User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


How has hospital medicine changed since you started?

HM19 attendees relay their perspectives on how the practice of hospital medicine has evolved over the course of their careers.

HM19 attendees relay their perspectives on how the practice of hospital medicine has evolved over the course of their careers.

HM19 attendees relay their perspectives on how the practice of hospital medicine has evolved over the course of their careers.
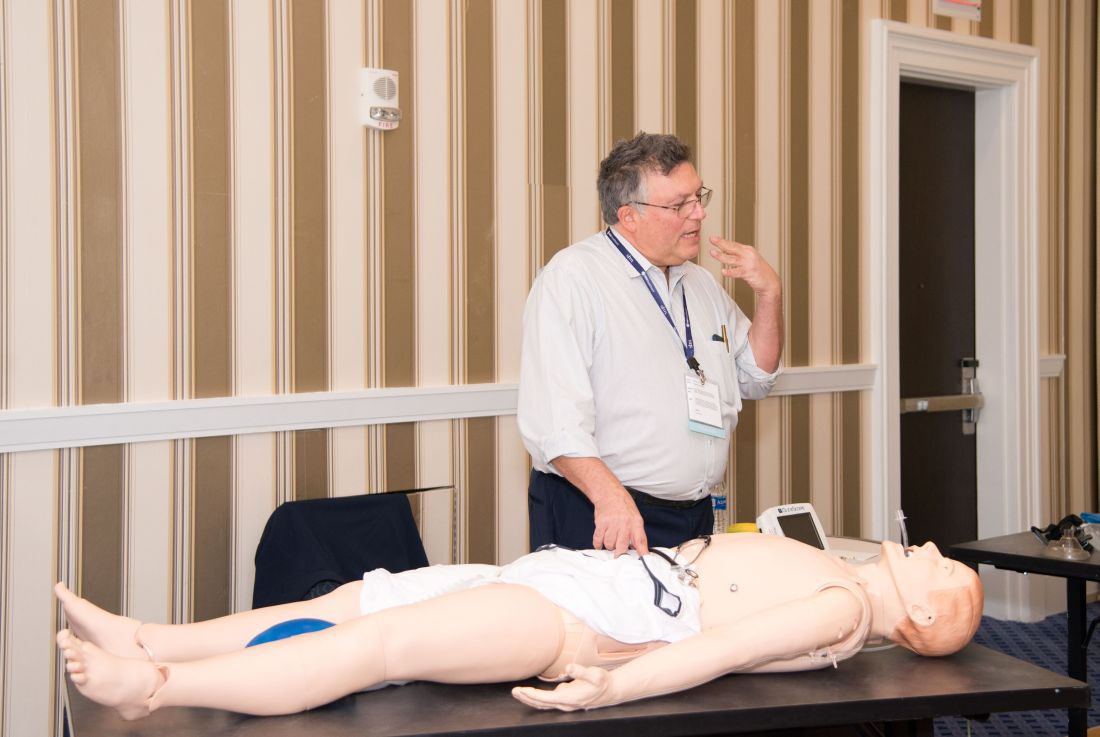
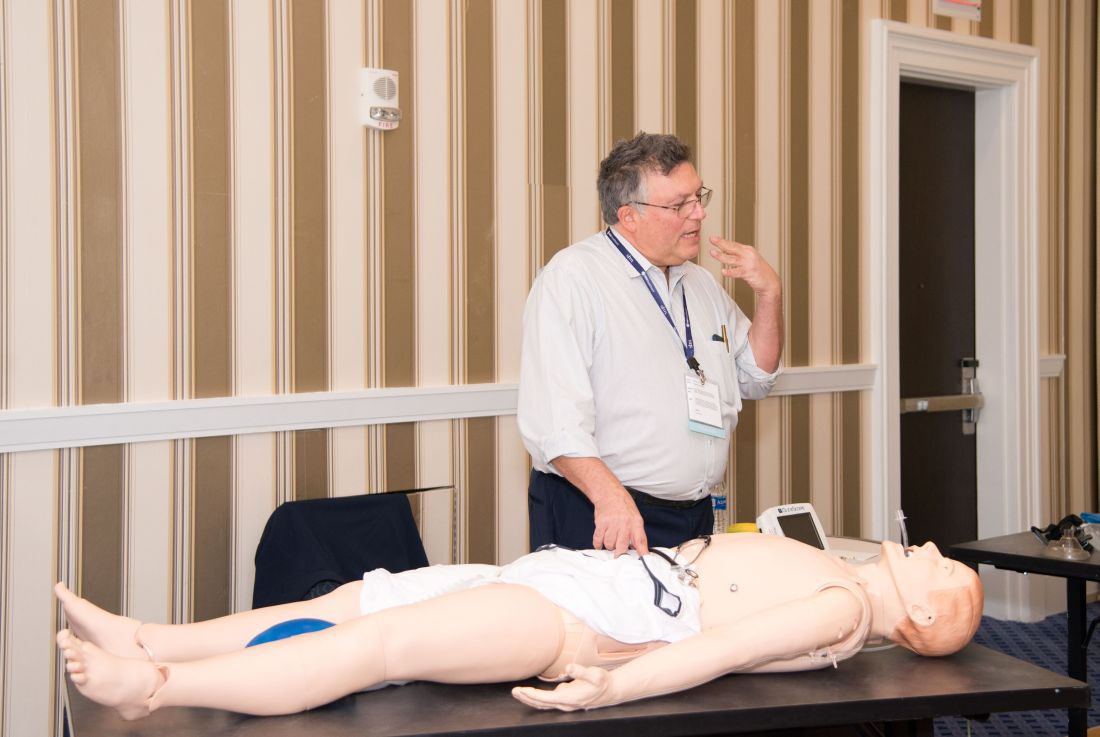
Hands-on critical care lessons provided at HM19
As the hospitalist tried to position the portable video laryngoscope properly in the airway of the critically ill “patient,” HM19 faculty moderator Brian Kaufman, MD, professor of medicine, anesthesiology, and neurology at New York University (NYU) School of Medicine, issued a word of caution: Rotating it into position should be done gently or there’s a risk of tearing tissue.
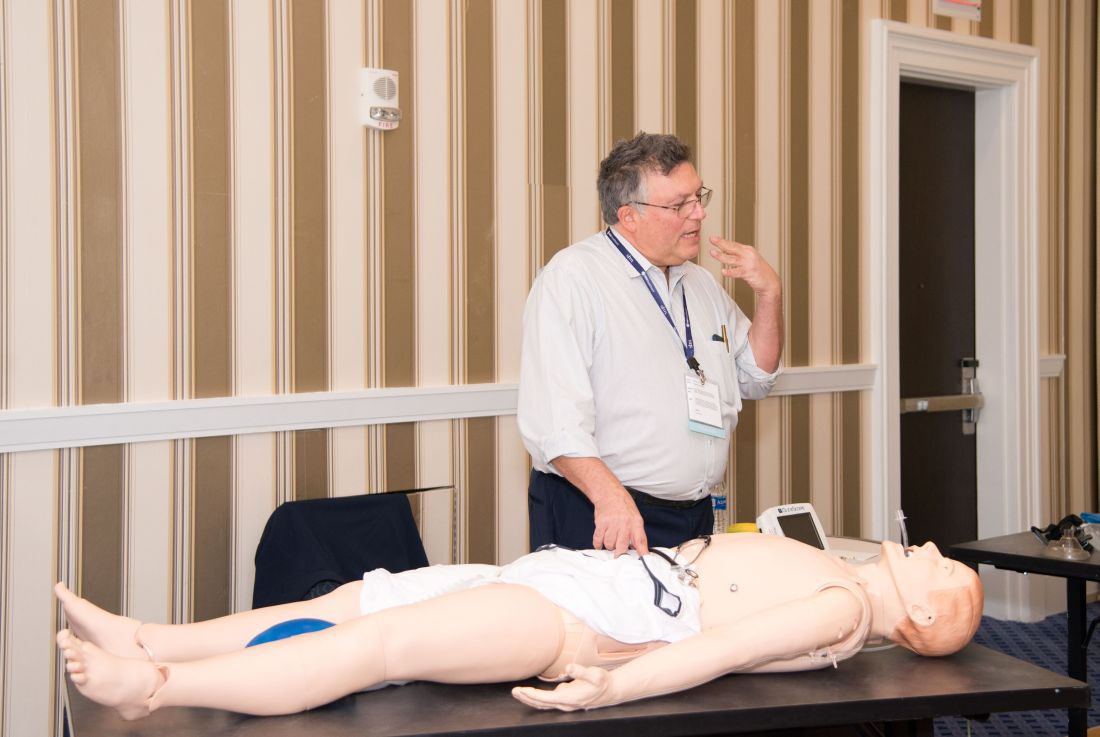
One step at a time, hospitalists attending the session grew more confident and knowledgeable in handling urgent matters involving patients who are critically ill, including cases of shock, mechanical ventilation, overdoses, and ultrasound.
Kevin Felner, MD, associate professor of medicine at NYU School of Medicine, said there’s a growing need for more exposure to caring for the critically ill, including intubation.
“There are a lot of hospitalists who are intubating, and they’re not formally trained in it because medicine residencies don’t typically train people to manage airways,” he said. “We’ve met hospitalists who’ve said, ‘I was hired and was told I had to manage an airway.’”
“It might massage some of the things you’re doing, make you afraid of things you should be afraid of, make you think about something that’s easy to do that you’re not doing, and make things safer,” Dr. Felner said.
In a simulation room, James Horowitz, MD, clinical assistant professor and cardiologist at NYU School of Medicine, demonstrated how to use a laryngeal mask airway (LMA), a simpler alternative to intubating the trachea for keeping an airway open. Dr. Kaufman, standing next to him, clarified how important a skill this is, especially when someone needs air in the next minute or is at risk of death.
“Knowing how to put an LMA in can be life-saving,” Dr. Kaufman said.
In a lecture on shock in the critically ill, Dr. Felner said it’s important to be nimble in handling this common problem –quickly identifying the cause, whether it’s a cardiogenic issue, a low-volume circulation problem, a question of vasodilation, or an obstructive problem. He said guidelines – such as aiming for a mean arterial pressure of 65 mm Hg –are helpful generally, but individuals routinely call for making exceptions to guidelines.
Anthony Andriotis, MD, a pulmonologist at NYU who specializes in critical care, offered an array of key points when managing patients with a ventilator. For instance, when you need to prolong a patient’s expiratory time so they can exhale air more effectively to get rid of entrapped air in their lungs, lowering their respiratory rate is far more effective than decreasing the time it takes them to breathe in or increasing the flow rate of the air they’re breathing.
Some basic points – such as remembering that it’s important to be aware of the pressure when volume control has been imposed and to be aware of volume control when the pressure has been set – are crucial, he said.
