shown to be relevant in psychiatric illness is the
glutamatergic system. Glutamate is the predominant excitatory neurotransmitter in the CNS, and it is responsible for many key functions, including synaptic plasticity, learning, memory, and locomotion.3 Normally, the glutamatergic system tightly regulates the amount of glutamate in the neuronal synapse via receptors on presynaptic and postsynaptic neurons, as well as on glial cells (Figure). When this equilibrium is disrupted in stressful situations, such as ischemia, trauma, or seizures, excess glutamate is released into the synapse. The resulting glutamatergic hyperactivity can lead to neurotoxicity and cell death when neuronal receptors are activated for an extended period.
A key component of the glutamatergic system that is responsible for removing excess glutamate from the synapse is membrane-bound transporters, which are similar to serotonin and norepinephrine transporters. These excitatory amino acid transporters (EAATs) are important because glutamate metabolism does not occur within the synapse and EAATS are responsible for removing most of the glutamate from the synapse into glial cells.3
The network of receptors within the synapse that are activated by glutamate is extensive and complex. There are at least 11 glutamate-responsive receptors: 3 are ionotropic action channels, and the remaining 8 are metabotropic G protein-coupled receptors. Previous studies have shown regional changes in glutamate receptors, as well as elevated levels of glutamate, in the brains of patients with major depressive disorder (MDD).4
Ketamine. The ionotropic receptor N-methyl-d-aspartate (NMDA) is one of the most studied glutamate receptors. Pharmacologically, ketamine is a noncompetitive NMDA receptor antagonist that also activates the amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor, which is another subtype of ionotropic glutamate receptors. In open-label clinical trials, ketamine has demonstrated rapid antidepressant action in patients with treatment-resistant MDD.4,5
Recently, Murrough et al6 performed the first randomized, psychoactive controlled trial using a single IV infusion of ketamine dosed below anesthesia ranges (0.5 mg/kg), or midazolam (0.045 mg/kg), in patients with treatment-resistant depression who had been antidepressant-free for at least 4 weeks. They found that 24 hours after medication administration, the likelihood of response to ketamine was significantly higher than the response to midazolam (OR: 2.18; 95% CI: 1.21 to 4.14), with a response rate of 64% in the ketamine group and 28% in the midazolam group.6
Psychotropic side effects, such as hallucinations, are a major concern with ketamine tolerability and abuse potential. This is largely because of ketamine’s antagonism of the NMDA receptor, which is a property shared with other abused drugs such as phencyclidine (PCP) and dextromethorphan. In the Murrough et al6 study, there were no reported cases of paranoia or hallucinations, but dissociative symptoms were relatively common (17%).
Although the results in this trial appear encouraging, there are several limitations to using ketamine to treat MDD, especially in an ambulatory setting. Concerns include ketamine’s IV administration, potential for abuse, long-term efficacy, and side-effect profile—particularly psychotic symptoms and hemodynamic changes. An ideal compound would have the rapid efficacy of ketamine, but with a safer side-effect profile, easier administration, and less potential for abuse.
Riluzole also acts on the glutamatergic system, but has not shown antidepressant efficacy as consistently as ketamine. Riluzole is FDA-approved for treating amyotrophic lateral sclerosis.5 Pharmacologically, riluzole is a glutamatergic modulator that increases glutamate reuptake into glial cells, decreases glutamate release, and increases AMPA trafficking. In open-label studies riluzole has shown efficacy in reducing depressive symptoms.4,5 However, when compared with placebo as a means of sustaining treatment response after a 1-time dose of ketamine, riluzole showed was no significant improvement in time to depressive relapse.7
Acamprosate, often used for treating alcohol abuse, is another a drug with glutamatergic activity that has been studied for possible use as an antidepressant.5
A review by Lapidus et al5 has a more extensive listing of current medications and investigational compounds that modulate glutamate transmission, and are of interest for their possible antidepressant activity. Given the relatively new “glutamatergic hypothesis” of depression, it is exciting that so many current and novel glutamatergic drug therapies are being evaluated.
Future of ketamine treatment
Glutamate has been shown to play an important part in the pathophysiology of depression. The rapid antidepressant efficacy of ketamine provides evidence that future medications with glutamate-modulating activity could be useful for patients who struggle to achieve symptom relief using available antidepressants. Several limitations exist regarding ketamine use, and more work in this important therapeutic area needs to be done. This last point is important to remember when speaking with patients such as Mrs. S. Although it is understandable for her to be excited about novel treatment options such as ketamine, stress to her that treating depression with ketamine at this time is strictly investigational, and that the drug needs to be thoroughly evaluated for safety and efficacy before it can be prescribed for this indication.
CASE CONTINUED
Mrs. S realizes that ketamine may not be the best next step for her, and she agrees to explore other approaches to treat her residual depressive symptoms.
Related Resources
• Machado-Vieira R, Ibrahim L, Henter ID, et al. Novel glutamatergic agents for major depressive disorder and bipolar disorder. Pharmacol Biochem Behav. 2012;100(4):678-687.
• Mathews DC, Henter ID, Zarate CA. Targeting the glutamatergic system to treat major depressive disorder: rationale and progress to date. Drugs. 2012;72(10):1313-1333.
Drug Brand Names
Acamprosate • Campral Duloxetine • Cymbalta
Aripiprazole • Abilify Ketamine • Ketalar
Bupropion • Wellbutrin, Zyban Riluzole • Rilutek
Disclosures
The authors report no financial relationships with any companies whose products are mentioned in this article or with manufacturers of competing products.
1. Niciu MJ, Ionescu DF, Richards EM, et al. Glutamate and its receptors in the pathophysiology and treatment of major depressive disorder. J Neural Transm. 2014;121(8):907-924.
2. Gaynes BN, Dusetzina SB, Ellis AR, et al. Treating depression after initial treatment failure: directly comparing switch and augmenting strategies in STAR*D. J Clin Psychopharmacol. 2012;32(1):114-119.
3. Curry SC, Mills KC, Ruha A, et al. Neurotransmitters and neuromodulators. In: Nelson LS, Lewin NA, Howland MA, et al, eds. Goldfrank’s toxicologic emergencies. 9th ed. New York, NY: McGraw-Hill; 2011:189-220.
4. Zarate C Jr, Machado-Vieira R, Henter I, et al. Glutamatergic modulators: the future of treating mood disorders? Harv Rev Psychiatry. 2010;18(5):293-303.
5. Lapidus KA, Soleimani L, Murrough JW. Novel glutamatergic drugs for the treatment of mood disorders. Neuropsychiatr Dis Treat. 2013;9:1101-1112.
6. Murrough JW, Iosifescu DV, Chang LC, et al. Antidepressant efficacy of ketamine in treatment-resistant major depression: a two-site randomized controlled trial. Am J Psychiatry. 2013;170(10):1134-1142.
7. Ibrahim L, Diazgranados N, Franco-Chaves J, et al. Course of improvement in depressive symptoms to a single intravenous infusion of ketamine vs add-on riluzole: results from a 4-week, double-blind, placebo-controlled study. Neuropsychopharmacology. 2012;37(6):1526-1533.
Mrs. S, age 46, has been struggling to manage depression for 7 years. She completed adequate trials of several selective serotonin reuptake inhibitors and bupropion. Currently, she is taking duloxetine, 60 mg/d, and aripiprazole, 5 mg/d.
At her most recent clinic visit, Mrs. S reports that she is doing “OK,” but that she still feels sad and disengaged most days of the week. She wants to know more about ketamine for treating depression after reading about it on the Internet and hearing it mentioned in a support group she attends. She asks if you think it would work for her, and gives you with a copy of an article about its use in patients with treatment-resistant depression. Mrs. S has no other health conditions and takes a daily vitamin D and calcium supplement.
