User login
In Case You Missed It: COVID
Why are boosters being given after 8 months? Experts weigh in
Following the White House administration’s announcement to start booster COVID-19 vaccinations for American adults in September, experts weighed in on the evidence for choosing an 8-month cutoff, how breakthrough infections figure in, and why calling one mRNA vaccine better than the other could be misleading.
Timing came up more than once at the Aug. 18 White House briefing announcing the booster plans. Reporters asked about the start time of Sept. 20 and people waiting at least 8 months after their second mRNA vaccine dose to get a booster.
Anthony Fauci, MD, chief medical adviser to the president and director of the National Institute of Allergy and Infectious Diseases, explained that late September gives the United States time to set up the logistics.
Centers for Disease Control and Prevention Director Rochelle Walensky, MD, MPH, added that 8 months is in part based on data from Israel and other countries on the waning of vaccine effectiveness over time.
“It is possible that 8 [months] is associated with the amount of time that we’ve been able to follow large groups of people, especially those who are 65 and older,” Julie Swann, PhD, said during a subsequent media briefing sponsored by Newswise on Aug. 18. “I know that Pfizer has said that they think a booster sometime between 6 and 12 months would be reasonable.”
Dr. Swann supported the administration’s booster shots plan. She said it is important “that we continue to get people the full amount of protection if it’s recommended by CDC and ACIP [Advisory Committee on Immunization Practices] that would come from a booster shot.” Dr. Swann is department head and A. Doug Allison Distinguished Professor at North Carolina State University and an adjunct professor in the joint department of biomedical engineering at the University of North Carolina at Chapel Hill.
Rising importance of breakthrough cases
Also on Aug. 18, news emerged that breakthrough cases are on the rise in seven U.S. states, likely because of the Delta variant.
These SARS-CoV-2 infections among the fully vaccinated account for 20% of cases in six of the seven states cited in a New York Times report, for example. Researchers also suggested that hospitalization and deaths associated with breakthrough cases could be higher than previously appreciated.
“It is expected that over time we will see more cases of Delta variant infections among vaccinated people. This points toward the need for booster vaccines and/or eventual modifications to the vaccine to capture new variants in the future,” Juan Wisnivesky, MD, DrPH, chief of the division of general internal medicine at Mount Sinai Health System in New York City, said during the briefing.
Vaccine comparisons unfair?
Following the release of a Mayo Clinic study reporting lower effectiveness of the Pfizer mRNA vaccine at 42% versus 76% for the Moderna product, some people started asking if one vaccine was better than the other.
“To begin with, the vaccines are not being compared side-by-side,” Dr. Wisnivesky said. “So we only know the effectiveness of each vaccine versus placebo, but we don’t know one versus the other.”
He added that different study designs, different populations, and other factors make direct comparisons difficult.
More evidence will be needed, Dr. Wisnivesky said, before public health officials can recommend that someone who received one mRNA vaccine switch to another for their booster shot.
Layering protections
Continuing to recommend masks is essential, Dr. Swann added. “With this Delta variant, it does appear that the possibility of reinfection or of a disease case breaking through vaccination can occur. So that makes it even more important to consider using nonpharmaceutical interventions while we continue to vaccinate people.”
Wearing or not wearing a mask is one of the behaviors that drive the transmission of disease, Dr. Swann said.
“What we saw across the board is that many people really wanted to go back to normal as much as they could. And we went back to normal a little bit too soon, especially given this new version of the virus that was circulating,” she said.
In poll, most favor boosters
A recent poll conducted by Medscape indicates that a majority of vaccinated physicians and nurses are ready and willing to take a COVID-19 booster vaccine. For example, 93% of 943 doctors and 87% of 1,680 nurses who responded want booster shots, either immediately or when they are authorized and recommended.
Among 510 WebMD readers responding to a similar poll, 82% indicated they wanted a booster shot.
A challenging task lies ahead
According to CDC data, as of Aug. 18, 2021, almost 169 million Americans are fully vaccinated, including the one-shot Johnson & Johnson adenovirus vaccine.
“I think it will be a challenge to get everyone who is fully vaccinated to come in for that booster,” Dr. Swann said.
Logistically speaking, Dr. Swann explained that many sites that were open for initial vaccinations, including drive-up locations and 24/7 vaccination sites, are no longer operating.
“We might see that rollout look a little bit differently. You might be able to go to your pharmacy or go to your primary care physician,” she said.
“But we may not see as many weekend events so it is going to be easier to get some people a booster than others.
“One interesting thing will also be whether a booster is effective in actually preventing you from giving a disease to someone else,” Dr. Swann said. “That could make a difference as well, because that might play into whether companies, hospitals, universities, or others require a booster.”
A version of this article first appeared on Medscape.com.
Following the White House administration’s announcement to start booster COVID-19 vaccinations for American adults in September, experts weighed in on the evidence for choosing an 8-month cutoff, how breakthrough infections figure in, and why calling one mRNA vaccine better than the other could be misleading.
Timing came up more than once at the Aug. 18 White House briefing announcing the booster plans. Reporters asked about the start time of Sept. 20 and people waiting at least 8 months after their second mRNA vaccine dose to get a booster.
Anthony Fauci, MD, chief medical adviser to the president and director of the National Institute of Allergy and Infectious Diseases, explained that late September gives the United States time to set up the logistics.
Centers for Disease Control and Prevention Director Rochelle Walensky, MD, MPH, added that 8 months is in part based on data from Israel and other countries on the waning of vaccine effectiveness over time.
“It is possible that 8 [months] is associated with the amount of time that we’ve been able to follow large groups of people, especially those who are 65 and older,” Julie Swann, PhD, said during a subsequent media briefing sponsored by Newswise on Aug. 18. “I know that Pfizer has said that they think a booster sometime between 6 and 12 months would be reasonable.”
Dr. Swann supported the administration’s booster shots plan. She said it is important “that we continue to get people the full amount of protection if it’s recommended by CDC and ACIP [Advisory Committee on Immunization Practices] that would come from a booster shot.” Dr. Swann is department head and A. Doug Allison Distinguished Professor at North Carolina State University and an adjunct professor in the joint department of biomedical engineering at the University of North Carolina at Chapel Hill.
Rising importance of breakthrough cases
Also on Aug. 18, news emerged that breakthrough cases are on the rise in seven U.S. states, likely because of the Delta variant.
These SARS-CoV-2 infections among the fully vaccinated account for 20% of cases in six of the seven states cited in a New York Times report, for example. Researchers also suggested that hospitalization and deaths associated with breakthrough cases could be higher than previously appreciated.
“It is expected that over time we will see more cases of Delta variant infections among vaccinated people. This points toward the need for booster vaccines and/or eventual modifications to the vaccine to capture new variants in the future,” Juan Wisnivesky, MD, DrPH, chief of the division of general internal medicine at Mount Sinai Health System in New York City, said during the briefing.
Vaccine comparisons unfair?
Following the release of a Mayo Clinic study reporting lower effectiveness of the Pfizer mRNA vaccine at 42% versus 76% for the Moderna product, some people started asking if one vaccine was better than the other.
“To begin with, the vaccines are not being compared side-by-side,” Dr. Wisnivesky said. “So we only know the effectiveness of each vaccine versus placebo, but we don’t know one versus the other.”
He added that different study designs, different populations, and other factors make direct comparisons difficult.
More evidence will be needed, Dr. Wisnivesky said, before public health officials can recommend that someone who received one mRNA vaccine switch to another for their booster shot.
Layering protections
Continuing to recommend masks is essential, Dr. Swann added. “With this Delta variant, it does appear that the possibility of reinfection or of a disease case breaking through vaccination can occur. So that makes it even more important to consider using nonpharmaceutical interventions while we continue to vaccinate people.”
Wearing or not wearing a mask is one of the behaviors that drive the transmission of disease, Dr. Swann said.
“What we saw across the board is that many people really wanted to go back to normal as much as they could. And we went back to normal a little bit too soon, especially given this new version of the virus that was circulating,” she said.
In poll, most favor boosters
A recent poll conducted by Medscape indicates that a majority of vaccinated physicians and nurses are ready and willing to take a COVID-19 booster vaccine. For example, 93% of 943 doctors and 87% of 1,680 nurses who responded want booster shots, either immediately or when they are authorized and recommended.
Among 510 WebMD readers responding to a similar poll, 82% indicated they wanted a booster shot.
A challenging task lies ahead
According to CDC data, as of Aug. 18, 2021, almost 169 million Americans are fully vaccinated, including the one-shot Johnson & Johnson adenovirus vaccine.
“I think it will be a challenge to get everyone who is fully vaccinated to come in for that booster,” Dr. Swann said.
Logistically speaking, Dr. Swann explained that many sites that were open for initial vaccinations, including drive-up locations and 24/7 vaccination sites, are no longer operating.
“We might see that rollout look a little bit differently. You might be able to go to your pharmacy or go to your primary care physician,” she said.
“But we may not see as many weekend events so it is going to be easier to get some people a booster than others.
“One interesting thing will also be whether a booster is effective in actually preventing you from giving a disease to someone else,” Dr. Swann said. “That could make a difference as well, because that might play into whether companies, hospitals, universities, or others require a booster.”
A version of this article first appeared on Medscape.com.
Following the White House administration’s announcement to start booster COVID-19 vaccinations for American adults in September, experts weighed in on the evidence for choosing an 8-month cutoff, how breakthrough infections figure in, and why calling one mRNA vaccine better than the other could be misleading.
Timing came up more than once at the Aug. 18 White House briefing announcing the booster plans. Reporters asked about the start time of Sept. 20 and people waiting at least 8 months after their second mRNA vaccine dose to get a booster.
Anthony Fauci, MD, chief medical adviser to the president and director of the National Institute of Allergy and Infectious Diseases, explained that late September gives the United States time to set up the logistics.
Centers for Disease Control and Prevention Director Rochelle Walensky, MD, MPH, added that 8 months is in part based on data from Israel and other countries on the waning of vaccine effectiveness over time.
“It is possible that 8 [months] is associated with the amount of time that we’ve been able to follow large groups of people, especially those who are 65 and older,” Julie Swann, PhD, said during a subsequent media briefing sponsored by Newswise on Aug. 18. “I know that Pfizer has said that they think a booster sometime between 6 and 12 months would be reasonable.”
Dr. Swann supported the administration’s booster shots plan. She said it is important “that we continue to get people the full amount of protection if it’s recommended by CDC and ACIP [Advisory Committee on Immunization Practices] that would come from a booster shot.” Dr. Swann is department head and A. Doug Allison Distinguished Professor at North Carolina State University and an adjunct professor in the joint department of biomedical engineering at the University of North Carolina at Chapel Hill.
Rising importance of breakthrough cases
Also on Aug. 18, news emerged that breakthrough cases are on the rise in seven U.S. states, likely because of the Delta variant.
These SARS-CoV-2 infections among the fully vaccinated account for 20% of cases in six of the seven states cited in a New York Times report, for example. Researchers also suggested that hospitalization and deaths associated with breakthrough cases could be higher than previously appreciated.
“It is expected that over time we will see more cases of Delta variant infections among vaccinated people. This points toward the need for booster vaccines and/or eventual modifications to the vaccine to capture new variants in the future,” Juan Wisnivesky, MD, DrPH, chief of the division of general internal medicine at Mount Sinai Health System in New York City, said during the briefing.
Vaccine comparisons unfair?
Following the release of a Mayo Clinic study reporting lower effectiveness of the Pfizer mRNA vaccine at 42% versus 76% for the Moderna product, some people started asking if one vaccine was better than the other.
“To begin with, the vaccines are not being compared side-by-side,” Dr. Wisnivesky said. “So we only know the effectiveness of each vaccine versus placebo, but we don’t know one versus the other.”
He added that different study designs, different populations, and other factors make direct comparisons difficult.
More evidence will be needed, Dr. Wisnivesky said, before public health officials can recommend that someone who received one mRNA vaccine switch to another for their booster shot.
Layering protections
Continuing to recommend masks is essential, Dr. Swann added. “With this Delta variant, it does appear that the possibility of reinfection or of a disease case breaking through vaccination can occur. So that makes it even more important to consider using nonpharmaceutical interventions while we continue to vaccinate people.”
Wearing or not wearing a mask is one of the behaviors that drive the transmission of disease, Dr. Swann said.
“What we saw across the board is that many people really wanted to go back to normal as much as they could. And we went back to normal a little bit too soon, especially given this new version of the virus that was circulating,” she said.
In poll, most favor boosters
A recent poll conducted by Medscape indicates that a majority of vaccinated physicians and nurses are ready and willing to take a COVID-19 booster vaccine. For example, 93% of 943 doctors and 87% of 1,680 nurses who responded want booster shots, either immediately or when they are authorized and recommended.
Among 510 WebMD readers responding to a similar poll, 82% indicated they wanted a booster shot.
A challenging task lies ahead
According to CDC data, as of Aug. 18, 2021, almost 169 million Americans are fully vaccinated, including the one-shot Johnson & Johnson adenovirus vaccine.
“I think it will be a challenge to get everyone who is fully vaccinated to come in for that booster,” Dr. Swann said.
Logistically speaking, Dr. Swann explained that many sites that were open for initial vaccinations, including drive-up locations and 24/7 vaccination sites, are no longer operating.
“We might see that rollout look a little bit differently. You might be able to go to your pharmacy or go to your primary care physician,” she said.
“But we may not see as many weekend events so it is going to be easier to get some people a booster than others.
“One interesting thing will also be whether a booster is effective in actually preventing you from giving a disease to someone else,” Dr. Swann said. “That could make a difference as well, because that might play into whether companies, hospitals, universities, or others require a booster.”
A version of this article first appeared on Medscape.com.
Annular lesions

This patient was given a diagnosis of disseminated granuloma annulare (DGA). While granuloma annulare usually manifests as a single lesion with a raised erythematous border (often with central pallor or hypopigmentation) it can also manifest as multiple large annular lesions on the extremities and occasionally the trunk, as was seen with this case of DGA.