The idea behind the pre-course, Dr. Felner said, was to give hospitalists a chance to enter tricky situations with everything to gain, but nothing to lose. He described it as giving students “learning scars” – those times you made a serious error that left you with a lesson you’ll never forget.
“We’re trying to create learning scars, but in a safe scenario.”
As the hospitalist tried to position the portable video laryngoscope properly in the airway of the critically ill “patient,” HM19 faculty moderator Brian Kaufman, MD, professor of medicine, anesthesiology, and neurology at New York University (NYU) School of Medicine, issued a word of caution: Rotating it into position should be done gently or there’s a risk of tearing tissue.
One step at a time, hospitalists attending the session grew more confident and knowledgeable in handling urgent matters involving patients who are critically ill, including cases of shock, mechanical ventilation, overdoses, and ultrasound.
Kevin Felner, MD, associate professor of medicine at NYU School of Medicine, said there’s a growing need for more exposure to caring for the critically ill, including intubation.
“There are a lot of hospitalists who are intubating, and they’re not formally trained in it because medicine residencies don’t typically train people to manage airways,” he said. “We’ve met hospitalists who’ve said, ‘I was hired and was told I had to manage an airway.’”
“It might massage some of the things you’re doing, make you afraid of things you should be afraid of, make you think about something that’s easy to do that you’re not doing, and make things safer,” Dr. Felner said.
In a simulation room, James Horowitz, MD, clinical assistant professor and cardiologist at NYU School of Medicine, demonstrated how to use a laryngeal mask airway (LMA), a simpler alternative to intubating the trachea for keeping an airway open. Dr. Kaufman, standing next to him, clarified how important a skill this is, especially when someone needs air in the next minute or is at risk of death.
“Knowing how to put an LMA in can be life-saving,” Dr. Kaufman said.
In a lecture on shock in the critically ill, Dr. Felner said it’s important to be nimble in handling this common problem –quickly identifying the cause, whether it’s a cardiogenic issue, a low-volume circulation problem, a question of vasodilation, or an obstructive problem. He said guidelines – such as aiming for a mean arterial pressure of 65 mm Hg –are helpful generally, but individuals routinely call for making exceptions to guidelines.
Anthony Andriotis, MD, a pulmonologist at NYU who specializes in critical care, offered an array of key points when managing patients with a ventilator. For instance, when you need to prolong a patient’s expiratory time so they can exhale air more effectively to get rid of entrapped air in their lungs, lowering their respiratory rate is far more effective than decreasing the time it takes them to breathe in or increasing the flow rate of the air they’re breathing.
Some basic points – such as remembering that it’s important to be aware of the pressure when volume control has been imposed and to be aware of volume control when the pressure has been set – are crucial, he said.
The idea behind the pre-course, Dr. Felner said, was to give hospitalists a chance to enter tricky situations with everything to gain, but nothing to lose. He described it as giving students “learning scars” – those times you made a serious error that left you with a lesson you’ll never forget.
“We’re trying to create learning scars, but in a safe scenario.”
As the hospitalist tried to position the portable video laryngoscope properly in the airway of the critically ill “patient,” HM19 faculty moderator Brian Kaufman, MD, professor of medicine, anesthesiology, and neurology at New York University (NYU) School of Medicine, issued a word of caution: Rotating it into position should be done gently or there’s a risk of tearing tissue.
One step at a time, hospitalists attending the session grew more confident and knowledgeable in handling urgent matters involving patients who are critically ill, including cases of shock, mechanical ventilation, overdoses, and ultrasound.
Kevin Felner, MD, associate professor of medicine at NYU School of Medicine, said there’s a growing need for more exposure to caring for the critically ill, including intubation.
“There are a lot of hospitalists who are intubating, and they’re not formally trained in it because medicine residencies don’t typically train people to manage airways,” he said. “We’ve met hospitalists who’ve said, ‘I was hired and was told I had to manage an airway.’”
“It might massage some of the things you’re doing, make you afraid of things you should be afraid of, make you think about something that’s easy to do that you’re not doing, and make things safer,” Dr. Felner said.
In a simulation room, James Horowitz, MD, clinical assistant professor and cardiologist at NYU School of Medicine, demonstrated how to use a laryngeal mask airway (LMA), a simpler alternative to intubating the trachea for keeping an airway open. Dr. Kaufman, standing next to him, clarified how important a skill this is, especially when someone needs air in the next minute or is at risk of death.
“Knowing how to put an LMA in can be life-saving,” Dr. Kaufman said.
In a lecture on shock in the critically ill, Dr. Felner said it’s important to be nimble in handling this common problem –quickly identifying the cause, whether it’s a cardiogenic issue, a low-volume circulation problem, a question of vasodilation, or an obstructive problem. He said guidelines – such as aiming for a mean arterial pressure of 65 mm Hg –are helpful generally, but individuals routinely call for making exceptions to guidelines.
Anthony Andriotis, MD, a pulmonologist at NYU who specializes in critical care, offered an array of key points when managing patients with a ventilator. For instance, when you need to prolong a patient’s expiratory time so they can exhale air more effectively to get rid of entrapped air in their lungs, lowering their respiratory rate is far more effective than decreasing the time it takes them to breathe in or increasing the flow rate of the air they’re breathing.
Some basic points – such as remembering that it’s important to be aware of the pressure when volume control has been imposed and to be aware of volume control when the pressure has been set – are crucial, he said.
The idea behind the pre-course, Dr. Felner said, was to give hospitalists a chance to enter tricky situations with everything to gain, but nothing to lose. He described it as giving students “learning scars” – those times you made a serious error that left you with a lesson you’ll never forget.
“We’re trying to create learning scars, but in a safe scenario.”
Occurrence of pulmonary embolisms in hospitalized patients nearly doubled during 2004-2015
NEW ORLEANS –
During 2004-2015 the incidence of all diagnosed pulmonary embolism (PE), based on discharge diagnoses, rose from 5.4 cases/1,000 hospitalized patients in 2004 to 9.7 cases/1,000 hospitalized patients in 2015, an 80% increase, Joshua B. Goldberg, MD said at the annual meeting of the American College of Cardiology. The incidence of major PE – defined as a patient who needed vasopressor treatment, mechanical ventilation, or had nonseptic shock – rose from 7.9% of all hospitalized PE diagnoses in 2004 to 9.7% in 2015, a 23% relative increase.
The data also documented a shifting pattern of treatment for all hospitalized patients with PE, and especially among patients with major PE. During the study period, treatment with systemic thrombolysis for all PE rose nearly threefold, and catheter-directed therapy began to show a steady rise in use from 0.2% of all patients in 2011 (and before) to 1% of all patients by 2015. Surgical intervention remained lightly used throughout, with about 0.2% of all PE patients undergoing surgery annually.
Most of these intervention options focused on patients with major PE. Among patients in this subgroup with more severe disease, use of one of these three types of interventions rose from 6% in 2004 to 12% in 2015, mostly driven by a rise in systemic thrombolysis, which jumped from 3% of major PE in 2004 to 9% in 2015. However, the efficacy of systemic thrombolysis in patients with major PE remains suspect. In 2004, 39% of patients with major PE treated with systemic thrombolysis died in hospital; in 2015 the number was 47%. “The data don’t support using systemic thrombolysis to treat major PE; the mortality is high,” noted Dr. Goldberg, a cardiothoracic surgeon at Westchester Medical Center in Valhalla, N.Y.
Although catheter-directed therapy began to be much more widely used in U.S. practice starting in about 2015, during the period studied its use for major PE held fairly steady at roughly 2%-3%, but this approach also showed substantial shortcomings for the major PE population. These sicker patients treated with catheter-directed therapy had 37% mortality in 2004 and a 31% mortality in 2015, a difference that was not statistically significant. In general, PE patients enrolled in the catheter-directed therapy trials were not as sick as the major PE patients who get treated with surgery in routine practice, Dr. Goldberg said in an interview.
The data showed much better performance using surgery, although only 1,237 patients of the entire group of 713,083 PE patients studied in the database underwent surgical embolectomy. Overall, in-hospital mortality in these patients was 22%, but in a time trend analysis, mortality among all PE patients treated with surgery fell from 32% in 2004 to 14% in 2015; among patients with major PE treated with surgery, mortality fell from 52% in 2004 to 21% in 2015.
Dr. Goldberg attributed the success of surgery in severe PE patients to the definitive nature of embolectomy and the concurrent use of extracorporeal membrane oxygenation that helps stabilize acutely ill PE patients. He also cited refinements that surgery underwent during the 2004-2015 period based on the experience managing chronic thromboembolic pulmonary hypertension, including routine use of cardiopulmonary bypass during surgery. “Very high risk [PE] patients should go straight to surgery, unless the patient is at high risk for surgery because of conditions like prior sternotomy or very advanced age, in which case catheter-directed therapy may be a safer option, he said. He cited a recent 5% death rate after surgery at his center among patients with major PE who did not require cardiopulmonary resuscitation.
The database Dr. Goldberg and his collaborator reviewed included 12,735 patients treated by systemic thrombolysis, and 2,595 treated by catheter-directed therapy. Patients averaged 63 years old. The most common indicator of major PE was mechanical ventilation, used on 8% of all PE patients in the study. Non-septic shock occurred in 2%, and just under 1% needed vasopressor treatment.
Published guidelines on PE management from several medical groups are “vague and have numerous caveats,” Dr. Goldberg said. He is participating in an update to the 2011 PE management statement from the American College of Cardiology and American Heart Association (Circulation. 2011 April 26;123[16]:1788-1830).
The study received no commercial funding. Dr. Goldberg had no disclosures.
SOURCE: Haider A et al. J Amer Coll Cardiol. 2019 March;73:9[suppl 1]: doi: 10.1016/S0735-1097(19)32507-0
At my center, Allegheny General Hospital, we often rely on catheter-directed therapy to treat major pulmonary embolism. We now perform more catheter-directed interventions than surgical embolectomies. Generally, when treating patients with major pulmonary embolism it comes down to a choice between those two options. We rarely use systemic thrombolysis for major pulmonary embolism any more.
Raymond L. Benza, MD , is professor of medicine at Temple University College of Medicine and program director for advanced heart failure at the Allegheny Health Network in Pittsburgh. He has been a consultant to Actelion, Gilead, and United Therapeutics, and he has received research funding from Bayer. He made these comments in an interview.
At my center, Allegheny General Hospital, we often rely on catheter-directed therapy to treat major pulmonary embolism. We now perform more catheter-directed interventions than surgical embolectomies. Generally, when treating patients with major pulmonary embolism it comes down to a choice between those two options. We rarely use systemic thrombolysis for major pulmonary embolism any more.