The monoamine hypothesis of depression postulates that symptoms originate from underactivity of monoamines, such as serotonin, norepinephrine, and dopamine, in the brain. This hypothesis was formulated in the 1960s after researchers observed that monoamine oxidase inhibitors and tricyclic antidepressants relieved depressive symptoms; both were known to increase monoamine concentrations in the synaptic cleft.1
Regrettably, these medications do not adequately relieve depressive symptoms for many people. In fact, symptom remission occurs in only one-third of treated patients.2 This low remission rate reflects a lack of understanding of the pathophysiology of depression, and the need for drugs with unique mechanisms of action.
One of the newest drug targets shown to be relevant in psychiatric illness is the
glutamatergic system. Glutamate is the predominant excitatory neurotransmitter in the CNS, and it is responsible for many key functions, including synaptic plasticity, learning, memory, and locomotion.3 Normally, the glutamatergic system tightly regulates the amount of glutamate in the neuronal synapse via receptors on presynaptic and postsynaptic neurons, as well as on glial cells (Figure). When this equilibrium is disrupted in stressful situations, such as ischemia, trauma, or seizures, excess glutamate is released into the synapse. The resulting glutamatergic hyperactivity can lead to neurotoxicity and cell death when neuronal receptors are activated for an extended period.
A key component of the glutamatergic system that is responsible for removing excess glutamate from the synapse is membrane-bound transporters, which are similar to serotonin and norepinephrine transporters. These excitatory amino acid transporters (EAATs) are important because glutamate metabolism does not occur within the synapse and EAATS are responsible for removing most of the glutamate from the synapse into glial cells.3
The network of receptors within the synapse that are activated by glutamate is extensive and complex. There are at least 11 glutamate-responsive receptors: 3 are ionotropic action channels, and the remaining 8 are metabotropic G protein-coupled receptors. Previous studies have shown regional changes in glutamate receptors, as well as elevated levels of glutamate, in the brains of patients with major depressive disorder (MDD).4
Ketamine. The ionotropic receptor N-methyl-d-aspartate (NMDA) is one of the most studied glutamate receptors. Pharmacologically, ketamine is a noncompetitive NMDA receptor antagonist that also activates the amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor, which is another subtype of ionotropic glutamate receptors. In open-label clinical trials, ketamine has demonstrated rapid antidepressant action in patients with treatment-resistant MDD.4,5
Recently, Murrough et al6 performed the first randomized, psychoactive controlled trial using a single IV infusion of ketamine dosed below anesthesia ranges (0.5 mg/kg), or midazolam (0.045 mg/kg), in patients with treatment-resistant depression who had been antidepressant-free for at least 4 weeks. They found that 24 hours after medication administration, the likelihood of response to ketamine was significantly higher than the response to midazolam (OR: 2.18; 95% CI: 1.21 to 4.14), with a response rate of 64% in the ketamine group and 28% in the midazolam group.6
Psychotropic side effects, such as hallucinations, are a major concern with ketamine tolerability and abuse potential. This is largely because of ketamine’s antagonism of the NMDA receptor, which is a property shared with other abused drugs such as phencyclidine (PCP) and dextromethorphan. In the Murrough et al6 study, there were no reported cases of paranoia or hallucinations, but dissociative symptoms were relatively common (17%).
Although the results in this trial appear encouraging, there are several limitations to using ketamine to treat MDD, especially in an ambulatory setting. Concerns include ketamine’s IV administration, potential for abuse, long-term efficacy, and side-effect profile—particularly psychotic symptoms and hemodynamic changes. An ideal compound would have the rapid efficacy of ketamine, but with a safer side-effect profile, easier administration, and less potential for abuse.
Riluzole also acts on the glutamatergic system, but has not shown antidepressant efficacy as consistently as ketamine. Riluzole is FDA-approved for treating amyotrophic lateral sclerosis.5 Pharmacologically, riluzole is a glutamatergic modulator that increases glutamate reuptake into glial cells, decreases glutamate release, and increases AMPA trafficking. In open-label studies riluzole has shown efficacy in reducing depressive symptoms.4,5 However, when compared with placebo as a means of sustaining treatment response after a 1-time dose of ketamine, riluzole showed was no significant improvement in time to depressive relapse.7
Acamprosate, often used for treating alcohol abuse, is another a drug with glutamatergic activity that has been studied for possible use as an antidepressant.5
A review by Lapidus et al5 has a more extensive listing of current medications and investigational compounds that modulate glutamate transmission, and are of interest for their possible antidepressant activity. Given the relatively new “glutamatergic hypothesis” of depression, it is exciting that so many current and novel glutamatergic drug therapies are being evaluated.
Future of ketamine treatment
Glutamate has been shown to play an important part in the pathophysiology of depression. The rapid antidepressant efficacy of ketamine provides evidence that future medications with glutamate-modulating activity could be useful for patients who struggle to achieve symptom relief using available antidepressants. Several limitations exist regarding ketamine use, and more work in this important therapeutic area needs to be done. This last point is important to remember when speaking with patients such as Mrs. S. Although it is understandable for her to be excited about novel treatment options such as ketamine, stress to her that treating depression with ketamine at this time is strictly investigational, and that the drug needs to be thoroughly evaluated for safety and efficacy before it can be prescribed for this indication.
CASE CONTINUED
Mrs. S realizes that ketamine may not be the best next step for her, and she agrees to explore other approaches to treat her residual depressive symptoms.
Related Resources
• Machado-Vieira R, Ibrahim L, Henter ID, et al. Novel glutamatergic agents for major depressive disorder and bipolar disorder. Pharmacol Biochem Behav. 2012;100(4):678-687.
• Mathews DC, Henter ID, Zarate CA. Targeting the glutamatergic system to treat major depressive disorder: rationale and progress to date. Drugs. 2012;72(10):1313-1333.
Drug Brand Names
Acamprosate • Campral Duloxetine • Cymbalta
Aripiprazole • Abilify Ketamine • Ketalar
Bupropion • Wellbutrin, Zyban Riluzole • Rilutek
Disclosures
The authors report no financial relationships with any companies whose products are mentioned in this article or with manufacturers of competing products.
Mrs. S, age 46, has been struggling to manage depression for 7 years. She completed adequate trials of several selective serotonin reuptake inhibitors and bupropion. Currently, she is taking duloxetine, 60 mg/d, and aripiprazole, 5 mg/d.
At her most recent clinic visit, Mrs. S reports that she is doing “OK,” but that she still feels sad and disengaged most days of the week. She wants to know more about ketamine for treating depression after reading about it on the Internet and hearing it mentioned in a support group she attends. She asks if you think it would work for her, and gives you with a copy of an article about its use in patients with treatment-resistant depression. Mrs. S has no other health conditions and takes a daily vitamin D and calcium supplement.
The monoamine hypothesis of depression postulates that symptoms originate from underactivity of monoamines, such as serotonin, norepinephrine, and dopamine, in the brain. This hypothesis was formulated in the 1960s after researchers observed that monoamine oxidase inhibitors and tricyclic antidepressants relieved depressive symptoms; both were known to increase monoamine concentrations in the synaptic cleft.1
Regrettably, these medications do not adequately relieve depressive symptoms for many people. In fact, symptom remission occurs in only one-third of treated patients.2 This low remission rate reflects a lack of understanding of the pathophysiology of depression, and the need for drugs with unique mechanisms of action.
