User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Application of the MASCC and CISNE risk-stratification scores to identify low-risk febrile neutropenic patients in the emergency department
Clinical Question: Does the Multinational Association for Supportive Care in Cancer (MASCC) or Clinical Index of Stable Febrile Neutropenia (CISNE) risk-stratification score better predict patient outcomes in patients presenting to emergency departments with febrile neutropenia?
Background: Risk-stratification metrics like the MASCC and CISNE identify subsets of relatively low-risk patients with febrile neutropenia after chemotherapy for treatment at home with empiric oral antibiotic therapy and close follow-up while awaiting results of infectious work-up. Prior studies have validated these tools for admitted, but not for ED, patients.
Setting: Two academic ED at National Institutes of Health–designated cancer centers.
Synopsis: Included patients (n = 230) were at least 16 years old with a documented fever of 38° C or greater related to chemotherapy and an absolute neutrophil count less than 1,000 cells/μL. MASCC and CISNE risk stratification scores were calculated based on the documentation from the ED and recent oncology clinic visits. Outcome measures included length of stay, upgrade in level of care, positive blood cultures, clinical deterioration, and death and were assessed for up to 30 days following discharge. Low-risk patients were defined as those who experienced no negative endpoints. The CISNE score was more specific than the MASCC in identifying low-risk patients (98.1% vs. 54.2%), suggesting that the CISNE may be useful for hospitalists in identifying patients who may be safely discharged with oral antibiotics and close follow-up.
Limitations include possible misclassification bias from indirect assessment of symptom severity, lack of recent ECOG scores for six patients in the CISNE arm, and possible undocumented symptoms during ED evaluation required for subsequent score calculation. Additionally, most patients in this study reported mild symptoms which weighted their MASCC classification toward low-risk.
Bottom Line: The CISNE score may aid in risk-stratification of patients with chemotherapy-related febrile neutropenia presenting to the ED.
Reference: Coyne CJ, Le V, Brennan JJ, et al. Application of the MASCC and CISNE risk-stratification scores to identify low-risk febrile neutropenic patients in the emergency department. Ann Emerg Med. Published online 29 Dec 2016. doi: 10.1016/j.annemergmed.2016.11.007.
Dr. Frederick is assistant clinical professor in the division of hospital Medicine, department of medicine, University of California, San Diego.
Clinical Question: Does the Multinational Association for Supportive Care in Cancer (MASCC) or Clinical Index of Stable Febrile Neutropenia (CISNE) risk-stratification score better predict patient outcomes in patients presenting to emergency departments with febrile neutropenia?
Background: Risk-stratification metrics like the MASCC and CISNE identify subsets of relatively low-risk patients with febrile neutropenia after chemotherapy for treatment at home with empiric oral antibiotic therapy and close follow-up while awaiting results of infectious work-up. Prior studies have validated these tools for admitted, but not for ED, patients.
Setting: Two academic ED at National Institutes of Health–designated cancer centers.
Synopsis: Included patients (n = 230) were at least 16 years old with a documented fever of 38° C or greater related to chemotherapy and an absolute neutrophil count less than 1,000 cells/μL. MASCC and CISNE risk stratification scores were calculated based on the documentation from the ED and recent oncology clinic visits. Outcome measures included length of stay, upgrade in level of care, positive blood cultures, clinical deterioration, and death and were assessed for up to 30 days following discharge. Low-risk patients were defined as those who experienced no negative endpoints. The CISNE score was more specific than the MASCC in identifying low-risk patients (98.1% vs. 54.2%), suggesting that the CISNE may be useful for hospitalists in identifying patients who may be safely discharged with oral antibiotics and close follow-up.
Limitations include possible misclassification bias from indirect assessment of symptom severity, lack of recent ECOG scores for six patients in the CISNE arm, and possible undocumented symptoms during ED evaluation required for subsequent score calculation. Additionally, most patients in this study reported mild symptoms which weighted their MASCC classification toward low-risk.
Bottom Line: The CISNE score may aid in risk-stratification of patients with chemotherapy-related febrile neutropenia presenting to the ED.
Reference: Coyne CJ, Le V, Brennan JJ, et al. Application of the MASCC and CISNE risk-stratification scores to identify low-risk febrile neutropenic patients in the emergency department. Ann Emerg Med. Published online 29 Dec 2016. doi: 10.1016/j.annemergmed.2016.11.007.
Dr. Frederick is assistant clinical professor in the division of hospital Medicine, department of medicine, University of California, San Diego.
Clinical Question: Does the Multinational Association for Supportive Care in Cancer (MASCC) or Clinical Index of Stable Febrile Neutropenia (CISNE) risk-stratification score better predict patient outcomes in patients presenting to emergency departments with febrile neutropenia?
Background: Risk-stratification metrics like the MASCC and CISNE identify subsets of relatively low-risk patients with febrile neutropenia after chemotherapy for treatment at home with empiric oral antibiotic therapy and close follow-up while awaiting results of infectious work-up. Prior studies have validated these tools for admitted, but not for ED, patients.
Setting: Two academic ED at National Institutes of Health–designated cancer centers.
Synopsis: Included patients (n = 230) were at least 16 years old with a documented fever of 38° C or greater related to chemotherapy and an absolute neutrophil count less than 1,000 cells/μL. MASCC and CISNE risk stratification scores were calculated based on the documentation from the ED and recent oncology clinic visits. Outcome measures included length of stay, upgrade in level of care, positive blood cultures, clinical deterioration, and death and were assessed for up to 30 days following discharge. Low-risk patients were defined as those who experienced no negative endpoints. The CISNE score was more specific than the MASCC in identifying low-risk patients (98.1% vs. 54.2%), suggesting that the CISNE may be useful for hospitalists in identifying patients who may be safely discharged with oral antibiotics and close follow-up.
Limitations include possible misclassification bias from indirect assessment of symptom severity, lack of recent ECOG scores for six patients in the CISNE arm, and possible undocumented symptoms during ED evaluation required for subsequent score calculation. Additionally, most patients in this study reported mild symptoms which weighted their MASCC classification toward low-risk.
Bottom Line: The CISNE score may aid in risk-stratification of patients with chemotherapy-related febrile neutropenia presenting to the ED.
Reference: Coyne CJ, Le V, Brennan JJ, et al. Application of the MASCC and CISNE risk-stratification scores to identify low-risk febrile neutropenic patients in the emergency department. Ann Emerg Med. Published online 29 Dec 2016. doi: 10.1016/j.annemergmed.2016.11.007.
Dr. Frederick is assistant clinical professor in the division of hospital Medicine, department of medicine, University of California, San Diego.
Atrial fibrillation blunts beta-blockers for HFrEF
PARIS – Maximal beta-blocker treatment and lower heart rates are effective at cutting all-cause mortality in patients with heart failure with reduced ejection fraction (HFrEF) who are also in sinus rhythm, but it’s a totally different story for patients with similar heart failure plus atrial fibrillation. In the atrial fibrillation subgroup, treatment with a beta-blocker linked with no mortality benefit, and lower heart rates – below 70 beats per minute – appeared to actually link with worse patient survival, based on a meta-analysis of data from 11 beta-blocker trials with a total of more than 17,000 patients.
“Beta blockers may be doing good in heart failure patients with atrial fibrillation, but they also are doing harm that neutralizes any good they do.” In patients with HFrEF and atrial fibrillation, “I don’t like to see the heart rate below 80 beats per minute,” John G.F. Cleland, MD, said at a meeting held by the Heart Failure Association of the ESC.

“We’ve perhaps been too aggressive with heart-rate control in HFrEF patients with atrial fibrillation,” he added in an interview. In these patients “in the range of 60-100 bpm it doesn’t seem to make a lot of difference what the heart rate is, and, if it is less than 70 bpm, patients seem to do a little worse. When we treat these patients with a beta-blocker we don’t see benefit in any way that we’ve looked at the data.”
In contrast, among HFrEF patients in sinus rhythm “beta-blocker treatment is similarly effective regardless of what the baseline heart rate was. The benefit was as great when the baseline rate was 70 bpm or 90 bpm, so heart rate is not a great predictor of beta-blocker benefit in these patients. Patients who tolerated the full beta-blocker dosage had the greatest benefit, and patients who achieved the slowest heart rates also had the greatest benefit.”
In the multivariate models that Dr. Cleland and his associates tested in their meta-analysis, in HFrEF patients in sinus rhythm, the relationship between reduced heart rate and mortality benefit was stronger statistically than between beta-blocker dosage and reduced mortality, he said. “This suggests to me that, while we should use the targeted beta-blocker dosages when we can, it’s more important to achieve a target heart rate in these patients of 55-65 bpm.”
Dr. Cleland hypothesized, based on a report presented at the same meeting by a different research group, that reduced heart rate is not beneficial in HFrEF patients with atrial fibrillation because in this subgroup slower heart rates linked with an increased number of brief pauses in left ventricular pumping. These pauses may result in ventricular arrhythmias, he speculated. “It may be that beta-blockers are equally effective at slowing heart rate in patients with or without atrial fibrillation, but there is also harm from beta-blockers because they’re causing pauses in patients with atrial fibrillation,” he said.
These days, if he has a HFrEF patient with atrial fibrillation whose heart rate slows to 60 bpm, he will stop digoxin treatment if the patient is on that drug, and he will also reduce the beta-blocker dosage but not discontinue it.
The findings came from the Collaborative Systematic Overview of Randomized Controlled Trials of Beta-Blockers in the Treatment of Heart Failure (BB-META-HF), which included data from 11 large beta-blocker randomized trials in heart failure that had been published during 1993-2005. The analysis included data from 17,378 HFrEF patients, with 14,313 (82%) in sinus rhythm and 3,065 (18%) with atrial fibrillation. Follow-up data of patients on treatment was available for 15,007 of these patients.
Dr. Cleland and his associates showed in multivariate analyses that, when they controlled for several baseline demographic and clinical variables among patients in sinus rhythm who received a beta-blocker, the follow-up all-cause mortality fell by 36%, compared with placebo, in patients with a resting baseline heart rate of less than 70 bpm; by 21%, compared with placebo, in patients with a baseline heart rate of 70-90 bpm; and by 38%, compared with placebo, in patients with a baseline heart rate of more than 90 bpm. All three reductions were statistically significant. In contrast, among patients who also had atrial fibrillation beta-blocker treatment linked with no significant mortality reduction, compared with placebo, for patients with any baseline heart rate. Concurrently with Dr. Cleland’s report at the meeting the results appeared online (J Amer Coll Cardiol. 2017 Apr 30. doi: 10.1016/j.jacc.2017.04.001).
[email protected]
On Twitter @mitchelzoler
The findings from this analysis have several implications. First, the association of reduced mortality with reduced heart rate occurred only in patients in sinus rhythm. The irregular heart rhythms in patients with atrial fibrillation may counterbalance any reverse remodeling effects that come from reducing heart rate.
Also, the beneficial effect of beta-blocker treatment was roughly similar regardless of whether baseline heart rate was high or low. This distinguishes beta-blockers from ivabradine, a drug that only reduces heart rate. The magnitude of benefit from ivabradine treatment depends on a patient’s baseline heart rate. The observation that beta-blockers do not have the same limitation suggests that the mechanism of action of beta-blockers may go beyond their heart rate effect. It may also result from the effect of beta-blockers on antagonizing toxic effects from beta-adrenergic stimulation.
The pooled analysis also showed that many patients with HFrEF in sinus rhythm continued to have a high heart rate despite beta-blocker treatment. These patients may get additional benefit from further treatment to reduce their heart rate, with an agent like ivabradine.
But we must be cautious in interpreting the findings because they represent a secondary analysis, and the endpoint studied does not take into account quality of life, exercise tolerance, heart rate control, and tachyarrhythmias. We need prospective, randomized trials of HFrEF patients in sinus rhythm and with atrial fibrillation to better understand how to optimally treat these different types of patients.
The findings highlight that beta-blockers remain a mainstay of treatment for patients with HFrEF in sinus rhythm, and that we have more limited treatment options for HFrEF patients with atrial fibrillation.
Michael Böhm, MD, is professor and director of the cardiology clinic at Saarland University Hospital in Homburg, Germany. He has received honoraria from Bayer, Medtronic, Servier, and Pfizer, and he was a coauthor on the report presented by Dr. Cleland. He made these comments as designated discussant for the study.
The findings from this analysis have several implications. First, the association of reduced mortality with reduced heart rate occurred only in patients in sinus rhythm. The irregular heart rhythms in patients with atrial fibrillation may counterbalance any reverse remodeling effects that come from reducing heart rate.
Also, the beneficial effect of beta-blocker treatment was roughly similar regardless of whether baseline heart rate was high or low. This distinguishes beta-blockers from ivabradine, a drug that only reduces heart rate. The magnitude of benefit from ivabradine treatment depends on a patient’s baseline heart rate. The observation that beta-blockers do not have the same limitation suggests that the mechanism of action of beta-blockers may go beyond their heart rate effect. It may also result from the effect of beta-blockers on antagonizing toxic effects from beta-adrenergic stimulation.
The pooled analysis also showed that many patients with HFrEF in sinus rhythm continued to have a high heart rate despite beta-blocker treatment. These patients may get additional benefit from further treatment to reduce their heart rate, with an agent like ivabradine.
But we must be cautious in interpreting the findings because they represent a secondary analysis, and the endpoint studied does not take into account quality of life, exercise tolerance, heart rate control, and tachyarrhythmias. We need prospective, randomized trials of HFrEF patients in sinus rhythm and with atrial fibrillation to better understand how to optimally treat these different types of patients.
The findings highlight that beta-blockers remain a mainstay of treatment for patients with HFrEF in sinus rhythm, and that we have more limited treatment options for HFrEF patients with atrial fibrillation.
Michael Böhm, MD, is professor and director of the cardiology clinic at Saarland University Hospital in Homburg, Germany. He has received honoraria from Bayer, Medtronic, Servier, and Pfizer, and he was a coauthor on the report presented by Dr. Cleland. He made these comments as designated discussant for the study.
The findings from this analysis have several implications. First, the association of reduced mortality with reduced heart rate occurred only in patients in sinus rhythm. The irregular heart rhythms in patients with atrial fibrillation may counterbalance any reverse remodeling effects that come from reducing heart rate.
Also, the beneficial effect of beta-blocker treatment was roughly similar regardless of whether baseline heart rate was high or low. This distinguishes beta-blockers from ivabradine, a drug that only reduces heart rate. The magnitude of benefit from ivabradine treatment depends on a patient’s baseline heart rate. The observation that beta-blockers do not have the same limitation suggests that the mechanism of action of beta-blockers may go beyond their heart rate effect. It may also result from the effect of beta-blockers on antagonizing toxic effects from beta-adrenergic stimulation.
The pooled analysis also showed that many patients with HFrEF in sinus rhythm continued to have a high heart rate despite beta-blocker treatment. These patients may get additional benefit from further treatment to reduce their heart rate, with an agent like ivabradine.
But we must be cautious in interpreting the findings because they represent a secondary analysis, and the endpoint studied does not take into account quality of life, exercise tolerance, heart rate control, and tachyarrhythmias. We need prospective, randomized trials of HFrEF patients in sinus rhythm and with atrial fibrillation to better understand how to optimally treat these different types of patients.
The findings highlight that beta-blockers remain a mainstay of treatment for patients with HFrEF in sinus rhythm, and that we have more limited treatment options for HFrEF patients with atrial fibrillation.
Michael Böhm, MD, is professor and director of the cardiology clinic at Saarland University Hospital in Homburg, Germany. He has received honoraria from Bayer, Medtronic, Servier, and Pfizer, and he was a coauthor on the report presented by Dr. Cleland. He made these comments as designated discussant for the study.
PARIS – Maximal beta-blocker treatment and lower heart rates are effective at cutting all-cause mortality in patients with heart failure with reduced ejection fraction (HFrEF) who are also in sinus rhythm, but it’s a totally different story for patients with similar heart failure plus atrial fibrillation. In the atrial fibrillation subgroup, treatment with a beta-blocker linked with no mortality benefit, and lower heart rates – below 70 beats per minute – appeared to actually link with worse patient survival, based on a meta-analysis of data from 11 beta-blocker trials with a total of more than 17,000 patients.
“Beta blockers may be doing good in heart failure patients with atrial fibrillation, but they also are doing harm that neutralizes any good they do.” In patients with HFrEF and atrial fibrillation, “I don’t like to see the heart rate below 80 beats per minute,” John G.F. Cleland, MD, said at a meeting held by the Heart Failure Association of the ESC.

“We’ve perhaps been too aggressive with heart-rate control in HFrEF patients with atrial fibrillation,” he added in an interview. In these patients “in the range of 60-100 bpm it doesn’t seem to make a lot of difference what the heart rate is, and, if it is less than 70 bpm, patients seem to do a little worse. When we treat these patients with a beta-blocker we don’t see benefit in any way that we’ve looked at the data.”
In contrast, among HFrEF patients in sinus rhythm “beta-blocker treatment is similarly effective regardless of what the baseline heart rate was. The benefit was as great when the baseline rate was 70 bpm or 90 bpm, so heart rate is not a great predictor of beta-blocker benefit in these patients. Patients who tolerated the full beta-blocker dosage had the greatest benefit, and patients who achieved the slowest heart rates also had the greatest benefit.”
In the multivariate models that Dr. Cleland and his associates tested in their meta-analysis, in HFrEF patients in sinus rhythm, the relationship between reduced heart rate and mortality benefit was stronger statistically than between beta-blocker dosage and reduced mortality, he said. “This suggests to me that, while we should use the targeted beta-blocker dosages when we can, it’s more important to achieve a target heart rate in these patients of 55-65 bpm.”
Dr. Cleland hypothesized, based on a report presented at the same meeting by a different research group, that reduced heart rate is not beneficial in HFrEF patients with atrial fibrillation because in this subgroup slower heart rates linked with an increased number of brief pauses in left ventricular pumping. These pauses may result in ventricular arrhythmias, he speculated. “It may be that beta-blockers are equally effective at slowing heart rate in patients with or without atrial fibrillation, but there is also harm from beta-blockers because they’re causing pauses in patients with atrial fibrillation,” he said.
These days, if he has a HFrEF patient with atrial fibrillation whose heart rate slows to 60 bpm, he will stop digoxin treatment if the patient is on that drug, and he will also reduce the beta-blocker dosage but not discontinue it.
