User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Hydrocortisone-fludrocortisone cuts deaths in septic shock
Hydrocortisone in combination with fludrocortisone significantly reduced 90-day mortality in septic shock patients in a double-blind, randomized, controlled trial.
Prior to this study, two large trials had displayed that corticosteroids were beneficial in improving hemodynamic status and organ function, but little was known about corticosteroids’ ability to increase survival in sepsis patients.
The study, named the Activated Protein C and Corticosteroids for Human Septic Shock (APROCCHSS) trial, was designed to assess the benefit/risk ratio of using activated protein C – drotrecogin alfa (activated) – and corticosteroids together or separately in septic shock patients. The original design of the study included Xigris (drotrecogin alfa) and was composed of four parallel groups, but Xigris was removed from the market in October of 2011, so the study continued with only two parallel groups.
A total of 1,241 patients experiencing chronic septic shock were recruited into the two double-blind, parallel groups, with patients in one group receiving hydrocortisone plus fludrocortisone and the other receiving placebos. The placebos used in this study were similar in appearance to the actual treatment drugs. The placebos for hydrocortisone and fludrocortisone were either parenteral mannitol (133.6 mg), disodium phosphate (8.73 mg), and sodium phosphate (0.92 mg) or tablets of microcrystalline cellulose (59.098 mg), respectively.
Hydrocortisone was given intravenously every 6 hours as a 50-mg intravenous bolus, and fludrocortisone was given once a day as a 50-mcg tablet through a nasogastric tube. Patients in ICUs who had septic shock for less than 24 hours were included in the study. Septic shock was identified by the presence of a clinically or microbiologically documented infection, a Sequential Organ Failure Assessment score of 3 or 4 for at least two organs and for at least 6 hours, and receipt of vasopressor therapy for at least 6 hours.
After 90 days, 264 of 614 of the patients (43%) in the hydrocortisone/fludrocortisone group and almost half (49.1%) of 627 patients in the placebo group had died (P = .03). The relative risk of death was 0.88 (95% confidence interval, 0.78-0.99), which favored the hydrocortisone/fludrocortisone group. The researchers also observed that death was significantly lower in the hydrocortisone/fludrocortisone group, compared with the placebo group, at time of ICU discharge (35.4% vs. 41.0%, respectively; P = .04).
While mortality was reduced, patients still experienced adverse events. 326 of 614 (53.1%) patients in the hydrocortisone/fludrocortisone group and 363 of 626 patients (58.0%) in the placebo group experienced at least one serious adverse event by day 180 (P = 0.08).
“Seven-day treatment with a 50-mg intravenous bolus of hydrocortisone every 6 hours and a daily dose of 50 mcg of oral fludrocortisone resulted in lower mortality at day 90 and at ICU and hospital discharge than placebo among adults with septic shock,” concluded Dr. Annane and his coauthors.
The majority of researchers had no relevant financial disclosures to report, while some doctors received grants and personal fees unrelated to this study. This study was funded in part by public grants from the French Ministry of Health.
SOURCE: Annana A et al. NEJM. 2018 Feb 28. doi: 10.1056/NEJMoa1705716.
The results of the Activated Protein C and Corticosteroids for Human Septic Shock (APROCCHSS) trial and the Adjunctive Corticosteroid Treatment in Critically Ill Patients with Septic Shock (ADRENAL), both reported in the latest issue of NEJM, are landmark studies detailing the largest analyses of hydrocortisone use in patients with septic shock.
Both of these trials were massive, with over 5,000 patients combined, which is much larger than all previous studies according to Anthony Suffredini, MD, of the National Institutes of Health. An additional useful feature of these trials was that they had clear criteria for entry into the study. These criteria included: “vasopressor-dependent shock and respiratory failure leading to the use of mechanical ventilation, details of antimicrobial therapy, assessment of survival at 90 days, and well-defined secondary outcomes and analyses of adverse events.”
The ADRENAL and APROCCHSS had vastly different 90-day mortality rates: ADRENAL had mortality rates of 27.9% with hydrocortisone and 28.8% with placebo (P = .50), while APROACCHSS had mortality rates of 43.0% with hydrocortisone plus fludrocortisone and 49.1% with placebo (P = .03). Despite this, they both display the beneficial effect anti-inflammatory therapies, such as hydrocortisone, have on secondary outcomes of shock reversal and the reduction in duration of mechanical ventilation. “It is unlikely that in the near future sufficiently powered trials will provide us with better data” than the ADRENAL and APROCCHSS trials, Dr. Suffredini wrote.
Dr. Suffredini made these comments in an editorial accompanying this study in the New England Journal of Medicine. He is the deputy chief of the critical care medicine department at the National Institutes of Health Clinical Center, and he has served on the executive committee of the Department of Veteran Affairs Cooperative Studies Program. He has no other relevant financial disclosures to report.
The results of the Activated Protein C and Corticosteroids for Human Septic Shock (APROCCHSS) trial and the Adjunctive Corticosteroid Treatment in Critically Ill Patients with Septic Shock (ADRENAL), both reported in the latest issue of NEJM, are landmark studies detailing the largest analyses of hydrocortisone use in patients with septic shock.
Both of these trials were massive, with over 5,000 patients combined, which is much larger than all previous studies according to Anthony Suffredini, MD, of the National Institutes of Health. An additional useful feature of these trials was that they had clear criteria for entry into the study. These criteria included: “vasopressor-dependent shock and respiratory failure leading to the use of mechanical ventilation, details of antimicrobial therapy, assessment of survival at 90 days, and well-defined secondary outcomes and analyses of adverse events.”
The ADRENAL and APROCCHSS had vastly different 90-day mortality rates: ADRENAL had mortality rates of 27.9% with hydrocortisone and 28.8% with placebo (P = .50), while APROACCHSS had mortality rates of 43.0% with hydrocortisone plus fludrocortisone and 49.1% with placebo (P = .03). Despite this, they both display the beneficial effect anti-inflammatory therapies, such as hydrocortisone, have on secondary outcomes of shock reversal and the reduction in duration of mechanical ventilation. “It is unlikely that in the near future sufficiently powered trials will provide us with better data” than the ADRENAL and APROCCHSS trials, Dr. Suffredini wrote.
Dr. Suffredini made these comments in an editorial accompanying this study in the New England Journal of Medicine. He is the deputy chief of the critical care medicine department at the National Institutes of Health Clinical Center, and he has served on the executive committee of the Department of Veteran Affairs Cooperative Studies Program. He has no other relevant financial disclosures to report.
The results of the Activated Protein C and Corticosteroids for Human Septic Shock (APROCCHSS) trial and the Adjunctive Corticosteroid Treatment in Critically Ill Patients with Septic Shock (ADRENAL), both reported in the latest issue of NEJM, are landmark studies detailing the largest analyses of hydrocortisone use in patients with septic shock.
Both of these trials were massive, with over 5,000 patients combined, which is much larger than all previous studies according to Anthony Suffredini, MD, of the National Institutes of Health. An additional useful feature of these trials was that they had clear criteria for entry into the study. These criteria included: “vasopressor-dependent shock and respiratory failure leading to the use of mechanical ventilation, details of antimicrobial therapy, assessment of survival at 90 days, and well-defined secondary outcomes and analyses of adverse events.”
The ADRENAL and APROCCHSS had vastly different 90-day mortality rates: ADRENAL had mortality rates of 27.9% with hydrocortisone and 28.8% with placebo (P = .50), while APROACCHSS had mortality rates of 43.0% with hydrocortisone plus fludrocortisone and 49.1% with placebo (P = .03). Despite this, they both display the beneficial effect anti-inflammatory therapies, such as hydrocortisone, have on secondary outcomes of shock reversal and the reduction in duration of mechanical ventilation. “It is unlikely that in the near future sufficiently powered trials will provide us with better data” than the ADRENAL and APROCCHSS trials, Dr. Suffredini wrote.
Dr. Suffredini made these comments in an editorial accompanying this study in the New England Journal of Medicine. He is the deputy chief of the critical care medicine department at the National Institutes of Health Clinical Center, and he has served on the executive committee of the Department of Veteran Affairs Cooperative Studies Program. He has no other relevant financial disclosures to report.
Hydrocortisone in combination with fludrocortisone significantly reduced 90-day mortality in septic shock patients in a double-blind, randomized, controlled trial.
Prior to this study, two large trials had displayed that corticosteroids were beneficial in improving hemodynamic status and organ function, but little was known about corticosteroids’ ability to increase survival in sepsis patients.
The study, named the Activated Protein C and Corticosteroids for Human Septic Shock (APROCCHSS) trial, was designed to assess the benefit/risk ratio of using activated protein C – drotrecogin alfa (activated) – and corticosteroids together or separately in septic shock patients. The original design of the study included Xigris (drotrecogin alfa) and was composed of four parallel groups, but Xigris was removed from the market in October of 2011, so the study continued with only two parallel groups.
A total of 1,241 patients experiencing chronic septic shock were recruited into the two double-blind, parallel groups, with patients in one group receiving hydrocortisone plus fludrocortisone and the other receiving placebos. The placebos used in this study were similar in appearance to the actual treatment drugs. The placebos for hydrocortisone and fludrocortisone were either parenteral mannitol (133.6 mg), disodium phosphate (8.73 mg), and sodium phosphate (0.92 mg) or tablets of microcrystalline cellulose (59.098 mg), respectively.
Hydrocortisone was given intravenously every 6 hours as a 50-mg intravenous bolus, and fludrocortisone was given once a day as a 50-mcg tablet through a nasogastric tube. Patients in ICUs who had septic shock for less than 24 hours were included in the study. Septic shock was identified by the presence of a clinically or microbiologically documented infection, a Sequential Organ Failure Assessment score of 3 or 4 for at least two organs and for at least 6 hours, and receipt of vasopressor therapy for at least 6 hours.
After 90 days, 264 of 614 of the patients (43%) in the hydrocortisone/fludrocortisone group and almost half (49.1%) of 627 patients in the placebo group had died (P = .03). The relative risk of death was 0.88 (95% confidence interval, 0.78-0.99), which favored the hydrocortisone/fludrocortisone group. The researchers also observed that death was significantly lower in the hydrocortisone/fludrocortisone group, compared with the placebo group, at time of ICU discharge (35.4% vs. 41.0%, respectively; P = .04).
While mortality was reduced, patients still experienced adverse events. 326 of 614 (53.1%) patients in the hydrocortisone/fludrocortisone group and 363 of 626 patients (58.0%) in the placebo group experienced at least one serious adverse event by day 180 (P = 0.08).
“Seven-day treatment with a 50-mg intravenous bolus of hydrocortisone every 6 hours and a daily dose of 50 mcg of oral fludrocortisone resulted in lower mortality at day 90 and at ICU and hospital discharge than placebo among adults with septic shock,” concluded Dr. Annane and his coauthors.
The majority of researchers had no relevant financial disclosures to report, while some doctors received grants and personal fees unrelated to this study. This study was funded in part by public grants from the French Ministry of Health.
SOURCE: Annana A et al. NEJM. 2018 Feb 28. doi: 10.1056/NEJMoa1705716.
Hydrocortisone in combination with fludrocortisone significantly reduced 90-day mortality in septic shock patients in a double-blind, randomized, controlled trial.
Prior to this study, two large trials had displayed that corticosteroids were beneficial in improving hemodynamic status and organ function, but little was known about corticosteroids’ ability to increase survival in sepsis patients.
The study, named the Activated Protein C and Corticosteroids for Human Septic Shock (APROCCHSS) trial, was designed to assess the benefit/risk ratio of using activated protein C – drotrecogin alfa (activated) – and corticosteroids together or separately in septic shock patients. The original design of the study included Xigris (drotrecogin alfa) and was composed of four parallel groups, but Xigris was removed from the market in October of 2011, so the study continued with only two parallel groups.
A total of 1,241 patients experiencing chronic septic shock were recruited into the two double-blind, parallel groups, with patients in one group receiving hydrocortisone plus fludrocortisone and the other receiving placebos. The placebos used in this study were similar in appearance to the actual treatment drugs. The placebos for hydrocortisone and fludrocortisone were either parenteral mannitol (133.6 mg), disodium phosphate (8.73 mg), and sodium phosphate (0.92 mg) or tablets of microcrystalline cellulose (59.098 mg), respectively.
Hydrocortisone was given intravenously every 6 hours as a 50-mg intravenous bolus, and fludrocortisone was given once a day as a 50-mcg tablet through a nasogastric tube. Patients in ICUs who had septic shock for less than 24 hours were included in the study. Septic shock was identified by the presence of a clinically or microbiologically documented infection, a Sequential Organ Failure Assessment score of 3 or 4 for at least two organs and for at least 6 hours, and receipt of vasopressor therapy for at least 6 hours.
After 90 days, 264 of 614 of the patients (43%) in the hydrocortisone/fludrocortisone group and almost half (49.1%) of 627 patients in the placebo group had died (P = .03). The relative risk of death was 0.88 (95% confidence interval, 0.78-0.99), which favored the hydrocortisone/fludrocortisone group. The researchers also observed that death was significantly lower in the hydrocortisone/fludrocortisone group, compared with the placebo group, at time of ICU discharge (35.4% vs. 41.0%, respectively; P = .04).
While mortality was reduced, patients still experienced adverse events. 326 of 614 (53.1%) patients in the hydrocortisone/fludrocortisone group and 363 of 626 patients (58.0%) in the placebo group experienced at least one serious adverse event by day 180 (P = 0.08).
“Seven-day treatment with a 50-mg intravenous bolus of hydrocortisone every 6 hours and a daily dose of 50 mcg of oral fludrocortisone resulted in lower mortality at day 90 and at ICU and hospital discharge than placebo among adults with septic shock,” concluded Dr. Annane and his coauthors.
The majority of researchers had no relevant financial disclosures to report, while some doctors received grants and personal fees unrelated to this study. This study was funded in part by public grants from the French Ministry of Health.
SOURCE: Annana A et al. NEJM. 2018 Feb 28. doi: 10.1056/NEJMoa1705716.
FROM NEJM
Key clinical point: Hydrocortisone in combination with fludrocortisone significantly reduced 90-day mortality in septic shock patients.
Major finding: Mortality rates were lower in patients treated with hydrocortisone plus fludrocortisone, compared with patients treated with placebos (43% vs. 49.1%, respectively; P = .03).