One of the newest drug targets shown to be relevant in psychiatric illness is the
glutamatergic system. Glutamate is the predominant excitatory neurotransmitter in the CNS, and it is responsible for many key functions, including synaptic plasticity, learning, memory, and locomotion.3 Normally, the glutamatergic system tightly regulates the amount of glutamate in the neuronal synapse via receptors on presynaptic and postsynaptic neurons, as well as on glial cells (Figure). When this equilibrium is disrupted in stressful situations, such as ischemia, trauma, or seizures, excess glutamate is released into the synapse. The resulting glutamatergic hyperactivity can lead to neurotoxicity and cell death when neuronal receptors are activated for an extended period.
A key component of the glutamatergic system that is responsible for removing excess glutamate from the synapse is membrane-bound transporters, which are similar to serotonin and norepinephrine transporters. These excitatory amino acid transporters (EAATs) are important because glutamate metabolism does not occur within the synapse and EAATS are responsible for removing most of the glutamate from the synapse into glial cells.3
The network of receptors within the synapse that are activated by glutamate is extensive and complex. There are at least 11 glutamate-responsive receptors: 3 are ionotropic action channels, and the remaining 8 are metabotropic G protein-coupled receptors. Previous studies have shown regional changes in glutamate receptors, as well as elevated levels of glutamate, in the brains of patients with major depressive disorder (MDD).4
Ketamine. The ionotropic receptor N-methyl-d-aspartate (NMDA) is one of the most studied glutamate receptors. Pharmacologically, ketamine is a noncompetitive NMDA receptor antagonist that also activates the amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor, which is another subtype of ionotropic glutamate receptors. In open-label clinical trials, ketamine has demonstrated rapid antidepressant action in patients with treatment-resistant MDD.4,5
Recently, Murrough et al6 performed the first randomized, psychoactive controlled trial using a single IV infusion of ketamine dosed below anesthesia ranges (0.5 mg/kg), or midazolam (0.045 mg/kg), in patients with treatment-resistant depression who had been antidepressant-free for at least 4 weeks. They found that 24 hours after medication administration, the likelihood of response to ketamine was significantly higher than the response to midazolam (OR: 2.18; 95% CI: 1.21 to 4.14), with a response rate of 64% in the ketamine group and 28% in the midazolam group.6
Psychotropic side effects, such as hallucinations, are a major concern with ketamine tolerability and abuse potential. This is largely because of ketamine’s antagonism of the NMDA receptor, which is a property shared with other abused drugs such as phencyclidine (PCP) and dextromethorphan. In the Murrough et al6 study, there were no reported cases of paranoia or hallucinations, but dissociative symptoms were relatively common (17%).
Although the results in this trial appear encouraging, there are several limitations to using ketamine to treat MDD, especially in an ambulatory setting. Concerns include ketamine’s IV administration, potential for abuse, long-term efficacy, and side-effect profile—particularly psychotic symptoms and hemodynamic changes. An ideal compound would have the rapid efficacy of ketamine, but with a safer side-effect profile, easier administration, and less potential for abuse.
Riluzole also acts on the glutamatergic system, but has not shown antidepressant efficacy as consistently as ketamine. Riluzole is FDA-approved for treating amyotrophic lateral sclerosis.5 Pharmacologically, riluzole is a glutamatergic modulator that increases glutamate reuptake into glial cells, decreases glutamate release, and increases AMPA trafficking. In open-label studies riluzole has shown efficacy in reducing depressive symptoms.4,5 However, when compared with placebo as a means of sustaining treatment response after a 1-time dose of ketamine, riluzole showed was no significant improvement in time to depressive relapse.7
Acamprosate, often used for treating alcohol abuse, is another a drug with glutamatergic activity that has been studied for possible use as an antidepressant.5
A review by Lapidus et al5 has a more extensive listing of current medications and investigational compounds that modulate glutamate transmission, and are of interest for their possible antidepressant activity. Given the relatively new “glutamatergic hypothesis” of depression, it is exciting that so many current and novel glutamatergic drug therapies are being evaluated.
Future of ketamine treatment
Glutamate has been shown to play an important part in the pathophysiology of depression. The rapid antidepressant efficacy of ketamine provides evidence that future medications with glutamate-modulating activity could be useful for patients who struggle to achieve symptom relief using available antidepressants. Several limitations exist regarding ketamine use, and more work in this important therapeutic area needs to be done. This last point is important to remember when speaking with patients such as Mrs. S. Although it is understandable for her to be excited about novel treatment options such as ketamine, stress to her that treating depression with ketamine at this time is strictly investigational, and that the drug needs to be thoroughly evaluated for safety and efficacy before it can be prescribed for this indication.
CASE CONTINUED
Mrs. S realizes that ketamine may not be the best next step for her, and she agrees to explore other approaches to treat her residual depressive symptoms.
Related Resources
• Machado-Vieira R, Ibrahim L, Henter ID, et al. Novel glutamatergic agents for major depressive disorder and bipolar disorder. Pharmacol Biochem Behav. 2012;100(4):678-687.
• Mathews DC, Henter ID, Zarate CA. Targeting the glutamatergic system to treat major depressive disorder: rationale and progress to date. Drugs. 2012;72(10):1313-1333.
Drug Brand Names
Acamprosate • Campral Duloxetine • Cymbalta
Aripiprazole • Abilify Ketamine • Ketalar
Bupropion • Wellbutrin, Zyban Riluzole • Rilutek
Disclosures
The authors report no financial relationships with any companies whose products are mentioned in this article or with manufacturers of competing products.
1. Niciu MJ, Ionescu DF, Richards EM, et al. Glutamate and its receptors in the pathophysiology and treatment of major depressive disorder. J Neural Transm. 2014;121(8):907-924.
2. Gaynes BN, Dusetzina SB, Ellis AR, et al. Treating depression after initial treatment failure: directly comparing switch and augmenting strategies in STAR*D. J Clin Psychopharmacol. 2012;32(1):114-119.
3. Curry SC, Mills KC, Ruha A, et al. Neurotransmitters and neuromodulators. In: Nelson LS, Lewin NA, Howland MA, et al, eds. Goldfrank’s toxicologic emergencies. 9th ed. New York, NY: McGraw-Hill; 2011:189-220.
4. Zarate C Jr, Machado-Vieira R, Henter I, et al. Glutamatergic modulators: the future of treating mood disorders? Harv Rev Psychiatry. 2010;18(5):293-303.
5. Lapidus KA, Soleimani L, Murrough JW. Novel glutamatergic drugs for the treatment of mood disorders. Neuropsychiatr Dis Treat. 2013;9:1101-1112.
6. Murrough JW, Iosifescu DV, Chang LC, et al. Antidepressant efficacy of ketamine in treatment-resistant major depression: a two-site randomized controlled trial. Am J Psychiatry. 2013;170(10):1134-1142.
7. Ibrahim L, Diazgranados N, Franco-Chaves J, et al. Course of improvement in depressive symptoms to a single intravenous infusion of ketamine vs add-on riluzole: results from a 4-week, double-blind, placebo-controlled study. Neuropsychopharmacology. 2012;37(6):1526-1533.
1. Niciu MJ, Ionescu DF, Richards EM, et al. Glutamate and its receptors in the pathophysiology and treatment of major depressive disorder. J Neural Transm. 2014;121(8):907-924.
2. Gaynes BN, Dusetzina SB, Ellis AR, et al. Treating depression after initial treatment failure: directly comparing switch and augmenting strategies in STAR*D. J Clin Psychopharmacol. 2012;32(1):114-119.
3. Curry SC, Mills KC, Ruha A, et al. Neurotransmitters and neuromodulators. In: Nelson LS, Lewin NA, Howland MA, et al, eds. Goldfrank’s toxicologic emergencies. 9th ed. New York, NY: McGraw-Hill; 2011:189-220.
