User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


When one patient decompensates, others on the ward may follow
CLINICAL QUESTION: How does the clinical decompensation of a ward patient affect the likelihood of another patient’s decompensation?
STUDY DESIGN: Observational cohort study.
SETTING: Thirteen geographically distinct, adult medical-surgical wards at an academic medical center.
SYNOPSIS: Of 83,723 admissions to medical-surgical wards, 4,286 patients experienced cardiac arrest (179) or were transferred to the ICU (4,107). When one or more of these events occurred, other patients on the same ward had an increased risk for either event over the subsequent 6 (OR 1.18; CI, 1.07-1.31) and 12 hours and the risk was higher if more than one event occurred. Importantly, for patients exposed to other patients on the same ward decompensating, there were no differences in the severity of illness for patients transferred to ICU or in overall mortality.
Intuitively, when one patient becomes critically ill, other patients receive less attention. Though the effect was small, this study highlights that diversion of resources may increase other patients to greater risk. Surprisingly, the increased risk was not significant during night-time hours, when resources are more limited, but data collection may have been also affected.
BOTTOM LINE: When a patient becomes critically ill, another patient on the same ward is more likely to decompensate within the next 6-12 hours, but the effect is small.
CITATIONS: Volchenboum SL, Mayampurath A, Göksu-Gürsoy G, et al. Association between in-hospital critical illness events and outcomes in patients on the same ward. JAMA. 2016;316(24):2674-5.
Dr. Anstett is Hospital Medicine Fellow in Quality and Systems Leadership, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: How does the clinical decompensation of a ward patient affect the likelihood of another patient’s decompensation?
STUDY DESIGN: Observational cohort study.
SETTING: Thirteen geographically distinct, adult medical-surgical wards at an academic medical center.
SYNOPSIS: Of 83,723 admissions to medical-surgical wards, 4,286 patients experienced cardiac arrest (179) or were transferred to the ICU (4,107). When one or more of these events occurred, other patients on the same ward had an increased risk for either event over the subsequent 6 (OR 1.18; CI, 1.07-1.31) and 12 hours and the risk was higher if more than one event occurred. Importantly, for patients exposed to other patients on the same ward decompensating, there were no differences in the severity of illness for patients transferred to ICU or in overall mortality.
Intuitively, when one patient becomes critically ill, other patients receive less attention. Though the effect was small, this study highlights that diversion of resources may increase other patients to greater risk. Surprisingly, the increased risk was not significant during night-time hours, when resources are more limited, but data collection may have been also affected.
BOTTOM LINE: When a patient becomes critically ill, another patient on the same ward is more likely to decompensate within the next 6-12 hours, but the effect is small.
CITATIONS: Volchenboum SL, Mayampurath A, Göksu-Gürsoy G, et al. Association between in-hospital critical illness events and outcomes in patients on the same ward. JAMA. 2016;316(24):2674-5.
Dr. Anstett is Hospital Medicine Fellow in Quality and Systems Leadership, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: How does the clinical decompensation of a ward patient affect the likelihood of another patient’s decompensation?
STUDY DESIGN: Observational cohort study.
SETTING: Thirteen geographically distinct, adult medical-surgical wards at an academic medical center.
SYNOPSIS: Of 83,723 admissions to medical-surgical wards, 4,286 patients experienced cardiac arrest (179) or were transferred to the ICU (4,107). When one or more of these events occurred, other patients on the same ward had an increased risk for either event over the subsequent 6 (OR 1.18; CI, 1.07-1.31) and 12 hours and the risk was higher if more than one event occurred. Importantly, for patients exposed to other patients on the same ward decompensating, there were no differences in the severity of illness for patients transferred to ICU or in overall mortality.
Intuitively, when one patient becomes critically ill, other patients receive less attention. Though the effect was small, this study highlights that diversion of resources may increase other patients to greater risk. Surprisingly, the increased risk was not significant during night-time hours, when resources are more limited, but data collection may have been also affected.
BOTTOM LINE: When a patient becomes critically ill, another patient on the same ward is more likely to decompensate within the next 6-12 hours, but the effect is small.
CITATIONS: Volchenboum SL, Mayampurath A, Göksu-Gürsoy G, et al. Association between in-hospital critical illness events and outcomes in patients on the same ward. JAMA. 2016;316(24):2674-5.
Dr. Anstett is Hospital Medicine Fellow in Quality and Systems Leadership, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
Principles learned from a successful improvement program can increase compliance and reduce hospital acquired VTEs (HA-VTEs) across multiple institutions
CLINICAL QUESTION: Can a single institution’s VTE prophylaxis program be scaled to increase prophylaxis and reduce HA-VTEs across multiple institutions?
STUDY DESIGN: prospective, unblinded, open-intervention study
SETTING: Inpatient medical and surgical services at five independent, cooperating academic hospitals
SYNOPSIS: Each site used common principles to develop their own multi-pronged VTE prophylaxis program including structured order-sets, simplified risk-assessment, feedback to providers, and education programs.
306,906 inpatient discharges were evaluated with average VTE prophylaxis bundle compliance reaching 89% across all institutions. HA-VTE rates declined from 0.90% to 0.69% (RR, 0.76; CI, 0.68-0.85) – equivalent to averting 81 pulmonary emboli and 89 deep venous thrombi. Of note, HA-VTE rates only declined at three of the five institutions with the greatest improvement at those with the highest baseline rates. Further, while HA-VTE rates improved across all patient populations, the incidence reduction was statistically significant in Oncologic and Surgical populations.
BOTTOM LINE: Hospital systems can reduce HA-VTE and increase VTE prophylaxis by implementing a bundle of interventions and these efforts are highest yield for Oncologic and Surgical populations.
CITATIONS: Jenkins IH, White RH, Amin AN, et al. Reducing the incidence of hospital-associated venous thromboembolism within a network of academic hospitals: findings from five University of California medical centers. J Hosp Med. 2016;11:S22-8.
Dr. Anstett is Hospital Medicine Fellow in Quality and Systems Leadership, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Can a single institution’s VTE prophylaxis program be scaled to increase prophylaxis and reduce HA-VTEs across multiple institutions?
STUDY DESIGN: prospective, unblinded, open-intervention study
SETTING: Inpatient medical and surgical services at five independent, cooperating academic hospitals
SYNOPSIS: Each site used common principles to develop their own multi-pronged VTE prophylaxis program including structured order-sets, simplified risk-assessment, feedback to providers, and education programs.
306,906 inpatient discharges were evaluated with average VTE prophylaxis bundle compliance reaching 89% across all institutions. HA-VTE rates declined from 0.90% to 0.69% (RR, 0.76; CI, 0.68-0.85) – equivalent to averting 81 pulmonary emboli and 89 deep venous thrombi. Of note, HA-VTE rates only declined at three of the five institutions with the greatest improvement at those with the highest baseline rates. Further, while HA-VTE rates improved across all patient populations, the incidence reduction was statistically significant in Oncologic and Surgical populations.
BOTTOM LINE: Hospital systems can reduce HA-VTE and increase VTE prophylaxis by implementing a bundle of interventions and these efforts are highest yield for Oncologic and Surgical populations.
CITATIONS: Jenkins IH, White RH, Amin AN, et al. Reducing the incidence of hospital-associated venous thromboembolism within a network of academic hospitals: findings from five University of California medical centers. J Hosp Med. 2016;11:S22-8.
Dr. Anstett is Hospital Medicine Fellow in Quality and Systems Leadership, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Can a single institution’s VTE prophylaxis program be scaled to increase prophylaxis and reduce HA-VTEs across multiple institutions?
STUDY DESIGN: prospective, unblinded, open-intervention study
SETTING: Inpatient medical and surgical services at five independent, cooperating academic hospitals
SYNOPSIS: Each site used common principles to develop their own multi-pronged VTE prophylaxis program including structured order-sets, simplified risk-assessment, feedback to providers, and education programs.
306,906 inpatient discharges were evaluated with average VTE prophylaxis bundle compliance reaching 89% across all institutions. HA-VTE rates declined from 0.90% to 0.69% (RR, 0.76; CI, 0.68-0.85) – equivalent to averting 81 pulmonary emboli and 89 deep venous thrombi. Of note, HA-VTE rates only declined at three of the five institutions with the greatest improvement at those with the highest baseline rates. Further, while HA-VTE rates improved across all patient populations, the incidence reduction was statistically significant in Oncologic and Surgical populations.
BOTTOM LINE: Hospital systems can reduce HA-VTE and increase VTE prophylaxis by implementing a bundle of interventions and these efforts are highest yield for Oncologic and Surgical populations.
CITATIONS: Jenkins IH, White RH, Amin AN, et al. Reducing the incidence of hospital-associated venous thromboembolism within a network of academic hospitals: findings from five University of California medical centers. J Hosp Med. 2016;11:S22-8.
Dr. Anstett is Hospital Medicine Fellow in Quality and Systems Leadership, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
On 15 years: Celebrating a nocturnist’s career longevity
“Nocturnist years are like dog years. So really we’re celebrating you for 105 years of service!”
Shawn Lee, MD, a day shift hospitalist at Overlake Medical Center in Bellevue, Wash. (where I work), said this about our colleague, Arash Nadershahi, MD, on the occasion of his 15th anniversary as a nocturnist with our group. Every hospitalist group should be so lucky to have someone like Arash among them, whether working nights or days.
When Arash joined our group the job simply entailed turning on the pager at 9 p.m. and coming in to the hospital only when the need arose. Some nights meant only answering some “cross-cover” calls from home, while other nights started with one or more patients needing admission right at the start of the shift.
As the months went by, patient volume climbed rapidly and Arash, as well as the nocturnists who joined us subsequently, began arriving at the hospital no later than the 9:00 p.m. shift start and staying in-house until 7 a.m. We never had a meeting or contentious conversation to make it official that the night shift changed to in-house all night instead of call-from-home. It just evolved that way to meet the need.
