User login
In Case You Missed It: COVID
Long COVID’s grip will likely tighten as infections continue
COVID-19 is far from done in the United States, with more than 111,000 new cases being recorded a day in the second week of August, according to Johns Hopkins University, and 625 deaths being reported every day. , a condition that already has affected between 7.7 million and 23 million Americans, according to U.S. government estimates.
“It is evident that long COVID is real, that it already impacts a substantial number of people, and that this number may continue to grow as new infections occur,” the U.S. Department of Health and Human Services (HHS) said in a research action plan released Aug. 4.
“We are heading towards a big problem on our hands,” says Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs Hospital in St. Louis. “It’s like if we are falling in a plane, hurtling towards the ground. It doesn’t matter at what speed we are falling; what matters is that we are all falling, and falling fast. It’s a real problem. We needed to bring attention to this, yesterday,” he said.
Bryan Lau, PhD, professor of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, and co-lead of a long COVID study there, says whether it’s 5% of the 92 million officially recorded U.S. COVID-19 cases, or 30% – on the higher end of estimates – that means anywhere between 4.5 million and 27 million Americans will have the effects of long COVID.
Other experts put the estimates even higher.
“If we conservatively assume 100 million working-age adults have been infected, that implies 10 to 33 million may have long COVID,” Alice Burns, PhD, associate director for the Kaiser Family Foundation’s Program on Medicaid and the Uninsured, wrote in an analysis.
And even the Centers for Disease Control and Prevention says only a fraction of cases have been recorded.
That, in turn, means tens of millions of people who struggle to work, to get to school, and to take care of their families – and who will be making demands on an already stressed U.S. health care system.
The HHS said in its Aug. 4 report that long COVID could keep 1 million people a day out of work, with a loss of $50 billion in annual pay.
Dr. Lau said health workers and policymakers are woefully unprepared.
“If you have a family unit, and the mom or dad can’t work, or has trouble taking their child to activities, where does the question of support come into play? Where is there potential for food issues, or housing issues?” he asked. “I see the potential for the burden to be extremely large in that capacity.”
Dr. Lau said he has yet to see any strong estimates of how many cases of long COVID might develop. Because a person has to get COVID-19 to ultimately get long COVID, the two are linked. In other words, as COVID-19 cases rise, so will cases of long COVID, and vice versa.
Evidence from the Kaiser Family Foundation analysis suggests a significant impact on employment: Surveys showed more than half of adults with long COVID who worked before becoming infected are either out of work or working fewer hours. Conditions associated with long COVID – such as fatigue, malaise, or problems concentrating – limit people’s ability to work, even if they have jobs that allow for accommodations.
Two surveys of people with long COVID who had worked before becoming infected showed that between 22% and 27% of them were out of work after getting long COVID. In comparison, among all working-age adults in 2019, only 7% were out of work. Given the sheer number of working-age adults with long COVID, the effects on employment may be profound and are likely to involve more people over time. One study estimates that long COVID already accounts for 15% of unfilled jobs.
The most severe symptoms of long COVID include brain fog and heart complications, known to persist for weeks for months after a COVID-19 infection.
A study from the University of Norway published in Open Forum Infectious Diseases found 53% of people tested had at least one symptom of thinking problems 13 months after infection with COVID-19. According to the HHS’ latest report on long COVID, people with thinking problems, heart conditions, mobility issues, and other symptoms are going to need a considerable amount of care. Many will need lengthy periods of rehabilitation.
Dr. Al-Aly worries that long COVID has already severely affected the labor force and the job market, all while burdening the country’s health care system.
“While there are variations in how individuals respond and cope with long COVID, the unifying thread is that with the level of disability it causes, more people will be struggling to keep up with the demands of the workforce and more people will be out on disability than ever before,” he said.
Studies from Johns Hopkins and the University of Washington estimate that 5%-30% of people could get long COVID in the future. Projections beyond that are hazy.
“So far, all the studies we have done on long COVID have been reactionary. Much of the activism around long COVID has been patient led. We are seeing more and more people with lasting symptoms. We need our research to catch up,” Dr. Lau said.
Theo Vos, MD, PhD, professor of health sciences at University of Washington, Seattle, said the main reasons for the huge range of predictions are the variety of methods used, as well as differences in sample size. Also, much long COVID data is self-reported, making it difficult for epidemiologists to track.
“With self-reported data, you can’t plug people into a machine and say this is what they have or this is what they don’t have. At the population level, the only thing you can do is ask questions. There is no systematic way to define long COVID,” he said.
Dr. Vos’s most recent study, which is being peer-reviewed and revised, found that most people with long COVID have symptoms similar to those seen in other autoimmune diseases. But sometimes the immune system can overreact, causing the more severe symptoms, such as brain fog and heart problems, associated with long COVID.
One reason that researchers struggle to come up with numbers, said Dr. Al-Aly, is the rapid rise of new variants. These variants appear to sometimes cause less severe disease than previous ones, but it’s not clear whether that means different risks for long COVID.
“There’s a wide diversity in severity. Someone can have long COVID and be fully functional, while others are not functional at all. We still have a long way to go before we figure out why,” Dr. Lau said.
A version of this article first appeared on WebMD.com.
COVID-19 is far from done in the United States, with more than 111,000 new cases being recorded a day in the second week of August, according to Johns Hopkins University, and 625 deaths being reported every day. , a condition that already has affected between 7.7 million and 23 million Americans, according to U.S. government estimates.
“It is evident that long COVID is real, that it already impacts a substantial number of people, and that this number may continue to grow as new infections occur,” the U.S. Department of Health and Human Services (HHS) said in a research action plan released Aug. 4.
“We are heading towards a big problem on our hands,” says Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs Hospital in St. Louis. “It’s like if we are falling in a plane, hurtling towards the ground. It doesn’t matter at what speed we are falling; what matters is that we are all falling, and falling fast. It’s a real problem. We needed to bring attention to this, yesterday,” he said.
Bryan Lau, PhD, professor of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, and co-lead of a long COVID study there, says whether it’s 5% of the 92 million officially recorded U.S. COVID-19 cases, or 30% – on the higher end of estimates – that means anywhere between 4.5 million and 27 million Americans will have the effects of long COVID.
Other experts put the estimates even higher.
“If we conservatively assume 100 million working-age adults have been infected, that implies 10 to 33 million may have long COVID,” Alice Burns, PhD, associate director for the Kaiser Family Foundation’s Program on Medicaid and the Uninsured, wrote in an analysis.
And even the Centers for Disease Control and Prevention says only a fraction of cases have been recorded.
That, in turn, means tens of millions of people who struggle to work, to get to school, and to take care of their families – and who will be making demands on an already stressed U.S. health care system.
The HHS said in its Aug. 4 report that long COVID could keep 1 million people a day out of work, with a loss of $50 billion in annual pay.
Dr. Lau said health workers and policymakers are woefully unprepared.
“If you have a family unit, and the mom or dad can’t work, or has trouble taking their child to activities, where does the question of support come into play? Where is there potential for food issues, or housing issues?” he asked. “I see the potential for the burden to be extremely large in that capacity.”
Dr. Lau said he has yet to see any strong estimates of how many cases of long COVID might develop. Because a person has to get COVID-19 to ultimately get long COVID, the two are linked. In other words, as COVID-19 cases rise, so will cases of long COVID, and vice versa.
Evidence from the Kaiser Family Foundation analysis suggests a significant impact on employment: Surveys showed more than half of adults with long COVID who worked before becoming infected are either out of work or working fewer hours. Conditions associated with long COVID – such as fatigue, malaise, or problems concentrating – limit people’s ability to work, even if they have jobs that allow for accommodations.
Two surveys of people with long COVID who had worked before becoming infected showed that between 22% and 27% of them were out of work after getting long COVID. In comparison, among all working-age adults in 2019, only 7% were out of work. Given the sheer number of working-age adults with long COVID, the effects on employment may be profound and are likely to involve more people over time. One study estimates that long COVID already accounts for 15% of unfilled jobs.
The most severe symptoms of long COVID include brain fog and heart complications, known to persist for weeks for months after a COVID-19 infection.
A study from the University of Norway published in Open Forum Infectious Diseases found 53% of people tested had at least one symptom of thinking problems 13 months after infection with COVID-19. According to the HHS’ latest report on long COVID, people with thinking problems, heart conditions, mobility issues, and other symptoms are going to need a considerable amount of care. Many will need lengthy periods of rehabilitation.
Dr. Al-Aly worries that long COVID has already severely affected the labor force and the job market, all while burdening the country’s health care system.
“While there are variations in how individuals respond and cope with long COVID, the unifying thread is that with the level of disability it causes, more people will be struggling to keep up with the demands of the workforce and more people will be out on disability than ever before,” he said.
Studies from Johns Hopkins and the University of Washington estimate that 5%-30% of people could get long COVID in the future. Projections beyond that are hazy.
“So far, all the studies we have done on long COVID have been reactionary. Much of the activism around long COVID has been patient led. We are seeing more and more people with lasting symptoms. We need our research to catch up,” Dr. Lau said.
Theo Vos, MD, PhD, professor of health sciences at University of Washington, Seattle, said the main reasons for the huge range of predictions are the variety of methods used, as well as differences in sample size. Also, much long COVID data is self-reported, making it difficult for epidemiologists to track.
“With self-reported data, you can’t plug people into a machine and say this is what they have or this is what they don’t have. At the population level, the only thing you can do is ask questions. There is no systematic way to define long COVID,” he said.
Dr. Vos’s most recent study, which is being peer-reviewed and revised, found that most people with long COVID have symptoms similar to those seen in other autoimmune diseases. But sometimes the immune system can overreact, causing the more severe symptoms, such as brain fog and heart problems, associated with long COVID.
One reason that researchers struggle to come up with numbers, said Dr. Al-Aly, is the rapid rise of new variants. These variants appear to sometimes cause less severe disease than previous ones, but it’s not clear whether that means different risks for long COVID.
“There’s a wide diversity in severity. Someone can have long COVID and be fully functional, while others are not functional at all. We still have a long way to go before we figure out why,” Dr. Lau said.
A version of this article first appeared on WebMD.com.
COVID-19 is far from done in the United States, with more than 111,000 new cases being recorded a day in the second week of August, according to Johns Hopkins University, and 625 deaths being reported every day. , a condition that already has affected between 7.7 million and 23 million Americans, according to U.S. government estimates.
“It is evident that long COVID is real, that it already impacts a substantial number of people, and that this number may continue to grow as new infections occur,” the U.S. Department of Health and Human Services (HHS) said in a research action plan released Aug. 4.
“We are heading towards a big problem on our hands,” says Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs Hospital in St. Louis. “It’s like if we are falling in a plane, hurtling towards the ground. It doesn’t matter at what speed we are falling; what matters is that we are all falling, and falling fast. It’s a real problem. We needed to bring attention to this, yesterday,” he said.
Bryan Lau, PhD, professor of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, and co-lead of a long COVID study there, says whether it’s 5% of the 92 million officially recorded U.S. COVID-19 cases, or 30% – on the higher end of estimates – that means anywhere between 4.5 million and 27 million Americans will have the effects of long COVID.
Other experts put the estimates even higher.
“If we conservatively assume 100 million working-age adults have been infected, that implies 10 to 33 million may have long COVID,” Alice Burns, PhD, associate director for the Kaiser Family Foundation’s Program on Medicaid and the Uninsured, wrote in an analysis.
And even the Centers for Disease Control and Prevention says only a fraction of cases have been recorded.
That, in turn, means tens of millions of people who struggle to work, to get to school, and to take care of their families – and who will be making demands on an already stressed U.S. health care system.
The HHS said in its Aug. 4 report that long COVID could keep 1 million people a day out of work, with a loss of $50 billion in annual pay.
Dr. Lau said health workers and policymakers are woefully unprepared.
“If you have a family unit, and the mom or dad can’t work, or has trouble taking their child to activities, where does the question of support come into play? Where is there potential for food issues, or housing issues?” he asked. “I see the potential for the burden to be extremely large in that capacity.”
Dr. Lau said he has yet to see any strong estimates of how many cases of long COVID might develop. Because a person has to get COVID-19 to ultimately get long COVID, the two are linked. In other words, as COVID-19 cases rise, so will cases of long COVID, and vice versa.
Evidence from the Kaiser Family Foundation analysis suggests a significant impact on employment: Surveys showed more than half of adults with long COVID who worked before becoming infected are either out of work or working fewer hours. Conditions associated with long COVID – such as fatigue, malaise, or problems concentrating – limit people’s ability to work, even if they have jobs that allow for accommodations.
Two surveys of people with long COVID who had worked before becoming infected showed that between 22% and 27% of them were out of work after getting long COVID. In comparison, among all working-age adults in 2019, only 7% were out of work. Given the sheer number of working-age adults with long COVID, the effects on employment may be profound and are likely to involve more people over time. One study estimates that long COVID already accounts for 15% of unfilled jobs.
The most severe symptoms of long COVID include brain fog and heart complications, known to persist for weeks for months after a COVID-19 infection.
A study from the University of Norway published in Open Forum Infectious Diseases found 53% of people tested had at least one symptom of thinking problems 13 months after infection with COVID-19. According to the HHS’ latest report on long COVID, people with thinking problems, heart conditions, mobility issues, and other symptoms are going to need a considerable amount of care. Many will need lengthy periods of rehabilitation.
Dr. Al-Aly worries that long COVID has already severely affected the labor force and the job market, all while burdening the country’s health care system.
“While there are variations in how individuals respond and cope with long COVID, the unifying thread is that with the level of disability it causes, more people will be struggling to keep up with the demands of the workforce and more people will be out on disability than ever before,” he said.
Studies from Johns Hopkins and the University of Washington estimate that 5%-30% of people could get long COVID in the future. Projections beyond that are hazy.
“So far, all the studies we have done on long COVID have been reactionary. Much of the activism around long COVID has been patient led. We are seeing more and more people with lasting symptoms. We need our research to catch up,” Dr. Lau said.
Theo Vos, MD, PhD, professor of health sciences at University of Washington, Seattle, said the main reasons for the huge range of predictions are the variety of methods used, as well as differences in sample size. Also, much long COVID data is self-reported, making it difficult for epidemiologists to track.
“With self-reported data, you can’t plug people into a machine and say this is what they have or this is what they don’t have. At the population level, the only thing you can do is ask questions. There is no systematic way to define long COVID,” he said.
Dr. Vos’s most recent study, which is being peer-reviewed and revised, found that most people with long COVID have symptoms similar to those seen in other autoimmune diseases. But sometimes the immune system can overreact, causing the more severe symptoms, such as brain fog and heart problems, associated with long COVID.
One reason that researchers struggle to come up with numbers, said Dr. Al-Aly, is the rapid rise of new variants. These variants appear to sometimes cause less severe disease than previous ones, but it’s not clear whether that means different risks for long COVID.
“There’s a wide diversity in severity. Someone can have long COVID and be fully functional, while others are not functional at all. We still have a long way to go before we figure out why,” Dr. Lau said.
A version of this article first appeared on WebMD.com.
Plasma biomarkers predict COVID’s neurological sequelae
SAN DIEGO – Even after recovery of an acute COVID-19 infection, some patients experience extended or even long-term symptoms that can range from mild to debilitating. Some of these symptoms are neurological: headaches, brain fog, cognitive impairment, loss of taste or smell, and even cerebrovascular complications such stroke. There are even hints that COVID-19 infection could lead to future neurodegeneration.
Those issues have prompted efforts to identify biomarkers that can help track and monitor neurological complications of COVID-19. “Throughout the course of the pandemic, it has become apparent that COVID-19 can cause various neurological symptoms. Because of this, ,” Jennifer Cooper said during a lecture at the Alzheimer’s Association International Conference. She presented new research suggesting that neurofilament light (NfL) and glial fibrillary acidic protein (GFAP) may prove useful.
Ms. Cooper is a master’s degree student at the University of British Columbia and Canada.
Looking for sensitivity and specificity in plasma biomarkers
The researchers turned to plasma-based markers because they can reflect underlying pathology in the central nervous system. They focused on NfL, which reflects axonal damage, and GFAP, which is a marker of astrocyte activation.
The researchers analyzed data from 209 patients with COVID-19 who were admitted to the Vancouver (B.C.) General Hospital intensive care unit. Sixty-four percent were male, and the median age was 61 years. Sixty percent were ventilated, and 17% died.
The researchers determined if an individual patient’s biomarker level at hospital admission fell within a normal biomarker reference interval. A total of 53% had NfL levels outside the normal range, and 42% had GFAP levels outside the normal range. In addition, 31% of patients had both GFAP and NfL levels outside of the normal range.
Among all patients, 12% experienced ischemia, 4% hemorrhage, 2% seizures, and 10% degeneration.
At admission, NfL predicted a neurological complication with an area under the curve (AUC) of 0.702. GFAP had an AUC of 0.722. In combination, they had an AUC of 0.743. At 1 week, NfL had an AUC of 0.802, GFAP an AUC of 0.733, and the combination an AUC of 0.812.
Using age-specific cutoff values, the researchers found increased risks for neurological complications at admission (NfL odds ratio [OR], 2.9; GFAP OR, 1.6; combined OR, 2.1) and at 1 week (NfL OR, not significant; GFAP OR, 4.8; combined OR, 6.6). “We can see that both NFL and GFAP have utility in detecting neurological complications. And combining both of our markers improves detection at both time points. NfL is a marker that provides more sensitivity, where in this cohort GFAP is a marker that provides a little bit more specificity,” said Ms. Cooper.
Will additional biomarkers help?
The researchers are continuing to follow up patients at 6 months and 18 months post diagnosis, using neuropsychiatric tests and additional biomarker analysis, as well as PET and MRI scans. The patient sample is being expanded to those in the general hospital ward and some who were not hospitalized.
During the Q&A session, Ms. Cooper was asked if the group had collected reference data from patients who were admitted to the ICU with non-COVID disease. She responded that the group has some of that data, but as the pandemic went on they had difficulty finding patients who had never been infected with COVID to serve as reliable controls. To date, they have identified 33 controls who had a respiratory condition when admitted to the ICU. “What we see is the neurological biomarker levels in COVID are slightly lower than those with another respiratory condition in the ICU. But the data has a massive spread and the significance is very small between the two groups,” said Ms. Cooper.
Unanswered questions
The study is interesting, but leaves a lot of unanswered questions, according to Wiesje van der Flier, PhD, who moderated the session where the study was presented. “There are a lot of unknowns still: Will [the biomarkers] become normal again, once the COVID is over? Also, there was an increased risk, but it was not a one-to-one correspondence, so you can also have the increased markers but not have the neurological signs or symptoms. So I thought there were lots of questions as well,” said Dr. van der Flier, professor of neurology at Amsterdam University Medical Center.
She noted that researchers at her institution in Amsterdam have observed similar relationships, and that the associations between neurological complications and plasma biomarkers over time will be an important topic of study.
The work could provide more information on neurological manifestations of long COVID, such as long-haul fatigue. “You might also think that’s some response in their brain. It would be great if we could actually capture that [using biomarkers],” said Dr. van der Flier.
Ms. Cooper and Dr. van der Flier have no relevant financial disclosures.
SAN DIEGO – Even after recovery of an acute COVID-19 infection, some patients experience extended or even long-term symptoms that can range from mild to debilitating. Some of these symptoms are neurological: headaches, brain fog, cognitive impairment, loss of taste or smell, and even cerebrovascular complications such stroke. There are even hints that COVID-19 infection could lead to future neurodegeneration.
Those issues have prompted efforts to identify biomarkers that can help track and monitor neurological complications of COVID-19. “Throughout the course of the pandemic, it has become apparent that COVID-19 can cause various neurological symptoms. Because of this, ,” Jennifer Cooper said during a lecture at the Alzheimer’s Association International Conference. She presented new research suggesting that neurofilament light (NfL) and glial fibrillary acidic protein (GFAP) may prove useful.
Ms. Cooper is a master’s degree student at the University of British Columbia and Canada.
Looking for sensitivity and specificity in plasma biomarkers
The researchers turned to plasma-based markers because they can reflect underlying pathology in the central nervous system. They focused on NfL, which reflects axonal damage, and GFAP, which is a marker of astrocyte activation.
The researchers analyzed data from 209 patients with COVID-19 who were admitted to the Vancouver (B.C.) General Hospital intensive care unit. Sixty-four percent were male, and the median age was 61 years. Sixty percent were ventilated, and 17% died.
The researchers determined if an individual patient’s biomarker level at hospital admission fell within a normal biomarker reference interval. A total of 53% had NfL levels outside the normal range, and 42% had GFAP levels outside the normal range. In addition, 31% of patients had both GFAP and NfL levels outside of the normal range.
Among all patients, 12% experienced ischemia, 4% hemorrhage, 2% seizures, and 10% degeneration.
At admission, NfL predicted a neurological complication with an area under the curve (AUC) of 0.702. GFAP had an AUC of 0.722. In combination, they had an AUC of 0.743. At 1 week, NfL had an AUC of 0.802, GFAP an AUC of 0.733, and the combination an AUC of 0.812.
Using age-specific cutoff values, the researchers found increased risks for neurological complications at admission (NfL odds ratio [OR], 2.9; GFAP OR, 1.6; combined OR, 2.1) and at 1 week (NfL OR, not significant; GFAP OR, 4.8; combined OR, 6.6). “We can see that both NFL and GFAP have utility in detecting neurological complications. And combining both of our markers improves detection at both time points. NfL is a marker that provides more sensitivity, where in this cohort GFAP is a marker that provides a little bit more specificity,” said Ms. Cooper.
Will additional biomarkers help?
The researchers are continuing to follow up patients at 6 months and 18 months post diagnosis, using neuropsychiatric tests and additional biomarker analysis, as well as PET and MRI scans. The patient sample is being expanded to those in the general hospital ward and some who were not hospitalized.
During the Q&A session, Ms. Cooper was asked if the group had collected reference data from patients who were admitted to the ICU with non-COVID disease. She responded that the group has some of that data, but as the pandemic went on they had difficulty finding patients who had never been infected with COVID to serve as reliable controls. To date, they have identified 33 controls who had a respiratory condition when admitted to the ICU. “What we see is the neurological biomarker levels in COVID are slightly lower than those with another respiratory condition in the ICU. But the data has a massive spread and the significance is very small between the two groups,” said Ms. Cooper.
Unanswered questions
The study is interesting, but leaves a lot of unanswered questions, according to Wiesje van der Flier, PhD, who moderated the session where the study was presented. “There are a lot of unknowns still: Will [the biomarkers] become normal again, once the COVID is over? Also, there was an increased risk, but it was not a one-to-one correspondence, so you can also have the increased markers but not have the neurological signs or symptoms. So I thought there were lots of questions as well,” said Dr. van der Flier, professor of neurology at Amsterdam University Medical Center.
She noted that researchers at her institution in Amsterdam have observed similar relationships, and that the associations between neurological complications and plasma biomarkers over time will be an important topic of study.
The work could provide more information on neurological manifestations of long COVID, such as long-haul fatigue. “You might also think that’s some response in their brain. It would be great if we could actually capture that [using biomarkers],” said Dr. van der Flier.
Ms. Cooper and Dr. van der Flier have no relevant financial disclosures.
SAN DIEGO – Even after recovery of an acute COVID-19 infection, some patients experience extended or even long-term symptoms that can range from mild to debilitating. Some of these symptoms are neurological: headaches, brain fog, cognitive impairment, loss of taste or smell, and even cerebrovascular complications such stroke. There are even hints that COVID-19 infection could lead to future neurodegeneration.
Those issues have prompted efforts to identify biomarkers that can help track and monitor neurological complications of COVID-19. “Throughout the course of the pandemic, it has become apparent that COVID-19 can cause various neurological symptoms. Because of this, ,” Jennifer Cooper said during a lecture at the Alzheimer’s Association International Conference. She presented new research suggesting that neurofilament light (NfL) and glial fibrillary acidic protein (GFAP) may prove useful.
Ms. Cooper is a master’s degree student at the University of British Columbia and Canada.
Looking for sensitivity and specificity in plasma biomarkers
The researchers turned to plasma-based markers because they can reflect underlying pathology in the central nervous system. They focused on NfL, which reflects axonal damage, and GFAP, which is a marker of astrocyte activation.
