User login
Welcome to Current Psychiatry, a leading source of information, online and in print, for practitioners of psychiatry and its related subspecialties, including addiction psychiatry, child and adolescent psychiatry, and geriatric psychiatry. This Web site contains evidence-based reviews of the prevention, diagnosis, and treatment of mental illness and psychological disorders; case reports; updates on psychopharmacology; news about the specialty of psychiatry; pearls for practice; and other topics of interest and use to this audience.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-current-psychiatry')]
div[contains(@class, 'pane-pub-home-current-psychiatry')]
div[contains(@class, 'pane-pub-topic-current-psychiatry')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Participatory pharmacotherapy: 10 strategies for enhancing adherence
Psychiatric patients stand to benefit greatly from adhering to prescribed pharmacotherapy, but many patients typically do not follow their medication regimens.1,2 Three months after pharmacotherapy is initiated, approximately 50% of patients with major depressive disorder (MDD) do not take their prescribed antidepressants.3 Adherence rates in patients with schizophrenia range from 50% to 60%, and patients with bipolar disorder have adherence rates as low as 35%.4-6 One possible explanation for “treatment-resistant” depression, schizophrenia, and bipolar disorder may simply be nonadherence to prescribed pharmacotherapy.
Several strategies have been used to address this vexing problem (Table 1).7,8 They include individual and family psychoeducation,9,10 cognitive-behavioral therapy,11 interpersonal and social rhythm therapy, and family-focused therapy. This article describes an additional strategy I call “participatory pharmacotherapy.” In this model, the patient becomes a partner in the process of treatment choices and decision-making. This encourages patients to provide their own opinions and points of view regarding medication use. The prescribing clinician makes the patient feel that he or she has been listened to and understood. This and other techniques emphasize forming a therapeutic alliance with the patient before initiating pharmacotherapy. The patient provides information on his or her family history, medical and psychiatric history, and experience with previous medications, with a specific focus on which medications worked best for the patient and family members diagnosed with a similar condition.
Getting patients to participate
One of the fundamental tasks is to encourage patients to accept a participatory role, determine their underlying diagnosis, and co-create a treatment plan that will be most compatible with their illness and their personality. There are 10 components of establishing and practicing participatory pharmacotherapy.
1. Encourage patients to share their opinion of what a desirable treatment outcome should be. Some patients have unrealistic expectations about what medications can achieve. Clarify with patients what would be a realistic expectation of pharmacotherapy, and modify the patient’s beliefs to be compatible with a more probable outcome. For example, Ms. D, a 46-year-old mother of 2, is diagnosed with MDD, recurrent type without psychotic features. She states she expects pharmacotherapy will alleviate all symptoms and allow her to achieve a new healthy, happy state in which she will be able to laugh, socialize, and have fun every day for the rest of her life. Although achieving remission is a realistic and desirable treatment goal, Ms. D’s expectations are idealistic. Helping Ms. D accept and agree to realistic and achievable outcomes will improve her adherence to prescribed medications.
2. Encourage patients to share their ideas of how a desirable outcome can be accomplished. Similar to their expectations of outcomes, some patients have an unrealistic understanding of how treatment is conducted. Some patients expect treatment to be limited to prescribed medications or a one-time injection of a curative drug. Others prefer to use herbs and supplements and want to avoid prescribed medications. Understanding the patient’s expectations of how treatment is carried out will allow clinicians to provide patients with a rational view of treatment and establish a partnership based on realistic expectations.
3. Engage patients in choosing the best medication for them. Many patients have preconceived ideas about medications and which medicine would be best for them. They get this information from various sources, including family members and friends who benefitted from a specific drug, personal experience with medications, and exposure to drug advertising.
Understanding the patient’s preference for a specific medication and why he or she made such a choice is critical because doing so can take advantage of the patient’s self-fulfilling prophecies and improve the chances of obtaining a better outcome. For example, Mr. O, a 52-year-old father of 3, has been experiencing recurrent episodes of severe panic attacks. His clinician asked him to describe medications that in his opinion were most helpful in the past. He said he preferred clonazepam because it had helped him control the panic attacks and had minimal side effects, but he discontinued it after a previous psychotherapist told him he would become addicted to it. Obtaining this information was valuable because the clinician was able to clarify guidelines for clonazepam use without the risk of dependence. Mr. O is prescribed clonazepam, which he takes consistently and responds to excellently.
4. Involve patients in setting treatment goals and targeting symptoms to be relieved. Actively listen when patients describe their symptoms, discomforts, and past experiences with treatments. I invite patients to speak uninterrupted for 5 to 10 minutes, even if they talk about issues that seem irrelevant. I then summarize the patient’s major points and ask, “And what else?” After he or she says, “That’s it,” I ask the patient to assign a priority to alleviating each symptom.
For example, Ms. J, a 38-year-old married mother of 2, was diagnosed with bipolar II disorder. She listed her highest priority as controlling her impulsive shopping rather than alleviating depression, insomnia, or overeating. She had been forced to declare bankruptcy twice, and she was determined to never do so again. She also wanted to regain her husband’s trust and her ability to manage her finances. Ensuring that Ms. J felt understood regarding this issue increased the chances of establishing a solid treatment partnership. Providing Ms. J with a menu of treatment choices and asking her to describe her previous experiences with medications helped her and the clinician choose a medication that is compatible with her desire to control her impulsive shopping.
5. Engage patients in choosing the best delivery system for the prescribed medication. For many medications, clinicians can choose from a variety of delivery systems, including pills, transdermal patches, rectal or vaginal suppositories, creams, ointments, orally disintegrating tablets, liquids, and intramuscular injections. Patients have varying beliefs about the efficacy of particular delivery systems, based on personal experiences or what they have learned from the media, their family and friends, or the Internet. For example, Ms. S, age 28, experienced recurrent, disabling anxiety attacks. When asked about the best way of providing medication to relieve her symptoms, she chose gluteal injections because, as a child, her pediatrician had treated her for an unspecified illness by injecting medication in her buttock, which rapidly relieved her symptoms. This left her with the impression that injectable medications were the best therapeutic delivery system. After discussing the practicalities and availability of fast-acting medications to control panic attacks, we agreed to use orally disintegrating clonazepam, which is absorbed swiftly and provides fast symptom relief. Ms. S reported favorable results and was pleased with the process of developing this strategy with her clinician.
6. Involve patients in choosing the times and frequency of medication administration. The timing and frequency of medication administration can be used to enhance desirable therapeutic effects. For example, an antidepressant that causes sedation and somnolence could be taken at bedtime to help alleviate insomnia. Some studies have shown that taking a medication once a day improves adherence compared with taking the same medication in divided doses.13 Other patients may wish to take a medication several times a day so they can keep the medication in their purse or briefcase and feel confident that if they need a medication for immediate symptom relief, it will be readily available.
7. Teach patients to self-monitor changes and improvements in target symptoms. Engaging patients in a system of self-monitoring improves their chances of achieving successful treatment outcomes.14 Instruct patients to create a list of symptoms and monitor the intensity of each symptom using a rating scale of 1 to 5, where 1 represents the lowest intensity and 5 represents the highest. As for frequency, patients can rate each symptom from “not present” to “present most of the time.”
Self-monitoring allows patients to observe which daily behaviors and lifestyle choices make symptoms better and which make them worse. For example, Mrs. P, a 38-year-old married mother of 2, had anxiety and panic attacks associated with low self-esteem and chronic depression. Her clinician instructed her to use a 1-page form to monitor the frequency and intensity of her anxiety and panic symptoms by focusing on the physical manifestations, such as rapid heartbeat, shortness of breath, nausea, tremors, dry mouth, frequent urination, and diarrhea to see if there was any correlation between her behaviors and her symptoms.
8. Instruct patients to call you to report any changes, including minor successes. Early in my career, toward the end of each appointment after I’d prescribed medications I’d tell patients, “Please call me if you have a problem.” Frequently, patients would call with a list of problems and side effects that they believed were caused by the newly prescribed medication. Later, I realized that I may have inadvertently encouraged patients to develop problems so they would have a reason to call me. To achieve a more favorable outcome I changed the way I communicate. I now say, “Please call me next week, even if you begin to feel better with this new medication.” The phone call is now associated with the idea that they will “get better,” and internalizing such a suggestion allows patients to talk with the clinician and report favorable treatment results.
9. Tell patients to monitor their successes by relabeling and reframing their symptoms. Mr. B, age 28, has MDD and reports irritability, insomnia, short temper, and restlessness. After reviewing his desired treatment outcome, we discuss the benefits of pharmacotherapy. I tell him the new medication will improve the quality and length of his sleep, which will allow his body and mind to recharge his “internal batteries” and restore health and energy. When we discuss side effects, I tell him to expect a dry mouth, which will be his signal that the medication is working. This discussion helps patients reframe side effects and improves their ability to tolerate side effects and adhere to pharmacotherapy.
10. Harness the placebo effect and the power of suggestion to increase chances of achieving the best treatment outcomes. In a previous article,12 I reviewed the principles of recognizing and enhancing the placebo effect and the power of suggestion to improve the chances of achieving better pharmacotherapy outcomes. When practicing participatory pharmacotherapy, clinicians are consciously aware of the power embedded in their words and are careful to use language that enhances the placebo effect and the power of suggestion when prescribing medications. Use the patient’s own language as a way of pacing yourself to the patient’s description of his or her distress. For example, Ms. R, a 42-year-old mother of 3, describes her experiences seeking help for her anxiety and depression, stating that she has not yet found the right combination of medications that provide benefits with tolerable side effects. Her clinician responds by focusing on the word “yet” (pacing) stating, “even though you have not yet found the right combination of medications to provide the most desirable benefit of beginning healing and restoring your hope, I promise to work with you and together we will try to achieve an improvement in your overall health and well-being.” This response includes several positive words and suggestions of future success, which are referred to as leading.
Not all patients will respond to participatory pharmacotherapy. Some factors will make patients good candidates for this approach, and others should be considered exclusionary qualities (Table 2).
Bottom Line
“Participatory pharmacotherapy” involves identifying patients as partners in the process of treatment choice and decision-making, encouraging them to provide their opinions regarding medication use, and making patients feel they have been heard and understood. This technique emphasizes forming a therapeutic alliance with the patient to improve patients’ adherence to pharmacotherapy and optimize treatment outcomes.
Related Resources
- Haynes RB, Ackloo E, Sahota N, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;16(2);CD000011.
- Mahone IH. Shared decision making and serious mental illness. Arch Psychiatr Nurs. 2008;22(6):334-343.
- Russel CL, Ruppar TM, Metteson M. Improving medication adherence: moving from intention and motivation to a personal systems approach. Nurs Clin North Am. 2011;46(3):271-281.
- Tibaldi G, Salvador-Carulla L, Garcia-Gutierrez JC. From treatment adherence to advanced shared decision making: New professional strategies and attitudes in mental health care. Curr Clin Pharmacol. 2011;6(2):91-99.
Drug Brand Name
Clonazepam • Klonopin
Disclosure
Dr. Torem reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Zygmunt A, Olfson M, Boyer CA, et al. Interventions to improve medication adherence in schizophrenia. Am J Psychiatry. 2002;159:1653-1664.
2. Nosé M, Barbui C, Gray R, et al. Clinical interventions for treatment non-adherence in psychosis: meta-analysis. Br J Psychiatry. 2003;183:197-206.
3. Vergouwen AC, van Hout HP, Bakker A. Methods to improve patient compliance in the use of antidepressants. Ned Tijdschr Geneeskd. 2002;146:204-207.
4. Lacro JP, Dunn LB, Dolder CR, et al. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature.
J Clin Psychiatry. 2002;63:892-909.
5. Perkins DO. Predictors of noncompliance in patients with schizophrenia. J Clin Psychiatry. 2002;63:1121-1128.
6. Colom F, Vieta E, Martinez-Aran A, et al. Clinical factors associated with treatment noncompliance in euthymic bipolar patients. J Clin Psychiatry. 2000;61:549-555.
7. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487-497.
8. Osterberg LG, Rudd R. Medication adherence for antihypertensive therapy. In: Oparil S, Weber MA, eds. Hypertension: a companion to Brenner and Rector’s the kidney. 2nd ed. Philadelphia. PA: Elsevier Saunders; 2005:848.
9. Velligan DI, Weiden PJ, Sajatovic M, et al. Strategies for addressing adherence problems in patients with serious and persistent mental illness: recommendations from expert consensus guidelines. J Psychiatr Pract. 2010;16:306-324.
10. Miklowitz DJ. Adjunctive psychotherapy for bipolar disorder: state of the evidence. Am J Psychiatry. 2008; 165:1408-1419.
11. Szentagotai A, David D. The efficacy of cognitive-behavioral therapy in bipolar disorder: a quantitative meta-analysis. J Clin Psychiatry. 2010;71:66-72.
12. Torem MS. Words to the wise: 4 secrets of successful pharmacotherapy. Current Psychiatry. 2008;7(12):19-24.
13. Medic G, Higashi K, Littlewood KJ, et al. Dosing frequency and adherence in chronic psychiatric disease: systematic review and meta-analysis. Neuropsychiatr Dis Treat. 2013; 9:119-131.
14. Virdi N, Daskiran M, Nigam S, et al. The association of self-monitoring of blood glucose use with medication adherence and glycemic control in patients with type 2 diabetes initiating non-insulin treatment. Diabetes Technol Ther. 2012;14(9):790-798.
Psychiatric patients stand to benefit greatly from adhering to prescribed pharmacotherapy, but many patients typically do not follow their medication regimens.1,2 Three months after pharmacotherapy is initiated, approximately 50% of patients with major depressive disorder (MDD) do not take their prescribed antidepressants.3 Adherence rates in patients with schizophrenia range from 50% to 60%, and patients with bipolar disorder have adherence rates as low as 35%.4-6 One possible explanation for “treatment-resistant” depression, schizophrenia, and bipolar disorder may simply be nonadherence to prescribed pharmacotherapy.
Several strategies have been used to address this vexing problem (Table 1).7,8 They include individual and family psychoeducation,9,10 cognitive-behavioral therapy,11 interpersonal and social rhythm therapy, and family-focused therapy. This article describes an additional strategy I call “participatory pharmacotherapy.” In this model, the patient becomes a partner in the process of treatment choices and decision-making. This encourages patients to provide their own opinions and points of view regarding medication use. The prescribing clinician makes the patient feel that he or she has been listened to and understood. This and other techniques emphasize forming a therapeutic alliance with the patient before initiating pharmacotherapy. The patient provides information on his or her family history, medical and psychiatric history, and experience with previous medications, with a specific focus on which medications worked best for the patient and family members diagnosed with a similar condition.
Getting patients to participate
One of the fundamental tasks is to encourage patients to accept a participatory role, determine their underlying diagnosis, and co-create a treatment plan that will be most compatible with their illness and their personality. There are 10 components of establishing and practicing participatory pharmacotherapy.
1. Encourage patients to share their opinion of what a desirable treatment outcome should be. Some patients have unrealistic expectations about what medications can achieve. Clarify with patients what would be a realistic expectation of pharmacotherapy, and modify the patient’s beliefs to be compatible with a more probable outcome. For example, Ms. D, a 46-year-old mother of 2, is diagnosed with MDD, recurrent type without psychotic features. She states she expects pharmacotherapy will alleviate all symptoms and allow her to achieve a new healthy, happy state in which she will be able to laugh, socialize, and have fun every day for the rest of her life. Although achieving remission is a realistic and desirable treatment goal, Ms. D’s expectations are idealistic. Helping Ms. D accept and agree to realistic and achievable outcomes will improve her adherence to prescribed medications.
2. Encourage patients to share their ideas of how a desirable outcome can be accomplished. Similar to their expectations of outcomes, some patients have an unrealistic understanding of how treatment is conducted. Some patients expect treatment to be limited to prescribed medications or a one-time injection of a curative drug. Others prefer to use herbs and supplements and want to avoid prescribed medications. Understanding the patient’s expectations of how treatment is carried out will allow clinicians to provide patients with a rational view of treatment and establish a partnership based on realistic expectations.
3. Engage patients in choosing the best medication for them. Many patients have preconceived ideas about medications and which medicine would be best for them. They get this information from various sources, including family members and friends who benefitted from a specific drug, personal experience with medications, and exposure to drug advertising.
Understanding the patient’s preference for a specific medication and why he or she made such a choice is critical because doing so can take advantage of the patient’s self-fulfilling prophecies and improve the chances of obtaining a better outcome. For example, Mr. O, a 52-year-old father of 3, has been experiencing recurrent episodes of severe panic attacks. His clinician asked him to describe medications that in his opinion were most helpful in the past. He said he preferred clonazepam because it had helped him control the panic attacks and had minimal side effects, but he discontinued it after a previous psychotherapist told him he would become addicted to it. Obtaining this information was valuable because the clinician was able to clarify guidelines for clonazepam use without the risk of dependence. Mr. O is prescribed clonazepam, which he takes consistently and responds to excellently.
4. Involve patients in setting treatment goals and targeting symptoms to be relieved. Actively listen when patients describe their symptoms, discomforts, and past experiences with treatments. I invite patients to speak uninterrupted for 5 to 10 minutes, even if they talk about issues that seem irrelevant. I then summarize the patient’s major points and ask, “And what else?” After he or she says, “That’s it,” I ask the patient to assign a priority to alleviating each symptom.
For example, Ms. J, a 38-year-old married mother of 2, was diagnosed with bipolar II disorder. She listed her highest priority as controlling her impulsive shopping rather than alleviating depression, insomnia, or overeating. She had been forced to declare bankruptcy twice, and she was determined to never do so again. She also wanted to regain her husband’s trust and her ability to manage her finances. Ensuring that Ms. J felt understood regarding this issue increased the chances of establishing a solid treatment partnership. Providing Ms. J with a menu of treatment choices and asking her to describe her previous experiences with medications helped her and the clinician choose a medication that is compatible with her desire to control her impulsive shopping.
5. Engage patients in choosing the best delivery system for the prescribed medication. For many medications, clinicians can choose from a variety of delivery systems, including pills, transdermal patches, rectal or vaginal suppositories, creams, ointments, orally disintegrating tablets, liquids, and intramuscular injections. Patients have varying beliefs about the efficacy of particular delivery systems, based on personal experiences or what they have learned from the media, their family and friends, or the Internet. For example, Ms. S, age 28, experienced recurrent, disabling anxiety attacks. When asked about the best way of providing medication to relieve her symptoms, she chose gluteal injections because, as a child, her pediatrician had treated her for an unspecified illness by injecting medication in her buttock, which rapidly relieved her symptoms. This left her with the impression that injectable medications were the best therapeutic delivery system. After discussing the practicalities and availability of fast-acting medications to control panic attacks, we agreed to use orally disintegrating clonazepam, which is absorbed swiftly and provides fast symptom relief. Ms. S reported favorable results and was pleased with the process of developing this strategy with her clinician.
6. Involve patients in choosing the times and frequency of medication administration. The timing and frequency of medication administration can be used to enhance desirable therapeutic effects. For example, an antidepressant that causes sedation and somnolence could be taken at bedtime to help alleviate insomnia. Some studies have shown that taking a medication once a day improves adherence compared with taking the same medication in divided doses.13 Other patients may wish to take a medication several times a day so they can keep the medication in their purse or briefcase and feel confident that if they need a medication for immediate symptom relief, it will be readily available.
7. Teach patients to self-monitor changes and improvements in target symptoms. Engaging patients in a system of self-monitoring improves their chances of achieving successful treatment outcomes.14 Instruct patients to create a list of symptoms and monitor the intensity of each symptom using a rating scale of 1 to 5, where 1 represents the lowest intensity and 5 represents the highest. As for frequency, patients can rate each symptom from “not present” to “present most of the time.”
Self-monitoring allows patients to observe which daily behaviors and lifestyle choices make symptoms better and which make them worse. For example, Mrs. P, a 38-year-old married mother of 2, had anxiety and panic attacks associated with low self-esteem and chronic depression. Her clinician instructed her to use a 1-page form to monitor the frequency and intensity of her anxiety and panic symptoms by focusing on the physical manifestations, such as rapid heartbeat, shortness of breath, nausea, tremors, dry mouth, frequent urination, and diarrhea to see if there was any correlation between her behaviors and her symptoms.
8. Instruct patients to call you to report any changes, including minor successes. Early in my career, toward the end of each appointment after I’d prescribed medications I’d tell patients, “Please call me if you have a problem.” Frequently, patients would call with a list of problems and side effects that they believed were caused by the newly prescribed medication. Later, I realized that I may have inadvertently encouraged patients to develop problems so they would have a reason to call me. To achieve a more favorable outcome I changed the way I communicate. I now say, “Please call me next week, even if you begin to feel better with this new medication.” The phone call is now associated with the idea that they will “get better,” and internalizing such a suggestion allows patients to talk with the clinician and report favorable treatment results.
9. Tell patients to monitor their successes by relabeling and reframing their symptoms. Mr. B, age 28, has MDD and reports irritability, insomnia, short temper, and restlessness. After reviewing his desired treatment outcome, we discuss the benefits of pharmacotherapy. I tell him the new medication will improve the quality and length of his sleep, which will allow his body and mind to recharge his “internal batteries” and restore health and energy. When we discuss side effects, I tell him to expect a dry mouth, which will be his signal that the medication is working. This discussion helps patients reframe side effects and improves their ability to tolerate side effects and adhere to pharmacotherapy.
10. Harness the placebo effect and the power of suggestion to increase chances of achieving the best treatment outcomes. In a previous article,12 I reviewed the principles of recognizing and enhancing the placebo effect and the power of suggestion to improve the chances of achieving better pharmacotherapy outcomes. When practicing participatory pharmacotherapy, clinicians are consciously aware of the power embedded in their words and are careful to use language that enhances the placebo effect and the power of suggestion when prescribing medications. Use the patient’s own language as a way of pacing yourself to the patient’s description of his or her distress. For example, Ms. R, a 42-year-old mother of 3, describes her experiences seeking help for her anxiety and depression, stating that she has not yet found the right combination of medications that provide benefits with tolerable side effects. Her clinician responds by focusing on the word “yet” (pacing) stating, “even though you have not yet found the right combination of medications to provide the most desirable benefit of beginning healing and restoring your hope, I promise to work with you and together we will try to achieve an improvement in your overall health and well-being.” This response includes several positive words and suggestions of future success, which are referred to as leading.
Not all patients will respond to participatory pharmacotherapy. Some factors will make patients good candidates for this approach, and others should be considered exclusionary qualities (Table 2).
Bottom Line
“Participatory pharmacotherapy” involves identifying patients as partners in the process of treatment choice and decision-making, encouraging them to provide their opinions regarding medication use, and making patients feel they have been heard and understood. This technique emphasizes forming a therapeutic alliance with the patient to improve patients’ adherence to pharmacotherapy and optimize treatment outcomes.
Related Resources
- Haynes RB, Ackloo E, Sahota N, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;16(2);CD000011.
- Mahone IH. Shared decision making and serious mental illness. Arch Psychiatr Nurs. 2008;22(6):334-343.
- Russel CL, Ruppar TM, Metteson M. Improving medication adherence: moving from intention and motivation to a personal systems approach. Nurs Clin North Am. 2011;46(3):271-281.
- Tibaldi G, Salvador-Carulla L, Garcia-Gutierrez JC. From treatment adherence to advanced shared decision making: New professional strategies and attitudes in mental health care. Curr Clin Pharmacol. 2011;6(2):91-99.
Drug Brand Name
Clonazepam • Klonopin
Disclosure
Dr. Torem reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Psychiatric patients stand to benefit greatly from adhering to prescribed pharmacotherapy, but many patients typically do not follow their medication regimens.1,2 Three months after pharmacotherapy is initiated, approximately 50% of patients with major depressive disorder (MDD) do not take their prescribed antidepressants.3 Adherence rates in patients with schizophrenia range from 50% to 60%, and patients with bipolar disorder have adherence rates as low as 35%.4-6 One possible explanation for “treatment-resistant” depression, schizophrenia, and bipolar disorder may simply be nonadherence to prescribed pharmacotherapy.