We all value Arash’s steady demeanor, excellent clinical skills, and good relationships with ED staff and nurses as well as patients. And for many years he and our other two nocturnists have covered all night shifts, including filling in when one of them is unexpectedly out for the birth of a child, illness, or other reason. The day doctors have never been called upon to work night shifts to cover an unexpected nocturnist absence.
Configuring the nocturnist position
A full-time nocturnist in our group works ten 10-hour night shifts and two 6-hour evening shifts (5-11 p.m.) per month. I like to think this has contributed to longevity for our nocturnists. One left last year after working nights for 10 years, and another just started his 9th year in the group.
The three nocturnists can work any schedule they like as long as one of them is on duty each night. For more than 10 years they’ve worked 7 consecutive night shifts followed by 14 off (that is sometimes interrupted by an evening shift). To my way of thinking, though, they’re essentially devoting 9 days to the practice for every seven consecutive shifts. The days before they start their rotation and after they complete it are spent preparing/recovering by adjusting their sleep, so aren’t really days of R&R.
For this work their compensation is very similar to that of full-time day shift doctors. The idea is that their compensation premium for working nights comes in the form of less work rather than more money; they work fewer and shorter shifts than their daytime counterparts. And we discourage moonlighting during all those days off. We want to provide the conditions for a healthy lifestyle to offset night work.
The longest-tenured nocturnist?
At 15 years of full-time work as a nocturnist, Arash may be one of the longest-tenured doctors in this role nationally. (I would love to hear about others who’ve been at it longer.) I like to think that our “pay ’em the same and work ’em less” approach may be a meaningful contributor to his longevity in the role, but I’m convinced his personal attributes are also a big factor.
His interests and creativity find their way into our workplace. For a while the day shift doctors would arrive to find our office full of motorcycle parts in various stages of assembly. Many of his doodles and drawings and witty writings are taped to the walls and cabinets. A few years ago he started writing haikus and before long everyone in the group joined in. This even led to one of our docs hosting a really fun party at which every guest wrote haikus and all had to guess the author of each one.
Other groups can’t count on finding someone as valuable as Arash, but they’ll have the best chance of it if they think carefully about how the nocturnist role is configured.
Dr. Nelson has had a career in clinical practice as a hospitalist starting in 1988. He is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses.
“Nocturnist years are like dog years. So really we’re celebrating you for 105 years of service!”
Shawn Lee, MD, a day shift hospitalist at Overlake Medical Center in Bellevue, Wash. (where I work), said this about our colleague, Arash Nadershahi, MD, on the occasion of his 15th anniversary as a nocturnist with our group. Every hospitalist group should be so lucky to have someone like Arash among them, whether working nights or days.
When Arash joined our group the job simply entailed turning on the pager at 9 p.m. and coming in to the hospital only when the need arose. Some nights meant only answering some “cross-cover” calls from home, while other nights started with one or more patients needing admission right at the start of the shift.
As the months went by, patient volume climbed rapidly and Arash, as well as the nocturnists who joined us subsequently, began arriving at the hospital no later than the 9:00 p.m. shift start and staying in-house until 7 a.m. We never had a meeting or contentious conversation to make it official that the night shift changed to in-house all night instead of call-from-home. It just evolved that way to meet the need.
We all value Arash’s steady demeanor, excellent clinical skills, and good relationships with ED staff and nurses as well as patients. And for many years he and our other two nocturnists have covered all night shifts, including filling in when one of them is unexpectedly out for the birth of a child, illness, or other reason. The day doctors have never been called upon to work night shifts to cover an unexpected nocturnist absence.
Configuring the nocturnist position
A full-time nocturnist in our group works ten 10-hour night shifts and two 6-hour evening shifts (5-11 p.m.) per month. I like to think this has contributed to longevity for our nocturnists. One left last year after working nights for 10 years, and another just started his 9th year in the group.
The three nocturnists can work any schedule they like as long as one of them is on duty each night. For more than 10 years they’ve worked 7 consecutive night shifts followed by 14 off (that is sometimes interrupted by an evening shift). To my way of thinking, though, they’re essentially devoting 9 days to the practice for every seven consecutive shifts. The days before they start their rotation and after they complete it are spent preparing/recovering by adjusting their sleep, so aren’t really days of R&R.
For this work their compensation is very similar to that of full-time day shift doctors. The idea is that their compensation premium for working nights comes in the form of less work rather than more money; they work fewer and shorter shifts than their daytime counterparts. And we discourage moonlighting during all those days off. We want to provide the conditions for a healthy lifestyle to offset night work.
The longest-tenured nocturnist?
At 15 years of full-time work as a nocturnist, Arash may be one of the longest-tenured doctors in this role nationally. (I would love to hear about others who’ve been at it longer.) I like to think that our “pay ’em the same and work ’em less” approach may be a meaningful contributor to his longevity in the role, but I’m convinced his personal attributes are also a big factor.
His interests and creativity find their way into our workplace. For a while the day shift doctors would arrive to find our office full of motorcycle parts in various stages of assembly. Many of his doodles and drawings and witty writings are taped to the walls and cabinets. A few years ago he started writing haikus and before long everyone in the group joined in. This even led to one of our docs hosting a really fun party at which every guest wrote haikus and all had to guess the author of each one.
Other groups can’t count on finding someone as valuable as Arash, but they’ll have the best chance of it if they think carefully about how the nocturnist role is configured.
Dr. Nelson has had a career in clinical practice as a hospitalist starting in 1988. He is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses.
“Nocturnist years are like dog years. So really we’re celebrating you for 105 years of service!”
Shawn Lee, MD, a day shift hospitalist at Overlake Medical Center in Bellevue, Wash. (where I work), said this about our colleague, Arash Nadershahi, MD, on the occasion of his 15th anniversary as a nocturnist with our group. Every hospitalist group should be so lucky to have someone like Arash among them, whether working nights or days.
When Arash joined our group the job simply entailed turning on the pager at 9 p.m. and coming in to the hospital only when the need arose. Some nights meant only answering some “cross-cover” calls from home, while other nights started with one or more patients needing admission right at the start of the shift.
As the months went by, patient volume climbed rapidly and Arash, as well as the nocturnists who joined us subsequently, began arriving at the hospital no later than the 9:00 p.m. shift start and staying in-house until 7 a.m. We never had a meeting or contentious conversation to make it official that the night shift changed to in-house all night instead of call-from-home. It just evolved that way to meet the need.
We all value Arash’s steady demeanor, excellent clinical skills, and good relationships with ED staff and nurses as well as patients. And for many years he and our other two nocturnists have covered all night shifts, including filling in when one of them is unexpectedly out for the birth of a child, illness, or other reason. The day doctors have never been called upon to work night shifts to cover an unexpected nocturnist absence.
Configuring the nocturnist position
A full-time nocturnist in our group works ten 10-hour night shifts and two 6-hour evening shifts (5-11 p.m.) per month. I like to think this has contributed to longevity for our nocturnists. One left last year after working nights for 10 years, and another just started his 9th year in the group.
The three nocturnists can work any schedule they like as long as one of them is on duty each night. For more than 10 years they’ve worked 7 consecutive night shifts followed by 14 off (that is sometimes interrupted by an evening shift). To my way of thinking, though, they’re essentially devoting 9 days to the practice for every seven consecutive shifts. The days before they start their rotation and after they complete it are spent preparing/recovering by adjusting their sleep, so aren’t really days of R&R.
For this work their compensation is very similar to that of full-time day shift doctors. The idea is that their compensation premium for working nights comes in the form of less work rather than more money; they work fewer and shorter shifts than their daytime counterparts. And we discourage moonlighting during all those days off. We want to provide the conditions for a healthy lifestyle to offset night work.
The longest-tenured nocturnist?
At 15 years of full-time work as a nocturnist, Arash may be one of the longest-tenured doctors in this role nationally. (I would love to hear about others who’ve been at it longer.) I like to think that our “pay ’em the same and work ’em less” approach may be a meaningful contributor to his longevity in the role, but I’m convinced his personal attributes are also a big factor.
His interests and creativity find their way into our workplace. For a while the day shift doctors would arrive to find our office full of motorcycle parts in various stages of assembly. Many of his doodles and drawings and witty writings are taped to the walls and cabinets. A few years ago he started writing haikus and before long everyone in the group joined in. This even led to one of our docs hosting a really fun party at which every guest wrote haikus and all had to guess the author of each one.
Other groups can’t count on finding someone as valuable as Arash, but they’ll have the best chance of it if they think carefully about how the nocturnist role is configured.
Dr. Nelson has had a career in clinical practice as a hospitalist starting in 1988. He is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses.
Alpha blockers may facilitate the expulsion of larger ureteric stones
CLINICAL QUESTION: Are alpha blockers efficacious in patients with ureteric stones?
STUDY DESIGN: Systematic review & meta-analysis.
SETTING: Randomized controlled trials (RCTs); most conducted in Europe and Asia.
SYNOPSIS: Fifty-five unique RCTs (5,990 subjects) examining alpha blockers as the main treatment of ureteric stones versus placebo or control were included regardless of language and publication status.
Treatment with alpha blockers resulted in a 49% greater likelihood of stone passage (RR, 1.49; CI, 1.39-1.61) with a number needed to treat of four. A priori subgroup analysis revealed treatment was only beneficial in patients with larger stones (5mm or greater) independent of stone location or type of alpha blocker.
Secondary outcomes included reduced time to stone passage, fewer episodes of pain, decreased risk of surgical intervention, and lower risk of hospital admission with alpha blocker treatment without an increase in serious adverse events.
The meta-analysis was limited by the overall lack of methodological rigor of and clinical heterogeneity between the pooled studies.