Study details: A randomized, double-blind study of 1,241 patients with septic shock.
Disclosures: The majority of researchers had no relevant financial disclosures to report, while some doctors received grants and personal fees unrelated to this study. This study was funded in part by public grants from the French Ministry of Health.
Source: Annane A et al. NEJM. 2018 Feb 28. doi: 10.1056/NEJMoa1705716.
Increasing sepsis survivorship creates new challenges
SAN ANTONIO – , results of a retrospective, single-center analysis suggest.
The number of sepsis survivors at risk for hospital readmission rose substantially in recent years, according to the analysis of 17,256 adult medical and surgical admissions to University of Pennsylvania Health System hospitals between July 1, 2010, and June 30, 2015. The journal Critical Care Medicine published these results online as Mark E. Mikkelsen, MD, was presenting them at the Critical Care Congress sponsored by the Society for Critical Care Medicine.
Over the time period that Dr. Mikkelsen and his colleagues analyzed, the proportion of sepsis hospitalizations more than doubled from 3.9% to 9.4%, while in-hospital mortality rates for sepsis hospitalizations fell from 24.1% to 14.8%. As a result, the proportion of discharged patients at risk for readmission increased from 2.7% to 7.8%, noted Dr. Mikkelsen, associate professor of medicine at the Hospital of the University Of Pennsylvania, Philadelphia.
Thirty-day hospital readmission rates modestly declined from 26.4% to 23.1% over that time period, driven by reduced readmissions among survivors of nonsevere and nonpneumonia sepsis, Dr. Mikkelsen said. This decline in overall sepsis patient readmissions was offset by an increase in emergency department treat-and-release visits. Such visits rose from 2.8% in 2010 to a peak of 5.4% in 2014, Dr. Mikkelsen explained. Generally, readmission rates for severe sepsis patients have not changed over time, he added.
“I anticipate that each and every hospital represented in this room will experience a similar phenomenon,” he said. “Therefore, high quality postdischarge care is in fact urgently needed,” he added. “It is warranted that there is an international spotlight on sepsis beginning in the hospital but now continuing thereafter into the phase of life after sepsis.”
These findings reflect “great sepsis survivorship” and suggest new challenges to address, said Timothy G. Buchman, MD, PhD, editor-in-chief of the Critical Care Medicine and past president of the Society for Critical Care Medicine.
“It’s really extraordinary to see that the efforts that have been made by the Surviving Sepsis campaign have paid off,” Dr. Buchman said in an interview. “Now we need to look much more carefully at both the readmission issues, as well as the consequences of long-term sepsis survivorship, not just on patients, but also on their families.”
Dr. Mikkelsen and a study coauthor received support for article research from the National Institutes of Health.
SOURCE: Meyer N et al. Crit Care Med. 2018 Mar. doi: 10.1097/CCM. 0000000000002872.
SAN ANTONIO – , results of a retrospective, single-center analysis suggest.
The number of sepsis survivors at risk for hospital readmission rose substantially in recent years, according to the analysis of 17,256 adult medical and surgical admissions to University of Pennsylvania Health System hospitals between July 1, 2010, and June 30, 2015. The journal Critical Care Medicine published these results online as Mark E. Mikkelsen, MD, was presenting them at the Critical Care Congress sponsored by the Society for Critical Care Medicine.
Over the time period that Dr. Mikkelsen and his colleagues analyzed, the proportion of sepsis hospitalizations more than doubled from 3.9% to 9.4%, while in-hospital mortality rates for sepsis hospitalizations fell from 24.1% to 14.8%. As a result, the proportion of discharged patients at risk for readmission increased from 2.7% to 7.8%, noted Dr. Mikkelsen, associate professor of medicine at the Hospital of the University Of Pennsylvania, Philadelphia.
Thirty-day hospital readmission rates modestly declined from 26.4% to 23.1% over that time period, driven by reduced readmissions among survivors of nonsevere and nonpneumonia sepsis, Dr. Mikkelsen said. This decline in overall sepsis patient readmissions was offset by an increase in emergency department treat-and-release visits. Such visits rose from 2.8% in 2010 to a peak of 5.4% in 2014, Dr. Mikkelsen explained. Generally, readmission rates for severe sepsis patients have not changed over time, he added.
“I anticipate that each and every hospital represented in this room will experience a similar phenomenon,” he said. “Therefore, high quality postdischarge care is in fact urgently needed,” he added. “It is warranted that there is an international spotlight on sepsis beginning in the hospital but now continuing thereafter into the phase of life after sepsis.”
These findings reflect “great sepsis survivorship” and suggest new challenges to address, said Timothy G. Buchman, MD, PhD, editor-in-chief of the Critical Care Medicine and past president of the Society for Critical Care Medicine.
“It’s really extraordinary to see that the efforts that have been made by the Surviving Sepsis campaign have paid off,” Dr. Buchman said in an interview. “Now we need to look much more carefully at both the readmission issues, as well as the consequences of long-term sepsis survivorship, not just on patients, but also on their families.”
Dr. Mikkelsen and a study coauthor received support for article research from the National Institutes of Health.
SOURCE: Meyer N et al. Crit Care Med. 2018 Mar. doi: 10.1097/CCM. 0000000000002872.
SAN ANTONIO – , results of a retrospective, single-center analysis suggest.
The number of sepsis survivors at risk for hospital readmission rose substantially in recent years, according to the analysis of 17,256 adult medical and surgical admissions to University of Pennsylvania Health System hospitals between July 1, 2010, and June 30, 2015. The journal Critical Care Medicine published these results online as Mark E. Mikkelsen, MD, was presenting them at the Critical Care Congress sponsored by the Society for Critical Care Medicine.
Over the time period that Dr. Mikkelsen and his colleagues analyzed, the proportion of sepsis hospitalizations more than doubled from 3.9% to 9.4%, while in-hospital mortality rates for sepsis hospitalizations fell from 24.1% to 14.8%. As a result, the proportion of discharged patients at risk for readmission increased from 2.7% to 7.8%, noted Dr. Mikkelsen, associate professor of medicine at the Hospital of the University Of Pennsylvania, Philadelphia.
Thirty-day hospital readmission rates modestly declined from 26.4% to 23.1% over that time period, driven by reduced readmissions among survivors of nonsevere and nonpneumonia sepsis, Dr. Mikkelsen said. This decline in overall sepsis patient readmissions was offset by an increase in emergency department treat-and-release visits. Such visits rose from 2.8% in 2010 to a peak of 5.4% in 2014, Dr. Mikkelsen explained. Generally, readmission rates for severe sepsis patients have not changed over time, he added.
“I anticipate that each and every hospital represented in this room will experience a similar phenomenon,” he said. “Therefore, high quality postdischarge care is in fact urgently needed,” he added. “It is warranted that there is an international spotlight on sepsis beginning in the hospital but now continuing thereafter into the phase of life after sepsis.”
These findings reflect “great sepsis survivorship” and suggest new challenges to address, said Timothy G. Buchman, MD, PhD, editor-in-chief of the Critical Care Medicine and past president of the Society for Critical Care Medicine.
“It’s really extraordinary to see that the efforts that have been made by the Surviving Sepsis campaign have paid off,” Dr. Buchman said in an interview. “Now we need to look much more carefully at both the readmission issues, as well as the consequences of long-term sepsis survivorship, not just on patients, but also on their families.”
Dr. Mikkelsen and a study coauthor received support for article research from the National Institutes of Health.
SOURCE: Meyer N et al. Crit Care Med. 2018 Mar. doi: 10.1097/CCM. 0000000000002872.
AT CCC47
Key clinical point: An analysis of one center’s sepsis cases revealed increases in sepsis survivors at risk for hospital readmission and returns of these patients to the hospital via the emergency department.
Major finding: The proportion of medical and surgical discharges at risk for hospital readmission after sepsis grew from 2.7% to 7.8%. The modest decline in 30-day readmission rates was offset by an increase in emergency department treat-and-release visits.
Data source: A retrospective, observational cohort study of more than 17,000 adult medical and surgical admissions in an academic health care system from 2010 to 2015.
Disclosures: The National Institutes of Health supported the work.
Source: Meyer N et al. Crit Care Med. 2018 Mar. doi: 10.1097/CCM.0000000000002872.
Team engagement and motivation critical to QI success
Thomas McIlraith, MD, SFHM, CLHM, never imagined he would be leading hospitalists and launching quality improvement (QI) initiatives, but only one year out of residency, he was doing just that.
In 2000, Dr. McIlraith had spent a year working as a hospitalist at South Sacramento (Calif.) Kaiser Permanente when he was tapped for the QI program director role.
“Obviously I didn’t have a lot of preparation,” he said of that first job as director. “All of a sudden I found myself in charge of 15 hospitalists, … and I really didn’t know what I was getting myself into.”
But a passion for quality improvement – for striving to always find ways to do better – put Dr. McIlraith on that path and kept him on it through two terms as chair of the hospital medicine department of Mercy Medical Group in Sacramento, where he was hired in 2004. He completed his second term in June 2016 (the department quintupled in size during his tenure), and then chose to return to the ranks as a hospitalist focusing on patient care – and on spending time with his kids before they finished high school.
But quality improvement is in his blood, and he can see himself returning to it someday, Dr. McIlraith said.
“For me it was never about rising up in the ranks of leadership. It was really about making the world I exist in better,” he said.
In recounting some of the lessons he learned over the last 17 years, Dr. McIlraith recalled his first and all-time favorite quality initiative: Central Coordination. It was a concept he implemented around 2002 at Kaiser Permanante that fundamentally changed the way patients were admitted from the emergency department.
The previous system had separate admitting and rounding physicians, which lead to too many patient hand-offs, increased risk of mistakes, poor efficiency, and low patient satisfaction, he said.
“We actually took the job of distributing patients out of physicians’ hands altogether,” Dr. McIlraith explained.
Under Central Coordination, patient assignments were coordinated by a clerical staffer who distributed them evenly among a team of six doctors.
“The most amazing thing was that after this was implemented we went back and looked at ER responsiveness, and our ability to respond to the needs of the ER improved dramatically,” he said. “That wasn’t even an outcome I intended to impact, or look at, but the data were unequivocal. It ended up being really enduring and substantial on many fronts.”
Mercy Medical Group still uses Central Coordination systemwide, and the results of Dr. McIlraith’s initiative were eventually published.
“At the same time, due to my lack of experience in 2002, I definitely made some mistakes,” he said of the undertaking. Among them was failing to recognize just how resistant people can be to change. “I thought [the plan] was so brilliant that everyone would see that and get in line behind me,” he said. “Then I had a rude awakening that not everyone sees things the same way I do. I was completely taken aback by the resistance.”
Even though the existing system left a lot to be desired, the doctors were comfortable with it, Dr. McIlraith explained, stressing that implementing change requires the buy-in of team members.
If he could do it over again, he would follow the eight-step “Road Map for Change” as outlined by Jeffrey Glasheen, MD, SFHM, during the Society of Hospital Medicine’s Leadership Academy, Dr. McIlraith said.
Dr. Glasheen’s road map emphasizes team engagement and motivation, as well as the importance of creating a “burning platform” (the imperative for change).
“You need to be systematic about it to get people to change behaviors,” Dr. McIlraith said, noting that behavioral change is one of the greatest challenges and one of the leading causes of failure to attain the “holy grail” of quality improvement: sustained results.
In fact, the main reason for the enduring success of Central Coordination was that it took the focus off of behavioral change and put it on the process. “We took the behavior aspect out of the equation and put form over function,” Dr. McIlraith said.
One recent quality improvement initiative involved increasing the percentage of discharge orders delivered before 11 a.m. Dr. McIlraith put the lessons he learned to work by creating an “excellence team” that met regularly to identify key problems and to create “SMART (Specific, Measurable, Attainable, Relevant, and Timely) goals,” which are necessary for success.
Because the team not only bought into the plan to meet the target but also helped create the plan, it wasn’t necessary to force behavioral change, Dr. McIlraith said. Instead the team lead the initiative, set the targets and goals, and ended up surpassing the initial goal of reaching 30% of discharge orders in by 11 a.m. (in fact, they hit 40%).
Dr. McIlraith’s advice for QI success is to know the problem you are trying to solve so that you can tell if the solution you implement is having the desired impact and also to measure the impact of that solution using the SMART goals.
For those who hope to follow a quality improvement career path to leadership, he strongly recommends the Society of Hospital Medicine’s Leadership Academies, which are excellent resources for mentorship, networking, and leadership training through SHM.
Ultimately, Dr. McIlraith stressed the importance of mentoring team members for development as future QI leaders. If mentoring relationships are successful, then when the time comes for a QI veteran to “step back” to focus more on family or take a different career path, there will be others who can step in and keep the quality momentum going.
Thomas McIlraith, MD, SFHM, CLHM, never imagined he would be leading hospitalists and launching quality improvement (QI) initiatives, but only one year out of residency, he was doing just that.
In 2000, Dr. McIlraith had spent a year working as a hospitalist at South Sacramento (Calif.) Kaiser Permanente when he was tapped for the QI program director role.
“Obviously I didn’t have a lot of preparation,” he said of that first job as director. “All of a sudden I found myself in charge of 15 hospitalists, … and I really didn’t know what I was getting myself into.”
But a passion for quality improvement – for striving to always find ways to do better – put Dr. McIlraith on that path and kept him on it through two terms as chair of the hospital medicine department of Mercy Medical Group in Sacramento, where he was hired in 2004. He completed his second term in June 2016 (the department quintupled in size during his tenure), and then chose to return to the ranks as a hospitalist focusing on patient care – and on spending time with his kids before they finished high school.
But quality improvement is in his blood, and he can see himself returning to it someday, Dr. McIlraith said.
“For me it was never about rising up in the ranks of leadership. It was really about making the world I exist in better,” he said.
In recounting some of the lessons he learned over the last 17 years, Dr. McIlraith recalled his first and all-time favorite quality initiative: Central Coordination. It was a concept he implemented around 2002 at Kaiser Permanante that fundamentally changed the way patients were admitted from the emergency department.
The previous system had separate admitting and rounding physicians, which lead to too many patient hand-offs, increased risk of mistakes, poor efficiency, and low patient satisfaction, he said.