Although the etiology of DGA is unknown, infections including HIV and hepatitis have been reported as possible triggers. Laboratory testing should be considered if the history or physical examination raises suspicion for either condition. Diabetes has also been associated with the disseminated form and the literature suggests a connection with autoimmune diseases of the liver and thyroid.1
Watchful waiting is usually the best treatment for localized disease, which can spontaneously regress within a year and is usually asymptomatic. Intralesional steroid injections into the raised annulus are more effective than topical steroids, as the effects of the topical steroids are sometimes augmented by occlusion.
Multiple treatments have been proposed for DGA, including UVA treatments, systemic retinoids, doxycycline, and hydroxychloroquine.1 Unfortunately, the disseminated form can persist for many years—even with treatment.
Due to the extent of the lesions, the patient in this case was not interested in intralesional steroid injections, and she had already tried topical steroids. She was prescribed topical tacrolimus to reduce the highly visible nature of her lesions.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
Beretta-Piccoli BT, Mainetti C, Peeters MA, et al. Cutaneous granulomatosis: a comprehensive review. Clin Rev Allergy Immunol. 2018;54:131-146. doi: 10.1007/s12016-017-8666-8

This patient was given a diagnosis of disseminated granuloma annulare (DGA). While granuloma annulare usually manifests as a single lesion with a raised erythematous border (often with central pallor or hypopigmentation) it can also manifest as multiple large annular lesions on the extremities and occasionally the trunk, as was seen with this case of DGA.
Although the etiology of DGA is unknown, infections including HIV and hepatitis have been reported as possible triggers. Laboratory testing should be considered if the history or physical examination raises suspicion for either condition. Diabetes has also been associated with the disseminated form and the literature suggests a connection with autoimmune diseases of the liver and thyroid.1
Watchful waiting is usually the best treatment for localized disease, which can spontaneously regress within a year and is usually asymptomatic. Intralesional steroid injections into the raised annulus are more effective than topical steroids, as the effects of the topical steroids are sometimes augmented by occlusion.
Multiple treatments have been proposed for DGA, including UVA treatments, systemic retinoids, doxycycline, and hydroxychloroquine.1 Unfortunately, the disseminated form can persist for many years—even with treatment.
Due to the extent of the lesions, the patient in this case was not interested in intralesional steroid injections, and she had already tried topical steroids. She was prescribed topical tacrolimus to reduce the highly visible nature of her lesions.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.

This patient was given a diagnosis of disseminated granuloma annulare (DGA). While granuloma annulare usually manifests as a single lesion with a raised erythematous border (often with central pallor or hypopigmentation) it can also manifest as multiple large annular lesions on the extremities and occasionally the trunk, as was seen with this case of DGA.
Although the etiology of DGA is unknown, infections including HIV and hepatitis have been reported as possible triggers. Laboratory testing should be considered if the history or physical examination raises suspicion for either condition. Diabetes has also been associated with the disseminated form and the literature suggests a connection with autoimmune diseases of the liver and thyroid.1
Watchful waiting is usually the best treatment for localized disease, which can spontaneously regress within a year and is usually asymptomatic. Intralesional steroid injections into the raised annulus are more effective than topical steroids, as the effects of the topical steroids are sometimes augmented by occlusion.
Multiple treatments have been proposed for DGA, including UVA treatments, systemic retinoids, doxycycline, and hydroxychloroquine.1 Unfortunately, the disseminated form can persist for many years—even with treatment.
Due to the extent of the lesions, the patient in this case was not interested in intralesional steroid injections, and she had already tried topical steroids. She was prescribed topical tacrolimus to reduce the highly visible nature of her lesions.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
Beretta-Piccoli BT, Mainetti C, Peeters MA, et al. Cutaneous granulomatosis: a comprehensive review. Clin Rev Allergy Immunol. 2018;54:131-146. doi: 10.1007/s12016-017-8666-8
Beretta-Piccoli BT, Mainetti C, Peeters MA, et al. Cutaneous granulomatosis: a comprehensive review. Clin Rev Allergy Immunol. 2018;54:131-146. doi: 10.1007/s12016-017-8666-8
The hateful patient
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
A 64-year-old White woman with very few medical problems complains of bug bites. She had seen no bugs and had no visible bites. There is no rash. “So what bit me?” she asked, pulling her mask down for emphasis. How should I know? I thought, but didn’t say. She and I have been through this many times.
Before I could respond, she filled the pause with her usual complaints including how hard it is to get an appointment with me and how every appointment with me is a waste of her time. Ignoring the contradistinction of her charges, I took some satisfaction realizing she has just given me a topic to write about: The hateful patient.
They are frustrating, troublesome, rude, sometimes racist, misogynistic, depressing, hopeless, and disheartening. They call you, email you, and come to see you just to annoy you (so it seems). And they’re everywhere. According to one study, nearly one in six are “difficult patients.” It feels like more lately because the vaccine has brought haters back into clinic, just to get us.
But hateful patients aren’t new. In 1978, James E. Groves, MD, a Harvard psychiatrist, wrote a now-classic New England Journal of Medicine article about them called: Taking Care of the Hateful Patient. Even Osler, back in 1889, covered these patients in his lecture to University of Pennsylvania students, advising us to “deal gently with this deliciously credulous old human nature in which we work ... restrain your indignation.” But like much of Osler’s advice, it is easier said than done.
Dr. Groves is more helpful, and presents a model to understand them. Difficult patients, as we’d now call them, fall into four stereotypes: dependent clingers, entitled demanders, manipulative help-rejectors, and self-destructive deniers. It’s Dr. Groves’s bottom line I found insightful. He says that, when patients create negative feelings in us, we’re more likely to make errors. He then gives sound advice: Set firm boundaries and learn to counter the countertransference these patients provoke. Don’t disavow or discharge, Dr. Groves advises, redirect these emotions to motivate you to dig deeper. There you’ll find clinical data that will facilitate understanding and enable better patient management. Yes, easier said.
In addition to Dr. Groves’s analysis of how we harm these patients, I’d add that these disagreeable, malingering patients also harm us doctors. The hangover from a difficult patient encounter can linger for several appointments later or, worse, carryover to home. And now with patient emails proliferating, demanding patients behave as if we have an inexhaustible ability to engage them. We don’t. Many physicians are struggling to care at all; their low empathy battery warnings are blinking red, less than 1% remaining.
What is toxic to us doctors is the maelstrom of cognitive dissonance these patients create in us. Have you ever felt relief to learn a difficult patient has “finally” died? How could we think such a thing?! Didn’t we choose medicine instead of Wall Street because we care about people? But manipulative patients can make us care less. We even use secret language with each other to protect ourselves from them, those GOMERs (get out of my emergency room), bouncebacks, patients with status dramaticus, and those ornery FTDs (failure to die). Save yourself, we say to each other, this patient will kill you.
Caring for my somatizing 64-year-old patient has been difficult, but writing this has helped me reframe our interaction. Unsurprisingly, at the end of her failed visit she asked when she could see me again. “I need to schedule now because I have to find a neighbor to watch my dogs. It takes two buses to come here and I can’t take them with me.” Ah, there’s the clinical data Dr. Groves said I’d find – she’s not here to hurt me, she’s here because I’m all she’s got. At least for this difficult patient, I have a plan. At the bottom of my note I type “RTC 3 mo.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Microbiome: Gut dysbiosis linked to development of alopecia areata
presented at the annual meeting of the Society for Investigative Dermatology.
There have been reports of gut microbiome dysbiosis associated with autoimmune diseases such as rheumatoid arthritis, diabetes, and celiac disease. “It is now clear that these events not just shape the immune response in the gut, but also distant sites and immune-privileged organs,” Tanya Sezin, a doctor of natural science from the University of Lübeck (Germany) and Columbia University, New York, said in her presentation.
Whether the gut microbiome may also play a role as an environmental factor in alopecia areata, another T-cell–mediated autoimmune disease for which there are few available treatment options, is being evaluated at the Christiano Laboratory at Columbia University, Dr. Sezin noted. “Much of the difficulty underlying the lack of an effective treatment has been the incomplete understanding of the pathogenesis of AA.”
She also referred to several case reports describing hair growth in patients who received fecal microbiota transplantation (FMT), including a 20-year-old with alopecia universalis, who experienced hair growth after receiving FMT for Crohn’s disease.
Dr. Sezin and colleagues at the lab first performed a study in mice to test whether the gut microbiome was involved in the pathogenesis of AA. Mice given an antibiotic cocktail of ampicillin, neomycin, and vancomycin prior to or at the time of a skin graft taken from a mouse model of AA to induce AA were protected from hair loss, while mice given the antibiotic cocktail after skin grafting were not protected from hair loss.
“16S rRNA sequencing analysis of the gut microbiota revealed a significant shift in gut microbiome composition in animals treated with antibiotics and protected from hair loss, as reflected by significant changes in alpha and beta diversity,” Dr. Sezin explained. “In AA mice, we also observed differential abundance of families from the Bacteroidetes and Firmicutes phyla.” Specifically, Lactobacillus murinus and Muribaculum intestinale were overrepresented in mice with AA.
The investigators then performed 16S rRNA sequencing on 26 patients with AA, who stopped treatment for 30 days beforehand, and 9 participants who did not have AA as controls. “Though we did not observe difference in alpha and beta diversity, we see changes in the relative abundance of several families belonging to the Firmicutes phyla,” in patients with AA, Dr. Sezin said.
In another cohort of 30 patients with AA and 20 participants without AA, who stopped treatment before the study, Dr. Sezin and colleagues found “differences in the relative abundance of members of the Firmicutes and Bacteroides phyla,” including Bacteroides caccae, Prevotella copri, Syntrophomonas wolfei, Blautia wexlerae, and Eubacterium eligens, she said. “Consistent with our findings, there are previous reports in the literature showing gut dysbiosis in several other autoimmune diseases associated with differential regulation of some of the top species we have identified.”
Dr. Sezin said her group is recruiting patients for a clinical trial evaluating FMT in patients with AA. “We plan to study the association between changes in the gut microbiome and immune cell composition in AA patients undergoing FMT,” she said. “Additionally, functional studies in mice are also currently [being conducted] to further pinpoint the contribution of gut microbiome to the pathogenesis of AA.”
When asked during the discussion session if there was any relationship between the skin microbiome and AA, Dr. Sezin said there was no connection found in mice studies, which she and her colleagues are investigating further. “In the human samples, we are currently recruiting more patients and healthy controls to try to get a better understanding of whether we see differences in the skin microbiome,” she added.
Dr. Sezin explained that how the gut microbiota “is really remediated in alopecia areata” is not well understood. “We think that it is possible that we see intestinal permeability in the gut due to the gut dysbiosis that we see in alopecia areata patients, and this might lead to systemic distribution of bacteria, which might cross-react or present cross reactivity with the antigens” identified in AA, which is also being investigated, she said.
FMT not a ‘simple fix’ for AA
Leslie Castelo-Soccio, MD, PhD, a dermatologist at the Children’s Hospital of Philadelphia, who was not involved with the research, said in an interview that the findings presented by Dr. Sezin show how AA shares similarities with other autoimmune diseases. “It does highlight how important the gut microbiome is to human disease, and that differences in relative abundance of bacteria play one part as a trigger in a genetically susceptible person.”
However, while some autoimmune diseases have a big difference in alpha and beta diversity, for example, “this has not been seen in people with alopecia areata,” Dr. Castelo-Soccio pointed out. “The differences are more subtle in terms of amounts of certain bacteria,” she said, noting that, in this study, the biggest differences were seen in the studies of mice.
Dr. Castelo-Soccio also said there may be also be differences in the gut microbiome in children and adults. “The gut microbiome shifts in very early childhood from a very diverse microbiome to a more ‘adult microbiome’ around age 4, which is the age we see the first peak of many autoimmune diseases, including alopecia areata. I think microbiome work in humans needs to focus on this transition point.”
As for the clinical trial at Columbia that is evaluating FMT in patients with AA, Dr. Castelo-Soccio said she is excited. “There is much to learn about fecal transplant for all diseases and about the role of the gut microbiome and environment. Most of what we know for fecal transplant centers on its use for Clostridium difficile infections.”
Patients and their families have been asking about the potential for FMT in alopecia area, Dr. Castelo-Soccio said, but some believe it is a “simple fix” when the reality is much more complex.
“When I speak to patients and families about this, I explain that currently the ‘active ingredient’ in fecal transplants is not definitively established. In any one donor, the community of bacteria is highly variable and can be from batch to batch. While the short-term risks are relatively low – cramping, diarrhea, discomfort, mode of delivery – there are reports of transmission of infectious bacteria from donors like [Escherichia] coli, which have led to severe infections.”
Long-term safety and durability of effects are also unclear, “so we do not know if a patient receiving one [FMT] will need many in the future. We do not know how changing the microbiome could affect the transplant recipient in terms of noninfectious diseases/disorders. We are learning about the role of microbiome in obesity, insulin resistance, mood disorders. We could be ‘fixing’ one trigger of alopecia but setting up [the] patient for other noninfectious conditions,” Dr. Castelo-Soccio said.
Dr. Sezin and Dr. Castelo-Soccio reported no relevant financial disclosures.
presented at the annual meeting of the Society for Investigative Dermatology.
There have been reports of gut microbiome dysbiosis associated with autoimmune diseases such as rheumatoid arthritis, diabetes, and celiac disease. “It is now clear that these events not just shape the immune response in the gut, but also distant sites and immune-privileged organs,” Tanya Sezin, a doctor of natural science from the University of Lübeck (Germany) and Columbia University, New York, said in her presentation.