BOTTOM LINE: Based on available evidence, it is reasonable to utilize an alpha blocker as medical expulsive therapy in patients with larger ureteric stones.
CITATIONS: Hollingsworth JM, Canales BK, Rogers MA, et al. Alpha blockers for treatment of ureteric stones: systematic review and meta-analysis. BMJ. 2016;355:i6112.
Dr. Ecker is the assistant director of education, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Are alpha blockers efficacious in patients with ureteric stones?
STUDY DESIGN: Systematic review & meta-analysis.
SETTING: Randomized controlled trials (RCTs); most conducted in Europe and Asia.
SYNOPSIS: Fifty-five unique RCTs (5,990 subjects) examining alpha blockers as the main treatment of ureteric stones versus placebo or control were included regardless of language and publication status.
Treatment with alpha blockers resulted in a 49% greater likelihood of stone passage (RR, 1.49; CI, 1.39-1.61) with a number needed to treat of four. A priori subgroup analysis revealed treatment was only beneficial in patients with larger stones (5mm or greater) independent of stone location or type of alpha blocker.
Secondary outcomes included reduced time to stone passage, fewer episodes of pain, decreased risk of surgical intervention, and lower risk of hospital admission with alpha blocker treatment without an increase in serious adverse events.
The meta-analysis was limited by the overall lack of methodological rigor of and clinical heterogeneity between the pooled studies.
BOTTOM LINE: Based on available evidence, it is reasonable to utilize an alpha blocker as medical expulsive therapy in patients with larger ureteric stones.
CITATIONS: Hollingsworth JM, Canales BK, Rogers MA, et al. Alpha blockers for treatment of ureteric stones: systematic review and meta-analysis. BMJ. 2016;355:i6112.
Dr. Ecker is the assistant director of education, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: Are alpha blockers efficacious in patients with ureteric stones?
STUDY DESIGN: Systematic review & meta-analysis.
SETTING: Randomized controlled trials (RCTs); most conducted in Europe and Asia.
SYNOPSIS: Fifty-five unique RCTs (5,990 subjects) examining alpha blockers as the main treatment of ureteric stones versus placebo or control were included regardless of language and publication status.
Treatment with alpha blockers resulted in a 49% greater likelihood of stone passage (RR, 1.49; CI, 1.39-1.61) with a number needed to treat of four. A priori subgroup analysis revealed treatment was only beneficial in patients with larger stones (5mm or greater) independent of stone location or type of alpha blocker.
Secondary outcomes included reduced time to stone passage, fewer episodes of pain, decreased risk of surgical intervention, and lower risk of hospital admission with alpha blocker treatment without an increase in serious adverse events.
The meta-analysis was limited by the overall lack of methodological rigor of and clinical heterogeneity between the pooled studies.
BOTTOM LINE: Based on available evidence, it is reasonable to utilize an alpha blocker as medical expulsive therapy in patients with larger ureteric stones.
CITATIONS: Hollingsworth JM, Canales BK, Rogers MA, et al. Alpha blockers for treatment of ureteric stones: systematic review and meta-analysis. BMJ. 2016;355:i6112.
Dr. Ecker is the assistant director of education, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
Interventions, especially those that are organization-directed, reduce burnout in physicians
CLINICAL QUESTION: How efficacious are interventions to reduce burnout in physicians?
BACKGROUND: Burnout is characterized by emotional exhaustion, depersonalization, and a diminished sense of personal accomplishment. It is driven by workplace stressors and affects nearly half of physicians practicing in the U.S.
SETTING: Randomized controlled trials and controlled before-after studies in primary, secondary, or intensive care settings; most conducted in North America and Europe.
SYNOPSIS: Twenty independent comparisons from 19 studies (1,550 physicians of any specialty including trainees) were included. All reported burnout outcomes after either physician- or organization-directed interventions designed to relieve stress and/or improve physician performance. Most physician-directed interventions utilized mindfulness-based stress reduction techniques or other educational interventions. Most organizational-directed interventions introduced reductions in workload or schedule changes.
Interventions were associated with small, significant reductions in burnout (standardized mean difference, –0.29; CI –0.42 to –0.16). A pre-specified subgroup analysis revealed organization-directed interventions had significantly improved effects, compared with physician-directed ones.
The generalizability of this meta-analysis is limited as the included studies significantly differed in their methodologies.
BOTTOM LINE: Burnout intervention programs for physicians are associated with small benefits, and the increased efficacy of organization-directed interventions suggest burnout is a problem of the health care system, rather than of individuals.
CITATIONS: Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med. 2017;177(2):195-205.
Dr. Ecker is the assistant director of education, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: How efficacious are interventions to reduce burnout in physicians?
BACKGROUND: Burnout is characterized by emotional exhaustion, depersonalization, and a diminished sense of personal accomplishment. It is driven by workplace stressors and affects nearly half of physicians practicing in the U.S.
SETTING: Randomized controlled trials and controlled before-after studies in primary, secondary, or intensive care settings; most conducted in North America and Europe.
SYNOPSIS: Twenty independent comparisons from 19 studies (1,550 physicians of any specialty including trainees) were included. All reported burnout outcomes after either physician- or organization-directed interventions designed to relieve stress and/or improve physician performance. Most physician-directed interventions utilized mindfulness-based stress reduction techniques or other educational interventions. Most organizational-directed interventions introduced reductions in workload or schedule changes.
Interventions were associated with small, significant reductions in burnout (standardized mean difference, –0.29; CI –0.42 to –0.16). A pre-specified subgroup analysis revealed organization-directed interventions had significantly improved effects, compared with physician-directed ones.
The generalizability of this meta-analysis is limited as the included studies significantly differed in their methodologies.
BOTTOM LINE: Burnout intervention programs for physicians are associated with small benefits, and the increased efficacy of organization-directed interventions suggest burnout is a problem of the health care system, rather than of individuals.
CITATIONS: Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med. 2017;177(2):195-205.
Dr. Ecker is the assistant director of education, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
CLINICAL QUESTION: How efficacious are interventions to reduce burnout in physicians?
BACKGROUND: Burnout is characterized by emotional exhaustion, depersonalization, and a diminished sense of personal accomplishment. It is driven by workplace stressors and affects nearly half of physicians practicing in the U.S.
SETTING: Randomized controlled trials and controlled before-after studies in primary, secondary, or intensive care settings; most conducted in North America and Europe.
SYNOPSIS: Twenty independent comparisons from 19 studies (1,550 physicians of any specialty including trainees) were included. All reported burnout outcomes after either physician- or organization-directed interventions designed to relieve stress and/or improve physician performance. Most physician-directed interventions utilized mindfulness-based stress reduction techniques or other educational interventions. Most organizational-directed interventions introduced reductions in workload or schedule changes.
Interventions were associated with small, significant reductions in burnout (standardized mean difference, –0.29; CI –0.42 to –0.16). A pre-specified subgroup analysis revealed organization-directed interventions had significantly improved effects, compared with physician-directed ones.
The generalizability of this meta-analysis is limited as the included studies significantly differed in their methodologies.
BOTTOM LINE: Burnout intervention programs for physicians are associated with small benefits, and the increased efficacy of organization-directed interventions suggest burnout is a problem of the health care system, rather than of individuals.
CITATIONS: Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med. 2017;177(2):195-205.
Dr. Ecker is the assistant director of education, Division of Hospital Medicine, University of Colorado School of Medicine, Aurora.
PPIs triple heart failure hospitalization risk in atrial fib patients
PARIS – Unwarranted prescriptions for proton pump inhibitors tripled the rate at which patients with atrial fibrillation needed hospitalization for a first episode of acute heart failure, in a retrospective study of 172 patients at a single center in Portugal.
About a third of the atrial fibrillation patients received a proton pump inhibitor (PPI) without a clear indication, and the PPI recipients developed heart failure at 2.9 times the rate as patients not on a PPI, a statistically significant difference, João B. Augusto, MD, reported at a meeting held by the Heart Failure Association of the European Society of Cardiology. Dr. Augusto believes that these patients largely had no need for PPI treatment, and the drug may have cut iron and vitamin B12 absorption by lowering gastric acid, resulting in deficiencies that produced anemia, and following that, heart failure, he suggested.
The study focused on 423 patients admitted to Fernando da Fonseca Hospital during January 2014–June 2015 with a primary or secondary diagnosis of atrial fibrillation. He excluded 101 patients with a history of heart failure, 109 patients on antiplatelet therapy, and 33 patients with a clear need for PPI treatment because of a gastrointestinal condition. Another 11 patients were lost to follow-up, leaving 172 patients followed for 1 year.
At the time of their initial hospitalization, 53 patients (31%) received a prescription for a PPI despite having no gastrointestinal diagnosis, likely a prophylactic step for patients receiving an oral anticoagulant, Dr. Augusto said. The patients averaged 69 years old, and nearly two-thirds were men.
During 1-year follow-up, the incidence of hospitalization for acute heart failure was 8% in the patients not on a PPI and 23% among those on a PPI, a statistically significant difference. In a regression analysis that controlled for age and chronic kidney disease, the incidence of acute heart failure was 2.9 times more common among patients on a PPI, Dr. Augusto said. He and his associates used these findings to educate their hospital’s staff to not needlessly prescribe a PPI to atrial fibrillation patients.
Dr. Augusto had no disclosures.
[email protected]
On Twitter @mitchelzoler
PARIS – Unwarranted prescriptions for proton pump inhibitors tripled the rate at which patients with atrial fibrillation needed hospitalization for a first episode of acute heart failure, in a retrospective study of 172 patients at a single center in Portugal.
About a third of the atrial fibrillation patients received a proton pump inhibitor (PPI) without a clear indication, and the PPI recipients developed heart failure at 2.9 times the rate as patients not on a PPI, a statistically significant difference, João B. Augusto, MD, reported at a meeting held by the Heart Failure Association of the European Society of Cardiology. Dr. Augusto believes that these patients largely had no need for PPI treatment, and the drug may have cut iron and vitamin B12 absorption by lowering gastric acid, resulting in deficiencies that produced anemia, and following that, heart failure, he suggested.