The findings came from the Collaborative Systematic Overview of Randomized Controlled Trials of Beta-Blockers in the Treatment of Heart Failure (BB-META-HF), which included data from 11 large beta-blocker randomized trials in heart failure that had been published during 1993-2005. The analysis included data from 17,378 HFrEF patients, with 14,313 (82%) in sinus rhythm and 3,065 (18%) with atrial fibrillation. Follow-up data of patients on treatment was available for 15,007 of these patients.
Dr. Cleland and his associates showed in multivariate analyses that, when they controlled for several baseline demographic and clinical variables among patients in sinus rhythm who received a beta-blocker, the follow-up all-cause mortality fell by 36%, compared with placebo, in patients with a resting baseline heart rate of less than 70 bpm; by 21%, compared with placebo, in patients with a baseline heart rate of 70-90 bpm; and by 38%, compared with placebo, in patients with a baseline heart rate of more than 90 bpm. All three reductions were statistically significant. In contrast, among patients who also had atrial fibrillation beta-blocker treatment linked with no significant mortality reduction, compared with placebo, for patients with any baseline heart rate. Concurrently with Dr. Cleland’s report at the meeting the results appeared online (J Amer Coll Cardiol. 2017 Apr 30. doi: 10.1016/j.jacc.2017.04.001).
[email protected]
On Twitter @mitchelzoler
PARIS – Maximal beta-blocker treatment and lower heart rates are effective at cutting all-cause mortality in patients with heart failure with reduced ejection fraction (HFrEF) who are also in sinus rhythm, but it’s a totally different story for patients with similar heart failure plus atrial fibrillation. In the atrial fibrillation subgroup, treatment with a beta-blocker linked with no mortality benefit, and lower heart rates – below 70 beats per minute – appeared to actually link with worse patient survival, based on a meta-analysis of data from 11 beta-blocker trials with a total of more than 17,000 patients.
“Beta blockers may be doing good in heart failure patients with atrial fibrillation, but they also are doing harm that neutralizes any good they do.” In patients with HFrEF and atrial fibrillation, “I don’t like to see the heart rate below 80 beats per minute,” John G.F. Cleland, MD, said at a meeting held by the Heart Failure Association of the ESC.

“We’ve perhaps been too aggressive with heart-rate control in HFrEF patients with atrial fibrillation,” he added in an interview. In these patients “in the range of 60-100 bpm it doesn’t seem to make a lot of difference what the heart rate is, and, if it is less than 70 bpm, patients seem to do a little worse. When we treat these patients with a beta-blocker we don’t see benefit in any way that we’ve looked at the data.”
In contrast, among HFrEF patients in sinus rhythm “beta-blocker treatment is similarly effective regardless of what the baseline heart rate was. The benefit was as great when the baseline rate was 70 bpm or 90 bpm, so heart rate is not a great predictor of beta-blocker benefit in these patients. Patients who tolerated the full beta-blocker dosage had the greatest benefit, and patients who achieved the slowest heart rates also had the greatest benefit.”
In the multivariate models that Dr. Cleland and his associates tested in their meta-analysis, in HFrEF patients in sinus rhythm, the relationship between reduced heart rate and mortality benefit was stronger statistically than between beta-blocker dosage and reduced mortality, he said. “This suggests to me that, while we should use the targeted beta-blocker dosages when we can, it’s more important to achieve a target heart rate in these patients of 55-65 bpm.”
Dr. Cleland hypothesized, based on a report presented at the same meeting by a different research group, that reduced heart rate is not beneficial in HFrEF patients with atrial fibrillation because in this subgroup slower heart rates linked with an increased number of brief pauses in left ventricular pumping. These pauses may result in ventricular arrhythmias, he speculated. “It may be that beta-blockers are equally effective at slowing heart rate in patients with or without atrial fibrillation, but there is also harm from beta-blockers because they’re causing pauses in patients with atrial fibrillation,” he said.
These days, if he has a HFrEF patient with atrial fibrillation whose heart rate slows to 60 bpm, he will stop digoxin treatment if the patient is on that drug, and he will also reduce the beta-blocker dosage but not discontinue it.
The findings came from the Collaborative Systematic Overview of Randomized Controlled Trials of Beta-Blockers in the Treatment of Heart Failure (BB-META-HF), which included data from 11 large beta-blocker randomized trials in heart failure that had been published during 1993-2005. The analysis included data from 17,378 HFrEF patients, with 14,313 (82%) in sinus rhythm and 3,065 (18%) with atrial fibrillation. Follow-up data of patients on treatment was available for 15,007 of these patients.
Dr. Cleland and his associates showed in multivariate analyses that, when they controlled for several baseline demographic and clinical variables among patients in sinus rhythm who received a beta-blocker, the follow-up all-cause mortality fell by 36%, compared with placebo, in patients with a resting baseline heart rate of less than 70 bpm; by 21%, compared with placebo, in patients with a baseline heart rate of 70-90 bpm; and by 38%, compared with placebo, in patients with a baseline heart rate of more than 90 bpm. All three reductions were statistically significant. In contrast, among patients who also had atrial fibrillation beta-blocker treatment linked with no significant mortality reduction, compared with placebo, for patients with any baseline heart rate. Concurrently with Dr. Cleland’s report at the meeting the results appeared online (J Amer Coll Cardiol. 2017 Apr 30. doi: 10.1016/j.jacc.2017.04.001).
[email protected]
On Twitter @mitchelzoler
AT HEART FAILURE 2017
Key clinical point:
Major finding: All-cause mortality was similar in patients with HFrEF and atrial fibrillation regardless of whether they received a beta-blocker or placebo.
Data source: BB-META-HF, a meta-analysis of 11 beta-blocker treatment trials with 17,378 HFrEF patients.
Disclosures: BB-META-HF received funding from Menarini and GlaxoSmithKline. Dr. Cleland has received research funding and honoraria from GlaxoSmithKline.
Bedside CGM boosts glucose control in hospital
BY RANDY DOTINGA
SAN DIEGO – Bedside continuous glucose monitoring (CGM) with a wireless hookup to a response team allowed doctors and nurses to gain better blood sugar control in hospitalized high-risk patients with diabetes, according to research reported at the annual scientific sessions of the American Diabetes Association.
“Continuous glucose monitoring and wireless connections can be useful in the hospital setting, not just in the outpatient setting,” said Maria Isabel Garcia, RN, of Scripps Whittier Diabetes Institute. “They help us to prevent problems rather than fixing them after they happen.”
Research suggests that complications due to dangerous blood sugar levels can lead to longer hospital stays, she noted.
For the study, researchers assigned 45 high-risk hospitalized patients with type 2 diabetes to be monitored by DexCom G4 CGM devices. The patients were being treated for a variety of conditions, and all were expected to be hospitalized for more than 2 days.
Researchers housed the normal-sized CGM devices in toolbox-sized containers at bedside. “We don’t want the equipment to get misplaced if the patient has to go from room to room or if the patient is discharged and takes the equipment by mistake,” Ms. Garcia said.
The patients were 43-82 years old (median, 61.4 years; standard deviation, 9.8), 56% male, 73% Hispanic (with 60% preferring to speak Spanish). The mean hemoglobin A1c was 10.2% (SD, 2.3), and the mean body mass index was 32.9 (SD, 8).
The patients were randomized to two groups. In both, the CGM devices were operative and tracked blood sugar levels. In one group, the information was transmitted via wireless hookup to a team of researchers (during the day) or a telemetry team (at night), who were alerted via alarms if blood sugar levels seemed too high or low. The teams would then alert nurses who’d confirm the levels via bedside testing and take appropriate action.
CGM data were gathered from the patients for an average of 4.2 days each (SD, 2.49; range 2-10), and the number of readings per patient ranged from 102 to 2,334 each (median 859.4; SD, 627.8).
The findings suggest that wireless transmission of CGM allowed hospital staff to improve blood sugar control. Readings under 70 mg/dL occurred 0.7% of the time in patients monitored via wireless hookup and 1.4% in the others. Readings over 250 mg/dL appeared 9.8% and 13.2% of the time, respectively and readings over 300 mg/dL appeared 2.6% and 5.1% of the time, respectively.
The investigators plan to recruit 460 patients for the study, Ms. Garcia said. Results may be available within a couple of years, she said.
DexCom provided the CGM devices for the study, which was funded by Diabetes Research Connection and the Confidence Foundation. Ms. Garcia reports no disclosures.
BY RANDY DOTINGA
SAN DIEGO – Bedside continuous glucose monitoring (CGM) with a wireless hookup to a response team allowed doctors and nurses to gain better blood sugar control in hospitalized high-risk patients with diabetes, according to research reported at the annual scientific sessions of the American Diabetes Association.
“Continuous glucose monitoring and wireless connections can be useful in the hospital setting, not just in the outpatient setting,” said Maria Isabel Garcia, RN, of Scripps Whittier Diabetes Institute. “They help us to prevent problems rather than fixing them after they happen.”
Research suggests that complications due to dangerous blood sugar levels can lead to longer hospital stays, she noted.
For the study, researchers assigned 45 high-risk hospitalized patients with type 2 diabetes to be monitored by DexCom G4 CGM devices. The patients were being treated for a variety of conditions, and all were expected to be hospitalized for more than 2 days.
Researchers housed the normal-sized CGM devices in toolbox-sized containers at bedside. “We don’t want the equipment to get misplaced if the patient has to go from room to room or if the patient is discharged and takes the equipment by mistake,” Ms. Garcia said.
The patients were 43-82 years old (median, 61.4 years; standard deviation, 9.8), 56% male, 73% Hispanic (with 60% preferring to speak Spanish). The mean hemoglobin A1c was 10.2% (SD, 2.3), and the mean body mass index was 32.9 (SD, 8).
The patients were randomized to two groups. In both, the CGM devices were operative and tracked blood sugar levels. In one group, the information was transmitted via wireless hookup to a team of researchers (during the day) or a telemetry team (at night), who were alerted via alarms if blood sugar levels seemed too high or low. The teams would then alert nurses who’d confirm the levels via bedside testing and take appropriate action.
CGM data were gathered from the patients for an average of 4.2 days each (SD, 2.49; range 2-10), and the number of readings per patient ranged from 102 to 2,334 each (median 859.4; SD, 627.8).
The findings suggest that wireless transmission of CGM allowed hospital staff to improve blood sugar control. Readings under 70 mg/dL occurred 0.7% of the time in patients monitored via wireless hookup and 1.4% in the others. Readings over 250 mg/dL appeared 9.8% and 13.2% of the time, respectively and readings over 300 mg/dL appeared 2.6% and 5.1% of the time, respectively.
The investigators plan to recruit 460 patients for the study, Ms. Garcia said. Results may be available within a couple of years, she said.
DexCom provided the CGM devices for the study, which was funded by Diabetes Research Connection and the Confidence Foundation. Ms. Garcia reports no disclosures.
BY RANDY DOTINGA
SAN DIEGO – Bedside continuous glucose monitoring (CGM) with a wireless hookup to a response team allowed doctors and nurses to gain better blood sugar control in hospitalized high-risk patients with diabetes, according to research reported at the annual scientific sessions of the American Diabetes Association.
“Continuous glucose monitoring and wireless connections can be useful in the hospital setting, not just in the outpatient setting,” said Maria Isabel Garcia, RN, of Scripps Whittier Diabetes Institute. “They help us to prevent problems rather than fixing them after they happen.”
Research suggests that complications due to dangerous blood sugar levels can lead to longer hospital stays, she noted.
For the study, researchers assigned 45 high-risk hospitalized patients with type 2 diabetes to be monitored by DexCom G4 CGM devices. The patients were being treated for a variety of conditions, and all were expected to be hospitalized for more than 2 days.
Researchers housed the normal-sized CGM devices in toolbox-sized containers at bedside. “We don’t want the equipment to get misplaced if the patient has to go from room to room or if the patient is discharged and takes the equipment by mistake,” Ms. Garcia said.
The patients were 43-82 years old (median, 61.4 years; standard deviation, 9.8), 56% male, 73% Hispanic (with 60% preferring to speak Spanish). The mean hemoglobin A1c was 10.2% (SD, 2.3), and the mean body mass index was 32.9 (SD, 8).
The patients were randomized to two groups. In both, the CGM devices were operative and tracked blood sugar levels. In one group, the information was transmitted via wireless hookup to a team of researchers (during the day) or a telemetry team (at night), who were alerted via alarms if blood sugar levels seemed too high or low. The teams would then alert nurses who’d confirm the levels via bedside testing and take appropriate action.
CGM data were gathered from the patients for an average of 4.2 days each (SD, 2.49; range 2-10), and the number of readings per patient ranged from 102 to 2,334 each (median 859.4; SD, 627.8).
The findings suggest that wireless transmission of CGM allowed hospital staff to improve blood sugar control. Readings under 70 mg/dL occurred 0.7% of the time in patients monitored via wireless hookup and 1.4% in the others. Readings over 250 mg/dL appeared 9.8% and 13.2% of the time, respectively and readings over 300 mg/dL appeared 2.6% and 5.1% of the time, respectively.
The investigators plan to recruit 460 patients for the study, Ms. Garcia said. Results may be available within a couple of years, she said.
DexCom provided the CGM devices for the study, which was funded by Diabetes Research Connection and the Confidence Foundation. Ms. Garcia reports no disclosures.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: about high or low readings.
Major finding: Readings under 70 mg/dL occurred 0.7% of the time in patients monitored via wireless hookup and 1.4% in other patients. Readings over 250 mg/dL appeared 9.8% and 13.2% of the time, respectively, and readings over 300 mg/dL appeared 2.6% and 5.1% of the time, respectively.
Data source: Early results from a pilot randomized, controlled study of 45 hospitalized, high-risk patients with type 2 diabetes. CGM devices measured glucose levels in all patients, but they were only transmitted via wireless hookup to teams in one group.
Disclosures: DexCom provided the CGM machines for the study, which was funded by Diabetes Research Connection and the Confidence Foundation. Garcia reports no disclosures.
Crossing the personal quality chasm: QI enthusiast to QI leader
Editor’s Note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Eric Howell, MD, MHM, professor of medicine at Johns Hopkins University, Baltimore.
For Eric Howell, MD, MHM, the journey to becoming a professor of medicine at Johns Hopkins University, past president of SHM, and director of SHM’s Leadership Academies commenced with a major quality improvement (QI) challenge.
Johns Hopkins Bayview Medical Center was struggling with throughput from the emergency department when Dr. Howell began practicing there in the early days of hospital medicine. “The ED said the medicine service was too slow, and the hospitalists said, ‘We’re working as fast as we can,’ ” Dr. Howell recalled of his real-world introduction to implementation science. “So, I took on triage oversight in 2000 and began streamlining flow.”
With a growing reputation for finding solutions to reduce readmissions and improve care transitions, Dr. Howell joined the Better Outcomes by Optimizing Safe Transitions (Project BOOST) project team in 2007 to codevelop one of SHM’s most successful programs. He humbly attributes some of this success to luck. “I happened to be at the right place at the right time. There was a problem, opportunity knocked, and I opened the door,” he said.
After some reflection, he pinpoints more tangible factors – a gift for innovative thinking and finding options that unify, rather than polarize, people and departments.
“I always ensure a solution makes the pie bigger, so that everyone benefits from it,” he said. “I don’t approach a problem like a sporting event, where one group wins and another loses.”
Dr. Howell says that an inclusive mindset is an important characteristic for anyone on a QI track because “it encourages buy-in from everyone who is impacted by a problem, and their investment in making the outcome successful.”
Skill development in areas such as leadership principles and processes such as lean will benefit those on a QI pathway, but finding the right mentors is just as critical. Dr. Howell looked to multiple people from diverse backgrounds, none of which included QI, to “help me move my skill set forward,” he said. “A clinical educator helped me to interact with other people, learn to facilitate an educational initiative, and lead people to change.”
Another mentor, he recalled, was an engineer who helped him figure out how to measure the success of his projects. And a third mentor cleared the pathway of obstructions, providing access to the people who would make his projects successful.
Being able to pivot is also important, Dr. Howell said. “Whether it is looking at data or the people you need to approach to solve a problem, be able to change your approach. Flip-flopping is a good thing in QI, because you’re always adjusting your tactics based on new information.”
Today, as SHM’s senior physician advisor to its Center for Quality Improvement, Dr. Howell holds multiple roles within the Johns Hopkins system and has received numerous awards for excellence in teaching and practice. The core principles that he started with on the path remain the same: “Be humble,” he said, “and give away credit. We are often collaborating with other professionals, so shining a light on the great work that they do will make projects more successful and improve the likelihood that they will want to collaborate with you in the future.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.
Editor’s Note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Eric Howell, MD, MHM, professor of medicine at Johns Hopkins University, Baltimore.
For Eric Howell, MD, MHM, the journey to becoming a professor of medicine at Johns Hopkins University, past president of SHM, and director of SHM’s Leadership Academies commenced with a major quality improvement (QI) challenge.
Johns Hopkins Bayview Medical Center was struggling with throughput from the emergency department when Dr. Howell began practicing there in the early days of hospital medicine. “The ED said the medicine service was too slow, and the hospitalists said, ‘We’re working as fast as we can,’ ” Dr. Howell recalled of his real-world introduction to implementation science. “So, I took on triage oversight in 2000 and began streamlining flow.”
With a growing reputation for finding solutions to reduce readmissions and improve care transitions, Dr. Howell joined the Better Outcomes by Optimizing Safe Transitions (Project BOOST) project team in 2007 to codevelop one of SHM’s most successful programs. He humbly attributes some of this success to luck. “I happened to be at the right place at the right time. There was a problem, opportunity knocked, and I opened the door,” he said.
After some reflection, he pinpoints more tangible factors – a gift for innovative thinking and finding options that unify, rather than polarize, people and departments.
“I always ensure a solution makes the pie bigger, so that everyone benefits from it,” he said. “I don’t approach a problem like a sporting event, where one group wins and another loses.”
Dr. Howell says that an inclusive mindset is an important characteristic for anyone on a QI track because “it encourages buy-in from everyone who is impacted by a problem, and their investment in making the outcome successful.”
Skill development in areas such as leadership principles and processes such as lean will benefit those on a QI pathway, but finding the right mentors is just as critical. Dr. Howell looked to multiple people from diverse backgrounds, none of which included QI, to “help me move my skill set forward,” he said. “A clinical educator helped me to interact with other people, learn to facilitate an educational initiative, and lead people to change.”
Another mentor, he recalled, was an engineer who helped him figure out how to measure the success of his projects. And a third mentor cleared the pathway of obstructions, providing access to the people who would make his projects successful.
Being able to pivot is also important, Dr. Howell said. “Whether it is looking at data or the people you need to approach to solve a problem, be able to change your approach. Flip-flopping is a good thing in QI, because you’re always adjusting your tactics based on new information.”