The researchers analyzed data from 209 patients with COVID-19 who were admitted to the Vancouver (B.C.) General Hospital intensive care unit. Sixty-four percent were male, and the median age was 61 years. Sixty percent were ventilated, and 17% died.
The researchers determined if an individual patient’s biomarker level at hospital admission fell within a normal biomarker reference interval. A total of 53% had NfL levels outside the normal range, and 42% had GFAP levels outside the normal range. In addition, 31% of patients had both GFAP and NfL levels outside of the normal range.
Among all patients, 12% experienced ischemia, 4% hemorrhage, 2% seizures, and 10% degeneration.
At admission, NfL predicted a neurological complication with an area under the curve (AUC) of 0.702. GFAP had an AUC of 0.722. In combination, they had an AUC of 0.743. At 1 week, NfL had an AUC of 0.802, GFAP an AUC of 0.733, and the combination an AUC of 0.812.
Using age-specific cutoff values, the researchers found increased risks for neurological complications at admission (NfL odds ratio [OR], 2.9; GFAP OR, 1.6; combined OR, 2.1) and at 1 week (NfL OR, not significant; GFAP OR, 4.8; combined OR, 6.6). “We can see that both NFL and GFAP have utility in detecting neurological complications. And combining both of our markers improves detection at both time points. NfL is a marker that provides more sensitivity, where in this cohort GFAP is a marker that provides a little bit more specificity,” said Ms. Cooper.
Will additional biomarkers help?
The researchers are continuing to follow up patients at 6 months and 18 months post diagnosis, using neuropsychiatric tests and additional biomarker analysis, as well as PET and MRI scans. The patient sample is being expanded to those in the general hospital ward and some who were not hospitalized.
During the Q&A session, Ms. Cooper was asked if the group had collected reference data from patients who were admitted to the ICU with non-COVID disease. She responded that the group has some of that data, but as the pandemic went on they had difficulty finding patients who had never been infected with COVID to serve as reliable controls. To date, they have identified 33 controls who had a respiratory condition when admitted to the ICU. “What we see is the neurological biomarker levels in COVID are slightly lower than those with another respiratory condition in the ICU. But the data has a massive spread and the significance is very small between the two groups,” said Ms. Cooper.
Unanswered questions
The study is interesting, but leaves a lot of unanswered questions, according to Wiesje van der Flier, PhD, who moderated the session where the study was presented. “There are a lot of unknowns still: Will [the biomarkers] become normal again, once the COVID is over? Also, there was an increased risk, but it was not a one-to-one correspondence, so you can also have the increased markers but not have the neurological signs or symptoms. So I thought there were lots of questions as well,” said Dr. van der Flier, professor of neurology at Amsterdam University Medical Center.
She noted that researchers at her institution in Amsterdam have observed similar relationships, and that the associations between neurological complications and plasma biomarkers over time will be an important topic of study.
The work could provide more information on neurological manifestations of long COVID, such as long-haul fatigue. “You might also think that’s some response in their brain. It would be great if we could actually capture that [using biomarkers],” said Dr. van der Flier.
Ms. Cooper and Dr. van der Flier have no relevant financial disclosures.
AT AAIC 2022
Guidance From the National Psoriasis Foundation COVID-19 Task Force
When COVID-19 emerged in March 2020, physicians were forced to evaluate the potential impacts of the pandemic on our patients and the conditions that we treat. For dermatologists, psoriasis came into particular focus, as many patients were being treated with biologic therapies. The initial concern was that these biologics might render our patients more susceptible to both COVID-19 infection and/or a more severe disease course.
In early 2020, the National Psoriasis Foundation (NPF) presented its own recommendations for treating patients with psoriatic disease during the pandemic.1 Some highlights included the following1:
• At the time, it was stipulated that patients with COVID-19 infection should stop taking a biologic.
• Psoriasis patients in high-risk groups (eg, concomitant systemic disease) should discuss with their dermatologist if their therapeutic regimen should be continued or altered.
• Patients taking oral immunosuppressive therapy may be at greater risk for COVID-19 infection, though there is no strong COVID-19–related evidence to provide specific guidelines or risk level.
In May 2020, the NPF COVID-19 Task Force was formed. This group—chaired by dermatologist Joel M. Gelfand, MD, MSCE (Philadelphia, Pennsylvania), and rheumatologist Christopher T. Ritchlin, MD, MPH (Rochester, New York)—was comprised of members from both the NPF Medical Board and Scientific Advisory Committee in dermatology, rheumatology, infectious disease, and critical care. The NPF COVID-19 Task Force has been critical in keeping the dermatology community apprised of the latest scientific thinking related to COVID-19 and publishing guidance statements that are updated and amended on a regular basis as new data becomes available.2 Key recommendations most relevant to the daily care of patients with psoriatic disease included the following2:
• Patients with psoriasis and/or psoriatic arthritis have similar rates of SARS-CoV-2 infection and COVID-19 outcomes as the general population based on existing data, with some exceptions.
• Therapies for psoriasis and/or psoriatic arthritis do not meaningfully alter the risk for acquiring SARS-CoV-2 infection or having worse COVID-19 outcomes.
• Patients should continue their biologic or oral therapies for psoriasis and/or psoriatic arthritis in most cases, unless they become infected with SARS-CoV-2.
• Chronic systemic steroid use for psoriatic disease in the setting of acute infection with COVID-19 may be associated with worse outcomes; however, steroids may improve outcomes for COVID-19 when initiated in hospitalized patients who require oxygen therapy.
• When local restrictions or pandemic conditions limit the ability for in-person visits, offer telemedicine to manage patients.
• Patients with psoriatic disease who do not have contraindications to vaccination should receive a messenger RNA (mRNA)–based COVID-19 vaccine and boosters, based on federal, state, and local guidance. Systemic medications for psoriasis or psoriatic arthritis are not a contraindication to the mRNA-based COVID-19 vaccine.
• Patients who are to receive an mRNA-based COVID-19 vaccine should continue their biologic or oral therapies for psoriasis and/or psoriatic arthritis in most cases.
• The use of hydroxychloroquine, chloroquine, and ivermectin is not suggested for the prevention or treatment of COVID-19 disease.
These guidelines have been critical in addressing some of the most pressing issues in psoriasis patient care, particularly the susceptibility to COVID-19, the role of psoriasis therapies in initial infection and health outcomes, and issues related to the administration of vaccines in those on systemic therapies. Based on these recommendations, we have been given a solid foundation that our current standard of care can (for the most part) continue with the continued presence of COVID-19 in our society. I encourage all providers to familiarize themselves with the NPF COVID-19 Task Force guidelines and keep abreast of updates as they become available (https://www.psoriasis.org/covid-19-task-force-guidance-statements/).
- Gelfand JM, Armstrong AW, Bell S, et al. National Psoriasis Foundation COVID-19 Task Force guidance for management of psoriatic disease during the pandemic: version 1. J Am Acad Dermatol. 2020;83:1704-1716.
- COVID-19 Task Force guidance statements. National Psoriasis Foundation website. Updated April 28, 2022. Accessed July 12, 2022. https://www.psoriasis.org/covid-19-task-force-guidance-statements/
When COVID-19 emerged in March 2020, physicians were forced to evaluate the potential impacts of the pandemic on our patients and the conditions that we treat. For dermatologists, psoriasis came into particular focus, as many patients were being treated with biologic therapies. The initial concern was that these biologics might render our patients more susceptible to both COVID-19 infection and/or a more severe disease course.
In early 2020, the National Psoriasis Foundation (NPF) presented its own recommendations for treating patients with psoriatic disease during the pandemic.1 Some highlights included the following1:
• At the time, it was stipulated that patients with COVID-19 infection should stop taking a biologic.
• Psoriasis patients in high-risk groups (eg, concomitant systemic disease) should discuss with their dermatologist if their therapeutic regimen should be continued or altered.
• Patients taking oral immunosuppressive therapy may be at greater risk for COVID-19 infection, though there is no strong COVID-19–related evidence to provide specific guidelines or risk level.
In May 2020, the NPF COVID-19 Task Force was formed. This group—chaired by dermatologist Joel M. Gelfand, MD, MSCE (Philadelphia, Pennsylvania), and rheumatologist Christopher T. Ritchlin, MD, MPH (Rochester, New York)—was comprised of members from both the NPF Medical Board and Scientific Advisory Committee in dermatology, rheumatology, infectious disease, and critical care. The NPF COVID-19 Task Force has been critical in keeping the dermatology community apprised of the latest scientific thinking related to COVID-19 and publishing guidance statements that are updated and amended on a regular basis as new data becomes available.2 Key recommendations most relevant to the daily care of patients with psoriatic disease included the following2:
• Patients with psoriasis and/or psoriatic arthritis have similar rates of SARS-CoV-2 infection and COVID-19 outcomes as the general population based on existing data, with some exceptions.
• Therapies for psoriasis and/or psoriatic arthritis do not meaningfully alter the risk for acquiring SARS-CoV-2 infection or having worse COVID-19 outcomes.
• Patients should continue their biologic or oral therapies for psoriasis and/or psoriatic arthritis in most cases, unless they become infected with SARS-CoV-2.
• Chronic systemic steroid use for psoriatic disease in the setting of acute infection with COVID-19 may be associated with worse outcomes; however, steroids may improve outcomes for COVID-19 when initiated in hospitalized patients who require oxygen therapy.
• When local restrictions or pandemic conditions limit the ability for in-person visits, offer telemedicine to manage patients.
• Patients with psoriatic disease who do not have contraindications to vaccination should receive a messenger RNA (mRNA)–based COVID-19 vaccine and boosters, based on federal, state, and local guidance. Systemic medications for psoriasis or psoriatic arthritis are not a contraindication to the mRNA-based COVID-19 vaccine.
• Patients who are to receive an mRNA-based COVID-19 vaccine should continue their biologic or oral therapies for psoriasis and/or psoriatic arthritis in most cases.
• The use of hydroxychloroquine, chloroquine, and ivermectin is not suggested for the prevention or treatment of COVID-19 disease.
These guidelines have been critical in addressing some of the most pressing issues in psoriasis patient care, particularly the susceptibility to COVID-19, the role of psoriasis therapies in initial infection and health outcomes, and issues related to the administration of vaccines in those on systemic therapies. Based on these recommendations, we have been given a solid foundation that our current standard of care can (for the most part) continue with the continued presence of COVID-19 in our society. I encourage all providers to familiarize themselves with the NPF COVID-19 Task Force guidelines and keep abreast of updates as they become available (https://www.psoriasis.org/covid-19-task-force-guidance-statements/).
When COVID-19 emerged in March 2020, physicians were forced to evaluate the potential impacts of the pandemic on our patients and the conditions that we treat. For dermatologists, psoriasis came into particular focus, as many patients were being treated with biologic therapies. The initial concern was that these biologics might render our patients more susceptible to both COVID-19 infection and/or a more severe disease course.
In early 2020, the National Psoriasis Foundation (NPF) presented its own recommendations for treating patients with psoriatic disease during the pandemic.1 Some highlights included the following1:
• At the time, it was stipulated that patients with COVID-19 infection should stop taking a biologic.
• Psoriasis patients in high-risk groups (eg, concomitant systemic disease) should discuss with their dermatologist if their therapeutic regimen should be continued or altered.
• Patients taking oral immunosuppressive therapy may be at greater risk for COVID-19 infection, though there is no strong COVID-19–related evidence to provide specific guidelines or risk level.
In May 2020, the NPF COVID-19 Task Force was formed. This group—chaired by dermatologist Joel M. Gelfand, MD, MSCE (Philadelphia, Pennsylvania), and rheumatologist Christopher T. Ritchlin, MD, MPH (Rochester, New York)—was comprised of members from both the NPF Medical Board and Scientific Advisory Committee in dermatology, rheumatology, infectious disease, and critical care. The NPF COVID-19 Task Force has been critical in keeping the dermatology community apprised of the latest scientific thinking related to COVID-19 and publishing guidance statements that are updated and amended on a regular basis as new data becomes available.2 Key recommendations most relevant to the daily care of patients with psoriatic disease included the following2:
• Patients with psoriasis and/or psoriatic arthritis have similar rates of SARS-CoV-2 infection and COVID-19 outcomes as the general population based on existing data, with some exceptions.
• Therapies for psoriasis and/or psoriatic arthritis do not meaningfully alter the risk for acquiring SARS-CoV-2 infection or having worse COVID-19 outcomes.
• Patients should continue their biologic or oral therapies for psoriasis and/or psoriatic arthritis in most cases, unless they become infected with SARS-CoV-2.
• Chronic systemic steroid use for psoriatic disease in the setting of acute infection with COVID-19 may be associated with worse outcomes; however, steroids may improve outcomes for COVID-19 when initiated in hospitalized patients who require oxygen therapy.
• When local restrictions or pandemic conditions limit the ability for in-person visits, offer telemedicine to manage patients.
• Patients with psoriatic disease who do not have contraindications to vaccination should receive a messenger RNA (mRNA)–based COVID-19 vaccine and boosters, based on federal, state, and local guidance. Systemic medications for psoriasis or psoriatic arthritis are not a contraindication to the mRNA-based COVID-19 vaccine.
• Patients who are to receive an mRNA-based COVID-19 vaccine should continue their biologic or oral therapies for psoriasis and/or psoriatic arthritis in most cases.
• The use of hydroxychloroquine, chloroquine, and ivermectin is not suggested for the prevention or treatment of COVID-19 disease.
These guidelines have been critical in addressing some of the most pressing issues in psoriasis patient care, particularly the susceptibility to COVID-19, the role of psoriasis therapies in initial infection and health outcomes, and issues related to the administration of vaccines in those on systemic therapies. Based on these recommendations, we have been given a solid foundation that our current standard of care can (for the most part) continue with the continued presence of COVID-19 in our society. I encourage all providers to familiarize themselves with the NPF COVID-19 Task Force guidelines and keep abreast of updates as they become available (https://www.psoriasis.org/covid-19-task-force-guidance-statements/).
- Gelfand JM, Armstrong AW, Bell S, et al. National Psoriasis Foundation COVID-19 Task Force guidance for management of psoriatic disease during the pandemic: version 1. J Am Acad Dermatol. 2020;83:1704-1716.
- COVID-19 Task Force guidance statements. National Psoriasis Foundation website. Updated April 28, 2022. Accessed July 12, 2022. https://www.psoriasis.org/covid-19-task-force-guidance-statements/
- Gelfand JM, Armstrong AW, Bell S, et al. National Psoriasis Foundation COVID-19 Task Force guidance for management of psoriatic disease during the pandemic: version 1. J Am Acad Dermatol. 2020;83:1704-1716.
- COVID-19 Task Force guidance statements. National Psoriasis Foundation website. Updated April 28, 2022. Accessed July 12, 2022. https://www.psoriasis.org/covid-19-task-force-guidance-statements/
Children and COVID: Severe illness rising as vaccination effort stalls
, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
After new child cases jumped by 22% during the week of July 15-21, the two successive weeks have produced increases of 3.9% (July 22-29) and 1.2% (July 30-Aug. 4). The latest weekly count from all states and territories still reporting was 96,599, the AAP and CHA said in their weekly COVID report, noting that several states have stopped reporting child cases and that others are reporting every other week.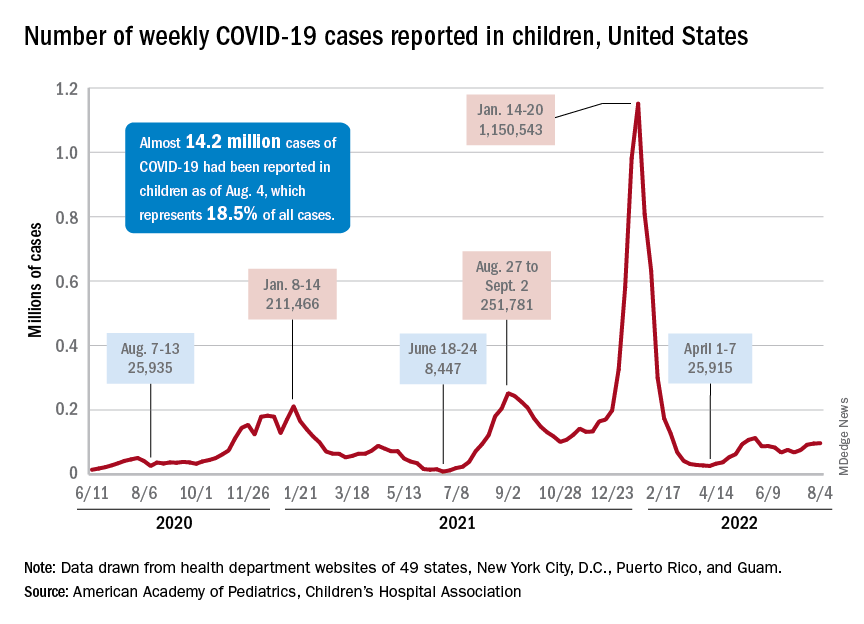
The deceleration in new cases, however, does not apply to emergency department visits and hospital admissions. The proportion of ED visits with diagnosed COVID rose steadily throughout June and July, as 7-day averages went from 2.6% on June 1 to 6.3% on July 31 for children aged 0-11 years, from 2.1% to 3.1% for children aged 12-15, and from 2.4% to 3.5% for 16- to 17-year-olds, according to data from the Centers for Disease Control and Prevention.
The rate of new admissions with confirmed COVID, which reached 0.46 per 100,000 population for children aged 0-17 years on July 30, has more than tripled since early April, when it had fallen to 0.13 per 100,000 in the wake of the Omicron surge, the CDC reported on its COVID Data Tracker.
A smaller but more detailed sample of children from the COVID-19–Associated Hospitalization Network (COVID-NET), which covers nearly 100 counties in 14 states, indicates that the increase in new admissions is occurring almost entirely among children aged 0-4 years, who had a rate of 5.6 per 100,000 for the week of July 17-23, compared with 0.8 per 100,000 for 5- to 11-year-olds and 1.5 per 100,000 for those aged 12-17, the CDC said.
Vaccine’s summer rollout gets lukewarm reception
As a group, children aged 0-4 years have not exactly flocked to the COVID-19 vaccine. As of Aug. 2 – about 6 weeks since the vaccine was authorized for children aged 6 months to 4 years – just 3.8% of those eligible had received at least one dose. Among children aged 5-11 the corresponding number on Aug. 2 was 37.4%, and for those aged 12-17 years it was 70.3%, the CDC data show.
That 3.8% of children aged less than 5 years represents almost 756,000 initial doses. That compares with over 6 million children aged 5-11 years who had received at least one dose through the first 6 weeks of their vaccination experience and over 5 million children aged 12-15, according to the COVID Data Tracker.
, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
After new child cases jumped by 22% during the week of July 15-21, the two successive weeks have produced increases of 3.9% (July 22-29) and 1.2% (July 30-Aug. 4). The latest weekly count from all states and territories still reporting was 96,599, the AAP and CHA said in their weekly COVID report, noting that several states have stopped reporting child cases and that others are reporting every other week.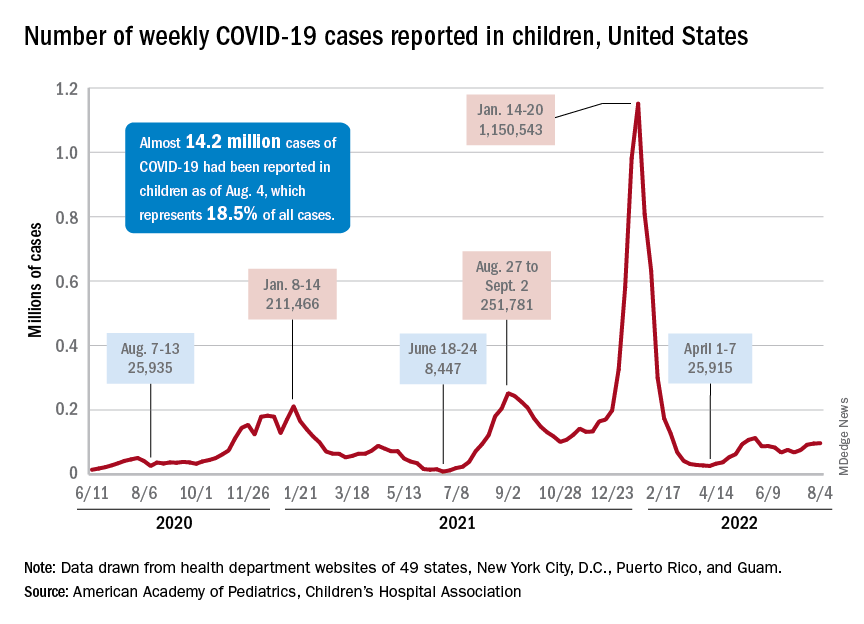
The deceleration in new cases, however, does not apply to emergency department visits and hospital admissions. The proportion of ED visits with diagnosed COVID rose steadily throughout June and July, as 7-day averages went from 2.6% on June 1 to 6.3% on July 31 for children aged 0-11 years, from 2.1% to 3.1% for children aged 12-15, and from 2.4% to 3.5% for 16- to 17-year-olds, according to data from the Centers for Disease Control and Prevention.
The rate of new admissions with confirmed COVID, which reached 0.46 per 100,000 population for children aged 0-17 years on July 30, has more than tripled since early April, when it had fallen to 0.13 per 100,000 in the wake of the Omicron surge, the CDC reported on its COVID Data Tracker.
A smaller but more detailed sample of children from the COVID-19–Associated Hospitalization Network (COVID-NET), which covers nearly 100 counties in 14 states, indicates that the increase in new admissions is occurring almost entirely among children aged 0-4 years, who had a rate of 5.6 per 100,000 for the week of July 17-23, compared with 0.8 per 100,000 for 5- to 11-year-olds and 1.5 per 100,000 for those aged 12-17, the CDC said.
Vaccine’s summer rollout gets lukewarm reception
As a group, children aged 0-4 years have not exactly flocked to the COVID-19 vaccine. As of Aug. 2 – about 6 weeks since the vaccine was authorized for children aged 6 months to 4 years – just 3.8% of those eligible had received at least one dose. Among children aged 5-11 the corresponding number on Aug. 2 was 37.4%, and for those aged 12-17 years it was 70.3%, the CDC data show.
That 3.8% of children aged less than 5 years represents almost 756,000 initial doses. That compares with over 6 million children aged 5-11 years who had received at least one dose through the first 6 weeks of their vaccination experience and over 5 million children aged 12-15, according to the COVID Data Tracker.
, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
After new child cases jumped by 22% during the week of July 15-21, the two successive weeks have produced increases of 3.9% (July 22-29) and 1.2% (July 30-Aug. 4). The latest weekly count from all states and territories still reporting was 96,599, the AAP and CHA said in their weekly COVID report, noting that several states have stopped reporting child cases and that others are reporting every other week.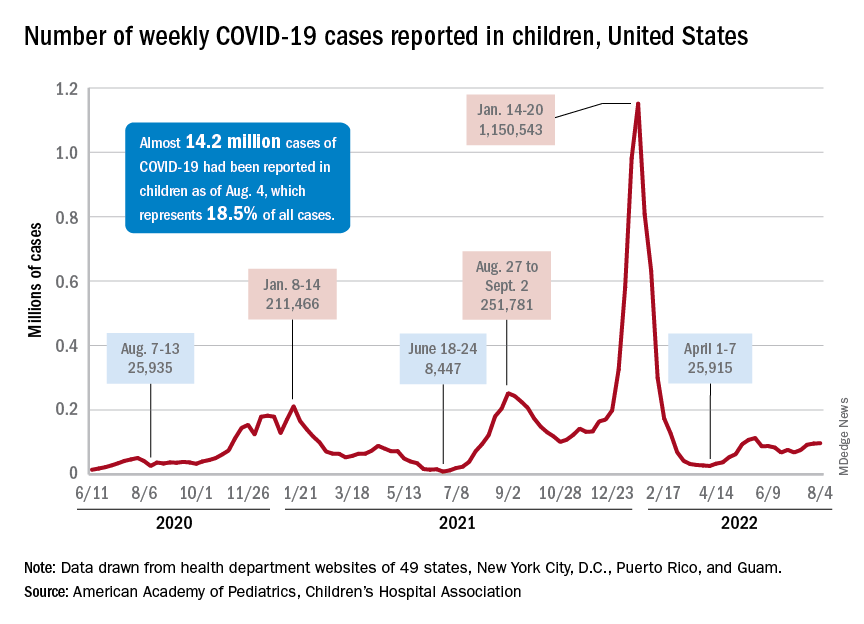
The deceleration in new cases, however, does not apply to emergency department visits and hospital admissions. The proportion of ED visits with diagnosed COVID rose steadily throughout June and July, as 7-day averages went from 2.6% on June 1 to 6.3% on July 31 for children aged 0-11 years, from 2.1% to 3.1% for children aged 12-15, and from 2.4% to 3.5% for 16- to 17-year-olds, according to data from the Centers for Disease Control and Prevention.