The study focused on 423 patients admitted to Fernando da Fonseca Hospital during January 2014–June 2015 with a primary or secondary diagnosis of atrial fibrillation. He excluded 101 patients with a history of heart failure, 109 patients on antiplatelet therapy, and 33 patients with a clear need for PPI treatment because of a gastrointestinal condition. Another 11 patients were lost to follow-up, leaving 172 patients followed for 1 year.
At the time of their initial hospitalization, 53 patients (31%) received a prescription for a PPI despite having no gastrointestinal diagnosis, likely a prophylactic step for patients receiving an oral anticoagulant, Dr. Augusto said. The patients averaged 69 years old, and nearly two-thirds were men.
During 1-year follow-up, the incidence of hospitalization for acute heart failure was 8% in the patients not on a PPI and 23% among those on a PPI, a statistically significant difference. In a regression analysis that controlled for age and chronic kidney disease, the incidence of acute heart failure was 2.9 times more common among patients on a PPI, Dr. Augusto said. He and his associates used these findings to educate their hospital’s staff to not needlessly prescribe a PPI to atrial fibrillation patients.
Dr. Augusto had no disclosures.
[email protected]
On Twitter @mitchelzoler
PARIS – Unwarranted prescriptions for proton pump inhibitors tripled the rate at which patients with atrial fibrillation needed hospitalization for a first episode of acute heart failure, in a retrospective study of 172 patients at a single center in Portugal.
About a third of the atrial fibrillation patients received a proton pump inhibitor (PPI) without a clear indication, and the PPI recipients developed heart failure at 2.9 times the rate as patients not on a PPI, a statistically significant difference, João B. Augusto, MD, reported at a meeting held by the Heart Failure Association of the European Society of Cardiology. Dr. Augusto believes that these patients largely had no need for PPI treatment, and the drug may have cut iron and vitamin B12 absorption by lowering gastric acid, resulting in deficiencies that produced anemia, and following that, heart failure, he suggested.
The study focused on 423 patients admitted to Fernando da Fonseca Hospital during January 2014–June 2015 with a primary or secondary diagnosis of atrial fibrillation. He excluded 101 patients with a history of heart failure, 109 patients on antiplatelet therapy, and 33 patients with a clear need for PPI treatment because of a gastrointestinal condition. Another 11 patients were lost to follow-up, leaving 172 patients followed for 1 year.
At the time of their initial hospitalization, 53 patients (31%) received a prescription for a PPI despite having no gastrointestinal diagnosis, likely a prophylactic step for patients receiving an oral anticoagulant, Dr. Augusto said. The patients averaged 69 years old, and nearly two-thirds were men.
During 1-year follow-up, the incidence of hospitalization for acute heart failure was 8% in the patients not on a PPI and 23% among those on a PPI, a statistically significant difference. In a regression analysis that controlled for age and chronic kidney disease, the incidence of acute heart failure was 2.9 times more common among patients on a PPI, Dr. Augusto said. He and his associates used these findings to educate their hospital’s staff to not needlessly prescribe a PPI to atrial fibrillation patients.
Dr. Augusto had no disclosures.
[email protected]
On Twitter @mitchelzoler
AT HEART FAILURE 2017
Key clinical point:
Major finding: Atrial fibrillation patients had a 2.9 times higher acute heart failure rate on a proton pump inhibitor, compared with no PPI.
Data source: Retrospective review of 172 atrial fibrillation patients seen during 2014-2015 at a single center in Portugal.
Disclosures: Dr. Augusto had no disclosures.
Is the doctor in?
Within hospital medicine, there has been a recent increase in programs that provide virtual or telehealth hospitalists, primarily to hospitals that are small, remote, and/or understaffed. According to a 2013 Cisco health care customer experience report, the number of telehealth consumers will likely markedly increase to at least 7 million by 2018.1
Since telehospitalist programs are still relatively new, there are many questions about why and how they exist and how they are (and can be) funded. Questions also remain about some limitations of telehospitalist programs for both the “givers” and the “receivers” of the services. I tackle some of these questions in this article.
What is a telehospitalist?
What are the drivers of telehospitalist programs?
One primary driver of telehealth (and specifically telehospitalist) programs is an ongoing shortage of hospitalists, especially in remote areas and critical access hospitals where coverage issues are especially prominent at night and/or on weekends. In many hospitals, there is also a growing unwillingness on the part of physicians to be routinely on call at night. Although working on call used to be on par with being a physician, many younger-generation physicians are less willing to blur “work and life.” This increases the need for dedicated night coverage in many hospitals.
Another driver for some programs (especially at tertiary care medical centers) is a desire to more thoroughly assess patients prior to transfer to their respective centers (the alternative being a phone conversation with the transferring center about the patient’s status). There is also a growing desire to keep patients local if possible, which is usually better for the patient and the family and can decrease the total cost of their care.
Another catalyst to telehospitalist program growth is the growing cultural comfort level with two-way video interactions, such as Skype and FaceTime. Since videoconferencing has permeated most of our professional and personal lives, telehealth seems familiar and comfortable for both providers and patients. In a recent consumer survey, three out of every four consumers responded that they are very comfortable communicating with providers via technology, as opposed to seeing them in person.1
Another driver for some programs is financial. Depending on the way the program is structured, it can be not only financially feasible but financially beneficial, especially if the program can consolidate coverage across multiple sites (more on this later).
One other driver for some health care systems is the need to cover areas with on-site nurse practitioners and physician assistants. Using a telehospitalist makes it easier to get appropriate and required oversight for this coverage model across time and space.
What are the advantages of being a telehospitalist?
Some of the career advantages of being a telehospitalist include the shift flexibility and convenience. This work allows a hospitalist to serve a shift from anywhere in the world and from the convenience of their home. Some telehospitalists can easily work local night shifts when they live many time zones away (and therefore, don’t actually have to work a night shift). Many programs are designed to have a single hospitalist cover many hospitals over a wide geography, which would be logistically impossible to do in person. This is especially appealing for multihospital systems that cannot afford to have a hospitalist on site at each location.
The earning potential can also be appealing, depending on the number of shifts a hospitalist is willing to work.
What are the limitations of being a telehospitalist?
There are limits to what a telehospitalist can perform, many of which depend on the manner in which the program and the technology are arranged. Telehealth can vary from a cart-based videoconferencing system that is transported into a patient’s room to an independent robot that travels throughout sites. The primary limitation is the need to rely on someone in the patient’s room to act as virtual hands. This usually falls to the bedside nurse and requires a good working relationship and patience on their part. The bedside nurses have to “buy into” the program in advance and may need to have scripting for how to explain the process to the patients.
Another major challenge is interacting with different electronic health record systems. Becoming agile with a single EHR is challenging enough, but maneuvering several of them in a single shift can be extremely trying. Telehospitalists can also be challenged by technology glitches or failures that need troubleshooting both on their end and on-site. Although these problems are rare, there will always be a concern that the patient will not get his or her needs met if the technology fails.
How does the financing work?
Although this is a rapidly changing landscape, telehospitalists are not currently able to generate much revenue from professional billing. Unlike in-person visits, Medicare will not reimburse professional fees for telehospitalist visits. Although each payer is unique, most other (nonMedicare) payers are also not willing to reimburse for televisits. This may change in the future, however, as Medicare does pay for virtual specialty services such as telestroke. In addition, many states have enacted telemedicine parity laws, which require private payers to pay for all health care services equally, regardless of modality (audio, video, or in person).
For now, the financial case for employing telehospitalists for most programs has to be made using benfits other than the generation of professional fees. For telehospitalist programs that can cover several sites, the cost is substantially less than employing individual on-site hospitalists to do low-volume work. Telehospitalist programs are also, likely, less costly than is locum tenens staffing. For programs that evaluate the need for transfers, a case can be made that keeping a patient in a smaller, low-cost venue, rather than transferring them to a larger, higher-cost venue, can also reduce overall cost for a health care system.
What about licensing and credentialing?
Telehospitalists can be hindered by the need to have a license in several states and to be credentialed in several systems. This can be cumbersome, time-consuming, and expensive. To ease the multistate licensing burden, the Interstate Medical Licensure Compact has been established.2 This is an accelerated licensure process for eligible physicians that improves license portability across states. There are currently 18 states that participate, and the number continues to increase.
For credentialing, most hospitals require initial credentialing and full recredentialing every 2 years. Maintaining credentials at several sites can be extremely time consuming. To ease this burden, some hospitals with telehealth programs have adopted “credentialing by proxy,” which means that one hospital will accept the credentialing process of another facility.
What next?
In summary, there has been and will likely continue to be explosive growth of telehospitalist programs and providers for all the reasons outlined above. Although some barriers to efficient and effective practice do exist, many of those barriers are being overcome quite rapidly. I expect this growth to continue for the betterment of hospitalists, our patients, and the systems in which we work. For a more in-depth look into telemedicine in hospital medicine, view a report created by a work group of SHM's Practice Management Committee.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
1.Cisco. (2013 March 4). Cisco Study Reveals 74 Percent of Consumers Open to Virtual Doctor Visit. Cisco: The Network. Retrieved from https://newsroom.cisco.com/press-release-content?type=webcontent&articleId=1148539.
2. Interstate Medical Licensure Compact Commission. (2017). Interstate Medical Licensure Compact. Retrieved from http://www.licenseportability.org/index.html.