Today, as SHM’s senior physician advisor to its Center for Quality Improvement, Dr. Howell holds multiple roles within the Johns Hopkins system and has received numerous awards for excellence in teaching and practice. The core principles that he started with on the path remain the same: “Be humble,” he said, “and give away credit. We are often collaborating with other professionals, so shining a light on the great work that they do will make projects more successful and improve the likelihood that they will want to collaborate with you in the future.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.
Editor’s Note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Eric Howell, MD, MHM, professor of medicine at Johns Hopkins University, Baltimore.
For Eric Howell, MD, MHM, the journey to becoming a professor of medicine at Johns Hopkins University, past president of SHM, and director of SHM’s Leadership Academies commenced with a major quality improvement (QI) challenge.
Johns Hopkins Bayview Medical Center was struggling with throughput from the emergency department when Dr. Howell began practicing there in the early days of hospital medicine. “The ED said the medicine service was too slow, and the hospitalists said, ‘We’re working as fast as we can,’ ” Dr. Howell recalled of his real-world introduction to implementation science. “So, I took on triage oversight in 2000 and began streamlining flow.”
With a growing reputation for finding solutions to reduce readmissions and improve care transitions, Dr. Howell joined the Better Outcomes by Optimizing Safe Transitions (Project BOOST) project team in 2007 to codevelop one of SHM’s most successful programs. He humbly attributes some of this success to luck. “I happened to be at the right place at the right time. There was a problem, opportunity knocked, and I opened the door,” he said.
After some reflection, he pinpoints more tangible factors – a gift for innovative thinking and finding options that unify, rather than polarize, people and departments.
“I always ensure a solution makes the pie bigger, so that everyone benefits from it,” he said. “I don’t approach a problem like a sporting event, where one group wins and another loses.”
Dr. Howell says that an inclusive mindset is an important characteristic for anyone on a QI track because “it encourages buy-in from everyone who is impacted by a problem, and their investment in making the outcome successful.”
Skill development in areas such as leadership principles and processes such as lean will benefit those on a QI pathway, but finding the right mentors is just as critical. Dr. Howell looked to multiple people from diverse backgrounds, none of which included QI, to “help me move my skill set forward,” he said. “A clinical educator helped me to interact with other people, learn to facilitate an educational initiative, and lead people to change.”
Another mentor, he recalled, was an engineer who helped him figure out how to measure the success of his projects. And a third mentor cleared the pathway of obstructions, providing access to the people who would make his projects successful.
Being able to pivot is also important, Dr. Howell said. “Whether it is looking at data or the people you need to approach to solve a problem, be able to change your approach. Flip-flopping is a good thing in QI, because you’re always adjusting your tactics based on new information.”
Today, as SHM’s senior physician advisor to its Center for Quality Improvement, Dr. Howell holds multiple roles within the Johns Hopkins system and has received numerous awards for excellence in teaching and practice. The core principles that he started with on the path remain the same: “Be humble,” he said, “and give away credit. We are often collaborating with other professionals, so shining a light on the great work that they do will make projects more successful and improve the likelihood that they will want to collaborate with you in the future.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.
Low-dose aspirin bests dual-antiplatelet therapy in TAVR
PARIS – Single-antiplatelet therapy with low-dose aspirin following transcatheter aortic valve replacement (TAVR) reduced the occurrence of major adverse events, compared with guideline-recommended dual-antiplatelet therapy (DAPT), in the randomized ARTE trial.
The TAVR guideline recommendation for DAPT with low-dose aspirin plus clopidogrel is not based on evidence. It relies on expert opinion. ARTE (Aspirin Versus Aspirin + Clopidogrel Following TAVR) is the first sizable randomized trial to address the safety and efficacy of aspirin alone versus DAPT in the setting of TAVR, Josep Rodés-Cabau, MD, noted in presenting the ARTE results at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
ARTE was a multicenter, prospective, international open-label study of 222 TAVR patients who were randomized to 3 months of single-antiplatelet therapy (SAPT) with aspirin at 80-100 mg/day or to DAPT with aspirin at 80-100 mg/day plus clopidogrel at 75 mg/day after a single 300-mg loading dose. Participants had a mean Society of Thoracic Surgery Predicted Risk of Mortality score of 6.3%. The vast majority of participants received the balloon-expandable Edwards Lifesciences Sapien XT valve. The remainder got the Sapien 3 valve.
The primary outcome was the 3-month composite of death, MI, major or life-threatening bleeding, or stroke or transient ischemic attack. It occurred in 15.3% of the DAPT group and 7.2% on SAPT, a difference that didn’t reach statistical significance (P = .065) because of small patient numbers.
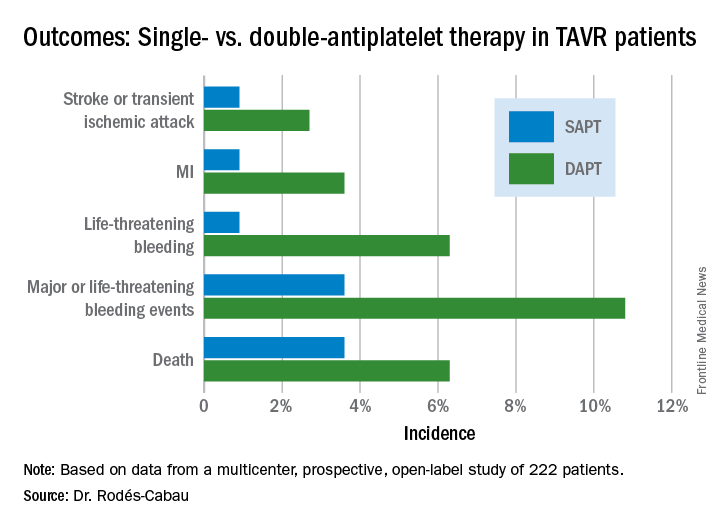
All subjects were on a proton pump inhibitor. The type, timing, and severity of bleeding events differed between the two study arms. All 4 bleeding events in the SAPT group were vascular in nature, while 5 of the 12 in the DAPT group were gastrointestinal. All the bleeding events in the SAPT group occurred within 72 hours after TAVR, whereas 5 of 12 in the DAPT recipients occurred later. Only one patient on SAPT experienced life-threatening bleeding, compared with seven DAPT patients who did.
“There were two prior smaller studies before ours,” according to Dr. Rodés-Cabau of Laval University in Quebec City. “One showed no differences, and an Italian one showed a tendency toward more bleeding with DAPT. So, I think there has been no sign to date that adding clopidogrel protects this group of patients from anything.”
Discussant Luis Nombela-Franco, MD, an interventional cardiologist at San Carlos Hospital in Madrid, pronounced the ARTE trial guideline-changing despite its limitations.
ARTE was supported by grants from Edwards Lifesciences and the Quebec Heart and Lung Institute.
Simultaneous with Dr. Rodés-Cabau’s presentation in Paris, the ARTE trial was published online (JACC Cardiovasc Interv. 2017 May 11. pii: S1936-8798[17]30812-9).
PARIS – Single-antiplatelet therapy with low-dose aspirin following transcatheter aortic valve replacement (TAVR) reduced the occurrence of major adverse events, compared with guideline-recommended dual-antiplatelet therapy (DAPT), in the randomized ARTE trial.
The TAVR guideline recommendation for DAPT with low-dose aspirin plus clopidogrel is not based on evidence. It relies on expert opinion. ARTE (Aspirin Versus Aspirin + Clopidogrel Following TAVR) is the first sizable randomized trial to address the safety and efficacy of aspirin alone versus DAPT in the setting of TAVR, Josep Rodés-Cabau, MD, noted in presenting the ARTE results at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
ARTE was a multicenter, prospective, international open-label study of 222 TAVR patients who were randomized to 3 months of single-antiplatelet therapy (SAPT) with aspirin at 80-100 mg/day or to DAPT with aspirin at 80-100 mg/day plus clopidogrel at 75 mg/day after a single 300-mg loading dose. Participants had a mean Society of Thoracic Surgery Predicted Risk of Mortality score of 6.3%. The vast majority of participants received the balloon-expandable Edwards Lifesciences Sapien XT valve. The remainder got the Sapien 3 valve.
The primary outcome was the 3-month composite of death, MI, major or life-threatening bleeding, or stroke or transient ischemic attack. It occurred in 15.3% of the DAPT group and 7.2% on SAPT, a difference that didn’t reach statistical significance (P = .065) because of small patient numbers.
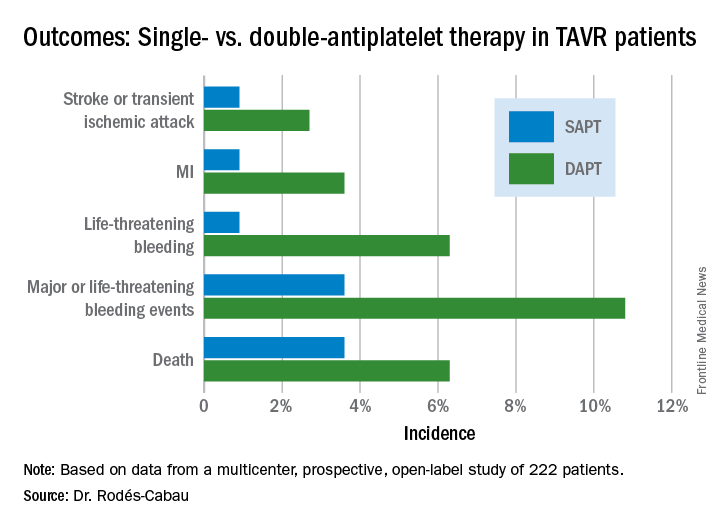
All subjects were on a proton pump inhibitor. The type, timing, and severity of bleeding events differed between the two study arms. All 4 bleeding events in the SAPT group were vascular in nature, while 5 of the 12 in the DAPT group were gastrointestinal. All the bleeding events in the SAPT group occurred within 72 hours after TAVR, whereas 5 of 12 in the DAPT recipients occurred later. Only one patient on SAPT experienced life-threatening bleeding, compared with seven DAPT patients who did.
“There were two prior smaller studies before ours,” according to Dr. Rodés-Cabau of Laval University in Quebec City. “One showed no differences, and an Italian one showed a tendency toward more bleeding with DAPT. So, I think there has been no sign to date that adding clopidogrel protects this group of patients from anything.”
Discussant Luis Nombela-Franco, MD, an interventional cardiologist at San Carlos Hospital in Madrid, pronounced the ARTE trial guideline-changing despite its limitations.
ARTE was supported by grants from Edwards Lifesciences and the Quebec Heart and Lung Institute.
Simultaneous with Dr. Rodés-Cabau’s presentation in Paris, the ARTE trial was published online (JACC Cardiovasc Interv. 2017 May 11. pii: S1936-8798[17]30812-9).
PARIS – Single-antiplatelet therapy with low-dose aspirin following transcatheter aortic valve replacement (TAVR) reduced the occurrence of major adverse events, compared with guideline-recommended dual-antiplatelet therapy (DAPT), in the randomized ARTE trial.
The TAVR guideline recommendation for DAPT with low-dose aspirin plus clopidogrel is not based on evidence. It relies on expert opinion. ARTE (Aspirin Versus Aspirin + Clopidogrel Following TAVR) is the first sizable randomized trial to address the safety and efficacy of aspirin alone versus DAPT in the setting of TAVR, Josep Rodés-Cabau, MD, noted in presenting the ARTE results at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
ARTE was a multicenter, prospective, international open-label study of 222 TAVR patients who were randomized to 3 months of single-antiplatelet therapy (SAPT) with aspirin at 80-100 mg/day or to DAPT with aspirin at 80-100 mg/day plus clopidogrel at 75 mg/day after a single 300-mg loading dose. Participants had a mean Society of Thoracic Surgery Predicted Risk of Mortality score of 6.3%. The vast majority of participants received the balloon-expandable Edwards Lifesciences Sapien XT valve. The remainder got the Sapien 3 valve.
The primary outcome was the 3-month composite of death, MI, major or life-threatening bleeding, or stroke or transient ischemic attack. It occurred in 15.3% of the DAPT group and 7.2% on SAPT, a difference that didn’t reach statistical significance (P = .065) because of small patient numbers.
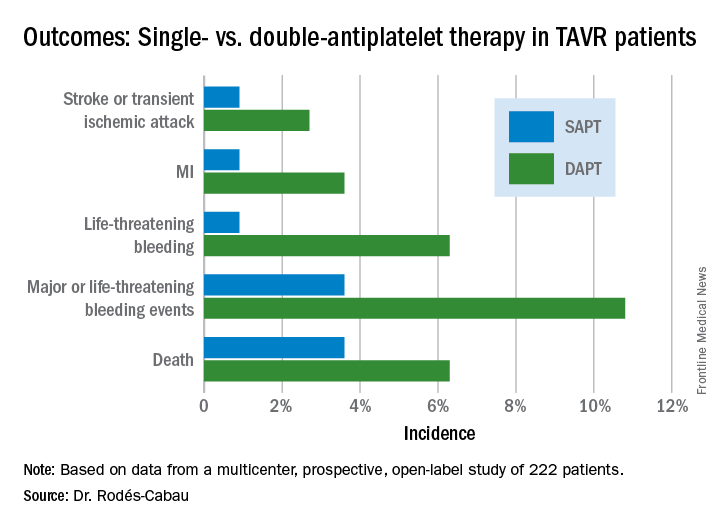
All subjects were on a proton pump inhibitor. The type, timing, and severity of bleeding events differed between the two study arms. All 4 bleeding events in the SAPT group were vascular in nature, while 5 of the 12 in the DAPT group were gastrointestinal. All the bleeding events in the SAPT group occurred within 72 hours after TAVR, whereas 5 of 12 in the DAPT recipients occurred later. Only one patient on SAPT experienced life-threatening bleeding, compared with seven DAPT patients who did.
“There were two prior smaller studies before ours,” according to Dr. Rodés-Cabau of Laval University in Quebec City. “One showed no differences, and an Italian one showed a tendency toward more bleeding with DAPT. So, I think there has been no sign to date that adding clopidogrel protects this group of patients from anything.”
Discussant Luis Nombela-Franco, MD, an interventional cardiologist at San Carlos Hospital in Madrid, pronounced the ARTE trial guideline-changing despite its limitations.
ARTE was supported by grants from Edwards Lifesciences and the Quebec Heart and Lung Institute.
Simultaneous with Dr. Rodés-Cabau’s presentation in Paris, the ARTE trial was published online (JACC Cardiovasc Interv. 2017 May 11. pii: S1936-8798[17]30812-9).
AT EUROPCR
Key clinical point:
Major finding: The 3-month composite of death, MI, major or life-threatening bleeding, or stroke or transient ischemic attack occurred in 15.3% of TAVR patients randomized to DAPT with low-dose aspirin plus clopidogrel, compared with 7.2% on aspirin only.
Data source: A randomized, multicenter, international, prospective open-label trial in 222 TAVR patients.
Disclosures: The presenter reported receiving research grants from Edwards Lifesciences and the Quebec Heart and Lung Institute, which supported the ARTE trial.
Everything We Say and Do: Setting discharge goals and visit expectations
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I always ensure at the end of my visit with a patient and their family that they know when to expect me to return to see their child again.
Why I do it
One of the biggest frustrations I hear from families pertains to the discharge process. In talking with families, they want to know the approximate time for discharge. Often, during morning rounds, we mention that the patient may be able to go home later in the day and we say that we will come in again later to check on them. However, unless we give families a time frame for when we will come back and do that check, they are left waiting without any clear expectations.
How I do it
One of our goals during morning family-centered rounds is to discuss discharge for every patient, every day. Along with discussing the possibility of going home, we try to give the family goals that they can work on throughout the day that are tied to discharge – for example, the approximate by-mouth intake for a toddler admitted for gastroenteritis and dehydration.
I also give the family an approximate time when either I or the resident team will come back to see if they have achieved this goal. This may be either late afternoon or first thing in the morning if we are planning an early-morning discharge before rounds. The families seem to find this helpful because they are not tied to the room all day waiting for the doctor to come back.
I also make sure that the families know they can contact their nurse any time if they need to see any of the doctors sooner than we planned. I let them know that a physician is here on the floor 24 hours a day and that the nurses can easily reach us at any time if they have further concerns. In my experience, this is reassuring to our families.
Christine Hrach is a pediatric hospitalist at Washington University School of Medicine in St. Louis.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I always ensure at the end of my visit with a patient and their family that they know when to expect me to return to see their child again.
Why I do it
One of the biggest frustrations I hear from families pertains to the discharge process. In talking with families, they want to know the approximate time for discharge. Often, during morning rounds, we mention that the patient may be able to go home later in the day and we say that we will come in again later to check on them. However, unless we give families a time frame for when we will come back and do that check, they are left waiting without any clear expectations.
How I do it
One of our goals during morning family-centered rounds is to discuss discharge for every patient, every day. Along with discussing the possibility of going home, we try to give the family goals that they can work on throughout the day that are tied to discharge – for example, the approximate by-mouth intake for a toddler admitted for gastroenteritis and dehydration.
I also give the family an approximate time when either I or the resident team will come back to see if they have achieved this goal. This may be either late afternoon or first thing in the morning if we are planning an early-morning discharge before rounds. The families seem to find this helpful because they are not tied to the room all day waiting for the doctor to come back.
I also make sure that the families know they can contact their nurse any time if they need to see any of the doctors sooner than we planned. I let them know that a physician is here on the floor 24 hours a day and that the nurses can easily reach us at any time if they have further concerns. In my experience, this is reassuring to our families.
Christine Hrach is a pediatric hospitalist at Washington University School of Medicine in St. Louis.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I always ensure at the end of my visit with a patient and their family that they know when to expect me to return to see their child again.
Why I do it
One of the biggest frustrations I hear from families pertains to the discharge process. In talking with families, they want to know the approximate time for discharge. Often, during morning rounds, we mention that the patient may be able to go home later in the day and we say that we will come in again later to check on them. However, unless we give families a time frame for when we will come back and do that check, they are left waiting without any clear expectations.
How I do it
One of our goals during morning family-centered rounds is to discuss discharge for every patient, every day. Along with discussing the possibility of going home, we try to give the family goals that they can work on throughout the day that are tied to discharge – for example, the approximate by-mouth intake for a toddler admitted for gastroenteritis and dehydration.
I also give the family an approximate time when either I or the resident team will come back to see if they have achieved this goal. This may be either late afternoon or first thing in the morning if we are planning an early-morning discharge before rounds. The families seem to find this helpful because they are not tied to the room all day waiting for the doctor to come back.