Raymond L. Benza, MD , is professor of medicine at Temple University College of Medicine and program director for advanced heart failure at the Allegheny Health Network in Pittsburgh. He has been a consultant to Actelion, Gilead, and United Therapeutics, and he has received research funding from Bayer. He made these comments in an interview.
At my center, Allegheny General Hospital, we often rely on catheter-directed therapy to treat major pulmonary embolism. We now perform more catheter-directed interventions than surgical embolectomies. Generally, when treating patients with major pulmonary embolism it comes down to a choice between those two options. We rarely use systemic thrombolysis for major pulmonary embolism any more.
Raymond L. Benza, MD , is professor of medicine at Temple University College of Medicine and program director for advanced heart failure at the Allegheny Health Network in Pittsburgh. He has been a consultant to Actelion, Gilead, and United Therapeutics, and he has received research funding from Bayer. He made these comments in an interview.
NEW ORLEANS –
During 2004-2015 the incidence of all diagnosed pulmonary embolism (PE), based on discharge diagnoses, rose from 5.4 cases/1,000 hospitalized patients in 2004 to 9.7 cases/1,000 hospitalized patients in 2015, an 80% increase, Joshua B. Goldberg, MD said at the annual meeting of the American College of Cardiology. The incidence of major PE – defined as a patient who needed vasopressor treatment, mechanical ventilation, or had nonseptic shock – rose from 7.9% of all hospitalized PE diagnoses in 2004 to 9.7% in 2015, a 23% relative increase.
The data also documented a shifting pattern of treatment for all hospitalized patients with PE, and especially among patients with major PE. During the study period, treatment with systemic thrombolysis for all PE rose nearly threefold, and catheter-directed therapy began to show a steady rise in use from 0.2% of all patients in 2011 (and before) to 1% of all patients by 2015. Surgical intervention remained lightly used throughout, with about 0.2% of all PE patients undergoing surgery annually.
Most of these intervention options focused on patients with major PE. Among patients in this subgroup with more severe disease, use of one of these three types of interventions rose from 6% in 2004 to 12% in 2015, mostly driven by a rise in systemic thrombolysis, which jumped from 3% of major PE in 2004 to 9% in 2015. However, the efficacy of systemic thrombolysis in patients with major PE remains suspect. In 2004, 39% of patients with major PE treated with systemic thrombolysis died in hospital; in 2015 the number was 47%. “The data don’t support using systemic thrombolysis to treat major PE; the mortality is high,” noted Dr. Goldberg, a cardiothoracic surgeon at Westchester Medical Center in Valhalla, N.Y.
Although catheter-directed therapy began to be much more widely used in U.S. practice starting in about 2015, during the period studied its use for major PE held fairly steady at roughly 2%-3%, but this approach also showed substantial shortcomings for the major PE population. These sicker patients treated with catheter-directed therapy had 37% mortality in 2004 and a 31% mortality in 2015, a difference that was not statistically significant. In general, PE patients enrolled in the catheter-directed therapy trials were not as sick as the major PE patients who get treated with surgery in routine practice, Dr. Goldberg said in an interview.
The data showed much better performance using surgery, although only 1,237 patients of the entire group of 713,083 PE patients studied in the database underwent surgical embolectomy. Overall, in-hospital mortality in these patients was 22%, but in a time trend analysis, mortality among all PE patients treated with surgery fell from 32% in 2004 to 14% in 2015; among patients with major PE treated with surgery, mortality fell from 52% in 2004 to 21% in 2015.
Dr. Goldberg attributed the success of surgery in severe PE patients to the definitive nature of embolectomy and the concurrent use of extracorporeal membrane oxygenation that helps stabilize acutely ill PE patients. He also cited refinements that surgery underwent during the 2004-2015 period based on the experience managing chronic thromboembolic pulmonary hypertension, including routine use of cardiopulmonary bypass during surgery. “Very high risk [PE] patients should go straight to surgery, unless the patient is at high risk for surgery because of conditions like prior sternotomy or very advanced age, in which case catheter-directed therapy may be a safer option, he said. He cited a recent 5% death rate after surgery at his center among patients with major PE who did not require cardiopulmonary resuscitation.
The database Dr. Goldberg and his collaborator reviewed included 12,735 patients treated by systemic thrombolysis, and 2,595 treated by catheter-directed therapy. Patients averaged 63 years old. The most common indicator of major PE was mechanical ventilation, used on 8% of all PE patients in the study. Non-septic shock occurred in 2%, and just under 1% needed vasopressor treatment.
Published guidelines on PE management from several medical groups are “vague and have numerous caveats,” Dr. Goldberg said. He is participating in an update to the 2011 PE management statement from the American College of Cardiology and American Heart Association (Circulation. 2011 April 26;123[16]:1788-1830).
The study received no commercial funding. Dr. Goldberg had no disclosures.
SOURCE: Haider A et al. J Amer Coll Cardiol. 2019 March;73:9[suppl 1]: doi: 10.1016/S0735-1097(19)32507-0
NEW ORLEANS –
During 2004-2015 the incidence of all diagnosed pulmonary embolism (PE), based on discharge diagnoses, rose from 5.4 cases/1,000 hospitalized patients in 2004 to 9.7 cases/1,000 hospitalized patients in 2015, an 80% increase, Joshua B. Goldberg, MD said at the annual meeting of the American College of Cardiology. The incidence of major PE – defined as a patient who needed vasopressor treatment, mechanical ventilation, or had nonseptic shock – rose from 7.9% of all hospitalized PE diagnoses in 2004 to 9.7% in 2015, a 23% relative increase.
The data also documented a shifting pattern of treatment for all hospitalized patients with PE, and especially among patients with major PE. During the study period, treatment with systemic thrombolysis for all PE rose nearly threefold, and catheter-directed therapy began to show a steady rise in use from 0.2% of all patients in 2011 (and before) to 1% of all patients by 2015. Surgical intervention remained lightly used throughout, with about 0.2% of all PE patients undergoing surgery annually.
Most of these intervention options focused on patients with major PE. Among patients in this subgroup with more severe disease, use of one of these three types of interventions rose from 6% in 2004 to 12% in 2015, mostly driven by a rise in systemic thrombolysis, which jumped from 3% of major PE in 2004 to 9% in 2015. However, the efficacy of systemic thrombolysis in patients with major PE remains suspect. In 2004, 39% of patients with major PE treated with systemic thrombolysis died in hospital; in 2015 the number was 47%. “The data don’t support using systemic thrombolysis to treat major PE; the mortality is high,” noted Dr. Goldberg, a cardiothoracic surgeon at Westchester Medical Center in Valhalla, N.Y.
Although catheter-directed therapy began to be much more widely used in U.S. practice starting in about 2015, during the period studied its use for major PE held fairly steady at roughly 2%-3%, but this approach also showed substantial shortcomings for the major PE population. These sicker patients treated with catheter-directed therapy had 37% mortality in 2004 and a 31% mortality in 2015, a difference that was not statistically significant. In general, PE patients enrolled in the catheter-directed therapy trials were not as sick as the major PE patients who get treated with surgery in routine practice, Dr. Goldberg said in an interview.
The data showed much better performance using surgery, although only 1,237 patients of the entire group of 713,083 PE patients studied in the database underwent surgical embolectomy. Overall, in-hospital mortality in these patients was 22%, but in a time trend analysis, mortality among all PE patients treated with surgery fell from 32% in 2004 to 14% in 2015; among patients with major PE treated with surgery, mortality fell from 52% in 2004 to 21% in 2015.
Dr. Goldberg attributed the success of surgery in severe PE patients to the definitive nature of embolectomy and the concurrent use of extracorporeal membrane oxygenation that helps stabilize acutely ill PE patients. He also cited refinements that surgery underwent during the 2004-2015 period based on the experience managing chronic thromboembolic pulmonary hypertension, including routine use of cardiopulmonary bypass during surgery. “Very high risk [PE] patients should go straight to surgery, unless the patient is at high risk for surgery because of conditions like prior sternotomy or very advanced age, in which case catheter-directed therapy may be a safer option, he said. He cited a recent 5% death rate after surgery at his center among patients with major PE who did not require cardiopulmonary resuscitation.
The database Dr. Goldberg and his collaborator reviewed included 12,735 patients treated by systemic thrombolysis, and 2,595 treated by catheter-directed therapy. Patients averaged 63 years old. The most common indicator of major PE was mechanical ventilation, used on 8% of all PE patients in the study. Non-septic shock occurred in 2%, and just under 1% needed vasopressor treatment.
Published guidelines on PE management from several medical groups are “vague and have numerous caveats,” Dr. Goldberg said. He is participating in an update to the 2011 PE management statement from the American College of Cardiology and American Heart Association (Circulation. 2011 April 26;123[16]:1788-1830).
The study received no commercial funding. Dr. Goldberg had no disclosures.
SOURCE: Haider A et al. J Amer Coll Cardiol. 2019 March;73:9[suppl 1]: doi: 10.1016/S0735-1097(19)32507-0
REPORTING FROM ACC 2019
Planning for change in hospitalist practice management
At Sunday’s HM19 pre-course “Oh, the Places We’ll Go! Practice Management Tools for Navigating the Changing Role of Your Hospital Medicine Group,” the theme was how to anticipate and embrace changing roles as hospital medicine groups are being asked to take on more responsibility.
“The scope of hospitalist practice is evolving rapidly, both clinically and in terms of all of the other things that hospitalists are being asked to do,” said Leslie Flores, MHA, SFHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., and course co-director, in an interview before the pre-course. “Our goals with this program are to help leaders position their hospitalist groups for success with this changing environment that they’re living in and the changing roles of hospitalists.”
In an audience poll at the beginning of the pre-course, attendees – a majority of whom were practicing hospitalists and managers of hospitalist groups – said their biggest challenge areas were related to compensation or workflows that have not evolved to match their changing role, and disagreements over who should admit patients.
One of the goals of the session was to give hospitalist leaders ideas to address these issues, which included information on how to implement better team-based care and interdisciplinary care models within their groups, as well as how to adjust their compensation, scheduling, and staffing models to prepare for this “new world of hospitalist medicine,” said Ms. Flores.
“One of the biggest sources of contention and stress that we see in hospitalist groups is that there’s just so much change, and it’s happening so rapidly, and people are having a hard time really figuring out how to deal with all of that,” she said.
The day began with John Nelson, MD, MHM, outlining the “Trends in Scope of Practice Evolution.” Dr. Nelson, a partner at Nelson Flores Hospital Medicine Consultants, medical director of Overlake Medical Center in Bellevue, Wash., and course co-director, said hospitalists are increasingly working more in outpatient care, post-acute care, and other specialty facilities. In addition, as group size increases, the likelihood a hospitalist group will be responsible for an observation or short stay unit increases, while a larger group is less likely to have a clinical responsibility for a code blue, cardiac arrest, or rapid response team.