Several strategies have been used to address this vexing problem (Table 1).7,8 They include individual and family psychoeducation,9,10 cognitive-behavioral therapy,11 interpersonal and social rhythm therapy, and family-focused therapy. This article describes an additional strategy I call “participatory pharmacotherapy.” In this model, the patient becomes a partner in the process of treatment choices and decision-making. This encourages patients to provide their own opinions and points of view regarding medication use. The prescribing clinician makes the patient feel that he or she has been listened to and understood. This and other techniques emphasize forming a therapeutic alliance with the patient before initiating pharmacotherapy. The patient provides information on his or her family history, medical and psychiatric history, and experience with previous medications, with a specific focus on which medications worked best for the patient and family members diagnosed with a similar condition.
Getting patients to participate
One of the fundamental tasks is to encourage patients to accept a participatory role, determine their underlying diagnosis, and co-create a treatment plan that will be most compatible with their illness and their personality. There are 10 components of establishing and practicing participatory pharmacotherapy.
1. Encourage patients to share their opinion of what a desirable treatment outcome should be. Some patients have unrealistic expectations about what medications can achieve. Clarify with patients what would be a realistic expectation of pharmacotherapy, and modify the patient’s beliefs to be compatible with a more probable outcome. For example, Ms. D, a 46-year-old mother of 2, is diagnosed with MDD, recurrent type without psychotic features. She states she expects pharmacotherapy will alleviate all symptoms and allow her to achieve a new healthy, happy state in which she will be able to laugh, socialize, and have fun every day for the rest of her life. Although achieving remission is a realistic and desirable treatment goal, Ms. D’s expectations are idealistic. Helping Ms. D accept and agree to realistic and achievable outcomes will improve her adherence to prescribed medications.
2. Encourage patients to share their ideas of how a desirable outcome can be accomplished. Similar to their expectations of outcomes, some patients have an unrealistic understanding of how treatment is conducted. Some patients expect treatment to be limited to prescribed medications or a one-time injection of a curative drug. Others prefer to use herbs and supplements and want to avoid prescribed medications. Understanding the patient’s expectations of how treatment is carried out will allow clinicians to provide patients with a rational view of treatment and establish a partnership based on realistic expectations.
3. Engage patients in choosing the best medication for them. Many patients have preconceived ideas about medications and which medicine would be best for them. They get this information from various sources, including family members and friends who benefitted from a specific drug, personal experience with medications, and exposure to drug advertising.
Understanding the patient’s preference for a specific medication and why he or she made such a choice is critical because doing so can take advantage of the patient’s self-fulfilling prophecies and improve the chances of obtaining a better outcome. For example, Mr. O, a 52-year-old father of 3, has been experiencing recurrent episodes of severe panic attacks. His clinician asked him to describe medications that in his opinion were most helpful in the past. He said he preferred clonazepam because it had helped him control the panic attacks and had minimal side effects, but he discontinued it after a previous psychotherapist told him he would become addicted to it. Obtaining this information was valuable because the clinician was able to clarify guidelines for clonazepam use without the risk of dependence. Mr. O is prescribed clonazepam, which he takes consistently and responds to excellently.
4. Involve patients in setting treatment goals and targeting symptoms to be relieved. Actively listen when patients describe their symptoms, discomforts, and past experiences with treatments. I invite patients to speak uninterrupted for 5 to 10 minutes, even if they talk about issues that seem irrelevant. I then summarize the patient’s major points and ask, “And what else?” After he or she says, “That’s it,” I ask the patient to assign a priority to alleviating each symptom.
For example, Ms. J, a 38-year-old married mother of 2, was diagnosed with bipolar II disorder. She listed her highest priority as controlling her impulsive shopping rather than alleviating depression, insomnia, or overeating. She had been forced to declare bankruptcy twice, and she was determined to never do so again. She also wanted to regain her husband’s trust and her ability to manage her finances. Ensuring that Ms. J felt understood regarding this issue increased the chances of establishing a solid treatment partnership. Providing Ms. J with a menu of treatment choices and asking her to describe her previous experiences with medications helped her and the clinician choose a medication that is compatible with her desire to control her impulsive shopping.
5. Engage patients in choosing the best delivery system for the prescribed medication. For many medications, clinicians can choose from a variety of delivery systems, including pills, transdermal patches, rectal or vaginal suppositories, creams, ointments, orally disintegrating tablets, liquids, and intramuscular injections. Patients have varying beliefs about the efficacy of particular delivery systems, based on personal experiences or what they have learned from the media, their family and friends, or the Internet. For example, Ms. S, age 28, experienced recurrent, disabling anxiety attacks. When asked about the best way of providing medication to relieve her symptoms, she chose gluteal injections because, as a child, her pediatrician had treated her for an unspecified illness by injecting medication in her buttock, which rapidly relieved her symptoms. This left her with the impression that injectable medications were the best therapeutic delivery system. After discussing the practicalities and availability of fast-acting medications to control panic attacks, we agreed to use orally disintegrating clonazepam, which is absorbed swiftly and provides fast symptom relief. Ms. S reported favorable results and was pleased with the process of developing this strategy with her clinician.
6. Involve patients in choosing the times and frequency of medication administration. The timing and frequency of medication administration can be used to enhance desirable therapeutic effects. For example, an antidepressant that causes sedation and somnolence could be taken at bedtime to help alleviate insomnia. Some studies have shown that taking a medication once a day improves adherence compared with taking the same medication in divided doses.13 Other patients may wish to take a medication several times a day so they can keep the medication in their purse or briefcase and feel confident that if they need a medication for immediate symptom relief, it will be readily available.
7. Teach patients to self-monitor changes and improvements in target symptoms. Engaging patients in a system of self-monitoring improves their chances of achieving successful treatment outcomes.14 Instruct patients to create a list of symptoms and monitor the intensity of each symptom using a rating scale of 1 to 5, where 1 represents the lowest intensity and 5 represents the highest. As for frequency, patients can rate each symptom from “not present” to “present most of the time.”
Self-monitoring allows patients to observe which daily behaviors and lifestyle choices make symptoms better and which make them worse. For example, Mrs. P, a 38-year-old married mother of 2, had anxiety and panic attacks associated with low self-esteem and chronic depression. Her clinician instructed her to use a 1-page form to monitor the frequency and intensity of her anxiety and panic symptoms by focusing on the physical manifestations, such as rapid heartbeat, shortness of breath, nausea, tremors, dry mouth, frequent urination, and diarrhea to see if there was any correlation between her behaviors and her symptoms.
8. Instruct patients to call you to report any changes, including minor successes. Early in my career, toward the end of each appointment after I’d prescribed medications I’d tell patients, “Please call me if you have a problem.” Frequently, patients would call with a list of problems and side effects that they believed were caused by the newly prescribed medication. Later, I realized that I may have inadvertently encouraged patients to develop problems so they would have a reason to call me. To achieve a more favorable outcome I changed the way I communicate. I now say, “Please call me next week, even if you begin to feel better with this new medication.” The phone call is now associated with the idea that they will “get better,” and internalizing such a suggestion allows patients to talk with the clinician and report favorable treatment results.
9. Tell patients to monitor their successes by relabeling and reframing their symptoms. Mr. B, age 28, has MDD and reports irritability, insomnia, short temper, and restlessness. After reviewing his desired treatment outcome, we discuss the benefits of pharmacotherapy. I tell him the new medication will improve the quality and length of his sleep, which will allow his body and mind to recharge his “internal batteries” and restore health and energy. When we discuss side effects, I tell him to expect a dry mouth, which will be his signal that the medication is working. This discussion helps patients reframe side effects and improves their ability to tolerate side effects and adhere to pharmacotherapy.
10. Harness the placebo effect and the power of suggestion to increase chances of achieving the best treatment outcomes. In a previous article,12 I reviewed the principles of recognizing and enhancing the placebo effect and the power of suggestion to improve the chances of achieving better pharmacotherapy outcomes. When practicing participatory pharmacotherapy, clinicians are consciously aware of the power embedded in their words and are careful to use language that enhances the placebo effect and the power of suggestion when prescribing medications. Use the patient’s own language as a way of pacing yourself to the patient’s description of his or her distress. For example, Ms. R, a 42-year-old mother of 3, describes her experiences seeking help for her anxiety and depression, stating that she has not yet found the right combination of medications that provide benefits with tolerable side effects. Her clinician responds by focusing on the word “yet” (pacing) stating, “even though you have not yet found the right combination of medications to provide the most desirable benefit of beginning healing and restoring your hope, I promise to work with you and together we will try to achieve an improvement in your overall health and well-being.” This response includes several positive words and suggestions of future success, which are referred to as leading.
Not all patients will respond to participatory pharmacotherapy. Some factors will make patients good candidates for this approach, and others should be considered exclusionary qualities (Table 2).
Bottom Line
“Participatory pharmacotherapy” involves identifying patients as partners in the process of treatment choice and decision-making, encouraging them to provide their opinions regarding medication use, and making patients feel they have been heard and understood. This technique emphasizes forming a therapeutic alliance with the patient to improve patients’ adherence to pharmacotherapy and optimize treatment outcomes.
Related Resources
- Haynes RB, Ackloo E, Sahota N, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;16(2);CD000011.
- Mahone IH. Shared decision making and serious mental illness. Arch Psychiatr Nurs. 2008;22(6):334-343.
- Russel CL, Ruppar TM, Metteson M. Improving medication adherence: moving from intention and motivation to a personal systems approach. Nurs Clin North Am. 2011;46(3):271-281.
- Tibaldi G, Salvador-Carulla L, Garcia-Gutierrez JC. From treatment adherence to advanced shared decision making: New professional strategies and attitudes in mental health care. Curr Clin Pharmacol. 2011;6(2):91-99.
Drug Brand Name
Clonazepam • Klonopin
Disclosure
Dr. Torem reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Zygmunt A, Olfson M, Boyer CA, et al. Interventions to improve medication adherence in schizophrenia. Am J Psychiatry. 2002;159:1653-1664.
2. Nosé M, Barbui C, Gray R, et al. Clinical interventions for treatment non-adherence in psychosis: meta-analysis. Br J Psychiatry. 2003;183:197-206.
3. Vergouwen AC, van Hout HP, Bakker A. Methods to improve patient compliance in the use of antidepressants. Ned Tijdschr Geneeskd. 2002;146:204-207.
4. Lacro JP, Dunn LB, Dolder CR, et al. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature.
J Clin Psychiatry. 2002;63:892-909.
5. Perkins DO. Predictors of noncompliance in patients with schizophrenia. J Clin Psychiatry. 2002;63:1121-1128.
6. Colom F, Vieta E, Martinez-Aran A, et al. Clinical factors associated with treatment noncompliance in euthymic bipolar patients. J Clin Psychiatry. 2000;61:549-555.
7. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487-497.
8. Osterberg LG, Rudd R. Medication adherence for antihypertensive therapy. In: Oparil S, Weber MA, eds. Hypertension: a companion to Brenner and Rector’s the kidney. 2nd ed. Philadelphia. PA: Elsevier Saunders; 2005:848.
9. Velligan DI, Weiden PJ, Sajatovic M, et al. Strategies for addressing adherence problems in patients with serious and persistent mental illness: recommendations from expert consensus guidelines. J Psychiatr Pract. 2010;16:306-324.
10. Miklowitz DJ. Adjunctive psychotherapy for bipolar disorder: state of the evidence. Am J Psychiatry. 2008; 165:1408-1419.
11. Szentagotai A, David D. The efficacy of cognitive-behavioral therapy in bipolar disorder: a quantitative meta-analysis. J Clin Psychiatry. 2010;71:66-72.
12. Torem MS. Words to the wise: 4 secrets of successful pharmacotherapy. Current Psychiatry. 2008;7(12):19-24.
13. Medic G, Higashi K, Littlewood KJ, et al. Dosing frequency and adherence in chronic psychiatric disease: systematic review and meta-analysis. Neuropsychiatr Dis Treat. 2013; 9:119-131.
14. Virdi N, Daskiran M, Nigam S, et al. The association of self-monitoring of blood glucose use with medication adherence and glycemic control in patients with type 2 diabetes initiating non-insulin treatment. Diabetes Technol Ther. 2012;14(9):790-798.
1. Zygmunt A, Olfson M, Boyer CA, et al. Interventions to improve medication adherence in schizophrenia. Am J Psychiatry. 2002;159:1653-1664.
2. Nosé M, Barbui C, Gray R, et al. Clinical interventions for treatment non-adherence in psychosis: meta-analysis. Br J Psychiatry. 2003;183:197-206.
3. Vergouwen AC, van Hout HP, Bakker A. Methods to improve patient compliance in the use of antidepressants. Ned Tijdschr Geneeskd. 2002;146:204-207.
4. Lacro JP, Dunn LB, Dolder CR, et al. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature.
J Clin Psychiatry. 2002;63:892-909.
5. Perkins DO. Predictors of noncompliance in patients with schizophrenia. J Clin Psychiatry. 2002;63:1121-1128.
6. Colom F, Vieta E, Martinez-Aran A, et al. Clinical factors associated with treatment noncompliance in euthymic bipolar patients. J Clin Psychiatry. 2000;61:549-555.
7. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487-497.
8. Osterberg LG, Rudd R. Medication adherence for antihypertensive therapy. In: Oparil S, Weber MA, eds. Hypertension: a companion to Brenner and Rector’s the kidney. 2nd ed. Philadelphia. PA: Elsevier Saunders; 2005:848.
9. Velligan DI, Weiden PJ, Sajatovic M, et al. Strategies for addressing adherence problems in patients with serious and persistent mental illness: recommendations from expert consensus guidelines. J Psychiatr Pract. 2010;16:306-324.
10. Miklowitz DJ. Adjunctive psychotherapy for bipolar disorder: state of the evidence. Am J Psychiatry. 2008; 165:1408-1419.
11. Szentagotai A, David D. The efficacy of cognitive-behavioral therapy in bipolar disorder: a quantitative meta-analysis. J Clin Psychiatry. 2010;71:66-72.
12. Torem MS. Words to the wise: 4 secrets of successful pharmacotherapy. Current Psychiatry. 2008;7(12):19-24.
13. Medic G, Higashi K, Littlewood KJ, et al. Dosing frequency and adherence in chronic psychiatric disease: systematic review and meta-analysis. Neuropsychiatr Dis Treat. 2013; 9:119-131.
14. Virdi N, Daskiran M, Nigam S, et al. The association of self-monitoring of blood glucose use with medication adherence and glycemic control in patients with type 2 diabetes initiating non-insulin treatment. Diabetes Technol Ther. 2012;14(9):790-798.
Neuropsychiatric impairment in a septic shock survivor
The effect of sepsis survivorship on cognition is a substantially under-recognized public health problem.1 Sepsis survivorship has implications for patients’ families and the health care system.2 Research has demonstrated that older patients may develop impaired cognition and functional capacity after severe sepsis3; limited evidence shows neurocognitive decline in non-geriatric patients.3 There are no reports of exacerbation of psychiatric illness after severe sepsis or septic shock, and existing literature indicates that the causative factors, epidemiology, and predisposition that may worsen psychiatric illness after septic shock are poorly defined.
Case: Sepsis-induced cognitive decline?
Following an intensive care admission for septic shock, Mr. J, age 49, presents to the outpatient behavioral medicine department with worsening mood, lethargy, agitation, suicidal ideations, hallucinations, and poor work performance for 10 months. He was diagnosed with major depressive disorder 13 years prior, but has no history of hospitalization for psychiatric illness. His depressive symptoms respond well to paroxetine, 60 mg/d. Subsequently, Mr. J becomes delusional, has intense command hallucinations, and attempts suicide, resulting in hospitalization. Neuropsychological testing reveals dementia and significant psychiatric distress, including elevated levels of depression and suicidal ideation. He is stabilized with duloxetine, 90 mg/d, and quetiapine, 50 mg/d. Two years later, Mr. J still exhibits cognitive and psychiatric disturbances.
Long-term results
The underlying mechanism of septic shock on the brain may be similar to the mechanisms that exacerbate psychiatric illnesses. This case validates the use of neuropsychological testing in septic shock survivors and encourages recognition of the effect septic shock has on neuropsychiatric illness.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers
of competing products.
References
1. Iwashyna TJ, Ely EW, Smith DM, et al. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787-1794.
2. Safdieh J. Cognition after sepsis. Neurology Alert. 2010; 29(4):30-31.
3. Williams GS. Older severe sepsis survivors are at risk for cognitive and developmental disability. Pulmonary Reviews. 2010;15(12):17-18.
The effect of sepsis survivorship on cognition is a substantially under-recognized public health problem.1 Sepsis survivorship has implications for patients’ families and the health care system.2 Research has demonstrated that older patients may develop impaired cognition and functional capacity after severe sepsis3; limited evidence shows neurocognitive decline in non-geriatric patients.3 There are no reports of exacerbation of psychiatric illness after severe sepsis or septic shock, and existing literature indicates that the causative factors, epidemiology, and predisposition that may worsen psychiatric illness after septic shock are poorly defined.
Case: Sepsis-induced cognitive decline?
Following an intensive care admission for septic shock, Mr. J, age 49, presents to the outpatient behavioral medicine department with worsening mood, lethargy, agitation, suicidal ideations, hallucinations, and poor work performance for 10 months. He was diagnosed with major depressive disorder 13 years prior, but has no history of hospitalization for psychiatric illness. His depressive symptoms respond well to paroxetine, 60 mg/d. Subsequently, Mr. J becomes delusional, has intense command hallucinations, and attempts suicide, resulting in hospitalization. Neuropsychological testing reveals dementia and significant psychiatric distress, including elevated levels of depression and suicidal ideation. He is stabilized with duloxetine, 90 mg/d, and quetiapine, 50 mg/d. Two years later, Mr. J still exhibits cognitive and psychiatric disturbances.
Long-term results
The underlying mechanism of septic shock on the brain may be similar to the mechanisms that exacerbate psychiatric illnesses. This case validates the use of neuropsychological testing in septic shock survivors and encourages recognition of the effect septic shock has on neuropsychiatric illness.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers
of competing products.
References
1. Iwashyna TJ, Ely EW, Smith DM, et al. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787-1794.
2. Safdieh J. Cognition after sepsis. Neurology Alert. 2010; 29(4):30-31.
3. Williams GS. Older severe sepsis survivors are at risk for cognitive and developmental disability. Pulmonary Reviews. 2010;15(12):17-18.
The effect of sepsis survivorship on cognition is a substantially under-recognized public health problem.1 Sepsis survivorship has implications for patients’ families and the health care system.2 Research has demonstrated that older patients may develop impaired cognition and functional capacity after severe sepsis3; limited evidence shows neurocognitive decline in non-geriatric patients.3 There are no reports of exacerbation of psychiatric illness after severe sepsis or septic shock, and existing literature indicates that the causative factors, epidemiology, and predisposition that may worsen psychiatric illness after septic shock are poorly defined.
Case: Sepsis-induced cognitive decline?
Following an intensive care admission for septic shock, Mr. J, age 49, presents to the outpatient behavioral medicine department with worsening mood, lethargy, agitation, suicidal ideations, hallucinations, and poor work performance for 10 months. He was diagnosed with major depressive disorder 13 years prior, but has no history of hospitalization for psychiatric illness. His depressive symptoms respond well to paroxetine, 60 mg/d. Subsequently, Mr. J becomes delusional, has intense command hallucinations, and attempts suicide, resulting in hospitalization. Neuropsychological testing reveals dementia and significant psychiatric distress, including elevated levels of depression and suicidal ideation. He is stabilized with duloxetine, 90 mg/d, and quetiapine, 50 mg/d. Two years later, Mr. J still exhibits cognitive and psychiatric disturbances.
Long-term results
The underlying mechanism of septic shock on the brain may be similar to the mechanisms that exacerbate psychiatric illnesses. This case validates the use of neuropsychological testing in septic shock survivors and encourages recognition of the effect septic shock has on neuropsychiatric illness.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers
of competing products.
References
1. Iwashyna TJ, Ely EW, Smith DM, et al. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787-1794.
2. Safdieh J. Cognition after sepsis. Neurology Alert. 2010; 29(4):30-31.
3. Williams GS. Older severe sepsis survivors are at risk for cognitive and developmental disability. Pulmonary Reviews. 2010;15(12):17-18.
Chronic non-cancer pain and substance use disorders: Challenges and strategies
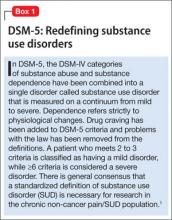
Patients with chronic non-cancer pain (CNCP) and a comorbid substance use disorder (SUD) are difficult to treat. There is a lack of high-quality clinical trials to guide management. This article focuses on current research, guidelines, and recommendations to best manage these patients. We present an analysis of recent statistics, patient characteristics, screening methods, as well as a discussion of changes to DSM-5 regarding substance abuse and addiction (Box 1).1
Opioid use and opioid-related overdoses have increased dramatically over the last decade (Box 2).2-5 Opioids are the primary medication used to treat CNCP, but their use in patients with comorbid SUDs is controversial. It is crucial for psychiatrists and other clinicians to know how to best identify, manage, and treat patients with CNCP/SUD.
Risk factors for CNCP/SUD
Evidence regarding the efficacy of screening methods to identify patients with chronic pain who are at high risk for substance misuse is insufficient. Key risk factors for developing chronic pain may include:
• elevated psychological distress
• negative beliefs and expectations about pain
• pain fear and avoidance
• disability
• anger or hostility
• maladaptive coping strategies
• catastrophic behaviors.5
In addition, these individuals may have a spouse who enables the sick role behavior.
Risk factors for developing a SUD related to prescribed opioids include:
• a history of problematic substance use
• sedative-hypnotic use
• positive family history for substance abuse
• legal problems
• heavy tobacco use
• age <50
• major depressive disorder or anxiety.5
In a review of 38 articles, Morasco et al6 found low-grade evidence with mixed results in attempt to find a correlation among sex, depression, anxiety, and tobacco use with CNCP/SUD. Other data suggest that the risk of addiction once opioids have been started increases with long refill periods and opioid morphine equivalents >120 mg.7 A history of childhood sexual abuse also may be a risk factor for chronic pain and addiction.5
Prevalence
The prevalence of opioid abuse among CNCP patients ranges from 3% to 48%; the highest rates are found among patients visiting the emergency room for opioid refills.7 These patients are more likely to exhibit aberrant behavior with their medications and may be prescribed higher opioid doses than patients who have CNCP only. Adherent CNCP/SUD patients show no difference in response to pain treatment compared with those with CNCP alone.6 Approximately 11.5% of CNCP patients taking opioids demonstrate aberrant medication use.6
Screening: Which method is best?
Data are scarce regarding the best screening methods to identify patients with CNCP/SUD. A survey of 48 patients by Moore et al8 found the combination of a clinical interview and the Screener and Opioid Assessment for Patients with Pain-Revised (SOAPP-R) is 90% sensitive in detecting CNCP/SUD. However, a systematic review by Chou et al9 found only 2 well-designed studies showing that the SOAPP-R weakly predicts future aberrant drug behavior and only 1 study showed that a high risk categorization on the Opioid Risk Tool (ORT) strongly increased the likelihood of predicting future abnormal drug-related behavior. Another well-designed study showed that the Current Opioid Misuse Measure (COMM) weakly raised the likelihood of detecting current aberrant drug behavior. No reliable data supported the efficacy of urine drug screens (UDS), pill counts, or prescription drug monitoring programs (PDMPs) for improving clinical outcomes.9 In a systematic review Starrels et al10 found only low-quality evidence supporting the effectiveness of opioid agreement contracts and UDS.