Within hospital medicine, there has been a recent increase in programs that provide virtual or telehealth hospitalists, primarily to hospitals that are small, remote, and/or understaffed. According to a 2013 Cisco health care customer experience report, the number of telehealth consumers will likely markedly increase to at least 7 million by 2018.1
Since telehospitalist programs are still relatively new, there are many questions about why and how they exist and how they are (and can be) funded. Questions also remain about some limitations of telehospitalist programs for both the “givers” and the “receivers” of the services. I tackle some of these questions in this article.
What is a telehospitalist?
What are the drivers of telehospitalist programs?
One primary driver of telehealth (and specifically telehospitalist) programs is an ongoing shortage of hospitalists, especially in remote areas and critical access hospitals where coverage issues are especially prominent at night and/or on weekends. In many hospitals, there is also a growing unwillingness on the part of physicians to be routinely on call at night. Although working on call used to be on par with being a physician, many younger-generation physicians are less willing to blur “work and life.” This increases the need for dedicated night coverage in many hospitals.
Another driver for some programs (especially at tertiary care medical centers) is a desire to more thoroughly assess patients prior to transfer to their respective centers (the alternative being a phone conversation with the transferring center about the patient’s status). There is also a growing desire to keep patients local if possible, which is usually better for the patient and the family and can decrease the total cost of their care.
Another catalyst to telehospitalist program growth is the growing cultural comfort level with two-way video interactions, such as Skype and FaceTime. Since videoconferencing has permeated most of our professional and personal lives, telehealth seems familiar and comfortable for both providers and patients. In a recent consumer survey, three out of every four consumers responded that they are very comfortable communicating with providers via technology, as opposed to seeing them in person.1
Another driver for some programs is financial. Depending on the way the program is structured, it can be not only financially feasible but financially beneficial, especially if the program can consolidate coverage across multiple sites (more on this later).
One other driver for some health care systems is the need to cover areas with on-site nurse practitioners and physician assistants. Using a telehospitalist makes it easier to get appropriate and required oversight for this coverage model across time and space.
What are the advantages of being a telehospitalist?
Some of the career advantages of being a telehospitalist include the shift flexibility and convenience. This work allows a hospitalist to serve a shift from anywhere in the world and from the convenience of their home. Some telehospitalists can easily work local night shifts when they live many time zones away (and therefore, don’t actually have to work a night shift). Many programs are designed to have a single hospitalist cover many hospitals over a wide geography, which would be logistically impossible to do in person. This is especially appealing for multihospital systems that cannot afford to have a hospitalist on site at each location.
The earning potential can also be appealing, depending on the number of shifts a hospitalist is willing to work.
What are the limitations of being a telehospitalist?
There are limits to what a telehospitalist can perform, many of which depend on the manner in which the program and the technology are arranged. Telehealth can vary from a cart-based videoconferencing system that is transported into a patient’s room to an independent robot that travels throughout sites. The primary limitation is the need to rely on someone in the patient’s room to act as virtual hands. This usually falls to the bedside nurse and requires a good working relationship and patience on their part. The bedside nurses have to “buy into” the program in advance and may need to have scripting for how to explain the process to the patients.
Another major challenge is interacting with different electronic health record systems. Becoming agile with a single EHR is challenging enough, but maneuvering several of them in a single shift can be extremely trying. Telehospitalists can also be challenged by technology glitches or failures that need troubleshooting both on their end and on-site. Although these problems are rare, there will always be a concern that the patient will not get his or her needs met if the technology fails.
How does the financing work?
Although this is a rapidly changing landscape, telehospitalists are not currently able to generate much revenue from professional billing. Unlike in-person visits, Medicare will not reimburse professional fees for telehospitalist visits. Although each payer is unique, most other (nonMedicare) payers are also not willing to reimburse for televisits. This may change in the future, however, as Medicare does pay for virtual specialty services such as telestroke. In addition, many states have enacted telemedicine parity laws, which require private payers to pay for all health care services equally, regardless of modality (audio, video, or in person).
For now, the financial case for employing telehospitalists for most programs has to be made using benfits other than the generation of professional fees. For telehospitalist programs that can cover several sites, the cost is substantially less than employing individual on-site hospitalists to do low-volume work. Telehospitalist programs are also, likely, less costly than is locum tenens staffing. For programs that evaluate the need for transfers, a case can be made that keeping a patient in a smaller, low-cost venue, rather than transferring them to a larger, higher-cost venue, can also reduce overall cost for a health care system.
What about licensing and credentialing?
Telehospitalists can be hindered by the need to have a license in several states and to be credentialed in several systems. This can be cumbersome, time-consuming, and expensive. To ease the multistate licensing burden, the Interstate Medical Licensure Compact has been established.2 This is an accelerated licensure process for eligible physicians that improves license portability across states. There are currently 18 states that participate, and the number continues to increase.
For credentialing, most hospitals require initial credentialing and full recredentialing every 2 years. Maintaining credentials at several sites can be extremely time consuming. To ease this burden, some hospitals with telehealth programs have adopted “credentialing by proxy,” which means that one hospital will accept the credentialing process of another facility.
What next?
In summary, there has been and will likely continue to be explosive growth of telehospitalist programs and providers for all the reasons outlined above. Although some barriers to efficient and effective practice do exist, many of those barriers are being overcome quite rapidly. I expect this growth to continue for the betterment of hospitalists, our patients, and the systems in which we work. For a more in-depth look into telemedicine in hospital medicine, view a report created by a work group of SHM's Practice Management Committee.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
1.Cisco. (2013 March 4). Cisco Study Reveals 74 Percent of Consumers Open to Virtual Doctor Visit. Cisco: The Network. Retrieved from https://newsroom.cisco.com/press-release-content?type=webcontent&articleId=1148539.
2. Interstate Medical Licensure Compact Commission. (2017). Interstate Medical Licensure Compact. Retrieved from http://www.licenseportability.org/index.html.
Within hospital medicine, there has been a recent increase in programs that provide virtual or telehealth hospitalists, primarily to hospitals that are small, remote, and/or understaffed. According to a 2013 Cisco health care customer experience report, the number of telehealth consumers will likely markedly increase to at least 7 million by 2018.1
Since telehospitalist programs are still relatively new, there are many questions about why and how they exist and how they are (and can be) funded. Questions also remain about some limitations of telehospitalist programs for both the “givers” and the “receivers” of the services. I tackle some of these questions in this article.
What is a telehospitalist?
What are the drivers of telehospitalist programs?
One primary driver of telehealth (and specifically telehospitalist) programs is an ongoing shortage of hospitalists, especially in remote areas and critical access hospitals where coverage issues are especially prominent at night and/or on weekends. In many hospitals, there is also a growing unwillingness on the part of physicians to be routinely on call at night. Although working on call used to be on par with being a physician, many younger-generation physicians are less willing to blur “work and life.” This increases the need for dedicated night coverage in many hospitals.
Another driver for some programs (especially at tertiary care medical centers) is a desire to more thoroughly assess patients prior to transfer to their respective centers (the alternative being a phone conversation with the transferring center about the patient’s status). There is also a growing desire to keep patients local if possible, which is usually better for the patient and the family and can decrease the total cost of their care.
Another catalyst to telehospitalist program growth is the growing cultural comfort level with two-way video interactions, such as Skype and FaceTime. Since videoconferencing has permeated most of our professional and personal lives, telehealth seems familiar and comfortable for both providers and patients. In a recent consumer survey, three out of every four consumers responded that they are very comfortable communicating with providers via technology, as opposed to seeing them in person.1
Another driver for some programs is financial. Depending on the way the program is structured, it can be not only financially feasible but financially beneficial, especially if the program can consolidate coverage across multiple sites (more on this later).
One other driver for some health care systems is the need to cover areas with on-site nurse practitioners and physician assistants. Using a telehospitalist makes it easier to get appropriate and required oversight for this coverage model across time and space.
What are the advantages of being a telehospitalist?
Some of the career advantages of being a telehospitalist include the shift flexibility and convenience. This work allows a hospitalist to serve a shift from anywhere in the world and from the convenience of their home. Some telehospitalists can easily work local night shifts when they live many time zones away (and therefore, don’t actually have to work a night shift). Many programs are designed to have a single hospitalist cover many hospitals over a wide geography, which would be logistically impossible to do in person. This is especially appealing for multihospital systems that cannot afford to have a hospitalist on site at each location.
The earning potential can also be appealing, depending on the number of shifts a hospitalist is willing to work.
What are the limitations of being a telehospitalist?
There are limits to what a telehospitalist can perform, many of which depend on the manner in which the program and the technology are arranged. Telehealth can vary from a cart-based videoconferencing system that is transported into a patient’s room to an independent robot that travels throughout sites. The primary limitation is the need to rely on someone in the patient’s room to act as virtual hands. This usually falls to the bedside nurse and requires a good working relationship and patience on their part. The bedside nurses have to “buy into” the program in advance and may need to have scripting for how to explain the process to the patients.
Another major challenge is interacting with different electronic health record systems. Becoming agile with a single EHR is challenging enough, but maneuvering several of them in a single shift can be extremely trying. Telehospitalists can also be challenged by technology glitches or failures that need troubleshooting both on their end and on-site. Although these problems are rare, there will always be a concern that the patient will not get his or her needs met if the technology fails.
How does the financing work?
Although this is a rapidly changing landscape, telehospitalists are not currently able to generate much revenue from professional billing. Unlike in-person visits, Medicare will not reimburse professional fees for telehospitalist visits. Although each payer is unique, most other (nonMedicare) payers are also not willing to reimburse for televisits. This may change in the future, however, as Medicare does pay for virtual specialty services such as telestroke. In addition, many states have enacted telemedicine parity laws, which require private payers to pay for all health care services equally, regardless of modality (audio, video, or in person).
For now, the financial case for employing telehospitalists for most programs has to be made using benfits other than the generation of professional fees. For telehospitalist programs that can cover several sites, the cost is substantially less than employing individual on-site hospitalists to do low-volume work. Telehospitalist programs are also, likely, less costly than is locum tenens staffing. For programs that evaluate the need for transfers, a case can be made that keeping a patient in a smaller, low-cost venue, rather than transferring them to a larger, higher-cost venue, can also reduce overall cost for a health care system.