Whether the gut microbiome may also play a role as an environmental factor in alopecia areata, another T-cell–mediated autoimmune disease for which there are few available treatment options, is being evaluated at the Christiano Laboratory at Columbia University, Dr. Sezin noted. “Much of the difficulty underlying the lack of an effective treatment has been the incomplete understanding of the pathogenesis of AA.”
She also referred to several case reports describing hair growth in patients who received fecal microbiota transplantation (FMT), including a 20-year-old with alopecia universalis, who experienced hair growth after receiving FMT for Crohn’s disease.
Dr. Sezin and colleagues at the lab first performed a study in mice to test whether the gut microbiome was involved in the pathogenesis of AA. Mice given an antibiotic cocktail of ampicillin, neomycin, and vancomycin prior to or at the time of a skin graft taken from a mouse model of AA to induce AA were protected from hair loss, while mice given the antibiotic cocktail after skin grafting were not protected from hair loss.
“16S rRNA sequencing analysis of the gut microbiota revealed a significant shift in gut microbiome composition in animals treated with antibiotics and protected from hair loss, as reflected by significant changes in alpha and beta diversity,” Dr. Sezin explained. “In AA mice, we also observed differential abundance of families from the Bacteroidetes and Firmicutes phyla.” Specifically, Lactobacillus murinus and Muribaculum intestinale were overrepresented in mice with AA.
The investigators then performed 16S rRNA sequencing on 26 patients with AA, who stopped treatment for 30 days beforehand, and 9 participants who did not have AA as controls. “Though we did not observe difference in alpha and beta diversity, we see changes in the relative abundance of several families belonging to the Firmicutes phyla,” in patients with AA, Dr. Sezin said.
In another cohort of 30 patients with AA and 20 participants without AA, who stopped treatment before the study, Dr. Sezin and colleagues found “differences in the relative abundance of members of the Firmicutes and Bacteroides phyla,” including Bacteroides caccae, Prevotella copri, Syntrophomonas wolfei, Blautia wexlerae, and Eubacterium eligens, she said. “Consistent with our findings, there are previous reports in the literature showing gut dysbiosis in several other autoimmune diseases associated with differential regulation of some of the top species we have identified.”
Dr. Sezin said her group is recruiting patients for a clinical trial evaluating FMT in patients with AA. “We plan to study the association between changes in the gut microbiome and immune cell composition in AA patients undergoing FMT,” she said. “Additionally, functional studies in mice are also currently [being conducted] to further pinpoint the contribution of gut microbiome to the pathogenesis of AA.”
When asked during the discussion session if there was any relationship between the skin microbiome and AA, Dr. Sezin said there was no connection found in mice studies, which she and her colleagues are investigating further. “In the human samples, we are currently recruiting more patients and healthy controls to try to get a better understanding of whether we see differences in the skin microbiome,” she added.
Dr. Sezin explained that how the gut microbiota “is really remediated in alopecia areata” is not well understood. “We think that it is possible that we see intestinal permeability in the gut due to the gut dysbiosis that we see in alopecia areata patients, and this might lead to systemic distribution of bacteria, which might cross-react or present cross reactivity with the antigens” identified in AA, which is also being investigated, she said.
FMT not a ‘simple fix’ for AA
Leslie Castelo-Soccio, MD, PhD, a dermatologist at the Children’s Hospital of Philadelphia, who was not involved with the research, said in an interview that the findings presented by Dr. Sezin show how AA shares similarities with other autoimmune diseases. “It does highlight how important the gut microbiome is to human disease, and that differences in relative abundance of bacteria play one part as a trigger in a genetically susceptible person.”
However, while some autoimmune diseases have a big difference in alpha and beta diversity, for example, “this has not been seen in people with alopecia areata,” Dr. Castelo-Soccio pointed out. “The differences are more subtle in terms of amounts of certain bacteria,” she said, noting that, in this study, the biggest differences were seen in the studies of mice.
Dr. Castelo-Soccio also said there may be also be differences in the gut microbiome in children and adults. “The gut microbiome shifts in very early childhood from a very diverse microbiome to a more ‘adult microbiome’ around age 4, which is the age we see the first peak of many autoimmune diseases, including alopecia areata. I think microbiome work in humans needs to focus on this transition point.”
As for the clinical trial at Columbia that is evaluating FMT in patients with AA, Dr. Castelo-Soccio said she is excited. “There is much to learn about fecal transplant for all diseases and about the role of the gut microbiome and environment. Most of what we know for fecal transplant centers on its use for Clostridium difficile infections.”
Patients and their families have been asking about the potential for FMT in alopecia area, Dr. Castelo-Soccio said, but some believe it is a “simple fix” when the reality is much more complex.
“When I speak to patients and families about this, I explain that currently the ‘active ingredient’ in fecal transplants is not definitively established. In any one donor, the community of bacteria is highly variable and can be from batch to batch. While the short-term risks are relatively low – cramping, diarrhea, discomfort, mode of delivery – there are reports of transmission of infectious bacteria from donors like [Escherichia] coli, which have led to severe infections.”
Long-term safety and durability of effects are also unclear, “so we do not know if a patient receiving one [FMT] will need many in the future. We do not know how changing the microbiome could affect the transplant recipient in terms of noninfectious diseases/disorders. We are learning about the role of microbiome in obesity, insulin resistance, mood disorders. We could be ‘fixing’ one trigger of alopecia but setting up [the] patient for other noninfectious conditions,” Dr. Castelo-Soccio said.
Dr. Sezin and Dr. Castelo-Soccio reported no relevant financial disclosures.
presented at the annual meeting of the Society for Investigative Dermatology.
There have been reports of gut microbiome dysbiosis associated with autoimmune diseases such as rheumatoid arthritis, diabetes, and celiac disease. “It is now clear that these events not just shape the immune response in the gut, but also distant sites and immune-privileged organs,” Tanya Sezin, a doctor of natural science from the University of Lübeck (Germany) and Columbia University, New York, said in her presentation.
Whether the gut microbiome may also play a role as an environmental factor in alopecia areata, another T-cell–mediated autoimmune disease for which there are few available treatment options, is being evaluated at the Christiano Laboratory at Columbia University, Dr. Sezin noted. “Much of the difficulty underlying the lack of an effective treatment has been the incomplete understanding of the pathogenesis of AA.”
She also referred to several case reports describing hair growth in patients who received fecal microbiota transplantation (FMT), including a 20-year-old with alopecia universalis, who experienced hair growth after receiving FMT for Crohn’s disease.
Dr. Sezin and colleagues at the lab first performed a study in mice to test whether the gut microbiome was involved in the pathogenesis of AA. Mice given an antibiotic cocktail of ampicillin, neomycin, and vancomycin prior to or at the time of a skin graft taken from a mouse model of AA to induce AA were protected from hair loss, while mice given the antibiotic cocktail after skin grafting were not protected from hair loss.
“16S rRNA sequencing analysis of the gut microbiota revealed a significant shift in gut microbiome composition in animals treated with antibiotics and protected from hair loss, as reflected by significant changes in alpha and beta diversity,” Dr. Sezin explained. “In AA mice, we also observed differential abundance of families from the Bacteroidetes and Firmicutes phyla.” Specifically, Lactobacillus murinus and Muribaculum intestinale were overrepresented in mice with AA.
The investigators then performed 16S rRNA sequencing on 26 patients with AA, who stopped treatment for 30 days beforehand, and 9 participants who did not have AA as controls. “Though we did not observe difference in alpha and beta diversity, we see changes in the relative abundance of several families belonging to the Firmicutes phyla,” in patients with AA, Dr. Sezin said.
In another cohort of 30 patients with AA and 20 participants without AA, who stopped treatment before the study, Dr. Sezin and colleagues found “differences in the relative abundance of members of the Firmicutes and Bacteroides phyla,” including Bacteroides caccae, Prevotella copri, Syntrophomonas wolfei, Blautia wexlerae, and Eubacterium eligens, she said. “Consistent with our findings, there are previous reports in the literature showing gut dysbiosis in several other autoimmune diseases associated with differential regulation of some of the top species we have identified.”
Dr. Sezin said her group is recruiting patients for a clinical trial evaluating FMT in patients with AA. “We plan to study the association between changes in the gut microbiome and immune cell composition in AA patients undergoing FMT,” she said. “Additionally, functional studies in mice are also currently [being conducted] to further pinpoint the contribution of gut microbiome to the pathogenesis of AA.”
When asked during the discussion session if there was any relationship between the skin microbiome and AA, Dr. Sezin said there was no connection found in mice studies, which she and her colleagues are investigating further. “In the human samples, we are currently recruiting more patients and healthy controls to try to get a better understanding of whether we see differences in the skin microbiome,” she added.
Dr. Sezin explained that how the gut microbiota “is really remediated in alopecia areata” is not well understood. “We think that it is possible that we see intestinal permeability in the gut due to the gut dysbiosis that we see in alopecia areata patients, and this might lead to systemic distribution of bacteria, which might cross-react or present cross reactivity with the antigens” identified in AA, which is also being investigated, she said.
FMT not a ‘simple fix’ for AA
Leslie Castelo-Soccio, MD, PhD, a dermatologist at the Children’s Hospital of Philadelphia, who was not involved with the research, said in an interview that the findings presented by Dr. Sezin show how AA shares similarities with other autoimmune diseases. “It does highlight how important the gut microbiome is to human disease, and that differences in relative abundance of bacteria play one part as a trigger in a genetically susceptible person.”
However, while some autoimmune diseases have a big difference in alpha and beta diversity, for example, “this has not been seen in people with alopecia areata,” Dr. Castelo-Soccio pointed out. “The differences are more subtle in terms of amounts of certain bacteria,” she said, noting that, in this study, the biggest differences were seen in the studies of mice.
Dr. Castelo-Soccio also said there may be also be differences in the gut microbiome in children and adults. “The gut microbiome shifts in very early childhood from a very diverse microbiome to a more ‘adult microbiome’ around age 4, which is the age we see the first peak of many autoimmune diseases, including alopecia areata. I think microbiome work in humans needs to focus on this transition point.”
As for the clinical trial at Columbia that is evaluating FMT in patients with AA, Dr. Castelo-Soccio said she is excited. “There is much to learn about fecal transplant for all diseases and about the role of the gut microbiome and environment. Most of what we know for fecal transplant centers on its use for Clostridium difficile infections.”
Patients and their families have been asking about the potential for FMT in alopecia area, Dr. Castelo-Soccio said, but some believe it is a “simple fix” when the reality is much more complex.
“When I speak to patients and families about this, I explain that currently the ‘active ingredient’ in fecal transplants is not definitively established. In any one donor, the community of bacteria is highly variable and can be from batch to batch. While the short-term risks are relatively low – cramping, diarrhea, discomfort, mode of delivery – there are reports of transmission of infectious bacteria from donors like [Escherichia] coli, which have led to severe infections.”
Long-term safety and durability of effects are also unclear, “so we do not know if a patient receiving one [FMT] will need many in the future. We do not know how changing the microbiome could affect the transplant recipient in terms of noninfectious diseases/disorders. We are learning about the role of microbiome in obesity, insulin resistance, mood disorders. We could be ‘fixing’ one trigger of alopecia but setting up [the] patient for other noninfectious conditions,” Dr. Castelo-Soccio said.
Dr. Sezin and Dr. Castelo-Soccio reported no relevant financial disclosures.
FROM SID 2021
COVID-19 booster shots to start in September: Officials
at a press briefing August 18.
Those who received the Pfizer-BioNTech and Moderna vaccines would be eligible to get a booster shot 8 months after they received the second dose of those vaccines, officials said. Information on boosters for those who got the one-dose Johnson & Johnson vaccine will be forthcoming.
“We anticipate a booster will [also] likely be needed,” said U.S. Surgeon General Vivek Murthy, MD. The J&J vaccine was not available in the U.S. until March, he said, and ‘’we expect more data on J&J in the coming weeks, so that plan is coming.”
The plan for boosters for the two mRNA vaccines is pending the FDA’s conducting of an independent review and authorizing the third dose of the Moderna and Pfizer-BioNTech vaccines, as well as an advisory committee of the CDC making the recommendation.
“We know that even highly effective vaccines become less effective over time,” Dr. Murthy said. “Having reviewed the most current data, it is now our clinical judgment that the time to lay out a plan for the COVID-19 boosters is now.”
Research released Aug. 18 shows waning effectiveness of the two mRNA vaccines.
At the briefing, Dr. Murthy and others continually reassured listeners that while effectiveness against infection declines, the vaccines continue to protect against severe infections, hospitalizations, and death.
“If you are fully vaccinated, you still have a high degree of protection against the worst outcomes,” Dr. Murthy said.
Data driving the plan
CDC Director Rochelle Walensky, MD, cited three research studies published Aug. 18 in the CDC’s Morbidity and Mortality Weekly Report that helped to drive the decision to recommend boosters.
Analysis of nursing home COVID-19 data from the CDC’s National Healthcare Safety Network showed a significant decline in the effectiveness of the full mRNA vaccine against lab-confirmed COVID-19 infection, from 74.7% before the Delta variant (March 1-May 9, 2021) to 53% when the Delta variant became predominant in the United States. The analysis during the Delta dominant period included 85,000 weekly reports from nearly 15,000 facilities.
Another study looked at more than 10 million New York adults who had been fully vaccinated with either the Moderna, Pfizer, or J&J vaccine by July 25. During the period from May 3 to July 25, overall, the age-adjusted vaccine effectiveness against infection decreased from 91.7% to 79.8%.
Vaccine effectiveness against hospitalization remains high, another study found. An analysis of 1,129 patients who had gotten two doses of an mRNA vaccine showed vaccine effectiveness against hospitalization after 24 weeks. It was 86% at weeks 2-12 and 84% at weeks 13-24.
Immunologic facts
Immunologic information also points to the need for a booster, said Anthony Fauci, MD, the chief medical advisor to the president and director of the National Institute of Allergy and Infectious Diseases.
“Antibody levels decline over time,” he said, “and higher antibody levels are associated with higher efficacy of the vaccine. Higher levels of antibody may be needed to protect against Delta.”