Treatment strategies
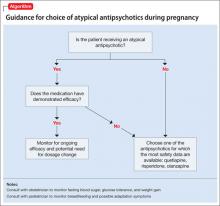
Once a patient with CNCP/SUD has been identified, it is important to categorize the severity of his (her) pain and substance use by using the decision tree (Figure) and screening tools such as SOAPP-R, ORT, and COMM. In a Veterans Administration (VA) study, only 35% of patients with an SUD received substance abuse treatment.11 The 2009 American Pain Society/American Academy of Pain Medicine guidelines recommended that opioids should considered for patients with substance abuse, serious aberrant drug-related behaviors, or psychiatric comorbidities only if frequent monitoring and treatment plan and mental health or addiction consultation were in place.12 These guidelines also recommended discontinuing opioids if repeated atypical behavior, substance abuse, diversion, lack of progress, or intolerable side effects occur. Repeated and more serious behaviors require a multidisciplinary team, expert consultation, therapy restructuring, and possibly discontinuation of opioids.12
The U.S. Office of National Drug Control Policy has created a council of federal agencies to spearhead the Prescription Drug Abuse Prevention Plan, which includes 4 major categories to reduce prescription drug abuse: education, monitoring, proper disposal, and enforcement.13 FDA commissioner Margaret Hamburg supports legislation to combine opioid education with Drug Enforcement Administration registration.14 The FDA began developing the risk evaluation and mitigation strategies in 2007 to educate physicians on proper prescribing of potentially dangerous medications.
Gourlay and Heit proposed a universal precautions method of opioid treatment for all pain patients.15 That includes:
• seeking differential diagnoses and comorbidities
• doing a baseline addiction assessment with UDS and PDMP evaluations
• obtaining informed consent for pain management
• creating pre- and post-treatment goals for pain and function
• evaluating the 4 “As” (analgesic response, increased activity, adverse events, and aberrant behavior)
• reviewing the evolution of the pain and comorbidities
• continuous documentation.5
Other helpful strategies include the Oregon’s SMART (Specific, Measurable, Action-oriented, Realistic, Time-Dependent) goal-setting, which helps physicians negotiate functional goals with patients and plan an exit strategy for those whose quality of life does not improve with opioids.5 Clinicians also can consider a sequential treatment model where patients with severe substance abuse and pain are detoxified of illicit drugs and alcohol before starting pain management. This approach is more effective if the pain is secondary to a more severe substance abuse problem that is not correlated to physical pain and acute rather than chronic.16
Psychotherapeutic interventions
In another VA study, a collaborative care intervention (CCI) combining education, self-efficacy, pain management, and feedback was not impeded by a history of SUD. The authors recommended CCI, stepped care, integrated interventions, and relapse prevention and stressed the importance of social support.17
A 10-week cognitive-behavioral therapy (CBT) program involving 44 patients enrolled in an integrated pain management program for recovering substance abusers found 50% of CNCP/SUD patients were opioid-free at 12 months.16 A combination of medication reduction and education resulted in less pain, increased functioning, decreased emotional distress, and less self-medicating. Additionally, patients reported 35% overall reduction in pain severity based on the McGill Pain Questionnaire but only 25% of patients showed a reliable improvement in their pain. Treatment changes lasted 1 year.16
A meta-analysis of psychological interventions such as CBT, behavioral treatment (BT), and self-regulated treatment (SRT) indicated that CBT and BT are moderately effective at lowering work-related disability and pain intensity for chronic low back pain alone or with multidisciplinary care and moderately lowered work-related disability. CBT had a moderate to large effect, while SRT with biofeedback and relaxation techniques had a large effect on lowering pain intensity. SRT also was shown to lower depression. Return-to-work rates were better with multidisciplinary care that included psychological interventions. These psychological interventions for chronic low back pain lowered self-reported pain, pain interference, depression, and disability while increasing quality of life; the largest effect was on pain intensity.18
A review by Williams et al19 analyzing the effects of BT and CBT on various outcome measures, including chronic pain, found small to moderate benefits for disability, mood, and catastrophic thinking with CBT, which lasted up to 6 months. Only weak improvements in pain were seen with CBT immediately after treatment. BT had a beneficial effect on catastrophic thinking but only right after treatment. CBT’s overall effect in these patients was positive, and changes lasted up to 6 months.
Pharmacologic treatments
Before and during opioid therapy, psychotherapy, physical therapy, and occupational therapy should be used with adjuvant medications appropriate to the pain condition, such as anticonvulsants (gabapentin, pregabalin, topiramate) and antidepressants including tricyclic antidepressants (amitriptyline, desipramine) and serotonin-norepinephrine reuptake inhibitors (duloxetine, venlafaxine, milnacipran).12 When considering opioids for patients with CNCP/SUD, adverse effects and safety is a primary consideration. Benzodiazepines generally should not be used with opioids because of their synergistic sedating effects.5
Opioids are misused more often by overingestion than by altering the delivery route, yet most efforts to create tamper-resistant medications has focused on
snorting or injection, which are considered more dangerous. Current tamper-resistance strategies include:
• creating a hard shell to prevent crushing and altering the medications
• chemical combinations, using agonists and antagonists such as buprenorphine combined with naloxone
• prodrugs, which become activated only in the GI system
• implants or patches.20,21
One prodrug in phase-I testing, compound PF329, becomes activated only in the GI tract by exposure to trypsin. Because it also contains trypsin inhibitors, overingestion will not lead to toxicity.20 These types of technologies may take years to develop and integrate into our therapeutic armamentarium.
If choosing opioid treatment for patients with CNCP/SUD, initially consider weak opioids such as codeine and tramadol.22 Tramadol, a partial μ agonist and weak inhibitor of serotonin and norepinephrine reuptake, is not a controlled substance and is indicated for moderate to severe pain; however, reports of its abuse potential are beginning to emerge. Tramadol has a frequency of abuse and withdrawal of approximately 2/100,000 patients taking the drug.23
Tapentadol has a dual mechanism of action—it combines a potent opioid agonist with a norepinephrine reuptake inhibitor—and is a schedule II medication. The norepinephrine and serotonin reuptake inhibition properties of tramadol and tapentadol can lead to undesired side effects and are less likely to be abused. Dart et al24 found tapentadol immediate release has the lowest abuse rate of all the opioids they studied, well below oxycodone and hydrocodone.
Methadone is a potent analgesic primarily used to treat opioid addiction, but it also is used for CNCP and cancer pain. With chronic use, methadone lacks the euphoric effect of other μ opioids; however, it can increase the QTc interval and has a long, variable half-life. As a result, methadone conversion tables are considered unreliable.
Methadone also has been associated with a disproportionate number of prescription opioid overdoses and deaths; it is present in 30% of all overdoses treated in emergency departments.4 Although methadone constitutes 5% of all opioid prescriptions in the United States, it is associated with one-third of opioid-related deaths, which is more than heroin and cocaine combined.14 Most methadone deaths occur within the first 7 days of initiating therapy, which suggests that patients were started on too high a dosage, were titrated too quickly, or had overestimated their tolerance.4 Reasons for methadone-related deaths are multifactorial and include:
• physician error and lack of knowledge
• patient nonadherence
• unanticipated comorbidities
• polypharmacy
• obstructive sleep apnea
• third-party payer policies listing it as first tier because of its low cost.4
In a Swedish study of 60 patients taking methadone, 75% had good pain relief on an average dose of 81.5 mg/d, whereas 25% had only moderate pain relief at a higher average dose of 157.5 mg/d. The authors described a methadone syndrome that included sedation, weakness, lethargy, weight gain, sweating, and sexual dysfunction, and that decreased the quality of life in 50% of patients.25 Another study found that among patients who died from sudden cardiac death and had methadone present in the toxicology screen, 45% were taking other psychotropics.26 Researchers also found a synergistic effect with benzodiazepines and an independent risk of sudden cardiac death and recommended obtaining pulmonary function tests and an electrocardiogram before starting methadone therapy, especially at higher doses.
Buprenorphine is a schedule III partial ì agonist opioid with a bell-shaped dose-response curve with a ceiling effect on respiratory depression, making it safe with an overdose. Although it is indicated for opioid dependence maintenance, it has been used off-label to treat chronic pain. It causes less euphoria than many other opioids including methadone. Buprenorphine is 25 to 50 times more potent than morphine and has a half-life of 20 to 44 hours but can be abused.27 It is available as a tablet, an injectable, and a 7-day patch. A combination of buprenorphine and naltrexone has a lower abuse potential,28 is administered sublingually and can be prescribed only by certified physicians.29 A subcutaneous implantable form of buprenorphine, which lasts 6 months, is under FDA review.30
Bottom Line
Multidisciplinary care paired with psychological interventions and a treatment plan has some evidence of efficacy in treating pain in patients with chronic non-cancer pain at high risk of substance abuse. Physician education in both pain and addiction is paramount. Frequent supervision, screening, monitoring and careful selection of medications will help physicians optimize outcomes and reduce risks.
Related Resources
- Agency Medical Directors Group. Intra-agency guideline on opioid dosing for chronic non-cancer pain. http://agencymeddirectors.wa.gov/files/opioidgdline.pdf.
- Stevenson E, Cole J, Walker R, et al. Association of chronic noncancer pain with substance abuse treatment outcomes among a community mental health center sample [published online January 3, 2013]. Addictive Disorders and their Treatment. doi: 10.1097/ADT.0b013e31827b0cd9.
Drug Brand Names
Amitriptyline • Elavil Buprenorphine • Subutex
Buprenorphine/naloxone • Suboxone Codeine • Tylenol with Codeine, others
Desipramine • Norpramin Duloxetine • Cymbalta
Gabapentin • Neurontin Methadone • Dolophine
Milnacipran • Savella Morphine • Roxanol
Oxycodone • Percolone, OxyContin Pregabalin • Lyrica
Tapentadol • Nucynta Topiramate • Topamax
Tramadol • Ultram Venlafaxine • Effexor
Hydrocodone/acetaminophen • Vicodin, Lorcet, others
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgements
The authors thank Zita Juska for her editorial assistance with this article.
Featured Audio
Mark Juska, MD, discusses strategies for treating patients with comorbid pain and substance use disorders. Dr. Juska is a Fellow, Department of Anesthesiology, Wayne State University, Detroit, Michigan.
1. Giordano J. Pain and addiction: words, meanings, actions in the age of DSM-5. Practical Pain Management. http://www.practicalpainmanagement.com/resources/ethics/pain-addiction-words-meanings-actions-age-dsm-5. November 1, 2010. Accessed May 28, 2013.
2. The Joint Commission. Facts about pain management. http://www.jointcommission.org/pain_management. Updated February 27, 2013. Accessed May 28, 2013.
3. Volkow ND, McLellan TA. Curtailing diversion and abuse of opioid analgesics without jeopardizing pain treatment. JAMA. 2011;305(13):1346-1347.
4. Webster LR, Cochella S, Dasgupta N, et al. An analysis of the root causes for opioid-related overdose deaths in the United States. Pain Med. 2011;12(suppl 2):S26-35.
5. Miotto K, Kaufman A, Kong A, et al. Managing co-occurring substance use and pain disorders. Psychiatr Clin North Am. 2012;35(2):393-410.
6. Morasco BJ, Gritzner S, Lewis L, et al. Systematic review of prevention, correlates and treatment outcomes for chronic non-cancer pain in patients with comorbid substance use disorders. Pain. 2011;152:488-497.
7. Edlund MJ, Martin BC, Fan MY, et al. Risks for opioid abuse and dependence among recipients of chronic opioid therapy: results from the TROUP Study. Drug Alcohol Depend. 2010;112(1-2):90-98.
8. Moore TM, Jones T, Browder JH, et al. A comparison of common screening methods for predicting aberrant drug-related behavior among patients receiving opioids for chronic pain management. Pain Med. 2009;10(8):1426-1433.
9. Chou R, Fanciullo GJ, Fine PG, et al. Opioids for chronic non cancer pain: prediction and identification of aberrant drug-related behaviors. A review of the evidence for an American Pain Society and American Academy of Pain Medicine clinical practice guidelines. J Pain. 2009;10(2):131-146.
10. Starrels JL, Becker WC, Alford DP, et al. Systematic review: treatment agreements and urine drug testing to reduce opioid misuse in patients with chronic pain. Ann Intern Med. 2010;152(11):712-720.
11. Morasco BJ, Duckart JP, Dobscha SK. Adherence to clinical guidelines for opioid therapy for chronic pain in patients with substance use disorder. J Gen Intern Med. 2011; 26(9):965-971.
12. Chou R, Fanciullo GJ, Fine PG, et al; American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):
113-130.
13. Office of National Drug Control Policy. Epidemic: responding to America’s prescription drug abuse crisis. http://www.whitehouse.gov/sites/default/files/ondcp/policy-and-research/rx_abuse_plan.pdf. Accessed May 28, 2013.
14. Kuehn BM. Methadone overdose deaths rise with increased prescribing for pain. JAMA. 2012;308(8):749-750.
15. Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6(2):107-112.
16. Currie SR, Hodgins DC, Crabtree A, et al. Outcome from integrated pain management treatment for recovering substance abusers. J Pain. 2003;4(2):91-100.
17. Morasco BJ, Corson K, Turk DC, et al. Association between substance use disorder status and pain-related function following 12 months of treatment in primary care patients with musculoskeletal pain. J Pain. 2011;12(3):352-359.
18. Hoffman BM, Papas RK, Chatkoff DK, et al. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol. 2007;26(1):1-9.
19. Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012;11:CD007407. doi: 10.1002/14651858.CD007407.pub3.
20. Moorman-Li R, Motycka CA, Inge LD, et al. A review of abuse-deterrent opioids for chronic nonmalignant pain. P T. 2012;37(7):412-418.
21. Stanos SP, Bruckenthal P, Barkin RL. Strategies to reduce the tampering and subsequent abuse of long-acting opioids: potential risks and benefits of formulations with physical or pharmacologic deterrents to tampering. Mayo Clinic Proc. 2012;87(7):683-694.
22. Substance Abuse and Mental Health Services Administration. Managing chronic pain in adults with or in recovery from substance use disorders. Treatment Improvement Protocol (TIP) Series 54. HHS Publication No. (SMA) 12-4671. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011.
23. Senay EC, Adams EH, Geller A, et al. Physical dependence on Ultram (tramadol hydrochloride): both opioid-like and atypical withdrawal symptoms occur. Drug Alcohol Depend. 2003;69:233-241.
24. Dart RC, Cicero TJ, Surratt HL, et al. Assessment of the abuse of tapentadol immediate release: the first 24 months. J Opioid Manag. 2012;8(6):395-402.
25. Rhodin A, Grönbladh L, Nilsson LH, et al. Methadone treatment of chronic non-malignant pain and opioid dependence—a long-term follow-up. Eur J Pain. 2006; 10(3):271-278.
26. Chuh SS, Socoteanu C, Reinier K, et al. A community-based evaluation of sudden death associated with therapeutic levels of methadone. Am J Med. 2008;121(1):66-71.
27. Drug Enforcement Administration. Buprenorphine. http://www.deadiversion.usdoj.gov/drug_chem_info/buprenorphine.pdf. Accessed June 6, 2013.
28. Gordon A, Rashiq S, Moulin DE, et al. Buprenorphine transdermal system for opioid therapy in patients with chronic low back pain. Pain Res Manag. 2010;15(3):169-178.
29. Substance Abuse and Mental Health Administration. Buprenorphine. http://buprenorphine.samhsa.gov/about.html. Accessed May 28, 2013.
30. Ling W, Casadonte P, Bigelow G, et al. Buprenorphine implants for treatment of opioid dependence: a randomized controlled trial. JAMA. 2010;304(14):1576-1583.
Patients with chronic non-cancer pain (CNCP) and a comorbid substance use disorder (SUD) are difficult to treat. There is a lack of high-quality clinical trials to guide management. This article focuses on current research, guidelines, and recommendations to best manage these patients. We present an analysis of recent statistics, patient characteristics, screening methods, as well as a discussion of changes to DSM-5 regarding substance abuse and addiction (Box 1).1
Opioid use and opioid-related overdoses have increased dramatically over the last decade (Box 2).2-5 Opioids are the primary medication used to treat CNCP, but their use in patients with comorbid SUDs is controversial. It is crucial for psychiatrists and other clinicians to know how to best identify, manage, and treat patients with CNCP/SUD.
Risk factors for CNCP/SUD
Evidence regarding the efficacy of screening methods to identify patients with chronic pain who are at high risk for substance misuse is insufficient. Key risk factors for developing chronic pain may include:
• elevated psychological distress
• negative beliefs and expectations about pain
• pain fear and avoidance
• disability
• anger or hostility
• maladaptive coping strategies
• catastrophic behaviors.5
In addition, these individuals may have a spouse who enables the sick role behavior.
Risk factors for developing a SUD related to prescribed opioids include:
• a history of problematic substance use
• sedative-hypnotic use
• positive family history for substance abuse
• legal problems
• heavy tobacco use
• age <50
• major depressive disorder or anxiety.5
In a review of 38 articles, Morasco et al6 found low-grade evidence with mixed results in attempt to find a correlation among sex, depression, anxiety, and tobacco use with CNCP/SUD. Other data suggest that the risk of addiction once opioids have been started increases with long refill periods and opioid morphine equivalents >120 mg.7 A history of childhood sexual abuse also may be a risk factor for chronic pain and addiction.5
Prevalence
The prevalence of opioid abuse among CNCP patients ranges from 3% to 48%; the highest rates are found among patients visiting the emergency room for opioid refills.7 These patients are more likely to exhibit aberrant behavior with their medications and may be prescribed higher opioid doses than patients who have CNCP only. Adherent CNCP/SUD patients show no difference in response to pain treatment compared with those with CNCP alone.6 Approximately 11.5% of CNCP patients taking opioids demonstrate aberrant medication use.6
Screening: Which method is best?
Data are scarce regarding the best screening methods to identify patients with CNCP/SUD. A survey of 48 patients by Moore et al8 found the combination of a clinical interview and the Screener and Opioid Assessment for Patients with Pain-Revised (SOAPP-R) is 90% sensitive in detecting CNCP/SUD. However, a systematic review by Chou et al9 found only 2 well-designed studies showing that the SOAPP-R weakly predicts future aberrant drug behavior and only 1 study showed that a high risk categorization on the Opioid Risk Tool (ORT) strongly increased the likelihood of predicting future abnormal drug-related behavior. Another well-designed study showed that the Current Opioid Misuse Measure (COMM) weakly raised the likelihood of detecting current aberrant drug behavior. No reliable data supported the efficacy of urine drug screens (UDS), pill counts, or prescription drug monitoring programs (PDMPs) for improving clinical outcomes.9 In a systematic review Starrels et al10 found only low-quality evidence supporting the effectiveness of opioid agreement contracts and UDS.
Treatment strategies
Once a patient with CNCP/SUD has been identified, it is important to categorize the severity of his (her) pain and substance use by using the decision tree (Figure) and screening tools such as SOAPP-R, ORT, and COMM. In a Veterans Administration (VA) study, only 35% of patients with an SUD received substance abuse treatment.11 The 2009 American Pain Society/American Academy of Pain Medicine guidelines recommended that opioids should considered for patients with substance abuse, serious aberrant drug-related behaviors, or psychiatric comorbidities only if frequent monitoring and treatment plan and mental health or addiction consultation were in place.12 These guidelines also recommended discontinuing opioids if repeated atypical behavior, substance abuse, diversion, lack of progress, or intolerable side effects occur. Repeated and more serious behaviors require a multidisciplinary team, expert consultation, therapy restructuring, and possibly discontinuation of opioids.12
The U.S. Office of National Drug Control Policy has created a council of federal agencies to spearhead the Prescription Drug Abuse Prevention Plan, which includes 4 major categories to reduce prescription drug abuse: education, monitoring, proper disposal, and enforcement.13 FDA commissioner Margaret Hamburg supports legislation to combine opioid education with Drug Enforcement Administration registration.14 The FDA began developing the risk evaluation and mitigation strategies in 2007 to educate physicians on proper prescribing of potentially dangerous medications.
Gourlay and Heit proposed a universal precautions method of opioid treatment for all pain patients.15 That includes:
• seeking differential diagnoses and comorbidities
• doing a baseline addiction assessment with UDS and PDMP evaluations
• obtaining informed consent for pain management
• creating pre- and post-treatment goals for pain and function
• evaluating the 4 “As” (analgesic response, increased activity, adverse events, and aberrant behavior)
• reviewing the evolution of the pain and comorbidities
• continuous documentation.5
Other helpful strategies include the Oregon’s SMART (Specific, Measurable, Action-oriented, Realistic, Time-Dependent) goal-setting, which helps physicians negotiate functional goals with patients and plan an exit strategy for those whose quality of life does not improve with opioids.5 Clinicians also can consider a sequential treatment model where patients with severe substance abuse and pain are detoxified of illicit drugs and alcohol before starting pain management. This approach is more effective if the pain is secondary to a more severe substance abuse problem that is not correlated to physical pain and acute rather than chronic.16
Psychotherapeutic interventions
In another VA study, a collaborative care intervention (CCI) combining education, self-efficacy, pain management, and feedback was not impeded by a history of SUD. The authors recommended CCI, stepped care, integrated interventions, and relapse prevention and stressed the importance of social support.17
A 10-week cognitive-behavioral therapy (CBT) program involving 44 patients enrolled in an integrated pain management program for recovering substance abusers found 50% of CNCP/SUD patients were opioid-free at 12 months.16 A combination of medication reduction and education resulted in less pain, increased functioning, decreased emotional distress, and less self-medicating. Additionally, patients reported 35% overall reduction in pain severity based on the McGill Pain Questionnaire but only 25% of patients showed a reliable improvement in their pain. Treatment changes lasted 1 year.16
A meta-analysis of psychological interventions such as CBT, behavioral treatment (BT), and self-regulated treatment (SRT) indicated that CBT and BT are moderately effective at lowering work-related disability and pain intensity for chronic low back pain alone or with multidisciplinary care and moderately lowered work-related disability. CBT had a moderate to large effect, while SRT with biofeedback and relaxation techniques had a large effect on lowering pain intensity. SRT also was shown to lower depression. Return-to-work rates were better with multidisciplinary care that included psychological interventions. These psychological interventions for chronic low back pain lowered self-reported pain, pain interference, depression, and disability while increasing quality of life; the largest effect was on pain intensity.18
A review by Williams et al19 analyzing the effects of BT and CBT on various outcome measures, including chronic pain, found small to moderate benefits for disability, mood, and catastrophic thinking with CBT, which lasted up to 6 months. Only weak improvements in pain were seen with CBT immediately after treatment. BT had a beneficial effect on catastrophic thinking but only right after treatment. CBT’s overall effect in these patients was positive, and changes lasted up to 6 months.
Pharmacologic treatments
Before and during opioid therapy, psychotherapy, physical therapy, and occupational therapy should be used with adjuvant medications appropriate to the pain condition, such as anticonvulsants (gabapentin, pregabalin, topiramate) and antidepressants including tricyclic antidepressants (amitriptyline, desipramine) and serotonin-norepinephrine reuptake inhibitors (duloxetine, venlafaxine, milnacipran).12 When considering opioids for patients with CNCP/SUD, adverse effects and safety is a primary consideration. Benzodiazepines generally should not be used with opioids because of their synergistic sedating effects.5
Opioids are misused more often by overingestion than by altering the delivery route, yet most efforts to create tamper-resistant medications has focused on
snorting or injection, which are considered more dangerous. Current tamper-resistance strategies include:
• creating a hard shell to prevent crushing and altering the medications
• chemical combinations, using agonists and antagonists such as buprenorphine combined with naloxone
• prodrugs, which become activated only in the GI system
• implants or patches.20,21
One prodrug in phase-I testing, compound PF329, becomes activated only in the GI tract by exposure to trypsin. Because it also contains trypsin inhibitors, overingestion will not lead to toxicity.20 These types of technologies may take years to develop and integrate into our therapeutic armamentarium.
If choosing opioid treatment for patients with CNCP/SUD, initially consider weak opioids such as codeine and tramadol.22 Tramadol, a partial μ agonist and weak inhibitor of serotonin and norepinephrine reuptake, is not a controlled substance and is indicated for moderate to severe pain; however, reports of its abuse potential are beginning to emerge. Tramadol has a frequency of abuse and withdrawal of approximately 2/100,000 patients taking the drug.23
Tapentadol has a dual mechanism of action—it combines a potent opioid agonist with a norepinephrine reuptake inhibitor—and is a schedule II medication. The norepinephrine and serotonin reuptake inhibition properties of tramadol and tapentadol can lead to undesired side effects and are less likely to be abused. Dart et al24 found tapentadol immediate release has the lowest abuse rate of all the opioids they studied, well below oxycodone and hydrocodone.