What about licensing and credentialing?
Telehospitalists can be hindered by the need to have a license in several states and to be credentialed in several systems. This can be cumbersome, time-consuming, and expensive. To ease the multistate licensing burden, the Interstate Medical Licensure Compact has been established.2 This is an accelerated licensure process for eligible physicians that improves license portability across states. There are currently 18 states that participate, and the number continues to increase.
For credentialing, most hospitals require initial credentialing and full recredentialing every 2 years. Maintaining credentials at several sites can be extremely time consuming. To ease this burden, some hospitals with telehealth programs have adopted “credentialing by proxy,” which means that one hospital will accept the credentialing process of another facility.
What next?
In summary, there has been and will likely continue to be explosive growth of telehospitalist programs and providers for all the reasons outlined above. Although some barriers to efficient and effective practice do exist, many of those barriers are being overcome quite rapidly. I expect this growth to continue for the betterment of hospitalists, our patients, and the systems in which we work. For a more in-depth look into telemedicine in hospital medicine, view a report created by a work group of SHM's Practice Management Committee.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
References
1.Cisco. (2013 March 4). Cisco Study Reveals 74 Percent of Consumers Open to Virtual Doctor Visit. Cisco: The Network. Retrieved from https://newsroom.cisco.com/press-release-content?type=webcontent&articleId=1148539.
2. Interstate Medical Licensure Compact Commission. (2017). Interstate Medical Licensure Compact. Retrieved from http://www.licenseportability.org/index.html.
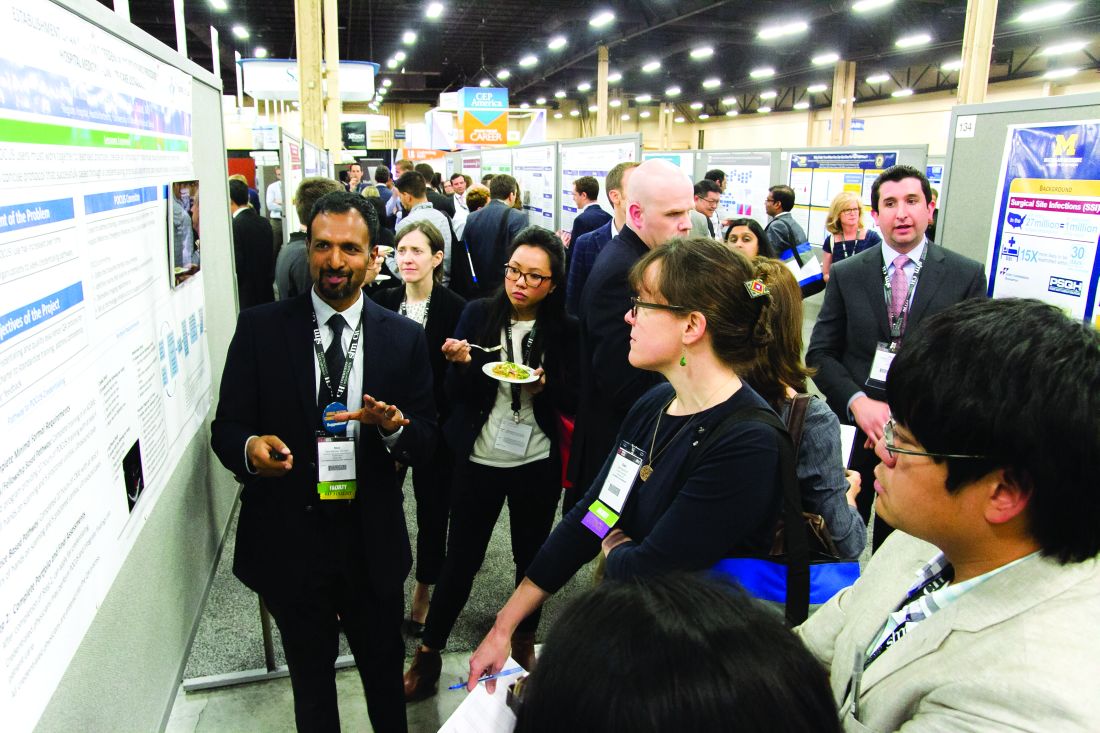
RIV spotlights HM-focused research in real-time
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
LAS VEGAS – Masih Shinwa, MD, stood beside a half-circle of judges at SHM’s annual Research, Innovations, and Clinical Vignettes poster competition and argued why his entry, already a finalist, should win.
To think, his work, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was borne simply of a group of medical students who incredulously said that they were amazed patients would be woken up in the night for tests.
Dr. Shinwa’s project shows just how an idea can blossom into a recognized poster.
Some 18 months ago, the students he works with at Mount Sinai Hospital in New York just couldn’t understand why so many tests had to be done overnight while a patient slept. So, Dr. Shinwa and his colleagues looked at ways to reduce unnecessary lab tests and chemistry testing.
Now, Dr. Shinwa was humbled to think his work and that of his colleagues could be a pathway to eliminating tests that don’t need to happen across the country, a focal point of SHM and the American Board of Internal Medicine Foundation’s Choosing Wisely Campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but, unless you attend these types of national meetings, it’s hard to get that perspective across (the country).”
That level of personal and professional collaboration is the purpose of the RIV, said Margaret Fang, MD, MPH, FHM, program chair for the HM17 competition.
“One of the amazing things is, everyone has their own poster. They’re doing their work,” she added. “But then they start up conversations with the people next to them. ... Seeing the organic networking and discussion that arise from that is really exciting. RIV serves as a way of connecting people who might not have know the other person was doing that kind of work.”
Dr. Fang said that the intergenerational aspect of the RIV, where early-career hospitalists mingle with the field’s founders and leaders, creates an environment where research is encouraged.
“Just seeing the intense interest that more senior hospitalists have in mentoring and guiding the next generation is delightful,” she added.
Dr. Shinwa said that the specialty’s focus on both clinical research and systems-level change is important, as the work positions the field to be leaders not just in patient care but for hospitals as a whole.
“We are physicians,” he said. “Our role is taking care of patients. Knowing that there are people who are not just focusing on taking care of specific patients but are actually there to improve the entire system and the process – that’s really gratifying.”
That’s the word that Merideth Prevost, MD, of New Mexico VA Health Care System, Albuquerque also used to describe presenting her poster, “Improving Accuracy in Measuring Fluid Balance on a General Medicine Ward.”
“If we can improve our little microcosm, then spread it to other folks, then patients all over the country can be helped by what we do,” she said. “And that’s a really cool thought.”
The RIV also has the unique advantage of letting people have immediate and direct access to lead researchers at the exact moment of reading their research. HM17 attendees had conversations that usually went beyond just the results, which can be downloaded at www.shmabstracts.com.
Dr. Prevost believes that the chats can helpfully highlight the behind-the-scenes pitfalls and mistakes of research that can sometimes be just as valuable as the published results.
“The things that don’t make it to the posters are all the challenges that people experienced on the way to get to this particular work,” she added. “Like ‘Oh, well, I’ve tried this before, and it didn’t work at all.’ Or, ‘Oh yeah we tried this and it didn’t work at all, but we tried this other thing that worked really great.’ Or, ‘This was the key to our success.’ You can brainstorm with every poster that you’re interested in, which is really exciting.”
Hospitalists share strategies to secure, excel at jobs
LAS VEGAS – In the view of academic hospitalist Alfred Burger, MD, SFHM, portability was long a dirty word in HM circles. But not anymore.
“My good friends in law and business do this all the time,” said Dr. Burger, associate program director of the internal medicine residency program at Mount Sinai Beth Israel in New York. “You’re not going to make partner in city X, but they’ve got an opening to be partner in city Y if you go there and perform for a year. People up and leave coasts, people up and leave states, people have up and left the country. ... Doctors are starting to view it the same way.”
The lessons of career development were a focal point of HM17, particularly for younger physicians who could take advantage of the Early-Career Hospitalists mini-track. But Dr. Burger said that those strategies of upward mobility can apply whether someone is chasing their first job or their fifth.
First, identify one’s strengths and play to those. Then identify the skills you don’t have or don’t excel at, and address those deficiencies.
“How can you acquire the skills to put yourself in the best position to move up, if you wish to develop your career as a leader?” Dr. Burger said. “If you wish to be the best clinician, you still need to stay on top of the game. Things like coming to SHM, staying on top of the content. That’s important.”
Another skill set is self-advocacy.
“Be your own champion,” said Brian Markoff, MD, SFHM, chief of hospital medicine at Mount Sinai St. Luke’s in New York. “Many of us are very good at this and many of us are terrible at this. You may fall somewhere in between, but you do have to be your own champion.”
Dr. Burger said that he understands that there is a fine line between too much self-promotion and too little. But he urged hospitalists at all career points to take responsibility for marketing themselves.
“Nobody is going to invest in your career unless you yourself invest in it,” he added. “You have to put it as a priority, and not in a selfish way, but in a way [that,] if you wish to move forward and move up, you’ve got to put the time in. It’s not a natural assumption anymore that, if you are the best and brightest of a group of doctors, you will just be chosen to lead.”
In a similar vein, networking is a major boon to career development that can be a double-edged scalpel.
“Having a great ‘social game’ is important, but if all you bring to the table is a social game, you’ll find yourself out of a job just as quickly as you found that job,” Dr. Burger said. “Meaning, you might be able to get it based on that, but you’re not going to be able to sustain it. At the same time, being highly accomplished and having no social graces is also a killer. So, you need to be sort of strong in both areas.”