The rate of new admissions with confirmed COVID, which reached 0.46 per 100,000 population for children aged 0-17 years on July 30, has more than tripled since early April, when it had fallen to 0.13 per 100,000 in the wake of the Omicron surge, the CDC reported on its COVID Data Tracker.
A smaller but more detailed sample of children from the COVID-19–Associated Hospitalization Network (COVID-NET), which covers nearly 100 counties in 14 states, indicates that the increase in new admissions is occurring almost entirely among children aged 0-4 years, who had a rate of 5.6 per 100,000 for the week of July 17-23, compared with 0.8 per 100,000 for 5- to 11-year-olds and 1.5 per 100,000 for those aged 12-17, the CDC said.
Vaccine’s summer rollout gets lukewarm reception
As a group, children aged 0-4 years have not exactly flocked to the COVID-19 vaccine. As of Aug. 2 – about 6 weeks since the vaccine was authorized for children aged 6 months to 4 years – just 3.8% of those eligible had received at least one dose. Among children aged 5-11 the corresponding number on Aug. 2 was 37.4%, and for those aged 12-17 years it was 70.3%, the CDC data show.
That 3.8% of children aged less than 5 years represents almost 756,000 initial doses. That compares with over 6 million children aged 5-11 years who had received at least one dose through the first 6 weeks of their vaccination experience and over 5 million children aged 12-15, according to the COVID Data Tracker.
Updates on treatment/prevention of VTE in cancer patients
Updated clinical practice guidelines for the treatment and prevention of venous thromboembolism for patients with cancer, including those with cancer and COVID-19, have been released by the International Initiative on Thrombosis and Cancer (ITAC), an academic working group of VTE experts.
“Because patients with cancer have a baseline increased risk of VTE, compared with patients without cancer, the combination of both COVID-19 and cancer – and its effect on VTE risk and treatment – is of concern,” said the authors, led by Dominique Farge, MD, PhD, Nord Universite de Paris.
they added.
The new guidelines were published online in The Lancet Oncology.
“Cancer-associated VTE remains an important clinical problem, associated with increased morbidity and mortality,” Dr. Farge and colleagues observed.
“The ITAC guidelines’ companion free web-based mobile application will assist the practicing clinician with decision making at various levels to provide optimal care of patients with cancer to treat and prevent VTE,” they emphasized. More information is available at itaccme.com.
Cancer patients with COVID
The new section of the guidelines notes that the treatment and prevention of VTE for cancer patients infected with SARS-CoV-2 remain the same as for patients without COVID.
Whether or not cancer patients with COVID-19 are hospitalized, have been discharged, or are ambulatory, they should be assessed for the risk of VTE, as should any other patient. For cancer patients with COVID-19 who are hospitalized, pharmacologic prophylaxis should be given at the same dose and anticoagulant type as for hospitalized cancer patients who do not have COVID-19.
Following discharge, VTE prophylaxis is not advised for cancer patients infected with SARS-CoV-2, and routine primary pharmacologic prophylaxis of VTE for ambulatory patients with COVID-19 is also not recommended, the authors noted.
Initial treatment of established VTE
Initial treatment of established VTE for up to 10 days of anticoagulation should include low-molecular-weight heparin (LMWH) when creatinine clearance is at least 30 mL/min.
“A regimen of LMWH, taken once per day, is recommended unless a twice-per-day regimen is required because of patients’ characteristics,” the authors noted. These characteristics include a high risk of bleeding, moderate renal failure, and the need for technical intervention, including surgery.
If a twice-a-day regimen is required, only enoxaparin at a dose of 1 mg/kg twice daily can be used, the authors cautioned.
For patients with a low risk of gastrointestinal or genitourinary bleeding, rivaroxaban (Xarelto) or apixaban (Eliquis) can be given in the first 10 days, as well as edoxaban (Lixiana). The latter should be started after at least 5 days of parenteral anticoagulation, provided creatinine clearance is at least 30 mL/min.
“Unfractionated heparin as well as fondaparinux (GlaxoSmithKline) can be also used for the initial treatment of established VTE when LMWH or direct oral anticoagulants are contraindicated,” Dr. Farge and colleagues wrote.
Thrombolysis can be considered on a case-by-case basis, although physicians must pay attention to specific contraindications, especially bleeding risk.
“In the initial treatment of VTE, inferior vena cava filters might be considered when anticoagulant treatment is contraindicated or, in the case of pulmonary embolism, when recurrence occurs under optimal anticoagulation,” the authors noted.
Maintenance VTE treatment
For maintenance therapy, which the authors define as early maintenance for up to 6 months and long-term maintenance beyond 6 months, they point out that LMWHs are preferred over vitamin K antagonists for the treatment of VTE when the creatinine clearance is again at least 30 mL/min.
Any of the direct oral anticoagulants (DOAs) – edoxaban, rivaroxaban, or apixaban – is also recommended for the same patients, provided there is no risk of inducing a strong drug-drug interaction or GI absorption is impaired.
However, the DOAs should be used with caution for patients with GI malignancies, especially upper GI cancers, because data show there is an increased risk of GI bleeding with both edoxaban and rivaroxaban.
“LMWH or direct oral anticoagulants should be used for a minimum of 6 months to treat established VTE in patients with cancer,” the authors wrote.
“After 6 months, termination or continuation of anticoagulation (LMWH, direct oral anticoagulants, or vitamin K antagonists) should be based on individual evaluation of the benefit-risk ratio,” they added.
Treatment of VTE recurrence
The guideline authors explain that three options can be considered in the event of VTE recurrence. These include an increase in the LMWH dose by 20%-25%, or a switch to a DOA, or, if patients are taking a DOA, a switch to an LMWH. If the patient is taking a vitamin K antagonist, it can be switched to either an LMWH or a DOA.
For treatment of catheter-related thrombosis, anticoagulant treatment is recommended for a minimum of 3 months and as long as the central venous catheter is in place. In this setting, the LMWHs are recommended.
The central venous catheter can be kept in place if it is functional, well positioned, and is not infected, provided there is good resolution of symptoms under close surveillance while anticoagulants are being administered.
In surgically treated patients, the LMWH, given once a day, to patients with a serum creatinine concentration of at least 30 mL/min can be used to prevent VTE. Alternatively, VTE can be prevented by the use low-dose unfractionated heparin, given three times a day.
“Pharmacological prophylaxis should be started 2-12 h preoperatively and continued for at least 7–10 days,” Dr. Farge and colleagues advised. In this setting, there is insufficient evidence to support the use of fondaparinux or a DOA as an alternative to an LMWH for the prophylaxis of postoperative VTE. “Use of the highest prophylactic dose of LMWH to prevent postoperative VTE in patients with cancer is recommended,” the authors advised.
Furthermore, extended prophylaxis of at least 4 weeks with LMWH is advised to prevent postoperative VTE after major abdominal or pelvic surgery. Mechanical methods are not recommended except when pharmacologic methods are contraindicated. Inferior vena cava filters are also not recommended for routine prophylaxis.
Patients with reduced mobility
For medically treated hospitalized patients with cancer whose mobility is reduced, the authors recommend prophylaxis with either an LMWH or fondaparinux, provided their creatinine clearance is at least 30 mL/min. These patients can also be treated with unfractionated heparin, they add.
In contrast, DOAs are not recommended – at least not routinely – in this setting, the authors cautioned. Primary pharmacologic prophylaxis of VTE with either LMWH or DOAs – either rivaroxaban or apixaban – is indicated in ambulatory patients with locally advanced or metastatic pancreatic cancer who are receiving systemic anticancer therapy, provided they are at low risk of bleeding.
However, primary pharmacologic prophylaxis with LMWH is not recommended outside of a clinical trial for patients with locally advanced or metastatic lung cancer who are undergoing systemic anticancer therapy, even for patients who are at low risk of bleeding.
For ambulatory patients who are receiving systemic anticancer therapy and who are at intermediate risk of VTE, primary prophylaxis with rivaroxaban or apixaban is recommended for those with myeloma who are receiving immunomodulatory therapy plus steroids or other systemic therapies.
In this setting, oral anticoagulants should consist of a vitamin K antagonist, given at low or therapeutic doses, or apixaban, given at prophylactic doses. Alternatively, LMWH, given at prophylactic doses, or low-dose aspirin, given at a dose of 100 mg/day, can be used.
Catheter-related thrombosis
Use of anticoagulation for routine prophylaxis of catheter-related thrombosis is not recommended. Catheters should be inserted on the right side in the jugular vein, and the distal extremity of the central catheter should be located at the junction of the superior vena cava and the right atrium. “In patients requiring central venous catheters, we suggest the use of implanted ports over peripheral inserted central catheter lines,” the authors noted.
The authors described a number of unique situations regarding the treatment of VTE. These situations include patients with a brain tumor, for whom treatment of established VTE should favor either LMWH or a DOA. The authors also recommended the use of LMWH or unfractionated heparin, started postoperatively, for the prevention of VTE for patients undergoing neurosurgery.
In contrast, pharmacologic prophylaxis of VTE in medically treated patients with a brain tumor who are not undergoing neurosurgery is not recommended. “In the presence of severe renal failure...we suggest using unfractionated heparin followed by early vitamin K antagonists (possibly from day 1) or LMWH adjusted to anti-Xa concentration of the treatment of established VTE,” Dr. Farge and colleagues wrote.
Anticoagulant treatment is also recommended for a minimum of 3 months for children with symptomatic catheter-related thrombosis and as long as the central venous catheter is in place. For children with acute lymphoblastic leukemia who are undergoing induction chemotherapy, LMWH is also recommended as thromboprophylaxis.
For children who require a central venous catheter, the authors suggested that physicians use implanted ports over peripherally inserted central lines.
A version of this article first appeared on Medscape.com.
Updated clinical practice guidelines for the treatment and prevention of venous thromboembolism for patients with cancer, including those with cancer and COVID-19, have been released by the International Initiative on Thrombosis and Cancer (ITAC), an academic working group of VTE experts.
“Because patients with cancer have a baseline increased risk of VTE, compared with patients without cancer, the combination of both COVID-19 and cancer – and its effect on VTE risk and treatment – is of concern,” said the authors, led by Dominique Farge, MD, PhD, Nord Universite de Paris.
they added.
The new guidelines were published online in The Lancet Oncology.
“Cancer-associated VTE remains an important clinical problem, associated with increased morbidity and mortality,” Dr. Farge and colleagues observed.
“The ITAC guidelines’ companion free web-based mobile application will assist the practicing clinician with decision making at various levels to provide optimal care of patients with cancer to treat and prevent VTE,” they emphasized. More information is available at itaccme.com.
Cancer patients with COVID
The new section of the guidelines notes that the treatment and prevention of VTE for cancer patients infected with SARS-CoV-2 remain the same as for patients without COVID.
Whether or not cancer patients with COVID-19 are hospitalized, have been discharged, or are ambulatory, they should be assessed for the risk of VTE, as should any other patient. For cancer patients with COVID-19 who are hospitalized, pharmacologic prophylaxis should be given at the same dose and anticoagulant type as for hospitalized cancer patients who do not have COVID-19.
Following discharge, VTE prophylaxis is not advised for cancer patients infected with SARS-CoV-2, and routine primary pharmacologic prophylaxis of VTE for ambulatory patients with COVID-19 is also not recommended, the authors noted.
Initial treatment of established VTE
Initial treatment of established VTE for up to 10 days of anticoagulation should include low-molecular-weight heparin (LMWH) when creatinine clearance is at least 30 mL/min.
“A regimen of LMWH, taken once per day, is recommended unless a twice-per-day regimen is required because of patients’ characteristics,” the authors noted. These characteristics include a high risk of bleeding, moderate renal failure, and the need for technical intervention, including surgery.
If a twice-a-day regimen is required, only enoxaparin at a dose of 1 mg/kg twice daily can be used, the authors cautioned.
For patients with a low risk of gastrointestinal or genitourinary bleeding, rivaroxaban (Xarelto) or apixaban (Eliquis) can be given in the first 10 days, as well as edoxaban (Lixiana). The latter should be started after at least 5 days of parenteral anticoagulation, provided creatinine clearance is at least 30 mL/min.
“Unfractionated heparin as well as fondaparinux (GlaxoSmithKline) can be also used for the initial treatment of established VTE when LMWH or direct oral anticoagulants are contraindicated,” Dr. Farge and colleagues wrote.
Thrombolysis can be considered on a case-by-case basis, although physicians must pay attention to specific contraindications, especially bleeding risk.
“In the initial treatment of VTE, inferior vena cava filters might be considered when anticoagulant treatment is contraindicated or, in the case of pulmonary embolism, when recurrence occurs under optimal anticoagulation,” the authors noted.
Maintenance VTE treatment
For maintenance therapy, which the authors define as early maintenance for up to 6 months and long-term maintenance beyond 6 months, they point out that LMWHs are preferred over vitamin K antagonists for the treatment of VTE when the creatinine clearance is again at least 30 mL/min.
Any of the direct oral anticoagulants (DOAs) – edoxaban, rivaroxaban, or apixaban – is also recommended for the same patients, provided there is no risk of inducing a strong drug-drug interaction or GI absorption is impaired.
However, the DOAs should be used with caution for patients with GI malignancies, especially upper GI cancers, because data show there is an increased risk of GI bleeding with both edoxaban and rivaroxaban.
“LMWH or direct oral anticoagulants should be used for a minimum of 6 months to treat established VTE in patients with cancer,” the authors wrote.
“After 6 months, termination or continuation of anticoagulation (LMWH, direct oral anticoagulants, or vitamin K antagonists) should be based on individual evaluation of the benefit-risk ratio,” they added.
Treatment of VTE recurrence
The guideline authors explain that three options can be considered in the event of VTE recurrence. These include an increase in the LMWH dose by 20%-25%, or a switch to a DOA, or, if patients are taking a DOA, a switch to an LMWH. If the patient is taking a vitamin K antagonist, it can be switched to either an LMWH or a DOA.
For treatment of catheter-related thrombosis, anticoagulant treatment is recommended for a minimum of 3 months and as long as the central venous catheter is in place. In this setting, the LMWHs are recommended.
The central venous catheter can be kept in place if it is functional, well positioned, and is not infected, provided there is good resolution of symptoms under close surveillance while anticoagulants are being administered.
In surgically treated patients, the LMWH, given once a day, to patients with a serum creatinine concentration of at least 30 mL/min can be used to prevent VTE. Alternatively, VTE can be prevented by the use low-dose unfractionated heparin, given three times a day.
“Pharmacological prophylaxis should be started 2-12 h preoperatively and continued for at least 7–10 days,” Dr. Farge and colleagues advised. In this setting, there is insufficient evidence to support the use of fondaparinux or a DOA as an alternative to an LMWH for the prophylaxis of postoperative VTE. “Use of the highest prophylactic dose of LMWH to prevent postoperative VTE in patients with cancer is recommended,” the authors advised.
Furthermore, extended prophylaxis of at least 4 weeks with LMWH is advised to prevent postoperative VTE after major abdominal or pelvic surgery. Mechanical methods are not recommended except when pharmacologic methods are contraindicated. Inferior vena cava filters are also not recommended for routine prophylaxis.
Patients with reduced mobility
For medically treated hospitalized patients with cancer whose mobility is reduced, the authors recommend prophylaxis with either an LMWH or fondaparinux, provided their creatinine clearance is at least 30 mL/min. These patients can also be treated with unfractionated heparin, they add.
In contrast, DOAs are not recommended – at least not routinely – in this setting, the authors cautioned. Primary pharmacologic prophylaxis of VTE with either LMWH or DOAs – either rivaroxaban or apixaban – is indicated in ambulatory patients with locally advanced or metastatic pancreatic cancer who are receiving systemic anticancer therapy, provided they are at low risk of bleeding.
However, primary pharmacologic prophylaxis with LMWH is not recommended outside of a clinical trial for patients with locally advanced or metastatic lung cancer who are undergoing systemic anticancer therapy, even for patients who are at low risk of bleeding.
For ambulatory patients who are receiving systemic anticancer therapy and who are at intermediate risk of VTE, primary prophylaxis with rivaroxaban or apixaban is recommended for those with myeloma who are receiving immunomodulatory therapy plus steroids or other systemic therapies.
In this setting, oral anticoagulants should consist of a vitamin K antagonist, given at low or therapeutic doses, or apixaban, given at prophylactic doses. Alternatively, LMWH, given at prophylactic doses, or low-dose aspirin, given at a dose of 100 mg/day, can be used.
Catheter-related thrombosis
Use of anticoagulation for routine prophylaxis of catheter-related thrombosis is not recommended. Catheters should be inserted on the right side in the jugular vein, and the distal extremity of the central catheter should be located at the junction of the superior vena cava and the right atrium. “In patients requiring central venous catheters, we suggest the use of implanted ports over peripheral inserted central catheter lines,” the authors noted.
The authors described a number of unique situations regarding the treatment of VTE. These situations include patients with a brain tumor, for whom treatment of established VTE should favor either LMWH or a DOA. The authors also recommended the use of LMWH or unfractionated heparin, started postoperatively, for the prevention of VTE for patients undergoing neurosurgery.
In contrast, pharmacologic prophylaxis of VTE in medically treated patients with a brain tumor who are not undergoing neurosurgery is not recommended. “In the presence of severe renal failure...we suggest using unfractionated heparin followed by early vitamin K antagonists (possibly from day 1) or LMWH adjusted to anti-Xa concentration of the treatment of established VTE,” Dr. Farge and colleagues wrote.
Anticoagulant treatment is also recommended for a minimum of 3 months for children with symptomatic catheter-related thrombosis and as long as the central venous catheter is in place. For children with acute lymphoblastic leukemia who are undergoing induction chemotherapy, LMWH is also recommended as thromboprophylaxis.
For children who require a central venous catheter, the authors suggested that physicians use implanted ports over peripherally inserted central lines.
A version of this article first appeared on Medscape.com.
Updated clinical practice guidelines for the treatment and prevention of venous thromboembolism for patients with cancer, including those with cancer and COVID-19, have been released by the International Initiative on Thrombosis and Cancer (ITAC), an academic working group of VTE experts.
“Because patients with cancer have a baseline increased risk of VTE, compared with patients without cancer, the combination of both COVID-19 and cancer – and its effect on VTE risk and treatment – is of concern,” said the authors, led by Dominique Farge, MD, PhD, Nord Universite de Paris.
they added.
The new guidelines were published online in The Lancet Oncology.
“Cancer-associated VTE remains an important clinical problem, associated with increased morbidity and mortality,” Dr. Farge and colleagues observed.
“The ITAC guidelines’ companion free web-based mobile application will assist the practicing clinician with decision making at various levels to provide optimal care of patients with cancer to treat and prevent VTE,” they emphasized. More information is available at itaccme.com.
Cancer patients with COVID
The new section of the guidelines notes that the treatment and prevention of VTE for cancer patients infected with SARS-CoV-2 remain the same as for patients without COVID.
Whether or not cancer patients with COVID-19 are hospitalized, have been discharged, or are ambulatory, they should be assessed for the risk of VTE, as should any other patient. For cancer patients with COVID-19 who are hospitalized, pharmacologic prophylaxis should be given at the same dose and anticoagulant type as for hospitalized cancer patients who do not have COVID-19.
Following discharge, VTE prophylaxis is not advised for cancer patients infected with SARS-CoV-2, and routine primary pharmacologic prophylaxis of VTE for ambulatory patients with COVID-19 is also not recommended, the authors noted.
Initial treatment of established VTE
Initial treatment of established VTE for up to 10 days of anticoagulation should include low-molecular-weight heparin (LMWH) when creatinine clearance is at least 30 mL/min.
“A regimen of LMWH, taken once per day, is recommended unless a twice-per-day regimen is required because of patients’ characteristics,” the authors noted. These characteristics include a high risk of bleeding, moderate renal failure, and the need for technical intervention, including surgery.
If a twice-a-day regimen is required, only enoxaparin at a dose of 1 mg/kg twice daily can be used, the authors cautioned.
For patients with a low risk of gastrointestinal or genitourinary bleeding, rivaroxaban (Xarelto) or apixaban (Eliquis) can be given in the first 10 days, as well as edoxaban (Lixiana). The latter should be started after at least 5 days of parenteral anticoagulation, provided creatinine clearance is at least 30 mL/min.
“Unfractionated heparin as well as fondaparinux (GlaxoSmithKline) can be also used for the initial treatment of established VTE when LMWH or direct oral anticoagulants are contraindicated,” Dr. Farge and colleagues wrote.
Thrombolysis can be considered on a case-by-case basis, although physicians must pay attention to specific contraindications, especially bleeding risk.
“In the initial treatment of VTE, inferior vena cava filters might be considered when anticoagulant treatment is contraindicated or, in the case of pulmonary embolism, when recurrence occurs under optimal anticoagulation,” the authors noted.
Maintenance VTE treatment
For maintenance therapy, which the authors define as early maintenance for up to 6 months and long-term maintenance beyond 6 months, they point out that LMWHs are preferred over vitamin K antagonists for the treatment of VTE when the creatinine clearance is again at least 30 mL/min.
Any of the direct oral anticoagulants (DOAs) – edoxaban, rivaroxaban, or apixaban – is also recommended for the same patients, provided there is no risk of inducing a strong drug-drug interaction or GI absorption is impaired.
However, the DOAs should be used with caution for patients with GI malignancies, especially upper GI cancers, because data show there is an increased risk of GI bleeding with both edoxaban and rivaroxaban.
“LMWH or direct oral anticoagulants should be used for a minimum of 6 months to treat established VTE in patients with cancer,” the authors wrote.
“After 6 months, termination or continuation of anticoagulation (LMWH, direct oral anticoagulants, or vitamin K antagonists) should be based on individual evaluation of the benefit-risk ratio,” they added.
Treatment of VTE recurrence
The guideline authors explain that three options can be considered in the event of VTE recurrence. These include an increase in the LMWH dose by 20%-25%, or a switch to a DOA, or, if patients are taking a DOA, a switch to an LMWH. If the patient is taking a vitamin K antagonist, it can be switched to either an LMWH or a DOA.
For treatment of catheter-related thrombosis, anticoagulant treatment is recommended for a minimum of 3 months and as long as the central venous catheter is in place. In this setting, the LMWHs are recommended.
The central venous catheter can be kept in place if it is functional, well positioned, and is not infected, provided there is good resolution of symptoms under close surveillance while anticoagulants are being administered.
In surgically treated patients, the LMWH, given once a day, to patients with a serum creatinine concentration of at least 30 mL/min can be used to prevent VTE. Alternatively, VTE can be prevented by the use low-dose unfractionated heparin, given three times a day.
“Pharmacological prophylaxis should be started 2-12 h preoperatively and continued for at least 7–10 days,” Dr. Farge and colleagues advised. In this setting, there is insufficient evidence to support the use of fondaparinux or a DOA as an alternative to an LMWH for the prophylaxis of postoperative VTE. “Use of the highest prophylactic dose of LMWH to prevent postoperative VTE in patients with cancer is recommended,” the authors advised.
Furthermore, extended prophylaxis of at least 4 weeks with LMWH is advised to prevent postoperative VTE after major abdominal or pelvic surgery. Mechanical methods are not recommended except when pharmacologic methods are contraindicated. Inferior vena cava filters are also not recommended for routine prophylaxis.
Patients with reduced mobility
For medically treated hospitalized patients with cancer whose mobility is reduced, the authors recommend prophylaxis with either an LMWH or fondaparinux, provided their creatinine clearance is at least 30 mL/min. These patients can also be treated with unfractionated heparin, they add.