4. Zarate C Jr, Machado-Vieira R, Henter I, et al. Glutamatergic modulators: the future of treating mood disorders? Harv Rev Psychiatry. 2010;18(5):293-303.
5. Lapidus KA, Soleimani L, Murrough JW. Novel glutamatergic drugs for the treatment of mood disorders. Neuropsychiatr Dis Treat. 2013;9:1101-1112.
6. Murrough JW, Iosifescu DV, Chang LC, et al. Antidepressant efficacy of ketamine in treatment-resistant major depression: a two-site randomized controlled trial. Am J Psychiatry. 2013;170(10):1134-1142.
7. Ibrahim L, Diazgranados N, Franco-Chaves J, et al. Course of improvement in depressive symptoms to a single intravenous infusion of ketamine vs add-on riluzole: results from a 4-week, double-blind, placebo-controlled study. Neuropsychopharmacology. 2012;37(6):1526-1533.
10 Recent paradigm shifts in the neurobiology and treatment of depression
Nowhere is that change in landscape more apparent than in major depression, the No. 1 disabling condition in all of medicine, according to the World Health Organization. The past decade has generated at least 10 paradigm shifts in the neurobiology and pharmacotherapeutics of depression.
Clinging to simplistic tradition
Most contemporary clinicians continue to practice the traditional model of depression, which is based on the assumption that depression is caused by a deficiency of monoamines: serotonin (5-HT) and norepinephrine (NE). The entire antidepressant armamentarium approved for use by the FDA was designed according to the amine deficiency hypothesis. Depressed patients uniformly receive reuptake inhibitors of 5-HT and NE, but few achieve full remission, as the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study showed.1
As scientific paradigm shifts infiltrate clinical practice, however, the tired notion of “chemical imbalance” will yield to more complex and evidence-based models.
Usually, it would be remarkable to witness a single paradigm shift in the understanding of a brain disorder. Imagine the disruptive impact of multiple scientific shifts within the past decade! Consider the following departures from the old dogma about the simplistic old explanation of depression.
1. From neurotransmitters to neuroplasticity
For half a century, our field tenaciously held to the monoamine theory, which posits that depression is caused by a deficiency of 5-HT or NE, or both. All antidepressants in use today were developed to increase brain monoamines by inhibiting their reuptake at the synaptic cleft. Now, research points to other causes:
• impaired neuroplasticity
• a decrement of neurogenesis
• synaptic deficits
• decreased neurotrophins (such as brain-derived neurotrophic factor)
• dendritic pathology.2,3
2. From ‘chemical imbalance’ to neuroinflammation
The simplistic notion that depression is a chemical imbalance, so to speak, in the brain is giving way to rapidly emerging evidence that depression is associated with neuroinflammation.4
Pro-inflammatory cytokines are elevated in the plasma of depressed patients, and subside when the acute episode is treated. Current antidepressants actually have anti-inflammatory effects that have gone unrecognized.5 A meta-analysis of the use of anti-inflammatory agents (such as nonsteroidal anti-inflammatory drugs and aspirin) in depression shows promising efficacy.6 Some inflammatory markers, such as C-reactive protein, already have been reported to predict response to some antidepressants, but not to others.7
3. From 5-HT and NE pathways to glutamate NMDA receptors
Recent landmark studies8 have, taken together, demonstrated that a single IV dose of the N-methyl-d-aspartate (NMDA) receptor antagonist ketamine (a psychotogenic drug of abuse FDA-approved only as an anesthetic) can produce clinical improvement of severe depression and even full remission for several days. Such studies demonstrate that the old dogma of 5-HT and NE deficiency might not be a valid overarching hypothesis of the depression syndrome.
Long-term maintenance studies of ketamine to document its safety and continued efficacy need to be conducted. The mechanism of action of ketamine is believed to be a rapid trigger for enhancing neuroplasticity.
4. From oral to parenteral administration
Several studies have been published showing the efficacy of IV or intranasal administration of new agents for depression. Ketamine studies, for example, were conducted using an IV infusion of a 150-mg dose over 1 hour. Other IV studies used the anticholinergic scopolamine.9
Intranasal ketamine also has been shown to be clinically efficacious.10 Inhalable nitrous oxide (laughing gas, an NMDA antagonist) recently was reported to improve depression as well.11
It is possible that parenteral administration of antidepressant agents may exert a different neurobiological effect and provide a more rapid response than oral medication.
5. From delayed efficacy (weeks) to immediate onset (1 or 2 hours)
The widely entrenched notion that depression takes several weeks to improve with an antidepressant has collapsed with emerging evidence that symptoms of the disorder (even suicidal ideation) can be reversed within 1 or 2 hours.12 IV ketamine isn’t the only example; IV scopolamine,9 inhalable nitrous oxide,11 and overnight sleep deprivation13 also exert a rapid therapeutic effect. This is a major rethinking of how quickly the curtain of severe depression can be lifted, and is great news for patients and their family.
6. From psychological symptoms to cortical or subcortical changes
Depression traditionally has been recognized as a clinical syndrome of sadness, self-deprecation, cognitive dulling, and vegetative symptoms. In recent studies, however, researchers report that low hippocampus volume14 in healthy young girls predicts future depression. Patients with unremitting depression have been reported to have an abnormally shaped hippocampus.15
In addition, gray-matter volume in the subgenual anterior cingulate (Brodmann area 24) is hypoplastic in depressed persons,16 making that area a target for deep-brain stimulation (DBS). Brain morphological changes such as a hypoplastic hippocampus might become useful biomarkers for identifying persons at risk of severe depression, and might become a useful adjunctive biomarker for making a clinical diagnosis.
7. From healing the mind to repairing the brain
It is well-established that depression is associated with loss of dendritic spines and arborizations, loss of synapses, and diminishment of glial cells, especially in the hippocampus17 and anterior cingulate.18 Treating depression, whether pharmaceutical or somatic, involves reversing these changes by increasing neurotrophic factors, enhancing neurogenesis and gliogenesis, and restoring synaptic and dendritic health and cell survival in the hippocampus and frontal cortex.19,20 Treating depression involves brain repair, which is reflected, ultimately, in healing the mind.
8. From pharmacotherapy to neuromodulation
Although drugs remain the predominant treatment modality for depression, there is palpable escalation in the use of neuromodulation methods.
The oldest of these neuromodulatory techniques is electroconvulsive therapy, an excellent treatment for severe depression (and one that enhances hippocampal neurogenesis). In addition, several novel neuromodulation methods have been approved (transcranial magnetic stimulation and vagus nerve stimulation) or are in development (transcranial direct-current stimulation, cranial electrotherapy stimulation, and DBS).21 These somatic approaches to treating the brain directly to alleviate depression target regions involved in depression and reduce the needless risks associated with exposing other organ systems to a drug.
9. From monotherapy to combination therapy
The use of combination therapy for depression has escalated with FDA approval of adjunctive use of atypical antipsychotics in unipolar and bipolar depression. In addition, the landmark STAR*D study1 demonstrated the value of augmentation therapy with a second antidepressant when 1 agent fails. Other controlled studies have shown that combining 2 antidepressants is superior to administering 1.22
Just as other serious medical disorders—such as cancer and hypertension—are treated with 2 or 3 medications, severe depression might require a similar strategy. The field gradually is adopting that approach.
10. From cortical folds to wrinkles on the face
Last, a new (and unexpected) paradigm shift recently emerged, which is genuinely intriguing—even baffling. Using placebo-controlled designs, several researchers have reported significant, persistent improvement of depressive symptoms after injection of onabotulinumtoxinA in the corrugator muscles of the glabellar region of the face, where the omega sign often appears in a depressed person.23,24
The longest of the studies25 was 6 months; investigators reported that improvement continued even after the effect of the botulinum toxin on the omega sign wore off. The proposed mechanism of action is the facial feedback hypothesis, which suggests that, biologically, facial expression has an impact on one’s emotional state.