I also make sure that the families know they can contact their nurse any time if they need to see any of the doctors sooner than we planned. I let them know that a physician is here on the floor 24 hours a day and that the nurses can easily reach us at any time if they have further concerns. In my experience, this is reassuring to our families.
Christine Hrach is a pediatric hospitalist at Washington University School of Medicine in St. Louis.
New SHM Members – February/March 2017
The Society of Hospital Medicine welcomes its newest members:
Kwie-Hoa Siem, MD, Alaska
Frank Abene, Alabama
Kayla Maldonado, Alabama
Kenny Murray, MD, Alabama
Shanthan Ramidi, MD, Alabama
Lauren Hancock, APRN, Arkansas
William Hawkins, MD, Arkansas
Matthew Law, Arkansas
Emily Smith, MD, Arkansas
Firas Abbas, MBchB, Arizona
Shahid Ahmad, MD, MBBS, Arizona
Praveen Bheemanathini, Arizona
Atoosa Hosseini, Arizona
William McGrade, DO, Arizona
Konstantin Mazursky, DO, Arizona
Ibrahim Taweel, MD, Arizona
Kevin Virk, MD, FACP, Arizona
Kevin Virk, MD, FACP, Arizona
Mohemmedd Khalid Abbas, Arizona
Hasan Chaudhry, MD, Arizona
Kelly Kelleher, FAAP, Arizona
Priyanka Sultania Dudani, MBBS, Arizona
Krishna Kasireddy, MD, Arizona
Melanie Meguro, Arizona
Puneet Tuli, MD, Arizona
Jonathan Byrdy, DO, Arizona
Sarah Corral, DO, Arizona
Edward Maharam, MD, Arizona
Arvind Satyanarayan, DO, Arizona
Mayank Aggarwal, MD, Arizona
Syed Jafri, Arizona
Bujji Ainapurapu, MD, Arizona
Aaron Fernandes, MD, Arizona
Sonal Gandhi, Arizona
Sudhir Tutiki, Arizona
Navaneeth Kumar, MD, Arizona
Brian T. Courtney, MD, California
Won Jin Jeon, California
Veena Panduranga, MD, California
Jennifer Tinloy, DO, California
Debra Buckland Coffey, MCUSN, MD, California
Kathleen Teves, MD, California
Paul Goebel, MD, ACMPE, California
Shainy Hegde, California
Summaiya Muhammad, California
Desmond Wah, California
Chonn Khristin Ng, California
Almira Yang, DO, California
Salimah Boghani, MD, California
Stella Abhyankar, California
Cherie Ginwalla, MD, California
Armond Esmaili, California
Sarah Schaeffer, MD, MPH, California
Sophia Virani, MD, California
Dipti Munshi, MD, California
Judy Nguyen, DO, California
Daniel Owyang, DO, California
Christian Chiavetta, DO, California
David Reinert, DO, California
Joseph Pawlowski, MD, California
Eleanor Yang, California
Adrian Campo, MD, California
Emerson De Jesus, MD, California
Zachary Edmonds, MD, California
Trit Garg, California
Alexandra G. Ianculescu, MD, PhD, California
Felix Karp, MD, California
Cara Lai, California
Kristen Lew, MD, California
John Mogannam, California
Ameer Moussa, California
Neil Parikh, MD, MBA, California
Priya Reddy, California
Adam Simons, California
Sanjay Vadgama, MD, California
Kristofer Wills, DO, California
Michael Yang, MD, MS, California
Victor Ekuta, California,
Donna Colobong, PA-C, Colorado
Janna B. Dreason, FNP-C, Colorado
Cheryl English, NP-C, Colorado
Melanie Gerrior, MD, Colorado
Marciann Harris, NP, Colorado
Marsha Henke, MD, Colorado
Brett Hesse, Colorado
Naomi J Hipp, MD, Colorado
Aurell Horing, Colorado
Rachel Koch, DO, Colorado
Ed Marino, PA-C, Colorado
Marcus Reinhardt, MD, Colorado
Carol Runge, Colorado
Harshal Shah, Colorado
Leo Soehnlen, DO, Colorado
Anna Villalobos, MD, Colorado
Kathryn Whitfield, PA-C, Colorado
Jonathan Bei-Shing Young, MD, Colorado
Leah Damiani, MD, Colorado
Kathy Lynch, MD, Colorado
Micah Friedman, Colorado
Rachael Hilton, MD, Colorado
Madeline Koerner, Colorado
Chi Zheng, MD, Colorado
Chin-Kun Baw, MD, Connecticut
Alexandra Hawkins, NP, Connecticut
Vasundhara Singh, MD, MBBS, Connecticut
Ryan Quarles, MD, Connecticut
Debra Hernandez, APRN, BC, Connecticut
Karine Karapetyan, MD, Delaware
Choosak Burr, ARNP, Florida
Nelsi Mora, Florida
Mary Quillinan, Florida
Thuntanat Rachanakul, Florida
Samual W. Sauer, MD, MPH, Florida
Jennifer Tibangin, Florida
Keith Williams, MD, Florida
Eric Penedo, MD, Florida
Margaret Webb, Florida
Mark Bender, Florida
Brett Waress, MD, MHA, Florida
Giselle Racho, Florida
Bryan Thiel, Florida
Juan Loor Tuarez, MD, Florida
Christine Stopyra, Florida
Betsy Screws, ARNP, Florida
Jaimie Weber, MD, Florida
Priti Amin, MHA, Georgia
Naga Doddapaneni, Georgia
Stephanie Fletcher, Georgia
Disha Spath, MD, Georgia
Rafaela Wesley, DO, Georgia
Nikky Keer, DO, Georgia
James Kim, Georgia
Todd Martin, Georgia
Eli Mlaver, Georgia
Andrew Ritter, Georgia
Ali Al-Zubaidi, MBchB, Georgia
Deann Bing, MD, Georgia
Tushar Shah, Georgia
Cameron Straughn, DO, Georgia
Nobuhiro Ariyoshi, MEd, Hawaii
Prerna Kumar, Iowa
Jonathan Sebolt, MD, Iowa
Amy Tesar, DO, Iowa
Houng Chea, NP, Idaho
Finnegan Greer, PA-C, Idaho
Thao Nelson, PA, Idaho
Malatesha Gangappa, Idaho
Gloria Alumona, ACNP, Illinois
Ram Sanjeev Alur, Illinois
James Antoon, MD, FAAP, PhD, Illinois
Stefania Bailuc, MD, Illinois
Richard Huh, Illinois
Bhakti Patel, MD, Illinois
Frances Uy, ACNP, Illinois
Fernando Velazquez Vazquez, MD, Illinois
Tiffany White, MD, Illinois
Bryan P. Tully, MD, Illinois
Swati Gobhil, MBBS, Illinois
Lianghe Gao, Illinois
Gopi Astik, MD, Illinois
Marina Kovacevic, MD, Illinois
Abbie Raymond, DO, Illinois
Timothy Yung, Illinois
Ahmed Zahid, MD, Illinois
Cristina Corsini, MEd, Illinois
Faisal Rashid, MD, FACP, Illinois
Mansoor Ahmad, MD, Illinois
Matthew A. Strauch, DO, Illinois
Purshotham Reddy Grinne, Illinois
Nadia Nasreen, MD, Illinois
Maham Ashraf, MD, Indiana
Jennifer Gross, Indiana
Debasmita Mohapatra, MBBS, Indiana
Eric Scheper, Indiana
Katherine Gray, APRNBC, FNP, Indiana
Venkata Kureti, Indiana
Omer Al-Buoshkor, MD, Indiana
David Johnson, FNP, MSN, Indiana
Jonathan Salisbury, MD, Indiana
Debra Shapert, MSN, RN, Iowa
Lisa Carter, ARNP, Iowa
Matthew Woodham, Iowa
Tomoharu Suzuki, MD, Pharm, Japan
Khaldoun Haj, Kansas
Will Rogers, ACMPE, MA, MBA, Kansas
Karen Shumate, Kansas
Lisa Unruh, MD, Kansas
Matthew George, Kansas
Katie Washburn, DO, Kansas
Edwin Avallone, DO, Kentucky
Matthew Morris, Kentucky
Samantha Cappetto, MD, Kentucky
Jaison John, Kentucky
Ammar Al Jajeh, Kentucky
Joseph Bolger, MD, PhD, Louisiana
Clairissa Mulloy, Louisiana
Harish Talla, MD, Louisiana
John Amadon, Louisiana
Karthik Krishnareddy, Louisiana
Cheryl DeGrandpre, PA-C, Maine
Katherine Liu, MD, Maine
Sarah Sedney, MD, Maine
Aksana Afanasenka, MD, Maryland
Syed Nazeer Mahmood, MBBS, Maryland
Joseph Apata, MD, Maryland
Russom Ghebrai, MD, Maryland
Musa Momoh, MD, Maryland
Antanina Voit, Maryland
Dejene Kassaye, MD, MSC, Maryland
Shams Quazi, MD, FACP, MS, Maryland
Dawn Roelofs, FNP, MSN, Maryland
Kirsten Austad, MD, Massachusetts
Yoel Carrasquillo Vega, MD, Massachusetts
Michele Gaudet, NP, Massachusetts
Karina Mejias, Massachusetts
Peter Rohloff, MD, PhD, Massachusetts
Jennifer Schaeffer, Massachusetts
James Shaw, MD, Massachusetts
Renee Wheeler, Massachusetts
Angela Freeman, PA, PA-C, Massachusetts
Supriya Parvatini, MD, Massachusetts
Karen Jiang, MD, Massachusetts
Roula E. Abou-Nader, MD, Massachusetts
Shreekant Vasudhev, MD, Massachusetts
Nivedita Adabala, MD, MBBS, Michigan
Robert Behrendt, RN, BSN, Michigan
Molly Belisle, Michigan
Christine Dugan, MD, Michigan
Baljinder Gill, Michigan
Kellie Herringa, PA-C, Michigan
Christine Klingert, Michigan
Kathy Mitchell, Michigan
Aimee Vos, Michigan
Alyssa Churchill, DO, Michigan
Mailvaganam Sridharan, MD, Michigan
Atul Kapoor, MD, MBBS, Michigan
Anitha Kompally, MD, MBBS, Michigan
Nicole Webb, PA-C, Michigan
Abdulqadir Ahmad, MD, Minnesota
John Patrick Eikens, Minnesota
Bobbi Jo Jensen, PA-C, Minnesota
Rachel Keuseman, Minnesota
Stephen Palmquist, Minnesota
Manit Singla, MD, Minnesota
Douglas Berg, Minnesota
Nathan Palmolea, Minnesota
Molly Tureson, PAC, Minnesota
Mehdi Dastrange, MD, MHA, Minnesota
Kent Svee, Minnesota
Ashley Viere, PA-C, Minnesota
Molly Yang, MD, Minnesota
Paige Sams, DO, Minnesota
Amit Reddy, MBBS, Mississippi
Jacqueline Brooke Banks, FNP-C, Mississippi
Lori Foxworth, CFNP, Mississippi
Nicki Lawson, FNP-C, Mississippi
Bikash Acharya, Missouri
Zafar Ahmad, PA-C, Missouri
Harleen Chela, MD, Missouri
Jeffrey Chung, MD, Missouri
Daniel Kornfeld, Missouri
Erika Leung, MD, MSc, Missouri
Lisa Moser, PA, Missouri
Mark Stiffler, Missouri
Tushar Tarun, MBBS, Missouri
Nicole McLaughlin, Missouri
Katy Lohmann, PA-C, Missouri
Jayasree Bodagala, MD, Missouri
Ravi Kiran Morumuru, ACMPE, Missouri
Matthew Brown, MD, FAAFP, Missouri
Ravikanth Tadi, Missouri
Bazgha Ahmad, DO, Missouri
Monica Hawkins, RN, Missouri
Karri Vesey, BSN, Montana
Madison Vertin, PA-C, Montana
Urmila Mukherjee, MD, Nebraska
Noah Wiedel, MD, Nebraska
Sidrah Sheikh, MD, MBBS, Nebraska
Mohammad Esmadi, MBBS, Nebraska
Jill Zabih, MD, Nebraska
Jody Frey-Burns, RN, Nevada
Adnan Akbar, MD, Nevada
Peter Gayed, MRCP, New Hampshire
Jonathan T. Huntington, MD, New Hampshire
Meghan Meehan, ACNP, New Hampshire
Saurabh Mehta, MD, New Jersey
Hanaa Benchekroun Belabbes, MD, MHA, New Jersey
Hwan Kim, MD, New Jersey
Mary Tobiasson, USA, New Jersey
Muhammad Khakwani, MD, New Jersey
Amita Maibam, MD, MPH, New Jersey
Kumar Rohit, MBBS, New Jersey
Crystal Benjamin, MD, New Jersey
Rafael Garabis, New Mexico
Sam MacBride, MD, New Mexico
Indra Peram, MD, New Mexico
Sarah Vertrees, DO, New Mexico
Aswani Kumar Alavala, MD, New Mexico
Christopher Anstine, New Mexico
Prathima Guruguri, MD, New Mexico
Diedre Hofinger, MD, FACP, New Mexico
Katharine Juarez, New Mexico
Amtul Mahavesh, MD, New Mexico
Francisco Marquez, New Mexico
Payal Sen, MD, New Mexico
Morgan Wong, DO, New Mexico
Kelly Berchou, New York
Ronald Cho, New York
Nishil Dalsania, New York
Carolyn Drake, MD, MPH, New York
Leanne Forman, New York
Valerie Gausman, New York
Laurie Jacobs, New York
Janice Jang, MD, New York
Sonia Kohli, MD, New York
Nancy Lee, PA, New York
Allen Lee, MD, New York
Matthew McCarthy, FACP, New York
Akram Mohammed, MD, New York
Jennifer Nead, New York
Kristal Persaud, PA, New York
Mariya Rozenblit, MD, New York
Christian Torres, MD, New York
Sasha De Jesus, MD, New York
Gabriella Polyak, New York
Nataliya Yuklyaeva, MD, New York
Riyaz Kamadoli, MD, New York
Ramanuj Chakravarty, New York
Adil Zaidi, MD, New York
Allison Walker, MD, New York
Himali Gandhi, New York
Alexey Yanilshtein, MD, New York
Ramsey Al-Khalil, New York
Latoya Codougan, MD, New York
Khan Najmi, MD, New York
Sara Stream, MD, New York
Bhuwan Poudyal, MD, New York
Khalil Anchouche, New York
Sarah Azarchi, New York
Susana Bejar, New York
Brian Chang, New York
Jonathan Chen, New York
Hailey Gupta, MD, New York
Medhavi Gupta, New York
Ali Khan, New York
Benjamin Kwok, MD, New York
Billy Lin, New York
Katherine Ni, New York
Jina Park, New York
Gabriel Perreault, New York
Luis Alberto Romero, New York
Payal Shah, New York
Punita Shroff, New York
Scott Statman, New York
Maria Sunseri, New York
Benjamin Verplanke, New York
Audrey Zhang, New York
Gaby Razzouk, MD, New York
Pranitha Mantrala, MD, New York
Marsha Antoine, New York
Kanica Yashi, New York
Navid Ahmed, New York
Tasha Richards, PA, New York
Connor Tryon, MD, New York
Naveen Yarlagadda, MD, New York
Alex Hogan, New York
Andrew Donohoe, CCM, MD, North Carolina
Brittany Forshay, MD, North Carolina
Kelly Hammerbeck, FNP, North Carolina
Jennifer Hausman, North Carolina
Babajide Obisesan, North Carolina
Kwadwo Ofori, MD, North Carolina
Eric Ofosu, MD, North Carolina
Kale Roth, North Carolina
Robert Soma, PA-C, North Carolina
Sommany Weber, North Carolina
Ronnie Jacobs, North Carolina
Muhammad Ghani, MD, MACP, MBBS, North Carolina
Madeline Treasure, North Carolina
Andrew McWilliams, MD, North Carolina
Karen Payne, ACNP, MPH, North Carolina
Rafal Poplawski, MD, North Carolina
James Seal, PA-C, North Carolina
Farheen Qureshi, DO, North Carolina
Basavatti Sowmya, MD, MBBS, North Carolina
Eshwar Lal, MD, North Carolina
Catherine Hathaway, MD, North Carolina
Sherif Naguib, FAAFP, North Carolina
Sara Skavroneck, North Carolina
Charles Ofosu, North Carolina
Alex Alburquerque, MD, Ohio
Isha Butler, DO, Ohio
Anne Carrol, MD, Ohio
Scott Childers, MD, Ohio
Philip Jonas, MD, Ohio
Ahmadreza Karimianpour, Ohio
Rahul Kumar, MD, Ohio
George Maidaa, MD, Ohio
Kevin McAninch, Ohio
Jill Mccourt, FNP, Ohio
Roxanne Oliver, Ohio
Farah Hussain, Ohio
Natasha Axton, PA-C, Ohio
Brooke Harris, ACNP, Ohio
Vidhya Murukesan, MD, Ohio
Sara Dong, Ohio
Christie Astor, FNP, Ohio
Sunita Mall, MD, Ohio
Sunita Mall, MD, Ohio
Fouzia Tariq, MD, Ohio
Kaveri Sivaruban, MD, Ohio
Eunice Quicho, Ohio
Smitha Achuthankutty, MD, Ohio
Harmanpreet Shinh, MD, Ohio
Maereg Tesfaye, Ohio
Kalyn Jolivette, MD, Ohio
Richelle Voth, PA-C, Oklahoma
Samuel J. Ratermann, MD, FAAFP, Oklahoma
Richelle Voth, PA-C, Oklahoma
Alden Forrester, MD, Oregon
Nicholas Brown, DO, Oregon
Ian Pennell-Walklin, MD, Oregon
Bruce Ramsey, Oregon
Kyle Brekke, DO, Oregon
Sarah Webber, MD, Oregon
Brian Beaudoin, MD, Pennsylvania
Glenn Bedell, MHSA, Pennsylvania
Cristina Green, AGACNP-DNP, Pennsylvania
Andrew Groff, Pennsylvania
Sulman Masood Hashmi, MBBS, Pennsylvania
Eric Kasprowicz, MD, MPH, Pennsylvania
Laura Leuenberger, Pennsylvania
James Liszewski, MD, Pennsylvania
Caitlyn Moss, Pennsylvania
Paul Seunghyun Nho, Pennsylvania
Rishan Patel, MD, Pennsylvania
Dilli R. Poudel, MBBS, Pennsylvania
Naveen Yellappa, MBBS, Pennsylvania
Usman Zulfiqar, Pennsylvania
Nina Jain, Pennsylvania
Bhumika Patel, DO, Pennsylvania
Jenna M. Diasio, PA-C, Pennsylvania
Malachi Courtney, MD, Pennsylvania
Sonia Arneja, MD, Pennsylvania
Ross Ellis, MD, Pennsylvania
Samreen Siddiqui, Pennsylvania
Jillian Zavodnick, Pennsylvania
Kinan Kassar, MD, Pennsylvania
Maritsa M. Scoulos-Hanson, Pennsylvania
Jennifer Taylor, PA-C, Pennsylvania
Steven Delaveris, DO, Pennsylvania
Danica Buzniak, DO, Rhode Island
Paul Browning, MD, South Carolina
Matt Coones, MD, South Carolina
Cedric Fisher, MD, South Carolina
Aloysius Jackson, MD, South Carolina
Katharine DuPont, MD, South Carolina
Michael Jenkins, MD, South Carolina
Jessica Hamilton, APRN, BC, FNP, South Carolina
Pamela Pyle, DO, South Carolina
Shakeel Ahmed, MBBS, MD, South Dakota
D. Bruce Eaton, MD, South Dakota
Drew Jorgensen, MD, South Dakota
Shelly Turbak, MSN, RN, South Dakota
Tamera Sturm, DO, South Dakota
Peggy Brooks, Tennessee
Joseph Garrido, MD, Tennessee
Lisa Grimes, FNP, Tennessee
Chennakesava Kummathi, MBBS, Tennessee
Victoria Okafor, Tennessee
Ashley Smith, Tennessee
Monisha Bhatia, Tennessee
Belinda Jenkins, APRN-BC, Tennessee
Kim Zahnke, MD, Tennessee
Robert Arias, Texas
Nicolas Batterton, MD, Texas
Scott DePaul, MD, Texas
Nancy Foster, Texas
Larry Hughes, Texas
Erin Koval, Texas
Femi Layiwola, MD, Texas
Krysta Lin, Texas
James J. Onorato, MD, PhD, Texas
Allison Stephenson, PA-C, Texas
Brandon Stormes, Texas
Rubin Simon, MD, Texas
Brian Anderson, DO, Texas
Hatim Chhatriwala, MD, Texas
Aziz Hammoud, Texas
Haru Yamamoto, MD, Texas
Lauren Schiegg, Texas
Victoria Grasso, DO, Texas
Victor Salcedo, MD, Texas
Rajiv Bhattarai, Texas
Iram Qureshi, DO, Texas
Lisa Hafemeister, FACHE, MHA, Texas
Helena Kurian, MD, Texas
Jessica Lin, Texas
Nathan Nowalk, MD, Texas
Keely Smith, MD, Texas
Jonathan Weiser, MD, Texas
Roland Prezas, DO, FAAFP, Texas
Allan Recto, AHIP, Texas
Regina Dimbo, Texas
Venkata Ghanta, Texas
Richmond Hunt, Texas
Vishal Patel, MD, Texas
Zain Sharif, MD, Texas
Rommel Del Rosario, MD, Texas
Khawer Khadimally, DO, Texas
Diogenes Valderrama, MD, Texas
Charles Ewoh, MD, Texas
Deepika Kilaru, Texas
Tilahun Belay, MD, Texas
Chandra S Reddy Navuluri, MD, Texas
Bradley Goad, DO, FACP, Virginia
Patrick Higdon, MD, Virginia
Gabriella Miller, MD, HMDC, Virginia
Miklos Szentirmai, MD, Virginia
Hyder Tamton, Virginia
Andra Mirescu, MD, Virginia
Olukayode Ojo, Virginia
Robert Szeles, MD, Virginia
Anya Cope, DO, Virginia
OsCiriah Press, MD, Virginia
Rikin Kadakia, MD, Virginia
Bryant Self, DO, Virginia
Sarah Sabo, ACNP, Virginia
Pedro A. Gonzales Alvarez, MD, Virginia
William Best, Virginia
Pushpanjali Basnyat, MD, Washington
Nikki Hartley-Jonason, Washington
Helen Johnsonwall, MD, Washington
Eric LaMotte, MD, Washington
Maher Muraywid, Washington
Evan Neal Paul, MD, Washington
Sarah Rogers, MD, Washington
Lindee Strizich, Washington
Maryam Tariq, MBBS, Washington
Meghaan Walsh, MD, Washington
Oleg Zbirun, MD, Washington
Meeta Sabnis, MD, Washington
James Kuo, MD, Washington
Liang Du, Washington
Syed Farhan Tabraiz Hashmi, MD, Washington
Jessica Jung, MD, Washington
Joshua Pelley, MD, Washington
Alex Yu, MD, Washington
Alfred Curnow, MD, Washington
Duhwan Kang, Washington
Gilbert Daniel, MD, Washington, D.C.