In contrast, DOAs are not recommended – at least not routinely – in this setting, the authors cautioned. Primary pharmacologic prophylaxis of VTE with either LMWH or DOAs – either rivaroxaban or apixaban – is indicated in ambulatory patients with locally advanced or metastatic pancreatic cancer who are receiving systemic anticancer therapy, provided they are at low risk of bleeding.
However, primary pharmacologic prophylaxis with LMWH is not recommended outside of a clinical trial for patients with locally advanced or metastatic lung cancer who are undergoing systemic anticancer therapy, even for patients who are at low risk of bleeding.
For ambulatory patients who are receiving systemic anticancer therapy and who are at intermediate risk of VTE, primary prophylaxis with rivaroxaban or apixaban is recommended for those with myeloma who are receiving immunomodulatory therapy plus steroids or other systemic therapies.
In this setting, oral anticoagulants should consist of a vitamin K antagonist, given at low or therapeutic doses, or apixaban, given at prophylactic doses. Alternatively, LMWH, given at prophylactic doses, or low-dose aspirin, given at a dose of 100 mg/day, can be used.
Catheter-related thrombosis
Use of anticoagulation for routine prophylaxis of catheter-related thrombosis is not recommended. Catheters should be inserted on the right side in the jugular vein, and the distal extremity of the central catheter should be located at the junction of the superior vena cava and the right atrium. “In patients requiring central venous catheters, we suggest the use of implanted ports over peripheral inserted central catheter lines,” the authors noted.
The authors described a number of unique situations regarding the treatment of VTE. These situations include patients with a brain tumor, for whom treatment of established VTE should favor either LMWH or a DOA. The authors also recommended the use of LMWH or unfractionated heparin, started postoperatively, for the prevention of VTE for patients undergoing neurosurgery.
In contrast, pharmacologic prophylaxis of VTE in medically treated patients with a brain tumor who are not undergoing neurosurgery is not recommended. “In the presence of severe renal failure...we suggest using unfractionated heparin followed by early vitamin K antagonists (possibly from day 1) or LMWH adjusted to anti-Xa concentration of the treatment of established VTE,” Dr. Farge and colleagues wrote.
Anticoagulant treatment is also recommended for a minimum of 3 months for children with symptomatic catheter-related thrombosis and as long as the central venous catheter is in place. For children with acute lymphoblastic leukemia who are undergoing induction chemotherapy, LMWH is also recommended as thromboprophylaxis.
For children who require a central venous catheter, the authors suggested that physicians use implanted ports over peripherally inserted central lines.
A version of this article first appeared on Medscape.com.
FROM THE LANCET ONCOLOGY
How well do vaccines protect against long COVID?
New York City veterinarian Erin Kulick used to be a weekend warrior. Only 2½ years ago, the 38-year-old new mother played ultimate Frisbee and flag football with friends. She went for regular 30-minute runs to burn off stress.
Now, Dr. Kulick is usually so exhausted, she can’t walk nonstop for 15 minutes. She recently tried to take her 4-year-old son, Cooper, to the American Museum of Natural History for his first visit, but ended up on a bench outside the museum, sobbing in the rain, because she couldn’t even get through the first hurdle of standing in line. “I just wanted to be there with my kid,” she said.
Dr. Kulick got sick with COVID-19 at the start of the pandemic in March 2020, 9 months before the first vaccine would be approved. Now she is among the estimated one in five infected Americans, or 19%, whose symptoms developed into long COVID.
Dr. Kulick also is now vaccinated and boosted. Had a vaccine been available sooner, could it have protected her from long COVID?
Evidence is starting to show it’s likely.
“The best way not to have long COVID is not to have COVID at all,” said Leora Horwitz, MD, a professor of population health and medicine at New York University. “To the extent that vaccination can prevent you from getting COVID at all, then it helps to reduce long COVID.”
And People with more serious initial illness appear more likely to have prolonged symptoms, but those with milder disease can certainly get it, too.
“You’re more likely to have long COVID with more severe disease, and we have ample evidence that vaccination reduces the severity of disease,” Dr. Horwitz said. “We also now have quite a lot of evidence that vaccination does reduce your risk of long COVID – probably because it reduces your risk of severe disease.”
There is little consensus about how much vaccines can lower the risk of long-term COVID symptoms, but several studies suggest that number lies anywhere from 15% to more than 80%.
That might seem like a big variation, but infectious disease experts argue that trying to interpret the gap isn’t as important as noticing what’s consistent across all these studies: “Vaccines do offer some protection, but it’s incomplete,” said Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs St. Louis Health Care System. Dr. Al-Aly, who has led several large studies on long COVID, said focusing on the fact that vaccines do offer some protection is a much better public health message than looking at the different levels of risk.
“Vaccines do a miraculous job for what they were designed to do,” said Dr. Al-Aly. “Vaccines were designed to reduce the risk of hospitalization ... and for that, vaccines are still holding up, even with all the changes in the virus.”
Still, Elena Azzolini, MD, PhD, head of the Humanitas Research Hospital’s vaccination center in Milan, thinks some studies may have underestimated the level of long COVID protection from vaccines because of limits in the study methods, such as not including enough women, who are more affected by long COVID. Her recent study, which looked at 2,560 health care professionals working in nine Italian centers from March 2020 to April 2022, focused on the risk for healthy women and men in their 20s to their 70s.
In the paper, Dr. Azzolini and associates reported that two or three doses of vaccine reduced the risk of hospitalization from COVID-19 from 42% among those who are unvaccinated to 16%-17%. In other words, they found unvaccinated people in the study were nearly three times as likely to have serious symptoms for longer than 4 weeks.
But Dr. Azzolini and Dr. Al-Aly still say that, even for the vaccinated, as long as COVID is around, masks are necessary. That’s because current vaccines don’t do enough to reduce transmission, said Dr. Al-Aly. “The only way that can really help [stop] transmission is covering our nose and mouth with a mask.”
How vaccinations affect people who already have long COVID
Some long COVID patients have said they got better after they get boosted, while some say they’re getting worse, said Dr. Horwitz, who is also a lead investigator at the National Institutes of Health’s flagship RECOVER program, a 4-year research project to study long COVID across the United States. (The NIH is still recruiting volunteers for these studies, which are also open to people who have never had COVID.)
One study published in the British Medical Journal analyzed survey data of more than 28,000 people infected with COVID in the United Kingdom and found a 13% reduction in long-term symptoms after a first dose of the vaccine, although it was unclear from the data if the improvement was sustained.
A second dose was associated with another 8% improvement over a 2-month period. “It’s reassuring that we see an average modest improvement in symptoms, not an average worsening in symptoms,” said Daniel Ayoubkhani, principal statistician at the U.K. Office for National Statistics and lead author of the study. Of course, the experience will differ among different people.
“It doesn’t appear that vaccination is the silver bullet that’s going to eradicate long COVID,” he said, but evidence from multiple studies suggests vaccines may help people with long-term symptoms.
Akiko Iwasaki, PhD, an immunobiologist at Yale University, New Haven, Conn., told a White House summit in July that one of the best ways to prevent long COVID is to develop the next generation of vaccines that also prevent milder cases by blocking transmission in the first place.
Back in New York, Dr. Kulick is now triple vaccinated. She’s due for a fourth dose soon but admits she’s “terrified every time” that she’s going to get sicker.
In her Facebook support group for long COVID, she reads that most people with prolonged symptoms handle it well. She has also noticed some of her symptoms eased after her first two doses of vaccine.
Since being diagnosed, Dr. Kulick learned she has a genetic condition, Ehlers-Danlos syndrome, which affects connective tissues that support skin, joints, organs, and blood vessels, and which her doctors say may have made her more prone to long COVID. She’s also being screened for autoimmune diseases, but for now, the only relief she has found has come from long COVID physical therapy, changes to her diet, and integrative medicine.
Dr. Kulick is still trying to figure out how she can get better while keeping her long hours at her veterinary job – and her health benefits. She is thankful her husband is a devoted caregiver to their son and a professional jazz musician with a schedule that allows for some flexibility.
“But it’s really hard when every week feels like I’ve run a marathon,” she said. “I can barely make it through.”
A version of this article first appeared on WebMD.com.
New York City veterinarian Erin Kulick used to be a weekend warrior. Only 2½ years ago, the 38-year-old new mother played ultimate Frisbee and flag football with friends. She went for regular 30-minute runs to burn off stress.
Now, Dr. Kulick is usually so exhausted, she can’t walk nonstop for 15 minutes. She recently tried to take her 4-year-old son, Cooper, to the American Museum of Natural History for his first visit, but ended up on a bench outside the museum, sobbing in the rain, because she couldn’t even get through the first hurdle of standing in line. “I just wanted to be there with my kid,” she said.
Dr. Kulick got sick with COVID-19 at the start of the pandemic in March 2020, 9 months before the first vaccine would be approved. Now she is among the estimated one in five infected Americans, or 19%, whose symptoms developed into long COVID.
Dr. Kulick also is now vaccinated and boosted. Had a vaccine been available sooner, could it have protected her from long COVID?
Evidence is starting to show it’s likely.
“The best way not to have long COVID is not to have COVID at all,” said Leora Horwitz, MD, a professor of population health and medicine at New York University. “To the extent that vaccination can prevent you from getting COVID at all, then it helps to reduce long COVID.”
And People with more serious initial illness appear more likely to have prolonged symptoms, but those with milder disease can certainly get it, too.
“You’re more likely to have long COVID with more severe disease, and we have ample evidence that vaccination reduces the severity of disease,” Dr. Horwitz said. “We also now have quite a lot of evidence that vaccination does reduce your risk of long COVID – probably because it reduces your risk of severe disease.”
There is little consensus about how much vaccines can lower the risk of long-term COVID symptoms, but several studies suggest that number lies anywhere from 15% to more than 80%.
That might seem like a big variation, but infectious disease experts argue that trying to interpret the gap isn’t as important as noticing what’s consistent across all these studies: “Vaccines do offer some protection, but it’s incomplete,” said Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs St. Louis Health Care System. Dr. Al-Aly, who has led several large studies on long COVID, said focusing on the fact that vaccines do offer some protection is a much better public health message than looking at the different levels of risk.
“Vaccines do a miraculous job for what they were designed to do,” said Dr. Al-Aly. “Vaccines were designed to reduce the risk of hospitalization ... and for that, vaccines are still holding up, even with all the changes in the virus.”
Still, Elena Azzolini, MD, PhD, head of the Humanitas Research Hospital’s vaccination center in Milan, thinks some studies may have underestimated the level of long COVID protection from vaccines because of limits in the study methods, such as not including enough women, who are more affected by long COVID. Her recent study, which looked at 2,560 health care professionals working in nine Italian centers from March 2020 to April 2022, focused on the risk for healthy women and men in their 20s to their 70s.
In the paper, Dr. Azzolini and associates reported that two or three doses of vaccine reduced the risk of hospitalization from COVID-19 from 42% among those who are unvaccinated to 16%-17%. In other words, they found unvaccinated people in the study were nearly three times as likely to have serious symptoms for longer than 4 weeks.
But Dr. Azzolini and Dr. Al-Aly still say that, even for the vaccinated, as long as COVID is around, masks are necessary. That’s because current vaccines don’t do enough to reduce transmission, said Dr. Al-Aly. “The only way that can really help [stop] transmission is covering our nose and mouth with a mask.”
How vaccinations affect people who already have long COVID
Some long COVID patients have said they got better after they get boosted, while some say they’re getting worse, said Dr. Horwitz, who is also a lead investigator at the National Institutes of Health’s flagship RECOVER program, a 4-year research project to study long COVID across the United States. (The NIH is still recruiting volunteers for these studies, which are also open to people who have never had COVID.)
One study published in the British Medical Journal analyzed survey data of more than 28,000 people infected with COVID in the United Kingdom and found a 13% reduction in long-term symptoms after a first dose of the vaccine, although it was unclear from the data if the improvement was sustained.
A second dose was associated with another 8% improvement over a 2-month period. “It’s reassuring that we see an average modest improvement in symptoms, not an average worsening in symptoms,” said Daniel Ayoubkhani, principal statistician at the U.K. Office for National Statistics and lead author of the study. Of course, the experience will differ among different people.
“It doesn’t appear that vaccination is the silver bullet that’s going to eradicate long COVID,” he said, but evidence from multiple studies suggests vaccines may help people with long-term symptoms.
Akiko Iwasaki, PhD, an immunobiologist at Yale University, New Haven, Conn., told a White House summit in July that one of the best ways to prevent long COVID is to develop the next generation of vaccines that also prevent milder cases by blocking transmission in the first place.
Back in New York, Dr. Kulick is now triple vaccinated. She’s due for a fourth dose soon but admits she’s “terrified every time” that she’s going to get sicker.
In her Facebook support group for long COVID, she reads that most people with prolonged symptoms handle it well. She has also noticed some of her symptoms eased after her first two doses of vaccine.
Since being diagnosed, Dr. Kulick learned she has a genetic condition, Ehlers-Danlos syndrome, which affects connective tissues that support skin, joints, organs, and blood vessels, and which her doctors say may have made her more prone to long COVID. She’s also being screened for autoimmune diseases, but for now, the only relief she has found has come from long COVID physical therapy, changes to her diet, and integrative medicine.
Dr. Kulick is still trying to figure out how she can get better while keeping her long hours at her veterinary job – and her health benefits. She is thankful her husband is a devoted caregiver to their son and a professional jazz musician with a schedule that allows for some flexibility.
“But it’s really hard when every week feels like I’ve run a marathon,” she said. “I can barely make it through.”
A version of this article first appeared on WebMD.com.
New York City veterinarian Erin Kulick used to be a weekend warrior. Only 2½ years ago, the 38-year-old new mother played ultimate Frisbee and flag football with friends. She went for regular 30-minute runs to burn off stress.
Now, Dr. Kulick is usually so exhausted, she can’t walk nonstop for 15 minutes. She recently tried to take her 4-year-old son, Cooper, to the American Museum of Natural History for his first visit, but ended up on a bench outside the museum, sobbing in the rain, because she couldn’t even get through the first hurdle of standing in line. “I just wanted to be there with my kid,” she said.
Dr. Kulick got sick with COVID-19 at the start of the pandemic in March 2020, 9 months before the first vaccine would be approved. Now she is among the estimated one in five infected Americans, or 19%, whose symptoms developed into long COVID.
Dr. Kulick also is now vaccinated and boosted. Had a vaccine been available sooner, could it have protected her from long COVID?
Evidence is starting to show it’s likely.
“The best way not to have long COVID is not to have COVID at all,” said Leora Horwitz, MD, a professor of population health and medicine at New York University. “To the extent that vaccination can prevent you from getting COVID at all, then it helps to reduce long COVID.”
And People with more serious initial illness appear more likely to have prolonged symptoms, but those with milder disease can certainly get it, too.
“You’re more likely to have long COVID with more severe disease, and we have ample evidence that vaccination reduces the severity of disease,” Dr. Horwitz said. “We also now have quite a lot of evidence that vaccination does reduce your risk of long COVID – probably because it reduces your risk of severe disease.”
There is little consensus about how much vaccines can lower the risk of long-term COVID symptoms, but several studies suggest that number lies anywhere from 15% to more than 80%.
That might seem like a big variation, but infectious disease experts argue that trying to interpret the gap isn’t as important as noticing what’s consistent across all these studies: “Vaccines do offer some protection, but it’s incomplete,” said Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs St. Louis Health Care System. Dr. Al-Aly, who has led several large studies on long COVID, said focusing on the fact that vaccines do offer some protection is a much better public health message than looking at the different levels of risk.
“Vaccines do a miraculous job for what they were designed to do,” said Dr. Al-Aly. “Vaccines were designed to reduce the risk of hospitalization ... and for that, vaccines are still holding up, even with all the changes in the virus.”
Still, Elena Azzolini, MD, PhD, head of the Humanitas Research Hospital’s vaccination center in Milan, thinks some studies may have underestimated the level of long COVID protection from vaccines because of limits in the study methods, such as not including enough women, who are more affected by long COVID. Her recent study, which looked at 2,560 health care professionals working in nine Italian centers from March 2020 to April 2022, focused on the risk for healthy women and men in their 20s to their 70s.
In the paper, Dr. Azzolini and associates reported that two or three doses of vaccine reduced the risk of hospitalization from COVID-19 from 42% among those who are unvaccinated to 16%-17%. In other words, they found unvaccinated people in the study were nearly three times as likely to have serious symptoms for longer than 4 weeks.
But Dr. Azzolini and Dr. Al-Aly still say that, even for the vaccinated, as long as COVID is around, masks are necessary. That’s because current vaccines don’t do enough to reduce transmission, said Dr. Al-Aly. “The only way that can really help [stop] transmission is covering our nose and mouth with a mask.”
How vaccinations affect people who already have long COVID
Some long COVID patients have said they got better after they get boosted, while some say they’re getting worse, said Dr. Horwitz, who is also a lead investigator at the National Institutes of Health’s flagship RECOVER program, a 4-year research project to study long COVID across the United States. (The NIH is still recruiting volunteers for these studies, which are also open to people who have never had COVID.)
One study published in the British Medical Journal analyzed survey data of more than 28,000 people infected with COVID in the United Kingdom and found a 13% reduction in long-term symptoms after a first dose of the vaccine, although it was unclear from the data if the improvement was sustained.
A second dose was associated with another 8% improvement over a 2-month period. “It’s reassuring that we see an average modest improvement in symptoms, not an average worsening in symptoms,” said Daniel Ayoubkhani, principal statistician at the U.K. Office for National Statistics and lead author of the study. Of course, the experience will differ among different people.
“It doesn’t appear that vaccination is the silver bullet that’s going to eradicate long COVID,” he said, but evidence from multiple studies suggests vaccines may help people with long-term symptoms.
Akiko Iwasaki, PhD, an immunobiologist at Yale University, New Haven, Conn., told a White House summit in July that one of the best ways to prevent long COVID is to develop the next generation of vaccines that also prevent milder cases by blocking transmission in the first place.
Back in New York, Dr. Kulick is now triple vaccinated. She’s due for a fourth dose soon but admits she’s “terrified every time” that she’s going to get sicker.
In her Facebook support group for long COVID, she reads that most people with prolonged symptoms handle it well. She has also noticed some of her symptoms eased after her first two doses of vaccine.
Since being diagnosed, Dr. Kulick learned she has a genetic condition, Ehlers-Danlos syndrome, which affects connective tissues that support skin, joints, organs, and blood vessels, and which her doctors say may have made her more prone to long COVID. She’s also being screened for autoimmune diseases, but for now, the only relief she has found has come from long COVID physical therapy, changes to her diet, and integrative medicine.
Dr. Kulick is still trying to figure out how she can get better while keeping her long hours at her veterinary job – and her health benefits. She is thankful her husband is a devoted caregiver to their son and a professional jazz musician with a schedule that allows for some flexibility.
“But it’s really hard when every week feels like I’ve run a marathon,” she said. “I can barely make it through.”
A version of this article first appeared on WebMD.com.
Increasing data link ME/CFS, long COVID, and dysautonomia
At the virtual annual meeting of the International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (IACFSME), speakers presented data showing similar pathophysiologic abnormalities in people with systemic symptoms associated with ME/CFS who had a prior SARS-CoV-2 infection and those who did not, including individuals whose illness preceded the COVID-19 pandemic.
Core clinical diagnostic criteria for ME/CFS established by the Institute of Medicine in 2015 include substantial decrement in functioning for 6 months or longer, postexertional malaise, or a worsening of symptoms following even minor exertion (often described by patients as “crashes”), unrefreshing sleep, and cognitive dysfunction and/or orthostatic intolerance that are frequent and severe.
Long COVID has been defined in several different ways using different terminology. The U.S. Centers for Disease Control and Prevention, for example, defines “post-COVID conditions” as those continuing four or more weeks beyond first symptoms. The World Health Organization’s clinical case definition of “post COVID-19 condition” includes otherwise unexplained symptoms 3 months from COVID-19 onset and lasting longer than 2 months.
Both ME/CFS and long COVID commonly involve numerous symptoms beyond the defining ones, affecting nearly every organ system in the body, including systemic, neurocognitive, endocrine, cardiovascular, pulmonary, musculoskeletal, and gastrointestinal, with wide variation among individuals. Autonomic dysfunction is common to both conditions, particularly postural orthostatic tachycardia syndrome (POTS).
“My way of understanding these illnesses is that they’re not just multisystem illnesses, but all these interactive systems that lean on each other are dysregulated. … I would say that a very common underlying mediator of both ME/CFS and long COVID is autonomic dysfunction, and it presents as POTS,” Nancy Klimas, MD, director of the Institute for Neuro-Immune Medicine at Nova Southeastern University, Fort Lauderdale, Fla., told this news organization.
Dr. Klimas, who is also director of Clinical Immunology Research at the Miami Veterans Affairs Medical Center, added that “if basic bioenergetics are disrupted and in an oxidative-stress state [then] they have downregulated energy production at the cellular level, which seems to be the case in ME/CFS and now in long COVID.”
New ICD-10 codes better characterize the syndromes
New ICD-10 codes for 2023, being implemented on Oct. 1, will enable clinicians to better document all of these interrelated conditions.
Under the existing G93.3, Postviral and related fatigue syndromes, there will now be:
- G93.31 – Postviral fatigue syndrome.
- G93.32 – Myalgic encephalomyelitis/chronic fatigue syndrome (and the separate terms).
- G93.39 – Other postinfection and related fatigue syndromes.
The old R53.82, “Chronic fatigue, unspecified” code now excludes all of the above conditions.
The additional code U09.9 for “post COVID-19 condition, unspecified,” may also be used if applicable.
In addition, a new code for POTS, G90.A, which wasn’t previously mentioned in ICD-10, may also be used starting Oct. 1.
Lucinda Bateman, MD, founder and director of the Bateman Horne Center, Salt Lake City, advises using all applicable codes for a given patient. “If a patient came into my office with long COVID and met criteria for ME/CFS, we would code both, and also any other syndrome criteria that they may meet, such as POTS or fibromyalgia.
“If people use the codes appropriately, then you can understand the overlap better. It increases the likelihood of reimbursement, creates a more accurate medical record for the patient, and provides them with a better tool should they require disability benefits.”
Dr. Bateman advises in-office orthostatic evaluation for all patients with this symptom constellation, using a passive standing evaluation such as the 10-minute NASA Lean test.
“Clinicians should take the time to do orthostatic testing in these patients because it provides objective markers and will help lead us to potential interventions to help improve people’s function.”
The Bateman Horne center offers clinician resources on management of ME/CFS and related conditions.
How common is ME/CFS after COVID-19?
According to one published meta-analysis, the global prevalence of “post-acute sequelae of SARS-CoV-2,” defined by any symptom, is about 43% of patients overall following infection, and 49% at 120 days. Fatigue was the most commonly reported symptom, followed by memory problems. As of March 22, the World Health Organization estimated that there have been more than 470 million COVID-19 cases, which would give a figure of about 200 million people who are experiencing a wide range of long-COVID symptoms.
On the final day of the IACFSME conference, Luis Nacul, MD, of the University of British Columbia, Vancouver, presented several sets of data from his group and others aiming to determine the proportion of individuals who develop symptoms suggestive of ME/CFS following a COVID-19 infection.
Among a cohort of 88 adults hospitalized with confirmed SARS-CoV-2 infections during the first pandemic wave in 2020 and followed up in the respiratory clinic, rates of reported generalized fatigue were 67% at 3 months and 59.5% at 6 months. Substantial fatigue (that is, present most days and affecting activity levels) were reported by 16% at 3 months and 7% at 6 months. “This should represent in principle the maximum prevalence of cases who would meet the criteria for ME/CFS,” Dr. Nacul said.
Baseline age was indirectly associated with fatigue at 3 and 6 months, while the number of comorbidities a patient had was directly associated. Comorbidities also predicted severe fatigue at 3 months, but the numbers were too small for assessment at 6 months.
Studies involving nonhospitalized patients suggested lower rates. One meta-analysis showed 1-year rates of fatigue in 32% and cognitive impairment in 22%. Another showed very similar rates, reporting fatigue in 28% and memory/concentration difficulties in 18%-19%.
Dr. Nacul cautioned that these figures are likely overestimates since many of the study populations are taken from respiratory or long-COVID clinics. “The evidence on ‘post-COVID fatigue syndrome’ or ME/CFS following COVID is still evolving. There is a huge need for studies looking more closely at cases meeting well-defined ME/CFS criteria. This unfortunately hasn’t been done for most studies.”