Big payoffs coming from research in neuroscience
These 10 paradigm shifts in a single psychiatric syndrome are emblematic of exciting clinical and research advances in our field. Like all syndromes, depression is associated with multiple genetic and environmental causes; it isn’t surprising that myriad treatment approaches are emerging.
The days of clinging to monolithic, serendipity-generated models surely are over. Evidence-based psychiatric brain research is shattering aging dogmas that have, for decades, stifled innovation in psychiatric therapeutics that is now moving in novel directions.
Take note, however, that the only paradigm shift that matters to depressed patients is the one that transcends mere control of their symptoms and restores their wellness, functional capacity, and quality of life. With the explosive momentum of neuroscience discovery, psychiatry is, at last, poised to deliver—in splendid, even seismic, fashion.
1. Trivedi MH, Fava M, Wisniewski SR, et al. Medication augmentation after the failure of SSRIs for depression. N Eng J Med. 2006;354(12):1243-1252.
2. Serafini G, Hayley S, Pompili M, et al. Hippocampal neurogenesis, neurotrophic factors and depression: possible therapeutic targets [published online November 30, 2014]? CNS Neurol Disord Drug Targets. doi: 10.2174/1871527313666141130223723.
3. Duman RS, Aghajanian GK. Synaptic dysfunction in depression: potential therapeutic targets. Science. 2012;338(6103):68-72.
4. Iwata M, Ota KT, Duman RS. The inflammasome: pathways linking psychological stress, depression, and systemic illnesses. Brain Behav Immun. 2013;31:105-114.
5. Sacre S, Medghalichi M, Gregory B, et al. Fluoxetine and citalopram exhibit potent anti-inflammatory activity in human and murine models of rheumatoid arthritis and inhibit toll-like receptors. Arthritis Rheum. 2010;62(3):683-693.
6. Köhler O, Benros ME, Nordentoft M, et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2014;71(12): 1381-1391.
7. Uher R, Tansey KE, Dew T, et al. An inflammatory biomarker as a differential predictor of outcome of depression treatment with escitalopram and nortiptyline. Am J Psychiatry. 2014;171(14):1278-1286.
8. Abdallah CG, Sanacora G, Duman RS, et al. Ketamine and rapid-acting antidepressants: a window into a new neurobiology for mood disorder therapeutics [published online October 17, 2014]. Annual Rev Med. doi: 10.1146/annurev-med-053013-062946.
9. Furey ML, Khanna A, Hoffman EM, et al. Scopolamine produces larger antidepressant and antianxiety effects in women than in men. Neuropsychopharmacology. 2010;35(12):2479-2488.
10. Lapidus KA, Levitch CF, Perez AM, et al. A randomized controlled trial of intranasal ketamine in major depressive disorder. Biol Psychiatry. 2014; 76(12):970-976.
11. Nagele P, Duma A, Kopec M, et al. Nitrous oxide for treatment-resistant major depression: a proof-of-concept trial [published December 14, 2014]. Biol Psychiatry. doi: http://dx.doi.org/10.1016/j.biopsych.2014.11.016.
12. Köhler O, Benros ME, Nordentoft M, et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2014;71(12): 1381-1391.
13. Bunney BG, Bunney WE. Mechanisms of rapid antidepressant effects of sleep deprivation therapy: clock genes and circadian rhythms. Biol Psychiatry. 2013;73(12):1164-1171.
14. Chen MC, Hamilton JP, Gotlib IH. Decreased hippocampal volume in healthy girls at risk for depression. Arch Gen Psychiatry. 2010;67(3):270-276.
15. Tae WS, Kim SS, Lee KU, et al. Hippocampal shape deformation in female patients with unremitting major depressive disorder. AJNR Am J Neuroradiol. 2011;32(4):671-676.
16. Hamani C, Mayberg H, Synder B, et al. Deep brain stimulation of the subcallosal cingulate gyrus for depression: anatomical location of active contacts in clinical responders and a suggested guideline for targeting. J Neurosurg. 2009;111(6):1209-1215.
17. Sheline YI, Gado MH, Kraemer HC. Untreated depression and hippocampal volume loss. Am J Psychiatry. 2003;160(8):1516-1518.
18. Redlich R, Almeoda JJ, Grotegerd D, et al. Brain morphometric biomarkers distinguishing unipolar and bipolar depression. A voxel-based morphometry-pattern classification approach. JAMA Psychiatry. 2014;71(11):1222-1230.
19. Mendez-David I, Hen R, Gardier AM, et al. Adult hippocampal neurogenesis: an actor in the antidepressant-like action. Ann Pharm Fr. 2013;71(3):143-149.
20. Serafini G. Neuroplasticity and major depression, the role of modern antidepressant drugs. World J Psychiatry. 2012;2(3):49-57.
21. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Neuropsychopharmacology. 2012;37(1):102-116.
22. Blier P, Ward HE, Tremblay P, et al. Combination of antidepressant medications from treatment initiation for major depressive disorder: a double-blind randomized study. Am J Psychiatry. 2010;167(3):281-288.
23. Wollmer MA, de Boer C, Kalak N, et al. Facing depression with botulinum toxin: a randomized controlled trial. J Psychiatr Res. 2012;46(5):574-581.
24. Finzi E, Rosenthal NE. Treatment of depression with onabotulinumtoxinA: a randomized, double-blind, placebo controlled trial. J Psychiatr Res. 2014;52:1-6.
25. Magid M, Reichenberg JS, Poth PE, et al. Treatment of major depressive disorder using botulinum toxin A: a 24-week randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2014;75(8):837-844.
Nowhere is that change in landscape more apparent than in major depression, the No. 1 disabling condition in all of medicine, according to the World Health Organization. The past decade has generated at least 10 paradigm shifts in the neurobiology and pharmacotherapeutics of depression.
Clinging to simplistic tradition
Most contemporary clinicians continue to practice the traditional model of depression, which is based on the assumption that depression is caused by a deficiency of monoamines: serotonin (5-HT) and norepinephrine (NE). The entire antidepressant armamentarium approved for use by the FDA was designed according to the amine deficiency hypothesis. Depressed patients uniformly receive reuptake inhibitors of 5-HT and NE, but few achieve full remission, as the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study showed.1
As scientific paradigm shifts infiltrate clinical practice, however, the tired notion of “chemical imbalance” will yield to more complex and evidence-based models.
Usually, it would be remarkable to witness a single paradigm shift in the understanding of a brain disorder. Imagine the disruptive impact of multiple scientific shifts within the past decade! Consider the following departures from the old dogma about the simplistic old explanation of depression.
1. From neurotransmitters to neuroplasticity
For half a century, our field tenaciously held to the monoamine theory, which posits that depression is caused by a deficiency of 5-HT or NE, or both. All antidepressants in use today were developed to increase brain monoamines by inhibiting their reuptake at the synaptic cleft. Now, research points to other causes:
• impaired neuroplasticity
• a decrement of neurogenesis
• synaptic deficits
• decreased neurotrophins (such as brain-derived neurotrophic factor)
• dendritic pathology.2,3
2. From ‘chemical imbalance’ to neuroinflammation
The simplistic notion that depression is a chemical imbalance, so to speak, in the brain is giving way to rapidly emerging evidence that depression is associated with neuroinflammation.4
Pro-inflammatory cytokines are elevated in the plasma of depressed patients, and subside when the acute episode is treated. Current antidepressants actually have anti-inflammatory effects that have gone unrecognized.5 A meta-analysis of the use of anti-inflammatory agents (such as nonsteroidal anti-inflammatory drugs and aspirin) in depression shows promising efficacy.6 Some inflammatory markers, such as C-reactive protein, already have been reported to predict response to some antidepressants, but not to others.7
3. From 5-HT and NE pathways to glutamate NMDA receptors
Recent landmark studies8 have, taken together, demonstrated that a single IV dose of the N-methyl-d-aspartate (NMDA) receptor antagonist ketamine (a psychotogenic drug of abuse FDA-approved only as an anesthetic) can produce clinical improvement of severe depression and even full remission for several days. Such studies demonstrate that the old dogma of 5-HT and NE deficiency might not be a valid overarching hypothesis of the depression syndrome.