Eleanor Fitall, Washington, D.C.
Vinay Srinivasan, Washington, D.C.
Scott Wine, West Virginia
Trevor Miller, MBA, PA-C, West Virginia
Audrey Hiltunen, Wisconsin
Elina Litinskaya, Wisconsin
John M. Murphy, MD, Wisconsin
Tanya Pedretti, PA, Wisconsin
Adine Rodemeyer, MD, Wisconsin
Oghomwen Sule, MBBS, Wisconsin
Terrence Witt, MD, Wisconsin
Mayank Arora, Wisconsin
John D. MacDonald, MD, Wisconsin
Abigail Cook, Wisconsin
Mohamed Ibrahim, MD, Wisconsin
Aymen Khogali, MD, Wisconsin
Nicholas Haun, Wisconsin
Sandra Brown, Victoria, Australia
Alessandra Gessner, Alberta, Canada
Courtney Carlucci, British Columbia, Canada
Muhanad Y. Al Habash, Canada
Karen Tong, MD, Canada
Taku Yabuki, Japan
Liza van Loon, the Netherlands
Edward Gebuis, MD, the Netherlands
Abdisalan Afrah, MD, Qatar
Akhnuwkh Jones, Qatar
Mashuk Uddin, MBBS, MRCP, FRCP, Qatar
Ibrahim Yusuf Abubeker, MRCP, Qatar
Chih-Wei Tseng, Taiwan
Sawsan Abdel-Razig, MD, FACP, United Arab Emirates
The Society of Hospital Medicine welcomes its newest members:
Kwie-Hoa Siem, MD, Alaska
Frank Abene, Alabama
Kayla Maldonado, Alabama
Kenny Murray, MD, Alabama
Shanthan Ramidi, MD, Alabama
Lauren Hancock, APRN, Arkansas
William Hawkins, MD, Arkansas
Matthew Law, Arkansas
Emily Smith, MD, Arkansas
Firas Abbas, MBchB, Arizona
Shahid Ahmad, MD, MBBS, Arizona
Praveen Bheemanathini, Arizona
Atoosa Hosseini, Arizona
William McGrade, DO, Arizona
Konstantin Mazursky, DO, Arizona
Ibrahim Taweel, MD, Arizona
Kevin Virk, MD, FACP, Arizona
Kevin Virk, MD, FACP, Arizona
Mohemmedd Khalid Abbas, Arizona
Hasan Chaudhry, MD, Arizona
Kelly Kelleher, FAAP, Arizona
Priyanka Sultania Dudani, MBBS, Arizona
Krishna Kasireddy, MD, Arizona
Melanie Meguro, Arizona
Puneet Tuli, MD, Arizona
Jonathan Byrdy, DO, Arizona
Sarah Corral, DO, Arizona
Edward Maharam, MD, Arizona
Arvind Satyanarayan, DO, Arizona
Mayank Aggarwal, MD, Arizona
Syed Jafri, Arizona
Bujji Ainapurapu, MD, Arizona
Aaron Fernandes, MD, Arizona
Sonal Gandhi, Arizona
Sudhir Tutiki, Arizona
Navaneeth Kumar, MD, Arizona
Brian T. Courtney, MD, California
Won Jin Jeon, California
Veena Panduranga, MD, California
Jennifer Tinloy, DO, California
Debra Buckland Coffey, MCUSN, MD, California
Kathleen Teves, MD, California
Paul Goebel, MD, ACMPE, California
Shainy Hegde, California
Summaiya Muhammad, California
Desmond Wah, California
Chonn Khristin Ng, California
Almira Yang, DO, California
Salimah Boghani, MD, California
Stella Abhyankar, California
Cherie Ginwalla, MD, California
Armond Esmaili, California
Sarah Schaeffer, MD, MPH, California
Sophia Virani, MD, California
Dipti Munshi, MD, California
Judy Nguyen, DO, California
Daniel Owyang, DO, California
Christian Chiavetta, DO, California
David Reinert, DO, California
Joseph Pawlowski, MD, California
Eleanor Yang, California
Adrian Campo, MD, California
Emerson De Jesus, MD, California
Zachary Edmonds, MD, California
Trit Garg, California
Alexandra G. Ianculescu, MD, PhD, California
Felix Karp, MD, California
Cara Lai, California
Kristen Lew, MD, California
John Mogannam, California
Ameer Moussa, California
Neil Parikh, MD, MBA, California
Priya Reddy, California
Adam Simons, California
Sanjay Vadgama, MD, California
Kristofer Wills, DO, California
Michael Yang, MD, MS, California
Victor Ekuta, California,
Donna Colobong, PA-C, Colorado
Janna B. Dreason, FNP-C, Colorado
Cheryl English, NP-C, Colorado
Melanie Gerrior, MD, Colorado
Marciann Harris, NP, Colorado
Marsha Henke, MD, Colorado
Brett Hesse, Colorado
Naomi J Hipp, MD, Colorado
Aurell Horing, Colorado
Rachel Koch, DO, Colorado
Ed Marino, PA-C, Colorado
Marcus Reinhardt, MD, Colorado
Carol Runge, Colorado
Harshal Shah, Colorado
Leo Soehnlen, DO, Colorado
Anna Villalobos, MD, Colorado
Kathryn Whitfield, PA-C, Colorado
Jonathan Bei-Shing Young, MD, Colorado
Leah Damiani, MD, Colorado
Kathy Lynch, MD, Colorado
Micah Friedman, Colorado
Rachael Hilton, MD, Colorado
Madeline Koerner, Colorado
Chi Zheng, MD, Colorado
Chin-Kun Baw, MD, Connecticut
Alexandra Hawkins, NP, Connecticut
Vasundhara Singh, MD, MBBS, Connecticut
Ryan Quarles, MD, Connecticut
Debra Hernandez, APRN, BC, Connecticut
Karine Karapetyan, MD, Delaware
Choosak Burr, ARNP, Florida
Nelsi Mora, Florida
Mary Quillinan, Florida
Thuntanat Rachanakul, Florida
Samual W. Sauer, MD, MPH, Florida
Jennifer Tibangin, Florida
Keith Williams, MD, Florida
Eric Penedo, MD, Florida
Margaret Webb, Florida
Mark Bender, Florida
Brett Waress, MD, MHA, Florida
Giselle Racho, Florida
Bryan Thiel, Florida
Juan Loor Tuarez, MD, Florida
Christine Stopyra, Florida
Betsy Screws, ARNP, Florida
Jaimie Weber, MD, Florida
Priti Amin, MHA, Georgia
Naga Doddapaneni, Georgia
Stephanie Fletcher, Georgia
Disha Spath, MD, Georgia
Rafaela Wesley, DO, Georgia
Nikky Keer, DO, Georgia
James Kim, Georgia
Todd Martin, Georgia
Eli Mlaver, Georgia
Andrew Ritter, Georgia
Ali Al-Zubaidi, MBchB, Georgia
Deann Bing, MD, Georgia
Tushar Shah, Georgia
Cameron Straughn, DO, Georgia
Nobuhiro Ariyoshi, MEd, Hawaii
Prerna Kumar, Iowa
Jonathan Sebolt, MD, Iowa
Amy Tesar, DO, Iowa
Houng Chea, NP, Idaho
Finnegan Greer, PA-C, Idaho
Thao Nelson, PA, Idaho
Malatesha Gangappa, Idaho
Gloria Alumona, ACNP, Illinois
Ram Sanjeev Alur, Illinois
James Antoon, MD, FAAP, PhD, Illinois
Stefania Bailuc, MD, Illinois
Richard Huh, Illinois
Bhakti Patel, MD, Illinois
Frances Uy, ACNP, Illinois
Fernando Velazquez Vazquez, MD, Illinois
Tiffany White, MD, Illinois
Bryan P. Tully, MD, Illinois
Swati Gobhil, MBBS, Illinois
Lianghe Gao, Illinois
Gopi Astik, MD, Illinois
Marina Kovacevic, MD, Illinois
Abbie Raymond, DO, Illinois
Timothy Yung, Illinois
Ahmed Zahid, MD, Illinois
Cristina Corsini, MEd, Illinois
Faisal Rashid, MD, FACP, Illinois
Mansoor Ahmad, MD, Illinois
Matthew A. Strauch, DO, Illinois
Purshotham Reddy Grinne, Illinois
Nadia Nasreen, MD, Illinois
Maham Ashraf, MD, Indiana
Jennifer Gross, Indiana
Debasmita Mohapatra, MBBS, Indiana
Eric Scheper, Indiana
Katherine Gray, APRNBC, FNP, Indiana
Venkata Kureti, Indiana
Omer Al-Buoshkor, MD, Indiana
David Johnson, FNP, MSN, Indiana
Jonathan Salisbury, MD, Indiana
Debra Shapert, MSN, RN, Iowa
Lisa Carter, ARNP, Iowa
Matthew Woodham, Iowa
Tomoharu Suzuki, MD, Pharm, Japan
Khaldoun Haj, Kansas
Will Rogers, ACMPE, MA, MBA, Kansas
Karen Shumate, Kansas
Lisa Unruh, MD, Kansas
Matthew George, Kansas
Katie Washburn, DO, Kansas
Edwin Avallone, DO, Kentucky
Matthew Morris, Kentucky
Samantha Cappetto, MD, Kentucky
Jaison John, Kentucky
Ammar Al Jajeh, Kentucky
Joseph Bolger, MD, PhD, Louisiana
Clairissa Mulloy, Louisiana
Harish Talla, MD, Louisiana
John Amadon, Louisiana
Karthik Krishnareddy, Louisiana
Cheryl DeGrandpre, PA-C, Maine
Katherine Liu, MD, Maine
Sarah Sedney, MD, Maine
Aksana Afanasenka, MD, Maryland
Syed Nazeer Mahmood, MBBS, Maryland
Joseph Apata, MD, Maryland
Russom Ghebrai, MD, Maryland
Musa Momoh, MD, Maryland
Antanina Voit, Maryland
Dejene Kassaye, MD, MSC, Maryland
Shams Quazi, MD, FACP, MS, Maryland
Dawn Roelofs, FNP, MSN, Maryland
Kirsten Austad, MD, Massachusetts
Yoel Carrasquillo Vega, MD, Massachusetts
Michele Gaudet, NP, Massachusetts
Karina Mejias, Massachusetts
Peter Rohloff, MD, PhD, Massachusetts
Jennifer Schaeffer, Massachusetts
James Shaw, MD, Massachusetts
Renee Wheeler, Massachusetts
Angela Freeman, PA, PA-C, Massachusetts
Supriya Parvatini, MD, Massachusetts
Karen Jiang, MD, Massachusetts
Roula E. Abou-Nader, MD, Massachusetts
Shreekant Vasudhev, MD, Massachusetts
Nivedita Adabala, MD, MBBS, Michigan
Robert Behrendt, RN, BSN, Michigan
Molly Belisle, Michigan
Christine Dugan, MD, Michigan
Baljinder Gill, Michigan
Kellie Herringa, PA-C, Michigan
Christine Klingert, Michigan
Kathy Mitchell, Michigan
Aimee Vos, Michigan
Alyssa Churchill, DO, Michigan
Mailvaganam Sridharan, MD, Michigan
Atul Kapoor, MD, MBBS, Michigan
Anitha Kompally, MD, MBBS, Michigan
Nicole Webb, PA-C, Michigan
Abdulqadir Ahmad, MD, Minnesota
John Patrick Eikens, Minnesota
Bobbi Jo Jensen, PA-C, Minnesota
Rachel Keuseman, Minnesota
Stephen Palmquist, Minnesota
Manit Singla, MD, Minnesota
Douglas Berg, Minnesota
Nathan Palmolea, Minnesota
Molly Tureson, PAC, Minnesota
Mehdi Dastrange, MD, MHA, Minnesota
Kent Svee, Minnesota
Ashley Viere, PA-C, Minnesota
Molly Yang, MD, Minnesota
Paige Sams, DO, Minnesota
Amit Reddy, MBBS, Mississippi
Jacqueline Brooke Banks, FNP-C, Mississippi
Lori Foxworth, CFNP, Mississippi
Nicki Lawson, FNP-C, Mississippi
Bikash Acharya, Missouri
Zafar Ahmad, PA-C, Missouri
Harleen Chela, MD, Missouri
Jeffrey Chung, MD, Missouri
Daniel Kornfeld, Missouri
Erika Leung, MD, MSc, Missouri
Lisa Moser, PA, Missouri
Mark Stiffler, Missouri
Tushar Tarun, MBBS, Missouri
Nicole McLaughlin, Missouri
Katy Lohmann, PA-C, Missouri
Jayasree Bodagala, MD, Missouri
Ravi Kiran Morumuru, ACMPE, Missouri
Matthew Brown, MD, FAAFP, Missouri
Ravikanth Tadi, Missouri
Bazgha Ahmad, DO, Missouri
Monica Hawkins, RN, Missouri
Karri Vesey, BSN, Montana
Madison Vertin, PA-C, Montana
Urmila Mukherjee, MD, Nebraska
Noah Wiedel, MD, Nebraska
Sidrah Sheikh, MD, MBBS, Nebraska
Mohammad Esmadi, MBBS, Nebraska
Jill Zabih, MD, Nebraska
Jody Frey-Burns, RN, Nevada
Adnan Akbar, MD, Nevada
Peter Gayed, MRCP, New Hampshire
Jonathan T. Huntington, MD, New Hampshire
Meghan Meehan, ACNP, New Hampshire
Saurabh Mehta, MD, New Jersey
Hanaa Benchekroun Belabbes, MD, MHA, New Jersey
Hwan Kim, MD, New Jersey
Mary Tobiasson, USA, New Jersey
Muhammad Khakwani, MD, New Jersey
Amita Maibam, MD, MPH, New Jersey
Kumar Rohit, MBBS, New Jersey
Crystal Benjamin, MD, New Jersey
Rafael Garabis, New Mexico
Sam MacBride, MD, New Mexico
Indra Peram, MD, New Mexico
Sarah Vertrees, DO, New Mexico
Aswani Kumar Alavala, MD, New Mexico
Christopher Anstine, New Mexico
Prathima Guruguri, MD, New Mexico
Diedre Hofinger, MD, FACP, New Mexico
Katharine Juarez, New Mexico
Amtul Mahavesh, MD, New Mexico
Francisco Marquez, New Mexico
Payal Sen, MD, New Mexico
Morgan Wong, DO, New Mexico
Kelly Berchou, New York
Ronald Cho, New York
Nishil Dalsania, New York
Carolyn Drake, MD, MPH, New York
Leanne Forman, New York
Valerie Gausman, New York
Laurie Jacobs, New York
Janice Jang, MD, New York
Sonia Kohli, MD, New York
Nancy Lee, PA, New York
Allen Lee, MD, New York
Matthew McCarthy, FACP, New York
Akram Mohammed, MD, New York
Jennifer Nead, New York
Kristal Persaud, PA, New York
Mariya Rozenblit, MD, New York
Christian Torres, MD, New York
Sasha De Jesus, MD, New York
Gabriella Polyak, New York
Nataliya Yuklyaeva, MD, New York
Riyaz Kamadoli, MD, New York
Ramanuj Chakravarty, New York
Adil Zaidi, MD, New York
Allison Walker, MD, New York
Himali Gandhi, New York
Alexey Yanilshtein, MD, New York
Ramsey Al-Khalil, New York
Latoya Codougan, MD, New York
Khan Najmi, MD, New York
Sara Stream, MD, New York
Bhuwan Poudyal, MD, New York
Khalil Anchouche, New York
Sarah Azarchi, New York
Susana Bejar, New York
Brian Chang, New York
Jonathan Chen, New York
Hailey Gupta, MD, New York
Medhavi Gupta, New York
Ali Khan, New York
Benjamin Kwok, MD, New York
Billy Lin, New York
Katherine Ni, New York
Jina Park, New York
Gabriel Perreault, New York
Luis Alberto Romero, New York
Payal Shah, New York
Punita Shroff, New York
Scott Statman, New York
Maria Sunseri, New York
Benjamin Verplanke, New York
Audrey Zhang, New York
Gaby Razzouk, MD, New York
Pranitha Mantrala, MD, New York
Marsha Antoine, New York
Kanica Yashi, New York
Navid Ahmed, New York
Tasha Richards, PA, New York
Connor Tryon, MD, New York
Naveen Yarlagadda, MD, New York
Alex Hogan, New York
Andrew Donohoe, CCM, MD, North Carolina
Brittany Forshay, MD, North Carolina
Kelly Hammerbeck, FNP, North Carolina
Jennifer Hausman, North Carolina
Babajide Obisesan, North Carolina
Kwadwo Ofori, MD, North Carolina
Eric Ofosu, MD, North Carolina
Kale Roth, North Carolina
Robert Soma, PA-C, North Carolina
Sommany Weber, North Carolina
Ronnie Jacobs, North Carolina
Muhammad Ghani, MD, MACP, MBBS, North Carolina