Immune system dysfunction appears to underlie many cases
In a keynote address during the conference, Akiko Iwasaki, PhD, of Yale University, New Haven, Conn., pointed out that long COVID and ME/CFS are among many unexplained postacute infection syndromes associated with a long list of viral pathogens, including Ebola, the prior SARS viruses, Epstein-Barr virus, and Dengue, as well as nonviral pathogens such as Coxiella burnetii (Q fever syndrome) and Borrelia (posttreatment Lyme disease syndrome).
Dr. Iwasaki cited a recent Nature Medicine review article that she coauthored on this topic with an ME/CFS patient, noting: “We really need to understand why some people are failing to recover from these types of diseases.”
Emerging evidence supports four different hypotheses regarding pathogenesis: viral reservoir/viral pathogen-associated molecular pattern molecules, autoimmunity, dysbiosis/viral reactivation, and tissue damage
“Right now, it’s too early to exclude or make any conclusions about these. We need to have an open mind to dissect these various possibilities,” she said.
Two speakers reported findings of immune dysregulation in both ME/CFS and long COVID. Wakiro Sato, MD, PhD, of the National Center of Neurology and Psychiatry, Tokyo, reported that anti–G-protein coupled receptor antibodies were found in 33 (55%) of 60 patients with long COVID, and more than 40% had peripheral immune cell profile abnormalities. These findings were similar to those found in patients with ME/CFS, published by Sato’s team (Brain Behav Immun. 2021 Mar 29. doi: 10.1016/j.bbi.2021.03.023) and other researchers in Germany.
Liisa K. Selin, MD, PhD, professor of pathology at the University of Massachusetts, Worcester, presented data for an analysis of peripheral blood mononuclear cells from 26 donors with ME/CFS (8 with long COVID) and 24 healthy controls. In both patient groups, they found altered expression of inflammatory markers and decreases in CD8 T-cell number and function. The patients with long COVID showed evidence of sustained activation of both T-cell populations with increased CD38 and HLA-DR, associated with a compensatory increased frequency of activated CD4+CD8+ T cells.
“These results are consistent with immune dysregulation associated with overactivation and exhaustion of CD8 T cells, as observed in chronic viral infections and tumor environments,” Dr. Selin said.
ME/CFS and long COVID ‘frighteningly similar, if not identical’
Data for a different system derangement in long COVID and ME/CFS, the pathophysiology of exercise intolerance, were presented in another keynote talk by David M. Systrom, MD, a pulmonary and critical care medicine specialist at Brigham and Women’s Hospital and director of the Massachusetts General Hospital cardiopulmonary laboratory, both in Boston. He has conducted invasive cardiopulmonary exercise testing in patients with ME/CFS and patients with long COVID.
Previously, Dr. Systrom and his team found that patients with ME/CFS have distinct defects in both ventricular filling pressure and oxygen extraction from the muscles. Neither of those are features of deconditioning, which is often blamed for exercise intolerance in people with ME/CFS. Rather, the major defect in deconditioning is decreased stroke volume and cardiac output. In ME/CFS patients, he found supranormal pulmonary blood flow, compared with VO2 max, suggesting peripheral left-to-right shunting.
In addition, Dr. Systrom and colleagues found that a large proportion of ME/CFS patients with these peripheral vascular defects also have biopsy-demonstrated small-fiber neuropathy, suggesting that acute exercise intolerance is related to underlying autonomic nervous system dysfunction.
In Dr. Systrom and colleagues’ long COVID study, invasive cardiopulmonary exercise testing in 10 patients who had recovered from COVID-19 at least 6 months prior and did not have cardiopulmonary disease had significantly revealed reduced peak exercise aerobic capacity (VO2 max), compared with 10 age- and sex-matched controls. The reduction in peak VO2 was associated with impaired systemic oxygen extraction, compared with the controls, despite a preserved peak cardiac index.
The long-COVID patients also showed greater ventilatory inefficiency, which “is entirely related to hyperventilation, not intrinsic lung disease,” Dr. Systrom said, adding that while there may be subsets of patients with interstitial lung disease after acute respiratory distress syndrome, these patients didn’t have that. “This for all the world looks like ME/CFS. We think they are frighteningly similar, if not identical,” Dr. Systrom said.
In a third study for which Dr. Systrom was a coauthor, published in Annals of Neurology, multisystem involvement was found in nine patients following mild COVID-19 infection, using standardized autonomic assessments including Valsalva maneuver, sudomotor and tilt tests, and skin biopsies for small-fiber neuropathy. The findings included cerebrovascular dysregulation with persistent cerebral arteriolar vasoconstriction, small-fiber neuropathy and related dysautonomia, respiratory dysregulation, and chronic inflammation.
Dr. Systrom’s conclusion: “Dyspnea and hyperventilation are common in ME/CFS and long COVID and there is significant overlap with POTS.”
Dr. Bateman disclosed that she is conducting research for Terra Biological. Dr. Systrom said he is conducting research for Astellas.
A version of this article first appeared on Medscape.com.
At the virtual annual meeting of the International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (IACFSME), speakers presented data showing similar pathophysiologic abnormalities in people with systemic symptoms associated with ME/CFS who had a prior SARS-CoV-2 infection and those who did not, including individuals whose illness preceded the COVID-19 pandemic.
Core clinical diagnostic criteria for ME/CFS established by the Institute of Medicine in 2015 include substantial decrement in functioning for 6 months or longer, postexertional malaise, or a worsening of symptoms following even minor exertion (often described by patients as “crashes”), unrefreshing sleep, and cognitive dysfunction and/or orthostatic intolerance that are frequent and severe.
Long COVID has been defined in several different ways using different terminology. The U.S. Centers for Disease Control and Prevention, for example, defines “post-COVID conditions” as those continuing four or more weeks beyond first symptoms. The World Health Organization’s clinical case definition of “post COVID-19 condition” includes otherwise unexplained symptoms 3 months from COVID-19 onset and lasting longer than 2 months.
Both ME/CFS and long COVID commonly involve numerous symptoms beyond the defining ones, affecting nearly every organ system in the body, including systemic, neurocognitive, endocrine, cardiovascular, pulmonary, musculoskeletal, and gastrointestinal, with wide variation among individuals. Autonomic dysfunction is common to both conditions, particularly postural orthostatic tachycardia syndrome (POTS).
“My way of understanding these illnesses is that they’re not just multisystem illnesses, but all these interactive systems that lean on each other are dysregulated. … I would say that a very common underlying mediator of both ME/CFS and long COVID is autonomic dysfunction, and it presents as POTS,” Nancy Klimas, MD, director of the Institute for Neuro-Immune Medicine at Nova Southeastern University, Fort Lauderdale, Fla., told this news organization.
Dr. Klimas, who is also director of Clinical Immunology Research at the Miami Veterans Affairs Medical Center, added that “if basic bioenergetics are disrupted and in an oxidative-stress state [then] they have downregulated energy production at the cellular level, which seems to be the case in ME/CFS and now in long COVID.”
New ICD-10 codes better characterize the syndromes
New ICD-10 codes for 2023, being implemented on Oct. 1, will enable clinicians to better document all of these interrelated conditions.
Under the existing G93.3, Postviral and related fatigue syndromes, there will now be:
- G93.31 – Postviral fatigue syndrome.
- G93.32 – Myalgic encephalomyelitis/chronic fatigue syndrome (and the separate terms).
- G93.39 – Other postinfection and related fatigue syndromes.
The old R53.82, “Chronic fatigue, unspecified” code now excludes all of the above conditions.
The additional code U09.9 for “post COVID-19 condition, unspecified,” may also be used if applicable.
In addition, a new code for POTS, G90.A, which wasn’t previously mentioned in ICD-10, may also be used starting Oct. 1.
Lucinda Bateman, MD, founder and director of the Bateman Horne Center, Salt Lake City, advises using all applicable codes for a given patient. “If a patient came into my office with long COVID and met criteria for ME/CFS, we would code both, and also any other syndrome criteria that they may meet, such as POTS or fibromyalgia.
“If people use the codes appropriately, then you can understand the overlap better. It increases the likelihood of reimbursement, creates a more accurate medical record for the patient, and provides them with a better tool should they require disability benefits.”
Dr. Bateman advises in-office orthostatic evaluation for all patients with this symptom constellation, using a passive standing evaluation such as the 10-minute NASA Lean test.
“Clinicians should take the time to do orthostatic testing in these patients because it provides objective markers and will help lead us to potential interventions to help improve people’s function.”
The Bateman Horne center offers clinician resources on management of ME/CFS and related conditions.
How common is ME/CFS after COVID-19?
According to one published meta-analysis, the global prevalence of “post-acute sequelae of SARS-CoV-2,” defined by any symptom, is about 43% of patients overall following infection, and 49% at 120 days. Fatigue was the most commonly reported symptom, followed by memory problems. As of March 22, the World Health Organization estimated that there have been more than 470 million COVID-19 cases, which would give a figure of about 200 million people who are experiencing a wide range of long-COVID symptoms.
On the final day of the IACFSME conference, Luis Nacul, MD, of the University of British Columbia, Vancouver, presented several sets of data from his group and others aiming to determine the proportion of individuals who develop symptoms suggestive of ME/CFS following a COVID-19 infection.
Among a cohort of 88 adults hospitalized with confirmed SARS-CoV-2 infections during the first pandemic wave in 2020 and followed up in the respiratory clinic, rates of reported generalized fatigue were 67% at 3 months and 59.5% at 6 months. Substantial fatigue (that is, present most days and affecting activity levels) were reported by 16% at 3 months and 7% at 6 months. “This should represent in principle the maximum prevalence of cases who would meet the criteria for ME/CFS,” Dr. Nacul said.
Baseline age was indirectly associated with fatigue at 3 and 6 months, while the number of comorbidities a patient had was directly associated. Comorbidities also predicted severe fatigue at 3 months, but the numbers were too small for assessment at 6 months.
Studies involving nonhospitalized patients suggested lower rates. One meta-analysis showed 1-year rates of fatigue in 32% and cognitive impairment in 22%. Another showed very similar rates, reporting fatigue in 28% and memory/concentration difficulties in 18%-19%.
Dr. Nacul cautioned that these figures are likely overestimates since many of the study populations are taken from respiratory or long-COVID clinics. “The evidence on ‘post-COVID fatigue syndrome’ or ME/CFS following COVID is still evolving. There is a huge need for studies looking more closely at cases meeting well-defined ME/CFS criteria. This unfortunately hasn’t been done for most studies.”
Immune system dysfunction appears to underlie many cases
In a keynote address during the conference, Akiko Iwasaki, PhD, of Yale University, New Haven, Conn., pointed out that long COVID and ME/CFS are among many unexplained postacute infection syndromes associated with a long list of viral pathogens, including Ebola, the prior SARS viruses, Epstein-Barr virus, and Dengue, as well as nonviral pathogens such as Coxiella burnetii (Q fever syndrome) and Borrelia (posttreatment Lyme disease syndrome).
Dr. Iwasaki cited a recent Nature Medicine review article that she coauthored on this topic with an ME/CFS patient, noting: “We really need to understand why some people are failing to recover from these types of diseases.”
Emerging evidence supports four different hypotheses regarding pathogenesis: viral reservoir/viral pathogen-associated molecular pattern molecules, autoimmunity, dysbiosis/viral reactivation, and tissue damage
“Right now, it’s too early to exclude or make any conclusions about these. We need to have an open mind to dissect these various possibilities,” she said.
Two speakers reported findings of immune dysregulation in both ME/CFS and long COVID. Wakiro Sato, MD, PhD, of the National Center of Neurology and Psychiatry, Tokyo, reported that anti–G-protein coupled receptor antibodies were found in 33 (55%) of 60 patients with long COVID, and more than 40% had peripheral immune cell profile abnormalities. These findings were similar to those found in patients with ME/CFS, published by Sato’s team (Brain Behav Immun. 2021 Mar 29. doi: 10.1016/j.bbi.2021.03.023) and other researchers in Germany.
Liisa K. Selin, MD, PhD, professor of pathology at the University of Massachusetts, Worcester, presented data for an analysis of peripheral blood mononuclear cells from 26 donors with ME/CFS (8 with long COVID) and 24 healthy controls. In both patient groups, they found altered expression of inflammatory markers and decreases in CD8 T-cell number and function. The patients with long COVID showed evidence of sustained activation of both T-cell populations with increased CD38 and HLA-DR, associated with a compensatory increased frequency of activated CD4+CD8+ T cells.
“These results are consistent with immune dysregulation associated with overactivation and exhaustion of CD8 T cells, as observed in chronic viral infections and tumor environments,” Dr. Selin said.
ME/CFS and long COVID ‘frighteningly similar, if not identical’
Data for a different system derangement in long COVID and ME/CFS, the pathophysiology of exercise intolerance, were presented in another keynote talk by David M. Systrom, MD, a pulmonary and critical care medicine specialist at Brigham and Women’s Hospital and director of the Massachusetts General Hospital cardiopulmonary laboratory, both in Boston. He has conducted invasive cardiopulmonary exercise testing in patients with ME/CFS and patients with long COVID.
Previously, Dr. Systrom and his team found that patients with ME/CFS have distinct defects in both ventricular filling pressure and oxygen extraction from the muscles. Neither of those are features of deconditioning, which is often blamed for exercise intolerance in people with ME/CFS. Rather, the major defect in deconditioning is decreased stroke volume and cardiac output. In ME/CFS patients, he found supranormal pulmonary blood flow, compared with VO2 max, suggesting peripheral left-to-right shunting.
In addition, Dr. Systrom and colleagues found that a large proportion of ME/CFS patients with these peripheral vascular defects also have biopsy-demonstrated small-fiber neuropathy, suggesting that acute exercise intolerance is related to underlying autonomic nervous system dysfunction.
In Dr. Systrom and colleagues’ long COVID study, invasive cardiopulmonary exercise testing in 10 patients who had recovered from COVID-19 at least 6 months prior and did not have cardiopulmonary disease had significantly revealed reduced peak exercise aerobic capacity (VO2 max), compared with 10 age- and sex-matched controls. The reduction in peak VO2 was associated with impaired systemic oxygen extraction, compared with the controls, despite a preserved peak cardiac index.
The long-COVID patients also showed greater ventilatory inefficiency, which “is entirely related to hyperventilation, not intrinsic lung disease,” Dr. Systrom said, adding that while there may be subsets of patients with interstitial lung disease after acute respiratory distress syndrome, these patients didn’t have that. “This for all the world looks like ME/CFS. We think they are frighteningly similar, if not identical,” Dr. Systrom said.
In a third study for which Dr. Systrom was a coauthor, published in Annals of Neurology, multisystem involvement was found in nine patients following mild COVID-19 infection, using standardized autonomic assessments including Valsalva maneuver, sudomotor and tilt tests, and skin biopsies for small-fiber neuropathy. The findings included cerebrovascular dysregulation with persistent cerebral arteriolar vasoconstriction, small-fiber neuropathy and related dysautonomia, respiratory dysregulation, and chronic inflammation.
Dr. Systrom’s conclusion: “Dyspnea and hyperventilation are common in ME/CFS and long COVID and there is significant overlap with POTS.”
Dr. Bateman disclosed that she is conducting research for Terra Biological. Dr. Systrom said he is conducting research for Astellas.
A version of this article first appeared on Medscape.com.
At the virtual annual meeting of the International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (IACFSME), speakers presented data showing similar pathophysiologic abnormalities in people with systemic symptoms associated with ME/CFS who had a prior SARS-CoV-2 infection and those who did not, including individuals whose illness preceded the COVID-19 pandemic.
Core clinical diagnostic criteria for ME/CFS established by the Institute of Medicine in 2015 include substantial decrement in functioning for 6 months or longer, postexertional malaise, or a worsening of symptoms following even minor exertion (often described by patients as “crashes”), unrefreshing sleep, and cognitive dysfunction and/or orthostatic intolerance that are frequent and severe.
Long COVID has been defined in several different ways using different terminology. The U.S. Centers for Disease Control and Prevention, for example, defines “post-COVID conditions” as those continuing four or more weeks beyond first symptoms. The World Health Organization’s clinical case definition of “post COVID-19 condition” includes otherwise unexplained symptoms 3 months from COVID-19 onset and lasting longer than 2 months.
Both ME/CFS and long COVID commonly involve numerous symptoms beyond the defining ones, affecting nearly every organ system in the body, including systemic, neurocognitive, endocrine, cardiovascular, pulmonary, musculoskeletal, and gastrointestinal, with wide variation among individuals. Autonomic dysfunction is common to both conditions, particularly postural orthostatic tachycardia syndrome (POTS).
“My way of understanding these illnesses is that they’re not just multisystem illnesses, but all these interactive systems that lean on each other are dysregulated. … I would say that a very common underlying mediator of both ME/CFS and long COVID is autonomic dysfunction, and it presents as POTS,” Nancy Klimas, MD, director of the Institute for Neuro-Immune Medicine at Nova Southeastern University, Fort Lauderdale, Fla., told this news organization.
Dr. Klimas, who is also director of Clinical Immunology Research at the Miami Veterans Affairs Medical Center, added that “if basic bioenergetics are disrupted and in an oxidative-stress state [then] they have downregulated energy production at the cellular level, which seems to be the case in ME/CFS and now in long COVID.”
New ICD-10 codes better characterize the syndromes
New ICD-10 codes for 2023, being implemented on Oct. 1, will enable clinicians to better document all of these interrelated conditions.
Under the existing G93.3, Postviral and related fatigue syndromes, there will now be:
- G93.31 – Postviral fatigue syndrome.
- G93.32 – Myalgic encephalomyelitis/chronic fatigue syndrome (and the separate terms).
- G93.39 – Other postinfection and related fatigue syndromes.
The old R53.82, “Chronic fatigue, unspecified” code now excludes all of the above conditions.
The additional code U09.9 for “post COVID-19 condition, unspecified,” may also be used if applicable.
In addition, a new code for POTS, G90.A, which wasn’t previously mentioned in ICD-10, may also be used starting Oct. 1.
Lucinda Bateman, MD, founder and director of the Bateman Horne Center, Salt Lake City, advises using all applicable codes for a given patient. “If a patient came into my office with long COVID and met criteria for ME/CFS, we would code both, and also any other syndrome criteria that they may meet, such as POTS or fibromyalgia.
“If people use the codes appropriately, then you can understand the overlap better. It increases the likelihood of reimbursement, creates a more accurate medical record for the patient, and provides them with a better tool should they require disability benefits.”
Dr. Bateman advises in-office orthostatic evaluation for all patients with this symptom constellation, using a passive standing evaluation such as the 10-minute NASA Lean test.
“Clinicians should take the time to do orthostatic testing in these patients because it provides objective markers and will help lead us to potential interventions to help improve people’s function.”
The Bateman Horne center offers clinician resources on management of ME/CFS and related conditions.
How common is ME/CFS after COVID-19?
According to one published meta-analysis, the global prevalence of “post-acute sequelae of SARS-CoV-2,” defined by any symptom, is about 43% of patients overall following infection, and 49% at 120 days. Fatigue was the most commonly reported symptom, followed by memory problems. As of March 22, the World Health Organization estimated that there have been more than 470 million COVID-19 cases, which would give a figure of about 200 million people who are experiencing a wide range of long-COVID symptoms.
On the final day of the IACFSME conference, Luis Nacul, MD, of the University of British Columbia, Vancouver, presented several sets of data from his group and others aiming to determine the proportion of individuals who develop symptoms suggestive of ME/CFS following a COVID-19 infection.
Among a cohort of 88 adults hospitalized with confirmed SARS-CoV-2 infections during the first pandemic wave in 2020 and followed up in the respiratory clinic, rates of reported generalized fatigue were 67% at 3 months and 59.5% at 6 months. Substantial fatigue (that is, present most days and affecting activity levels) were reported by 16% at 3 months and 7% at 6 months. “This should represent in principle the maximum prevalence of cases who would meet the criteria for ME/CFS,” Dr. Nacul said.
Baseline age was indirectly associated with fatigue at 3 and 6 months, while the number of comorbidities a patient had was directly associated. Comorbidities also predicted severe fatigue at 3 months, but the numbers were too small for assessment at 6 months.
Studies involving nonhospitalized patients suggested lower rates. One meta-analysis showed 1-year rates of fatigue in 32% and cognitive impairment in 22%. Another showed very similar rates, reporting fatigue in 28% and memory/concentration difficulties in 18%-19%.
Dr. Nacul cautioned that these figures are likely overestimates since many of the study populations are taken from respiratory or long-COVID clinics. “The evidence on ‘post-COVID fatigue syndrome’ or ME/CFS following COVID is still evolving. There is a huge need for studies looking more closely at cases meeting well-defined ME/CFS criteria. This unfortunately hasn’t been done for most studies.”
Immune system dysfunction appears to underlie many cases
In a keynote address during the conference, Akiko Iwasaki, PhD, of Yale University, New Haven, Conn., pointed out that long COVID and ME/CFS are among many unexplained postacute infection syndromes associated with a long list of viral pathogens, including Ebola, the prior SARS viruses, Epstein-Barr virus, and Dengue, as well as nonviral pathogens such as Coxiella burnetii (Q fever syndrome) and Borrelia (posttreatment Lyme disease syndrome).
Dr. Iwasaki cited a recent Nature Medicine review article that she coauthored on this topic with an ME/CFS patient, noting: “We really need to understand why some people are failing to recover from these types of diseases.”
Emerging evidence supports four different hypotheses regarding pathogenesis: viral reservoir/viral pathogen-associated molecular pattern molecules, autoimmunity, dysbiosis/viral reactivation, and tissue damage
“Right now, it’s too early to exclude or make any conclusions about these. We need to have an open mind to dissect these various possibilities,” she said.
Two speakers reported findings of immune dysregulation in both ME/CFS and long COVID. Wakiro Sato, MD, PhD, of the National Center of Neurology and Psychiatry, Tokyo, reported that anti–G-protein coupled receptor antibodies were found in 33 (55%) of 60 patients with long COVID, and more than 40% had peripheral immune cell profile abnormalities. These findings were similar to those found in patients with ME/CFS, published by Sato’s team (Brain Behav Immun. 2021 Mar 29. doi: 10.1016/j.bbi.2021.03.023) and other researchers in Germany.
Liisa K. Selin, MD, PhD, professor of pathology at the University of Massachusetts, Worcester, presented data for an analysis of peripheral blood mononuclear cells from 26 donors with ME/CFS (8 with long COVID) and 24 healthy controls. In both patient groups, they found altered expression of inflammatory markers and decreases in CD8 T-cell number and function. The patients with long COVID showed evidence of sustained activation of both T-cell populations with increased CD38 and HLA-DR, associated with a compensatory increased frequency of activated CD4+CD8+ T cells.
“These results are consistent with immune dysregulation associated with overactivation and exhaustion of CD8 T cells, as observed in chronic viral infections and tumor environments,” Dr. Selin said.
ME/CFS and long COVID ‘frighteningly similar, if not identical’
Data for a different system derangement in long COVID and ME/CFS, the pathophysiology of exercise intolerance, were presented in another keynote talk by David M. Systrom, MD, a pulmonary and critical care medicine specialist at Brigham and Women’s Hospital and director of the Massachusetts General Hospital cardiopulmonary laboratory, both in Boston. He has conducted invasive cardiopulmonary exercise testing in patients with ME/CFS and patients with long COVID.
Previously, Dr. Systrom and his team found that patients with ME/CFS have distinct defects in both ventricular filling pressure and oxygen extraction from the muscles. Neither of those are features of deconditioning, which is often blamed for exercise intolerance in people with ME/CFS. Rather, the major defect in deconditioning is decreased stroke volume and cardiac output. In ME/CFS patients, he found supranormal pulmonary blood flow, compared with VO2 max, suggesting peripheral left-to-right shunting.
In addition, Dr. Systrom and colleagues found that a large proportion of ME/CFS patients with these peripheral vascular defects also have biopsy-demonstrated small-fiber neuropathy, suggesting that acute exercise intolerance is related to underlying autonomic nervous system dysfunction.