Other topics in the pre-course focused on how to change the culture in a group to an environment where team members are empowered to ask questions or voice concerns, improve patient flow by removing reasons for delays in discharge, recruit the right team members to a group, handle transitions of care, and anticipate change in a group. In addition, the speakers participated in discussions where they shared their biggest successes and failures in practice as leaders and participated in a lightning round where they provided “off-the-cuff” responses to questions from Ms. Flores.
Although hospitalists did not create the current environment that is expanding their role in the health care system, they can position themselves to decide what the scope of their role is, said Dr. Nelson.
“What we should do is navigate our group through these changes in the way that’s going to be most effective for ourselves, the providers in our group, and our organization,” he said. “Those groups that try to dig their heels in or resist all change, they fail. . . and they frustrate themselves. So instead, if you engage in planning for changes in the scope of your practice, you have a chance to make it go the way you’d like it to go, and you’re going to be more satisfied.”
At Sunday’s HM19 pre-course “Oh, the Places We’ll Go! Practice Management Tools for Navigating the Changing Role of Your Hospital Medicine Group,” the theme was how to anticipate and embrace changing roles as hospital medicine groups are being asked to take on more responsibility.
“The scope of hospitalist practice is evolving rapidly, both clinically and in terms of all of the other things that hospitalists are being asked to do,” said Leslie Flores, MHA, SFHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., and course co-director, in an interview before the pre-course. “Our goals with this program are to help leaders position their hospitalist groups for success with this changing environment that they’re living in and the changing roles of hospitalists.”
In an audience poll at the beginning of the pre-course, attendees – a majority of whom were practicing hospitalists and managers of hospitalist groups – said their biggest challenge areas were related to compensation or workflows that have not evolved to match their changing role, and disagreements over who should admit patients.
One of the goals of the session was to give hospitalist leaders ideas to address these issues, which included information on how to implement better team-based care and interdisciplinary care models within their groups, as well as how to adjust their compensation, scheduling, and staffing models to prepare for this “new world of hospitalist medicine,” said Ms. Flores.
“One of the biggest sources of contention and stress that we see in hospitalist groups is that there’s just so much change, and it’s happening so rapidly, and people are having a hard time really figuring out how to deal with all of that,” she said.
The day began with John Nelson, MD, MHM, outlining the “Trends in Scope of Practice Evolution.” Dr. Nelson, a partner at Nelson Flores Hospital Medicine Consultants, medical director of Overlake Medical Center in Bellevue, Wash., and course co-director, said hospitalists are increasingly working more in outpatient care, post-acute care, and other specialty facilities. In addition, as group size increases, the likelihood a hospitalist group will be responsible for an observation or short stay unit increases, while a larger group is less likely to have a clinical responsibility for a code blue, cardiac arrest, or rapid response team.
Other topics in the pre-course focused on how to change the culture in a group to an environment where team members are empowered to ask questions or voice concerns, improve patient flow by removing reasons for delays in discharge, recruit the right team members to a group, handle transitions of care, and anticipate change in a group. In addition, the speakers participated in discussions where they shared their biggest successes and failures in practice as leaders and participated in a lightning round where they provided “off-the-cuff” responses to questions from Ms. Flores.
Although hospitalists did not create the current environment that is expanding their role in the health care system, they can position themselves to decide what the scope of their role is, said Dr. Nelson.
“What we should do is navigate our group through these changes in the way that’s going to be most effective for ourselves, the providers in our group, and our organization,” he said. “Those groups that try to dig their heels in or resist all change, they fail. . . and they frustrate themselves. So instead, if you engage in planning for changes in the scope of your practice, you have a chance to make it go the way you’d like it to go, and you’re going to be more satisfied.”
At Sunday’s HM19 pre-course “Oh, the Places We’ll Go! Practice Management Tools for Navigating the Changing Role of Your Hospital Medicine Group,” the theme was how to anticipate and embrace changing roles as hospital medicine groups are being asked to take on more responsibility.
“The scope of hospitalist practice is evolving rapidly, both clinically and in terms of all of the other things that hospitalists are being asked to do,” said Leslie Flores, MHA, SFHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., and course co-director, in an interview before the pre-course. “Our goals with this program are to help leaders position their hospitalist groups for success with this changing environment that they’re living in and the changing roles of hospitalists.”
In an audience poll at the beginning of the pre-course, attendees – a majority of whom were practicing hospitalists and managers of hospitalist groups – said their biggest challenge areas were related to compensation or workflows that have not evolved to match their changing role, and disagreements over who should admit patients.
One of the goals of the session was to give hospitalist leaders ideas to address these issues, which included information on how to implement better team-based care and interdisciplinary care models within their groups, as well as how to adjust their compensation, scheduling, and staffing models to prepare for this “new world of hospitalist medicine,” said Ms. Flores.
“One of the biggest sources of contention and stress that we see in hospitalist groups is that there’s just so much change, and it’s happening so rapidly, and people are having a hard time really figuring out how to deal with all of that,” she said.
The day began with John Nelson, MD, MHM, outlining the “Trends in Scope of Practice Evolution.” Dr. Nelson, a partner at Nelson Flores Hospital Medicine Consultants, medical director of Overlake Medical Center in Bellevue, Wash., and course co-director, said hospitalists are increasingly working more in outpatient care, post-acute care, and other specialty facilities. In addition, as group size increases, the likelihood a hospitalist group will be responsible for an observation or short stay unit increases, while a larger group is less likely to have a clinical responsibility for a code blue, cardiac arrest, or rapid response team.
Other topics in the pre-course focused on how to change the culture in a group to an environment where team members are empowered to ask questions or voice concerns, improve patient flow by removing reasons for delays in discharge, recruit the right team members to a group, handle transitions of care, and anticipate change in a group. In addition, the speakers participated in discussions where they shared their biggest successes and failures in practice as leaders and participated in a lightning round where they provided “off-the-cuff” responses to questions from Ms. Flores.
Although hospitalists did not create the current environment that is expanding their role in the health care system, they can position themselves to decide what the scope of their role is, said Dr. Nelson.
“What we should do is navigate our group through these changes in the way that’s going to be most effective for ourselves, the providers in our group, and our organization,” he said. “Those groups that try to dig their heels in or resist all change, they fail. . . and they frustrate themselves. So instead, if you engage in planning for changes in the scope of your practice, you have a chance to make it go the way you’d like it to go, and you’re going to be more satisfied.”
Syncope session showcases latest research and guidance for practice
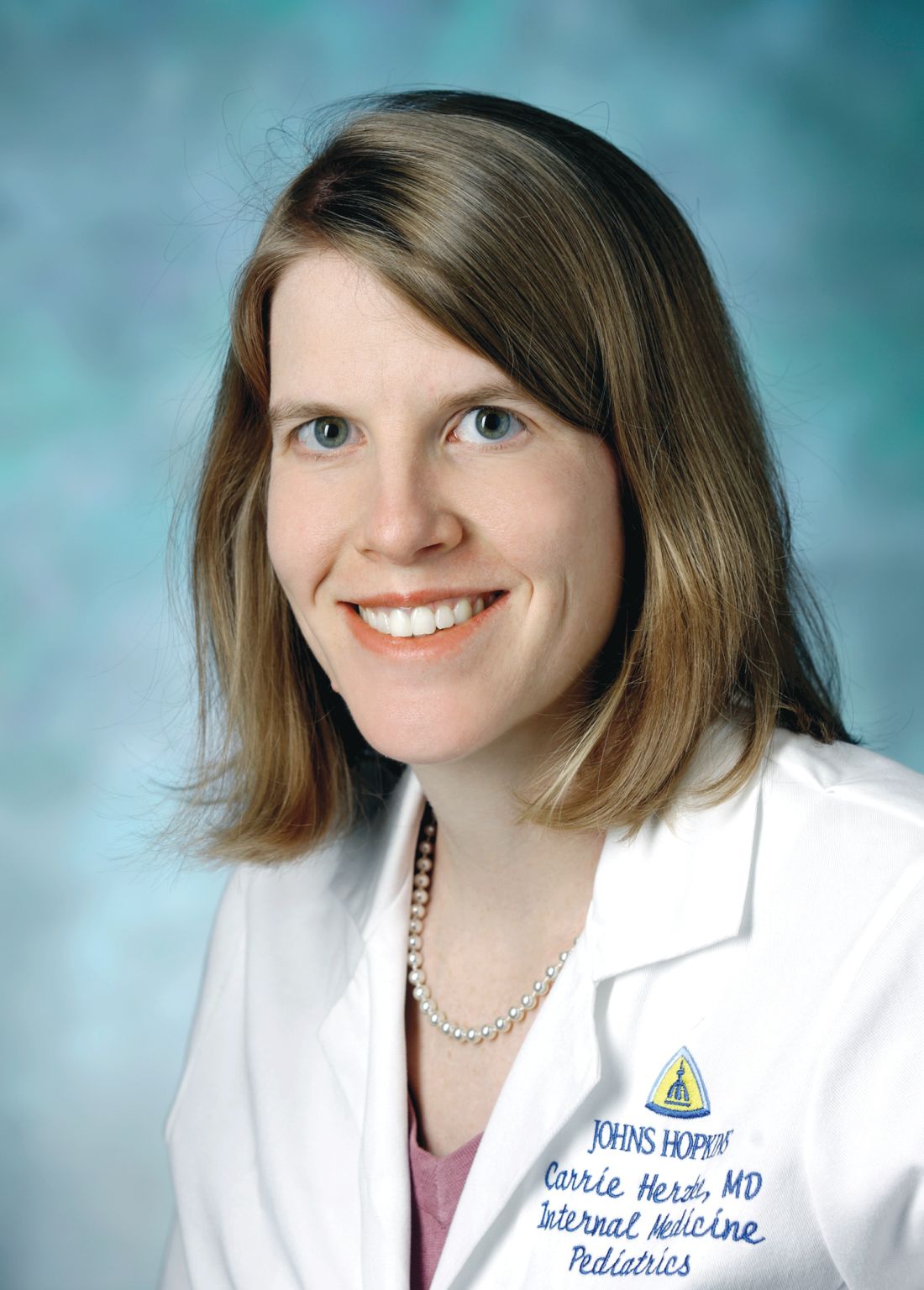
Syncope is a common problem, but an area in which practice likely varies by region and provider, according to Carrie Herzke, MD, SFHM, of Johns Hopkins University in Baltimore.
The variation in practice also suggests opportunities to safely cut costs, Dr. Herzke said in an interview.
Dr. Herzke will review the recent literature and summarize the current guidelines related to the treatment of syncope in her session, “SyncopE – Effective, Efficient and Economic Evaluations,” on Monday, March 25, at HM19.
“At the end of this session I am hopeful attendees will have a better understanding of the current guidelines, as well as which tests are most likely to be high value in the evaluation of syncope,” Dr. Herzke said. But before testing, clinicians should keep in mind that a history and physical examination are key components to evaluating syncope, she noted.