A booster increased antibody levels by ‘’at least tenfold and possibly more,” he said. And higher levels of antibody may be required to protect against Delta. Taken together, he said, the data support the use of a booster to increase the overall level of protection.
Booster details
“We will make sure it is convenient and easy to get the booster shot,” said Jeff Zients, the White House COVID-19 response coordinator. As with the previous immunization, he said, the booster will be free, and no one will be asked about immigration status.
The plan for booster shots is an attempt to stay ahead of the virus, officials stressed
Big picture
Not everyone agrees with the booster dose idea. At a World Health Organization briefing Aug. 18, WHO’s Chief Scientist Soumya Swaminathan, MD, an Indian pediatrician, said that the right thing to do right now ‘’is to wait for the science to tell us when boosters, which groups of people, and which vaccines need boosters.”
Like others, she also broached the ‘’moral and ethical argument of giving people third doses, when they’re already well protected and while the rest of the world is waiting for their primary immunization.”
Dr. Swaminathan does see a role for boosters to protect immunocompromised people but noted that ‘’that’s a small number of people.” Widespread boosters ‘’will only lead to more variants, to more escape variants, and perhaps we’re heading into more dire situations.”
A version of this article first appeared on WebMD.com.
at a press briefing August 18.
Those who received the Pfizer-BioNTech and Moderna vaccines would be eligible to get a booster shot 8 months after they received the second dose of those vaccines, officials said. Information on boosters for those who got the one-dose Johnson & Johnson vaccine will be forthcoming.
“We anticipate a booster will [also] likely be needed,” said U.S. Surgeon General Vivek Murthy, MD. The J&J vaccine was not available in the U.S. until March, he said, and ‘’we expect more data on J&J in the coming weeks, so that plan is coming.”
The plan for boosters for the two mRNA vaccines is pending the FDA’s conducting of an independent review and authorizing the third dose of the Moderna and Pfizer-BioNTech vaccines, as well as an advisory committee of the CDC making the recommendation.
“We know that even highly effective vaccines become less effective over time,” Dr. Murthy said. “Having reviewed the most current data, it is now our clinical judgment that the time to lay out a plan for the COVID-19 boosters is now.”
Research released Aug. 18 shows waning effectiveness of the two mRNA vaccines.
At the briefing, Dr. Murthy and others continually reassured listeners that while effectiveness against infection declines, the vaccines continue to protect against severe infections, hospitalizations, and death.
“If you are fully vaccinated, you still have a high degree of protection against the worst outcomes,” Dr. Murthy said.
Data driving the plan
CDC Director Rochelle Walensky, MD, cited three research studies published Aug. 18 in the CDC’s Morbidity and Mortality Weekly Report that helped to drive the decision to recommend boosters.
Analysis of nursing home COVID-19 data from the CDC’s National Healthcare Safety Network showed a significant decline in the effectiveness of the full mRNA vaccine against lab-confirmed COVID-19 infection, from 74.7% before the Delta variant (March 1-May 9, 2021) to 53% when the Delta variant became predominant in the United States. The analysis during the Delta dominant period included 85,000 weekly reports from nearly 15,000 facilities.
Another study looked at more than 10 million New York adults who had been fully vaccinated with either the Moderna, Pfizer, or J&J vaccine by July 25. During the period from May 3 to July 25, overall, the age-adjusted vaccine effectiveness against infection decreased from 91.7% to 79.8%.
Vaccine effectiveness against hospitalization remains high, another study found. An analysis of 1,129 patients who had gotten two doses of an mRNA vaccine showed vaccine effectiveness against hospitalization after 24 weeks. It was 86% at weeks 2-12 and 84% at weeks 13-24.
Immunologic facts
Immunologic information also points to the need for a booster, said Anthony Fauci, MD, the chief medical advisor to the president and director of the National Institute of Allergy and Infectious Diseases.
“Antibody levels decline over time,” he said, “and higher antibody levels are associated with higher efficacy of the vaccine. Higher levels of antibody may be needed to protect against Delta.”
A booster increased antibody levels by ‘’at least tenfold and possibly more,” he said. And higher levels of antibody may be required to protect against Delta. Taken together, he said, the data support the use of a booster to increase the overall level of protection.
Booster details
“We will make sure it is convenient and easy to get the booster shot,” said Jeff Zients, the White House COVID-19 response coordinator. As with the previous immunization, he said, the booster will be free, and no one will be asked about immigration status.
The plan for booster shots is an attempt to stay ahead of the virus, officials stressed
Big picture
Not everyone agrees with the booster dose idea. At a World Health Organization briefing Aug. 18, WHO’s Chief Scientist Soumya Swaminathan, MD, an Indian pediatrician, said that the right thing to do right now ‘’is to wait for the science to tell us when boosters, which groups of people, and which vaccines need boosters.”
Like others, she also broached the ‘’moral and ethical argument of giving people third doses, when they’re already well protected and while the rest of the world is waiting for their primary immunization.”
Dr. Swaminathan does see a role for boosters to protect immunocompromised people but noted that ‘’that’s a small number of people.” Widespread boosters ‘’will only lead to more variants, to more escape variants, and perhaps we’re heading into more dire situations.”
A version of this article first appeared on WebMD.com.
at a press briefing August 18.
Those who received the Pfizer-BioNTech and Moderna vaccines would be eligible to get a booster shot 8 months after they received the second dose of those vaccines, officials said. Information on boosters for those who got the one-dose Johnson & Johnson vaccine will be forthcoming.
“We anticipate a booster will [also] likely be needed,” said U.S. Surgeon General Vivek Murthy, MD. The J&J vaccine was not available in the U.S. until March, he said, and ‘’we expect more data on J&J in the coming weeks, so that plan is coming.”
The plan for boosters for the two mRNA vaccines is pending the FDA’s conducting of an independent review and authorizing the third dose of the Moderna and Pfizer-BioNTech vaccines, as well as an advisory committee of the CDC making the recommendation.
“We know that even highly effective vaccines become less effective over time,” Dr. Murthy said. “Having reviewed the most current data, it is now our clinical judgment that the time to lay out a plan for the COVID-19 boosters is now.”
Research released Aug. 18 shows waning effectiveness of the two mRNA vaccines.
At the briefing, Dr. Murthy and others continually reassured listeners that while effectiveness against infection declines, the vaccines continue to protect against severe infections, hospitalizations, and death.
“If you are fully vaccinated, you still have a high degree of protection against the worst outcomes,” Dr. Murthy said.
Data driving the plan
CDC Director Rochelle Walensky, MD, cited three research studies published Aug. 18 in the CDC’s Morbidity and Mortality Weekly Report that helped to drive the decision to recommend boosters.
Analysis of nursing home COVID-19 data from the CDC’s National Healthcare Safety Network showed a significant decline in the effectiveness of the full mRNA vaccine against lab-confirmed COVID-19 infection, from 74.7% before the Delta variant (March 1-May 9, 2021) to 53% when the Delta variant became predominant in the United States. The analysis during the Delta dominant period included 85,000 weekly reports from nearly 15,000 facilities.
Another study looked at more than 10 million New York adults who had been fully vaccinated with either the Moderna, Pfizer, or J&J vaccine by July 25. During the period from May 3 to July 25, overall, the age-adjusted vaccine effectiveness against infection decreased from 91.7% to 79.8%.
Vaccine effectiveness against hospitalization remains high, another study found. An analysis of 1,129 patients who had gotten two doses of an mRNA vaccine showed vaccine effectiveness against hospitalization after 24 weeks. It was 86% at weeks 2-12 and 84% at weeks 13-24.
Immunologic facts
Immunologic information also points to the need for a booster, said Anthony Fauci, MD, the chief medical advisor to the president and director of the National Institute of Allergy and Infectious Diseases.
“Antibody levels decline over time,” he said, “and higher antibody levels are associated with higher efficacy of the vaccine. Higher levels of antibody may be needed to protect against Delta.”
A booster increased antibody levels by ‘’at least tenfold and possibly more,” he said. And higher levels of antibody may be required to protect against Delta. Taken together, he said, the data support the use of a booster to increase the overall level of protection.
Booster details
“We will make sure it is convenient and easy to get the booster shot,” said Jeff Zients, the White House COVID-19 response coordinator. As with the previous immunization, he said, the booster will be free, and no one will be asked about immigration status.
The plan for booster shots is an attempt to stay ahead of the virus, officials stressed
Big picture
Not everyone agrees with the booster dose idea. At a World Health Organization briefing Aug. 18, WHO’s Chief Scientist Soumya Swaminathan, MD, an Indian pediatrician, said that the right thing to do right now ‘’is to wait for the science to tell us when boosters, which groups of people, and which vaccines need boosters.”
Like others, she also broached the ‘’moral and ethical argument of giving people third doses, when they’re already well protected and while the rest of the world is waiting for their primary immunization.”
Dr. Swaminathan does see a role for boosters to protect immunocompromised people but noted that ‘’that’s a small number of people.” Widespread boosters ‘’will only lead to more variants, to more escape variants, and perhaps we’re heading into more dire situations.”
A version of this article first appeared on WebMD.com.
Latest data show increase in breakthrough COVID-19 cases
Breakthrough cases accounted for about one in five newly diagnosed cases in six of the states, according to the New York Times. Hospitalizations and deaths among vaccinated people may be higher than previously thought as well.
“Remember when the early vaccine studies came out, it was like nobody gets hospitalized, nobody dies,” Robert Wachter, MD, chairman of the department of medicine at the University of California, San Francisco, said in an interview. “That clearly is not true.”
The New York Times analyzed data in seven states – California, Colorado, Massachusetts, Oregon, Utah, Vermont, and Virginia – that are tracking the most detailed information. The trends in these states may not reflect the numbers throughout the country, the newspaper reported.
Even still, the numbers back up the idea that vaccinated people may need booster shots this fall to support their earlier vaccine doses. Federal health officials are scheduled to approve the extra shots in coming weeks, potentially in September. The first people to receive booster shots will likely be health care workers and nursing home residents who took the first vaccines in December and January.
“If the chances of a breakthrough infection have gone up considerably, and I think the evidence is clear that they have, and the level of protection against severe illness is no longer as robust as it was, I think the case for boosters goes up pretty quickly,” Dr. Wachter said.
Previous analyses of breakthrough cases included data from June and earlier, the newspaper reported. But since July, COVID-19 cases have soared again because of the Delta variant, and the most recent numbers show an uptick among vaccinated people. In Los Angeles County, for instance, fully vaccinated people account for 20% of new COVID-19 cases, which is up from 11% in May, 5% in April, and 2% in March, according to a late July report from the Los Angeles County Department of Public Health.
What’s more, breakthrough infections in the seven states accounted for 12%-24% of COVID-19 hospitalizations in those states. About 8,000 breakthrough hospitalizations have been reported to the CDC. Still, the overall numbers remain low – in California, for instance, about 1,615 people have been hospitalized with breakthrough infections, which accounts for 0.007% of the state’s 22 million vaccinated people, the Times reported.
The breakthrough infections appear to be more severe among vaccinated people who are older or have weakened immune systems. About 74% of breakthrough cases are among adults 65 or older, the CDC reported.
The increase may shift how vaccinated people see their risks for infection and interact with loved ones. Public health officials have suggested that people follow some COVID-19 safety protocols again, such as wearing masks in public indoor spaces regardless of vaccination status.
As the Delta variant continues to circulate this fall, public health researchers will be researching more about breakthrough cases among vaccinated people, including whether they have prolonged symptoms and how easily they may pass the virus to others.
“I think some of us have been challenged by the numbers of clusters that we’ve seen,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, told this news organization.
“I think that really needs to be examined more,” he said.
A version of this article first appeared on WebMD.com.
Breakthrough cases accounted for about one in five newly diagnosed cases in six of the states, according to the New York Times. Hospitalizations and deaths among vaccinated people may be higher than previously thought as well.
“Remember when the early vaccine studies came out, it was like nobody gets hospitalized, nobody dies,” Robert Wachter, MD, chairman of the department of medicine at the University of California, San Francisco, said in an interview. “That clearly is not true.”
The New York Times analyzed data in seven states – California, Colorado, Massachusetts, Oregon, Utah, Vermont, and Virginia – that are tracking the most detailed information. The trends in these states may not reflect the numbers throughout the country, the newspaper reported.
Even still, the numbers back up the idea that vaccinated people may need booster shots this fall to support their earlier vaccine doses. Federal health officials are scheduled to approve the extra shots in coming weeks, potentially in September. The first people to receive booster shots will likely be health care workers and nursing home residents who took the first vaccines in December and January.
“If the chances of a breakthrough infection have gone up considerably, and I think the evidence is clear that they have, and the level of protection against severe illness is no longer as robust as it was, I think the case for boosters goes up pretty quickly,” Dr. Wachter said.
Previous analyses of breakthrough cases included data from June and earlier, the newspaper reported. But since July, COVID-19 cases have soared again because of the Delta variant, and the most recent numbers show an uptick among vaccinated people. In Los Angeles County, for instance, fully vaccinated people account for 20% of new COVID-19 cases, which is up from 11% in May, 5% in April, and 2% in March, according to a late July report from the Los Angeles County Department of Public Health.
What’s more, breakthrough infections in the seven states accounted for 12%-24% of COVID-19 hospitalizations in those states. About 8,000 breakthrough hospitalizations have been reported to the CDC. Still, the overall numbers remain low – in California, for instance, about 1,615 people have been hospitalized with breakthrough infections, which accounts for 0.007% of the state’s 22 million vaccinated people, the Times reported.
The breakthrough infections appear to be more severe among vaccinated people who are older or have weakened immune systems. About 74% of breakthrough cases are among adults 65 or older, the CDC reported.
The increase may shift how vaccinated people see their risks for infection and interact with loved ones. Public health officials have suggested that people follow some COVID-19 safety protocols again, such as wearing masks in public indoor spaces regardless of vaccination status.