“We actually took the job of distributing patients out of physicians’ hands altogether,” Dr. McIlraith explained.
Under Central Coordination, patient assignments were coordinated by a clerical staffer who distributed them evenly among a team of six doctors.
“The most amazing thing was that after this was implemented we went back and looked at ER responsiveness, and our ability to respond to the needs of the ER improved dramatically,” he said. “That wasn’t even an outcome I intended to impact, or look at, but the data were unequivocal. It ended up being really enduring and substantial on many fronts.”
Mercy Medical Group still uses Central Coordination systemwide, and the results of Dr. McIlraith’s initiative were eventually published.
“At the same time, due to my lack of experience in 2002, I definitely made some mistakes,” he said of the undertaking. Among them was failing to recognize just how resistant people can be to change. “I thought [the plan] was so brilliant that everyone would see that and get in line behind me,” he said. “Then I had a rude awakening that not everyone sees things the same way I do. I was completely taken aback by the resistance.”
Even though the existing system left a lot to be desired, the doctors were comfortable with it, Dr. McIlraith explained, stressing that implementing change requires the buy-in of team members.
If he could do it over again, he would follow the eight-step “Road Map for Change” as outlined by Jeffrey Glasheen, MD, SFHM, during the Society of Hospital Medicine’s Leadership Academy, Dr. McIlraith said.
Dr. Glasheen’s road map emphasizes team engagement and motivation, as well as the importance of creating a “burning platform” (the imperative for change).
“You need to be systematic about it to get people to change behaviors,” Dr. McIlraith said, noting that behavioral change is one of the greatest challenges and one of the leading causes of failure to attain the “holy grail” of quality improvement: sustained results.
In fact, the main reason for the enduring success of Central Coordination was that it took the focus off of behavioral change and put it on the process. “We took the behavior aspect out of the equation and put form over function,” Dr. McIlraith said.
One recent quality improvement initiative involved increasing the percentage of discharge orders delivered before 11 a.m. Dr. McIlraith put the lessons he learned to work by creating an “excellence team” that met regularly to identify key problems and to create “SMART (Specific, Measurable, Attainable, Relevant, and Timely) goals,” which are necessary for success.
Because the team not only bought into the plan to meet the target but also helped create the plan, it wasn’t necessary to force behavioral change, Dr. McIlraith said. Instead the team lead the initiative, set the targets and goals, and ended up surpassing the initial goal of reaching 30% of discharge orders in by 11 a.m. (in fact, they hit 40%).
Dr. McIlraith’s advice for QI success is to know the problem you are trying to solve so that you can tell if the solution you implement is having the desired impact and also to measure the impact of that solution using the SMART goals.
For those who hope to follow a quality improvement career path to leadership, he strongly recommends the Society of Hospital Medicine’s Leadership Academies, which are excellent resources for mentorship, networking, and leadership training through SHM.
Ultimately, Dr. McIlraith stressed the importance of mentoring team members for development as future QI leaders. If mentoring relationships are successful, then when the time comes for a QI veteran to “step back” to focus more on family or take a different career path, there will be others who can step in and keep the quality momentum going.
Thomas McIlraith, MD, SFHM, CLHM, never imagined he would be leading hospitalists and launching quality improvement (QI) initiatives, but only one year out of residency, he was doing just that.
In 2000, Dr. McIlraith had spent a year working as a hospitalist at South Sacramento (Calif.) Kaiser Permanente when he was tapped for the QI program director role.
“Obviously I didn’t have a lot of preparation,” he said of that first job as director. “All of a sudden I found myself in charge of 15 hospitalists, … and I really didn’t know what I was getting myself into.”
But a passion for quality improvement – for striving to always find ways to do better – put Dr. McIlraith on that path and kept him on it through two terms as chair of the hospital medicine department of Mercy Medical Group in Sacramento, where he was hired in 2004. He completed his second term in June 2016 (the department quintupled in size during his tenure), and then chose to return to the ranks as a hospitalist focusing on patient care – and on spending time with his kids before they finished high school.
But quality improvement is in his blood, and he can see himself returning to it someday, Dr. McIlraith said.
“For me it was never about rising up in the ranks of leadership. It was really about making the world I exist in better,” he said.
In recounting some of the lessons he learned over the last 17 years, Dr. McIlraith recalled his first and all-time favorite quality initiative: Central Coordination. It was a concept he implemented around 2002 at Kaiser Permanante that fundamentally changed the way patients were admitted from the emergency department.
The previous system had separate admitting and rounding physicians, which lead to too many patient hand-offs, increased risk of mistakes, poor efficiency, and low patient satisfaction, he said.
“We actually took the job of distributing patients out of physicians’ hands altogether,” Dr. McIlraith explained.
Under Central Coordination, patient assignments were coordinated by a clerical staffer who distributed them evenly among a team of six doctors.
“The most amazing thing was that after this was implemented we went back and looked at ER responsiveness, and our ability to respond to the needs of the ER improved dramatically,” he said. “That wasn’t even an outcome I intended to impact, or look at, but the data were unequivocal. It ended up being really enduring and substantial on many fronts.”
Mercy Medical Group still uses Central Coordination systemwide, and the results of Dr. McIlraith’s initiative were eventually published.
“At the same time, due to my lack of experience in 2002, I definitely made some mistakes,” he said of the undertaking. Among them was failing to recognize just how resistant people can be to change. “I thought [the plan] was so brilliant that everyone would see that and get in line behind me,” he said. “Then I had a rude awakening that not everyone sees things the same way I do. I was completely taken aback by the resistance.”
Even though the existing system left a lot to be desired, the doctors were comfortable with it, Dr. McIlraith explained, stressing that implementing change requires the buy-in of team members.
If he could do it over again, he would follow the eight-step “Road Map for Change” as outlined by Jeffrey Glasheen, MD, SFHM, during the Society of Hospital Medicine’s Leadership Academy, Dr. McIlraith said.
Dr. Glasheen’s road map emphasizes team engagement and motivation, as well as the importance of creating a “burning platform” (the imperative for change).
“You need to be systematic about it to get people to change behaviors,” Dr. McIlraith said, noting that behavioral change is one of the greatest challenges and one of the leading causes of failure to attain the “holy grail” of quality improvement: sustained results.
In fact, the main reason for the enduring success of Central Coordination was that it took the focus off of behavioral change and put it on the process. “We took the behavior aspect out of the equation and put form over function,” Dr. McIlraith said.
One recent quality improvement initiative involved increasing the percentage of discharge orders delivered before 11 a.m. Dr. McIlraith put the lessons he learned to work by creating an “excellence team” that met regularly to identify key problems and to create “SMART (Specific, Measurable, Attainable, Relevant, and Timely) goals,” which are necessary for success.
Because the team not only bought into the plan to meet the target but also helped create the plan, it wasn’t necessary to force behavioral change, Dr. McIlraith said. Instead the team lead the initiative, set the targets and goals, and ended up surpassing the initial goal of reaching 30% of discharge orders in by 11 a.m. (in fact, they hit 40%).
Dr. McIlraith’s advice for QI success is to know the problem you are trying to solve so that you can tell if the solution you implement is having the desired impact and also to measure the impact of that solution using the SMART goals.
For those who hope to follow a quality improvement career path to leadership, he strongly recommends the Society of Hospital Medicine’s Leadership Academies, which are excellent resources for mentorship, networking, and leadership training through SHM.
Ultimately, Dr. McIlraith stressed the importance of mentoring team members for development as future QI leaders. If mentoring relationships are successful, then when the time comes for a QI veteran to “step back” to focus more on family or take a different career path, there will be others who can step in and keep the quality momentum going.
Preoperative penicillin allergy tests could decrease SSI
Patients with reported penicillin allergies are significantly more likely to develop surgical site infections, according to a study conducted at Massachusetts General Hospital in Boston.
With new evidence reporting 90%-99% of patients with a reported allergy are not actually allergic, conducting a preoperative allergy test could improve treatment choice and decrease the risk of SSI, as well as the notable financial burden associated with it. Thus, “systematic, preoperative penicillin allergy evaluations in surgical patients may not only improve antibiotic choice but also decrease SSI risk,” according to Kimberly Blumenthal, MD, the quality director for the department of allergy and immunology at Massachusetts General Hospital, and her fellow investigators.
Surgeries performed were hip arthroplasty, knee arthroplasty, hysterectomy, colon surgery, or coronary artery bypass grafting.
Of the patients studied, 922 (11%) reported a penicillin allergy; most had minor reactions, such as rashes (37.5%) or urticaria (18%). “Only 5 reactions to penicillin represented contraindications to receiving a beta-lactam; the vast majority of patients would have tolerated first-line recommended cephalosporin prophylaxis had allergy evaluation been pursued,“ according to Dr. Blumenthal and her colleagues.
Overall, a total of 241 (2.7%) patients contracted an SSI. In a multivariate analysis, patients who had reported a penicillin allergy were 50% more likely to develop an SSI than those who had no reported allergy (adjusted odds ratio, 1.5; P = .04).
Risk may even be higher than 50% in the general health care population because this health center has a relatively low rate of SSIs, compared with many other hospitals, Dr. Blumenthal and her fellow investigators stated.
The increased risk primarily concerns the treatment used because those with a reported allergy were more likely than those without the allergy to be given clindamycin (48.8% vs. 3.1%, respectively), vancomycin (34.7% vs. 3.3%), gentamicin (24% vs. 2.8%), or fluoroquinolones (6.8% vs. 1.3%) instead of the most commonly used antibiotic, cefazolin (12.2% vs. 92.4%).
Patients given antibiotics other than cefazolin were usually given treatment outside of the perioperative window, which could severely increase the likelihood for developing an SSI, according to investigators. Of patients given vancomycin, 97.5% did not receive their treatment in the recommended time frame, compared with 1.7% of those given cefazolin.
“Increased odds of SSI among patients reporting a penicillin allergy in this cohort was entirely due to the use of beta-lactam–alternative perioperative antibiotics,” wrote to Dr. Blumenthal and her colleagues. “Patients with reported penicillin allergy in this study were not only less likely to receive the most effective perioperative antibiotic, they were also less likely to receive prophylaxis in the recommended time frame for optimal tissue concentration.”
While allergy assessments before surgery are currently recommended, there are no specifically outlined methods for these evaluations, which leads many providers to take what has been deemed the safer route of giving patients beta-lactam–alternative antibiotics instead, Dr. Blumenthal and her colleagues suggested.
The research was supported by the National Institutes of Health, and the investigators reported having no relevant conflicts.
SOURCE: Blumenthal K et al. Clin Infect Dis. 2018 Jan 18;66(3):329-36.
Patients with reported penicillin allergies are significantly more likely to develop surgical site infections, according to a study conducted at Massachusetts General Hospital in Boston.
With new evidence reporting 90%-99% of patients with a reported allergy are not actually allergic, conducting a preoperative allergy test could improve treatment choice and decrease the risk of SSI, as well as the notable financial burden associated with it. Thus, “systematic, preoperative penicillin allergy evaluations in surgical patients may not only improve antibiotic choice but also decrease SSI risk,” according to Kimberly Blumenthal, MD, the quality director for the department of allergy and immunology at Massachusetts General Hospital, and her fellow investigators.
Surgeries performed were hip arthroplasty, knee arthroplasty, hysterectomy, colon surgery, or coronary artery bypass grafting.
Of the patients studied, 922 (11%) reported a penicillin allergy; most had minor reactions, such as rashes (37.5%) or urticaria (18%). “Only 5 reactions to penicillin represented contraindications to receiving a beta-lactam; the vast majority of patients would have tolerated first-line recommended cephalosporin prophylaxis had allergy evaluation been pursued,“ according to Dr. Blumenthal and her colleagues.
Overall, a total of 241 (2.7%) patients contracted an SSI. In a multivariate analysis, patients who had reported a penicillin allergy were 50% more likely to develop an SSI than those who had no reported allergy (adjusted odds ratio, 1.5; P = .04).
Risk may even be higher than 50% in the general health care population because this health center has a relatively low rate of SSIs, compared with many other hospitals, Dr. Blumenthal and her fellow investigators stated.
The increased risk primarily concerns the treatment used because those with a reported allergy were more likely than those without the allergy to be given clindamycin (48.8% vs. 3.1%, respectively), vancomycin (34.7% vs. 3.3%), gentamicin (24% vs. 2.8%), or fluoroquinolones (6.8% vs. 1.3%) instead of the most commonly used antibiotic, cefazolin (12.2% vs. 92.4%).
Patients given antibiotics other than cefazolin were usually given treatment outside of the perioperative window, which could severely increase the likelihood for developing an SSI, according to investigators. Of patients given vancomycin, 97.5% did not receive their treatment in the recommended time frame, compared with 1.7% of those given cefazolin.
“Increased odds of SSI among patients reporting a penicillin allergy in this cohort was entirely due to the use of beta-lactam–alternative perioperative antibiotics,” wrote to Dr. Blumenthal and her colleagues. “Patients with reported penicillin allergy in this study were not only less likely to receive the most effective perioperative antibiotic, they were also less likely to receive prophylaxis in the recommended time frame for optimal tissue concentration.”
While allergy assessments before surgery are currently recommended, there are no specifically outlined methods for these evaluations, which leads many providers to take what has been deemed the safer route of giving patients beta-lactam–alternative antibiotics instead, Dr. Blumenthal and her colleagues suggested.
The research was supported by the National Institutes of Health, and the investigators reported having no relevant conflicts.
SOURCE: Blumenthal K et al. Clin Infect Dis. 2018 Jan 18;66(3):329-36.
Patients with reported penicillin allergies are significantly more likely to develop surgical site infections, according to a study conducted at Massachusetts General Hospital in Boston.
With new evidence reporting 90%-99% of patients with a reported allergy are not actually allergic, conducting a preoperative allergy test could improve treatment choice and decrease the risk of SSI, as well as the notable financial burden associated with it. Thus, “systematic, preoperative penicillin allergy evaluations in surgical patients may not only improve antibiotic choice but also decrease SSI risk,” according to Kimberly Blumenthal, MD, the quality director for the department of allergy and immunology at Massachusetts General Hospital, and her fellow investigators.
Surgeries performed were hip arthroplasty, knee arthroplasty, hysterectomy, colon surgery, or coronary artery bypass grafting.