The European Society of Cardiology Guidelines for Syncope, published in 2018, feature several new concepts for evaluating and managing syncope in clinical settings and testing, including tilt testing, a greater role for prolonged ECG monitoring, use of video recording for suspected syncope, consideration of adenosine sensitive syncope, and consideration of neurological causes of syncope.
The ESC guidelines include using algorithms to determine the appropriate therapy for reflex syncope based on age, severity, and clinical forms. The guidelines also address diagnostic tests, monitoring in and out of the hospital, and treatment options including lifestyle changes and education as well as pharmacotherapy.
Dr. Herzke also will review the 2017 ACC/AHA/HRS Guideline for Patients With Syncope, published in 2017 in the journal Circulation. This guideline has an algorithm for initial evaluation of patients with syncope that includes a history, physical, and ECG. If the cause is known, patients should be assessed for risk and treated; syncope of unknown cause requires further evaluation, and the guideline presents recommendations for additional assessment through means including cardiac imaging, stress testing, blood testing, neurological testing, and tilt table testing.
“The selection of a given diagnostic test, after the initial history, physical examination, and baseline ECG, is a clinical decision based on the patient’s clinical presentation, risk stratification, and a clear understanding of diagnostic and prognostic value of any further testing,” according to the guideline authors.
The 2017 ACC/AHA/HRS Guideline for Patients With Syncope also provides recommendations for the management of cardiovascular conditions, including arrhythmic and structural conditions.
Dr. Herzke said she thinks that the topic of pulmonary embolism and syncope may prompt the liveliest discussion, and she will include several recent articles on this topic in her literature review.
“There has been some debate about how often PE is present in patients presenting after a syncopal episode,” she said. A recent study published in JAMA Internal Medicine found a prevalence of PE from 0.06% to 0.55% among all adults presenting to an ED with syncope and a prevalence of PE from 0.14% to 0.83%.
SyncopE – Effective, Efficient and Economic Evaluations
Monday 1:10 pm
Maryland BD/4-6
Syncope is a common problem, but an area in which practice likely varies by region and provider, according to Carrie Herzke, MD, SFHM, of Johns Hopkins University in Baltimore.
The variation in practice also suggests opportunities to safely cut costs, Dr. Herzke said in an interview.
Dr. Herzke will review the recent literature and summarize the current guidelines related to the treatment of syncope in her session, “SyncopE – Effective, Efficient and Economic Evaluations,” on Monday, March 25, at HM19.
“At the end of this session I am hopeful attendees will have a better understanding of the current guidelines, as well as which tests are most likely to be high value in the evaluation of syncope,” Dr. Herzke said. But before testing, clinicians should keep in mind that a history and physical examination are key components to evaluating syncope, she noted.
The European Society of Cardiology Guidelines for Syncope, published in 2018, feature several new concepts for evaluating and managing syncope in clinical settings and testing, including tilt testing, a greater role for prolonged ECG monitoring, use of video recording for suspected syncope, consideration of adenosine sensitive syncope, and consideration of neurological causes of syncope.
The ESC guidelines include using algorithms to determine the appropriate therapy for reflex syncope based on age, severity, and clinical forms. The guidelines also address diagnostic tests, monitoring in and out of the hospital, and treatment options including lifestyle changes and education as well as pharmacotherapy.
Dr. Herzke also will review the 2017 ACC/AHA/HRS Guideline for Patients With Syncope, published in 2017 in the journal Circulation. This guideline has an algorithm for initial evaluation of patients with syncope that includes a history, physical, and ECG. If the cause is known, patients should be assessed for risk and treated; syncope of unknown cause requires further evaluation, and the guideline presents recommendations for additional assessment through means including cardiac imaging, stress testing, blood testing, neurological testing, and tilt table testing.
“The selection of a given diagnostic test, after the initial history, physical examination, and baseline ECG, is a clinical decision based on the patient’s clinical presentation, risk stratification, and a clear understanding of diagnostic and prognostic value of any further testing,” according to the guideline authors.
The 2017 ACC/AHA/HRS Guideline for Patients With Syncope also provides recommendations for the management of cardiovascular conditions, including arrhythmic and structural conditions.
Dr. Herzke said she thinks that the topic of pulmonary embolism and syncope may prompt the liveliest discussion, and she will include several recent articles on this topic in her literature review.
“There has been some debate about how often PE is present in patients presenting after a syncopal episode,” she said. A recent study published in JAMA Internal Medicine found a prevalence of PE from 0.06% to 0.55% among all adults presenting to an ED with syncope and a prevalence of PE from 0.14% to 0.83%.
SyncopE – Effective, Efficient and Economic Evaluations
Monday 1:10 pm
Maryland BD/4-6
Syncope is a common problem, but an area in which practice likely varies by region and provider, according to Carrie Herzke, MD, SFHM, of Johns Hopkins University in Baltimore.
The variation in practice also suggests opportunities to safely cut costs, Dr. Herzke said in an interview.
Dr. Herzke will review the recent literature and summarize the current guidelines related to the treatment of syncope in her session, “SyncopE – Effective, Efficient and Economic Evaluations,” on Monday, March 25, at HM19.
“At the end of this session I am hopeful attendees will have a better understanding of the current guidelines, as well as which tests are most likely to be high value in the evaluation of syncope,” Dr. Herzke said. But before testing, clinicians should keep in mind that a history and physical examination are key components to evaluating syncope, she noted.
The European Society of Cardiology Guidelines for Syncope, published in 2018, feature several new concepts for evaluating and managing syncope in clinical settings and testing, including tilt testing, a greater role for prolonged ECG monitoring, use of video recording for suspected syncope, consideration of adenosine sensitive syncope, and consideration of neurological causes of syncope.
The ESC guidelines include using algorithms to determine the appropriate therapy for reflex syncope based on age, severity, and clinical forms. The guidelines also address diagnostic tests, monitoring in and out of the hospital, and treatment options including lifestyle changes and education as well as pharmacotherapy.
Dr. Herzke also will review the 2017 ACC/AHA/HRS Guideline for Patients With Syncope, published in 2017 in the journal Circulation. This guideline has an algorithm for initial evaluation of patients with syncope that includes a history, physical, and ECG. If the cause is known, patients should be assessed for risk and treated; syncope of unknown cause requires further evaluation, and the guideline presents recommendations for additional assessment through means including cardiac imaging, stress testing, blood testing, neurological testing, and tilt table testing.
“The selection of a given diagnostic test, after the initial history, physical examination, and baseline ECG, is a clinical decision based on the patient’s clinical presentation, risk stratification, and a clear understanding of diagnostic and prognostic value of any further testing,” according to the guideline authors.
The 2017 ACC/AHA/HRS Guideline for Patients With Syncope also provides recommendations for the management of cardiovascular conditions, including arrhythmic and structural conditions.
Dr. Herzke said she thinks that the topic of pulmonary embolism and syncope may prompt the liveliest discussion, and she will include several recent articles on this topic in her literature review.
“There has been some debate about how often PE is present in patients presenting after a syncopal episode,” she said. A recent study published in JAMA Internal Medicine found a prevalence of PE from 0.06% to 0.55% among all adults presenting to an ED with syncope and a prevalence of PE from 0.14% to 0.83%.
SyncopE – Effective, Efficient and Economic Evaluations
Monday 1:10 pm
Maryland BD/4-6
The past and future of hospital medicine
Challenges faced, and overcome
While I hope I’ll still be doing much the same work for many more years, I’m clearly at a stage of life that most of my career is behind me. So I guess it’s natural that I think about the past a little more than I used to. And one of the things that makes me smile is how I’m like George Costanza in The Comeback episode of “Seinfeld.”
In 1997 I had just delivered a presentation about what the future might hold for hospitalists to the roughly 110 attendees at the first in-person meeting of SHM (then known as the National Association of Inpatient Physicians). During the Q&A that followed, someone asked me what clinical content I would include in the hospitalist-specific test or board exam that I had speculated might be in our future. I took his tone and body language to suggest his main intent was to convey that I was crazy to think that such a test might ever be worthwhile.
A pregnant silence followed his question, after which I gave a tentative response that I worried made me sound dumb. So like George in “Seinfeld,” I continued to think about this, and days later came up with what I’m sure would have been a terrific comeback that would have gotten a robust laugh from the audience without being demeaning to the questioner. For the last 22 years I’ve been waiting for someone to ask me the same question so I can finally deliver my winner of a response.
There have been other missed opportunities, but when I think about the past and future of our field and our Society, I’m reminded of many past accomplishments and a promising future.
When Dr. Win Whitcomb and I founded SHM, I had the idea that, among its most important roles, would be serving as a forum for exchange of ideas among hospitalists and providing robust practice management resources for hospitalist groups. Through the efforts of so many people, including Angela Musial, the first SHM staff person, and so many other staff and members, we now have dozens of active special interest groups, informative publications, an active online discussion forum, and blogs. And our annual conference has grown a lot from that first meeting of 110 people; HM19 will bring together nearly 5,000 of us to educate, inspire, and support one another. Collectively, there are a lot of ideas being exchanged through SHM.
When SHM was brand new I had hope that it would grow. But I never guessed that hospital medicine would become the fastest-growing field in the history of U.S. health care.
I also never guessed that the term “nocturnist” would become a standard part of our field’s lexicon. I used it solely as a reliable way to get a laugh and find it really funny and delightful that it caught on.
And OB hospitalists? Neurohospitalists? I never saw these and the many other variations coming at all. But I see it as validating an idea first adopted by medicine and pediatrics. But dermatology hospitalists? Yep, that’s a thing too. The hospitalist model has been adopted, in at least a few places, by nearly every specialty in medicine.
And it is terrific that March 7, 2019, is the first National Hospitalist Day. SHM made this happen too.
I also think about the future of our field and see some pretty big challenges, though our past success as a field makes me confident we’ll navigate them effectively.
The burden of administrative, regulatory, and EHR-related tasks just keeps growing for hospitalists. This often means it is difficult or impossible see as many patients in a day as might have been reasonable in the past. In the near term, the only solution might be to reduce patient loads, but that isn’t a sustainable solution in the long term. I’m convinced we need to offload much of the work we do today that isn’t purely clinical, so that a typical hospitalist in the future can see more patients each day without working harder or longer.
I imagine a future in which the typical hospitalist goes home after seeing 20 or more patients in a day and isn’t completely exhausted and stressed, but sees it as a good day at work. I’m not sure exactly how we’ll get there, but it will probably include things like no longer having to devote any time or attention to whether the patient is inpatient or observation status, or whether they have had a qualifying 3-midnight stay so Medicare will cover a skilled nursing facility. I’m excited to see how this will evolve.