Madeline Treasure, North Carolina
Andrew McWilliams, MD, North Carolina
Karen Payne, ACNP, MPH, North Carolina
Rafal Poplawski, MD, North Carolina
James Seal, PA-C, North Carolina
Farheen Qureshi, DO, North Carolina
Basavatti Sowmya, MD, MBBS, North Carolina
Eshwar Lal, MD, North Carolina
Catherine Hathaway, MD, North Carolina
Sherif Naguib, FAAFP, North Carolina
Sara Skavroneck, North Carolina
Charles Ofosu, North Carolina
Alex Alburquerque, MD, Ohio
Isha Butler, DO, Ohio
Anne Carrol, MD, Ohio
Scott Childers, MD, Ohio
Philip Jonas, MD, Ohio
Ahmadreza Karimianpour, Ohio
Rahul Kumar, MD, Ohio
George Maidaa, MD, Ohio
Kevin McAninch, Ohio
Jill Mccourt, FNP, Ohio
Roxanne Oliver, Ohio
Farah Hussain, Ohio
Natasha Axton, PA-C, Ohio
Brooke Harris, ACNP, Ohio
Vidhya Murukesan, MD, Ohio
Sara Dong, Ohio
Christie Astor, FNP, Ohio
Sunita Mall, MD, Ohio
Sunita Mall, MD, Ohio
Fouzia Tariq, MD, Ohio
Kaveri Sivaruban, MD, Ohio
Eunice Quicho, Ohio
Smitha Achuthankutty, MD, Ohio
Harmanpreet Shinh, MD, Ohio
Maereg Tesfaye, Ohio
Kalyn Jolivette, MD, Ohio
Richelle Voth, PA-C, Oklahoma
Samuel J. Ratermann, MD, FAAFP, Oklahoma
Richelle Voth, PA-C, Oklahoma
Alden Forrester, MD, Oregon
Nicholas Brown, DO, Oregon
Ian Pennell-Walklin, MD, Oregon
Bruce Ramsey, Oregon
Kyle Brekke, DO, Oregon
Sarah Webber, MD, Oregon
Brian Beaudoin, MD, Pennsylvania
Glenn Bedell, MHSA, Pennsylvania
Cristina Green, AGACNP-DNP, Pennsylvania
Andrew Groff, Pennsylvania
Sulman Masood Hashmi, MBBS, Pennsylvania
Eric Kasprowicz, MD, MPH, Pennsylvania
Laura Leuenberger, Pennsylvania
James Liszewski, MD, Pennsylvania
Caitlyn Moss, Pennsylvania
Paul Seunghyun Nho, Pennsylvania
Rishan Patel, MD, Pennsylvania
Dilli R. Poudel, MBBS, Pennsylvania
Naveen Yellappa, MBBS, Pennsylvania
Usman Zulfiqar, Pennsylvania
Nina Jain, Pennsylvania
Bhumika Patel, DO, Pennsylvania
Jenna M. Diasio, PA-C, Pennsylvania
Malachi Courtney, MD, Pennsylvania
Sonia Arneja, MD, Pennsylvania
Ross Ellis, MD, Pennsylvania
Samreen Siddiqui, Pennsylvania
Jillian Zavodnick, Pennsylvania
Kinan Kassar, MD, Pennsylvania
Maritsa M. Scoulos-Hanson, Pennsylvania
Jennifer Taylor, PA-C, Pennsylvania
Steven Delaveris, DO, Pennsylvania
Danica Buzniak, DO, Rhode Island
Paul Browning, MD, South Carolina
Matt Coones, MD, South Carolina
Cedric Fisher, MD, South Carolina
Aloysius Jackson, MD, South Carolina
Katharine DuPont, MD, South Carolina
Michael Jenkins, MD, South Carolina
Jessica Hamilton, APRN, BC, FNP, South Carolina
Pamela Pyle, DO, South Carolina
Shakeel Ahmed, MBBS, MD, South Dakota
D. Bruce Eaton, MD, South Dakota
Drew Jorgensen, MD, South Dakota
Shelly Turbak, MSN, RN, South Dakota
Tamera Sturm, DO, South Dakota
Peggy Brooks, Tennessee
Joseph Garrido, MD, Tennessee
Lisa Grimes, FNP, Tennessee
Chennakesava Kummathi, MBBS, Tennessee
Victoria Okafor, Tennessee
Ashley Smith, Tennessee
Monisha Bhatia, Tennessee
Belinda Jenkins, APRN-BC, Tennessee
Kim Zahnke, MD, Tennessee
Robert Arias, Texas
Nicolas Batterton, MD, Texas
Scott DePaul, MD, Texas
Nancy Foster, Texas
Larry Hughes, Texas
Erin Koval, Texas
Femi Layiwola, MD, Texas
Krysta Lin, Texas
James J. Onorato, MD, PhD, Texas
Allison Stephenson, PA-C, Texas
Brandon Stormes, Texas
Rubin Simon, MD, Texas
Brian Anderson, DO, Texas
Hatim Chhatriwala, MD, Texas
Aziz Hammoud, Texas
Haru Yamamoto, MD, Texas
Lauren Schiegg, Texas
Victoria Grasso, DO, Texas
Victor Salcedo, MD, Texas
Rajiv Bhattarai, Texas
Iram Qureshi, DO, Texas
Lisa Hafemeister, FACHE, MHA, Texas
Helena Kurian, MD, Texas
Jessica Lin, Texas
Nathan Nowalk, MD, Texas
Keely Smith, MD, Texas
Jonathan Weiser, MD, Texas
Roland Prezas, DO, FAAFP, Texas
Allan Recto, AHIP, Texas
Regina Dimbo, Texas
Venkata Ghanta, Texas
Richmond Hunt, Texas
Vishal Patel, MD, Texas
Zain Sharif, MD, Texas
Rommel Del Rosario, MD, Texas
Khawer Khadimally, DO, Texas
Diogenes Valderrama, MD, Texas
Charles Ewoh, MD, Texas
Deepika Kilaru, Texas
Tilahun Belay, MD, Texas
Chandra S Reddy Navuluri, MD, Texas
Bradley Goad, DO, FACP, Virginia
Patrick Higdon, MD, Virginia
Gabriella Miller, MD, HMDC, Virginia
Miklos Szentirmai, MD, Virginia
Hyder Tamton, Virginia
Andra Mirescu, MD, Virginia
Olukayode Ojo, Virginia
Robert Szeles, MD, Virginia
Anya Cope, DO, Virginia
OsCiriah Press, MD, Virginia
Rikin Kadakia, MD, Virginia
Bryant Self, DO, Virginia
Sarah Sabo, ACNP, Virginia
Pedro A. Gonzales Alvarez, MD, Virginia
William Best, Virginia
Pushpanjali Basnyat, MD, Washington
Nikki Hartley-Jonason, Washington
Helen Johnsonwall, MD, Washington
Eric LaMotte, MD, Washington
Maher Muraywid, Washington
Evan Neal Paul, MD, Washington
Sarah Rogers, MD, Washington
Lindee Strizich, Washington
Maryam Tariq, MBBS, Washington
Meghaan Walsh, MD, Washington
Oleg Zbirun, MD, Washington
Meeta Sabnis, MD, Washington
James Kuo, MD, Washington
Liang Du, Washington
Syed Farhan Tabraiz Hashmi, MD, Washington
Jessica Jung, MD, Washington
Joshua Pelley, MD, Washington
Alex Yu, MD, Washington
Alfred Curnow, MD, Washington
Duhwan Kang, Washington
Gilbert Daniel, MD, Washington, D.C.
Eleanor Fitall, Washington, D.C.
Vinay Srinivasan, Washington, D.C.
Scott Wine, West Virginia
Trevor Miller, MBA, PA-C, West Virginia
Audrey Hiltunen, Wisconsin
Elina Litinskaya, Wisconsin
John M. Murphy, MD, Wisconsin
Tanya Pedretti, PA, Wisconsin
Adine Rodemeyer, MD, Wisconsin
Oghomwen Sule, MBBS, Wisconsin
Terrence Witt, MD, Wisconsin
Mayank Arora, Wisconsin
John D. MacDonald, MD, Wisconsin
Abigail Cook, Wisconsin
Mohamed Ibrahim, MD, Wisconsin
Aymen Khogali, MD, Wisconsin
Nicholas Haun, Wisconsin
Sandra Brown, Victoria, Australia
Alessandra Gessner, Alberta, Canada
Courtney Carlucci, British Columbia, Canada
Muhanad Y. Al Habash, Canada
Karen Tong, MD, Canada
Taku Yabuki, Japan
Liza van Loon, the Netherlands
Edward Gebuis, MD, the Netherlands
Abdisalan Afrah, MD, Qatar
Akhnuwkh Jones, Qatar
Mashuk Uddin, MBBS, MRCP, FRCP, Qatar
Ibrahim Yusuf Abubeker, MRCP, Qatar
Chih-Wei Tseng, Taiwan
Sawsan Abdel-Razig, MD, FACP, United Arab Emirates
The Society of Hospital Medicine welcomes its newest members:
Kwie-Hoa Siem, MD, Alaska
Frank Abene, Alabama
Kayla Maldonado, Alabama
Kenny Murray, MD, Alabama
Shanthan Ramidi, MD, Alabama
Lauren Hancock, APRN, Arkansas
William Hawkins, MD, Arkansas
Matthew Law, Arkansas
Emily Smith, MD, Arkansas
Firas Abbas, MBchB, Arizona
Shahid Ahmad, MD, MBBS, Arizona
Praveen Bheemanathini, Arizona
Atoosa Hosseini, Arizona
William McGrade, DO, Arizona
Konstantin Mazursky, DO, Arizona
Ibrahim Taweel, MD, Arizona
Kevin Virk, MD, FACP, Arizona
Kevin Virk, MD, FACP, Arizona
Mohemmedd Khalid Abbas, Arizona
Hasan Chaudhry, MD, Arizona
Kelly Kelleher, FAAP, Arizona
Priyanka Sultania Dudani, MBBS, Arizona
Krishna Kasireddy, MD, Arizona
Melanie Meguro, Arizona
Puneet Tuli, MD, Arizona
Jonathan Byrdy, DO, Arizona
Sarah Corral, DO, Arizona
Edward Maharam, MD, Arizona
Arvind Satyanarayan, DO, Arizona
Mayank Aggarwal, MD, Arizona
Syed Jafri, Arizona
Bujji Ainapurapu, MD, Arizona
Aaron Fernandes, MD, Arizona
Sonal Gandhi, Arizona
Sudhir Tutiki, Arizona
Navaneeth Kumar, MD, Arizona
Brian T. Courtney, MD, California
Won Jin Jeon, California
Veena Panduranga, MD, California
Jennifer Tinloy, DO, California
Debra Buckland Coffey, MCUSN, MD, California
Kathleen Teves, MD, California
Paul Goebel, MD, ACMPE, California
Shainy Hegde, California
Summaiya Muhammad, California
Desmond Wah, California
Chonn Khristin Ng, California
Almira Yang, DO, California
Salimah Boghani, MD, California
Stella Abhyankar, California
Cherie Ginwalla, MD, California
Armond Esmaili, California
Sarah Schaeffer, MD, MPH, California
Sophia Virani, MD, California
Dipti Munshi, MD, California
Judy Nguyen, DO, California
Daniel Owyang, DO, California
Christian Chiavetta, DO, California
David Reinert, DO, California
Joseph Pawlowski, MD, California
Eleanor Yang, California
Adrian Campo, MD, California
Emerson De Jesus, MD, California
Zachary Edmonds, MD, California
Trit Garg, California
Alexandra G. Ianculescu, MD, PhD, California
Felix Karp, MD, California
Cara Lai, California
Kristen Lew, MD, California
John Mogannam, California
Ameer Moussa, California
Neil Parikh, MD, MBA, California
Priya Reddy, California
Adam Simons, California
Sanjay Vadgama, MD, California
Kristofer Wills, DO, California
Michael Yang, MD, MS, California
Victor Ekuta, California,
Donna Colobong, PA-C, Colorado
Janna B. Dreason, FNP-C, Colorado
Cheryl English, NP-C, Colorado
Melanie Gerrior, MD, Colorado
Marciann Harris, NP, Colorado
Marsha Henke, MD, Colorado
Brett Hesse, Colorado
Naomi J Hipp, MD, Colorado
Aurell Horing, Colorado
Rachel Koch, DO, Colorado
Ed Marino, PA-C, Colorado
Marcus Reinhardt, MD, Colorado
Carol Runge, Colorado
Harshal Shah, Colorado
Leo Soehnlen, DO, Colorado
Anna Villalobos, MD, Colorado
Kathryn Whitfield, PA-C, Colorado
Jonathan Bei-Shing Young, MD, Colorado
Leah Damiani, MD, Colorado
Kathy Lynch, MD, Colorado
Micah Friedman, Colorado
Rachael Hilton, MD, Colorado
Madeline Koerner, Colorado
Chi Zheng, MD, Colorado
Chin-Kun Baw, MD, Connecticut
Alexandra Hawkins, NP, Connecticut
Vasundhara Singh, MD, MBBS, Connecticut
Ryan Quarles, MD, Connecticut
Debra Hernandez, APRN, BC, Connecticut
Karine Karapetyan, MD, Delaware
Choosak Burr, ARNP, Florida
Nelsi Mora, Florida
Mary Quillinan, Florida
Thuntanat Rachanakul, Florida
Samual W. Sauer, MD, MPH, Florida
Jennifer Tibangin, Florida
Keith Williams, MD, Florida
Eric Penedo, MD, Florida
Margaret Webb, Florida
Mark Bender, Florida
Brett Waress, MD, MHA, Florida
Giselle Racho, Florida
Bryan Thiel, Florida
Juan Loor Tuarez, MD, Florida
Christine Stopyra, Florida
Betsy Screws, ARNP, Florida
Jaimie Weber, MD, Florida
Priti Amin, MHA, Georgia
Naga Doddapaneni, Georgia
Stephanie Fletcher, Georgia
Disha Spath, MD, Georgia
Rafaela Wesley, DO, Georgia
Nikky Keer, DO, Georgia
James Kim, Georgia
Todd Martin, Georgia
Eli Mlaver, Georgia
Andrew Ritter, Georgia
Ali Al-Zubaidi, MBchB, Georgia
Deann Bing, MD, Georgia
Tushar Shah, Georgia
Cameron Straughn, DO, Georgia
Nobuhiro Ariyoshi, MEd, Hawaii
Prerna Kumar, Iowa
Jonathan Sebolt, MD, Iowa
Amy Tesar, DO, Iowa
Houng Chea, NP, Idaho
Finnegan Greer, PA-C, Idaho
Thao Nelson, PA, Idaho
Malatesha Gangappa, Idaho
Gloria Alumona, ACNP, Illinois
Ram Sanjeev Alur, Illinois
James Antoon, MD, FAAP, PhD, Illinois
Stefania Bailuc, MD, Illinois
Richard Huh, Illinois
Bhakti Patel, MD, Illinois
Frances Uy, ACNP, Illinois
Fernando Velazquez Vazquez, MD, Illinois
Tiffany White, MD, Illinois
Bryan P. Tully, MD, Illinois
Swati Gobhil, MBBS, Illinois
Lianghe Gao, Illinois
Gopi Astik, MD, Illinois
Marina Kovacevic, MD, Illinois
Abbie Raymond, DO, Illinois
Timothy Yung, Illinois
Ahmed Zahid, MD, Illinois
Cristina Corsini, MEd, Illinois
Faisal Rashid, MD, FACP, Illinois
Mansoor Ahmad, MD, Illinois
Matthew A. Strauch, DO, Illinois
Purshotham Reddy Grinne, Illinois
Nadia Nasreen, MD, Illinois
Maham Ashraf, MD, Indiana
Jennifer Gross, Indiana
Debasmita Mohapatra, MBBS, Indiana
Eric Scheper, Indiana
Katherine Gray, APRNBC, FNP, Indiana
Venkata Kureti, Indiana
Omer Al-Buoshkor, MD, Indiana
David Johnson, FNP, MSN, Indiana
Jonathan Salisbury, MD, Indiana
Debra Shapert, MSN, RN, Iowa
Lisa Carter, ARNP, Iowa
Matthew Woodham, Iowa
Tomoharu Suzuki, MD, Pharm, Japan
Khaldoun Haj, Kansas
Will Rogers, ACMPE, MA, MBA, Kansas
Karen Shumate, Kansas
Lisa Unruh, MD, Kansas
Matthew George, Kansas
Katie Washburn, DO, Kansas
Edwin Avallone, DO, Kentucky
Matthew Morris, Kentucky
Samantha Cappetto, MD, Kentucky
Jaison John, Kentucky
Ammar Al Jajeh, Kentucky
Joseph Bolger, MD, PhD, Louisiana
Clairissa Mulloy, Louisiana
Harish Talla, MD, Louisiana
John Amadon, Louisiana
Karthik Krishnareddy, Louisiana
Cheryl DeGrandpre, PA-C, Maine
Katherine Liu, MD, Maine
Sarah Sedney, MD, Maine
Aksana Afanasenka, MD, Maryland
Syed Nazeer Mahmood, MBBS, Maryland
Joseph Apata, MD, Maryland
Russom Ghebrai, MD, Maryland
Musa Momoh, MD, Maryland
Antanina Voit, Maryland