Methadone is a potent analgesic primarily used to treat opioid addiction, but it also is used for CNCP and cancer pain. With chronic use, methadone lacks the euphoric effect of other μ opioids; however, it can increase the QTc interval and has a long, variable half-life. As a result, methadone conversion tables are considered unreliable.
Methadone also has been associated with a disproportionate number of prescription opioid overdoses and deaths; it is present in 30% of all overdoses treated in emergency departments.4 Although methadone constitutes 5% of all opioid prescriptions in the United States, it is associated with one-third of opioid-related deaths, which is more than heroin and cocaine combined.14 Most methadone deaths occur within the first 7 days of initiating therapy, which suggests that patients were started on too high a dosage, were titrated too quickly, or had overestimated their tolerance.4 Reasons for methadone-related deaths are multifactorial and include:
• physician error and lack of knowledge
• patient nonadherence
• unanticipated comorbidities
• polypharmacy
• obstructive sleep apnea
• third-party payer policies listing it as first tier because of its low cost.4
In a Swedish study of 60 patients taking methadone, 75% had good pain relief on an average dose of 81.5 mg/d, whereas 25% had only moderate pain relief at a higher average dose of 157.5 mg/d. The authors described a methadone syndrome that included sedation, weakness, lethargy, weight gain, sweating, and sexual dysfunction, and that decreased the quality of life in 50% of patients.25 Another study found that among patients who died from sudden cardiac death and had methadone present in the toxicology screen, 45% were taking other psychotropics.26 Researchers also found a synergistic effect with benzodiazepines and an independent risk of sudden cardiac death and recommended obtaining pulmonary function tests and an electrocardiogram before starting methadone therapy, especially at higher doses.
Buprenorphine is a schedule III partial ì agonist opioid with a bell-shaped dose-response curve with a ceiling effect on respiratory depression, making it safe with an overdose. Although it is indicated for opioid dependence maintenance, it has been used off-label to treat chronic pain. It causes less euphoria than many other opioids including methadone. Buprenorphine is 25 to 50 times more potent than morphine and has a half-life of 20 to 44 hours but can be abused.27 It is available as a tablet, an injectable, and a 7-day patch. A combination of buprenorphine and naltrexone has a lower abuse potential,28 is administered sublingually and can be prescribed only by certified physicians.29 A subcutaneous implantable form of buprenorphine, which lasts 6 months, is under FDA review.30
Bottom Line
Multidisciplinary care paired with psychological interventions and a treatment plan has some evidence of efficacy in treating pain in patients with chronic non-cancer pain at high risk of substance abuse. Physician education in both pain and addiction is paramount. Frequent supervision, screening, monitoring and careful selection of medications will help physicians optimize outcomes and reduce risks.
Related Resources
- Agency Medical Directors Group. Intra-agency guideline on opioid dosing for chronic non-cancer pain. http://agencymeddirectors.wa.gov/files/opioidgdline.pdf.
- Stevenson E, Cole J, Walker R, et al. Association of chronic noncancer pain with substance abuse treatment outcomes among a community mental health center sample [published online January 3, 2013]. Addictive Disorders and their Treatment. doi: 10.1097/ADT.0b013e31827b0cd9.
Drug Brand Names
Amitriptyline • Elavil Buprenorphine • Subutex
Buprenorphine/naloxone • Suboxone Codeine • Tylenol with Codeine, others
Desipramine • Norpramin Duloxetine • Cymbalta
Gabapentin • Neurontin Methadone • Dolophine
Milnacipran • Savella Morphine • Roxanol
Oxycodone • Percolone, OxyContin Pregabalin • Lyrica
Tapentadol • Nucynta Topiramate • Topamax
Tramadol • Ultram Venlafaxine • Effexor
Hydrocodone/acetaminophen • Vicodin, Lorcet, others
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgements
The authors thank Zita Juska for her editorial assistance with this article.
Featured Audio
Mark Juska, MD, discusses strategies for treating patients with comorbid pain and substance use disorders. Dr. Juska is a Fellow, Department of Anesthesiology, Wayne State University, Detroit, Michigan.
Patients with chronic non-cancer pain (CNCP) and a comorbid substance use disorder (SUD) are difficult to treat. There is a lack of high-quality clinical trials to guide management. This article focuses on current research, guidelines, and recommendations to best manage these patients. We present an analysis of recent statistics, patient characteristics, screening methods, as well as a discussion of changes to DSM-5 regarding substance abuse and addiction (Box 1).1
Opioid use and opioid-related overdoses have increased dramatically over the last decade (Box 2).2-5 Opioids are the primary medication used to treat CNCP, but their use in patients with comorbid SUDs is controversial. It is crucial for psychiatrists and other clinicians to know how to best identify, manage, and treat patients with CNCP/SUD.
Risk factors for CNCP/SUD
Evidence regarding the efficacy of screening methods to identify patients with chronic pain who are at high risk for substance misuse is insufficient. Key risk factors for developing chronic pain may include:
• elevated psychological distress
• negative beliefs and expectations about pain
• pain fear and avoidance
• disability
• anger or hostility
• maladaptive coping strategies
• catastrophic behaviors.5
In addition, these individuals may have a spouse who enables the sick role behavior.
Risk factors for developing a SUD related to prescribed opioids include:
• a history of problematic substance use
• sedative-hypnotic use
• positive family history for substance abuse
• legal problems
• heavy tobacco use
• age <50
• major depressive disorder or anxiety.5
In a review of 38 articles, Morasco et al6 found low-grade evidence with mixed results in attempt to find a correlation among sex, depression, anxiety, and tobacco use with CNCP/SUD. Other data suggest that the risk of addiction once opioids have been started increases with long refill periods and opioid morphine equivalents >120 mg.7 A history of childhood sexual abuse also may be a risk factor for chronic pain and addiction.5
Prevalence
The prevalence of opioid abuse among CNCP patients ranges from 3% to 48%; the highest rates are found among patients visiting the emergency room for opioid refills.7 These patients are more likely to exhibit aberrant behavior with their medications and may be prescribed higher opioid doses than patients who have CNCP only. Adherent CNCP/SUD patients show no difference in response to pain treatment compared with those with CNCP alone.6 Approximately 11.5% of CNCP patients taking opioids demonstrate aberrant medication use.6
Screening: Which method is best?
Data are scarce regarding the best screening methods to identify patients with CNCP/SUD. A survey of 48 patients by Moore et al8 found the combination of a clinical interview and the Screener and Opioid Assessment for Patients with Pain-Revised (SOAPP-R) is 90% sensitive in detecting CNCP/SUD. However, a systematic review by Chou et al9 found only 2 well-designed studies showing that the SOAPP-R weakly predicts future aberrant drug behavior and only 1 study showed that a high risk categorization on the Opioid Risk Tool (ORT) strongly increased the likelihood of predicting future abnormal drug-related behavior. Another well-designed study showed that the Current Opioid Misuse Measure (COMM) weakly raised the likelihood of detecting current aberrant drug behavior. No reliable data supported the efficacy of urine drug screens (UDS), pill counts, or prescription drug monitoring programs (PDMPs) for improving clinical outcomes.9 In a systematic review Starrels et al10 found only low-quality evidence supporting the effectiveness of opioid agreement contracts and UDS.
Treatment strategies
Once a patient with CNCP/SUD has been identified, it is important to categorize the severity of his (her) pain and substance use by using the decision tree (Figure) and screening tools such as SOAPP-R, ORT, and COMM. In a Veterans Administration (VA) study, only 35% of patients with an SUD received substance abuse treatment.11 The 2009 American Pain Society/American Academy of Pain Medicine guidelines recommended that opioids should considered for patients with substance abuse, serious aberrant drug-related behaviors, or psychiatric comorbidities only if frequent monitoring and treatment plan and mental health or addiction consultation were in place.12 These guidelines also recommended discontinuing opioids if repeated atypical behavior, substance abuse, diversion, lack of progress, or intolerable side effects occur. Repeated and more serious behaviors require a multidisciplinary team, expert consultation, therapy restructuring, and possibly discontinuation of opioids.12
The U.S. Office of National Drug Control Policy has created a council of federal agencies to spearhead the Prescription Drug Abuse Prevention Plan, which includes 4 major categories to reduce prescription drug abuse: education, monitoring, proper disposal, and enforcement.13 FDA commissioner Margaret Hamburg supports legislation to combine opioid education with Drug Enforcement Administration registration.14 The FDA began developing the risk evaluation and mitigation strategies in 2007 to educate physicians on proper prescribing of potentially dangerous medications.
Gourlay and Heit proposed a universal precautions method of opioid treatment for all pain patients.15 That includes:
• seeking differential diagnoses and comorbidities
• doing a baseline addiction assessment with UDS and PDMP evaluations
• obtaining informed consent for pain management
• creating pre- and post-treatment goals for pain and function
• evaluating the 4 “As” (analgesic response, increased activity, adverse events, and aberrant behavior)
• reviewing the evolution of the pain and comorbidities
• continuous documentation.5
Other helpful strategies include the Oregon’s SMART (Specific, Measurable, Action-oriented, Realistic, Time-Dependent) goal-setting, which helps physicians negotiate functional goals with patients and plan an exit strategy for those whose quality of life does not improve with opioids.5 Clinicians also can consider a sequential treatment model where patients with severe substance abuse and pain are detoxified of illicit drugs and alcohol before starting pain management. This approach is more effective if the pain is secondary to a more severe substance abuse problem that is not correlated to physical pain and acute rather than chronic.16
Psychotherapeutic interventions
In another VA study, a collaborative care intervention (CCI) combining education, self-efficacy, pain management, and feedback was not impeded by a history of SUD. The authors recommended CCI, stepped care, integrated interventions, and relapse prevention and stressed the importance of social support.17
A 10-week cognitive-behavioral therapy (CBT) program involving 44 patients enrolled in an integrated pain management program for recovering substance abusers found 50% of CNCP/SUD patients were opioid-free at 12 months.16 A combination of medication reduction and education resulted in less pain, increased functioning, decreased emotional distress, and less self-medicating. Additionally, patients reported 35% overall reduction in pain severity based on the McGill Pain Questionnaire but only 25% of patients showed a reliable improvement in their pain. Treatment changes lasted 1 year.16
A meta-analysis of psychological interventions such as CBT, behavioral treatment (BT), and self-regulated treatment (SRT) indicated that CBT and BT are moderately effective at lowering work-related disability and pain intensity for chronic low back pain alone or with multidisciplinary care and moderately lowered work-related disability. CBT had a moderate to large effect, while SRT with biofeedback and relaxation techniques had a large effect on lowering pain intensity. SRT also was shown to lower depression. Return-to-work rates were better with multidisciplinary care that included psychological interventions. These psychological interventions for chronic low back pain lowered self-reported pain, pain interference, depression, and disability while increasing quality of life; the largest effect was on pain intensity.18
A review by Williams et al19 analyzing the effects of BT and CBT on various outcome measures, including chronic pain, found small to moderate benefits for disability, mood, and catastrophic thinking with CBT, which lasted up to 6 months. Only weak improvements in pain were seen with CBT immediately after treatment. BT had a beneficial effect on catastrophic thinking but only right after treatment. CBT’s overall effect in these patients was positive, and changes lasted up to 6 months.
Pharmacologic treatments
Before and during opioid therapy, psychotherapy, physical therapy, and occupational therapy should be used with adjuvant medications appropriate to the pain condition, such as anticonvulsants (gabapentin, pregabalin, topiramate) and antidepressants including tricyclic antidepressants (amitriptyline, desipramine) and serotonin-norepinephrine reuptake inhibitors (duloxetine, venlafaxine, milnacipran).12 When considering opioids for patients with CNCP/SUD, adverse effects and safety is a primary consideration. Benzodiazepines generally should not be used with opioids because of their synergistic sedating effects.5
Opioids are misused more often by overingestion than by altering the delivery route, yet most efforts to create tamper-resistant medications has focused on
snorting or injection, which are considered more dangerous. Current tamper-resistance strategies include:
• creating a hard shell to prevent crushing and altering the medications
• chemical combinations, using agonists and antagonists such as buprenorphine combined with naloxone
• prodrugs, which become activated only in the GI system
• implants or patches.20,21
One prodrug in phase-I testing, compound PF329, becomes activated only in the GI tract by exposure to trypsin. Because it also contains trypsin inhibitors, overingestion will not lead to toxicity.20 These types of technologies may take years to develop and integrate into our therapeutic armamentarium.
If choosing opioid treatment for patients with CNCP/SUD, initially consider weak opioids such as codeine and tramadol.22 Tramadol, a partial μ agonist and weak inhibitor of serotonin and norepinephrine reuptake, is not a controlled substance and is indicated for moderate to severe pain; however, reports of its abuse potential are beginning to emerge. Tramadol has a frequency of abuse and withdrawal of approximately 2/100,000 patients taking the drug.23
Tapentadol has a dual mechanism of action—it combines a potent opioid agonist with a norepinephrine reuptake inhibitor—and is a schedule II medication. The norepinephrine and serotonin reuptake inhibition properties of tramadol and tapentadol can lead to undesired side effects and are less likely to be abused. Dart et al24 found tapentadol immediate release has the lowest abuse rate of all the opioids they studied, well below oxycodone and hydrocodone.
Methadone is a potent analgesic primarily used to treat opioid addiction, but it also is used for CNCP and cancer pain. With chronic use, methadone lacks the euphoric effect of other μ opioids; however, it can increase the QTc interval and has a long, variable half-life. As a result, methadone conversion tables are considered unreliable.
Methadone also has been associated with a disproportionate number of prescription opioid overdoses and deaths; it is present in 30% of all overdoses treated in emergency departments.4 Although methadone constitutes 5% of all opioid prescriptions in the United States, it is associated with one-third of opioid-related deaths, which is more than heroin and cocaine combined.14 Most methadone deaths occur within the first 7 days of initiating therapy, which suggests that patients were started on too high a dosage, were titrated too quickly, or had overestimated their tolerance.4 Reasons for methadone-related deaths are multifactorial and include:
• physician error and lack of knowledge
• patient nonadherence
• unanticipated comorbidities
• polypharmacy
• obstructive sleep apnea
• third-party payer policies listing it as first tier because of its low cost.4
In a Swedish study of 60 patients taking methadone, 75% had good pain relief on an average dose of 81.5 mg/d, whereas 25% had only moderate pain relief at a higher average dose of 157.5 mg/d. The authors described a methadone syndrome that included sedation, weakness, lethargy, weight gain, sweating, and sexual dysfunction, and that decreased the quality of life in 50% of patients.25 Another study found that among patients who died from sudden cardiac death and had methadone present in the toxicology screen, 45% were taking other psychotropics.26 Researchers also found a synergistic effect with benzodiazepines and an independent risk of sudden cardiac death and recommended obtaining pulmonary function tests and an electrocardiogram before starting methadone therapy, especially at higher doses.
Buprenorphine is a schedule III partial ì agonist opioid with a bell-shaped dose-response curve with a ceiling effect on respiratory depression, making it safe with an overdose. Although it is indicated for opioid dependence maintenance, it has been used off-label to treat chronic pain. It causes less euphoria than many other opioids including methadone. Buprenorphine is 25 to 50 times more potent than morphine and has a half-life of 20 to 44 hours but can be abused.27 It is available as a tablet, an injectable, and a 7-day patch. A combination of buprenorphine and naltrexone has a lower abuse potential,28 is administered sublingually and can be prescribed only by certified physicians.29 A subcutaneous implantable form of buprenorphine, which lasts 6 months, is under FDA review.30
Bottom Line
Multidisciplinary care paired with psychological interventions and a treatment plan has some evidence of efficacy in treating pain in patients with chronic non-cancer pain at high risk of substance abuse. Physician education in both pain and addiction is paramount. Frequent supervision, screening, monitoring and careful selection of medications will help physicians optimize outcomes and reduce risks.
Related Resources
- Agency Medical Directors Group. Intra-agency guideline on opioid dosing for chronic non-cancer pain. http://agencymeddirectors.wa.gov/files/opioidgdline.pdf.
- Stevenson E, Cole J, Walker R, et al. Association of chronic noncancer pain with substance abuse treatment outcomes among a community mental health center sample [published online January 3, 2013]. Addictive Disorders and their Treatment. doi: 10.1097/ADT.0b013e31827b0cd9.
Drug Brand Names
Amitriptyline • Elavil Buprenorphine • Subutex
Buprenorphine/naloxone • Suboxone Codeine • Tylenol with Codeine, others
Desipramine • Norpramin Duloxetine • Cymbalta
Gabapentin • Neurontin Methadone • Dolophine
Milnacipran • Savella Morphine • Roxanol
Oxycodone • Percolone, OxyContin Pregabalin • Lyrica
Tapentadol • Nucynta Topiramate • Topamax
Tramadol • Ultram Venlafaxine • Effexor
Hydrocodone/acetaminophen • Vicodin, Lorcet, others
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgements
The authors thank Zita Juska for her editorial assistance with this article.
Featured Audio
Mark Juska, MD, discusses strategies for treating patients with comorbid pain and substance use disorders. Dr. Juska is a Fellow, Department of Anesthesiology, Wayne State University, Detroit, Michigan.
1. Giordano J. Pain and addiction: words, meanings, actions in the age of DSM-5. Practical Pain Management. http://www.practicalpainmanagement.com/resources/ethics/pain-addiction-words-meanings-actions-age-dsm-5. November 1, 2010. Accessed May 28, 2013.
2. The Joint Commission. Facts about pain management. http://www.jointcommission.org/pain_management. Updated February 27, 2013. Accessed May 28, 2013.
3. Volkow ND, McLellan TA. Curtailing diversion and abuse of opioid analgesics without jeopardizing pain treatment. JAMA. 2011;305(13):1346-1347.
4. Webster LR, Cochella S, Dasgupta N, et al. An analysis of the root causes for opioid-related overdose deaths in the United States. Pain Med. 2011;12(suppl 2):S26-35.
5. Miotto K, Kaufman A, Kong A, et al. Managing co-occurring substance use and pain disorders. Psychiatr Clin North Am. 2012;35(2):393-410.
6. Morasco BJ, Gritzner S, Lewis L, et al. Systematic review of prevention, correlates and treatment outcomes for chronic non-cancer pain in patients with comorbid substance use disorders. Pain. 2011;152:488-497.
7. Edlund MJ, Martin BC, Fan MY, et al. Risks for opioid abuse and dependence among recipients of chronic opioid therapy: results from the TROUP Study. Drug Alcohol Depend. 2010;112(1-2):90-98.
8. Moore TM, Jones T, Browder JH, et al. A comparison of common screening methods for predicting aberrant drug-related behavior among patients receiving opioids for chronic pain management. Pain Med. 2009;10(8):1426-1433.
9. Chou R, Fanciullo GJ, Fine PG, et al. Opioids for chronic non cancer pain: prediction and identification of aberrant drug-related behaviors. A review of the evidence for an American Pain Society and American Academy of Pain Medicine clinical practice guidelines. J Pain. 2009;10(2):131-146.
10. Starrels JL, Becker WC, Alford DP, et al. Systematic review: treatment agreements and urine drug testing to reduce opioid misuse in patients with chronic pain. Ann Intern Med. 2010;152(11):712-720.
11. Morasco BJ, Duckart JP, Dobscha SK. Adherence to clinical guidelines for opioid therapy for chronic pain in patients with substance use disorder. J Gen Intern Med. 2011; 26(9):965-971.
12. Chou R, Fanciullo GJ, Fine PG, et al; American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):
113-130.
13. Office of National Drug Control Policy. Epidemic: responding to America’s prescription drug abuse crisis. http://www.whitehouse.gov/sites/default/files/ondcp/policy-and-research/rx_abuse_plan.pdf. Accessed May 28, 2013.
14. Kuehn BM. Methadone overdose deaths rise with increased prescribing for pain. JAMA. 2012;308(8):749-750.
15. Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6(2):107-112.
16. Currie SR, Hodgins DC, Crabtree A, et al. Outcome from integrated pain management treatment for recovering substance abusers. J Pain. 2003;4(2):91-100.
17. Morasco BJ, Corson K, Turk DC, et al. Association between substance use disorder status and pain-related function following 12 months of treatment in primary care patients with musculoskeletal pain. J Pain. 2011;12(3):352-359.
18. Hoffman BM, Papas RK, Chatkoff DK, et al. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol. 2007;26(1):1-9.
19. Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012;11:CD007407. doi: 10.1002/14651858.CD007407.pub3.
20. Moorman-Li R, Motycka CA, Inge LD, et al. A review of abuse-deterrent opioids for chronic nonmalignant pain. P T. 2012;37(7):412-418.
21. Stanos SP, Bruckenthal P, Barkin RL. Strategies to reduce the tampering and subsequent abuse of long-acting opioids: potential risks and benefits of formulations with physical or pharmacologic deterrents to tampering. Mayo Clinic Proc. 2012;87(7):683-694.
22. Substance Abuse and Mental Health Services Administration. Managing chronic pain in adults with or in recovery from substance use disorders. Treatment Improvement Protocol (TIP) Series 54. HHS Publication No. (SMA) 12-4671. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011.
23. Senay EC, Adams EH, Geller A, et al. Physical dependence on Ultram (tramadol hydrochloride): both opioid-like and atypical withdrawal symptoms occur. Drug Alcohol Depend. 2003;69:233-241.
24. Dart RC, Cicero TJ, Surratt HL, et al. Assessment of the abuse of tapentadol immediate release: the first 24 months. J Opioid Manag. 2012;8(6):395-402.
25. Rhodin A, Grönbladh L, Nilsson LH, et al. Methadone treatment of chronic non-malignant pain and opioid dependence—a long-term follow-up. Eur J Pain. 2006; 10(3):271-278.
26. Chuh SS, Socoteanu C, Reinier K, et al. A community-based evaluation of sudden death associated with therapeutic levels of methadone. Am J Med. 2008;121(1):66-71.
27. Drug Enforcement Administration. Buprenorphine. http://www.deadiversion.usdoj.gov/drug_chem_info/buprenorphine.pdf. Accessed June 6, 2013.
28. Gordon A, Rashiq S, Moulin DE, et al. Buprenorphine transdermal system for opioid therapy in patients with chronic low back pain. Pain Res Manag. 2010;15(3):169-178.
29. Substance Abuse and Mental Health Administration. Buprenorphine. http://buprenorphine.samhsa.gov/about.html. Accessed May 28, 2013.
30. Ling W, Casadonte P, Bigelow G, et al. Buprenorphine implants for treatment of opioid dependence: a randomized controlled trial. JAMA. 2010;304(14):1576-1583.
1. Giordano J. Pain and addiction: words, meanings, actions in the age of DSM-5. Practical Pain Management. http://www.practicalpainmanagement.com/resources/ethics/pain-addiction-words-meanings-actions-age-dsm-5. November 1, 2010. Accessed May 28, 2013.
2. The Joint Commission. Facts about pain management. http://www.jointcommission.org/pain_management. Updated February 27, 2013. Accessed May 28, 2013.
3. Volkow ND, McLellan TA. Curtailing diversion and abuse of opioid analgesics without jeopardizing pain treatment. JAMA. 2011;305(13):1346-1347.
4. Webster LR, Cochella S, Dasgupta N, et al. An analysis of the root causes for opioid-related overdose deaths in the United States. Pain Med. 2011;12(suppl 2):S26-35.
5. Miotto K, Kaufman A, Kong A, et al. Managing co-occurring substance use and pain disorders. Psychiatr Clin North Am. 2012;35(2):393-410.
6. Morasco BJ, Gritzner S, Lewis L, et al. Systematic review of prevention, correlates and treatment outcomes for chronic non-cancer pain in patients with comorbid substance use disorders. Pain. 2011;152:488-497.
7. Edlund MJ, Martin BC, Fan MY, et al. Risks for opioid abuse and dependence among recipients of chronic opioid therapy: results from the TROUP Study. Drug Alcohol Depend. 2010;112(1-2):90-98.