Long-term maintenance studies of ketamine to document its safety and continued efficacy need to be conducted. The mechanism of action of ketamine is believed to be a rapid trigger for enhancing neuroplasticity.
4. From oral to parenteral administration
Several studies have been published showing the efficacy of IV or intranasal administration of new agents for depression. Ketamine studies, for example, were conducted using an IV infusion of a 150-mg dose over 1 hour. Other IV studies used the anticholinergic scopolamine.9
Intranasal ketamine also has been shown to be clinically efficacious.10 Inhalable nitrous oxide (laughing gas, an NMDA antagonist) recently was reported to improve depression as well.11
It is possible that parenteral administration of antidepressant agents may exert a different neurobiological effect and provide a more rapid response than oral medication.
5. From delayed efficacy (weeks) to immediate onset (1 or 2 hours)
The widely entrenched notion that depression takes several weeks to improve with an antidepressant has collapsed with emerging evidence that symptoms of the disorder (even suicidal ideation) can be reversed within 1 or 2 hours.12 IV ketamine isn’t the only example; IV scopolamine,9 inhalable nitrous oxide,11 and overnight sleep deprivation13 also exert a rapid therapeutic effect. This is a major rethinking of how quickly the curtain of severe depression can be lifted, and is great news for patients and their family.
6. From psychological symptoms to cortical or subcortical changes
Depression traditionally has been recognized as a clinical syndrome of sadness, self-deprecation, cognitive dulling, and vegetative symptoms. In recent studies, however, researchers report that low hippocampus volume14 in healthy young girls predicts future depression. Patients with unremitting depression have been reported to have an abnormally shaped hippocampus.15
In addition, gray-matter volume in the subgenual anterior cingulate (Brodmann area 24) is hypoplastic in depressed persons,16 making that area a target for deep-brain stimulation (DBS). Brain morphological changes such as a hypoplastic hippocampus might become useful biomarkers for identifying persons at risk of severe depression, and might become a useful adjunctive biomarker for making a clinical diagnosis.
7. From healing the mind to repairing the brain
It is well-established that depression is associated with loss of dendritic spines and arborizations, loss of synapses, and diminishment of glial cells, especially in the hippocampus17 and anterior cingulate.18 Treating depression, whether pharmaceutical or somatic, involves reversing these changes by increasing neurotrophic factors, enhancing neurogenesis and gliogenesis, and restoring synaptic and dendritic health and cell survival in the hippocampus and frontal cortex.19,20 Treating depression involves brain repair, which is reflected, ultimately, in healing the mind.
8. From pharmacotherapy to neuromodulation
Although drugs remain the predominant treatment modality for depression, there is palpable escalation in the use of neuromodulation methods.
The oldest of these neuromodulatory techniques is electroconvulsive therapy, an excellent treatment for severe depression (and one that enhances hippocampal neurogenesis). In addition, several novel neuromodulation methods have been approved (transcranial magnetic stimulation and vagus nerve stimulation) or are in development (transcranial direct-current stimulation, cranial electrotherapy stimulation, and DBS).21 These somatic approaches to treating the brain directly to alleviate depression target regions involved in depression and reduce the needless risks associated with exposing other organ systems to a drug.
9. From monotherapy to combination therapy
The use of combination therapy for depression has escalated with FDA approval of adjunctive use of atypical antipsychotics in unipolar and bipolar depression. In addition, the landmark STAR*D study1 demonstrated the value of augmentation therapy with a second antidepressant when 1 agent fails. Other controlled studies have shown that combining 2 antidepressants is superior to administering 1.22
Just as other serious medical disorders—such as cancer and hypertension—are treated with 2 or 3 medications, severe depression might require a similar strategy. The field gradually is adopting that approach.
10. From cortical folds to wrinkles on the face
Last, a new (and unexpected) paradigm shift recently emerged, which is genuinely intriguing—even baffling. Using placebo-controlled designs, several researchers have reported significant, persistent improvement of depressive symptoms after injection of onabotulinumtoxinA in the corrugator muscles of the glabellar region of the face, where the omega sign often appears in a depressed person.23,24
The longest of the studies25 was 6 months; investigators reported that improvement continued even after the effect of the botulinum toxin on the omega sign wore off. The proposed mechanism of action is the facial feedback hypothesis, which suggests that, biologically, facial expression has an impact on one’s emotional state.
Big payoffs coming from research in neuroscience
These 10 paradigm shifts in a single psychiatric syndrome are emblematic of exciting clinical and research advances in our field. Like all syndromes, depression is associated with multiple genetic and environmental causes; it isn’t surprising that myriad treatment approaches are emerging.
The days of clinging to monolithic, serendipity-generated models surely are over. Evidence-based psychiatric brain research is shattering aging dogmas that have, for decades, stifled innovation in psychiatric therapeutics that is now moving in novel directions.
Take note, however, that the only paradigm shift that matters to depressed patients is the one that transcends mere control of their symptoms and restores their wellness, functional capacity, and quality of life. With the explosive momentum of neuroscience discovery, psychiatry is, at last, poised to deliver—in splendid, even seismic, fashion.
Nowhere is that change in landscape more apparent than in major depression, the No. 1 disabling condition in all of medicine, according to the World Health Organization. The past decade has generated at least 10 paradigm shifts in the neurobiology and pharmacotherapeutics of depression.
Clinging to simplistic tradition
Most contemporary clinicians continue to practice the traditional model of depression, which is based on the assumption that depression is caused by a deficiency of monoamines: serotonin (5-HT) and norepinephrine (NE). The entire antidepressant armamentarium approved for use by the FDA was designed according to the amine deficiency hypothesis. Depressed patients uniformly receive reuptake inhibitors of 5-HT and NE, but few achieve full remission, as the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study showed.1
As scientific paradigm shifts infiltrate clinical practice, however, the tired notion of “chemical imbalance” will yield to more complex and evidence-based models.
Usually, it would be remarkable to witness a single paradigm shift in the understanding of a brain disorder. Imagine the disruptive impact of multiple scientific shifts within the past decade! Consider the following departures from the old dogma about the simplistic old explanation of depression.
1. From neurotransmitters to neuroplasticity
For half a century, our field tenaciously held to the monoamine theory, which posits that depression is caused by a deficiency of 5-HT or NE, or both. All antidepressants in use today were developed to increase brain monoamines by inhibiting their reuptake at the synaptic cleft. Now, research points to other causes:
• impaired neuroplasticity
• a decrement of neurogenesis
• synaptic deficits
• decreased neurotrophins (such as brain-derived neurotrophic factor)
• dendritic pathology.2,3
2. From ‘chemical imbalance’ to neuroinflammation
The simplistic notion that depression is a chemical imbalance, so to speak, in the brain is giving way to rapidly emerging evidence that depression is associated with neuroinflammation.4
Pro-inflammatory cytokines are elevated in the plasma of depressed patients, and subside when the acute episode is treated. Current antidepressants actually have anti-inflammatory effects that have gone unrecognized.5 A meta-analysis of the use of anti-inflammatory agents (such as nonsteroidal anti-inflammatory drugs and aspirin) in depression shows promising efficacy.6 Some inflammatory markers, such as C-reactive protein, already have been reported to predict response to some antidepressants, but not to others.7
3. From 5-HT and NE pathways to glutamate NMDA receptors
Recent landmark studies8 have, taken together, demonstrated that a single IV dose of the N-methyl-d-aspartate (NMDA) receptor antagonist ketamine (a psychotogenic drug of abuse FDA-approved only as an anesthetic) can produce clinical improvement of severe depression and even full remission for several days. Such studies demonstrate that the old dogma of 5-HT and NE deficiency might not be a valid overarching hypothesis of the depression syndrome.