Dr. Nelson is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses.
Challenges faced, and overcome
Challenges faced, and overcome
While I hope I’ll still be doing much the same work for many more years, I’m clearly at a stage of life that most of my career is behind me. So I guess it’s natural that I think about the past a little more than I used to. And one of the things that makes me smile is how I’m like George Costanza in The Comeback episode of “Seinfeld.”
In 1997 I had just delivered a presentation about what the future might hold for hospitalists to the roughly 110 attendees at the first in-person meeting of SHM (then known as the National Association of Inpatient Physicians). During the Q&A that followed, someone asked me what clinical content I would include in the hospitalist-specific test or board exam that I had speculated might be in our future. I took his tone and body language to suggest his main intent was to convey that I was crazy to think that such a test might ever be worthwhile.
A pregnant silence followed his question, after which I gave a tentative response that I worried made me sound dumb. So like George in “Seinfeld,” I continued to think about this, and days later came up with what I’m sure would have been a terrific comeback that would have gotten a robust laugh from the audience without being demeaning to the questioner. For the last 22 years I’ve been waiting for someone to ask me the same question so I can finally deliver my winner of a response.
There have been other missed opportunities, but when I think about the past and future of our field and our Society, I’m reminded of many past accomplishments and a promising future.
When Dr. Win Whitcomb and I founded SHM, I had the idea that, among its most important roles, would be serving as a forum for exchange of ideas among hospitalists and providing robust practice management resources for hospitalist groups. Through the efforts of so many people, including Angela Musial, the first SHM staff person, and so many other staff and members, we now have dozens of active special interest groups, informative publications, an active online discussion forum, and blogs. And our annual conference has grown a lot from that first meeting of 110 people; HM19 will bring together nearly 5,000 of us to educate, inspire, and support one another. Collectively, there are a lot of ideas being exchanged through SHM.
When SHM was brand new I had hope that it would grow. But I never guessed that hospital medicine would become the fastest-growing field in the history of U.S. health care.
I also never guessed that the term “nocturnist” would become a standard part of our field’s lexicon. I used it solely as a reliable way to get a laugh and find it really funny and delightful that it caught on.
And OB hospitalists? Neurohospitalists? I never saw these and the many other variations coming at all. But I see it as validating an idea first adopted by medicine and pediatrics. But dermatology hospitalists? Yep, that’s a thing too. The hospitalist model has been adopted, in at least a few places, by nearly every specialty in medicine.
And it is terrific that March 7, 2019, is the first National Hospitalist Day. SHM made this happen too.
I also think about the future of our field and see some pretty big challenges, though our past success as a field makes me confident we’ll navigate them effectively.
The burden of administrative, regulatory, and EHR-related tasks just keeps growing for hospitalists. This often means it is difficult or impossible see as many patients in a day as might have been reasonable in the past. In the near term, the only solution might be to reduce patient loads, but that isn’t a sustainable solution in the long term. I’m convinced we need to offload much of the work we do today that isn’t purely clinical, so that a typical hospitalist in the future can see more patients each day without working harder or longer.
I imagine a future in which the typical hospitalist goes home after seeing 20 or more patients in a day and isn’t completely exhausted and stressed, but sees it as a good day at work. I’m not sure exactly how we’ll get there, but it will probably include things like no longer having to devote any time or attention to whether the patient is inpatient or observation status, or whether they have had a qualifying 3-midnight stay so Medicare will cover a skilled nursing facility. I’m excited to see how this will evolve.
Dr. Nelson is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses.
While I hope I’ll still be doing much the same work for many more years, I’m clearly at a stage of life that most of my career is behind me. So I guess it’s natural that I think about the past a little more than I used to. And one of the things that makes me smile is how I’m like George Costanza in The Comeback episode of “Seinfeld.”
In 1997 I had just delivered a presentation about what the future might hold for hospitalists to the roughly 110 attendees at the first in-person meeting of SHM (then known as the National Association of Inpatient Physicians). During the Q&A that followed, someone asked me what clinical content I would include in the hospitalist-specific test or board exam that I had speculated might be in our future. I took his tone and body language to suggest his main intent was to convey that I was crazy to think that such a test might ever be worthwhile.
A pregnant silence followed his question, after which I gave a tentative response that I worried made me sound dumb. So like George in “Seinfeld,” I continued to think about this, and days later came up with what I’m sure would have been a terrific comeback that would have gotten a robust laugh from the audience without being demeaning to the questioner. For the last 22 years I’ve been waiting for someone to ask me the same question so I can finally deliver my winner of a response.
There have been other missed opportunities, but when I think about the past and future of our field and our Society, I’m reminded of many past accomplishments and a promising future.
When Dr. Win Whitcomb and I founded SHM, I had the idea that, among its most important roles, would be serving as a forum for exchange of ideas among hospitalists and providing robust practice management resources for hospitalist groups. Through the efforts of so many people, including Angela Musial, the first SHM staff person, and so many other staff and members, we now have dozens of active special interest groups, informative publications, an active online discussion forum, and blogs. And our annual conference has grown a lot from that first meeting of 110 people; HM19 will bring together nearly 5,000 of us to educate, inspire, and support one another. Collectively, there are a lot of ideas being exchanged through SHM.
When SHM was brand new I had hope that it would grow. But I never guessed that hospital medicine would become the fastest-growing field in the history of U.S. health care.
I also never guessed that the term “nocturnist” would become a standard part of our field’s lexicon. I used it solely as a reliable way to get a laugh and find it really funny and delightful that it caught on.
And OB hospitalists? Neurohospitalists? I never saw these and the many other variations coming at all. But I see it as validating an idea first adopted by medicine and pediatrics. But dermatology hospitalists? Yep, that’s a thing too. The hospitalist model has been adopted, in at least a few places, by nearly every specialty in medicine.
And it is terrific that March 7, 2019, is the first National Hospitalist Day. SHM made this happen too.
I also think about the future of our field and see some pretty big challenges, though our past success as a field makes me confident we’ll navigate them effectively.
The burden of administrative, regulatory, and EHR-related tasks just keeps growing for hospitalists. This often means it is difficult or impossible see as many patients in a day as might have been reasonable in the past. In the near term, the only solution might be to reduce patient loads, but that isn’t a sustainable solution in the long term. I’m convinced we need to offload much of the work we do today that isn’t purely clinical, so that a typical hospitalist in the future can see more patients each day without working harder or longer.
I imagine a future in which the typical hospitalist goes home after seeing 20 or more patients in a day and isn’t completely exhausted and stressed, but sees it as a good day at work. I’m not sure exactly how we’ll get there, but it will probably include things like no longer having to devote any time or attention to whether the patient is inpatient or observation status, or whether they have had a qualifying 3-midnight stay so Medicare will cover a skilled nursing facility. I’m excited to see how this will evolve.
Dr. Nelson is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses.
FDA chief calls for stricter scrutiny of electronic health records
“What we really need is a much more tailored approach, so that we have appropriate oversight of EHRs when they’re doing things that could create risk for patients,” Dr. Gottlieb said in an interview with Kaiser Health News.
Dr. Gottlieb was responding to “Botched Operation,” a report published March 18 by KHN and Fortune magazine. The investigation found that the federal government has spent more than $36 billion over the past 10 years to switch doctors and hospitals from paper to digital records systems. In that time, thousands of reports of deaths, injuries, and near misses linked to EHRs have piled up in databases – including at least one run by the FDA.
Dr. Gottlieb said Congress would need to enact legislation to define when an EHR would require government oversight. He said that the digital records systems, which store a patient’s medical history, don’t fit neatly under the agency’s existing mandate to regulate items such as drugs and medical devices.
Dr. Gottlieb said the best approach might be to say that an EHR that has a certain capability becomes a medical device. He called EHRs a “unique tool,” noting that the risks posed by their use aren’t the same as for a traditional medical device implanted in a patient. “You need a much different regulatory scheme,” he said.
The 21st Century Cures Act of 2016 excludes the FDA from having oversight over EHRs as a medical device.
Dr. Gottlieb said that health IT companies could add new functions that would improve EHRs, but they have been reluctant to do so because they didn’t want their products to fall under FDA jurisdiction. He added that he was “not calling” for FDA to take over such a duty, however, and suggested that any new approach could be years away. Proponents have long argued that widespread use of EHRs can make medicine safer by alerting doctors to potential medical errors, though critics counter that software glitches and user errors may cause new varieties of medical mistakes.
How closely the FDA should watch over the digital medical record revolution has been controversial for years. The agency’s interest in the issue perked up after Congress decided in February 2009 to spend billions of dollars on digital medical records as part of an economic stimulus program.
At the time, many industry groups argued that FDA regulation would “stifle innovation” and stall the national drive to bring medicine into the modern era. Federal officials responsible for doling out billions in subsidies to doctors and hospitals generally sympathized with that view and were skeptical of allowing the FDA to play a role.
The debate became public in February 2010, when Jeffrey Shuren, MD, an FDA official, testified at a public hearing that the agency had tied 6 deaths and more than 200 injuries to health information technology. In all, the FDA said, it had logged 260 reports in the previous 2 years of “malfunctions with the potential for patient harm.”
The agency said the findings were based largely on reports voluntarily submitted to the FDA and suggested “significant clinical implications and public safety issues.” In one case cited, lab tests done in a hospital emergency department were sent to the wrong patient’s file. Since then, several government and private repositories have associated thousands of injuries, near misses, and deaths to EHR technology.
Dr. Shuren said in 2010 that the agency recognized that health information technology had great potential to improve patient care, but also needed oversight to “assure patient safety.”
While some safety proponents agree that EHRs offer tremendous benefits, they also see a greater opportunities to improve their safety.
Dean Sittig, PhD, a professor of bioinformatics and bioengineering at the University of Texas, Houston, said EHRs have improved safety within the health care system, but they have not eliminated errors to the extent that he would have expected. Federal officials were initially pushing for rapid adoption and ‘there wasn’t a lot of interest in talking about things that could go wrong,’ ” Dr. Sittig told KHN and Fortune.
Earlier in March, Gottlieb announced his resignation from the FDA. His last day is scheduled to be April 5.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente. KHN correspondents Sarah Jane Tribble, Sydney Lupkin, and Julie Rovner contributed to this report.
“What we really need is a much more tailored approach, so that we have appropriate oversight of EHRs when they’re doing things that could create risk for patients,” Dr. Gottlieb said in an interview with Kaiser Health News.
Dr. Gottlieb was responding to “Botched Operation,” a report published March 18 by KHN and Fortune magazine. The investigation found that the federal government has spent more than $36 billion over the past 10 years to switch doctors and hospitals from paper to digital records systems. In that time, thousands of reports of deaths, injuries, and near misses linked to EHRs have piled up in databases – including at least one run by the FDA.