8. Moore TM, Jones T, Browder JH, et al. A comparison of common screening methods for predicting aberrant drug-related behavior among patients receiving opioids for chronic pain management. Pain Med. 2009;10(8):1426-1433.
9. Chou R, Fanciullo GJ, Fine PG, et al. Opioids for chronic non cancer pain: prediction and identification of aberrant drug-related behaviors. A review of the evidence for an American Pain Society and American Academy of Pain Medicine clinical practice guidelines. J Pain. 2009;10(2):131-146.
10. Starrels JL, Becker WC, Alford DP, et al. Systematic review: treatment agreements and urine drug testing to reduce opioid misuse in patients with chronic pain. Ann Intern Med. 2010;152(11):712-720.
11. Morasco BJ, Duckart JP, Dobscha SK. Adherence to clinical guidelines for opioid therapy for chronic pain in patients with substance use disorder. J Gen Intern Med. 2011; 26(9):965-971.
12. Chou R, Fanciullo GJ, Fine PG, et al; American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):
113-130.
13. Office of National Drug Control Policy. Epidemic: responding to America’s prescription drug abuse crisis. http://www.whitehouse.gov/sites/default/files/ondcp/policy-and-research/rx_abuse_plan.pdf. Accessed May 28, 2013.
14. Kuehn BM. Methadone overdose deaths rise with increased prescribing for pain. JAMA. 2012;308(8):749-750.
15. Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6(2):107-112.
16. Currie SR, Hodgins DC, Crabtree A, et al. Outcome from integrated pain management treatment for recovering substance abusers. J Pain. 2003;4(2):91-100.
17. Morasco BJ, Corson K, Turk DC, et al. Association between substance use disorder status and pain-related function following 12 months of treatment in primary care patients with musculoskeletal pain. J Pain. 2011;12(3):352-359.
18. Hoffman BM, Papas RK, Chatkoff DK, et al. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol. 2007;26(1):1-9.
19. Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012;11:CD007407. doi: 10.1002/14651858.CD007407.pub3.
20. Moorman-Li R, Motycka CA, Inge LD, et al. A review of abuse-deterrent opioids for chronic nonmalignant pain. P T. 2012;37(7):412-418.
21. Stanos SP, Bruckenthal P, Barkin RL. Strategies to reduce the tampering and subsequent abuse of long-acting opioids: potential risks and benefits of formulations with physical or pharmacologic deterrents to tampering. Mayo Clinic Proc. 2012;87(7):683-694.
22. Substance Abuse and Mental Health Services Administration. Managing chronic pain in adults with or in recovery from substance use disorders. Treatment Improvement Protocol (TIP) Series 54. HHS Publication No. (SMA) 12-4671. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011.
23. Senay EC, Adams EH, Geller A, et al. Physical dependence on Ultram (tramadol hydrochloride): both opioid-like and atypical withdrawal symptoms occur. Drug Alcohol Depend. 2003;69:233-241.
24. Dart RC, Cicero TJ, Surratt HL, et al. Assessment of the abuse of tapentadol immediate release: the first 24 months. J Opioid Manag. 2012;8(6):395-402.
25. Rhodin A, Grönbladh L, Nilsson LH, et al. Methadone treatment of chronic non-malignant pain and opioid dependence—a long-term follow-up. Eur J Pain. 2006; 10(3):271-278.
26. Chuh SS, Socoteanu C, Reinier K, et al. A community-based evaluation of sudden death associated with therapeutic levels of methadone. Am J Med. 2008;121(1):66-71.
27. Drug Enforcement Administration. Buprenorphine. http://www.deadiversion.usdoj.gov/drug_chem_info/buprenorphine.pdf. Accessed June 6, 2013.
28. Gordon A, Rashiq S, Moulin DE, et al. Buprenorphine transdermal system for opioid therapy in patients with chronic low back pain. Pain Res Manag. 2010;15(3):169-178.
29. Substance Abuse and Mental Health Administration. Buprenorphine. http://buprenorphine.samhsa.gov/about.html. Accessed May 28, 2013.
30. Ling W, Casadonte P, Bigelow G, et al. Buprenorphine implants for treatment of opioid dependence: a randomized controlled trial. JAMA. 2010;304(14):1576-1583.
Atypical antipsychotics during pregnancy
Although clinicians and patients generally are cautious when prescribing or using antipsychotics during pregnancy, inadequately controlled psychiatric illness poses risks to both mother and child. Calculating the risks and benefits of antipsychotic use during pregnancy is limited by an incomplete understanding of the true effectiveness and full spectrum of risks of these medications. Ethical principles prohibit the type of rigorous research that would be needed to achieve clarity on this issue. This article reviews studies that might help guide clinicians who are considering prescribing an atypical antipsychotic to manage psychiatric illness in a pregnant woman.
Antipsychotic efficacy in pregnancy
All atypical antipsychotics available in the United States are FDA-approved for treating schizophrenia; some also have been approved for treating bipolar disorder, unipolar depression, or symptoms associated with autism (Table 1). Atypical antipsychotics frequently are used off-label for these and other categories of psychiatric illness, including unipolar depression, generalized anxiety disorder, and obsessive-compulsive disorder.
Studies of pharmacotherapy in pregnant women tend to focus more on safety rather than efficacy. Clinical decisions for an individual patient are best made based on knowledge about which medications have been effective for that patient in the past (Algorithm).
However, safety concerns in pregnancy may require modifying an existing regimen. In other cases, new symptoms arise during pregnancy and necessitate new medications. Additionally, a drug’s effectiveness may be affected by physiologic changes of pregnancy that can alter drug metabolism,1 potentially necessitating dose changes (Box 1).
Risks of treatment vs illness
Complete safety data on the use of any psychotropic medication during pregnancy are not available. To date, studies of atypical antipsychotics do not support any increased risk for congenital malformations large enough to be detected in medium-sized samples,2-4 although it is possible that there are increases in risk that are below the detection limit of these studies. Data regarding delivery outcomes are conflicting and difficult to interpret.
Several studies2-4 have yielded inconsistent results, including:
• risks for increased birth weight and large for gestational age3
• risks for low birth weight and small for gestational age2
• no significant differences from controls.4
Atypical antipsychotics increase the risk of gestational diabetes, whereas typical antipsychotics do not appear to increase this risk.4
Until recently, research has been limited by difficulties in separating the effects of treatment from the effects of psychiatric illness, which include intrauterine growth retardation, prematurity, preterm birth, low Apgar scores, and congenital defects.5 In addition, most studies address early and easily measurable outcomes such as preterm labor, birth weight, and congenital malformations. Researchers are just beginning to investigate more subtle and long-term potential behavioral effects.
Several recent studies have explored outcomes associated with antipsychotic use during pregnancy while attempting to separate the effects of treatment from those of disease (Box 2).
Data on atypicals
Aripiprazole. Case reports of aripiprazole use during pregnancy have reported difficulties including transient unexplained fetal tachycardia that required emergent caesarean section6 and transient respiratory distress.7 Several small case series were not powered to detect risks related to aripiprazole.8,9
Animal data suggest teratogenic potential at dosages 3 and 10 times the maximum recommended human dose.10,11 Two studies7,12 that measured placental transfer of aripiprazole found cord-to-maternal serum concentration ratios ranging from 0.47 to 0.63, which is similar to the ratios for quetiapine and risperidone and lower than those for olanzapine and haloperidol.13
There are insufficient data to identify risks related to aripiprazole compared with other drugs in its class, and fewer reports are available than for other atypical antipsychotics such as quetiapine and olanzapine. Placental transfer appears to be on the lower end of the spectrum for drugs in this class. Aripiprazole would be an acceptable choice for a woman who had a history of response to aripiprazole but likely would not be a first choice for a woman requiring a new medication during pregnancy.
Clozapine. In case reports, adverse effects associated with clozapine exposure during pregnancy include major malformations, gestational metabolic complications, poor pregnancy outcome, and perinatal adverse reactions. In one case, neonatal plasma clozapine concentrations were found to be twice that found in maternal plasma.14 Animal data have shown no evidence of increased teratogenicity at 2 to 4 times the maximum recommended human dosages.15 Boden et al8 found an increased risk for gestational diabetes and macrocephaly with clozapine (11 exposures). Four other series2-4,16 were underpowered to detect concerns related specifically to clozapine.
There are insufficient data to identify risks related specifically to clozapine use during pregnancy. However, the rare but severe adverse effects associated with clozapine in other patient populations—including agranulocytosis and severe constipation17—could be devastating in a pregnant patient, which suggests this medication would not be a first-line treatment.
Olanzapine. In postmarketing surveillance studies and case reports, there have been have anecdotal cases of fetal malformations related to olanzapine use during pregnancy. Several larger studies2-4,8,16 did not find higher rates of congenital malformations or any pattern of malformation types, although none were designed or powered to examine rare events. Animal data show no evidence of teratogenicity.18 A study comparing rates of placental passage of antipsychotics13 found higher rates for olanzapine than for quetiapine and risperidone, as well as higher prevalence of low birth weight and perinatal complications. A neonatal withdrawal syndrome has also been reported.19 Boden et al8 found an increased risk for gestational diabetes and macrocephaly with olanzapine.
Data suggest that olanzapine may be associated with somewhat higher rates of the adverse effects attributable to atypical antipsychotics (gestational diabetes and possibly macrocephaly), which could be related to olanzapine’s relatively higher rate of placental passage. Olanzapine could be a reasonable choice in a woman who had a history of good response to this medication, but would be lower priority than quetiapine when a new drug is indicated during pregnancy.
Quetiapine. In clinical trials, quetiapine had lower rates of placental passage compared with risperidone and olanzapine.13 One case report found only small changes in quetiapine serum levels during pregnancy.20 Prospective studies (90 exposures,8 36 exposures,2 7 exposures,16 4 exposures,3 and 4 exposures4) show no increase in fetal malformations or adverse neonatal health outcomes related to quetiapine, and manufacturer safety data reveal no teratogenic effect, although delays in fetal skeletal ossification were seen in rats and rabbits at doses comparable to the recommended human range.21
Quetiapine is a reasonable first choice when a new atypical antipsychotic is indicated for a pregnant patient.
Risperidone. Rates of placental passage of risperidone are higher compared with quetiapine.13 Postmarketing surveillance data (265 exposures22 and 10 exposures23) and prospective studies (including 72 exposures,8 49 exposures,2 51 exposures,4 16 exposures,16 and 5 exposures3) suggest risperidone has no major teratogenic effect. When malformations were present, they were similar to expected rates and types of malformations, and no specific malformation type was overrepresented. However, in some cases, researchers noted a withdrawal-emergent syndrome that included various combinations of tremors, irritability, poor feeding, and somnolence.22 Animal data are similarly reassuring, although increases in early fetal mortality and (potentially related) changes in maternal behavior have been observed in rats.24,25 A major caveat with risperidone is its propensity to cause hyperprolactinemia, which is detrimental to efforts to conceive and maintain a pregnancy.26,27
Risperidone is not associated with higher rates of adverse events in pregnancy than other atypical antipsychotics. It would not be a first choice for a woman trying to conceive or in the early stages of pregnancy, but would be a reasonable choice for a woman already well into pregnancy.
Ziprasidone. Available reports are few and generally do not report findings on ziprasidone separately.8,28 Manufacturer data includes 5 spontaneous abortions, one malformation, and one stillbirth among 57 exposures,4 and available animal data suggest significant developmental toxicity and impaired fertility.29 In pregnant rats, ziprasidone dosed as low as 0.5 times the maximum human recommended dose resulted in delayed fetal skeletal ossification, increased stillbirths, and decreased fetal weight and postnatal survival, and ziprasidone dosed as low as 0.2 times the maximum recommended human dose resulted in developmental delays and neurobehavioral impairments in offspring. In pregnant rabbits, ziprasidone dosed at 3 times the maximum recommended human dose resulted in cardiac and renal malformations.29
Although available data are too sparse to draw reliable conclusions, the small amount of human data plus animal data suggest that ziprasidone should be less preferred than other atypical antipsychotics during pregnancy.
Lurasidone. No data addressing lurasidone use in humans during pregnancy are available. Material submitted to the FDA includes no evidence of teratogenicity or embryo-fetal toxicity in rat and rabbit studies using 3 and 12 times the maximum recommended human dose (80 mg) based on a body surface area comparison.30
Asenapine. No data specifically addressing asenapine use in humans during pregnancy are available. Studies in rats and rabbits found no increase in teratogenicity, but did find increases in postimplantation loss and decreases in pup survival and weight gain with maternal doses equivalent to less than the maximum recommended human dose.31
Iloperidone. No data specifically addressing iloperidone use in humans during pregnancy are available. Animal studies of iloperidone found multiple developmental toxicities when iloperidone was administered during gestation.32 In one study, pregnant rats were given up to 26 times the maximum recommended human dose of 24 mg/d during the period of organogenesis. The highest dose caused increased early intrauterine deaths, decreased fetal weight and length, decreased fetal skeletal ossification, and increased minor fetal skeletal anomalies and variations. In a similar study using pregnant rabbits, the highest dose caused increased early intrauterine deaths and decreased fetal viability at term.
Paliperidone. In animal studies, there were no increases in fetal abnormalities when pregnant rats and rabbits were treated with up to 8 times the maximum recommended human dose of paliperidone during the period of organogenesis.33
A single case report34 measured levels of risperidone and its 9-hydroxy metabolite, paliperidone, in the breast milk of a mother who had taken risperidone during pregnancy and in the serum of her child. 9-OH-risperidone dose in breast milk was calculated as 4.7% of the weight-adjusted maternal dose, and serum levels in the infant were undetectable. No ill effects on the child were observed.
It is not possible to draw solid conclusions about atypical antipsychotics’ potential effects on human development from animal studies. Because of the lack of human data for the newer atypical antipsychotics—asenapine, iloperidone, lurasidone, paliperidone—in general these agents would not be advisable as first-line medications for treating pregnant women.
A few caveats
All atypical antipsychotics share the propensity to trigger or worsen glucose intolerance, which can have significant negative consequences in a pregnant patient. When deciding to use an atypical antipsychotic during pregnancy, blood glucose should be monitored carefully and regularly.
Because all atypical antipsychotics (except clozapine) are FDA pregnancy class C—indicating that animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks—the decision to use these medications must be based on an individualized assessment of risks and benefits. Patients and their providers together should make a fully informed decision.
There is an urgent need for larger and better-designed investigations that will be sufficiently powered to detect differences in outcomes—particularly major malformations, preterm delivery, adverse events in labor and delivery, metabolic and anthropometric effects on the newborn, and neurodevelopmental and psychiatric outcomes for individuals exposed in utero—between women without mental illness, untreated women with mental illness, and women receiving atypical antipsychotics during pregnancy. Further research into the pharmacokinetics and clinical efficacy of antipsychotics in pregnant women also would be useful. Clinicians can assist with these efforts by submitting their patient data to a pregnancy registry maintained by the Massachusetts General Hospital (see Related Resources).
Bottom Line
Treatment with atypical antipsychotics during pregnancy may increase the risk of adverse birth outcomes, but inadequately controlled mental illness also carries some degree of risk. The decision to use any atypical antipsychotic during pregnancy must be based on an individualized assessment of risks and benefits and made by the pregnant patient and her provider.
Related Resources
- Gentile S. Antipsychotic therapy during early and late pregnancy. A systematic review. Schizophr Bull. 2010;36(3):518-544. www.ncbi.nlm.nih.gov/pmc/articles/PMC2879689.
- Massachusetts General Hospital National Pregnancy Registry for Atypical Antipsychotics. www.womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry.
Drug Brand Names
Aripiprazole • Abilify Olanzapine • Zyprexa
Asenapine • Saphris Paliperidone • Invega
Clozapine • Clozaril Quetiapine • Seroquel
Haloperidol • Haldol Risperidone • Risperdal
Iloperidone • Fanapt Ziprasidone • Geodon
Lurasidone • Latuda
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Chang J, Streitman D. Physiologic adaptations to pregnancy. Neurol Clin. 2012;30(3):781-789.
2. McKenna K, Koren G, Tetelbaum M, et al. Pregnancy outcome of women using atypical antipsychotic drugs: a prospective comparative study. J Clin Psychiatry. 2005;66(4): 444-449; quiz 546.
3. Newham JJ, Thomas SH, MacRitchie K, et al. Birth weight of infants after maternal exposure to typical and atypical antipsychotics: prospective comparison study. Br J Psychiatry. 2008;192(5):333-337.
4. Reis M, Kallen B. Maternal use of antipsychotics in early pregnancy and delivery outcome. J Clin Psychopharmacol. 2008;28(3):279-288.
5. Matevosyan NR. Pregnancy and postpartum specifics in women with schizophrenia: a meta-study. Arch Gynecol Obstet. 2011;283(2):141-147.
6. Mendhekar DN, Sunder KR, Andrade C. Aripiprazole use in a pregnant schizoaffective woman. Bipolar Disord. 2006;8(3):299-300.
7. Watanabe N, Kasahara M, Sugibayashi R, et al. Perinatal use of aripiprazole: a case report. J Clin Psychopharmacol. 2011;31(3):377-379.
8. Bodén R, Lundgren M, Brandt L, et al. Antipsychotics during pregnancy: relation to fetal and maternal metabolic effects. Arch Gen Psychiatry. 2012;69(7):715-721.
9. Maáková E, Hubicˇková L. Antidepressant drug exposure during pregnancy. CZTIS small prospective study. Neuro Endocrinol Lett. 2011;32(suppl 1):53-56.
10. Bristol-Myers Squibb (Ed.). Aripiprazole: Drugdex drug evaluations, 1974-2003. Princeton, NJ: Thomson Micromedex; 2003.
11. U.S. Food and Drug Administration. FDA datasheet: Aripiprazole. http://www.accessdata.fda.gov/drugsatfda_docs/label/2004/21436slr006_abilify_lbl.pdf. Accessed April 8, 2013.
12. Nguyen T, Teoh S, Hackett LP, et al. Placental transfer of aripiprazole. Aust N Z J Psychiatry. 2011;45(6):500-501.
13. Newport DJ, Calamaras MR, DeVane CL, et al. Atypical antipsychotic administration during late pregnancy: placental passage and obstetrical outcomes. Am J Psychiatry. 2007;164(8):1214-1220.
14. Barnas C, Bergant A, Hummer M, et al. Clozapine concentrations in maternal and fetal plasma, amniotic fluid, and breast milk. Am J Psychiatry. 1994;151(6):945.
15. Clozaril [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2013.
16. Lin H, Chen I, Chen Y, et al. Maternal schizophrenia and pregnancy outcome: does the use of antipsychotics make a difference? Schizophr Res. 2010;116(1):55-60.
17. Young CR, Bowers MB Jr, Mazure CM. Management of the adverse effects of clozapine. Schizophr Bull. 1998;24(3):
381-390.
18. Zyprexa [package insert]. Indianapolis, IN: Eli Lilly and Company; 1997.
19. Gilad O, Merlob P, Stahl B, et al. Outcome of infants exposed to olanzapine during breastfeeding. Breastfeed Med. 2011;6(2):55-58.
20. Klier CM, Mossaheb N, Saria A, et al. Pharmacokinetics and elimination of quetiapine, venlafaxine, and trazodone during pregnancy and postpartum. J Clin Psychopharmacol. 2007;27(6):720-722.
21. U.S. Food and Drug Administration. FDA datasheet: quetiapine. http://www.accessdata.fda.gov/drugsatfda_docs/label/2004/20639se1-017,016_seroquel_lbl.pdf. Accessed April 11, 2013.
22. Coppola D, Russo LJ, Kwarta RF Jr, et al. Evaluating the postmarketing experience of risperidone use during pregnancy: pregnancy and neonatal outcomes. Drug Saf. 2007;30(3):247-264.
23. Mackay FJ, Wilton LV, Pearce GL, et al. The safety of risperidone: a post-marketing study on 7,684 patients. Hum Psychopharmacol. 1998;13(6):413-418.
24. Risperdal [package insert]. Titusville, NJ: Janssen Pharmaceuticals, Inc.; 2012.
25. U.S. Food and Drug Administration. FDA datasheet: risperidone. http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020272s056,020588s044,021346s033,021444s03lbl.pdf. Accessed April 11, 2013.
26. Katz E, Adashi EY. Hyperprolactinemic disorders. Clin Obstet Gynecol. 1990;33(3):622-639.
27. Davis JR. Prolactin and reproductive medicine. Curr Opin Obstet Gynecol. 2004;16(4):331-337.
28. Johnson KC, Laprairie JL, Brennan PA, et al. Prenatal antipsychotic exposure and neuromotor performance during infancy. Arch Gen Psychiatry. 2012;69(8):787-794. doi: 10.1001/archgenpsychiatry.2012.160.
29. U.S. Food and Drug Administration. FDA datasheet: ziprasidone. http://www.fda.gov/downloads/Advisory
Committees/CommitteesMeetingMaterials/Pediatric AdvisoryCommittee/UCM191883.pdf. Accessed March 15, 2013.
30. U.S. Food and Drug Administration. FDA datasheet: lurasidone. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/200603Orig1s000PharmR.pdf. Accessed March 15, 2013.
31. U.S. Food and Drug Administration. FDA datasheet: asenapine. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2009/022117s000_OtherR.pdf. Accessed March 15, 2013.
32. U.S. Food and Drug Administration. FDA datasheet: iloperidone. http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/022192lbl.pdf. Accessed March 15, 2013.
33. U.S. Food and Drug Administration. FDA datasheet: paliperidone. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021999s018lbl.pdf. Accessed March 15, 2013.
34. Weggelaar NM, Keijer WJ, Janssen PK. A case report of risperidone distribution and excretion into human milk: how to give good advice if you have not enough data available. J Clin Psychopharmacol. 2011;31(1):129-131.
Although clinicians and patients generally are cautious when prescribing or using antipsychotics during pregnancy, inadequately controlled psychiatric illness poses risks to both mother and child. Calculating the risks and benefits of antipsychotic use during pregnancy is limited by an incomplete understanding of the true effectiveness and full spectrum of risks of these medications. Ethical principles prohibit the type of rigorous research that would be needed to achieve clarity on this issue. This article reviews studies that might help guide clinicians who are considering prescribing an atypical antipsychotic to manage psychiatric illness in a pregnant woman.
Antipsychotic efficacy in pregnancy
All atypical antipsychotics available in the United States are FDA-approved for treating schizophrenia; some also have been approved for treating bipolar disorder, unipolar depression, or symptoms associated with autism (Table 1). Atypical antipsychotics frequently are used off-label for these and other categories of psychiatric illness, including unipolar depression, generalized anxiety disorder, and obsessive-compulsive disorder.
Studies of pharmacotherapy in pregnant women tend to focus more on safety rather than efficacy. Clinical decisions for an individual patient are best made based on knowledge about which medications have been effective for that patient in the past (Algorithm).
However, safety concerns in pregnancy may require modifying an existing regimen. In other cases, new symptoms arise during pregnancy and necessitate new medications. Additionally, a drug’s effectiveness may be affected by physiologic changes of pregnancy that can alter drug metabolism,1 potentially necessitating dose changes (Box 1).
Risks of treatment vs illness
Complete safety data on the use of any psychotropic medication during pregnancy are not available. To date, studies of atypical antipsychotics do not support any increased risk for congenital malformations large enough to be detected in medium-sized samples,2-4 although it is possible that there are increases in risk that are below the detection limit of these studies. Data regarding delivery outcomes are conflicting and difficult to interpret.
Several studies2-4 have yielded inconsistent results, including:
• risks for increased birth weight and large for gestational age3
• risks for low birth weight and small for gestational age2
• no significant differences from controls.4
Atypical antipsychotics increase the risk of gestational diabetes, whereas typical antipsychotics do not appear to increase this risk.4
Until recently, research has been limited by difficulties in separating the effects of treatment from the effects of psychiatric illness, which include intrauterine growth retardation, prematurity, preterm birth, low Apgar scores, and congenital defects.5 In addition, most studies address early and easily measurable outcomes such as preterm labor, birth weight, and congenital malformations. Researchers are just beginning to investigate more subtle and long-term potential behavioral effects.