Many of the meeting’s opportunities for tips on professional development are personal, but HM group leaders have to consider developing the careers of their employees. One of the main planks of that is physician engagement, said Flora Kisuule, MD, MPH, SFHM, of Johns Hopkins University, Baltimore.
“I don’t believe your institution or your organization can go anywhere if your employees are not engaged or if the people you work with are not engaged,” she said, adding that disengaged employees “are actively working against you. You don’t want that. You can’t go in any direction when there are people rowing in the opposite direction. At best, you stay in one place. At worst, you can end up losing ground.”
Hospitalist Christie Masters, MD, MBA, MHA, who practices at UCLA, disclosed during a session that she also runs a wellness coaching firm. She added that a focus on personal wellness and well-being is its own form of career development. It works in tandem with engagement, morale, and professional growth.
“If you’re only focusing on wellness and you don’t have hospitalists or a group that’s engaged or with high morale, they’re going to burnout or they’re going to leave,” Dr. Masters said. “And nobody wants that for their group. So, if we surround ourselves with people who feel well and feel whole, that’s going to have intangible benefits ... that affect the bottom line.”
LAS VEGAS – In the view of academic hospitalist Alfred Burger, MD, SFHM, portability was long a dirty word in HM circles. But not anymore.
“My good friends in law and business do this all the time,” said Dr. Burger, associate program director of the internal medicine residency program at Mount Sinai Beth Israel in New York. “You’re not going to make partner in city X, but they’ve got an opening to be partner in city Y if you go there and perform for a year. People up and leave coasts, people up and leave states, people have up and left the country. ... Doctors are starting to view it the same way.”
The lessons of career development were a focal point of HM17, particularly for younger physicians who could take advantage of the Early-Career Hospitalists mini-track. But Dr. Burger said that those strategies of upward mobility can apply whether someone is chasing their first job or their fifth.
First, identify one’s strengths and play to those. Then identify the skills you don’t have or don’t excel at, and address those deficiencies.
“How can you acquire the skills to put yourself in the best position to move up, if you wish to develop your career as a leader?” Dr. Burger said. “If you wish to be the best clinician, you still need to stay on top of the game. Things like coming to SHM, staying on top of the content. That’s important.”
Another skill set is self-advocacy.
“Be your own champion,” said Brian Markoff, MD, SFHM, chief of hospital medicine at Mount Sinai St. Luke’s in New York. “Many of us are very good at this and many of us are terrible at this. You may fall somewhere in between, but you do have to be your own champion.”
Dr. Burger said that he understands that there is a fine line between too much self-promotion and too little. But he urged hospitalists at all career points to take responsibility for marketing themselves.
“Nobody is going to invest in your career unless you yourself invest in it,” he added. “You have to put it as a priority, and not in a selfish way, but in a way [that,] if you wish to move forward and move up, you’ve got to put the time in. It’s not a natural assumption anymore that, if you are the best and brightest of a group of doctors, you will just be chosen to lead.”
In a similar vein, networking is a major boon to career development that can be a double-edged scalpel.
“Having a great ‘social game’ is important, but if all you bring to the table is a social game, you’ll find yourself out of a job just as quickly as you found that job,” Dr. Burger said. “Meaning, you might be able to get it based on that, but you’re not going to be able to sustain it. At the same time, being highly accomplished and having no social graces is also a killer. So, you need to be sort of strong in both areas.”
Many of the meeting’s opportunities for tips on professional development are personal, but HM group leaders have to consider developing the careers of their employees. One of the main planks of that is physician engagement, said Flora Kisuule, MD, MPH, SFHM, of Johns Hopkins University, Baltimore.
“I don’t believe your institution or your organization can go anywhere if your employees are not engaged or if the people you work with are not engaged,” she said, adding that disengaged employees “are actively working against you. You don’t want that. You can’t go in any direction when there are people rowing in the opposite direction. At best, you stay in one place. At worst, you can end up losing ground.”
Hospitalist Christie Masters, MD, MBA, MHA, who practices at UCLA, disclosed during a session that she also runs a wellness coaching firm. She added that a focus on personal wellness and well-being is its own form of career development. It works in tandem with engagement, morale, and professional growth.
“If you’re only focusing on wellness and you don’t have hospitalists or a group that’s engaged or with high morale, they’re going to burnout or they’re going to leave,” Dr. Masters said. “And nobody wants that for their group. So, if we surround ourselves with people who feel well and feel whole, that’s going to have intangible benefits ... that affect the bottom line.”
LAS VEGAS – In the view of academic hospitalist Alfred Burger, MD, SFHM, portability was long a dirty word in HM circles. But not anymore.
“My good friends in law and business do this all the time,” said Dr. Burger, associate program director of the internal medicine residency program at Mount Sinai Beth Israel in New York. “You’re not going to make partner in city X, but they’ve got an opening to be partner in city Y if you go there and perform for a year. People up and leave coasts, people up and leave states, people have up and left the country. ... Doctors are starting to view it the same way.”
The lessons of career development were a focal point of HM17, particularly for younger physicians who could take advantage of the Early-Career Hospitalists mini-track. But Dr. Burger said that those strategies of upward mobility can apply whether someone is chasing their first job or their fifth.
First, identify one’s strengths and play to those. Then identify the skills you don’t have or don’t excel at, and address those deficiencies.
“How can you acquire the skills to put yourself in the best position to move up, if you wish to develop your career as a leader?” Dr. Burger said. “If you wish to be the best clinician, you still need to stay on top of the game. Things like coming to SHM, staying on top of the content. That’s important.”
Another skill set is self-advocacy.
“Be your own champion,” said Brian Markoff, MD, SFHM, chief of hospital medicine at Mount Sinai St. Luke’s in New York. “Many of us are very good at this and many of us are terrible at this. You may fall somewhere in between, but you do have to be your own champion.”
Dr. Burger said that he understands that there is a fine line between too much self-promotion and too little. But he urged hospitalists at all career points to take responsibility for marketing themselves.
“Nobody is going to invest in your career unless you yourself invest in it,” he added. “You have to put it as a priority, and not in a selfish way, but in a way [that,] if you wish to move forward and move up, you’ve got to put the time in. It’s not a natural assumption anymore that, if you are the best and brightest of a group of doctors, you will just be chosen to lead.”
In a similar vein, networking is a major boon to career development that can be a double-edged scalpel.
“Having a great ‘social game’ is important, but if all you bring to the table is a social game, you’ll find yourself out of a job just as quickly as you found that job,” Dr. Burger said. “Meaning, you might be able to get it based on that, but you’re not going to be able to sustain it. At the same time, being highly accomplished and having no social graces is also a killer. So, you need to be sort of strong in both areas.”
Many of the meeting’s opportunities for tips on professional development are personal, but HM group leaders have to consider developing the careers of their employees. One of the main planks of that is physician engagement, said Flora Kisuule, MD, MPH, SFHM, of Johns Hopkins University, Baltimore.
“I don’t believe your institution or your organization can go anywhere if your employees are not engaged or if the people you work with are not engaged,” she said, adding that disengaged employees “are actively working against you. You don’t want that. You can’t go in any direction when there are people rowing in the opposite direction. At best, you stay in one place. At worst, you can end up losing ground.”
Hospitalist Christie Masters, MD, MBA, MHA, who practices at UCLA, disclosed during a session that she also runs a wellness coaching firm. She added that a focus on personal wellness and well-being is its own form of career development. It works in tandem with engagement, morale, and professional growth.
“If you’re only focusing on wellness and you don’t have hospitalists or a group that’s engaged or with high morale, they’re going to burnout or they’re going to leave,” Dr. Masters said. “And nobody wants that for their group. So, if we surround ourselves with people who feel well and feel whole, that’s going to have intangible benefits ... that affect the bottom line.”
Hospitalists’ EMR frustrations continue: SHM report
LAS VEGAS – Ronald Schaefer, MD, a hospitalist with Hawaii Pacific Health who also works on creating digital templates for his hospital, can’t input hemoglobin A1c levels from three different labs into his electronic medical records (EMR) system the same way.
Hospitalist George Dimitriou, MD, FHM, who splits his time at Allegheny Health Network in Pittsburgh between clinical work and medical informatics, worries there are so many fields in his EMR that physicians can get distracted.
Yevgeniy “Eugene” Gitelman, MD, a clinical informatics manager at the Perelman School of Medicine at University of Pennsylvania Health in Philadelphia, wonders how good any systems can be with the privacy concerns related to HIPAA.
This was the nexus of IT and HM17, a time when hospitalists said they are stymied and frustrated by continuing issues of interoperability, functionality, and access. The meeting highlighted new smartphone and tablet applications, as well as medical devices available to hospitalists, but tech-focused physicians say the biggest issue remains the day-to-day workings of EMR.
“If you build something really good, people will use it. If you build something that makes their documentation process a lot easier and a lot faster and a lot better, they’ll use it,” said Dr. Schaefer. “The tools aren’t there yet. I don’t think the technology is mature enough.”
If the tech hasn’t yet come of full age, the concerns surely have. SHM unveiled a white paper at HM17 that codified hospitalists’ worries about the current state of IT. The report, “Hospitalist Perspectives on Electronic Medical Records,” found that “a staggering” 85% of providers said they spend more time interacting with their inpatient EMR than their actual inpatients.
Rupesh Prasad, MD, MPH, SFHM, chair of SHM’s Health IT Committee, says the report is meant to foster discussion about the issues surrounding EMRs. The data points, generated from 462 respondents, are stark. Just 40% said they were happy with their EMR. Some 52% would change vendors if they could. One-quarter of respondents would revert to using paper if given the option.
“By sharing these results, we hope to raise awareness of the unacceptable performance of existing systems,” the report states. “This continues to contribute to our slower than desired improvement in quality and safety, as well as increasing provider frustration. We strongly believe that we need a renewed focus on initial goals of technology adoption in health care.”