In Dr. Systrom and colleagues’ long COVID study, invasive cardiopulmonary exercise testing in 10 patients who had recovered from COVID-19 at least 6 months prior and did not have cardiopulmonary disease had significantly revealed reduced peak exercise aerobic capacity (VO2 max), compared with 10 age- and sex-matched controls. The reduction in peak VO2 was associated with impaired systemic oxygen extraction, compared with the controls, despite a preserved peak cardiac index.
The long-COVID patients also showed greater ventilatory inefficiency, which “is entirely related to hyperventilation, not intrinsic lung disease,” Dr. Systrom said, adding that while there may be subsets of patients with interstitial lung disease after acute respiratory distress syndrome, these patients didn’t have that. “This for all the world looks like ME/CFS. We think they are frighteningly similar, if not identical,” Dr. Systrom said.
In a third study for which Dr. Systrom was a coauthor, published in Annals of Neurology, multisystem involvement was found in nine patients following mild COVID-19 infection, using standardized autonomic assessments including Valsalva maneuver, sudomotor and tilt tests, and skin biopsies for small-fiber neuropathy. The findings included cerebrovascular dysregulation with persistent cerebral arteriolar vasoconstriction, small-fiber neuropathy and related dysautonomia, respiratory dysregulation, and chronic inflammation.
Dr. Systrom’s conclusion: “Dyspnea and hyperventilation are common in ME/CFS and long COVID and there is significant overlap with POTS.”
Dr. Bateman disclosed that she is conducting research for Terra Biological. Dr. Systrom said he is conducting research for Astellas.
A version of this article first appeared on Medscape.com.
FROM IACFSME 2022
Treatments explored to ease postviral symptoms of ME/CFS and long COVID
A variety of treatments, most already commercially available, are under investigation for treating the constellation of overlapping symptoms associated with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), “long COVID,” and dysautonomia.
At the virtual annual meeting of the International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis, speakers presented data for a variety of approaches to ease symptoms common across postviral conditions, such as extreme fatigue, postexertional malaise (“crash”), cognitive dysfunction (“brain fog”), orthostatic intolerance including postural orthostatic tachycardia syndrome (POTS), and chronic pain. Most of the modalities are already commercially available for other indications, although some are costly and not covered by payers for these conditions.
“ ... In the past, patients were told ‘you have chronic fatigue syndrome but there’s nothing we can do for it.’ That certainly is not the case. There aren’t cures, but there are many management techniques to improve symptoms,” Charles W. Lapp, MD, medical director of the Hunter-Hopkins Center, Charlotte, N.C., said in an interview.
A current mainstay of treatment for ME/CFS – including that triggered by COVID-19 – is activity pacing, in which patients learn to stay within their “energy envelopes” in order to avoid postexertional malaise, a worsening of all symptoms with exertion. The use of “graded exercise” is no longer recommended, per U.K. and U.S. guidelines.
Data for the following approaches were presented at the IACFS/ME conference:
Pyridostigmine (mestinon, others)
Pyridostigmine, an acetylcholinesterase inhibitor, is approved for the treatment of muscle weakness resulting from myasthenia gravis and is available in generic form. It has previously been shown to produce significant improvement in both symptom burden and heart rate response in POTS.
At the IACFS/ME conference, David M. Systrom, MD, a pulmonary and critical care medicine specialist at Brigham and Women’s Hospital and director of the Massachusetts General Hospital Cardiopulmonary laboratory, both in Boston, summarized his group’s study in patients with ME/CFS using pyridostigmine as both a potential treatment for improving exercise capacity and a proof-of-concept that neurovascular dysregulation underlies exertional intolerance in the condition.
A total of 45 patients were randomized to 60 mg oral pyridostigmine or placebo after an invasive cardiopulmonary exercise test, and a second test performed 50 minutes later. Peak VO2 increased after pyridostigmine but decreased after placebo (+13.3 mL/min vs. –40.2 mL/min, P < .05). Cardiac output and right atrial pressure were also significantly improved with pyridostigmine and worse with placebo.
“We suggest that treatable neurovascular dysregulation underlies acute exercise intolerance in ME/CFS. ... Pyridostigmine may be a useful repurposed off-label treatment [for] a subset of patients with exercise intolerance,” Dr. Systrom said.
Asked to comment, Dr. Lapp said: “We’ve used Mestinon for years because it helps with POTS and also with neurally mediated hypotension. Systrom is taking it to a new level because he’s shown that it increases preload to the heart.” However, he noted that it’s unclear whether the drug will help patients who don’t have POTS specifically. On the other hand, patients rarely experience side effects from the drug.
Since the generic tablets come only in 60-mg doses, and the starting dose is 30 mg three times a day, he advised cutting the tablets in half during titration up to 60 mg three times a day.
Oxaloacetate (benaGene)
David Lyons Kaufman, MD, of the Center for Complex Diseases, Mountain View, Calif., summarized data from his group’s recently published open-label, nonrandomized, “proof-of-concept” study on use of the commercially available nutritional supplement anhydrous enol-oxaloacetate for treating mental and physical fatigue in 76 patients with longstanding ME/CFS and 43 with long-COVID fatigue.
Oxaloacetate is a major step in the Krebs cycle within the mitochondria that are depleted in patients with ME/CFS. It is also an energy metabolite that has multiple effects in cells and mitochondria, Dr. Kaufman explained.
Doses ranging from 500 mg twice daily up to 1,000 mg three times a day were given for 6 weeks. Up to 33% of the patients with ME/CFS and up to 46.8% of the long-COVID group achieved clinical efficacy as measured by physical and mental fatigue scores, compared with just 5.9% of historical ME/CFS controls. All doses showed highly significant improvements.
The only adverse effects were occasional dyspepsia, which was avoided by taking the supplement with food, and insomnia, resolved by having them dose at breakfast and lunch, Dr. Kaufman said.
Following those preliminary data, there is now an ongoing 90-day, randomized, placebo-controlled clinical trial of 80 patients with ME/CFS using 2,000 mg anhydrous enol-oxaloacetate per day. Endpoints include multiple objective measures.
“We have a health care crisis with long COVID, and we’ve had this smoldering crisis with ME/CFS for decades that’s never been addressed. ME/CFS and long COVID, if not identical, are certainly overlapping. ... We have to pursue these translational medicine pilot studies as rapidly as possible,” Dr. Kaufman remarked.
Dr. Lapp told this news organization that it makes sense to use constituents of the Krebs cycle to improve mitochondrial function, but the problem with oxaloacetate is its cost. Dr. Kaufman mentioned that based on the preliminary trial, the therapeutic “sweet spot” appeared to be 1,000 mg twice daily. The manufacturer’s website lists the price for a single bottle of 30 250-mg capsules at $49, or $42 if purchased via a monthly subscription.
“It’s a benign drug, and it’s over the counter. I would give it to any patient who’s got a big wallet,” Dr. Lapp quipped, adding: “If they’ve got the money, they can order it tonight.”
Inspiritol
Inspiritol is an investigational “nebulized, inhaled, multimechanism medication designed to treat the major symptoms of respiratory distress with antioxidant, anti-inflammatory, and broad-spectrum antiviral and antibacterial properties. Inspiritol is composed of both endogenously produced and naturally occurring, well-tolerated biochemicals,” according to the company website.
The hypothesis, Liisa K. Selin, MD, PhD, professor of pathology at the University of Massachusetts, Worcester, said at the meeting, is that “ME/CFS and long COVID-19 result from an aberrant response to an immunological trigger like infection, which results in a permanently dysregulated immune system as a result of overactivation of CD8 T cells and subsequent exhaustion.”
Inspiritol, containing five antioxidants, acts as an immune modulator to reverse the CD8 T cell exhaustion and improve symptoms. Administration by inhaler delivers it directly to the brain from the lung. It was originally designed for use in chronic obstructive pulmonary disease and asthma and has shown efficacy for acute COVID-19, Dr. Selin said.
In a preliminary study, four patients with ME/CFS and five with long COVID have been treated with Inspiritol for 2-15 months, and all have self-reported improved symptoms. Cough has been the only reported side effect.
The company is pursuing an Investigational New Drug Application for the product with the Food and Drug Administration and has several patents pending. Dr. Lapp called Inspiritol “very interesting,” and said that reversal of CD8 “exhaustion” also would appear to be a promising approach. However, he noted, “the problem is that we don’t know what’s in it.”
Stellate ganglion block
Injection of local anesthetic near the stellate ganglion to block activity of the entire cervical sympathetic chain has been used for nearly a century to treat a variety of sympathetically mediated conditions, including complex regional pain syndrome (CRPS), shingles, and phantom-limb pain. More recently, it has been used in a variety of other conditions, including PTSD, Raynaud’s disease, menopausal hot flashes, and hyperhidrosis.
Insurance companies typically cover it for CRPS, neuropathic upper-extremity pain, hyperhidrosis, and Raynaud’s, said Luke Liu, MD, an anesthesiologist who is founder and chief executive officer of Alaska-based pain management company Neuroversion.
Deborah Duricka, PhD, also with Neuroversion, presented results from a now-published case series of 11 patients with long COVID who underwent stellate ganglion block by a board-certified anesthesiologist, first on one side at the level of C6, then on the contralateral side the following day.
Clinically meaningful benefits were seen in at least five of the patients in fatigue, memory problems, problems concentrating, rapid heartbeat, orthostatic intolerance, sleep problems, postexertional malaise, anxiety, and depression.
The hypothetical mechanism, she said, is that “sympathetic block prevents sympathetically driven vasoconstriction in carotid and vertebral arteries.”
Dr. Liu presented another case series of five patients with ME/CFS who underwent the procedure with ultrasound guidance, again on one side and the other side the next day. All had upper-limb autonomic issues such as Raynaud’s and/or neuropathic pain that had been refractory to more conventional treatments.
All five patients reported improvements in symptoms of ME/CFS, including energy level, cognition, pain, and postexertional malaise. One patient reported “feeling well for the first time in decades.” However, that patient relapsed after a mild viral illness 3.5 months after treatment. Some of the patients have required further treatments.
Dr. Lapp commented that, although the procedure is generally safe when performed by an experienced clinician, “Any time you do an injection like that, there’s a high risk that you could nick an artery or a vein or hit an essential nerve in the neck. That’s why it has to be done under fluoroscopy or ultrasound.”
He said he’s had a few patients undergo the procedure, mostly for CRPS, and they seem to have benefited from it. “It might increase cerebral blood flow and preload to the heart, so it might decrease ME/CFS symptoms and help with POTS as well.”
Nonetheless, Dr. Lapp said he wouldn’t consider stellate ganglion block as first-line treatment for ME/CFS or long COVID. “I think it would be for the treatment-resistant patient, when you’ve gone through all the treatments that we know and addressed all the comorbidities and they’re still not getting better.”
But, he added, it is a standard procedure. “Any pain clinic can do a stellate block.”
Transcutaneous auricular vagus nerve stimulation
Nicola Clague-Baker, PhD, a physiotherapist at the University of Liverpool (England), presented findings from an international survey of people with ME/CFS regarding their experience with transcutaneous auricular vagus nerve stimulation (taVNS) to manage their autonomic symptoms. The technique involves stimulation of the autonomic nervous system via the vagus nerve using electrodes applied to part of the ear. The theory is that the technique stimulates the parasympathetic nervous system and improves autonomic balance.
Two small previous trials showing benefit of vagus nerve stimulation for people with ME/CFS used more invasive and less comfortable methods of applying the stimulation rather than to the ear, Dr. Clague-Baker and colleagues noted in a poster. It has also been used successfully in treating POTS, another conference speaker noted.
A total of 131 people with ME/CFS (called simply “ME” in the United Kingdom) responded to a survey advertised on social media and websites. The majority (60%) were from the United Kingdom while the rest were from Europe, Australia, and North America. Most were female, and slightly more than half had lived with ME for 10 or more years.
The majority (72%) were still using taVNS, while 28% had stopped using it. Only 9% had used the modality for longer than a year. Respondents identified more than 30 benefits in symptoms and activities, with improvements in postexertional malaise (39%) and brain fog (37%) being the most common. One reported significant reduction in constipation.
However, respondents also mentioned more than 20 short- and long-term negatives, including headaches (15%) and long-term irritation at the site (9%). One participant reported a “big improvement in neuropathic pain, but not so much for muscles and joints.”
Overall, 80% reported that they would continue using taVNS and 67% said they would recommend it to others with ME, and 56% said that the system was mildly to very beneficial.
Dr. Lapp noted that several types of transcutaneous electrical nerve stimulation units with ear clips are sold online, and he’s seen them work well for migraine treatment. However, he cautioned that some patients have had side effects from the treatment, such as headaches and dizziness. “It’s putting an electrical current through your brain. In my mind, it’s another last-ditch measure.”
Dr. Lapp reported no financial disclosures.
A version of this article first appeared on Medscape.com.
A variety of treatments, most already commercially available, are under investigation for treating the constellation of overlapping symptoms associated with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), “long COVID,” and dysautonomia.
At the virtual annual meeting of the International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis, speakers presented data for a variety of approaches to ease symptoms common across postviral conditions, such as extreme fatigue, postexertional malaise (“crash”), cognitive dysfunction (“brain fog”), orthostatic intolerance including postural orthostatic tachycardia syndrome (POTS), and chronic pain. Most of the modalities are already commercially available for other indications, although some are costly and not covered by payers for these conditions.
“ ... In the past, patients were told ‘you have chronic fatigue syndrome but there’s nothing we can do for it.’ That certainly is not the case. There aren’t cures, but there are many management techniques to improve symptoms,” Charles W. Lapp, MD, medical director of the Hunter-Hopkins Center, Charlotte, N.C., said in an interview.
A current mainstay of treatment for ME/CFS – including that triggered by COVID-19 – is activity pacing, in which patients learn to stay within their “energy envelopes” in order to avoid postexertional malaise, a worsening of all symptoms with exertion. The use of “graded exercise” is no longer recommended, per U.K. and U.S. guidelines.
Data for the following approaches were presented at the IACFS/ME conference:
Pyridostigmine (mestinon, others)
Pyridostigmine, an acetylcholinesterase inhibitor, is approved for the treatment of muscle weakness resulting from myasthenia gravis and is available in generic form. It has previously been shown to produce significant improvement in both symptom burden and heart rate response in POTS.
At the IACFS/ME conference, David M. Systrom, MD, a pulmonary and critical care medicine specialist at Brigham and Women’s Hospital and director of the Massachusetts General Hospital Cardiopulmonary laboratory, both in Boston, summarized his group’s study in patients with ME/CFS using pyridostigmine as both a potential treatment for improving exercise capacity and a proof-of-concept that neurovascular dysregulation underlies exertional intolerance in the condition.
A total of 45 patients were randomized to 60 mg oral pyridostigmine or placebo after an invasive cardiopulmonary exercise test, and a second test performed 50 minutes later. Peak VO2 increased after pyridostigmine but decreased after placebo (+13.3 mL/min vs. –40.2 mL/min, P < .05). Cardiac output and right atrial pressure were also significantly improved with pyridostigmine and worse with placebo.
“We suggest that treatable neurovascular dysregulation underlies acute exercise intolerance in ME/CFS. ... Pyridostigmine may be a useful repurposed off-label treatment [for] a subset of patients with exercise intolerance,” Dr. Systrom said.
Asked to comment, Dr. Lapp said: “We’ve used Mestinon for years because it helps with POTS and also with neurally mediated hypotension. Systrom is taking it to a new level because he’s shown that it increases preload to the heart.” However, he noted that it’s unclear whether the drug will help patients who don’t have POTS specifically. On the other hand, patients rarely experience side effects from the drug.
Since the generic tablets come only in 60-mg doses, and the starting dose is 30 mg three times a day, he advised cutting the tablets in half during titration up to 60 mg three times a day.
Oxaloacetate (benaGene)
David Lyons Kaufman, MD, of the Center for Complex Diseases, Mountain View, Calif., summarized data from his group’s recently published open-label, nonrandomized, “proof-of-concept” study on use of the commercially available nutritional supplement anhydrous enol-oxaloacetate for treating mental and physical fatigue in 76 patients with longstanding ME/CFS and 43 with long-COVID fatigue.
Oxaloacetate is a major step in the Krebs cycle within the mitochondria that are depleted in patients with ME/CFS. It is also an energy metabolite that has multiple effects in cells and mitochondria, Dr. Kaufman explained.
Doses ranging from 500 mg twice daily up to 1,000 mg three times a day were given for 6 weeks. Up to 33% of the patients with ME/CFS and up to 46.8% of the long-COVID group achieved clinical efficacy as measured by physical and mental fatigue scores, compared with just 5.9% of historical ME/CFS controls. All doses showed highly significant improvements.
The only adverse effects were occasional dyspepsia, which was avoided by taking the supplement with food, and insomnia, resolved by having them dose at breakfast and lunch, Dr. Kaufman said.
Following those preliminary data, there is now an ongoing 90-day, randomized, placebo-controlled clinical trial of 80 patients with ME/CFS using 2,000 mg anhydrous enol-oxaloacetate per day. Endpoints include multiple objective measures.
“We have a health care crisis with long COVID, and we’ve had this smoldering crisis with ME/CFS for decades that’s never been addressed. ME/CFS and long COVID, if not identical, are certainly overlapping. ... We have to pursue these translational medicine pilot studies as rapidly as possible,” Dr. Kaufman remarked.
Dr. Lapp told this news organization that it makes sense to use constituents of the Krebs cycle to improve mitochondrial function, but the problem with oxaloacetate is its cost. Dr. Kaufman mentioned that based on the preliminary trial, the therapeutic “sweet spot” appeared to be 1,000 mg twice daily. The manufacturer’s website lists the price for a single bottle of 30 250-mg capsules at $49, or $42 if purchased via a monthly subscription.
“It’s a benign drug, and it’s over the counter. I would give it to any patient who’s got a big wallet,” Dr. Lapp quipped, adding: “If they’ve got the money, they can order it tonight.”
Inspiritol
Inspiritol is an investigational “nebulized, inhaled, multimechanism medication designed to treat the major symptoms of respiratory distress with antioxidant, anti-inflammatory, and broad-spectrum antiviral and antibacterial properties. Inspiritol is composed of both endogenously produced and naturally occurring, well-tolerated biochemicals,” according to the company website.
The hypothesis, Liisa K. Selin, MD, PhD, professor of pathology at the University of Massachusetts, Worcester, said at the meeting, is that “ME/CFS and long COVID-19 result from an aberrant response to an immunological trigger like infection, which results in a permanently dysregulated immune system as a result of overactivation of CD8 T cells and subsequent exhaustion.”
Inspiritol, containing five antioxidants, acts as an immune modulator to reverse the CD8 T cell exhaustion and improve symptoms. Administration by inhaler delivers it directly to the brain from the lung. It was originally designed for use in chronic obstructive pulmonary disease and asthma and has shown efficacy for acute COVID-19, Dr. Selin said.
In a preliminary study, four patients with ME/CFS and five with long COVID have been treated with Inspiritol for 2-15 months, and all have self-reported improved symptoms. Cough has been the only reported side effect.
The company is pursuing an Investigational New Drug Application for the product with the Food and Drug Administration and has several patents pending. Dr. Lapp called Inspiritol “very interesting,” and said that reversal of CD8 “exhaustion” also would appear to be a promising approach. However, he noted, “the problem is that we don’t know what’s in it.”
Stellate ganglion block
Injection of local anesthetic near the stellate ganglion to block activity of the entire cervical sympathetic chain has been used for nearly a century to treat a variety of sympathetically mediated conditions, including complex regional pain syndrome (CRPS), shingles, and phantom-limb pain. More recently, it has been used in a variety of other conditions, including PTSD, Raynaud’s disease, menopausal hot flashes, and hyperhidrosis.
Insurance companies typically cover it for CRPS, neuropathic upper-extremity pain, hyperhidrosis, and Raynaud’s, said Luke Liu, MD, an anesthesiologist who is founder and chief executive officer of Alaska-based pain management company Neuroversion.
Deborah Duricka, PhD, also with Neuroversion, presented results from a now-published case series of 11 patients with long COVID who underwent stellate ganglion block by a board-certified anesthesiologist, first on one side at the level of C6, then on the contralateral side the following day.
Clinically meaningful benefits were seen in at least five of the patients in fatigue, memory problems, problems concentrating, rapid heartbeat, orthostatic intolerance, sleep problems, postexertional malaise, anxiety, and depression.
The hypothetical mechanism, she said, is that “sympathetic block prevents sympathetically driven vasoconstriction in carotid and vertebral arteries.”
Dr. Liu presented another case series of five patients with ME/CFS who underwent the procedure with ultrasound guidance, again on one side and the other side the next day. All had upper-limb autonomic issues such as Raynaud’s and/or neuropathic pain that had been refractory to more conventional treatments.
All five patients reported improvements in symptoms of ME/CFS, including energy level, cognition, pain, and postexertional malaise. One patient reported “feeling well for the first time in decades.” However, that patient relapsed after a mild viral illness 3.5 months after treatment. Some of the patients have required further treatments.
Dr. Lapp commented that, although the procedure is generally safe when performed by an experienced clinician, “Any time you do an injection like that, there’s a high risk that you could nick an artery or a vein or hit an essential nerve in the neck. That’s why it has to be done under fluoroscopy or ultrasound.”
He said he’s had a few patients undergo the procedure, mostly for CRPS, and they seem to have benefited from it. “It might increase cerebral blood flow and preload to the heart, so it might decrease ME/CFS symptoms and help with POTS as well.”
Nonetheless, Dr. Lapp said he wouldn’t consider stellate ganglion block as first-line treatment for ME/CFS or long COVID. “I think it would be for the treatment-resistant patient, when you’ve gone through all the treatments that we know and addressed all the comorbidities and they’re still not getting better.”
But, he added, it is a standard procedure. “Any pain clinic can do a stellate block.”
Transcutaneous auricular vagus nerve stimulation
Nicola Clague-Baker, PhD, a physiotherapist at the University of Liverpool (England), presented findings from an international survey of people with ME/CFS regarding their experience with transcutaneous auricular vagus nerve stimulation (taVNS) to manage their autonomic symptoms. The technique involves stimulation of the autonomic nervous system via the vagus nerve using electrodes applied to part of the ear. The theory is that the technique stimulates the parasympathetic nervous system and improves autonomic balance.
Two small previous trials showing benefit of vagus nerve stimulation for people with ME/CFS used more invasive and less comfortable methods of applying the stimulation rather than to the ear, Dr. Clague-Baker and colleagues noted in a poster. It has also been used successfully in treating POTS, another conference speaker noted.
A total of 131 people with ME/CFS (called simply “ME” in the United Kingdom) responded to a survey advertised on social media and websites. The majority (60%) were from the United Kingdom while the rest were from Europe, Australia, and North America. Most were female, and slightly more than half had lived with ME for 10 or more years.
The majority (72%) were still using taVNS, while 28% had stopped using it. Only 9% had used the modality for longer than a year. Respondents identified more than 30 benefits in symptoms and activities, with improvements in postexertional malaise (39%) and brain fog (37%) being the most common. One reported significant reduction in constipation.
However, respondents also mentioned more than 20 short- and long-term negatives, including headaches (15%) and long-term irritation at the site (9%). One participant reported a “big improvement in neuropathic pain, but not so much for muscles and joints.”
Overall, 80% reported that they would continue using taVNS and 67% said they would recommend it to others with ME, and 56% said that the system was mildly to very beneficial.
Dr. Lapp noted that several types of transcutaneous electrical nerve stimulation units with ear clips are sold online, and he’s seen them work well for migraine treatment. However, he cautioned that some patients have had side effects from the treatment, such as headaches and dizziness. “It’s putting an electrical current through your brain. In my mind, it’s another last-ditch measure.”
Dr. Lapp reported no financial disclosures.
A version of this article first appeared on Medscape.com.
A variety of treatments, most already commercially available, are under investigation for treating the constellation of overlapping symptoms associated with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), “long COVID,” and dysautonomia.
At the virtual annual meeting of the International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis, speakers presented data for a variety of approaches to ease symptoms common across postviral conditions, such as extreme fatigue, postexertional malaise (“crash”), cognitive dysfunction (“brain fog”), orthostatic intolerance including postural orthostatic tachycardia syndrome (POTS), and chronic pain. Most of the modalities are already commercially available for other indications, although some are costly and not covered by payers for these conditions.