As the Delta variant continues to circulate this fall, public health researchers will be researching more about breakthrough cases among vaccinated people, including whether they have prolonged symptoms and how easily they may pass the virus to others.
“I think some of us have been challenged by the numbers of clusters that we’ve seen,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, told this news organization.
“I think that really needs to be examined more,” he said.
A version of this article first appeared on WebMD.com.
Breakthrough cases accounted for about one in five newly diagnosed cases in six of the states, according to the New York Times. Hospitalizations and deaths among vaccinated people may be higher than previously thought as well.
“Remember when the early vaccine studies came out, it was like nobody gets hospitalized, nobody dies,” Robert Wachter, MD, chairman of the department of medicine at the University of California, San Francisco, said in an interview. “That clearly is not true.”
The New York Times analyzed data in seven states – California, Colorado, Massachusetts, Oregon, Utah, Vermont, and Virginia – that are tracking the most detailed information. The trends in these states may not reflect the numbers throughout the country, the newspaper reported.
Even still, the numbers back up the idea that vaccinated people may need booster shots this fall to support their earlier vaccine doses. Federal health officials are scheduled to approve the extra shots in coming weeks, potentially in September. The first people to receive booster shots will likely be health care workers and nursing home residents who took the first vaccines in December and January.
“If the chances of a breakthrough infection have gone up considerably, and I think the evidence is clear that they have, and the level of protection against severe illness is no longer as robust as it was, I think the case for boosters goes up pretty quickly,” Dr. Wachter said.
Previous analyses of breakthrough cases included data from June and earlier, the newspaper reported. But since July, COVID-19 cases have soared again because of the Delta variant, and the most recent numbers show an uptick among vaccinated people. In Los Angeles County, for instance, fully vaccinated people account for 20% of new COVID-19 cases, which is up from 11% in May, 5% in April, and 2% in March, according to a late July report from the Los Angeles County Department of Public Health.
What’s more, breakthrough infections in the seven states accounted for 12%-24% of COVID-19 hospitalizations in those states. About 8,000 breakthrough hospitalizations have been reported to the CDC. Still, the overall numbers remain low – in California, for instance, about 1,615 people have been hospitalized with breakthrough infections, which accounts for 0.007% of the state’s 22 million vaccinated people, the Times reported.
The breakthrough infections appear to be more severe among vaccinated people who are older or have weakened immune systems. About 74% of breakthrough cases are among adults 65 or older, the CDC reported.
The increase may shift how vaccinated people see their risks for infection and interact with loved ones. Public health officials have suggested that people follow some COVID-19 safety protocols again, such as wearing masks in public indoor spaces regardless of vaccination status.
As the Delta variant continues to circulate this fall, public health researchers will be researching more about breakthrough cases among vaccinated people, including whether they have prolonged symptoms and how easily they may pass the virus to others.
“I think some of us have been challenged by the numbers of clusters that we’ve seen,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, told this news organization.
“I think that really needs to be examined more,” he said.
A version of this article first appeared on WebMD.com.
Health care workers share stories of Delta variant’s toll
With the Delta variant surging across the country, already spread-thin health care workers are facing even sicker –and younger – Americans affected by COVID-19 than at the start of the pandemic.
While the exact toll the pandemic will take on essential workers will remain unknown, one thing is clear: The COVID-19 outbreak they’re experiencing right now on the front lines is a far cry from the original strain. They’re scared, exasperated, and crying out for us to pay attention and get vaccinated.
Five health care workers told this news organization about their experiences working the front lines amid the recent surge and what they think needs to happen – fast.
COVID-19 perspective from a paramedic in Connecticut
Michael Battistelli has been an emergency medical services worker for over 20 years and a licensed paramedic in Stratford, Conn., for a decade. He’s also the father of a 5-year-old daughter who isn’t eligible for a vaccination yet. For him, every day has been the same since the start of the pandemic: Surgical mask, N95 mask, face shield, change clothes before going home, and shower as soon as he walks in the door. He’s worried about Delta right now and wants you to be, too.
What keeps him up at night: “It seems like the last time, COVID-19 hit the Pacific Northwest and Northeast first. I hope it’s not the reverse and that it isn’t working its way back up to us here in Connecticut. I’ll add that if we start seeing young people dying, that might be it for me. That might be my final stand as an EMS.”
Why he’s frustrated: “For people to say COVID-19 isn’t real is mind-blowing. I’ve been at this for over a year, and all I think about is how to keep my daughter safe and protect my parents, especially my mom, who is a cancer survivor. When this first started, I brought people into the hospital who thought they would be fine after a day or week in the hospital. They ended up being on ventilators for months – and these were healthy people.”
What he wants to see: “I try not to judge people, but please understand how hard health care workers are working. We’re fatigued and burned out, and we are begging you: Please get vaccinated.”
COVID-19 perspective from an ICU director in Tennessee
Todd Rice, MD, FCCP, is an associate professor of medicine in the division of allergy, pulmonary and critical care at Vanderbilt Medical Center in Nashville, Tenn. While this father of two – ages 15 and 17 – trained for a pandemic, specifically Ebola and H1N1, the sheer volume of young COVID-19 patients in the ICU right now is taking a huge toll on him and his staff.
Why he’s frustrated: “First, there are a group of people that are adamantly against getting vaccinated. It doesn’t matter what we do or say. Second, a lot of people are confused and tell me that they don’t have somebody they trust to answer their questions about the vaccine. Third, some of this is driven by our colleagues: In the last 2 weeks, eight pregnant women with COVID-19 were admitted to our ICU. At least six said that their [obstetrician] told them not to get the vaccine while pregnant. That myth is still out there.”
What’s going on in the ICU: “I want people to know that our unvaccinated infected COVID-19 patients are the sickest patients we take care of. Their condition can change on a dime. We think they’re getting better, and suddenly we turn around and they’re near death or they die in seconds. What’s hard for our staff is that many of these patients have been with us for several weeks, and we get to know them. So when this happens, it hurts us even more because we’ve gotten to know them.”
What we need to do: “While it may take time, we have to talk to vaccine-hesitant people one by one and ask them what questions they have and then provide them with the answers they need. I think the next 6 months is going to be all about getting people who are still movable on this and get them to be comfortable that the vaccine is safe, that we didn’t cut corners. Yes, it was developed faster than anything we’ve ever done before, but that’s because it had to be.”
COVID-19 perspective from a cardiopulmonary doctor in Florida
Yvonne Billings, MD, director of cardiopulmonary medicine at Cleveland Clinic Martin Health in Stuart, Fla., says the “explosion” of COVID-19 cases right after July 4 has left her and her staff emotionally and physically overwhelmed.
What worries her: “We have great PPE, but we’re all worries because Delta is so contagious, and our colleagues have gotten it. We’ll eat lunch next to each other – socially distanced, of course – and we won’t know if we’ve gotten it by just sitting down to eat.”
What she wants us to do – now: “Everyone needs to listen to the real medical science and understand how much this is impacting everyone’s care. For example, if you need to come to the hospital for something other than COVID-19, you will receive slower care because everyone is so tied up caring for COVID-19 patients.”
Health care workers need to get on board, too: “I look at some of my respiratory therapists who chose not to be vaccinated until this last surge. Many told me that when the younger patients started coming in, they could relate to that. One said: ‘I see this gentleman is 27. I’m 27. I could be in the exact same position.’ I don’t want to see anyone get sick, but I’m hoping that when people see that this affects anyone at any age, they can push politics and what they thought was true about the vaccine aside, and make different choices and move forward.”
COVID-19 perspective from a registered nurse in Louisiana
Gina McNemar, 37, an ICU nurse at Baton Rouge General Medical Center in Baton Rouge, La., is wiped out. Her ICU unit is currently full of COVID-19 patients. This mom of 5-year-old twins is so upset about the onslaught of patients in her unit that she sent an email to the CEO of the hospital, which he then shared on Facebook with hundreds of followers. From the email: “This Covid is different. Let me repeat myself: THIS COVID IS NOT THE SAME. ... For the first time since April 2020, I kneeled on top of a patient in the middle of CPR and saw myself. She was 41 years old, no comorbidities, a full life ahead of her. The first time we fought Covid, everyone was old and sickly. They weren’t ‘me.’ This sweet woman was ‘me.’ We ran a full code on her for 1 hour and 26 minutes in front of her fiancé. He cried out to God to save her. He cried out to us to save her. We did everything in our power to save her. We weren’t able to. Three nurses, a pharmacy tech, an x-ray tech, and our HMG doctor hugged, prayed, and cried together after. She was living her life, got Covid, and died.”
Why she wants people to pay attention: “Our COVID-19 patients are young, they’re healthy, they’re able to answer our questions and immediately crash. We don’t have time to catch our breath between one code to the next. This COVID-19 is a much more violent disease, and I can no longer keep quiet. Someone has to say it. Someone has to say, ‘You can believe what you want to believe,’ but I’m seeing it with my own eyes, I’m holding their hands while they die, I’m bagging their body for the morgue. See this crisis through my eyes – please!”
What’s happening with her coworkers: “We’ve had some pretty bad days. We’re all crying and we’re afraid for each other now. We feel like it could be any of us at any point. I’m feeling that I don’t want to let it get to me, but it is. At home, we pray every night. The other night, one of my twins said: ‘I pray that you don’t get coronavirus and die.’ I can’t help but think: 5-year-olds should pray for unicorns and rainbows, not that their mom could die at work.”
Please stop playing politics: “America has become so divided and the vaccine somehow became the evil thing instead of the fact that the vaccine is the savior. I waited in line to get my vaccine because the scientists came up with something to end all this, but not everyone sees it that way. I feel like people don’t want to see and it shouldn’t matter if you’re a Republican or Democrat – after all, Biden is vaccinated [and] Trump is vaccinated.”
COVID-19 perspective from an ED doctor in New York City
Amanda Smith, MD, an ED doctor at Staten Island University Hospital in New York, says she’s sensing a “slow wave coming” when it comes to the Delta variant. The mom of three kids (she has 10-year-old twins and a 12-year-old) thinks often of the first signs of COVID-19 in 2020 and hopes that there won’t be a repeat surge like the initial one in New York City.
It’s hard not to feel frustrated: “I’m annoyed about the Delta variant. Of course, I’ve experienced the ‘I’m not getting the vaccine’ argument, and I’ve been at this long enough that I’m able to compartmentalize my own feelings, but I’m worn down, and I’m aware that I have compassion fatigue. When people complain about their COVID-19 symptoms and say things like ‘If I knew I would feel this horrible, I would have gotten the vaccine,’ I can’t help but feel that this was avoidable. It’s hard to talk to those people. I want to say ‘600,000 dead people weren’t enough to get vaccinated?’ ”
The people avoiding the vaccine: “There are the absolute deniers who will never get vaccinated and aren’t going to change their minds. Then there are the people who feel invincible, and then there are the folks who think that COVID-19 isn’t that bad, it’s just like the flu, it’s only old people dying and they’re not getting information from an appropriate source. It’s not the flu, it does kill you. Delta kills younger people, and it’s very easy to spread. Every one person who was infected with the original strain could infect two to three others. The Delta variant can infect 8-9, and measles, at 13, is the most contagious, so we need to keep reminding people about this.”
It’s not just about you: “Vaccination campaigns were never about the individual. We live together in a civilized society, and the vaccine is something you do for each other. People don’t understand the importance of breaking the chain of transmission and doing this to help each other and eradicate the spread. I just don’t understand what happened to us that we forgot this.”
A version of this article first appeared on WebMD.com.
With the Delta variant surging across the country, already spread-thin health care workers are facing even sicker –and younger – Americans affected by COVID-19 than at the start of the pandemic.
While the exact toll the pandemic will take on essential workers will remain unknown, one thing is clear: The COVID-19 outbreak they’re experiencing right now on the front lines is a far cry from the original strain. They’re scared, exasperated, and crying out for us to pay attention and get vaccinated.
Five health care workers told this news organization about their experiences working the front lines amid the recent surge and what they think needs to happen – fast.
COVID-19 perspective from a paramedic in Connecticut
Michael Battistelli has been an emergency medical services worker for over 20 years and a licensed paramedic in Stratford, Conn., for a decade. He’s also the father of a 5-year-old daughter who isn’t eligible for a vaccination yet. For him, every day has been the same since the start of the pandemic: Surgical mask, N95 mask, face shield, change clothes before going home, and shower as soon as he walks in the door. He’s worried about Delta right now and wants you to be, too.
What keeps him up at night: “It seems like the last time, COVID-19 hit the Pacific Northwest and Northeast first. I hope it’s not the reverse and that it isn’t working its way back up to us here in Connecticut. I’ll add that if we start seeing young people dying, that might be it for me. That might be my final stand as an EMS.”
Why he’s frustrated: “For people to say COVID-19 isn’t real is mind-blowing. I’ve been at this for over a year, and all I think about is how to keep my daughter safe and protect my parents, especially my mom, who is a cancer survivor. When this first started, I brought people into the hospital who thought they would be fine after a day or week in the hospital. They ended up being on ventilators for months – and these were healthy people.”
What he wants to see: “I try not to judge people, but please understand how hard health care workers are working. We’re fatigued and burned out, and we are begging you: Please get vaccinated.”
COVID-19 perspective from an ICU director in Tennessee
Todd Rice, MD, FCCP, is an associate professor of medicine in the division of allergy, pulmonary and critical care at Vanderbilt Medical Center in Nashville, Tenn. While this father of two – ages 15 and 17 – trained for a pandemic, specifically Ebola and H1N1, the sheer volume of young COVID-19 patients in the ICU right now is taking a huge toll on him and his staff.