Dejene Kassaye, MD, MSC, Maryland
Shams Quazi, MD, FACP, MS, Maryland
Dawn Roelofs, FNP, MSN, Maryland
Kirsten Austad, MD, Massachusetts
Yoel Carrasquillo Vega, MD, Massachusetts
Michele Gaudet, NP, Massachusetts
Karina Mejias, Massachusetts
Peter Rohloff, MD, PhD, Massachusetts
Jennifer Schaeffer, Massachusetts
James Shaw, MD, Massachusetts
Renee Wheeler, Massachusetts
Angela Freeman, PA, PA-C, Massachusetts
Supriya Parvatini, MD, Massachusetts
Karen Jiang, MD, Massachusetts
Roula E. Abou-Nader, MD, Massachusetts
Shreekant Vasudhev, MD, Massachusetts
Nivedita Adabala, MD, MBBS, Michigan
Robert Behrendt, RN, BSN, Michigan
Molly Belisle, Michigan
Christine Dugan, MD, Michigan
Baljinder Gill, Michigan
Kellie Herringa, PA-C, Michigan
Christine Klingert, Michigan
Kathy Mitchell, Michigan
Aimee Vos, Michigan
Alyssa Churchill, DO, Michigan
Mailvaganam Sridharan, MD, Michigan
Atul Kapoor, MD, MBBS, Michigan
Anitha Kompally, MD, MBBS, Michigan
Nicole Webb, PA-C, Michigan
Abdulqadir Ahmad, MD, Minnesota
John Patrick Eikens, Minnesota
Bobbi Jo Jensen, PA-C, Minnesota
Rachel Keuseman, Minnesota
Stephen Palmquist, Minnesota
Manit Singla, MD, Minnesota
Douglas Berg, Minnesota
Nathan Palmolea, Minnesota
Molly Tureson, PAC, Minnesota
Mehdi Dastrange, MD, MHA, Minnesota
Kent Svee, Minnesota
Ashley Viere, PA-C, Minnesota
Molly Yang, MD, Minnesota
Paige Sams, DO, Minnesota
Amit Reddy, MBBS, Mississippi
Jacqueline Brooke Banks, FNP-C, Mississippi
Lori Foxworth, CFNP, Mississippi
Nicki Lawson, FNP-C, Mississippi
Bikash Acharya, Missouri
Zafar Ahmad, PA-C, Missouri
Harleen Chela, MD, Missouri
Jeffrey Chung, MD, Missouri
Daniel Kornfeld, Missouri
Erika Leung, MD, MSc, Missouri
Lisa Moser, PA, Missouri
Mark Stiffler, Missouri
Tushar Tarun, MBBS, Missouri
Nicole McLaughlin, Missouri
Katy Lohmann, PA-C, Missouri
Jayasree Bodagala, MD, Missouri
Ravi Kiran Morumuru, ACMPE, Missouri
Matthew Brown, MD, FAAFP, Missouri
Ravikanth Tadi, Missouri
Bazgha Ahmad, DO, Missouri
Monica Hawkins, RN, Missouri
Karri Vesey, BSN, Montana
Madison Vertin, PA-C, Montana
Urmila Mukherjee, MD, Nebraska
Noah Wiedel, MD, Nebraska
Sidrah Sheikh, MD, MBBS, Nebraska
Mohammad Esmadi, MBBS, Nebraska
Jill Zabih, MD, Nebraska
Jody Frey-Burns, RN, Nevada
Adnan Akbar, MD, Nevada
Peter Gayed, MRCP, New Hampshire
Jonathan T. Huntington, MD, New Hampshire
Meghan Meehan, ACNP, New Hampshire
Saurabh Mehta, MD, New Jersey
Hanaa Benchekroun Belabbes, MD, MHA, New Jersey
Hwan Kim, MD, New Jersey
Mary Tobiasson, USA, New Jersey
Muhammad Khakwani, MD, New Jersey
Amita Maibam, MD, MPH, New Jersey
Kumar Rohit, MBBS, New Jersey
Crystal Benjamin, MD, New Jersey
Rafael Garabis, New Mexico
Sam MacBride, MD, New Mexico
Indra Peram, MD, New Mexico
Sarah Vertrees, DO, New Mexico
Aswani Kumar Alavala, MD, New Mexico
Christopher Anstine, New Mexico
Prathima Guruguri, MD, New Mexico
Diedre Hofinger, MD, FACP, New Mexico
Katharine Juarez, New Mexico
Amtul Mahavesh, MD, New Mexico
Francisco Marquez, New Mexico
Payal Sen, MD, New Mexico
Morgan Wong, DO, New Mexico
Kelly Berchou, New York
Ronald Cho, New York
Nishil Dalsania, New York
Carolyn Drake, MD, MPH, New York
Leanne Forman, New York
Valerie Gausman, New York
Laurie Jacobs, New York
Janice Jang, MD, New York
Sonia Kohli, MD, New York
Nancy Lee, PA, New York
Allen Lee, MD, New York
Matthew McCarthy, FACP, New York
Akram Mohammed, MD, New York
Jennifer Nead, New York
Kristal Persaud, PA, New York
Mariya Rozenblit, MD, New York
Christian Torres, MD, New York
Sasha De Jesus, MD, New York
Gabriella Polyak, New York
Nataliya Yuklyaeva, MD, New York
Riyaz Kamadoli, MD, New York
Ramanuj Chakravarty, New York
Adil Zaidi, MD, New York
Allison Walker, MD, New York
Himali Gandhi, New York
Alexey Yanilshtein, MD, New York
Ramsey Al-Khalil, New York
Latoya Codougan, MD, New York
Khan Najmi, MD, New York
Sara Stream, MD, New York
Bhuwan Poudyal, MD, New York
Khalil Anchouche, New York
Sarah Azarchi, New York
Susana Bejar, New York
Brian Chang, New York
Jonathan Chen, New York
Hailey Gupta, MD, New York
Medhavi Gupta, New York
Ali Khan, New York
Benjamin Kwok, MD, New York
Billy Lin, New York
Katherine Ni, New York
Jina Park, New York
Gabriel Perreault, New York
Luis Alberto Romero, New York
Payal Shah, New York
Punita Shroff, New York
Scott Statman, New York
Maria Sunseri, New York
Benjamin Verplanke, New York
Audrey Zhang, New York
Gaby Razzouk, MD, New York
Pranitha Mantrala, MD, New York
Marsha Antoine, New York
Kanica Yashi, New York
Navid Ahmed, New York
Tasha Richards, PA, New York
Connor Tryon, MD, New York
Naveen Yarlagadda, MD, New York
Alex Hogan, New York
Andrew Donohoe, CCM, MD, North Carolina
Brittany Forshay, MD, North Carolina
Kelly Hammerbeck, FNP, North Carolina
Jennifer Hausman, North Carolina
Babajide Obisesan, North Carolina
Kwadwo Ofori, MD, North Carolina
Eric Ofosu, MD, North Carolina
Kale Roth, North Carolina
Robert Soma, PA-C, North Carolina
Sommany Weber, North Carolina
Ronnie Jacobs, North Carolina
Muhammad Ghani, MD, MACP, MBBS, North Carolina
Madeline Treasure, North Carolina
Andrew McWilliams, MD, North Carolina
Karen Payne, ACNP, MPH, North Carolina
Rafal Poplawski, MD, North Carolina
James Seal, PA-C, North Carolina
Farheen Qureshi, DO, North Carolina
Basavatti Sowmya, MD, MBBS, North Carolina
Eshwar Lal, MD, North Carolina
Catherine Hathaway, MD, North Carolina
Sherif Naguib, FAAFP, North Carolina
Sara Skavroneck, North Carolina
Charles Ofosu, North Carolina
Alex Alburquerque, MD, Ohio
Isha Butler, DO, Ohio
Anne Carrol, MD, Ohio
Scott Childers, MD, Ohio
Philip Jonas, MD, Ohio
Ahmadreza Karimianpour, Ohio
Rahul Kumar, MD, Ohio
George Maidaa, MD, Ohio
Kevin McAninch, Ohio
Jill Mccourt, FNP, Ohio
Roxanne Oliver, Ohio
Farah Hussain, Ohio
Natasha Axton, PA-C, Ohio
Brooke Harris, ACNP, Ohio
Vidhya Murukesan, MD, Ohio
Sara Dong, Ohio
Christie Astor, FNP, Ohio
Sunita Mall, MD, Ohio
Sunita Mall, MD, Ohio
Fouzia Tariq, MD, Ohio
Kaveri Sivaruban, MD, Ohio
Eunice Quicho, Ohio
Smitha Achuthankutty, MD, Ohio
Harmanpreet Shinh, MD, Ohio
Maereg Tesfaye, Ohio
Kalyn Jolivette, MD, Ohio
Richelle Voth, PA-C, Oklahoma
Samuel J. Ratermann, MD, FAAFP, Oklahoma
Richelle Voth, PA-C, Oklahoma
Alden Forrester, MD, Oregon
Nicholas Brown, DO, Oregon
Ian Pennell-Walklin, MD, Oregon
Bruce Ramsey, Oregon
Kyle Brekke, DO, Oregon
Sarah Webber, MD, Oregon
Brian Beaudoin, MD, Pennsylvania
Glenn Bedell, MHSA, Pennsylvania
Cristina Green, AGACNP-DNP, Pennsylvania
Andrew Groff, Pennsylvania
Sulman Masood Hashmi, MBBS, Pennsylvania
Eric Kasprowicz, MD, MPH, Pennsylvania
Laura Leuenberger, Pennsylvania
James Liszewski, MD, Pennsylvania
Caitlyn Moss, Pennsylvania
Paul Seunghyun Nho, Pennsylvania
Rishan Patel, MD, Pennsylvania
Dilli R. Poudel, MBBS, Pennsylvania
Naveen Yellappa, MBBS, Pennsylvania
Usman Zulfiqar, Pennsylvania
Nina Jain, Pennsylvania
Bhumika Patel, DO, Pennsylvania
Jenna M. Diasio, PA-C, Pennsylvania
Malachi Courtney, MD, Pennsylvania
Sonia Arneja, MD, Pennsylvania
Ross Ellis, MD, Pennsylvania
Samreen Siddiqui, Pennsylvania
Jillian Zavodnick, Pennsylvania
Kinan Kassar, MD, Pennsylvania
Maritsa M. Scoulos-Hanson, Pennsylvania
Jennifer Taylor, PA-C, Pennsylvania
Steven Delaveris, DO, Pennsylvania
Danica Buzniak, DO, Rhode Island
Paul Browning, MD, South Carolina
Matt Coones, MD, South Carolina
Cedric Fisher, MD, South Carolina
Aloysius Jackson, MD, South Carolina
Katharine DuPont, MD, South Carolina
Michael Jenkins, MD, South Carolina
Jessica Hamilton, APRN, BC, FNP, South Carolina
Pamela Pyle, DO, South Carolina
Shakeel Ahmed, MBBS, MD, South Dakota
D. Bruce Eaton, MD, South Dakota
Drew Jorgensen, MD, South Dakota
Shelly Turbak, MSN, RN, South Dakota
Tamera Sturm, DO, South Dakota
Peggy Brooks, Tennessee
Joseph Garrido, MD, Tennessee
Lisa Grimes, FNP, Tennessee
Chennakesava Kummathi, MBBS, Tennessee
Victoria Okafor, Tennessee
Ashley Smith, Tennessee
Monisha Bhatia, Tennessee
Belinda Jenkins, APRN-BC, Tennessee
Kim Zahnke, MD, Tennessee
Robert Arias, Texas
Nicolas Batterton, MD, Texas
Scott DePaul, MD, Texas
Nancy Foster, Texas
Larry Hughes, Texas
Erin Koval, Texas
Femi Layiwola, MD, Texas
Krysta Lin, Texas
James J. Onorato, MD, PhD, Texas
Allison Stephenson, PA-C, Texas
Brandon Stormes, Texas
Rubin Simon, MD, Texas
Brian Anderson, DO, Texas
Hatim Chhatriwala, MD, Texas
Aziz Hammoud, Texas
Haru Yamamoto, MD, Texas
Lauren Schiegg, Texas
Victoria Grasso, DO, Texas
Victor Salcedo, MD, Texas
Rajiv Bhattarai, Texas
Iram Qureshi, DO, Texas
Lisa Hafemeister, FACHE, MHA, Texas
Helena Kurian, MD, Texas
Jessica Lin, Texas
Nathan Nowalk, MD, Texas
Keely Smith, MD, Texas
Jonathan Weiser, MD, Texas
Roland Prezas, DO, FAAFP, Texas
Allan Recto, AHIP, Texas
Regina Dimbo, Texas
Venkata Ghanta, Texas
Richmond Hunt, Texas
Vishal Patel, MD, Texas
Zain Sharif, MD, Texas
Rommel Del Rosario, MD, Texas
Khawer Khadimally, DO, Texas
Diogenes Valderrama, MD, Texas
Charles Ewoh, MD, Texas
Deepika Kilaru, Texas
Tilahun Belay, MD, Texas
Chandra S Reddy Navuluri, MD, Texas
Bradley Goad, DO, FACP, Virginia
Patrick Higdon, MD, Virginia
Gabriella Miller, MD, HMDC, Virginia
Miklos Szentirmai, MD, Virginia
Hyder Tamton, Virginia
Andra Mirescu, MD, Virginia
Olukayode Ojo, Virginia
Robert Szeles, MD, Virginia
Anya Cope, DO, Virginia
OsCiriah Press, MD, Virginia
Rikin Kadakia, MD, Virginia
Bryant Self, DO, Virginia
Sarah Sabo, ACNP, Virginia
Pedro A. Gonzales Alvarez, MD, Virginia
William Best, Virginia
Pushpanjali Basnyat, MD, Washington
Nikki Hartley-Jonason, Washington
Helen Johnsonwall, MD, Washington
Eric LaMotte, MD, Washington
Maher Muraywid, Washington
Evan Neal Paul, MD, Washington
Sarah Rogers, MD, Washington
Lindee Strizich, Washington
Maryam Tariq, MBBS, Washington
Meghaan Walsh, MD, Washington
Oleg Zbirun, MD, Washington
Meeta Sabnis, MD, Washington
James Kuo, MD, Washington
Liang Du, Washington
Syed Farhan Tabraiz Hashmi, MD, Washington
Jessica Jung, MD, Washington
Joshua Pelley, MD, Washington
Alex Yu, MD, Washington
Alfred Curnow, MD, Washington
Duhwan Kang, Washington
Gilbert Daniel, MD, Washington, D.C.
Eleanor Fitall, Washington, D.C.
Vinay Srinivasan, Washington, D.C.
Scott Wine, West Virginia
Trevor Miller, MBA, PA-C, West Virginia
Audrey Hiltunen, Wisconsin
Elina Litinskaya, Wisconsin
John M. Murphy, MD, Wisconsin
Tanya Pedretti, PA, Wisconsin
Adine Rodemeyer, MD, Wisconsin
Oghomwen Sule, MBBS, Wisconsin
Terrence Witt, MD, Wisconsin
Mayank Arora, Wisconsin
John D. MacDonald, MD, Wisconsin
Abigail Cook, Wisconsin
Mohamed Ibrahim, MD, Wisconsin
Aymen Khogali, MD, Wisconsin
Nicholas Haun, Wisconsin
Sandra Brown, Victoria, Australia
Alessandra Gessner, Alberta, Canada
Courtney Carlucci, British Columbia, Canada
Muhanad Y. Al Habash, Canada
Karen Tong, MD, Canada
Taku Yabuki, Japan
Liza van Loon, the Netherlands
Edward Gebuis, MD, the Netherlands
Abdisalan Afrah, MD, Qatar
Akhnuwkh Jones, Qatar
Mashuk Uddin, MBBS, MRCP, FRCP, Qatar
Ibrahim Yusuf Abubeker, MRCP, Qatar
Chih-Wei Tseng, Taiwan
Sawsan Abdel-Razig, MD, FACP, United Arab Emirates
Noninvasive therapy cut COPD readmissions
WASHINGTON – The addition of noninvasive ventilation to home oxygen therapy regimens correlated with increased time to readmission or death among patients with exacerbated chronic obstructive pulmonary diseases (COPD), according to a study presented at an international conference of the American Thoracic Society.
Among 116 patients observed with COPD, the 57 patients given home oxygen and noninvasive ventilation reported an average time to readmission of 4.3 months, compared with 1.4 months among the 59 patients given only home oxygen, according to Patrick B. Murphy, PhD, of St. Thomas’ Hospital, London (JAMA. 2017 May 21. doi: 10.1001/jama.2017.4451), who presented this research on the same day it was published in JAMA.
Dr. Murphy said the findings are encouraging for patients with COPD suffering from exacerbations from the disease.