“ ... In the past, patients were told ‘you have chronic fatigue syndrome but there’s nothing we can do for it.’ That certainly is not the case. There aren’t cures, but there are many management techniques to improve symptoms,” Charles W. Lapp, MD, medical director of the Hunter-Hopkins Center, Charlotte, N.C., said in an interview.
A current mainstay of treatment for ME/CFS – including that triggered by COVID-19 – is activity pacing, in which patients learn to stay within their “energy envelopes” in order to avoid postexertional malaise, a worsening of all symptoms with exertion. The use of “graded exercise” is no longer recommended, per U.K. and U.S. guidelines.
Data for the following approaches were presented at the IACFS/ME conference:
Pyridostigmine (mestinon, others)
Pyridostigmine, an acetylcholinesterase inhibitor, is approved for the treatment of muscle weakness resulting from myasthenia gravis and is available in generic form. It has previously been shown to produce significant improvement in both symptom burden and heart rate response in POTS.
At the IACFS/ME conference, David M. Systrom, MD, a pulmonary and critical care medicine specialist at Brigham and Women’s Hospital and director of the Massachusetts General Hospital Cardiopulmonary laboratory, both in Boston, summarized his group’s study in patients with ME/CFS using pyridostigmine as both a potential treatment for improving exercise capacity and a proof-of-concept that neurovascular dysregulation underlies exertional intolerance in the condition.
A total of 45 patients were randomized to 60 mg oral pyridostigmine or placebo after an invasive cardiopulmonary exercise test, and a second test performed 50 minutes later. Peak VO2 increased after pyridostigmine but decreased after placebo (+13.3 mL/min vs. –40.2 mL/min, P < .05). Cardiac output and right atrial pressure were also significantly improved with pyridostigmine and worse with placebo.
“We suggest that treatable neurovascular dysregulation underlies acute exercise intolerance in ME/CFS. ... Pyridostigmine may be a useful repurposed off-label treatment [for] a subset of patients with exercise intolerance,” Dr. Systrom said.
Asked to comment, Dr. Lapp said: “We’ve used Mestinon for years because it helps with POTS and also with neurally mediated hypotension. Systrom is taking it to a new level because he’s shown that it increases preload to the heart.” However, he noted that it’s unclear whether the drug will help patients who don’t have POTS specifically. On the other hand, patients rarely experience side effects from the drug.
Since the generic tablets come only in 60-mg doses, and the starting dose is 30 mg three times a day, he advised cutting the tablets in half during titration up to 60 mg three times a day.
Oxaloacetate (benaGene)
David Lyons Kaufman, MD, of the Center for Complex Diseases, Mountain View, Calif., summarized data from his group’s recently published open-label, nonrandomized, “proof-of-concept” study on use of the commercially available nutritional supplement anhydrous enol-oxaloacetate for treating mental and physical fatigue in 76 patients with longstanding ME/CFS and 43 with long-COVID fatigue.
Oxaloacetate is a major step in the Krebs cycle within the mitochondria that are depleted in patients with ME/CFS. It is also an energy metabolite that has multiple effects in cells and mitochondria, Dr. Kaufman explained.
Doses ranging from 500 mg twice daily up to 1,000 mg three times a day were given for 6 weeks. Up to 33% of the patients with ME/CFS and up to 46.8% of the long-COVID group achieved clinical efficacy as measured by physical and mental fatigue scores, compared with just 5.9% of historical ME/CFS controls. All doses showed highly significant improvements.
The only adverse effects were occasional dyspepsia, which was avoided by taking the supplement with food, and insomnia, resolved by having them dose at breakfast and lunch, Dr. Kaufman said.
Following those preliminary data, there is now an ongoing 90-day, randomized, placebo-controlled clinical trial of 80 patients with ME/CFS using 2,000 mg anhydrous enol-oxaloacetate per day. Endpoints include multiple objective measures.
“We have a health care crisis with long COVID, and we’ve had this smoldering crisis with ME/CFS for decades that’s never been addressed. ME/CFS and long COVID, if not identical, are certainly overlapping. ... We have to pursue these translational medicine pilot studies as rapidly as possible,” Dr. Kaufman remarked.
Dr. Lapp told this news organization that it makes sense to use constituents of the Krebs cycle to improve mitochondrial function, but the problem with oxaloacetate is its cost. Dr. Kaufman mentioned that based on the preliminary trial, the therapeutic “sweet spot” appeared to be 1,000 mg twice daily. The manufacturer’s website lists the price for a single bottle of 30 250-mg capsules at $49, or $42 if purchased via a monthly subscription.
“It’s a benign drug, and it’s over the counter. I would give it to any patient who’s got a big wallet,” Dr. Lapp quipped, adding: “If they’ve got the money, they can order it tonight.”
Inspiritol
Inspiritol is an investigational “nebulized, inhaled, multimechanism medication designed to treat the major symptoms of respiratory distress with antioxidant, anti-inflammatory, and broad-spectrum antiviral and antibacterial properties. Inspiritol is composed of both endogenously produced and naturally occurring, well-tolerated biochemicals,” according to the company website.
The hypothesis, Liisa K. Selin, MD, PhD, professor of pathology at the University of Massachusetts, Worcester, said at the meeting, is that “ME/CFS and long COVID-19 result from an aberrant response to an immunological trigger like infection, which results in a permanently dysregulated immune system as a result of overactivation of CD8 T cells and subsequent exhaustion.”
Inspiritol, containing five antioxidants, acts as an immune modulator to reverse the CD8 T cell exhaustion and improve symptoms. Administration by inhaler delivers it directly to the brain from the lung. It was originally designed for use in chronic obstructive pulmonary disease and asthma and has shown efficacy for acute COVID-19, Dr. Selin said.
In a preliminary study, four patients with ME/CFS and five with long COVID have been treated with Inspiritol for 2-15 months, and all have self-reported improved symptoms. Cough has been the only reported side effect.
The company is pursuing an Investigational New Drug Application for the product with the Food and Drug Administration and has several patents pending. Dr. Lapp called Inspiritol “very interesting,” and said that reversal of CD8 “exhaustion” also would appear to be a promising approach. However, he noted, “the problem is that we don’t know what’s in it.”
Stellate ganglion block
Injection of local anesthetic near the stellate ganglion to block activity of the entire cervical sympathetic chain has been used for nearly a century to treat a variety of sympathetically mediated conditions, including complex regional pain syndrome (CRPS), shingles, and phantom-limb pain. More recently, it has been used in a variety of other conditions, including PTSD, Raynaud’s disease, menopausal hot flashes, and hyperhidrosis.
Insurance companies typically cover it for CRPS, neuropathic upper-extremity pain, hyperhidrosis, and Raynaud’s, said Luke Liu, MD, an anesthesiologist who is founder and chief executive officer of Alaska-based pain management company Neuroversion.
Deborah Duricka, PhD, also with Neuroversion, presented results from a now-published case series of 11 patients with long COVID who underwent stellate ganglion block by a board-certified anesthesiologist, first on one side at the level of C6, then on the contralateral side the following day.
Clinically meaningful benefits were seen in at least five of the patients in fatigue, memory problems, problems concentrating, rapid heartbeat, orthostatic intolerance, sleep problems, postexertional malaise, anxiety, and depression.
The hypothetical mechanism, she said, is that “sympathetic block prevents sympathetically driven vasoconstriction in carotid and vertebral arteries.”
Dr. Liu presented another case series of five patients with ME/CFS who underwent the procedure with ultrasound guidance, again on one side and the other side the next day. All had upper-limb autonomic issues such as Raynaud’s and/or neuropathic pain that had been refractory to more conventional treatments.
All five patients reported improvements in symptoms of ME/CFS, including energy level, cognition, pain, and postexertional malaise. One patient reported “feeling well for the first time in decades.” However, that patient relapsed after a mild viral illness 3.5 months after treatment. Some of the patients have required further treatments.
Dr. Lapp commented that, although the procedure is generally safe when performed by an experienced clinician, “Any time you do an injection like that, there’s a high risk that you could nick an artery or a vein or hit an essential nerve in the neck. That’s why it has to be done under fluoroscopy or ultrasound.”
He said he’s had a few patients undergo the procedure, mostly for CRPS, and they seem to have benefited from it. “It might increase cerebral blood flow and preload to the heart, so it might decrease ME/CFS symptoms and help with POTS as well.”
Nonetheless, Dr. Lapp said he wouldn’t consider stellate ganglion block as first-line treatment for ME/CFS or long COVID. “I think it would be for the treatment-resistant patient, when you’ve gone through all the treatments that we know and addressed all the comorbidities and they’re still not getting better.”
But, he added, it is a standard procedure. “Any pain clinic can do a stellate block.”
Transcutaneous auricular vagus nerve stimulation
Nicola Clague-Baker, PhD, a physiotherapist at the University of Liverpool (England), presented findings from an international survey of people with ME/CFS regarding their experience with transcutaneous auricular vagus nerve stimulation (taVNS) to manage their autonomic symptoms. The technique involves stimulation of the autonomic nervous system via the vagus nerve using electrodes applied to part of the ear. The theory is that the technique stimulates the parasympathetic nervous system and improves autonomic balance.
Two small previous trials showing benefit of vagus nerve stimulation for people with ME/CFS used more invasive and less comfortable methods of applying the stimulation rather than to the ear, Dr. Clague-Baker and colleagues noted in a poster. It has also been used successfully in treating POTS, another conference speaker noted.
A total of 131 people with ME/CFS (called simply “ME” in the United Kingdom) responded to a survey advertised on social media and websites. The majority (60%) were from the United Kingdom while the rest were from Europe, Australia, and North America. Most were female, and slightly more than half had lived with ME for 10 or more years.
The majority (72%) were still using taVNS, while 28% had stopped using it. Only 9% had used the modality for longer than a year. Respondents identified more than 30 benefits in symptoms and activities, with improvements in postexertional malaise (39%) and brain fog (37%) being the most common. One reported significant reduction in constipation.
However, respondents also mentioned more than 20 short- and long-term negatives, including headaches (15%) and long-term irritation at the site (9%). One participant reported a “big improvement in neuropathic pain, but not so much for muscles and joints.”
Overall, 80% reported that they would continue using taVNS and 67% said they would recommend it to others with ME, and 56% said that the system was mildly to very beneficial.
Dr. Lapp noted that several types of transcutaneous electrical nerve stimulation units with ear clips are sold online, and he’s seen them work well for migraine treatment. However, he cautioned that some patients have had side effects from the treatment, such as headaches and dizziness. “It’s putting an electrical current through your brain. In my mind, it’s another last-ditch measure.”
Dr. Lapp reported no financial disclosures.
A version of this article first appeared on Medscape.com.
FROM IACFSME 2022
One in eight COVID patients likely to develop long COVID: Large study
a large study published in The Lancet indicates.
The researchers determined that percentage by comparing long-term symptoms in people infected by SARS-CoV-2 with similar symptoms in uninfected people over the same time period.
Among the group of infected study participants in the Netherlands, 21.4% had at least one new or severely increased symptom 3-5 months after infection compared with before infection. When that group of 21.4% was compared with 8.7% of uninfected people in the same study, the researchers were able to calculate a prevalence 12.7% with long COVID.
“This finding shows that post–COVID-19 condition is an urgent problem with a mounting human toll,” the study authors wrote.
The research design was novel, two editorialists said in an accompanying commentary.
Christopher Brightling, PhD, and Rachael Evans, MBChB, PhD, of the Institute for Lung Health, University of Leicester (England), noted: “This is a major advance on prior long COVID prevalence estimates as it includes a matched uninfected group and accounts for symptoms before COVID-19 infection.”
Symptoms that persist
The Lancet study found that 3-5 months after COVID (compared with before COVID) and compared with the non-COVID comparison group, the symptoms that persist were chest pain, breathing difficulties, pain when breathing, muscle pain, loss of taste and/or smell, tingling extremities, lump in throat, feeling hot and cold alternately, heavy limbs, and tiredness.
The authors noted that symptoms such as brain fog were found to be relevant to long COVID after the data collection period for this paper and were not included in this research.
Researcher Aranka V. Ballering, MSc, PhD candidate, said in an interview that the researchers found fever is a symptom that is clearly present during the acute phase of the disease and it peaks the day of the COVID-19 diagnosis, but also wears off.
Loss of taste and smell, however, rapidly increases in severity when COVID-19 is diagnosed, but also persists and is still present 3-5 months after COVID.
Ms. Ballering, with the department of psychiatry at the University of Groningen (the Netherlands), said she was surprised by the sex difference made evident in their research: “Women showed more severe persistent symptoms than men.”
Closer to a clearer definition
The authors said their findings also pinpoint symptoms that bring us closer to a better definition of long COVID, which has many different definitions globally.
“These symptoms have the highest discriminative ability to distinguish between post–COVID-19 condition and non–COVID-19–related symptoms,” they wrote.
Researchers collected data by asking participants in the northern Netherlands, who were part of the population-based Lifelines COVID-19 study, to regularly complete digital questionnaires on 23 symptoms commonly associated with long COVID. The questionnaire was sent out 24 times to the same people between March 2020 and August 2021. At that time, people had the Alpha or earlier variants.
Participants were considered COVID-19 positive if they had either a positive test or a doctor’s diagnosis of COVID-19.
Of 76,422 study participants, the 5.5% (4,231) who had COVID were matched to 8,462 controls. Researchers accounted for sex, age, and time of completing questionnaires.
Effect of hospitalization, vaccination unclear
Ms. Ballering said it’s unclear from this data whether vaccination or whether a person was hospitalized would change the prevalence of persistent symptoms.
Because of the period when the data were collected, “the vast majority of our study population was not fully vaccinated,” she said.
However, she pointed to recent research that shows that immunization against COVID is only partially effective against persistent somatic symptoms after COVID.
Also, only 5% of men and 2.5% of women in the study were hospitalized as a result of COVID-19, so the findings can’t easily be generalized to hospitalized patients.
The Lifelines study was an add-on study to the multidisciplinary, prospective, population-based, observational Dutch Lifelines cohort study examining 167,729 people in the Netherlands. Almost all were White, a limitation of the study, and 58% were female. Average age was 54.
The editorialists also noted additional limitations of the study were that this research “did not fully consider the impact on mental health” and was conducted in one region in the Netherlands.
Janko Nikolich-Žugich, MD, PhD, director of the Aegis Consortium for Pandemic-Free Future and head of the immunobiology department at University of Arizona, Tucson, said in an interview that he agreed with the editorialists that a primary benefit of this study is that it corrected for symptoms people had before COVID, something other studies have not been able to do.
However, he cautioned about generalizing the results for the United States and other countries because of the lack of diversity in the study population with regard to education level, socioeconomic factors, and race. He pointed out that access issues are also different in the Netherlands, which has universal health care.
He said brain fog as a symptom of long COVID is of high interest and will be important to include in future studies that are able to extend the study period.
The work was funded by ZonMw; the Dutch Ministry of Health, Welfare, and Sport; Dutch Ministry of Economic Affairs; University Medical Center Groningen, University of Groningen; and the provinces of Drenthe, Friesland, and Groningen. The study authors and Dr. Nikolich-Žugich have reported no relevant financial relationships. Dr. Brightling has received consultancy and or grants paid to his institution from GlaxoSmithKline, AstraZeneca, Boehringer Ingelheim, Novartis, Chiesi, Genentech, Roche, Sanofi, Regeneron, Mologic, and 4DPharma for asthma and chronic obstructive pulmonary disease research. Dr. Evans has received consultancy fees from AstraZeneca on the topic of long COVID and from GlaxoSmithKline on digital health, and speaker’s fees from Boehringer Ingelheim on long COVID.
A version of this article first appeared on Medscape.com.
a large study published in The Lancet indicates.
The researchers determined that percentage by comparing long-term symptoms in people infected by SARS-CoV-2 with similar symptoms in uninfected people over the same time period.
Among the group of infected study participants in the Netherlands, 21.4% had at least one new or severely increased symptom 3-5 months after infection compared with before infection. When that group of 21.4% was compared with 8.7% of uninfected people in the same study, the researchers were able to calculate a prevalence 12.7% with long COVID.
“This finding shows that post–COVID-19 condition is an urgent problem with a mounting human toll,” the study authors wrote.
The research design was novel, two editorialists said in an accompanying commentary.
Christopher Brightling, PhD, and Rachael Evans, MBChB, PhD, of the Institute for Lung Health, University of Leicester (England), noted: “This is a major advance on prior long COVID prevalence estimates as it includes a matched uninfected group and accounts for symptoms before COVID-19 infection.”
Symptoms that persist
The Lancet study found that 3-5 months after COVID (compared with before COVID) and compared with the non-COVID comparison group, the symptoms that persist were chest pain, breathing difficulties, pain when breathing, muscle pain, loss of taste and/or smell, tingling extremities, lump in throat, feeling hot and cold alternately, heavy limbs, and tiredness.
The authors noted that symptoms such as brain fog were found to be relevant to long COVID after the data collection period for this paper and were not included in this research.
Researcher Aranka V. Ballering, MSc, PhD candidate, said in an interview that the researchers found fever is a symptom that is clearly present during the acute phase of the disease and it peaks the day of the COVID-19 diagnosis, but also wears off.
Loss of taste and smell, however, rapidly increases in severity when COVID-19 is diagnosed, but also persists and is still present 3-5 months after COVID.
Ms. Ballering, with the department of psychiatry at the University of Groningen (the Netherlands), said she was surprised by the sex difference made evident in their research: “Women showed more severe persistent symptoms than men.”
Closer to a clearer definition
The authors said their findings also pinpoint symptoms that bring us closer to a better definition of long COVID, which has many different definitions globally.
“These symptoms have the highest discriminative ability to distinguish between post–COVID-19 condition and non–COVID-19–related symptoms,” they wrote.
Researchers collected data by asking participants in the northern Netherlands, who were part of the population-based Lifelines COVID-19 study, to regularly complete digital questionnaires on 23 symptoms commonly associated with long COVID. The questionnaire was sent out 24 times to the same people between March 2020 and August 2021. At that time, people had the Alpha or earlier variants.
Participants were considered COVID-19 positive if they had either a positive test or a doctor’s diagnosis of COVID-19.
Of 76,422 study participants, the 5.5% (4,231) who had COVID were matched to 8,462 controls. Researchers accounted for sex, age, and time of completing questionnaires.
Effect of hospitalization, vaccination unclear
Ms. Ballering said it’s unclear from this data whether vaccination or whether a person was hospitalized would change the prevalence of persistent symptoms.
Because of the period when the data were collected, “the vast majority of our study population was not fully vaccinated,” she said.
However, she pointed to recent research that shows that immunization against COVID is only partially effective against persistent somatic symptoms after COVID.
Also, only 5% of men and 2.5% of women in the study were hospitalized as a result of COVID-19, so the findings can’t easily be generalized to hospitalized patients.
The Lifelines study was an add-on study to the multidisciplinary, prospective, population-based, observational Dutch Lifelines cohort study examining 167,729 people in the Netherlands. Almost all were White, a limitation of the study, and 58% were female. Average age was 54.
The editorialists also noted additional limitations of the study were that this research “did not fully consider the impact on mental health” and was conducted in one region in the Netherlands.
Janko Nikolich-Žugich, MD, PhD, director of the Aegis Consortium for Pandemic-Free Future and head of the immunobiology department at University of Arizona, Tucson, said in an interview that he agreed with the editorialists that a primary benefit of this study is that it corrected for symptoms people had before COVID, something other studies have not been able to do.
However, he cautioned about generalizing the results for the United States and other countries because of the lack of diversity in the study population with regard to education level, socioeconomic factors, and race. He pointed out that access issues are also different in the Netherlands, which has universal health care.
He said brain fog as a symptom of long COVID is of high interest and will be important to include in future studies that are able to extend the study period.
The work was funded by ZonMw; the Dutch Ministry of Health, Welfare, and Sport; Dutch Ministry of Economic Affairs; University Medical Center Groningen, University of Groningen; and the provinces of Drenthe, Friesland, and Groningen. The study authors and Dr. Nikolich-Žugich have reported no relevant financial relationships. Dr. Brightling has received consultancy and or grants paid to his institution from GlaxoSmithKline, AstraZeneca, Boehringer Ingelheim, Novartis, Chiesi, Genentech, Roche, Sanofi, Regeneron, Mologic, and 4DPharma for asthma and chronic obstructive pulmonary disease research. Dr. Evans has received consultancy fees from AstraZeneca on the topic of long COVID and from GlaxoSmithKline on digital health, and speaker’s fees from Boehringer Ingelheim on long COVID.
A version of this article first appeared on Medscape.com.
a large study published in The Lancet indicates.
The researchers determined that percentage by comparing long-term symptoms in people infected by SARS-CoV-2 with similar symptoms in uninfected people over the same time period.
Among the group of infected study participants in the Netherlands, 21.4% had at least one new or severely increased symptom 3-5 months after infection compared with before infection. When that group of 21.4% was compared with 8.7% of uninfected people in the same study, the researchers were able to calculate a prevalence 12.7% with long COVID.
“This finding shows that post–COVID-19 condition is an urgent problem with a mounting human toll,” the study authors wrote.
The research design was novel, two editorialists said in an accompanying commentary.
Christopher Brightling, PhD, and Rachael Evans, MBChB, PhD, of the Institute for Lung Health, University of Leicester (England), noted: “This is a major advance on prior long COVID prevalence estimates as it includes a matched uninfected group and accounts for symptoms before COVID-19 infection.”
Symptoms that persist
The Lancet study found that 3-5 months after COVID (compared with before COVID) and compared with the non-COVID comparison group, the symptoms that persist were chest pain, breathing difficulties, pain when breathing, muscle pain, loss of taste and/or smell, tingling extremities, lump in throat, feeling hot and cold alternately, heavy limbs, and tiredness.
The authors noted that symptoms such as brain fog were found to be relevant to long COVID after the data collection period for this paper and were not included in this research.
Researcher Aranka V. Ballering, MSc, PhD candidate, said in an interview that the researchers found fever is a symptom that is clearly present during the acute phase of the disease and it peaks the day of the COVID-19 diagnosis, but also wears off.
Loss of taste and smell, however, rapidly increases in severity when COVID-19 is diagnosed, but also persists and is still present 3-5 months after COVID.
Ms. Ballering, with the department of psychiatry at the University of Groningen (the Netherlands), said she was surprised by the sex difference made evident in their research: “Women showed more severe persistent symptoms than men.”
Closer to a clearer definition
The authors said their findings also pinpoint symptoms that bring us closer to a better definition of long COVID, which has many different definitions globally.
“These symptoms have the highest discriminative ability to distinguish between post–COVID-19 condition and non–COVID-19–related symptoms,” they wrote.
Researchers collected data by asking participants in the northern Netherlands, who were part of the population-based Lifelines COVID-19 study, to regularly complete digital questionnaires on 23 symptoms commonly associated with long COVID. The questionnaire was sent out 24 times to the same people between March 2020 and August 2021. At that time, people had the Alpha or earlier variants.
Participants were considered COVID-19 positive if they had either a positive test or a doctor’s diagnosis of COVID-19.
Of 76,422 study participants, the 5.5% (4,231) who had COVID were matched to 8,462 controls. Researchers accounted for sex, age, and time of completing questionnaires.
Effect of hospitalization, vaccination unclear
Ms. Ballering said it’s unclear from this data whether vaccination or whether a person was hospitalized would change the prevalence of persistent symptoms.
Because of the period when the data were collected, “the vast majority of our study population was not fully vaccinated,” she said.
However, she pointed to recent research that shows that immunization against COVID is only partially effective against persistent somatic symptoms after COVID.
Also, only 5% of men and 2.5% of women in the study were hospitalized as a result of COVID-19, so the findings can’t easily be generalized to hospitalized patients.
The Lifelines study was an add-on study to the multidisciplinary, prospective, population-based, observational Dutch Lifelines cohort study examining 167,729 people in the Netherlands. Almost all were White, a limitation of the study, and 58% were female. Average age was 54.
The editorialists also noted additional limitations of the study were that this research “did not fully consider the impact on mental health” and was conducted in one region in the Netherlands.
Janko Nikolich-Žugich, MD, PhD, director of the Aegis Consortium for Pandemic-Free Future and head of the immunobiology department at University of Arizona, Tucson, said in an interview that he agreed with the editorialists that a primary benefit of this study is that it corrected for symptoms people had before COVID, something other studies have not been able to do.