Why he’s frustrated: “First, there are a group of people that are adamantly against getting vaccinated. It doesn’t matter what we do or say. Second, a lot of people are confused and tell me that they don’t have somebody they trust to answer their questions about the vaccine. Third, some of this is driven by our colleagues: In the last 2 weeks, eight pregnant women with COVID-19 were admitted to our ICU. At least six said that their [obstetrician] told them not to get the vaccine while pregnant. That myth is still out there.”
What’s going on in the ICU: “I want people to know that our unvaccinated infected COVID-19 patients are the sickest patients we take care of. Their condition can change on a dime. We think they’re getting better, and suddenly we turn around and they’re near death or they die in seconds. What’s hard for our staff is that many of these patients have been with us for several weeks, and we get to know them. So when this happens, it hurts us even more because we’ve gotten to know them.”
What we need to do: “While it may take time, we have to talk to vaccine-hesitant people one by one and ask them what questions they have and then provide them with the answers they need. I think the next 6 months is going to be all about getting people who are still movable on this and get them to be comfortable that the vaccine is safe, that we didn’t cut corners. Yes, it was developed faster than anything we’ve ever done before, but that’s because it had to be.”
COVID-19 perspective from a cardiopulmonary doctor in Florida
Yvonne Billings, MD, director of cardiopulmonary medicine at Cleveland Clinic Martin Health in Stuart, Fla., says the “explosion” of COVID-19 cases right after July 4 has left her and her staff emotionally and physically overwhelmed.
What worries her: “We have great PPE, but we’re all worries because Delta is so contagious, and our colleagues have gotten it. We’ll eat lunch next to each other – socially distanced, of course – and we won’t know if we’ve gotten it by just sitting down to eat.”
What she wants us to do – now: “Everyone needs to listen to the real medical science and understand how much this is impacting everyone’s care. For example, if you need to come to the hospital for something other than COVID-19, you will receive slower care because everyone is so tied up caring for COVID-19 patients.”
Health care workers need to get on board, too: “I look at some of my respiratory therapists who chose not to be vaccinated until this last surge. Many told me that when the younger patients started coming in, they could relate to that. One said: ‘I see this gentleman is 27. I’m 27. I could be in the exact same position.’ I don’t want to see anyone get sick, but I’m hoping that when people see that this affects anyone at any age, they can push politics and what they thought was true about the vaccine aside, and make different choices and move forward.”
COVID-19 perspective from a registered nurse in Louisiana
Gina McNemar, 37, an ICU nurse at Baton Rouge General Medical Center in Baton Rouge, La., is wiped out. Her ICU unit is currently full of COVID-19 patients. This mom of 5-year-old twins is so upset about the onslaught of patients in her unit that she sent an email to the CEO of the hospital, which he then shared on Facebook with hundreds of followers. From the email: “This Covid is different. Let me repeat myself: THIS COVID IS NOT THE SAME. ... For the first time since April 2020, I kneeled on top of a patient in the middle of CPR and saw myself. She was 41 years old, no comorbidities, a full life ahead of her. The first time we fought Covid, everyone was old and sickly. They weren’t ‘me.’ This sweet woman was ‘me.’ We ran a full code on her for 1 hour and 26 minutes in front of her fiancé. He cried out to God to save her. He cried out to us to save her. We did everything in our power to save her. We weren’t able to. Three nurses, a pharmacy tech, an x-ray tech, and our HMG doctor hugged, prayed, and cried together after. She was living her life, got Covid, and died.”
Why she wants people to pay attention: “Our COVID-19 patients are young, they’re healthy, they’re able to answer our questions and immediately crash. We don’t have time to catch our breath between one code to the next. This COVID-19 is a much more violent disease, and I can no longer keep quiet. Someone has to say it. Someone has to say, ‘You can believe what you want to believe,’ but I’m seeing it with my own eyes, I’m holding their hands while they die, I’m bagging their body for the morgue. See this crisis through my eyes – please!”
What’s happening with her coworkers: “We’ve had some pretty bad days. We’re all crying and we’re afraid for each other now. We feel like it could be any of us at any point. I’m feeling that I don’t want to let it get to me, but it is. At home, we pray every night. The other night, one of my twins said: ‘I pray that you don’t get coronavirus and die.’ I can’t help but think: 5-year-olds should pray for unicorns and rainbows, not that their mom could die at work.”
Please stop playing politics: “America has become so divided and the vaccine somehow became the evil thing instead of the fact that the vaccine is the savior. I waited in line to get my vaccine because the scientists came up with something to end all this, but not everyone sees it that way. I feel like people don’t want to see and it shouldn’t matter if you’re a Republican or Democrat – after all, Biden is vaccinated [and] Trump is vaccinated.”
COVID-19 perspective from an ED doctor in New York City
Amanda Smith, MD, an ED doctor at Staten Island University Hospital in New York, says she’s sensing a “slow wave coming” when it comes to the Delta variant. The mom of three kids (she has 10-year-old twins and a 12-year-old) thinks often of the first signs of COVID-19 in 2020 and hopes that there won’t be a repeat surge like the initial one in New York City.
It’s hard not to feel frustrated: “I’m annoyed about the Delta variant. Of course, I’ve experienced the ‘I’m not getting the vaccine’ argument, and I’ve been at this long enough that I’m able to compartmentalize my own feelings, but I’m worn down, and I’m aware that I have compassion fatigue. When people complain about their COVID-19 symptoms and say things like ‘If I knew I would feel this horrible, I would have gotten the vaccine,’ I can’t help but feel that this was avoidable. It’s hard to talk to those people. I want to say ‘600,000 dead people weren’t enough to get vaccinated?’ ”
The people avoiding the vaccine: “There are the absolute deniers who will never get vaccinated and aren’t going to change their minds. Then there are the people who feel invincible, and then there are the folks who think that COVID-19 isn’t that bad, it’s just like the flu, it’s only old people dying and they’re not getting information from an appropriate source. It’s not the flu, it does kill you. Delta kills younger people, and it’s very easy to spread. Every one person who was infected with the original strain could infect two to three others. The Delta variant can infect 8-9, and measles, at 13, is the most contagious, so we need to keep reminding people about this.”
It’s not just about you: “Vaccination campaigns were never about the individual. We live together in a civilized society, and the vaccine is something you do for each other. People don’t understand the importance of breaking the chain of transmission and doing this to help each other and eradicate the spread. I just don’t understand what happened to us that we forgot this.”
A version of this article first appeared on WebMD.com.
With the Delta variant surging across the country, already spread-thin health care workers are facing even sicker –and younger – Americans affected by COVID-19 than at the start of the pandemic.
While the exact toll the pandemic will take on essential workers will remain unknown, one thing is clear: The COVID-19 outbreak they’re experiencing right now on the front lines is a far cry from the original strain. They’re scared, exasperated, and crying out for us to pay attention and get vaccinated.
Five health care workers told this news organization about their experiences working the front lines amid the recent surge and what they think needs to happen – fast.
COVID-19 perspective from a paramedic in Connecticut
Michael Battistelli has been an emergency medical services worker for over 20 years and a licensed paramedic in Stratford, Conn., for a decade. He’s also the father of a 5-year-old daughter who isn’t eligible for a vaccination yet. For him, every day has been the same since the start of the pandemic: Surgical mask, N95 mask, face shield, change clothes before going home, and shower as soon as he walks in the door. He’s worried about Delta right now and wants you to be, too.
What keeps him up at night: “It seems like the last time, COVID-19 hit the Pacific Northwest and Northeast first. I hope it’s not the reverse and that it isn’t working its way back up to us here in Connecticut. I’ll add that if we start seeing young people dying, that might be it for me. That might be my final stand as an EMS.”
Why he’s frustrated: “For people to say COVID-19 isn’t real is mind-blowing. I’ve been at this for over a year, and all I think about is how to keep my daughter safe and protect my parents, especially my mom, who is a cancer survivor. When this first started, I brought people into the hospital who thought they would be fine after a day or week in the hospital. They ended up being on ventilators for months – and these were healthy people.”
What he wants to see: “I try not to judge people, but please understand how hard health care workers are working. We’re fatigued and burned out, and we are begging you: Please get vaccinated.”
COVID-19 perspective from an ICU director in Tennessee
Todd Rice, MD, FCCP, is an associate professor of medicine in the division of allergy, pulmonary and critical care at Vanderbilt Medical Center in Nashville, Tenn. While this father of two – ages 15 and 17 – trained for a pandemic, specifically Ebola and H1N1, the sheer volume of young COVID-19 patients in the ICU right now is taking a huge toll on him and his staff.
Why he’s frustrated: “First, there are a group of people that are adamantly against getting vaccinated. It doesn’t matter what we do or say. Second, a lot of people are confused and tell me that they don’t have somebody they trust to answer their questions about the vaccine. Third, some of this is driven by our colleagues: In the last 2 weeks, eight pregnant women with COVID-19 were admitted to our ICU. At least six said that their [obstetrician] told them not to get the vaccine while pregnant. That myth is still out there.”
What’s going on in the ICU: “I want people to know that our unvaccinated infected COVID-19 patients are the sickest patients we take care of. Their condition can change on a dime. We think they’re getting better, and suddenly we turn around and they’re near death or they die in seconds. What’s hard for our staff is that many of these patients have been with us for several weeks, and we get to know them. So when this happens, it hurts us even more because we’ve gotten to know them.”
What we need to do: “While it may take time, we have to talk to vaccine-hesitant people one by one and ask them what questions they have and then provide them with the answers they need. I think the next 6 months is going to be all about getting people who are still movable on this and get them to be comfortable that the vaccine is safe, that we didn’t cut corners. Yes, it was developed faster than anything we’ve ever done before, but that’s because it had to be.”
COVID-19 perspective from a cardiopulmonary doctor in Florida
Yvonne Billings, MD, director of cardiopulmonary medicine at Cleveland Clinic Martin Health in Stuart, Fla., says the “explosion” of COVID-19 cases right after July 4 has left her and her staff emotionally and physically overwhelmed.
What worries her: “We have great PPE, but we’re all worries because Delta is so contagious, and our colleagues have gotten it. We’ll eat lunch next to each other – socially distanced, of course – and we won’t know if we’ve gotten it by just sitting down to eat.”
What she wants us to do – now: “Everyone needs to listen to the real medical science and understand how much this is impacting everyone’s care. For example, if you need to come to the hospital for something other than COVID-19, you will receive slower care because everyone is so tied up caring for COVID-19 patients.”
Health care workers need to get on board, too: “I look at some of my respiratory therapists who chose not to be vaccinated until this last surge. Many told me that when the younger patients started coming in, they could relate to that. One said: ‘I see this gentleman is 27. I’m 27. I could be in the exact same position.’ I don’t want to see anyone get sick, but I’m hoping that when people see that this affects anyone at any age, they can push politics and what they thought was true about the vaccine aside, and make different choices and move forward.”
COVID-19 perspective from a registered nurse in Louisiana
Gina McNemar, 37, an ICU nurse at Baton Rouge General Medical Center in Baton Rouge, La., is wiped out. Her ICU unit is currently full of COVID-19 patients. This mom of 5-year-old twins is so upset about the onslaught of patients in her unit that she sent an email to the CEO of the hospital, which he then shared on Facebook with hundreds of followers. From the email: “This Covid is different. Let me repeat myself: THIS COVID IS NOT THE SAME. ... For the first time since April 2020, I kneeled on top of a patient in the middle of CPR and saw myself. She was 41 years old, no comorbidities, a full life ahead of her. The first time we fought Covid, everyone was old and sickly. They weren’t ‘me.’ This sweet woman was ‘me.’ We ran a full code on her for 1 hour and 26 minutes in front of her fiancé. He cried out to God to save her. He cried out to us to save her. We did everything in our power to save her. We weren’t able to. Three nurses, a pharmacy tech, an x-ray tech, and our HMG doctor hugged, prayed, and cried together after. She was living her life, got Covid, and died.”
Why she wants people to pay attention: “Our COVID-19 patients are young, they’re healthy, they’re able to answer our questions and immediately crash. We don’t have time to catch our breath between one code to the next. This COVID-19 is a much more violent disease, and I can no longer keep quiet. Someone has to say it. Someone has to say, ‘You can believe what you want to believe,’ but I’m seeing it with my own eyes, I’m holding their hands while they die, I’m bagging their body for the morgue. See this crisis through my eyes – please!”
What’s happening with her coworkers: “We’ve had some pretty bad days. We’re all crying and we’re afraid for each other now. We feel like it could be any of us at any point. I’m feeling that I don’t want to let it get to me, but it is. At home, we pray every night. The other night, one of my twins said: ‘I pray that you don’t get coronavirus and die.’ I can’t help but think: 5-year-olds should pray for unicorns and rainbows, not that their mom could die at work.”
Please stop playing politics: “America has become so divided and the vaccine somehow became the evil thing instead of the fact that the vaccine is the savior. I waited in line to get my vaccine because the scientists came up with something to end all this, but not everyone sees it that way. I feel like people don’t want to see and it shouldn’t matter if you’re a Republican or Democrat – after all, Biden is vaccinated [and] Trump is vaccinated.”
COVID-19 perspective from an ED doctor in New York City
Amanda Smith, MD, an ED doctor at Staten Island University Hospital in New York, says she’s sensing a “slow wave coming” when it comes to the Delta variant. The mom of three kids (she has 10-year-old twins and a 12-year-old) thinks often of the first signs of COVID-19 in 2020 and hopes that there won’t be a repeat surge like the initial one in New York City.
It’s hard not to feel frustrated: “I’m annoyed about the Delta variant. Of course, I’ve experienced the ‘I’m not getting the vaccine’ argument, and I’ve been at this long enough that I’m able to compartmentalize my own feelings, but I’m worn down, and I’m aware that I have compassion fatigue. When people complain about their COVID-19 symptoms and say things like ‘If I knew I would feel this horrible, I would have gotten the vaccine,’ I can’t help but feel that this was avoidable. It’s hard to talk to those people. I want to say ‘600,000 dead people weren’t enough to get vaccinated?’ ”
The people avoiding the vaccine: “There are the absolute deniers who will never get vaccinated and aren’t going to change their minds. Then there are the people who feel invincible, and then there are the folks who think that COVID-19 isn’t that bad, it’s just like the flu, it’s only old people dying and they’re not getting information from an appropriate source. It’s not the flu, it does kill you. Delta kills younger people, and it’s very easy to spread. Every one person who was infected with the original strain could infect two to three others. The Delta variant can infect 8-9, and measles, at 13, is the most contagious, so we need to keep reminding people about this.”