Several recent studies have explored outcomes associated with antipsychotic use during pregnancy while attempting to separate the effects of treatment from those of disease (Box 2).
Data on atypicals
Aripiprazole. Case reports of aripiprazole use during pregnancy have reported difficulties including transient unexplained fetal tachycardia that required emergent caesarean section6 and transient respiratory distress.7 Several small case series were not powered to detect risks related to aripiprazole.8,9
Animal data suggest teratogenic potential at dosages 3 and 10 times the maximum recommended human dose.10,11 Two studies7,12 that measured placental transfer of aripiprazole found cord-to-maternal serum concentration ratios ranging from 0.47 to 0.63, which is similar to the ratios for quetiapine and risperidone and lower than those for olanzapine and haloperidol.13
There are insufficient data to identify risks related to aripiprazole compared with other drugs in its class, and fewer reports are available than for other atypical antipsychotics such as quetiapine and olanzapine. Placental transfer appears to be on the lower end of the spectrum for drugs in this class. Aripiprazole would be an acceptable choice for a woman who had a history of response to aripiprazole but likely would not be a first choice for a woman requiring a new medication during pregnancy.
Clozapine. In case reports, adverse effects associated with clozapine exposure during pregnancy include major malformations, gestational metabolic complications, poor pregnancy outcome, and perinatal adverse reactions. In one case, neonatal plasma clozapine concentrations were found to be twice that found in maternal plasma.14 Animal data have shown no evidence of increased teratogenicity at 2 to 4 times the maximum recommended human dosages.15 Boden et al8 found an increased risk for gestational diabetes and macrocephaly with clozapine (11 exposures). Four other series2-4,16 were underpowered to detect concerns related specifically to clozapine.
There are insufficient data to identify risks related specifically to clozapine use during pregnancy. However, the rare but severe adverse effects associated with clozapine in other patient populations—including agranulocytosis and severe constipation17—could be devastating in a pregnant patient, which suggests this medication would not be a first-line treatment.
Olanzapine. In postmarketing surveillance studies and case reports, there have been have anecdotal cases of fetal malformations related to olanzapine use during pregnancy. Several larger studies2-4,8,16 did not find higher rates of congenital malformations or any pattern of malformation types, although none were designed or powered to examine rare events. Animal data show no evidence of teratogenicity.18 A study comparing rates of placental passage of antipsychotics13 found higher rates for olanzapine than for quetiapine and risperidone, as well as higher prevalence of low birth weight and perinatal complications. A neonatal withdrawal syndrome has also been reported.19 Boden et al8 found an increased risk for gestational diabetes and macrocephaly with olanzapine.
Data suggest that olanzapine may be associated with somewhat higher rates of the adverse effects attributable to atypical antipsychotics (gestational diabetes and possibly macrocephaly), which could be related to olanzapine’s relatively higher rate of placental passage. Olanzapine could be a reasonable choice in a woman who had a history of good response to this medication, but would be lower priority than quetiapine when a new drug is indicated during pregnancy.
Quetiapine. In clinical trials, quetiapine had lower rates of placental passage compared with risperidone and olanzapine.13 One case report found only small changes in quetiapine serum levels during pregnancy.20 Prospective studies (90 exposures,8 36 exposures,2 7 exposures,16 4 exposures,3 and 4 exposures4) show no increase in fetal malformations or adverse neonatal health outcomes related to quetiapine, and manufacturer safety data reveal no teratogenic effect, although delays in fetal skeletal ossification were seen in rats and rabbits at doses comparable to the recommended human range.21
Quetiapine is a reasonable first choice when a new atypical antipsychotic is indicated for a pregnant patient.
Risperidone. Rates of placental passage of risperidone are higher compared with quetiapine.13 Postmarketing surveillance data (265 exposures22 and 10 exposures23) and prospective studies (including 72 exposures,8 49 exposures,2 51 exposures,4 16 exposures,16 and 5 exposures3) suggest risperidone has no major teratogenic effect. When malformations were present, they were similar to expected rates and types of malformations, and no specific malformation type was overrepresented. However, in some cases, researchers noted a withdrawal-emergent syndrome that included various combinations of tremors, irritability, poor feeding, and somnolence.22 Animal data are similarly reassuring, although increases in early fetal mortality and (potentially related) changes in maternal behavior have been observed in rats.24,25 A major caveat with risperidone is its propensity to cause hyperprolactinemia, which is detrimental to efforts to conceive and maintain a pregnancy.26,27
Risperidone is not associated with higher rates of adverse events in pregnancy than other atypical antipsychotics. It would not be a first choice for a woman trying to conceive or in the early stages of pregnancy, but would be a reasonable choice for a woman already well into pregnancy.
Ziprasidone. Available reports are few and generally do not report findings on ziprasidone separately.8,28 Manufacturer data includes 5 spontaneous abortions, one malformation, and one stillbirth among 57 exposures,4 and available animal data suggest significant developmental toxicity and impaired fertility.29 In pregnant rats, ziprasidone dosed as low as 0.5 times the maximum human recommended dose resulted in delayed fetal skeletal ossification, increased stillbirths, and decreased fetal weight and postnatal survival, and ziprasidone dosed as low as 0.2 times the maximum recommended human dose resulted in developmental delays and neurobehavioral impairments in offspring. In pregnant rabbits, ziprasidone dosed at 3 times the maximum recommended human dose resulted in cardiac and renal malformations.29
Although available data are too sparse to draw reliable conclusions, the small amount of human data plus animal data suggest that ziprasidone should be less preferred than other atypical antipsychotics during pregnancy.
Lurasidone. No data addressing lurasidone use in humans during pregnancy are available. Material submitted to the FDA includes no evidence of teratogenicity or embryo-fetal toxicity in rat and rabbit studies using 3 and 12 times the maximum recommended human dose (80 mg) based on a body surface area comparison.30
Asenapine. No data specifically addressing asenapine use in humans during pregnancy are available. Studies in rats and rabbits found no increase in teratogenicity, but did find increases in postimplantation loss and decreases in pup survival and weight gain with maternal doses equivalent to less than the maximum recommended human dose.31
Iloperidone. No data specifically addressing iloperidone use in humans during pregnancy are available. Animal studies of iloperidone found multiple developmental toxicities when iloperidone was administered during gestation.32 In one study, pregnant rats were given up to 26 times the maximum recommended human dose of 24 mg/d during the period of organogenesis. The highest dose caused increased early intrauterine deaths, decreased fetal weight and length, decreased fetal skeletal ossification, and increased minor fetal skeletal anomalies and variations. In a similar study using pregnant rabbits, the highest dose caused increased early intrauterine deaths and decreased fetal viability at term.
Paliperidone. In animal studies, there were no increases in fetal abnormalities when pregnant rats and rabbits were treated with up to 8 times the maximum recommended human dose of paliperidone during the period of organogenesis.33
A single case report34 measured levels of risperidone and its 9-hydroxy metabolite, paliperidone, in the breast milk of a mother who had taken risperidone during pregnancy and in the serum of her child. 9-OH-risperidone dose in breast milk was calculated as 4.7% of the weight-adjusted maternal dose, and serum levels in the infant were undetectable. No ill effects on the child were observed.
It is not possible to draw solid conclusions about atypical antipsychotics’ potential effects on human development from animal studies. Because of the lack of human data for the newer atypical antipsychotics—asenapine, iloperidone, lurasidone, paliperidone—in general these agents would not be advisable as first-line medications for treating pregnant women.
A few caveats
All atypical antipsychotics share the propensity to trigger or worsen glucose intolerance, which can have significant negative consequences in a pregnant patient. When deciding to use an atypical antipsychotic during pregnancy, blood glucose should be monitored carefully and regularly.
Because all atypical antipsychotics (except clozapine) are FDA pregnancy class C—indicating that animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks—the decision to use these medications must be based on an individualized assessment of risks and benefits. Patients and their providers together should make a fully informed decision.
There is an urgent need for larger and better-designed investigations that will be sufficiently powered to detect differences in outcomes—particularly major malformations, preterm delivery, adverse events in labor and delivery, metabolic and anthropometric effects on the newborn, and neurodevelopmental and psychiatric outcomes for individuals exposed in utero—between women without mental illness, untreated women with mental illness, and women receiving atypical antipsychotics during pregnancy. Further research into the pharmacokinetics and clinical efficacy of antipsychotics in pregnant women also would be useful. Clinicians can assist with these efforts by submitting their patient data to a pregnancy registry maintained by the Massachusetts General Hospital (see Related Resources).
Bottom Line
Treatment with atypical antipsychotics during pregnancy may increase the risk of adverse birth outcomes, but inadequately controlled mental illness also carries some degree of risk. The decision to use any atypical antipsychotic during pregnancy must be based on an individualized assessment of risks and benefits and made by the pregnant patient and her provider.
Related Resources
- Gentile S. Antipsychotic therapy during early and late pregnancy. A systematic review. Schizophr Bull. 2010;36(3):518-544. www.ncbi.nlm.nih.gov/pmc/articles/PMC2879689.
- Massachusetts General Hospital National Pregnancy Registry for Atypical Antipsychotics. www.womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry.
Drug Brand Names
Aripiprazole • Abilify Olanzapine • Zyprexa
Asenapine • Saphris Paliperidone • Invega
Clozapine • Clozaril Quetiapine • Seroquel
Haloperidol • Haldol Risperidone • Risperdal
Iloperidone • Fanapt Ziprasidone • Geodon
Lurasidone • Latuda
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Although clinicians and patients generally are cautious when prescribing or using antipsychotics during pregnancy, inadequately controlled psychiatric illness poses risks to both mother and child. Calculating the risks and benefits of antipsychotic use during pregnancy is limited by an incomplete understanding of the true effectiveness and full spectrum of risks of these medications. Ethical principles prohibit the type of rigorous research that would be needed to achieve clarity on this issue. This article reviews studies that might help guide clinicians who are considering prescribing an atypical antipsychotic to manage psychiatric illness in a pregnant woman.
Antipsychotic efficacy in pregnancy
All atypical antipsychotics available in the United States are FDA-approved for treating schizophrenia; some also have been approved for treating bipolar disorder, unipolar depression, or symptoms associated with autism (Table 1). Atypical antipsychotics frequently are used off-label for these and other categories of psychiatric illness, including unipolar depression, generalized anxiety disorder, and obsessive-compulsive disorder.
Studies of pharmacotherapy in pregnant women tend to focus more on safety rather than efficacy. Clinical decisions for an individual patient are best made based on knowledge about which medications have been effective for that patient in the past (Algorithm).
However, safety concerns in pregnancy may require modifying an existing regimen. In other cases, new symptoms arise during pregnancy and necessitate new medications. Additionally, a drug’s effectiveness may be affected by physiologic changes of pregnancy that can alter drug metabolism,1 potentially necessitating dose changes (Box 1).
Risks of treatment vs illness
Complete safety data on the use of any psychotropic medication during pregnancy are not available. To date, studies of atypical antipsychotics do not support any increased risk for congenital malformations large enough to be detected in medium-sized samples,2-4 although it is possible that there are increases in risk that are below the detection limit of these studies. Data regarding delivery outcomes are conflicting and difficult to interpret.
Several studies2-4 have yielded inconsistent results, including:
• risks for increased birth weight and large for gestational age3
• risks for low birth weight and small for gestational age2
• no significant differences from controls.4
Atypical antipsychotics increase the risk of gestational diabetes, whereas typical antipsychotics do not appear to increase this risk.4
Until recently, research has been limited by difficulties in separating the effects of treatment from the effects of psychiatric illness, which include intrauterine growth retardation, prematurity, preterm birth, low Apgar scores, and congenital defects.5 In addition, most studies address early and easily measurable outcomes such as preterm labor, birth weight, and congenital malformations. Researchers are just beginning to investigate more subtle and long-term potential behavioral effects.
Several recent studies have explored outcomes associated with antipsychotic use during pregnancy while attempting to separate the effects of treatment from those of disease (Box 2).
Data on atypicals
Aripiprazole. Case reports of aripiprazole use during pregnancy have reported difficulties including transient unexplained fetal tachycardia that required emergent caesarean section6 and transient respiratory distress.7 Several small case series were not powered to detect risks related to aripiprazole.8,9
Animal data suggest teratogenic potential at dosages 3 and 10 times the maximum recommended human dose.10,11 Two studies7,12 that measured placental transfer of aripiprazole found cord-to-maternal serum concentration ratios ranging from 0.47 to 0.63, which is similar to the ratios for quetiapine and risperidone and lower than those for olanzapine and haloperidol.13
There are insufficient data to identify risks related to aripiprazole compared with other drugs in its class, and fewer reports are available than for other atypical antipsychotics such as quetiapine and olanzapine. Placental transfer appears to be on the lower end of the spectrum for drugs in this class. Aripiprazole would be an acceptable choice for a woman who had a history of response to aripiprazole but likely would not be a first choice for a woman requiring a new medication during pregnancy.
Clozapine. In case reports, adverse effects associated with clozapine exposure during pregnancy include major malformations, gestational metabolic complications, poor pregnancy outcome, and perinatal adverse reactions. In one case, neonatal plasma clozapine concentrations were found to be twice that found in maternal plasma.14 Animal data have shown no evidence of increased teratogenicity at 2 to 4 times the maximum recommended human dosages.15 Boden et al8 found an increased risk for gestational diabetes and macrocephaly with clozapine (11 exposures). Four other series2-4,16 were underpowered to detect concerns related specifically to clozapine.
There are insufficient data to identify risks related specifically to clozapine use during pregnancy. However, the rare but severe adverse effects associated with clozapine in other patient populations—including agranulocytosis and severe constipation17—could be devastating in a pregnant patient, which suggests this medication would not be a first-line treatment.
Olanzapine. In postmarketing surveillance studies and case reports, there have been have anecdotal cases of fetal malformations related to olanzapine use during pregnancy. Several larger studies2-4,8,16 did not find higher rates of congenital malformations or any pattern of malformation types, although none were designed or powered to examine rare events. Animal data show no evidence of teratogenicity.18 A study comparing rates of placental passage of antipsychotics13 found higher rates for olanzapine than for quetiapine and risperidone, as well as higher prevalence of low birth weight and perinatal complications. A neonatal withdrawal syndrome has also been reported.19 Boden et al8 found an increased risk for gestational diabetes and macrocephaly with olanzapine.
Data suggest that olanzapine may be associated with somewhat higher rates of the adverse effects attributable to atypical antipsychotics (gestational diabetes and possibly macrocephaly), which could be related to olanzapine’s relatively higher rate of placental passage. Olanzapine could be a reasonable choice in a woman who had a history of good response to this medication, but would be lower priority than quetiapine when a new drug is indicated during pregnancy.
Quetiapine. In clinical trials, quetiapine had lower rates of placental passage compared with risperidone and olanzapine.13 One case report found only small changes in quetiapine serum levels during pregnancy.20 Prospective studies (90 exposures,8 36 exposures,2 7 exposures,16 4 exposures,3 and 4 exposures4) show no increase in fetal malformations or adverse neonatal health outcomes related to quetiapine, and manufacturer safety data reveal no teratogenic effect, although delays in fetal skeletal ossification were seen in rats and rabbits at doses comparable to the recommended human range.21
Quetiapine is a reasonable first choice when a new atypical antipsychotic is indicated for a pregnant patient.
Risperidone. Rates of placental passage of risperidone are higher compared with quetiapine.13 Postmarketing surveillance data (265 exposures22 and 10 exposures23) and prospective studies (including 72 exposures,8 49 exposures,2 51 exposures,4 16 exposures,16 and 5 exposures3) suggest risperidone has no major teratogenic effect. When malformations were present, they were similar to expected rates and types of malformations, and no specific malformation type was overrepresented. However, in some cases, researchers noted a withdrawal-emergent syndrome that included various combinations of tremors, irritability, poor feeding, and somnolence.22 Animal data are similarly reassuring, although increases in early fetal mortality and (potentially related) changes in maternal behavior have been observed in rats.24,25 A major caveat with risperidone is its propensity to cause hyperprolactinemia, which is detrimental to efforts to conceive and maintain a pregnancy.26,27
Risperidone is not associated with higher rates of adverse events in pregnancy than other atypical antipsychotics. It would not be a first choice for a woman trying to conceive or in the early stages of pregnancy, but would be a reasonable choice for a woman already well into pregnancy.
Ziprasidone. Available reports are few and generally do not report findings on ziprasidone separately.8,28 Manufacturer data includes 5 spontaneous abortions, one malformation, and one stillbirth among 57 exposures,4 and available animal data suggest significant developmental toxicity and impaired fertility.29 In pregnant rats, ziprasidone dosed as low as 0.5 times the maximum human recommended dose resulted in delayed fetal skeletal ossification, increased stillbirths, and decreased fetal weight and postnatal survival, and ziprasidone dosed as low as 0.2 times the maximum recommended human dose resulted in developmental delays and neurobehavioral impairments in offspring. In pregnant rabbits, ziprasidone dosed at 3 times the maximum recommended human dose resulted in cardiac and renal malformations.29
Although available data are too sparse to draw reliable conclusions, the small amount of human data plus animal data suggest that ziprasidone should be less preferred than other atypical antipsychotics during pregnancy.
Lurasidone. No data addressing lurasidone use in humans during pregnancy are available. Material submitted to the FDA includes no evidence of teratogenicity or embryo-fetal toxicity in rat and rabbit studies using 3 and 12 times the maximum recommended human dose (80 mg) based on a body surface area comparison.30
Asenapine. No data specifically addressing asenapine use in humans during pregnancy are available. Studies in rats and rabbits found no increase in teratogenicity, but did find increases in postimplantation loss and decreases in pup survival and weight gain with maternal doses equivalent to less than the maximum recommended human dose.31
Iloperidone. No data specifically addressing iloperidone use in humans during pregnancy are available. Animal studies of iloperidone found multiple developmental toxicities when iloperidone was administered during gestation.32 In one study, pregnant rats were given up to 26 times the maximum recommended human dose of 24 mg/d during the period of organogenesis. The highest dose caused increased early intrauterine deaths, decreased fetal weight and length, decreased fetal skeletal ossification, and increased minor fetal skeletal anomalies and variations. In a similar study using pregnant rabbits, the highest dose caused increased early intrauterine deaths and decreased fetal viability at term.
Paliperidone. In animal studies, there were no increases in fetal abnormalities when pregnant rats and rabbits were treated with up to 8 times the maximum recommended human dose of paliperidone during the period of organogenesis.33
A single case report34 measured levels of risperidone and its 9-hydroxy metabolite, paliperidone, in the breast milk of a mother who had taken risperidone during pregnancy and in the serum of her child. 9-OH-risperidone dose in breast milk was calculated as 4.7% of the weight-adjusted maternal dose, and serum levels in the infant were undetectable. No ill effects on the child were observed.
It is not possible to draw solid conclusions about atypical antipsychotics’ potential effects on human development from animal studies. Because of the lack of human data for the newer atypical antipsychotics—asenapine, iloperidone, lurasidone, paliperidone—in general these agents would not be advisable as first-line medications for treating pregnant women.
A few caveats
All atypical antipsychotics share the propensity to trigger or worsen glucose intolerance, which can have significant negative consequences in a pregnant patient. When deciding to use an atypical antipsychotic during pregnancy, blood glucose should be monitored carefully and regularly.
Because all atypical antipsychotics (except clozapine) are FDA pregnancy class C—indicating that animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks—the decision to use these medications must be based on an individualized assessment of risks and benefits. Patients and their providers together should make a fully informed decision.
There is an urgent need for larger and better-designed investigations that will be sufficiently powered to detect differences in outcomes—particularly major malformations, preterm delivery, adverse events in labor and delivery, metabolic and anthropometric effects on the newborn, and neurodevelopmental and psychiatric outcomes for individuals exposed in utero—between women without mental illness, untreated women with mental illness, and women receiving atypical antipsychotics during pregnancy. Further research into the pharmacokinetics and clinical efficacy of antipsychotics in pregnant women also would be useful. Clinicians can assist with these efforts by submitting their patient data to a pregnancy registry maintained by the Massachusetts General Hospital (see Related Resources).
Bottom Line
Treatment with atypical antipsychotics during pregnancy may increase the risk of adverse birth outcomes, but inadequately controlled mental illness also carries some degree of risk. The decision to use any atypical antipsychotic during pregnancy must be based on an individualized assessment of risks and benefits and made by the pregnant patient and her provider.
Related Resources
- Gentile S. Antipsychotic therapy during early and late pregnancy. A systematic review. Schizophr Bull. 2010;36(3):518-544. www.ncbi.nlm.nih.gov/pmc/articles/PMC2879689.
- Massachusetts General Hospital National Pregnancy Registry for Atypical Antipsychotics. www.womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry.
Drug Brand Names
Aripiprazole • Abilify Olanzapine • Zyprexa
Asenapine • Saphris Paliperidone • Invega
Clozapine • Clozaril Quetiapine • Seroquel
Haloperidol • Haldol Risperidone • Risperdal
Iloperidone • Fanapt Ziprasidone • Geodon
Lurasidone • Latuda
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Chang J, Streitman D. Physiologic adaptations to pregnancy. Neurol Clin. 2012;30(3):781-789.
2. McKenna K, Koren G, Tetelbaum M, et al. Pregnancy outcome of women using atypical antipsychotic drugs: a prospective comparative study. J Clin Psychiatry. 2005;66(4): 444-449; quiz 546.
3. Newham JJ, Thomas SH, MacRitchie K, et al. Birth weight of infants after maternal exposure to typical and atypical antipsychotics: prospective comparison study. Br J Psychiatry. 2008;192(5):333-337.
4. Reis M, Kallen B. Maternal use of antipsychotics in early pregnancy and delivery outcome. J Clin Psychopharmacol. 2008;28(3):279-288.
5. Matevosyan NR. Pregnancy and postpartum specifics in women with schizophrenia: a meta-study. Arch Gynecol Obstet. 2011;283(2):141-147.
6. Mendhekar DN, Sunder KR, Andrade C. Aripiprazole use in a pregnant schizoaffective woman. Bipolar Disord. 2006;8(3):299-300.
7. Watanabe N, Kasahara M, Sugibayashi R, et al. Perinatal use of aripiprazole: a case report. J Clin Psychopharmacol. 2011;31(3):377-379.
8. Bodén R, Lundgren M, Brandt L, et al. Antipsychotics during pregnancy: relation to fetal and maternal metabolic effects. Arch Gen Psychiatry. 2012;69(7):715-721.
9. Maáková E, Hubicˇková L. Antidepressant drug exposure during pregnancy. CZTIS small prospective study. Neuro Endocrinol Lett. 2011;32(suppl 1):53-56.
10. Bristol-Myers Squibb (Ed.). Aripiprazole: Drugdex drug evaluations, 1974-2003. Princeton, NJ: Thomson Micromedex; 2003.
11. U.S. Food and Drug Administration. FDA datasheet: Aripiprazole. http://www.accessdata.fda.gov/drugsatfda_docs/label/2004/21436slr006_abilify_lbl.pdf. Accessed April 8, 2013.
12. Nguyen T, Teoh S, Hackett LP, et al. Placental transfer of aripiprazole. Aust N Z J Psychiatry. 2011;45(6):500-501.
13. Newport DJ, Calamaras MR, DeVane CL, et al. Atypical antipsychotic administration during late pregnancy: placental passage and obstetrical outcomes. Am J Psychiatry. 2007;164(8):1214-1220.
14. Barnas C, Bergant A, Hummer M, et al. Clozapine concentrations in maternal and fetal plasma, amniotic fluid, and breast milk. Am J Psychiatry. 1994;151(6):945.
15. Clozaril [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2013.
16. Lin H, Chen I, Chen Y, et al. Maternal schizophrenia and pregnancy outcome: does the use of antipsychotics make a difference? Schizophr Res. 2010;116(1):55-60.
17. Young CR, Bowers MB Jr, Mazure CM. Management of the adverse effects of clozapine. Schizophr Bull. 1998;24(3):
381-390.