Dr. Gottlieb said Congress would need to enact legislation to define when an EHR would require government oversight. He said that the digital records systems, which store a patient’s medical history, don’t fit neatly under the agency’s existing mandate to regulate items such as drugs and medical devices.
Dr. Gottlieb said the best approach might be to say that an EHR that has a certain capability becomes a medical device. He called EHRs a “unique tool,” noting that the risks posed by their use aren’t the same as for a traditional medical device implanted in a patient. “You need a much different regulatory scheme,” he said.
The 21st Century Cures Act of 2016 excludes the FDA from having oversight over EHRs as a medical device.
Dr. Gottlieb said that health IT companies could add new functions that would improve EHRs, but they have been reluctant to do so because they didn’t want their products to fall under FDA jurisdiction. He added that he was “not calling” for FDA to take over such a duty, however, and suggested that any new approach could be years away. Proponents have long argued that widespread use of EHRs can make medicine safer by alerting doctors to potential medical errors, though critics counter that software glitches and user errors may cause new varieties of medical mistakes.
How closely the FDA should watch over the digital medical record revolution has been controversial for years. The agency’s interest in the issue perked up after Congress decided in February 2009 to spend billions of dollars on digital medical records as part of an economic stimulus program.
At the time, many industry groups argued that FDA regulation would “stifle innovation” and stall the national drive to bring medicine into the modern era. Federal officials responsible for doling out billions in subsidies to doctors and hospitals generally sympathized with that view and were skeptical of allowing the FDA to play a role.
The debate became public in February 2010, when Jeffrey Shuren, MD, an FDA official, testified at a public hearing that the agency had tied 6 deaths and more than 200 injuries to health information technology. In all, the FDA said, it had logged 260 reports in the previous 2 years of “malfunctions with the potential for patient harm.”
The agency said the findings were based largely on reports voluntarily submitted to the FDA and suggested “significant clinical implications and public safety issues.” In one case cited, lab tests done in a hospital emergency department were sent to the wrong patient’s file. Since then, several government and private repositories have associated thousands of injuries, near misses, and deaths to EHR technology.
Dr. Shuren said in 2010 that the agency recognized that health information technology had great potential to improve patient care, but also needed oversight to “assure patient safety.”
While some safety proponents agree that EHRs offer tremendous benefits, they also see a greater opportunities to improve their safety.
Dean Sittig, PhD, a professor of bioinformatics and bioengineering at the University of Texas, Houston, said EHRs have improved safety within the health care system, but they have not eliminated errors to the extent that he would have expected. Federal officials were initially pushing for rapid adoption and ‘there wasn’t a lot of interest in talking about things that could go wrong,’ ” Dr. Sittig told KHN and Fortune.
Earlier in March, Gottlieb announced his resignation from the FDA. His last day is scheduled to be April 5.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente. KHN correspondents Sarah Jane Tribble, Sydney Lupkin, and Julie Rovner contributed to this report.
“What we really need is a much more tailored approach, so that we have appropriate oversight of EHRs when they’re doing things that could create risk for patients,” Dr. Gottlieb said in an interview with Kaiser Health News.
Dr. Gottlieb was responding to “Botched Operation,” a report published March 18 by KHN and Fortune magazine. The investigation found that the federal government has spent more than $36 billion over the past 10 years to switch doctors and hospitals from paper to digital records systems. In that time, thousands of reports of deaths, injuries, and near misses linked to EHRs have piled up in databases – including at least one run by the FDA.
Dr. Gottlieb said Congress would need to enact legislation to define when an EHR would require government oversight. He said that the digital records systems, which store a patient’s medical history, don’t fit neatly under the agency’s existing mandate to regulate items such as drugs and medical devices.
Dr. Gottlieb said the best approach might be to say that an EHR that has a certain capability becomes a medical device. He called EHRs a “unique tool,” noting that the risks posed by their use aren’t the same as for a traditional medical device implanted in a patient. “You need a much different regulatory scheme,” he said.
The 21st Century Cures Act of 2016 excludes the FDA from having oversight over EHRs as a medical device.
Dr. Gottlieb said that health IT companies could add new functions that would improve EHRs, but they have been reluctant to do so because they didn’t want their products to fall under FDA jurisdiction. He added that he was “not calling” for FDA to take over such a duty, however, and suggested that any new approach could be years away. Proponents have long argued that widespread use of EHRs can make medicine safer by alerting doctors to potential medical errors, though critics counter that software glitches and user errors may cause new varieties of medical mistakes.
How closely the FDA should watch over the digital medical record revolution has been controversial for years. The agency’s interest in the issue perked up after Congress decided in February 2009 to spend billions of dollars on digital medical records as part of an economic stimulus program.
At the time, many industry groups argued that FDA regulation would “stifle innovation” and stall the national drive to bring medicine into the modern era. Federal officials responsible for doling out billions in subsidies to doctors and hospitals generally sympathized with that view and were skeptical of allowing the FDA to play a role.
The debate became public in February 2010, when Jeffrey Shuren, MD, an FDA official, testified at a public hearing that the agency had tied 6 deaths and more than 200 injuries to health information technology. In all, the FDA said, it had logged 260 reports in the previous 2 years of “malfunctions with the potential for patient harm.”
The agency said the findings were based largely on reports voluntarily submitted to the FDA and suggested “significant clinical implications and public safety issues.” In one case cited, lab tests done in a hospital emergency department were sent to the wrong patient’s file. Since then, several government and private repositories have associated thousands of injuries, near misses, and deaths to EHR technology.
Dr. Shuren said in 2010 that the agency recognized that health information technology had great potential to improve patient care, but also needed oversight to “assure patient safety.”
While some safety proponents agree that EHRs offer tremendous benefits, they also see a greater opportunities to improve their safety.
Dean Sittig, PhD, a professor of bioinformatics and bioengineering at the University of Texas, Houston, said EHRs have improved safety within the health care system, but they have not eliminated errors to the extent that he would have expected. Federal officials were initially pushing for rapid adoption and ‘there wasn’t a lot of interest in talking about things that could go wrong,’ ” Dr. Sittig told KHN and Fortune.
Earlier in March, Gottlieb announced his resignation from the FDA. His last day is scheduled to be April 5.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente. KHN correspondents Sarah Jane Tribble, Sydney Lupkin, and Julie Rovner contributed to this report.
Hospitalists and PTs: Building strong relationships
Optimizing discharge disposition and longitudinal recovery
Sanctimonious, self-righteous, discharge saboteurs. These are just a few descriptors I’ve heard hospitalists use to describe my physical therapy (PT) colleagues.
These charged comments come mostly after a hospitalist reads therapy notes and encounters a contradiction to their chosen discharge location for a patient.
I recently met with hospitalists from four different hospitals. They echoed the frustrations of their physician colleagues across the country. The PTs they work with write “the patient requires 24-hour supervision and 3 hours of therapy a day,” or “the patient is unsafe to go home and needs continued therapy at an inpatient rehabilitation center.” The hospitalists in turn want to know “If I discharge the patient home am I liable if the patient falls or has some other negative outcome?” The frustration hospitalists experience is palpable and understandable as their attempts to support a home recovery are often contradicted.
Outside the four walls
The transition from fee-for-service to value-based care now calls upon hospitalists to be innovators in managing patients in alternative payment models, such as accountable care organizations, bundled payment programs, and Medicare Advantage plans. Each model looks to support a home recovery whenever possible and prevent readmissions.
Case managers for Medicare Advantage programs routinely review PT notes to inform hospital discharge disposition and post-acute authorization for skilled nursing facility (SNF) admissions and days in SNF. Hospitalists, working with care managers, can follow suit to succeed in alternative payment models. They have the advantage of in-person access to PT colleagues for elaboration and push-back as necessary. For hospitalists, working collaboratively with PTs is crucial to improving the value of care provided as patients transition beyond the four walls of the hospital.
The evolution of PT in acute care
Prior to diagnosis-related groups (DRGs), PTs were profit centers for hospitals – rehabilitation departments were well staffed and easily accommodated consults and requests for mobility.
With the advent of DRGs, physical therapy became a cost center, and rehabilitation staffs were reduced. PTs became overextended, were less available for consultations for mobilization, and patients suffered the deleterious effects of immobility. With reduced staffing and a rush to get patients out of the hospital, acute PT practice morphed into evaluating functional status and determining discharge destination.
Now, as members of an aligned health care team, PTs need to facilitate a safe home discharge whenever possible and determine what skilled services a patient needs post-acute stay, not where they should receive them.
Discharge disposition and longitudinal recovery
PTs, as experts in function, have a series of “special tests” at their disposal beyond pain, range of motion, and strength assessments. These include: Activity Measure for Post-Acute Care (AM-PAC) or “6-Clicks” Mobility Score, Timed Up and Go, Six-Minute Walk Test, Tinetti, Berg Balance Scale, Modified Barthel Index, Five Times Chair Rise, and Thirty-Second Chair Rise. These are all objective measures of function that can be used to inform discharge disposition and guide longitudinal recovery.
To elaborate on one tool, the 6-Clicks Mobility Score is a validated test that allows PTs to assess basic mobility.1,2 It rates six functional tasks (hence 6 clicks) that include: turning over in bed, moving from lying to sitting, moving to/from bed to chair, transitioning from sitting to standing from a chair, walking in a hospital room, and climbing three to five steps. These functional tasks are scored based on the amount of assistance needed. The scores, in turn, have been shown to support discharge destination planning.1 In addition to informing discharge destination decisions, hospitalists and the rest of the health care team can use 6-Clicks to estimate prolonged hospital stays, readmissions, and emergency department (ED) visits.3
Of course, discharge disposition is influenced by many factors in addition to functional status. Hospitalists are the obvious choice to lead the health care team in interpreting relevant data and test results, and to communicate these results to patients and caregivers so together they can decide the most appropriate discharge destination.
I envision a conversation between a fully informed hospitalist and a patient as follows: “Based on your past history, your living situation, all of your test results including labs, x-rays and the functional tests performed by your PT, your potential for a full recovery is good. You have a moderate decline in function with a high likelihood of returning home in the next 7-10 days. I recommend you go to a SNF for high-intensity rehabilitation for 7 days and that the SNF order PT and OT twice a day and walks with nursing every evening.”
This fully informed conversation can only take place if hospitalists are provided clear, concise documentation, including results of objective functional testing, by their physical therapy colleagues.
In conclusion, PTs working in the acute setting need to use validated tests to objectively assess function and educate their hospitalist colleagues on the meaning of these tests. Hospitalists in turn can incorporate these assessments into a discussion of discharge disposition and longitudinal recovery with patients. In this way, hospitalists and physical therapists can work together to achieve patient-centered, high-value care during and following a hospitalization.
Ms. Tammany is SVP of clinical strategy & innovation for Remedy Partners, Norwalk, Conn.