It’s not just about you: “Vaccination campaigns were never about the individual. We live together in a civilized society, and the vaccine is something you do for each other. People don’t understand the importance of breaking the chain of transmission and doing this to help each other and eradicate the spread. I just don’t understand what happened to us that we forgot this.”
A version of this article first appeared on WebMD.com.
Secretary of Defense Seeks Approval To Make COVID Vaccines Mandatory For DoD Employees
New policy hopes to be in line with full FDA approval expected in September. When the largest employer in the world makes any significant decision, everyone sits up and takes notice.
That’s what happened when Secretary of Defense Lloyd Austin III sent out a memo to all US Department of Defense (DoD) employees saying he was seeking President Biden’s approval to make COVID-19 vaccines mandatory. His decision affects not only the 3.2 million employees on the payroll, but their families, communities, and states. Florida, for instance, where approximately 40% of the population remains unvaccinated has about 55,000 active duty service members and 36,000 reservists.
Vaccination rates in the military have lagged behind other populations, especially among Black and Hispanic service members. An April study published in Medical Surveillance Monthly Report found that “non-Hispanic Blacks, as well as those who were female, younger, of lower rank, with lower education levels, and those serving in the Army were less likely to initiate COVID-19 vaccination after adjusting for other factors.”
The decision had been in the offing for some time but when cases of the Delta variant of the virus began to spike in July, President Biden asked Sec. Austin to consider how and when the COVID vaccine could be added to the list of required vaccines for service members. It’s a long list already: Depending on their location, service members can get as many as 17 vaccines. It also folllows on the heals of the decision by the US Department of Veterans Affairs to require vaccinations for frontline health care workers.
Austin promised to “not let grass grow.” He consulted with Army Gen. Mark Milley, the Joint Chiefs of Staff, service chiefs, service secretaries, and medical professionals. Based on those discussions, he decided to ask for approval to make the vaccines mandatory no later than mid-September or immediately upon FDA licensure, whichever comes first.
However, he added, “[t]o defend this Nation, we need a healthy and ready force. I strongly encourage all DoD military and civilian personnel—as well as contractor personnel—to get vaccinated now and for military Service members to not wait for the mandate.” Currently, 73% of active-duty personnel have had at least one dose of the vaccine.
Leaping upon the news—and based on the wording in the memo—some in the media were reporting that it meant all troops have to be vaccinated by mid-September. “He’ll make the request by mid-September, unless or until FDA licensure occurs before that time, at which point the Secretary has the authority he needs…to make whatever vaccine is then given that license mandatory.” That’s not the case, said Pentagon press secretary John Kirby in a briefing. Some voices also have called on the DoD to do more to dispel vaccine hesitancy among the troops.
In the meantime, Kirby said, “[T]wo things are going to happen. One, the services are going to be tasked to come back to the Secretary with implementation plans for how they’re going to get this moving.” Noting that mid-September isn’t far away, he pointed out that the services have a “fair but limited amount of time” to arrange their implementation plans. “I have every confidence that service leadership and your commanders will implement this new vaccination program with professionalism, skill, and compassion,” Austin wrote in his memo.
The second thing, Kirby said, was that DoD would be developing policies that comply with the President’s direction that the unvaccinated will have to be subjected to “certain requirements and restrictions.” The Delta variant is hitting the unvaccinated hardest. Austin said the DoD will keep a close eye on infection rates “and the impact these rates might have on our readiness. I will not hesitate to act sooner or recommend a different course to the President if I feel the need to do so.”
Kirby said he didn’t have all the details for that yet, but the department is “working hard” on a policy directive that will clarify what those requirements and restrictions might be.
President Biden replied almost immediately to Austin’s message. “I strongly support Secretary Austin’s message to the force today…. Secretary Austin and I share an unshakeable commitment to making sure our troops have every tool they need to do their jobs as safely as possible. These vaccines will save lives. Period.”
“All FDA-authorized COVID-19 vaccines are safe and highly effective,” Austin said in the close to his memo. “They will protect you and your family. They will protect your unit, your ship, and your co-workers. …Get the shot. Stay healthy. Stay ready.”
New policy hopes to be in line with full FDA approval expected in September. When the largest employer in the world makes any significant decision, everyone sits up and takes notice.
That’s what happened when Secretary of Defense Lloyd Austin III sent out a memo to all US Department of Defense (DoD) employees saying he was seeking President Biden’s approval to make COVID-19 vaccines mandatory. His decision affects not only the 3.2 million employees on the payroll, but their families, communities, and states. Florida, for instance, where approximately 40% of the population remains unvaccinated has about 55,000 active duty service members and 36,000 reservists.
Vaccination rates in the military have lagged behind other populations, especially among Black and Hispanic service members. An April study published in Medical Surveillance Monthly Report found that “non-Hispanic Blacks, as well as those who were female, younger, of lower rank, with lower education levels, and those serving in the Army were less likely to initiate COVID-19 vaccination after adjusting for other factors.”
The decision had been in the offing for some time but when cases of the Delta variant of the virus began to spike in July, President Biden asked Sec. Austin to consider how and when the COVID vaccine could be added to the list of required vaccines for service members. It’s a long list already: Depending on their location, service members can get as many as 17 vaccines. It also folllows on the heals of the decision by the US Department of Veterans Affairs to require vaccinations for frontline health care workers.
Austin promised to “not let grass grow.” He consulted with Army Gen. Mark Milley, the Joint Chiefs of Staff, service chiefs, service secretaries, and medical professionals. Based on those discussions, he decided to ask for approval to make the vaccines mandatory no later than mid-September or immediately upon FDA licensure, whichever comes first.
However, he added, “[t]o defend this Nation, we need a healthy and ready force. I strongly encourage all DoD military and civilian personnel—as well as contractor personnel—to get vaccinated now and for military Service members to not wait for the mandate.” Currently, 73% of active-duty personnel have had at least one dose of the vaccine.
Leaping upon the news—and based on the wording in the memo—some in the media were reporting that it meant all troops have to be vaccinated by mid-September. “He’ll make the request by mid-September, unless or until FDA licensure occurs before that time, at which point the Secretary has the authority he needs…to make whatever vaccine is then given that license mandatory.” That’s not the case, said Pentagon press secretary John Kirby in a briefing. Some voices also have called on the DoD to do more to dispel vaccine hesitancy among the troops.
In the meantime, Kirby said, “[T]wo things are going to happen. One, the services are going to be tasked to come back to the Secretary with implementation plans for how they’re going to get this moving.” Noting that mid-September isn’t far away, he pointed out that the services have a “fair but limited amount of time” to arrange their implementation plans. “I have every confidence that service leadership and your commanders will implement this new vaccination program with professionalism, skill, and compassion,” Austin wrote in his memo.
The second thing, Kirby said, was that DoD would be developing policies that comply with the President’s direction that the unvaccinated will have to be subjected to “certain requirements and restrictions.” The Delta variant is hitting the unvaccinated hardest. Austin said the DoD will keep a close eye on infection rates “and the impact these rates might have on our readiness. I will not hesitate to act sooner or recommend a different course to the President if I feel the need to do so.”
Kirby said he didn’t have all the details for that yet, but the department is “working hard” on a policy directive that will clarify what those requirements and restrictions might be.
President Biden replied almost immediately to Austin’s message. “I strongly support Secretary Austin’s message to the force today…. Secretary Austin and I share an unshakeable commitment to making sure our troops have every tool they need to do their jobs as safely as possible. These vaccines will save lives. Period.”
“All FDA-authorized COVID-19 vaccines are safe and highly effective,” Austin said in the close to his memo. “They will protect you and your family. They will protect your unit, your ship, and your co-workers. …Get the shot. Stay healthy. Stay ready.”
New policy hopes to be in line with full FDA approval expected in September. When the largest employer in the world makes any significant decision, everyone sits up and takes notice.
That’s what happened when Secretary of Defense Lloyd Austin III sent out a memo to all US Department of Defense (DoD) employees saying he was seeking President Biden’s approval to make COVID-19 vaccines mandatory. His decision affects not only the 3.2 million employees on the payroll, but their families, communities, and states. Florida, for instance, where approximately 40% of the population remains unvaccinated has about 55,000 active duty service members and 36,000 reservists.
Vaccination rates in the military have lagged behind other populations, especially among Black and Hispanic service members. An April study published in Medical Surveillance Monthly Report found that “non-Hispanic Blacks, as well as those who were female, younger, of lower rank, with lower education levels, and those serving in the Army were less likely to initiate COVID-19 vaccination after adjusting for other factors.”
The decision had been in the offing for some time but when cases of the Delta variant of the virus began to spike in July, President Biden asked Sec. Austin to consider how and when the COVID vaccine could be added to the list of required vaccines for service members. It’s a long list already: Depending on their location, service members can get as many as 17 vaccines. It also folllows on the heals of the decision by the US Department of Veterans Affairs to require vaccinations for frontline health care workers.
Austin promised to “not let grass grow.” He consulted with Army Gen. Mark Milley, the Joint Chiefs of Staff, service chiefs, service secretaries, and medical professionals. Based on those discussions, he decided to ask for approval to make the vaccines mandatory no later than mid-September or immediately upon FDA licensure, whichever comes first.
However, he added, “[t]o defend this Nation, we need a healthy and ready force. I strongly encourage all DoD military and civilian personnel—as well as contractor personnel—to get vaccinated now and for military Service members to not wait for the mandate.” Currently, 73% of active-duty personnel have had at least one dose of the vaccine.
Leaping upon the news—and based on the wording in the memo—some in the media were reporting that it meant all troops have to be vaccinated by mid-September. “He’ll make the request by mid-September, unless or until FDA licensure occurs before that time, at which point the Secretary has the authority he needs…to make whatever vaccine is then given that license mandatory.” That’s not the case, said Pentagon press secretary John Kirby in a briefing. Some voices also have called on the DoD to do more to dispel vaccine hesitancy among the troops.
In the meantime, Kirby said, “[T]wo things are going to happen. One, the services are going to be tasked to come back to the Secretary with implementation plans for how they’re going to get this moving.” Noting that mid-September isn’t far away, he pointed out that the services have a “fair but limited amount of time” to arrange their implementation plans. “I have every confidence that service leadership and your commanders will implement this new vaccination program with professionalism, skill, and compassion,” Austin wrote in his memo.
The second thing, Kirby said, was that DoD would be developing policies that comply with the President’s direction that the unvaccinated will have to be subjected to “certain requirements and restrictions.” The Delta variant is hitting the unvaccinated hardest. Austin said the DoD will keep a close eye on infection rates “and the impact these rates might have on our readiness. I will not hesitate to act sooner or recommend a different course to the President if I feel the need to do so.”
Kirby said he didn’t have all the details for that yet, but the department is “working hard” on a policy directive that will clarify what those requirements and restrictions might be.
President Biden replied almost immediately to Austin’s message. “I strongly support Secretary Austin’s message to the force today…. Secretary Austin and I share an unshakeable commitment to making sure our troops have every tool they need to do their jobs as safely as possible. These vaccines will save lives. Period.”
“All FDA-authorized COVID-19 vaccines are safe and highly effective,” Austin said in the close to his memo. “They will protect you and your family. They will protect your unit, your ship, and your co-workers. …Get the shot. Stay healthy. Stay ready.”
Psychiatrists’ income, wealth gain ground despite COVID-19 challenges
Although many physicians endured pandemic-related income struggles in 2020, psychiatrists are doing fairly well with building their nest egg and paying down debt, according to the Medscape Psychiatrist Wealth and Debt Report 2021.
Surprisingly, despite COVID-19, psychiatrists’ income improved somewhat this year – from $268,000 in 2020 to $275,000 in 2021.
However, that still puts psychiatrists among the lower-paid specialists.
The highest-paying specialty is plastic surgery ($526,000), followed by orthopedics and orthopedic surgery ($511,000) and cardiology ($459,000), according to the overall Medscape Physician Wealth and Debt Report 2021. The report is based on responses from nearly 18,000 physicians in 29 specialties. All were surveyed between Oct. 6, 2020, and Feb. 11, 2021.
Psychiatrists’ overall wealth gained some ground over the past year, with 40% reporting a net worth of $1 million to $5 million this year – up from 38% last year. Just 6% of psychiatrists have a net worth north of $5 million, up slightly from 5% last year.
Keeping up with bills
based in St. Louis Park, Minn. He noted that the rise in the stock market also played a role, with the S&P 500 finishing the year up over 18%.
“I’ve seen clients accumulate cash, which has added to their net worth. They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” Dr. Greenwald said.
The percentage of psychiatrists with a net worth under $500,000 decreased from 37% last year to 32% this year. Psychiatry is still among the specialties reporting a high percentage of members with net worth below $500,000.
But gender matters. Earnings overall are higher for male than female psychiatrists, and that is reflected in net worth. Fewer female than male psychiatrists are worth more than $5 million (4% vs. 7%), and more female psychiatrists have a net worth of less than $500,000 (41% vs. 26%).
As in prior years, most psychiatrists are paying down a home mortgage on their primary residence (66%). Psychiatrists’ mortgage payments span a wide range, from less than $100,000 (23%) to more than $500,000 (15%). However, 27% report having no mortgage.
Mortgage aside, other top expenses or debts for psychiatrists are car loan payments (36%), paying off college and medical school debt (26%), credit card debt (25%), and medical expenses for self or loved ones (19%).