18. Zyprexa [package insert]. Indianapolis, IN: Eli Lilly and Company; 1997.
19. Gilad O, Merlob P, Stahl B, et al. Outcome of infants exposed to olanzapine during breastfeeding. Breastfeed Med. 2011;6(2):55-58.
20. Klier CM, Mossaheb N, Saria A, et al. Pharmacokinetics and elimination of quetiapine, venlafaxine, and trazodone during pregnancy and postpartum. J Clin Psychopharmacol. 2007;27(6):720-722.
21. U.S. Food and Drug Administration. FDA datasheet: quetiapine. http://www.accessdata.fda.gov/drugsatfda_docs/label/2004/20639se1-017,016_seroquel_lbl.pdf. Accessed April 11, 2013.
22. Coppola D, Russo LJ, Kwarta RF Jr, et al. Evaluating the postmarketing experience of risperidone use during pregnancy: pregnancy and neonatal outcomes. Drug Saf. 2007;30(3):247-264.
23. Mackay FJ, Wilton LV, Pearce GL, et al. The safety of risperidone: a post-marketing study on 7,684 patients. Hum Psychopharmacol. 1998;13(6):413-418.
24. Risperdal [package insert]. Titusville, NJ: Janssen Pharmaceuticals, Inc.; 2012.
25. U.S. Food and Drug Administration. FDA datasheet: risperidone. http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020272s056,020588s044,021346s033,021444s03lbl.pdf. Accessed April 11, 2013.
26. Katz E, Adashi EY. Hyperprolactinemic disorders. Clin Obstet Gynecol. 1990;33(3):622-639.
27. Davis JR. Prolactin and reproductive medicine. Curr Opin Obstet Gynecol. 2004;16(4):331-337.
28. Johnson KC, Laprairie JL, Brennan PA, et al. Prenatal antipsychotic exposure and neuromotor performance during infancy. Arch Gen Psychiatry. 2012;69(8):787-794. doi: 10.1001/archgenpsychiatry.2012.160.
29. U.S. Food and Drug Administration. FDA datasheet: ziprasidone. http://www.fda.gov/downloads/Advisory
Committees/CommitteesMeetingMaterials/Pediatric AdvisoryCommittee/UCM191883.pdf. Accessed March 15, 2013.
30. U.S. Food and Drug Administration. FDA datasheet: lurasidone. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/200603Orig1s000PharmR.pdf. Accessed March 15, 2013.
31. U.S. Food and Drug Administration. FDA datasheet: asenapine. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2009/022117s000_OtherR.pdf. Accessed March 15, 2013.
32. U.S. Food and Drug Administration. FDA datasheet: iloperidone. http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/022192lbl.pdf. Accessed March 15, 2013.
33. U.S. Food and Drug Administration. FDA datasheet: paliperidone. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021999s018lbl.pdf. Accessed March 15, 2013.
34. Weggelaar NM, Keijer WJ, Janssen PK. A case report of risperidone distribution and excretion into human milk: how to give good advice if you have not enough data available. J Clin Psychopharmacol. 2011;31(1):129-131.
1. Chang J, Streitman D. Physiologic adaptations to pregnancy. Neurol Clin. 2012;30(3):781-789.
2. McKenna K, Koren G, Tetelbaum M, et al. Pregnancy outcome of women using atypical antipsychotic drugs: a prospective comparative study. J Clin Psychiatry. 2005;66(4): 444-449; quiz 546.
3. Newham JJ, Thomas SH, MacRitchie K, et al. Birth weight of infants after maternal exposure to typical and atypical antipsychotics: prospective comparison study. Br J Psychiatry. 2008;192(5):333-337.
4. Reis M, Kallen B. Maternal use of antipsychotics in early pregnancy and delivery outcome. J Clin Psychopharmacol. 2008;28(3):279-288.
5. Matevosyan NR. Pregnancy and postpartum specifics in women with schizophrenia: a meta-study. Arch Gynecol Obstet. 2011;283(2):141-147.
6. Mendhekar DN, Sunder KR, Andrade C. Aripiprazole use in a pregnant schizoaffective woman. Bipolar Disord. 2006;8(3):299-300.
7. Watanabe N, Kasahara M, Sugibayashi R, et al. Perinatal use of aripiprazole: a case report. J Clin Psychopharmacol. 2011;31(3):377-379.
8. Bodén R, Lundgren M, Brandt L, et al. Antipsychotics during pregnancy: relation to fetal and maternal metabolic effects. Arch Gen Psychiatry. 2012;69(7):715-721.
9. Maáková E, Hubicˇková L. Antidepressant drug exposure during pregnancy. CZTIS small prospective study. Neuro Endocrinol Lett. 2011;32(suppl 1):53-56.
10. Bristol-Myers Squibb (Ed.). Aripiprazole: Drugdex drug evaluations, 1974-2003. Princeton, NJ: Thomson Micromedex; 2003.
11. U.S. Food and Drug Administration. FDA datasheet: Aripiprazole. http://www.accessdata.fda.gov/drugsatfda_docs/label/2004/21436slr006_abilify_lbl.pdf. Accessed April 8, 2013.
12. Nguyen T, Teoh S, Hackett LP, et al. Placental transfer of aripiprazole. Aust N Z J Psychiatry. 2011;45(6):500-501.
13. Newport DJ, Calamaras MR, DeVane CL, et al. Atypical antipsychotic administration during late pregnancy: placental passage and obstetrical outcomes. Am J Psychiatry. 2007;164(8):1214-1220.
14. Barnas C, Bergant A, Hummer M, et al. Clozapine concentrations in maternal and fetal plasma, amniotic fluid, and breast milk. Am J Psychiatry. 1994;151(6):945.
15. Clozaril [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2013.
16. Lin H, Chen I, Chen Y, et al. Maternal schizophrenia and pregnancy outcome: does the use of antipsychotics make a difference? Schizophr Res. 2010;116(1):55-60.
17. Young CR, Bowers MB Jr, Mazure CM. Management of the adverse effects of clozapine. Schizophr Bull. 1998;24(3):
381-390.
18. Zyprexa [package insert]. Indianapolis, IN: Eli Lilly and Company; 1997.
19. Gilad O, Merlob P, Stahl B, et al. Outcome of infants exposed to olanzapine during breastfeeding. Breastfeed Med. 2011;6(2):55-58.
20. Klier CM, Mossaheb N, Saria A, et al. Pharmacokinetics and elimination of quetiapine, venlafaxine, and trazodone during pregnancy and postpartum. J Clin Psychopharmacol. 2007;27(6):720-722.
21. U.S. Food and Drug Administration. FDA datasheet: quetiapine. http://www.accessdata.fda.gov/drugsatfda_docs/label/2004/20639se1-017,016_seroquel_lbl.pdf. Accessed April 11, 2013.
22. Coppola D, Russo LJ, Kwarta RF Jr, et al. Evaluating the postmarketing experience of risperidone use during pregnancy: pregnancy and neonatal outcomes. Drug Saf. 2007;30(3):247-264.
23. Mackay FJ, Wilton LV, Pearce GL, et al. The safety of risperidone: a post-marketing study on 7,684 patients. Hum Psychopharmacol. 1998;13(6):413-418.
24. Risperdal [package insert]. Titusville, NJ: Janssen Pharmaceuticals, Inc.; 2012.
25. U.S. Food and Drug Administration. FDA datasheet: risperidone. http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020272s056,020588s044,021346s033,021444s03lbl.pdf. Accessed April 11, 2013.
26. Katz E, Adashi EY. Hyperprolactinemic disorders. Clin Obstet Gynecol. 1990;33(3):622-639.
27. Davis JR. Prolactin and reproductive medicine. Curr Opin Obstet Gynecol. 2004;16(4):331-337.
28. Johnson KC, Laprairie JL, Brennan PA, et al. Prenatal antipsychotic exposure and neuromotor performance during infancy. Arch Gen Psychiatry. 2012;69(8):787-794. doi: 10.1001/archgenpsychiatry.2012.160.
29. U.S. Food and Drug Administration. FDA datasheet: ziprasidone. http://www.fda.gov/downloads/Advisory
Committees/CommitteesMeetingMaterials/Pediatric AdvisoryCommittee/UCM191883.pdf. Accessed March 15, 2013.
30. U.S. Food and Drug Administration. FDA datasheet: lurasidone. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/200603Orig1s000PharmR.pdf. Accessed March 15, 2013.
31. U.S. Food and Drug Administration. FDA datasheet: asenapine. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2009/022117s000_OtherR.pdf. Accessed March 15, 2013.
32. U.S. Food and Drug Administration. FDA datasheet: iloperidone. http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/022192lbl.pdf. Accessed March 15, 2013.
33. U.S. Food and Drug Administration. FDA datasheet: paliperidone. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021999s018lbl.pdf. Accessed March 15, 2013.
34. Weggelaar NM, Keijer WJ, Janssen PK. A case report of risperidone distribution and excretion into human milk: how to give good advice if you have not enough data available. J Clin Psychopharmacol. 2011;31(1):129-131.
Chronic non-cancer pain and substance use disorders
Take CAUTION in emergency and inpatient psychiatric settings
Mental health care professionals are at increased risk of being assaulted by patients, especially in emergency and inpatient settings. Less experienced clinicians are at an even higher risk: Studies estimate that up to 56% percent of psychiatric residents have been physically assaulted by a patient.1 Some researchers have examined systematic approaches to improving violence risk assessment2; however, the assessment and interview process itself poses a risk to residents and medical students. We recommend using the mnemonic CAUTION to remind clinicians about safety considerations when working in psychiatric settings.
Communication. Talking about safety should be a priority during daily rounds. Routinely ask staff and other personnel about safety concerns. In inpatient settings, post a safety board where hospital staff can record aggressive behaviors and other safety issues displayed by patients. Notify staff whenever you plan to interact with patients at risk for aggression or when a patient seems agitated.
Attire. Follow proper dress codes to ensure personal safety and improve your ability to quickly assist others in need. Avoid wearing necklaces, ties, and high heels in inpatient psychiatric units. Valuable accessories (eg, expensive wrist watches) should not be worn because they may be broken during a “take down.”
Untreated symptoms. Be aware of patients with untreated or undertreated symptoms, including psychosis or substance intoxication. Emergency room patients or newly admitted inpatients often present the greatest risk because of their untreated symptoms (eg, patients with paranoid delusions).
Threats. Patients who express threats are at significantly increased risk of assaulting someone.3 Patients who have recently voiced threats should not be engaged alone or without adequate staff support. Inform all residents and students about specific patients who have voiced threats. Agitated and threatening patients can pose a risk to everyone in the unit, regardless of whether they have worked directly with the clinician.
Impulsivity. Approach impulsive and aggressive patients with particular caution. Until the aggression is controlled, these patients are at risk for sudden assaults when they feel provoked. Warning signs include punching a wall or breaking objects on the unit, facial muscle tightening, clenching of fists, and pacing. If a patient does not respond to redirection from staff, he or she may require seclusion, emergency medications, or both.
Options. Whenever possible, provide patients with choices, especially when a patient requests discharge or demands a particular medication. Avoid taking an authoritarian stance by clarifying reasons why the patient’s requests are being denied and by providing alternatives and options. For instance, if discharge is not indicated, direct a patient to contact the patients’ rights advocate. You also can give some agitated patients the option of taking a voluntary “timeout” or going to an isolated area to calm down.
Navigate safely. Identify potential exits from the room before the encounter. Residents and medical students should have a clear understanding of where to escape from a potential assault. Also, it is important to point out to patients where the door is should they feel threatened. Do not block the door when interviewing paranoid patients.
We suggest that less experienced clinicians refer to this mnemonic before starting work in emergency and inpatient psychiatric settings. Safety is an important consideration. By considering these basic concepts, we believe that safety can be improved.
1. Antonius D, Fuchs L, Herbert F, et al. Psychiatric assessment of aggressive patients: a violent attack on a resident. Am J Psychiatry. 2010;167(3):253-259.
2.Teo AR, Holley SR, Leary M, et al. The relationship between level of training and accuracy of violence risk assessment. Psychiatr Serv. 2012;63(11):1089-1094.
3. Maier GJ. Managing threatening behavior: the role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
Mental health care professionals are at increased risk of being assaulted by patients, especially in emergency and inpatient settings. Less experienced clinicians are at an even higher risk: Studies estimate that up to 56% percent of psychiatric residents have been physically assaulted by a patient.1 Some researchers have examined systematic approaches to improving violence risk assessment2; however, the assessment and interview process itself poses a risk to residents and medical students. We recommend using the mnemonic CAUTION to remind clinicians about safety considerations when working in psychiatric settings.
Communication. Talking about safety should be a priority during daily rounds. Routinely ask staff and other personnel about safety concerns. In inpatient settings, post a safety board where hospital staff can record aggressive behaviors and other safety issues displayed by patients. Notify staff whenever you plan to interact with patients at risk for aggression or when a patient seems agitated.
Attire. Follow proper dress codes to ensure personal safety and improve your ability to quickly assist others in need. Avoid wearing necklaces, ties, and high heels in inpatient psychiatric units. Valuable accessories (eg, expensive wrist watches) should not be worn because they may be broken during a “take down.”
Untreated symptoms. Be aware of patients with untreated or undertreated symptoms, including psychosis or substance intoxication. Emergency room patients or newly admitted inpatients often present the greatest risk because of their untreated symptoms (eg, patients with paranoid delusions).
Threats. Patients who express threats are at significantly increased risk of assaulting someone.3 Patients who have recently voiced threats should not be engaged alone or without adequate staff support. Inform all residents and students about specific patients who have voiced threats. Agitated and threatening patients can pose a risk to everyone in the unit, regardless of whether they have worked directly with the clinician.
Impulsivity. Approach impulsive and aggressive patients with particular caution. Until the aggression is controlled, these patients are at risk for sudden assaults when they feel provoked. Warning signs include punching a wall or breaking objects on the unit, facial muscle tightening, clenching of fists, and pacing. If a patient does not respond to redirection from staff, he or she may require seclusion, emergency medications, or both.
Options. Whenever possible, provide patients with choices, especially when a patient requests discharge or demands a particular medication. Avoid taking an authoritarian stance by clarifying reasons why the patient’s requests are being denied and by providing alternatives and options. For instance, if discharge is not indicated, direct a patient to contact the patients’ rights advocate. You also can give some agitated patients the option of taking a voluntary “timeout” or going to an isolated area to calm down.
Navigate safely. Identify potential exits from the room before the encounter. Residents and medical students should have a clear understanding of where to escape from a potential assault. Also, it is important to point out to patients where the door is should they feel threatened. Do not block the door when interviewing paranoid patients.
We suggest that less experienced clinicians refer to this mnemonic before starting work in emergency and inpatient psychiatric settings. Safety is an important consideration. By considering these basic concepts, we believe that safety can be improved.
Mental health care professionals are at increased risk of being assaulted by patients, especially in emergency and inpatient settings. Less experienced clinicians are at an even higher risk: Studies estimate that up to 56% percent of psychiatric residents have been physically assaulted by a patient.1 Some researchers have examined systematic approaches to improving violence risk assessment2; however, the assessment and interview process itself poses a risk to residents and medical students. We recommend using the mnemonic CAUTION to remind clinicians about safety considerations when working in psychiatric settings.
Communication. Talking about safety should be a priority during daily rounds. Routinely ask staff and other personnel about safety concerns. In inpatient settings, post a safety board where hospital staff can record aggressive behaviors and other safety issues displayed by patients. Notify staff whenever you plan to interact with patients at risk for aggression or when a patient seems agitated.
Attire. Follow proper dress codes to ensure personal safety and improve your ability to quickly assist others in need. Avoid wearing necklaces, ties, and high heels in inpatient psychiatric units. Valuable accessories (eg, expensive wrist watches) should not be worn because they may be broken during a “take down.”
Untreated symptoms. Be aware of patients with untreated or undertreated symptoms, including psychosis or substance intoxication. Emergency room patients or newly admitted inpatients often present the greatest risk because of their untreated symptoms (eg, patients with paranoid delusions).
Threats. Patients who express threats are at significantly increased risk of assaulting someone.3 Patients who have recently voiced threats should not be engaged alone or without adequate staff support. Inform all residents and students about specific patients who have voiced threats. Agitated and threatening patients can pose a risk to everyone in the unit, regardless of whether they have worked directly with the clinician.
Impulsivity. Approach impulsive and aggressive patients with particular caution. Until the aggression is controlled, these patients are at risk for sudden assaults when they feel provoked. Warning signs include punching a wall or breaking objects on the unit, facial muscle tightening, clenching of fists, and pacing. If a patient does not respond to redirection from staff, he or she may require seclusion, emergency medications, or both.
Options. Whenever possible, provide patients with choices, especially when a patient requests discharge or demands a particular medication. Avoid taking an authoritarian stance by clarifying reasons why the patient’s requests are being denied and by providing alternatives and options. For instance, if discharge is not indicated, direct a patient to contact the patients’ rights advocate. You also can give some agitated patients the option of taking a voluntary “timeout” or going to an isolated area to calm down.
Navigate safely. Identify potential exits from the room before the encounter. Residents and medical students should have a clear understanding of where to escape from a potential assault. Also, it is important to point out to patients where the door is should they feel threatened. Do not block the door when interviewing paranoid patients.
We suggest that less experienced clinicians refer to this mnemonic before starting work in emergency and inpatient psychiatric settings. Safety is an important consideration. By considering these basic concepts, we believe that safety can be improved.
1. Antonius D, Fuchs L, Herbert F, et al. Psychiatric assessment of aggressive patients: a violent attack on a resident. Am J Psychiatry. 2010;167(3):253-259.
2.Teo AR, Holley SR, Leary M, et al. The relationship between level of training and accuracy of violence risk assessment. Psychiatr Serv. 2012;63(11):1089-1094.
3. Maier GJ. Managing threatening behavior: the role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
1. Antonius D, Fuchs L, Herbert F, et al. Psychiatric assessment of aggressive patients: a violent attack on a resident. Am J Psychiatry. 2010;167(3):253-259.
2.Teo AR, Holley SR, Leary M, et al. The relationship between level of training and accuracy of violence risk assessment. Psychiatr Serv. 2012;63(11):1089-1094.
3. Maier GJ. Managing threatening behavior: the role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
Anxiety during pregnancy
Haloperidol clearly is neurotoxic. Should it be banned?
Few medications remain in use 50 years after they were launched. Advances in drug development often render older drugs obsolete because newer drugs are more efficacious or safer, or both. Consider reserpine: Nowadays, no internist would use this drug to treat hypertension, even though it was the top-selling antihypertensive 50 years ago. Why? The adverse effects profile is no longer acceptable, with safer alternatives available.
Astonishingly, almost all first-generation psychotropics discovered 5 decades ago (neuroleptics, tricyclic antidepressants, monoamine oxidase inhibitors) are still on the formularies of most health care facilities and are used by many clinicians, especially those working with managed care organizations. Jails and prisons in the United States, where hundreds of thousands of seriously mentally ill patients are incarcerated, also use 50-year-old agents, without regard to the downside of older drugs on the body, brain, and quality of life of those incarcerated medically ill patients.
If clinicians who use these decades-old drugs were to keep up with medical research and advances in knowledge, we would realize what a travesty it is to use a brain-unfriendly drug such as haloperidol when we have many safer alternatives. A massive volume of knowledge has emerged over the past 15 years about the neurotoxicity of older neuroleptics, especially haloperidol—knowledge that was completely unknown before.a Second-generation antipsychotics have been shown to be much safer for the brain than their older-generation counterparts (although they are not more efficacious).
Changing awareness and changing practice
I used haloperidol for 20 years, and can vouch for its unquestionable efficacy in treating delusions and hallucinations. But I have avoided using it over the past 15 years, as the neuroscience literature about its harmful effects on brain tissue emerged and multiplied.
In addition, I came to realize that most psychiatric practitioners were unaware of the alarming deleterious neurologic effects of haloperidol—largely because the studies that reported those effects were published in neuroscience journals rarely read by practicing psychiatrists and nurse practitioners, and the pharmacists in charge of drug formularies at hospitals.
Evidence for the grave neurotoxicity of haloperidol and other older neuroleptics, compared with atypical antipsychotics, is substantial and multifaceted. The FDA would never approve haloperidol today, given the serious harm it can do to the brain, despite its efficacy for psychosis. (It’s interesting how the FDA bans a drug immediately if it causes tragic birth defects, such as thalidomide, but not if a drug is destructive to the brain tissue of a disabled adult patient. Invisible damage can be less alarming or urgent than visible damage.)
Twenty-eight studies reporting the various destructive effects of older antipsychotics (especially haloperidol) on brain tissue have been published in prominent neuroscience journals, based on work in animal models, cell culture, and post-mortem human tissue. Multiple molecular mechanisms, pathways, and cascades are involved, eventuating in neuronal death. The first review and discussion of these 28 neurotoxicity studies was presented at the annual meetings of the Society of Biological Psychiatry1 and the American Psychiatric Association2; a manuscript will soon be submitted for publication. See the bibliography below for a list of the 28 published studies.
The molecular mechanisms of neurotoxicity of older-generation antipsychotics, including haloperidol, fall into several major categories:
• apoptosis
• necrosis
• decreased cell viability
• inhibition of cell growth
• increased caspase activity (the “death spiral”)
• impaired glutamate transport
• mitochondrial damage.
Examples of specific mechanisms of neurotoxicity among older-generation antipsychotics appear in this Table.
With this massive evidence of the serious neurotoxic effects of haloperidol, should it be banned? The risks of the drug far exceed the benefits—especially given the availability of 9 atypical antipsychotics that have been shown to exert neuroprotective properties, such as inducing neurogenesis and increasing neurotrophic factors.3 One of our foremost duties as medical professionals is to protect patients from harmful treatments that could exacerbate their disability. It’s time to retire this aging neuroleptic.
1. Nasrallah HA, Rush SJ. First generation antipsychotics are neurotoxic and impair neuroplasticity via multiple mechanisms. Biol Psychiatry. 2013;73:61S.
2. Rush SJ, Nasrallah HA. Neurotoxic effects of the older antipsychotics: a review of several molecular mechanisms of action. Paper presented at: American Psychiatric Association Annual Meeting; May 18-22, 2013; San Francisco, CA.
3. Nandra KS, Agius M. The difference between typical and atypical antipsychotics: the effects on neurogenesis. Psychiatria Danub. 2012;24(supp1):95-99.
Few medications remain in use 50 years after they were launched. Advances in drug development often render older drugs obsolete because newer drugs are more efficacious or safer, or both. Consider reserpine: Nowadays, no internist would use this drug to treat hypertension, even though it was the top-selling antihypertensive 50 years ago. Why? The adverse effects profile is no longer acceptable, with safer alternatives available.
Astonishingly, almost all first-generation psychotropics discovered 5 decades ago (neuroleptics, tricyclic antidepressants, monoamine oxidase inhibitors) are still on the formularies of most health care facilities and are used by many clinicians, especially those working with managed care organizations. Jails and prisons in the United States, where hundreds of thousands of seriously mentally ill patients are incarcerated, also use 50-year-old agents, without regard to the downside of older drugs on the body, brain, and quality of life of those incarcerated medically ill patients.
If clinicians who use these decades-old drugs were to keep up with medical research and advances in knowledge, we would realize what a travesty it is to use a brain-unfriendly drug such as haloperidol when we have many safer alternatives. A massive volume of knowledge has emerged over the past 15 years about the neurotoxicity of older neuroleptics, especially haloperidol—knowledge that was completely unknown before.a Second-generation antipsychotics have been shown to be much safer for the brain than their older-generation counterparts (although they are not more efficacious).
Changing awareness and changing practice
I used haloperidol for 20 years, and can vouch for its unquestionable efficacy in treating delusions and hallucinations. But I have avoided using it over the past 15 years, as the neuroscience literature about its harmful effects on brain tissue emerged and multiplied.
In addition, I came to realize that most psychiatric practitioners were unaware of the alarming deleterious neurologic effects of haloperidol—largely because the studies that reported those effects were published in neuroscience journals rarely read by practicing psychiatrists and nurse practitioners, and the pharmacists in charge of drug formularies at hospitals.