Dr. Prasad said that he hopes hospitalists heed that call to action and use the report in discussions with various stakeholders, including vendors, public policy officials, and their own bosses.
“We want to give hospitalists ammunition to go back to their systems and talk to their administrators to see if they can influence [it],” he said.
Dr. Prasad is pleased that the society is sensitive to the issues surrounding technology. He encourages hospitalists to actively participate in HMX, SHM’s online portal to discuss health IT issues and crowd-source potential solutions. Patrick Vulgamore, MPH, SHM’s director of governance and practice management, said the society is formulating a potential special-interest working group to further seek to solve problems.
Hospitalists were also urged to apply for American Board of Medical Specialties (ABMS) certification in clinical informatics. Physicians can grandfather into eligibility via the “practice pathway” through the end of the year, if they’ve been working in informatics professionally for at least 25% of their time during any three of the previous five years. Next year, only graduates of two-year Accreditation Council for Graduate Medical Education–accredited fellowships will be board eligible.
“As end users of technology, we understand the problems better than anybody else,” Dr. Prasad said. “Obviously, the next step would be try to solve the problems. And what better way then to get involved and become experts in what you do?”
While much of the meeting’s tech talk was frustration, both former National Coordinator for Health IT Karen DeSalvo, MD, MPH, MSc, and HM Dean Robert Wachter, MD, MHM, forecast a future when artificial intelligence and intuitive computers work alongside physicians. Imagine the user-friendliness of Apple’s Siri or Google’s Alexa married to the existing functionalities provided by firms such as Epic or Cerner.
But that’s years away, and hospitalists like Dr. Dimitriou want help now.
“The speed of medicine, the speed of what’s happening in real time, is still faster than what our electronic tools seem to be able to keep up with,” he said. “There are encouraging signs that we’ve definitely moved in the right direction. We’ve come a long way ... but again, the speed at which things are moving? We aren’t keeping up. We’ve got to do more.”
LAS VEGAS – Ronald Schaefer, MD, a hospitalist with Hawaii Pacific Health who also works on creating digital templates for his hospital, can’t input hemoglobin A1c levels from three different labs into his electronic medical records (EMR) system the same way.
Hospitalist George Dimitriou, MD, FHM, who splits his time at Allegheny Health Network in Pittsburgh between clinical work and medical informatics, worries there are so many fields in his EMR that physicians can get distracted.
Yevgeniy “Eugene” Gitelman, MD, a clinical informatics manager at the Perelman School of Medicine at University of Pennsylvania Health in Philadelphia, wonders how good any systems can be with the privacy concerns related to HIPAA.
This was the nexus of IT and HM17, a time when hospitalists said they are stymied and frustrated by continuing issues of interoperability, functionality, and access. The meeting highlighted new smartphone and tablet applications, as well as medical devices available to hospitalists, but tech-focused physicians say the biggest issue remains the day-to-day workings of EMR.
“If you build something really good, people will use it. If you build something that makes their documentation process a lot easier and a lot faster and a lot better, they’ll use it,” said Dr. Schaefer. “The tools aren’t there yet. I don’t think the technology is mature enough.”
If the tech hasn’t yet come of full age, the concerns surely have. SHM unveiled a white paper at HM17 that codified hospitalists’ worries about the current state of IT. The report, “Hospitalist Perspectives on Electronic Medical Records,” found that “a staggering” 85% of providers said they spend more time interacting with their inpatient EMR than their actual inpatients.
Rupesh Prasad, MD, MPH, SFHM, chair of SHM’s Health IT Committee, says the report is meant to foster discussion about the issues surrounding EMRs. The data points, generated from 462 respondents, are stark. Just 40% said they were happy with their EMR. Some 52% would change vendors if they could. One-quarter of respondents would revert to using paper if given the option.
“By sharing these results, we hope to raise awareness of the unacceptable performance of existing systems,” the report states. “This continues to contribute to our slower than desired improvement in quality and safety, as well as increasing provider frustration. We strongly believe that we need a renewed focus on initial goals of technology adoption in health care.”
Dr. Prasad said that he hopes hospitalists heed that call to action and use the report in discussions with various stakeholders, including vendors, public policy officials, and their own bosses.
“We want to give hospitalists ammunition to go back to their systems and talk to their administrators to see if they can influence [it],” he said.
Dr. Prasad is pleased that the society is sensitive to the issues surrounding technology. He encourages hospitalists to actively participate in HMX, SHM’s online portal to discuss health IT issues and crowd-source potential solutions. Patrick Vulgamore, MPH, SHM’s director of governance and practice management, said the society is formulating a potential special-interest working group to further seek to solve problems.
Hospitalists were also urged to apply for American Board of Medical Specialties (ABMS) certification in clinical informatics. Physicians can grandfather into eligibility via the “practice pathway” through the end of the year, if they’ve been working in informatics professionally for at least 25% of their time during any three of the previous five years. Next year, only graduates of two-year Accreditation Council for Graduate Medical Education–accredited fellowships will be board eligible.
“As end users of technology, we understand the problems better than anybody else,” Dr. Prasad said. “Obviously, the next step would be try to solve the problems. And what better way then to get involved and become experts in what you do?”
While much of the meeting’s tech talk was frustration, both former National Coordinator for Health IT Karen DeSalvo, MD, MPH, MSc, and HM Dean Robert Wachter, MD, MHM, forecast a future when artificial intelligence and intuitive computers work alongside physicians. Imagine the user-friendliness of Apple’s Siri or Google’s Alexa married to the existing functionalities provided by firms such as Epic or Cerner.
But that’s years away, and hospitalists like Dr. Dimitriou want help now.
“The speed of medicine, the speed of what’s happening in real time, is still faster than what our electronic tools seem to be able to keep up with,” he said. “There are encouraging signs that we’ve definitely moved in the right direction. We’ve come a long way ... but again, the speed at which things are moving? We aren’t keeping up. We’ve got to do more.”
LAS VEGAS – Ronald Schaefer, MD, a hospitalist with Hawaii Pacific Health who also works on creating digital templates for his hospital, can’t input hemoglobin A1c levels from three different labs into his electronic medical records (EMR) system the same way.
Hospitalist George Dimitriou, MD, FHM, who splits his time at Allegheny Health Network in Pittsburgh between clinical work and medical informatics, worries there are so many fields in his EMR that physicians can get distracted.
Yevgeniy “Eugene” Gitelman, MD, a clinical informatics manager at the Perelman School of Medicine at University of Pennsylvania Health in Philadelphia, wonders how good any systems can be with the privacy concerns related to HIPAA.
This was the nexus of IT and HM17, a time when hospitalists said they are stymied and frustrated by continuing issues of interoperability, functionality, and access. The meeting highlighted new smartphone and tablet applications, as well as medical devices available to hospitalists, but tech-focused physicians say the biggest issue remains the day-to-day workings of EMR.
“If you build something really good, people will use it. If you build something that makes their documentation process a lot easier and a lot faster and a lot better, they’ll use it,” said Dr. Schaefer. “The tools aren’t there yet. I don’t think the technology is mature enough.”
If the tech hasn’t yet come of full age, the concerns surely have. SHM unveiled a white paper at HM17 that codified hospitalists’ worries about the current state of IT. The report, “Hospitalist Perspectives on Electronic Medical Records,” found that “a staggering” 85% of providers said they spend more time interacting with their inpatient EMR than their actual inpatients.
Rupesh Prasad, MD, MPH, SFHM, chair of SHM’s Health IT Committee, says the report is meant to foster discussion about the issues surrounding EMRs. The data points, generated from 462 respondents, are stark. Just 40% said they were happy with their EMR. Some 52% would change vendors if they could. One-quarter of respondents would revert to using paper if given the option.
“By sharing these results, we hope to raise awareness of the unacceptable performance of existing systems,” the report states. “This continues to contribute to our slower than desired improvement in quality and safety, as well as increasing provider frustration. We strongly believe that we need a renewed focus on initial goals of technology adoption in health care.”
Dr. Prasad said that he hopes hospitalists heed that call to action and use the report in discussions with various stakeholders, including vendors, public policy officials, and their own bosses.
“We want to give hospitalists ammunition to go back to their systems and talk to their administrators to see if they can influence [it],” he said.
Dr. Prasad is pleased that the society is sensitive to the issues surrounding technology. He encourages hospitalists to actively participate in HMX, SHM’s online portal to discuss health IT issues and crowd-source potential solutions. Patrick Vulgamore, MPH, SHM’s director of governance and practice management, said the society is formulating a potential special-interest working group to further seek to solve problems.
Hospitalists were also urged to apply for American Board of Medical Specialties (ABMS) certification in clinical informatics. Physicians can grandfather into eligibility via the “practice pathway” through the end of the year, if they’ve been working in informatics professionally for at least 25% of their time during any three of the previous five years. Next year, only graduates of two-year Accreditation Council for Graduate Medical Education–accredited fellowships will be board eligible.
“As end users of technology, we understand the problems better than anybody else,” Dr. Prasad said. “Obviously, the next step would be try to solve the problems. And what better way then to get involved and become experts in what you do?”
While much of the meeting’s tech talk was frustration, both former National Coordinator for Health IT Karen DeSalvo, MD, MPH, MSc, and HM Dean Robert Wachter, MD, MHM, forecast a future when artificial intelligence and intuitive computers work alongside physicians. Imagine the user-friendliness of Apple’s Siri or Google’s Alexa married to the existing functionalities provided by firms such as Epic or Cerner.
But that’s years away, and hospitalists like Dr. Dimitriou want help now.
“The speed of medicine, the speed of what’s happening in real time, is still faster than what our electronic tools seem to be able to keep up with,” he said. “There are encouraging signs that we’ve definitely moved in the right direction. We’ve come a long way ... but again, the speed at which things are moving? We aren’t keeping up. We’ve got to do more.”