Of the patients studied, 922 (11%) reported a penicillin allergy; most had minor reactions, such as rashes (37.5%) or urticaria (18%). “Only 5 reactions to penicillin represented contraindications to receiving a beta-lactam; the vast majority of patients would have tolerated first-line recommended cephalosporin prophylaxis had allergy evaluation been pursued,“ according to Dr. Blumenthal and her colleagues.
Overall, a total of 241 (2.7%) patients contracted an SSI. In a multivariate analysis, patients who had reported a penicillin allergy were 50% more likely to develop an SSI than those who had no reported allergy (adjusted odds ratio, 1.5; P = .04).
Risk may even be higher than 50% in the general health care population because this health center has a relatively low rate of SSIs, compared with many other hospitals, Dr. Blumenthal and her fellow investigators stated.
The increased risk primarily concerns the treatment used because those with a reported allergy were more likely than those without the allergy to be given clindamycin (48.8% vs. 3.1%, respectively), vancomycin (34.7% vs. 3.3%), gentamicin (24% vs. 2.8%), or fluoroquinolones (6.8% vs. 1.3%) instead of the most commonly used antibiotic, cefazolin (12.2% vs. 92.4%).
Patients given antibiotics other than cefazolin were usually given treatment outside of the perioperative window, which could severely increase the likelihood for developing an SSI, according to investigators. Of patients given vancomycin, 97.5% did not receive their treatment in the recommended time frame, compared with 1.7% of those given cefazolin.
“Increased odds of SSI among patients reporting a penicillin allergy in this cohort was entirely due to the use of beta-lactam–alternative perioperative antibiotics,” wrote to Dr. Blumenthal and her colleagues. “Patients with reported penicillin allergy in this study were not only less likely to receive the most effective perioperative antibiotic, they were also less likely to receive prophylaxis in the recommended time frame for optimal tissue concentration.”
While allergy assessments before surgery are currently recommended, there are no specifically outlined methods for these evaluations, which leads many providers to take what has been deemed the safer route of giving patients beta-lactam–alternative antibiotics instead, Dr. Blumenthal and her colleagues suggested.
The research was supported by the National Institutes of Health, and the investigators reported having no relevant conflicts.
SOURCE: Blumenthal K et al. Clin Infect Dis. 2018 Jan 18;66(3):329-36.
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point: Patients with reported penicillin allergies are at higher risk of developing a surgical site infection.
Major finding: Having a penicillin allergy was associated with a 50% increased risk of developing a surgical site infection, compared with those without the allergy (adjusted odds ratio, 1.5; P = .04).
Study details: Retrospective cohort study of 8,385 patients operated on at Massachusetts General Hospital, Boston, during 2010-2014.
Disclosures: The research was supported by the National Institutes of Health, and the investigators reported having no relevant conflicts.
Source: Blumenthal K et al. Clin Infect Dis. 2018 Jan 18;66(3):329-36.
How should electrolyte abnormalities be managed in patients with chronic kidney disease?
Case
A 55-year-old woman with diabetes, hypertension, and chronic kidney disease (CKD) stage 4 is admitted to the hospital for treatment of left lower-extremity cellulitis. Laboratory studies on admission show a creatinine level of 2.5 mg/dL (glomerular filtration rate [GFR] is 20 mL/min per 1.73 m2; baseline creatinine is between 2.2 and 2.6 mg/dL), potassium level of 3.0 mEq/L, magnesium level of 1.5 mEq/L, bicarbonate level of 18 mEq/L, phosphate level of 6.5 mg/dL, and calcium level of 7.5 mg/dL.
She is put on renally dosed vancomycin to treat her cellulitis. As the hospitalist, how should you manage her multiple electrolyte abnormalities?
Overview of the issue
CKD is also an important risk factor for acute kidney injury. Additionally, rates of readmission for CKD patients are higher than those without CKD. Given that CKD is a “silent disease” that many patients do not realize they have, it is very possible that the first documentation of CKD could happen during an acute hospitalization.
Among the various manifestations of CKD, electrolyte abnormalities are the most likely ones hospitalists will run into.
Overview of the data
Hypokalemia and Hypomagnesemia
Hypokalemia (potassium levels less than 3.5 mEq/L) is not as common as hyperkalemia (potassium levels greater than 5.0 mEq/L) in CKD, which is the result of impaired renal excretion of potassium. Hypokalemia can occur as a result of GI losses, urinary losses, or decreased intake and can be worsened by the use of certain drugs, such as non–K-sparing diuretics.
In the setting of diuretic use involving thiazides and loop diuretics, hypokalemia is dose and sodium-intake dependent. Potassium deficiency worsens the effects of detrimental sodium excess, which plays a role in hypertension and its associated complications. Potassium also has a protective vascular effect, which is a major reason why potassium should be kept normal in patients with CKD.
Acutely, hypokalemia can cause arrhythmias, ileus, and paralysis, which are all indications for immediate repletion. In these cases, hypokalemia must be repleted carefully in small increments (some suggest 20 mEq doses), and the patient must be monitored frequently to avoid hyperkalemia. If patients are persistently hypokalemic, several options can be considered based on the underlying cause. Dietary modifications with foods rich in potassium (containing 250mg/100g) can be suggested. Daily potassium chloride supplementation can be used in those on diuretic therapy who have hypokalemia and metabolic alkalosis (bicarbonate levels greater than 30 mEq/L). Alkalinizing salts, containing citrate or bicarbonate, can be used in hypokalemia without metabolic alkalosis. Initiation of angiotensin-converting-enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta-adrenergic blockers, and K-sparing diuretics can be used as well.
Potassium supplementation and K-sparing diuretics should be used with extreme caution in CKD 3 and 4 given the risk of overcorrection. If potassium supplements or drugs to raise serum potassium are initiated in house, potassium should be rechecked within a week. These treatments should be avoided in individuals with diabetes, who are at highest risk for hyperkalemia given hyporeninemic hypoaldosteronism (type IV renal tubular acidosis).
There is emerging evidence that hypomagnesemia can play a part in progression to end-stage renal disease. In the setting of cardiovascular disease, which often co-exists with CKD, the risk of hypomagnesemia precipitating arrhythmia necessitates repletion to a normal level. Any of the magnesium salts and antacids can be used for treatment. K-sparing diuretics are also magnesium sparing. An important side effect of magnesium repletion is diarrhea, which can potentiate electrolyte losses and reduce long-term adherence rates.
Metabolic acidosis
Acid-base balance is maintained by the kidney through urinary excretion of hydrogen ions both as titratable acids and ammonium. In CKD, renal excretion of the daily acid load is impaired, primarily from decreased ammonium excretion caused by there being too few functioning nephrons.
Metabolic acidosis in CKD is defined as a serum bicarbonate concentration of persistently less than 22 mEq/L. The overall prevalence of metabolic acidosis in cases of CKD that don’t require dialysis is about 15% and increases linearly with a decline in GFR. In the Chronic Renal Insufficiency Cohort study, 7%, 13%, and 37% of participants with CKD stages 2, 3, and 4 respectively had metabolic acidosis.
Metabolic acidosis has a variety of adverse outcomes, including bone demineralization, increased protein catabolism and muscle wasting, impaired cardiac function, impaired glucose homeostasis, and systemic inflammation. Additionally, multiple studies have shown an association between metabolic acidosis and progression of CKD and increased mortality.
The 2013 Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend maintaining the serum bicarbonate level within the reference range (23-29 mEq/L) with alkali therapy. Options include sodium bicarbonate or sodium citrate (which is rapidly metabolized to bicarbonate) in doses of 0.5-1.0 mEq/kg once per day. Sodium bicarbonate is inexpensive; however, it can lead to gastrointestinal upset as the bicarbonate is converted into CO2 in the stomach. This side effect is usually self-limited and improves with time. Typical starting doses are 650 mg twice a day if the serum bicarbonate level is 19-21 mEq/L or 1300 mg twice a day if the serum bicarbonate level is less than or equal to 18 mEq/L.
Sodium citrate can be used if gastrointestinal upset occurs, although caution should be used in those on aluminum binders or with liver disease. Alkali treatment should be started when bicarbonate levels are persistently low (for weeks or months) or if very low (less than or equal to 18 mEq/L) without an acute reversible cause. After patients have begun therapy, they should be monitored for the development of worsening hypertension or edema caused by sodium-mediated fluid retention, although this rarely occurs.
Hyperphosphatemia and Hypocalcemia
Hyperphosphatemia (phosphate levels greater than 4.6 mg/dL) develops early in CKD because of a reduced filtered-phosphate load. Hypocalcemia and hyperphosphatemia can lead to secondary hyperparathyroidism. Given that hyperphosphatemia has been associated with an increased mortality among patients with CKD, treatment is warranted, but the optimal phosphorus range is unknown. According to the KDIGO guidelines, the goal phosphorus level is less than 4.5 mg/dL in patients with CKD who are not on dialysis.
Treatment includes dietary restriction to 900 mg/day and phosphate binders. There is a high phosphate load in processed foods and colas because of food additives. It is therefore recommended to reduce consumption of these foods while encouraging consumption of meat and eggs, which offer additional nutritional value. Those who have failed dietary restrictions should be put on a phosphate binder, either calcium containing (calcium carbonate, calcium acetate) or non–calcium containing (Sevelamer, lanthanum). Non–calcium-containing binders are recommended for patients with hypercalcemia (levels greater than 9.5 mg/dL). There is some data that suggests that non–calcium-containing binders are superior to calcium-containing binders in terms of vascular disease outcomes, but non–calcium-containing binders are sometimes difficult to obtain because of cost and insurance coverage.
Hypocalcemia (calcium levels below 8.4 mg/dL) occurs in the setting of late stage untreated CKD because of decreased GI uptake of calcium from diet in the context of vitamin D deficiency (less than 30 ng/mL) in addition to hyperphosphatemia. Phosphate and vitamin D correction is preferred to calcium supplementation because hyperphosphatemia and vitamin D deficiency occur earlier in CKD. Phosphate reduction is described above.
Regarding vitamin D deficiency, it is recommended to start supplementation with either vitamin D2 or D3. Doses should be adjusted if GFR is less than 30 mL/min per 1.73 m2. It is important to monitor for hypercalcemia, which can also occur in CKD in this context, because it has also been associated with increased morbidity and mortality. If calcium levels are greater than 10.2 mg/dL, all vitamin D supplementation should be discontinued.
Back to the case
Our patient who was admitted for cellulitis has concomitant hypokalemia, hypomagnesemia, acidosis, and hyperphosphatemia with related hypocalcemia. She revealed that her diet was poor prior to her admission for her infection. She was given 20 mEq of potassium orally and placed on a potassium rich diet until potassium levels normalized. She was also given magnesium oxide orally on the first and second day of admission, with repeat levels that were normal. Her acidosis was treated with sodium bicarbonate – 1,300 mg orally twice daily. For her hyperphosphatemia and hypocalcemia, she was placed on phosphate restriction with nutritional counseling with plans to follow up as an outpatient to determine need for phosphate binders. In addition, vitamin D levels were checked, and she was started on repletion for vitamin D deficiency (27 ng/mL). Daily BMP, magnesium, and phosphorus were checked while in house until they were normal for 2 days, and follow-up lab work was requested with her nephrology appointment, which was scheduled for within 1 week.
Bottom line
Electrolyte abnormalities in CKD are numerous and have multiple adverse clinical outcomes. Early intervention and management, especially of metabolic acidosis and hyperphosphatemia, can have a significant effect, including prevention of progression of CKD and possibly reduced mortality.
Dr. Daya, Dr. Apgar, and Dr. Eniasivam are assistant clinical professors in the division of hospital medicine at the University of California, San Francisco.
References
1. Coresh J et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007 Nov 7;298(17):2038-47.
2. Dhondup T et al. Electrolyte and acid-base disorders in chronic kidney disease and end-stage kidney failure. Blood Purif. 2017;43(1-3):179-188.
3. K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004 May;43(5 Suppl 1):S1-290.
4. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl (2011). 2013 Jan;3(1):1–150.
5. Sakaguchi Y et al. Hypomagnesemia in type 2 diabetic nephropathy: A novel predictor of end-stage renal disease. Diabetes Care. 2012 Jul;35(7):1591-7.
6. Palmer SC et al. Serum levels of phosphorus, parathyroid hormone, and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease: A systematic review and meta-analysis. JAMA. 2011 Mar 16;305(11):1119-27.
7. Patel L et al. Sevelamer versus calcium-based binders for treatment of hyperphosphatemia in CKD: A meta-analysis of randomized controlled trials. Clin J Am Soc Nephrol. 2016 Feb 5;11(2):232-44.
8. Raphael KL. Approach to the treatment of chronic metabolic acidosis in CKD. Am J Kidney Dis. 2016 Apr;67(4):696-702.
9. Raphael KL et al. Prevalence of and risk factors for reduced serum bicarbonate in chronic kidney disease. Nephrology (Carlton). 2014 Oct;19(10):648-54.
Additional reading
1. Chapter 3: Management of Progression and Complications of CKD. Kidney Int Suppl (2011). 2013 Jan:3(1):73-90.
2. Raphael KL. Approach to the treatment of chronic metabolic acidosis in CKD. Am J Kidney Dis. 2016 Apr;67(4):696-702.
Quiz
A 75-year-old male with hypertension and CKD Stage 4 is admitted to the hospital for a hip fracture following a fall. Laboratory studies on admission show a potassium level of 3.2 mEq/L, vitamin D level of 45 ng/mL, bicarbonate level of 17 mEq/L, phosphate level of 5.0 mg/dL, and calcium level of 10.3 mg/dL.
What electrolyte replacements should be initiated?
A. Dietary restriction of phosphate, sodium bicarbonate, potassium chloride, and vitamin D.
B. Non–calcium-containing phosphate binder, vitamin D, and potassium chloride.
C. Calcium-containing phosphate binder and sodium bicarbonate.
D. Non–calcium-containing phosphate binder, sodium bicarbonate, and potassium chloride.
Answer: D. Given the patient’s hypokalemia, potassium supplementation should be considered. Additionally, given his hyperphosphatemia and hypercalcemia, a non–calcium-containing phosphate binder like Sevelamer should be started. His metabolic acidosis should be corrected with sodium bicarbonate. There is no indication to supplement vitamin D based on his current lab values.