Long-term maintenance studies of ketamine to document its safety and continued efficacy need to be conducted. The mechanism of action of ketamine is believed to be a rapid trigger for enhancing neuroplasticity.
4. From oral to parenteral administration
Several studies have been published showing the efficacy of IV or intranasal administration of new agents for depression. Ketamine studies, for example, were conducted using an IV infusion of a 150-mg dose over 1 hour. Other IV studies used the anticholinergic scopolamine.9
Intranasal ketamine also has been shown to be clinically efficacious.10 Inhalable nitrous oxide (laughing gas, an NMDA antagonist) recently was reported to improve depression as well.11
It is possible that parenteral administration of antidepressant agents may exert a different neurobiological effect and provide a more rapid response than oral medication.
5. From delayed efficacy (weeks) to immediate onset (1 or 2 hours)
The widely entrenched notion that depression takes several weeks to improve with an antidepressant has collapsed with emerging evidence that symptoms of the disorder (even suicidal ideation) can be reversed within 1 or 2 hours.12 IV ketamine isn’t the only example; IV scopolamine,9 inhalable nitrous oxide,11 and overnight sleep deprivation13 also exert a rapid therapeutic effect. This is a major rethinking of how quickly the curtain of severe depression can be lifted, and is great news for patients and their family.
6. From psychological symptoms to cortical or subcortical changes
Depression traditionally has been recognized as a clinical syndrome of sadness, self-deprecation, cognitive dulling, and vegetative symptoms. In recent studies, however, researchers report that low hippocampus volume14 in healthy young girls predicts future depression. Patients with unremitting depression have been reported to have an abnormally shaped hippocampus.15
In addition, gray-matter volume in the subgenual anterior cingulate (Brodmann area 24) is hypoplastic in depressed persons,16 making that area a target for deep-brain stimulation (DBS). Brain morphological changes such as a hypoplastic hippocampus might become useful biomarkers for identifying persons at risk of severe depression, and might become a useful adjunctive biomarker for making a clinical diagnosis.
7. From healing the mind to repairing the brain
It is well-established that depression is associated with loss of dendritic spines and arborizations, loss of synapses, and diminishment of glial cells, especially in the hippocampus17 and anterior cingulate.18 Treating depression, whether pharmaceutical or somatic, involves reversing these changes by increasing neurotrophic factors, enhancing neurogenesis and gliogenesis, and restoring synaptic and dendritic health and cell survival in the hippocampus and frontal cortex.19,20 Treating depression involves brain repair, which is reflected, ultimately, in healing the mind.
8. From pharmacotherapy to neuromodulation
Although drugs remain the predominant treatment modality for depression, there is palpable escalation in the use of neuromodulation methods.
The oldest of these neuromodulatory techniques is electroconvulsive therapy, an excellent treatment for severe depression (and one that enhances hippocampal neurogenesis). In addition, several novel neuromodulation methods have been approved (transcranial magnetic stimulation and vagus nerve stimulation) or are in development (transcranial direct-current stimulation, cranial electrotherapy stimulation, and DBS).21 These somatic approaches to treating the brain directly to alleviate depression target regions involved in depression and reduce the needless risks associated with exposing other organ systems to a drug.
9. From monotherapy to combination therapy
The use of combination therapy for depression has escalated with FDA approval of adjunctive use of atypical antipsychotics in unipolar and bipolar depression. In addition, the landmark STAR*D study1 demonstrated the value of augmentation therapy with a second antidepressant when 1 agent fails. Other controlled studies have shown that combining 2 antidepressants is superior to administering 1.22
Just as other serious medical disorders—such as cancer and hypertension—are treated with 2 or 3 medications, severe depression might require a similar strategy. The field gradually is adopting that approach.
10. From cortical folds to wrinkles on the face
Last, a new (and unexpected) paradigm shift recently emerged, which is genuinely intriguing—even baffling. Using placebo-controlled designs, several researchers have reported significant, persistent improvement of depressive symptoms after injection of onabotulinumtoxinA in the corrugator muscles of the glabellar region of the face, where the omega sign often appears in a depressed person.23,24
The longest of the studies25 was 6 months; investigators reported that improvement continued even after the effect of the botulinum toxin on the omega sign wore off. The proposed mechanism of action is the facial feedback hypothesis, which suggests that, biologically, facial expression has an impact on one’s emotional state.
Big payoffs coming from research in neuroscience
These 10 paradigm shifts in a single psychiatric syndrome are emblematic of exciting clinical and research advances in our field. Like all syndromes, depression is associated with multiple genetic and environmental causes; it isn’t surprising that myriad treatment approaches are emerging.
The days of clinging to monolithic, serendipity-generated models surely are over. Evidence-based psychiatric brain research is shattering aging dogmas that have, for decades, stifled innovation in psychiatric therapeutics that is now moving in novel directions.
Take note, however, that the only paradigm shift that matters to depressed patients is the one that transcends mere control of their symptoms and restores their wellness, functional capacity, and quality of life. With the explosive momentum of neuroscience discovery, psychiatry is, at last, poised to deliver—in splendid, even seismic, fashion.
1. Trivedi MH, Fava M, Wisniewski SR, et al. Medication augmentation after the failure of SSRIs for depression. N Eng J Med. 2006;354(12):1243-1252.
2. Serafini G, Hayley S, Pompili M, et al. Hippocampal neurogenesis, neurotrophic factors and depression: possible therapeutic targets [published online November 30, 2014]? CNS Neurol Disord Drug Targets. doi: 10.2174/1871527313666141130223723.
3. Duman RS, Aghajanian GK. Synaptic dysfunction in depression: potential therapeutic targets. Science. 2012;338(6103):68-72.
4. Iwata M, Ota KT, Duman RS. The inflammasome: pathways linking psychological stress, depression, and systemic illnesses. Brain Behav Immun. 2013;31:105-114.
5. Sacre S, Medghalichi M, Gregory B, et al. Fluoxetine and citalopram exhibit potent anti-inflammatory activity in human and murine models of rheumatoid arthritis and inhibit toll-like receptors. Arthritis Rheum. 2010;62(3):683-693.
6. Köhler O, Benros ME, Nordentoft M, et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2014;71(12): 1381-1391.
7. Uher R, Tansey KE, Dew T, et al. An inflammatory biomarker as a differential predictor of outcome of depression treatment with escitalopram and nortiptyline. Am J Psychiatry. 2014;171(14):1278-1286.
8. Abdallah CG, Sanacora G, Duman RS, et al. Ketamine and rapid-acting antidepressants: a window into a new neurobiology for mood disorder therapeutics [published online October 17, 2014]. Annual Rev Med. doi: 10.1146/annurev-med-053013-062946.
9. Furey ML, Khanna A, Hoffman EM, et al. Scopolamine produces larger antidepressant and antianxiety effects in women than in men. Neuropsychopharmacology. 2010;35(12):2479-2488.