However, he cautioned about generalizing the results for the United States and other countries because of the lack of diversity in the study population with regard to education level, socioeconomic factors, and race. He pointed out that access issues are also different in the Netherlands, which has universal health care.
He said brain fog as a symptom of long COVID is of high interest and will be important to include in future studies that are able to extend the study period.
The work was funded by ZonMw; the Dutch Ministry of Health, Welfare, and Sport; Dutch Ministry of Economic Affairs; University Medical Center Groningen, University of Groningen; and the provinces of Drenthe, Friesland, and Groningen. The study authors and Dr. Nikolich-Žugich have reported no relevant financial relationships. Dr. Brightling has received consultancy and or grants paid to his institution from GlaxoSmithKline, AstraZeneca, Boehringer Ingelheim, Novartis, Chiesi, Genentech, Roche, Sanofi, Regeneron, Mologic, and 4DPharma for asthma and chronic obstructive pulmonary disease research. Dr. Evans has received consultancy fees from AstraZeneca on the topic of long COVID and from GlaxoSmithKline on digital health, and speaker’s fees from Boehringer Ingelheim on long COVID.
A version of this article first appeared on Medscape.com.
FROM THE LANCET
New Omicron COVID boosters coming soon: What to know now
– a month ahead of schedule, the Biden administration announced this week.
Moderna has signed a $1.74 billion federal contract to supply 66 million initial doses of the “bivalent” booster, which includes the original “ancestral” virus strain and elements of the Omicron BA.4 and BA.5 variants. Pfizer also announced a $3.2 billion U.S. agreement for another 105 million shots. Both vaccine suppliers have signed options to provide millions more boosters in the months ahead.
About 83.5% of Americans have received at least one COVID-19 shot, with 71.5% fully vaccinated with the initial series, 48% receiving one booster shot, and 31% two boosters, according to the CDC. With about 130,000 new COVID cases per day, and about 440 deaths, officials say the updated boosters may help rein in those figures by targeting the highly transmissible and widely circulating Omicron strains.
Federal health officials are still hammering out details of guidelines and recommendations of who should get the boosters, which are expected to come from the CDC and FDA. For now, authorities have decided not to expand eligibility for second boosters of the existing vaccines – now recommended only for adults over 50 and those 12 and older with immune deficiencies. Children 5 through 11 are advised to receive a single booster, 5 months after their initial vaccine series.
For a preview of what to expect from the CDC and FDA, this news organization spoke with Keri Althoff, PhD, an epidemiologist at Johns Hopkins University, Baltimore.
Q: Based on what we know now, who should be getting one of these new bivalent boosters?A: Of course, there is a process here regarding the specific recommendations, but it appears there will likely be a recommendation for all individuals to get this bivalent booster, similar to the first booster. And there will likely be a recommended time frame as to time since the last booster.
Right now, we have a recommendation for adults over the age of 50 or adults who are at higher risk for severe COVID-related illness [to get] a second booster. For them, there will probably be a timeline that says you should get the booster if you’re X amount of months or more from your second booster; or X amount of months or more from your first booster, if you’ve only had one.
Q: What about pregnant women or those being treated for chronic health conditions?A: I would imagine that once this bivalent booster becomes available, it will be recommended for all adults.
Q: And for children?A: That’s a good question. It’s something I have been digging into, [and] I think parents are really interested in this. Most kids, 5 and above, are supposed to be boosted with one shot right now, if they’re X amount of days from their primary vaccine series. Of course those 6 months to 4.99 years are not yet eligible [for boosters].
As a parent, I would love to see my children become eligible for the bivalent booster. It would be great if these boosters are conveying some additional protection that the kids could get access to before we send them off to school this fall. But there are questions as to whether or not that is going to happen.
Q: If you never received a booster, but only the preliminary vaccine series, do you need to get those earlier boosters before having the new bivalent booster shot?A: I don’t think they will likely make that a requirement – to restrict the bivalent booster only to those who are already boosted or up to date on their vaccines at the time the bivalent booster becomes available. But that will be up to the [CDC] vaccine recommendation committee to decide.
Q: Are there any new risks associated with these boosters, since they were developed so rapidly?A: No. We continue to monitor this technology, and with all the mRNA vaccines that have been delivered, you have seen all that monitoring play out with the detection, for example, of different forms of inflammation of the heart tissue and who that may impact. So, those monitoring systems work, and they work really, really well, so we can detect those things. And we know these vaccines are definitely safe.
Q: Some health experts are concerned “vaccine fatigue” will have an impact on the booster campaign. What’s your take?A: We have seen this fatigue in the proportion of individuals who are boosted with a first booster and even boosted with a second. But having those earlier boosters along with this new bivalent booster is important, because essentially, what we’re doing is really priming the immune system.
We’re trying to expedite the process of getting people’s immune system up to speed so that when the virus comes our way – as we know it will, because [of] these Omicron strains that are highly infectious and really whipping through our communities – we’re able to get the highest level of population immunity, you don’t end up in the hospital.
Q: What other challenges do you see in persuading Americans to get another round of boosters?A: One of the things that I’ve been hearing a lot, which I get very nervous about, is people saying: “Oh, I got fully vaccinated, I did or did not get the booster, and I had COVID anyway and it was really nothing, it didn’t feel like much to me, and so I’m not going to be boosted anymore.” We are not in a place quite yet where those guidelines are being rolled back in any way, shape, or form. We still have highly vulnerable people to severe disease and death in our communities, and we’re seeing hundreds of deaths every day.
There are consequences, even if it isn’t in severity of disease, meaning hospitalization and death. And let’s not let the actual quality of the vaccine being so successful that it can keep you out of the hospital. Don’t mistake that for “I don’t need another one.”
Q: Unlike the flu shot, which is reformulated each year to match circulating strains, the new COVID boosters offer protection against older strains as well as the newer ones. Why?A: It’s all about creating a broader immune response in individuals so that as more strains emerge, which they likely will, we can create a broader population immune response [to all strains]. Our individual bodies are seeing differences in these strains through vaccination that helps everyone stay healthy.
Q: There haven’t been clinical trials of these new mRNA boosters. How strong is the evidence that they will be effective against the emerging Omicron variants?A: There have been some studies – some great studies – looking at things like neutralizing antibodies, which we use as a surrogate for clinical trials. But that is not the same as studying the outcome of interest, which would be hospitalizations. So, part of the challenge is to be able to say: “Okay, this is what we know about the safety and effectiveness of the prior vaccines ... and how can we relate that to outcomes with these new boosters at an earlier stage [before] clinical data is available?”
Q: How long will the new boosters’ protections last – do we know yet?A: That timing is still a question, but of course what plays a big role in that is what COVID strains are circulating. If we prep these boosters that are Omicron specific, and then we have something totally new emerge ... we have to be more nimble because the variants are outpacing what we’re able to do.
This turns out to be a bit of a game of probability – the more infection we have, the more replication of the virus; the more replication, the more opportunity for mutations and subsequent variants.
Q: What about a combined flu-COVID vaccine; is that on the horizon?A: My children, who like most children do not like vaccines, always tell me: “Mom, why can’t they just put the influenza vaccine and the COVID vaccine into the same shot?” And I’m like: “Oh, from your lips to some scientist’s ears.”
At a time like this, where mRNA technology has totally disrupted what we can do with vaccines, in such a good way, I think we should push for the limits, because that would be incredible.
Q: If you’ve received a non-mRNA COVID vaccine, like those produced by Johnson & Johnson and Novavax, should you also get an mRNA booster?A: Right now, the CDC guidelines do state that if your primary vaccine series was not with an mRNA vaccine then being boosted with an mRNA is a fine thing to do, and it’s actually encouraged. So that’s not going to change with the bivalent booster.
Q: Is it okay to get a flu shot and a COVID booster at the same time, as the Centers for Disease Control and Prevention has recommended with past vaccines?A: I don’t anticipate there being recommendations against that. But I would also say watch for the recommendations that come out this fall on the bivalent boosters.
I do hope in the recommendations the CDC makes about the COVID boosters, they will say think about also getting your influenza vaccine, too. You could also get your COVID booster first, then by October get your influenza vaccine.
Q: Once you’re fully boosted, is it safe to stop wearing a mask, social distancing, avoiding crowded indoor spaces, and taking other precautions to avoid COVID-19?A: The virus is going to do what it does, which is infect whomever it can, and make them sick. So, if you see a lot of community transmission – you know who is ill with COVID in your kids’ schools, you know in your workplace and when people go out – that still signals there’s some increases in the circulation of virus. So, look at that to understand what your risk is.
If you know someone or have a colleague who is currently pregnant or immune suppressed, think about how you can protect them with mask-wearing, even if it’s just when you’re in one-on-one closed-door meetings with that individual.
So, your masking question is an important one, and it’s important for people to continue to hang onto those masks and wear them the week before you go see Grandma, for instance, to further reduce your risk so you don’t bring anything to here.
The high-level community risk nationwide is high right now. COVID is here.
A version of this article first appeared on WebMd.com.
– a month ahead of schedule, the Biden administration announced this week.
Moderna has signed a $1.74 billion federal contract to supply 66 million initial doses of the “bivalent” booster, which includes the original “ancestral” virus strain and elements of the Omicron BA.4 and BA.5 variants. Pfizer also announced a $3.2 billion U.S. agreement for another 105 million shots. Both vaccine suppliers have signed options to provide millions more boosters in the months ahead.
About 83.5% of Americans have received at least one COVID-19 shot, with 71.5% fully vaccinated with the initial series, 48% receiving one booster shot, and 31% two boosters, according to the CDC. With about 130,000 new COVID cases per day, and about 440 deaths, officials say the updated boosters may help rein in those figures by targeting the highly transmissible and widely circulating Omicron strains.
Federal health officials are still hammering out details of guidelines and recommendations of who should get the boosters, which are expected to come from the CDC and FDA. For now, authorities have decided not to expand eligibility for second boosters of the existing vaccines – now recommended only for adults over 50 and those 12 and older with immune deficiencies. Children 5 through 11 are advised to receive a single booster, 5 months after their initial vaccine series.
For a preview of what to expect from the CDC and FDA, this news organization spoke with Keri Althoff, PhD, an epidemiologist at Johns Hopkins University, Baltimore.
Q: Based on what we know now, who should be getting one of these new bivalent boosters?A: Of course, there is a process here regarding the specific recommendations, but it appears there will likely be a recommendation for all individuals to get this bivalent booster, similar to the first booster. And there will likely be a recommended time frame as to time since the last booster.
Right now, we have a recommendation for adults over the age of 50 or adults who are at higher risk for severe COVID-related illness [to get] a second booster. For them, there will probably be a timeline that says you should get the booster if you’re X amount of months or more from your second booster; or X amount of months or more from your first booster, if you’ve only had one.
Q: What about pregnant women or those being treated for chronic health conditions?A: I would imagine that once this bivalent booster becomes available, it will be recommended for all adults.
Q: And for children?A: That’s a good question. It’s something I have been digging into, [and] I think parents are really interested in this. Most kids, 5 and above, are supposed to be boosted with one shot right now, if they’re X amount of days from their primary vaccine series. Of course those 6 months to 4.99 years are not yet eligible [for boosters].
As a parent, I would love to see my children become eligible for the bivalent booster. It would be great if these boosters are conveying some additional protection that the kids could get access to before we send them off to school this fall. But there are questions as to whether or not that is going to happen.
Q: If you never received a booster, but only the preliminary vaccine series, do you need to get those earlier boosters before having the new bivalent booster shot?A: I don’t think they will likely make that a requirement – to restrict the bivalent booster only to those who are already boosted or up to date on their vaccines at the time the bivalent booster becomes available. But that will be up to the [CDC] vaccine recommendation committee to decide.
Q: Are there any new risks associated with these boosters, since they were developed so rapidly?A: No. We continue to monitor this technology, and with all the mRNA vaccines that have been delivered, you have seen all that monitoring play out with the detection, for example, of different forms of inflammation of the heart tissue and who that may impact. So, those monitoring systems work, and they work really, really well, so we can detect those things. And we know these vaccines are definitely safe.
Q: Some health experts are concerned “vaccine fatigue” will have an impact on the booster campaign. What’s your take?A: We have seen this fatigue in the proportion of individuals who are boosted with a first booster and even boosted with a second. But having those earlier boosters along with this new bivalent booster is important, because essentially, what we’re doing is really priming the immune system.
We’re trying to expedite the process of getting people’s immune system up to speed so that when the virus comes our way – as we know it will, because [of] these Omicron strains that are highly infectious and really whipping through our communities – we’re able to get the highest level of population immunity, you don’t end up in the hospital.
Q: What other challenges do you see in persuading Americans to get another round of boosters?A: One of the things that I’ve been hearing a lot, which I get very nervous about, is people saying: “Oh, I got fully vaccinated, I did or did not get the booster, and I had COVID anyway and it was really nothing, it didn’t feel like much to me, and so I’m not going to be boosted anymore.” We are not in a place quite yet where those guidelines are being rolled back in any way, shape, or form. We still have highly vulnerable people to severe disease and death in our communities, and we’re seeing hundreds of deaths every day.
There are consequences, even if it isn’t in severity of disease, meaning hospitalization and death. And let’s not let the actual quality of the vaccine being so successful that it can keep you out of the hospital. Don’t mistake that for “I don’t need another one.”
Q: Unlike the flu shot, which is reformulated each year to match circulating strains, the new COVID boosters offer protection against older strains as well as the newer ones. Why?A: It’s all about creating a broader immune response in individuals so that as more strains emerge, which they likely will, we can create a broader population immune response [to all strains]. Our individual bodies are seeing differences in these strains through vaccination that helps everyone stay healthy.
Q: There haven’t been clinical trials of these new mRNA boosters. How strong is the evidence that they will be effective against the emerging Omicron variants?A: There have been some studies – some great studies – looking at things like neutralizing antibodies, which we use as a surrogate for clinical trials. But that is not the same as studying the outcome of interest, which would be hospitalizations. So, part of the challenge is to be able to say: “Okay, this is what we know about the safety and effectiveness of the prior vaccines ... and how can we relate that to outcomes with these new boosters at an earlier stage [before] clinical data is available?”
Q: How long will the new boosters’ protections last – do we know yet?A: That timing is still a question, but of course what plays a big role in that is what COVID strains are circulating. If we prep these boosters that are Omicron specific, and then we have something totally new emerge ... we have to be more nimble because the variants are outpacing what we’re able to do.
This turns out to be a bit of a game of probability – the more infection we have, the more replication of the virus; the more replication, the more opportunity for mutations and subsequent variants.
Q: What about a combined flu-COVID vaccine; is that on the horizon?A: My children, who like most children do not like vaccines, always tell me: “Mom, why can’t they just put the influenza vaccine and the COVID vaccine into the same shot?” And I’m like: “Oh, from your lips to some scientist’s ears.”
At a time like this, where mRNA technology has totally disrupted what we can do with vaccines, in such a good way, I think we should push for the limits, because that would be incredible.
Q: If you’ve received a non-mRNA COVID vaccine, like those produced by Johnson & Johnson and Novavax, should you also get an mRNA booster?A: Right now, the CDC guidelines do state that if your primary vaccine series was not with an mRNA vaccine then being boosted with an mRNA is a fine thing to do, and it’s actually encouraged. So that’s not going to change with the bivalent booster.
Q: Is it okay to get a flu shot and a COVID booster at the same time, as the Centers for Disease Control and Prevention has recommended with past vaccines?A: I don’t anticipate there being recommendations against that. But I would also say watch for the recommendations that come out this fall on the bivalent boosters.
I do hope in the recommendations the CDC makes about the COVID boosters, they will say think about also getting your influenza vaccine, too. You could also get your COVID booster first, then by October get your influenza vaccine.
Q: Once you’re fully boosted, is it safe to stop wearing a mask, social distancing, avoiding crowded indoor spaces, and taking other precautions to avoid COVID-19?A: The virus is going to do what it does, which is infect whomever it can, and make them sick. So, if you see a lot of community transmission – you know who is ill with COVID in your kids’ schools, you know in your workplace and when people go out – that still signals there’s some increases in the circulation of virus. So, look at that to understand what your risk is.
If you know someone or have a colleague who is currently pregnant or immune suppressed, think about how you can protect them with mask-wearing, even if it’s just when you’re in one-on-one closed-door meetings with that individual.
So, your masking question is an important one, and it’s important for people to continue to hang onto those masks and wear them the week before you go see Grandma, for instance, to further reduce your risk so you don’t bring anything to here.
The high-level community risk nationwide is high right now. COVID is here.
A version of this article first appeared on WebMd.com.
– a month ahead of schedule, the Biden administration announced this week.
Moderna has signed a $1.74 billion federal contract to supply 66 million initial doses of the “bivalent” booster, which includes the original “ancestral” virus strain and elements of the Omicron BA.4 and BA.5 variants. Pfizer also announced a $3.2 billion U.S. agreement for another 105 million shots. Both vaccine suppliers have signed options to provide millions more boosters in the months ahead.
About 83.5% of Americans have received at least one COVID-19 shot, with 71.5% fully vaccinated with the initial series, 48% receiving one booster shot, and 31% two boosters, according to the CDC. With about 130,000 new COVID cases per day, and about 440 deaths, officials say the updated boosters may help rein in those figures by targeting the highly transmissible and widely circulating Omicron strains.
Federal health officials are still hammering out details of guidelines and recommendations of who should get the boosters, which are expected to come from the CDC and FDA. For now, authorities have decided not to expand eligibility for second boosters of the existing vaccines – now recommended only for adults over 50 and those 12 and older with immune deficiencies. Children 5 through 11 are advised to receive a single booster, 5 months after their initial vaccine series.
For a preview of what to expect from the CDC and FDA, this news organization spoke with Keri Althoff, PhD, an epidemiologist at Johns Hopkins University, Baltimore.
Q: Based on what we know now, who should be getting one of these new bivalent boosters?A: Of course, there is a process here regarding the specific recommendations, but it appears there will likely be a recommendation for all individuals to get this bivalent booster, similar to the first booster. And there will likely be a recommended time frame as to time since the last booster.
Right now, we have a recommendation for adults over the age of 50 or adults who are at higher risk for severe COVID-related illness [to get] a second booster. For them, there will probably be a timeline that says you should get the booster if you’re X amount of months or more from your second booster; or X amount of months or more from your first booster, if you’ve only had one.
Q: What about pregnant women or those being treated for chronic health conditions?A: I would imagine that once this bivalent booster becomes available, it will be recommended for all adults.
Q: And for children?A: That’s a good question. It’s something I have been digging into, [and] I think parents are really interested in this. Most kids, 5 and above, are supposed to be boosted with one shot right now, if they’re X amount of days from their primary vaccine series. Of course those 6 months to 4.99 years are not yet eligible [for boosters].
As a parent, I would love to see my children become eligible for the bivalent booster. It would be great if these boosters are conveying some additional protection that the kids could get access to before we send them off to school this fall. But there are questions as to whether or not that is going to happen.
Q: If you never received a booster, but only the preliminary vaccine series, do you need to get those earlier boosters before having the new bivalent booster shot?A: I don’t think they will likely make that a requirement – to restrict the bivalent booster only to those who are already boosted or up to date on their vaccines at the time the bivalent booster becomes available. But that will be up to the [CDC] vaccine recommendation committee to decide.
Q: Are there any new risks associated with these boosters, since they were developed so rapidly?A: No. We continue to monitor this technology, and with all the mRNA vaccines that have been delivered, you have seen all that monitoring play out with the detection, for example, of different forms of inflammation of the heart tissue and who that may impact. So, those monitoring systems work, and they work really, really well, so we can detect those things. And we know these vaccines are definitely safe.
Q: Some health experts are concerned “vaccine fatigue” will have an impact on the booster campaign. What’s your take?A: We have seen this fatigue in the proportion of individuals who are boosted with a first booster and even boosted with a second. But having those earlier boosters along with this new bivalent booster is important, because essentially, what we’re doing is really priming the immune system.
We’re trying to expedite the process of getting people’s immune system up to speed so that when the virus comes our way – as we know it will, because [of] these Omicron strains that are highly infectious and really whipping through our communities – we’re able to get the highest level of population immunity, you don’t end up in the hospital.
Q: What other challenges do you see in persuading Americans to get another round of boosters?A: One of the things that I’ve been hearing a lot, which I get very nervous about, is people saying: “Oh, I got fully vaccinated, I did or did not get the booster, and I had COVID anyway and it was really nothing, it didn’t feel like much to me, and so I’m not going to be boosted anymore.” We are not in a place quite yet where those guidelines are being rolled back in any way, shape, or form. We still have highly vulnerable people to severe disease and death in our communities, and we’re seeing hundreds of deaths every day.
There are consequences, even if it isn’t in severity of disease, meaning hospitalization and death. And let’s not let the actual quality of the vaccine being so successful that it can keep you out of the hospital. Don’t mistake that for “I don’t need another one.”
Q: Unlike the flu shot, which is reformulated each year to match circulating strains, the new COVID boosters offer protection against older strains as well as the newer ones. Why?A: It’s all about creating a broader immune response in individuals so that as more strains emerge, which they likely will, we can create a broader population immune response [to all strains]. Our individual bodies are seeing differences in these strains through vaccination that helps everyone stay healthy.
Q: There haven’t been clinical trials of these new mRNA boosters. How strong is the evidence that they will be effective against the emerging Omicron variants?A: There have been some studies – some great studies – looking at things like neutralizing antibodies, which we use as a surrogate for clinical trials. But that is not the same as studying the outcome of interest, which would be hospitalizations. So, part of the challenge is to be able to say: “Okay, this is what we know about the safety and effectiveness of the prior vaccines ... and how can we relate that to outcomes with these new boosters at an earlier stage [before] clinical data is available?”
Q: How long will the new boosters’ protections last – do we know yet?A: That timing is still a question, but of course what plays a big role in that is what COVID strains are circulating. If we prep these boosters that are Omicron specific, and then we have something totally new emerge ... we have to be more nimble because the variants are outpacing what we’re able to do.
This turns out to be a bit of a game of probability – the more infection we have, the more replication of the virus; the more replication, the more opportunity for mutations and subsequent variants.
Q: What about a combined flu-COVID vaccine; is that on the horizon?A: My children, who like most children do not like vaccines, always tell me: “Mom, why can’t they just put the influenza vaccine and the COVID vaccine into the same shot?” And I’m like: “Oh, from your lips to some scientist’s ears.”
At a time like this, where mRNA technology has totally disrupted what we can do with vaccines, in such a good way, I think we should push for the limits, because that would be incredible.
Q: If you’ve received a non-mRNA COVID vaccine, like those produced by Johnson & Johnson and Novavax, should you also get an mRNA booster?A: Right now, the CDC guidelines do state that if your primary vaccine series was not with an mRNA vaccine then being boosted with an mRNA is a fine thing to do, and it’s actually encouraged. So that’s not going to change with the bivalent booster.
Q: Is it okay to get a flu shot and a COVID booster at the same time, as the Centers for Disease Control and Prevention has recommended with past vaccines?A: I don’t anticipate there being recommendations against that. But I would also say watch for the recommendations that come out this fall on the bivalent boosters.
I do hope in the recommendations the CDC makes about the COVID boosters, they will say think about also getting your influenza vaccine, too. You could also get your COVID booster first, then by October get your influenza vaccine.
Q: Once you’re fully boosted, is it safe to stop wearing a mask, social distancing, avoiding crowded indoor spaces, and taking other precautions to avoid COVID-19?A: The virus is going to do what it does, which is infect whomever it can, and make them sick. So, if you see a lot of community transmission – you know who is ill with COVID in your kids’ schools, you know in your workplace and when people go out – that still signals there’s some increases in the circulation of virus. So, look at that to understand what your risk is.
If you know someone or have a colleague who is currently pregnant or immune suppressed, think about how you can protect them with mask-wearing, even if it’s just when you’re in one-on-one closed-door meetings with that individual.
So, your masking question is an important one, and it’s important for people to continue to hang onto those masks and wear them the week before you go see Grandma, for instance, to further reduce your risk so you don’t bring anything to here.
The high-level community risk nationwide is high right now. COVID is here.
A version of this article first appeared on WebMd.com.