Key Points
- Identify and treat underlying causes of hypokalemia and hypomagnesemia.
- Do not hesitate to treat metabolic acidosis in CKD.
- Manage hyperphosphatemia and hypocalcemia by ordering appropriate lab studies and providing nutritional consultation with outpatient nephrology follow-up as indicated.
Case
A 55-year-old woman with diabetes, hypertension, and chronic kidney disease (CKD) stage 4 is admitted to the hospital for treatment of left lower-extremity cellulitis. Laboratory studies on admission show a creatinine level of 2.5 mg/dL (glomerular filtration rate [GFR] is 20 mL/min per 1.73 m2; baseline creatinine is between 2.2 and 2.6 mg/dL), potassium level of 3.0 mEq/L, magnesium level of 1.5 mEq/L, bicarbonate level of 18 mEq/L, phosphate level of 6.5 mg/dL, and calcium level of 7.5 mg/dL.
She is put on renally dosed vancomycin to treat her cellulitis. As the hospitalist, how should you manage her multiple electrolyte abnormalities?
Overview of the issue
CKD is also an important risk factor for acute kidney injury. Additionally, rates of readmission for CKD patients are higher than those without CKD. Given that CKD is a “silent disease” that many patients do not realize they have, it is very possible that the first documentation of CKD could happen during an acute hospitalization.
Among the various manifestations of CKD, electrolyte abnormalities are the most likely ones hospitalists will run into.
Overview of the data
Hypokalemia and Hypomagnesemia
Hypokalemia (potassium levels less than 3.5 mEq/L) is not as common as hyperkalemia (potassium levels greater than 5.0 mEq/L) in CKD, which is the result of impaired renal excretion of potassium. Hypokalemia can occur as a result of GI losses, urinary losses, or decreased intake and can be worsened by the use of certain drugs, such as non–K-sparing diuretics.
In the setting of diuretic use involving thiazides and loop diuretics, hypokalemia is dose and sodium-intake dependent. Potassium deficiency worsens the effects of detrimental sodium excess, which plays a role in hypertension and its associated complications. Potassium also has a protective vascular effect, which is a major reason why potassium should be kept normal in patients with CKD.
Acutely, hypokalemia can cause arrhythmias, ileus, and paralysis, which are all indications for immediate repletion. In these cases, hypokalemia must be repleted carefully in small increments (some suggest 20 mEq doses), and the patient must be monitored frequently to avoid hyperkalemia. If patients are persistently hypokalemic, several options can be considered based on the underlying cause. Dietary modifications with foods rich in potassium (containing 250mg/100g) can be suggested. Daily potassium chloride supplementation can be used in those on diuretic therapy who have hypokalemia and metabolic alkalosis (bicarbonate levels greater than 30 mEq/L). Alkalinizing salts, containing citrate or bicarbonate, can be used in hypokalemia without metabolic alkalosis. Initiation of angiotensin-converting-enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta-adrenergic blockers, and K-sparing diuretics can be used as well.
Potassium supplementation and K-sparing diuretics should be used with extreme caution in CKD 3 and 4 given the risk of overcorrection. If potassium supplements or drugs to raise serum potassium are initiated in house, potassium should be rechecked within a week. These treatments should be avoided in individuals with diabetes, who are at highest risk for hyperkalemia given hyporeninemic hypoaldosteronism (type IV renal tubular acidosis).
There is emerging evidence that hypomagnesemia can play a part in progression to end-stage renal disease. In the setting of cardiovascular disease, which often co-exists with CKD, the risk of hypomagnesemia precipitating arrhythmia necessitates repletion to a normal level. Any of the magnesium salts and antacids can be used for treatment. K-sparing diuretics are also magnesium sparing. An important side effect of magnesium repletion is diarrhea, which can potentiate electrolyte losses and reduce long-term adherence rates.
Metabolic acidosis
Acid-base balance is maintained by the kidney through urinary excretion of hydrogen ions both as titratable acids and ammonium. In CKD, renal excretion of the daily acid load is impaired, primarily from decreased ammonium excretion caused by there being too few functioning nephrons.
Metabolic acidosis in CKD is defined as a serum bicarbonate concentration of persistently less than 22 mEq/L. The overall prevalence of metabolic acidosis in cases of CKD that don’t require dialysis is about 15% and increases linearly with a decline in GFR. In the Chronic Renal Insufficiency Cohort study, 7%, 13%, and 37% of participants with CKD stages 2, 3, and 4 respectively had metabolic acidosis.
Metabolic acidosis has a variety of adverse outcomes, including bone demineralization, increased protein catabolism and muscle wasting, impaired cardiac function, impaired glucose homeostasis, and systemic inflammation. Additionally, multiple studies have shown an association between metabolic acidosis and progression of CKD and increased mortality.
The 2013 Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend maintaining the serum bicarbonate level within the reference range (23-29 mEq/L) with alkali therapy. Options include sodium bicarbonate or sodium citrate (which is rapidly metabolized to bicarbonate) in doses of 0.5-1.0 mEq/kg once per day. Sodium bicarbonate is inexpensive; however, it can lead to gastrointestinal upset as the bicarbonate is converted into CO2 in the stomach. This side effect is usually self-limited and improves with time. Typical starting doses are 650 mg twice a day if the serum bicarbonate level is 19-21 mEq/L or 1300 mg twice a day if the serum bicarbonate level is less than or equal to 18 mEq/L.
Sodium citrate can be used if gastrointestinal upset occurs, although caution should be used in those on aluminum binders or with liver disease. Alkali treatment should be started when bicarbonate levels are persistently low (for weeks or months) or if very low (less than or equal to 18 mEq/L) without an acute reversible cause. After patients have begun therapy, they should be monitored for the development of worsening hypertension or edema caused by sodium-mediated fluid retention, although this rarely occurs.
Hyperphosphatemia and Hypocalcemia
Hyperphosphatemia (phosphate levels greater than 4.6 mg/dL) develops early in CKD because of a reduced filtered-phosphate load. Hypocalcemia and hyperphosphatemia can lead to secondary hyperparathyroidism. Given that hyperphosphatemia has been associated with an increased mortality among patients with CKD, treatment is warranted, but the optimal phosphorus range is unknown. According to the KDIGO guidelines, the goal phosphorus level is less than 4.5 mg/dL in patients with CKD who are not on dialysis.
Treatment includes dietary restriction to 900 mg/day and phosphate binders. There is a high phosphate load in processed foods and colas because of food additives. It is therefore recommended to reduce consumption of these foods while encouraging consumption of meat and eggs, which offer additional nutritional value. Those who have failed dietary restrictions should be put on a phosphate binder, either calcium containing (calcium carbonate, calcium acetate) or non–calcium containing (Sevelamer, lanthanum). Non–calcium-containing binders are recommended for patients with hypercalcemia (levels greater than 9.5 mg/dL). There is some data that suggests that non–calcium-containing binders are superior to calcium-containing binders in terms of vascular disease outcomes, but non–calcium-containing binders are sometimes difficult to obtain because of cost and insurance coverage.
Hypocalcemia (calcium levels below 8.4 mg/dL) occurs in the setting of late stage untreated CKD because of decreased GI uptake of calcium from diet in the context of vitamin D deficiency (less than 30 ng/mL) in addition to hyperphosphatemia. Phosphate and vitamin D correction is preferred to calcium supplementation because hyperphosphatemia and vitamin D deficiency occur earlier in CKD. Phosphate reduction is described above.
Regarding vitamin D deficiency, it is recommended to start supplementation with either vitamin D2 or D3. Doses should be adjusted if GFR is less than 30 mL/min per 1.73 m2. It is important to monitor for hypercalcemia, which can also occur in CKD in this context, because it has also been associated with increased morbidity and mortality. If calcium levels are greater than 10.2 mg/dL, all vitamin D supplementation should be discontinued.
Back to the case
Our patient who was admitted for cellulitis has concomitant hypokalemia, hypomagnesemia, acidosis, and hyperphosphatemia with related hypocalcemia. She revealed that her diet was poor prior to her admission for her infection. She was given 20 mEq of potassium orally and placed on a potassium rich diet until potassium levels normalized. She was also given magnesium oxide orally on the first and second day of admission, with repeat levels that were normal. Her acidosis was treated with sodium bicarbonate – 1,300 mg orally twice daily. For her hyperphosphatemia and hypocalcemia, she was placed on phosphate restriction with nutritional counseling with plans to follow up as an outpatient to determine need for phosphate binders. In addition, vitamin D levels were checked, and she was started on repletion for vitamin D deficiency (27 ng/mL). Daily BMP, magnesium, and phosphorus were checked while in house until they were normal for 2 days, and follow-up lab work was requested with her nephrology appointment, which was scheduled for within 1 week.
Bottom line
Electrolyte abnormalities in CKD are numerous and have multiple adverse clinical outcomes. Early intervention and management, especially of metabolic acidosis and hyperphosphatemia, can have a significant effect, including prevention of progression of CKD and possibly reduced mortality.
Dr. Daya, Dr. Apgar, and Dr. Eniasivam are assistant clinical professors in the division of hospital medicine at the University of California, San Francisco.
References
1. Coresh J et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007 Nov 7;298(17):2038-47.
2. Dhondup T et al. Electrolyte and acid-base disorders in chronic kidney disease and end-stage kidney failure. Blood Purif. 2017;43(1-3):179-188.
3. K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004 May;43(5 Suppl 1):S1-290.
4. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl (2011). 2013 Jan;3(1):1–150.
5. Sakaguchi Y et al. Hypomagnesemia in type 2 diabetic nephropathy: A novel predictor of end-stage renal disease. Diabetes Care. 2012 Jul;35(7):1591-7.
6. Palmer SC et al. Serum levels of phosphorus, parathyroid hormone, and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease: A systematic review and meta-analysis. JAMA. 2011 Mar 16;305(11):1119-27.
7. Patel L et al. Sevelamer versus calcium-based binders for treatment of hyperphosphatemia in CKD: A meta-analysis of randomized controlled trials. Clin J Am Soc Nephrol. 2016 Feb 5;11(2):232-44.
8. Raphael KL. Approach to the treatment of chronic metabolic acidosis in CKD. Am J Kidney Dis. 2016 Apr;67(4):696-702.
9. Raphael KL et al. Prevalence of and risk factors for reduced serum bicarbonate in chronic kidney disease. Nephrology (Carlton). 2014 Oct;19(10):648-54.
Additional reading
1. Chapter 3: Management of Progression and Complications of CKD. Kidney Int Suppl (2011). 2013 Jan:3(1):73-90.
2. Raphael KL. Approach to the treatment of chronic metabolic acidosis in CKD. Am J Kidney Dis. 2016 Apr;67(4):696-702.
Quiz
A 75-year-old male with hypertension and CKD Stage 4 is admitted to the hospital for a hip fracture following a fall. Laboratory studies on admission show a potassium level of 3.2 mEq/L, vitamin D level of 45 ng/mL, bicarbonate level of 17 mEq/L, phosphate level of 5.0 mg/dL, and calcium level of 10.3 mg/dL.
What electrolyte replacements should be initiated?
A. Dietary restriction of phosphate, sodium bicarbonate, potassium chloride, and vitamin D.
B. Non–calcium-containing phosphate binder, vitamin D, and potassium chloride.
C. Calcium-containing phosphate binder and sodium bicarbonate.
D. Non–calcium-containing phosphate binder, sodium bicarbonate, and potassium chloride.
Answer: D. Given the patient’s hypokalemia, potassium supplementation should be considered. Additionally, given his hyperphosphatemia and hypercalcemia, a non–calcium-containing phosphate binder like Sevelamer should be started. His metabolic acidosis should be corrected with sodium bicarbonate. There is no indication to supplement vitamin D based on his current lab values.
Key Points
- Identify and treat underlying causes of hypokalemia and hypomagnesemia.
- Do not hesitate to treat metabolic acidosis in CKD.
- Manage hyperphosphatemia and hypocalcemia by ordering appropriate lab studies and providing nutritional consultation with outpatient nephrology follow-up as indicated.
Case
A 55-year-old woman with diabetes, hypertension, and chronic kidney disease (CKD) stage 4 is admitted to the hospital for treatment of left lower-extremity cellulitis. Laboratory studies on admission show a creatinine level of 2.5 mg/dL (glomerular filtration rate [GFR] is 20 mL/min per 1.73 m2; baseline creatinine is between 2.2 and 2.6 mg/dL), potassium level of 3.0 mEq/L, magnesium level of 1.5 mEq/L, bicarbonate level of 18 mEq/L, phosphate level of 6.5 mg/dL, and calcium level of 7.5 mg/dL.
She is put on renally dosed vancomycin to treat her cellulitis. As the hospitalist, how should you manage her multiple electrolyte abnormalities?
Overview of the issue
CKD is also an important risk factor for acute kidney injury. Additionally, rates of readmission for CKD patients are higher than those without CKD. Given that CKD is a “silent disease” that many patients do not realize they have, it is very possible that the first documentation of CKD could happen during an acute hospitalization.
Among the various manifestations of CKD, electrolyte abnormalities are the most likely ones hospitalists will run into.
Overview of the data
Hypokalemia and Hypomagnesemia
Hypokalemia (potassium levels less than 3.5 mEq/L) is not as common as hyperkalemia (potassium levels greater than 5.0 mEq/L) in CKD, which is the result of impaired renal excretion of potassium. Hypokalemia can occur as a result of GI losses, urinary losses, or decreased intake and can be worsened by the use of certain drugs, such as non–K-sparing diuretics.
In the setting of diuretic use involving thiazides and loop diuretics, hypokalemia is dose and sodium-intake dependent. Potassium deficiency worsens the effects of detrimental sodium excess, which plays a role in hypertension and its associated complications. Potassium also has a protective vascular effect, which is a major reason why potassium should be kept normal in patients with CKD.