10. Lapidus KA, Levitch CF, Perez AM, et al. A randomized controlled trial of intranasal ketamine in major depressive disorder. Biol Psychiatry. 2014; 76(12):970-976.
11. Nagele P, Duma A, Kopec M, et al. Nitrous oxide for treatment-resistant major depression: a proof-of-concept trial [published December 14, 2014]. Biol Psychiatry. doi: http://dx.doi.org/10.1016/j.biopsych.2014.11.016.
12. Köhler O, Benros ME, Nordentoft M, et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2014;71(12): 1381-1391.
13. Bunney BG, Bunney WE. Mechanisms of rapid antidepressant effects of sleep deprivation therapy: clock genes and circadian rhythms. Biol Psychiatry. 2013;73(12):1164-1171.
14. Chen MC, Hamilton JP, Gotlib IH. Decreased hippocampal volume in healthy girls at risk for depression. Arch Gen Psychiatry. 2010;67(3):270-276.
15. Tae WS, Kim SS, Lee KU, et al. Hippocampal shape deformation in female patients with unremitting major depressive disorder. AJNR Am J Neuroradiol. 2011;32(4):671-676.
16. Hamani C, Mayberg H, Synder B, et al. Deep brain stimulation of the subcallosal cingulate gyrus for depression: anatomical location of active contacts in clinical responders and a suggested guideline for targeting. J Neurosurg. 2009;111(6):1209-1215.
17. Sheline YI, Gado MH, Kraemer HC. Untreated depression and hippocampal volume loss. Am J Psychiatry. 2003;160(8):1516-1518.
18. Redlich R, Almeoda JJ, Grotegerd D, et al. Brain morphometric biomarkers distinguishing unipolar and bipolar depression. A voxel-based morphometry-pattern classification approach. JAMA Psychiatry. 2014;71(11):1222-1230.
19. Mendez-David I, Hen R, Gardier AM, et al. Adult hippocampal neurogenesis: an actor in the antidepressant-like action. Ann Pharm Fr. 2013;71(3):143-149.
20. Serafini G. Neuroplasticity and major depression, the role of modern antidepressant drugs. World J Psychiatry. 2012;2(3):49-57.
21. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Neuropsychopharmacology. 2012;37(1):102-116.
22. Blier P, Ward HE, Tremblay P, et al. Combination of antidepressant medications from treatment initiation for major depressive disorder: a double-blind randomized study. Am J Psychiatry. 2010;167(3):281-288.
23. Wollmer MA, de Boer C, Kalak N, et al. Facing depression with botulinum toxin: a randomized controlled trial. J Psychiatr Res. 2012;46(5):574-581.
24. Finzi E, Rosenthal NE. Treatment of depression with onabotulinumtoxinA: a randomized, double-blind, placebo controlled trial. J Psychiatr Res. 2014;52:1-6.
25. Magid M, Reichenberg JS, Poth PE, et al. Treatment of major depressive disorder using botulinum toxin A: a 24-week randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2014;75(8):837-844.
1. Trivedi MH, Fava M, Wisniewski SR, et al. Medication augmentation after the failure of SSRIs for depression. N Eng J Med. 2006;354(12):1243-1252.
2. Serafini G, Hayley S, Pompili M, et al. Hippocampal neurogenesis, neurotrophic factors and depression: possible therapeutic targets [published online November 30, 2014]? CNS Neurol Disord Drug Targets. doi: 10.2174/1871527313666141130223723.
3. Duman RS, Aghajanian GK. Synaptic dysfunction in depression: potential therapeutic targets. Science. 2012;338(6103):68-72.
4. Iwata M, Ota KT, Duman RS. The inflammasome: pathways linking psychological stress, depression, and systemic illnesses. Brain Behav Immun. 2013;31:105-114.
5. Sacre S, Medghalichi M, Gregory B, et al. Fluoxetine and citalopram exhibit potent anti-inflammatory activity in human and murine models of rheumatoid arthritis and inhibit toll-like receptors. Arthritis Rheum. 2010;62(3):683-693.
6. Köhler O, Benros ME, Nordentoft M, et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2014;71(12): 1381-1391.
7. Uher R, Tansey KE, Dew T, et al. An inflammatory biomarker as a differential predictor of outcome of depression treatment with escitalopram and nortiptyline. Am J Psychiatry. 2014;171(14):1278-1286.
8. Abdallah CG, Sanacora G, Duman RS, et al. Ketamine and rapid-acting antidepressants: a window into a new neurobiology for mood disorder therapeutics [published online October 17, 2014]. Annual Rev Med. doi: 10.1146/annurev-med-053013-062946.
9. Furey ML, Khanna A, Hoffman EM, et al. Scopolamine produces larger antidepressant and antianxiety effects in women than in men. Neuropsychopharmacology. 2010;35(12):2479-2488.
10. Lapidus KA, Levitch CF, Perez AM, et al. A randomized controlled trial of intranasal ketamine in major depressive disorder. Biol Psychiatry. 2014; 76(12):970-976.
11. Nagele P, Duma A, Kopec M, et al. Nitrous oxide for treatment-resistant major depression: a proof-of-concept trial [published December 14, 2014]. Biol Psychiatry. doi: http://dx.doi.org/10.1016/j.biopsych.2014.11.016.
12. Köhler O, Benros ME, Nordentoft M, et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2014;71(12): 1381-1391.
13. Bunney BG, Bunney WE. Mechanisms of rapid antidepressant effects of sleep deprivation therapy: clock genes and circadian rhythms. Biol Psychiatry. 2013;73(12):1164-1171.
14. Chen MC, Hamilton JP, Gotlib IH. Decreased hippocampal volume in healthy girls at risk for depression. Arch Gen Psychiatry. 2010;67(3):270-276.
15. Tae WS, Kim SS, Lee KU, et al. Hippocampal shape deformation in female patients with unremitting major depressive disorder. AJNR Am J Neuroradiol. 2011;32(4):671-676.
16. Hamani C, Mayberg H, Synder B, et al. Deep brain stimulation of the subcallosal cingulate gyrus for depression: anatomical location of active contacts in clinical responders and a suggested guideline for targeting. J Neurosurg. 2009;111(6):1209-1215.
17. Sheline YI, Gado MH, Kraemer HC. Untreated depression and hippocampal volume loss. Am J Psychiatry. 2003;160(8):1516-1518.
18. Redlich R, Almeoda JJ, Grotegerd D, et al. Brain morphometric biomarkers distinguishing unipolar and bipolar depression. A voxel-based morphometry-pattern classification approach. JAMA Psychiatry. 2014;71(11):1222-1230.
19. Mendez-David I, Hen R, Gardier AM, et al. Adult hippocampal neurogenesis: an actor in the antidepressant-like action. Ann Pharm Fr. 2013;71(3):143-149.
20. Serafini G. Neuroplasticity and major depression, the role of modern antidepressant drugs. World J Psychiatry. 2012;2(3):49-57.
21. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Neuropsychopharmacology. 2012;37(1):102-116.
22. Blier P, Ward HE, Tremblay P, et al. Combination of antidepressant medications from treatment initiation for major depressive disorder: a double-blind randomized study. Am J Psychiatry. 2010;167(3):281-288.
23. Wollmer MA, de Boer C, Kalak N, et al. Facing depression with botulinum toxin: a randomized controlled trial. J Psychiatr Res. 2012;46(5):574-581.
24. Finzi E, Rosenthal NE. Treatment of depression with onabotulinumtoxinA: a randomized, double-blind, placebo controlled trial. J Psychiatr Res. 2014;52:1-6.
25. Magid M, Reichenberg JS, Poth PE, et al. Treatment of major depressive disorder using botulinum toxin A: a 24-week randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2014;75(8):837-844.