References
1. Jette DU et al. AM-PAC “6-Clicks” functional assessment scores predict acute care hospital discharge destination. Phys Ther. 2014 Sep;94(9):1252-61.
2. Jette DU et al. Validity of the AM-PAC “6-Clicks” inpatient daily activity and basic mobility short forms. Phys Ther. 2014 Mar;94(3):379-91.
3. Menendez ME et al. Does “6-Clicks” Day 1 Postoperative Mobility Score Predict Discharge Disposition After Total Hip and Knee Arthroplasties?” J Arthroplasty. 2016 Sep;31(9):1916-20.
Optimizing discharge disposition and longitudinal recovery
Optimizing discharge disposition and longitudinal recovery
Sanctimonious, self-righteous, discharge saboteurs. These are just a few descriptors I’ve heard hospitalists use to describe my physical therapy (PT) colleagues.
These charged comments come mostly after a hospitalist reads therapy notes and encounters a contradiction to their chosen discharge location for a patient.
I recently met with hospitalists from four different hospitals. They echoed the frustrations of their physician colleagues across the country. The PTs they work with write “the patient requires 24-hour supervision and 3 hours of therapy a day,” or “the patient is unsafe to go home and needs continued therapy at an inpatient rehabilitation center.” The hospitalists in turn want to know “If I discharge the patient home am I liable if the patient falls or has some other negative outcome?” The frustration hospitalists experience is palpable and understandable as their attempts to support a home recovery are often contradicted.
Outside the four walls
The transition from fee-for-service to value-based care now calls upon hospitalists to be innovators in managing patients in alternative payment models, such as accountable care organizations, bundled payment programs, and Medicare Advantage plans. Each model looks to support a home recovery whenever possible and prevent readmissions.
Case managers for Medicare Advantage programs routinely review PT notes to inform hospital discharge disposition and post-acute authorization for skilled nursing facility (SNF) admissions and days in SNF. Hospitalists, working with care managers, can follow suit to succeed in alternative payment models. They have the advantage of in-person access to PT colleagues for elaboration and push-back as necessary. For hospitalists, working collaboratively with PTs is crucial to improving the value of care provided as patients transition beyond the four walls of the hospital.
The evolution of PT in acute care
Prior to diagnosis-related groups (DRGs), PTs were profit centers for hospitals – rehabilitation departments were well staffed and easily accommodated consults and requests for mobility.
With the advent of DRGs, physical therapy became a cost center, and rehabilitation staffs were reduced. PTs became overextended, were less available for consultations for mobilization, and patients suffered the deleterious effects of immobility. With reduced staffing and a rush to get patients out of the hospital, acute PT practice morphed into evaluating functional status and determining discharge destination.
Now, as members of an aligned health care team, PTs need to facilitate a safe home discharge whenever possible and determine what skilled services a patient needs post-acute stay, not where they should receive them.
Discharge disposition and longitudinal recovery
PTs, as experts in function, have a series of “special tests” at their disposal beyond pain, range of motion, and strength assessments. These include: Activity Measure for Post-Acute Care (AM-PAC) or “6-Clicks” Mobility Score, Timed Up and Go, Six-Minute Walk Test, Tinetti, Berg Balance Scale, Modified Barthel Index, Five Times Chair Rise, and Thirty-Second Chair Rise. These are all objective measures of function that can be used to inform discharge disposition and guide longitudinal recovery.
To elaborate on one tool, the 6-Clicks Mobility Score is a validated test that allows PTs to assess basic mobility.1,2 It rates six functional tasks (hence 6 clicks) that include: turning over in bed, moving from lying to sitting, moving to/from bed to chair, transitioning from sitting to standing from a chair, walking in a hospital room, and climbing three to five steps. These functional tasks are scored based on the amount of assistance needed. The scores, in turn, have been shown to support discharge destination planning.1 In addition to informing discharge destination decisions, hospitalists and the rest of the health care team can use 6-Clicks to estimate prolonged hospital stays, readmissions, and emergency department (ED) visits.3
Of course, discharge disposition is influenced by many factors in addition to functional status. Hospitalists are the obvious choice to lead the health care team in interpreting relevant data and test results, and to communicate these results to patients and caregivers so together they can decide the most appropriate discharge destination.
I envision a conversation between a fully informed hospitalist and a patient as follows: “Based on your past history, your living situation, all of your test results including labs, x-rays and the functional tests performed by your PT, your potential for a full recovery is good. You have a moderate decline in function with a high likelihood of returning home in the next 7-10 days. I recommend you go to a SNF for high-intensity rehabilitation for 7 days and that the SNF order PT and OT twice a day and walks with nursing every evening.”
This fully informed conversation can only take place if hospitalists are provided clear, concise documentation, including results of objective functional testing, by their physical therapy colleagues.
In conclusion, PTs working in the acute setting need to use validated tests to objectively assess function and educate their hospitalist colleagues on the meaning of these tests. Hospitalists in turn can incorporate these assessments into a discussion of discharge disposition and longitudinal recovery with patients. In this way, hospitalists and physical therapists can work together to achieve patient-centered, high-value care during and following a hospitalization.
Ms. Tammany is SVP of clinical strategy & innovation for Remedy Partners, Norwalk, Conn.
References
1. Jette DU et al. AM-PAC “6-Clicks” functional assessment scores predict acute care hospital discharge destination. Phys Ther. 2014 Sep;94(9):1252-61.
2. Jette DU et al. Validity of the AM-PAC “6-Clicks” inpatient daily activity and basic mobility short forms. Phys Ther. 2014 Mar;94(3):379-91.
3. Menendez ME et al. Does “6-Clicks” Day 1 Postoperative Mobility Score Predict Discharge Disposition After Total Hip and Knee Arthroplasties?” J Arthroplasty. 2016 Sep;31(9):1916-20.
Sanctimonious, self-righteous, discharge saboteurs. These are just a few descriptors I’ve heard hospitalists use to describe my physical therapy (PT) colleagues.
These charged comments come mostly after a hospitalist reads therapy notes and encounters a contradiction to their chosen discharge location for a patient.
I recently met with hospitalists from four different hospitals. They echoed the frustrations of their physician colleagues across the country. The PTs they work with write “the patient requires 24-hour supervision and 3 hours of therapy a day,” or “the patient is unsafe to go home and needs continued therapy at an inpatient rehabilitation center.” The hospitalists in turn want to know “If I discharge the patient home am I liable if the patient falls or has some other negative outcome?” The frustration hospitalists experience is palpable and understandable as their attempts to support a home recovery are often contradicted.
Outside the four walls
The transition from fee-for-service to value-based care now calls upon hospitalists to be innovators in managing patients in alternative payment models, such as accountable care organizations, bundled payment programs, and Medicare Advantage plans. Each model looks to support a home recovery whenever possible and prevent readmissions.
Case managers for Medicare Advantage programs routinely review PT notes to inform hospital discharge disposition and post-acute authorization for skilled nursing facility (SNF) admissions and days in SNF. Hospitalists, working with care managers, can follow suit to succeed in alternative payment models. They have the advantage of in-person access to PT colleagues for elaboration and push-back as necessary. For hospitalists, working collaboratively with PTs is crucial to improving the value of care provided as patients transition beyond the four walls of the hospital.
The evolution of PT in acute care
Prior to diagnosis-related groups (DRGs), PTs were profit centers for hospitals – rehabilitation departments were well staffed and easily accommodated consults and requests for mobility.
With the advent of DRGs, physical therapy became a cost center, and rehabilitation staffs were reduced. PTs became overextended, were less available for consultations for mobilization, and patients suffered the deleterious effects of immobility. With reduced staffing and a rush to get patients out of the hospital, acute PT practice morphed into evaluating functional status and determining discharge destination.
Now, as members of an aligned health care team, PTs need to facilitate a safe home discharge whenever possible and determine what skilled services a patient needs post-acute stay, not where they should receive them.
Discharge disposition and longitudinal recovery
PTs, as experts in function, have a series of “special tests” at their disposal beyond pain, range of motion, and strength assessments. These include: Activity Measure for Post-Acute Care (AM-PAC) or “6-Clicks” Mobility Score, Timed Up and Go, Six-Minute Walk Test, Tinetti, Berg Balance Scale, Modified Barthel Index, Five Times Chair Rise, and Thirty-Second Chair Rise. These are all objective measures of function that can be used to inform discharge disposition and guide longitudinal recovery.
To elaborate on one tool, the 6-Clicks Mobility Score is a validated test that allows PTs to assess basic mobility.1,2 It rates six functional tasks (hence 6 clicks) that include: turning over in bed, moving from lying to sitting, moving to/from bed to chair, transitioning from sitting to standing from a chair, walking in a hospital room, and climbing three to five steps. These functional tasks are scored based on the amount of assistance needed. The scores, in turn, have been shown to support discharge destination planning.1 In addition to informing discharge destination decisions, hospitalists and the rest of the health care team can use 6-Clicks to estimate prolonged hospital stays, readmissions, and emergency department (ED) visits.3
Of course, discharge disposition is influenced by many factors in addition to functional status. Hospitalists are the obvious choice to lead the health care team in interpreting relevant data and test results, and to communicate these results to patients and caregivers so together they can decide the most appropriate discharge destination.
I envision a conversation between a fully informed hospitalist and a patient as follows: “Based on your past history, your living situation, all of your test results including labs, x-rays and the functional tests performed by your PT, your potential for a full recovery is good. You have a moderate decline in function with a high likelihood of returning home in the next 7-10 days. I recommend you go to a SNF for high-intensity rehabilitation for 7 days and that the SNF order PT and OT twice a day and walks with nursing every evening.”
This fully informed conversation can only take place if hospitalists are provided clear, concise documentation, including results of objective functional testing, by their physical therapy colleagues.
In conclusion, PTs working in the acute setting need to use validated tests to objectively assess function and educate their hospitalist colleagues on the meaning of these tests. Hospitalists in turn can incorporate these assessments into a discussion of discharge disposition and longitudinal recovery with patients. In this way, hospitalists and physical therapists can work together to achieve patient-centered, high-value care during and following a hospitalization.
Ms. Tammany is SVP of clinical strategy & innovation for Remedy Partners, Norwalk, Conn.
References
1. Jette DU et al. AM-PAC “6-Clicks” functional assessment scores predict acute care hospital discharge destination. Phys Ther. 2014 Sep;94(9):1252-61.
2. Jette DU et al. Validity of the AM-PAC “6-Clicks” inpatient daily activity and basic mobility short forms. Phys Ther. 2014 Mar;94(3):379-91.
3. Menendez ME et al. Does “6-Clicks” Day 1 Postoperative Mobility Score Predict Discharge Disposition After Total Hip and Knee Arthroplasties?” J Arthroplasty. 2016 Sep;31(9):1916-20.