Acutely, hypokalemia can cause arrhythmias, ileus, and paralysis, which are all indications for immediate repletion. In these cases, hypokalemia must be repleted carefully in small increments (some suggest 20 mEq doses), and the patient must be monitored frequently to avoid hyperkalemia. If patients are persistently hypokalemic, several options can be considered based on the underlying cause. Dietary modifications with foods rich in potassium (containing 250mg/100g) can be suggested. Daily potassium chloride supplementation can be used in those on diuretic therapy who have hypokalemia and metabolic alkalosis (bicarbonate levels greater than 30 mEq/L). Alkalinizing salts, containing citrate or bicarbonate, can be used in hypokalemia without metabolic alkalosis. Initiation of angiotensin-converting-enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta-adrenergic blockers, and K-sparing diuretics can be used as well.
Potassium supplementation and K-sparing diuretics should be used with extreme caution in CKD 3 and 4 given the risk of overcorrection. If potassium supplements or drugs to raise serum potassium are initiated in house, potassium should be rechecked within a week. These treatments should be avoided in individuals with diabetes, who are at highest risk for hyperkalemia given hyporeninemic hypoaldosteronism (type IV renal tubular acidosis).
There is emerging evidence that hypomagnesemia can play a part in progression to end-stage renal disease. In the setting of cardiovascular disease, which often co-exists with CKD, the risk of hypomagnesemia precipitating arrhythmia necessitates repletion to a normal level. Any of the magnesium salts and antacids can be used for treatment. K-sparing diuretics are also magnesium sparing. An important side effect of magnesium repletion is diarrhea, which can potentiate electrolyte losses and reduce long-term adherence rates.
Metabolic acidosis
Acid-base balance is maintained by the kidney through urinary excretion of hydrogen ions both as titratable acids and ammonium. In CKD, renal excretion of the daily acid load is impaired, primarily from decreased ammonium excretion caused by there being too few functioning nephrons.
Metabolic acidosis in CKD is defined as a serum bicarbonate concentration of persistently less than 22 mEq/L. The overall prevalence of metabolic acidosis in cases of CKD that don’t require dialysis is about 15% and increases linearly with a decline in GFR. In the Chronic Renal Insufficiency Cohort study, 7%, 13%, and 37% of participants with CKD stages 2, 3, and 4 respectively had metabolic acidosis.
Metabolic acidosis has a variety of adverse outcomes, including bone demineralization, increased protein catabolism and muscle wasting, impaired cardiac function, impaired glucose homeostasis, and systemic inflammation. Additionally, multiple studies have shown an association between metabolic acidosis and progression of CKD and increased mortality.
The 2013 Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend maintaining the serum bicarbonate level within the reference range (23-29 mEq/L) with alkali therapy. Options include sodium bicarbonate or sodium citrate (which is rapidly metabolized to bicarbonate) in doses of 0.5-1.0 mEq/kg once per day. Sodium bicarbonate is inexpensive; however, it can lead to gastrointestinal upset as the bicarbonate is converted into CO2 in the stomach. This side effect is usually self-limited and improves with time. Typical starting doses are 650 mg twice a day if the serum bicarbonate level is 19-21 mEq/L or 1300 mg twice a day if the serum bicarbonate level is less than or equal to 18 mEq/L.
Sodium citrate can be used if gastrointestinal upset occurs, although caution should be used in those on aluminum binders or with liver disease. Alkali treatment should be started when bicarbonate levels are persistently low (for weeks or months) or if very low (less than or equal to 18 mEq/L) without an acute reversible cause. After patients have begun therapy, they should be monitored for the development of worsening hypertension or edema caused by sodium-mediated fluid retention, although this rarely occurs.
Hyperphosphatemia and Hypocalcemia
Hyperphosphatemia (phosphate levels greater than 4.6 mg/dL) develops early in CKD because of a reduced filtered-phosphate load. Hypocalcemia and hyperphosphatemia can lead to secondary hyperparathyroidism. Given that hyperphosphatemia has been associated with an increased mortality among patients with CKD, treatment is warranted, but the optimal phosphorus range is unknown. According to the KDIGO guidelines, the goal phosphorus level is less than 4.5 mg/dL in patients with CKD who are not on dialysis.
Treatment includes dietary restriction to 900 mg/day and phosphate binders. There is a high phosphate load in processed foods and colas because of food additives. It is therefore recommended to reduce consumption of these foods while encouraging consumption of meat and eggs, which offer additional nutritional value. Those who have failed dietary restrictions should be put on a phosphate binder, either calcium containing (calcium carbonate, calcium acetate) or non–calcium containing (Sevelamer, lanthanum). Non–calcium-containing binders are recommended for patients with hypercalcemia (levels greater than 9.5 mg/dL). There is some data that suggests that non–calcium-containing binders are superior to calcium-containing binders in terms of vascular disease outcomes, but non–calcium-containing binders are sometimes difficult to obtain because of cost and insurance coverage.
Hypocalcemia (calcium levels below 8.4 mg/dL) occurs in the setting of late stage untreated CKD because of decreased GI uptake of calcium from diet in the context of vitamin D deficiency (less than 30 ng/mL) in addition to hyperphosphatemia. Phosphate and vitamin D correction is preferred to calcium supplementation because hyperphosphatemia and vitamin D deficiency occur earlier in CKD. Phosphate reduction is described above.
Regarding vitamin D deficiency, it is recommended to start supplementation with either vitamin D2 or D3. Doses should be adjusted if GFR is less than 30 mL/min per 1.73 m2. It is important to monitor for hypercalcemia, which can also occur in CKD in this context, because it has also been associated with increased morbidity and mortality. If calcium levels are greater than 10.2 mg/dL, all vitamin D supplementation should be discontinued.
Back to the case
Our patient who was admitted for cellulitis has concomitant hypokalemia, hypomagnesemia, acidosis, and hyperphosphatemia with related hypocalcemia. She revealed that her diet was poor prior to her admission for her infection. She was given 20 mEq of potassium orally and placed on a potassium rich diet until potassium levels normalized. She was also given magnesium oxide orally on the first and second day of admission, with repeat levels that were normal. Her acidosis was treated with sodium bicarbonate – 1,300 mg orally twice daily. For her hyperphosphatemia and hypocalcemia, she was placed on phosphate restriction with nutritional counseling with plans to follow up as an outpatient to determine need for phosphate binders. In addition, vitamin D levels were checked, and she was started on repletion for vitamin D deficiency (27 ng/mL). Daily BMP, magnesium, and phosphorus were checked while in house until they were normal for 2 days, and follow-up lab work was requested with her nephrology appointment, which was scheduled for within 1 week.
Bottom line
Electrolyte abnormalities in CKD are numerous and have multiple adverse clinical outcomes. Early intervention and management, especially of metabolic acidosis and hyperphosphatemia, can have a significant effect, including prevention of progression of CKD and possibly reduced mortality.
Dr. Daya, Dr. Apgar, and Dr. Eniasivam are assistant clinical professors in the division of hospital medicine at the University of California, San Francisco.
References
1. Coresh J et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007 Nov 7;298(17):2038-47.
2. Dhondup T et al. Electrolyte and acid-base disorders in chronic kidney disease and end-stage kidney failure. Blood Purif. 2017;43(1-3):179-188.
3. K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004 May;43(5 Suppl 1):S1-290.
4. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl (2011). 2013 Jan;3(1):1–150.
5. Sakaguchi Y et al. Hypomagnesemia in type 2 diabetic nephropathy: A novel predictor of end-stage renal disease. Diabetes Care. 2012 Jul;35(7):1591-7.
6. Palmer SC et al. Serum levels of phosphorus, parathyroid hormone, and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease: A systematic review and meta-analysis. JAMA. 2011 Mar 16;305(11):1119-27.
7. Patel L et al. Sevelamer versus calcium-based binders for treatment of hyperphosphatemia in CKD: A meta-analysis of randomized controlled trials. Clin J Am Soc Nephrol. 2016 Feb 5;11(2):232-44.
8. Raphael KL. Approach to the treatment of chronic metabolic acidosis in CKD. Am J Kidney Dis. 2016 Apr;67(4):696-702.
9. Raphael KL et al. Prevalence of and risk factors for reduced serum bicarbonate in chronic kidney disease. Nephrology (Carlton). 2014 Oct;19(10):648-54.
Additional reading
1. Chapter 3: Management of Progression and Complications of CKD. Kidney Int Suppl (2011). 2013 Jan:3(1):73-90.
2. Raphael KL. Approach to the treatment of chronic metabolic acidosis in CKD. Am J Kidney Dis. 2016 Apr;67(4):696-702.
Quiz
A 75-year-old male with hypertension and CKD Stage 4 is admitted to the hospital for a hip fracture following a fall. Laboratory studies on admission show a potassium level of 3.2 mEq/L, vitamin D level of 45 ng/mL, bicarbonate level of 17 mEq/L, phosphate level of 5.0 mg/dL, and calcium level of 10.3 mg/dL.
What electrolyte replacements should be initiated?
A. Dietary restriction of phosphate, sodium bicarbonate, potassium chloride, and vitamin D.
B. Non–calcium-containing phosphate binder, vitamin D, and potassium chloride.
C. Calcium-containing phosphate binder and sodium bicarbonate.
D. Non–calcium-containing phosphate binder, sodium bicarbonate, and potassium chloride.
Answer: D. Given the patient’s hypokalemia, potassium supplementation should be considered. Additionally, given his hyperphosphatemia and hypercalcemia, a non–calcium-containing phosphate binder like Sevelamer should be started. His metabolic acidosis should be corrected with sodium bicarbonate. There is no indication to supplement vitamin D based on his current lab values.
Key Points
- Identify and treat underlying causes of hypokalemia and hypomagnesemia.
- Do not hesitate to treat metabolic acidosis in CKD.
- Manage hyperphosphatemia and hypocalcemia by ordering appropriate lab studies and providing nutritional consultation with outpatient nephrology follow-up as indicated.
Blood transfusions are dropping in U.S. hospitals
The number of red blood cell (RBC) and plasma transfusions conducted in U.S. hospitals has declined steadily since 2011, perhaps as a result of hospitals instituting new blood management programs after randomized trials showed the safety of restrictive transfusion strategies.
There has been no change in the frequency of platelet transfusions since 2011.
The researchers analyzed data from the National Inpatient Sample, using ICD-9-CM procedure codes to identify transfusion procedures. They examined the percentage of hospitalizations with one or more RBC transfusions, since these represent the majority of transfusions. Secondary outcomes included hospitalizations with one or more plasma or one or more platelet transfusions. The findings were published in a research letter in JAMA.
The study included data from the period of 1993-2014. The frequency of transfusions has trended upward since 1993, but a joinpoint analysis found an inflection point at 2011. The researchers then focused their analysis on the period from 2011 to 2014.
The researchers found reductions in RBC transfusions among all sexes, race/ethnicities, patient risk severities, payer types, and admission types. They found no statistically significant reductions in RBC transfusions in private investor–owned hospitals or in patients under the age of 18, though they noted that there is limited evidence to guide clinical practice in the pediatric population.
The decline in RBC transfusions was greater for elective admissions (aRR, 0.74, 95% CI, 0.67-0.80) than it was for nonelective admissions (aRR, 0.86; 95% CI, 0.81-0.91; P for interaction less than .001).
“The observed decreases in RBC and plasma transfusions from 2011 to 2014 may reflect evidence demonstrating the safety of restricting RBC transfusions, patient blood management programs, conservation initiatives (e.g., cell salvage, pharmacotherapy, improved surgical techniques), advocacy from medical organizations, and publication of transfusion guidelines,” the researchers wrote.
The study is limited by its retrospective design and may not be generalizable to outpatient settings.
The study was supported by grants from the National Institutes of Health and Weill Cornell Medical College. Two of the study authors reported personal fees from Terumo BCT, Haemonetics, and Octapharma. No other disclosures were reported.
SOURCE: Goel R et al. JAMA. 2018 Feb 27;319(8):825-7.
The number of red blood cell (RBC) and plasma transfusions conducted in U.S. hospitals has declined steadily since 2011, perhaps as a result of hospitals instituting new blood management programs after randomized trials showed the safety of restrictive transfusion strategies.
There has been no change in the frequency of platelet transfusions since 2011.
The researchers analyzed data from the National Inpatient Sample, using ICD-9-CM procedure codes to identify transfusion procedures. They examined the percentage of hospitalizations with one or more RBC transfusions, since these represent the majority of transfusions. Secondary outcomes included hospitalizations with one or more plasma or one or more platelet transfusions. The findings were published in a research letter in JAMA.
The study included data from the period of 1993-2014. The frequency of transfusions has trended upward since 1993, but a joinpoint analysis found an inflection point at 2011. The researchers then focused their analysis on the period from 2011 to 2014.
The researchers found reductions in RBC transfusions among all sexes, race/ethnicities, patient risk severities, payer types, and admission types. They found no statistically significant reductions in RBC transfusions in private investor–owned hospitals or in patients under the age of 18, though they noted that there is limited evidence to guide clinical practice in the pediatric population.
The decline in RBC transfusions was greater for elective admissions (aRR, 0.74, 95% CI, 0.67-0.80) than it was for nonelective admissions (aRR, 0.86; 95% CI, 0.81-0.91; P for interaction less than .001).
“The observed decreases in RBC and plasma transfusions from 2011 to 2014 may reflect evidence demonstrating the safety of restricting RBC transfusions, patient blood management programs, conservation initiatives (e.g., cell salvage, pharmacotherapy, improved surgical techniques), advocacy from medical organizations, and publication of transfusion guidelines,” the researchers wrote.
The study is limited by its retrospective design and may not be generalizable to outpatient settings.
The study was supported by grants from the National Institutes of Health and Weill Cornell Medical College. Two of the study authors reported personal fees from Terumo BCT, Haemonetics, and Octapharma. No other disclosures were reported.
SOURCE: Goel R et al. JAMA. 2018 Feb 27;319(8):825-7.
The number of red blood cell (RBC) and plasma transfusions conducted in U.S. hospitals has declined steadily since 2011, perhaps as a result of hospitals instituting new blood management programs after randomized trials showed the safety of restrictive transfusion strategies.
There has been no change in the frequency of platelet transfusions since 2011.
The researchers analyzed data from the National Inpatient Sample, using ICD-9-CM procedure codes to identify transfusion procedures. They examined the percentage of hospitalizations with one or more RBC transfusions, since these represent the majority of transfusions. Secondary outcomes included hospitalizations with one or more plasma or one or more platelet transfusions. The findings were published in a research letter in JAMA.