Evidence for the grave neurotoxicity of haloperidol and other older neuroleptics, compared with atypical antipsychotics, is substantial and multifaceted. The FDA would never approve haloperidol today, given the serious harm it can do to the brain, despite its efficacy for psychosis. (It’s interesting how the FDA bans a drug immediately if it causes tragic birth defects, such as thalidomide, but not if a drug is destructive to the brain tissue of a disabled adult patient. Invisible damage can be less alarming or urgent than visible damage.)
Twenty-eight studies reporting the various destructive effects of older antipsychotics (especially haloperidol) on brain tissue have been published in prominent neuroscience journals, based on work in animal models, cell culture, and post-mortem human tissue. Multiple molecular mechanisms, pathways, and cascades are involved, eventuating in neuronal death. The first review and discussion of these 28 neurotoxicity studies was presented at the annual meetings of the Society of Biological Psychiatry1 and the American Psychiatric Association2; a manuscript will soon be submitted for publication. See the bibliography below for a list of the 28 published studies.
The molecular mechanisms of neurotoxicity of older-generation antipsychotics, including haloperidol, fall into several major categories:
• apoptosis
• necrosis
• decreased cell viability
• inhibition of cell growth
• increased caspase activity (the “death spiral”)
• impaired glutamate transport
• mitochondrial damage.
Examples of specific mechanisms of neurotoxicity among older-generation antipsychotics appear in this Table.
With this massive evidence of the serious neurotoxic effects of haloperidol, should it be banned? The risks of the drug far exceed the benefits—especially given the availability of 9 atypical antipsychotics that have been shown to exert neuroprotective properties, such as inducing neurogenesis and increasing neurotrophic factors.3 One of our foremost duties as medical professionals is to protect patients from harmful treatments that could exacerbate their disability. It’s time to retire this aging neuroleptic.
Few medications remain in use 50 years after they were launched. Advances in drug development often render older drugs obsolete because newer drugs are more efficacious or safer, or both. Consider reserpine: Nowadays, no internist would use this drug to treat hypertension, even though it was the top-selling antihypertensive 50 years ago. Why? The adverse effects profile is no longer acceptable, with safer alternatives available.
Astonishingly, almost all first-generation psychotropics discovered 5 decades ago (neuroleptics, tricyclic antidepressants, monoamine oxidase inhibitors) are still on the formularies of most health care facilities and are used by many clinicians, especially those working with managed care organizations. Jails and prisons in the United States, where hundreds of thousands of seriously mentally ill patients are incarcerated, also use 50-year-old agents, without regard to the downside of older drugs on the body, brain, and quality of life of those incarcerated medically ill patients.
If clinicians who use these decades-old drugs were to keep up with medical research and advances in knowledge, we would realize what a travesty it is to use a brain-unfriendly drug such as haloperidol when we have many safer alternatives. A massive volume of knowledge has emerged over the past 15 years about the neurotoxicity of older neuroleptics, especially haloperidol—knowledge that was completely unknown before.a Second-generation antipsychotics have been shown to be much safer for the brain than their older-generation counterparts (although they are not more efficacious).
Changing awareness and changing practice
I used haloperidol for 20 years, and can vouch for its unquestionable efficacy in treating delusions and hallucinations. But I have avoided using it over the past 15 years, as the neuroscience literature about its harmful effects on brain tissue emerged and multiplied.
In addition, I came to realize that most psychiatric practitioners were unaware of the alarming deleterious neurologic effects of haloperidol—largely because the studies that reported those effects were published in neuroscience journals rarely read by practicing psychiatrists and nurse practitioners, and the pharmacists in charge of drug formularies at hospitals.
Evidence for the grave neurotoxicity of haloperidol and other older neuroleptics, compared with atypical antipsychotics, is substantial and multifaceted. The FDA would never approve haloperidol today, given the serious harm it can do to the brain, despite its efficacy for psychosis. (It’s interesting how the FDA bans a drug immediately if it causes tragic birth defects, such as thalidomide, but not if a drug is destructive to the brain tissue of a disabled adult patient. Invisible damage can be less alarming or urgent than visible damage.)
Twenty-eight studies reporting the various destructive effects of older antipsychotics (especially haloperidol) on brain tissue have been published in prominent neuroscience journals, based on work in animal models, cell culture, and post-mortem human tissue. Multiple molecular mechanisms, pathways, and cascades are involved, eventuating in neuronal death. The first review and discussion of these 28 neurotoxicity studies was presented at the annual meetings of the Society of Biological Psychiatry1 and the American Psychiatric Association2; a manuscript will soon be submitted for publication. See the bibliography below for a list of the 28 published studies.
The molecular mechanisms of neurotoxicity of older-generation antipsychotics, including haloperidol, fall into several major categories:
• apoptosis
• necrosis
• decreased cell viability
• inhibition of cell growth
• increased caspase activity (the “death spiral”)
• impaired glutamate transport
• mitochondrial damage.
Examples of specific mechanisms of neurotoxicity among older-generation antipsychotics appear in this Table.
With this massive evidence of the serious neurotoxic effects of haloperidol, should it be banned? The risks of the drug far exceed the benefits—especially given the availability of 9 atypical antipsychotics that have been shown to exert neuroprotective properties, such as inducing neurogenesis and increasing neurotrophic factors.3 One of our foremost duties as medical professionals is to protect patients from harmful treatments that could exacerbate their disability. It’s time to retire this aging neuroleptic.
1. Nasrallah HA, Rush SJ. First generation antipsychotics are neurotoxic and impair neuroplasticity via multiple mechanisms. Biol Psychiatry. 2013;73:61S.
2. Rush SJ, Nasrallah HA. Neurotoxic effects of the older antipsychotics: a review of several molecular mechanisms of action. Paper presented at: American Psychiatric Association Annual Meeting; May 18-22, 2013; San Francisco, CA.
3. Nandra KS, Agius M. The difference between typical and atypical antipsychotics: the effects on neurogenesis. Psychiatria Danub. 2012;24(supp1):95-99.
1. Nasrallah HA, Rush SJ. First generation antipsychotics are neurotoxic and impair neuroplasticity via multiple mechanisms. Biol Psychiatry. 2013;73:61S.
2. Rush SJ, Nasrallah HA. Neurotoxic effects of the older antipsychotics: a review of several molecular mechanisms of action. Paper presented at: American Psychiatric Association Annual Meeting; May 18-22, 2013; San Francisco, CA.
3. Nandra KS, Agius M. The difference between typical and atypical antipsychotics: the effects on neurogenesis. Psychiatria Danub. 2012;24(supp1):95-99.
Adoption by mentally ill individuals: What to recommend
Ms. T, age 28, wishes to adopt a child. She has a history of bipolar disorder, but has been stable for several years. She asks her psychiatrist if her diagnosis will disqualify her as a potential parent. She also wants to know how the psychiatrist can help with the adoption process because he has been treating her long-term and is familiar with her psychiatric history.
Many adults with a history of psychiatric illness prefer to adopt rather than have biological children. Their preference may be fueled by concerns regarding psychiatric destabilization during pregnancy or fear of psychotropic-induced fetal teratogenicity. Child adoption laws vary from state to state. Although some licensed adoption agencies sympathize with potential adoptive parents with a history of mental illness, the law usually considers the following factors:
• the potential adopter’s emotional ties to the child
• their parenting skills
• emotional needs of the child
• the potential adopter’s desire to maintain continuity of the child’s care
• permanence of the family unit of the proposed home
• the physical, moral, and mental fitness of the potential parent.
The psychiatrist’s role
So long as the adoptee’s well-being is the reason for adoption, and the adoption is in the “best interest of the child,”1 a history of mental illness does not necessarily exclude an individual from adopting a child. The psychiatrist needs to consider the potential adopter’s motives, intellectual capacity, and judgment with regards to caregiving. The psychiatrist needs to assess the degree to which the patient’s mental disorder may or may not interfere with their parenting. The clinician also needs to consider potential changes that may occur in the adopter’s personal life, work hours, recreational and social activities, and sleep patterns.
It also is important to estimate the changes that an adoption may cause in the potential adopter’s living arrangements, daily schedule, and life events such as family vacations. Based on knowledge of the patient’s psychiatric history, a clinician may need to consider whether adoption-related stress could destabilize or exacerbate the potential parent’s psychiatric condition.2 Other psychosocial factors of importance are the reliability of the adopter’s support system, their history of previous child-rearing success, care-taking arrangements, etc.1
What to consider
The potential adoptee’s unique needs also should be considered. Is the child physically handicapped or mentally challenged, and is your patient capable of handling these issues? Would there be a good temperament fit between the potential adoptive parent and child?
Because child adoption laws vary from state to state, there are no established criteria for determining the eligibility of an individual with a history of mental illness. The success of a child adoption by an individual with a history of mental illness will depend on state laws and the policy of the adoption agency. Some U.S. states and territories (Alaska, Arizona, California, Kentucky, North Dakota, and Puerto Rico) regard parental mental illness as “aggravated circumstances.”1
Although psychiatrists are not expected to be able to accurately predict the future, courts and adoption agencies may request a psychiatrist’s professional opinion on a specific adoption. See the Table for a list of suggested information to share when approached by an adoption agency or court.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Bacani-Oropilla T, Lippmann SB, Turns DM. Should the mentally ill adopt children? How physicians can influence the decision. Postgrad Med. 1988;84(6):201-205.
2. Linn L. Clinical manifestations of psychiatric disorder: the Homes-Rahe scale of stress of adjusting to change. In: Fredman A, Kaplan H, Sadock B, eds. Modern synopsis of comprehensive textbook of psychiatry, II. 2nd ed. Baltimore, MD: Williams & Wilkins; 1976:785.
Ms. T, age 28, wishes to adopt a child. She has a history of bipolar disorder, but has been stable for several years. She asks her psychiatrist if her diagnosis will disqualify her as a potential parent. She also wants to know how the psychiatrist can help with the adoption process because he has been treating her long-term and is familiar with her psychiatric history.
Many adults with a history of psychiatric illness prefer to adopt rather than have biological children. Their preference may be fueled by concerns regarding psychiatric destabilization during pregnancy or fear of psychotropic-induced fetal teratogenicity. Child adoption laws vary from state to state. Although some licensed adoption agencies sympathize with potential adoptive parents with a history of mental illness, the law usually considers the following factors:
• the potential adopter’s emotional ties to the child
• their parenting skills
• emotional needs of the child
• the potential adopter’s desire to maintain continuity of the child’s care
• permanence of the family unit of the proposed home
• the physical, moral, and mental fitness of the potential parent.
The psychiatrist’s role
So long as the adoptee’s well-being is the reason for adoption, and the adoption is in the “best interest of the child,”1 a history of mental illness does not necessarily exclude an individual from adopting a child. The psychiatrist needs to consider the potential adopter’s motives, intellectual capacity, and judgment with regards to caregiving. The psychiatrist needs to assess the degree to which the patient’s mental disorder may or may not interfere with their parenting. The clinician also needs to consider potential changes that may occur in the adopter’s personal life, work hours, recreational and social activities, and sleep patterns.
It also is important to estimate the changes that an adoption may cause in the potential adopter’s living arrangements, daily schedule, and life events such as family vacations. Based on knowledge of the patient’s psychiatric history, a clinician may need to consider whether adoption-related stress could destabilize or exacerbate the potential parent’s psychiatric condition.2 Other psychosocial factors of importance are the reliability of the adopter’s support system, their history of previous child-rearing success, care-taking arrangements, etc.1
What to consider
The potential adoptee’s unique needs also should be considered. Is the child physically handicapped or mentally challenged, and is your patient capable of handling these issues? Would there be a good temperament fit between the potential adoptive parent and child?
Because child adoption laws vary from state to state, there are no established criteria for determining the eligibility of an individual with a history of mental illness. The success of a child adoption by an individual with a history of mental illness will depend on state laws and the policy of the adoption agency. Some U.S. states and territories (Alaska, Arizona, California, Kentucky, North Dakota, and Puerto Rico) regard parental mental illness as “aggravated circumstances.”1
Although psychiatrists are not expected to be able to accurately predict the future, courts and adoption agencies may request a psychiatrist’s professional opinion on a specific adoption. See the Table for a list of suggested information to share when approached by an adoption agency or court.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Ms. T, age 28, wishes to adopt a child. She has a history of bipolar disorder, but has been stable for several years. She asks her psychiatrist if her diagnosis will disqualify her as a potential parent. She also wants to know how the psychiatrist can help with the adoption process because he has been treating her long-term and is familiar with her psychiatric history.
Many adults with a history of psychiatric illness prefer to adopt rather than have biological children. Their preference may be fueled by concerns regarding psychiatric destabilization during pregnancy or fear of psychotropic-induced fetal teratogenicity. Child adoption laws vary from state to state. Although some licensed adoption agencies sympathize with potential adoptive parents with a history of mental illness, the law usually considers the following factors:
• the potential adopter’s emotional ties to the child
• their parenting skills
• emotional needs of the child
• the potential adopter’s desire to maintain continuity of the child’s care
• permanence of the family unit of the proposed home
• the physical, moral, and mental fitness of the potential parent.
The psychiatrist’s role
So long as the adoptee’s well-being is the reason for adoption, and the adoption is in the “best interest of the child,”1 a history of mental illness does not necessarily exclude an individual from adopting a child. The psychiatrist needs to consider the potential adopter’s motives, intellectual capacity, and judgment with regards to caregiving. The psychiatrist needs to assess the degree to which the patient’s mental disorder may or may not interfere with their parenting. The clinician also needs to consider potential changes that may occur in the adopter’s personal life, work hours, recreational and social activities, and sleep patterns.
It also is important to estimate the changes that an adoption may cause in the potential adopter’s living arrangements, daily schedule, and life events such as family vacations. Based on knowledge of the patient’s psychiatric history, a clinician may need to consider whether adoption-related stress could destabilize or exacerbate the potential parent’s psychiatric condition.2 Other psychosocial factors of importance are the reliability of the adopter’s support system, their history of previous child-rearing success, care-taking arrangements, etc.1
What to consider
The potential adoptee’s unique needs also should be considered. Is the child physically handicapped or mentally challenged, and is your patient capable of handling these issues? Would there be a good temperament fit between the potential adoptive parent and child?
Because child adoption laws vary from state to state, there are no established criteria for determining the eligibility of an individual with a history of mental illness. The success of a child adoption by an individual with a history of mental illness will depend on state laws and the policy of the adoption agency. Some U.S. states and territories (Alaska, Arizona, California, Kentucky, North Dakota, and Puerto Rico) regard parental mental illness as “aggravated circumstances.”1
Although psychiatrists are not expected to be able to accurately predict the future, courts and adoption agencies may request a psychiatrist’s professional opinion on a specific adoption. See the Table for a list of suggested information to share when approached by an adoption agency or court.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Bacani-Oropilla T, Lippmann SB, Turns DM. Should the mentally ill adopt children? How physicians can influence the decision. Postgrad Med. 1988;84(6):201-205.
2. Linn L. Clinical manifestations of psychiatric disorder: the Homes-Rahe scale of stress of adjusting to change. In: Fredman A, Kaplan H, Sadock B, eds. Modern synopsis of comprehensive textbook of psychiatry, II. 2nd ed. Baltimore, MD: Williams & Wilkins; 1976:785.
1. Bacani-Oropilla T, Lippmann SB, Turns DM. Should the mentally ill adopt children? How physicians can influence the decision. Postgrad Med. 1988;84(6):201-205.
2. Linn L. Clinical manifestations of psychiatric disorder: the Homes-Rahe scale of stress of adjusting to change. In: Fredman A, Kaplan H, Sadock B, eds. Modern synopsis of comprehensive textbook of psychiatry, II. 2nd ed. Baltimore, MD: Williams & Wilkins; 1976:785.
Preventing prescription drug abuse: Make it LAST
Medications that psychiatrists routinely prescribe—such as benzodiazepines for anxiety and psychostimulants for attention-deficit/hyperactivity disorder—often are diverted and abused. In 2011, 6.1 million Americans age ≥12 abused prescription drugs.1
The mnemonic LAST can bring to mind 4 clinical “red flags” that can assist you in determining whether prescription abuse or diversion is occurring. Incorporating these 4 warning signs in your clinical assessment and medication reviews will make it easier for you to detect when medications are not being taken as prescribed.
Lost or stolen prescriptions. Patients who want to obtain a new or replacement prescription may claim that their medication was lost or stolen. Although this can occur, the prescriber should be suspicious if this becomes a recurrent situation. Some clinicians require patients to produce a filed police report for stolen medications before they will consider writing a new prescription.
Alternating medications/providers. Patients may obtain similar medications from multiple providers. Prescription Drug Monitoring Programs (PDMPs), which are databases that allow physicians to track where patients are getting their prescriptions, may help prevent this. According to the Alliance of States with Prescription Monitoring Programs, as of January 2010, 48 states had instituted PDMPs or passed legislation to implement them.2
Specific medication. Patients may have an allergy or respond better to a particular drug; however, be cautious when a patient refuses to consider an alternate medication or claims he or she has taken a specific medication without a prescription and it was the only thing that worked for them.
Time between prescriptions. Patients may get a prescription for a medication, then shortly after their visit claim the medication doesn’t work and request a second prescription for a similar medication. One way to address this is to require the patient to return the unused portion of the first medication before writing a new prescription. A patient also may complain that they have to come to your office too frequently and ask for multiple refills of medication, which would decrease your ability to monitor his or her response to treatment.
A patient who meets ≥1 of the above criteria could be a higher risk for prescription drug abuse or diversion. Documenting these findings and talking with the patient could help justify the need to switch to a medication with a lower abuse potential or possibly referral to a drug treatment program.
In a 2009 survey, 56% of teens stated that prescription medications were easier to obtain than illicit drugs.3 Medications such as benzodiazepines and stimulants can be beneficial to patients, but because of their abuse potential, they may be underprescribed. Be vigilant when prescribing these medications, and monitor patients carefully to ensure that they are taking all medications as directed.
Disclosure
Dr. Wiley reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Summary of findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. http://www.samhsa.gov/data/NSDUH/2k11Results/NSDUHresults2011.htm. Accessed May 2, 2013.
2. Alliance of States with Prescription Monitoring Programs. http://www.pmpalliance.org/content/about-alliance. Accessed May 1, 2013.
3. Partnership for a Drug-Free America. 2009 parents and teens attitude tracking study report. New York, NY: Partnership for a Drug-Free America; 2010. http://www.drugfree.org/wp-content/uploads/2011/04/FULL-REPORT-PATS-2009-3-2-10.pdf. Accessed May 2, 2013.
Medications that psychiatrists routinely prescribe—such as benzodiazepines for anxiety and psychostimulants for attention-deficit/hyperactivity disorder—often are diverted and abused. In 2011, 6.1 million Americans age ≥12 abused prescription drugs.1
The mnemonic LAST can bring to mind 4 clinical “red flags” that can assist you in determining whether prescription abuse or diversion is occurring. Incorporating these 4 warning signs in your clinical assessment and medication reviews will make it easier for you to detect when medications are not being taken as prescribed.
Lost or stolen prescriptions. Patients who want to obtain a new or replacement prescription may claim that their medication was lost or stolen. Although this can occur, the prescriber should be suspicious if this becomes a recurrent situation. Some clinicians require patients to produce a filed police report for stolen medications before they will consider writing a new prescription.
Alternating medications/providers. Patients may obtain similar medications from multiple providers. Prescription Drug Monitoring Programs (PDMPs), which are databases that allow physicians to track where patients are getting their prescriptions, may help prevent this. According to the Alliance of States with Prescription Monitoring Programs, as of January 2010, 48 states had instituted PDMPs or passed legislation to implement them.2
Specific medication. Patients may have an allergy or respond better to a particular drug; however, be cautious when a patient refuses to consider an alternate medication or claims he or she has taken a specific medication without a prescription and it was the only thing that worked for them.
Time between prescriptions. Patients may get a prescription for a medication, then shortly after their visit claim the medication doesn’t work and request a second prescription for a similar medication. One way to address this is to require the patient to return the unused portion of the first medication before writing a new prescription. A patient also may complain that they have to come to your office too frequently and ask for multiple refills of medication, which would decrease your ability to monitor his or her response to treatment.
A patient who meets ≥1 of the above criteria could be a higher risk for prescription drug abuse or diversion. Documenting these findings and talking with the patient could help justify the need to switch to a medication with a lower abuse potential or possibly referral to a drug treatment program.
In a 2009 survey, 56% of teens stated that prescription medications were easier to obtain than illicit drugs.3 Medications such as benzodiazepines and stimulants can be beneficial to patients, but because of their abuse potential, they may be underprescribed. Be vigilant when prescribing these medications, and monitor patients carefully to ensure that they are taking all medications as directed.
Disclosure
Dr. Wiley reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Summary of findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. http://www.samhsa.gov/data/NSDUH/2k11Results/NSDUHresults2011.htm. Accessed May 2, 2013.
2. Alliance of States with Prescription Monitoring Programs. http://www.pmpalliance.org/content/about-alliance. Accessed May 1, 2013.
3. Partnership for a Drug-Free America. 2009 parents and teens attitude tracking study report. New York, NY: Partnership for a Drug-Free America; 2010. http://www.drugfree.org/wp-content/uploads/2011/04/FULL-REPORT-PATS-2009-3-2-10.pdf. Accessed May 2, 2013.
Medications that psychiatrists routinely prescribe—such as benzodiazepines for anxiety and psychostimulants for attention-deficit/hyperactivity disorder—often are diverted and abused. In 2011, 6.1 million Americans age ≥12 abused prescription drugs.1
The mnemonic LAST can bring to mind 4 clinical “red flags” that can assist you in determining whether prescription abuse or diversion is occurring. Incorporating these 4 warning signs in your clinical assessment and medication reviews will make it easier for you to detect when medications are not being taken as prescribed.
Lost or stolen prescriptions. Patients who want to obtain a new or replacement prescription may claim that their medication was lost or stolen. Although this can occur, the prescriber should be suspicious if this becomes a recurrent situation. Some clinicians require patients to produce a filed police report for stolen medications before they will consider writing a new prescription.
Alternating medications/providers. Patients may obtain similar medications from multiple providers. Prescription Drug Monitoring Programs (PDMPs), which are databases that allow physicians to track where patients are getting their prescriptions, may help prevent this. According to the Alliance of States with Prescription Monitoring Programs, as of January 2010, 48 states had instituted PDMPs or passed legislation to implement them.2
Specific medication. Patients may have an allergy or respond better to a particular drug; however, be cautious when a patient refuses to consider an alternate medication or claims he or she has taken a specific medication without a prescription and it was the only thing that worked for them.
Time between prescriptions. Patients may get a prescription for a medication, then shortly after their visit claim the medication doesn’t work and request a second prescription for a similar medication. One way to address this is to require the patient to return the unused portion of the first medication before writing a new prescription. A patient also may complain that they have to come to your office too frequently and ask for multiple refills of medication, which would decrease your ability to monitor his or her response to treatment.
A patient who meets ≥1 of the above criteria could be a higher risk for prescription drug abuse or diversion. Documenting these findings and talking with the patient could help justify the need to switch to a medication with a lower abuse potential or possibly referral to a drug treatment program.
In a 2009 survey, 56% of teens stated that prescription medications were easier to obtain than illicit drugs.3 Medications such as benzodiazepines and stimulants can be beneficial to patients, but because of their abuse potential, they may be underprescribed. Be vigilant when prescribing these medications, and monitor patients carefully to ensure that they are taking all medications as directed.
Disclosure
Dr. Wiley reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Summary of findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. http://www.samhsa.gov/data/NSDUH/2k11Results/NSDUHresults2011.htm. Accessed May 2, 2013.
2. Alliance of States with Prescription Monitoring Programs. http://www.pmpalliance.org/content/about-alliance. Accessed May 1, 2013.
3. Partnership for a Drug-Free America. 2009 parents and teens attitude tracking study report. New York, NY: Partnership for a Drug-Free America; 2010. http://www.drugfree.org/wp-content/uploads/2011/04/FULL-REPORT-PATS-2009-3-2-10.pdf. Accessed May 2, 2013.