“Patients with established chronic respiratory failure secondary to COPD have poor outcomes with limited treatment options available,” the investigators noted. “The results of the current trial are reassuring, suggesting that home noninvasive ventilation added to home oxygen therapy in this population improved the overall clinical outcome without adding to the health burden of the patient.”
In this 12-month, phase III, multicenter, randomized clinical trial, the average age of the patients was 67 years, and the average body mass index was 21.6 mg/k2. The patients had an average partial pressure of carbon dioxide (PaCo2) level of 59, indicating persistent hypercapnia.
The investigators gave those in the intervention group one of three noninvasive home ventilators – nasal, oronasal, or total face mask – to use for a minimum of 6 hours nightly. Patients in both groups received 15 hours of oxygen therapy daily.
Doctors gathered data from patients after 6 weeks, 3 months, 6 months, and 12 months.
After 12 months, risk of readmission or death in the intervention group was 63.4%, while those in the oxygen-only group reported a risk of 80.4%. Despite a 17% risk reduction, a similar number of patients died during the experiment in both groups: five in the noninvasive intervention group and four in the control group, according to the investigators.
At the end of the trial, 16 patients (28%) in the intervention group and 19 (32%) in the control group died.
Dr. Murphy and his peers asserted that these deaths do not take away from the success of the treatment, as the focus of the study was to find a way to reduce readmissions, not necessarily mortality.
“The driver of the clinical improvement in the home oxygen therapy plus home noninvasive ventilation group was readmission avoidance with no significant difference in mortality,” they wrote. “This study has major clinical relevance because readmission avoidance is beneficial to the patient in terms of preservation of lung function and health-related quality of life, as well as providing a direct and indirect cost saving.”
The study was limited by the lack of a double-blind design; however, investigators said that a sham device may have made patients’ respiratory failure worse.
Some patients in the control group were later given ventilation treatment for safety reasons. Eighteen patients were given noninvasive ventilation, although reportedly after the primary endpoint was reached.
Philips Respironics, ResMed, the ResMed Foundation, and the Guy’s and St. Thomas’ Charity funded the study. Dr. Murphy and his coinvestigators reported receiving some manner of financial support from ResMed, Philips Respironics, and B&D Electromedical.
[email protected]
On Twitter @eaztweets
Vera A. De Palo, MD, FCCP, MBA, comments: A goal for any patient with a chronic disease is the best possible quality of life. Increasing hospital-free and exacerbation-free days helps to improve that quality of life. The authors report that the addition of noninvasive ventilation therapy increased the time to readmission due to COPD exacerbation. This adds another tool to the armamentarium to help improve outcomes for our COPD patients.
Vera A. De Palo, MD, FCCP, MBA, comments: A goal for any patient with a chronic disease is the best possible quality of life. Increasing hospital-free and exacerbation-free days helps to improve that quality of life. The authors report that the addition of noninvasive ventilation therapy increased the time to readmission due to COPD exacerbation. This adds another tool to the armamentarium to help improve outcomes for our COPD patients.
Vera A. De Palo, MD, FCCP, MBA, comments: A goal for any patient with a chronic disease is the best possible quality of life. Increasing hospital-free and exacerbation-free days helps to improve that quality of life. The authors report that the addition of noninvasive ventilation therapy increased the time to readmission due to COPD exacerbation. This adds another tool to the armamentarium to help improve outcomes for our COPD patients.
WASHINGTON – The addition of noninvasive ventilation to home oxygen therapy regimens correlated with increased time to readmission or death among patients with exacerbated chronic obstructive pulmonary diseases (COPD), according to a study presented at an international conference of the American Thoracic Society.
Among 116 patients observed with COPD, the 57 patients given home oxygen and noninvasive ventilation reported an average time to readmission of 4.3 months, compared with 1.4 months among the 59 patients given only home oxygen, according to Patrick B. Murphy, PhD, of St. Thomas’ Hospital, London (JAMA. 2017 May 21. doi: 10.1001/jama.2017.4451), who presented this research on the same day it was published in JAMA.
Dr. Murphy said the findings are encouraging for patients with COPD suffering from exacerbations from the disease.
“Patients with established chronic respiratory failure secondary to COPD have poor outcomes with limited treatment options available,” the investigators noted. “The results of the current trial are reassuring, suggesting that home noninvasive ventilation added to home oxygen therapy in this population improved the overall clinical outcome without adding to the health burden of the patient.”
In this 12-month, phase III, multicenter, randomized clinical trial, the average age of the patients was 67 years, and the average body mass index was 21.6 mg/k2. The patients had an average partial pressure of carbon dioxide (PaCo2) level of 59, indicating persistent hypercapnia.
The investigators gave those in the intervention group one of three noninvasive home ventilators – nasal, oronasal, or total face mask – to use for a minimum of 6 hours nightly. Patients in both groups received 15 hours of oxygen therapy daily.
Doctors gathered data from patients after 6 weeks, 3 months, 6 months, and 12 months.
After 12 months, risk of readmission or death in the intervention group was 63.4%, while those in the oxygen-only group reported a risk of 80.4%. Despite a 17% risk reduction, a similar number of patients died during the experiment in both groups: five in the noninvasive intervention group and four in the control group, according to the investigators.
At the end of the trial, 16 patients (28%) in the intervention group and 19 (32%) in the control group died.
Dr. Murphy and his peers asserted that these deaths do not take away from the success of the treatment, as the focus of the study was to find a way to reduce readmissions, not necessarily mortality.
“The driver of the clinical improvement in the home oxygen therapy plus home noninvasive ventilation group was readmission avoidance with no significant difference in mortality,” they wrote. “This study has major clinical relevance because readmission avoidance is beneficial to the patient in terms of preservation of lung function and health-related quality of life, as well as providing a direct and indirect cost saving.”
The study was limited by the lack of a double-blind design; however, investigators said that a sham device may have made patients’ respiratory failure worse.
Some patients in the control group were later given ventilation treatment for safety reasons. Eighteen patients were given noninvasive ventilation, although reportedly after the primary endpoint was reached.
Philips Respironics, ResMed, the ResMed Foundation, and the Guy’s and St. Thomas’ Charity funded the study. Dr. Murphy and his coinvestigators reported receiving some manner of financial support from ResMed, Philips Respironics, and B&D Electromedical.
[email protected]
On Twitter @eaztweets
WASHINGTON – The addition of noninvasive ventilation to home oxygen therapy regimens correlated with increased time to readmission or death among patients with exacerbated chronic obstructive pulmonary diseases (COPD), according to a study presented at an international conference of the American Thoracic Society.
Among 116 patients observed with COPD, the 57 patients given home oxygen and noninvasive ventilation reported an average time to readmission of 4.3 months, compared with 1.4 months among the 59 patients given only home oxygen, according to Patrick B. Murphy, PhD, of St. Thomas’ Hospital, London (JAMA. 2017 May 21. doi: 10.1001/jama.2017.4451), who presented this research on the same day it was published in JAMA.
Dr. Murphy said the findings are encouraging for patients with COPD suffering from exacerbations from the disease.
“Patients with established chronic respiratory failure secondary to COPD have poor outcomes with limited treatment options available,” the investigators noted. “The results of the current trial are reassuring, suggesting that home noninvasive ventilation added to home oxygen therapy in this population improved the overall clinical outcome without adding to the health burden of the patient.”
In this 12-month, phase III, multicenter, randomized clinical trial, the average age of the patients was 67 years, and the average body mass index was 21.6 mg/k2. The patients had an average partial pressure of carbon dioxide (PaCo2) level of 59, indicating persistent hypercapnia.
The investigators gave those in the intervention group one of three noninvasive home ventilators – nasal, oronasal, or total face mask – to use for a minimum of 6 hours nightly. Patients in both groups received 15 hours of oxygen therapy daily.
Doctors gathered data from patients after 6 weeks, 3 months, 6 months, and 12 months.
After 12 months, risk of readmission or death in the intervention group was 63.4%, while those in the oxygen-only group reported a risk of 80.4%. Despite a 17% risk reduction, a similar number of patients died during the experiment in both groups: five in the noninvasive intervention group and four in the control group, according to the investigators.
At the end of the trial, 16 patients (28%) in the intervention group and 19 (32%) in the control group died.
Dr. Murphy and his peers asserted that these deaths do not take away from the success of the treatment, as the focus of the study was to find a way to reduce readmissions, not necessarily mortality.
“The driver of the clinical improvement in the home oxygen therapy plus home noninvasive ventilation group was readmission avoidance with no significant difference in mortality,” they wrote. “This study has major clinical relevance because readmission avoidance is beneficial to the patient in terms of preservation of lung function and health-related quality of life, as well as providing a direct and indirect cost saving.”
The study was limited by the lack of a double-blind design; however, investigators said that a sham device may have made patients’ respiratory failure worse.
Some patients in the control group were later given ventilation treatment for safety reasons. Eighteen patients were given noninvasive ventilation, although reportedly after the primary endpoint was reached.
Philips Respironics, ResMed, the ResMed Foundation, and the Guy’s and St. Thomas’ Charity funded the study. Dr. Murphy and his coinvestigators reported receiving some manner of financial support from ResMed, Philips Respironics, and B&D Electromedical.
[email protected]
On Twitter @eaztweets
FROM ATS 2017
Key clinical point:
Major finding: The average time until readmission or death was 4.3 months for patients using both oxygen therapy and ventilation, compared with an average of 1.4 months for patients using only oxygen therapy.
Data source: Phase III, multicenter, randomized clinical trial of 116 COPD patients gathered from 13 U.K. medical centers between February, 2010, and April, 2015.
Disclosures: Philips Respironics, ResMed, the ResMed Foundation, and the Guy’s and St. Thomas’ Charity funded the study. Dr. Patrick B. Murphy and his coinvestigators reported receiving some manner of financial support from ResMed, Philips Respironics, and B&D Electromedical.
Committee and chapter involvement allows SHM member to give back
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Paul Grant, MD, SFHM, assistant professor of medicine at the University of Michigan Medical School, Ann Arbor. Dr. Grant is the chair of SHM’s Membership Committee and an active member of SHM’s Michigan Chapter.
Why did you choose a career in hospital medicine, and how did you become an SHM member?
After residency, I completed a hospital medicine fellowship at the Cleveland Clinic. During my fellowship, I joined SHM. At that time, I knew nothing about the society, but that soon changed. My fellowship required me to attend the annual meeting and submit an abstract in the RIV competition, which was an extremely valuable experience for me. Not only was I blown away by the meeting, but my poster won the clinical vignette competition, as well! Needless to say, I’ve been an SHM member ever since.
What prompted you to join the Membership Committee? Can you discuss some of the projects the committee is currently working on?
Because SHM has done so much for my career as a hospitalist, I’ve tried to give back by volunteering on committees. After spending several years on the Early Career Hospitalist Committee, I felt the transition to the Membership Committee was a natural fit. Because SHM membership had been growing every year, our committee felt some pressure to keep this trend going. Thankfully, we have continued to see growth each year in every membership category.
Our committee has been working on several projects. One of the key demographics we have been targeting is the resident member. Residents play a significant role in the future of hospital medicine, as well as SHM membership. We are developing ways to reach out to residency program directors – particularly those running a hospital medicine track – to find ways they can benefit from SHM’s educational offerings. Additionally, our committee has been discussing ways to attract international members to SHM. Because hospital medicine is quite developed in the United States, we believe we have much to offer to hospitalists around the world.
Tell TH about your involvement with SHM’s Michigan Chapter. What does a typical chapter meeting entail?
A few years ago, at the end of SHM’s annual meeting, several of my hospital medicine colleagues in southeast Michigan happened to be on the same flight home. At the departure gate in the airport, we all agreed we should start an SHM chapter. After drawing straws, it was decided that I would be chapter president for our inaugural year. In a few short years, our chapter has grown into one of the largest in the country.
As for a typical meeting, each starts with a cocktail hour to encourage our members to network. We have a guest speaker, who presents on a hospital medicine topic, and then, we end the evening with a business meeting. We encourage students and residents to attend. More recently, we’ve been using interactive technology to broadcast our meetings to large hospital medicine groups in the western and northern parts of the state. Our chapter was thrilled to learn that we’d won the Outstanding Chapter award this year!
What value do you find in connecting with hospital medicine professionals at the local level?
Whether it’s a hospitalist working at a large, tertiary care center or one working in a small rural setting, it seems we all face similar challenges.
As a chapter, we can pull together our resources to address these issues. Furthermore, we have the ability to reach out to more trainees and show them what hospital medicine is all about. Our chapter has been able to partially fund both medical students and residents so they could attend SHM’s annual meeting. I’m always amazed at what I can learn from other hospitalists – in the state of Michigan and beyond.
Find a chapter near you and get involved at the local level at hospitalmedicine.org/chapters .
Felicia Steele is SHM’s communications coordinator.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Paul Grant, MD, SFHM, assistant professor of medicine at the University of Michigan Medical School, Ann Arbor. Dr. Grant is the chair of SHM’s Membership Committee and an active member of SHM’s Michigan Chapter.
Why did you choose a career in hospital medicine, and how did you become an SHM member?
After residency, I completed a hospital medicine fellowship at the Cleveland Clinic. During my fellowship, I joined SHM. At that time, I knew nothing about the society, but that soon changed. My fellowship required me to attend the annual meeting and submit an abstract in the RIV competition, which was an extremely valuable experience for me. Not only was I blown away by the meeting, but my poster won the clinical vignette competition, as well! Needless to say, I’ve been an SHM member ever since.
What prompted you to join the Membership Committee? Can you discuss some of the projects the committee is currently working on?
Because SHM has done so much for my career as a hospitalist, I’ve tried to give back by volunteering on committees. After spending several years on the Early Career Hospitalist Committee, I felt the transition to the Membership Committee was a natural fit. Because SHM membership had been growing every year, our committee felt some pressure to keep this trend going. Thankfully, we have continued to see growth each year in every membership category.
Our committee has been working on several projects. One of the key demographics we have been targeting is the resident member. Residents play a significant role in the future of hospital medicine, as well as SHM membership. We are developing ways to reach out to residency program directors – particularly those running a hospital medicine track – to find ways they can benefit from SHM’s educational offerings. Additionally, our committee has been discussing ways to attract international members to SHM. Because hospital medicine is quite developed in the United States, we believe we have much to offer to hospitalists around the world.
Tell TH about your involvement with SHM’s Michigan Chapter. What does a typical chapter meeting entail?
A few years ago, at the end of SHM’s annual meeting, several of my hospital medicine colleagues in southeast Michigan happened to be on the same flight home. At the departure gate in the airport, we all agreed we should start an SHM chapter. After drawing straws, it was decided that I would be chapter president for our inaugural year. In a few short years, our chapter has grown into one of the largest in the country.
As for a typical meeting, each starts with a cocktail hour to encourage our members to network. We have a guest speaker, who presents on a hospital medicine topic, and then, we end the evening with a business meeting. We encourage students and residents to attend. More recently, we’ve been using interactive technology to broadcast our meetings to large hospital medicine groups in the western and northern parts of the state. Our chapter was thrilled to learn that we’d won the Outstanding Chapter award this year!
What value do you find in connecting with hospital medicine professionals at the local level?
Whether it’s a hospitalist working at a large, tertiary care center or one working in a small rural setting, it seems we all face similar challenges.
As a chapter, we can pull together our resources to address these issues. Furthermore, we have the ability to reach out to more trainees and show them what hospital medicine is all about. Our chapter has been able to partially fund both medical students and residents so they could attend SHM’s annual meeting. I’m always amazed at what I can learn from other hospitalists – in the state of Michigan and beyond.
Find a chapter near you and get involved at the local level at hospitalmedicine.org/chapters .
Felicia Steele is SHM’s communications coordinator.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Paul Grant, MD, SFHM, assistant professor of medicine at the University of Michigan Medical School, Ann Arbor. Dr. Grant is the chair of SHM’s Membership Committee and an active member of SHM’s Michigan Chapter.
Why did you choose a career in hospital medicine, and how did you become an SHM member?
After residency, I completed a hospital medicine fellowship at the Cleveland Clinic. During my fellowship, I joined SHM. At that time, I knew nothing about the society, but that soon changed. My fellowship required me to attend the annual meeting and submit an abstract in the RIV competition, which was an extremely valuable experience for me. Not only was I blown away by the meeting, but my poster won the clinical vignette competition, as well! Needless to say, I’ve been an SHM member ever since.
What prompted you to join the Membership Committee? Can you discuss some of the projects the committee is currently working on?
Because SHM has done so much for my career as a hospitalist, I’ve tried to give back by volunteering on committees. After spending several years on the Early Career Hospitalist Committee, I felt the transition to the Membership Committee was a natural fit. Because SHM membership had been growing every year, our committee felt some pressure to keep this trend going. Thankfully, we have continued to see growth each year in every membership category.
Our committee has been working on several projects. One of the key demographics we have been targeting is the resident member. Residents play a significant role in the future of hospital medicine, as well as SHM membership. We are developing ways to reach out to residency program directors – particularly those running a hospital medicine track – to find ways they can benefit from SHM’s educational offerings. Additionally, our committee has been discussing ways to attract international members to SHM. Because hospital medicine is quite developed in the United States, we believe we have much to offer to hospitalists around the world.
Tell TH about your involvement with SHM’s Michigan Chapter. What does a typical chapter meeting entail?
A few years ago, at the end of SHM’s annual meeting, several of my hospital medicine colleagues in southeast Michigan happened to be on the same flight home. At the departure gate in the airport, we all agreed we should start an SHM chapter. After drawing straws, it was decided that I would be chapter president for our inaugural year. In a few short years, our chapter has grown into one of the largest in the country.
As for a typical meeting, each starts with a cocktail hour to encourage our members to network. We have a guest speaker, who presents on a hospital medicine topic, and then, we end the evening with a business meeting. We encourage students and residents to attend. More recently, we’ve been using interactive technology to broadcast our meetings to large hospital medicine groups in the western and northern parts of the state. Our chapter was thrilled to learn that we’d won the Outstanding Chapter award this year!
What value do you find in connecting with hospital medicine professionals at the local level?
Whether it’s a hospitalist working at a large, tertiary care center or one working in a small rural setting, it seems we all face similar challenges.
As a chapter, we can pull together our resources to address these issues. Furthermore, we have the ability to reach out to more trainees and show them what hospital medicine is all about. Our chapter has been able to partially fund both medical students and residents so they could attend SHM’s annual meeting. I’m always amazed at what I can learn from other hospitalists – in the state of Michigan and beyond.
Find a chapter near you and get involved at the local level at hospitalmedicine.org/chapters .
Felicia Steele is SHM’s communications coordinator.