The study included data from the period of 1993-2014. The frequency of transfusions has trended upward since 1993, but a joinpoint analysis found an inflection point at 2011. The researchers then focused their analysis on the period from 2011 to 2014.
The researchers found reductions in RBC transfusions among all sexes, race/ethnicities, patient risk severities, payer types, and admission types. They found no statistically significant reductions in RBC transfusions in private investor–owned hospitals or in patients under the age of 18, though they noted that there is limited evidence to guide clinical practice in the pediatric population.
The decline in RBC transfusions was greater for elective admissions (aRR, 0.74, 95% CI, 0.67-0.80) than it was for nonelective admissions (aRR, 0.86; 95% CI, 0.81-0.91; P for interaction less than .001).
“The observed decreases in RBC and plasma transfusions from 2011 to 2014 may reflect evidence demonstrating the safety of restricting RBC transfusions, patient blood management programs, conservation initiatives (e.g., cell salvage, pharmacotherapy, improved surgical techniques), advocacy from medical organizations, and publication of transfusion guidelines,” the researchers wrote.
The study is limited by its retrospective design and may not be generalizable to outpatient settings.
The study was supported by grants from the National Institutes of Health and Weill Cornell Medical College. Two of the study authors reported personal fees from Terumo BCT, Haemonetics, and Octapharma. No other disclosures were reported.
SOURCE: Goel R et al. JAMA. 2018 Feb 27;319(8):825-7.
FROM JAMA
Key clinical point:
Major finding: The frequency of red blood cell transfusions among hospital inpatients dropped from 6.8% to 5.7% from 2011 to 2014.
Study details: A retrospective analysis of procedures codes at U.S. hospitals from 1993 to 2014.
Disclosures: The study was supported by grants from the National Institutes of Health and Weill Cornell Medical College. Two of the study authors reported personal fees from Terumo BCT, Haemonetics, and Octapharma. No other disclosures were reported.
Source: Goel R et al. JAMA. 2018 Feb 27;319(8):825-7.
Dexmedetomidine: ‘Silver bullet’ for ventilator liberation?
SAN ANTONIO – Among medications to facilitate extubation, dexmedetomidine offers favorable attributes, but whether it’s the best choice for patients who have difficulty being liberated from the ventilator remains to be proven, said Gilles L. Fraser, BS Pharm, PharmD.
The current CHEST/ATS guidelines on liberation from mechanical ventilation in critically ill adults strongly suggest extubation to noninvasive mechanical ventilation in high-risk patients (Chest. 2017 Jan;151[1]:160-5. doi: 10.1016/j.chest.2016.10.037). Guideline authors also suggested protocols attempting to minimize sedation for acutely hospitalized patients ventilated for more than 24 hours, based on some evidence showing a trend toward shorter ventilation time and ICU stay, as well as lower short-term mortality.
, one of the coauthors of the guidelines, during his presentation at the Critical Care Congress sponsored by the Society for Critical Care Medicine.
“I’ll leave you up to your own devices,” he told attendees at a session on conundrums in critical care that are not addressed in current guidelines. “We use it all the time, frankly, but I don’t have any firm data to support that contention.”
Despite best practices, extubation attempts are not always successful: “If you follow the rules of the road, success is going to occur about 85% of the time,” said Dr. Fraser, who is a clinical pharmacist at Maine Medical Center, Portland, and professor of medicine at Tufts University, Boston. “That means that about 15% of our patients have difficulties in being liberated from the ventilator.”
In terms of medications to facilitate ventilator liberation, benzodiazepines, dexmedetomidine, and propofol all have roles to play, according to Dr. Fraser. Clinicians have to consider agent-specific side effects, pharmacokinetics and dynamics, and “econotoxicity,” or the cost of care, he added.
Although there are few comparative data available to guide choice of medication, Dr. Fraser and his colleagues have published a systematic review and meta-analysis of randomized trials of benzodiazepine versus nonbenzodiazepine-based sedation for mechanically ventilated, critically ill adult patients (Crit Care Med. 2013 Sep;41[9 Suppl 1]:S30-8. doi: 10.1097/CCM.0b013e3182a16898).
They found that dexmedetomidine- or propofol-based sedation regimens appeared to reduce mechanical ventilation duration and length of ICU stay versus benzodiazepine-based sedation, but they stated that larger controlled studies would be needed to further define outcomes in this setting.
More recently, other investigators reported an evaluation of 9,603 consecutive mechanical ventilation episodes (Chest. 2016 Jun;149[6]:1373-9. doi: 10.1378/chest.15-1389). In this large, real-world experience, propofol and dexmedetomidine were both associated with less time to extubation versus benzodiazepines, and dexmedetomidine was associated with less time to extubation versus propofol.
Relatively few patients (about 12%), however, received dexmedetomidine in that large series, and that was mostly in the setting of cardiac surgery, Dr. Fraser noted. Moreover, the investigators reported finding no differences between any two agents in hospital discharge or mortality hazard ratio.
“We’re not suggesting the benzodiazepines as routine sedative agents in our patient populations,” Dr. Fraser said in his presentation. “The primary reason is that they result in a longer time on the vent, typically between 1 and 2 days.”
But this doesn’t mean that the benzodiazepines are the “devil’s handiwork,” he added, noting that they may be useful in patients with anxiety related to ventilator weaning and those recovering from hemodynamic instability or at risk for GABA-agonist withdrawal.
Dexmedetomidine is opioid sparing and has a minimal effect on respiratory drive, among other advantages; however, some potential drawbacks include its hemodynamic effects and its cost, according to Dr. Fraser.
Dr. Fraser said that his institution’s daily acquisition cost for dexmedetomidine is $500, compared with $120 for propofol and $40 for benzodiazepines, but some pharmacoeconomic evaluations suggest use of dexmedetomidine may actually save between $3,000 and $9,000 per ICU admission. “At least in our place, one day in the ICU costs about $5,000, so that all makes sense … and I can argue fairly effectively that dexmedetomidine really isn’t that expensive compared to midazolam,” he said.
Dr. Fraser said that he had no disclosures related to his presentation.
SAN ANTONIO – Among medications to facilitate extubation, dexmedetomidine offers favorable attributes, but whether it’s the best choice for patients who have difficulty being liberated from the ventilator remains to be proven, said Gilles L. Fraser, BS Pharm, PharmD.
The current CHEST/ATS guidelines on liberation from mechanical ventilation in critically ill adults strongly suggest extubation to noninvasive mechanical ventilation in high-risk patients (Chest. 2017 Jan;151[1]:160-5. doi: 10.1016/j.chest.2016.10.037). Guideline authors also suggested protocols attempting to minimize sedation for acutely hospitalized patients ventilated for more than 24 hours, based on some evidence showing a trend toward shorter ventilation time and ICU stay, as well as lower short-term mortality.
, one of the coauthors of the guidelines, during his presentation at the Critical Care Congress sponsored by the Society for Critical Care Medicine.
“I’ll leave you up to your own devices,” he told attendees at a session on conundrums in critical care that are not addressed in current guidelines. “We use it all the time, frankly, but I don’t have any firm data to support that contention.”
Despite best practices, extubation attempts are not always successful: “If you follow the rules of the road, success is going to occur about 85% of the time,” said Dr. Fraser, who is a clinical pharmacist at Maine Medical Center, Portland, and professor of medicine at Tufts University, Boston. “That means that about 15% of our patients have difficulties in being liberated from the ventilator.”
In terms of medications to facilitate ventilator liberation, benzodiazepines, dexmedetomidine, and propofol all have roles to play, according to Dr. Fraser. Clinicians have to consider agent-specific side effects, pharmacokinetics and dynamics, and “econotoxicity,” or the cost of care, he added.
Although there are few comparative data available to guide choice of medication, Dr. Fraser and his colleagues have published a systematic review and meta-analysis of randomized trials of benzodiazepine versus nonbenzodiazepine-based sedation for mechanically ventilated, critically ill adult patients (Crit Care Med. 2013 Sep;41[9 Suppl 1]:S30-8. doi: 10.1097/CCM.0b013e3182a16898).
They found that dexmedetomidine- or propofol-based sedation regimens appeared to reduce mechanical ventilation duration and length of ICU stay versus benzodiazepine-based sedation, but they stated that larger controlled studies would be needed to further define outcomes in this setting.
More recently, other investigators reported an evaluation of 9,603 consecutive mechanical ventilation episodes (Chest. 2016 Jun;149[6]:1373-9. doi: 10.1378/chest.15-1389). In this large, real-world experience, propofol and dexmedetomidine were both associated with less time to extubation versus benzodiazepines, and dexmedetomidine was associated with less time to extubation versus propofol.
Relatively few patients (about 12%), however, received dexmedetomidine in that large series, and that was mostly in the setting of cardiac surgery, Dr. Fraser noted. Moreover, the investigators reported finding no differences between any two agents in hospital discharge or mortality hazard ratio.
“We’re not suggesting the benzodiazepines as routine sedative agents in our patient populations,” Dr. Fraser said in his presentation. “The primary reason is that they result in a longer time on the vent, typically between 1 and 2 days.”
But this doesn’t mean that the benzodiazepines are the “devil’s handiwork,” he added, noting that they may be useful in patients with anxiety related to ventilator weaning and those recovering from hemodynamic instability or at risk for GABA-agonist withdrawal.
Dexmedetomidine is opioid sparing and has a minimal effect on respiratory drive, among other advantages; however, some potential drawbacks include its hemodynamic effects and its cost, according to Dr. Fraser.
Dr. Fraser said that his institution’s daily acquisition cost for dexmedetomidine is $500, compared with $120 for propofol and $40 for benzodiazepines, but some pharmacoeconomic evaluations suggest use of dexmedetomidine may actually save between $3,000 and $9,000 per ICU admission. “At least in our place, one day in the ICU costs about $5,000, so that all makes sense … and I can argue fairly effectively that dexmedetomidine really isn’t that expensive compared to midazolam,” he said.
Dr. Fraser said that he had no disclosures related to his presentation.
SAN ANTONIO – Among medications to facilitate extubation, dexmedetomidine offers favorable attributes, but whether it’s the best choice for patients who have difficulty being liberated from the ventilator remains to be proven, said Gilles L. Fraser, BS Pharm, PharmD.
The current CHEST/ATS guidelines on liberation from mechanical ventilation in critically ill adults strongly suggest extubation to noninvasive mechanical ventilation in high-risk patients (Chest. 2017 Jan;151[1]:160-5. doi: 10.1016/j.chest.2016.10.037). Guideline authors also suggested protocols attempting to minimize sedation for acutely hospitalized patients ventilated for more than 24 hours, based on some evidence showing a trend toward shorter ventilation time and ICU stay, as well as lower short-term mortality.
, one of the coauthors of the guidelines, during his presentation at the Critical Care Congress sponsored by the Society for Critical Care Medicine.
“I’ll leave you up to your own devices,” he told attendees at a session on conundrums in critical care that are not addressed in current guidelines. “We use it all the time, frankly, but I don’t have any firm data to support that contention.”
Despite best practices, extubation attempts are not always successful: “If you follow the rules of the road, success is going to occur about 85% of the time,” said Dr. Fraser, who is a clinical pharmacist at Maine Medical Center, Portland, and professor of medicine at Tufts University, Boston. “That means that about 15% of our patients have difficulties in being liberated from the ventilator.”
In terms of medications to facilitate ventilator liberation, benzodiazepines, dexmedetomidine, and propofol all have roles to play, according to Dr. Fraser. Clinicians have to consider agent-specific side effects, pharmacokinetics and dynamics, and “econotoxicity,” or the cost of care, he added.
Although there are few comparative data available to guide choice of medication, Dr. Fraser and his colleagues have published a systematic review and meta-analysis of randomized trials of benzodiazepine versus nonbenzodiazepine-based sedation for mechanically ventilated, critically ill adult patients (Crit Care Med. 2013 Sep;41[9 Suppl 1]:S30-8. doi: 10.1097/CCM.0b013e3182a16898).
They found that dexmedetomidine- or propofol-based sedation regimens appeared to reduce mechanical ventilation duration and length of ICU stay versus benzodiazepine-based sedation, but they stated that larger controlled studies would be needed to further define outcomes in this setting.
More recently, other investigators reported an evaluation of 9,603 consecutive mechanical ventilation episodes (Chest. 2016 Jun;149[6]:1373-9. doi: 10.1378/chest.15-1389). In this large, real-world experience, propofol and dexmedetomidine were both associated with less time to extubation versus benzodiazepines, and dexmedetomidine was associated with less time to extubation versus propofol.
Relatively few patients (about 12%), however, received dexmedetomidine in that large series, and that was mostly in the setting of cardiac surgery, Dr. Fraser noted. Moreover, the investigators reported finding no differences between any two agents in hospital discharge or mortality hazard ratio.
“We’re not suggesting the benzodiazepines as routine sedative agents in our patient populations,” Dr. Fraser said in his presentation. “The primary reason is that they result in a longer time on the vent, typically between 1 and 2 days.”
But this doesn’t mean that the benzodiazepines are the “devil’s handiwork,” he added, noting that they may be useful in patients with anxiety related to ventilator weaning and those recovering from hemodynamic instability or at risk for GABA-agonist withdrawal.
Dexmedetomidine is opioid sparing and has a minimal effect on respiratory drive, among other advantages; however, some potential drawbacks include its hemodynamic effects and its cost, according to Dr. Fraser.
Dr. Fraser said that his institution’s daily acquisition cost for dexmedetomidine is $500, compared with $120 for propofol and $40 for benzodiazepines, but some pharmacoeconomic evaluations suggest use of dexmedetomidine may actually save between $3,000 and $9,000 per ICU admission. “At least in our place, one day in the ICU costs about $5,000, so that all makes sense … and I can argue fairly effectively that dexmedetomidine really isn’t that expensive compared to midazolam,” he said.
Dr. Fraser said that he had no disclosures related to his presentation.
EXPERT ANALYSIS FROM CCC47
Combo therapy does not improve outcomes for A. Baumannii
, based on data from 406 patients.
In a study published online in The Lancet Infectious Diseases, Mical Paul, MD, of Rambam Health Care Campus, Haifa, Israel, and colleagues randomized 198 patients to colistin alone and 208 to colistin plus meropenem (Lancet Infect Dis. 2018 Feb 15. doi: 10.1016/S1473-3099[18]30099-9).