Other expenses include college tuition for children (16%), car lease payments (14%), mortgage on a second home (13%), private-school tuition for a child (12%), and child care (12%).
Despite some financially challenging months, the vast majority of psychiatrists (94%) kept up with paying their bills.
That’s better than what much of America experienced. According to a U.S. Census Bureau survey conducted last July, roughly 25% of adults missed a mortgage or rent payment because of COVID-related difficulties.
About half of psychiatrists pool their income to pay for bills. One-quarter do not have joint accounts with a spouse or partner.
Spender or saver?
About three-quarters of psychiatrists continued to spend as usual in 2020. About one-quarter took significant steps to lower their expenses, such as refinancing their home or moving to a less costly home.
In line with prior Medscape surveys, about half of psychiatrists have a general idea of how much they spend and on what, but they do not track or formalize it.
According to a recent survey by Intuit, only 35% of Americans say they know how much they spent last month. Viewed by age, 27% of millennials, 34% of Gen Xers, and 46% of baby boomers knew how much they spent.
Many psychiatrists have a higher-than-average number of credit cards; 42% have at least five. By comparison, the average American has four.
Savings was mixed for psychiatrists this past year; 61% put in the same amount or more each month into their 401(k) plans, but 33% put in less money, compared with last year.
For taxable savings accounts, half of psychiatrists put the same amount or more into after-tax accounts – but 22% put in less money, compared with last year. Another one-quarter did not use these savings accounts at all.
The percentage of psychiatrists who experienced losses because of practice problems rose from 6% to 9% in the past year. Much of that was likely because of COVID. However, about the same percentage reported no financial losses this year (76%), compared with last year (75%).
The vast majority of psychiatrists report living within or below their means; only 5% live above their means.
“There are certainly folks who believe that, as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said.
However, “living within one’s means is having a 3-6 months’ emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip,” he added.
A version of this article first appeared on Medscape.com.
Although many physicians endured pandemic-related income struggles in 2020, psychiatrists are doing fairly well with building their nest egg and paying down debt, according to the Medscape Psychiatrist Wealth and Debt Report 2021.
Surprisingly, despite COVID-19, psychiatrists’ income improved somewhat this year – from $268,000 in 2020 to $275,000 in 2021.
However, that still puts psychiatrists among the lower-paid specialists.
The highest-paying specialty is plastic surgery ($526,000), followed by orthopedics and orthopedic surgery ($511,000) and cardiology ($459,000), according to the overall Medscape Physician Wealth and Debt Report 2021. The report is based on responses from nearly 18,000 physicians in 29 specialties. All were surveyed between Oct. 6, 2020, and Feb. 11, 2021.
Psychiatrists’ overall wealth gained some ground over the past year, with 40% reporting a net worth of $1 million to $5 million this year – up from 38% last year. Just 6% of psychiatrists have a net worth north of $5 million, up slightly from 5% last year.
Keeping up with bills
based in St. Louis Park, Minn. He noted that the rise in the stock market also played a role, with the S&P 500 finishing the year up over 18%.
“I’ve seen clients accumulate cash, which has added to their net worth. They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” Dr. Greenwald said.
The percentage of psychiatrists with a net worth under $500,000 decreased from 37% last year to 32% this year. Psychiatry is still among the specialties reporting a high percentage of members with net worth below $500,000.
But gender matters. Earnings overall are higher for male than female psychiatrists, and that is reflected in net worth. Fewer female than male psychiatrists are worth more than $5 million (4% vs. 7%), and more female psychiatrists have a net worth of less than $500,000 (41% vs. 26%).
As in prior years, most psychiatrists are paying down a home mortgage on their primary residence (66%). Psychiatrists’ mortgage payments span a wide range, from less than $100,000 (23%) to more than $500,000 (15%). However, 27% report having no mortgage.
Mortgage aside, other top expenses or debts for psychiatrists are car loan payments (36%), paying off college and medical school debt (26%), credit card debt (25%), and medical expenses for self or loved ones (19%).
Other expenses include college tuition for children (16%), car lease payments (14%), mortgage on a second home (13%), private-school tuition for a child (12%), and child care (12%).
Despite some financially challenging months, the vast majority of psychiatrists (94%) kept up with paying their bills.
That’s better than what much of America experienced. According to a U.S. Census Bureau survey conducted last July, roughly 25% of adults missed a mortgage or rent payment because of COVID-related difficulties.
About half of psychiatrists pool their income to pay for bills. One-quarter do not have joint accounts with a spouse or partner.
Spender or saver?
About three-quarters of psychiatrists continued to spend as usual in 2020. About one-quarter took significant steps to lower their expenses, such as refinancing their home or moving to a less costly home.
In line with prior Medscape surveys, about half of psychiatrists have a general idea of how much they spend and on what, but they do not track or formalize it.
According to a recent survey by Intuit, only 35% of Americans say they know how much they spent last month. Viewed by age, 27% of millennials, 34% of Gen Xers, and 46% of baby boomers knew how much they spent.
Many psychiatrists have a higher-than-average number of credit cards; 42% have at least five. By comparison, the average American has four.
Savings was mixed for psychiatrists this past year; 61% put in the same amount or more each month into their 401(k) plans, but 33% put in less money, compared with last year.
For taxable savings accounts, half of psychiatrists put the same amount or more into after-tax accounts – but 22% put in less money, compared with last year. Another one-quarter did not use these savings accounts at all.
The percentage of psychiatrists who experienced losses because of practice problems rose from 6% to 9% in the past year. Much of that was likely because of COVID. However, about the same percentage reported no financial losses this year (76%), compared with last year (75%).
The vast majority of psychiatrists report living within or below their means; only 5% live above their means.
“There are certainly folks who believe that, as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said.
However, “living within one’s means is having a 3-6 months’ emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip,” he added.
A version of this article first appeared on Medscape.com.
Although many physicians endured pandemic-related income struggles in 2020, psychiatrists are doing fairly well with building their nest egg and paying down debt, according to the Medscape Psychiatrist Wealth and Debt Report 2021.
Surprisingly, despite COVID-19, psychiatrists’ income improved somewhat this year – from $268,000 in 2020 to $275,000 in 2021.
However, that still puts psychiatrists among the lower-paid specialists.
The highest-paying specialty is plastic surgery ($526,000), followed by orthopedics and orthopedic surgery ($511,000) and cardiology ($459,000), according to the overall Medscape Physician Wealth and Debt Report 2021. The report is based on responses from nearly 18,000 physicians in 29 specialties. All were surveyed between Oct. 6, 2020, and Feb. 11, 2021.
Psychiatrists’ overall wealth gained some ground over the past year, with 40% reporting a net worth of $1 million to $5 million this year – up from 38% last year. Just 6% of psychiatrists have a net worth north of $5 million, up slightly from 5% last year.
Keeping up with bills
based in St. Louis Park, Minn. He noted that the rise in the stock market also played a role, with the S&P 500 finishing the year up over 18%.
“I’ve seen clients accumulate cash, which has added to their net worth. They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” Dr. Greenwald said.
The percentage of psychiatrists with a net worth under $500,000 decreased from 37% last year to 32% this year. Psychiatry is still among the specialties reporting a high percentage of members with net worth below $500,000.
But gender matters. Earnings overall are higher for male than female psychiatrists, and that is reflected in net worth. Fewer female than male psychiatrists are worth more than $5 million (4% vs. 7%), and more female psychiatrists have a net worth of less than $500,000 (41% vs. 26%).
As in prior years, most psychiatrists are paying down a home mortgage on their primary residence (66%). Psychiatrists’ mortgage payments span a wide range, from less than $100,000 (23%) to more than $500,000 (15%). However, 27% report having no mortgage.
Mortgage aside, other top expenses or debts for psychiatrists are car loan payments (36%), paying off college and medical school debt (26%), credit card debt (25%), and medical expenses for self or loved ones (19%).
Other expenses include college tuition for children (16%), car lease payments (14%), mortgage on a second home (13%), private-school tuition for a child (12%), and child care (12%).
Despite some financially challenging months, the vast majority of psychiatrists (94%) kept up with paying their bills.
That’s better than what much of America experienced. According to a U.S. Census Bureau survey conducted last July, roughly 25% of adults missed a mortgage or rent payment because of COVID-related difficulties.
About half of psychiatrists pool their income to pay for bills. One-quarter do not have joint accounts with a spouse or partner.
Spender or saver?
About three-quarters of psychiatrists continued to spend as usual in 2020. About one-quarter took significant steps to lower their expenses, such as refinancing their home or moving to a less costly home.
In line with prior Medscape surveys, about half of psychiatrists have a general idea of how much they spend and on what, but they do not track or formalize it.
According to a recent survey by Intuit, only 35% of Americans say they know how much they spent last month. Viewed by age, 27% of millennials, 34% of Gen Xers, and 46% of baby boomers knew how much they spent.
Many psychiatrists have a higher-than-average number of credit cards; 42% have at least five. By comparison, the average American has four.
Savings was mixed for psychiatrists this past year; 61% put in the same amount or more each month into their 401(k) plans, but 33% put in less money, compared with last year.
For taxable savings accounts, half of psychiatrists put the same amount or more into after-tax accounts – but 22% put in less money, compared with last year. Another one-quarter did not use these savings accounts at all.
The percentage of psychiatrists who experienced losses because of practice problems rose from 6% to 9% in the past year. Much of that was likely because of COVID. However, about the same percentage reported no financial losses this year (76%), compared with last year (75%).
The vast majority of psychiatrists report living within or below their means; only 5% live above their means.
“There are certainly folks who believe that, as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said.
However, “living within one’s means is having a 3-6 months’ emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip,” he added.
A version of this article first appeared on Medscape.com.
Children and COVID: New cases rise to winter levels
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
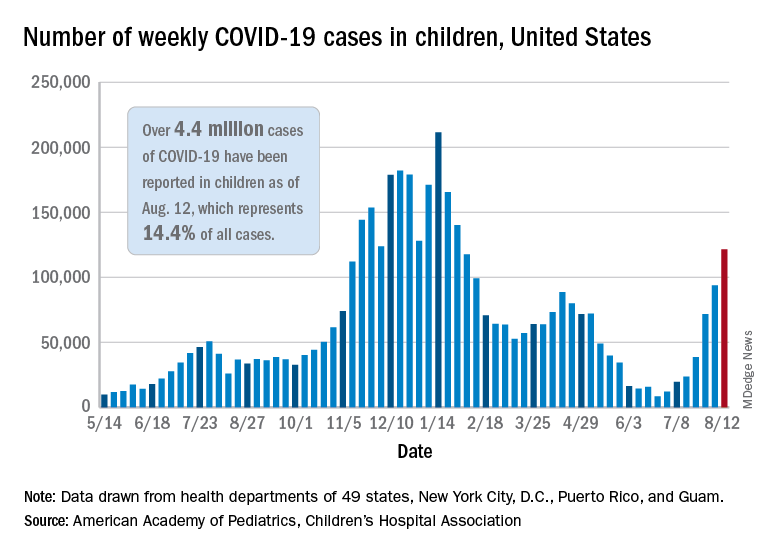
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
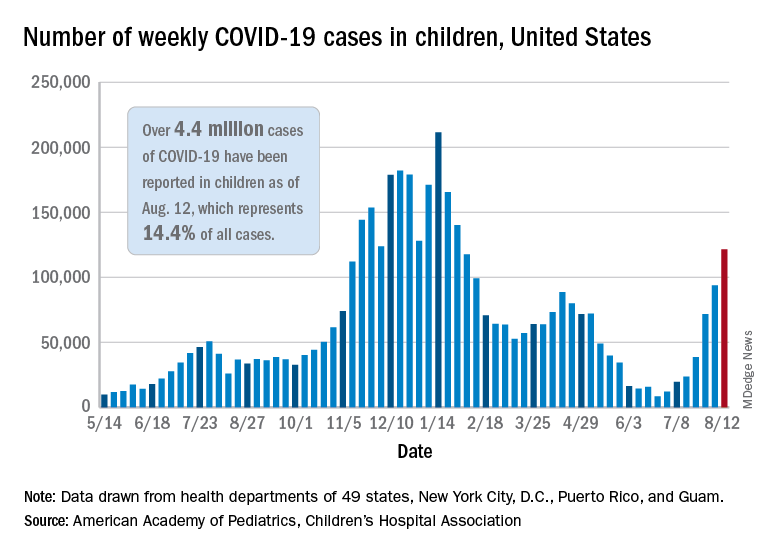
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
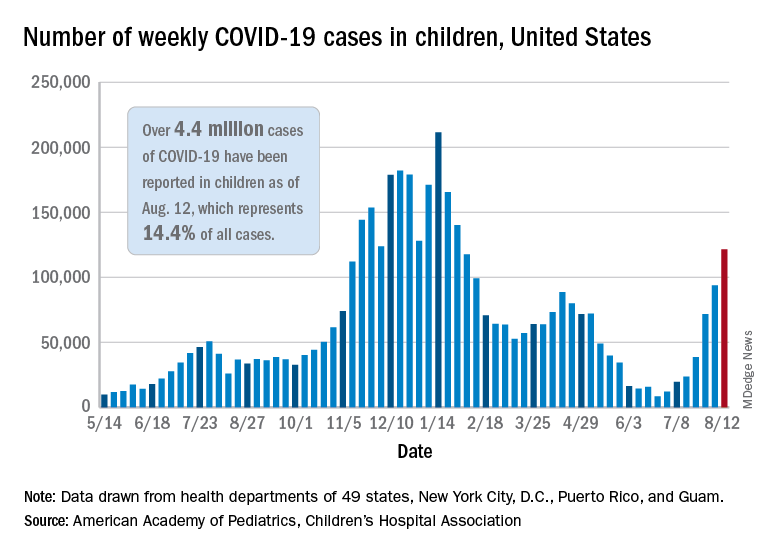
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.