The demographics were similar between the groups and approximately 77% of patients in each group were infected with A. baumannii.
The results highlight “the necessity of assessing combination therapy in randomized trials before adopting it into clinical use,” the researchers said.
The study was not designed to examine the effect of the two types of therapy on bacteria other than A. baumannii, the researchers noted. However, based on the findings, “we recommend against the routine use of carbapenems for the treatment of carbapenem-resistant A. baumannii infections,” they said.
The study was supported by EU AIDA grant Health-F3-2011-278348. Dr. Paul had no financial conflicts to disclose.
SOURCE: Paul M et al. Lancet Infect Dis. 2018 Feb 15. doi: 10.1016/S1473-3099(18)30099-9.
, based on data from 406 patients.
In a study published online in The Lancet Infectious Diseases, Mical Paul, MD, of Rambam Health Care Campus, Haifa, Israel, and colleagues randomized 198 patients to colistin alone and 208 to colistin plus meropenem (Lancet Infect Dis. 2018 Feb 15. doi: 10.1016/S1473-3099[18]30099-9).
The demographics were similar between the groups and approximately 77% of patients in each group were infected with A. baumannii.
The results highlight “the necessity of assessing combination therapy in randomized trials before adopting it into clinical use,” the researchers said.
The study was not designed to examine the effect of the two types of therapy on bacteria other than A. baumannii, the researchers noted. However, based on the findings, “we recommend against the routine use of carbapenems for the treatment of carbapenem-resistant A. baumannii infections,” they said.
The study was supported by EU AIDA grant Health-F3-2011-278348. Dr. Paul had no financial conflicts to disclose.
SOURCE: Paul M et al. Lancet Infect Dis. 2018 Feb 15. doi: 10.1016/S1473-3099(18)30099-9.
, based on data from 406 patients.
In a study published online in The Lancet Infectious Diseases, Mical Paul, MD, of Rambam Health Care Campus, Haifa, Israel, and colleagues randomized 198 patients to colistin alone and 208 to colistin plus meropenem (Lancet Infect Dis. 2018 Feb 15. doi: 10.1016/S1473-3099[18]30099-9).
The demographics were similar between the groups and approximately 77% of patients in each group were infected with A. baumannii.
The results highlight “the necessity of assessing combination therapy in randomized trials before adopting it into clinical use,” the researchers said.
The study was not designed to examine the effect of the two types of therapy on bacteria other than A. baumannii, the researchers noted. However, based on the findings, “we recommend against the routine use of carbapenems for the treatment of carbapenem-resistant A. baumannii infections,” they said.
The study was supported by EU AIDA grant Health-F3-2011-278348. Dr. Paul had no financial conflicts to disclose.
SOURCE: Paul M et al. Lancet Infect Dis. 2018 Feb 15. doi: 10.1016/S1473-3099(18)30099-9.
FROM THE LANCET INFECTIOUS DISEASES
Flu season shows signs of slowing
Flu-related outpatient activity dropped for the second week in a row as the cumulative hospitalization rate continues to rise, according to data from the Centers for Disease Control and Prevention.
For the week ending Feb. 17, the proportion of outpatient visits for influenza-like illness (ILI) was 6.4%, which was down from 7.4% the previous week (Feb. 10) and down from the seasonal high of 7.5% set 2 weeks earlier, the CDC said in its weekly flu surveillance report. The rate for the week ending Feb. 10 was reported last week as 7.5%, but it has been revised downward.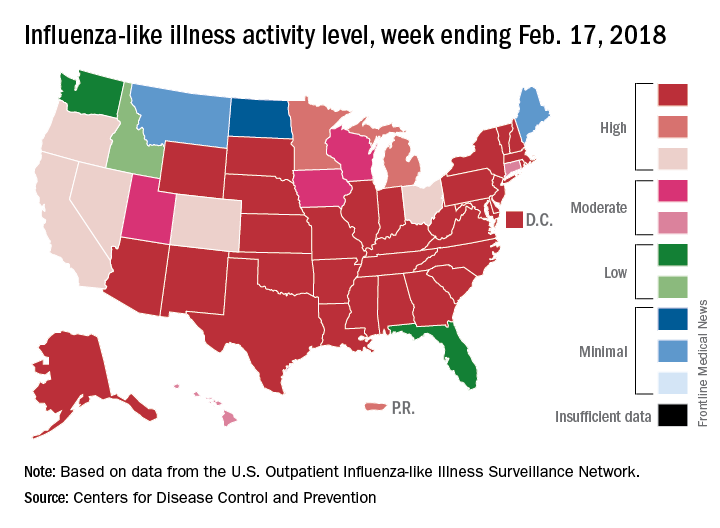
State reports of ILI activity support the decreases seen in the national outpatient rate. There were 33 states at level 10 on the CDC’s 1-10 scale for the week ending Feb. 17 – down from 39 the week before – and a total of 41 states in the “high” range from levels 8-10, compared with 45 the previous week, CDC’s FluView website shows.
Reports of flu-related pediatric deaths continued: 13 deaths were reported during the week, although 9 occurred in previous weeks. The total for the 2017-2018 season is now 97. There were 110 pediatric deaths in the entire 2016-2017 season, 93 during the 2015-2016 season, and 149 in 2014-2015, the CDC said.
Flu-related outpatient activity dropped for the second week in a row as the cumulative hospitalization rate continues to rise, according to data from the Centers for Disease Control and Prevention.
For the week ending Feb. 17, the proportion of outpatient visits for influenza-like illness (ILI) was 6.4%, which was down from 7.4% the previous week (Feb. 10) and down from the seasonal high of 7.5% set 2 weeks earlier, the CDC said in its weekly flu surveillance report. The rate for the week ending Feb. 10 was reported last week as 7.5%, but it has been revised downward.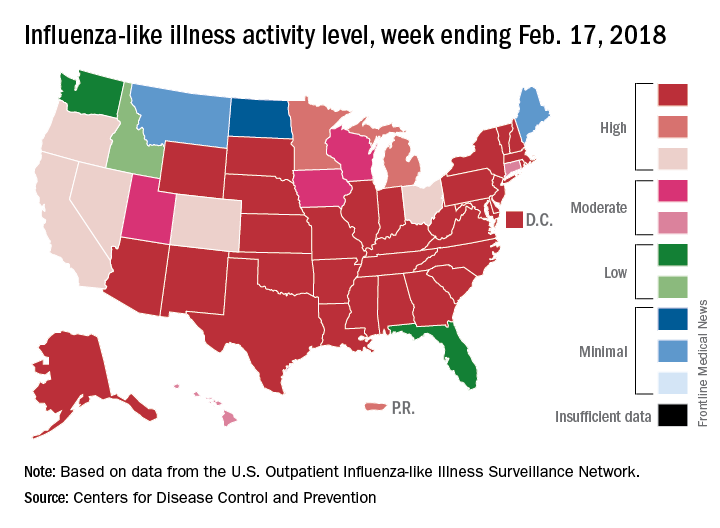
State reports of ILI activity support the decreases seen in the national outpatient rate. There were 33 states at level 10 on the CDC’s 1-10 scale for the week ending Feb. 17 – down from 39 the week before – and a total of 41 states in the “high” range from levels 8-10, compared with 45 the previous week, CDC’s FluView website shows.
Reports of flu-related pediatric deaths continued: 13 deaths were reported during the week, although 9 occurred in previous weeks. The total for the 2017-2018 season is now 97. There were 110 pediatric deaths in the entire 2016-2017 season, 93 during the 2015-2016 season, and 149 in 2014-2015, the CDC said.
Flu-related outpatient activity dropped for the second week in a row as the cumulative hospitalization rate continues to rise, according to data from the Centers for Disease Control and Prevention.
For the week ending Feb. 17, the proportion of outpatient visits for influenza-like illness (ILI) was 6.4%, which was down from 7.4% the previous week (Feb. 10) and down from the seasonal high of 7.5% set 2 weeks earlier, the CDC said in its weekly flu surveillance report. The rate for the week ending Feb. 10 was reported last week as 7.5%, but it has been revised downward.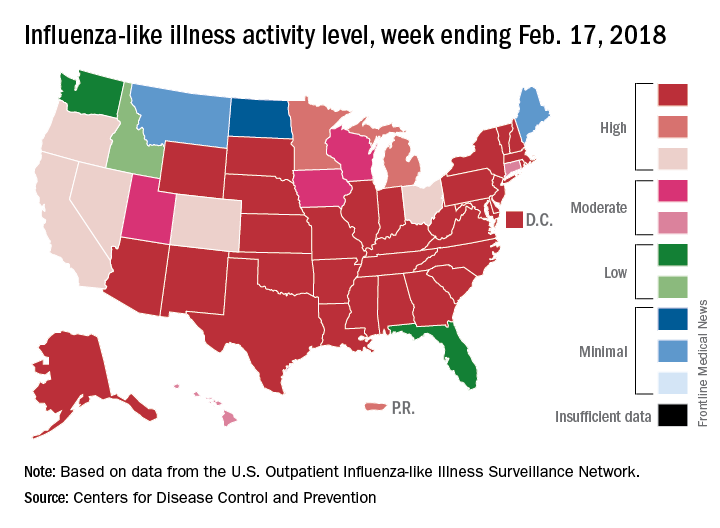
State reports of ILI activity support the decreases seen in the national outpatient rate. There were 33 states at level 10 on the CDC’s 1-10 scale for the week ending Feb. 17 – down from 39 the week before – and a total of 41 states in the “high” range from levels 8-10, compared with 45 the previous week, CDC’s FluView website shows.
Reports of flu-related pediatric deaths continued: 13 deaths were reported during the week, although 9 occurred in previous weeks. The total for the 2017-2018 season is now 97. There were 110 pediatric deaths in the entire 2016-2017 season, 93 during the 2015-2016 season, and 149 in 2014-2015, the CDC said.
FDA warns against clarithromycin use in patients with heart disease
The Food and Drug Administration has added a new warning for an increased risk of death in patients with heart disease who have used clarithromycin (Biaxin), on the basis of results of a 10-year follow-up from the CLARICOR trial.
The CLARICOR trial followed 4,372 randomized patients for at least 2 years after undergoing 14 days of treatment with daily doses of 500 mg clarithromycin. Among these patients, researchers observed an unexpected increase in deaths in patients with coronary heart disease. (The Feb. 22 FDA statement announcing the alert did not provide data from CLARICOR.) As of yet, there is no clear explanation of how clarithromycin would lead to more deaths, compared with a placebo, the agency said.
Regardless, two of the six observational studies published found a link between clarithromycin use and long-term risks; four did not. The CLARICOR trial provides the strongest evidence of increased health risks, the statement said.
The FDA is recommending that health care professionals be aware of the risks associated with clarithromycin use and consider the benefits and risks of use in patients with heart disease. If at all possible, the use of other antibiotics may be a better option. Doctors should advise patients to be aware of signs and symptoms associated with cardiovascular issues.
Patients are also an important piece of the puzzle and should communicate with their health care providers about heart disease, particularly when taking antibiotics to treat for an infection.
The FDA has added the results of the CLARICOR trial to the clarithromycin drug labels. The agency will continue to monitor the safety reports in patients using clarithromycin.
Serious adverse events associated with clarithromycin should be reported to the FDA’s MedWatch program at 800-332-1088 or www.fda.gov/medwatch/.
The Food and Drug Administration has added a new warning for an increased risk of death in patients with heart disease who have used clarithromycin (Biaxin), on the basis of results of a 10-year follow-up from the CLARICOR trial.
The CLARICOR trial followed 4,372 randomized patients for at least 2 years after undergoing 14 days of treatment with daily doses of 500 mg clarithromycin. Among these patients, researchers observed an unexpected increase in deaths in patients with coronary heart disease. (The Feb. 22 FDA statement announcing the alert did not provide data from CLARICOR.) As of yet, there is no clear explanation of how clarithromycin would lead to more deaths, compared with a placebo, the agency said.
Regardless, two of the six observational studies published found a link between clarithromycin use and long-term risks; four did not. The CLARICOR trial provides the strongest evidence of increased health risks, the statement said.
The FDA is recommending that health care professionals be aware of the risks associated with clarithromycin use and consider the benefits and risks of use in patients with heart disease. If at all possible, the use of other antibiotics may be a better option. Doctors should advise patients to be aware of signs and symptoms associated with cardiovascular issues.
Patients are also an important piece of the puzzle and should communicate with their health care providers about heart disease, particularly when taking antibiotics to treat for an infection.
The FDA has added the results of the CLARICOR trial to the clarithromycin drug labels. The agency will continue to monitor the safety reports in patients using clarithromycin.
Serious adverse events associated with clarithromycin should be reported to the FDA’s MedWatch program at 800-332-1088 or www.fda.gov/medwatch/.
The Food and Drug Administration has added a new warning for an increased risk of death in patients with heart disease who have used clarithromycin (Biaxin), on the basis of results of a 10-year follow-up from the CLARICOR trial.
The CLARICOR trial followed 4,372 randomized patients for at least 2 years after undergoing 14 days of treatment with daily doses of 500 mg clarithromycin. Among these patients, researchers observed an unexpected increase in deaths in patients with coronary heart disease. (The Feb. 22 FDA statement announcing the alert did not provide data from CLARICOR.) As of yet, there is no clear explanation of how clarithromycin would lead to more deaths, compared with a placebo, the agency said.
Regardless, two of the six observational studies published found a link between clarithromycin use and long-term risks; four did not. The CLARICOR trial provides the strongest evidence of increased health risks, the statement said.
The FDA is recommending that health care professionals be aware of the risks associated with clarithromycin use and consider the benefits and risks of use in patients with heart disease. If at all possible, the use of other antibiotics may be a better option. Doctors should advise patients to be aware of signs and symptoms associated with cardiovascular issues.
Patients are also an important piece of the puzzle and should communicate with their health care providers about heart disease, particularly when taking antibiotics to treat for an infection.
The FDA has added the results of the CLARICOR trial to the clarithromycin drug labels. The agency will continue to monitor the safety reports in patients using clarithromycin.
Serious adverse events associated with clarithromycin should be reported to the FDA’s MedWatch program at 800-332-1088 or www.fda.gov/medwatch/.